Page 301
8
Interventions in the Workplace
This chapter examines the hypothesis that prevention strategies in the workplace can reduce the incidence and impact of musculoskeletal injuries, illnesses, and disorders. Primary prevention occurs when the intervention is undertaken before members of the population at risk have acquired a condition of concern, for example, educational programs to reduce the number of new cases (incidence) of low back pain. Secondary prevention occurs when the intervention is undertaken after individuals have experienced the condition of concern, for example, introduction of job redesign for workers with symptoms of carpal tunnel syndrome. Tertiary prevention strategies are designed for individuals with chronically disabling musculoskeletal disorders; the goal is to achieve maximal functional capacity within the limitations of the individual's impairments.
In this chapter we review the scientific data about interventions in the workplace particularly related to primary and secondary prevention. We have not addressed specific medical interventions, such as drugs, manipulative therapy, and surgery. The scientific bases for medical treatment of musculoskeletal conditions, particularly back pain, have been reviewed in detail by a number of panels of experts, such as the Quebec Task Force and the Agency for Health Care Policy and Research (AHCPR). Although there is significant overlap between secondary and tertiary prevention strategies, we have not addressed the extremely complex issues regarding the medical management of or workplace accommodations for those with chronic musculoskeletal disabilities.
In tertiary prevention the accommodations are usually made on a case by case basis. There often are complex psychosocial issues that may involve a wide array of treatment options, and the medical treatment
Page 302
often involves the management of failed surgical procedures, the utilization of pain clinics, functional restoration programs, and controversial drug regimens and surgical procedures. The panel examined the broader systems approach, dealing with primary and secondary prevention, and thought these more applicable to the interface between job demands and the population of workers.
This chapter is organized as follows: First, we revisit the conceptual model ( Figure 1.2) that forms the framework for workplace interventions and discuss the related principles of ergonomics. We then summarize the intervention literature specific to the back and upper extremities. Practical considerations, including assessment of cost-outcome effectiveness, are included, particularly as a framework for future research. Finally, we draw conclusions based on the weight of current evidence and suggest efforts to coordinate the gathering and sharing of further information to assess and prevent musculoskeletal disorders in the workplace.
CONTEXT
The conceptual model described in Figure 1.2 illustrates how the complex relationship among external loads, organizational factors, individual factors, and the social environment of work can lead to adverse outcomes that include pain, impairment, and disability. This conceptual model is also useful to understand how workplace interventions are used to control potentially adverse conditions.
Primary and secondary interventions may prevent adverse outcomes by reducing or eliminating external loads, changing organizational factors, altering the social environment, improving individual stress-coping skills, or matching the physical demands of the job with the employee's physical capacities. The literature suggests that some of these approaches are more successful than others. Some interventions have not yet been adequately assessed.
External loads in the work environment act on the body to create internal loads on tissues and other anatomical structures. Interventions that focus on the reduction or elimination of exposure to external loads must first identify and quantify the motions and forces acting on the individual, including vibration and thermal exposures. Often a systematic study of the work is required to evaluate these physical exposures and their characteristic properties. When specific physical stress factors are identified, the sources of these loads are ascertained. Workplace redesign may include alterations in tools, equipment, workstations, materials handled, tasks, work methods, work processes, and work environment, based on their contributions to the identified stresses. The majority of the intervention literature is based on this approach to injury reduction.
Page 303
Work organizational factors broadly consist of job content and organization characteristics, as well as temporal and economic aspects of the work and task. Job content is the array of tasks and procedures that make up an employee's workload. These requirements have a direct effect on the exposure to external loads associated with the use of equipment and tools. Other aspects of job content may include specifications to handle certain objects, operate machinery, or work under potentially adverse environmental conditions. Interventions in job content may reduce or eliminate exposure to physical stresses by directly altering the job requirements. Examples include assigning a worker to different tasks or eliminating a specific operation through automation.
Organizational characteristics describe the management structure of the organization and the level of autonomy an employee has when performing a job. These factors may affect employees' attitudes about their work or influence physical stress exposure. Interpersonal relationships among employees and supervisors may also influence physical stress exposure. For example, physical stresses in a cooperative work environment often are reduced when employees informally assist one other. Temporal aspects include job scheduling such as shift work, number of hours on deadline, job rotation, or the frequency and duration of specific tasks. For example, the continuous performance of a monotonous, repetitive task has been associated with physical and psychological stress.
Finally, the economic and compensation policies of a company can affect physical exposures. For example, overtime and extended work can increase the daily duration of exposure to musculoskeletal stressors. Compensation incentives also may affect intensity, frequency, and duration of work and may discourage rest breaks.
PRINCIPLES OF ERGONOMICS
The application of ergonomic principles forms the basis for much of the intervention literature. Ergonomics is the study of work, including workplace interventions to establish compatibility among the worker, the job, and the work environment. Ergonomics professionals, both researchers and practitioners, reflect the variety of factors that affect safety and productivity in the workplace; the disciplines involved include researchers and practitioners in, for example, medicine, epidemiology, psychology, and industrial engineering and other health-related, technical/ engineering, and behavioral disciplines. The process whereby ergonomics is applied to intervention adheres to the scientific method: available data are gathered and analyzed (e.g., through broad or local surveillance and through analysis of jobs); hypotheses are developed (e.g., specific engineering controls are proposed to address specific factors or condi-
Page 304
tions of the physical workplace and job characteristics; administrative controls are proposed to address characteristics of the organization and management thought to be relevant; and such individual modifiers as age, gender, body mass index, smoking habits, comorbidity, and reaction to the psychosocial environment at home and at work are addressed); the hypotheses are tested (i.e., the effectiveness of the intervention is assessed); and the hypotheses are maintained (for effective interventions) or refined (an intervention is improved or replaced) in response to the outcomes.
Emerging evidence indicates that work-related musculoskeletal disorders and associated disability are the consequence of a complex interplay among medical, social, work organizational, biomechanical, and workplace and individual psychosocial factors. As with most areas of scientific endeavor, the ergonomics of intervention in the workplace is providing an expanding knowledge base and an evolving set of interventions, and continued development of innovative models is needed to allow for the effective management and prevention of these complex disorders. The practice of ergonomics relies on a process that tailors interventions to specific circumstances currently found effective, continues to assess the effectiveness of these interventions in the face of changing workplace and worker factors, and evaluates new interventions. It is therefore neither feasible nor desirable to propose generic interventions expected to apply to every industry, job, and worker, nor “once for all” interventions whose effectiveness need not be regularly assessed. It is, rather, both feasible and desirable to encourage application—with continued assessment—of interventions found useful and promising to date, and to encourage cooperative endeavor and information exchange among researchers, practitioners, and workers/managers in industry/labor, government, and academia. Surveillance and job analysis are critical components of intervention research and practice.
Surveillance
Surveillance is the ongoing, systematic collection, analysis, and interpretation of health and exposure information in the process of describing and monitoring work-related musculoskeletal disorders and evaluating the effectiveness of the program. Surveillance may include the analysis of existing medical records, worker compensation records (passive surveillance), or the surveying of workers with questionnaire and physical examination (active surveillance).
The analysis of existing records is generally less costly, but the reliability of such data is difficult to assess. Standardized questionnaires and physical examinations can be as sensitive as the use of unusually thor-
Page 305
ough existing occupational medical records; however, it is unclear whether the additional cost of an active surveillance system will deter the routine use of such systems (Fine et al., 1986). Symptoms questionnaires and checklist-based hazard surveillance are feasible within the context of joint labor-management ergonomics programs and are more sensitive indicators of ergonomic problems than preexisting data sources (Silverstein et al., 1997).
Surveillance systems are key methods of collecting information that describes the characteristics of workers (individual factors) that may interact with workplace factors to cause or mitigate musculoskeletal disorders or to affect the success of interventions. Surveillance systems may also be used to evaluate the effectiveness of interventions. In addition, surveillance systems (e.g., employee surveys, absentee and turnover analysis) can be used to gather information that complements that of other analytical procedures (e.g., job analysis, work flow analysis, productivity study) in defining relevant features of tasks, jobs, worker satisfaction, and organizational culture. Surveillance is most important in times of rapid change in the economy and when resources for prevention may be limited (Fine, 1999).
Surveillance data may be collected and analyzed at different levels of task, job, occupation, and industry (see Chapter 2), and they may elucidate features of the physical work environment, work tasks, work organization, psychosocial environment, and worker characteristics relevant to intervention (see Figure 1.2). Intervention can be indicated by case, data, and risk factors identified through surveillance. Case-initiated interventions are triggered by employee reports of symptoms, concerns, or recommendations. An intervention is data-initiated when it is the outcome of an analysis of medical records and injury reports. An intervention is risk-factor initiated when factors known to be significantly related to musculoskeletal disorders are shown to be present.
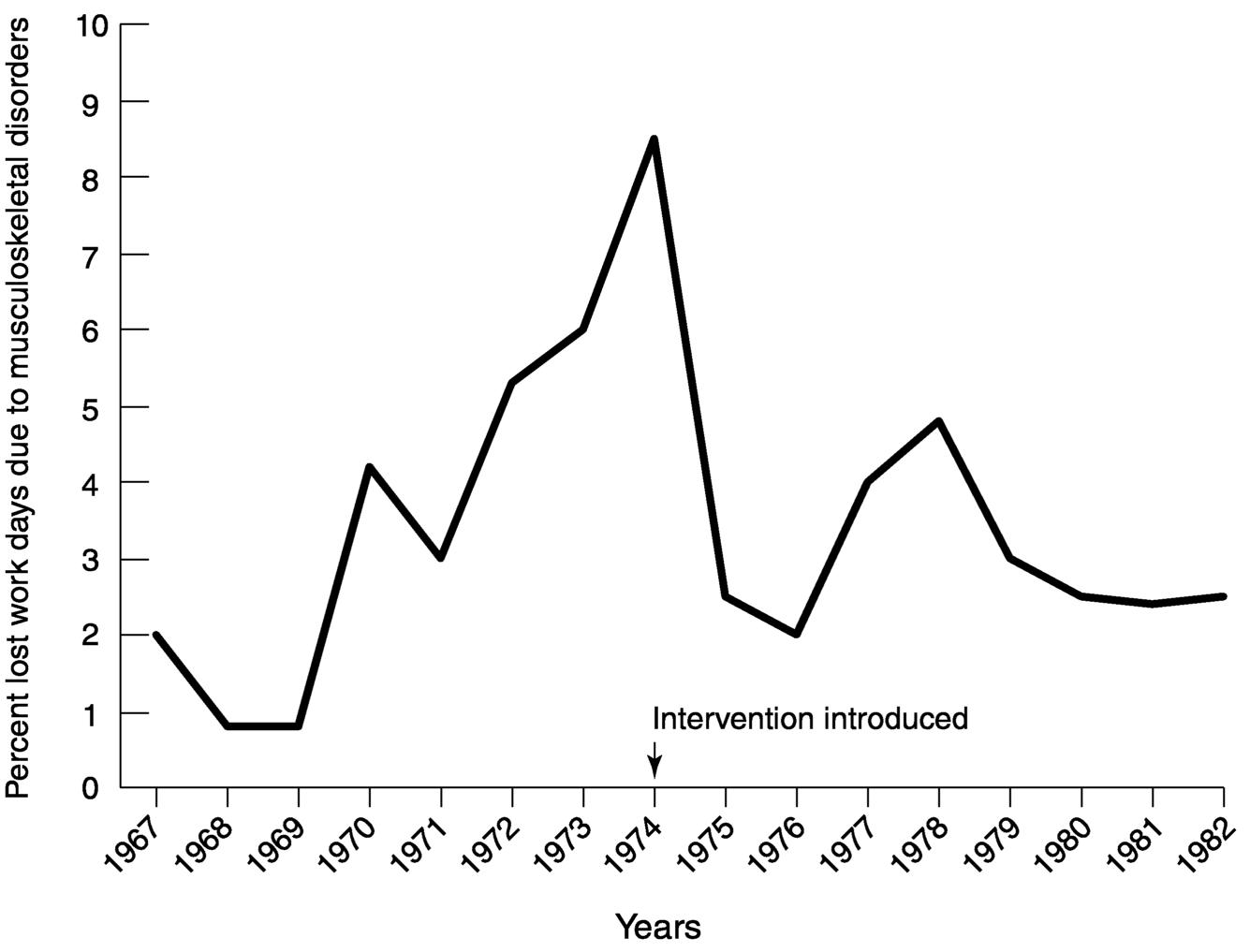
Surveillance systems at the company level serve as an invaluable resource for evaluating the impact of efforts to reduce risk and to find new risks early, before they cause irreparable harm. For example, in an electronics company in Norway, new cases of sick leave attributed to musculoskeletal disorders were tracked over a number of years. Regular examination of the trends led the company to recognize an increase in the sick leave rates and prompted it to introduce a number of improvements in the work setting. The surveillance of sick leave also served to document the impact of the interventions, showing reductions in the sick leave following the changes. Figure 8.1 (from Westgaard and Aaräs, 1985) shows the percentage of lost work days, due to musculoskeletal disorders, of total work force in the electronics company. Record analyses may also reveal trends across jobs, operations, or other common conditions. Inter-
Page 306
~ enlarge ~
FIGURE 8.1 Percentage lost work days due to musculoskeletal disorders of total work force in an electronics company (based on data from Westgaard and Aaräs, 1985).
ventions may be initiated when risk factors are identified from proactive job surveys or other risk factor reviews.
Job Analysis
When it is determined, based on the clinical evaluation and exposure information, that an employee has a work-related disorder, the employer performs an analysis of the employee's job or of a sample of representative jobs. Job analysis is a procedure used to identify potential exposure to risk factors and to evaluate their characteristic properties. When risk factors are identified, job design or redesign, including engineering or administrative controls, is used for eliminating or reducing work-related risk factors or exposure to those factors.
Job analysis consists of a work methods analysis, based on traditional techniques of time-and-motion study to determine the work content of the job, and a systematic analysis of risk factors (Armstrong et al., 1986).
Page 307
Work methods analysis involves describing the work content of each task as a series of steps or elements and identifying risk factors for each work element. After the major physical stresses have been identified, ergonomic interventions may be applied to minimize exposure to risk factors. Such interventions are often categorized as engineering controls, administrative or production controls, or personal modifiers. Although risk factors are frequently cited in the literature, acceptable exposure levels have not yet been determined for all individual and combined factors. The presence of a risk factor does not necessarily mean that the person doing the job is at excessive risk of an injury or that ergonomic changes are worth their cost. When the presence of risk factors is combined with a history of musculoskeletal disorders among persons doing that job, the risk may be considered excessively high and ergonomic interventions may be worth their cost. In many cases, it is desirable to make changes regardless of the history, because job changes are often inexpensive, and injuries are often very expensive. This is particularly the case when jobs are being initially designed and set up.
Examples of Process-Based Ergonomics Intervention Programs
The Occupational Safety and Health Administration has issued a standard of practice for assessing and addressing musculoskeletal disorders in the workplace. The American National Standards Institute has accredited a national committee (Accredited Standards Committee, 2000) charged with developing a standard process or program for reducing musculoskeletal disorders associated with work. Within industry, Ford Motor Company, for example, uses a team-based approach at each facility, establishing ergonomic committees consisting of labor and management representatives who collect and analyze local data (reviewing surveillance records and medical cases), propose interventions, and assess their effectiveness (Joseph, 2000). Though not targeting specifically the issue of musculoskeletal disorders in the workplace, the Department of Defense has demonstrated for decades that the elements of an effective ergonomics program can be formally defined in broad scope, and that these elements can be successfully tailored to the needs and features of specific workplaces and workers (see U.S. Army Missile Command, no date). We note here that each of these approaches to ergonomics interventions is process-based (i.e., applies a process of analysis, implementation, and assessment of effectiveness), and that any ergonomics program benefits when the scientific method is applied by researchers and practitioners in those programs who collect and analyze data, propose and implement interventions, and assess their effectiveness.
Page 308
SPECIFIC INTERVENTIONS: BACK
Few high-quality scientific intervention studies related to the primary and secondary prevention of low back pain are available in the literature. The vast majority of the literature consists of retrospective analyses and case reports of intervention effectiveness, better assessed through prospective studies and, if possible, randomized controlled trials.
In order to provide insight as to the effectiveness of interventions in controlling the risk of back pain, the reviewed literature was categorized in three ways. First, high-quality reviews of the literature were evaluated for common indications and trends. Second, since most of these efforts consisted of reviews dating back to the mid-1990s, a review of the literature since that time was performed using similar quality criteria. Finally, a review of reported “best practices” was performed to assess how reported experiences in industry relate to the more rigorous controlled studies of interventions. Collectively, this approach has provided insight into the effectiveness of low back interventions.
Results of High-Quality Reviews Through the Mid-1990s
Six high-quality reviews of the literature were identified that assess the state of knowledge associated with the ability of ergonomic interventions to influence low back disorders. Based on its criteria for quality, this assessment selected reviews that accepted only studies that met rigorous methodological constraints and reviews that comprehensively examined the basic science behind intervention logic. Six reports met these criteria.
The first review, performed by Westgaard and Winkel (1997), assessed 91 studies that met seven inclusion criteria. By these criteria each reviewed study included: (1) field intervention; (2) involvement of a primary or secondary intervention; (3) an exposure-effect analysis; (4) sufficient documentation for repeatability; (5) a unit of analysis that was the entire job (not a task); (6) outcome analyses that included internal exposure, acute responses, and/or health effects; and (7) documentation in English. In addition to these inclusion criteria, this review selected interventions based on seven quality criteria. These quality criteria included: (1) proper statistical analyses, (2) reasonable study group size, (3) variables that were generalizable to other settings, (4) consideration of reliability and sensitivity of variables, (5) inclusion of a control group, (6) an adequate observation period with follow-up measurements, and (7) proper documentation of the intervention process.
The inclusion criteria of the second review (van Poppel et al., 1997) accepted studies that included: (1) a controlled clinical trial that is prospective in nature in which the intervention group is randomly assigned
Page 309
and compared with a randomly assigned control group derived from the same setting as the intervention group; (2) intervention intended to prevent back pain and consisting of education, exercise, or lumbar support; (3) no restrictions on subjects at the start of the study, and (4) intervention occurring in an industrial setting. A total of 14 studies met these inclusion criteria.
The third review (Volinn, 1999) closely examined six studies that based their interventions on various principles. These principles included promotion of back safety, back belt use, introduction of ergonomic devices, and back strengthening exercises. By Volinn's inclusion criteria, these studies contained: (1) use of a primary prevention, (2) a dependent measure consisting of a recordable back injury, (3) only workplace-related injuries, and (4) successful outcomes.
In the fourth review, Kaplansky and colleagues (Kaplansky, Wei, and Reecer, 1998) evaluated 133 studies of occupational low back pain prevention. Their review categorized the interventions by type and collectively assessed the literature within each intervention type. The inclusion criteria considered the state of the body of knowledge associated with each intervention type, focused on the intervention logic, and used selection criteria that varied across the intervention types. The literature reviewed did not consist only of field studies. The assessment was generally of a critical nature.
A fifth review (Scheer, Watanabe, and Radack, 1997) searched 4,000 articles but accepted for review only randomized, controlled trials of interventions: 12 studies met this criterion. The sixth review (Hsiang, Brogmus, and Courtney, 1997) summarized the results of 70 biomechanical and physiological publications. Although the review did not focus on field interventions, it examined the logic behind the advantages and disadvantages of lifting techniques. This represents an alternative assessment of a low back pain intervention approach.
Collectively, the data in these six reviews indicate that certain engineering controls (e.g., ergonomic workplace redesign), administrative controls (specifically, adjusting organizational culture), addressing modifying individual factors (specifically, employee exercise), and the inclusion of a combination of interventions are the only strategies that have been shown to be positively associated with the reduction of work-related low back pain. An important finding in these studies is the observation that multiple interventions that actively involve workers in medical management of workers at risk, physical training, and technique education, in combination, can also be effective in controlling risk. Isolated approaches such as control of the production process, use of back belts, training, relaxation, physiotherapy, health education, and worker selection either have not been proven effective or have proven ineffective.
Page 310
Results of Recent High-Quality Studies
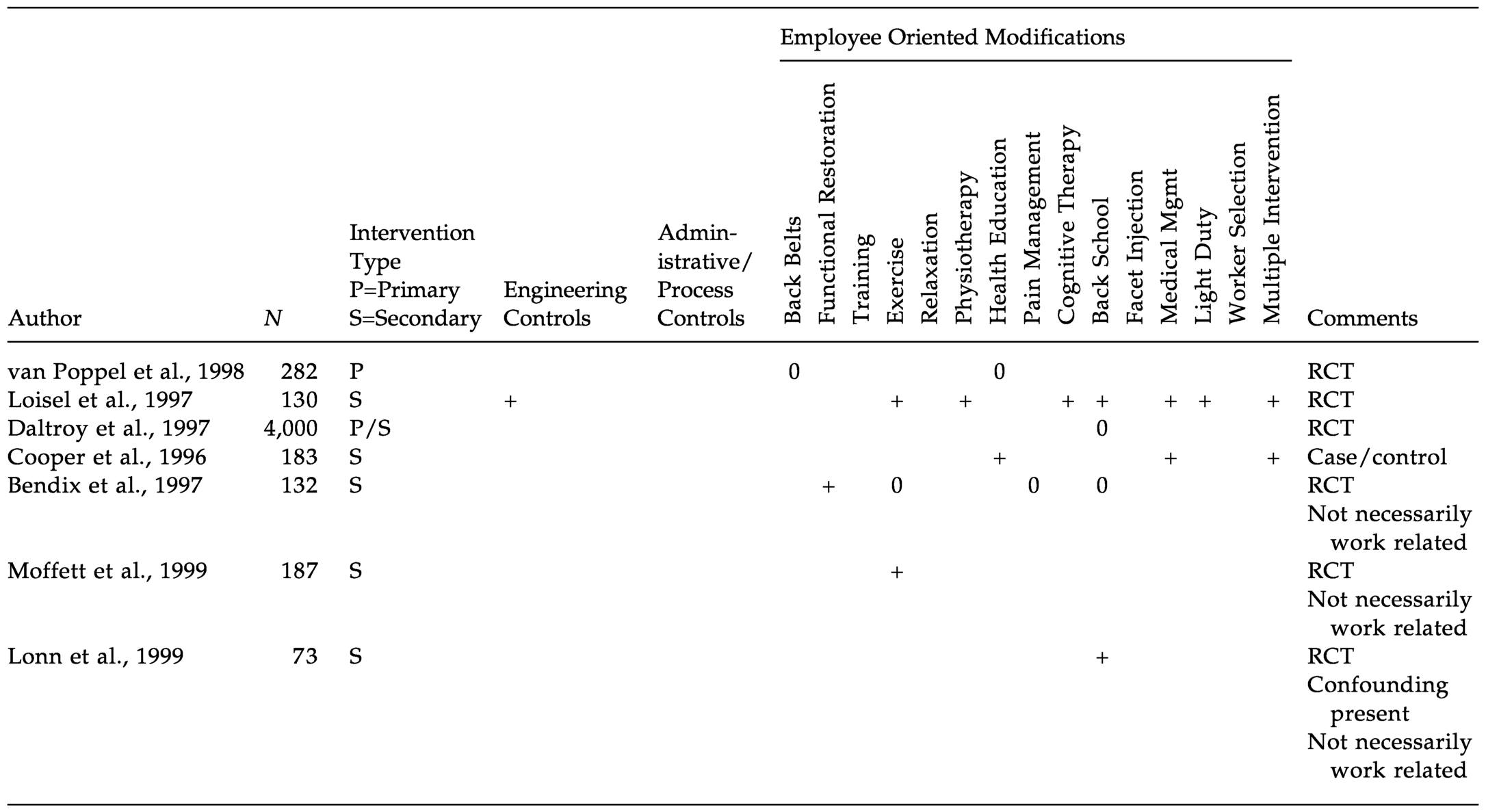
The high-quality reviews discussed above evaluated the back intervention literature up until the mid-1990s. A search of the back intervention literature published since that time identified seven additional high-quality studies. All but one of these studies involved randomized controlled designs; the remaining study was of a case-control design. These studies are summarized in Table 8.1. Three of the studies were not necessarily related to work. Only two of the studies addressed primary interventions, evaluating the effectiveness of back belts, health education, and back schools: none of these interventions was found to be effective. These findings are consistent with the literature reviews discussed in the previous section.
The findings of the six secondary intervention studies were also in agreement with the literature reviews described above in reporting that engineering controls, exercise (two of three studies), and multiple interventions are effective. The other positive findings for secondary interventions consisted of functional restoration (one study), physiotherapy (one study), cognitive therapy (one study), medical management (two studies), and light duty (one study). Conflicting results were found for back schools (positive findings in two of four studies) and health education (positive results in one of two studies). Back belts and pain management approaches to interventions were found to be ineffective.
Best Practices
Since practical experience with interventions can also be of use in interpreting the effectiveness of ergonomic interventions, we reviewed the literature of best practices interventions to see how it compared with the more rigorous scientific studies. To this end, we reviewed the transcripts from the Effective Workplace Practices and Programs Conference held in Chicago in 1997. A total of 13 interventions relating to the control of low back pain were found; these are reported in Table 8.2. These best practices illustrate the type of intervention approaches that are often applied by industry. As the table shows, many of these approaches are the same as those identified in the high-quality reviews and high-quality studies previously discussed.
Table 8.2 shows that engineering controls are one of the most commonly used interventions in industry. Many of the industries that employ engineering controls as an intervention also report a positive effect on low back pain control. The second most common control is training, which is typically applied along with engineering controls. Many of the industries reported positive control of low back pain through training. These data
Page 311
~ enlarge ~ |
Page 312
|
Environment/Industry |
Engineering Controls |
Administration/Production |
Personal Modifiers |
|
Large Manufacturing |
|||
|
PPG |
• |
||
|
Hay & Forge |
• |
||
|
Ford |
• |
||
|
Small Manufacturing |
|||
|
Charleston Ford |
• |
• |
|
|
Cross Association |
• |
||
|
Perdue, Inc. |
• rotate/ramp in |
||
|
Apparel |
|||
|
UNITE |
• |
||
|
Sequins |
• |
||
|
Crest-Caravan |
• |
• |
|
|
Healthcare |
|||
|
Mayo Clinic |
• patient transfer team |
||
|
University of Washington |
• |
||
|
University of California, Los Angeles |
• lift assist |
||
|
Warehousing |
|||
|
Murphy Warehousing Co. |
• |
• light duty |
|
are consistent with the high-quality reviews, which found no effect of training, in that there was no instance of a positive effect of the program reported when training was the only intervention applied. In many of the cases, engineering controls were also applied; such interventions were often reported as effective in the high-quality analyses.
Review of this table further indicates that administrative controls were also used, often in conjunction with engineering controls, and these cases quite often reported a positive impact on low back pain. The administrative controls reported consisted of worker rotation and ramping in of work, lifting teams for patient transfer in health care, and process control. One industry reported a benefit of light duty or transitional work assignments. Two industries reported the importance of employee involvement, and two reported the importance of employee support, although the associations with impacts are not clearly reported. Medical management and process control were frequently reported interventions. Multiple interventions are often reported as means used to control the risk of low back
Page 313
|
Multiple Interventions |
Employee Involvement |
Management Support |
Training |
Medical Management |
Process Conrol |
Positive Impact Reported |
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
||||
|
• |
• |
|||||
|
• |
||||||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
||||
|
• |
• |
|||||
|
• |
||||||
|
• |
||||||
|
• |
||||||
|
• |
• |
pain in industry. These reports do not clearly stipulate which interventions are considered primary versus secondary.
Consistency of Findings
Overall, the pattern of effectiveness described in the high-quality reviews and studies is consistent with the observations described from the best practices reported by industry.
The classes of interventions described in this review are plausible. Considering the mechanisms by which various interventions influence the sequence of events described in the model illustrated in Figure 1.2, one can identify the consistent logical pathways that correspond to the interventions judged effective by both the high-quality and best practices assessments. For example, on one hand, engineering and administrative controls would be expected to affect the physical exposure to structure loading, thereby reducing risk. Exercise, on the other hand, can have an
Page 314
effect on the individual's tolerance to load. Multiple interventions may affect the system not only by influencing internal mechanical loading, but also through reducing psychological stressors. Collectively, then, the results reported in the high-quality reviews and high-quality studies are consistent with many of the observations noted in the reports of best practices ( Table 8.2) as well as with the overall logic influencing musculoskeletal risk described in Figure 1.2.
SPECIFIC INTERVENTIONS: UPPER EXTREMITIES
Evidence from the epidemiologic literature suggests that a number of important risk factors, both physical and psychosocial, are associated with the development of musculoskeletal disorders of the upper extremities. The importance of these risk factors is documented through the study-based estimates of attributable risk already cited (see Chapter 4). The prominent physical risk factors reported include excessive force, repetitive movements, vibration, and cold temperatures, separately and together. The prominent psychosocial factors reported are not so easily characterized, but standardized measures that have been associated with upper extremity musculoskeletal disorders include high job stress; high job demands; nonwork-related worry, tension, and psychological distress; perceptions of the degree of support from supervisors and coworkers; and perceived lack of control over high work demands.
A wide variety of workplace interventions have been implemented in many different industrial settings in order to reduce upper extremity musculoskeletal disorders. Focused interventions can be grouped into two general categories: worker-focused (such as exercises) and workplace-focused (such as redesigning workstations). Broader programs are designed to affect the production system (addressing improved productivity and musculoskeletal health) or the organizational culture (addressing behaviors and attitudes of management, health personnel, and workers, sometimes in participatory group structures organized to address musculoskeletal problems). While there have been formal efforts to study these process or system interventions, reports of these interventions and their effectiveness are provided, for the most part, in the form of case studies. Though not rigorous studies, these case reports provide useful evidence for the potential effectiveness of a number of different approaches (General Accounting Office, 1997; Gjessing et al., 1994).
A recent comprehensive review of studies of intervention to prevent musculoskeletal conditions provided a foundation for considering the value of interventions (Westgaard and Winkel, 1997). The authors acknowledged, however, that their review was narrowly focused and excluded a number of useful studies that were laboratory-based, focused on
Page 315
tool design, limited to task (not job) redesign, aimed at vibration, or focused on the worker rather than the workplace. That review grouped primary and secondary interventions to reduce the incidence of upper extremity musculoskeletal disorders into three general categories: engineering controls, administrative controls, and modifier interventions.
Engineering Controls
There have been several studies of interventions in circumstances in which the initial physical exposures to the upper extremities are high (e.g., repetition rate, grip force, and posture extremes) that demonstrate the positive impact of reduction in the exposures (Aaräs, 1994; Parenmark, Malmkvist, and Örtengren, 1993). At the time of the Westgaard and Winkel (1997) review, there were few studies evaluating interventions in settings that involved low grip force. A number of recent studies of workers, primarily in settings involving work with computers, now provide supporting evidence that prevalence of upper extremity pain is reduced when sustained awkward postures are mitigated (Nelson and Silverstein, 1998; Aaräs, Ro, and Thoresen, 1999; Tittiranonda, Burastero, and Rempel, 1999; Brisson, Montreuil, and Punnett, 1999). In these studies furniture or hand tools were modified to alter postures while working. For example, in the study by Aaräs et al., use of a different computer mouse that reduced forearm rotation from full pronation to a neutral posture led to a significant reduction in upper extremity pain after six months.
In addition, studies of engineering interventions for computer-related work that reduce static postural loads, sustained posture extremes, and rapid motions have demonstrated decreases in upper extremity pain reports. Further study of these interventions is needed to determine the amount of pain reduction possible, the duration of the salutary effect, and which upper extremity clinical conditions could benefit from these interventions. Some of these studies involved single interventions (e.g., alternative keyboard); however, interventions to control physical exposures must more commonly be studied in the context of multiple interventions.
Administrative Controls
Multidimensional interventions can be classified into two categories. The first, rationalization strategies, includes efforts to improve productivity and musculoskeletal health. Although some studies have successfully demonstrated the accomplishment of these two desirable outcomes, the studies are limited by a lack of specificity. Studies have also demonstrated success in reducing overall absenteeism, turnover, and relevant exposures, but either these studies have included too many variables or the
Page 316
follow-up period has been too short to permit documentation of the simultaneous improvement in productivity and reduction in musculoskeletal disorders (Johansson et al., 1993; Kadefors et al., 1996; Bao, Mathiassen, and Winkel, 1996). The second strategy, modifying organizational culture, places emphasis on participatory team involvement. Several of these studies report success, but they do not clearly distinguish which elements of a complex program are essential, except that the commitment of management, together with the involvement of employees, has been demonstrated to play a major role in successful production system interventions (Geras, Pepper, and Rodgers, 1989; Lockhart, 1986; Narayan and Rudolph, 1993).
Modifier Interventions
These studies are worker-focused and are more often designed like clinical trials. One limitation is that these studies do not isolate the effects of the intervention from those of parallel changes, including psychosocial improvements, such as improved employee/supervisor relationships. Therefore, posited successes may be as much due to a change in the work process as to a change in worker capacity, for example through exercise, education, or training in work technique (Kukkonen, Lammi, and Anttï-Poika, 1991; Silverstein et al., 1988; Wigaeus et al., 1992).
Recent Intervention Studies
Several pre-/postintervention studies have been conducted since the review by Westgaard and Winkle. These studies have evaluated various primary and secondary interventions that could affect upper extremity musculoskeletal disorders. The interventions range from the redesign of work to training, across many industries, including, for example, meatpacking (Jones, 1997; Moore and Garg, 1998), health care (Evanoff et al., 1999; Bernacki et al., 1999), computer work (Brisson, Montreuil, and Punnett, 1999; Fernström and Åborg, 1999; Lie and Watten, 1994; Galinsky et al., 2000), and manufacturing (Bonsall et al., 1991; Melhorn et al., 1999; Halpern and Dawson, 1997). In general, these studies report reductions in lost time, rate of musculoskeletal disorders, or turnover and changes in other health endpoints.
A few additional well-controlled intervention studies have also been recently published. Generally, these studies, summarized in Table 8.3, compare one group of workers who receive an intervention to another group who do not, while controlling for covariates. Symptom ratings, such as pain scores, are the primary outcome measure, but a few of the studies also incorporate parallel measures, such as physical examination,
Page 317
sick leave, or turnover rates. All of the studies are of adequate duration (6 to 18 months) to avoid missing an effect. One study (Tittiranonda, Burastero, and Rempel, 1999) found that the benefit of an alternate keyboard intervention was not evident until four months into the study.
Six of the studies in Table 8.3 involve computer users and evaluate interventions aimed at decreasing static muscle loading by providing body support or by reducing sustained posture extremes. For example, in the study by Aaräs and colleagues (1999), half of the employees were assigned a new computer mouse that required less pinch force and forearm pronation to use. After six months, this group reported significant reduction in shoulder, forearm, and hand/wrist pain compared with the control group. The authors concluded that the effects of this single intervention may be due to reduced shoulder abduction and an elimination of full forearm pronation.
A similar logic was invoked by Tittranonda and colleagues (1999), who found that an alternative geometry keyboard significantly reduced hand and arm pain after six months when compared with a conventional keyboard. In the study by Brisson and colleagues (1999), subjects receiving six hours of ergonomics training, which focused on decreasing neck twisting and flexion and wrist deviation through use of accessories and adjustment of the workstation, were compared with a reference group. After six months the prevalence of all musculoskeletal disorders was significantly reduced in comparison to the reference group in subjects less than 40 years old. An examination of the body postures while working on the computer revealed that subjects under 40 years of age were more likely to have reduced neck twisting and bending than subjects over 40.
Taken together, these studies provide some limited evidence that reducing sustained awkward postures, a risk factor among computer users identified in the epidemiology chapter (Appendix Table 4.6), can lead to a reduction in pain in the associated region of the upper extremity and neck. The effects of a comprehensive ergonomics program, which included training to reduce shoulder muscle loads, employee participation in the redesign of work methods, changes in production incentives, among other factors, was evaluated by Parenmark and colleagues (1993) in a chain saw assembly plant in comparison to another plant. The ergonomic program led to a 20 percent reduction in sick leave and a 70 percent reduction in turnover rate. The authors attributed these positive outcomes to a number of factors, including an awareness among employees of how to avoid high muscle loads.
There is a paucity of studies on the use of conditioning exercise to prevent injury. Most available studies are of limited scientific rigor or generalizability to the workplace. Seradge, Bear, and Bithell (1993) report the case study of a meatpacking company that achieved a 45 percent
Page 318
|
Reference |
Total Initial Participants |
Completion Rate |
Work |
Intervention |
|
Nelson and Silverstein, 1998 |
632 |
47% |
Office work |
New chairs, workstations |
|
Aaräs, Ro, and Thoresen, 1999 |
181 |
91% |
Computer |
Worksurface with forearm support |
|
Rempel et al., 1999 |
20 |
100% |
Computer |
Keyboards |
|
Tittiranonda et al., 1999 |
80 |
86% |
Computer |
Alternative keyboards |
|
Aaräs, Ro, and Thorsen, 1999 |
67 |
100% |
Computer |
Alternative mouse |
|
Parenmark, Malmkvist, and Örtengren., 1993 |
534 |
— |
Chain saw assembly |
Work technique, pace, layout, staffing, wages |
|
Brisson, Montreuil, and Punnett, 1999 |
627 |
96% |
Computer |
Ergonomics training |
|
Kamwendo and Linton, 1991 |
79 |
96% |
Secretarial |
Neck school, exercises |
|
Gerdle et al., 1995 |
97 |
81% |
Home care |
Exercise |
|
Silverstein et al., 1988 |
178 |
80% |
Assembly |
Exercise |
aOnly for participants under 40 years of age.
NOTE: The table includes only studies that were published in a peer-reviewed scientific journal, included a control group, were of longer duration than one month, and measured a health endpoint.
reduction in the incidence of reported carpal tunnel syndrome after 1 year of a program of exercises designed to prevent carpal tunnel syndrome. Silverstein et al. (1988), in a more controlled study of the effects of in-plant exercise on musculoskeletal symptoms, found no statistically significant difference in localized posture discomfort scores between employees who did and did not participate in an on-the-job exercise program aimed at controlling musculoskeletal symptoms of the neck and upper limb.
Page 319
|
Duration |
Control co-variates |
Outcome measures |
Positive Effect? |
|
1 year |
Yes |
Hand/arm symptom |
Yes |
|
Neck/shoulder/back symptoms |
Yes |
||
|
2 year |
No |
Neck/shoulder pain |
Yes |
|
Forearm/hand pain |
No |
||
|
3 months |
Yes |
Hand pain |
Yes |
|
Physical examination |
Yes |
||
|
Nerve conduction |
No |
||
|
6 months |
Yes |
Hand/arm pain |
Yes |
|
Physical examination |
No |
||
|
6 months |
Yes |
Shoulder/forearm/wrist pain |
Yes |
|
Sick leave |
Yes |
||
|
18 months |
No |
Sick leave |
Yes |
|
Turnover |
Yes |
||
|
Production costs |
Yes |
||
|
6 months |
Yes |
Neck/upper extremity pain |
Yesa |
|
Physical examination |
Yesa |
||
|
6 months |
Yes |
Neck pain |
No |
|
Neck range of motion |
No |
||
|
Sick leave |
No |
||
|
1 year |
Yes |
Musculoskeletal complaints |
Yes |
|
Physical examination |
Yes |
||
|
Lost time |
No |
||
|
1 year |
Yes |
Neck shoulder discomfort |
No |
Studies of the effects of stretching exercises provide only suggestive results. Moore and Garg (1998) found, in a pre-/post-test study of 60 workers, that participants in a stretching exercise program achieved, after 36 sessions over 2 months, greater physical flexibility. Conditioning exercise programs may make participants feel better about themselves (Silverstein, 1988; Moore and Garg, 1998) and may encourage workers to attend to physical activity.
Page 320
Taken together, these studies generally demonstrate a benefit of changes in workstation design, tool design, or training on upper extremity symptoms. The effect on related physical examination findings is less consistent. The value of exercise in reducing musculoskeletal symptoms has found mixed support.
Best Practices
Table 8.4 summarizes the best practices reported by industry representatives at the 1997 conference on effective workplace practices and programs relating to the management and control of upper extremity work-related musculoskeletal disorders. The table reveals a trend similar to that found for the interventions previously described for low back pain. Interventions for upper extremity and neck work-related musculoskeletal disorders involving engineering controls, administrative processes and personal modifiers resulted in positive outcomes for 27 companies. In particular, engineering controls and administrative controls, such as periodic rest breaks and job rotation, were most frequently accompanied by employee involvement, management support, and training. All programs included either engineering or administrative controls in addition to personal modifiers (such as exercise, training, light duty, or medical management). None of the reports demonstrated that personal modifiers were successful by themselves. Companies that instituted exercise or stretching programs also employed engineering or administrative controls. These findings are consistent with the approaches discussed in the high-quality reviews of back interventions in Table 8.1.
CHALLENGES DURING THE PROCESS OF ERGONOMIC INTERVENTION
Those who develop and implement interventions that address the complexity of factors potentially affecting musculoskeletal disorders in the workplace face challenges during the phases of gathering information, applying it to implement interventions and assess their effectiveness, and disseminating both research and practical knowledge. Given the magnitude and the complexity of the problem of musculoskeletal disorders in the workplace, in response to these challenges it would be beneficial to coordinate the efforts of researchers and practitioners in industry, labor, government, and academia.
Collection of Information: Surveillance
Challenges to the collection of information exist in the areas of methods and measures for surveillance. Surveillance of information pertinent
Page 321
to interventions for musculoskeletal disorders in the workplace can be improved by the development of more reliable, valid, sensitive, and specific medical diagnostic tests for relevant musculoskeletal disorders, as well as development of specific criteria that can be used for surveillance for determining cases of musculoskeletal disorders. Criteria should include, separately or in combination as appropriate, systematic methods for the collection of symptom information, minimum physical examination test findings, or physiological measurements. Criteria should also be relevant to specific purposes (for example, surveillance for early identification versus diagnosis for treatment). In addition, effective surveillance would be facilitated by further development of self-report instruments (e.g., by the application of computer technologies).
Collection of Information: Research Pertaining to Developing Interventions
Challenges to the collection of information also exist in the areas of methods and measures for research on ways to improve interventions and more effectively tailor them to the needs of specific workers, jobs, and industries. The development of interventions would benefit from more research to better quantify exposure limits, including cumulative risk for exposure, to apply them to job design to prevent injury, and to use such data as part of the effort to improve biomechanical models for predicting risk of musculoskeletal disorders in designing jobs. Furthermore, useful research would also define the most effective methods for applying multifactorial interventions (e.g., engineering controls, administrative controls, individual modifiers) and for reducing exposure for targeted industries (e.g., better ways of turning and lifting patients, better hand tools that reduce vibration). A continuing program of cooperative research would provide further understanding of the features of specific interventions that best account for their effectiveness (e.g., elucidating the characteristics of relevant work organizational factors, assessing the effect of job rotation as an intervention, and clarifying the mechanisms whereby psychosocial factors, individual worker characteristics, and organizational culture interact with interventions.
Assessing Interventions
The development of the repertoire of effective interventions would be facilitated by an infrastructure that supports standardization of test instruments, standardized reporting, and agreed-on outcome measures that would assist researchers and practitioners to assess the effectiveness of interventions and to define the contexts within which specific inter-
Page 322
|
Personal Modifiers |
|||
|
Environment/Industry |
Engineering Controls |
Administrative/ Production |
Exercise/ Stretching |
|
Large Manufacturing |
|||
|
3M |
• |
• Process |
|
|
PPG |
• |
• Process |
|
|
Hay & Forge |
• |
• Process |
|
|
Ford |
• |
• Process |
|
|
Samsonite |
• |
• Process |
|
|
Frito-Lay |
• |
• Process/Rotation |
|
|
Construction |
|||
|
Bechtel |
• Periodic breaks |
• |
|
|
TDC |
• |
• |
|
|
Apparel |
|||
|
Red Wing Shoe |
• |
• Rotation |
• |
|
Sequins International |
• |
||
|
Fieldcrest-Cannon |
• |
• Process |
|
|
Sara Lee Knit Products |
• |
• Process |
|
|
Small Manufacturing |
|||
|
Rocco Enterprises |
• |
• Process/Rotation |
• |
|
Charleston Forge |
• |
• Process/Rotation |
|
|
Lunt Silversmiths |
• |
||
|
Perdue, Inc. |
• |
• Process/Rotation |
|
|
Woodpro Cabinetry |
• Rotation |
||
|
Farmland Foods |
|||
|
Maritime |
|||
|
Bath Iron Works |
• |
• Process/Rotation |
• |
|
Newport News Shipbuilding |
• |
• Process |
|
|
Utilities |
|||
|
PG&E |
• |
• |
|
|
Montana Power |
• |
• Rest breaks |
• |
|
Warehousing |
|||
|
Murphy Warehousing Co. |
• |
• Process |
|
|
Office |
|||
|
3M |
• Process |
||
|
American Express Financial Advisors |
• |
• Process |
|
|
L.L. Bean |
• |
• Process |
|
|
US West |
• |
• Process |
Page 323
|
Light Duty |
Multiple Interventions |
Employee Involvement |
Management Support |
Training |
Medical Management |
Positive Impact Reported |
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
||||
|
• |
• |
• |
• |
• |
• |
• |
|
• |
• |
|||||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
• |
||
|
• |
• |
|||||
|
• |
• |
• |
||||
|
• |
• |
• |
• |
|||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
|||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
||||
|
• |
• |
• |
||||
|
• |
• |
• |
• |
• |
||
|
• |
• |
• |
• |
• |
• |
|
|
• |
• |
• |
• |
|||
|
• |
• |
• |
• |
|||
|
• |
• |
• |
• |
• |
Page 324
ventions are found to be effective. These methods and measures would also be beneficially applied to assessment of the adjuncts to interventions, including training programs and aids (for workers, managers, researchers, and practitioners), work standards on musculoskeletal disorders and prevention, and manuals for interventions and for ergonomics programs. There is a need, addressed below, for the development of standardized methods for cost-effectiveness analysis of interventions.
Cost-Outcome Effectiveness Analysis
Public and private policy makers, managers, and other leaders and decision makers are faced with the practical challenges of allocating limited resources. They must therefore be informed of the ratio between a program's marginal monetary costs and the marginal effectiveness, expressed both in terms of monetary savings and marginal improvements in health outcomes. Under such rubrics as prevention effectiveness (Haddix et al., 1996) and economic evaluation (Goossens et al., 1999), a set of analytical techniques is available to address questions of cost outcome. These techniques include: cost-benefit analysis, which expresses both costs and benefits in monetary terms; cost-effectiveness analysis, which expresses outcomes in terms that may not be monetary (e.g., lost work days, reported pain); and cost-utility analysis, which expresses outcome in the common form “quality adjusted life years.”
Despite their availability, these techniques have not been widely applied to the study of interventions to relieve or prevent musculoskeletal disorders. Therefore, it is not possible, given existing studies, to provide a systematic summary, or comparison across programs, of the cost-outcome effectiveness of such interventions. Few studies of the effects of interventions for musculoskeletal disorders describe the costs associated with the intervention. Studies of interventions for musculoskeletal disorders employ a wide variety of outcome measures, and methods for determining cost also vary across studies that consider costs. Cost and outcome factors can differ widely, depending on the level of intervention (primary, secondary). In fact, most reports of cost-outcome effectiveness for such interventions provide only anecdotal or case data. Goossens et al. (1999) noted that three recently performed reviews of the economic evaluation of interventions for musculoskeletal pain pointed to the impossibility of reaching confident conclusions, because of the lack of clarity and low quality of the costing methodologies employed.
There are several key methodological issues associated with cost/outcome analysis in this area:
Page 325
1. Different interventions and the circumstances to which they are applied may result in different time profiles. Some costs may be spread over a long period of time, while others are incurred at the beginning of the intervention; similarly, some outcomes appear quickly, while others require long periods of time.
2. Reduction in cost related to a disorder can be deemed a benefit of the intervention (e.g., when an intervention results in a decrease in the prevalence of a disorder at a workplace). This is sometimes clearly demonstrable with a methodology that controls for the effects of competing—or no—interventions. Moreover, predicted reduction in cost is sometimes taken as a benefit (e.g., when an intervention is predicted to prevent cases of a disorder that will not be observed, because they have, by prediction, been prevented). Similarly, assumptions are sometimes made about the interrelationships of benefits to one another (e.g., the assumption that an outcome of improved job satisfaction will imply also an outcome of improved productivity). In all cases, care must be exercised to validate the relationships and predictions.
3. Costs reported under the same label can be determined by different accounting methods (e.g., overhead costs); similarly, outcomes described in similar terms can mask operationally different variables (e.g., job satisfaction, reported pain). The methodology whereby cost and outcome are determined should be precisely explained in any study that assesses cost-outcome effectiveness—a principle violated often in case reports and best practice description.
4. The results of cost-outcome effectiveness studies must be considered only one part of policy and decision analysis, which must also consider such factors as who pays what costs, who reaps what benefits, and what cost/outcome ratio is acceptable. One method of quantifying values is to measure the evaluator's willingness to pay for units of risk reduction.
Despite the current dearth of rigorous, comprehensive cost-outcome effectiveness studies of interventions for musculoskeletal disorders, direction can be found in, for example, Haddix et al. (1996), who provide a general framework applicable to public health prevention initiatives, and Goossens et al. (1999), who propose a framework specific to musculoskeletal disorders. The combined framework (see Box 8.1) is augmented by factors described in existing cost-outcome studies for musculoskeletal disorders; this framework identifies types of costs and benefits that can be considered as part of future efforts toward the development of an accepted methodology that will permit comparison across alternative interventions.
Page 326
BOX 8.1 Framework for Cost-Outcome Effectiveness ResearchExamples of Cost Factors for Intervention/Prevention Programs Direct Health Care Costs Institutional inpatient care Institutional outpatient services Home health care Physician services Ancillary services (other professionals and volunteers) Overhead (facility, equipment, etc.) Medications Devices and appliances Diagnostic tests Rehabilitation Direct Nonhealth Care Costs Program development (analysis, program design) Training and education (personnel, materials, facilities) Program management Transportation Modification to workplace (time and cost to design, fabricate/purchase, implement) Indirect Costs: Wages/Time Lost productivity during implementation Psychosocial costs (adjustment, stress due to change) Examples of Beneficial Outcomes of Intervention/Prevention Programs Number of reported injuries Number of Workers' Compensation claims Amount of Workers' Compensation indemnity paid Reduction in lost days Reduction in absenteeism Reduction in recurrences Reduced number of worker replacements and reduced training of new workers Improved physical functioning Motivation Morale Job satisfaction Productivity Improved perceived quality of life Reduction in risky behaviors Reduced fatigue Improved knowledge of workers about safety |
Page 327
Return to Work
Return to work is one desirable outcome of interventions. Research that elucidates the factors that operate on behalf of return to work would further the understanding of the systematic description of factors presented in Figure 1.2. Such research would usefully address development of prognostic indicators of clinical outcomes; determination of how return to work is affected by functional capacities of the worker and by workplace accommodations; identification of barriers to timely access to health care and to filing workers' compensation claims; and identification of disincentives to compliance with suggested programs.
Dissemination of Information
There is also a challenge of disseminating—to workers, managers, and researchers and practitioners in government, industry, and academia— the surveillance, research, assessment, and effectiveness information discussed above. Features of an improved infrastructure to foster this dissemination would include regular meetings that bring together scientific and best practices experience; an intervention trials network; development and sharing of common tools, training programs, and standards—tailored to users—for implementing ergonomic programs; and mechanisms for disseminating validated best practices.
Particularly helpful would be the expansion of education and training programs to assist workers and employers (especially small employers) in understanding and utilizing the range of possible workplace interventions designed to reduce musculoskeletal disorders. Expanding continuing education for a broad range of professionals concerning risk factors for musculoskeletal disorders—in and out of the workplace—and concerning interventions would also be useful.
SUMMARY
Musculoskeletal injuries in the workplace result from a complex interaction of mechanical stresses, individual host factors, and organizational policy and structure. Furthermore, due to the rapidly changing nature of work and the intense focus on production goals, it is extremely difficult to design and carry out intervention studies in the workplace, particularly those that are prospective, randomized, and controlled. When interpreting the results of existing intervention studies, there are important methodological considerations that must be taken into account to determine the validity of each study.
Page 328
There is a very large body of published literature about workplace interventions for the primary and secondary prevention of back and upper extremity work-related disorders. Despite the large number of studies published, few meet the strictest criteria for scientific validity. At the same time, there is a another body of information derived from quality improvement studies and best practices that reflect the practical experience within industry. To the degree that there is agreement between the more scientific literature and best practices, this congruence is important in establishing a weight or pattern of evidence. In applying this information, there are several ethical and cost-benefit considerations, as well as practical barriers particularly in optimizing secondary prevention strategies.
The complexity of musculoskeletal disorders in the workplace requires a variety of strategies that may involve the worker, the workforce, and management. The literature shows that no single strategy is or will be effective for all types of industry; interventions are best tailored to the individual situation. Although we have no measure of their relative contributions, there are, however, some program elements that consistently recur within successful programs: management commitment, employee involvement, and directly addressing workplace physical and work organizational factors.
The weight and pattern of the evidence supports the conclusion that primary and secondary prevention interventions to reduce the incidence, severity, and consequences of musculoskeletal injuries in the workplace are effective when properly implemented. The evidence suggests that the most effective strategies involve a combined approach that takes into account the complex interplay between physical stressors and the policies and procedures of industries. When the scientific information is combined with the very practical quality improvement data, the panel is persuaded that continued focus on primary and secondary prevention can reduce the incidence and severity of these widespread musculoskeletal conditions affecting the worker in the workplace. Specifically, the panel concludes that:
1. Interventions must mediate physical stressors, largely through the application of principles of ergonomics.
2. Employee involvement is essential to successful implementation.
3. Employer commitment, demonstrated by an integrated program and supported by best practices review, is important for success.
4. Because of limitations in the scientific literature, a comprehensive and systematic research program, supported by an infrastructure linking industry, labor, government, and academic efforts, is needed to further
Page 329
clarify and distinguish the features that make interventions effective for specific musculoskeletal disorders.
5. Although generic guidelines have been developed and successfully applied in intervention programs, no single specific design, restriction, or practice for universal application is supported by the existing scientific literature.
6. Study of the relationship between exposure to physical and psychosocial risk factors and musculoskeletal disorders has been constrained by inadequate techniques for quantitative measurement of “dose,” analogous to available measures for noise or chemicals. Existing measures are often based on self-report or qualitative metrics. New tools and research instruments are necessary to provide more reliable and valid exposure estimates; these are most important for the study of the effects, if any, at lower-level exposures and for evaluation of the possibility of interaction among different factors when more than one is present. Better measures of exposures and outcomes would permit more effective evaluation of interventions.





























