Summary
Many achievements in reducing mortality and morbidity during the past century can be traced directly to public health initiatives. The extent to which we are able to make additional improvements in the health of the public depends, in large part, upon the quality and preparedness of the public health workforce, which is, in turn, dependent upon the relevance and quality of its education and training. This report examines an essential component of the public health workforce—public health professionals.
COMMITTEE CHARGE
The charge of this committee was to develop a framework for how, over the next 5 to 10 years, education, training, and research in schools of public health could be strengthened to meet the needs of future public health professionals to improve population-level health. The committee also was asked to develop recommendations for overall improvements in public health professional education, training, research, and leadership. A wide range of institutional settings, including not only schools of public health but also degree-granting programs in public health, medical schools, schools of nursing, other professional schools (e.g., law), and local, state, and federal public health agencies, play important roles in public health education, training, research, and leadership development. This report presents conclusions and recommendations for each of these institutional settings that are directed toward improving the future of public health professional education in the United States.
DEFINITION
Public health professionals receive education and training in a wide range of disciplines, come from a variety of professions, work in many types of settings, and are engaged in numerous kinds of activities. One thing public health professionals have in common is a focus on population-level health. For purposes of this study, therefore, the committee developed the following definition: A public health professional is a person educated in public health or a related discipline who is employed to improve health through a population focus. Nearly all public health professionals encompassed by this definition have earned at least a baccalaureate degree.
CHALLENGES
As we begin the 21st century, public health professionals are faced with major challenges including globalization, scientific and technological advances, and demographic changes. The health of the U.S. population is increasingly affected by globalization and its accompanying environmental changes. Increased travel, trade, economic growth, and diffusion of technology have been accompanied by negative social and environmental conditions, a greater disparity between rich and poor, environmental degradation, and food security issues. There is increasing cause for concern about drug-resistant strains of emerging and re-emerging diseases (e.g., HIV/AIDS, tuberculosis, hepatitis B, malaria, cholera, diptheria, and Ebola). Along with the transmission of microbes and viruses, the increase in international trade is fostering the distribution of products associated with major health risks, for example, alcohol and tobacco.
Major challenges related to advances in science and medical technologies include important ethical, legal, and social questions. Communication technology, for example, offers increased opportunity for dissemination of health information but also requires response to the misleading or incorrect information spread through the use of this same technology. Public health informatics (i.e., the systematic application of information and computer science and technology to public health practice, research, and learning [Yasnoff et al., 2000]) offers great potential for improving our public health surveillance capacity and response but is accompanied by concerns regarding confidentiality and security of the information systems. Genomics holds the promise of helping us understand the role that genetic factors play in morbidity and mortality in the United States. However, we will need to ensure that individuals with certain genetic traits and predispositions are not discriminated against in the workplace or in obtaining insurance. While scientific advances in the biomedical field have improved the health of the public, about half of all causes of mortality in
the United States are linked to social and behavioral factors and accidents (McGinnis and Foege, 1993). However, the vast majority of the nation’s health research resources have been directed toward biomedical research, with comparatively few resources devoted to supporting health research on social and behavioral determinants of health (IOM, 2000).
Major demographic transformations are taking place in the United States and around the world that also present public health with new challenges. The population is aging, and this aging is accompanied by an increase in multiple chronic diseases, geriatric conditions, and mental health conditions. We are faced with the challenge of better understanding how to prevent, delay, or mitigate the effects of these diseases, thereby increasing the chances for healthful, functional aging. The U.S. population is also increasing in racial and ethnic diversity. There are large racial and ethnic health disparities reflected in increased rates among minorities of such health problems as heart disease, cancer, accidents, diabetes, and HIV infections. Improving health outcomes for all populations in American society is a major challenge for public health in the 21st century.
THE FUTURE OF PUBLIC HEALTH EDUCATION
Public health professionals have a major role to play in addressing these complex health challenges, but to do so effectively they must have a framework for action and an understanding of the ways in which what they do affects the health of individuals and populations. Several models have been proposed for understanding the forces that impact on health, that is, the determinants of health (Lalonde, 1974; Evans and Stoddart, 1994; IOM, 1999; Kaplan et al., 2000). While each model differs, determinants include broad social, economic, cultural, health, and environmental conditions; living and working conditions; social, family, and community networks; individual behavior; individual traits such as age, sex, race, and biological factors, and the biology of disease. Kaplan and colleagues (2000), Grzywacz and Fuqua (2000), and others propose that the multiple determinants of health are related and linked in many ways. A model of health that emphasizes the linkages and relationships among multiple factors (or determinants) affecting health is an ecological model. An example of the ecological model can be found in Figure S-1. It is important to note that the committee is not recommending any single model, but rather emphasizing the concept that there are linkages and relationships among the multiple determinants of health.
The committee believes that public health professionals must understand this ecological model. They must look beyond the biological risk factors that affect health and seek to also understand the impact on health of environmental, social, and behavioral factors. They must be aware of how these multiple factors interact in order to evaluate the effectiveness
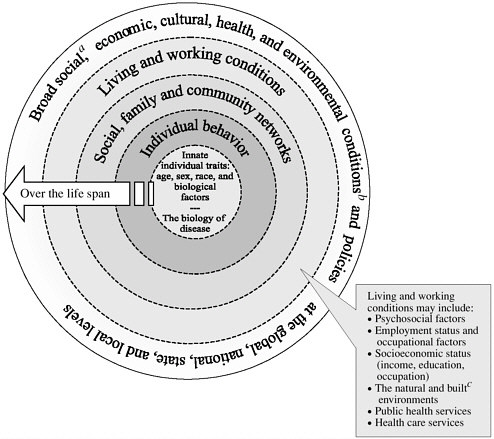
SOURCE: The Future of the Public's Health (IOM 2003).
NOTES: Adapted from Dahlgren and Whitehead, 1991. The dashed lines between levels of the model denote interaction effects between and among the various levels of health determinants (Worthman, 1999).
a Social conditions include, but are not limited to: economic inequality, urbanization, mobility, cultural values, attitudes and policies related to discrimination and intolerance on the basis of race, gender, and other differences.
b Other conditions at the national level might include major sociopolitical shifts, such as recession, war, and governmental collapse.
c The built environment includes transportation, water and sanitation, housing, and other dimensions of urban planning.
FIGURE S-1 A guide to thinking about the determinants of population health.
of their interventions. They must understand the theoretical underpinnings of the ecological model in order to develop research that further explicates the pathways and interrelationships of the multiple determinants of health. It is through this understanding that public health professionals will be able to more effectively address the challenges of the 21st
century, including globalization, scientific and medical technologies, and demographic transformations.
While an ecological model addresses the interactions and linkages among determinants of health, an ecological view of health is a perspective that involves knowledge of the ecological model of determinants of health and an attempt to understand a specific problem or situation in terms of that model. Further, an ecological approach to health is one in which multiple strategies are developed to impact determinants of health relevant to the desired health outcomes.
The committee acknowledges that the traditional core areas of epidemiology, biostatistics, environmental health, health services administration, and social and behavioral sciences remain important for public health professional education. However, the committee believes that the following eight content areas are now and will continue to be significant to public health and public health education in programs and schools of public health for some time to come: informatics, genomics, communication, cultural competence, community-based participatory research, global health, policy and law, and public health ethics. These areas are natural outgrowths of the traditional core public health sciences as they have evolved in response to ongoing social, economic, technological, and demographic changes. For example, community-based participatory research (CBPR) can be viewed as epidemiology enriched by contemporary social and behavioral science because it incorporates what we have learned about community processes and engagement, and the complex nature of interventions with epidemiology, in order to understand how the multiple determinants of health interact to influence health in a particular community.
Education in these eight areas is important to preparing high-quality, effective public health professionals. Understanding and being able to apply information and computer science technology to public health practice and learning (i.e., public health informatics) are necessary competencies for public health professionals in this information age in which we are vitally dependent upon data. Genomics is helping us understand the role of genetic factors in leading causes of morbidity in the Unites States, information that public health professionals must be familiar with to improve health.
Public health professionals must be proficient in communication to interact effectively with multiple audiences. They must also be able to understand and incorporate the needs and perspectives of culturally diverse communities in public health interventions and research, and to inform the development of policies, laws, and regulations. New approaches to research that involve practitioners, researchers, and the community in joint efforts to improve health are becoming necessary as we recognize the importance of multiple determinants of health, for ex-
ample, social relationships, living conditions, neighborhoods, and communities. Understanding global health issues is increasingly important as public health professionals are called upon to address problems that transcend national boundaries. Finally, public health professionals must be able to identify and address the numerous ethical issues that arise in public health practice and research.
Therefore, for each of these eight emerging content areas, the committee recommends that
-
competencies be identified;
-
each area be included in graduate level public health education;
-
continuing development and creation of new knowledge be pursued; and
-
opportunity for specialization be offered.
The committee believes that the progress made in understanding and incorporating these eight important areas into public health practice, education, and research will enable us, in the future, to identify other new and emerging areas that must be addressed. The committee also believes that it is important to enhance the development of the public health profession. While many of the things that need to be done to enhance the profession are beyond the scope of this study, certification is related to public health education. Within the various professions in the world of health and illness, specialty certification is common. Specialty certification attests to skills beyond the legal minimums that apply to a limited set of patients (e.g., pediatrics), conditions (e.g., infectious diseases), or interventions (e.g., anesthesia).
The range of individuals entering masters of public health (M.P.H.) programs, many with no previous health-specific education and with no access to any of the public health-related certifications currently in existence, makes M.P.H. students likely candidates for a certification program. Therefore, the committee recommends the development of a voluntary certification of competence in the ecological approach to public health as a mechanism for encouraging the development of new M.P.H. graduates.
SCHOOLS OF PUBLIC HEALTH
The basic public health degree is the master of public health (M.P.H.), while the doctor of public health (Dr.P.H.) is offered for advanced training in public health leadership. Schools of public health also offer a doctorate (Ph.D.) in various public health-related disciplines, as well as a range of masters’ degrees. Schools of public health produce the bulk of degree graduates. In 1998-1999, there were 5,568 graduates from the then 29 accredited schools of public health (ASPH, 2000). Davis and Dandoy
(2001) reported that the 45 accredited programs in Community Health/ Preventive Medicine (CHPM) and in Community Health Education (CHE) graduate an additional 700 to 800 master’s degree students each year. There are other programs in which students receive master’s-level training in public health including programs in public administration and affairs, health administration, and community health nursing, and M.P.H. programs in schools of medicine (in 1998, 36 of the 125 accredited U.S. medical schools offered a combined M.D./M.P.H. degree).
The history of education in schools of public health has been one of evolution and change in response to new knowledge, the needs of the times, funding sources, and opportunities for improvement. Schools again are faced with the need to evolve, in part because current problems demand new knowledge and approaches, and in part because of scientific advances and the increased understanding of the determinants of health, their linkages, and their interactions. The ecological model for public health provides a focus for the discussion of future directions in public health education.
The committee determined that schools of public health have six major responsibilities. These are to:
-
educate the educators, practitioners, and researchers as well as to prepare public health leaders and managers;
-
serve as a focal point for multi-school transdisciplinary research as well as traditional public health research to improve the health of the public;
-
contribute to policy that advances the health of the public;
-
work collaboratively with other professional schools to assure quality public health content in their programs;
-
assure access to life-long learning for the public health workforce; and
-
engage actively with various communities to improve the public’s health.
Education
Only a small portion of the total public health workforce receives any formal public health education, and those who do, do so primarily through certificate programs, short courses and continuing education programs, conferences, workshops, and institutes offered by a variety of institutions and organizations. While schools of public health may play crucial roles via curriculum setting, distance learning, cross-training, and continuing education for the larger public health workforce, the committee believes that the focus of education in schools of public health should be to educate masters and doctoral level students to fill many professional
positions within public health, and to educate those destined for positions of senior responsibility and leadership in public health practice, research, and teaching. Some, but not all, schools of public health will continue to directly educate the broader public health workforce. However, the committee recommends that schools embrace as a primary educational mission the preparation of individuals for positions of senior responsibility in public health practice, research, and teaching. The committee reaffirms the importance of the long recognized core areas of public health education (biostatistics, epidemiology, environmental health, health services administration, and social and behavioral sciences). Further, the committee endorses the idea that education should be competency based and supports educational programs built upon the competency domains identified by the Council on Linkages Between Academia and Public Health Practice. However, public health professionals in the 21st century also need to understand the ecological nature of the determinants of health, that is, their linkages and relationships. Therefore, schools of public health should emphasize the importance and centrality of the ecological approach. Further, schools have a primary role in influencing the incorporation of this ecological view of public health, as well as a population focus, into all health professional education and practice.
The present structure of education in schools of public health is heavily oriented towards teaching the basic public health sciences, augmented by specialization in one such area. Teaching is conducted primarily by faculty with backgrounds in one of the core public health sciences with minimal participation by those in senior practice positions or those with unique skills in areas such as communication, cultural competence, leadership development, or planning. Radical change is called for and, since the goal is to inculcate a broad ecologic perspective and the amount of content material is increasingly vast, integrative teaching techniques may prove more appropriate than traditional single discipline courses. Further, the practical intention of the education would suggest that classroom teaching be substituted to the extent feasible by hands-on “rotations” with agencies and organizations of the type in which trainees are being prepared to function.
The focus on preparing individuals for leadership roles and senior practice positions requires re-design of curricula and teaching approaches to incorporate:
-
enhanced participation in the educational process by those in senior practice positions or with comparable experiences, experts in medicine or its practice, or those with unique skills in areas such as communication, cultural competence, leadership development, policy, or planning;
-
reconsideration of M.P.H. admission requirements to ensure that selected candidates are adequately prepared for the expanded didactic and practical training envisioned;
-
vastly expanded practice rotations; and
-
enhanced education for competence in specific careers (e.g., biostatistician or health care administrator).
The committee recommends a significant expansion of supervised practice opportunities and sites (e.g., community-based public health programs, delivery systems, and health agencies). Such field work must be organized and supervised by faculty who have appropriate practical experience.
The range of future research in public health will also be radically different from what we see today. To a far greater degree, public health research will be transdisciplinary in nature, involving applications of basic biology and social sciences, and direct participation of the community. In the current paradigm, so-called multi-disciplinary research is the predominant research mode. Transdisciplinary research involves broadly constituted teams of researchers that work across disciplines in the development of the research questions to be addressed. Research methodology typically reflects the repertoire of the principal investigator’s discipline, complemented by consultant co-investigators with additional skills. For example, at present a chronic disease epidemiologist might study the effect of an ambient air pollutant on mortality, obtaining input from an environmental chemist to help measure the independent variable (air pollutants) and a biostatistician to help explore advanced causal models.
In the future, study of the health impact of air pollutants will likely involve more broadly constituted “teams” comprised of social scientists (to measure covariation in health status caused by social factors which in the present paradigm would be viewed as “confounders”), experts in lung and cardiovascular biology (to evaluate early markers of health effect because mortality, while easily measured, is too crude an end-point given the broad and diverse population at risk), and, most novely, industrial engineers and economists to evaluate in the research context the feasibility and costs associated with alternative strategies for modifying air quality. Moreover, a far larger portion of the research portfolio is likely to be evaluative and/or intervention-focused, with interventions at the individual, community organizational, and even societal levels.
Educating individuals to conduct this research will require new approaches to the current strategy of advanced degree education at the doctorate level. The breadth of the envisioned future enterprise, and its many intersections with other scientific, biomedical and social scientific fields, suggests that an important component of science training will be
directed at those who enter public health with an advanced degree in another discipline, typically an M.D. or Ph.D. Others may choose to obtain their primary doctoral-level education at a school of public health. Doctoral research candidates should have exposure to core public health disciplines as well as the eight content areas identified earlier and researchers must be trained to understand communities and to engage in transdisciplinary research. The committee recommends that doctoral research training in public health should include an understanding of the multiple determinants of health within the ecological model.
Research
Public health research differs from biomedical research in that its focus is on the health of groups, communities, and populations. The most striking change in public health research in the coming decades is the transition from research dominated by single disciplines or a small number to transdisciplinary research. Closely related to the move toward more transdisciplinary approaches to complex health issues will be the move toward more intervention-oriented research. The study of interventions will, in turn, dictate the third sea-change in public health research: community participation. Whereas the study of clinical interventions can most usually be achieved by recruitment of consenting patients or subjects, interventions at the community level require an altogether different paradigm, in which investigators and the community or population to be studied are partners. Models for such research already exist, for example the ten-year community trials funded by the National Heart, Lung and Blood Institute (Farquhar et al., 1985; Elder et al., 1986; Jacobs et al., 1986; Mittelmark et al., 1993). However, the preeminence of such research in schools of public health in the coming decades will mandate new expertise in these research modalities. In addition, such research will fundamentally alter relationships among schools of public health, the communities in which they are embedded, and the public and private agencies with responsibility for the health of these communities or populations.
The committee recommends that schools of public health reevaluate their research portfolios as plans are developed for curricular and faculty reform. To foster the envisioned transdisciplinary research, schools of public health may need to establish new relationships with other health science schools, community organizations, health agencies, and groups within their region.
Policy
Public health professionals across the disciplines of public health cannot be fully effective without an understanding of how policies are made
and put into practice (Burris, 1997; Gostin et al., 1999; Gebbie and Hwang, 2000; Reutter and Williamson, 2000; Weed and Mink, 2002). An ecological understanding of public health only makes this skill set more salient; identifying social determinants of health means challenging settled practices, institutional arrangements, and beliefs that are or are not perceived to be beneficial to at least some members of the community.
Although the importance of policy in public health has long been recognized (IOM, 1998), education in policy at many schools of public health is currently minimal. Education in policy analysis, policy development, and the application of policy, must be addressed. Should schools wish to be significant players in the future of public health and health care, dwelling on the science of public health without paying appropriate attention to both politics and policy will not be enough.
Law is another essential component of education in policy. Most public health policies are embodied in or effectuated through law, and law provides the institutional framework and procedures through which policies are debated, codified, implemented, and interpreted (Burris, 1994; Gostin, 2000). From an ecological view, laws and legal practices may be important constituents of the “fundamental social causes of disease” that broadly determine population vulnerability to and immunity from illness (Link and Phelan, 1995; Sweat, 1995; Sumartojo, 2000; Burris et al., 2002); therefore a critical area in public health policy research is engagement with law.
Engagement in policy also requires a set of practical political skills, for example understanding the dynamics of community politics, identifying and working with stakeholders, identifying legal and policy structures currently influencing community health, and motivating and educating stakeholders and officials. Finally, ethics and consideration of the relationship of human rights to health play important roles in politics and policy development. They are tools through which public health professionals can interrogate their own values, formulate policy goals, and articulate a rationale for change in policy.
The committee believes that it is the responsibility of schools of public health to better prepare their graduates to understand, study, and participate in policy related activities. Therefore, the committee recommends that schools of public health:
-
enhance faculty involvement in policy development and implementation for relevant issues;
-
provide increased academic recognition and reward for policy-related activities;
-
play a leadership role in public policy discussions about the future of the U.S. health care system, including its relation to population health;
-
enhance dissemination of scientific findings and knowledge to broad audiences, including encouraging the translation of these findings into policy recommendations and implementation; and
-
actively engage with other parts of the academic enterprise that participate in policy activities.
Academic Collaboration
Many senior positions in public health will continue to demand or attract physicians, nurses, trained managers, lawyers, and others (e.g., some states require that the executive of the department of health be a physician). Streamlined variations of the new practice curriculum that are oriented toward these individuals will need to be developed to inculcate the core public health competencies. Ideally, such training might be incorporated into the initial professional training experience, particularly into the curricula of medical schools and schools of nursing. The committee believes that schools of public health should embrace the large number of programs in public-health-related fields that have developed within medical schools and schools of nursing and initiate and foster scientific and educational collaborations.
Further, the committee recommends that schools of public health actively seek opportunities for collaboration in education, research, and faculty development with other academic schools and departments, to increase the number of graduates in health and related disciplines who have had an introduction to public health content and interdisciplinary practice, and to foster research across disciplines.
Access to Life-long Learning
In addition to preparing new graduates in public health, there is an existing public health workforce that requires education and training, either of workers who have no previous training in the public health aspects of their positions or of those who need to update existing skills because of evolutions in the field. While it is unclear exactly how many public health workers there are in the United States today, it is estimated that about 450,000 people are employed in salaried positions in public health, and an additional 2,850,000 volunteer their services (Center for Health Policy, 2000). Schools of public health are not necessarily primary direct providers of such training, but they do have a responsibility to assure that appropriate, quality education and training are available to the current and future public health workforce. The assurance role is analogous to that of the public health system, which does not always provide the necessary health services to individuals or communities but assures that their health care needs are met.
Schools can help other institutions and organizations develop training materials, and they can provide expertise in the delivery, presentation, and evaluation of materials and in the assessment of student learning. Schools are also in a good position to coordinate the sharing of “best practices” and to provide individualized education on specialized topics. Schools’ broad knowledge and expertise in the public health disciplines and educational methodology positions them to assure that comprehensive, quality public health workforce education and training is available in the region served by each school. Therefore, the committee recommends that schools of public health fulfill their responsibility for assuring access to life long learning opportunities for several disparate groups including:
-
public health professionals;
-
other members of the public health workforce; and
-
other health professionals who participate in public health activities.
Community Collaboration
Implementing effective interventions to improve the health of communities will increasingly require community understanding, involvement, and collaboration. Schools of public health have a responsibility to work with communities to educate them about what it takes to be healthy and to learn from them how to improve public health interventions. Through research and service, schools of public health have the opportunity to engage communities in the task of improving the health of the public. Community organizations and leaders have the opportunity to contribute to and influence research that has the potential to address local needs; the school can direct its expertise toward generating and analyzing appropriate local-level data and targeting significant problems. By working with the community, students in schools of public health will be exposed to far more coherent and visible community-based learning experiences.
Schools of public health will be most effective in engaging in new relationships with their communities if they take a leadership role in collaborating with other important academic units, for example, medicine, nursing, education, urban planning, and public policy. Given the premise of a future in which the boundaries of medicine and public health continue to blur, not to mention the recognition that protecting and promoting population health requires consideration of a broad array of non-biological factors, schools of public health would be well served to not go down this path alone. Therefore, the committee recommends that schools of public health should
-
position themselves as active participants in community-based research, learning, and service;
-
collaborate with other academic units (e.g., medicine, nursing, education, and urban planning) to provide transdisciplinary approaches to active community involvement to improve population health; and
-
provide students with didactic and practical training in community-based public health activities, including policy development and implementation.
Further, community-based organizations should have enhanced presence in schools’ advisory, planning, and teaching activities.
Faculties for Schools of Public Health
The curricular changes envisioned by the previous discussion will likely require substantial changes in the composition and backgrounds of future faculties of schools of public health, requiring both research-oriented and practice-focused components. A major barrier to increasing the emphasis on practice and service relates to faculty rewards, promotion and tenure because, within academic institutions, public health practice is not valued as highly as research activity nor is it rewarded by most academic institutions.
So that faculties with the appropriate mix of backgrounds and skills can be recruited and sustained, the committee recommends major changes in the criteria used to hire and promote school of public health faculty. Criteria should reward experiential excellence in the classroom and the practical training of practitioners. Unfortunately, the historical funding stream for schools of public health has fostered an emphasis on the research function. Such an imbalance has impeded maximizing the contributions of schools in practice and education. Currently, funding for schools of public health is problematic, making it difficult for schools, as well as other programs of public health education, to institute the necessary changes recommended by this report.
The committee acknowledges the major contributions of philanthropic foundations to the development of public health education in the United States and emphasizes the renewed importance of foundation support to fund new initiatives and experiments in public health education. However, greater support for public health education is needed from state and federal governments to ensure that a competent, well-educated public health workforce is available. Public health professionals, knowledgeable about the ecological approach to health and educated in a transdisciplinary fashion, are essential to preserving and improving the health of the public. Schools of public health are positioned to
educate these professionals but can only do so if sufficient funding is available to develop the programs and approaches necessary to prepare future public health professionals for the challenges and opportunities of the 21st century.
OTHER PROGRAMS AND SCHOOLS
Although the primary focus of this committee’s work is on schools of public health, other programs, schools, and institutions play major roles in educating public health professionals. The committee believes that to provide a coherent approach to educating public health professionals for the 21st century, it is important to examine and understand the potential contributions these other institutions and programs can make.
Graduate Programs in Public Health
A 1999 survey conducted by the Association of Teachers of Preventive Medicine (ATPM) in collaboration with the Council on Education for Public Health (CEPH) found that there were 75 M.P.H. programs in public health in the United States (Davis and Dandoy, 2001). These programs are practice oriented and are generating about one in every eight M.P.H. degrees, thereby contributing significantly to the formal educational process of public health professionals. The committee recommends that these graduate M.P.H. programs in public health institute curricular changes that
-
emphasize the importance and centrality of the ecological model; and
-
address the eight critical areas of informatics, genomics, communication, cultural competence, community-based participatory research, global health, policy and law, and public health ethics.
Medical Schools
Physicians have historically played a central, though not exclusive, role in insuring the health of the public. Beginning in the 20th century, however, the association between public health and mainstream medicine declined (although many physicians continue to lead or participate in local, state, and national public health efforts). In fact, increasing tensions resulted in a schism between medicine and public health. However, meeting the public health challenges of the 21st century will require that medical, scientific, and public health communities work together.
The committee’s goal in developing recommendations for programs and approaches for public health education in medical schools is to foster
improved public health training for all medical students. While such education presents challenges, there are existing examples (e.g., the programs at Duke University, the University of California at San Francisco, and the University of Southern California) that, with some modification, could produce professionals with M.D., M.P.H., and Ph.D. degrees in public health. Graduates of these programs would have the requisite training to become leaders and bridge the chasm between the two disciplines.
An ecological understanding of health and a transdisciplinary approach require physicians who are fully prepared to work with others to improve health. Therefore, the committee strongly recommends that
-
all medical students receive basic public health training in the population-based prevention approaches to health;
-
serious efforts be undertaken by academic health centers to provide joint classes and clinical training in public health and medicine; and
-
a significant proportion of medical school graduates should be fully trained in the ecological approach to public health at the M.P.H. level.
Further, when a school of public health is not available to collaborate in teaching the ecological approach to medical students, the committee recommends that medical schools should partner with accredited programs in public health to provide for public health education.
Medical schools and schools of public health should collaborate on educational and scientific programs that address some of our most prevalent and troublesome chronic diseases, such as Alzheimer’s disease, obesity, and severe/unremitting psychiatric disorders. Ongoing collaborations between schools of medicine and public health could, for example, focus on understanding how recent advances in genomics and biomedicine, in general, will have an impact on the public’s health over time. Students should be exposed to dialogues between leaders in medicine and leaders in public health on central topics related to the public’s health (for example, regarding the impact upon and cost to society of new-generation, subject-specific pharmaceutical products).
Therefore, schools of medicine and schools of public health should develop an infrastructure to support research collaborations linking public health and medicine in the prevention and care of chronic diseases.
Schools of Nursing
Nurses constitute the single largest group of professionals practicing public health. The estimated numbers available are somewhat inconsis-
tent, given various data sources and definitions. In the 2000 estimated enumeration of the public health workforce, nearly 11 percent of the professionals identified were nurses, and there are probably a good many more practicing under more general job titles (Center for Health Policy, 2000). As is also true for physicians, all nurses at some level are a part of the public health system, given their potential contributions to the control of nosocomial infections, the identification of conditions of public health importance, and the education of patients and families about disease prevention and health promotion. Because of their important contributions, it is critical that all nurses have at least an introductory grasp of the role of public health in the community and of the principles of health promotion and disease prevention.
The roles for nurses in public health practice in public health agencies, community-based practices, and elsewhere is such that the long-standing identification of the baccalaureate degree as the entry to public health practice is likely to remain the standard, even though it is often honored in the breach. Undergraduate schools of nursing will continue to be a major source of entry-level public health workers. The committee recommends that these undergraduate schools be encouraged to assure that curricula are designed to develop an understanding of the ecological model of health and core competencies in population-focused practice. Because of the ongoing debate about preparation of the associate degree graduates in community skills, the public health community should offer assistance in identifying the appropriate level and type of position for these graduates as well. In support of sound baccalaureate-level preparation in public health nursing, the public health community should be attentive to the need for student clinical experience, should collaborate in making appropriate sites available, and should consider ways to assure that nursing education does not occur in a vacuum apart from the full range of professionals practicing in public health.
The graduate-level role for schools of nursing is not so clear. The inclusion of public health perspectives and skills in clinical programs in a range of specialties, as advocated by the National Organization of Nurse Practitioner Faculty (NONPF), continues the appropriate orientation of clinicians to their roles in collaboration with public health. With the exception of employment as clinicians in specific program areas, however, these are not the nurses to which public health will be looking for leadership. Schools of nursing that offer master’s degree programs in public health nursing should be encouraged to partner with schools of public health to assure that current thinking about public health is integrated into the nursing curricula content, and to facilitate development of interdisciplinary skills and capacities.
Programs offering joint degrees in nursing and public health that
bring the two schools together formally can offer a viable and effective option for advancing public health nursing practice.
Other Schools
Given the centrality of health in all our lives and the complexity of organizing collectively in a democracy to achieve it, there is a strong case to be made that curricula at all levels should include more training on health and human ecology. “Health literacy” can and should be a goal of our educational system as a whole (St. Leger, 2001). More specifically, the committee believes that the diffusion of health issues and responsibilities in society creates a need for health training in a range of jobs without health in the title. The enterprise of public health cannot succeed as a niche specialty. Creating the conditions in which Americans can be healthy requires the informed collaboration of planners, executives, and lawyers, to name just a few. There are many professions whose practitioners play an important role in health, and whose trainees are appropriate candidates for public health training.
The committee believes that public health is an essential part of training citizens, and that it is immediately pertinent to a number of professions. Specialized interdisciplinary training programs, such as the J.D./ M.P.H. or M.P.H./M.U.P. (master of urban planning) can create specialists and are important. Our view, however, is that more is needed: public health literacy, entailing a recognition and basic understanding of how health is shaped by the social and physical environment, is an appropriate and worthy social goal. Further, education directed at improving health literacy at the undergraduate level could also serve to introduce persons to possible careers in public health and, in so doing, increase the cultural diversity of the future public health professional workforce. The committee recommends that all undergraduates should have access to education in public health.
It is beyond both our charge and our capacity to make specific recommendations about how to incorporate health into diverse curricula. Doubtless the usual challenges to curricular change will arise—faculty flexibility, scarce resources of time, and student interest. The committee does, however, stress the importance and recommend the integration of a more accurate and ecologically oriented view of health into primary, secondary, and post-secondary education in the United States.
PUBLIC HEALTH AGENCIES
While the committee is aware that public health professionals work in a variety of settings, there is a special relationship with the governmental public health agencies at the local, state, and federal level. These agencies
have a major interest in educating and training the current public health workforce and future public health workers.
The nearly 3,000 local health departments (LHDs) in the United States vary tremendously in many ways, including size, nature of population served, economic circumstances, and governing structure. The majority of LHDs provide a wide variety of services to diverse communities with limited resources. Even with this considerable variation, more than two-thirds of local health departments provide the following core services: adult and childhood immunizations, communicable disease control, community outreach and education, epidemiology and surveillance, food safety services, restaurant inspections, and tuberculosis testing (NACCHO, 2001).
Local health departments have urgent and serious needs for upgrading the skills of those currently employed and for educating new professionals (NACCHO, 2001). Much of the training for local public health staff is obtained through the initiative of individual employees, seeking continuing education in areas of special interest or to maintain their professional credentials.
LHDs themselves provide a significant amount of direct training, primarily for narrow technical skills specific to their programs. However, LHDs can play a broader role in training and education by assessing the skills and training needs of the workforce; a role proposed in the National Public Health Performance Standards (NPHPS) (CDC, 1998), Essential Service 8 (Public Health Functions Steering Committee, 1994). Further, increased linkages between schools and programs of public health and LHDs offer many potential benefits. For example, local health department staff could serve as adjunct faculty in schools and programs of public health, thereby enhancing practical education for students. LHDs are also an important partner in community-based research because of their direct linkages to communities and awareness of local public health issues.
State public health departments are also important to the education of the public health workforce. All states, territories, and the District of Columbia have a designated entity known formally as the state public health department. The mission, authority, governance, and accountability of these public health departments vary according to the state statutes that establish them. The state health department’s role in any given state is to facilitate the implementation of the Essential Public Health Services, either by carrying them out directly or indirectly through support of local public health agency efforts, and by articulating the needs of the global public health workforce to federal partners.
The responsibilities of state health departments in assuring a competent public and personal health care workforce are described in the NPHPS and include regulation, education, training, development, and
assessment of health professionals to meet statewide needs for public and personal health services. States, working in partnership with the federal government are engaged in developing multiple strategies to strengthen the public health infrastructure, including the developmental and educational needs of the public health workforce.
Federal agencies’ roles in public health education and research are multiple and varied including contributing to the research base that forms the content of education, testing educational approaches, helping schools develop infrastructure, supporting faculty development, and providing funding for students. Agencies involved include predecessors and current iterations of the National Institutes of Health (NIH), the Health Resources and Services Administration (HRSA), the Centers for Disease Control and Prevention (CDC), the Substance Abuse and Mental Health Services Administration (SAMHSA), and the Agency for Healthcare Research and Quality (AHRQ), all of which are branches of the Department of Health and Human Services. From the general perspective of public health education, HRSA and CDC have played the major roles.
HRSA includes the Bureau of Health Professions (BHPr), which has the stated mission to help assure access to quality health care professionals in all geographic areas and to all segments of society. BHPr puts new research findings into practice, encourages health professionals to serve individuals and communities where the need is greatest, and promotes cultural and ethnic diversity within the health professions workforce.
The programs of CDC have supported technical training for public health laboratory staff, and for program staff in tuberculosis control, sexually transmitted disease control, HIV/AIDS prevention, school health, and, more recently, in chronic disease prevention and injury prevention. The Public Health Practice Program Office (PHPPO) has provided a home base for the multi-organization Public Health Workforce Collaborative, a partnership with HRSA that involves nearly every identifiable organization representing some segment of public health workforce development. An Office of Workforce Planning and Policy was created as the organizational locus for external workforce development activities.
The potential roles for federal agencies in developing the public health workforce for the 21st century could take several forms and fall into the categories of research, development of academic programs, development of faculty, support for students, continuing education, technology development, and modeling.
Local state and federal health agencies all play critical roles in educating public health professionals for the 21st century. Local health departments are the backbone of service in public health, meeting a broad range of public health needs of the diverse communities within their areas. State health departments facilitate the implementation of the Essential Public
Health Services either by carrying out these services directly or by supporting the efforts of the local public health agencies. The importance of leadership and action at the federal level is crucial to success in educating public health professionals and the public workforce.
Therefore, the committee recommends that local, state, and federal health agencies
-
actively assess the public health workforce development needs in their own state or region, including the needs of both those who work in official public health agencies and those who engage in public health activities in other organizations;
-
develop plans, in partnership with schools of public health and accredited public health programs in their region, for assuring that public health education and training needs are addressed;
-
develop incentives to encourage continuing education and degree program learning;
-
engage in faculty and staff exchanges and collaborations with schools of public health and accredited public health education programs; and
-
assure that those in public health leadership and management positions within federal, state, and local public health agencies are public health professionals with M.P.H. level education or experience in the ecological approach to public health.
While assessment of workforce education and training needs, and development and implementation of programs to meet those needs are major roles for local, state, and federal agencies, it is also important that the leaders of these agencies be fully knowledgeable and educated in public health. CDC and other public health agencies and organizations, including NACCHO, the Association of State and Territorial Health Officers (ASTHO), ASPH, and American Public Health Association (APHA), are examining the feasibility of creating a credentialing system for public health workers based on competencies linked to the Essential Public Health Services framework.
While local, state, and federal agencies all play a role in developing a competent workforce, there is a role that is primarily the responsibility of the federal agencies, that is, providing funding support for efforts throughout the system. Public health teaching, research, and infrastructure support was well funded during the 1960s and 1970s. Major decreases in funding occurred in the 1980s, and those decreased levels remained fairly constant through the 1990s. During that time, tuition and other costs continued to increase, resulting in a reduction in the amount of public health professional education actually provided.
The committee has carefully considered the rationale and feasibility
of implementing recommendations to significantly enhance federal funding for both public health education and leadership development and for public health research overall, including research on population health, public health systems, and public health policy. Investment in public health education is inadequate. Federal support for non-physician graduate public health training is minimal, and funding for residencies in preventive medicine is only about $1 million (Glass, 2000).
Therefore, the committee recommends that federal agencies provide increased funding to
-
develop competencies and curriculum in emerging areas of practice;
-
fund degree-oriented public health fellowship programs;
-
provide incentives for developing academic/practice partnerships;
-
support increased participation of public health professionals in the education and training activities of schools and programs of public health; especially, but not solely, practitioners from local and state public health agencies; and
-
improve practice experiences for public health students through support for increased numbers and types of agencies and organizations that would serve as sites for practice rotations.*
In terms of research funding, comparatively few resources have been devoted to supporting prevention research, community-based research, transdisciplinary research, or the translation of research findings into practice. Current funding for research is focused almost entirely on two components of the ecological model of health—biologic determinants and medical cures. According to Scrimshaw and colleagues (2001), only 1 to 2 percent of the U.S. health care budget is spent on prevention and a like imbalance exists between funding for basic biomedical research and population-based prevention research. Analysis shows that at least 50 percent of mortality is due to factors other than biology or medical care (McGinnis and Foege, 1993).
Although it is not realistic at this time to propose a shift in funding for public health research to levels commensurate with the burden of need, the committee believes that significant steps in this direction are now amply justified and warranted. Accordingly, the committee recommends that
-
there be a significant increase in public health research support
-
(i.e., population health, primary prevention, community-based, and public health systems research), with emphasis on transdisciplinary efforts;
-
the Agency for Healthcare Research and Quality spearhead a new effort in public health systems research;
-
NIH launch a new series of faculty development awards (“K” awards) for population health and related areas; and
-
there be a redirection of current CDC extramural research to increase peer reviewed investigator-initiated awards in population health, prevention, community-based, and public health policy research, reallocating a significant portion of current categorical public health research funding to competitive extramural grants in these areas.*
Educating public health professionals to effectively respond to the new and emerging challenges requires funding support. Public health professionals can most effectively continue to contribute to improving the public’s health through practice, teaching, and research if we are willing to provide quality support to the education of those professionals.
CONCLUSION
At no time in the history of this nation has the public health mission of promoting the public’s health and safety resonated more clearly with the public and the government than now. The events of September 11, 2001, brought public health glaringly into the limelight. All citizens now have reason to understand what public health is and how the public health system interacts and shares responsibility for managing public health risks with national, regional, and local levels of government and with the health care system.
Addressing public health challenges requires an ecological approach, and the committee has developed recommendations for a framework for education, training, research, and practice based on the ecological model. The ecological model recognizes that the health of individuals and the community is determined by multiple factors and by their interactions, including biology, the social and physical environment, education, employment, and behavior (e.g., healthy ones such as exercise and unhealthy ones such as overeating).
We need high quality public health professionals contributing through practice, teaching, and research to improved health in our communities.
This report provides a framework and recommendations for strengthening public health education, research, and practice that can be used by the institutions and organizations responsible for educating public health professionals and supporting public health education. Public health professionals’ education and preparedness should be of concern to everyone, for it is well-educated public health professionals who will be able to effectively shape the programs and policies needed to improve population health during the coming century. If we want high quality public health professionals, then we must be willing to provide the support necessary to educate those professionals.
























