2
Magnitude of the Problem
Suicide is a global problem, a leading cause of death in the world claiming about 30,000 lives in the United States each year, almost 1 million annually world-wide. In the United States, the suicide rate was 10.7 per 100,000 in 1999. It greatly exceeded the rate of homicide (6.2 per 100,000) in 1999, as it has for the last 100 years (Figure 2-1) (Bureau of Justice Statistics, 2001; Bureau of the Census, 1976; Hoyert et al., 2001; Minino and Smith, 2001; NCHS, 2001; NCIPC, 2000). Suicide is the third leading cause of death in youth 15–24 years old. White males over 85 have the highest rate of suicide, about 65 per 100,000. Suicide rates are also elevated in some ethnic groups. For example, suicide is about 1.5 times more prevalent than average among Native Americans. While whites continue to have higher suicide rates than blacks, the gap seems to be narrowing in young males.
Suicides in males outnumber those in females in almost all nations, including the United States. While males are more likely to complete suicide, females are more likely to attempt suicide. Nationally and internationally there is geographic heterogeneity, suggesting that social and cultural differences have a significant impact on suicide rates (see also Chapter 6). In the United States in 1998, firearms accounted for the majority of suicides both in general (57.0%) and among youth 15–24 (61%) (NCIPC, 2000). Suffocation (18.7%; 25%), poisoning (16.6%, 7%), and falls (2.0% both) follow in usage. This differs in other nations; for example, self-poisoning, especially with insecticides, is the most common method in both Pakistan (Khan and Reza, 2000) and rural China (Yip, 2001).
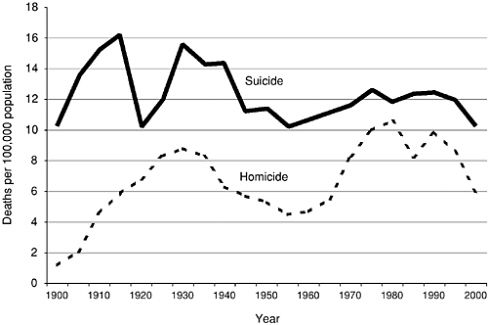
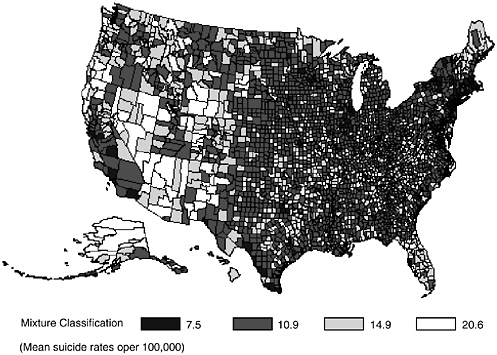
FIGURE 2-1 Rates of Suicide and Homicide in the United States: 1900–2000. Based on data from the Bureau of Justice Statistics (2001), Bureau of the Census (1976), Hoyert et al. (2001), Minino and Smith (2001), and NCHS (2001). Inconsistencies in reporting before 1933 may account for some of the early fluctuations in rates.
This chapter reviews the characteristics of some of the populations at risk, describes the geographical differences, and briefly explores the limitations of the epidemiological data. The chapter closes with an analysis of the economic cost to society that suicide presents.
GEOGRAPHIC TRENDS
Suicide rates are generally higher in northern European nations than in southern European nations (see Table 2-1). For example, Hungary’s suicide rate was over 33 per 100,000 as of 1999 (WHO, 2001a). In comparison, Greece has had low suicide rates, only 3.8 per 100,000 as of 1998 (WHO, 2001a). Suicide rates have been high in recent years in many, but not all, of the former Soviet states. For example, suicide rates are over 35 per 100,000 in the Russian Federation and Lithuania, but are less than 5 per 100,000 in Armenia, Azerbaijan, and Georgia (WHO, 2001a).
TABLE 2-1 National Suicide Rates per 100,000 for Selected Countries. Most Recent Data from the World Health Organization (WHO, 2001a)
|
Country |
Total |
Male |
Female |
Year |
|
Armenia |
1.8 |
2.7 |
0.9 |
1999 |
|
Austria |
19.2 |
28.7 |
10.3 |
1999 |
|
Azerbaijan |
0.7 |
1.1 |
0.2 |
1999 |
|
Belarus |
34.0 |
61.1 |
10.0 |
1999 |
|
Brazil |
4.1 |
6.6 |
1.8 |
1995 |
|
Canada |
12.3 |
19.6 |
5.1 |
1997 |
|
China |
14.1 |
13.4 |
14.8 |
1998 |
|
Rural Areas |
23.3 |
21.9 |
24.8 |
1998 |
|
Urban Areas |
6.8 |
6.8 |
6.8 |
1998 |
|
Finland |
23.8 |
38.3 |
10.1 |
1998 |
|
Georgia |
4.3 |
6.6 |
2.1 |
1992 |
|
Greece |
3.8 |
6.1 |
1.7 |
1998 |
|
Hungary |
33.1 |
53.1 |
14.8 |
1999 |
|
India |
10.7 |
12.2 |
9.1 |
1998 |
|
Italy |
8.2 |
12.7 |
3.9 |
1997 |
|
Japan |
18.8 |
26.0 |
11.9 |
1997 |
|
Kuwait |
2.2 |
2.7 |
1.6 |
1999 |
|
Lithuania |
41.9 |
73.8 |
13.6 |
1999 |
|
Mexico |
3.1 |
5.4 |
1.0 |
1995 |
|
Norway |
12.1 |
17.8 |
6.6 |
1997 |
|
Philippines |
2.1 |
2.5 |
1.7 |
1993 |
|
Poland |
14.3 |
24.1 |
4.6 |
1996 |
|
Republic of Korea |
13.0 |
17.8 |
8.0 |
1997 |
|
Russian Federation |
35.5 |
62.6 |
11.6 |
1998 |
|
Singapore |
11.7 |
13.9 |
9.5 |
1998 |
|
Sri Lanka |
31.0 |
44.6 |
16.8 |
1991a |
|
Sweden |
14.2 |
20.0 |
8.5 |
1996 |
|
Tajikistan |
3.5 |
5.1 |
1.8 |
1995 |
|
Thailand |
4.0 |
5.6 |
2.4 |
1994 |
|
Ukraine |
29.1 |
51.2 |
10.0 |
1999 |
|
United Kingdom of Great Britain & Northern Ireland |
7.4 |
11.7 |
3.3 |
1998 |
|
United States |
10.7 |
17.6 |
4.1 |
1999 |
|
aThe more recent total suicide rate for 1996 was 21.6, but rates by sex were not available. |
||||
Overall, suicide rates are lower in other Asian nations compared to China, including Singapore (11.7 per 100,000), Japan (18.8 per 100,000), and Thailand, which reports a very low rate of 4.0 per 100,000 (Table 2-1, WHO, 2001a). The suicide rate for China has decreased dramatically in recent years, dropping from 23 per 100,000 in 1999 to 17 per 100,000 in 2000 (WHO, 2001b).
Studies from across the world find higher rates of suicide in rural versus urban areas (Plotnikov, 2001; Yip, 2001; Yip et al., 2000). In China, for example, the rate is two to five times greater in rural regions (Ji et al., 2001; Jianlin, 2000; Phillips et al., 1999; Yip, 2001). Higher rates in rural regions have also been documented for young males in Australia (Wilkinson and Gunnell, 2000) and in the Ukraine (Kryzhanovskaya and Pilyagina, 1999). Even among adolescents in Greece, where the suicide rate is relatively low, urban areas report significantly lower rates than rural areas (Beratis, 1991). In China (Yip et al., 2000), unlike Australia for example (Morrell et al., 1999), the usual pattern of more suicides among men than women is reversed in rural areas due to the very high female suicide rate, especially among young women (Ji et al., 2001; Yip, 2001; Yip et al., 2000).
Like the United States (see below), suicide rates are higher in rural areas in China. In 1998, women in rural China completed suicide at a rate of over 30 per 100,000 for ages 25–34 and 45–64, with increasing rates at older ages (WHO, 2001a). The male rate surpasses that for women starting at age 55, with over 129 per 100,000 dying by suicide over the age of 75 in rural China (WHO, 2001a). In comparison, the overall rate for females and males in urban China is 6.8 per 100,000 in 1998, with the highest rate for males over 75 at about 32 per 100,000 (WHO, 2001a).
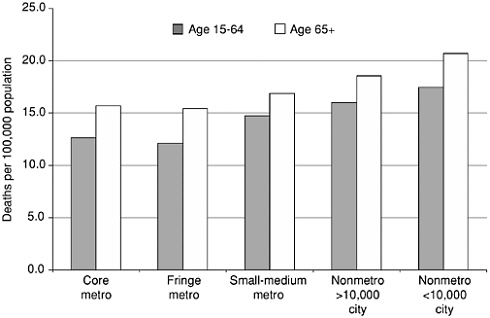
Suicide rates vary greatly across the United States, with higher rates generally in the western states. New Jersey is the lowest with 6.4/100,000 in 1998. Nevada and Alaska are the highest with rates in excess of 21/ 100,000 (Murphy, 2000). Mapping the rates by county (see Appendix A and Figure 2-2) illustrates that those counties with the highest rates are predominantly in the western states with lowest population density. Counties with the lowest rates (7.5 suicides per 100,000) appear to be clustered in the central United States. Finally, counties classified with intermediate rates are largely in the eastern portion of the United States. Population density has been suggested as a factor in these differences (Saunderson and Langford, 1996). Examining the suicide rates by urbanization in the United States reveals that the rates are higher in less populated area compared to densely populated cities (Figure 2-3). For the most part this difference is a reflection of the decrease in firearm suicides with urbanization (Figure 2-4). This relationship of suicide by firearms and population density is even more dramatic when suicide among elderly persons is explored. Among the elderly, suicide by firearms decreases dramatically with increased urbanization (Figure 2-5), but non-firearm suicides are more common in urban areas. When controlling for education, employment status, and divorce rate, Birckmayer and Hemenway (2001) also found that living in urban areas was associated with increases in U.S. suicide rates for non-firearm suicides among adults.
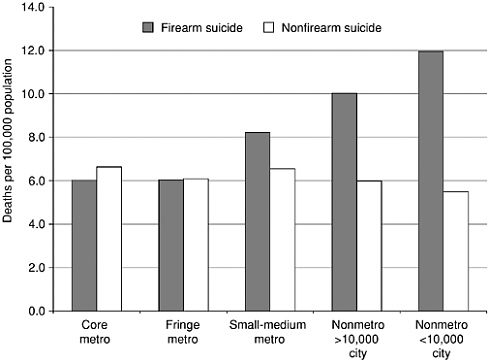
FIGURE 2-4 Suicide Rates by Urbanization and Use of Firearms Among Persons 15–64 Years: United States, 1996–1998. Source: NCHS (2001). Provided by LA Fingerhut.
Limited access to mental health services and to emergency care have been implicated in the increased rates seen in some rural areas. Rural residents suffer higher overall mortality rates from accidents and injuries of all intents because of isolation from care facilities (IOM, 1999). Mental health services are poor in many rural areas (e.g., Howland, 1995) and travel distance to mental health treatment impedes use by rural residents (Fortney et al., 1999, see also Chapter 9).
The reported suicide rates are confounded by the effects of race, sex, and age. A statistical analysis described in Appendix A illustrates an approach to adjust rates for these variables. That analysis reveals that even after accounting for these important demographic variables, considerable spatial variability remains. Again, the highest adjusted rates are typically found in the less densely populated areas of the western United States. The analysis also reveals that there are spatial anomolies; in the western United States and Alaska, where suicide rates are typically high, there are a few counties that have calculated estimates that are consistent with the national average. Similarly, in the central United States, where
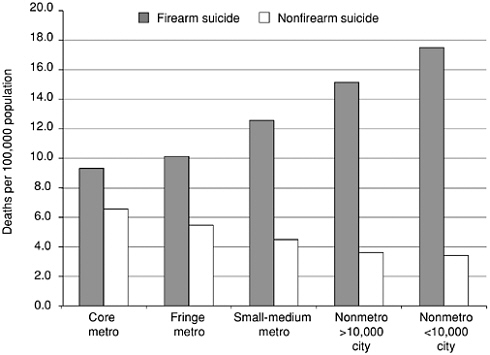
FIGURE 2-5 Suicide Rates by Urbanization and Use of Firearms Among Persons 65 Years and Older: United States, 1996–1998. Source: NCHS (2001). Provided by LA Fingerhut.
there is a high concentration of counties with the lowest suicide rates, there are a few counties that exhibit the highest suicide rates. What are the protective factors that have produced these spatial anomalies? Are these spatial anomalies simply due to reporting bias or some other unmeasured characteristic that has produced the outliers? Examining these spatial anomalies in greater detail is certainly a fruitful area for further research.
POPULATIONS AT RISK
Gender Differences
In western nations such as Greece, Mexico, and the United States, male suicides outnumber female suicides 3- to 5-fold (WHO, 2001a). The gender gap is narrower in Asian nations, where the difference tends to be less than 2-fold. China is singular in this regard, with more female than male suicides, although this gap has narrowed in recent years (WHO, 2001a). Risk factors for suicide differ significantly by gender. Although
women are twice as likely as men to experience episodes of major depression in the United States, they are 25 percent less likely than men to complete suicide (Murphy, 1998). There are several factors that may explain this. Men who are depressed have a higher prevalence of comorbid alcohol and substance abuse than women. Also, men’s depression in later life is more likely to go unrecognized and untreated than women’s depression (Rihmer et al., 1995). Murphy (1998) suggests that men may regard a need for help as a weakness and consequently avoid help seeking; while women may place a higher value on interdependence and consider how their actions will affect others to a greater degree than do men.
A comparison of male and female suicide victims provides additional clues as to the gender differences for completed suicide (Brent et al., 1999). First, females are more likely to engage in suicidal behavior using potentially reversible methods, such as overdose. Second, females are less likely to use alcohol during a suicide completion. Third, alcohol intoxication in the context of a suicide increases the likelihood of use of a gun for completion of suicide in males, but not females.
Youth
Although suicide rates for all age groups have been relatively stable since the 1950s, the reported rate among adolescents has increased markedly. Between 1970 and 1990, the rates for youth aged 15 through 19 nearly doubled; the rate tripled since the mid 1950s. Since 1990, the overall suicide rate for this age group has stabilized at approximately 11 deaths per 100,000. One national school-based study of youth found high one-year prevalence rates for suicide attempts (7.7 percent), ideation (20.5 percent), and making a plan (15.7 percent) (Kann et al., 1998). The increase in the suicide rate is thought to be attributable to an increase in alcohol and substance abuse and increased availability of firearms over this period of time (Brent et al., 1987). Being unemployed or out of school was associated with completed suicide in a large case-control study completed in New York (Gould et al., 1996; Shaffer et al., 1996). In other countries that experienced a dramatic increase in suicide in the past 10 years, such as New Zealand and in the province of Quebec, social change, including diminishing opportunities for employment, is thought to be a primary factor (Beautrais, 2000).
Suicide victims under the age of 30 are more likely to have problems with substance abuse, impulsive aggressive personality disorders, and precipitants such as interpersonal and legal problems (Rich et al., 1986b) than those over 30. Co-occurrences of mental illness, substance abuse, conduct disorder, or all three are significant risk factors for suicide, but
especially in adolescent males (Brent et al., 1999; Shaffer et al., 1996). In general, suicidal behavior is a more impulsive act in younger people. Younger people are less likely to complete a suicide than older people. Even within the adolescent age range, younger adolescents who complete suicide show lower suicidal intent than older ones (Brent et al., 1999; Groholt et al., 1998). Furthermore, youth are more likely to be influenced by media presentations of suicide and to die in cluster suicides1 (although even so, only about 5% of youth suicides occur in clusters; Gould and Shaffer, 1986; Gould et al., 1990; Phillips and Carstensen, 1986).
Guns are the most common mechanism of suicide among youths. In a case-control study of suicide, the availability of guns in the home conveyed the largest risk in adolescents and young adults (Kellermann et al., 1992). A comparison of the suicide rates in Seattle and Vancouver (see also Chapter 8) showed that when gun control was absent (in the United States) youth (15–24) suicide was significantly greater, with 10-fold more suicide by firearms (Sloan et al., 1990).
Moreover, guns in the home, particularly loaded guns, pose up to a 30-fold increased risk for suicide, especially among individuals without major mental disorder (Brent et al., 1993; Kellermann et al., 1992). The rate of psychopathology among younger adolescent suicide victims is much lower than among older adolescents, so that the availability of guns becomes the paramount risk factor for younger, impulsive individuals (Brent et al., 1999; Shaffer et al., 1996).
Elderly
In almost all industrialized countries, men 75 years of age and older have the highest suicide rate among all age groups (Pearson et al., 1997). Of the countries that provide suicide data, Hungary has the highest suicide rates for both elderly men and women: in 1991–1992, the suicide rate for men 75 years and older was as high as 177.5/100,000 (Sartorius, 1996). The lowest rates for both elderly men and women were in Northern Ireland and England/Wales, with rates for men of 20/100,000 and 18/ 100,000, respectively (Schweizer et al., 1988).
In 1990 the United States had a suicide rate of 24.9/100,000 for men aged 75–84. In 1998 the rate had risen to 42.0/100,000. Although older individuals comprise approximately 10% of the U.S. population, they account for 20% of the completed suicides (Hoyert et al., 2001; Hoyert et al., 1999). Men account for about four out of five completed suicides among those older than 65. This is partly explained by the fact that men are more
likely to use more lethal methods. Seventy-six percent of men and 33% of women who completed suicide used firearms, while 3% of men and 33% of women who completed suicide used overdose on medications in the United States (NCHS, 1992).
Risk factors that predispose to suicide differ across the life span. Widowhood (Smith et al., 1988), serious medical illness, and social isolation (Draper, 1994) are more likely to be salient vulnerability factors among older as opposed to younger adults. Whereas affective illness is a vulnerability factor across all age groups (Asgard, 1990; Rich et al., 1986b), the limited findings for dual diagnosis tend to be weak or negative in later life but consistently positive among young people (Asgard, 1990; Barraclough et al., 1974; Rich et al., 1986b). It is important to note that risk factors often co-occur, such as social isolation and depression, or social isolation and drug abuse, or depression and drug abuse. Considerations specific to suicide in the elderly include: (1) the greater likelihood that the elderly will die in or following a suicide attempt; (2) the greater prevalence of indirect self-destructive behaviors such as poor-adherence to treatment regimens in the elderly; and (3) co-morbid conditions that increase suicide risk, including bereavement, depression, and terminal illness.
There is greater likelihood of death in or following a suicide attempt in the elderly. While in younger age groups suicide attempts are more often impulsive and communicative acts, in later life most attempts can be considered “failed suicides.” Older individuals make fewer suicide attempts per completed suicide. The highest suicide attempt to completion rate is in younger women (200:1), compared with 4:1 in the elderly. Suicide attempts in the elderly are more likely to lead to completed suicide than in any other age group: 6% of individuals aged 55 and older died by suicide within a year of a suicide attempt compared to 2% of younger attempters (Gardner et al., 1964). The reasons for this low attempt to completion ratio are complex. The elderly are more medically fragile and frequently live alone, which increases the probability of a fatal outcome. Suicides in older people are often with high intent, long-planned and frequently involve highly lethal methods. The elderly are often less rescuable because of these aspects of their suicidal behavior. Furthermore, suicide methods selected by the elderly are less likely to be affected by short-term modeling effects, such as suicide epidemics. Although most people who kill themselves give direct or indirect warnings, older people are less likely to directly communicate their intent to die. As the elderly are often preoccupied with death and dying, their environment is more likely to miss the indirect warning that they give, such as “nothing is in front of me anymore.” However, contrary to common belief, lack of hope and depression are not part of normal aging, not even in the terminally ill elderly.
Indirect self-destructive behavior in the elderly are particularly notable. In addition to overt suicide attempts, there are subtle behaviors especially in the elderly, with conscious or unconscious intent to die, such as refusal to eat or drink, noncompliance with treatment, or extreme self-neglect. Farberow (1980) used the term “sub-intentional suicide” to refer to indirect self-destructive behaviors which often lead to premature death, and are common in certain settings such as nursing homes (where more immediate means to complete suicide are limited), and among people whose religion forbids suicide. Osgood et al. (1991) found that the rate of completed suicide among elderly nursing home residents was 15.8/100,000 as compared to 19.2/100,000 for elderly living in the community. By contrast they estimated the rate of indirect self-destructive behavior leading to death to be 79.9/100,000 among nursing home residents, and the rate of such behavior not resulting in death to be 227/ 100,000. Kastenbaum and Mishara (1971) found that 44% of men and 22% of women who were hospitalized for chronic medical illnesses exhibited indirect self-destructive behavior during a 1-week period.
Bereavement is an important risk factor in the elderly. The effect of spousal loss on suicidality appears to be the most pronounced in elderly men. In the United States, the highest suicide rate is among bereaved elderly white men: 84/100,000 (NCHS, 1992). Rates of suicidal ideation are also elevated in elderly with complicated or traumatic grief, which differs from bereavement-related depression and includes PTSD-like symptoms (Szanto et al., 1997).
Although chronic physical illness has been associated with an increased suicide risk in depressed patients (Duggan et al., 1991), depression and not physical illness differentiated elderly suicide completers from non-completers (Conwell et al., 2000). A 1-year follow-up study of psychiatric register cases observed that depressed patients aged 55 years or older had more than twice the rate of suicide (475/100,000) than younger depressed patients (207/100,000) (Gardner et al., 1964). In the 60–90 year old age group, the rates of suicide attempts associated with untreated mood disorders increase with each subsequent decade (Bostwick and Pankratz, 2000). Psychological autopsy studies have found depression to be the most common psychiatric diagnosis in elderly suicide victims, while alcoholism is the most common diagnosis in younger adults (Conwell and Brent, 1996; Dorpat and Ripley, 1960). Conwell and Brent (1996) reported that 76 percent of elderly suicide victims had diagnosable psychopathology, including 54 percent with major depression and 11 percent with minor depression.
Seventy percent or more of elderly suicide victims were seen by their primary care physician within one month from their death (Barraclough et al., 1971; Conwell, 1994; Miller, 1976). Terminal illness needs to be
considered when assessing risk factors, particularly in the elderly, although only 2–4 percent of terminally ill elderly complete suicide. Suicidal ideation is rare without depression even in the terminally ill. Untreated or under-treated pain, anticipatory anxiety regarding the progression of medical illness, fear of dependence, and fear of burdening the family are the major contributing factors in the suicidality of elderly with medical illness. Adequate management of chronic pain decreases the request to die among cancer patients (Foley, 1991). When pain and depression are adequately treated, most previously suicidal elderly express a wish to live (Hendin, 1999). In one study, two-thirds of the patients who requested euthanasia changed their minds during a 2-week follow-up period (Hendin, 1999).
Race and Ethnicity
Suicide, like many health outcomes, varies widely across different racial and ethnic groups in the United States (IOM, 2002). Over the last twenty years, when considering all age groups and both sexes, whites and Native Americans have the highest suicide rates, varying from approximately 11 to 14 per 100,000 (NCIPC, 2000). Asian-Pacific Islanders and African-Americans and Hispanics2 have rates at approximately half— averaging 6.14 to 6.53 per 100,000 across this same time-span (NCIPC, 2000). These differences are even more complex when examined by gender (Figure 2-6), as well as age group. Mining the reasons underlying such differences may hold important information for reducing suicide (Chapter 6). Below we discuss the differences in suicide rates for African Americans and Native Americans in greater detail.
African-Americans
The rate of suicide among African Americans has historically been lower than that of whites, but in young black males the gap has been gradually closing (see Table 2-2; Griffith and Bell, 1989). In fact, the rate of increase in young black males has been a cause for concern. From 1980 to 1995, the suicide rates for black youth ages 10–19 increased from 2.1 to 4.5 per 100,000—an increase of 114 percent. For comparison over the same time, the rates in white males of the same ages increased from 5.4 to 6.4 per 100,000. The suicide rate increased the most for blacks ages 10–14 years (233 percent; CDC, 1998). The convergence of black and white rates was more dramatic with different age groups. For example in 1986 in
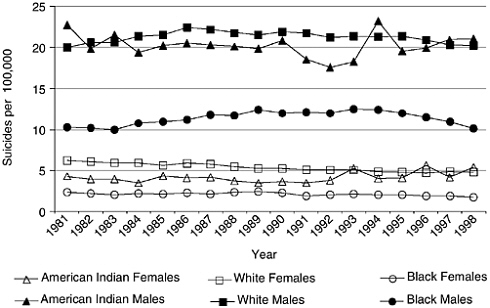
FIGURE 2-6 Suicides Rates by Race and Gender: United States, 1981–1998. Source: NCIPC (2000).
black men 25–34 the rate (20/100,000) was nearly the same as in the same aged white male (26/100,000) (Griffith and Bell, 1989; Hollinger et al., 1994). In 1993 for ages 25–34 the suicide rates for white men was 25.6/ 100,000 and for black men was 24.0/100,000.
The suicide rates for black women are remarkably low. The suicide rates among black women have held steady at about 2/100,000 for the past two decades (Griffith and Bell, 1989). The difference between black and white women is diminished when suicide attempts, rather than completed suicides are considered. The suicide rate among elderly black men is also strikingly low, in dramatic contrast to elderly white men. For men over 65, the rates are currently approximately 12/100,000 in African Americans compared to 37/100,000 in white men (NCIPC, 2000).
The rising rates among African American males has been noted with considerable concern. As early as 1938, Prudhome (1938) predicted that as Blacks acculturated into White middle class society, their suicide rates would go up. In support of this hypothesis, Clark (1965) noted that the suicide rates in Harlem were half those of New York City rates, but there were three middle class black communities in Harlem where the suicide rates were equal to the city as a whole. Others have suggested that young black men, like elderly white men, feel that society has no place for them (Bell, 1986; Bell and Clark, 1998; Robins et al., 1977).
TABLE 2-2 Suicide Rate per 100,000 for Young (15–24) Black and White Males
|
Year |
Black |
White |
|
1989 |
16.63 |
22.48 |
|
1990 |
15.13 |
23.19 |
|
1991 |
16.43 |
23.08 |
|
1992 |
17.92 |
22.68 |
|
1993 |
20.00 |
23.07 |
|
1994 |
20.53 |
23.94 |
|
1995 |
17.94 |
23.34 |
|
1996 |
16.72 |
20.99 |
|
1997 |
16.00 |
19.64 |
|
1998 |
14.98 |
19.28 |
The statistical analysis using detailed county-level data (as described in Chapter 10 and Appendix A) can be applied to the question of the rise in rate of suicides in young black males. Comparing suicide rates in young white and black males, ages 15–24, from 1989–1998 reveals that the overall suicide rates have been decreasing over the past ten years and that, in 1989, the suicide rate in white males was significantly larger than the suicide rate in black males. However, the rate of young black suicides was increasing relative to young white males over the past 10 years. The increase in young black suicides was largest in 1993 and 1994, but has decreased somewhat since then.
The low rates of suicide among African Americans, especially women, has also been subject to some debate. Spirituality is one of the leading hypotheses regarding the low rates of suicide among black women. This may extend some protection to black males. While almost half the whites believed that suicide is sometimes justified, only one-fifth of blacks did (Robins et al., 1977). Furthermore, fewer whites believe in an after-life. One might also propose that similar to young white males, young black males may have more secular attitudes toward suicide and an after-life, but these attitudes change with age as black men mature. Another suggestion put forward (Comer, 1973) is that black women’s connections to community institutions such as the black church would protect black women from suicide. In fact, two-thirds of the African-American respondents to a National Mental Health Association (NMHA) survey on attitudes and beliefs about depression reported that they believed prayer and faith alone will successfully treat depression “almost all of the time” or “some of the time” (NMHA, 2000).
Since mental illness is a risk factor for suicide (see Chapter 3), the high prevalence of mental disorders among African-Americans compared with
Whites must be considered. In the Epidemiologic Catchment Area study (ECA) of the 1980s, African Americans had higher levels of any lifetime or current disorder than whites (Robins and Regier, 1991). This was true both over the respondent’s lifetime (Robins and Regier, 1991) and over the past month (Regier et al., 1993). When the ECA study and the more recent National Comorbidity Survey (NCS) (Kessler et al., 1994) took into account differences in age, gender, marital status, and socioeconomic status, the black–white difference was eliminated.
The impact of these findings on suicide is difficult to discern, especially in light of the findings of the NMHA (2000) survey on attitudes and beliefs about depression in the African-American community. This survey revealed that the majority think depression is a “personal weakness” and only a third (compared to 69% of the general population) recognize depression as a “health problem” for which they would be willing to take prescribed medication. For further discussion of these issues, see Chapter 6, and the sections in Chapter 7 on faith-based interventions, and Chapter 9 on barriers to treatment.
Native Americans3 and Alaska Natives
The rate of suicide among Indians and Alaska Natives of the United States is about 1.7 times the rate of the nation as a whole (Indian Health Service, 1999). Between 1975 and 1977 the rates peaked at 22.5/100,000 and decreased to a low of 16.0 in 1984 through 1986. Since then it increased to its current rate of 19.3 per 100,000 in 1995 (Indian Health Service, 1999). In contrast, over the past 40 years, rates of violence have generally declined for American Indians (Hisnanick, 1994). Suicide takes a significant toll.
As illustrated in Figure 2-6, suicide deaths for American Indian males are substantially higher overall than for other ethnic groups. They also show a different pattern across the life-span. For ages 5 through 14 the suicide rate is three times higher for Indian males than the general population, ages 15 through 34 years it is 2.5 times higher, and for ages 35 through 44 years it is 1.5 times higher (Indian Health Service, 1999). The male rate peaks at 67 per 100,000 in ages 25–34, and is somewhat lower for the next youngest age group (15–24) at 54 per 100,000. However, by age 45 Indian males complete suicide at a rate that is approximately the same as
males in the general population. Over the age of 55 the rate declines dramatically to half that of general population males. For Indian and Alaska Native males, the risk is highest in the young years but tapers off substantially in the older years, the very years when white males most commonly complete suicide.
Young Indian females (5–34) have rates of suicide that are 2.2 to 3.6 times higher than females in the general population. For example, for ages 15–24 the rate is 11/100,000. However, by 35 through 44 years, the rate is 1.5 times the general population, and 45 years to 75 years is approximately the same as or slightly less than the general female population. At 55–75, the rate is 5/100,000. American Indian women 75 years of age and older do not complete suicide with any measurable frequency. Therefore, while Indian and Alaska Native females have substantially lower rates than Indian and Alaska Native males, their rates are higher than other women in the country until age 44, and then they are approximately the same until age 75, when suicides no longer occur (Indian Health Service, 1999).
The decrease in Indian suicide during the early 1980s has been attributed to the changing denominators in the United States, stemming from better enumeration of Indians in Census data and an increased tendency for self-identification as Indian or Native. But the more stable and easily-monitored data from the State of New Mexico, where neither of these phenomena have occurred over the same time period, has also shown a definite and similar reduction in incidence of suicide among Indians. Among the three major Indian cultural groups (the Navajo, Pueblo, and Apache) in the late 1980s, a substantial drop occurred and a leveling of rates was evident in the 1990s (New Mexico Vital Records and Health Statistics, 2000; VanWinkle and May, 1993). In fact, the aggregate rates for the nineteen Pueblo Indian tribes have continued to drop throughout the 1990s (VanWinkle and Williams, 2001).
Among American Indian and Alaska Native suicide, gunshot wounds, hanging, and other violent means predominate (Wallace et al., 1996). American Indians also have high rates of other violent deaths including motor vehicle crashes (Guerin, 1991; Guerin, 1998; Jarvis and Boldt, 1982; Katz and May, 1979; May, 1989), a small percentage of which are believed to be covert suicides (Hackenberg and Gallagher, 1972; May, 1987; Stull, 1972; Stull, 1973; Stull, 1977; Wills, 1969). In studies of Alaska Natives, firearms have been the predominant method of suicide at 75 to 85 percent (Forbes and Van Der Hyde, 1988; Hlady and Middaugh, 1988; Kost-Grant, 1983), as in studies of the American Plains, and 55 percent in the American Southwest during the same period (Shuck et al., 1980; VanWinkle and May, 1986; VanWinkle and May, 1993). In Canada the same pattern prevails where firearms account for 55 to 82 percent (Butler,
1965; Garro, 1988; Jarvis and Boldt, 1982; Spaulding, 1985–1986). Hanging is the second most common cause of suicidal death among Indians and Alaska Natives in most studies in most areas of the continent (Kraus, 1974; Wallace et al., 1996; Wissow, 2000). The range is great, with hanging accounting for an unusually low 7 percent in one study to a more usual 26–40 percent in others (Butler, 1965; Garro, 1988; Spaulding, 1985–1986; VanWinkle and May, 1993). In a state like New Mexico, suicide by firearms and hanging combined account for over 90 percent of all American Indian suicides (VanWinkle and May, 1993).
Social and familial disruption, cultural conflict, and social disorganization are often cited as major influences on American Indian suicide rates. Suicide rates among American Indians vary with the degree of social and cultural change and acculturation pressure (Garro, 1988; Levy, 1965; VanWinkle and May, 1986; 1993). The high suicide rates among youth in Indian families and communities have been attributed to acute acculturation stress (Levy, 1965; May and Dizmang, 1974; Spaulding, 1985–1986; Travis, 1984; VanWinkle and May, 1986; 1993), cultural conflict (Kahn, 1982; Kettl and Bixler, 1991; Opler, 1969; Patterson, 1969) and social disorganization (EchoHawk, 1997; Expert Working Group, 1994; Joe, 2001; Resnik and Dizmang, 1971). While American Indian and Alaska Native adolescents face the same turmoil as mainstream youth, they are also challenged by self-identity and actualization in their minority status and complex choices as to whether to adhere to mainstream or traditional, native culture (Bechtold, 1994; Howard-Pitney et al., 1992; Sack et al., 1994; U.S. Congress, 1990). The stress of these dilemmas can increase the risk of alcohol or drug abuse, depression or other psychopathology, and parasuicidal and suicidal behavior (Beauvais, 1998; Elliot et al., 1990; Kettl and Bixler, 1993; Manson et al., 1989; May, 1982; Norton et al., 1995; Prince, 1988; Sack et al., 1994).
Immigrants and Refugees
Between 1980 and 1991 the United States immigrant population tripled; almost 20 million immigrants resided in the United States in 1990. Suicide in immigrants is a public health concern because this population is subject to many sociocultural risk factors. Immigration also provides opportunities to study the impact of culture and environment on prevalence of mental illness and suicide. In general, suicide rates tend to reflect that of the country of origin, with convergence toward that of the host country over time (Singh and Siahpush, 2001).
A careful review of the data on immigrants reveals some interesting patterns, which may differ across nations. Higher suicide rates have been reported for immigrants to some countries. For example, Finnish immi-
grants in Sweden had a higher rate of suicide (similar to that in Finland) than native-born Swedes and other immigrants. Social isolation and low social class acted as confounding factors, although they do not completely account for the increased rates (Ferrada-Noli et al., 1995). A comparison of suicide rates in high- and low-income areas of Stockholm county revealed the highest suicide rates in the low-income areas, regardless of ethnicity, though low-income immigrants still completed suicide at higher rates (Ferrada-Noli and Asberg, 1997). In contrast, immigrants to the United State have lower or comparable rates to native-born individuals. In their review of death certificates from 1970 to 1992 in California for 15– 34 year olds, Sorenson and Shen (1996) found that although foreign-born individuals had significantly higher rates of homicide deaths, they had fewer suicides. This study did not control for demographic variables, however. Singh and Siapush (2001) reviewed national death certificate data investigating all-cause and cause-specific mortality of foreign-born versus native-born in the United States, controlling for the demographic factors sex, race/ethnicity, age, income, and education. They found that foreign-born males had 52 percent lower suicide rate than U.S.-born males when demographic variables were controlled. On the other hand, demographically adjusted suicide rates for foreign-born females did not significantly differ from that of native-born U.S. females. While some studies in Britain and Australia found a similar concordance of foreign- versus native-born suicide rates in women (e.g., Morrell et al., 1999), others have found increased suicides and suicide attempts in female immigrants compared to their male counterparts or to native-born females (Merrill and Owens, 1988; Patel and Gaw, 1996).
Research on immigration and suicide has initiated contextual psychological studies on the stresses of immigration as related to suicidality. These studies all involved immigrants to the United States unless otherwise noted. Hovey and King (1997) for example, expanded previous models of acculturation (i.e., Williams and Berry, 1991) to include the development of depression and suicidality. Aspects of acculturative stress include disrupted social support and family support networks, low education and income, lack of knowledge of the language and culture of the new country, motives for immigrating, spiritual beliefs, tolerance of the host country toward immigrants, and positive or negative views of the acculturative process itself. Studies of various Hispanic and Asian immigrant groups demonstrate that lack of English skills predicts distress, depression, and suicidal ideation among immigrants, sometimes over and above the effects of pre-arrival trauma (Hinton et al., 1997; Hovey, 2000a; Hovey, 2000b). Spiritual beliefs, social support, and marital status, protective factors and processes (see Chapter 6), appear to buffer the effects of
acculturation stress on suicidality both in the United States (Hovey, 1999) and in Israel (Hinton et al., 1997; Hovey, 2000b; Ponizovsky et al., 1997). Disagreement with the decision to migrate and expectations for the future have predicted depression and sucidial ideation in samples of Hispanic immigrants (Hovey, 2000a; 2000b).
Guarnaccia and Lopez (1998) note that since children do not wield the power to decide whether to migrate, those children with refugee experiences and those whose families evidence significant migratory stress likely represent a particularly vulnerable group. In corroboration, Tousignant and colleagues (1999) note that familial variables such as father’s long-term unemployment after migration correlates with youth psychopathology. Two recent reports from the National Academies (NRC 1998; 1999) provide in-depth analyses of the physical and mental health of immigrant children in the United States.
Refugee status among immigrants is often associated with trauma. Recent Southeast Asian and Central American immigrants represent refugee populations with high prevalence of trauma exposure who have increasingly immigrated to the U.S. (Holman et al., 2000; Hovey, 2000a; O’Hare and Van Tran, 1998). While various studies show Mexican-born and overall numbers of Asian-born immigrants attempt and complete suicide less frequently than their American-born peers (Shiang et al., 1997; Sorenson and Golding, 1988; Sorenson and Shen, 1996), studies have not differentiated between suicide rates of Central American versus other Hispanic or Southeast Asian versus other Asian immigrants. Some studies document higher rates of Posttraumatic Stress Disorder (PTSD), depression, and anxiety in these sub-groups (Hinton et al., 1997; Hovey, 2000a). Given the relationship between such disorders and suicide (see Chapter 3), studying suicidality in these populations is likely pertinent.
Incarcerated Populations
Suicide rates for jail inmates are 9 times greater than that of the general population (Hayes, 1989) and 15 times higher for men alone. For example, in county jail rates are 107 per 100,000. Most suicide victims in jails of all types and sizes (e.g., rural and urban county jails, city jails, and police department lock-ups) are young white males arrested for nonviolent offenses and intoxicated upon arrest (Hayes, 1998). Suicide was usually by hanging within 24 hours of incarceration (Hayes, 1989). Patterns in prisons were similar but considerably lower than in jails, about 1.5 times higher than in the general population (Anno, 1985; Anno, 1991).
The reasons for the higher rate of suicide in jails and prisons are unclear. However, mental illness, a strong risk factor for suicide (see Chapter 3), is prevalent in correctional facilities.
Studies in jails and prisons estimate that between 6 and 15 percent of the population have serious and persistent mental illnesses (Bland et al., 1990; Brooke et al., 1996; Jemelka et al., 1989; Manderscheid and Sonnenschein, 1999; Morrissey et al., 1993; National Commission on Correctional Health Care, 2000; Steadman et al., 1987; Taylor and Gunn, 1984; Veysey and Bichler-Robertson, 1999). In jails, prevalence rates of mental illness are two to three times higher than those in the general population (Teplin, 1990). In prison, with the longer terms, nearly 10 percent of state prison inmates received some form of mental health counseling or psychotherapy from a physician, nurse, psychologist, or social worker (Morrissey et al., 1993). State and federal prisons have a minimum of 13 percent who will require psychiatric care for an acute episode of serious mental illness at some time during their incarceration (National Commission on Correctional Health Care, 2000).
In addition, more than 30 percent of male mentally ill inmates and 78 percent of females reported prior physical or sexual abuse (Ditton, 1999), another risk factor for suicide (see Chapter 5). Mentally ill in correctional facilities are more likely than other offenders to have a higher prevalence of homelessness, unemployment, alcohol and drug abuse, and physical and sexual abuse before their current incarceration (US DHHS, 2001). These risk factors are likely to contribute to the prevalence of suicide among those incarcerated.
Occupations at Risk
Several professions (e.g. police, doctors, dentists) have been noted as having suicide rates that are higher than the population averages. These assessments, however, are confounded by demographic variables including age, sex, socioeconomic class and marital status, all of which affect suicide rates independently from occupation (Stack, 2001). For example, suicide rates for elementary school teachers are 44 percent lower than the general population, but this difference is not significant when controlling for gender (Stack, 2001).
Models of occupation’s influence on suicidality propose stressors and access to lethal means as the causal variables. Stressors includes level of prestige and dependency on a client base (e.g., Labovitz and Hagedorn, 1971). Holding infrequent roles, such as female chemists and soldiers, or other rare roles, appears to increase suicide rates, as well (Bedeian, 1982; Seiden and Gleiser, 1990; Stack, 1995). Studies regarding the effect of availability of lethal means such as firearms or lethal drugs on suicide rates for certain occupations have found inconsistent results, though the evidence is stronger for medical professions (see Stack, 2001 review).
Higher rates of suicide are more frequent in occupations of lower prestige, class, and salary (Boxer et al., 1995). When demographic factors of race, gender, age, and, particularly, marital status are controlled, this relationship between manual labor occupations and suicide does not remain significant (Charlton, 1995; Stack, 2001). In fact, Stack’s (2001) recent study found that clerks are 15 percent and farm workers 30 percent less likely to complete suicide after controlling for demographic variables.
A population-based study from Denmark examining the income-suicide relationship suggests that for higher income/occupational level, hospital admission for serious mental illness may be associated with greater suicide risk (Agerbo et al., 2001). These investigators speculate that those in prestigious occupations may face greater stigma, and may have greater illness severity before hospital admittance due to delaying treatment. A smaller study in the United States found similar results with high education level (Martin et al., 1985). A large, prospective Finnish study found fewer violent suicides and greater admissions for psychoses among those in higher occupational levels (Koskinen et al., in press).
Health professions carry increased suicide risk independently from demographic factors. Adjusted odds ratios for suicide have been calculated as 5.4 for dentists, 2.3 for physicians, and 1.6 for nurses (Stack, 2001). The reasons for high suicide risk within medical professions remain unclear; these occupations are largely client-dependent and afford easy access to lethal methods. Mathematicians and scientists, artists, and social workers also appear to experience occupation-related increased suicide risk (Stack, 2001).
The police force has often been cited as at higher risk for suicide, but closer examination reveals inconsistent results. A few controlled studies (e.g., Schmidtke et al., 1999) show moderately increased suicide rates for police that vary according to region and across time (Hem et al., 2001). Violanti and colleagues (1998) conducted a cohort mortality survey from 1950 to 1990 and found higher than expected mortality rates among male officers for all-cause mortality, including suicide. When compared to other working-age men, as opposed to the general population, however, police appear to have only a slightly increased suicide risk (Burnett et al., 1992; Hem et al., 2001; Stack and Kelly, 1994).
Sexual Orientation
Fewer than 5 percent of adults in the United States identify themselves as homosexual or bisexual (Michaels, 1996). This population faces societal stigma, discrimination, and violence victimization, among other stressors (Faulkner and Cranston, 1998; Herek, 1996; Hershberger and
D’Augelli, 1995). Awareness of their exposure to stressful events has spawned a growing research literature on whether they face an increased risk of suicidality.
Young homosexual or bisexual males are at greater risk than heterosexuals for suicide attempts, but findings are less clear regarding suicide completion (McDaniel et al., 2001). According to two population-based studies in San Diego (Rich et al., 1986a) and New York City (Shaffer et al., 1995), rates of suicide completion do not appear to be higher for gay men and lesbians than for heterosexuals. These two studies were the first psychological autopsy studies to assess retrospectively the sexual orientation of those who completed suicide. Such assessment can be inaccurate because individuals may conceal their sexual orientation and because baseline prevalence for homosexuality in the relevant comparison population is difficult to obtain. A recent review of these studies determined that firm conclusions were unwarranted (McDaniel et al., 2001).
For suicide attempts, several recent population- and school-based studies provide strong support for a relationship between sexual orientation and suicidal behavior in males. Population-based studies of homosexual or bisexual males (ages 18 to 40 or so) found them to be 5–14 times more likely than heterosexual males to have reported a suicide attempt (Bagley and Tremblay, 1997; Cochran and Mays, 2000). Similarly, five studies of high school students in several states found elevated rates of suicide attempts among males engaging in same-sex behavior compared to their heterosexual peers (DuRant et al., 1998; Faulkner and Cranston, 1998; Garofalo et al., 1998; Garofalo et al., 1999; Remafedi et al., 1998), with relative risk calculated at 2- to 5-fold. Strikingly, most of the school-based studies among gay or bisexual adolescents found about 30 percent had attempted suicide. In young adult and middle-aged homosexuals, the prevalence is lower but still significantly elevated compared to controls (Cochran and Mays, 2000; Herrell et al., 1999).
Most studies on suicidality in homosexuals document the elevation of risk in young males (McDaniel et al., 2001), not young females. This contrasts with the general population, in which female teenagers and young adults attempt suicide more frequently than do males. The reasons for this reversal are not well understood (McDaniel et al., 2001). However, a recent nationally representative study (Russell and Joyner, 2001) of adolescents found increased risk for suicide ideation and attempts for both males and females when factors such as depression, hopelessness, and substance use were controlled. The authors speculate this difference may have arisen because the study measured self-reported same-sex romantic attraction/relationships, not self-identification as gay or lesbian.
Several studies explored the reasons behind the elevated risk of suicidality in homosexual or bisexual men. A longitudinal study of chil-
dren from New Zealand (birth to age 21) found that gay, lesbian, and bisexual youth had higher risk not only of suicidal behavior, but also of depression, anxiety, substance abuse. The increased risk was greatest (a 6-fold increase) for suicide behavior and having multiple mental disorders (Fergusson et al., 1999). Harrell et al. (1999) used a co-twin control method to assess suicidality in relation to sexual orientation. They found that middle-aged male twins reporting same-gender sexual orientation were at higher risk for several lifetime measures of suicidality. The strong association could not be explained by abuse of alcohol and other substances, by depressive symptoms, or by unmeasured genetic and familial factors. The contribution of unique risk factors such as disclosure of sexual orientation to friends and family (McDaniel et al., 2001) remains to be fully assessed.
LIMITATIONS OF DATA
Official suicide rates capture completed suicides only. They have been used to chart trends in suicide, monitor the impact of change in legislation, treatment policies, and social change, and to compare suicides across regions, both within and across countries. In addition, suicide rates have offered a way to assess risk and protective factors for geographical areas (counties, states, and countries). However, official suicide statistics are fraught with inaccuracies. Undetermined cases and open verdicts and under-reporting limit their strength. The methodological weaknesses and promising approaches to resolve them are discussed more fully in Chapter 10. In brief, there are four primary sources of variability in suicide statistics (Jobes et al., 1987; O’Carroll, 1989). First, there are regional differences in the definition of suicide and in how ambiguous cases are classified. Legally a classification of suicide requires that it be beyond a reasonable doubt (O’Donnell and Farmer, 1995). Second, there are regional differences in the training and background of the coroner or medical examiner. Third, there are differences in terms of the extent to which cases are investigated. Fourth, there are sources of variability that have to do with the quality of data management involved in preparing official statistics. In fact, in many developing countries, suicide statistics are imputed, rather than based on actual death registries (Kleinman, 2001). This is discussed further in Chapter 6.
COST TO SOCIETY
The emotional cost of suicide is severe, and for family and friends of suicide victims, the personal loss is paramount. There is an additional economic cost that society incurs with these untimely deaths. The eco-
nomic4 cost of suicide encompasses four factors. (1) Medical expenses of emergency intervention and non-emergency treatment for suicidality. These medical costs are not borne by the health care industry alone, but by all of society through higher health care costs that are ultimately passed on to workers and taxpayers. (2) The lost and/or reduced productivity of people suffering from suicidality. (3) The lost productivity of the loved ones’ grieving a suicide. (4) Lost wages of those completing suicide, with the greatest absolute numbers of suicides occurring before retirement. Even if the analysis is restricted to the estimate of lost wages of suicide victims, the financial impact of suicide is enormous. By doing this analysis, the Committee found that for suicide in 1998 alone, the value of lost productivity was calculated to be $11.8 billion (in 1998 dollars). The basis of this analysis is described below.
Lost productivity was defined as the discounted present value of expected future age-, sex- and race-specific earnings. The average annual earnings by age, race/origin, and sex were estimated from the March 1998 supplement to the Current Population Survey (Bureau of Labor Statistics, 1998). The Current Population Survey (CPS) is a monthly survey of about 50,000 households conducted by the Bureau of the Census for the Bureau of Labor Statistics. The March supplement CPS contains detailed information on income and work experience in the United States. In constructing our estimates of average annual earnings, we did not weight observations by their probability of being sampled for the CPS. This should not have much impact on the representativeness of our estimates, except in cases where there were a very small number of observations in a stratum (e.g., the average annual earnings of female Asian/Pacific Islanders, 85 years old and over was based on seven observations in this stratum). Even in such cases, the lack of sample weighting in estimating earnings is not likely to have a meaningful influence on the overall estimate of lost productivity due to suicide. Average annual earnings were estimated for the mid-point age of each of seven age intervals: 15–24 years old, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85 and over. In addition, it should be noted that this estimate using the cross-sectional perspective probably underestimates the real economic loss from suicide for two reasons. First, real wages are likely to rise over time. Second the non-market productivity of older persons (for example in caring for a disabled spouse) has also not been included in this analysis of the cost of suicide.
We used five mutually exclusive categories of race/ethnicity: white non-Hispanic, black-non-Hispanic, American Indian/Aleutian/Eskimo
non-Hispanic, Asian/Pacific Islander non-Hispanic, and Hispanic of any race. Next, we estimated the present value of future earnings by discounting and summing the stream of expected annual earnings. Race- and sex-adjusted life expectancy at the mid-point of each age interval was taken from the 1998 U.S. Life Tables (Anderson, 2001). This method of estimating future earnings is based on a cross-sectional perspective, rather than a longitudinal birth cohort perspective. For example, the 1998 earnings of a 60 year old black man are used to estimate the annual earnings of a 50 year old black man 10 years later. Future earnings were discounted at an annual rate of 3 percent to yield their present values. This is based on the real value of the short-term United States T-bill, in an effort to approximate the risk-free time-value of money.
To estimate the total lost earnings due to suicide, we multiplied the number of suicides in each age/sex/race group (data from the National Center of Disease Control’s WISQARS™, Web-based Injury Statistics Query and Reporting System) in 1998 by age-, sex-, race-specific estimated future earnings and summed across groups. As described above, the cost of lost earnings from suicide in just the one year (1998) was calculated to be $11.8 billion.
A similar analysis was done for suicides in New Brunswick, Canada, during 1996 (Clayton and Barcelo, 1999). The direct costs (health care services, autopsies, funerals, and police investigations) for the 94 reported suicides came to $535,158. Indirect costs, which include the lost productivity, came to $79,353,354 for a mean total cost per suicide death in 1996 of $849,878. For 30,000 deaths each year, this totals about 25 billion dollars.
Although the issue can be raised that any premature death (e.g., from smoking) can save society money (Viscusi, 1995), the Committee decided not to even broach this argument, considering it contrary to the goals of public health and morally unacceptable.
FINDINGS
-
Suicide rates vary widely across demographic groups. African Americans have had significantly lower rates historically than whites despite higher incidence of major risk factors. The rates of completed suicide are particularly low among African American women. In contrast, the suicide rates among Native Americans have been and continue to be extremely high. Older white males have the highest rate in the United States. Males have higher rates across the globe except in rural China where women complete suicide at a higher rate.
-
The suicide rate in the United States has remained relatively unchanged for the last 50 years. The rate for youth in the United States,
-
however, has been increasing. While the rates in African American adolescents has increased through the 1990s, the rates appear to have leveled off.
-
The differences in suicide rates among ethnic groups in the United States, among immigrant populations, and among countries throughout the world point to the influence of social and cultural factors. Risk factors vary in their importance for different groups. Youth suicide is more highly associated with impulsiveness than for other age groups. On the other hand, older persons are at greater risk for completing suicide because of the seriousness of the intent and social isolation.
Studies of the differences in the risk of suicide among populations can enhance our understanding of the impact of risk and protective factors. This is best accomplished by collection of specific data from well defined and characterized populations whose community level social descriptions are well known, which would allow the integration of population-based approaches with studies of individual characteristics.
-
Suicide rates vary across geographic region. Rates are lower in more densely populated areas around the world. When rates within the United States are analyzed county by county, striking variations in some adjacent counties are revealed. This approach bridges traditional sociological and anthropological studies that use ecological data and case controlled approaches that examine individual risk factors for suicide.
Future studies could identify social factors that differ between two communities that are adjacent, or otherwise similar, but have dramatically different suicide rates. This approach could provide more precise assessments of the roles of social factors in suicide including public health issues such as access to and the quality of health care.
-
Costs to Society: The annual cost of lost productivity due to suicide deaths was calculated to be $11.8 billion (in 1998 dollars). This does not include medical care costs, or costs incurred by loss of productivity of either those suffering from suicidality or the close family and friends of a suicide victim.
REFERENCES
Agerbo E, Mortensen PB, Eriksson T, Qin P, Westergaard-Nielsen N. 2001. Risk of suicide in relation to income level in people admitted to hospital with mental illness: Nested case-control study. British Medical Journal, 322(7282): 334-335.
Anderson RN. 2001. United States Life Tables, 1998. National Vital Statistics Report, 48(18): 1-40.
Anno BJ. 1985. Patterns of suicide in the Texas Department of Corrections, 1980-1985. Journal of Prison and Jail Health, 2: 82-93.
Anno BJ. 1991. Prison Health Care: Guidelines for the Management of an Adequate Delivery System. Washington, DC: U.S. Department of Justice, Department of Corrections.
Asgard U. 1990. A psychiatric study of suicide among urban Swedish women. Acta Psychiatrica Scandinavica, 82(2): 115-124.
Bagley C, Tremblay P. 1997. Suicide behaviors in homosexual and bisexual males. Crisis, 18(1): 24-34.
Barraclough B, Bunch J, Nelson B, Sainsbury P. 1974. A hundred cases of suicide: Clinical aspects. British Journal of Psychiatry, 125: 355-373.
Barraclough BM, Nelson B, Bunch J, Sainsbury P. 1971. Suicide and barbiturate prescribing. Journal of the Royal College of General Practitioners, 21(112): 645-653.
Beautrais AL. 2000. Risk factors for suicide and attempted suicide among young people. Australian and New Zealand Journal of Psychiatry, 34(3): 420-436.
Beauvais F. 1998. American Indians and alcohol. Alcohol Health and Research World, 22(4): 253-259.
Bechtold DW. 1994. Indian adolescent suicide: Clinical and developmental considerations. American Indian and Alaska Native Mental Health Research Monograph Series, 4: 71-80.
Bedeian AG. 1982. Suicide and occupation: A review. Journal of Vocational Behavior, 21(2): 206-223.
Bell CC. 1986. Impaired black health professionals: Vulnerabilities and treatment approaches. Journal of the National Medical Association, 78(10): 925-930.
Bell CC, Clark DC. 1998. Adolescent suicide. Pediatric Clinics of North America, 45(2): 365-380.
Beratis S. 1991. Suicide among adolescents in Greece. British Journal of Psychiatry, 159: 515-519.
Birckmayer J, Hemenway D. 2001. Suicide and firearm prevalence: Are youth disproportionately affected? Suicide and Life-Threatening Behavior, 31(3): 303-310.
Bland RC, Newman SC, Dyck RJ, Orn H. 1990. Prevalence of psychiatric disorders and suicide attempts in a prison population. Canadian Journal of Psychiatry, 35(5): 407-413.
Bostwick JM, Pankratz VS. 2000. Affective disorders and suicide risk: A reexamination. American Journal of Psychiatry, 157(12): 1925-1932.
Boxer PA, Burnett C, Swanson N. 1995. Suicide and occupation: A review of the literature. Journal of Occupational and Environmental Medicine, 37(4): 442-452.
Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. 1999. Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child and Adolescent Psychiatry, 38(12): 1497-1505.
Brent DA, Perper JA, Allman CJ. 1987. Alcohol, firearms, and suicide among youth: Temporal trends in Allegheny County, Pennsylvania, 1960 to 1983. Journal of the American Medical Association, 257(24): 3369-3372.
Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C. 1993. Firearms and adolescent suicide. A community case-control study. American Journal of Diseases of Children, 147(10): 1066-1071.
Brooke D, Taylor C, Gunn J, Maden A. 1996. Point prevalence of mental disorder in unconvicted male prisoners in England and Wales . British Medical Journal, 313(7071): 1524-1527.
Bureau of Justice Statistics, U.S. Department of Justice. 2001. Homicide Victimization, 1950– 1999. [Online]. Available: http://www.ojp.usdoj.gov/bjs/ [accessed October 12, 2001].
Bureau of Labor Statistics, U.S. Department of Labor and Bureau of the Census, U.S. Department of Commerce. 1998. Current Population Survey, Annual Demographic Supplement.
Bureau of the Census. 1976. Historical Statistics of the United States: Colonial Times to 1970, Part 1. Washington, DC: U.S. Department of Commerce.
Burnett C, Boxer P, Swanson N. 1992. Suicide and Occupation: Is There a Relationship? Cincinnati, OH: National Institute for Occupational Safety and Health.
Butler GC. 1965. Incidence of suicide among ethnic groups of the Northwest Territories and Yukon Territory. Medical Services Journal of Canada, 21(4): 252-256.
CDC (Centers for Disease Control and Prevention). 1998. Suicide among black youths— United States, 1980–1995. Morbidity and Mortality Weekly Report, 47(10): 193-196.
Charlton J. 1995. Trends and patterns in suicide in England and Wales. International Journal of Epidemiology, 24 (Suppl 1): S45-S52.
Clark K. 1965. Dark Ghetto. New York: Harper and Row.
Clayton D, Barcelo A. 1999. The cost of suicide mortality in New Brunswick, 1996. Chronic Diseases in Canada, 20: 89-95.
Cochran SD, Mays VM. 2000. Lifetime prevalence of suicide symptoms and affective disorders among men reporting same-sex sexual partners: Results from NHANES III. American Journal of Public Health, 90(4): 573-578.
Comer JP. 1973. Black suicide: A hidden crisis. Urban Health, 2: 41-44.
Conwell Y. 1994. Suicide in elderly patients. In: Schneider LS, Reynolds CFIII, Lebowitz BD, Friedhoff AJ, Editors. Diagnosis and Treatment of Depression in Late Life: Results of the NIH Consensus Development Conference. (pp. 397-418). Washington, DC: American Psychiatric Press.
Conwell Y, Brent D. 1996. Suicide and aging I: Patterns of psychiatric diagnosis. In: Pearson JL, Conwell Y, Editors. Suicide and Aging: International Perspectives. (pp. 15-30). New York: Springer Publishing.
Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, Caine ED. 2000. Completed suicide among older patients in primary care practices: A controlled study. Journal of the American Geriatrics Society, 48: 23-29.
Ditton PM. 1999. Mental Health and Treatment of Inmates and Probationers. NCJ 174463. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics.
Dorpat TL, Ripley HS. 1960. A study of suicide in the Seattle area. Comprehensive Psychiatry, 1: 349-359.
Draper B. 1994. Suicidal behaviors in the elderly. International Journal of Geriatric Psychiatry, 8: 655-661.
Duggan CF, Sham P, Lee AS, Murray RM. 1991. Can future suicidal behaviour in depressed patients be predicted? Journal of Affective Disorders, 22(3): 111-118.
DuRant RH, Krowchuk DP, Sinal SH. 1998. Victimization, use of violence, and drug use at school among male adolescents who engage in same-sex sexual behavior. Journal of Pediatrics, 133(1): 113-118.
EchoHawk M. 1997. Suicide: The scourge of Native American people. Suicide and Life-Threatening Behavior, 27(1): 60-67.
Elliot CA, Kral MJ, Wilson KG. 1990. Suicidal concerns among native youth. In: Lester D, Editor. Suicide ’90: Proceedings of the 23rd Annual Meeting of the American Association of Suicidology. (pp. 283-285). Denver, Colorado: American Association of Suicidology.
Expert Working Group. 1994. Suicide in Canada: Update of the Report of the Task Force on Suicide in Canada. Ottawa: Minister of National Health and Welfare.
Farberow NL. 1980. Indirect self-destructive behavior: Classification and characteristics. In: Farberow NL, Editor. The Many Faces of Suicide: Indirect Self-Destructive Behavior. (pp. 15-27). New York: McGraw-Hill.
Faulkner AH, Cranston K. 1998. Correlates of same-sex sexual behavior in a random sample of Massachusetts high school students. American Journal of Public Health, 88(2): 262-266.
Fergusson DM, Horwood LJ, Beautrais AL. 1999. Is sexual orientation related to mental health problems and suicidality in young people? Archives of General Psychiatry, 56(10): 876-880.
Ferrada-Noli M, Asberg M. 1997. Psychiatric health, ethnicity and socioeconomic factors among suicides in Stockholm. Psychological Reports, 81(1): 323-332.
Ferrada-Noli M, Asberg M, Ormstad K, Nordstrom P. 1995. Definite and undetermined forensic diagnoses of suicide among immigrants in Sweden. Acta Psychiatrica Scandinavica, 91(2): 130-135.
Foley KM. 1991. The relationship of pain and symptom management to patient requests for physician-assisted suicide. Journal of Pain and Symptom Management, 6(5): 289-297.
Forbes N, Van Der Hyde V. 1988. Suicide in Alaska from 1978 to 1985: Updated data from state files. American Indian and Alaska Native Mental Health Research, 1(3): 36-55.
Fortney J, Rost K, Zhang M, Warren J. 1999. The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care, 37(9): 884-893.
Gardner EA, Bahn AK, Mack M. 1964. Suicide and psychiatric care in the aging. Archives of General Psychiatry, 10(6): 547-553.
Garofalo R, Wolf RC, Kessel S, Palfrey SJ, DuRant RH. 1998. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics, 101(5): 895-902.
Garofalo R, Wolf RC, Wissow LS, Woods ER, Goodman E. 1999. Sexual orientation and risk of suicide attempts among a representative sample of youth. Archives of Pediatrics and Adolescent Medicine, 153(5): 487-493.
Garro LC. 1988. Suicides by status Indians in Manitoba. Arctic Medical Research, 47 (Suppl 1): 590-592.
Gould MS, Fisher P, Parides M, Flory M, Shaffer D. 1996. Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry, 53(12): 1155-1162.
Gould MS, Shaffer D. 1986. The impact of suicide in television movies. Evidence of imitation. New England Journal of Medicine, 315(11): 690-694.
Gould MS, Wallenstein S, Kleinman M. 1990. Time-space clustering of teenage suicide. American Journal of Epidemiology, 131(1): 71-78.
Griffith EEH, Bell CC. 1989. Recent trends in suicide and homicide among blacks. Journal of the American Medical Association, 262(16): 2265-2269.
Groholt B, Ekeberg O, Wichstrom L, Haldorsen T. 1998. Suicide among children and younger and older adolescents in Norway: A comparative study. Journal of the American Academy of Child and Adolescent Psychiatry, 37(5): 473-481.
Guarnaccia PJ, Lopez S. 1998. The mental health and adjustment of immigrant and refugee children. Child and Adolescent Psychiatric Clinics of North America, 7(3): 537-553, viii-ix.
Guerin PE. 1991. Alcohol-Related Traffic Fatalities in New Mexico. Masters Thesis, Department of Sociology, University of New Mexico.
Guerin PE. 1998. Motor Vehicle Crashes in New Mexico: Developing Risk Profiles Utilizing Race/ Ethnicity and Alcohol Involvement. Doctoral Dissertation, University of New Mexico.
Hackenberg RA, Gallagher MM. 1972. The costs of cultural change: Accident injury and modernization among the Papago Indians. Human Organization, 31(2): 211-226.
Hayes LM. 1989. National study of jail suicides: Seven years later. Psychiatric Quarterly, 60(1): 7-29.
Hayes LM. 1998. Suicide prevention in correctional facilities: An overview. In: Puisis M, Editor. Clinical Practice in Correctional Medicine. (pp. 245-256). St. Louis, MO: Mosby.
Hem E, Berg AM, Ekeberg AO. 2001. Suicide in police—a critical review. Suicide and Life-Threatening Behavior, 31(2): 224-233.
Hendin H. 1999. Suicide, assisted suicide, and euthanasia. In: Jacobs DG, Editor. The Harvard Medical School Guide to Suicide Assessment and Intervention. (pp. 540-560). San Fransisco: Jossey-Bass Publishers.
Herek GM. 1996. Heterosexism and homophobia. In: Cabaj RP, Stein TS, Editors. Textbook of Homosexuality and Mental Health. (pp. 101-113). Washington, D.C.: American Psychiatric Press.
Herrell R, Goldberg J, True WR, Ramakrishan V, Lyons M, Eisen S, Tsuang MT. 1999. Sexual orientation and suicidality: A co-twin control study in adult men. Archives of General Psychiatry, 56: 867-874.
Hershberger SL, D’Augelli AR. 1995. The impact of victimization on the mental health and suicidality of lesbian, gay and bisexual youths. Developmental Psychology, 31: 65-74.
Hinton WL, Tiet Q, Tran CG, Chesney M. 1997. Predictors of depression among refugees from Vietnam: A longitudinal study of new arrivals. Journal of Nervous and Mental Disease, 185(1): 39-45.
Hisnanick JJ. 1994. Comparative analysis of violent deaths in American Indians and Alaska Natives. Social Biology, 41(1-2): 96-109.
Hlady WG, Middaugh JP. 1988. Suicides in Alaska: Firearms and alcohol. American Journal of Public Health, 78(2): 179-180.
Hollinger PC, Offer D, Barter JT, Bell. C.C. 1994. Suicide and Homicide Among Adolescents. New York: The Guilford Press.
Holman EA, Silver RC, Waitzkin H. 2000. Traumatic life events in primary care patients: A study in an ethnically diverse sample. Archives of Family Medicine, 9(9): 802-810.
Hovey JD. 1999. Religion and suicidal ideation in a sample of Latin American immigrants. Psychological Reports, 85(1): 171-177.
Hovey JD. 2000a. Acculturative stress, depression, and suicidal ideation among Central American immigrants. Suicide and Life-Threatening Behavior, 30(2): 125-139.
Hovey JD. 2000b. Acculturative stress, depression, and suicidal ideation in Mexican immigrants. Cultural Diversity and Ethnic Minority Psychology, 6(2): 134-151.
Hovey JD, King CA. 1997. Suicidality among acculturating Mexican Americans: Current knowledge and directions for research. Suicide and Life-Threatening Behavior, 27(1): 92-103.
Howard-Pitney B, LaFromboise TD, Basil M, September B, Johnson M. 1992. Psychological and social indicators of suicide ideation and suicide attempts in Zuni adolescents. Journal of Consulting and Clinical Psychology, 60(3): 473-476.
Howland RH. 1995. The treatment of persons with dual diagnoses in a rural community. Psychiatric Quarterly, 66(1): 33-49.
Hoyert DL, Arias E, Smith BL, Murphy SL, Kochanek KD. 2001. Deaths: Final data for 1999. National Vital Statistics Reports, 49(8): 1-113.
Hoyert DL, Kochanek KD, Murphy SL. 1999. Deaths: Final data for 1997. National Vital Statistics Reports, 47(19): 1-104.
Indian Health Service. 1999. Trends in Indian Health, 1998-1999. Rockville, MD: U.S. Department of Health and Human Services.
IOM (Institute of Medicine). 1999. Bonnie RJ, Fulco CE, Liverman CT, Editors. Reducing the Burden of Injury: Advancing Prevention and Treatment. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 2002. B.D. Smedley, A.Y. Stith, A.R. Nelson, Editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academy Press.
Jarvis GK, Boldt M. 1982. Death styles among Canada’s Indians. Social Science and Medicine, 16(14): 1345-1352.
Jemelka R, Trupin E, Chiles JA. 1989. The mentally ill in prisons: A review. Hospital and Community Psychiatry, 40(5): 481-491.
Ji J, Kleinman A, Becker AE. 2001. Suicide in contemporary China: A review of China’s distinctive suicide demographics in their sociocultural context. Harvard Review of Psychiatry, 9(1): 1-12.
Jianlin J. 2000. Suicide rates and mental health services in modern China. Crisis, 21(3): 118-121.
Jobes DA, Berman AL, Josselson AR. 1987. Improving the validity and reliability of medical–legal certifications of suicide. Suicide and Life-Threatening Behavior, 17(4): 310-325.
Joe JR. 2001. Out of harmony: Health problems and young Native American men. Journal of American College Health, 49(5): 237-242.
Kahn MW. 1982. Cultural clash and psychopathology in three Aboriginal cultures. Academic Psychology Bulletin, 4(3): 553-561.
Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Hill CV, Grunbaum JA, Blumson PS, Collins JL, Kolbe LJ. 1998. Youth Risk Behavior Surveillance—United States, 1997. State and Local YRBSS Coordinators. Journal of School Health, 68(9): 355-369.
Kastenbaum R, Mishara BL. 1971. Premature death and self-injurious behavior in old age. Geriatrics, 26(7): 71-81.
Katz PA, May PA. 1979. Motor Vehicle Accidents on the Navajo Reservation: 1973–1975. Window Rock, AZ: The Navajo Health Authority.
Kellermann AL, Rivara FP, Somes G, Reay DT, Francisco J, Banton JG, Prodzinski J, Fligner C, Hackman BB. 1992. Suicide in the home in relation to gun ownership. New England Journal of Medicine, 327(7): 467-472.
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. 1994. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1): 8-19.
Kettl P, Bixler EO. 1993. Alcohol and suicide in Alaska Natives. American Indian and Alaska Native Mental Health Research , 5(2): 34-45.
Kettl PA, Bixler EO. 1991. Suicide in Alaska Natives, 1979-1984. Psychiatry: Interpersonal and Biological Processes, 54(1): 55-63.
Khan MM, Reza H. 2000. The pattern of suicide in Pakistan. Crisis, 21(1): 31-35.
Kleinman A. 2001. Cross-cultural psychiatry: A psychiatric perspective on global change. Harvard Review of Psychiatry, 9(1): 46-47.
Koskinen O, Pukkila K, Hakko H, Tiihonen J, Väisänen E, Säkioja Teal. in press. Is occupation relevant for suicide. Journal of Affective Disorders.
Kost-Grant BL. 1983. Self-inflicted gunshot wounds among Alaska Natives. Public Health Reports, 98(1): 72-78.
Kraus R. 1974. Suicidal behavior in Alaska natives. Alaska Medicine, 16(1): 2-6.
Kryzhanovskaya L, Pilyagina G. 1999. Suicidal behavior in the Ukraine, 1988–1998. Crisis, 20(4): 184-190.
Labovitz S, Hagedorn R. 1971. An analysis of suicide rates among occupational categories. Sociological Inquiry, 41: 67-72.
Levy JE. 1965. Navaho suicide. Human Organization, 24(4): 308-318.
Manderscheid RW, Sonnenschein MA, Editors. 1999. Mental Health, United States, 1998. Rockville, MD: U.S. Department of Health and Human Services.
Manson SM, Beals J, Dick RW, Duclos C. 1989. Risk factors for suicide among Indian adolescents at a boarding school. Public Health Reports, 104(6): 609-614.
Martin RL, Cloninger CR, Guze SB, Clayton PJ. 1985. Mortality in a follow-up of 500 psychiatric outpatients. II. Cause-specific mortality. Archives of General Psychiatry, 42: 58-66.
May PA. 1982. Substance abuse and American Indians: Prevalence and susceptibility. International Journal of the Addictions, 17(7): 1185-1209.
May PA. 1987. Suicide and self-destruction among American Indian youths. American Indian and Alaska Native Mental Health Research, 1(1): 52-69.
May PA. 1989. Motor vehicle crashes and alcohol among American Indians and Alaska Natives. In. The Surgeon General’s Workshop on Drunk Driving: Background Papers. (pp. 207-223). Washington, DC: U.S. Department of Health and Human Services.
May PA, Dizmang LH. 1974. Suicide and the American Indian. Psychiatric Annals, 4(11): 22-28.
McDaniel JS, Purcell D, D’Augelli AR. 2001. The relationship between sexual orientation and risk for suicide: Research findings and future directions for research and prevention. Suicide and Life-Threatening Behavior, 31 (Suppl): 84-105.
Merrill J, Owens J. 1988. Self-poisoning among four immigrant groups. Acta Psychiatrica Scandinavica, 77(1): 77-80.
Michaels S. 1996. The prevalence of homosexuality in the United States. In: Cabaj RP, Stein TS, Editors. Textbook of Homosexuality and Mental Health. (pp. 43-63). Washington, D.C.: American Psychiatric Press.
Miller M. 1976. Geriatric suicide: The Arizona Study. Gerontologist, 18: 488-495.
Minino AM, Smith BL. 2001. Deaths: Preliminary data for 2000. National Vital Statistics Reports, 49(12): 1-40.
Morrell S, Taylor R, Slaytor E, Ford P. 1999. Urban and rural suicide differentials in migrants and the Australian-born, New South Wales, Australia 1985–1994. Social Science and Medicine, 49(1): 81-91.
Morrissey JP, Swanson JW, Goldstrom I, Rudolph L, Manderscheid RW. 1993. Overview of mental health services provided by state adult correctional facilities: United States, 1988. Mental Health Statistical Note, 207: 1-13.
Murphy GE. 1998. Why women are less likely than men to commit suicide. Comprehensive Psychiatry, 39(4): 165-175.
Murphy SL. 2000. Deaths: Final data for 1998. National Vital Statistics Reports, 48(11): 1-105.
National Commission on Correctional Health Care. 2000. The Health Status of Soon-to-Be-Released Inmates. Chicago, IL: National Commission on Correctional Health Care.
National Mental Health Association. 2000. Depression and African-Americans Fact Sheet. Alexandria, VA: National Mental Health Association.
NCHS (National Center for Health Statistics). 2001. Data From the National Vital Statistics System. Hyattsville, MD: Centers for Disease Control and Prevention. [Online]. Available: http://www.cdc.gov/nchs/nvss.htm [accessed September 2001].
NCHS (National Center for Health Statistics). 1992. Advance report of final mortality statistics, report No. 40. NCHS Monthly Vital Statistics Report.
NCIPC (National Center for Injury Prevention and Control). 2000. Web-Based Injury Statistics Query and Reporting System. [Online]. Available: http://www.cdc.gov/ncipc/wisqars/ [accessed December 13, 2001].
New Mexico Vital Records and Health Statistics. 2000. 1998 New Mexico Selected Health Statistics: Annual Report.
Norton GR, Rockman GE, Malan J, Cox BJ, Hewitt PL. 1995. Panic attacks, chemical abuse, and suicidal ideation: A comparison of native and non-native Canadians. Alcoholism Treatment Quarterly, 12(3): 33-41.
NRC (National Research Council). 1998. Hernandez DJ, Charney E, Editors. From Generation to Generation: The Health and Well-Being of Children in Immigrant Families. Washington, DC: National Academy Press.
NRC (National Research Council). 1999. Hernandez DJ, Editor. Children of Immigrants: Health, Adjustment, and Public Assistance. Washington, DC: National Academy Press.
O’Carroll PW. 1989. A consideration of the validity and reliability of suicide mortality data. Suicide and Life-Threatening Behavior, 19(1): 1-16.
O’Donnell I, Farmer R. 1995. The limitations of official suicide statistics. British Journal of Psychiatry, 166(4): 458-461.
O’Hare T, Van Tran T. 1998. Substance abuse among Southeast Asians in the U.S.: Implications for practice and research. Social Work in Health Care, 26(3): 69-80.
Opler MK. 1969. International and cultural conflicts affecting mental health. Violence, suicide and withdrawal. American Journal of Psychotherapy, 23(4): 608-620.
Osgood NJ, Brant BA, Lipman A. Suicide Among the Elderly in Long-Term Care Facilities. 1991. New York: Greenwood Press.
Patel SP, Gaw AC. 1996. Suicide among immigrants from the Indian subcontinent: A review. Psychiatric Services, 47(5): 517-521.
Patterson HL. 1969. Suicide among the youth on the Quinault Indian Reservation. In U.S. Senate Committee on Labor and Public Welfare, Part 5, Subcommittee on Indian Education. (pp. 2016-2021). Washington, DC: U.S. Government Printing Office.
Pearson JL, Conwell Y, Lindesay J, Takahashi Y, Caine ED. 1997. Elderly suicide: A multinational view. Aging and Mental Health, 1(2): 107-111.
Phillips DP, Carstensen LL. 1986. Clustering of teenage suicides after television news stories about suicide. New England Journal of Medicine, 315(11): 685-689.
Phillips MR, Liu H, Zhang Y. 1999. Suicide and social change in China. Culture, Medicine and Psychiatry, 23: 25-50.
Plotnikov N. 2001. Suicide in Russia. Russian Social Science Review, 42(3): 41-43.
Ponizovsky A, Safro S, Ginath Y, Ritsner M. 1997. Suicide ideation among recent immigrants: An epidemiological study. Israel Journal of Psychiatry and Related Sciences, 34(2): 139-148.
Prince C. 1988. Recognition of predisposing factors which affect the high suicide rate of Canadian Indians. Arctic Medical Research, 47 (Suppl 1): 588-589.
Prudhome C. 1938. The problem of suicide in the American negro. Psychoanalytic Review, 25: 187-204; 372-391.
Regier DA, Farmer ME, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ. 1993. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: The Epidemiologic Catchment Area study. Acta Psychiatrica Scandinavica, 88(1): 35-47.
Remafedi G, French S, Story M, Resnick MD, Blum R. 1998. The relationship between suicide risk and sexual orientation: Results of a population-based study. American Journal of Public Health, 88(1): 57-60.
Resnik HLP, Dizmang LH. 1971. Observations on suicidal behavior among American Indians. American Journal of Psychiatry, 127(7): 882-887.
Rich CL, Fowler RC, Young D, Blenkush M. 1986a. San Diego suicide study: Comparison of gay to straight males. Suicide and Life-Threatening Behavior, 16(4): 448-457.
Rich CL, Young D, Fowler RC. 1986b. San Diego suicide study. I. Young vs old subjects. Archives of General Psychiatry, 43(6): 577-582.
Rihmer Z, Rutz W, Pihlgren. 1995. Depression and suicide on Gotland: An intensive study of all suicides before and after a depression—training programme for general practitioners. Journal of Affective Disorders, 35: 147-152.
Robins L, Regier DA. 1991. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York: The Free Press.
Robins LN, West PA, Murphy GE. 1977. The high rate of suicide in older White men: A study testing ten hypotheses. Social Psychiatry, 12(1): 1-20.
Russell ST, Joyner K. 2001. Adolescent sexual orientation and suicide risk: Evidence from a national study. American Journal of Public Health, 91(8): 1276-1281.
Sack WH, Beiser M, Baker-Brown G, Redshirt R. 1994. Depressive and suicidal symptoms in Indian school children: Findings from the Flower of Two Soils. American Indian and Alaska Native Mental Health Research Monograph Series, 4: 81-94; discussion 94-6.
Sartorius N. 1996. Recent changes in suicide rates in selected eastern European and other European countries. In: Pearson JL, Conwell Y, Editors. Suicide and Aging: International Perspectives. (pp. 169-176). New York: Springer Publishing.
Saunderson TR, Langford IH. 1996. A study of the geographical distribution of suicide rates in England and Wales 1989-92 using empirical bayes estimates. Social Science and Medicine, 43(4): 489-502.
Schmidtke A, Fricke S, Lester D. 1999. Suicide among German federal and state police officers. Psychological Reports, 84(1): 157-166.
Schweizer E, Dever A, Clary C. 1988. Suicide upon recovery from depression. A clinical note. Journal of Nervous and Mental Disease, 176(10): 633-636.
Seiden RH, Gleiser M. 1990. Sex differences in suicide among chemists. Omega—Journal of Death and Dying, 21(3): 177-189.
Shaffer D, Fisher P, Hicks RH, Parides M, Gould M. 1995. Sexual orientation in adolescents who commit suicide. Suicide and Life-Threatening Behavior, 25 (Suppl): 64-71.
Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, Flory M. 1996. Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry, 53: 339-348.
Shiang J, Blinn R, Bongar B, Stephens B, Allison D, Schatzberg A. 1997. Suicide in San Francisco, CA: A comparison of Caucasian and Asian groups, 1987–1994. Suicide and Life-Threatening Behavior, 27(1): 80-91.
Shuck LW, Orgel MG, Vogel AV. 1980. Self-inflicted gunshot wounds to the face: A review of 18 cases. Journal of Trauma, 20(5): 370-377.
Singh GK, Siahpush M. 2001. All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health, 91(3): 392-399.
Sloan JH, Rivara FP, Reay DT, Ferris JAJ, Path MRC, Kellermann AL. 1990. Firearms regulations and rates of suicide: A comparison of two metropolitan areas. New England Journal of Medicine, 322(6): 369-373.
Smith JC, Mercy JA, Conn JM. 1988. Marital status and the risk of suicide. American Journal of Public Health, 78(1): 78-80.
Sorenson SB, Golding JM. 1988. Prevalence of suicide attempts in a Mexican-American population: Prevention implications of immigration and cultural issues. Suicide and Life-Threatening Behavior, 18(4): 322-333.
Sorenson SB, Shen H. 1996. Youth suicide trends in California: An examination of immigrant and ethnic group risk. Suicide and Life-Threatening Behavior, 26(2): 143-154.
Spaulding JM. 1985–1986. Recent suicide rates among ten Ojibwa Indian bands in northwestern Ontario. Omega—Journal of Death and Dying, 16(4): 347-354.
Stack S. 1995. Gender and suicide among laborers. Archives of Suicide Research, 1(1): 19-26.
Stack S. 2001. Occupation and suicide. Social Science Quarterly, 82(2): 384-396.
Stack S, Kelly T. 1994. Police suicide: An analysis. American Journal of Police, 13(4): 73-90.
Steadman HJ, Fabisiak S, Dvoskin J, Holohean EJ Jr. 1987. A survey of mental disability among state prison inmates. Hospital and Community Psychiatry, 38(10): 1086-1090.
Stull DD. 1972. Victims of modernization: Accident rates and Papago Indian adjustment. Human Organization, 31(2): 227-240.
Stull DD. 1973. Modernization and Symptoms of Stress: Attitudes, Accidents and Alcohol Use Among Urban Papago Indians. Doctoral Dissertation, University of Colorado.
Stull DD. 1977. New data on accident victims rates among Papago Indians: The urban case. Human Organization, 36(4): 395-398.
Szanto K, Prigerson H, Houck P, Ehrenpreis L, Reynolds CF 3rd. 1997. Suicidal ideation in elderly bereaved: The role of complicated grief. Suicide and Life-Threatening Behavior, 27(2): 194-207.
Taylor PJ, Gunn J. 1984. Violence and psychosis. I. Risk of violence among psychotic men. British Medical Journal (Clinical Research Edition), 288(6435): 1945-1949.
Teplin LA. 1990. The prevalence of severe mental disorder among male urban jail detainees: Comparison with the Epidemiologic Catchment Area Program. American Journal of Public Health, 80(6): 663-669.
Tousignant M, Habimana E, Biron C, Malo C, Sidoli-LeBlanc E, Bendris N. 1999. The Quebec Adolescent Refugee Project: Psychopathology and family variables in a sample from 35 nations. Journal of the American Academy of Child and Adolescent Psychiatry, 38(11): 1426-1432.
Travis RM. 1984. Suicide and economic development among the Inupiat Eskimo. White Cloud Journal, 3(3): 14-21.
U.S. Congress, Office of Technology Assessment. 1990. Indian Adolescent Mental Health OTAH-446. Washington, DC: U.S. Government Printing Office.
US DHHS (U.S. Department of Health and Human Services). 2001. Mental Health: Culture, Race and Ethnicity—A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health.
VanWinkle NW, May PA. 1986. Native American suicide in New Mexico, 1957–1979: A comparative study. Human Organization, 45(4): 296-309.
VanWinkle NW, May PA. 1993. An update on American Indian suicide in New Mexico, 1980–1987. Human Organization, 52(3): 304-315.
VanWinkle NW, Williams M. 2001. Evaluation of the National Model Adolescent Suicide Prevention Project: A Comparison of Suicide Rates Among New Mexico American Indian Tribes, 1980–1998. Tulsa, Oklahoma: Oklahoma State University, College of Osteopathic Medicine.
Veysey BM, Bichler-Robertson G. 1999. Prevalence Estimates for Psychiatric Disorders in Correctional Settings. Chicago, IL: National Commission on Correctional Health Care.
Violanti JM, Vena JE, Petralia S. 1998. Mortality of a police cohort: 1950–1990. American Journal of Industrial Medicine, 33(4): 366-373.
Viscusi WK. 1995. Cigarette taxation and the social consequences of smoking. In: National Bureau of Economic Research. Tax Policy and the Economy. Vol. 9. (pp. 51-101). Cambridge, MA: MIT Press.
Wallace LJ, Calhoun AD, Powell KE, O’Neil J, James SP. 1996. Homicide and Suicide Among Native Americans, 1979–1992. Atlanta, Georgia: National Center for Injury Prevention and Control Violence Surveillance Summary Series, No.2.
WHO (World Health Organization). 2001a. Mental Health and Brain Disorders. Suicide Rates (Per 100,000). Geneva: World Health Organization. [Online]. Available: http://www.who.int/mental_health/Topic_Suicide/Suicide_rates.html [accessed January 7, 2002].
WHO (World Health Organization). 2001b. The World Health Report, 2001. Mental Health: New Understanding, New Hope. Geneva: World Health Organization.
Wilkinson D, Gunnell D. 2000. Youth suicide trends in Australian metropolitan and non-metropolitan areas, 1988–1997. Australian and New Zealand Journal of Psychiatry, 34(5): 822-828.
Williams CL, Berry JW. 1991. Primary prevention of acculturative stress among refugees. Application of psychological theory and practice. American Psychologist, 46(6): 632-641.
Wills JE. 1969. Psychological problems of the Sioux Indians resulting in the accident phenomenon. Pine Ridge Research Bulletin, 8: 49-63.
Wissow LS. 2000. Suicide among American Indians and Alaska Natives. In: Rhoades ER, Editor. American Indian Health. (pp. 260-280). Baltimore, MD: The Johns Hopkins University Press.
Yip PS. 2001. An epidemiological profile of suicides in Beijing, China. Suicide and Life-Threatening Behavior, 31(1): 62-70.
Yip PS, Callana C, Yuen HP. 2000. Urban/rural and gender differentials in suicide rates: East and west. Journal of Affective Disorders, 57(1-3): 99-106.
Psychosis can create a particularly terrible kind of pain that leads to suicidal behavior. Robert Bayley, who suffered for years from schizophrenia, recounted his struggles with extremely frightening hallucinations:
The reality for myself is almost constant pain and torment. The voices and visions, which are so commonly experienced, intrude and so disturb my everyday life. The voices are predominantly destructive, either rambling in alien tongues or screaming orders to carry out violent acts. They also persecute me by way of unwavering commentary and ridicule to deceive, derange, and force me into a world of crippling paranoia. Their commands are abrasive and all-encompassing and have resulted in periods of suicidal behavior and self-mutilation. I have run in front of speeding cars and severed arteries while feeling this compulsion to destroy my own life. As their tenacity gains momentum, there is often no element of choice, which leaves me feeling both tortured and drained.
—ROBERT BAYLEY
“First person account: Schizophrenia”