The Impact of Uninsured Populations on the Availability of Hospital Services and Financial Status of Hospitals in Urban Areas
Darrell J. Gaskin and Jack Needleman
ABSTRACT
Objective: To identify the effects of the percentage of uninsured persons in a community on the availability of hospital services for the entire community.
Data and Study Design: Our analysis focuses on the 85 largest metropolitan statistical areas (MSAs) during the 1990s and relies on data from the March Current Population Survey, the American Hospital Association’s (AHA) Survey of Hospitals and Medicare Cost Reports. We estimate the impact of the uninsured rate on hospital margins and four measures of hospital service availability, i.e., capacity, services to vulnerable populations, community services, and high-tech services. We estimate two sets of regression models, MSA-level and hospital-level models.
Findings: We find that as the uninsured rate increased the availability of some hospital services declined. The results of the MSA and hospital level analyses aare consistent for the measures of capacity, services to vulnerable populations and community services. The uninsured rate was negatively related to beds per capita in the MSA and the average hospital size. The availability of services for vulnerable populations and community services and the propensity for hospitals to offer these services is negatively associated with the percentage of uninsured residents. The results for hi-tech services for the MSA- and hospital-level analyses are not congruent. The results from the MSA-level analysis suggest that the uninsured rate is negatively
associated with the availability of some high-tech services. However, the results of the hospital-level analysis suggest that as the uninsured rate increases, hospitals are more likely to offer some high-tech services, specifically extracorporeal shock-wave lithotripsy (ESWL), angioplasty, and magnetic resonance imaging (MRI). The results of the MSA- and hospital-level analyses also differ for hospitals’ financial health. The MSA level results suggest that hospitals are negatively impacted by the rate of uninsurance. The hospital-level results suggest that there is no association.
Conclusion: Our findings suggest that the lack of health insurance not only creates an access to care problem for uninsured individuals but also reduces the availability of hospital services to the entire community.
INTRODUCTION
An estimated 41 million Americans or 16.5 percent of the population under age 65 lacked health insurance in 2001 (Mills, 2002). The lack of health insurance has a significant impact on the health and well-being of uninsured persons. A number of studies have shown that uninsured persons have less access to health care services and as a result have worse health outcomes and lower overall health status (IOM, 2002a; 2002b). The uninsured are less likely to receive preventive and screening services compared to persons with health insurance. Uninsured persons with chronic conditions are less likely to receive appropriate care to manage their health conditions (Mandelblatt et al., 1999; Powell-Griner et al., 1999; Zambrana et al, 1999; Ayanian et al., 2000; Cummings et al., 2000; Breen et al., 2001). Compared to insured persons, uninsured persons are less likely to have a usual source of care and less likely to seek care when they felt they needed it (IOM, 2001a). When hospitalized, the uninsured receive fewer services, are more likely to receive substandard care than insured patients, and are at greater risk of dying during the hospital stay or soon after discharge (Hadley et al., 1991; Burstin et al., 1992; Haas and Goldman, 1994; Blustein et al., 1995). Persons without health insurance have poorer heath outcomes for an episode of illness and higher overall mortality rates (Ayanian et al., 1993; Blustein et al., 1995; Canto et al., 2000; Roetzheim et al., 2000).
While research has shown the persons who are uninsured face significant barriers to health care, little is known about how the overall percentage of those without health insurance, i.e., the uninsured rate, affects access to care for their community. Theoretically, the size and scope of the health care delivery system in a community is determined by the intersection of the demand for health care in a community with health care providers’ ability and willingness to offer services. Because insurance pays for a large proportion of health care services, the distribution of community residents by source of payment will partially determine their demand for health care services. In particular, health insurance coverage does tend
to increase individuals’ demand for health care services. Uninsured persons use fewer health care services than do similar insured persons. Also, hospitals, physicians and other health care providers receive substantially less reimbursement for the care provided to uninsured patients compared to similar insured patients. Consequently, a high uninsured rate should reduce overall demand for health services in a community.
We are concerned particularly about the impact of uninsurance on the availability of hospital services. Several studies have shown that market forces that have depressed demand for hospital services have had an impact on the size of the hospital delivery system. For example, Medicare’s transition from a cost-based reimbursement system to prospective payment and its subsequent reduction in growth of hospital payment rates resulted in lower hospital utilization, a reduction in the intensity of hospital services, and encouraged a reduction in hospital size (Coulam and Gaumer, 1991; Hodgkin and McGuire, 1994). The introduction of managed care also reduced demand for hospital services. Several studies have demonstrated that increased HMO penetration is associated with reduction in hospital utilization, hospital beds, slower hospital cost inflation, and slower revenue growth (Miller and Luft, 1994; Chernew, 1995; Robinson, 1996; Gaskin and Hadley, 1997). Dranove and colleagues (1986) have modeled the impact of managed care penetration on hospitals, and they conclude that downward pressure on hospital prices would result in a reduction in hospital capacity. Given these major changes in the nature of demand for hospital services, hospital behavior in less concentrated markets has transformed from non-price competition to price competition. Prior to the implementation of Medicare prospective payment and the growth of managed care, the empirical evidence indicated that hospitals in less concentrated markets competed on the basis of technology, amenities, and services, e.g., Luft’s so called “medical arms race” (Robinson and Luft, 1985; Luft et al., 1986; Noether, 1988; Frech, 1996). However, studies based on data from the late 1980s and early 1990s present strong evidence of price competition in hospital markets (Robinson and Luft, 1988; Zwanziger and Melnick, 1988; Melnick et al., 1992; Keeler et al., 1999). Hospitals in less concentrated areas charged significantly lower prices compared with those in more concentrated areas.
We postulate that similar to other market forces that reduce the demand for hospital services, high uninsured rates will be associated with reduction in hospital capacity. This potentially can have a negative spillover effect on insured patients. For example, if a hospital is unable to maintain its trauma center because of a high uninsured rate, an ambulance may have to carry insured patients further to obtain trauma care. In this study we attempt to identify the effects of the percentage of uninsured persons in a community on the availability of hospital services for the entire community. In particular, we address the following questions: (1) Are hospitals smaller in communities with high uninsured rates? (2) Are hospitals less likely to offer particular types of services in communities with uninsured rates? (3) Does the availability of hospital services for the entire community decline as the
percentage of uninsured persons on a community increases? (4) Does uninsurance negatively affect the financial status of hospitals?
CONCEPTUAL FRAMEWORK
As stated above, we hypothesize that the uninsured rate is negatively related to the demand for hospital services. Specifically, as the uninsured rate increases, the overall demand for hospital services by insured patients decreases while the overall demand for hospital services by uninsured patients (i.e., charity or discount care) increases. Uninsured patients, however, tend to use less hospital care than do insured patients for similar health care needs because of their limited financial resources. As a result, an increase in the uninsured rate should lower and flatten the demand for hospital services in a geographic market. For simplification, assume that hospitals serve two types of patients: insured and uninsured. Payment rates for treating insured patients are typically greater than average costs. Reimbursements for treating uninsured patients are typically less than average cost. Assume hospitals have a cost structure that exhibits increasing or constant returns to scale, that is, total cost increases with the volume of services at an increasing rate. Empirically, hospitals exhibit scale economies up to a moderate size, 150 to 250 beds (Folland et al., 2001). Beyond this size the evidence is mixed regarding whether hospitals experience constant or decreasing returns to scale. Assume that the typical urban hospital operates at volume levels where marginal cost equals average cost. Hospitals use their marginal cost to determine their supply of hospital services. They equate marginal costs with either marginal revenues or average revenues depending upon their market structure (Tirole, 1998). Hospitals that are monopolies or part of oligopolies will set marginal costs equal to marginal revenues. Hospitals that are in monopolistic competitive markets will set their marginal costs equal to average revenues (Chamberlin, 1962).
For simplification, suppose that the distribution of each hospital’s patients by source of payment is equal to the distribution of persons in the market by insurance status. In such a market, as the uninsured rate increases, the percentage of uninsured patients treated by each hospital increases and therefore their average and marginal revenues decline. Consequently, each hospital will reduce its supply of services. Obviously, this is a simplification that does not reflect most hospital markets because hospitals differ with respect to serving the uninsured in their geographic markets. However, the general notion that an increase in the uninsured rate places downward pressure on the supply of hospital services is correct.
Now relax the assumption that hospitals care for uninsured patients proportionally to their presence in the market area. Suppose in some markets there are safety-net hospitals that provide a disproportionate share of the care to the uninsured while other hospitals provide less than a proportionate share of uninsured patients. In such a market, an increase in the uninsured rate would have a larger effect on safety-net hospitals than on other hospitals. However, if as the uninsured rate increases, non-safety-net hospitals in the community become proportionately
more involved in the care for the uninsured, then these hospitals will be more affected by the change in demand.
Another assumption implicit in our model is that uninsured and insured patients use hospitals for the same mix of services. However, suppose there is a set of hospital services that the uninsured are more likely to use than insured patients. For these services, hospitals’ profits will tend to be lower than profits associated with other hospital services because of their payer mix. Therefore, we expect that hospitals will cut back on services that the uninsured are more likely to use as the uninsured rate increases.
The discussion above assumed that each hospital bases its decisions on its own revenue and cost structure. The framework can also be extended to consider strategic interactions among hospitals in multi-hospital markets. Hospitals facing demand for services from uninsured or nonpaying patients for specific services may prefer to shift these patients to other hospitals. Where this cannot be accomplished directly, an option is to not provide the service or restrict the size of the service by reducing beds available for the service. This will shift uninsured patients to other hospitals but can also increase the travel time and inconvenience for insured patients to obtain the service. In markets where care for the uninsured is concentrated in a few safety net hospitals, this effect may be small. In markets where care for the uninsured is more widely shared or where there are fewer hospitals, these strategic interactions may reduce the availability of services beyond the level needed to adjust for the lower demand from the uninsured.
DATA
This study relies primarily on three databases:
-
The March Current Population Survey (CPS)
-
the AHA Annual Survey of Hospitals and
-
the Medicare Cost Reports
We used data from the March CPS from 1990 to 2000 to calculate the percentage of uninsured residents in the 85 largest MSAs. See the addendum for the list of MSAs. We focus on the 85 largest MSAs because they had large enough subsamples in the CPS data to yield reliable estimates of the uninsured rate. The size of the subsamples range from 143 to 6,148 with a mean of 900, standard deviation of 145, and a median of 623. To improve the accuracy of our estimates, we calculated the percentage of uninsured persons in an MSA by combining data for 3 years, i.e., the current year and the years before and after. The analysis focuses on the years 1991, 1994, 1996, and 1999. In addition, we calculated the percentage of the MSA’s population covered by Medicare and Medicaid using the CPS data.
To measure the availability of hospital services, we used data from the AHA Survey of Hospitals for the years 1991, 1994, 1996, and 1999. In particular, we
used four measures of hospital service availability: hospital capacity, services to vulnerable populations, high tech services, and community services. To measure capacity we used the number of hospital beds, medical/surgical beds, psychiatric beds, intensive care unit (ICU) beds, and beds devoted to patients diagnosed with alcoholism, drug abuse, or chemical dependency. Five services for vulnerable populations were examined: psychiatric outpatient services, psychiatric emergency room services, psychiatric inpatient services, outpatient, and rehabilitation services for persons diagnosed with alcoholism, drug abuse, or chemical dependency, and services for patients diagnosed with HIV-AIDS. Nine high-tech services were examined. Four require investments in beds as well as in equipment and personnel: trauma center, neonatal intensive care unit, transplant services, and burn units. Five involve investments in equipment and personnel: magnetic resonance imaging (MRI), radiation therapy, angioplasty, single photo emission computerized tomography (SPECT), and extracorporeal shock-wave lithotripsy (ESWL). Three community services were examined: community outreach centers, transportation services, and Meals on Wheels. We have data on these three services only for 1994, 1996, and 1999 because AHA did not collect information on them in 1991. For each of the 17 services, we created a variable that indicates whether the hospital or one of its subsidiaries provided the service. If the hospital reported that it provided the service locally through a partner in its health system, network, or a joint venture, we did not designate this hospital as a provider of the service. This eliminated some double counting. Consider a local health system that consists of an academic health center (AHC) hospital and three community hospitals, a configuration common in New York City (Salit et al., 2002). Suppose the AHC hospital has a burn unit but the community hospitals do not have one. The AHC hospital would report that it provided the service at the hospital. The community hospitals would report that they provided the service locally through the health system. To avoid counting this burn unit four times, we only recognized those that are provided at the hospital or a subsidiary. Ideally, we would use the number of beds provided or volume of visits to measure the magnitude of these services. However, this information is not available for all of the services on the AHA survey.
To measure hospital financial status, we used hospital margins calculated from the Medicare Cost Reports. Other hospital characteristics used in the analysis were ownership status, teaching status based on the residents-to-bed ratio, and the percentage of the hospital inpatient days that were covered by Medicaid. When modeling the hospital service availability, we obtained the hospital characteristics from the AHA data and when modeling hospital financial status, we obtained these hospital characteristics from the Medicare Cost Reports.
In these analyses we controlled for four health care market factors: hospital market competition, HMO penetration, local costs, and overall demand. To control for the level of hospital competition, we calculated a Herfindahl index, which is equal to the sum of the squares of the market shares, using staffed hospital beds. We obtained HMO penetration data from InterStudy. We used the HCFA
wage index as a measure of cost. To control for overall demand adjusting for geographic convenience, we used population density (Porell and Adams, 1995).
METHODOLOGY
We conducted MSA- and hospital-level analysis on three sets of variables: hospital beds, hospital services, and hospital margins.
Beds
In the MSA level analysis, we regressed beds per capita for total beds, medical-surgical beds, beds in intensive care units, psychiatric inpatient beds, and beds for treatment of alcohol and chemical dependency on the percent of uninsured residents in the MSA, the other MSA characteristics, (i.e., percent Medicaid, percent Medicare, percent HMO enrollment, level of hospital competition, hospital wage index, and population density) and year categorical variables to control for fixed time effects. We estimated these models using generalized least squares with robust standard errors, controlling for clustering at the MSA level. We gave greater weight to larger MSAs by using the average MSA population as a weight in the regression analysis.
We conducted hospital-level regressions of the natural log of beds in each of the five bed categories on the MSA-level variables, plus controls for hospital characteristics such as ownership, teaching status, size, and percent Medicaid patients. We used a general estimating equations framework to construct random effects regression models controlling for unobserved hospital and time effects. We prefer random effects models because the uninsured rate does not vary substantially over time within an MSA, and within MSA variation over the time period we examine is unlikely to drive hospital behavior. For psychiatric beds and alcohol/chemical dependency beds, because a high proportion of hospitals did not provide beds for the service, we used random effect negative binominal count models. For each model, we calculated standard errors using the Huber-White correction and weighted each hospital by its average number of beds during the study period. Since hospitals are nested within MSAs, we adjusted the estimated standard errors to reflect MSA clustering. We also verified that the models were homoscledastic with respect to the uninsured rate using the Breusch-Pagan Test (Greene, 2000).
Services
For the MSA analysis, we regressed the proportion of hospitals offering specific services on the percent of uninsured in the MSA and the other MSA-level variables described above. We also conducted this regression weighting the proportion of hospitals offering the service by total hospital beds in these hospitals. This weighted analysis gives larger hospitals offering the service more importance
and implicitly uses as the dependent variable the proportion of hospital beds in the MSA that are in hospitals offering the service. In both regressions, we estimated these models with robust standard errors and weighted each MSA by its population size.
For the hospital-level analysis, we estimated random effect logistic regression models that controlled for hospital-specific effects for each service. The MSA- and hospital-level variables were those described above, with adjustments for clustering at the MSA level.
Margin
To determine whether the uninsured rate affected the financial status of hospitals, we estimated MSA-level and hospital-level models. For the MSA-level model, the aggregate margin was the dependent variable. This is a measure used by the Medicare Payment Advisory Commission (MedPAC) to characterize the financial health of a category of hospitals. Aggregate margin equals total hospital revenues in the MSA, minus total hospital expenses in the MSA, divided by total revenues. The independent variables were the percent of uninsured residents in the MSA, the percent Medicaid and Medicare enrollees, the percent of public and for-profit hospitals in the MSA, hospital wage index, population density, and year categorical variables to control for fixed time effects.
For the hospital-level models, we used the total hospital margin as the dependent variable. Because of outliers, we excluded observations with margins below the third percentile and above 97th percentile. The independent variables in this model were the uninsured rate, the other MSA characteristics, and the hospital characteristics. Similar to the other hospital-level models, we estimated random effects controlling for unobserved hospital and time effects, weighting by hospital beds and calculating robust standard errors using the Huber-White correction.
RESULTS
Means and standard deviations for the percent uninsured at the MSA level, beds per 100,000 population, the proportion of hospitals offering each service (unweighted), and percentage of beds in hospitals with each service (weighted), and MSA-level margin are presented in Table D.1. The regression coefficients on the proportion of uninsured in the MSA for regressions on beds, services, and margins are presented in Table D.2. Results from regressions of services using the unweighted and weighted availability measure are both presented. Hospital-level regressions are presented in Table D.3.
Proportion of Uninsured
On average 12.2 percent of the total population in the 85 MSAs studied was uninsured in 1999. The range varied from 6.2 percent uninsured in Allentown-
TABLE D.1 Means and Standard Deviations for Percent Uninsured in MSA and Dependent Variables
|
|
Unweighted |
Weighted |
||||
|
Variable |
N |
Mean |
SD |
N |
Mean |
SD |
|
Percent Uninsured in MSA |
340 |
14.6 |
5.3 |
|
||
|
Beds per 100,000 Population |
||||||
|
Total |
340 |
316.2 |
106.6 |
|||
|
Medical-Surgical |
340 |
173.2 |
78.0 |
|||
|
ICU |
340 |
29.7 |
10.3 |
|||
|
Psychiatric |
340 |
18.5 |
12.1 |
|||
|
Alcohol and chemical dependence |
340 |
3.9 |
4.3 |
|||
|
|
% |
% |
|
% |
% |
|
|
Services for Vulnerable Populations |
||||||
|
Psychiatric inpatient |
340 |
39.6 |
18.1 |
340 |
59.2 |
21.6 |
|
Psychiatric emergency |
340 |
40.5 |
19.4 |
340 |
58.4 |
22.1 |
|
Psychiatric outpatient |
340 |
32.5 |
16.7 |
340 |
49.3 |
21.8 |
|
Alcohol and chemical dependence |
340 |
25.8 |
16.7 |
340 |
37.8 |
22.4 |
|
AIDS |
340 |
54.1 |
21.0 |
340 |
73.7 |
18.9 |
|
High Technology Services |
||||||
|
Trauma |
340 |
22.3 |
13.8 |
340 |
38.5 |
19.8 |
|
NICU |
340 |
25.8 |
12.6 |
340 |
42.9 |
17.9 |
|
Transplant |
340 |
16.5 |
11.2 |
340 |
32.2 |
17.3 |
|
Burn |
340 |
5.2 |
4.9 |
340 |
11.1 |
11.0 |
|
MRI |
340 |
47.2 |
20.6 |
340 |
66.2 |
23.3 |
|
Radiation therapy |
340 |
37.2 |
15.3 |
340 |
61.0 |
18.5 |
|
Angioplasty |
340 |
34.2 |
14.9 |
340 |
60.4 |
18.8 |
|
SPECT |
340 |
41.2 |
16.8 |
340 |
57.3 |
19.4 |
|
ESWL |
340 |
14.5 |
10.7 |
340 |
26.0 |
19.0 |
|
Community Services |
||||||
|
Community outreach |
255 |
56.9 |
17.8 |
255 |
75.4 |
17.5 |
|
Transportation |
255 |
24.8 |
15.6 |
255 |
33.7 |
22.0 |
|
Meals on Wheels |
255 |
12.3 |
12.7 |
255 |
14.2 |
15.7 |
|
Margin |
340 |
3.4 |
4.8 |
|
||
TABLE D.2 Regression Coefficients of Beds, Services, and Margin on Percentage of Uninsured in Metropolitan Area and Other Variables, MSA-Level Regressions
|
|
Coefficients and Standard Errors (SE) for Percent Uninsured in MSA |
||||
|
|
Unweighted Regression |
Weighted Regression |
|||
|
Variable |
N |
Coefficient |
SE |
Coefficient |
SE |
|
Beds per 100,000 Population |
|||||
|
Total |
339 |
–2.67 |
(1.27)a |
|
|
|
Medical-surgical |
339 |
–2.00 |
(0.82)a |
||
|
ICU |
339 |
–0.12 |
(0.13) |
||
|
Psychiatric |
339 |
–0.61 |
(0.17)c |
||
|
Alcohol and chemical dependence |
339 |
–0.19 |
(0.04)c |
||
|
Services for Vulnerable Populations |
|||||
|
Psychiatric inpatient |
339 |
–1.10 |
(0.26)c |
–1.10 |
(0.29)c |
|
Psychiatric emergency |
339 |
–1.40 |
(0.27)c |
–1.30 |
(0.29)c |
|
Psychiatric outpatient |
339 |
–1.27 |
(0.22)c |
–1.36 |
(0.26)c |
|
Alcohol and chemical dependence |
339 |
–1.13 |
(0.22)c |
-1.31 |
(0.31)c |
|
AIDS |
339 |
–0.47 |
(0.20)a |
-0.20 |
(0.21) |
|
High Technology Services |
|||||
|
Trauma |
339 |
–0.62 |
(0.21)b |
–0.63 |
(0.24)b |
|
NICU |
339 |
0.26 |
(0.19) |
0.61 |
(0.23)b |
|
Transplant |
339 |
–0.19 |
(0.17) |
–0.32 |
(0.23) |
|
Burn |
339 |
–0.17 |
(0.04)c |
–0.17 |
(0.13) |
|
MRI |
339 |
–0.14 |
(0.19) |
0.10 |
(0.22) |
|
Radiation therapy |
339 |
–0.33 |
(0.19) |
–0.14 |
(0.26) |
|
Angioplasty |
339 |
0.24 |
(0.18) |
0.46 |
(0.21)a |
|
SPECT |
339 |
–0.65 |
(0.23)b |
–0.32 |
(0.19) |
|
ESWL |
339 |
0.22 |
(0.13) |
0.24 |
(0.22) |
|
Community Services |
|||||
|
Community outreach |
255 |
–1.15 |
(0.23)c |
–0.77 |
(0.24)b |
|
Transportation |
255 |
0.10 |
(0.29) |
0.37 |
(0.38) |
|
Meals on Wheels |
255 |
–0.52 |
(0.21)a |
–0.42 |
(0.28) |
|
Margin |
340 |
-0.14 |
(0.04)b |
|
|
|
ap<0.05 bp<0.01 cp<0.001 NOTES: Regressions of beds and services include percent MSA Medicaid, percent MSA Medicare, HMO penetration, Herfindahl index, population density, CMS wage index, and dummies for years 1994, 1996, and 1999. Regressions of margin include percent MSA Medicaid, percent MSA Medicare, percent hospitals in MSA for-profit, percent hospitals in MSA public, percent hospitals in MSA major teaching hospitals, and dummies for years 1994, 1996, and 1999. |
|||||
TABLE D.3 Regression Coefficients of Beds, Services, and Margin on Percentage of Uninsured in Metropolitan Area and Other Variables, Hospital Level Regressions
|
|
Coefficients and Standard Errors (SE) for Percent Uninsured in MSA |
||
|
Variable |
N |
Coefficient |
SE |
|
Log (Beds in Hospital) |
|||
|
Total |
7157 |
-0.0070 |
(0.0027)b |
|
Medical-surgical |
6261 |
-0.0103 |
(0.0045)a |
|
ICU |
6261 |
0.0082 |
(0.0040)a |
|
Psychiatric |
6261 |
-0.0103 |
(0.0004)c |
|
Alcohol and chemical dependence |
6261 |
-0.0163 |
(0.0006)c |
|
Services for Vulnerable Populations |
|||
|
Psychiatric inpatient |
6261 |
-0.022 |
(0.013) |
|
Psychiatric emergency |
6261 |
-0.030 |
(0.016) |
|
Psychiatric outpatient |
6261 |
-0.024 |
(0.016) |
|
Alcohol and chemical dependence |
6261 |
-0.041 |
(0.018)a |
|
AIDS |
6261 |
-0.020 |
(0.016) |
|
High Technology Services |
|||
|
Trauma |
6261 |
0.005 |
(0.017) |
|
NICU |
6261 |
0.041 |
(0.016)b |
|
Transplant |
6261 |
0.007 |
(0.017) |
|
Burn |
6261 |
-0.020 |
(0.016) |
|
MRI |
6261 |
0.051 |
(0.033) |
|
Radiation therapy |
6261 |
0.006 |
(0.016) |
|
Angioplasty |
6261 |
0.045 |
(0.019)a |
|
SPECT |
6261 |
0.002 |
(0.014) |
|
ESWL |
6261 |
0.022 |
(0.021) |
|
Community Services |
|||
|
Community outreach |
4493 |
-0.009 |
(0.016) |
|
Transportation |
4493 |
0.024 |
(0.020) |
|
Meals on Wheels |
4493 |
-0.039 |
(0.029) |
|
Margin |
6459 |
0.027 |
(0.059) |
|
ap<0.05 bp<0.01 cp<0.001 NOTES: Regressions of beds and services include percent MSA Medicaid, percent MSA Medicare, HMO penetration, Herfindahl index, population density, CMS wage index, and dummies for years 1994, 1996, and 1999. Regressions of margin include percent MSA Medicaid, percent MSA Medicare, percent hospitals in MSA for-profit, percent hospitals in MSA public, percent hospitals in MSA major teaching hospitals, and dummies for years 1994, 1996, and 1999. Standard errors are adjusted for hospital and MSA level clustering. |
|||
Bethlehem, Pennsylvania and Harrisburg, Pennsylvania, to 26.6 percent uninsured in Jersey City, New Jersey. During the 1990s, the average uninsured rate fell 3.8 percentage points. Most of these MSAs, 76 of 85, experienced a decline in the uninsured rate during the 1990s. Almost a third had declines of greater than 5 percentage points. Of those MSAs in which the uninsured rate increased, the largest occurred in San Francisco, which increased from 14.8 to 18.7 percent, and Jersey City, which increased from 22.7 to 26 percent.
Beds
Across the 85 metropolitan areas in this analysis, there were 316 beds per 100,000 population. More than half of these were in medical-surgical beds. Approximately 10 percent of beds were in ICUs. There were far fewer psychiatric and alcohol and chemical dependence treatment beds (18.5 and 3.9 per 100,000 respectively), but there is much wider variation across MSAs in the supply of these beds than in any other category.
In the MSA-level regressions, there is evidence that beds per capita and all categories of beds studied except ICU beds were lower where the proportion of the population uninsured is higher. In the hospital-level regressions, for all bed categories except ICU beds, hospitals offer fewer beds where the local uninsured rate is higher. An increase in the uninsured rate of 5.3 percentage points, one standard deviation, is associated with a 4.5 percent decrease in beds overall, a 6.1 percent decrease in medical–surgical beds, a 17.5 percent decrease in psychiatric beds, and 25.8 percent decrease in alcohol and chemical dependence beds at the mean level of beds per capita.
Services for Vulnerable Populations
With respect to services for vulnerable populations, AIDS services are the most common. Over half the hospitals offer these services, and nearly three-quarters of hospital beds are in hospitals that offer these services. Psychiatric inpatient and emergency services are available in approximately 40 percent of hospitals (with 60 percent of the beds), while psychiatric outpatient and alcohol and chemical dependence treatment are available in between one-quarter to one-third of hospitals.
In the MSA-level regressions, the availability of all three psychiatric services and alcohol and chemical dependence services are found to be lower in metropolitan areas with higher uninsurance, with an increase in the uninsured rate of 5.3 percent associated with 5.8 to 7.4 percent fewer hospitals offering the service. AIDS services are also lower, although statistically significant only in the unweighted regression. In hospital-level regressions, there is a negative association between all these services and the uninsured rate, but only the association with alcohol and chemical dependency services is statistically significant.
High-Technology Services
Bed-based high-technology services (trauma, neonatal ICU [NICU], transplant, and burn) were much less commonly available than services for vulnerable populations, with the proportion of hospitals offering such services varying from 25.8 percent for NICU to 5.2 percent for burn. Because these services were more likely to be offered by larger hospitals, the proportion of beds in hospitals offering these services varied from 42.9 percent for NICU to 11.1 percent for burn care.
Among these four services, in the MSA-level regressions, trauma services are less likely to be available in communities with higher uninsured rates, a finding observed in both the unweighted and weighted regressions. (In the hospital-level regression, the results are of the opposite sign but not statistically significant.) The estimates of the negative impact of MSA uninsured rate on the MSA-level analysis of burn service availability are consistent in the unweighted and weighted model, but only statistically significant for the unweighted model. There is no statistically significant association of transplant services and uninsured rates in any model. The availability of NICU services is higher in MSAs with higher uninsured rates, a finding that is statistically significant in the weighted MSA regression and hospital-level regression.
High-technology services that do not have dedicated beds associated with them were much more likely to be provided by hospitals. With the exception of lithotripsy (present on average in only 14.5 percent of the hospitals in our sample), approximately 30 to 50 percent of the hospitals provided the services we studied. The proportion of beds in hospitals with these services varied from 57.3 percent for SPECT to two-thirds for MRI. We find no consistent pattern of association between the availability of other high-technology services and uninsured rates in the regression analysis.
Community Services
The frequency with which the community services we studied were provided by hospitals varied widely. Community outreach was the most common, present in 60 percent of the hospitals in our sample and in hospitals with 75 percent of beds, on average. Transportation services were provided by one-quarter of the hospitals in our sample and Meals on Wheels by 12 percent.
In the MSA-level regressions, a smaller proportion of hospitals are likely to provide community outreach services in MSAs with high uninsured rates. This is true whether availability is measured in terms of the proportion of hospitals or the proportion of beds. The results in the hospital level regressions are consistent with this finding but not statistically significant.
There is some evidence that hospitals in communities with high uninsured rates are less likely to offer Meals on Wheels, but no evidence of lower levels of transportation services.
Hospital Margins
The average hospital margin in our MSAs was 3.4 percent. There is wide variation among aggregate MSA margins. We observe no statistically significant association in either the MSA or hospital-level regressions of margin on uninsured rates.
DISCUSSION
In our analysis, we find inconsistent results between the MSA and hospital-level models. Within MSAs, the impact of uninsured patients on hospital decisions to offer services may differ across institutions in ways that our hospital-level models do not currently capture. We place more weight on the MSA-level models. The hospital-level models indicate how average individual hospitals may respond to increased demand for hospital care from the uninsured as measured by the MSA-wide uninsured rate. However, it is unlikely that the overall market response is merely the weighted average of individual hospital responses in the market. This would assume that hospitals neither behave strategically nor respond to the actions of their competitors. For example, a safety-net hospital may eliminate a high-tech service because they cannot support it with its payer mix. However, this may pave the way for a competing hospital to offer the service. The competing hospital, because of its location, amenities, and reputation in the market, may be able to attract more privately insured patients, thus making the service financially solvent. The competing hospital may have higher aggregate volume that can improve quality and lower per-patient costs associated with the service, and this might be a positive aspect of consolidation. Alternatively, the shift of the service away from hospitals that serve the uninsured might reduce its availability to the uninsured and insured populations who use that hospital, a negative consequence of the shift. None of this is observable in the hospital-level models. The MSA-level models allow us to observe the overall association of uninsurance and the availability of hospital services, net of the strategic behavior by individual hospitals.
There are also inconsistencies between the unweighted and weighted MSA-level models of service availability. The unweighted models examine the proportion of hospitals offering the service; the weighted model, the proportion of beds in hospitals with the service. This gives greater weight to larger hospitals. Implicitly this presumes that a service offered by a large hospital will more likely be larger and have a greater impact on the geographic market than the same service offered at a smaller facility.
A possible explanation for the weak association we observe between margins and the uninsured rate is the presence of other revenue sources that support hospital care of the uninsured in some MSAs. For example, hospitals in Maryland, Massachusetts, New Jersey, and New York received some state and local subsidy from charity care or indigent care pools. These funds offset financial losses due to
care for the uninsured and improve hospital margins. Their presence may cloud the statistical association between uninsured rates and hospital margins. State and local governments are more likely to establish these revenue sources in communities with high uninsured rates. We may not have adequately controlled for the existence of these alternate revenue sources in our analyses.
The lack of an association between margins and the uninsured rate for urban hospitals differs from our finding for rural hospitals. There, we find a consistent association of lower margins with higher uninsured admissions. We believe these contrasting findings reflect a difference in strategies between urban hospital administrators and rural hospital administrators when faced with financial pressure due to the uninsured rate. Urban hospital administrators are more likely to reduce or eliminate services in order to maintain the overall financial health of the institution. Compared to their rural counterparts, urban hospital administrators are more likely to employ this strategy because there may be other alternatives for the service in their metropolitan area. Although overall capacity for the service is reduced, the community does not lose the service completely. Conversely, in rural areas, the hospital may be the sole provider of that service in the geographic area. This reality may encourage rural hospital administrators to maintain services when faced with low (or even negative) margins.
With the exception of trauma care, we did not find a strong association between the uninsured rate and the availability of high-tech services. A possible explanation is that uninsured persons do not have good access to elective hospital services. For some of these high-tech services, particularly when provided on an outpatient basis, patients need a physician referral. For the most part, uninsured patients will only get referred to these services if they are admitted to the hospital through the emergency room and the hospital-assigned physician orders the services. Consequently, hospitals are better able to control their patient mix by source of payment for their high-tech services. This ensures that these services will not incur losses due to high demand from uninsured patients. Of the high-tech services in our study, only trauma units and to some extent burn units do not present this access problem for the uninsured. Because trauma care patients are emergent and their admission is not discretionary or readily controlled by hospital policies, trauma units can incur losses due to large volumes of uninsured patients. Hospital administrators must take this into account in deciding whether to offer trauma care. Hence, the availability of trauma care is sensitive to the uninsured rate.
Notwithstanding these inconsistencies and limitations in the analysis, in this analysis, we find robust associations between MSA uninsured rates and availability of psychiatric and alcohol and substance abuse services. We find this association in our MSA- and hospital-level analyses of beds and services. We find some evidence of an association of uninsured rates and the provision of trauma services and community outreach services by hospitals and weaker evidence of an impact on burn services and Meals on Wheels. The common feature of these services (with the exception of Meals on Wheels services) is that they have the potential to bring
into the hospital uninsured patients whose care may be expensive. The presence of higher numbers of uninsured persons in a market may discourage hospitals from offering services for fear that they will not be reimbursed for a significant portion of the care they provide.
ADDENDUM 85 LARGEST U.S. METROPOLITAN STATISTICAL AREAS
|
Akron, OH |
Greenville, SC |
Orlando, FL |
|
Albany, NY |
Harrisburg, PA |
Philadelphia, PA-NJ |
|
Albuquerque, NM |
Hartford, CT |
Phoenix-Mesa, AZ |
|
Allentown, PA |
Honolulu, HI |
Pittsburgh, PA |
|
Ann Arbor, MI |
Houston, TX |
Portland, OR-WA |
|
Atlanta, GA |
Indianapolis, IN |
Providence, RI-MA |
|
Austin-San Marcos, TX |
Jacksonville, FL |
Raleigh, NC |
|
Bakersfield, CA |
Jersey City, NJ |
Richmond, VA |
|
Baltimore, MD |
Kansas City, MO-KS |
Riverside-San Bernardino, CA |
|
Bergen-Passaic, NJ |
Knoxville, TN |
Rochester, NY |
|
Birmingham, AL |
La Vegas, NV-AZ |
Sacramento, CA |
|
Boston, MA-NH |
Los Angeles, CA |
Salt Lake City, UT |
|
Buffalo-Niagara, NY |
Louisville, KY-IN |
San Antonio, TX |
|
Charlotte, NC-SC |
Memphis, TN-AR-MS |
San Diego, CA |
|
Chicago, IL |
Miami, FL |
San Francisco, CA |
|
Cincinnati, OH-KY-IN |
Middlesex, NJ |
San Jose, CA |
|
Cleveland, OH |
Milwaukee, WI |
Seattle, WA |
|
Columbus, GA-AL |
Minneapolis, MN-WI |
St. Louis, MO-IL |
|
Columbus, OH |
Monmouth, NJ |
Syracuse, NY |
|
Dallas, TX |
Nashville, TN |
Tacoma, WA |
|
Dayton, OH |
Nassau-Suffolk, NY |
Tampa, FL |
|
Denver, CO |
New Orleans, LA |
Tucson, AZ |
|
Detroit, MI |
New York, NY |
Tulsa, AZ |
|
El Paso, TX |
Newark, NJ |
Ventura, CA |
|
Fort Lauderdale, FL |
Norfolk, VA-NC |
Washington, DC-MD-VA-WV |
|
Fort Worth, TX |
Oakland, CA |
West Palm Beach, FL |
|
Fresno, CA |
Oklahoma City, OK |
Youngstown, OH |
|
Grand Rapids, MI |
Omaha, NE-IA |
|
|
Greensboro, NC |
Orange County, CA |
The Impact of Uninsured Discharges on the Availability of Hospital Services and Hospital Margins in Rural Areas
Jack Needleman and Darrell J. Gaskin
ABSTRACT
Objective: To identify the effects of the percentage of uninsured persons in a rural community on the availability of hospital services for the entire community.
Data and Study Design: Our analysis focuses on rural counties in seven states: CA, MA, NJ, NY, PA, WA, and WI. We use data on state hospital discharges for 1991, 1994, and 1996 to calculate the proportion of discharges of county residents that were either self-pay or charity care. Data from the Medicare Cost Reports and American Hospital Association’s (AHA) Survey of Hospitals were used to estimate the impact of the uninsured rate on hospital margins and four measures of hospital service availability, i.e., capacity, services to vulnerable populations, community services, and high-tech services. We estimate county-level models.
Findings: We find some evidence that in counties with higher proportions of uninsured patients who are not concentrated in a subset of hospitals, hospitals are less likely to offer psychiatric inpatient services. We also find some evidence that there are fewer intensive care unit (ICU) and psychiatric beds. There is a consistent association of higher uninsured admissions and a lower likelihood of hospitals offering high-technology services, although the association is statistically significant only for transplant, magnetic reso
nance imaging (MRI), radiation therapy, and lithotripsy (ESWL) services. There is strong evidence that hospital margins are lower in counties with higher proportions of uninsured discharges.
Conclusion: Admissions of uninsured patients in rural counties are associated with lower hospital financial status and less availability of psychiatric and high-technology services.
INTRODUCTION
Prior research has shown that the lack of health insurance coverage is a barrier to care for the uninsured and can lead to negative health outcomes. The uninsured receive about two-thirds of the care obtained by comparable insured population (Long and Marquis, 1994; Marquis and Long, 1994-1995). However, little is known about how the presence of uninsured persons affects the health care delivery system in their communities. According to the AHA, hospitals provided over $18 billion in uncompensated care in 1997. Most of this care was provided as charity to low-income persons who lacked health insurance coverage (Weissman et al., 1999). Providing hospital care to patients who are inadequately insured can be a financial burden to hospitals. This financial stress could affect hospitals’ ability to deliver services to the broader community. Needleman (2000) identifies three ways this financial stress could affect hospitals care for the entire community: (1) cutbacks in services, (2) reductions in quality, and (3) closures of facilities. In particular, he argues that hospitals that are faced with a high demand for charity care may respond by reducing staff, cutting back hours, increasing waiting times and eliminating services. Potentially these types of changes can affect the hospitals’ ability to provide high-quality services. Theoretically, it follows that if the financial stress due to high demand for charity care is great enough, hospitals would eventually have to close due to a lack of resources.
In the 1980s, approximately 700 hospitals closed. While there have been numerous studies on the determinants of hospital closures, none have examined the role of hospital’s payer mix or community uninsurance. However, researchers have found a relationship between hospital closures and three community characteristics that are correlated with high uninsured rates: the percentage of residents who are low-income or minority and high unemployment rates.
In a similar study that focuses on hospitals in the 85 largest metropolitan statistical areas (MSAs) during the 1990s, we present evidence that high uninsured rates were associated with reductions in hospital services. The uninsured rate was negatively related to beds per capita in the MSA and the average hospital size. In addition, the availability of services for vulnerable populations and community services and the propensity for hospitals to offer these services was negatively associated with the uninsured rate.
In this study, we examine the effect of uninsurance on rural hospitals. In 1999, 18.9 percent of residents of rural areas lacked health insurance coverage
(NCHS, 2001). How does their presence affect the availability of hospital services in rural areas? Similar to urban hospitals, we expect the overall effect to be negative. However, there should be some differences. When faced with financial pressure, rural hospital administrators may try to offer a full range of services to meet the broad needs of their communities because residents have few alternatives. In contrast, urban hospital administrators may be more likely to maintain niche “specialty” services in the face of financial pressure because there are more alternatives in their communities for basic or routine hospital services.
Detailed data on the number of uninsured persons or the uninsured rate at the county or hospital market level are not available. (See Appendix B of this report for further discussion of data and measurement issues for local uninsured rates.) As a surrogate for the uninsured rate, we use the proportion of hospital discharges from a county that is uninsured (Rask, 1994; Turner and Campbell, 1999). We examine whether there is an association between the proportion of uninsured hospital discharges among a rural county’s residents and lesser availability of hospital services in the county. Our specific research questions are
-
Are there fewer hospital beds per capita in rural counties with high proportions of uninsured discharges?
-
Does the availability of hospital services for the entire county decline as the proportion of uninsured discharges in the county increases?
-
Does the proportion of uninsured discharges negatively affect the financial status of hospitals?
-
Does the impact of the proportion of uninsured discharges on the hospital delivery system decline as hospital care for the uninsured become more concentrated in a few hospitals?
CONCEPTUAL FRAMEWORK
As stated above, we hypothesize that the uninsured rate is negatively related to the demand for hospital services. Several studies have shown that market forces that have depressed demand for hospital services have had an impact on the size of the hospital delivery system. For example, Medicare’s transition from a cost-based reimbursement system to prospective payment and the subsequent reduction in the growth of Medicare hospital payment rates resulted in lower hospital utilization, a reduction in the intensity of hospital services, and encouraged a reduction in hospital size (Coulam and Gaumer, 1991; Hodgkin and McGuire, 1994). The introduction of managed care also reduced demand for hospital services. Several studies have demonstrated that increased HMO penetration is associated with reduction in hospital utilization, hospital beds, slower hospital cost inflation, and slower revenue growth (Miller and Luft, 1994; Chernew, 1995; Robinson, 1996; Gaskin and Hadley, 1997). Dranove and colleagues (1986) modeled the impact of managed care penetration on hospitals, and they concluded that downward pressure on hospital prices would result in a reduction in hospital capacity.
For simplicity, assume that hospitals serve two types of patients, insured and uninsured, and that every hospital in the market serves each type of patient proportionate to their presence in the hospital market area. Payment rates for treating insured patients are typically greater than average cost. Reimbursement rates for treating uninsured patients are typically less than average cost. If, at the volumes at which the rural hospital operates, the cost structure exhibits increasing returns to scale (e.g., total cost increases with the volume of services at a decreasing rate), cost-minimizing hospitals will operate at volume levels where marginal cost is less than average cost (Folland et al., 2001). In choosing the volume of services they provide, hospitals will equate marginal costs with marginal revenues where average revenues exceed average costs depending upon their market structure (Tirole, 1988). Hospitals that are monopolies or part of oligopolies will set marginal costs equal to marginal revenues. Hospitals that are in monopolistic competitive markets will compete until their average costs equal average revenues (Chamberlin, 1962). In such a market, as the uninsured rate increases, average and marginal revenues at each hospital decline. In response, each hospital will reduce its supply of services. This implies that overall market supply will decline as the overall demand curve shifts downward. Also, because there are more uninsured patients, the need for hospital services at discounted rates (or for free) will increase. As shown in Figure D.1, this results in a downward rotation of the demand curve for hospital services.
In some markets, there are safety-net hospitals that provide a disproportionate share of the care to the uninsured while other hospitals provide less than their proportionate share of the market for uninsured patients. In such a market, an increase in the uninsured rate would have a larger effect on safety-net hospitals than on other hospitals, if the safety-net hospitals absorbed the increase in the demand for care for uninsured patients. However if, as the uninsured rate increases, non-safety net hospitals in the co mmunity become proportionately more involved in the care for the uninsured, then these hospitals will be more affected by the change in demand.
Another assumption implicit in our model is that the uninsured and insured patients use the hospital for the same mix of services. However, suppose there is a set of hospital services that the uninsured are more likely to use than insured patients. Profits for these services will tend to be lower than profits associated with other hospital services because of their payer mix. Therefore, we expect that hospitals will cut back on services that the uninsured are more likely to use as the uninsured rate increases. In rural areas, this will often have a negative spillover effect on insured patients in county. Because rural communities have few alternative providers, insured patients may have to travel long distances to obtain services dropped by their local hospital.
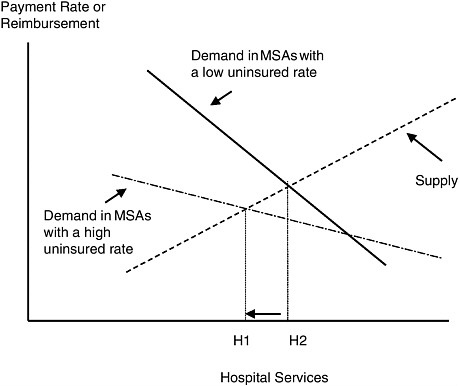
FIGURE D.1 The impact of uninsurance rate on the demand and supply of hospital services.
DATA
Data for this study come from four sources:
-
state hospital discharge data from seven states
-
the AHA Annual Survey of Hospitals
-
the Medicare Cost Reports and
-
the Area Resource File compiled by the Bureau of Health Professions
We used hospital discharge data from California, Massachusetts, New Jersey, New York, Pennsylvania, Washington, and Wisconsin for 1991, 1994, and 1996. These states were chosen because they distinguished whether patients’ expected source of payment was self pay or charity care.
Our analysis focuses on the availability of hospital services in 168 rural counties in our seven states: 23 counties in California, 25 in Florida, 2 in Massachusetts, 21 in New York, 29 in Pennsylvania and 23 in Washington and 45 in Wisconsin. We defined rural counties as those that were not located within an MSA. Of the 168 counties, 56 percent have only one hospital and 69 percent were located
TABLE D.4 Comparison of Counties Included in Analysis to All U.S. Rural Counties
|
|
Sample |
U.S. |
|
Number |
168 |
2,369 |
|
Average County Population, 1997 |
46,229 |
22,250 |
|
Population Density (people per square mile) |
55.9 |
44.1 |
|
Per Capita Income, 1998 |
$20,748 |
$18,917 |
|
Poverty Rate (percent), 1997 |
13.5 |
16.0 |
|
Percent Adjacent to Metropolitan Area |
69.6 |
43.4 |
adjacent to an MSA. As shown in Table D.4, compared to U.S. rural counties as a whole, the counties included in this analysis have larger populations, are more densely populated, have somewhat higher per capita income, and are more likely to be adjacent to metropolitan areas.
We identified patients from rural counties using their county of residence information in the discharge database. For each rural county, we calculated the proportion of discharges originating in that county where the expected sources of payment were self-pay or charity, Medicaid, Medicare, or HMO. For ease of exposition, we refer to these proportions as the county’s percent of uninsured discharges, Medicaid discharges, Medicare discharges, and HMO discharges, respectively. We used these measures as proxies for the rate of insurance coverage for hospital care in the county. The percentage of uninsured discharges indicates the amount of inpatient services provided to uninsured persons relative to the entire inpatient market. This is a reasonable proxy for uninsured persons’ share of the demand for hospital services.
To measure the availability of hospital services, we used data from the AHA Survey of Hospitals for the years 1991, 1994, and 1996. We used four measures of hospital service availability: hospital capacity, services to vulnerable populations, community services, and high-tech services. To measure capacity we used the number of hospital beds, medical-surgical beds, psychiatric beds, ICU beds, and beds devoted to patients diagnosed with alcoholism, drug abuse, or chemical dependency. Five services for vulnerable populations were examined: psychiatric outpatient services, psychiatric emergency room services, psychiatric inpatient services, outpatient and rehabilitation services for persons diagnosed with alcoholism, drug abuse, or chemical dependency, and services for patients diagnosed with HIV-AIDS. Eight high-tech services were examined. Three require investments in beds, in addition to equipment and personnel: trauma center, neonatal intensive care unit (NICU), and transplant services. Five involve investments in equipment and personnel: magnetic resonance imaging (MRI), radiation therapy, angioplasty, single photo emission computerized tomography (SPECT), and extracorporeal shock-wave lithotripsy (ESWL). Three community services were examined: community outreach centers, transportation services, and Meals on Wheels. We have
data on these services for 1994 and 1996 only because the AHA did not collect this information in 1991. For each of the 16 services, we create a variable that indicates whether the hospital or one of its subsidiaries provided the service. If the hospital indicated that it provided the service locally through a partner in its health system, network, or a joint venture, we did not designate this hospital as a provider of the service. This eliminated some double counting. To measure hospital financial status, we used hospital margins calculated from the Medicare Cost Reports.
In our analyses, we are specifically interested in how the relative concentration of uninsured discharges affects the availability of hospital services. To measure the relative concentration of uninsured discharges we calculated two Herfindahl indexes, which equal the sum of the squares of the market shares. The first measures the concentration of all hospital discharges in the county and the second measures the concentration of uninsured discharges in the county. We then divided the Herfindahl index for uninsured discharges by the Herfindahl index for all discharges. In counties where this ratio equals one, the uninsured discharges are no more concentrated within a subset of hospitals than are all discharges. In counties where this ratio exceeds one, the uninsured discharges are more concentrated than all discharges. This is an indication that one or a few hospitals in area have assumed a disproportionate role in providing these counties’ safety-net services. We include in our regression the main effect of percent uninsured, main effect of the concentration ratio, and the interaction of the concentration ratio with percent uninsured. Our hypothesis is that the county-level effect of the uninsured percentage will be smaller where the uninsured are concentrated.
We examine the interaction of this ratio with the county’s percentage uninsured discharges to determine whether relative concentration dampens the effect of uninsured discharges on the availability of hospital services. To facilitate the interpretation of the coefficients on the percentage of uninsured discharges, the main effect of the relative concentration ratio, and the interaction term, we centered the relative concentration ratio on its mean. We examine the overall effect of percent of uninsured discharges in counties with low and high concentration of uninsured discharges by summing the coefficient on the percent uninsured discharges with the product of the coefficient on the interaction term and relative concentration ratio evaluated at the three distinct points. Specifically, we interpreted the effects of uninsured discharges at the 25th percentile (counties where the uninsured discharges are dispersed relative to all discharges), at the mean (which is equivalent to the main effect of the percent uninsured measure), and the 75th percentile (counties where the uninsured are concentrated relative to all discharges).
In addition, we controlled for three other health care market factors. To control for the level of hospital competition, we used the Herfindahl index for all discharges. We use the HCFA wage index as a measure of cost and population density as a measure of overall demand adjusted for geographic convenience (Porell and Adams, 1995).
METHODS
To address our research questions, we analyzed three sets of variables: hospital beds, hospital services, and hospital margins.
Beds
We regressed beds per capita in each county in the following categories: total beds, medical–surgical beds, beds in ICUs, psychiatric inpatient beds, and beds for treatment of alcohol and chemical dependency, on the percent of uninsured discharges in the county, relative concentration of uninsured, other county characteristics (i.e., percent Medicaid discharges, percent Medicare discharges, percent HMO discharges, level of hospital competition, hospital wage index, and population density), and year categorical variables to control for fixed time effects. We estimated these models using generalized least squares with robust standard errors, controlling for clustering at the county level. We gave greater weight to larger counties by using the average county population as a weight in the regression analysis.
Services
We regressed the proportion of hospitals offering specific services on the percent of uninsured discharges in the county, relative concentration of uninsured, and the other county- level variables described above. Because this formulation of the dependent variable does not distinguish the size of the service, we estimated a second set of models using a weighted proportion of hospitals offering specific services. To give larger hospitals offering the specific services more importance, we recalculated this dependent variable using hospital beds as weights. In both regressions, we estimated these models with robust standard errors, and controlled for clustering at the county level. Results from both models are comparable, and we report results only from the weighted regression.
Margin
To determine whether the percentage of uninsured discharges negatively affects the financial status of hospitals, we estimated a model with aggregate margin as the dependent variable. The aggregate margin is a measure used by MedPAC to characterize the financial health of a category of hospitals. It equals total hospital revenues in the county minus total hospital expenses in the county divided by total revenues. The independent variables were the percent of uninsured discharges in the county, the percents Medicaid and Medicare discharges, the percents of public and for-profit hospitals in the county, hospital wage index, population density, and year categorical variables to control for fixed time effects.
RESULTS
Means and standard deviations for the percent of discharges for uninsured patients, beds per 100,000 population, the proportion of hospitals offering each service, (unweighted) percentage of beds in hospitals with each service (weighted), and county-level hospital margins for the rural counties in this analysis are presented in Table D.5. The regression coefficients on the proportion of discharges for the uninsured and the interaction of the percentage of uninsured and uninsured concentration ratios for the regressions on beds, services, and margins are presented in Table D.6. Table D.6 also includes the coefficient on percent uninsured at the 25th and 75th percentile of the relative concentration index and the statistical significance of these coefficients.
Proportion of Uninsured
The proportion of discharges for patients without insurance in the rural counties studied averaged 4.4 percent. This is substantially lower than the percent of uninsured in rural counties, and reflects the fact that the uninsured are younger than the average person in the population and therefore less likely to be hospitalized. (Persons over age 65, virtually all of whom have coverage through Medicare, are disproportionately represented among hospital discharges.) The variation in the proportion of discharges from the uninsured is very large. The standard deviation for the proportion of uninsured is 4.4, as large as the mean, with a range from 0 to 8.8 percent.
Beds
In the 168 counties in this study, there are an average of 423.3 hospital beds per 100,000 population, with wide variation across the counties (standard deviation = 392.3). The average number of beds per capita and variation in beds is larger among these rural counties than was observed in metropolitan areas (Gaskin and Needleman, 2003). Forty-four percent are medical or surgical beds. ICU beds represent only 4 percent of the beds. There are fewer psychiatric and alcohol and chemical dependence beds (10.0 and 4.2 beds per 100,000, respectively) with wide variation across the counties.
There is some evidence that beds per capita are influenced by the percent uninsured in the county. The coefficients on the percent uninsured are consistently negative, although statistically significant only for ICU beds. There is a statistically significant association of ICU beds with percent uninsured at all three levels of uninsured concentration tested. In addition, for psychiatric beds there is a statistically significant association of percent uninsured and bed supply at low levels of concentration of the uninsured (see Table D.6).
TABLE D.5 Means and Standard Deviations for Percent Uninsured Discharges and Dependent Variables
|
|
Unweighted |
Weighted |
||||
|
Variable |
N |
Mean |
SD |
N |
Mean |
SD |
|
Percent Uninsured Discharges |
426 |
4.4 |
4.4 |
|
||
|
Beds per 100,000 Population |
||||||
|
Total |
422 |
423.3 |
392.3 |
|||
|
Medical-Surgical |
396 |
186.8 |
146.5 |
|||
|
ICU |
396 |
17.8 |
22.1 |
|||
|
Psychiatric |
396 |
10.0 |
19.1 |
|||
|
Alcohol and chemical dependence |
396 |
4.2 |
16.0 |
|||
|
|
% |
% |
|
% |
% |
|
|
Services for Vulnerable Populations |
|
|||||
|
Psychiatric inpatient |
396 |
21.7 |
37.2 |
396 |
23.7 |
39.0 |
|
Psychiatric emergency |
396 |
35.1 |
43.7 |
396 |
37.4 |
44.9 |
|
Psychiatric outpatient |
396 |
15.7 |
33.5 |
396 |
16.5 |
34.5 |
|
Alcohol and chemical dependence |
396 |
17.3 |
33.1 |
396 |
17.7 |
34.1 |
|
AIDS |
400 |
39.6 |
44.1 |
396 |
42.4 |
45.9 |
|
High-Technology Services |
||||||
|
Trauma |
396 |
16.1 |
33.4 |
396 |
16.6 |
34.1 |
|
NICU |
426 |
2.7 |
12.9 |
422 |
3.7 |
16.7 |
|
Transplant |
400 |
6.0 |
21.8 |
396 |
6.4 |
22.8 |
|
MRI |
396 |
20.1 |
36.0 |
396 |
21.3 |
37.4 |
|
Radiation therapy |
400 |
13.4 |
29.9 |
396 |
15.5 |
32.6 |
|
Angioplasty |
396 |
3.6 |
16.0 |
396 |
4.5 |
18.5 |
|
SPECT |
396 |
20.6 |
36.6 |
396 |
21.6 |
37.8 |
|
ESWL |
396 |
6.6 |
21.9 |
396 |
7.4 |
23.8 |
|
Community Services |
||||||
|
Community outreach |
258 |
51.8 |
44.4 |
258 |
52.5 |
45.1 |
|
Transportation |
258 |
9.9 |
25.0 |
258 |
10.5 |
27.1 |
|
Meals on Wheels |
258 |
18.9 |
35.2 |
258 |
18.5 |
35.8 |
|
Margin |
414 |
1.8 |
5.9 |
410 |
2.0 |
5.8 |
Services for Vulnerable Populations
With respect to services for vulnerable populations, AIDS services are the most common, with nearly 40 percent of hospitals (with 42.4 percent of the beds) offering these services. Psychiatric emergency services are available in approximately 35 percent of hospitals (with 37 percent of beds), while psychiatric inpa-
tient, outpatient, and alcohol and chemical dependence treatment are available in approximately one-in-five to one-in-six hospitals.
For all services for vulnerable populations except AIDS services, the coefficient on percent uninsured, although not statistically significant, is negative. For both psychiatric inpatient and psychiatric emergency services there is a statistically significant association of the interaction of the uninsured concentration and percent uninsured on the proportion of hospitals offering this service. At the lower level of concentration, there is a statistically significant association of percent uninsured with availability of inpatient psychiatric services.
High-Technology Services
Bed-based high-technology services (trauma, NICU, and transplant) are much less commonly available than services for vulnerable populations, with the proportion of hospitals offering such services varying from 16.1 percent for trauma to 2.7 percent for NICU.
Among these three services, transplant services are less likely to be available in communities with lower concentrations of uninsured and higher uninsured rates. For trauma and NICU services, while the coefficients on percent uninsured are negative, they are not statistically significant.
High-technology services that do not have dedicated beds associated with them vary in their availability in these rural counties. The two imaging services studied—MRI and SPECT—are available in approximately 20 percent of hospitals. Radiation therapy is available in one out of seven hospitals. Lithotripsy and angioplasty are available in relatively few hospitals (6.6 and 3.6 percent of hospitals, respectively). With the exception of SPECT, there is a negative association between these services and the percent uninsured in the county. The association with percent uninsured is statistically significant for MRI and lithotripsy services across the range of uninsured concentrations and statistically significant for radiation therapy when the concentration of the uninsured is low.
Community Services
Community outreach services were available from approximately half the hospitals in our sample. By contrast, Meals on Wheels services were only available from 19 percent and transportation services from only 10 percent. Provision of Meals on Wheels services was negatively associated with percent uninsured in counties where the concentration of uninsured were low.
Hospital Margins
The average county hospital margin in our sample is 1.8 percent, with a standard deviation of 5.9 percentage points, reflecting the substantial variation across counties in margins. We observe statistically significant associations between
TABLE D.6 Regression Coefficients of Beds, Services, and Margin on Percent Uninsured and Interaction of Percent Uninsured With Uninsured Concentration, County-Level Regressions (Weighted)
|
Variable |
N |
Percent Uninsured |
SE |
|
Beds per Capita |
|||
|
Total |
411 |
–2.31 |
(3.08) |
|
Medical-Surgical |
411 |
–1.80 |
(1.18) |
|
ICU |
386 |
–0.45a |
(0.22) |
|
Psychiatric |
386 |
–0.37 |
(0.21) |
|
Alcohol and chemical dependence |
386 |
–0.17 |
(0.12) |
|
Services for Vulnerable Populations |
|||
|
Psychiatric inpatient |
386 |
–0.91 |
(0.59) |
|
Psychiatric emergency |
386 |
–0.77 |
(0.63) |
|
Psychiatric outpatient |
386 |
–0.67 |
(0.46) |
|
Alcohol and chemical dependence |
386 |
–0.16 |
(0.54) |
|
AIDS |
389 |
0.71 |
(0.90) |
|
High-Technology Services |
|||
|
Trauma |
386 |
–0.85 |
(0.57) |
|
NICU |
411 |
–0.35 |
(0.30) |
|
Transplant |
386 |
–0.49 |
(0.28) |
|
MRI |
386 |
–1.67c |
(0.51) |
|
Radiation therapy |
389 |
–0.90 |
(0.51) |
|
Angioplasty |
386 |
–0.43 |
(0.27) |
|
SPECT |
386 |
0.61 |
(0.84) |
|
ESWL |
386 |
–0.91a |
(10.36) |
|
Community Services |
|||
|
Community outreach |
255 |
–0.48 |
(0.70) |
|
Transportation |
255 |
0.22 |
(0.56) |
|
Meals on Wheels |
255 |
–0.58 |
(0.51) |
|
Margin |
402 |
–0.17b |
(0.06) |
|
ap<0.05 bp<0.01 cp<0.001 |
|||
|
Percent Uninsured × Uninsured Concentration |
SE |
25th Percentile of Uninsured Concentration |
75th Percentile of Uninsured Concentration |
|
0.56 |
(1.07) |
–2.75 |
–2.15 |
|
1.10 |
(0.50)a |
–2.66 |
–1.48 |
|
0.11 |
(0.07) |
–0.54a |
–0.42a |
|
0.34 |
(0.07)c |
–0.64a |
–0.28 |
|
0.10 |
(0.05) |
–0.25 |
–0.14 |
|
0.60 |
(0.18)c |
–1.38a |
–0.73 |
|
0.64 |
(0.22)b |
–1.28 |
–0.59 |
|
0.03 |
(0.14) |
–0.69 |
–0.66 |
|
0.00 |
(0.20) |
–0.16 |
–0.16 |
|
0.04 |
(0.30) |
0.68 |
0.73 |
|
0.18 |
0.19 |
–1.00 |
–0.80 |
|
0.15 |
(0.12) |
–0.46 |
–0.30 |
|
0.60 |
(0.08)c |
–0.96b |
–0.32 |
|
0.41 |
(0.17)a |
–1.99c |
–1.56b |
|
0.66 |
(0.18)c |
–1.41a |
–0.71 |
|
–0.10 |
(0.11) |
–0.35 |
–0.46 |
|
–0.11 |
(0.30) |
0.69 |
0.57 |
|
0.18 |
(0.12) |
–1.04a |
–0.86a |
|
1.13 |
0.85 |
–1.37 |
–0.16 |
|
–0.19 |
(0.37) |
0.37 |
0.16 |
|
0.88 |
(0.67) |
–1.27a |
–0.33 |
|
0.07 |
(0.02)b |
–0.22b |
–0.15a |
|
NOTES: Regressions of beds and services include percent county Medicaid, percent county Medicare, percent county HMO, Herfindahl index, ratio of uninsured Herfindahl index to total Herfindahl index, population density, CMS wage index, and dummies for years 1994 and 1996. Regressions of margin include percent county Medicaid, percent county Medicare, percent county HMO, percent hospitals in county for-profit, percent hospitals in county public, Herfindahl index, ratio of uninsured Herfindahl index to total Herfindahl index (the uninsured concentration), county population density, and dummies for years 1994, 1996, and 1999. |
|||
higher proportions of uninsured admissions and lower margins across the range of uninsured concentrations.
DISCUSSION
In this analysis of hospitals in rural counties, we find some evidence that in counties with higher proportions of uninsured patients and low concentration of these patients across hospitals, hospitals are less likely to offer psychiatric inpatient services. We also find some evidence that there are fewer psychiatric and ICU beds. There is a consistent association of higher uninsured admissions with a lower likelihood of hospitals offering high-technology services, although the association is statistically significant only for transplant, MRI, radiation therapy, and lithotripsy services. There is strong evidence that hospital margins are lower in counties with higher proportions of uninsured admissions.
The findings on beds and services for vulnerable populations generally parallel those in our analysis of metropolitan areas, although in this analysis we find fewer statistically significant associations with bed supply and services for vulnerable populations. Specifically, in the metropolitan analysis, we find statistically significant associations with psychiatric outpatient services, alcohol and chemical dependence services, and beds that we do not observe here.
Likewise, the findings on high technology services are similar, with most services in both samples displaying a negative association with uninsured admissions. However, for only a few services are the associations statistically significant and, with the exception of transplant services, the services for which the associations are statistically significant differ across the two samples.
One feature shared by several of the services for which we observe statistically significant associations with uninsured admissions—inpatient psychiatric services and transplant—is that they have the potential to bring into the hospital uninsured patients whose care may be expensive. The presence of higher numbers of uninsured in a market may discourage hospitals from offering services for fear that they will not be reimbursed for a significant portion of the care they provide.
For some of these services, a statistically significant association is only observed at low levels of concentration of the uninsured among the hospitals serving the county. The fact that we observe higher average rates of offering beds or services when care for the uninsured is more concentrated in counties may reflect strategic interactions among hospitals. This illustrates the variability among rural counties in their capacity to maintain hospital services and the impact of higher uninsured rates on hospitals in these counties. One limitation of this study is that it includes principally rural counties in the north and Pacific west. It should be replicated in a broader cross-section of rural hospitals, especially those in the south and southwest.
In sharp contrast to the findings in metropolitan areas, for rural counties and hospitals we find a consistent association of lower margins to higher uninsured admissions. This may reflect rural hospital administrators’ preference to maintain
services when faced with low (or even negative) margins. This strategy, while preserving a rural hospital’s ability to serve its community in the short-term, has implications for hospital’s ability to provide, maintain, and improve services in the future. Because of lower margins, rural hospitals in areas with high uninsured rates may have difficulty maintaining and replacing their physical plant, investing in new technologies, and expanding their scope of services to meet new community health needs. The lower margins may account in part for the lower likelihood of offering specific costly, high-technology services. Lower margins may also affect quality or staffing in ways that are not observable in this analysis.

































