Part II
INTRODUCTION
In addition to reviewing the overall burden of disease attributable to brain disorders and formulating a strategic framework to reduce that burden in developing countries, presented in Part I of this report, the committee was also charged to address specifically the following group of representative disorders: developmental disabilities, epilepsy, bipolar disorder, schizophrenia, unipolar depression, and stroke. The committee reviewed evidence of the impact of each of these disorders in developing countries and identified strategies to reduce that impact through prevention and low-cost treatment, research and development, and capacity building. The results of this process are presented in the next six chapters, which comprise Part II of this report.
Several factors were considered in selecting these particular disorders for study. First, each ranks among the most prevalent of neurological, psychiatric, or developmental disorders worldwide and is known to cause significant disability. Second, these disorders represent a spectrum of disease affecting people at every stage of life, from fetal development through old age; their order of presentation in the following chapters, which begins with developmental disabilities and concludes with stroke, reflects this chronological progression. Finally, these particular classes of disorder appeared to be strong candidates for cost-effective interventions, and therefore critical targets for reducing the overall burden of disease associated with brain disorders. It is hoped that future studies on other brain disorders of public health significance, such as Alzheimer's disease, injuries to the central nervous system, substance abuse, and posttraumatic stress disorder, will build on this initial effort.
The framework for studying each of the selected disorders or groups of disorders included an overview of the available epidemiological parameters, a review of the existing knowledge base to support intervention, and projections of the feasibility, cost, and expected impact of proposed interventions. Wherever possible, the committee based its review and recommendations on evidence from a broad range of settings in the developing world; unfortunately, due to the limited available research on most brain disorders in developing countries, they were frequently forced to make qualified extrapolations based on data from the developed world. In most cases, direct correlations appear to exist between developed and developing countries. For example, many proven risk factors for stroke have been established in developed countries (such as hypertension, high-fat and sodium diets, and diabetes), and these risk factors are of growing concern in developing countries. Though extensive data do not exist on prevention methods for controlling or eliminating these risk factors in developing countries, it can be said that such efforts would bear similar reduction in stroke mortality as has been observed in developed countries. In the few instances where correlations might be skewed by differences between developed and developing countries, these limitations are clearly noted.
As one might expect, several observations regarding the impact and outlook for reducing the burden of specific disorders presented in the chapters of Part II mirror comments in Part I that pertain to many or all brain disorders. These points are reiterated in order to build the most complete picture possible of each individual disorder. However, since the discussions of specific brain disorders presented in Part II are ultimately intended to be viewed in the context of the general discussion and strategies that appear in Part I, readers are advised to familiarize themselves with the introductory chapters of this report before proceeding to the chapters in Part II.
|
Summary of Findings: Developmental Disabilities in Developing Countries
|
5
Developmental Disabilities
DEFINITION
Developmental disabilities include limitations in function resulting from disorders of the developing nervous system. These limitations manifest during infancy or childhood as delays in reaching developmental milestones or as lack of function in one or multiple domains, including cognition, motor performance, vision, hearing and speech, and behavior. Table 5-1 provides a listing of the major categories of developmental disability with corresponding International Classification of Diseases (ICD)-10 codes.[1]
To varying degrees, the causes of many other neurological and psychiatric disorders not typically designated as developmental disabilities may also be traced to early neurodevelopment. For several of the disorders discussed in subsequent chapters—specifically epilepsy, depression, and schizophrenia—evidence indicates such a causal relationship.[ 2,3,4,5,6,7,8,9,10 and 11]
The clinical features of developmental disabilities are variable in severity as well as in the specific areas of function that are limited. Brief descriptions of the clinical features of each of the broad categories of developmental disability are provided below. It may be noted that children with developmental disabilities are often affected in multiple domains of function because of the nature and extent of brain impairment or increased susceptibility to other causes of disability (e.g., malnutrition, trauma, infection) among children with a single disability.
TABLE 5-1 Major Categories of Developmental Disability with Corresponding ICD-10 Diagnostic Codes (when available)
|
ICD-10 Code |
|
|
Cognitive |
|
|
Mental Retardation |
|
|
Mild (IQ approximately 50–69) |
F70 |
|
Moderate (IQ approximately 35–49) |
F71 |
|
Severe (IQ approximately 20–34) |
F72 |
|
Profound (IQ below 20) |
F73 |
|
Specific Learning Disabilities |
F81 |
|
Reading (Dyslexia) |
F81.0 |
|
Mathematics (Dyscalculia) |
F81.2 |
|
Other |
|
|
Motor |
|
|
Cerebral Palsy |
G80 |
|
Post-Polio Paralysis |
B91 |
|
Muscular Dystrophies |
G71.0 |
|
Spina Bifida |
Q05 |
|
Spinal Muscular Atrophies |
G12 |
|
Other |
M01–M03. |
|
Q65–Q79 |
|
|
Vision |
|
|
Refraction Disorders |
H52 |
|
Cataract infantile and juvenile |
H26.0 |
|
Chorioretinal Inflammation, infectious or parasitic |
H32.0 |
|
Nightblindness, due to vitamin A deficiency |
E50.5 |
|
Other |
Q10–Q15 |
|
Hearing |
|
|
Conductive and Sensorineural |
H90 |
|
Other |
Q16 |
|
Hearing and Speech |
|
|
Specific Speech Articulation Disorder |
F80.0 |
|
Expressive Language Disorder |
F80.1 |
|
Receptive Language Disorder |
F80.2 |
|
Behavior |
|
|
Attention-Deficit Hyperactivity Disorder |
F90.0 |
|
Pervasive Developmental Disorder, including autism |
F84 |
|
Other |
F80–F98 |
|
Source: [1] |
|
Cognitive Disabilities
Cognitive disabilities in children include mental retardation as well as specific learning disabilities in children of normal intelligence. Mental retardation is defined as subnormal intelligence (intelligence quotient [IQ] more than two standard deviations below that of the population mean), accompanied by deficits in adaptive behavior. Grades of mental retardation are typically defined in terms
of IQ. Children with mild mental retardation, the most common form, are limited in academic performance and consequently have somewhat limited vocational opportunities. Adults with mild mental retardation typically lead independent lives. Children with more severe grades of mental retardation (moderate, severe, and profound) are more likely to have multiple disabilities (e.g., vision, hearing, motor, and/or seizure in addition to cognitive disability) and to be dependent on others for basic needs throughout their lives.
In contrast, specific learning disabilities result not from global intellectual deficit, but from impairments in one or more of the specific “processes of speech, language, reading, spelling, writing or arithmetic resulting from possible cerebral dysfunction.”[12] Children with specific learning disabilities are usually identified as such only after entering school, where a significant discrepancy is noted between their achievements in specific domains and their overall abilities. With special educational accommodations, these children may learn to overcome their limitations and demonstrate normal or even superior levels of achievement.
Motor Disabilities
Motor disabilities include limitations in walking and in use of the upper extremities (arms and/or hands). Some motor disabilities also affect speech and swallowing. Severity can range from mild to profound. Motor disabilities diagnosed in infancy or childhood include cerebral palsy, which results from damage to motor tracts of the developing brain; paralysis following conditions such as poliomyelitis and spinal cord injuries; congenital and acquired limb abnormalities; and progressive disorders, such as the muscular dystrophies and spinal muscular atrophies. Cerebral palsy results from a permanent, nonprogressive damage or insult to the developing brain. Affected children therefore may manifest a variety of motor dysfunctions, depending on the specific location of the damage. Involvement of the motor cortex produces spasticity, while involvement of the cerebellum results in hypotonia with or without ataxia. Involvement of the basal ganglia leads to dyskinesia and dystonia. Individuals with cerebral palsy often have other disabilities as a result of concomitant insults to various areas of the brain. Such disabilities include mental retardation, learning disabilities, epilepsy, language disorders, and behavioral problems. Similarly, some of the progressive motor disorders, such as muscular dystrophy, can be accompanied by cognitive disabilities. In contrast, in many forms of paralysis, such as that due to poliomyelitis or spinal cord injury, and congenital or acquired limb abnormalities, the disability is more likely to be restricted to motor skills or mobility.
Vision, Hearing and Speech Disabilities
The prevalence of low vision, blindness, and hearing loss increases with age, making these disabilities conditions that affect primarily adults. A number of important causes of vision as well as hearing disability have their onset early
in life, however, and may be considered neurodevelopmental (as discussed further below). Refractive errors, the most common form of vision impairment, are especially problematic for children in low-income countries because eyeglasses and basic vision care services are unavailable to many. However, refractive errors are readily amenable to low-cost methods of diagnosis and intervention, which can become a component of primary care screening services.[13,14,15,16,17 and 18]
Learning to speak depends on the ability to hear and repeat sounds. The optimal period for speech acquisition is the first 2 years of life; a child who does not speak by the age of 5–6 will have difficulty developing intelligible speech thereafter. It is therefore important to screen young children for hearing impairment and to evaluate the hearing of a child who is suspected of having mental retardation or delay in speech development.
Behavioral Disorders
In most of the developing world, resources for mental health care are far more limited than those for physical care. Therefore, the majority of children with psychological or behavioral disorders go undiagnosed or untreated. Although formal data are lacking, it is probable that behavioral problems are more common in low-income than in wealthier countries because of the excess prevalence of poverty, war, famine, and natural disasters in the developing world.[19,20] Moreover, recent social transformations and rapid urbanization in many low-income countries have produced adverse effects, such as residential displacement and disruption of traditional family systems, that have in turn resulted in large numbers of homeless and displaced children. Behavioral disorders not necessarily linked to psychosocial precursors include autism and attention-deficit and hyperactivity disorders. These disorders can have profound effects on academic achievement and on families. Current research is seeking to identify structural and functional correlates in the brain for a range of behavioral disorders.
SCOPE OF THE PROBLEM
Developmental disabilities impose enormous personal, social, and economic costs because of their early onset and the lifetime of dependence that often ensues. Children with disabilities often have limited educational opportunities, and as they grow older, limited employment options, productivity, and quality of life. Yet the costs of developmental disabilities are difficult to quantify in settings where relevant data and services are lacking. As a result, in low-income countries today, where more than 80 percent of the world's children are born, the magnitude of the impacts of developmental disabilities on individuals, families, societies, and economic development remains largely unrecognized and has yet to be addressed from a policy perspective.
While disability-adjusted life years (DALYs; for definition see Chapter 2) have been computed for some of the specific causes of developmental disability, such as meningitis and iodine deficiency,1 these figures do not convey the full proportion of cases within a given category of disorder that result in early and lifelong disability or death. Nor are DALY estimates currently available for the broad categories of developmental disability listed in Table 5-1 or for developmental disability as a whole. What is needed before useful DALY or other measures of impact can be calculated for developmental disabilities is accurate and up-to-date information from low-income countries on the prevalence and impacts of long-term functional limitations originating early in life as a result of both known and unknown causes. These data would allow an assessment of the costs and impacts of developmental disabilities against the costs of their prevention, which would in turn facilitate rational decision making and resource allocation with respect to child health and development. Without this information, there is a tendency to conclude that in low-income countries, more pressing issues preclude the allocation of resources for the prevention of developmental disabilities.
While the focus of this report is on the public health dimensions of developmental disabilities in children, including etiology, quantitative indicators, and strategies for prevention, we cannot neglect the fact that the major impacts of developmental disabilities in all countries are borne by families and individuals as a result of experiences that are difficult to quantify. These experiences include stigma, lost hopes and opportunities, discrimination, increased stress and daily challenges brought on by lifelong impairment, handicap, and social isolation. It is hoped that as countries and governments begin to take responsibility for the public health dimensions of developmental disabilities, improved awareness and management of the human dimensions of these disorders will follow.
As societies and economies become increasingly information-oriented and dependent on highly skilled and literate workers, it is critical that children everywhere have an opportunity to attain their optimal levels of cognitive and neurological development. The persistence of excess prevalence rates of developmental disabilities observed in low-income countries today is both a consequence of poverty and poor resource allocation and an impediment to future social and economic development.
|
1 |
The most recent DALY figures in low- and middle-income countries for risk factors discussed in this chapter include HIV/AIDS, 5.5 percent; polio, 0.0 percent; measles, 2.4 percent; tetanus, 1.0 percent; meningitis, 0.4 percent; malaria, 3.1 percent; Japanese encephalitis, 0 percent; trachoma, 0.1 percent; protein-energy malnutrition, 1.2 percent; iodine deficiency, 0.1 percent; vitamin A deficiency; 0.2 percent; anemias, 1.9 percent; road traffic accidents, 2.7 percent; homicide and violence, 1.6 percent; war, 1.7 percent. |
PREVALENCE AND INCIDENCE
Valid generalizations about the frequency and causes of developmental disabilities are difficult to make for any population because of the lack of true incidence data. Data on incidence (i.e., the frequency of newly occurring cases) are preferable to those on prevalence (i.e., the number of existing cases in a population) for investigating etiology because they allow causes to be distinguished from factors associated with survival. For developmental disabilities, incidence data are not available because only a minority of cases survive long enough to be identified, while for those who do survive, the onset of recognizable disability is often insidious as development unfolds.[21] In relatively wealthy countries, epidemiological studies of developmental disabilities are generally cross-sectional and use service records or registries to ascertain prevalent cases. Thus, in contrast to incidence, a great deal is known about the prevalence of developmental disabilities in populations where affected children receive services.
In populations lacking universal schooling and formal services for children with disabilities, the relatively few prevalence studies conducted to date have employed door-to-door surveys designed to identify all children with developmental disabilities in defined populations. The validity and interstudy comparability of prevalence estimates from these surveys depend on the quality and comparability of the assessment methods and diagnostic criteria used, which can be difficult to appraise from published reports. In addition, even when valid methods have been employed, there may be questions about the cross-cultural appropriateness of standardized tests of intelligence and behavior used to diagnose disabilities in children of diverse cultural and socioeconomic backgrounds.[22]
An additional problem in comparing prevalence studies from developing countries is that elevated infant and child mortality rates may curtail the prevalence of developmental disabilities in the population. If improvements in child survival are made without concomitant reductions in the occurrence of new cases of developmental disabilities, the result will be an increase in the population prevalence of disability due to the increased longevity of children with disabilities.[23,24 and 25]
A review of the prevalence studies of developmental disabilities published between 1970 and 1999 shows that most of the available data are restricted to the relatively high-income populations of developed countries in Europe, North America, and eastern Asia. Yet during this period, more than 80 percent of the world's children resided in low- and middle-income countries. This imbalanced knowledge is both a cause and a consequence of the fact that the public health impact of childhood disabilities has received little attention in low-income countries. Available evidence, however, suggests that many of the causes of disability in children are more prevalent in developing than in developed countries.
Prevalence of Cognitive Disabilities
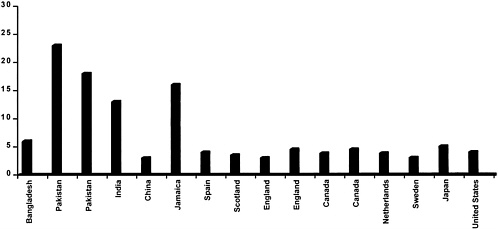
Prevalence data on an aggregate of cognitive disabilities in developing countries are not available. Figure 5-1 summarizes the range of prevalence estimates for severe mental retardation among children in populations throughout the world. The studies are listed in descending order by per capita income of the countries in which they were conducted. These estimates show a clear tendency toward elevated prevalence in low-income countries. In developed countries, the prevalence of severe cognitive disability is consistently found to be in the range of 3 to 5 per 1,000 children. By contrast, the prevalence of severe cognitive disability in developing countries ranges from a low of 2.9 per 1,000 children in Beijing to a high of 22 per 1,000 in slum areas surrounding Lahore, Pakistan. The majority of estimates from low-income countries are above 5 per 1,000, while no estimates from developed countries are this high.
Prevalence of Motor Disabilities
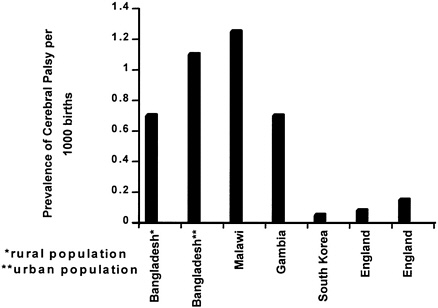
The prevalence of motor disability among children in developing countries is not well defined. Figure 5-2 provides prevalence data on cerebral palsy from available sources.
Prevalence of Vision Disabilities
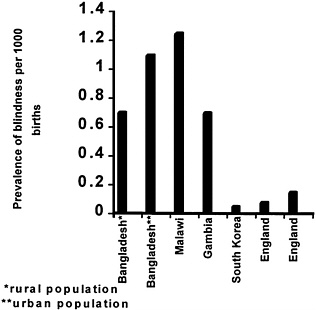
The World Health Organization (WHO) estimates the worldwide prevalence of childhood blindness to be 1.5 million, with the numbers of affected children being 1 million in Asia and 0.3 million in Africa. In addition, an estimated 5 million children have low vision.[43,44] The prevalence of blindness in northern Nigeria has been estimated to be 1.5 percent, more than seven times the prevalence in the United Kingdom.[45] Specific prevalence data on vision disorders among children in low-income countries are scarce. Figure 5-3 illustrates the findings of these limited studies. For all ages combined, the prevalence of vision disorders is clearly higher in less developed than in developed countries (see Figure 5-4). Several studies have estimated that as much as 47 percent of blindness and low vision is preventable or curable.[15,16,17 and 18,44,45]
Prevalence of Hearing and Speech Disabilities
Estimates of hearing loss and profound deafness vary from 1 per 1,000 in developed countries to 1.4 to 4 per 1,000 in developing countries. WHO estimates the worldwide prevalence of hearing impairment to be 120 million, with 78 million of those affected living in developing countries.[46] Limited studies from developing countries reflect the frequent variability found in prevalence data on disabilities described earlier due to non-standardized methods of testing and reporting.[47] A study from Kenya revealed rates from 1 to 3 percent while studies in Sri Lanka and Thailand found rates as high as 12 and 13.6 percent, respectively.[48,49 and 50] Studies in India have estimated that 80 million individuals suffer from some level of disabling hearing impairment.[51] A 1990 official survey of the handicapped in China reported 23.1 million hearing-impaired individuals among which six million suffered from profound hearing loss.[52] Prevalence rates of profound hearing loss of 2.7 per 1,000 in the Gambia and 4 per 1,000 in Sierra Leone are three to four times the prevalence rates of developed countries.[53,54 and 55] Chronic otitis media (CMO) has been determined as the most frequent cause of hearing impairment in many developing countries.[55,56,57,58 and 59] High prevalence of the infectious diseases that cause CMO, such as meningitis and measles, in developing countries suggests a greater risk for hearing impairment in these populations. Estimates suggest that as much as 50 to 66 percent of all hearing impairment is preventable.[ 54,60,61 and 62]
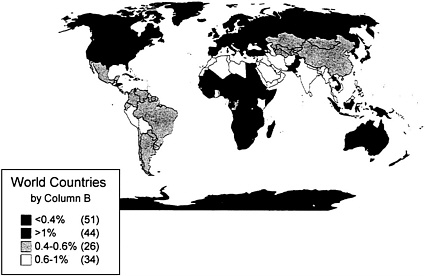
FIGURE 5-4 World Prevalence of Blindness Source: [74]
Prevalence of Behavioral Disabilities
Autism and autistic disorders are relatively rare among the developmental disabilities, affecting fewer than 5 per 1,000 children. Before the advent of explicit diagnostic criteria for autism, this condition was thought to be restricted to severe forms and was found in studies in a number of developed countries to affect about 4 per 10,000 children in the general population.[75,76] More recent prevalence studies based on explicit diagnostic criteria and including Asperger's syndrome report a range of severity with overall prevalence as high as 4 per 1,000 children.[77] Similar studies of the prevalence of autistic disorders in developing countries could not be identified.
Attention-deficit hyperactivity disorder is a common childhood behavioral disorder with increasing recognition and reported prevalence in developed countries. Epidemiological studies in the United States have reported prevalence to be approximately 4 percent, with figures as high as 11 percent in some studies.[78] Studies of the prevalence of attention-deficit hyperactivity disorder in developing countries could not be identified.
RISK FACTORS
The causes of developmental disabilities include damage to or anomalies in the developing nervous system. The human nervous system is especially vulnerable during the period of its most rapid growth, which begins during gestation and extends into early childhood.
A large proportion of developmental disabilities have their origin in inherited or sporadically occurring genetic or chromosomal aberrations or in the combined effects of genetic traits and environmental exposures. Other causes include infections, nutritional deficiencies, and other exogenous insults or exposures during critical periods of neurodevelopment. The consequences of these exposures often depend on the precise timing of the insult to the developing nervous system. For example, maternal rubella infection has devastating effects on the nervous system of the fetus, but only if exposure occurs between the first and thirteenth weeks of pregnancy.
The following subsections describe the major classes of risk factors for developmental disabilities: genetic factors, nutritional deficiencies, infection, exposure to environmental toxins, perinatal and neonatal factors, and poverty and trauma. Rather than providing an exhaustive review, this section highlights risk factors for which evidence exists from developing countries of both (1) high frequency and/or public health and economic impacts, and (2) viable, if unrealized, potential for prevention.
Genetic
Genetic components within the heterogeneous and multifactorial etiology of most developmental disabilities may appear to be overshadowed in low-income countries by the high frequency of infectious, parasitic, and nutritional disorders and traumatic causes. Nevertheless, genetic factors and congenital anomalies are of considerable importance in these countries. In West Africa, 2–3 percent of all children have a serious hemoglobinopathy (sickle cell anemia, thalassaemia).[79,80 and 81] Children with hemoglobinopathies are at risk for nervous system complications, the frequency of which may be as high as 12.8 percent.[ 82] Complications of sickle cell disease in children include mental changes; cerebrovascular accidents (strokes); cranial nerve palsies; dural sinus thrombosis; and increased susceptibility to meningitis, especially salmonella meningitis and pneumococcal meningitis. A recent study in the United States revealed that 33 percent of the children observed with sickle-cell disese were functioning in the range of mild mental retardation.[83]
In populations lacking effective contraception, family planning, and prenatal screening, the proportion of births to women over age 35 and the prevalence of Down syndrome are high. In low-income countries, the proportion of births contributed by mothers over 35 is 11–15 percent, compared with 9 percent in industrialized countries.[84]
Another factor contributing to the high levels of developmental disabilities observed in some populations, notably in South Asia, the Middle East, and North Africa, is the prevalence of consanguineous marriage, resulting in increased homozygosity for deleterious mutations. In some parts of Africa, the Middle East, and South Asia, the prevalence of consanguinity ranges from 25 to 61 percent among all parents.[85,86,87,88 and 89] Consanguinity has been linked to elevated rates of perinatal mortality and disabling childhood conditions in a number of populations.[90,91,92,93,94 and 95]
Some inborn errors of metabolism, such as galactosemia, mucopolysaccharidoses, maple syrup urine disease, and homocystinuria, are occasionally reported from centers in low-income countries with adequate laboratory facilities.[ 96] Others may be distinctly rare in certain low-income countries. For example, phenylketonuria (PKU) is rare in black African children. By contrast, some dominantly inherited neurocutaneous disorders, specifically neurofibromatosis and tuberous sclerosis, appear to be especially common among black African children.[97,98 and 99]
The major genetic causes of childhood motor disability, such as Duchenne muscular dystrophy, are found in virtually all countries. Others, such as the congenital myopathies (central core disease, Nemaline myopathy, myotubular myopathy) have been reported mainly from Southeast Asia, and also among Arabs in the Middle East and North Africa. Spinal muscular atrophies are particularly common in Southern Africa, while congenital muscular dystrophies are very common in North Africa and the Middle East.[100,101,102 and 103]
PKU, a rare defect of amino acid metabolism occurring in 1/15,000 Caucasian live births and somewhat less frequently in Africans,[ 98,104,105 and 106] results from a mutation at the phenylalanine hydroxylase gene and is inherited in an autosomal recessive manner. Deficient metabolism of phenylalanine causes accumulation, which if untreated leads to hyperphenylalaninaemia, progressive damage to the developing brain during the neonatal and postnatal periods, and severe mental retardation in most cases. In populations where newborn screening and dietary treatment for PKU are feasible (as discussed in the following section on interventions), the diet must be continued for females throughout the child-bearing years to prevent brain damage in offspring from prenatal exposure to elevated maternal phenylalanine.
Nutritional Deficiencies
Micronutrient Deficiencies
Iodine deficiency occurs on all continents and is associated with a range of adverse reproductive and developmental outcomes, including miscarriage; perinatal mortality; and cognitive, motor, and hearing disabilities.[107] Sustained exposure to severe maternal iodine deficiency through the second trimester of pregnancy can result in cretinism or iodine-deficiency syndrome, a severe form
of congenital disability involving cognitive and motor deficits, and often hearing loss and speech impairment. Milder cases of maternal iodine deficiency result in a range of intellectual, motor, and hearing deficits among children in iodine-deficient regions.[108] In addition, continued iodine deficiency in the postnatal period may increase infant mortality [109] and impair mental performance in subsequent years.[110,111]
Vitamin A deficiency contributes to childhood disability in two ways. One is through its effects on ocular tissue. When severe and prolonged, the deficiency leads to xerophthalmia, which ranges in severity from night blindness to permanent corneal scarring and blindness. Vitamin A deficiency also increases the severity of serious childhood infections, such as measles, making the deficiency a major contributor to child mortality in low-income countries and potentially the cause of long-term disability among survivors.[112] WHO (1995) has estimated that 250 million infants and children under age 5 in low-income countries have low vitamin A stores, and an additional 3 million are clinically deficient in vitamin A with evidence of xerophthalmia and are at risk for blindness. In 1992, WHO estimated that at least half of the prevalent cases of childhood blindness worldwide were the result of vitamin A deficiency.[44]
Iron deficiency anemia is a widespread public health problem in low-income countries, where it affects a high percentage of women, infants, and children. Although iron deficiency may not be a sufficient cause of developmental disability, it contributes to the risk of such disability by lowering immunity, impairing fat and vitamin A absorption, impairing thyroid hormone transformation, increasing lead absorption, and increasing the risk for low birth weight.[113,114] Evidence of direct, central nervous system effects of iron deficiency anemia during infancy was recently found in Chile.[115] An association has been observed between iron deficiency anemia in childhood and persistent deficits in cognition, attention, and learning capacity, though confounding effects of socioeconomic disadvantage are difficult to disentangle.[116,117] In addition to dietary iron deficiency, major risk factors for iron deficiency anemia in low-income countries include hookworm and other helminthic infestations, malaria, diarrheal disease, and poverty.[ 118]
Folate deficiency early in pregnancy contributes to the occurrence of neural tube defects, such as spina bifida, which result in motor disability and in some cases intellectual impairment among surviving infants. Epidemiological studies reveal large geographic differences in the prevalence of neural tube defects, and an association between preconceptional and periconceptional folate consumption during pregnancy and the occurrence of neural tube defects in offspring. This association is due, at least in part, to a gene–environment interaction. Mutations of the methylenetetra hydrofolate reductase gene in the absence of a folate-rich diet is associated with elevated maternal plasma homocysteine and the occurrence of neural tube defects in offspring.[119,120] Supplementation of 400 micrograms of folic acid per day is sufficient to increase the activity of the vari-
ant methylenetetra hydrofolate reductase; correct maternal hyperhomocysteinemia; and, when initiated prior to conception or very early in pregnancy, prevent the occurrence of a substantial portion of neural tube defects.[ 121]
Protein-Energy Malnutrition
The clinical consequences of severe malnutrition for the developing nervous system may include compromised intersensory integration, poor language development, and retarded behavioral and learning skills.[ 106,122,123 and 124] Malnutrition can also lead to various neuropathies, including tropical ataxic neuropathy and pellagrous neuropathy. Yet the contribution of protein-energy malnutrition to developmental disabilities is less clear than that of micronutrient deficiencies. Animal studies have long shown that nutritional deprivation during the phase of maximum brain growth can adversely and, under some circumstances, irreversibly affect the brain.[125] The effects of such deprivation on behavior in animals, and on mental performance in human beings, are not fully understood, however.[ 126,127] Poor nutrition is typically confounded with poverty and poor education, two of the strongest predictors of poor mental performance.
Evidence regarding the independent effects of general nutrition on children's mental development suggests that nutritional changes from gestation through 6 months of age, as well as between 42 and 75 months of age, appear to produce no measurable effects on mental performance later in childhood.[126,128,129,130,131 and 132] Dietary supplementation of undernourished infants and children in Bogota between 6 and 36 months of age was followed by improved mental performance from 12 to 36 months, but follow-up beyond 36 months was not done. If supplementation between 6 and 36 months could be shown to produce persistent gains in mental performance, this would suggest the existence of a critical period when nutrition can affect mental development. If, on the other hand, the effect of early supplementation does not persist, it may be that children need food to perform well on developmental tests,[133] but malnutrition severe enough to retard physical growth does not produce long-term cognitive delay or disability.
On the whole, studies of mental development indicate that the association between socioeconomic deprivation and developmental disabilities is better explained by lack of access to education and intellectual stimulation and by micro-nutrient deficiencies than by protein-energy malnutrition.[126] Even if irreversible effects of protein-energy malnutrition per se on the developing nervous system of humans cannot be demonstrated, however, it is clear that chronic malnutrition is detrimental to children's survival, growth, and cognitive and physical performance. Prevention of protein-energy malnutrition is therefore a top international priority.[134] Moreover, malnutrition among children with developmental disabilities impacts adversely on survival, as well as on the ability to benefit from educational interventions.[135]
Infection
Numerous prenatal, perinatal, and postnatal infections can damage the developing nervous system or senses and cause long-term disabilities in children, and are important causes of developmental disability in low-income countries. In Nigeria, for example, the majority of cases of blindness and deafness in children are secondary to infections such as measles, rubella, onchocerciasis, meningitis, and chlamydia.[ 45,136]
Congenital rubella can manifest with deafness, cataract and visual impairment, mental retardation, and failure to thrive. This cause of developmental disability has been virtually eliminated in successfully vaccinated populations, but epidemics of rubella continue to occur in some developing countries.[ 137,138 and 139] Congenital syphilis remains rampant in some developing countries, with neurological manifestations that include deafness, interstitial keratitis, and mental retardation.[ 140,141,142 and 143] Congenital toxoplasmosis manifests as necrotizing encephalopathy, microcephaly, cranial nerve palsies, spastic quadriparesis, intracranial calcification, and chorioretinitis; seizures can also be a presenting feature.[144,145 and 146] Congenital cytomegalovirus infection can result in microcephaly, mental retardation, seizures, and deafness.[147] Herpes simplex may be acquired congenially or during parturition, resulting in microcephaly, intracranial calcification, microphthalmia, and retinal dysplasia.[ 148]
HIV is now an important cause of developmental disability, particularly in populations where it affects a high proportion of childbearing women and where access to effective antiretroviral therapies and cesarean delivery are not available. In some high-risk populations, the prevalence of infection in women of reproductive age is 20–30 percent or higher.[105,149,150 and 151] With the emergence of antiretroviral therapy (zidovudine) to prevent perinatal transmission of HIV,[152] the risk of vertical transmission of the virus from infected mothers to offspring has been reduced from about 25 percent to less than 10 percent in European and North American populations. When treatment is combined with delivery by cesarean section, transmission can be reduced to as low as 2 percent.[153,154] In low-income populations—which include the majority of HIV-infected women worldwide and in which prenatal screening, counseling, and treatment options are limited —the probability of vertical transmission from untreated infected mothers remains as high as 30 to 40 percent. Recently, short-course antiretroviral prophylaxis regimens have been shown to provide a relatively low-cost and effective strategy for preventing vertical transmission of HIV in low-income populations.[155,156] Once a child has been infected, the ensuing effects of pediatric AIDS include central nervous system impairment, acquired microcephaly, and cognitive and movement disabilities in virtually all cases.[ 157] Thus, HIV infection is now a leading, fatal cause of developmental disability in many populations.
Brain damage from many intrauterine infections (toxoplasmosis, cytomegalovirus, varicella, HIV) may follow either prenatal or perinatal transmission.[ 158,159] When exposure occurs during the first or second trimester of pregnancy, several impairments are recognizable at birth, including microcephaly, hydrocephaly, growth retardation, cataracts, seizures, rashes, jaundice, and hepatosplenomegaly.[160,161] Exposure late in pregnancy or during delivery may result in inapparent infection at birth and onset of developmental delay during infancy or childhood.[162] In the case of toxoplasmosis, early detection and treatment (prenatal or neonatal) with antiparasitics is believed to reduce the occurrence of hydrocephalus and cognitive sequelae, though even among treated infants the frequency of severe mental retardation in one follow-up study of infected infants was 21 percent.[163]
Postnatally acquired infections are important causes of developmental disabilities among children in low-income countries, where access to prophylaxis and treatment is often limited and delayed. These infections include malaria, bacterial meningitis, viral encephalitis, measles, poliomyelitis, tetanus, and trachoma.[93,164,165]
Malaria is a public health problem in about 90 countries and is estimated to cause several hundred million cases and approximately 1 million deaths among children each year.[165,166 and 167] A major complication of malaria is cerebral malaria, the major clinical manifestations of which are convulsions and an alteration in the level of consciousness that starts as drowsiness and rapidly proceeds to deep coma. Repeated episodes of malaria are responsible for poor school attendance and childhood anemia. During pregnancy, malaria may result in placental parasitemia and intrauterine growth restriction, as well as maternal anemia and death.[168,169]
Meningitis from major bacterial agents probably occurs more commonly in developing than in developed countries, though specific data are lacking. Children under age 5 and especially under age 1, as well as the elderly, are at highest risk.[170,171 and 172] In developing countries, pneumonia is the most common presentation of Haemophilus influenzae Type b meningitis; it has been estimated that this cause of meningitis in developing countries has a case fatality rate of 30 percent and results in permanent nervous system impairment in 20 percent of survivors.[ 166,173,174] Meningococcal meningitis occurs sporadically in developed countries, but major epidemics of the disease occur every several years in sub-Saharan Africa and South America.[166] Case fatality exceeds 50 percent in the absence of early and adequate treatment, and it is estimated that 15 to 20 percent of survivors are left with deafness, seizures, and mental retardation.[166] Otitis media is most often secondary to meningitis and the most common cause of hearing loss in many developing countries.[55,56,57,58 and 59]
Japanese viral encephalitis is the leading cause of viral encephalitis in Asia, where it is responsible for at least 50,000 cases of clinical disease each year, primarily among children.[166,175,176] Case fatality is as high as 20 per-
cent, and the frequency of neuropsychiatric sequelae among survivors is high, ranging from 30 to 50 percent in several developing country studies.[176,177,178 and 179] Following an infectious mosquito bite, the virus replicates in the lymph nodes, spreads to the central nervous system, and propagates in the brain, leading to seizures, cognitive and motor disabilities, and progressive coma.[166]
Measles is an acute viral disease that is still a leading cause of death worldwide, largely because of its occurrence among children under age 5 in developing countries.[180,181 and 182] Rarely (about 1/1000 cases), measles infection causes encephalitis, which can result in long-term nervous system sequelae among survivors. While Vitamin A deficiency has been shown to increase the severity of measles infection, it is thought the infection can, in turn, exacerbate Vitamin A deficiency and lead to blindness.[183,184,185 and 186]
Following a concerted international initiative, paralytic poliomyelitis was eradicated from the Western Hemisphere, the Western Pacific region, and Eastern Europe.[187] This enteroviral disease, however, remains a major problem among children in tropical Africa and to a lesser extent in South and Southeast Asia. Once established in the intestines, poliovirus can enter the blood stream and invade the central nervous system. As it multiplies, the virus destroys motor neurons and leads to irreversible paralysis.
Tetanus, especially neonatal tetanus, is still prevalent in many developing countries. Various studies have shown that it is not only associated with high mortality, but also followed by adverse developmental sequelae in those who survive.[182,188,189 and 190] Neonatal tetanus is due mainly to improper management of the umbilical cord, which is often cut by traditional birth attendants with items such as bamboo knives, broken bottles, and unsterilized razors, and dressed with herbal concoctions and cow's dung that are heavily contaminated with Clostridium tetani. Tetanus, like poliomyelitis, is preventable by appropriate immunization of infants, while neonatal tetanus can be prevented by immunizing pregnant mothers.[182,188,189 and 190]
Trachoma is a bacterial disease of the conjunctiva caused by Chlamydia trachomatis.[191] Repeated infections, which often begin in childhood, result in blindness in adulthood. Trachoma is endemic in many impoverished areas of the world where access to clean water is compromised. An estimated 5.9 million people worldwide have become blind or are at immediate risk for blindness as a result of trachoma infection.[ 191,192 and 193]
Environmental Toxins
Children may be exposed to toxins that predispose them to developmental disabilities through a variety of routes. Some, such as lead, are present in either the prenatal (maternal) or postnatal environment. Others may be introduced systemically, as through the maternal use of alcohol or teratogenic medications. Lead, which can be absorbed from paint flakes on the floor or painted toys and
from the fumes of burning batteries, has long been known to cause the serious and often fatal condition of lead encephalopathy in children. In low-income countries, children continue to be exposed to lead from gasoline and other sources.[194,195] Persistence of the effects of early lead exposure into adolescence and young adulthood has also been demonstrated.[196,197] Overall, a dose–response relationship between lead exposure in early childhood and mental performance, as well as hyperactivity and other behavioral problems, is well documented.[198]
Heavy alcohol abuse during pregnancy is associated with fetal alcohol syndrome in offspring. This syndrome includes cognitive disability (usually mild to moderate in severity), low birth weight, microcephaly, and subtle facial abnormalities that may diminish over time. Ototoxic drugs capable of causing congenital hearing loss if ingested during pregnancy include streptomycin and salicylates. Thalidomide, a well-documented and once-banned teratogen, has recently been reintroduced in developing countries for patients with leprosy and HIV infection.[199] Without appropriate precautions, this drug could lead to an epidemic of birth defects in low-income countries. In addition, prenatal exposure to ubiquitous environmental contaminants such as polychlorinated biphenyls (PCBs) and tobacco smoke may also have detrimental effects on the developing nervous system.[200,201]
Perinatal and Neonatal
Perinatal events such as preterm birth, low birth weight, intrauterine growth restriction, and birth asphyxia are associated with elevated risk of impaired physical, sensory, and mental development during infancy and childhood.[202] Many factors contribute to the elevated frequency of these events in low-income countries. These factors include the scarcity of resources for obstetrical care and management of complications of labor and delivery; dietary deficiencies, some of which are encouraged by the fear of increased delivery complications associated with larger babies in settings where professional obstetrical services are lacking; anemia; and increased risk of maternal infections, such as malaria and genital tract infections, in some settings.
Perinatal complications are important risk factors for developmental disabilities. For example, retinopathy of prematurity is a leading cause of childhood blindness worldwide.[203] In addition, prematurity is an important risk factor for cerebral palsy and cognitive disabilities in childhood. Yet the etiology of many perinatal complications, as well as the nature and direction of their causal association with developmental disabilities, is often not clear, limiting efforts at prevention. Research is urgently needed on the etiology and prevention of adverse perinatal outcomes such as low birth weight, preterm birth, and intrauterine growth restriction; on the causal relationships between these factors and de-
velopmental disabilities; and on the impact of their prevention on the prevalence of neurodevelopmental disabilities in low-income countries.
Neonatal factors that can be devastating to the developing nervous system, resulting in long-term disability, include severe, untreated hyperbilirubinemia and neonatal infections.[204] A cross-sectional, retrospective study in Bangladesh found both of these exposures to be significant risk factors for serious mental retardation in childhood.[205]
Poverty and Trauma
Poverty greatly increases children's risk for developmental disabilities (see Chapter 2). Low socioeconomic status of the family and suboptimal maternal education have both been shown to be associated with deficits in cognitive development among children in developing countries.[88,205] Low socioeconomic status appears to be the strongest and most consistent predictor of mild mental retardation throughout the world.[206,207] Moreover, impoverished physical environments, war, land mines, natural and human-induced disasters, lack of road safety and injury prevention initiatives, and child abuse and neglect together expose children in many low-income countries to excess hazards that potentially contribute to the prevalence of developmental disabilities,[19,208,209,210,211 and 212] though evidence from follow-up studies linking these exposures to the occurrence of developmental disabilities is lacking.
INTERVENTIONS
Comprehensive prevention of developmental disabilities involves primary prevention, secondary prevention or treatment, and tertiary prevention or rehabilitation.
Primary and Secondary Prevention
Primary prevention includes efforts to control the underlying cause or condition resulting in developmental disability. Examples are vaccination to prevent congenital rubella and salt iodination to prevent iodine deficiency. Secondary prevention is aimed at preventing an existing illness or injury from progressing to long-term disability. Examples of such interventions are newborn screening for PKU, followed by dietary modifications, and emergency medical care for trauma.
Genetic Factors
Expansion of family planning and contraception to prevent unplanned births to women over age 35 is a cost-effective strategy for prevention of mental retardation, specifically of Down syndrome (trisomy 21).
Another clear risk factor for genetic causes of developmental disability —the practice of consanguineous marriage[213]—may be difficult to modify, being integral to the culture, social structure, and land tenure systems of many
integral to the culture, social structure, and land tenure systems of many populations. However, educational campaigns and genetic counseling are potential strategies for reducing this important contributor to the prevalence of developmental disabilities in many countries.
In countries with routine newborn screening programs and effective follow-up of affected children, disabilities due to conditions such as hypothyroidism and PKU are rarely seen. Newborn screening and intervention programs for treatable conditions may be cost-effective in low-income countries, as they are in wealthier countries, when weighed against the costs of disability that are incurred when these conditions go undetected and untreated.[105,106,214,215]
Nutritional Deficiencies
There are four broad categories of interventions designed to correct or prevent micronutrient deficiencies: education regarding dietary sources of essential nutrients and strategies for ensuring adequate dietary intake; fortification of the food supply; supplementation to ensure adequate intake by targeted individuals, such as by means of vitamin A capsules or iron tablets; and control of infectious and parasitic diseases that deplete bodily stores or interfere with absorption of micronutrients.[216]
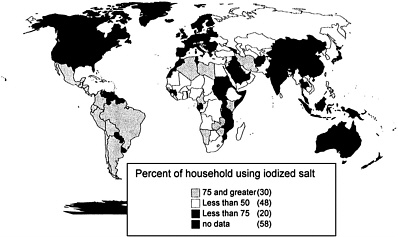
Iodine Deficiency. Correction of maternal iodine deficiency immediately before conception is necessary if the adverse effects of the deficiency on neurodevelopment and cognition are to be prevented in children. The only practical way to achieve this from a public health perspective is through universal dietary fortification. Salt iodination is now being implemented in many developing countries,[217] though difficulties with distribution and quality control remain, and the success of this intervention requires major commitments from governments and international agencies (see Figure 5-5 for the percentage of households worldwide using iodized salt). In 1993, the World Bank estimated a DALY cost of US$8 for elimination of iodine deficiency by means of salt fortification, but this estimate did not take account of the full impact of iodine deficiency disorder on the intellectual capacity of affected populations.[218] Thus, the actual cost per DALY is likely to be even less than US$8. Iodination of drinking water has been shown to be a safe and cost-effective alternative in some settings.[219] Iodine deficiency is still a prevalent cause of developmental disability in many communities, and its elimination will require sustained efforts.[ 218]
Vitamin A. Elimination of blindness due to Vitamin A deficiency is feasible through increased dietary intake of foods naturally rich in the vitamin, fortified foods, and supplements.[216] For economic and cultural reasons, it may not be possible to eliminate vitamin A deficiency through education aimed at promoting dietary intake of foods naturally rich in vitamin A. Fortification of a staple food is a long-term, low-cost intervention. Supplements are also inexpensive, at less than US$0.03 per capsule, and may be cost-effective to implement through immunization and maternal and child health care programs. Control of diarrheal diseases in children is also a necessary component of the prevention and correction of vitamin A deficiency.[ 221]
Iron. Nutrition education will have limited effectiveness against iron deficiency in populations where this deficiency is prevalent because foods rich in bioavailable iron are not accessible to economically disadvantaged women and children, who are at greatest risk. Fortification of staple foods, such as processed cereals, is feasible and cost-effective in some populations.[222] Fortification is generally not sufficient for preventing or correcting iron deficiency anemia in pregnant women, however, and supplementation is often required. The cost of fortifying cereals or flour is very low in populations where this is feasible, at US$0.05 per person per year.[222] The cost of supplementing women during pregnancy is about US$1.20 for 9 months, and the cost of fortifying infant diets has been estimated to be US$0.20 per person per year. In areas where hookworm or malaria is prevalent, treatment and prevention of these diseases is a necessary component of programs to prevent iron deficiency. Overall, the World Bank has estimated the benefit-to-cost ratio for a comprehensive iron deficiency prevention program to be as high as 500, implying that for the equivalent of every dollar spent on program costs, $500 is saved in costs associated with mortality, morbidity, and reduced functional capacity due to iron deficiency.[222]
Folic acid. Folic acid supplementation or fortification of the food supply is effective against neural tube defects, but only if the folate requirements of childbearing women are met periconceptionally or very early in pregnancy. Folates are present in leafy vegetables, legumes, and citrus, but it is doubtful whether dietary advice alone can result in consumption of sufficient amounts by those at risk. The strategy adopted in the some countries (e.g., the United States, Chile) is to supplement the entire population at an estimated level of 100 micrograms per day by fortifying bread flour with folic acid. Folic acid supplementation of the whole population at the level shown to prevent neural tube defects (i.e., 400 micrograms per day) raises two safety concerns that require monitoring, however. One is that doing so could mask pernicious anemia due to vitamin B12 deficiency, allowing neural damage characteristic of pernicious anemia to progress undetected. The other is the potential for drug interaction between high folate levels and certain medications. It has been estimated that folic acid supplementation could prevent 50 to 70 percent of neural tube defects.
Infections
Congenital Rubella. Vaccination of the population against rubella can prevent virtually all cases of congenital rubella. The availability of a combined measles and rubella vaccine increases the feasibility of eradicating rubella infection, though this goal is not currently recognized as a priority in low-income countries.[137] The cost-effectiveness of programs to ensure that all women of childbearing age are vaccinated against rubella has been demonstrated in the United States (benefit-to-cost ratio of 11.1:1), but not specifically in low-income countries.[137]
Malaria. Measures to prevent malaria infection include use of protective clothing, insect repellents, insecticide-treated bednets, and environmental management to control mosquito vectors. Once infection has occurred, chemoprophylaxis may be effective against the development of severe disease. The cost-effectiveness of malaria prophylaxis and treatment programs is well established in populations where malaria is endemic, even without accounting for the potential for long-term neurological deficits in children who survive cerebral malaria.[223,224]
Bacterial Meningitis. Primary prevention of Haemophilus influenzae Type b meningitis can be achieved by means of vaccination of all infants or by chemoprophylaxis following close contact with an affected child. Vaccination is the only practical method of preventing infection on a population level. In developed countries where immunization against this disease during infancy is routine, the incidence of Haemophilus influenzae Type b meningitis has dropped dramatically [164]. It has been argued that vaccination against Haemophilus influenzae Type b infection is cost-effective in developing countries as well,[ 225] but information on the frequency of the disease and its sequelae in developing countries is needed to guide the implementation of control strategies.[170,171,174]
With regard to meningococcal meningitis, epidemics can be controlled effectively by means of mass immunization campaigns resulting in at least 80 percent coverage, while infection in endemic situations can be prevented by chemoprophylaxis administered to close contacts of patients.[166] Information on the cost-effectiveness of these interventions in developing countries is needed.
Japanese encephalitis. An effective mouse brain-derived vaccine is available against the viral agent that causes Japanese encephalitis, and has been incorporated effectively into the national childhood vaccination program of Thailand.[ 226] The high cost of this vaccine and the potential for serious neurological sequelae, however, are barriers to its widespread use in endemic and epidemic situations.[226]
Trachoma. Improvements in hygiene, including access to clean water and education to promote frequent face washing, are highly cost-effective in the prevention of blindness due to trachoma.[191,192]
Measles. Vaccination using live, attenuated measles virus produces long-lasting immunity. Eradication of measles is theoretically feasible, given the effectiveness of available vaccines and the likelihood that humans are the only reservoir capable of sustaining transmission of the measles virus. Widespread vaccination has successfully prevented the spread of measles in a number of developing countries, and is considered one of the most cost-effective public health interventions ever undertaken.[183,227,228] However, measles continues to be a major contributor to childhood death and disease worldwide. Global eradication of this cause of developmental disability will require sustained efforts.
Poliomyelitis. Immunization programs have effectively eradicated poliomyelitis from much of the world, but the disease remains endemic in much of sub-Saharan Africa and parts of South and Southeast Asia.[187] Reported immunization coverage with the oral polio vaccine is still low in most African countries.[229] Although worldwide eradication of polio as a cause of childhood paralysis can be achieved by vaccination during infancy, meeting this goal will require major commitments that may be difficult to sustain in the face of the decline of the disease in much of the world.[187,229]
HIV. Efforts must focus on cost-effective and accessible methods of preventing maternal infection, as well as maternal–infant transmission. Low-cost provision of antiretroviral drugs to women infected with HIV in low-income populations should be viewed as an international priority. Vaccine development, the role of breastfeeding in transmission and prevention, and the effectiveness of modified treatment regimens and vaginal antimicrobials are currently areas of active research.[155,230,231,232,233 and 234]
Environmental Toxins
Preventing childhood lead poisoning should be both universally feasible and cost-effective when balanced against the improved cognition and occupational potential that result.[235] Prevention of lead exposure can be accomplished by controlling lead-based industrial processes, removing lead from gasoline and paint, and maintaining low lead levels in soil. Screening of blood lead levels in young children can be used to monitor risks and identify those requiring intervention. When elevated lead levels are detected, removal of the child from the source of exposure, developmental monitoring, and possibly chelation treatment to increase the excretion level are indicated. In developed countries, universal childhood screening of blood lead levels followed by intervention has proven cost-effective in high-risk populations, while targeted screening based on risk factor profiles is preferable in low-risk populations.[236,237] Research is needed on the feasibility and cost-effectiveness of interventions to prevent lead poisoning in low-income countries. In addition to such measures, prevention of industrial disasters resulting in neurotoxic exposures requires monitoring and enforcement of safety measures.[238]
In view of evidence that alcohol consumption during pregnancy is associated with a variety of adverse fetal outcomes, abstinence or restricted drinking during pregnancy should be a public health objective in all populations. Moreover, education and access regulations are necessary to prevent exposure to teratogenic medications during pregnancy; both of these measures appear to be underutilized in developing countries.[ 239]
Prenatal Care and Perinatal Services
Several specific interventions discussed in other sections of this chapter that are effective in the primary prevention of developmental disabilities may be implemented through prenatal and perinatal services. These include prenatal and newborn screening and intervention, prevention and treatment of prenatal infections, and avoidance of teratogenic exposures during pregnancy. Other interventions, such as rubella immunization and correction of maternal iodine deficiency, must be undertaken prior to pregnancy or before the initiation of prenatal care, and thus may need to target all women of childbearing age.
Models for providing prenatal care, obstetrical services, and neonatal care in low-income countries have been discussed and developed primarily with two goals in mind: prevention of maternal mortality and prevention of infant mortality.[240,241] Little attention has been given in low-income countries to the role of these interventions in the prevention of developmental disabilities. To some extent, perinatal and neonatal interventions to promote survival are also effective in the prevention of developmental disabilities. For example, effective management of maternal infections, of other complications of labor and delivery such as birth asphyxia, and of neonatal complications may prevent fetal and neonatal brain injuries. However, interventions aimed exclusively at improving survival by increasing the survival of infants with neurodevelopmental disorders can be expected to increase the prevalence of developmental disabilities in the population.[241,242] Research is urgently needed in low-income countries to identify specific causes of adverse perinatal and neonatal outcomes that are amenable to intervention, and to evaluate the effectiveness and cost-effectiveness of alternative interventions in terms of the prevention of not only mortality but also developmental disabilities.
Trauma
Prevention of childhood neurological injuries includes a wide range of measures that have been shown to be effective in developed countries. Notable examples are seat belts, helmets designed for bicycling and certain sports, side-walks, road safety equipment, education regarding traffic and pedestrian safety, window guards to prevent falls, and playground renovation. Such measures appear to be uncommon in low-income countries, though studies remain to be done in these countries on the incidence of various causes of neurotrauma, on
long-term impacts, and on the use and cost-effectiveness of relevant interventions. Effective strategies are needed for the prevention of intentional causes of injury that can result in developmental disabilities, such as child abuse and war-related trauma.
Secondary Prevention
Opportunities abound for secondary prevention of developmental disabilities in low-income countries through early recognition of potentially disabling conditions and interventions aimed at preventing or minimizing disability. These include early identification and correction of vitamin A deficiency and other forms of malnutrition; PKU screening followed by dietary modifications; accurate and early detection and effective management of bacterial infections that can lead to meningitis or hearing loss [51,54]; effective treatment of malaria; provision of vision and hearing screening, eye and ear care, and refractive and hearing aid services at the primary health care level [15,243,244,245,246,247,248 and 249]; improved access to emergency medical services to prevent trauma-associated disability; and educational interventions to overcome specific learning and sensory disabilities.[51,54,250,251,252,253 and 254]
Children in high-income countries have benefited for decades from interventions such as prenatal and newborn screening, iodine fortification of the food supply, and maternal vaccination to prevent congenital rubella.[223] Recently, antiretroviral therapies have become available in high-income countries to prevent pediatric HIV transmission, but cost barriers prevent access for children at greatest risk in the developing world. Extension of such interventions to low-income countries will be vital to the long-term goal of reducing international inequalities in child health.
Recommendation 5-1. Proven methods of preventing developmental disabilities and enhancing children's functioning should be implemented and expanded in low-income countries. These methods should be tailored to local resources and needs, and should include the following:
-
Nutritional interventions to prevent iodine, vitamin A, iron, and folic acid deficiencies, and to ensure adequate overall nutrition, especially among women of childbearing age, infants, and children.
-
Vaccination to prevent conditions such as congenital rubella, bacterial meningitis, pertussis, diphtheria, tuberculosis, tetanus, and poliomyelitis, and commitment of resources to prevent other infectious diseases, such as pediatric AIDS, malaria, and neuro-cysticercosis (see Annex 5-1 in Chapter 5).
-
Identification of specific causes of adverse perinatal and neonatal outcomes that are amenable to intervention, and evaluation of the effectiveness and cost-effectiveness of alternative interventions in terms of the prevention of developmental disabilities.
-
Prenatal, newborn, and childhood screening for potentially disabling conditions that are amenable to intervention, such as sickle cell disease, hypothyroidism, PKU, and vision and hearing impairments.
-
Early identification and special educational interventions to improve outcomes for children with cognitive disabilities, including specific learning and sensory disabilities.
-
Child injury prevention.
The results of screening will increase recognition of both the impacts of developmental disabilities and the importance of identifying cost-effective interventions. Indicators currently exist for infant, child, and maternal mortality, as well as for numerous other outcomes, bringing visibility to these problems and suggesting priorities for prevention. Comparable indicators are needed for the prevalence of developmental disabilities among surviving children to allow estimates of impact, such as DALYs, which at present cannot be derived for developmental disabilities. Surveillance of developmental disabilities will allow countries to identify locally relevant priorities for prevention, consistent with the risk factor and prevalence patterns of specific populations. Once surveillance data are available, it will be possible to monitor and evaluate trends over time in the prevalence of developmental disabilities, evaluate policies and programs, and identify emerging problems requiring intervention in the future.
Recommendation 5-2. Screening and surveillance of developmental disabilities should be implemented in low-income countries for the purposes of early identification and treatment, as well as generation of the data needed to quantify the prevalence, causes, impacts, and costs of these disabilities.
Rehabilitation
Article 23 of the United Nations Convention on the Rights of the Child states that a child with a disability “should enjoy a full and decent life, in conditions that ensure dignity, promote self-reliance and facilitate the child's active participation in the community. ”[242] Member states are charged to ensure that a child with a disability “receives education, training, health care services, rehabilitation services, preparation for employment and recreation opportunities in a manner conducive to the child's achieving the fullest possible integration and individual development, including his or her cultural and spiritual development.”
While admirable, these goals are ideals yet to be fully realized in any nation. In low-income countries and communities, allocation of the limited resources available for all forms of intervention addressing developmental disorders demands careful consideration and an evidence base that has yet to be developed. Even if rehabilitation proves to be less cost-efficient than primary prevention of disability, however, it is likely to be cost-effective when one considers the benefits of reduced dependency, improved productivity and quality of life, particularly since there are low-cost rehabilitation strategies that can be integrated into comprehensive treatment programs for developmental disabilities in settings where resources are extremely scarce. Though this report focuses on the range of implications of developmental disabilities for children, it is important to note that rehabilitation programs must be extended as well to adult populations that are impaired by these life-long conditions. In many cases, appropriate educational rehabilitation in adults with such conditions as mild mental retardation can vastly increase their ability to function independently and contribute to family and community responsibilities.
Models for Rehabilitation
Multiple models are feasible and may be necessary for providing rehabilitation services to children with developmental disabilities and their families in settings where professional resources are extremely limited. These models include community-based rehabilitation, school-based models, institution- and hospital-based models, and various primary health care models and national strategies.
Community-Based Rehabilitation (CBR). CBR has been defined as a strategy within community development for the rehabilitation, equalization of opportunities, and social integration of all people with disabilities.[255,256] The strategy relies on mobilization of local resources and focuses on families of persons with disabilities as an important resource, seeking to enable people with disabilities and their communities to evolve their own solutions and programs. CBR also aims to eliminate the isolation and stigmatization experienced by people with disabilities, and has as its guiding principal normalization of the lives of people with disabilities and their integration into society. Thus, wherever possible, children should attend normal schools, and the model of institutionalization should be abandoned. Implicit in the CBR approach is the idea that social expectations and environmental constraints contribute to the degree of functional limitation and other consequences experienced by persons with disabilities.[257] This concept is also central to revisions of the Classification of Impairments, Diseases and Handicaps (ICIDHI) currently under consideration.[ 258] The terms “disability” and “handicap,” which have negative connotations, are replaced in the revised ICIDH with “activity” and “participation,” respectively.[259] Thus, the focus has expanded from restoring functions to individuals with disabilities to recognition of the need to change public attitudes and
other contextual factors that limit function. Persons with disabilities are viewed as partners in national development, rather than as a burden on the country's economy. Box 6-1 describes an example of a CBR program in Jamaica.
|
BOX 5-1 Community-Based Rehabilitation in Jamaica 3D Projects, Jamaica's first community-based rehabilitation (CBR) program, began in 1985. At that time, few services for people with disabilities existed outside the capital, Kingston. With continued support from its European donors, the program has gradually expanded, and it is now receiving government support amounting to about 25 percent of the annual budget. In the late 1980s, two other CBR programs, both run by nongovernmental organizations, adopted the 3D model and began providing services elsewhere in the country. By the year 2000, the whole country had CBR coverage, although not all residents with disabilities have yet been reached. The 3D model involves several components, the majority of which are carried out by community personnel, most of whom are parents of children with disabilities. Detection occurs mainly in the community health service in Kingston and in rural hospital clinics, after which children or adults are referred to 3D clinics in the parish for identification and assessment of their disability. There a doctor or nurse practitioner works alongside the community workers using basic assessment devices that have been standardized and validated in an international epidemiological study. An individual program plan is drawn up, and the child is assigned to a community worker in the area where he or she lives. If the child has a developmental disability, the community worker performs a developmental assessment and designs a program of training and, in some cases, physical therapy. The community worker demonstrates the chosen activities to the mother or caregiver, who is then expected to carry out the activities and exercises between weekly visits by the community worker. From time to time the child's progress is reviewed in the clinic. The 3D program also coordinates activities designed to strengthen family and community involvement in rehabilitation, including parent orientation sessions; community workshops; and the training of health care workers, police, social workers, and teachers. An adult/adolescent program, which is mainly prevocational, and a stroke rehabilitation program are also sponsored. The total projected (though not achieved) budget for the four parishes of the 3D program for 1999 was approximately US$500,000. This funding provided for a clientele of approximately 1,000 children and adolescents. In other words, the program costs about US$500 per child per year. Two evaluations of the program have been conducted. |
CBR models emerged in the 1970s, when there was increasing realization of the inadequacy of rehabilitation services in low-income countries, and of the fact that service models from developed countries would never be able to close the gap. Since 1983, WHO has produced detailed training manuals for CBR workers and has promoted CBR as the most appropriate model of rehabilitation for people with disabilities in developing countries.[258,263,264] While the WHO approach to CBR is largely home-based, model center-based approaches have also been developed.[265]
Advantages of the CBR approach are its accessibility to low-income families and reliance on low-cost and locally available resources. Disadvantages include a lack of skilled resources, funding, and time to devote to rehabilitation on the part of family members; difficulty in monitoring quality and outcomes; and isolation and lack of ongoing training and career opportunities for rehabilitation workers. Despite these drawbacks, CBR may be the most viable and cost-effective model for rehabilitative care in developing countries.
The idea that ready-made models for CBR can be implemented throughout the developing world may be naive given the complexity of the problems involved. Interventions must be flexible, sensitive to cultural beliefs, appropriate to the target country's current level of development, and compatible with local development priorities.
School-Based Models. A variety of educational options are available to some extent in developing countries, but for children with disabilities, the choices range from few to none. When available, they range from highly segregated, specialized residential and day schools, to special classes in regular schools, to full mainstreaming or inclusive education. Little information is readily available on the extent to which mainstreaming is practiced in low-income countries. Promotion of this approach began internationally following agreements such as the UNESCO Declaration of Education for All, which stipulates that all countries have a responsibility to provide equal access to education to children with disabilities as an integral part of the education system.[266] It appears likely that CBR and inclusive education are mutually reinforcing, since CBR programs need to place children in regular schools, and teachers find support from CBR workers when they accept children with disabilities.[267] Box 5-2 describes school-based programs and other activities of the Bangladesh Protibondhi Foundation.
|
BOX 5-2 Bangladesh Protibondhi Foundation The Bangladesh Protibondhi Foundation (BPF), a foundation for developmentally disabled children established in 1985, has been a pioneer in the fields of service provision and research for disabled children in Bangladesh. Key activities and achievements include the following. Kalyani Special School. The Kalyani school for children with disabilities (mainly intellectual and motor disabilities) was established in Dhaka. All children are first seen at a clinic, where they undergo a multidisciplinary assessment. Infants can also be enrolled in a mother-child early intervention program. There are special classes for children with cerebral palsy, speech and language problems, and behavioral problems such as autism. Within a sheltered workshop, adolescent boys and girls are taught carpentry, weaving, and painting. An affiliated school serving both disabled and nondisabled children was established to promote mainstreaming. Dhamrai Rural School. In Dhamrai, a rural area 50 km north of Dhaka, the BPF runs a primary school for both normal and intellectually disabled children, who work together in class. There are services for children with motor disabilities and sensory impairments. A mother–child early intervention program is also offered. Parents of disabled children are enrolled in adult literacy programs. Distance Training Packages. The BPF developed these packages for those families who cannot come to a center regularly. The packages consist of pictorial manuals that serve as reminders of the training mothers have received in handling or teaching their young disabled child in various aspects of care, including motor development, speech and communication, cognitive development, and activities of daily living. An evaluation revealed that use of the packages was as effective as regular attendance at a center.[268] Community-Based Rehabilitation. The BPF runs several programs in collaboration with partner organizations, both governmental and nongovernmental, in various districts of Bangladesh. These programs use the TQ (ten questions) and two-phase method of door-to-door screening for disabilities, followed by assessment by a professional team.[269] Institute of Special Education. A postgraduate institute was approved in 1998 by the National University. A 1-year course that leads to a B.Ed, in Special Education is administered through this institute. Department of Special Education, Dhaka University. In 1996, the BPF team founded the first department for training teachers of intellectually, visually, and hearing disabled children within Dhaka University. |
|
Research in Developmental Disabilities. BPF has initiated a rigorous program of research and development in the field of developmental disabilities. This program includes the following:
|
In Zimbabwe, the Ministry of Education has developed a program for disabled children focused on special-needs education, with an emphasis on integrating disabled children into mainstream schools when possible. Assessment offices, staffed by trained educational psychologists, reside in each provincial capital. The psychologist assesses students before they are in special units. The ministry supports both day and boarding special schools for children with physical, visual, and auditory disabilities. For children with mild to moderate learning difficulties, the ministry has established special classes in both primary and secondary schools. In keeping with its policy of integrating disabled children into mainstream schools, the ministry has also created resource units in both primary and secondary schools for children with moderate to severe learning disabilities and visual and hearing impairments.[273] Yet while this system provides good and expanding coverage, the program has not met the demand for places in special education.[ 274]
Reports from some low-income countries indicate that schools do not necessarily have the accessible facilities, trained teachers, or positive attitudes required to accommodate children with disabilities.[ 275] Given the already over-crowded environment of government schools in most low-income countries, a major commitment of resources will be required to accommodate these children.
Institution- and Hospital-Based Models. Institutional care and hospital-based services for children with developmental disabilities are present in many low-income countries, but serve only a small fraction of children with disabilities. There is general agreement among rehabilitation specialists that institutional care is not appropriate and should be discouraged, as it promotes psychological dependency, and prevents children from competing and interacting with their peers and from integrating into society when they eventually leave the institution. Perhaps the strongest argument against the institutional model is the cost and the limited coverage provided. The current monthly expenditure per
child in an institution for disabled children in Harare, for example, is US$80, a figure that exceeds the monthly income of the majority of Zimbabwean families.
Existing institutions can, however, be adapted to play useful supporting roles in community-based approaches. Several Zimbabwean institutions, for example, have incorporated community outreach programs into their activities. Institutions that previously offered long-term residential care have been converted to boarding schools for severely disabled children, who return to their families during school vacations. Institutions can also provide short-term rehabilitation for rural children who require surgery or the fitting of appliances. Hospital rehabilitation departments that traditionally focused on the short-term rehabilitation of patients with an acute disability, particularly those at the district and provincial levels, now provide technical, administrative, and training support to community-based programs through outreach activities. Rehabilitation villages have been constructed in a number of rural hospitals, where disabled children and their caregivers can be accommodated for group activities and workshops.
Primary Health Care Models and National Strategies. There are a number of examples of primary health care models and national strategies for rehabilitation services for addressing developmental disabilities. Selected examples from two countries are given below.
In Zimbabwe, which has an extensive health care system, rehabilitation services have been established at all levels, including among individual communities. Four tertiary and eight provincial-level hospitals are staffed by therapists and rehabilitation technicians, while services at 55 district-level hospitals are provided by rehabilitation technicians who are supervised by therapists at the provincial level. The CBR program operates at a grassroots level and is supported by rehabilitation staff at district hospitals. The rehabilitation technicians, who have received 2 years of generic training in rehabilitation, staff rehabilitation units at the district hospitals and are actively involved in supporting the CBR program at the grassroots level. They have sufficient expertise to bridge the gap between the trained therapists at the provincial level and the village health workers responsible for implementing CBR at the village level.[276] To date, CBR has been introduced in 31 of the 55 districts in Zimbabwe, and three urban programs have been established in Harare and Bulawayo. If expansion continues at the current rate, every district will be covered by 2005.[277] The cornerstone of the Zimbabwean system of rehabilitative care for developmental disorders is the Children's Rehabilitation Unit at Harare Central Hospital (see Box 5-3), which coordinates a variety of services for children with disabilities.
|
BOX 5-3 Children's Rehabilitation Unit, Harare Central Hospital, Zimbabwe The Children's Rehabilitation Unit (CRU) was established in 1986 as a joint project between the Department of Pediatrics, University of Zimbabwe, and the Department of Rehabilitation within the Ministry of Health. The CRU was intended to provide several key services, including coordination of multidisciplinary treatment for children with disabilities and their families; tertiary-level assessment, diagnostic, and treatment planning services for rehabilitation programs at the provincial and district levels, as well as for municipal clinics in urban Harare; training for medical students, therapists, rehabilitation technicians, and nurses in children's disability and rehabilitation; maintenance of a detailed computerized client register and database; and workshops intended to teach parents about their children's specific disorders and to create a sense of common purpose. The multidiscipiinary team that initially staffed the unit consisted of two physiotherapists, an occupational therapist, two speech therapists, two rehabilitation technicians, a social worker, a nursing sister, a pediatrician, and a secretary. Although the program has received some donations from non-governmental organizations, major financial support for the unit is provided by the Ministry of Health through the Harare Central Hospital budget. For more than a decade, the CRU has provided training in childhood disability and community-based rehabilitation (CBR) for health care and rehabilitation staff who rotate through the unit during their courses. As a result of this effort, these subjects now form part of the curricula of nurses, medical students, and postgraduate trainees in pediatrics, as well as trainee therapists. The result has been increased awareness among health professionals of the problems facing children with disabilities and their families and initiatives taking place to address them. The main objective of the CRU is to support the development of CBR. Therefore, as a matter of policy, ongoing therapy is carried out in the community after initial assessment and training at the unit. To this end, 11 outreach groups were established in the impoverished suburbs of Harare. While providing easier access to rehabilitation services, the more important objective of the outreach program is to facilitate the formation of community-based support groups centered on the parents of disabled children. It is hoped that these groups will initiate self-help programs and lobby for disabled children at local government levels. The initiative has led to the establishment of a number of projects, based mainly on handicrafts, that provide mothers with a source of regular income. Five groups have been able to secure funds to build small centers at which they are able to provide day care and preschool facilities for their |
|
children. The CRU continues to visit the groups on a weekly or fortnightly basis to provide rehabilitation services. The CRU staff also organized the Zimbabwe Parents of Handicapped Children's Association, which now has 23 branches throughout the country and more than 4,500 members. The association's main objective is to serve as an advocate for children with disabilities and their families. Instead of placing high priority on the provision of rehabilitation services, however, parents have focused their attention on the social and economic problems affecting their families. Issues such as receiving priority in allocation of housing, obtaining access to special education for their children, developing income-generating projects, and addressing negative family and cultural attitudes toward people with disabilities are high on their agenda. Although the CRU has received regular funding from external donors since its inception, the allocation of resources from the Harare Hospital administration has been sufficient to keep external donor support at a low level. To date, external support for recurrent expenditures has not exceeded US$5,000 per year. However, as support from the hospital has diminished over the last 2 years, it has become increasingly difficult to maintain the unit's activities at present levels. Initial and recurrent funding for planned expansion of the outreach program and the establishment of a resource center for children with disabilities at the unit will have to come from external donor sources, at least until there is a sustained turnaround in the national economy. As a result, service provision is vulnerable to interruptions in donor support. Source: [278] |
In Bangladesh, the Ministry of Social Welfare is mandated to provide services for disabled people. Presently it runs five schools for the visually impaired and seven schools for the hearing impaired. The National Centre for Special Education for children with sensory and intellectual disabilities was started a decade ago. The National Disability Foundation to support development activities for persons with disabilities has also been formed, as have the National Coordination Committee and the National Committee for Inclusive Education. The national policy on disability has been formulated and is expected to be introduced in parliament soon.
Under the Education Ministry, a Department of Special Education within the University of Dhaka was founded in 1995 to train teachers of children with sensory and intellectual disabilities (see Box 5-2). Under the Health Ministry, a Rehabilitation Institute and Hospital for the Disabled provides treatment and rehabilitation services for the physically and orthopedically disabled. The Shishu Bikash Kendro (Child Development Center) of the Dhaka Shishu hospital, an autonomous national institute, was started in 1992, and now has networks in
some other major hospitals within the capital city of Dhaka and other divisional and district towns (see Box 5-4).
|
BOX 5-4 Shishu Bikash Kendro, Child Development and Neurology Unit, Dhaka Shishu Hospital, Bangladesh The Child Development and Neurology Unit began operating in 1992 within the national children's acute care hospital in Dhaka city. It was the first multidisciplinary service in the health sector, with doctors, psychologists, and therapists working as a team to provide services to children presenting with a range of acute and long-standing neurological problems and developmental disabilities. The unit includes the Shishu Bikash Kendro (SBK), or Child Development Centre; an inpatient neurology ward; and the Agargaon Community Project, which provides child development and therapy services to an adjacent, economically deprived population. Cerebral palsy, epilepsy, and developmental delay are the three major diagnoses made in the unit. To prioritize rehabilitation needs, each child is categorized for type and severity of specific functional disabilities. While motor disability is the most frequent presenting complaint, perhaps because it is so obvious to parents, other disabilities are also presented in a significant number of children. In 1996, to overcome the problems resulting from the lack of any pediatric therapist within the country, the SBK started to train college graduates in certain aspects of the three major therapies (occupational therapy, physiotherapy, and speech and language therapy). The trainees have evolved to become developmental therapists. A diploma course in developmental therapy is now being planned in collaboration with the Institute of Special Education, Bangladesh Protibondhi Foundation (see Box 5-2). The provision of epilepsy services has been another emphasis of the center. Certain diagnostic and treatment issues have emerged during the course of service development. While early diagnosis of treatable seizure disorders remains a problem because of the unavailability of accessible services and a lack of parental awareness, many children are being given medication for their “seizures” without a valid diagnosis. Diagnostic services have been strengthened by the development of the first pediatric electroencephalogram (EEG) services in Bangladesh by the SBK. Of 1,000 children presenting to EEG services with a diagnosis of seizure disorders (55 percent of whom were referred from other institutions and practitioners), over 50 percent did not have a seizure disorder. All these children had been on long-term medication with anti-epileptic drugs. Therefore, overmedication of very young children who may not have epilepsy is a common practice being addressed by the SBK. |
|
The SBK also provides psychological services. Developmental psychologists see children with a range of cognitive, behavioral, and psychosocial problems. Child protection issues have emerged from this service as an aspect of children's development in which social support is required. Counseling for distressed children and families is also emerging as an important service. The SBK runs regular courses in family counseling jointly with other organizations, and also with a psychotherapist in the Psychiatric Department of Bangabandhu Sheikh Mujib Medical University. A pediatric clinical psychology service is also run biweekly by students in the Department of Clinical Psychology, Dhaka University. A range of standardized, cognitive, and developmental tests are being developed within this service. After finding that access to services by the poorest families living close to the Shishu Hospital was limited, largely because of poor attitudes and behavior among service providers within the hospital, the SBK established the Agargaon Community Project. The project undertakes screening for childhood disability in door-to-door surveys and has led a campaign to promote optimum child development. An information booth staffed by a community health visitor and a part-time physician was constructed within the general outpatient department of the hospital. In addition to referral for rehabilitation services, the project assists with the placement of children in local schools and provides family planning and other medical and social services. Very insignificant amounts of money have been spent on infrastructure for the services provided, such as construction of office space and equipment, because all the services were developed within well-established public health institutions at little extra cost. These modest costs are borne by each institution. Most of the necessary equipment, such as toys, assessment kits, and testing materials, has been purchased or made locally. Human resource development was the area in which the greatest investment had to be made. The SBK has been in active collaboration with academic institutions in the United Kingdom through an Academic Link Program. Through this program, several personnel have been trained in the United Kingdom, and U.K. professionals have visited Bangladesh to provide training to others. As the field of developmental therapy has yet to be acknowledged in Bangladesh and the posts are ad hoc, funding for monthly remuneration has been obtained from local businesspeople who have been convinced about the benefits of the services provided. Demands for SBK services have increased. Efforts are currently under way, both within Dhaka and nationally, to adapt and replicate the services. |
Nongovernmental organizations play a major role in developing services for disabled children in Bangladesh. The National Forum of Organizations Working with the Disabled coordinates the activities of organizations that work with all kinds of disabilities in both children and adults. At present, 80 organizations are active members of the forum. And the Bangladesh Scouts and Girls in Scouting have established open groups for disabled children so that even those children not enrolled in regular schools can form groups to become members.
Bangladesh is an active member of the South Asian CBR Network. A South Asian Assistance for Regional Cooperation (SAARC) Centre for the Disabled has also been recently established. Bangladesh has proposed a SAARC Disability Fund that has been accepted and is awaiting implementation. Bangladesh is also a member of the Special Olympics, and its participants have won several prizes in the past few years in various athletic events.
Barriers to Implementation
There are a number of barriers to the implementation of rehabilitation programs for children with developmental disabilities in low-income countries.
Lack of Program Funding. The costs of sustaining programs, failure to generate adequate government support, and a scarcity of trained or available professionals are major barriers to the expansion of rehabilitation programs for children with disabilities in low-income countries. In addition, the view is widely held that it is not worth spending money on children who, it is believed, are likely always to be dependent.
Negative Styles of Communication in Health Services. The experience of parents with health services is another major inhibiting factor. A survey in Jamaica showed that parents found the information given them by health personnel (mainly doctors and nurses) too vague or too difficult to understand. They therefore had unrealistic ideas and stopped going to clinics. Most of the problems stemmed from poor communication related to a lack of training in disability issues, lack of a sense of responsibility for the care of children with disabilities, and inappropriate communication styles.
Impact of Cultural Practices. An ethnographic study in Jamaica noted several childrearing practices that could have a negative effect on children with disabilities.[ 40] These included the use of corporal punishment to discipline a child and restrictions placed on the movement of children outside the home, especially girls; withdrawal of food as another form of punishment; and limited use of praise, for it is believed to make the child conceited.
Structure of Medical Services. Medically oriented paradigms, which have been followed thus far in undergraduate and postgraduate medical curricula in low-income countries to resolve all issues related to health, may be a key impediment to the provision of services for children with developmental disabilities in some countries. Most health programs are hierarchical, with the physician
acting as the chief decision maker for any health team. This has been a barrier to the development of multidisciplinary teams in which each professional has a key role to play. In addition, negative attitudes and behavior on the part of health professionals have repeatedly been cited by those seeking care as barriers to their using services or seeking help in established centers.[273] Another impediment is a lack of accountability. People want service from someone they can come to repeatedly, or the same person visiting their homes. In public health institutions, where personnel are often temporary, this is not possible.
Poverty and Sparse Services Only in Major Cities. Distance from services has been cited as a key deterrent to the use of services, as money and resources are required to travel and stay overnight in a large town or city.[274] In addition, lack of pharmaceuticals at primary health care centers is cited by parents as a reason for not coming to these centers for child health and disability prevention services.[274] The cost of medicine has been given as a reason for lack of adherence to treatment for children requiring regular medication for epilepsy, while the cost of diagnostic services has been quoted as exorbitant, with public hospitals not investing in quality diagnostic services at subsidized costs.
Recommendation 5-3. It is apparent from the multitude of highly prevalent diseases and common environmental factors that contribute to or increase the risks for developmental disabilities, that recognition of these disabilities must become a public health priority in developing countries. Inclusive educational policies at both the national and local levels should be implemented to ensure that all children, including those with disabilities, have access to appropriate schooling. Resources must be provided in developing countries for special training and support of teachers in the recognition and teaching of children with developmental disabilities, including mental retardation and specific learning disabilities. Proven interventions detailed in the report for the prevention and treatment of causative factors for developmental disabilities should be implemented through community-based demonstration projects and subsequently adapted to meet the local needs of the communities they serve.
Cost Analysis
Cost-effectiveness studies have been done for interventions in low-income countries that target some of the causes of developmental disabilities, interventions such as malaria prophylaxis, micronutrient supplementation and fortification, and immunization programs.[278,279 and 280] These studies have shown the interventions to be highly cost-effective in terms of their impacts on child mortality and morbidity, though they do not incorporate estimates of the number
of years of disability potentially prevented.[278] Nonetheless, if an intervention is shown to be cost-effective even when the benefit of preventing long-term disability is not accounted for, the existing evidence for cost-effectiveness may be considered a lower-bound estimate of the intervention's true cost-effectiveness.
In general, when the full direct and indirect costs to individuals and society of disabilities arising early in life are considered, cost-effectiveness should be relatively easy to achieve for interventions that are effective in preventing developmental disabilities and improving children's functioning and self-sufficiency. Yet specific evidence regarding the cost-effectiveness of preventing developmental disabilities in low-income countries is lacking. Measures of the costs and benefits of rehabilitation of developmental disabilities are particularly difficult to obtain.
The cost-effectiveness of newborn screening in general is dependent on the frequency and severity of the conditions being screened for; the effectiveness of early (newborn) identification and treatment; and the availability of laboratory facilities for testing and confirmation, genetic counseling, treatment, and follow-up services. Newborn screening requires a government commitment and regulation and should include all births unless clear risk categories can be identified and subpopulations targeted. Quality control to maintain high accuracy of screening and confirmatory test results is crucial. It is usually necessary for the laboratory infrastructure and procedures for newborn screening to be centralized. A regional center for medical genetics is necessary to provide the laboratory infrastructure for newborn screening, confirmation of diagnoses, counselling, treatment, and follow-up of cases. A cost-effective strategy may be the regional development of networks of laboratories that complement each other and cover very large populations of one or more countries.[281]
The decision whether to develop a newborn screening program and for which conditions will vary from country to country. Conditions with high priority for newborn screening should be clinically severe and relatively frequent, capable of early detection and diagnosis with simple and low-cost methods, and amenable to treatment that will be most beneficial if initiated immediately after birth.
CAPACITY
Training and expertise are needed at all levels of health care, as well as in the educational and research sectors, to address the issues and recommendations included in this chapter. Training in these areas not only produces specialists who can appropriately diagnose and treat developmental disabilities, but also provides the knowledge required to train health care personnel at all levels with the skills required for intervention.[282,283,284,285,286,287,288,289,290,291,292 and 293] Major areas of importance include, but are not limited to, the following training programs:
Research training programs
-
These programs are needed to ensure the availability of adequate numbers of researchers to carry out policy, clinical, and basic research relevant to the prevention and rehabilitation of developmental disabilities in low-income countries. Areas of training for this research would include but not be limited to immunology; medical genetics; pathology; child psychology; psychiatry and neurology; neurosciences; nutrition; pediatrics; audiology; ophthalmology; epidemiology; biostatistics; and health services management, research, and policy.
Regional rehabilitation training programs
-
Such programs are necessary to produce cadres of rehabilitation workers, and to provide continuing education focused on CBR and other therapeutic interventions as well as on appropriate referrals for children with disabilities. Certificate and degree programs should be designed that are relevant to local needs and cultural contexts. Programs that might be included are developmental psychology, audiology, speech and language therapy, orthopedics, prosthetics, occupational therapy, and physical therapy.
Clinical training programs
-
These programs are needed to provide expertise in areas vital to the prevention of and additional research on developmental disabilities. These programs should include pediatrics, pediatric neurology, neonatology, psychiatry, optometry, ophthalmology, obstetrics, midwifery, infectious disease control, diagnostic imaging, and nutrition.
Special education training programs
-
Such programs are required to train cadres of teachers working in low-income countries in the recognition and teaching of children with special educational needs due to low cognitive abilities; specific learning disabilities; and vision, hearing, and behavioral disorders. These skills would require training in areas such as child development and special education.
Most of the immediate responsibility for prevention, early intervention, and rehabilitation occurs at the primary health care/community level. However, the range of services that can be made available, the training of health care workers, and access to more complex diagnostic and therapeutic help when needed all improve significantly when the primary care system is linked integrally to a regional or national center (see Chapter 3). Additionally, the research that is needed to further improve services often requires community participation.
While each country should develop a rehabilitation strategy suited to its own needs and development priorities, it is necessary to seek areas of conver-
gence in which outside agencies can assist countries in the implementation of their rehabilitation programs. An obvious field for cooperation is in capacity building, particularly in the areas of training, research, and infrastructural development. This cooperation might be facilitated on a regional level through the establishment of regional training and research centers. These centers could provide training for rehabilitation staff, and assist regional governments in the development of rehabilitation programs by supporting operational research and funding infrastructure development. In the longer term, research efforts might focus on the development of strategies for prevention.
Training initiatives should be given priority to provide a foundation of skilled staff that can support the development of rehabilitation services. In establishing training courses, careful consideration should be given to the development of appropriate curricula. Consideration should also be given to reviewing the existing curricula of degree courses for therapists with a view to making them more relevant to local needs. The courses should be modified to provide broader training in rehabilitation and to include training in community development. Box 5-5 reviews some of the consequences of using a curriculum that has not been adapted to the context of developing countries.
Finally, qualified therapists are often reluctant to leave urban areas to live and work in remote rural locations. They may opt instead to leave government employment and work in the private sector, where conditions and remuneration are usually superior.
|
BOX 5-5 Importance of Contextually Appropriate Training Professionals currently responsible for the delivery of rehabilitation services in the majority of African countries are graduates of Western universities or have graduated from local universities whose curricula have been adapted from Western models. This has a number of consequences. First, Western curricula train therapists in only one aspect of rehabilitation, e.g., speech therapy. This restricts the usefulness of the curricula in the context of developing countries. Therapists are often overqualified for the tasks they are expected to perform, and the sophisticated equipment used in modern therapy is seldom available. Moreover, it is necessary to employ three therapists at each site to provide comprehensive service, and this adds considerably to costs. Second, conventional training does not equip graduates with the skills needed to mobilize communities and develop sustainable community-based programs. |
Recommendation 5-4. Training programs should be established to develop expertise in low-income countries in areas vital to the prevention and treatment of developmental disabilities and to the provision of effective rehabilitation services as detailed in the above descriptions.
Currently, disability prevention and rehabilitation specialists and workers in developing countries are isolated, and could benefit from opportunities to interact and exchange information with colleagues in similar but geographically distant contexts. The Internet could offer a low-cost means of facilitating this communication, but support is needed for the development and maintenance of the necessary information systems and for the purchase of the hardware needed to connect sites throughout the world. The Internet could serve as a relatively low-cost means of linking rehabilitation programs at multiple sites throughout the world. It could also provide information resources and continuing education, as well as opportunities for professional exchange and contact.
Recommendation 5-5. Internet capabilities should be developed and maintained to facilitate international communication among those involved in the implementation of primary prevention and rehabilitation programs for children with developmental disabilities in low-income countries.
Essential to the provision of adequate services for children and the prevention of developmental disabilities is a universal policy of adequate and sustained primary health care that will be health promotive, disease preventive, curative, and rehabilitative. Exemplary programs include under-five clinics [294,295 and 296] that provide immunization; nutrition and growth assessment; developmental, vision, and hearing screening; health education; and identification of risk factors for disabilities. Children are seen by primary health workers in these clinics regularly and frequently for monitoring and treatment. The success of these clinics requires adequate supplies of essential medications. Findings and progress are recorded on a home-based child health record, with growth charts being kept by mothers. Appropriate referrals are made for treatment and rehabilitation when indicated. This approach has been shown to be highly effective against child mortality and has also resulted in significantly accelerated motor development [282]; however, research is needed regarding its effects on other developmental parameters.
Strengthening and further development of the infrastructure and capacity of maternal and child health services are needed to ensure that the prevention of developmental disabilities is integral to the goals and activities of these services. Specific activities to be incorporated include nutritional supplementation; food fortification; immunization; antiparasitic prophylaxis; educational and counseling programs relevant to the prevention of nutritional, infectious, environmental,
and genetic causes of developmental disabilities; prenatal and newborn screening for developmental disabilities, followed by relevant interventions; and referral of infants and young children with disabilities or at risk for disability to rehabilitation programs or other educational or therapeutic interventions to prevent or minimize disability. In addition, support is needed for locally relevant and appropriate rehabilitation programs, linked to primary health care, to which children with developmental disabilities and their caretakers can be referred to ensure that they achieve their potential in terms of function, independence, productivity and quality of life.
Recommendation 5-6. In the context of the successes of current primary health care child survival initiatives, it is essential in low-income countries that increased emphasis be placed on prevention and early identification of developmental disabilities within the primary and maternal and child health care systems. Those systems must in turn be linked to and supported by secondary and tertiary medical services. Additionally, to provide appropriate guidance to those in need of rehabilitation services for developmental disabilities, primary and maternal and child health care systems should be linked to local rehabilitation programs.
Recommendation 5-7. The capacity for relevant evidence-based research should be developed. As recommended earlier in this report, national centers for training and research based in low-income countries can play an essential role in establishing this capacity (see Chapter 4). The role of these centers should include conducting clinical and community trials through demonstration projects to test the effectiveness of interventions in the prevention of developmental disabilities as well as training personnel to implement prevention and intervention strategies. The capacity of these centers should be further advanced through collaboration and communication with other centers in both the developing world and in high-income countries. For developmental disabilities, collaboration is recommended with such existing organizations as UNICEF, Save the Children, Rehabilitation International, the U.S. National Institute of Child Health and Human Development, the U.S. Centers for Disease Control and Prevention, the U.S. National Institute of Mental Health, the World Health Organization Expanded Program on Immunization, the World Health Organization Prevention of Blindness and Deafness Program, and the Commonwealth Association for Mental Handicap and Developmental Disabilities.
Recommendation 5-8. Based on the findings of studies regarding the etiology, risk factors, and interventions for developmental disabilities presented earlier in this chapter, some specific areas of research for national centers for training and research might include the following:
-
The cost-effectiveness of prenatal and newborn screening in specific settings.
-
The reliability, validity, and feasibility of surveillance methods and information systems.
-
Models for extending effective rehabilitation for children with developmental disabilities in low-income countries.
-
Nervous system sequelae of cerebral malaria and their prevention.
-
The cost-effectiveness of specific nutritional interventions for the prevention of developmental disabilities. These include interventions such as salt iodination; vitamin A, folate, and iron food fortification and supplementation; and education about local food sources.
-
The cost-effectiveness of methods for the prevention of prevalent infections that result in developmental disabilities, including vaccination and/or prophylaxis for such diseases as congenital rubella, Haemophilus influenzae Type b meningitis, measles, and malaria.
-
The etiology and prevention of adverse pregnancy outcomes, such as maternal morbidity and mortality, low birth weight, intrauterine growth restriction, and premature birth and birth defects with an emphasis not only on maternal and infant survival, but also on the prevention of developmental disabilities.
-
The impact of maternal education, injury-prevention public awareness programs, and alleviation of poverty on the prevention of developmental disabilities.
-
Methodological and prevalence studies to ensure that developmental disabilities are effectively represented by DALYs or other measures of impact so that the costs and effects of these disorders can be appropriately measured.
CONCLUSION
Epidemiological studies have provided some basic knowledge about developmental disabilities in low-income countries, including evidence of relatively high population frequencies, the contribution of various causes, and prospects for prevention. While the data are, on the whole, extremely limited, the prevalence of many of the specific causes of developmental disabilities (including genetic, nutritional, infectious, and traumatic causes) appears to be elevated in
low-income countries, and many of these causes are preventable. Educational and rehabilitation interventions can help minimize disability and maximize the function of children with developmental disabilities. Nonetheless, few resources are devoted to relevant programs for children with developmental disabilities in low-income countries. The number of children with disabilities and at risk for developmental disabilities in low income countries is huge, as are the impacts of disability on national economies and quality of life. Yet the capacity for prevention, treatment, and rehabilitation is insufficient. The need to reduce the prevalence of developmental disabilities in the developing world is urgent and calls for innovative and sustained public health efforts and financial commitments.
REFERENCES
1. World Health Organization (WHO). ICD-10:International statistical classification of diseases and related health problems. 10th revision. World Health Organization: Geneva, 1992.
2. M. Procopio and P.K. Marriott. Seasonality of birth in epilepsy: A Danish study. Acta Neurologica Scandanavica. Nov;98(5):297–301, 1998.
3. K.L. Kwong, S.N. Wong, and K.T. So. Epilepsy in children with cerebral palsy. Pediatric Neurology Jul;19(1):31–36, 1998.
4. M. Procopio, P.K. Marriott, and P. Williams. Season of birth: Aetiological implications for epilepsy. Seizure Apr;6(2):99–105, 1997.
5. C. Garaizar and J.M. Prats-Vinas. Brain lesions of perinatal and late prenatal origin in a neuropediatric context. Review of Neurology Jun;26(154):934–950, 1998.
6. P. Pitche, A.D. Agbere, A.J. Gbadoe, A. Tatagan, and K. Tchangai-Walla. Bourneville's tuberous sclerosis and childhood epilepsy Apropos of 4 cases in Togo. Bulletin of Social Pathology Exot 91(3):235–237, 1998.
7. T.D. Cannon, I.M. Rosso, C.E. Bearden, L.E. Sanchez, and T. Hadley. A prospective cohort study of neurodevelopmental processes in the genesis and epigenesis of schizophrenia. Developmental Psychopathology Summer;11(3):467–485, 1999.
8. L.A. Rosenblum and M.W. Andrews. Influences of environmental demand on maternal behavior and infant development. Acta Paediatrica Supplement Jun;397:57–63, 1994.
9. S.E. Arnold. Neurodevelopmental abnormalities in schizophrenia: Insights from neuropathology. Development and Psychopathology Summer; 11 (3):439–456, 1999.
10. I.M. Sawhney, A.V. Subrahmanyan, C.P. Das, N. Khandelwal, H. Sawhney, and K. Vasishta. Neurological complications of eclampsia. Journal of Associate Physicians of India. Nov;47(11):1068–1071 1999.
11. D. Rice and S. Barone Jr. Critical Periods of Vulnerability for the Developing Nervous System: Evidence from Humans and Animal Models. Environmental Health Perspectives Jun;108(3):511–533, 2000.
12. S.A. Kirk. Educating Exceptional Children. Houghton Mifflin: Boston, 1962.
13. J.P. Heldt and I.F. Wessels. Community eye care 10 years after Alma Ata: Progress, problems, and priorities for private voluntary organizations in developing nations . Ophthalmic Surgery Jan;19(1):47–55, 1998.
14. L. Schwab and K. Kagame. Blindness in Africa: Zimbabwe schools for the blind survey. British Journal of Ophthalmology Jul;77(7):410–412, 1993.
15. J. Silver, C.E. Gilbert, P. Spoerer, and A. Foster. Low vision in east African blind school students: Need for optical low vision services. British Journal of Ophthalmology Sep;7(9):814–820, 1995.
16. N. Zerihun and D. Mabey. Blindness and low vision in Jimma Zone, Ethopia: Results of a population-based survey. Ophthalmic Epidemiology Mar;4(1):19–26, 1997.
17. S.N. Nwosu. Ocular problems of young adults in rural Nigeria. International Ophthalmology 22;(5):259–263, 1998.
18. A.D. Negrel, Z. Avognon, D. C. Minassian, M. Babegbeto, G. Oussa, and S. Bassabi. Blindness in Benin. Marseille médical 55(4 Pt 2):409–414, 1995.
19. N. Richman. After the flood. American Journal of Public Health, 83(11):1522–1524, 1993.
20. M.S.Durkin, N. Khan, L.L Davidson, S.S. Zaman, Z.A. Stein. Effects of a natural disaster on child behavior: Evidence for posttraumatic stress. American Journal of Public Health, 1993; 83(11):1549–1553.
21. E.B. Hook. Incidence and prevalence as measures of the frequency of birth defects American Journal of Epidemiology 116:743–747, 1982.
22. L.A. Suzuki and R.R.Valencia. Race-ethnicity and measured intelligence: Educational implications American Psychologist 52(10): 1103–1114, 1997.
23. G. Altar and J.C. Riley. Frailty, sickness and death: Models of morbidity and mortality in historical populations. Population Studies 43:25–45, 1989.
24. M. Kramer. The rising pandemic of mental disorders and associated chronic diseases and disabilities. Acta Psychiatrica Scandinavica 62(supplement):282–297, 1980.
25. S.J. Olshansky, et al. Trading off longer life for worsening health: the expansion of morbidity hypothesis. Journal of Aging and Health 3:194–216, 1991.
26. H.G. Birch, S.A. Richardson, D. Baird et al. Mental Subnormality in the Community: A Clinical and Epidemiologic Study. Williams and Wilkins: Baltimore, 1970.
27. F. Diaz-Fernandez. Descriptive epidemiology of registered mentally retarded persons in Galicia (northwest Spain). American Journal of Mental Retardation 92(4):385–392, 1988.
28. M.S. Durkin, Z.M. Hasan, and K.Z. Hasan. Prevalence and correlates of mental retardation among children in Karachi, Pakistan. American Journal of Epidemiology 147(3):281–288, 1998.
29. T. Fryers and R.I. Mackay. The epidemiology of severe mental handicap. Early Human Development 3:277–294, 1979.
30. K.H. Gustavson, B. Hagberg, G. Hagberg, and K. Sars. Severe mental retardation in a Swedish county. 1. Epidemiology, gestational age, birth weight and associated CNS handicaps in children born 1959 –1970. Acta Paediatrica Scandinavica 66:373–279, 1977.
31. Z. Hasan and A. Hasan. Report on a population survey of mental retardation in Pakistan. International Journal of Mental Health 10:23–27, 1981.
32. A.D. McDonald. Severely retarded children in Quebec: Prevalence, causes and care American Journal of Mental Deficiency Research 78:205–215, 1973.
33. P.C. McQueen, M.W. Spence, J.B. Garner, L.H. Pereira, and E.J.T. Winsor. Prevalence of major mental retardation and associated disabilities in the Canadian maritime provinces. American Journal of Mental Deficiency 91(5):460–466, 1987.
34. C.C. Murphy, M. Yeargin-Allsopp, P. Decoufle, and C.D. Drews. The administrative prevalence of mental retardation in 10-year-old children in metropolitan Atlanta, 1985 through 1987. American Journal of Public Health 85(3):319–323, 1995.
35. H.S. Narayanan. A study of the prevalence of mental retardation in southern India International Journal of Mental Health 10:28–36, 1981.
36. C. Peckham and R. Pearson. The prevalence and nature of ascertained handicap in the National Child Development Study (1958 cohort). Public Health 90:111–121.
37. M. Rutter, J. Tizard, and K. Whitmore, eds. Education, Health and Behaviour. Longman: London, 1970.
38. Y. Shiotsuki, T. Matsuishi, K. Yoshimura, F. Yamashita, K. Yano, H. Tokimasa, et al. The prevalence of mental retardation in Kurume City. Brain Development 6:487–490, 1984.
39. Z.A. Stein. M.W. Susser, G. Saenger, and F. Marolla. Mental retardation in a national population of young men in The Netherlands: 1. Prevalence of severe mental retardation. American Journal of Epidemiology 103:477–489, 1976.
40. M. Thorburn, P. Desai, T. J. Paul, L. Malcolm, M. Durkin, and L. Davidson. Identification of childhood disability in Jamaica: The ten question screen. International Journal of Rehabilitation Research 15:115–127, 1992.
41. S.S. Zaman, N.Z. Khan, M.S. Durkin, and S. Islam. Childhood Disabilities in Bangladesh. Protibondhi Foundation: Dhaka, 1992.
42. Q.H. Zuo, X.Z. Zhang, Z. Li, Y.P. Qian, X.R. Wu, Q. Lin, et al. An epidemiological study on mental retardation among children in Chang-Qiao area of Beijing. Chinese Medical Journal 99(1):9–14, 1986.
43. B. Thylefors, A.D. Negrel, R. Pararajasegaram, and K.Y. Dadzie. Global data on blindness. Bulletin of the World Health Organization 73(1):115–121, 1995.
44. World Health Organization. Vision 2020: The Right to Sight. Program for the prevalence of blindness, 1997. Available online: www.who.int/pbd/Vision2020.
45. A. Adeoye. Survey of blindness in rural communities of south western Nigeria Tropical Medicine and International Health Oct. 1(5):672–676, 1996.
46. WHO, WHA, Prevention of hearing impairment: Resolution of the 8th World Health Assembly, 48.9, 1995.
47. G.T. Mencher. Challenge of epidemiological research in the developing world: Overview Audiology Jul–Aug; 39(4):178–183, 2000.
48. World Health Organization. Report of a WHO workshop in Nairobi (Octorber 1995): Prevention of hearing impairment in Africa in Nairobi, Kenya. October, 24–27, 1995 (WHO?PDH/96.3/AFR/NCD/96.1). Brazzaville, 1996.
49. S. Prasuansuk. Otological centre: Bangkok unit, prevention of hearing impairment and deafness. Hearing International 6(4):16–17, 1997.
50. P. Ratnesar. Surveying the prevalence of hearing impairment in school children in central Sri Lanka. Hearing International 4(3):11, 1995.
51. S. Kumar. Deafness and its prevention—Indian scenario. Indian Journal of Pediatrics. Nov–Dec;64(6):801–809, 1997.
52. People's Daily, China, October 20, 1990.
53. B. McPherson and C.A. Holborow. A study of deafness in West Africa: The Gambian hearing health project International Journal of Pediatrics and Otorhinolaryngology 10,115–135, 1985.
54. B. McPherson and S.M. Swart. Childhood hearing loss in sub-Saharan Africa; A review and recommendations International Journal of Pediatrics and Otorhinolaryngology May 4;40(1):1–18, 1997.
55. D.R. Seely, S.S. Gloyd, A.D. Omope Wright, and S.J. Norton. Hearing loss prevalence and risk factors among Sierra Leonean children Archives of Otolaryngology—Head & Neck Surgery 121,853–858, 1995.
56. P. Little, A. Bridges, R. Guragain, D. Friedman, R. Prasad, and N. Weir. Hearing impairment and ear pathology in Nepal. Journal of Laryngology and Otology May;107(5): 395–400, 1993.
57. A.W. Smith, J. Hatcher, I.J. Mackenzie, S. Thompson, I. Bal, I. Macharia, et al. Randomized controlled trial of treatment of chronic suppurative otitis media in Kenyan schoolchildren. Lancet 348:1128–1133, 1996.
58. J.O. Klein. The burden of otitis media. Vaccine Dec8;19(supplement) I:S2–S8, 2000.
59. Prevention of Hearing Impairment from Chronic Otitis Media, Report of a WHO/CIBA Foundation Workshop. November 19–21, WHO/PDH 98.4. Geneva, 1998.
60. A.B. Chukuezi. Profound and total deafness in Owerri, Nigeria. East African Medical Journal Nov;68(11):905–912, 1991.
61. P.W. Alberti. The prevention of hearing loss worldwide. Scandinavian Audiology 25(supplement 42),15–19, 1996.
62. A. Smith and J. Hatcher. Preventing deafness in Africa's children. Africa Health Nov; 33–35, 1992.
63. P.O. Pharoah, T. Cooke, M.A. Johnson, R. King, and L. Mutch. Epidemiology of cerebral palsy in England and Scotland, 1984–1989. Archives of Disease in Childhood. Fetal and Neonatal Edition. 79(1):21–25, 1998.
64. J.M. Liu, S. Li, Q. Lin, and Z. Li. Prevalence of cerebral palsy in China. International Journal of Epidemiology 28(5):949–954, 1999.
65. A. Kavcic and M. V. Perat. Prevalence of cerebral palsy in Slovenia: Birth years 1981 to 1990 Developmental Education and Child Neurology 40(7):459–463, 1998.
66. C. Sciberras and N. Spencer. Cerebral palsy in Malta 1981 to 1990. Developmental Medicine and Child Neurology 41(8):508–511, 1999.
67. M.G. Rosen and J.C. Dickinson. The incidence of cerebral palsy. American Journal of Obstetrics and Gynecology 167:417–423, 1992.
68. S. Razdan, R. L. Kaul, A. Motta, S. Kaul, and R.K. Bhatt. Prevalence and pattern of major neurological disorders in rural Kashmir (India) in 1986. Neuroepidemiology 13(3):113–119, 1994.
69. Initial Demographic Study. A review of the available data on the visually disabled population Royal National Institute for the Blind: London, 1985.
70. N. Cohen, H. Rahman, J. Sprague, M. Jahl, E. Laembujis. and M. Mitra. Prevalence and determinants of nutritional blindness in Bangladeshi children. World Health Statistics Quarterly 38:317–329.
71. E. Brilliant. The epidemiology of blindness in Nepal. The Seva Foundation: Berkeley, CA, 1988.
72. World Health Organization: Available data on blindness (Update 1987) WHO: Geneva, WHO/PBL/87.14, 1987.
73. H. Faal, D. Minassian, S. Sowa, and A. Foster. National survey of blindness and low vision in the Gambia: Results British Journal of Ophthalmology 73:82–87, 1989.
74. World Health Organization (WHO). World Prevalence of Blindness. http//:www.who.int/pbd/Vision2020/V2020slides/sld004.htm., 2000.
75. C. Gillberg and M. Coleman. The biology of the autistic syndromes, 2nd edition. Mac Keith Press: London, 1992.
76. E.R. Ritvo, B. J. Freeman, C. Pingree A. Mason-Brothers, L. Jorde, W.R. Jenson, et al. The UCLA-University of Utah epidemiologic survey of autism: Prevalence American Journal of Psychiatry 146:194–199, 1989.
77. I. Rapin. Austism. New England Journal of Medicine Jul 10;337(2):97–104, 1997.
78. P. Szatmari. The epidemiology of attention deficit hyperactivity disorder. Child and Adolescent Clinics of North America 1:361–371, 1992.
79. A. Adeloye. Sickle-cell anaemia. British Medical Journal May 5;2(861):304, 1973.
80. U. Omanga, D. Shako, M. Ntihinyurwa, and M. Mashako. [Cerebrovascular occlusion in children with sickle cell anemia seen in Kinshasa, Zaire (author's transl)]. Annal of Pediatrics (Paris). May;29(5):371–374, 1982.
81. M.T. Obama, L. Dongmo, C. Nkemayim, J. Mbede, and P. Hagbe. Stroke in children in Yaounde, Cameroon. Indian Pediatrics Jul;31(7):791–795, 1994.
82. A. Adeloye and E.L. Odeku. The Nervous System in Sickle Cell Disease. African Journal of Medical Sciences Jan;1(1):33–48, 1970.
83. R.G. Steen, X. Xiong, R.K. Mulhern, J.W. Langston, and W.C. Wang. Subtle brain abnormalities in children with sickle cell disease: Relationship to blood hematocrit. Annals of Neurology Mar;45(3):279–286, 1999.
84. A. Drugan, Y.Yaron, R. Zamir, S.A.D. Ebrahim, M.P. Johnson, and M.I. Evans. Differential Effect of Advanced Maternal Age on Prenatal Diagnosis of Trisomies 13, 18, and 21. Fetal Diagnosis and Therapy 14:181–184, 1999.
85. M. Khlat and M. Khoury. Inbreeding and diseases: Demographic genetic and epidemiologic perspectives Epidemiology Review. 13:28–41, 1991.
86. A. H. Bittles, W.M. Mason, J. Greene, and N.A. Rao. Reproductive behavior and health in consanguineous marriages. Science 252: 789–794, 1991.
87. M. Khlat. Endogamy in the Arab World. In: A.S. Teebi and T.I. Farag, eds. Genetic Disorders Among Arab Populations. Oxford University Press: New York, Oxford, 1997.
88. M.S. Durkin, Z.M. Hasan, and K.Z. Hasan. Prevalence and correlates of mental retardation among children in Karachi, Pakistan. American Journal of Epidemiology Feb 1;147(3):281–288, 1998.
89. M.M. Mokhtar, S.M. Kotb and S.R. Ismail. Autosomal recessive disorders among patients attending the genetics clinic in Alexandria. Eastern Mediterranean Health Journal 4(3):470–479, 1998.
90. A.R.R. Devi, N.A. Roa, A.H.Bittles. Inbreeding and the incidence of childhood genetic disorders in Karnataka, south India. Journal of Medical Genetics 24: 362–365, 1987.
91. S. Bundey and H. Alam. A five-year prospective study of the health of children in different ethnic groups, with particular reference to the effect of inbreeding European Journal of Human Genetics 1(3): 206–219, 1993.
92. L. Jaber, G. J. Halpern, and M. Shohat. The impact of consanguinity worldwide. Community Genetics 1:12–17, 1998.
93. World Health Organization (WHO). Report of the WHO Scientific Group. Control of Hereditary Diseases: WHO Technical Report Series 865, Geneva, 1996.
94. M.C. Braga, P.A. Otto, and O. Frota-Pessoa. Calculation of recurrence risks for heterogeneous genetic disorders American Journal of Medicine and Genetics Nov6;95(1):36–42, 2000.
95. S.M. Zakzouk. Epidemiology and etiology of hearing impairment among infants and children in a developing country. Part I. Journal of Otolaryngology Oct;26(5):335–344, 1997.
96. ICMR Collaborating Centres and Central Coordinating Units, Multicentric study on genetic causes of mental retardation in India. Indian Journal of Medical Research, 94:161–169, 1991.
97. J.B. Familusi. Presentation at the Workshop of the IOM Committee on Neurological, Psychiatric, and Developmental Disorders: Meeting the Challenge in the Developing Countries, November 1999, Washington, D.C.
98. J.B. Familusi and J. O. Bolodeoku. Blood phenylalanine levels in mentally retarded African children: A study of 138 patients from Ibadan, Nigeria. Tropical Geographical Medicine Jun;28(2):96–100, 1976.
99. P. Kiepiela, A.A. Dawood, A. Moosa, H.M. Coovadia, and P. Coward. Evaluation of immunoregulatory cells in Duchenne muscular dystrophy and spinal muscular atrophy among African and Indian patients. Journal of Neurology Science Apr;84(2–3):247–255, 1988.
100. S.P. Lin, J.C. Chang, Y.J. Jong, T.Y. Yang, C.H. Tsai, N. M Wang, et al.. Prenatal prediction of spinal muscular atrophy in Chinese. Prenatal Diagnosis Jul;19(7):657–661, 1999.
101. S.P. Saha, S.K. Das, P.K.Gangopadhyay, T.N. Roy, and B. Maiti. Pattern of motor neurone disease in eastern India. Acta Neurologica Scandanavica Jul;96(1):14–21, 1997.
102. M.A. Salih, A.H. Malhdi, A.A. al-Jarallah, A.S. al Jarallah, M. al-Saadi, M.A. Hafeez, and S.A. Aziz. Childhood neuromuscular disorders: A decade's experience in Saudi Arabia. Annals of Tropical Paediatrics Dec: 16(4):271–280, 1996.
103. J. B. Peiris. Spinal muscular atrophy, East and West. Ceylon Medical Journal Mar;38(1):9–11, 1993.
104. H. W. Hitzeroth, C. E. Niehaus, and D.C. Brill. Phenylketonuria in South Africa. South Africa Medical Journal Jan;85(1):33–36, 1995.
105. P.M. Jeena, A. G. Wesley, and H. M. Coovadia. Admission patterns and outcomes in a paediatric intensive care unit in South Africa over a 25-year period (1971–1995). Intensive Care Medicine Jan;25(1):88–94, 1999.
106. A. Tomkins. Malnutrition, morbidity, and mortality in children and their mothers Proceedings of the Nutritional Society Feb;59(1):135–146, 2000.
107. B.S. Hetzel. Iodine deficiency disorders (IDD) and their eradication. Lancet ii:1126–1128, 1983.
108. J.B. Stanbury, ed. The Damaged Brain of Iodine Deficiency: Cognitive, Behavioural Neuromotor, and Educative Aspects, Cognizant Communications: Elmsford, NY, 1994.
109. C. Cobra, R. Kusnandi, D.Rustama, S.S. Suwardi, D. Permaesih, S. Martuti, and R.D. Semba. Infant survival is improved by oral iodine supplementation. Journal of Nutrition, 127:574–578, 1997.
110. S.N. Huda, S.M. Grantham-McGregor, M.R. Khan, and A. Tomkins. Biochemical hypothyroidism secondary to iodine deficiency is associated with poor school achievement
and cognition in Bangladeshi children Journal of Nutrition, 129(5):908–907, 1999.
111. A. Bautista, P.A. Barker, J.T. Dunn, M. Sanchez, and D.L. Kaiser. The effects of oral iodized oil on intelligence, thyroid status, and somatic growth in school-age children from an area of endemic goiter. American Journal of Clinical Nutrition, 35:127–134, 1982.
112. A. Sommer and K.P. West Jr.. The duration of the effect of Vitamin A supplementation. American Journal of Public Health Mar; 87(3):467–469, 1997.
113. F.E. Viteri. Prevention of iron deficiency. In Institute of Medicine, Prevention of Micronutrient Deficiencies. National Academy Press: Washington, D.C., pp. 45–102, 1998.
114. T.O. Scholl and M.L. Hediger. Anemia and iron-deficiency anemia: compilation of data on pregnancy outcome. American Journal of Clinical Nutrition 59(2 Suppl):492S–500S, 1994.
115. M. Roncagliolo Mgarrido, T. Walter, P. Peirano, and B. Lozoff. Evidence of altered central nervous system development in infants with iron deficiency anemia at 6 mo: Delayed maturation of auditory brainstem responses. American Journal of Clinical Nutrition 68(3):683–690, 1998.
116. B. Lozoff, E. Jimenez, and A.W. Wolf. Long-term developmental outcome of infants with iron deficiency. New England Journal of Medicine 325(10):687–694, 1991.
117. B. Lozoff, A.W. Wolf, and E. Jimenez. Iron-deficiency anemia and infant development: Effects of extended oral iron therapy. Journal of Pediatrics 129(3):382–389, 1996.
118. W.E. Watkins and E. Pollitt. “Stupidity or worms”: Do intestinal parasites impair mental performance? Psychological Bulletin 121(2):171–191, 1997.
119. D.L. Wilcken. MTHFR 677C → T mutation, folate intake, neural-tube-defects, and the risk of cardiovascular disease. Lancet 350: 603–604, 1997.
120. N.M.J. Van der Put, F. Gabreels, E.M.B. Stevens, J.A.N. Smeitink, F. J. M. Trijbels, and T.K. A. P. Eskes, et al. A second common mutation in the methylenetetra hydrofolate reductase gene: An additional risk factor for neural-tube-defects? American Journal of Human Genetics 62: 1044–1051, 1998.
121. MRC Vitamin Study Group. Prevention of neural tube defects: Results of the Medical Research Council vitamin study. Lancet 338: 131–137, 1991.
122. J. Cravioto. [Protein-calorie malnutrition and psychological development in the child]. [article in Spanish] Boletin de la Oficina Sanitaria Panamericana. Oct;61(4):285–306, 1966.
123. B.O. Osuntokun. The effects of malnutrition on the development of cognitive functions of the nervous system in childhood. Tropical Geographical Medicine Dec;24(4):311–326, 1972.
124. J.H. French and J.B. Familusi. Cerebellar disorders in childhood. Pediatrics Annals Nov;12(11):825–831, 835–844, 1983.
125. M. Winick and A. Noble. Cellular responses in rats during malnutrition at various ages. Journal of Nutrition Jul; 89(3):300–306, 1966.
126. M.W. Susser. The challenge of causality: Human nutrition, brain development and mental performance. Bulletin of the New York Academy of Medicine 65(10):1032–1049, 1989.
127. M. Levav, A.F. Mirsky, P.M. Schantz, S. Castro, and M.E. Cruz. Parasitic infection in malnourished school children: Effects on behaviour and EEG. Parasitology Jan;110(Pt.1):103–111, 1995.
128. Z.A. Stein, M.W. Susser, G. Saenger, and F. Marolla. Famine and Human Development: The Dutch Hunger Winter of 1944/45. Oxford University Press: New York, 1975a.
129. H.E. Freeman, R.E. Klien, J.W. Townsend, and A. Lechtig. Nutrition and cognitive development among rural Guatemalan children American Journal of Public Health 70:1277–1285, 1980.
130. D. Rush, Z.A. Stein, M.W. Susser. A randomized controlled trial of prenatal nutritional supplementation Pediatrics 65: 683–697, 1980.
131. D.P. Waber, L. Vuori-Christiansen, N. Ortiz, J.R. Clement, and N.E. Christiansen. Nutritional supplementation, maternal education and cognitive development in infants at risk of malnutrition. American Journal of Clinical Nutrition 34:807–813, 1981.
132. E. Pollitt, W.E. Watkins, and M.A. Husaini. Three-month nutritional supplementation in Indonesian infants and toddlers benefits memory function 8 y later. American Journal of Clinical Nutrition 66(6):1357–1363, 1997.
133. E. Pollitt and R. Mathews. Breakfast and cognition: An integrative summary. American Journal of Clinical Nutrition. 67(4):804S–813S, 1998.
134. S. Rasheed. Major causes and consequences of childhood disability. UNICEF 2(4), 1999.
135. N.Z. Khan, S. Ferdous, S. Munir, S. Huq, and H. McConachie. Mortality of Urban and Rural Young Children with Cerebral Palsy in Bangladesh. Developmental Medicine and Child Neurology, 40: 749–753, 1998.
136. C. Holborrow, F. Martinson, and N. Anger. A study of deafness in West Africa. International Journal of Pediatric Otorhinolaryngology 4:107–132, 1982.
137. F.T. Cutts and E. Vynnycky. Modelling the incidence of congenital rubella syndrome in developing countries. International Journal of Epidemiology Dec;28(6):1176–1184, 1999.
138. M.A. St. John and S. Benjamin. An epidemic of congenital rubella in Barbados. Annal Tropica Paediatrica Sep;20(3):231–235, 2000.
139. J.E. Lawn, S. Reef, B. Baffoe-Bonnie, S. Adadevoh, E.O. Caul, and G.E. Griffin. Unseen blindness, unheard deafness, and unrecorded death and disability: Congenital rubella in Kumasi, Ghana. American Journal of Public Health Oct;90(10):1555–1561, 2000.
140. C. Hoarau, V. Ranivoharimina, M.S. Chavet-Queru, I. Rason, H. Rasatemalala, G. Rakotonirina, et al. [Congenital syphilis: update and perspectives]. [French]. Santé Jan-Feb;9(1):38–45, 1999.
141. P.C. van Voorst Vader. Syphilis management and treatment. Dermatology Clinic Oct;16(4):699–711, xi, 1998.
142. M.L. Cohen. Candidate bacterial conditions. Bulletin of the World Health Organization 76(supplement) 2:61–63, 1998.
143. R. Davanzo, C. Antonio, A. Pulella, O. Lincetto, and S. Schierano. Neonatal and post-neonatal onset of early congenital syphillis: A report from Mozambique. Annal Tropica Paediatrica 12(4):445–450, 1992.
144. P. Zuber and P. Jacquier. [ Epidemiology of toxoplasmosis: worldwide status]. Schweizerische Medizinische Wochenschrift. Supplementum 65:S19–S22, 1995.
145. P. Sharma, I. Gupta, N.K. Ganguly, R.C. Mahajan, and N. Malla. Increasing toxoplasma seropositivity in women with bad obstetric history and in newborn. National Medical Journal of India Mar-Apr;10(2):65–66, 1997.
146. A. el-Nawawy, A.T. Soliman, O. el Azzouni, el-S Amer, M.A. Karim, S. Demian, et al. Maternal and neonatal prevalence of toxoplasma and cytomegalovirus (CMV) antibodies and hepatitis-B antigens in an Egyptian rural areas Journal of Tropical Pediatrics Jun;42(3):154–157, 1996.
147. M.D. de Jong, G.J. Galasso, B. Gazzard, P.D. Griffiths, D.A. Jabs, E.R. Kern, et al. Summary of the II International Symposium on Cytomegalovirus. Antiviral Research Oct;39(3):141–162, 1998.
148. N. O'Farrell. Increasing prevalence of genital herpes in developing countries: Implications for heterosexual HIV transmission and STI control programmes Sexual Transmission and Infection Dec;75(6):377–384, 1999.
149. L. Boylan and Z. Stein. The epidemiology of HIV infection in children and their mothers—vertical transmission. Epidemiologic Reviews 13: 143–177, 1991.
150. S.F. Davis, D.H. Rosen, S. Steinberg, P.M. Wortley, J.M. Karon, and M. Gwinn. Trends in HIV prevalence among childbearing women in the United States, 1989–1994. JAIDS: The Journal of Acquired Immune Deficiency Syndromes 19(2):158–164, 1998.
151. H.S. Amar, J.J. Ho, and A.J. Mohan. Human immunodeficiency virus prevalence in women at delivery using unlinked anonymous testing of newborns in the Malaysian setting. Journal of Paediatrics and Child Health 35(1): 63–66, 1999.
152. E.M. Connor, R.S. Sperling, R. Gelber, P. Kiselev, G. Scott, M.J. O'Sullivan, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. New England Journal of Medicine 331(180):1173–1180, 1994.
153. European Mode of Delivery Collaboration. Elective caesarean-section versus vaginal delivery in prevention of vertical HIV-1 transmission: A randomized clinical trial. Lancet 353(9158): 1030–1031, 1999.
154. International Perinatal HIV Group. The mode of delivery and the risk of vertical transmission of human immunodeficiency virus type 1: A meta-analysis of 15 prospective cohort studies. New England Journal of Medicine 340(13),977–987, 1999.
155. L.M. Mofenson. Short-course zidovudine for prevention of perinatal infection. Lancet; 353:766–767, 1999.
156. C. Chase, J. Ware, J. Hittleman, I. Blasini, R. Smith, A. Llorente et al. Early cognitive and motor development among infants born to women infected with human immunodeficiency virus. Women and Infants Transmission Study Group. Pediatrics Aug;106(2):E25, 2000.
157. A.L. Belman. AIDS and pediatric neurology. Neurologic Clinics of North America. 8(3):571–602, 1992.
158. R.A Oberhelman, E.S. Guerrero, M.L. Fernandez, M. Silio, D. Mercado, N. Comiskey, et al. Correlations between intestinal parasitosis, physical growth, and psychomotor development among infants and children from rural Nicaragua American Journal of Tropical Medical Hygiene Apr;58(4):470–475, 1998.
159. A.O. Coker, R.D. Isokpehi, B.N. Thomas, A.F. Fagbenro-Beyioku, and S.A. Omilabu. Zoonotic infections in Nigeria: Overview from a medical perspective Acta Tropica Jul 21;76(1):59–63, 2000.
160. J.S. Remington, R. McLeod, and G. Desmonts. Toxoplasmosis. In: Infectious Diseases of the Fetus and Newborn Infant, 4th edn. Remington, J.S. and Klein, J.O., eds. W.B. Saunders: Philadelphia, pp. 140–267, 1995.
161. D. Dunn, M. Wallon, F. Peyron, E. Peterson, C. Peckham, and R. Gilbert. Mother-to-child transmission of toxoplasmosis: Risk estimates for clinical counselling. Lancet 353: 1929–1933, 1999.
162. J. Koppe, D. Loewer-Sieger, and H.de Roever-Bonnet. Results of 20 year follow-up of congenital toxoplasmosis. Lancet ii: 254–256, 1986.
163. N. Roizen, C.N. Swisher, and M. A. Stein. Neurologic and developmental outcome in treated congenital toxoplasmosis Pediatrics 95: 11–20, 1995.
164. World Health Organization Haemophilus influenzae type b. Available: http://www.who.int/inf-fs/en/fact 105.html. 1998a.
165. World Health Organization. Malaria. Available: http://www.who.int/inf-fs/en/fact094.html, 1998b.
166. World Health Organization. Epidemic meningococcal disease, Fact Sheet Number 105. Available: http://www.who.org/vaccines-diseases/diseases.hib.html, 2000.
167. D. Nabarro. Roll back malaria. Parasitologia 41:501–504, 1999.
168. B.J. Brabin. The risks and severity of malaria in pregnant women. In: Applied Field Research in Malaria. Report No.1. WHO: Geneva, pp.1–34, 1991.
169. C. Menendez. Malaria during pregnancy: A priority area of malaria research and control. Parasitologia Today 11:178–183, 1995.
170. G. Norheim, E. Rosenqvist, P. Aavitsland, and D. A. Caugant. Meningococcal disease in Africa-Epidemiology and prevention. Tidsskrift for den Norske Laegoforening Jun 10; 120(15):1735–1739, 2000.
171. T. Goetghebuer, T. E. West, V. Wermenbol, A. L. Cadbury, P. Milligan, N. Lloyd-Evans, and R. A. Adegbola. Outcome of meningitis caused by Streptococcus pneumoniae and Haemophilus influenzae type b in children in The Gambia. Tropical Medicine and International Health Mar;5(3):207–213, 2000.
172. G.O. Akpede, S.O. Dawodu, and M. E. Umoffia. Response to antimicrobial therapy in childhood bacterial meningitis in tropical Africa: report of a bi-centre experience in Nigeria, 1993–1998. Annals of Tropical Paediatrics Sep;19(3):237–243, 1999.
173. M. A. Bouskela, S. Grisi, and A.M. Escobar. Epidemiologic aspects of Haemophilus influenzae type b infection. Review of Panama Salud Publica May;7(5):332–339, 2000.
174. P.M. Kurkdjian, A. Bourrillon, L. Holvoet-Vermau, and E. Bingen. Pathology of Haemophilus infections: Current situation in pediatrics Archives of Pediatrics Jun;7(3):S551–558, 2000.
175. K.T. Wong. Annotation: Emerging and re-emerging epidemic encephalitis: A tale of two viruses. Neuropathology Applied Neurobiology Aug;26(4):313–318, 2000.
176. T.J. Victoria, M. Malathi, V. Ravi, G. Palani, and N.C. Appavoo. First outbreak of Japanese encephalitis in two villages of Dharmapuri district in Tamil Nadu. Indian Journal of Medical Research Dec; 112:193–197, 2000.
177. D. Lou, J. Song, H. Ying, R. Yao, and Z. Wang. Prognostic factors of early sequelae and fatal outcome of Japanese encephalitis. Southeast Asian Journal of Tropical Medicine and Public Health Dec;26(4):694–698, 1995.
178. B.V. Huy, H.C. Tu, T.V. Luan, and R. Lindqvist. Early mental and neurological sequelae after Japanese B encephalitis Southeast Asian Journal of Tropical Medicine and Public Health Sep;25(3):549–553, 1994.
179. R. Kumar, A. Mathur, K.B. Singh, P. Sitholey, M. Prasad, R. Shukla, et al. Clinical sequelae of Japanese encephalitis in children. Indian Journal of Medical Research Jan;97:9–13, 1993
180. H.K. Hartter, O.I. Oyedele, K. Dietz, S. Kreis, J.P. Hoffman, and C.P. Muller. Placental transfer and decay of maternally acquired antimeasles antibodies in Nigerian children. Pediatric Infectious Disease Journal Jul;19(7):635–641, 2000.
181. P.V. Taneja and N.G. Vaidya. Infant and child mortality in Bhil tribe of Jhabua district. Indian Journal of Pediatrics. May-Jun;64(3):409–413, 1997.
182. M. Hodges and R.A. Williams. Registered infant and under-five deaths in Freetown, Sierra Leone from 1987–1991 and a comparison with 1969–1979. West African Journal of Medicine Apr-Jun;17(2):95–98, 1998.
183. P.M. Strebel. Measles. Bulletin of the World Health Organization 76 (Suppl.2):154–155, 1998
184. A.S. Narita and H.R. Taylor. Blindness in the tropics. Medical Journal of Australia Sep 29;159(6):416–420, 1993.
185. R. Whitfield, L. Schwab, D. Ross-Degnan, P. Steinkuller, and J. Swartwood. Blindness and eye disease in Kenya: ocular status survey results form the Kenya Rural Blindness Prevention Project. British Journal of Ophthalmology Jun;74(6):333–340, 1990.
186. S.M. Shukla. Eye diseases and control of blindness in Zambia. Social Science and Medicine 17(22):1781–1783, 1983.
187. World Health Organization. Global Polio Eradication Initiative. Available: http://www.who.polioeradication.org/global_status.html, 2000.
188. S. Awasthi and V.K. Pande. Cause-specific mortality in under five in the urban slums of Lucknow, north India. Journal of Tropical Pediatrics Dec;44(60):358–361, 1998.
189. J.A. Owa and A.I. Osinaike. Neonatal morbidity and mortality in Nigeria. Indian Journal of Pediatrics May–Jun;65(3):441–449, 1998.
190. K. Jamil, A. Bhuiya, K. Streatfield, and N. Chakrabarty. The immunization programme in Bangladesh: Impressive gains in coverage, but gaps remain. Health Policy and Planning Mar;14(1):49–58, 1999.
191. J.A. Cook. Trachoma. Bulletin of the World Health Organization 76(Suppl. 2):139–140, 1998.
192. P.J. Dolin, H. Faal, G.J. Johnson, D. Minassian, S. Sowa, S. Day et al. Reduction of trachoma in a sub-Saharan village in absence of a disease control programme. Lancet May 24;349(9064):1511–1512, 1997.
193. D. Kaimbo W.A. Kaimbo and L. Missotten. Ocular refraction in Zaire. Bulletin de la Societe Belge D'Ophtalmologie 261:101–105, 1996.
194. A. Kumar, P. K. Dey, P.N. Singla, R. S. Ambasht, and S.K. Upadhyay. Blood lead levels in children with neurological disorders. Journal of Tropical Pediatrics 44(6):320–322, 1998.
195. N.Z. Khan and A.H. Khan. Lead poisoning and psychomotor delay in Bangladeshi children. Lancet 353:754, 1999.
196. H.L. Needleman and C.A.Gatsonis. Low-level lead exposure and the IQ of children. A meta-analysis of modern studies. Journal of the American Medical Association Feb 2;263(5):673–678, 1990.
197. H. L. Needleman, M.A. Schell, D. Bellinger, A. Leviton, and E.N. Allred. The long-term effects of exposure to low doses of lead in childhood: An 11-year follow-up report. New England Journal of Medicine 322: 83–88, 1990.
198. J.M. Burns, P. A. Baghurst, M. G. Sawyer, A. J. McMichael, and S.L. Tong. Life-time low-level exposure to environmental lead and children's emotional and behavioral development at ages 11–13 years. The Port Pirie Cohort Study. American Journal of Epidemiology 149(8): 740–749, 1990.
199. E. E. Castilla, P. Ashton-Prolla, E. Barreda-Mejia, D. Brunoni, D.P. Cavalcanti, J.L. Delgadillo, et al., Thalidomide, a current teratogen in South America. Teratology 54:273–277, 1996.
200. J.L. Jacobson and S.W. Jacobson. Intellectual impairment in children exposed to polychlorinated biphenyls in utero. New England Journal of Medicine 335:783–789, 1996.
201. M.C. Ramsey and C.R. Reynolds. Does smoking by pregnant women influence IQ, birth weight, and developmental disabilities in their infants? A methodological review and multivariate analysis. Neuropsychology Review 10(1):1–40, 2000
202. N. Breslau, J.E. DelDotto, and G.G. Brown. A gradient relationship between low birth weight and IQ at age 6 years. Archives of Pediatric and Adolescent Medicine 148: 377–383, 1994.
203. World Health Organization. Control of Major Blinding Diseases and Disorders, Fact Sheet Number 214. Available: http://www.who.int/inf-fs/en/fact214.html, 2000.
204. M.J. Wolf, B. Wolf, G. Beunen, and P. Casaer. Neurodevelopmental outcome at 1 year in Zimbabwean neonates with extreme hyperbilirubinemia. European Journal of Pediatrics, 158(2):111–114, 1999.
205. M.S. Durkin, N.Z. Khan, L.L. Davidson, S. Huq, S. Munir, I. Rasul, and S. S. Zaman. Prenatal and postnatal risk factors for mental retardation among children in Bangladesh. American Journal of Epidemiology, (in press).
206. Z. A. Stein and M. W. Susser. The epidemiology of mental retardation. In: Stress and Disability in Childhood. Butler, N.R. and Connor, B.D., eds., Wright, Bristol, pp.21–46, 1984.
207. S. Islam, M. S. Durkin, and S.S. Zaman. Socioeconomic status and the prevalence of mental retardation in Bangladesh. Mental Retardation December; 31(6):412–417, 1993.
208. M. F. Lechat. The epidemiology of health effects of disasters. Epidemiologic Reviews 12:192–198, 1990.
209. G. S. Smith and P. Barss. Unintentional injuries in developing countries: The epidemiology of a neglected problem. Epidemiologic Reviews 13:228–266, 1991.
210. P. Chabasse. The proliferation of anti-personnel landmines in developing countries: Considerable damage in human terms and a dramatically insufficient medico-social response. In: International Committee of the Red Cross. Symposium on Antipersonnel Mines. Montreux, 21–23 April, 1993. International Committee of the Red Cross Report: Geneva, pp. 85–95, 1993.
211. N.Z. Khan and M.A. Lynch. Recognizing child maltreatment in Bangladesh. Child Abuse & Neglect 21(8):815–818, 1997.
212. C. N. Mock, F. Abantanga, P. Cummings, and T. D. Koepsell. Incidence and outcome of injury in Ghana: A community-based survey Bulletin of the World Health Organization 77(12):955–964, 1999.
213. A.A. al-Qudah. Clinical patterns of neuronal migrational disorders and parental consanguinity. Journal of Tropical Pediatrics. Dec;44(6):351–354, 1998.
214. A. Mutirangura, T. Norapucsunton, Y. Tannirandorn, and S. Jongpiputvanich. DNA diagnosis for clinical and prenatal diagnosis of spinal muscular atrophy in Thai patients. Journal of the Medical Association of Thailand Dec;79(1):S11–S14, 1996.
215. I.C. Verma. Molecular diagnosis of neurological disorders in India Indian Journal of Pediatrics Sep–Oct;64(5):661–666, 1997.
216. B. Underwood. Perspectives from micronutrient malnutrition elimination/eradication programmes. Bulletin of the World Health Organization 76(Suppl. 2):34–37, 1998.
217. C. Bellamy. The State of the World's Children 2001. UNICEF: OxfordUniversity Press; Oxford, England, 2001.
218. WHO (World Health Organization). Bulletin of the World Health Organization. World Health Organization: Geneva 76, Suppl. 2:118–120, 1998.
219. B. Elnager, M. Eltom, F.A. Karlsson, P.P. Bourdoux, and M. Gebre-Medhin. Control of iodine deficiency using iodination of water in a goiter endemic area. International Journal of Food Sciences and Nutrition 48(2): 119–127, 1997.
220. UNICEF. Percent of household using iodized salt. http://www.unicef.org/statis/country_pick.cgi, 2000.
221. C.P. Howson, E.T. Kennedy, A. Horwitz, eds. Prevention of Micronutrient Deficiencies: Tools for Policymakers and Public Health Workers. National Academy Press: Washington, D.C., 1998.
222. WHO (World Health Organization). Bulletin of the World Health Organization. WHO: Geneva 76 suppl 2:156–157, 1998.
223. R.W. Steketee, J.J. Wirima, A.W. Hightower, L. Slutsker, D.L. Heymann, and J.G. Breman. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. American Journal of Tropical Medical Hygiene 55(1):33–41, 1996.
224. M.E. Parise, J.G. Ayisi, B.L. Nahlen, L.J. Schultz, J.M. Roberts, A. Misore, et al. Efficacy of sulfadoxine-pyrimethamine for prevention of placental malaria in an area of Kenya with a high prevalence of malaria and human immunodeficiency virus infection. American Journal of Tropical Medical Hygiene 59:813–822, 1998
225. O.S. Levine, B. Schwartz, N. Pierce, and M. Kane. Development, evaluation and implementation of Haemophilus influenzae type b vaccines for young children in developing countries: Current status and priority actions. Pediatric Infectious Diseases 17:95–113, 1998.
226. T. Siraprapasiri, W. Sawaddiwudhipong, and S. Rojanasuphot. Cost benefit analysis of Japanese encephalitis vaccination program in Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 28(1):143–148, 1997.
227. P. Bonnanni. Demographic impact of vaccination: A review. Vaccine Oct 29;17(3):S120–125, 1999.
228. T.A. Ruff. Immunization strategies for viral diseases in developing countries Review of Medical Virology Apr–Jun;9(2):121–138, 1999
229. R.B. Aylward, H.F. Hull, S.L. Cochi, R.W. Sutter, J.M. Olive and B. Melgaard. Disease eradication as a public health strategy: A case study of poliomyelitis eradication. Bulletin of the World Health Organization 78(3):285–297, 2000.
230. L. Kuhn and Z. Stein. Infant survival, HIV infection, and feeding alternatives in less-developed countries. American Journal of Public Health 87(6):926–931, 1997.
231. N.A. Wade, G.S. Birkhead, B.L. Warren, T.T. Charbonneau, P.T. French, and L. Wang. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. New England Journal of Medicine 339(20):1409–1414, 1998
232. N.T. Rotta, C. Silva, L. Ohlweiler, I. Lago, R. Cabral, F. Goncalves et al. AIDS neurologic manifestations in childhood. Review of Neurology Aug 16–31;29(4):319–322, 1999.
233. C. Butler, J. Hittelman, and S.B. Hauger. Guidelines for the care of children and adolescents with HIV infection. Approach to neurodevelopmental and neurologic complications in pediatric HIV infection. Journal of Pediatrics Jul;119(1 Pt 2):S41–46, 1991.
234. H.L. Needleman. Childhood lead poisoning: A disease for the history texts. American Journal of Public Health 81(6): 685–687, 1991
235. A.R. Kemper, W.C. Bordley, and S.M. Downs. Cost-effectiveness analysis of lead poisoning screening strategies following the 1997 guidelines of the Centers for Disease Control and Prevention. Archives of Pediatrics & Adolescent Medicine 152(12): 1202–1208, 1998.
236. S.J. Rolnick, J. Nordin, and L.M. Cherney. A comparison of costs of universal versus targeted lead screening for young children. Environmental Research 80(1):84–91, 1999.
237. J.S. Bajaj, A. Misra, M. Rajalakshmi, and R. Madan. Environmental release of chemicals and reproductive ecology. Environmental Health Perspectives 101(Suppl. 2):125–130, 1993.
238. E.E. Castilla, J.S. Lopez-Camelo, G.P. Dutra, and J.E. Paz. Birth defects monitoring in underdeveloped countries: An example from Uruguay. International Journal of Risk & Safety in Medicine 2:271–288, 1991.
239. M.A. Koblinsky, O. Campbell, and J. Heichelheim. Organizing delivery care: What works for safe motherhood? Bulletin of the World Health Organization 77(5):399–406, 1999.
240. A.T. Bang, R.A. Bang, S.B. Baitule, M.H. Reddy, and M.D. Deshmuck. Effect of home-based care and management of sepsis on neonatal mortality: Field trial in rural India. Lancet 354(9194):1955–1961, 1999.
241. P.M. Shah. Birth asphyxia: A crucial issue in the prevention of developmental disabilities. Midwifery Jun;6(2):99–107, 1990.
242. United Nations General Assembly, Convention on the Rights of the Child. 1989.
243. J.E. Keefe, J.E. Lovie-Kitchin, H. Maclean, and H.R. Taylor. A simplified screening test for identifying people with low vision in developing countries. Bulletin of the World Health Organization 74(5):525–532, 1996.
244. S.J. Hornby, S. Adolph, V.K. Gothwal, C.E. Gilbert, L. Dandona, A. Foster, et al. Requirements for optical services in children with microphthalmos, coloboma and microcornea in southern India. Eye Apr;14(PT 2):219–224, 2000.
245. R. Gopal, S.R. Hugo, and B. Louw. Identification and follow-up of children with hearing loss in Mauritius International Journal of Pediatrics and Otorhinolaryngology Feb;57(2):99–113, 2001.
246. V.E. Newton, I.I. Macharia, P. Mugwe, B. Ototo, and S.W. Kan. Evaluation of the use of a questionnaire to detect hearing loss in Kenyan pre-school children. International Journal of Pediatrics and Otorhinolaryngology Mar 1;57(3):229–234, 2001.
247. B.O. Olusanya, A.A. Okolo, and G.T. Ijaduola. The hearing profile of Nigerian school children. International Journal of Pediatrics and Otorhinolaryngology Oct 16;55(3):173–179, 2000.
248. H. Furuta and T. Yoshino. The present situation of the use of hearing aids in rural areas of Sri Lanka: Problems and future prospects. International Journal of Rehabilitative Research Mar;21(1):103–107, 1998.
249. C.A. Prescott, S.S. Omoding, J. Fermor, and D. Ogilvy. An evaluation of the ‘voice test' as a method for assessing hearing in children with particular reference to the situation in developing countries. International Journal of Pediatrics and Otorhinolaryngology Dec 15;51(3):165–170, 1999.
250. S. Ramaa. Two decades of research on learning disabilities in India. Dyslexia Oct-Dec;6(4):268–283, 2000.
251. B. O'Toole and R. McConkey. A training strategy for personnel working in developing countries International Journal of Rehabilitative Research Sep;21(3):311–321, 1998.
252. L.M. Stough and A.R. Aguirre-Roy. Learning disabilities in Costa Rica: Challenges for an “army of teachers.” Journal of Learning Disabilities Sep–Oct;30(50):566–571, 1997.
253. D.E. Bender, C. Auer, J. Baran, S. Rodriguez, and R. Simeonsson. Assessment of infant and early childhood development in a periurban Bolivian population. International Journal of Rehabilitative Research Mar; 17(1):75–81, 1994.
254. M.J. Armstrong. Disability self-help organizations in the developing world: A case study from Malaysia. International Journal of Rehabilitative Research Sep;16(3):185–194, 1993.
255. UNESCO and the Ministry of Education and Science, Spain. The Salamanca Statement. The Final Report of the World Conference on Special Needs Education, Access and Quality. United Nations Educational, Scientific and Cultural Organization: Paris, 1994.
256. ILO, UNESCO, WHO. Community Based Rehabilitation for and with People with Disabilities Joint Position Paper, World Health Organization: Geneva, 1994.
257. N.E. Groce. Disability in cross-cultural perspective: Rethinking disability. Lancet 354(9180):756–757, 1999.
258. World Health Organization(WHO). International Classification of Impairments, Disabilities and Handicaps World Health Organization: Geneva, 1980.
259. R.J. Simeonsson, D. Lollar, J. Hollowell, and M. Adams. Revision of the International Classification of Impairments, Disabilities and Handicaps: Developmental issues. Journal of Clinical Epidemiology 53:113–124, 2000.
260. M.J. Thorburn. Recent developments in low-cost screening and assessment of childhood disabilities in Jamaica. Part I: Screening. West Indian Medical Journal Mar;42(1):10–20, 1993.
261. M.J. Thorburn, T.J. Paul, and L.M. Malcolm. Recent developments in low-cost screening and assessment of childhood disabilities in Jamaica. Part II: Assessment. West Indian Medical Journal Jun;42(2):46–52, 1993.
262. T. Jonsson. OMAR in rehabilitation: A Guide on Operations Monitoring and Results. UNDP Interregional Programme for Disabled People. United Nations Development Program: Geneva, 1994.
263. E. Helander, P. Mendis, and G. Nelson. Training Disabled People in the Community. World Health Organization: Geneva, 1979–1991.
264. World Health Organization (WHO). Promoting the Development of Young Children with Cerebral Palsy: A Guide for Mid-Level Rehabilitation Workers. World Health Organization: Geneva, 1993.
265. D. Werner. Disabled Village Children. Hesperian Foundation: Palo Alto, CA, 1988.
266. E. Haddad. World Declaration of Education for All. UNESCO: Paris, 1990.
267. M.J. Thorburn. Training of CBR personnel: Current issues and future trends. Asia Pacific Disability Rehabilitation Journal 11:12–17, 2000.
268. R. McConkey and B. O'Toole. Towards the new millenium. In: Developing Countries for People with Disabilities. O'Toole, B. and McConkey, R., eds., Lisieux Hall Publications: Chorley, Lancs, England, p. 8, 1999.
269. S.S. Zaman, N. Khan, S. Islam, S. Banu, P. Dixit, P. Shrout, et al. Validity of the Ten Questions for screening serious childhood disability: Results from urban Bangladesh. International Journal of Epidemiology 19(3):613–620, 1990.
270. S.S. Zaman, N.Z. Khan, and S. Islam, eds. From Awareness to Action: Ensuring Health, Education and Rights of Disabled. Bangladesh Protibondhi Foundation: Dhaka, 1996.
271. H. McConachie, S. Huq, S. Munir, S. Ferdous, S. S. Zaman, and N. Z. Khan. A randomized controlled trial of alternative modes of service provision for children with cerebral palsy in Bangladesh. Journal of Pediatrics 137(6):769–776, 2000.
272. K.M. Munir and W.R. Beardslee. Developmental psychiatry: Is there any other kind? Harvard Review of Psychiatry Jan–Feb;6(5):250–262, 1999.
273. Zimbabwe Ministry of Education, Sports and Culture. School Psychological Services and Special Needs Education. Annual Report 1998.
274. G. Powell. Report on Childhood Disability in Sub-Saharan Africa. Department of Pediatrics and Child Health, University of Zimbabwe Medical School; Harare, 2000.
275. L. Mariga and L. Phachaka. Integrating Children with Special Education Needs into Regular Schools in Lesotho. Report of a Feasibility Study. UNICEF: Lesotho, 1993.
276. H. House et al. Zimbabwe Steps Ahead. Russell Publications: Nottingham, U.K., 1990.
277. S. Chidayausiku. Community Based Rehabilitation Programme in Zimbabwe, Sida Evaluation 15, 1998.
278. N.J. Cook and N.K. Rogers. Blindness and poverty go hand in hand. Acta Ophthalmologica Scandinavica Apr;74(2):204–209, 1996.
279. A. Kroeger, M. Gonzalez, and J. Ordonez-Gonzalez. Insecticide-treated materials for malaria control in Latin America: To use or not to use? Transactions of the Royal Society of Tropical Medicine and Hygiene Nov–Dec;93(6):565–570, 1999.
280. D.T. Jamison and W.H. Mosley. Disease control priorities in developing countries: health policy responses to epidemiological change. American Journal of Public Health Jan;81(1):15–22, 1991.
281. WHO-WAOPBD. Services for the Prevention and Management of Genetic Disorders and Birth Defects in Developing Countries. Report from Joint WHO-WAOPBD Meeting on Prevention and Care of Genetic Diseases and Birth Defects in Developing Countries. The Hague, 5–7 Jan. 1999; World Health Organization Genetics Unit: Geneva, (in press).
282. S. Hartley. Service development to meet the needs of ‘people with communication disabilities' in developing countries. Disability Rehabilitation Aug;20(8):277–284, 1998.
283. M. Gracey. The pediatrician's role in the twenty-first century. Acta Paediatrica Japan Oct;40(5):393–399, 1998.
284. D. Shah, S. Shroff, and S. Sheth. Reproductive and sexual health and safe motherhood in the developing world. European Journal of Contraception and Reproductive Health Care Dec;4(4):217–228, 1999.
285. G.L. Stidham. Emergencies in international child health. Current Opinon Pediatrics Jun;9(3):254–258, 1997.
286. O.F. Fafowora. Some practical aspects of teaching medicine in Africa. African Journal of Medicine and Medical Science Jun;23(2):187–188, 1994.
287. P.W. Alberti. Health care economics: Impact on hearing loss prevetion in the developing world. Scandinavian Audiology (supplement);42:49–51, 1996.
288. P. Huguet, A. Auzemery, J.F. Ceccon, and J.F. Schemann. The Institute of Tropical Ophthalmology of Africa. [French] MARS 55(4 Pt 2):466–468, 1995.
289. C. Boudet, P. Bensaid, and M.S. Sanner. Ophthalmologists without borders in Northern Cameroon. [French]. MARS 55(4 Pt 2); 415–420, 1995.
290. N. Kinabo. Eye diseases and services in Tanzania. Social Science and Medicine 17(22):1767–1772, 1983.
291. R.A. Mitchell, D.H. Zhou, and G.H. Watts. Emerging patterns of disability distribution in developing countries International Disability Studies Oct-Dec;11(4):145–148, 1989.
292. S.L. Wirz and I. Lichtig. The use of non-specialist personnel in providing a service for children disabled by hearing impairment. Disability Rehabilitation May;20(5):189–194, 1998.
293. P.W. Alberti. Pediatric ear, nose and throat services' demands and resources: a global perspective. International Journal of Pediatric Otorhinolaryngology Oct 5(supplement);49(1):S1–S9, 1999.
294. D. Morley. The spread of comprehensive care through under-fives' clinics. Transactions of the Royal Society of Tropical Medicine and Hygiene 67(2):155–170, 1973.
295. D. Morley. A medical service for children under five years of age in West Africa Transactions of the Royal Society of Tropical Medicine and Hygiene 57:79–88, 1963.
296. N. Cunningham. The under fives clinic. What difference does it make? Journal of Tropical Pediatrics and Environmental Child Health Dec;24(6):239–334, 1978.
|
Summary of Findings: Epilepsy in Developing Countries
|