|
BOX 6.1 Summary of Findings
|
6
Health-Related Outcomes for Children, Pregnant Women, and Newborns
This chapter examines clinical and epidemiological evidence about the effects of health insurance status on the health of children, pregnant women, and newborns.1 It extends the assessment of health outcomes that the Committee presented in Care Without Coverage to pediatric and pregnancy-related care and outcomes. It places this analysis within the broader context of family interests, behavior, and constraints of this report because, as demonstrated in the previous chapter, children’s access to and use of health care is highly dependent on their parents’ opportunities and actions. The financially constrained patterns of use by uninsured families, as documented in Chapter 4, can affect the overall health and development of their members, particularly of children. Table 6.1 summarizes the health insurance status of American children by age, race and ethnicity, and family income.
The Committee reviewed studies that compare the access to and use of health care services by insured and uninsured children, pregnant women, and newborns as well as research that relates their insurance status to health outcomes.2 Only
TABLE 6.1 Number of Uninsured Children by Age, Race or Ethnicity, and Family Income, 2000, United States
|
|
Total Number (millions) |
Total Uninsureda (millions) |
Percent Uninsured |
|
All children |
72.6 |
8.4 |
11.6 |
|
Age |
|||
|
Under 3 years |
11.9 |
1.3 |
11.3 |
|
3–5 years |
11.8 |
1.3 |
10.8 |
|
6–11 years |
24.8 |
2.8 |
11.5 |
|
12–17 years |
24.1 |
2.9 |
12.2 |
|
Race or ethnicity |
|||
|
Non-Hispanic white |
45.4 |
3.3 |
7.3 |
|
Black |
11.6 |
1.6 |
13.5 |
|
Asian and Pacific Islander |
3.1 |
0.4 |
14.3 |
|
Hispanic origin |
12.0 |
3.0 |
24.9 |
|
Family income |
|||
|
0–99% FPL |
12.2 |
2.7 |
22.1 |
|
100–149% FPL |
7.7 |
1.5 |
19.5 |
|
150–199% FPL |
7.6 |
1.1 |
14.5 |
|
200% FPL and over |
45.0 |
3.1 |
6.9 |
|
NOTE: FPL = federal poverty level. aThe Current Population Survey (CPS) defines uninsured as having no form of health insurance during an entire calendar year. SOURCES: Census Bureau, CPS Annual Demographic Survey, March Supplement, 2001, Table HI08. Available at: http://ferret.bls.census.gov/macro/032001/health/h08_000.htm. Accessed April 21, 2002; and Fronstin, 2001. |
|||
studies that the Committee judged methodologically sound are presented in this chapter. Additional studies reviewed by the Committee and the Subcommittee are included in Appendix C.
Opportunities for low and lower-income children and pregnant women to obtain coverage through public health insurance programs have increased substantially over the past one and a half decades. Many of the studies reviewed in this chapter are evaluations of these program expansions. Others of the studies of access, use and health outcomes pre-date most of these expansions. The Committee believes that the general patterns of utilization and outcomes that are reported for insured and uninsured children, pregnant women and infants remain valid even as
|
|
journal articles and unpublished studies brought to the Committee’s attention by experts were included if they met the other criteria mentioned above. Appendix C provides brief descriptions of all the studies that met the review criteria. |
the relative proportions of insured and uninsured populations have shifted over time.
Appropriate health care interventions for children and pregnant women have been related to educational achievement, exit from welfare or social services, and ultimate employment—all outcomes that extend well beyond traditional health. For children, using health care services routinely and appropriately is considered a positive health outcome in its own right because well-child care is a practice grounded in evidence of its effectiveness in enhancing longer-term health and development. Early intervention, even in the face of severe physical or mental problems, often can minimize long-term health and developmental problems and thus can benefit society overall. Without opportunities for health and developmental assessments, particularly with an ongoing source of care, problems go undetected and children may suffer consequences that limit their life chances in both obvious and less evident ways. Before birth, good prenatal care also provides opportunities to ensure the best possible health for both mother and child. To the extent that having health insurance can remove access barriers and foster timely assessments of development and health, the health of children measured on a population-wide basis will improve.
Of course, health insurance is not the only factor influencing use of health care, and use of health care is but one of many factors that influence health outcomes. For example, poverty, presence of chronic disease, socioeconomic status, educational attainment (and, for children, their parents’ educational attainment), and health-related behaviors such as diet, exercise, drug use, and smoking may affect utilization and outcomes as much as health insurance status (Szilagyi and Schor, 1998). Figure 1.1 in Chapter 1 depicts the multiple factors and characteristics that relate health insurance to access, use, and outcomes. A full discussion of the conceptual framework that depicts the relationships among personal characteristics, health care, and outcomes is presented in Appendix A.
Ideally, to answer the question, Does health insurance enhance health status?, one would perform a true experiment, in which some individuals would be randomly assigned to receive insurance and others not. Because of the ethical and practical obstacles to conducting a health insurance experiment that leaves some participants uninsured, none have been conducted.3 Instead, most of the evidence for the effect of insurance on health outcomes is based on observational studies of insured and uninsured individuals. A few studies with quasi-experimental designs
have been conducted within the past decade and a half. These so-called natural experiments are ones in which
-
a population of children or pregnant women gains coverage because of policy changes (e.g., as a result of increases in the Medicaid income eligibility standard or the introduction of the State Children’s Health Insurance Program [SCHIP]) allowing comparisons of access, use, and outcomes before and after coverage policy changes; or
-
differences in income eligibility levels among state Medicaid programs provide an opportunity to evaluate the impact of the different levels.
These quasi-experimental studies allow for greater confidence in the validity of their results than do cross-sectional studies that rely on analytic controls for characteristics that co-vary with health insurance status.4
Other factors that can influence health outcomes, such as income, educational attainment, race and ethnicity, or immigrant status, often coincide with lack of insurance. This report relies on studies that account for these factors with analytic adjustments that isolate the effects of health insurance status. Studies report adjusted statistics (e.g., odds ratios [ORs]5) that account for such characteristics as family income, race or ethnicity, age, gender, and sometimes health status. Quantified study results are presented only if they are statistically significant at the conventional p = 0.05 level or at higher significance levels, unless otherwise noted.
The first section of this chapter reviews the link between children’s health insurance status and their access to and appropriate use of services. The second section presents empirical studies that examine specific health outcomes for children and youth as related to coverage status. The third section reviews longer-term adverse outcomes for children’s health and development for specific conditions that have not been studied in terms of their relationship to health insurance status that merit further investigation. The fourth and last section assesses the evidence regarding the relationship between pre- and perinatal care and birth outcomes for mothers and infants.
ACCESS TO AND USE OF HEALTH CARE BY CHILDREN
Access is most simply understood as the ability to see a physician or other health care provider when one wants to do so. Access and use of health care services are closely connected. A child without good access is expected to have a harder time using care and thus expected to have fewer visits and more unmet needs than one with good access to care. Research examining the impact of insurance on access employs a variety of measures, such as whether a child or pregnant woman has a regular source of care or a “medical home,” a usual physician within a regular place of care (i.e., a medical home), ability to obtain care outside of normal business hours, a regular dentist (for children), and unmet health needs or delays in care due to cost.6 Measurement of utilization has two aspects, the number of visits and the appropriate use of health care services (e.g., receipt of indicated services on a timely basis or inappropriate use of emergency departments as the site of primary care). Empirical studies support the link between access to care, use, and improved health outcomes (Bindman et al., 1995; Starfield, 1995; Hadley, 2002; IOM, 2002a).
Finding: Uninsured children have less access to health care, are less likely to have a regular source of primary care, and use medical and dental care less often compared to children who have insurance. Children with gaps in health insurance coverage have worse access than do those with continuous coverage.
Studies using databases with national probability samples, such as the National Health Insurance Survey (NHIS), the Medical Expenditure Panel Survey (MEPS), and the National Survey of America’s Families (NSAF), consistently report that uninsured children have poorer access to health care and use health services less frequently than their insured counterparts. Insurance status remains a significant factor even after studies control for income, race and ethnicity, and health status.
Children with health insurance are more likely to have a usual source of health care than uninsured children. A study based on the 1993–1994 NHIS reported an odds ratio of 6.1 between insured and uninsured children’s likelihood of having a usual source of care (Newacheck et al., 1998b).7 Among those
|
6 |
The American Academy of Pediatrics (AAP) characterizes a “medical home” for infants, children, and adolescents as one that provides continuous, comprehensive, family-centered, coordinated, and compassionate care delivered by well-trained physicians known to the child and family who are able to develop a relationship of mutual responsibility and trust with them (AAP, Medical Home Statement. Available at: http:www/aap.org. Accessed December 28, 2001). |
|
7 |
Health insurance is not the only factor in parental decision-making on whether to develop a relationship with a health care provider for their children. An analysis of the 1996 MEPS reports that parents of children who did not have a regular source of care give as the main reasons, that the child is seldom or never sick (66 percent) and, that they cannot afford one (10 percent) (Weinick et al., 1998). Financial reasons do, however, constitute the main barriers to receiving care perceived as needed. |
children whose parents reported having a usual site of care, uninsured children were more likely to lack a regular physician and to be unable to obtain medical care after normal business hours. Uninsured children were also more likely than those with insurance to go without care that parents reported they needed (OR = 5.8), to go without any dental care (OR = 4.3), and more likely to have had no contact with a physician during the previous year (OR = 2.1) (Newacheck et al., 1998b). Not surprisingly, the parents of uninsured children were more likely to be dissatisfied with at least some aspect of their child’s care. This comprehensive survey analysis adjusted for age, sex, race, family income, family structure and size, region of the country, population density, and health status. These results confirmed those of an earlier study using 1988 NHIS data. Holl and colleagues (1995) reported that uninsured children were more likely than those with insurance never to have had a regular source of care (OR = 1.8) and more likely not to meet standards of timeliness for well-child visits (OR = 1.3). Furthermore, uninsured children were more likely to obtain routine and sick care from different sources than were insured children (Holl et al., 1995).
Uninsured children are less likely to have received medical care for common childhood illnesses than are children with health insurance. In a study based on the 1987 National Medical Expenditure Survey (NMES), uninsured children were significantly less likely to visit a physician for pharyngitis, acute earache, recurrent ear infection or asthma, conditions for which medical attention is usually considered necessary (ORs = 1.7, 1.85, 2.1, 1.7, respectively) (Stoddard et al., 1994). The uninsured child’s worse odds remained despite extensive sociodemographic and health status adjustments.
Most studies combine both children with private and children with public insurance into a single “insured” category. The impact of insurance on access and utilization differs depending on whether it is private or public insurance, with better access and higher use rates among those with private insurance.8 However, children with no insurance still have the worst measures of access and utilization, below those of publicly insured poor children. Although not all of the differences in access and use among children of differing health insurance status are due to their coverage status, these differences are pronounced.
Children with private insurance have considerably more medical office visits, dental visits, and filled prescriptions than do both children who have public insurance and those who are uninsured. An analysis of 1996 MEPS data shows the following differences in the use of any service within a year for
-
physician office visits (76, 67, and 51 percent for privately insured, publicly insured, and uninsured children, respectively);
-
dental visits (50, 29, and 21 percent, respectively); and
-
prescriptions filled (61, 56, and 43 percent, respectively) (McCormick et al., 2001).
Despite being the least likely to have a regular source of care, uninsured children on average receive less care from emergency departments than do children with any kind of coverage (McCormick et al., 2001). Hospitalizations and emergency department visits are highest for children with public insurance, possibly reflecting inadequate access to other ambulatory care providers. Publicly insured children are hospitalized at more than twice the rate of the privately insured and uninsured (5.4, versus 2.4 and 1.9 percent with any hospital stay for publicly insured, privately insured, and uninsured, respectively). Emergency department visits are also highest for the publicly insured (15.5, versus 12.5 and 10.8 percent with a visit for publicly insured, privately insured, and uninsured, respectively) (McCormick et al., 2001).
Finding: Previously uninsured children experience significant increases in both access to and more appropriate use of health care services following their enrollment in public health insurance programs.
Studies that have evaluated Medicaid program expansions since the mid-1980s and, more recently, children’s health insurance demonstrations that preceded SCHIP conclude that increased eligibility for and enrollment in public programs results in greater and more appropriate use of health services among children. Between 1984 and 1992, the first period of expansions in Medicaid eligibility and enrollment, Currie and Gruber (1996b) analyzed National Health Interview Survey (NHIS) data as a function of state Medicaid eligibility standards and found that eligibility for Medicaid was associated across the child population with reducing the likelihood that a child would go without any physician visit within a year by half. They also found an association between increases in Medicaid eligibility at the state level and reductions in child mortality after the first year of life.
A second study by Currie (2000) that used NHIS data from 1989 to 1992 (prior to the enactment of Medicaid restrictions on eligibility for immigrants) to compare the effects of Medicaid eligibility on insurance coverage and use of services between children of U.S.-born and immigrant parents found that the effects of increased Medicaid eligibility on utilization of ambulatory care were twice as great for the children of immigrants, whose average use of physician services was lower, as for children of U.S.-born parents. As discussed later in this chapter, a national study of Medicaid eligibility expansions between 1983 and 1996 concluded that these expansions reduced potentially avoidable hospitalizations among children (Dafny and Gruber, 2000).
Enactment of SCHIP in 1997, with implementation beginning the next year, provided the opportunity for states to insure children at higher family income
levels than those established for Medicaid. States vary in how much they raised the income eligibility threshold for public health insurance, but expansion to 200 percent FPL was most common. Studies of the earliest state demonstration programs in two states, New York and Pennsylvania, report a significant increase in both access and utilization for previously uninsured children after receipt of health insurance.
The New York program evaluation involved an examination of the state as a whole (Szilagyi et al., 2000c) as well as a focused study on six upstate counties (Rodewald et al., 1997; Holl et al., 2000; Szilagyi et al., 2000a, 2000b). In both cases, the researchers compared children’s health care use and health outcomes for the year before they entered the New York program to those for the first year after enrollment. A study of a similar program in 29 counties in western Pennsylvania also used a before-and-after design (and also had a comparison group of later enrollees) and surveyed newly enrolled children at 6 and 12 months following enrollment (Lave et al., 1998a).
The findings of these three evaluations consistently show that the newly insured children had increased access to a medical home, paving the way for more timely and appropriate care and greater satisfaction with services. In Pennsylvania, 12 months after enrollment, 99 percent of the children had a regular source of medical care and 85 percent had a regular dentist, up from 89 and 60 percent, respectively, at baseline. Further, the proportion of children reporting any unmet need or delayed medical care in the previous six months decreased from 57 percent at baseline to 16 percent at 12 months (Lave et al., 1998a). The proportion of children with any physician visit increased from 59 to 64 percent, accompanied by a 5 percentage point decrease in the proportion with an emergency room visit, from 22 percent to 17 percent (Lave et al., 1998a). The proportion of children seeing a dentist increased from 40 percent at enrollment to 65 percent after 12 months (Lave et al., 1998a). Because the separate comparison group of later-enrolling children were similar to those initially enrolling, these changes over time in the insured group can be attributed to the coverage with greater confidence.
In New York State, enrollment in the state insurance program also reduced the number of children without a medical home (from 5 percent before the expansion to 1 percent after enrollment), and one in three parents of newly insured children reported improved quality of care for their children (Szilagyi et al., 2000c). Visits to primary care physicians for preventive, acute, and total care increased markedly (up by 25, 52, and 42 percent, respectively). Visits to specialists following enrollment more than doubled from before enrollment. Emergency department (ED) use did not change significantly, but hospitalization declined by 36 percent statewide (Szilagyi et al., 2000c). In the upstate program, the parents of one-quarter of the enrolled children reported that their children’s health had improved as a result of the coverage (Holl et al., 2000).
Tracking specific services and childhood conditions also reveals changes in access and use. For example, throughout New York, use of public health depart-
ments for immunizations decreased by 67 percent after implementation of the program, with more immunizations delivered in the medical home during the period of expanded coverage (Rodewald et al., 1997). The upstate evaluation reported that visits to medical homes increased for children with chronic conditions (from 5.7 to 7.1 visits annually), a sign of better care (Szilagyi et al., 2000b). The impact of insurance status on one chronic condition, asthma, was also documented. Following enrollment in the insurance program, parents perceived that their child’s severity level and quality of care for asthma had improved, and about half of these parents reported that their asthmatic child’s overall health had improved as a result of the program services (Szilagyi et al., 2000a). Primary care visits increased following enrollment; with no significant changes in ED or hospital use for asthma care, suggesting increased access to ambulatory services for these children. The authors hypothesize that uninsured children with asthma who gained health insurance coverage were more likely to receive care both for acute exacerbations of their conditions and for routine services because of reduced financial barriers (Szilagyi et al., 2000a).
The results of these program evaluations suggest that the nation’s near-poor children will likely benefit from the recently implemented SCHIP program. The Pennsylvania study did not focus on the urban population, and although the New York statewide study did include New York City and both urban and rural regions throughout the state, low-income urban populations were still under-represented. Because the problems of poverty and lack of insurance may be distinctive for residents of large cities, the effects of insurance program expansion within major metropolitan areas may be even greater than those noted in the early demonstration programs. For example, the portion of children lacking a medical home in New York City was more than twice that of the state as a whole (11 percent versus 5 percent prior to expansion), and many of the access measures improved most in New York City, where baseline levels of access had been the poorest (Szilagyi et al., 2000c).
In examining children’s health insurance expansions and anticipating the impact of SCHIP, it is important to keep in mind that children enrolled in SCHIP are from families with higher income than children enrolled in Medicaid and may have different characteristics and respond to insurance and health care differently. One study based on 1993–1994 NHIS data suggests that SCHIP-eligible children have markedly different socioeconomic and health status characteristics than either Medicaid or privately insured children (Byck, 2000). SCHIP-eligible children more often live with college-educated and employed adults than do Medicaid-eligible children, but less often than privately insured children. SCHIP-eligible children are more likely to be in excellent health than Medicaid children but also are twice as likely to be in fair or poor health than privately insured children (Byck, 2000).
Interactions and Covariance of Race and Ethnicity, Income, Immigrant Status, and Health Insurance
Finding: Lower-income, minority, non-citizen, or uninsured children consistently have worse access and utilization than do children with none of these characteristics. These factors overlap to a large extent. However, each exerts its own independent effect on access and utilization.
The finding that lower-income, minority, and uninsured children have worse access to and lower use of health care services than other children is well established (Newacheck et al., 2000a; Weinick et al., 2000; McCormick et al, 2001). Further, there is high overlap between poverty, minority status, and lack of insurance. Among children in one of these at-risk groups, 40 percent also belong to other at-risk groups (Newacheck et al., 1996).
This high degree of overlap among risk groups means that results from studies on the impact of gaining insurance must be interpreted with caution. For example, when it is found that poor children have fewer physician visits, this result could be attributable partly to lack of insurance but also to the interplay of other characteristics (e.g., a parent’s inability to take time off from work or a different conception of the value of medical attention for certain kinds of health problems). The results presented in the preceding sections examine the effect of insurance on access and use that are isolated analytically from the effects of income and race or ethnicity. These adjustments help to measure the impact of health insurance status alone. However, more information would be helpful about the effect on utilization for a child who is both uninsured and a member of a minority group or who is uninsured and poor.
Because these risk factors exert independent effects on access and utilization, children who are members of more than one at-risk group (e.g., African American and uninsured; poor and uninsured) tend to have even more difficulty using medical services than do children who are members of only one at-risk group.
Using 1987 NMES data, researchers report that with few exceptions, being low income (below 100 percent FPL), a member of a minority racial or ethnic group, or uninsured is each independently and significantly related to six different measures of access to or use of primary care (Newacheck et al., 1996). When compared with the reference group of children who are white, not low income, and insured, children in each of these at-risk groups are less likely to have a usual source of care and more likely to not see a specific physician even if they have a usual source of care. They are also more likely to wait 60 minutes or more at their sites of care and more likely to go without after-hours emergency care. Uninsured children are least likely to have a usual source of care than the reference group (OR = 0.47), while low-income and minority children are least likely to see a consistent physician within their care site and are most likely to wait a long time for care at their care site (Newacheck et al., 1996).
Dubay and Kenney (2001) investigated differences in access and use for insured and uninsured children below 200 percent of FPL, a group of special interest because it is the target population for Medicaid and SCHIP. In a cross-sectional analysis with extensive sociodemographic and health status adjustments, they found that lower-income children (in families with income less than 200 percent FPL) who have no insurance had significantly worse access to care and lower utilization than either lower-income children insured privately or those who had Medicaid coverage. Uninsured, lower-income children were more likely to have no usual source of care or to use the emergency department as a usual source of care, and to postpone or forgo medical, surgical, and dental care. Their families were less confident about their ability to obtain needed care and less satisfied with whatever care they did receive. In this study, children insured by Medicaid and private plans had similar access measures (i.e., reporting a regular source of care or delays in care) (Dubay and Kenney, 2001).
Race–Ethnicity and Income
Racial and ethnic disparities in access to health care actually increased between 1977 and 1996, particularly for Hispanic Americans (Weinick et al., 2000). Black and Hispanic children are substantially less likely to have a usual source of care than are white, non-Hispanic children, after controlling for health insurance and socioeconomic status (Weinick and Krauss, 2000). Controlling for language, however, eliminates differences between Hispanic and white non-Hispanic children, suggesting that differences in access may be related to English language fluency. The differences between black and white non-Hispanic children remain.
Low-income children of any race are more likely to experience access problems than those with family incomes above the federal poverty level. Newacheck and colleagues (2000a) used NHIS data spanning 1993 to 1996 to examine unmet health needs of America’s children under age 18.9 They found that overall, 7.3 percent of U.S. children (an estimated 4.7 million) experience at least one unmet health care need, but both children below 100 percent FPL and those with family incomes between 100 and 200 percent FPL were more likely to have an unmet need (medical, dental, medication, or vision) than were higher income children, after controlling for health insurance status.
Immigrant Children
Immigrant children have a high risk of being uninsured and face additional barriers to care resulting from language and cultural differences. Parents’ unfamiliarity with U.S. health care, attitudes about accepting public benefits, and fears of challenges to their immigration status all deter immigrants from seeking care for themselves and their children. About 54 percent of non-citizen children with non-citizen parents are uninsured (Ku and Matani, 2001). The Institute of Medicine– National Research Council Committee on the Health and Adjustment of Immigrant Children and Families concluded that health care for children in immigrant families benefits both from insurance coverage and from families’ efforts to establish an ongoing connection with the health care system, as is the case for all children (Hernandez and Charney, 1998).
Only 66 percent of foreign-born children of lower-income working families have access to a regular source of care compared with 92 percent of lower-income U.S.-born children (Guendelman et al., 2001). U.S.-born children of immigrants with no regular source of care and no insurance are the least likely to have seen a physician (Hernandez and Charney, 1998). Immigrants are particularly reliant on safety-net health care providers (Ku and Freilich, 2001).
Differences persist between the health care utilization patterns of immigrant children and those of children of citizens, but disparities are less when only those children in both of these groups who have health insurance are compared. Whereas 43 percent of uninsured immigrant children reported having had no physician visit within the previous 12 months in 1996, the comparable proportion was 28 percent for immigrant children with private coverage and 16 percent for those with Medicaid (Brown et al., 1999).
Special Issues for Adolescents
Finding: Uninsured adolescents are more likely to lack a regular source of care and have unmet health needs than are insured adolescents.
Just as access and use are declining, adolescents encounter new and challenging health care needs. Specifically, reproductive health needs may come into play as many high school students report being sexually active. The need for mental health screening and treatment increases as depression, exposure to violence, and risky behaviors including substance abuse rise. Trips to the emergency department tend to double from the preteen to older adolescent years. The seeds of many behaviors that can lead to chronic diseases—obesity, hypertension, diabetes—are set during this formative period (NCHS, 2000). Finally, late adolescence may be the last time for several years that some youths have ready access to regular care within a medical home because more than a quarter of young adults age 18–25 (7.3 million) are uninsured (Mills, 2001).
McCormick and colleagues (2001) report that as age increases, the percentage of children with any office visits generally declines. Adolescents ages 15 to 17 years have the highest uninsured rate of all children (17 percent), due in part to the age-related income eligibility standards in Medicaid (McCormick et al., 2001). In addition to the risk of increasing age, adolescents with minority status, with lower family income, or who live with a single parent have a greater likelihood of being uninsured (Lieu et al., 1993; Newacheck et al., 1999). Higher proportions of African-American and Hispanic adolescents than white non-Hispanics are uninsured (16 and 28 versus 11 percent, respectively) (Lieu et al., 1993).
Older adolescents’ risk of being uninsured increases markedly with decreasing family income. Among 16–17-year-olds in families with incomes less than 100 percent of the FPL, 38 percent are uninsured; among those in families with incomes in the range of 100–200 percent FPL, 29 percent are uninsured, whereas just 7 percent of adolescents in higher-income families are uninsured.
The percentage of uninsured teens who do not have a health care visit within a year is 2.6 times higher than that for insured teens (NCHS, 2000). Compared with their insured counterparts, uninsured adolescents are substantially less likely to have a regular source of care (71 percent versus 96 percent) or to have had contact with a physician during the course of the past year (75 percent versus 90 percent) (Newacheck et al., 1999). Adolescents who are uninsured are also more likely to have unmet health needs (24 percent versus 6 percent).
Despite having worse reported health status, African-American and Hispanic adolescents have fewer doctor visits annually than their white non-Hispanic peers (1.8, 1.7, and 2.6, respectively) and are more apt to lack a regular source of care. Having health insurance is associated with relatively higher rates of access and use for minority youth than for white non-Hispanic youth (Lieu et al., 1993). In 1988, African-American adolescents with coverage averaged 2.2 visits annually compared to 1.4 for those who were uninsured. Hispanic adolescents with insurance averaged 2.2 visits compared to 1.1 visits annually for those who were uninsured, while non-Hispanic white adolescents had comparable annual visit rates of 2.8 and 2.0.
Children with Special Health Care Needs
Finding: Uninsured children with special health care needs are more likely than are those who have insurance coverage to be without a usual source of health care; to have gone without seeing a doctor in the last 12 months; and to be unable to get needed medical, dental, vision, and mental health care and prescriptions.
Approximately 18 percent of U.S. children under 18 years of age, or 12.6 million children nationally, have a chronic physical, developmental, behavioral, or emotional condition that causes impairment in a basic function such as hearing, seeing, or learning. These children require health and related services of a type or
amount beyond those required by most children (Newacheck et al., 1998a).10 Children with special needs are disproportionately lower income and otherwise socially disadvantaged. Despite their greater expected use of health care services, one out of every nine children with special needs (roughly the same rate as among all children) remains uninsured (Newacheck et al., 1998a). Uninsured children with special needs also are disproportionately likely to be Hispanic and to have mothers with less than a high school education (Aday et al., 1993).
Although the associations between poverty, minority race or ethnicity, and lack of insurance and diminished access hold true for all children, the consequences for children with special needs are particularly concrete and immediate. Both low-income special needs children and those in families with incomes between 100 and 200 percent FPL are more than four times as likely to be uninsured as are children in families with higher incomes (17, 18, and 4 percent, respectively) (Newacheck et al., 2000b). Not surprisingly, given the association between lack of insurance and poverty, parents cite the high cost of health insurance as the primary reason for being without coverage for three of every four children. Further, uninsured special needs children are far more likely than special needs children who have insurance to be unable to get medical care due to cost (adjusted OR = 11.4), according to their parents (Newacheck et al., 2000b).
As is true for uninsured children generally, uninsured children with special needs are more likely than insured children to
-
be without a usual source of health care (OR = 5.8 ),
-
have gone without seeing a doctor in the last 12 months (OR = 2.5), and
-
be unable to get needed medical (OR = 5.8), dental (OR = 4.0), prescriptions or vision care (OR = 3.2) and mental health care (OR = 3.4) (Newacheck et al., 2000b).
This analysis adjusted for sociodemographic factors and measures of health status. These findings confirm results of similar examinations using older surveys (Aday, 1992; Newacheck, 1992; Aday et al. 1993).
HEALTH OUTCOMES FOR CHILDREN AND YOUTH
Establishing the links between health insurance status and clinical outcomes and then estimating population-wide health effects involves several analytical steps.
Population-wide effects may be harder to discern in children than in adults because an even smaller proportion of the child population than the adult population has diagnosed health problems and chronic conditions. Consequently, the immediately apparent effects of health insurance status on health are muted within the largely healthy-child population.
One recent analysis has examined health and functional outcomes for children under age 15 on a broad population basis using the variability among states in instituting Medicaid eligibility expansions to assess the effect of health insurance coverage on episodes of acute illness, restricted activity days, and bed days. Lykens and Jargowsky (2002) combined the NHIS Child Health Supplements data for 1988 and 1991 for children in lower-income families (under 185 percent of FPL) and analyzed these outcomes as a function of the state Medicaid eligibility level. They found a statistically significant decrease for acute illness episodes for non-Hispanic white children and statistically insignificant decreases for non-Hispanic black and Hispanic children. The authors note that these insignificant findings could either be due to small sample sizes or to worse access to care for minority children (Lykens and Jargowsky, 2002). In all cases the findings for restricted activity and bed days were not statistically significant but inversely related to Medicaid income eligibility standards.
It is important also to consider subacute or asymptomatic conditions for which no medical visit is ever sought, particularly as the conditions affect the development of children’s physical and mental capabilities. When no care is sought, this introduces a methodological limitation to studies of health outcomes dependent on insurance status: rates of “no shows” can be quantified only indirectly and the attendant health consequence may be difficult to quantify. Pent-up demand for care clearly exists for uninsured children, as illustrated by the evaluation of the Pennsylvania insurance expansion described earlier: the portion of children reporting unmet need dropped from 57 percent to 16 percent 12 months following the program expansion (Lave et al., 1998a).
When uninsured sick children do not receive appropriate care, the consequences may be serious. This section examines the relationship between health insurance and health outcomes, including mortality, disease severity, condition-specific morbidity, and avoidable hospitalizations. Lack of insurance results in poorer access to and use of health care, which in turn leads to delays in seeking care for a serious medical condition and possibly no visits for less serious conditions. Delaying care has several consequences:
-
it may be detrimental for the health and survival of a child because the condition or disease can become more advanced;
-
this increased severity frequently demands a more intense level of treatment (e.g., hospitalization) when it is finally obtained; and
-
any lingering physical and mental health problems may affect a child’s chances for success in school and life.
Delays in Care for Uninsured Children and Youth
Finding: Uninsured children often receive care late in the development of a health problem or do not receive any care. As a result, they are at higher risk for hospitalization for conditions amenable to timely outpatient care and for missed diagnoses of serious and even life-threatening conditions.
Parents of uninsured children often opt not to seek care for what appear to be non-life-threatening conditions and for which insured families in otherwise similar circumstances would consider medical attention necessary, as would medical providers. This lack of care can have both physical and psychosocial repercussions. Studies of injuries and mental health problems illustrate diminished care seeking for uninsured children with these conditions. Some conditions (e.g., asthma, ear, nose, and throat [ENT] infections and their complications; vaccine-preventable diseases) respond to timely outpatient care, and without that care, unnecessary hospitalizations frequently follow. In the worst cases of delayed care seeking on the part of families and the failure of the health care system to provide the same intensity of services to uninsured children, the uninsured child has a greater risk of dying.
Uninsured children with certain diagnoses have been found to be more likely to die than insured children, due to failure to reach a hospital or receive appropriate specialized care until late in the course of the illness and to the greater severity of illness at presentation resulting from delayed care. Two studies illustrate worse survival rates for uninsured children, one for coarctation of the aorta and the other for trauma.11
In one study, uninsured infants under 1 year of age with coarctation of the aorta were more likely to die than infants with any type of health insurance (33 versus 3.8 percent), controlling for case severity (Kuehl et al., 2000).12 Fifty-five (55) percent of the deaths occurred prior to surgical treatment, and one-third occurred without diagnoses. The authors report that parents had unsuccessfully attempted to obtain medical care for their children, delaying their diagnosis and an intervention that could improve their chances for survival.
Using data in the National Pediatric Trauma Registry, Li and Davis (2001) report that compared to pediatric trauma patients with commercial insurance, both patients with public insurance and those without any coverage had a significantly increased risk of in-hospital mortality (relative risk [RR] = 1.48 and 2.02, respectively). This increased risk existed in different age groups and for both blunt and penetrating trauma patients, and the increased risk remained statistically significant after adjusting for injury severity.
Uninsured children are less likely to receive medical attention for their injuries. Overpeck and Kotch (1995) report that children without insurance had lower rates of both total and serious injuries that received medical attention, compared with the rates for children covered by Medicaid or private insurance. They estimated that uninsured children are 30 percent less likely to receive medical attention for their injuries than are insured children and 40 percent less likely to receive medical attention for serious injuries than are insured children. Further analysis by these authors found that this experience of lower rates of medically attended injuries for uninsured children applied across racial and ethnic groups (African-American, non-Hispanic white, and Mexican-American children) (Overpeck et al., 1997).
Hospitalization for conditions that could have been treated at a less advanced stage, sometimes called ambulatory-care-sensitive conditions (ACSCs), has been used as a population-level indicator of access to appropriate outpatient services. For children, some common, potentially avoidable hospitalizations are for asthma, pneumonia, seizures, and gastrointestinal infections. Prompt and, for chronic conditions such as asthma, regular attention by a primary care provider can better manage the underlying condition and forestall its exacerbation to a point where hospitalization is required.
Lack of insurance is one barrier to timely and appropriate primary care, and several studies have explored ACSCs for child populations and their relationship to insurance status. As in cross-sectional studies of ACSCs for adults, cross-sectional studies of children find that those enrolled in Medicaid have higher population rates of hospitalizations for ACSCs than do either privately insured or uninsured children (Pappas et al., 1997; Parker and Schoendorf, 2000; Shi and Lu, 2000). Some, but not all, studies report higher rates of avoidable hospitalizations among uninsured as compared with privately insured children. These researchers attribute the lower rates of hospitalization for these conditions among uninsured children to access barriers that they face even for exacerbated conditions that often require hospital care. Younger children, children who live in poorer neighborhoods, and African-American children also have higher rates of ACSCs than do older children, children in wealthier areas, and white, non-Hispanic children (Parker and Schoendorf, 2000; Shi and Lu, 2000).
Studies of a population over time, however, suggest that increased Medicaid coverage may have reduced rates of avoidable hospitalizations. Dafny and Gruber (2000) evaluated avoidable hospitalizations among children under age 16 between 1983 and 1996 as a function of state-level Medicaid eligibility standards and found that Medicaid eligibility expansions over this period reduced avoidable hospitalizations on a population basis 22 percent.
Kaestner and colleagues (2001) examined the effect on ACSC hospitalizations by comparing NHIS data before (1988) and after (1992) the Medicaid eligibility expansions initiated in the late 1980s. They report that the incidence of ACSC hospitalizations decreased among children ages 2–6 years living in the lowest-income areas (family income <$25,000 annually), those most likely to have gained
Medicaid coverage following the expansions. However, for children ages 7–9 (the only other group studied) the results were mixed. Children in this older age group were less likely to have been affected by the expanded Medicaid programs, which increased eligibility and enrollment to a greater extent for children under age 6.
Timely receipt of immunizations for childhood diseases is important in its own right and also indicates a population’s access to primary health care services. An evaluation of the children’s health insurance expansion in New York found that the immunization rate in New York State rose from 83 to 88 percent for all children ages 1 to 5 following the introduction of this program (Rodewald et al., 1997). The increase was greatest among previously uninsured children and among those who had had a gap in insurance coverage longer than six months. As noted previously, visits to health department immunization clinics decreased by 67 percent and visits to primary care providers’ offices increased by 27 percent (Rodewald et al., 1997). Thus, insurance coverage for children who were previously uninsured results not only in an improved overall immunization rate but also in a shift in the provision of services from health departments to a medical home.
EFFECT OF HEALTH ON CHILDREN’S LIFE CHANCES
Finding: Undiagnosed and untreated conditions that are amenable to control, cure, or prevention can affect children’s functioning and opportunities over the course of their lives. Such conditions include iron deficiency anemia, otitis media, asthma, and attention deficit– hyperactivity disorder.
Adverse impacts on the health of children have special significance because childhood illnesses, left untreated, can affect not only present health but also future development. For example, illnesses may result in absences from school, which may in turn affect learning (Wolfe, 1985). Achievement may also be lowered by moderate or severe psychological problems (Wolfe, 1985). Further, specific illnesses (e.g., untreated and chronic ear infections), can hurt a child’s life chances in more direct ways (by impairing hearing). Of course, health is only one in a constellation of factors that affect a child’s life chances.
In this section, the Committee examines five conditions or diseases: iron deficiency anemia, dental disease, otitis media, asthma, and attention deficit– hyperactivity disorder. They were selected from among the many conditions that may affect children’s life chances because these are very common, have extensive literatures, and most importantly, are amenable to therapy. There is limited or no research that directly connects the evidence about long-term impacts of these untreated health conditions in children to their health insurance status. However, studies of overall access to and utilization of care by children demonstrate that a lack of insurance can lead to delayed therapy or no therapy. Research that evaluates
and documents the relationships between particular child health outcomes and health insurance status would help make this argument more definitive.
Iron Deficiency Anemia
Iron deficiency anemia, the most prevalent nutritional deficiency in childhood, has been linked to mental retardation and poor school performance (Dallman et al., 1984; Lozoff et al., 1998). Approximately 9 percent of toddlers, 9–11 percent of adolescent girls, and 11 percent of women of childbearing age in the United States are iron deficient (Looker et al., 1997). There is an increased likelihood of mild or moderate mental retardation associated with anemia, the risk increasing with the severity of the anemia (Hurtado et al., 1999). Academic deficiencies and developmental delays are seen in children who were iron deficient early in life and then followed throughout their school career, as well as in students of all ages whose iron levels are currently too low (Otero et al., 1999; Lozoff et al., 2000; Grantham-McGregor and Ani, 2001; Halterman et al., 2001). Importantly, the long-term health risks of iron deficiency are frequently interrelated with other detrimental environmental exposures and social and economic deprivations, which may intensify the likelihood of poorer outcomes (Lozoff et al., 1998; Shonkoff and Phillips, 2000).
Dental Disease
Dental care is incorporated into employment-based health insurance plans less often than it is excluded (KPMG, 1998). For children, however, dental services have been part of the basic Medicaid benefit package through the Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Program and are frequently included in SCHIP plans as well. Thus, the Committee includes dental services in this review focused on children, while it did not consider dental services in its review of health outcomes for working-age adults. Dental care was recently identified as the most prevalent unmet health need among American children (Newacheck et al., 2000a). Among 5–17-year-olds, dental caries are five times as common as a reported history of asthma (NCHS, 1996). Children in families with incomes below the federal poverty level are more likely not only to have decayed teeth, but also to have them go untreated: 37 percent of poor children (aged 2 to 9 years) compared to 17 percent of non-poor children have one or more untreated decayed primary teeth (Litt et al., 1995; NCHS, 1996; Vargas et al., 1998). Just 20 percent of lower-income children had a preventive dental care visit in 1996, less than half the proportion of children under 18 overall (43%) who had such a visit (DHHS, 2000). Untreated oral disease in children is associated with compromised nutrition (Acs et al., 1999), serious general health problems, pain, problems with eating, overuse of emergency rooms, activity limitation, sick bed days, and lost school time (Brunelle, 1989; NCHS, 1997; Edmunds and Coye, 1998).
Otitis Media
Recurrent otitis media and otitis media with effusion (middle-ear disease) are common in children before 3 years of age and may be associated with hearing loss (Lanphear et al., 1997). A substantial body of research exists demonstrating the negative impact of these conditions on expressive language ability, cognitive ability, auditory perception, school readiness for preschoolers, and school performance for students (Teele et al., 1990; Zargi and Boltezar, 1992; Lous, 1995; Mody et al., 1999; Roberts et al., 2000; Casby, 2001).
Asthma
Asthma is the most common chronic childhood illness (CDC, 1996a). Asthma disproportionately affects poor and minority populations (Gergen and Weiss, 1990; Carr et al., 1992; Lang and Polansky, 1994; Taragonski et al., 1994). Children with asthma miss significantly more days of school than do nonasthmatic children (McCowen et al., 1996; Silverstein et al., 2001). A number of studies suggest that asthmatic children do not do worse academically than their non-asthmatic classmates (Gutstadt et al., 1989; Lindgren et al., 1992; Celano and Geller, 1993; Rietveld and Colland, 1999; Silverstein et al., 2001). However, children with uncontrolled and more severe asthma may be at greater risk for language and/or learning disorders and poor academic performance (Celano and Geller, 1993; Lubker et al., 1999). Children whose asthma is not under control may be either diagnosed and receiving poor medical management or undiagnosed with no proper management.
One multicenter study of children with asthma assessed the quality of asthma care received by uninsured children as significantly worse than that received by insured children (Ferris et al., 2001). As discussed earlier in this chapter, a before-and-after comparison study of an SCHIP prototype program in New York found that asthma care and parent-evaluated health outcomes for children with asthma improved after enrollment in the program (Szilagyi et al., 2000a).
Attention Deficit–Hyperactivity Disorder (ADHD)
ADHD is the most commonly diagnosed behavioral disorder of childhood and is estimated to affect between 3 and 5 percent of school-aged children. Symptoms of ADHD include developmentally inappropriate levels of attention, concentration, activity, distractability, and impulsivity both in early childhood and during the school years. ADHD has been linked to lower school readiness (DuPaul et al., 2001), poorer academic performance (Fischer et al., 1990; Frick et al., 1991; Shelton et al., 1998; Marshall et al., 1999; Willcutt et al., 2000; Merrell and Tymms, 2001), lower vocational attainment (Mannuzza et al., 1997), and less optimal social and emotional development (NIH, 2000). The general incapacity to sustain attention, even in children who are not formally diagnosed with ADHD, is
also linked to having to repeat a grade more often than children without behavioral problems (Gordon et al., 1994).
Mannuzza and Klein (2000) examine the developmental course of ADHD and conclude that in adolescence, there remain relative deficits in academic and social functioning for two-thirds to three-quarters of these children. These deficits are manifested in lower grades, more courses failed, worse performance on standardized tests, having fewer friends, and lower psychosocial adjustment.
Lack of insurance is one important barrier to evaluation and treatment of ADHD (NIH, 1998). For those who do have insurance, many families cannot afford out-of-pocket costs for services not covered, and coverage of mental health services in private insurance plans is often very limited. Although evidence of the importance of ADHD as a health and developmental problem is plentiful, the impact of health insurance coverage on receipt of appropriate care for this condition is lacking, as it is for child mental health services in general.
PRENATAL AND PERINATAL CARE AND OUTCOMES
This section examines how health insurance status affects the receipt of health care by uninsured pregnant women and outcomes for both mother and child. The expected relationships between health insurance, health care, and health outcomes for pregnant women and infants are illustrated in Figure 6.1. The section is organized according to the following:
-
access to and use of prenatal care,
-
hospital-based perinatal care, and
-
health outcomes for mother and infant.
Insurance status can affect whether a pregnant woman seeks care and how often, the services and facilities available to her, and ultimately her own health and that of her infant. Both cross-sectional studies and natural experiments provide evidence of the influence of insurance status on prenatal care.13 Factors that covary with health insurance status and also affect access to and use of care include socioeconomic status, educational attainment, and racial and ethnic identity (IOM, 2002a; IOM, 2002b). These factors are controlled for in the most rigorous studies, although sometimes adjustments for characteristics such as income are imputed from aggregate-level data if this information is not available from individual
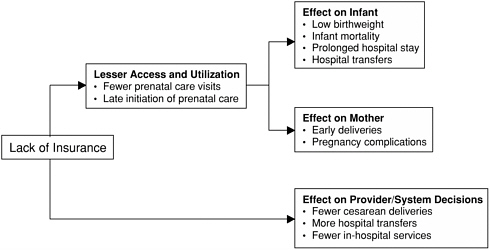
FIGURE 6.1 Effects of having no insurance on outcomes for pregnant women and infants.
Access and Use of Prenatal Care
Finding: Uninsured women receive fewer prenatal care services than their insured counterparts and report greater difficulty in obtaining the care that they believe they need. Studies find large differences in use between privately insured and uninsured women and smaller differences between uninsured and publicly insured women.
Box 6.2 summarizes professional standards and national statistics for prenatal care.
A recent study based on the national Community Tracking Study Household Survey conducted in 1996 and 1997 reports that, on average, uninsured women have fewer prenatal care visits that women with health insurance and 15 percent had no prenatal visits, compared to 4 percent of women with private or public coverage (Bernstein, 1999). This same study found that 29 percent of uninsured pregnant women did not have a usual source of care, compared to 14 percent of women with Medicaid and 9 percent of those with private health insurance. Eighteen (18) percent of uninsured women also reported an unmet need for care, more than twice the rate of privately or publicly insured pregnant woman (Bernstein, 1999).
State-specific studies also find less use of prenatal care among uninsured women than among women with insurance. In California, investigators report that uninsured women were more likely than privately insured women to initiate
|
BOX 6.2 Prenatal Care
|
prenatal care late (OR = 2.54) and to have too few prenatal visits (Braveman et al. 1993).
A number of studies examine changes in care patterns across entire populations when insurance coverage changes. These studies have taken advantage of the large-scale expansions of Medicaid coverage for previously uninsured women that began in 1986. Prior to these expansions, pregnant women were eligible for Medicaid only if they were single and received income support benefits or if they met very low income thresholds. By 1990, Medicaid eligibility was universal for all pregnant women and newborns in families with incomes below 133 percent of FPL, although states were allowed to raise the income ceiling to 185 percent FPL.
Enrollment grew rapidly and the number of pregnant women with health insurance grew substantially (Howell, 2001).14 By 1991, 43 percent of women of childbearing age were eligible for Medicaid coverage and about a third of deliveries
in that year were covered by Medicaid (Singh et al., 1994; Currie and Gruber, 1996a). However, a significant percentage of pregnant women remained uninsured. In California, for example, 11 percent of births in 1990 were to women who remained uninsured for prenatal care (Braveman et al., 1993).
Some of the studies of the impact of the Medicaid program expansions examine changes in utilization across entire populations, rather than by comparing insured and uninsured groups. In general, these studies have found that among low-income women within a particular state, the timeliness with which prenatal care is initiated and the total number of visits are improved (Cole, 1995; Kenney and Dubay, 1995; Ray et al., 1997; Long and Marquis, 1998; Currie and Grogger, 2002). For example, a study in Florida in 1991 after its Medicaid expansion, found that the percentage of low-income women (including both uninsured and publicly insured women) who received no prenatal care dropped from 2.3 to 1.6, their total number of visits increased on average, and fewer women entered care late than had done so prior to the expansion in 1989 (Long and Marquis, 1998).
Three nationwide studies comparing prenatal care indicators in counties that had expanded coverage to those without expansions report that the rate of timely initiation of prenatal care in counties with expanded programs is slightly higher (Cole, 1995; Kenney and Dubay, 1995; Dubay et al., 2001). Other studies have shown that improvements in prenatal use are limited to certain geographic areas (i.e., South and Midwest) and to some groups of women (e.g., white women, teenagers) (Cole, 1995; Coulam et al., 1995; Howell, 2001).
State-level studies in four states (Tennessee, California, Massachusetts, and Wisconsin) show no difference in prenatal care use before and after expansion (Piper et al., 1990; Braveman et al, 1993; Haas et al. 1993b) whereas studies in three states (a later study in Tennessee, Missouri, and Florida) do find better prenatal care use following expansion (Coulam et al., 1995; Ray et al., 1997; Long and Marquis, 1998). The states with improvements in prenatal care use were those that had the most restrictive eligibility standards for Medicaid prior to the expansions (Howell, 2001).
Several studies have examined the quality of prenatal care used by a cross section of privately insured, publicly insured, and uninsured women at a point in time, controlling for variables such as maternal education, marital status, race and ethnicity.15 The investigators find large differences in utilization between privately insured and uninsured women and smaller differences or no differences between uninsured and publicly insured women (Braveman et al., 1993; Amini et al., 1996; Bernstein, 1999). The researchers evaluating the California experience with a Medicaid expansion reported that uninsured and Medicaid-enrolled women as a single group are much more likely than those with private insurance to receive no prenatal care (OR = 6.7) (Braveman et al., 1993).
Hospital-Based Perinatal Care
Finding: Health insurance status affects the care received by women giving birth and their newborns. Uninsured women and their newborns receive, on average, less prenatal care and fewer expensive perinatal services.
At the time of delivery, the care received by uninsured women and their newborns differs from the care received by women and newborns that are covered by health insurance. Studies that have examined providers’ and pregnant women’s decision making find that uninsured pregnant women and their newborns are less likely to have certain more expensive maternity and neonatal services. Procedures and services such as cesarean sections and neonatal intensive care can have a substantial financial impact on providers. Researchers have also looked at whether patients of lower socioeconomic status have lower expectations for the care that they receive.
Obstetric Services
Insurance coverage affects the services women receive at childbirth. A study based on hospital data over the period 1987–1992 of rates of use of four obstetric procedures: cesarean section, use of fetal monitor, ultrasound, and induction of labor among women covered by Medicaid found that, among those most likely to have been without Medicaid prior to coverage expansions, use of each of these procedures increased. However, among those women who were most likely to have been covered by private health insurance before expanded Medicaid coverage, increased Medicaid coverage resulted in lesser use of these technologies at birth (Currie and Gruber, 2001).
There is a strong relationship between insurance status and cesarean section rates, with uninsured women less likely to receive cesarean sections (Keeler and Brodie, 1993). It is difficult to determine the extent to which the differences in cesarean section rates between insured and uninsured women are due to overuse of the procedure among women with coverage and to underuse of the procedure among uninsured women. Overuse of cesarean section is well documented (ACOG, 2000; DHHS, 2000). Nonetheless, it is apparent that economic incentives are at work in the case of both insured women’s rates of cesarean section and uninsured women’s rates, incentives that act in opposite directions.
At the time data were collected by Keeler and Brodie (1993), cesarean section charges, including both hospital and physician fees, were 66 percent higher than those for vaginal deliveries. Hospitals are unlikely to recoup fully the costs of care provided to uninsured women, and hospitals lose more money when deliveries are by cesarean section than when they are vaginal.
Financial incentives also exist for the women themselves who are giving birth. Whereas out-of-pocket costs for mothers with fee-for-service insurance may be
low, uninsured mothers may face substantial out-of-pocket costs. Because of limited resources to pay for the deliveries of uninsured women, these women, their physicians, and hospitals all have incentives to opt for less expensive alternatives when clinical considerations allow for choice.
Studies of cesarean section rates have the same methodological problem as other outcomes studies; health insurance status is associated with other factors such as age, race and ethnicity, income, and education that also affect these rates. Analyses adjust for at least some of these factors to isolate and measure the contribution of health insurance status to the likelihood of being delivered by cesarean section. Studies in California (Stafford, 1990; Stafford et al., 1993), Ohio, and Maine, New Hampshire, and Vermont (Aron et al., 2000) found substantial differences in adjusted cesarean section rates by payment source, with uninsured women having the lowest rates. The rates for women with public insurance tend to fall between those for uninsured and privately insured women. Haas et al. (1993a) reported an increase in cesarean section rates after expansion of Medicaid in Massachusetts.
Some studies that have examined the relationship between health insurance status and rates of cesarean section have also taken clinical appropriateness into account. One study reported that in cases where cesarean section was more clearly indicated, such as with breech presentation, fetal distress, or failure of labor to progress, uninsured women were still significantly less likely than those with any form of insurance to receive a cesarean section (Stafford, 1990). Aron and colleagues (2000) found that after adjusting for a wide variety of maternal and neonatal risk factors, uninsured women were less likely to receive a cesarean section (OR = 0.65, p = .067). While not statistically significant at the conventional .05 level, this finding was consistent across all levels of clinical risk. Of particular concern is the lower rate of cesarean section among the very high-risk women who were uninsured.
Site of Care
Differences in the care received by low-birthweight babies with differing health insurance status may stem from differences in the resources available to the hospitals that predominantly treat patients with either private, public, or no coverage. A study conducted among maternity patients in San Francisco revealed that privately insured women at high risk for complications were much more likely to deliver at a hospital with neonatal intensive care facilities than were similar women with Medicaid or without insurance (Phibbs et al., 1993). Hospitals with more privately insured patients, especially those with more privately insured low-birthweight newborns, have more neonatal intensive care beds than do those with fewer such patients (Glied and Gnanasekaran, 1996). The result persists within hospital categories (public, private nonprofit, and proprietary) and after adjusting for low birthweight and other measures of patient need.
Uninsured pregnant women and newborns may be more likely to be trans-
ferred between hospitals than are those with private insurance. A study conducted in southeastern Pennsylvania found that uninsured newborns were twice as likely (RR = 1.96) to be transferred to another general or specialty acute care hospital than were similar infants with private insurance, after controlling for prematurity, severity of illness, and expertise of neonatal care in the referring hospital (Durbin et al., 1997).
Health Outcomes for Mother and Infant
As depicted in Figure 6.1, health insurance status is hypothesized to affect the extent of premature deliveries and pregnancy complications in mothers and of low birthweight, mortality, and prolonged hospital stays for infants. The benefits of appropriate prenatal care accrue to both the newborn and the mother, resulting in improved birth outcomes, particularly in reduced rates of low birthweight and a subsequent reduction in infant mortality. For the mother, good prenatal care is expected to translate into reduced complications of pregnancy.
Birth Outcomes
Finding: Uninsured newborns are more likely to have adverse outcomes, including low birthweight and death than are insured newborns. Evidence of improvement in outcomes for newborns as a result of increased population health insurance rates is mixed, however.
Box 6.3 presents national statistics on birth outcomes. Investigators have examined the effect of insurance on birth outcomes using measures such as low birthweight, prematurity, prolonged hospital stays, in-hospital services, and infant mortality.
Low Birth Weight and Prematurity. Evaluations of Medicaid expansions to previously uninsured women have yielded mixed results for improvements in birthweight and rates of prematurity. Two of five national studies found no effect of increased insurance coverage of the population overall on these factors (Kenney and Dubay, 1995; Currie and Gruber, 1996a) while the remaining three found improvements only for select subgroups (white women and black teenagers [Cole, 1995]; white women without a high school diploma [Dubay et al., 2001]; white women had a lower incidence of very low birthweight babies [Currie and Grogger, 2002]).
State-level studies also show mixed effects after widening Medicaid eligibility and expanding benefits. In Florida, Long and Marquis (1998) report a reduction in low birthweight for the expansion group relative to low-income women with private insurance. An expansion in Washington that includes supportive services and counseling was associated with a reduction in the ratio of low birthweight infants. Reduction was greatest among high-risk women with preexisting condi-
|
BOX 6.3 Neonatal Outcomes
|
tions such as diabetes or hypertension (Baldwin et al., 1998). In Colorado, a state without additional supportive services, the rate of low-birthweight infants among medically high-risk women increased slightly during the same period.
Infant Mortality. Infants of uninsured women are more likely to die than are those of insured women. In one region of West Virginia, the fetal death rate dropped from 35.4 to 7.0 per 1,000 live births after introduction of a prenatal care program for the uninsured (Foster et al., 1992). Despite this decline, the fetal death rate among uninsured women was still twice that among privately insured women, and the rate for the uninsured climbed again to 10.3 after the program was discontinued (Foster et al., 1992).
A nationwide analysis of insurance coverage and Women, Infants, and Children (WIC) program participation based on the 1988 National Maternal and Infant Health Survey (NMIHS) found that despite the more adverse risk profile of infants born to mothers with Medicaid coverage compared to those born to uninsured mothers, uninsured infants had a significantly higher risk of death due to endogenous causes (i.e., those that are closely related to pregnancy and delivery) (OR = 1.42) than did either Medicaid (OR = 1.04) or privately insured infants (the comparison group) (Moss and Carver, 1998).
Two studies of Medicaid expansions examined their impact on infant mortality (Currie and Gruber, 1996a; Howell, 2001). Currie and Gruber calculated an overall population reduction in infant mortality of 8.5 percent associated with a 30
percentage point increase in Medicaid coverage among women 15–44 between 1979 and 1992. The authors acknowledge that they are unable to determine whether the mortality decrease should be credited to better prenatal care or to more intensive hospital care after birth. Howell’s original analysis finds no significant differences in the rates of change in infant mortality for unmarried women as a function of the extent of Medicaid expansions between 1985 and 1991. She concludes that the decline in infant mortality found by some investigators after Medicaid expansions is in part a consequence of improvements in the care of fragile infants during the same time period and suggests that the Medicaid expansions provided additional resources to hospitals that allowed them to add, improve, or expand neonatal intensive care services (Howell, 2001).
In Tennessee, no decrease was observed in infant mortality but there was also no increase in the use of prenatal care in the first trimester (Piper et al., 1990). In Missouri, Coulam and colleagues (1995) likewise found no impact on mortality but also report improvements in prenatal care among enrolled low-income teens.
Prolonged Hospital Stays and In-Hospital Services. In the several years before Medicaid expansion (1982 to 1986), the percentage of newborns without health insurance in California increased by 45 percent (from 5.5 to 8.0 percent). Hospital discharge data on births to residents of selected counties show the consequences of this decline in coverage (Braveman et al., 1989). Researchers found that the increasing uninsured rate over time was associated with an elevated and increasing risk of adverse outcomes in newborns (defined as prolonged hospital stay, transfer of the newborn to another institution, or death), after adjusting for race or ethnicity. These results are most marked in African-American (OR = 2.24) and Hispanic populations (OR = 1.56). The authors suggest that inadequate and diminishing access to care accounts for the increased rates of adverse outcomes and that this disproportionately affects minority populations.
Looking at length of hospital stay alone, on average, uninsured infants do not stay as long in the hospital or receive the same scope of services while in the hospital as do privately or publicly insured infants. A retrospective analysis of discharge data from all California acute care hospitals demonstrated a link between newborns’ insurance coverage and the allocation of hospital services as measured by total hospital charges and charges per day (Braveman et al., 1991). After controlling for race and ethnicity, diagnoses, hospital characteristics, and disposition, sick newborns without insurance received fewer inpatient services than did comparable privately insured newborns. The mean stay was 15.7 days for privately insured newborns, 14.8 days for Medicaid-covered newborns, and 13.2 days for uninsured newborns. Resources for newborns covered by Medicaid were generally greater than for uninsured and less than for privately insured newborns, despite the fact that both uninsured and Medicaid-covered newborns had more severe medical problems than did those with private coverage.
Maternal Outcomes
Finding: Uninsured women are more likely to have poor outcomes during pregnancy and delivery than are women with insurance. Studies have not demonstrated an improvement in maternal outcomes related to health insurance alone.
Studies find that uninsured women have higher rates of adverse maternal outcomes, such as pregnancy-related hypertension, placental abruption, and extended hospital stays, than do privately insured women (Weis, 1992; Haas et al., 1993a). Despite the greater likelihood of maternal complications, uninsured women have shorter hospital stays than either publicly or privately insured women (Weis, 1992).
Although better prenatal care may be associated with better obstetrical outcomes, insurance coverage alone may not be enough to improve infant or maternal outcomes detectable at the population level (Weis, 1992; Haas et al., 1993b). Smoking, substance use, poor diet, and other health-related behaviors affect birth outcomes and providing health insurance coverage alone is unlikely to change these behaviors (Joyce, 1987). With respect to the use of prenatal care, other factors beyond insurance, such as the mother’s level of education, the availability of providers in general and a regular source of care in particular, may also be important determinants (Braveman et al., 2000).
The point at which health insurance becomes available to women of childbearing age also affects the adequacy and timeliness of prenatal care, which become important when examining the effect of coverage on birth outcomes. Ellwood and Kenney (1995) note that depending on the state, 39 to 54 percent of women enrolled in Medicaid after the first trimester of pregnancy. When the State of Washington, in addition to providing insurance coverage, also provided assessment, education intervention, and nutritional and psychosocial counseling to pregnant women and targeted case management to women needing further services, substantial improvements in birthweight were achieved for high-risk mothers (Baldwin et al., 1998). Another study in California reports that provision of at least one nutrition, psychosocial, and health education service session each trimester of care is significantly associated with better birth outcomes, compared to provision of fewer sessions (Homan and Korenbrot, 1998). Nonetheless, insurance remains an important determinant of access to and utilization of health care by low-income women, who have significantly more trouble obtaining care, receive fewer recommended services, and are more dissatisfied with the care they receive than their insured counterparts (Salganicoff and Wyn, 1999).
SUMMARY
Having health insurance increases the chances that infants, children, and pregnant women will receive preventive services when well and timely medical
care when sick or at high risk of poor outcomes. These, in turn, help avoid unnecessary hospitalizations, premature births, extended morbidity, or even death.
Less Access and Use
Uninsured children have poorer access to health care, use fewer services, and delay seeking care. This scenario repeats itself for uninsured pregnant women and newborns. Having a medical home is a hallmark of quality pediatric care, and uninsured children are less likely to have a medical home than are children with health insurance of any kind. The deficits in health services for the uninsured extend to
-
preventive medical, dental, and mental health care for children and youth;
-
care when a child is sick or has special health care needs;
-
access to prescription medications;
-
prenatal care, more expensive obstetrical procedures, and length of maternal stay; and
-
specialized care such as interventions for children with injuries or coarctation of aorta.
Too often uninsured parents do not seek care that insured parents and their providers would consider necessary. Disparities stem from their financial constraints and from providers’ decisions to provide less intensive services to uninsured patients or the failure to develop health facilities that are geographically accessible to uninsured populations.
Interplay of Insurance with Race, Poverty, and Immigrant Status
Low-income, minority, non-citizen, and uninsured children and pregnant women fare worse than those with health insurance in access to care. Uninsured children and pregnant women usually have one or more of these additional risk factors. Each characteristic exerts its own independent effect on access and utilization, but insurance remains a significant factor even after controlling in research studies for poverty, race, and ethnicity (Haas and Adler, 2001). Those who are members of more than one risk group have greater difficulty obtaining care and worse health outcomes.
Type of Insurance
Children and pregnant women with private health insurance are most likely to receive adequate health care. Generally, those with no health insurance have the least adequate care, and those with Medicaid coverage have access and utilization experiences intermediate between the privately insured and the uninsured.
Lack of private insurance is a strong risk factor for receiving inadequate medical care for children or inadequate prenatal care. On measures of access and use, generally the uninsured have the least access to and use of health care services, with persons with Medicaid coverage being intermediate between those who are uninsured and those with private insurance. Sometimes, however, there is little difference between having Medicaid coverage and being uninsured. Children insured through public programs are at greater risk than privately insured children of experiencing periods without coverage because of the frequent need to reestablish eligibility. These gaps may interrupt relationships with a usual source of care, resulting in access problems comparable to those faced by the uninsured.
Studies of Expanded Insurance Coverage
Natural experiments that compare the experiences of a population before and after expansion of public insurance coverage demonstrate improvements in access to and use of care for uninsured children and frequently for pregnant women as well. These natural experiments allow assessment of population-wide changes in care patterns when insurance coverage is made available.
In the public program expansions and demonstrations reviewed earlier in this chapter, newly insured children experienced increased access to a medical home and were more likely to visit primary care practitioners, specialists, and dentists. In one state, this increased access was accompanied by a 5 percent decrease in emergency department use and, in the other, by a 36 percent decline in hospitalizations.
Investigators generally, but not always, find that timeliness of initiating prenatal care and the total number of prenatal visits for low-income women are better after the Medicaid expansions. The states with the greatest improvements tended to be those that had the most restrictive eligibility prior to expansion.
Health Impact of Delayed or No Care
When needed care is delayed or nonexistent, health can deteriorate. We have the ability to prevent or control many of the health problems associated with common childhood conditions that can have a long-term detrimental impact on children’s development and opportunities in life. This argues for access to well-child care for all children to identify problems early and manage chronic conditions effectively. Delays in receipt of care when acutely ill are also more common for uninsured children than for those with coverage. Uninsured children are more likely to be hospitalized than privately insured children for conditions such as pneumonia or asthma because they are less likely to receive appropriate care early in the course of their illness. Similarly, women with less prenatal care, particularly those at high risk of complications, may have worse obstetrical outcomes. The newborns of uninsured mothers have longer hospital stays and have a higher mortality rate. Uninsured mothers themselves have higher rates of complications
of delivery than do privately insured women but have shorter hospital stays despite more maternal complications.
Improving Health Outcomes Through Expanded Insurance Coverage
Evaluations of expansions in health insurance coverage for children and pregnant women indicate that health outcomes improve with coverage. Children’s access to and utilization of appropriate health care, a positive outcome in itself, improves with higher rates of insurance coverage. In examining population-wide improvements in birthweight and prematurity due to public insurance expansions, some states found no improvement while others identified progress for selected groups (e.g., white women and black teenagers). Attributing improvements in infant mortality to insurance expansions is complicated by co-occurring improvements in neonatalogy. The population effect of public insurance eligibility expansions on utilization and health outcomes is less than some experts would predict based on the substantial number of pregnant women who are eligible. However, a significant number of eligible women do not enter prenatal care in the first trimester or enroll at all.
This chapter has reviewed the research addressing the impact of insurance status on access to health care, its use, and ultimately, health outcomes for children, pregnant women, and newborns. Although having insurance makes a difference, simply making insurance available may not be enough to improve health care and health outcomes for all of the uninsured. Some high-risk groups may require additional services (e.g., educational interventions, targeted case management) if they are to obtain good preventive and routine care.


































