H
Anticipating Unintended Consequences of Vaccine-Like Immunotherapies and Depot Medications for Addictive Drug Use
Robert J. MacCoun
University of California, Berkeley
Immunotherapy or depot medication (henceforth I/DM) programs that would prevent addiction or relapse to such drugs as tobacco or cocaine are largely unprecedented. These interventions differ in important respects from other pharmacological treatments for drug addiction and, for that matter, from vaccines used to prevent viral diseases. I/DMs may significantly alter the complex system of relationships among users, sellers, treatment providers, and social control agents. These actors are likely to change their behavior in both desirable and unintended ways.
Given the novelty of such interventions and uncertainty about how they might be implemented, it is not possible to forecast either the likelihood or the magnitude of unintended behavioral responses. Nevertheless, it is desirable to design I/DM interventions that might minimize such risks. This appendix identifies plausible mechanisms by which I/DMs might produce unintended consequences and reviews available evidence on the effects of these mechanisms in the research and clinical literatures on drug use and other risky behaviors. “Plausible” is defined here as something more than simply possible but not necessarily “more likely than not.”
Judgments about whether and how to implement I/DM programs should not necessarily be based solely on worst-case scenarios. Economists and risk analysts have long noted the opportunity costs in foregone benefits that can result from extreme risk aversion (e.g., Viscusi, 1992; cf.
Shrader-Frechette, 1991).1 But the literature on technological risks also documents the dangers posed by excessive optimism on the part of enthusiastic program designers (e.g., Janis, 1983; MacCoun, 1998a; Tenner, 1996; Vaughan, 1996). Thus, in the spirit of “devil’s advocacy,” it has been chosen in this appendix to err on the side of caution, giving greater attention to arguments in support of various unintended consequences than to possible counterarguments (which are nevertheless noted).
CONCEPTUAL FRAMEWORK
Program Prototypes
The committee has identified three types of immunotherapy or depot medication treatment protocols: overdose treatment, relapse prevention, and protection from addiction. Overdose treatment appears to be less susceptible than the other two categories to unintended consequences created by behavioral responses to the intervention, at least with respect to the mechanisms considered here. And to the extent that overdose treatment might operate via those mechanisms, its effects are likely to be similar to those of a relapse prevention program, only weaker. Thus, this appendix focuses primarily on relapse prevention and secondarily on the somewhat more remote prospect of addiction protection.
For simplicity the focus here is on interventions that target tobacco and cocaine use. Tobacco illustrates issues involved in pharmacological treatments for a legal, commercially available drug, and cocaine exemplifies issues posed for an illicit recreational drug.
Relevant Actors and Drug Use States
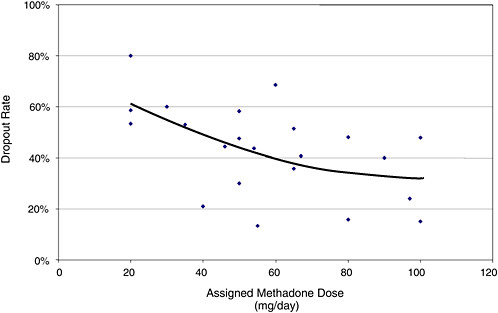
Psychoactive drug use is a multidimensional behavior characterized by many continuous parameters: age of onset, length of drug-use career, variety of drugs used, frequency of use, quantity consumed per use, and so on. To simplify the discussion, all this detail is abstracted away and drug use is characterized in terms of four mutually exclusive states. Figure H-1 presents a stochastic flow diagram, modified from a similar diagram used by Everingham and Rydell (1994). The figure depicts drug-using careers as patterns of movement among four “states”: never used, light use, heavy use, and former use. Among users, program participants are distinguished from nonparticipants and use of the target drug versus
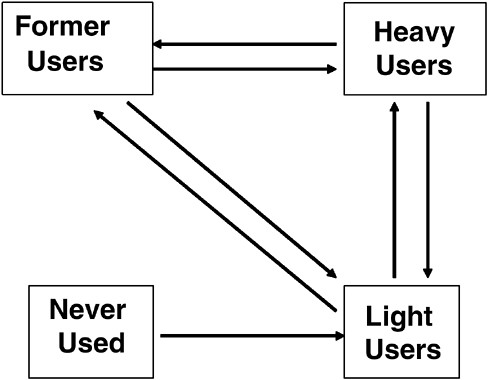
FIGURE H-1 Drug use conceptualized in terms of flows among four distinct drug use states.
use of other drugs. Behavioral effects on drug dealers, politicians, and the general public are also considered.
Presumably a relapse prevention program would target some fraction of heavy users. If effective, it should increase the flow of heavy users into nonuse and reduce the flow of nonusers back into use. An addiction protection program would target some fraction of light users and perhaps (not shown) newly heavy users and (more controversially) those at high risk who have never used. If effective, it should increase the flow of light users into nonuse and reduce the flow of nonusers into use.
In addition to these flows, it is important to consider the “stocks”—the distribution of individuals across these states. The distribution of consumption across users is strongly positively skewed for most drugs (see Everingham and Rydell, 1994; Skog, 1993)—though less dramatically so for tobacco than cocaine. As a result, the harmful consequences of substance use are not uniform but are disproportionately concentrated among the heaviest users.
The relative viability of targeting the median user versus hard-core users in the right tail of the distribution will probably vary as a function of several factors (Edwards et al., 1994; MacCoun, 1998b; Rose, 1992). Everything else being equal, it will be more effective to target typical users when the dose-response curve for various harms rises very quickly with small doses and when typical users account for a large fraction of total consumption. It will be more effective to target heavy users when the dose-response curve for various harms rises slowly at low doses and when the statistical distribution of consumption is heavily skewed. Relapse prevention I/DMs would disproportionately target right-tail users; addiction protection I/DMs would presumably include individuals from the whole range of the use distribution (even including some who would never use anyway), depending on their recruitment process and our accuracy at predicting who is “at risk” for addiction. But of course the choice of users to target for a pharmacological intervention will also be determined by legal, ethical, economic, and political considerations not considered in this chapter.
Voluntary Versus Mandated Participation
The consequences of an I/DM program are likely to differ depending on whether participation is solely voluntary versus mandated by legal or other authorities (e.g., employers). The voluntary-mandatory distinction hinges in part on the legal status of the drug in question. MacCoun and Reuter (2001) and MacCoun, Reuter, and Schelling (1996) examine the effects of a drug’s legal status on its prevalence and harmful consequences. Here a few key points of relevance to the comparison of pharmacological interventions for a licit drug (e.g., tobacco) versus an illicit drug (e.g., cocaine) are summarized.
-
Prohibition almost certainly raises the price of a prohibited substance, probably substantially (MacCoun and Reuter, 2001; National Research Council, 2001; cf. Miron, 2003). This is one reason why cocaine users might be more likely than tobacco users to commit income-generating crimes, even in the absense of any pharmacologically mediated disinhibition or aggression.
-
Prohibited drugs are marketed quite differently from licit drugs; there is less quality control and far greater violence. The lack of quality control may make it more difficult to determine appropriate pharmacological dosages for cocaine addicts than for tobacco addicts. And the nature of black markets creates a risk that pharmacological interventions for illicit drugs might have nonpharmacological effects on violence.
-
Prohibition increases the stigma associated with a drug, although stigma can have both desirable and undesirable consequences (see “Social Norm Effects” this appendix).
In addition to a drug’s legal status, a related consideration is whether participation in a pharmacological program would be voluntary or mandatory.2 Voluntary relapse prevention for either drug seems most feasible and would face few ethical and legal obstacles. For cocaine, mandatory participation would pose thorny ethical, legal, and political questions, but the drug’s illicit status makes such programs plausible (see National Research Council, 2001, Chapters 6 and 8 and Appendix E). On the other hand, mandatory participation in a relapse or addiction prevention seems implausible for tobacco, a licit drug.
Although the distinction between voluntary and mandatory programs has legal and political relevance, it may have less clinical and behavioral relevance. Many experts contend that mandatory treatment is as effective as voluntary treatment,3 and that conclusion seems even more plausible for these pharmacological interventions than for more traditional psychotherapeutic modalities. The behavioral mechanisms examined here seem as applicable to voluntary as to mandatory programs, given the severe self-control problems involved in drug addiction. Indeed, the very concept of “voluntariness” is problematic in the case of addictions, which are often characterized as “diseases of will” (see Elster and Skog, 1999; Vuchinich and Heather, 2003).
EFFECTS OF PRICE CHANGES
The first mechanism considered here involves the behavioral effects (on use and on criminality) of a change in drug prices brought about by I/DM programs.
Price Elasticity of Demand
Some readers may question the relevance of a drug’s price for the behavior of a consumer who is addicted. Traditionally, many have assumed that addicts, by the very nature of their addiction, are oblivious to price changes; they will obtain their drug no matter what the cost, committing income-generating crime if need be to finance their habit. Thus, it has been surprising to learn that illicit drug use is in fact fairly sensitive to price variations.
Economists estimate sensitivity to prices in terms of the price elasticity of demand—the percentage change in consumption for a 1 percent change in price. Estimates for the price elasticity of cigarette demand are in the −0.3 to −0.5 range (Chaloupka and Pacula, 2000; Manning et al., 1991), suggesting that a 10 percent increase in the price of cigarettes would reduce overall consumption by only 3 to 5 percent. Thus tobacco users are in fact somewhat but not completely unresponsive to price. Cocaine users are more price sensitive; low estimates are around −0.4, but some studies find elasticities of −1.0 or more (see reviews by Caulkins and Reuter, 1996, and Chaloupka and Pacula, 2000). A drawback is that most estimates are based on users in the household population and may overrepresent casual users. But Reuter and Kleiman (1986) argue that, if anything, budget constraints tend to make heavy users more rather than less price sensitive. And Caulkins (2001) has shown that trends in emergency room incidents involving cocaine are highly responsive to trends in cocaine price, suggesting that heavy users are also price sensitive.
Assumptions Underlying a Shift in Demand
The analysis of drug price effects presented here is premised on four “best-case” assumptions about the effectiveness of I/DM programs. Later mechanisms will challenge each of these assumptions; to the extent that these assumptions are false, any price effects will probably be smaller than those contemplated here. Specifically, assume that: (1) targeted users cooperate fully with the intervention program; (2) the intervention completely discourages use of the target by program participants; (3) participants do not substitute other psychoactive drugs; and (4) the program has no direct effect on the behavior of nonparticipants, and any indirect effects are benign. Under these conditions, a successful psychopharmacological relapse or addiction prevention program ought to shift the demand curve downward, such that less cocaine (or tobacco) is demanded at any price. The magnitude of the demand shift would be determined by the number of users targeted and their previous levels of consumption.
Effects Predicted by a Traditional Model of Supply and Demand
Figure H-2 presents a rudimentary “comparative statics” analysis of the implications of this shift in drug demand. In this type of micro-economic analysis, a product’s price and the quantity supplied are inferred from the equilibrium point where the supply curve (reflecting supplier responses) and the demand curve (reflecting consumer responses) intersect. Ceteris paribus, a downward shift in the demand curve ought to produce a reduction in the quantity supplied and a drop in the equilibrium price of the drug.4
In the short run, this reduced price should not in itself lead to increased use; by definition, the equilibrium price and quantity already reflect consumer and supplier preferences. But in the long run, reduced prices pose a risk of increased consumption, for two reasons. First, existing drug users may be more responsive to price changes over the long run than the short run (e.g., Reuter and Kleiman, 1986; Caulkins, 2001). Second, adolescents may be more likely to initiate use if they perceive the drug as inexpensive rather than expensive. This latter effect may be qualitative as well as quantitative; the reputation of a drug as “cheap” versus “expensive” can change over time. Compare cocaine’s reputation in the late 1970s versus the late 1980s.
On the other hand, a consequence of reduced cocaine demand is that any “psychopharmacological” criminality produced by the direct effects of the drug (Goldstein, 1985) should be reduced.5 Moreover, a price drop might reduce crime even among users not enrolled in an I/DM program. Presumably, some fraction of those nonparticipant cocaine users commit income-generating crimes to finance their use—what Goldstein calls “economic-compulsive” criminality. A reduction in price means that they might be expected to reduce their criminal involvement—a collateral benefit of a successful program. The effects of a price change on criminality, if any, will depend in part on whether the users who participate in I/DM programs differ from nonparticipants in their price sensitivity. If the two
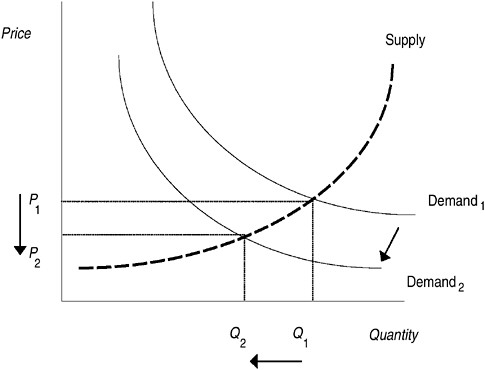
FIGURE H-2 Price and quantity decreases following a downward shift in demand, assuming a traditional supply curve.
NOTE: P1 = initial price, P2 = new price; Q1 = initial quantity supplied, Q2 = new quantity supplied.
classes of users differ, I/DM programs might alter the slope of the demand function by changing the composition of the remaining user pool.
Predicted Effects if the Supply Function Is Downward Sloping
The traditional analysis in Figure H-2 is plausible as a qualitative depiction of the tobacco market.6 But several experts (e.g., Kleiman, 1993;
Reuter and Kleiman, 1986; Reuter et al., 1988; Rydell and Everingham, 1994) argue that the illicit nature of the cocaine business might produce a supply curve that is downsloping, as seen in Figure H-3. This conclusion follows if the marginal cost of producing a kilogram of cocaine does not increase with the total number of kilograms produced and the per-unit risk of seizures and other enforcement actions falls with the total quantity of cocaine that is produced. The assumption of a downward sloping cocaine supply curve is controversial (see Caulkins, Chiesa, and Everingham, 2000; National Research Council, 1999) but is important to consider because it has implications for the effect of a downward shift in the demand curve.
Figure H-3 indicates that with a downsloping supply curve a downward shift in the demand curve would still produce a reduction in the quantity supplied, but prices would actually rise. This is obviously a desirable effect if users not receiving an I/DM intervention are price sensitive because they can be expected to reduce their consumption even though they are not in the program. Moreover, the higher prices should discourage potential users from initiating drug use.
On the other hand, if those still using cocaine are relatively price insensitive, they might increase their rate of income-generating crime to
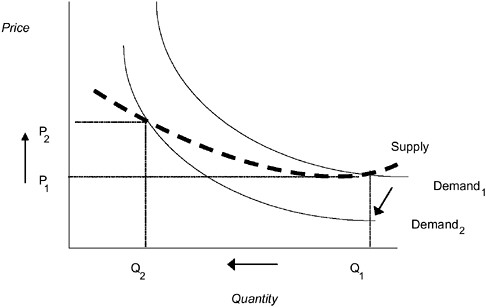
FIGURE H-3 Price increase and quantity decrease following a downward shift in demand, assuming a downsloping supply curve
NOTE: P1 = initial price, P2 = new price; Q1 = initial quantity supplied, Q2 = new quantity supplied.
maintain their preferred level of consumption—clearly an unintended consequence of the program. This effect would be mitigated to the extent that those users targeted for the program were the ones most heavily involved in criminal activity—as might occur through a court-mandated program.
This discussion of price and criminality effects suggests the importance of additional empirical research on users’ responsiveness to price changes. To accurately predict the consequences of an I/DM intervention on drug markets, better information is needed on short- versus long-run price elasticities and on differences in the price sensitivity of likely participants versus other users.
NONPARTICIPATION AND NONCOMPLIANCE
The analysis of price effects presented above was premised on the best-case assumption that I/DM programs produce their intended shift in demand. The remaining mechanisms considered here each challenge that assumption. The simplest and least speculative challenge to the best-case scenario is the likelihood that some nontrivial fraction of targeted users will fail to participate.
It may be difficult to enroll targeted participants at high rates and sustain their participation for the desired length of time. In the Drug Abuse Treatment Outcome Study, a nationwide naturalistic examination of nonexperimental treatment settings, median retention in treatment ranged from 29 to 177 days across 18 long-term residential programs and from 42 to 144 days for 16 outpatient drug-free programs (Joe, Simpson, and Broome, 1998). Methadone clinics fared somewhat better, with a median of 117 to 583 days across 13 programs; across these programs, half of all clients participated for at least a year. But an examination of the evidence from a variety of at least partially analogous interventions suggests that high dropout rates are the norm.7
Evidence from Partially Analogous Programs
Smoking Cessation Programs
The smoking cessation evaluation literature has largely ignored the question of program attrition. For example, dropout rates are not ana-
lyzed in many major metanalyses of this literature (e.g., Cepeda-Benito, 1993; Viswesvaran and Schmidt, 1992). In a recent methodological analysis of seven carefully controlled clinical trials (Shadish et al., 1998), the dropout rate ranged from 0 to 30 percent, with a mean of 13 percent But Borrelli et al. (2002, p. 23) suggest that “proactive recruitment and population-based studies demonstrate no-show rates approaching 50 percent.”
Pharmacological Treatment of Cocaine Dependence
Table H-1 summarizes data from 45 clinical trial arms on the effects of 15 different pharmacological interventions for cocaine dependence, computed from data presented in a recent metanalysis by Silva de Lima et al. (2002). Discouragingly, no significant effects from any of these interventions were found. But the participation rates were also discouraging, with dropout rates ranging from 15 to 79 percent, with an overall rate of 48 percent; the same rate was observed across placebo conditions. High attrition rates are also common in psychosocial cocaine treatments (Gottheil, Sterling, and Weinstein, 1995; Siqueland et al., 1998; Van Horn and Frank, 1998; White, Winn, and Young, 1998).
TABLE H-1 Dropout Rates in Pharmacological Treatment Trials for Cocaine Dependence
|
|
|
Active Drug Condition |
Placebo Condition |
|
||||
|
Active Drug |
No. of Studies |
Dropouts |
N |
Rate (%) |
Dropouts |
N |
Rate (%) |
Relative Risk |
|
Bupropion |
1 |
11 |
74 |
15 |
13 |
75 |
17 |
0.86 |
|
Desipramine |
8 |
72 |
185 |
39 |
39 |
136 |
29 |
1.36 |
|
Fluoxetine |
1 |
8 |
16 |
50 |
15 |
16 |
94 |
0.53 |
|
Gepirone |
1 |
9 |
20 |
45 |
11 |
21 |
52 |
0.86 |
|
Imipramine |
1 |
24 |
59 |
41 |
27 |
54 |
50 |
0.81 |
|
Ritanserin |
1 |
11 |
40 |
28 |
13 |
40 |
33 |
0.85 |
|
Amantadine |
6 |
68 |
144 |
47 |
55 |
140 |
39 |
1.20 |
|
Bromocriptine |
3 |
32 |
70 |
46 |
31 |
72 |
43 |
1.06 |
|
Pergolide |
1 |
111 |
156 |
71 |
89 |
153 |
58 |
1.22 |
|
Carbamzaepine |
4 |
92 |
152 |
61 |
110 |
161 |
68 |
0.89 |
|
Disulfiram |
2 |
14 |
47 |
30 |
6 |
40 |
15 |
1.99 |
|
Mazindol |
2 |
10 |
40 |
25 |
12 |
40 |
30 |
0.83 |
|
Naltrexone |
1 |
18 |
24 |
75 |
15 |
22 |
68 |
1.10 |
|
Phenytoin |
1 |
23 |
29 |
79 |
25 |
31 |
81 |
0.98 |
|
Risperidone |
1 |
23 |
30 |
77 |
42 |
45 |
93 |
0.82 |
|
TOTAL |
|
526 |
1,086 |
48 |
503 |
1,046 |
48 |
1.01 |
|
SOURCE: Adapted from Silva de Lima et al. (2002). |
||||||||
Methadone Maintenance
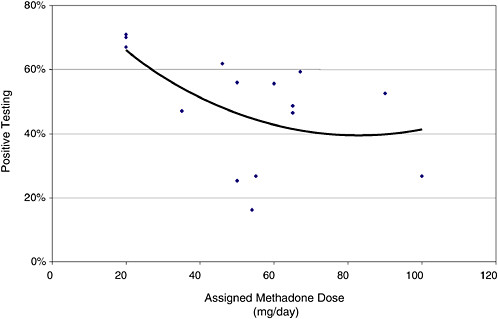
One might hope participation rates would be higher for a more effective pharmacological intervention. But dropout rates computed from data on 22 controlled methadone maintenance trials (reported in Farré et al., 2002) range from 13 to 80 percent, with a mean of 43 percent and a median of 46 percent. As might be expected, dropout rates are lower in programs with higher daily methadone doses (see Figure H-4), but even at the highest studied doses (100 mg/day), one-quarter of participants dropped out. (Participants receiving a placebo or another treatment are excluded from this analysis.)
Drug Court Graduation Rates
One might also assume that participation rates might be higher in mandatory, court-administered programs, where clients face possible criminal sanctions for noncompliance. But the drug court literature suggests that as many as half of assigned participants fail to “graduate” (averaging 47 percent in studies reviewed by Belenko, 2001). This low rate may seem to contradict the notion of a “mandatory” program, but Belenko (1998, p. 25) notes that in a recent Department of Justice survey “only 25 percent of probationers reported that they were required to undergo drug testing” and “one quarter of felony probationers had had no contact of any type with their probation officer during the past month.”8
Disease Vaccine Programs
Finally, nonparticipation is a serious problem in vaccination programs for many serious diseases (Szilagyi et al., 2000). For example, Carter, Beach, and Inui (1986) found that only one-quarter to one-third of high-risk patients who were actively urged to get influenza shots actually did so. Moore-Caldwell et al. (1997) report that compliance with a hepatitis B vaccine series was reduced because “most teens perceived their risk of acquiring hepatitis B infection as slight or none,” yet Lawrence and Goldstein (1995) report that the hepatitis B immunization has been hampered by the inability of medical providers to identify high-risk individuals. On the other hand, in a recent intervention targeting over a thousand heroin addicts in Italy, 88 percent completed a full hepatitis B vaccine series (Quaglio et al., 2002). So high compliance is possible even in heavy drug-using populations.
Conclusion
Neither a voluntary nor a compulsory vaccination program can be expected to achieve high rates of compliance without aggressive recruitment and follow-up. Among a variety of roughly comparable interventions each routinely loses about one-half of its clients. Perhaps if I/DM programs were perceived to be less onerous (or more efficacious) than traditional substance abuse treatments, they might fare better—but not necessarily. High treatment dropout rates probably have less to do with treatment management than with the inherent difficulty of changing addictive behaviors (De Leon, 1998; Joe et al., 1998). Most addiction treatment clients are at best ambivalent about the prospect of total abstinence, and for that reason these interventions may be both encouraging and somewhat threatening. Indeed, addicts at risk of coerced treatment may even volunteer for traditional psychosocial programs to avoid participating in pharmacological programs.
Program designers will have to attend to a variety of factors that might increase participation:
-
confronting fear and distrust of a novel and intrusive medical technology that has both medical and social control objectives,
-
minimizing logistical barriers to participation (location, hours, etc.),
-
carefully crafted persuasive appeals and outreach for voluntary programs, and
-
monitoring and clear sanctioning of court-mandated clients (see Kleiman, 1997a, 1997b).
INCREASED CONSUMPTION TO “SWAMP” THE TREATMENT
The previous section examined incomplete participation—an across-client effect. This section considers the effects of an only partially effective intervention—a within-client effect. Thus, rather than (or in addition to) only a fraction of targeted people participating, this section considers what would happen if participating clients experience no reduction, or only a partial reduction, in drug craving and/or participating clients are able to produce the same subjective drug effects by significantly increasing their consumption (frequency and/or quantity)—in essence, “swamping” the treatment.9
The results of such a scenario are potentially quite serious. The down-
ward shift in the demand curve plotted in Figure H-2 might not be expected. Users who maintain their previous level of consumption will experience fewer drug effects. From a clinical perspective this may produce a significant improvement in functioning, but from a market perspective there may be no observable behavioral change. This is particularly troubling for an illicit drug like cocaine because many of the harms associated with illicit drug use are primarily attributable to illicit markets rather than the effects of the drug per se (MacCoun et al., 1996; MacCoun and Reuter, 2001). Worse yet, participating users might simply increase their consumption of their drug of dependency in an attempt to achieve the same subjective effects. To the extent that this happened it would reduce the magnitude of reduction in demand and in theory could even produce a net increase in demand.
Although the analogies are not perfect, experiences with existing pharmacological treatments for addiction are not comforting. Positive urine tests for illicit opiates are found in methadone maintenance clinical trials in anywhere from 16 to 71 percent of the clients, with a median rate of 53 percent (Farre et al., 2002). Figure H-4 plots the results of 15 such trials as a function of experimentally assigned methadone dose. As might be expected, illicit opiate use declines with increasing maintenance dose, but even at the highest observed dose, 100 mg per day, over one-fourth of all clients continued using street opiates. Similarly, clinical trials for pharmacological treatment of tobacco dependence—bupropion SR and nicotine gums, inhalers, nasal sprays, and patches—routinely find that a majority of clients continue smoking (see Fiore et al., 1994; Fiore et al., 2000).
Of course, studies of these interventions provide no indication that users actually increase their consumption. And the immunotherapies and depot medications under consideration here surely differ from other interventions in important ways. But some of the differences could make the picture less encouraging rather than more.
A key consideration is the extent to which these interventions reduce the motivation to use the targeted drug, rather than (or in addition to) simply blocking the physical and/or subjective effects of the drug. Methadone and nicotine treatments do so, but the proposed I/DM interventions do not, at least not directly. They do not provide a substitute or maintainence substance, nor do they directly alter the brain mechanisms thought to be responsible for cravings and/or withdrawal.
Still, Pentel (this volume) suggests that “the hope in using this strategy is to reduce the rewarding effects of the drug that lead to and sustain addiction. For example, a cocaine addict who is vaccinated and then takes a puff of crack cocaine would feel little effect and therefore have little reason to continue using it.” One way to characterize this argument is in terms of what behavior analysts call “extinction.” In classical conditioning, extinction occurs when a conditioned stimulus is no longer paired
with unconditioned stimuli. In operant conditioning, extinction occurs when a learned behavior no longer receives a positive reinforcement. Treatments that prevent an addictive drug from crossing the blood-brain barrier are likely to produce both types of extinction.10
Extinction can produce lasting behavioral changes, but it has other predictable consequences as well (Azrin, Hutchinson, and Hake, 1966; Neuringer, Kornell, and Olufs, 2001; Skinner, 1953; Sulzer-Azaroff and Mayer, 1977):
-
The target behavior does not cease immediately; responding may temporarily increase in frequency and variability.
-
Occasional repairing behavior and the reinforcer change the extinction noncontingency to an intermittent schedule of reinforcement, which can encourage persistent responding.
-
During extinction, conditioned associations are not unlearned so much as they are “forgotten,” or put into competition with newly learned alternative contingencies, which means that even in the absense of further reinforcement the response can “spontaneously recover” (Bouton, 1994).
-
Increased responding may be accompanied by aggressive behavior—the so-called vending machine phenomenon (Sulzer-Azaroff and Mayer, 1977).
-
Ceteris paribus, extinction produces a net reduction in positive reinforcement, which if not replaced by substitute rewards can produce lethargy, apathy, and depression.
Moreover, a traditional extinction account may fail to capture important subtleties of addictive drug use. Both classical conditioning and operant conditioning have long been implicated in drug addiction, but they do not account for many aspects of the phenomenon (Robinson and Berridge, 2003). There is increasing evidence that chronic drug use can produce enduring changes in the brain’s sensitivity to drug-related cues, producing a heightened motivational state that may persist long after drug use has been stopped (see Gardner and David, 1999; Robinson and Berridge, 2003).11 Gardner and David (1999, p. 117) suggest that “strong
and persistent drug craving may outlast drug detoxification and withdrawal by months or years.”
Thus, there are reasons to be concerned that these new interventions will fail to fully block drug taking. Users may attempt to “swamp” the treatment by increasing their consumption. These effects may be temporary, but they could be extremely serious. For example, the immunotherapeutic effects are expected to dissipate between treatments (Pentel, this volume). If so, the effects of a given dose of the targeted drug will vary over time; a dose that produces no response or a mild response soon after a treatment may produce a very large response if attempted some weeks later. It seems unlikely that users will be able to accurately anticipate such effects and titrate their doses accordingly. Thus, users who attempt to overcome the I/DM blocking effect will be at serious risk of extreme psychiatric reactions, cardiac failure, respiratory failure, or other reactions to toxicity.
Consider also the implications if the user’s previous consumption level was already at the outer limits of what he or she could afford. (This is more plausible for cocaine than tobacco.) If so, efforts to swamp the treatment with high doses could motivate increased income-generating “economic compulsive” criminal behavior.
For all these reasons, it is crucial to use monitoring and counseling to discourage users from attempting to swamp the treatment by increasing their consumption. I/DM treatments should not be viewed as a cure for addiction but rather a prolonged respite from it—an opportunity for the addict to regain control of his or her life and invest in a repertoire of alternative activities.
Later in this chapter, another mechanism is identified that might produce heightened risky behavior in response to a vaccine (Blower and McLean, 1994). The mechanism there is somewhat different, involving compensatory responses to perceived risk reduction.
DRUG SUBSTITUTION
Another major concern is whether a pharmacological relapse prevention or addiction protection program would inadvertently motivate participants to increase their use of other drugs—a substitution effect. Note that the substitute drug may have either more or less harmful physical and behavioral effects than the targeted drug.
Psychopharmacological researchers often study drug substitution using a drug discrimination paradigm (Kamien et al., 1993), which is useful for studying agonist and antogonist mechanisms. But while a client in a cocaine relapse prevention program may substitute another drug based on its similar pharmacological properties, the choice might be influenced
as much or more by situational factors—availability, price, peer use, etc. Moreover, the closer two drugs are in pharmacology, the more likely it is that I/DM treatments may at least partially block the effects of the substitute (Pentel, this volume). Thus, it is worthwhile to construe the notion of a “substitute” more broadly rather than in the drug discrimination tradition.
Economists have a purely behavioral way of operationalizing substitutes and complements that has been adapted by the behavioral economic research community in psychology (e.g., Petry and Bickel, 1998). Two goods are considered substitutes if an increase in the price of the first good leads to an increase in demand for the second good—a positive cross-price elasticity. Two goods are considered complements if an increase in the price of the first good leads to a decrease in demand for both goods—negative price and cross-price elasticities.
One might reasonably ask whether evidence on cross-price elasticities is relevant for understanding I/DM effects. Is an increase in the preferred drug’s price analogous to decreases in the preferred drug’s effects on the brain? Several arguments suggest the answer is probably yes. First, laboratory experiments have established that manipulations of effort, price, available income, and reinforcement magnitude have roughly equivalent effects on the rates of drug consumption (e.g., DeGrandpre and Bickel, 1995). Second, some of the econometric studies of substitution operationalize “price” using proxies like drug enforcement risk, marijuana eradication, and variations in state drinking ages, all of which involve reduced availability to the consumer.
In econometric studies, substitution and complementarity can be estimated in situ, capturing actual behavior outside the laboratory, though the relevant data are often sparse and poor, and there are serious concerns about endogeneity and spurious correlation (National Research Council, 2001). Bickel and colleagues (DeGrandpre and Bickel, 1995; Petry and Bickel, 1998) have developed a laboratory paradigm that avoids these problems by manipulating prices in a simulated market, but their participants, though experienced addicts, are nevertheless “behaving” in an artificial setting that may distort their choices. Because there are inevitable tradeoffs between experimental control and realism, both approaches seem necessary (see Mook, 1983).
Relevant Evidence
Marijuana-Alcohol Link
The most studied linkage has been between marijuana and alcohol—a relationship that has little bearing for the interventions examined here.
Still, the literature illustrates the methodological challenges to correctly estimating the relationship. Some studies find a substitution relationship between marijuana and alcohol use (Chaloupka and Laixuthai, 1994; DiNardo and Lemieux, 1992), while others suggest the relationship is complementary (Pacula, 1998; Williams, Pacula, and Chaloupka, 2001). Chaloupka and Pacula (2000, p. 105) argue that “The mixed evidence with respect to alcohol and marijuana can be attributed to differences in the level of aggregation of the data as well as to differences in the populations being studied. When individual-level data are employed, and demand equations for marijuana can also be estimated, the findings are generally supportive of the complementary relationship between alcohol and marijuana. Until good measures of the money price of marijuana are obtained, however, this cannot be known with certainty.”
Marijuana-Tobacco Link
Econometric studies of the relationship between marijuana and cigarette consumption suggest a complementary relationship (Cameron and Williams, 2001; Chaloupka et al., 1999; Farrelly et al., 1999; Pacula, 1998). If so, this implies that a successful pharmacological tobacco intervention ought to bring about some reduction in marijuana use.
Alcohol-Tobacco Link
The evidence on the alcohol-tobacco relationship is similarly ambiguous. Cameron and Williams et al. (2001) found an inverse association between the price of cigarettes and alcohol consumption, while alcohol prices are positively but insignificantly associated with cigarette consumption. Decker and Schwartz (2000) found that increases in the price of cigarettes are associated with increases in the prevalence of drinking and the amount consumed by drinkers.
Marijuana-Hard Drug Link
Model’s (1993) analysis of Drug Abuse Warning Network emergency room data for the years 1975 to 1978 found higher rates of marijuana incidents and lower rates of hard drug incidents in states that had depenalized marijuana. Model interpreted this as evidence for a substitution effect, in which users shifted from harder drugs to marijuana after its legal risks decreased. A laboratory study of hypothetical drug purchase choices by heroin addicts also suggests that marijuana and heroin are substitutes (Petry and Bickel, 1998). On the other hand, Saffer and Chaloupka (1995) found that marijuana had a complementary relationship with cocaine and
heroin, but their data source (the National Household Survey on Drug Abuse) captures only a small and possibly unrepresentative fraction of cocaine and heroin users. The methodological differences across these studies are so great that the contradictory findings are difficult to resolve without more research.
Relationships Among Hard Drugs
It appears that only one econometric study has examined the cross-price elasticities between hard drugs, finding that cocaine and heroin were complements rather than substitutes (Saffer and Chaloupka, 1995). Again, the household sample may be quite unrepresentative of hard drug users. Petry and Bickel’s (1998) simulation experiments using heroin addicts suggest that valium and cocaine substituted for heroin; mock “purchases” of these drugs rose with simulated rises in heroin prices. Heroin purchases were unresponsive to rises in the price of valium. Unfortunately for our purposes, cocaine prices were not manipulated. Despite the obvious limitations of the simulation (no legal risks, no actual consumption), a conceptual replication of this paradigm using cocaine addicts and manipulated cocaine prices might provide valuable insights into possible substitutes for cocaine.
In addition to these economic studies, there are large clinical literatures on cocaine-alcohol (Pennings, Leccese, and de Wolff, 2002) and cocaine-heroine (Leri, Bruneau, and Stewart, 2003) poly-drug use. Popular lore suggests that a cocaine-heroin mix (a speedball) has particularly attractive effects for addicts, which would suggest complementarity, but Leri et al. (2003, p. 7) argue that “clinical and preclinical experimental evidence indicates that the simultaneous administration … does not induce a novel set of subjective effects, nor is it more reinforcing than either drug alone.”
Effects of Methadone Maintenance on Use of Other Drugs
Methadone maintenance provides a partial analogy to the pharmacological treatments at issue here. Methadone itself is a substitute for heroin in the empirical sense that it is inversely related to heroin use among former heroin users. Though methadone at adequate doses significantly reduces heroin use (e.g., Farre et al., 2002) (see Figure H-5), use of other street drugs is common among methadone clients (Leri et al., 2003; Preston et al., 1998). For example, one study reported that “more than half of the sample tested positive at least once for opiates (61 percent) other than methadone, almost half tested positive for cocaine (48 percent), almost half tested positive for benzodiazepines (46 percent), and more than three
quarters tested positive for cannabis (78 percent)” (Nirenberg, Cellucci, Liepman, Swift, and Sirota, 1996, p. 225).
Naturally, there is a concern that use of these other drugs reflects a substitution effect of the methadone maintenance regimen. Clients do not appear to be substituting cocaine for heroin. Longitudinal studies suggest that many clients were already using cocaine prior to starting methadone and that participation in the maintenance program is associated with a decline in cocaine use (see Dunteman, Condelli, and Fairbank, 1992; Fairbank, Dunteman, and Condelli, 1993; Shaffer and LaSalvia, 1992; but see Compton et al., 1995, p. 109). Indeed, Kidorf and Stitzer (1993) were able to reduce cocaine use among clients by making methadone contingent on cocaine-free urine for 7 weeks (see also Caulkins and Satel, 1999).
Cigarette smoking is also common among methadone clients (Frosch et al., 2000), but experimental manipulations of methadone dose levels have produced inconsistent effects on smoking levels (Schmitz, Grabowski, and Rhoades, 1994; Stark and Campbell, 1993). On the other hand, buprenorphine maintenance appears to increase tobacco consumption, at least among concurrent opiate and cocaine users (Mutschler et al., 2002).
Conclusion
At present, the only substitution effect that can be predicted with any confidence for a tobacco relapse prevention or addiction prevention intervention involves food, as weight gain is a common consequence of smoking cessation (Cabanac and Frankham, 2002). Tobacco appears to have a complementary relationship with marijuana, but there is evidence for both complementarity and substitution between tobacco and alcohol. For cocaine cessation there is mixed evidence for a possible substitution effect involving marijuana and simply too little evidence to predict effects on the consumption of amphetamines, opiates, or alcohol. Pharmacologically, the use of stimulants seems plausible, but again, social and economic factors may be more determinative (price, availability, peer use).
It is apparent that additional research on drug substitution effects in natural, clinical, and experimental settings ought to be considered a high priority for the addiction research community. In the meantime, in the face of such scanty evidence, a conservative assumption would be that some sort of substitution is a plausible response to these interventions. Use of other drugs should be closely monitored, and appropriate preventive counseling should be provided.
COMPENSATORY RESPONSES TO RISK REDUCTION
Unlike the previously discussed mechanism, the remaining mechanisms suggest unintended effects on drug use by those not receiving I/DM treatment.
Risk analysts have learned that technological risk reduction often has the unintended consequence of increasing the prevalence and/or intensity of that behavior. According to MacCoun and Reuter (2001, p. 392):
When technological innovations successfully reduce the probability of harm given unsafe conduct, they make that conduct less risky. And if the perceived risks were motivating actors to behave somewhat self-protectively, a reduction in risk should lead them to take fewer precautions than before, raising the probability of their unsafe conduct to a higher level. This notion has been variously labeled compensatory behavior, risk compensation, offsetting behavior, or in its most extreme form, risk homeostasis—a term that implies efforts to maintain a constant level of risk (Wilde, 1982).
Compensatory behavioral responses to risk reduction are now well established in a number of risk domains (see reviews in MacCoun, 1998b; Institute of Medicine, 2001). For example, people drive faster and more recklessly in cars with seat belts and air bags (Chirinko and Harper, 1993; Stetzer and Hofman, 1996). Similarly, smokers compensate for filters and low-tar tobacco by smoking more cigarettes, inhaling more deeply, or blocking the filter vents (Hughes, 1995; Institute of Medicine, 2001). In both domains, some of the safety gains brought about by a reduction in the probability of harm given unsafe conduct have been offset by increases in the probability of that conduct.
The total harm produced by a risky activity (e.g., addictive drug use) is a function of the average harm per incident, multiplied by the total amount of the activity (MacCoun, 1998b; MacCoun and Reuter, 2001). In theory, if a technological innovation reduces but does not eliminate the riskiness of an activity, and if the risk reduction motivates sufficiently large increases in the frequency or quantity of that activity, then average harm might fall, but total harm might increase.
In many settings, technological risk reduction provides little evidence that behavioral responses produce net increases in harm or even the constant level of harm predicted by Wilde’s (1982) “homeostatic” version of the theory. Rather, such effects are sufficiently small relative to the benefits of the intervention they reduce but do not eliminate the gains in safety (Institute of Medicine, 2001; MacCoun, 1998a).
But there are some important cautionary tales. For example, in 1994, Blower and McLean published epidemiological simulations suggesting
that an HIV vaccine, unless perfectly prophylactic, could actually exacerbate the San Francisco AIDS epidemic. This would occur if individuals behaved less cautiously in response to their increased sense of safety.
In the decade that has followed, it has become increasingly clear that a similar scenario is playing out in response to highly active antiretroviral therapy (HAART; see Blower, 2001; Katz et al., 2002; Ostrow et al., 2002; Stolte, Dukers, de Wit, Fennema, and Coutinho, 2002). Katz et al. report that the percentage of San Francisco men who have reported unprotected anal sex increased from 24 to 45 percent between 1994 and 1999. The authors present correlational and anecdotal evidence linking this increase in risky sex to reduced fears of HIV since the advent of HAART. Survey results reported by Ostrow et al. (2002) also show a correlation between unsafe sex and perceptions that HAART reduces the harmful consequences of HIV infection.
Immunotherapies or depot medications for drug dependence are potentially vulnerable to compensatory behavioral responses. The decision to take risks is influenced by the expected outcome of an activity but also by perceived worst-case scenarios (March and Shapira, 1992; Slovic, Fischhoff, and Lichtenstein, 1979). Thus, the perceived risk of becoming addicted is an important predictor of the decision to initiate and/or escalate recreational drug use (e.g., Benthin, Slovic, and Severson, 1993; Goldberg and Fischhoff, 2000). As such, this risk is a major focus of the curriculum of primary drug prevention activities (National Research Council, 2001). An effective and accessible I/DM program may actually reduce the perceived risk of addiction.
Compensatory responses to I/DM might well be larger than those observed in studies of seat belts, needle exchanges, and other interventions. The reason is perceptual: Those other interventions are at best seen as ways to reduce the relevant risks at the margin. But the existence of an I/DM program for relapse prevention or addiction protection, if widely publicized, may convey—rightly or wrongly—a widespread belief that “addiction has been cured” (see MacCoun, 2003). Psychologically, the perceived elimination of a small risk has a much larger impact than perceived reductions of equivalent magnitude elsewhere in the risk distribution (Kahneman and Tversky, 1984). If so, current users who are not enrolled in a pharmacological program may increase their consumption. And current nonusers may, at the margin, be more willing to begin using the addictive substance.
The magnitude of such effects is unknown. There is no a priori reason to believe that such effects would be so large as to offset the benefits of reducing drug use among participants. But program designers should anticipate the possibility that an I/DM program might inadvertently encourage nonaddicts to risk becoming addicts.
SOCIAL NORM EFFECTS
Another way that I/DM programs might influence drug use by non-program participants is by altering networks of social influence. One such effect is beneficial. A reduction in use by light users could have “social multiplier” effects on nonusers and current light users (see Caulkins et al., 1999). This follows under the assumption that current users socially reinforce, encourage, and facilitate use among those around them. There is much correlational evidence for this assumption, at least among adolescents (e.g., Elliott, Huizinga, and Ageton, 1985), although the correlation conflates a social influence effect with a selection effect, since high-risk peers tend to select each other as friends (Bauman and Ennett, 1996; Kandel, 1996).
But it is possible that this social influence effect would be inverted in the case of hard-core dependent users.12 Musto (1971/1987) and Johnston (1991) each offer versions of a “generational forgetting” model of drug epidemics, in which the increasing visibility of the deleterious effects of addiction triggers a reduction in initiation.13 Behrens and colleagues (1999, 2000, 2002) have incorporated this process into Everingham and Rydell’s (1994) model of the cocaine epidemic. Their analyses led to the disturbing prediction that if Musto and Johnston are correct, widespread drug treatment early in an epidemic could actually exacerbate it by slowing the social learning process. Similarly, if the generational forgetting model is correct, then ceteris paribus, reducing the visibility of the harms of addiction might reduce a social deterrent to drug use. This prediction is admittedly speculative. The generational forgetting model remains largely untested; there are simply too few “cycles” of data to test the cyclicity of drug epidemics. Still, this line of reasoning bolsters the concern that I/ DMs might well encourage drug use by reducing the perceived risks.
UNINTENDED EFFECTS ON DRUG MARKETING
Putting aside the unintended consequences discussed thus far, assume again for the sake of argument that a successful pharmacological intervention is widely implemented and reduces the prevalence and
severity of tobacco or cocaine addiction. This would almost certainly threaten the profitability of tobacco or cocaine production and sales. Producers and sellers, whether licit or illicit, may well respond in a compensatory fashion.
Illicit Drug Sellers
Sellers of cocaine or other targeted street drugs may respond in various ways. Drug sellers might move into the production and/or sales of other psychoactive drugs (e.g., Constantine, 1995; Thompson, 2002) or develop new synthetics that mimic the targeted drug without being blocked by I/DM pharmacologies. At least in the short run, dealers may act more aggressively to protect and expand their share of the diminishing market. There might be (at least temporarily) an upsurge in violence as sellers compete for a shrinking pool of addicts. Drug-selling organizations might also attempt to expand into regions where the relevant I/DM interventions are less available or less widely used. It has long been rumored that urban cocaine-trafficking organizations expanded into rural areas as urban drug enforcement became more aggressive in the 1990s (Butterfield, 2002; Johnson, 2003; National Alliance of Gang Investigators Associations, 2000; cf. Maxson, 1998).
The Tobacco Industry
If I/DM interventions against tobacco addiction were to become popular, the tobacco industry might also seek new users who are not currently targeted for these interventions (e.g., young people, rural communities, other nations) and seek to establish or strengthen these alternative markets. For example, as U.S. tobacco consumption has declined, tobacco companies have become more aggressive in international markets, especially in developing nations (World Health Organization, 2001). There might be new forms of advertising, perhaps subtly hinting that tobacco addiction is now a more manageable risk of their product.
The Pharmaceutical Industry
For manufacturers of immunotherapeuties or depot medications, the largest market will involve addiction protection rather than relapse prevention simply because the population of potential clients is so much larger. There are many more potential addicts than actual addicts, especially if “at risk” is defined broadly. (This is especially likely to be true for the tobacco market, which is roughly an order of magnitude larger than
the market for illicit drugs other than marijuana.14) Many parents may feel a moral (or perhaps social) obligation to protect their children against the risk of future addiction. The industry might market the treatments in a manner that reinforces or amplifies this sense of responsibility.
Much may depend on the decision by public and private health insurance providers about whether to reimburse I/DM addiction protection and by any professional guidelines for off-label use established by professional medical societies (e.g., the American Medical Association). Broad coverage of youth addiction protection is likely to be socially inefficient. If parents and physicians define “addiction risk” too broadly, there will be a “moral hazard” problem of excessive utilization of the intervention. On the other hand, if insurers set strict limits on coverage (ex ante), they may face lawsuits if some youth who were denied coverage later became addicted.
UNINTENDED SOCIAL AND POLITICAL CONSEQUENCES
Again, assuming that a pharmacological intervention is widely implemented and is at least perceived to be successful in reducing addiction, other actors might also respond in unintended ways:
-
Nonusers may further stigmatize or ostracize smokers and drug users who have not availed themselves of a pharmacological relapse intervention. While this stigma may help to discourage initiation and escalation by casual users, the labeling theory tradition in sociology suggests that it could actually intensify the drug involvement of heavy users (MacCoun, 1993).
-
Law enforcement officials may demote cocaine offenses as an enforcement priority, increasingly viewing cocaine as a medical problem rather than a social control problem. This would be particularly troubling if these officials overestimated the actual “capture” or effectiveness rates of the pharmacological intervention.
-
Politicians and the general public may be less willing to actively support more traditional forms of treatment, primary prevention, and law enforcement. This would be particularly troubling if in fact a large fraction of existing users were ineligible for such a pharmacological intervention. Also, a reduction in support could have pernicious effects on substance abuse control efforts involving drugs for which no pharmacological intervention is available.
|
14 |
According to the National Household Survey on Drug Abuse, in 2001 there were 7 million current users of illicit drugs other than marijuana versus 66.5 million current users of a tobacco product. See http://www.samhsa.gov/oas/nhsda.htm#NHSDAinfo. |
-
There may be a political backlash against the coercive use (by legal authorities or parents) of this invasive technology. This seems particularly likely if mandated clients are disproportionately drawn from ethnic and racial minority groups, which is not implausible given the disproportionately high rates at which those groups are apprehended for drug use (MacCoun and Reuter, 2001).
CONCLUSIONS
This appendix raises a number of potential unintended consequences of a depot medication or immunotherapy program for addiction, including increased use of the target drug by some program clients (if the treatment is only partially effective and fails to reduce drug motivation, increased use of other drugs by program clients (a substitution effect), increased use of the target drug by those not in the program (through reductions in the perceived riskiness of the drug, and increased dealer violence (through increased competition for fewer customers and/or effects of the program on prices). There is little basis for estimating the likelihood of these potential outcomes other than to suggest that their probabilities are nontrivial (i.e., below 1.0 but closer to 0.50 than to 0).
Of course, these effects are not the only factors to consider when evaluating such a program. Even if all these consequences occurred, they may well be completely offset by the program’s benefits. A full analysis of the desirability of an I/DM program should consider other factors assessed elsewhere in this volume, including the ethical obligation to treat drug dependence if possible; the ethical, legal, and political objections to the intervention; the administrative and medical costs of the program; the cost effectiveness of the program relative to other interventions; and the program’s cost-benefit ratio. Nevertheless, the scenarios considered here are not implausible on their face. Each is based on familiar theoretical mechanisms, evidence from at least partially analogous interventions, or both. Program designers have an obligation to take these risks seriously and to minimize them through careful program implementation, monitoring, and evaluation.
ACKNOWLEDGMENTS
Helpful comments were received from Gantt Galloway, Rick Harwood, Mark Kleiman, Rosalie Pacula, Peter Reuter, Steve Sugarman, and especially Jon Caulkins.
REFERENCES
Anglin, M.D., and Hser, Y.I. (1990). Treatment of drug abuse. In M. Tonry and J.Q. Wilson (Eds.), Drugs and crime (Crime and justice): A review of research, Vol. 13 (pp. 393-460). Chicago: University of Chicago Press.
Azrin, N.H., Hutchinson, R.R., and Hake, D.J. (1966). Extinction-induced aggression. Journal of the Experimental Analysis of Behavior, 9, 191-204.
Bauman, K.E., and Ennett, S.T. (1996). On the importance of peer influence for adolescent drug use: Commonly neglected considerations. Addiction, 91, 185-198.
Behrens, D.A., Caulkins, J.P., Tragler, G., Haunschmied, J.L., and Feichtinger, G. (1999). A dynamic model of drug initiation: Implications for treatment and drug control. Mathematical Biosciences, 159, 1-20.
Behrens, D.A., Caulkins, J.P., Tragler, G., and Feichtinger, G. (2000). Optimal control of drug epidemics: Prevent and treat—but not at the same time. Management Science, 46, 333-347.
Behrens, D.A., Caulkins, J.P., Tragler, G., and Feichtinger, G. (2002). Why present-oriented societies undergo cycles of drug epidemics. Journal of Economic Dynamics and Control, 26, 919-936.
Belenko, S. (1998). Research on drug courts: A critical review. New York: National Center on Addiction and Substance Abuse, Columbia University.
Belenko, S. (2001). Research on drug courts: A critical review, 2001 update. New York: National Center on Addiction and Substance Abuse, Columbia University.
Benthin, A., Slovic, P., and Severson, H. (1993). A psychometric study of adolescent risk perception. Journal of Adolescence, 16, 153-168.
Blower, S. (2001). Calculating the consequences: HAART and risky sex. AIDS, 15, 1309-1310.
Blower, S.M., and McLean, A.R. (1994). Prophylactic vaccines, risk behavior change, and the probability of eradicating HIV in San Francisco. Science, 265, 1451-1454.
Borelli, B., Hogan, J.W., Bock, B., Pinto, B., Roberts, M., and Marcus, B. (2002). Predictors of quitting and dropout among women in a clinic-based smoking cessation program. Psychology of Addictive Behaviors, 16, 22-27.
Bouton, M.E. (1994). Conditioning, remembering, and forgetting. Journal of Experimental Psychology: Animal Behavior Processes, 20, 219-231.
Butterfield, F. (2002). As drug use drops in big cities, small towns confront upsurge. The New York Times, February 11.
Cabanac, M., and Frankham, P. (2002). Evidence that transient nicotine lowers the body weight set point. Physiology and Behavior, 76(4-5), 539-542.
Cameron, L., and Williams, J. (2001). Cannabis, alcohol, and cigarettes: Substitutes or complements? The Economic Record, 77, 19-34.
Carter, W.B., Beach, L.R., and Inui, T.S. (1986). The flu shot study: Using multiattribute utility theory to design a vaccination intervention. Organizational Behavior and Human Decision Processes, 38(3), 378-391.
Carver, C.S., and Scheier, M.F. (1998). On the self-regulation of behavior. New York: Cambridge University Press.
Caulkins, J.P. (2001). Drug prices and emergency department mentions for cocaine and heroin. American Journal of Public Health, 91, 1446-1448.
Caulkins, J.P., and Reuter, P. (1996). The meaning and utility of drug prices. Addiction, 91, 1261-1264.
Caulkins, J.P., and Satel, S.L. (1999). Methadone patients should not be allowed to persist in cocaine use. Drug Policy Analysis Bulletin, January(6), 1-2.
Caulkins, J.P., Rydell, C.P., Everingham, S.S., Chiesa, J., and Bushway, S. (1999). An ounce of prevention, a pound of uncertainty. Santa Monica, CA: RAND Corporation.
Caulkins, J.P., Chiesa, J.R., and Everingham, S.S. (2000). Response to the National Research Council’s assessment of RAND’s “Controlling Cocaine” study. Santa Monica, CA: RAND Corporation.
Cepeda-Benito, A. (1993). A meta analytical review of the efficacy of nicotine chewing gum in smoking treatment programs. Journal of Consulting and Clinical Psychology, 61, 822-830.
Chaloupka, F., and Laixuthai, A. (1994). Do youths substitute alcohol and marijuana? Some econometric evidence. National Bureau of Economic Research Working Paper w4662. Available: http://www.nber.org/papers/w4662 [November 26, 2003].
Chaloupka, F., and Pacula, R. (2000). Economics and antihealth beahavior: The economic analysis of substance use and misuse. In W. Bickel and R. Vuchinich (Eds.), Reframing health behaviour change with behavioural economics (pp. 89-111). Mahwah, NJ: Lawrence Erlbaum.
Chaloupka, F., Pacula, R., Farrelly, M., Johnston, L., O’Malley, P., and Bray, J. (1999). Do higher cigarette prices encourage youth to use marijuana? Cambridge, MA: National Bureau of Economic Research.
Chirinko, R.S., and Harper, E.P. (1993). Buckle up or slow down? New estimates of offsetting behavior and their implications for automobile safety regulation. Journal of Policy Analysis and Management, 12, 270-296.
Compton, P.A., Ling, W., Charuvastra, V.C., and Wesson, D.R. (1995). Buprenorphine as a pharmacology for cocaine abuse: A review of the evidence. Journal of the Addictive Diseases, 14, 97-113.
Constantine, T.A. (1995). International drug trafficking organizations in Mexico. Testimony before the Senate Foreign Relations Committee, August 8.
Decker, S.L., and Schwartz, A.E. (2000). Cigarettes and alcohol: Substitutes or complements? National Bureau of Economic Research Working Paper 7535. Available: http://ideas.repec.org/p/nbr/nberwo/7535.html [November 26, 2003].
DeGrandpre, R.J., and Bickel, W.K. (1995). Human drug self-administration in a medium of exchange. Experimental and Clinical Psychopharmacology, 3, 349-357.
DeLeon, G. (1998). Reconsidering the self-selection factor in addiction treatment research. Psychology of Addictive Behaviors, 12, 71-77.
DiNardo, J., and Lemieux, T. (1992). Alcohol, marijuana, and American youth: The unintended consequences of government regulation. (Working draft WD-59220-DPRC). Santa Monica, CA: RAND Corporation.
Dunteman, G.H., Condelli, W.S., and Fairbank, J.A. (1992). Predicting cocaine use among methadone patients: Analysis of findings from a national study. Hospital and Community Psychiatry, 43(6) 608-611.
Edwards, G., Anderson, P., Babor, T.F., Casswell, S., Ferrence, R., Giesbrecht, N., Godfrey, C., Holder, H.D., Lemmens, P., Mäkelä, K., Midanik, L.T., Norström, T., Österberg, E., Romesljö, A., Room, R., Simpura, J., and Skog, O.-J. (1994). Alcohol policy and the public good. Oxford, England: Oxford University Press.
Elliot, D.S., Huizinga, D., and Ageton, S.S. (1985). Explaining delinquency and drug use. Thousand Oaks, CA: Sage.
Elster, J., and Skog, O.-J. (Ed.). (1999). Getting hooked: Rationality and addiction. Cambridge, MA: Cambridge University Press.
Everingham, S.S., and Rydell, C.P. (1994). Modeling the demand for cocaine. Santa Monica, CA: RAND Corporation.
Fairbank, J.A., Dunteman, G.H., and Condelli, W.S. (1993). Do methadone patients substitute other drugs for heroin? Predicting substance use at 1-year follow-up. American Journal of Drug and Alcohol Abuse, 19, 465-474.
Farabee, D., Prendergast, M., and Anglin, M.D. (1998). The effectiveness of coerced treatment for drug-abusing offenders. Federal Probation, 62, 3-10.
Farre, M., Mas, A., Torrens, M., Moreno, V., and Cami, J. (2002). Retention rate and illicit opioid use during methadone maintenance interventions: A meta-analysis. Drug and Alcohol Dependence, 65, 283-290.
Farrelly, M., Bray, J.W., Zarkin, G.A., Wendling, B.W., and Pacula, R.L. (1999). The effects of prices and policies on the demand for marijuana: Evidence from the National Household Surveys on Drug Abuse. Cambridge, MA: National Bureau of Economic Research.
Fiore, M.C., Smith, S.S., Jorenby, D.E., and Baker, T.B. (1994). The effectiveness of the nicotine patch for smoking cessation: A meta-analysis. Journal of the American Medical Association, 271(24), 1940-1947.
Fiore, M.C., Bailey, W.C., Cohen, S.J., Dorfman, S.F., Goldstein, M.G., Gritz, E.R., Heyman, R.B., Jaen, C.R., Kottke, T.E., Lando, H.A., Mecklenburg, R.E., Mullen, P.D., Nett, L.M., Robinson, L., Stitzer, M.L., Tommasello, A.C., Villejo, L., and Wewers, M.E. (2000). Treating tobacco use and dependence: Clinical practice guideline. Rockville, MD: U.S. Department of Health and H uman Services.
Frosch, D.L., Shoptaw, S., Nahom, D., and Jarvik, M.E. (2000). Associations between tobacco smoking and illicit drug use among methadone-maintained opiate-dependent individuals. Experimental and Clinical Psychopharmacology, 8, 97-103.
Gardner, E.L., and David, J. (1999). The neurobiology of chemical addiction. In J. Elster and O.-J. Skog (Eds.), Getting hooked: Rationality and addiction (pp. 93-136). Cambridge, England: Cambridge University Press.
Goldberg, J., and Fischhoff, B. (2000). The long-term risks in the short-term benefits: Perceptions of potentially addictive activities. Health Psychology, 19, 299-303.
Goldstein, P. (1985). The drug/violence nexus: A tripartite conceptual framework. Journal of Drug Issues, 14, 493-506.
Gottheil, E., Sterling, R.C., and Weinstein, S.P. (1995). Generalizing from controlled treatment outcome studies: Sample data from a cocaine treatment program. American Journal on Addictions, 4, 331-338.
Hughes, J.R. (1995). Applying harm reduction to smoking. Tobacco Control, 4, S33-S38.
Inciardi, J.A., Martin, S.S., Butzin, C.A., Hooper, R.M., and Harrison, L.D. (1997). An effective model of prison-based treatment for drug-involved offenders. Journal of Drug Issues, 27, 261-278.
Institute of Medicine. (2001). Clearing the smoke: Assessing the science base for tobacco harm reduction. Committee to Assess the Science Base for Tobacco Harm Reduction, K. Stratton, P. Shetty, R. Wallace, and S. Bondurant (Eds.). Board on Health Promotion and Disease Prevention. Washington, DC: National Academy Press.
Janis, I. (1983). Groupthink, 2nd rev. ed. Boston: Houghton Mifflin.
Joe, G.W., Simpson, D.D., and Broome, K.M. (1998). Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction, 93, 1177-1190.
Johnson, A. (2003). Yardie drug gangs expanding to suburbs and villages, say police. The Independent, June 15.
Johnston, L.D. (1991). Toward a theory of drug epidemics. In L. Donohew and H.E. Sypher (Eds.), Persuasive communication and drug abuse prevention (pp. 93-131). Mahwah, NJ: Lawrence Erlbaum.
Kahneman, D., and Tversky, A. (1984). Choices, values, and frames. American Psychologist, 39, 341-350.
Kamien, J.B., Bickel, W.K., Hughes, J.R., Higgins, S.T., and Smith, B. (1993). Drug discrimination by humans compared to nonhumans: Current status and future directions. Psychopharmacology, 111, 259-270.
Kandel, D.B. (1996). The parental and peer contexts of adolescent deviance: An algebra of interpersonal influences. Journal of Drug Issues, 26, 289-315.
Katz, M.H., Schwarcz, S.K., Kellogg, T.A., Klausner, J.D., Dilley, J.W., Gibson, S., and McFarland, W. (2002). Impact of highly active antiretroviral treatment on HIV sero-incidence among men who have sex with men: San Francisco. American Journal of Public Health, 92, 388-394.
Kidorf, M., and Stitzer, M.L. (1993). Contingent access to methadone maintenance treatment: Effects on cocaine use of mixed opiate-cocaine abusers. Experimental and Clinical Psychopharmacology, 1(1-4), 200-206.
Kleiman, M.A.R. (1993). Enforcement swamping: A positive-feedback mechanism in rates of illicit activity. Mathematical and Computer Modeling, 17, 65-75.
Kleiman, M.A.R. (1997a). Coerced abstinence: A neopaternalist drug policy punitiative. In L. Mead (Ed.), The new paternalism: Supervisory approaches to poverty (pp. 182-219). Washington, DC: Brookings Institution.
Kleiman, M.A.R. (1997b). The problem of replacement and the logic of drug law enforcement. Drug Policy Analysis Bulletin, 3, 8-10. Available: http://www.fas.org/drugs/issue3.htm [January 8, 2004].
Lawental, E., McLellan, A.T., Grissom, G.R., Brill, P., and O’Brien, C. (1996). Coerced treatment for substance abuse problems detected through workplace urine surveillance: Is it effective? Journal of Substance Abuse, 8, 115-128.
Lawrence, M.H., and Goldstein, M.A. (1995). Hepatitis B immunization in adolescents. Journal of Adolescent Health, 17(4), 234-243.
Leri, F., Bruneau, J., and Stewart, J. (2003). Understanding polydrug use: Review of heroin and cocaine co-use. Addiction, 98, 7-22.
MacCoun, R.J. (1993). Drugs and the law: A psychological analysis of drug prohibition. Psychological Bulletin, 113, 497-512.
MacCoun, R.J. (1998a). Biases in the interpretation and use of research results. Annual Review of Psychology, 49, 259-287.
MacCoun, R.J. (1998b). Toward a psychology of harm reduction. American Psychologist, 53, 1199-1208.
MacCoun, R.J. (2003). Is the addiction concept useful for drug policy? In R. Vuchinich and N. Heather (Eds.), Choice, behavioural economics and addiction. Oxford, England: Elsevier Science.
MacCoun, R.J., and Reuter, P. (2001). Drug war heresies: Learning from other vices, times, and places. Cambridge, England: Cambridge University Press.
MacCoun, R.J., Reuter, P., and Schelling, T. (1996). Assessing alternative drug control regimes. Journal of Policy Analysis and Management, 15, 1-23.
Manning, W., Keeler, E., Newhouse, J., Sloss, E., and Wasserman, J. (1991). The costs of poor health habits. Cambridge, MA: Harvard University Press.
March, J.G., and Shapira, Z. (1992). Variable risk preferences and the focus of attention. Psychological Review, 99, 172-183.
Maxson, C. (1998). Gang members on the move. Washington, DC: Office of Juvenile Justice and Delinquency Prevention, U.S. Department of Justice.
Maxwell, S.R. (2000). Sanction threats in court-ordered programs: Examining their effects on offenders mandated into drug treatment. Crime and Delinquency, 46(4), 542-563.
Miller, N.S., and Flaherty, J.A. (2000). Effectiveness of coerced addiction treatment (alternative consequences): A review of the clinical research. Journal of Substance Abuse Treatment, 18(1), 9-16.
Miron, J.A. (2003). Do prohibitions raise prices? Evidence from the market for cocaine. Unpublished manuscript, Boston University. Available: http://econ.bu.edu/miron/images/prices_submit.pdf [January 8, 2004].
Model, K.E. (1993). The effect of marijuana decriminalization on hospital emergency room drug episodes: 1975-1978. Journal of the American Statistical Association, 88, 737-747.
Mook, D.G. (1983). In defense of external invalidity. American Psychologist, 38, 379-387.
Moore-Caldwell, S.Y., Werner, M.J., Powell, L., and Greene, J.W. (1997). Hepatitis B vaccination in adolescents: Knowledge, perceived risk, and compliance. Journal of Adolescent Health, 20(4), 294-299.
Musto, D.F. (1971/1987). The American disease: Origins of narcotic control. New York: Oxford University Press.
Mutschler, N.H., Stephen, B.J., Teoh, S.K., Mendelson, J.H., and Mello, N.K. (2002). An inpatient study of the effects of buprenorphine on cigarette smoking in men concurrently dependent on cocaine and opioids. Nicotine and Tobacco Research, 4, 223-228.
National Alliance of Gang Investigators Associations. (2000). Regional gang assessments. Available: http://www.nagia.org/NGTASection_III.htm [January 8, 2004].
National Research Council. (1999). Assessment of two cost-effectiveness studies on cocaine control policy. Committee on Data and Research for Policy on Illegal Drugs. C.F. Mansiki, J.V. Pepper, and Y. Thomas (Eds.). Committee on Law and Justice and Committee on National Statistics. Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press.
National Research Council. (2001). Informing America’s policy on illegal drugs: What we don’t know keeps hurting us. Committee on Data and Research for Policy on Illegal Drugs, C.F. Mansiki, J.V. Pepper, and C.V. Petrie (Eds.). Committee on Law and Justice and Committee on National Statistics. Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press.
Neuringer, A., Kornell, N., and Olufs, M. (2001). Stability and variability in extinction. Journal of Experimental Psychology: Animal Behavior Processes, 27, 79-94.
Nirenberg, T.D., Cellucci, T., Liepman, M.R., Swift, R.M., and Sirota, A.D. (1996). Cannabis versus other illicit drug use among methadone maintenance patients. Psychology of Addictive Behaviors, 10(4), 222-227.
Nishimoto, R.H., and Roberts, A.C. (2001). Coercion and drug treatment for postpartum women. American Journal of Drug and Alcohol Abuse, 27(1), 161-181.
Ostrow, D.E., Fox, K.J., Chmiel, J.S., Silvestre, A., Visscher, B.R., Vanable, P.A., Jacobson, L.P., and Strathdee, S.A. (2002). Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS, 16, 775-780.
Pacula, R. (1998). Adolescent alcohol and marijuana consumption: Is there really a gateway effect? Cambridge, MA: National Bureau of Economic Research.
Pennings, E.J.M., Leccese, A.P., and de Wolff, F.A. (2002). Effects of concurrent use of alcohol and cocaine. Addiction, 97, 773-783.
Pentel, P.R. (2004). Vaccines and depot medications for drug addiction: Rationale, mechanisms of action, and treatment implications. In H.J. Harwood and T.G. Myers (Eds.), New treatments for addiction: Behavioral, ethical, legal, and social questions. National Research Council and Institute of Medicine. Washington, DC: The National Academies Press.
Petry, N.M., and Bickel, W.K. (1998). Polydrug abuse in heroin addicts: A behavioral economic analysis. Addiction, 93, 321-335.
Preston, K.L., Silverman, K., Higgens, S.T., Brooner, R.K., Montoya, I., Schuster, C.R., and Cone, E.J. (1998). Cocaine use early in treatment predicts outcome in a behavioral treatment program. Journal of Consulting and Clinical Psychology, 66, 691-696.
Quaglio, G., Talamini, G., Lugoboni, F., Lechi, A., Venturini, L., Accordini, A., Bellio, G., Bossi, C., Cantiero, D., Ceravolo, R., Cicciu, G., Civitelli, P., Corso, F., Faccini, M., Forza, G., Manera, R., Manzato, E., Mecenero, V., Pajusco, B., Parolin, A., Residori, M., Sabbion, R., Saccardi, C., Schifano, F., Smacchia, C., Vendramin, A., Des Jarlais, D.C., and Mezzelani, P. (2002). Compliance with hepatitis B vaccination in 1175 heroin users and risk factors associated with lack of vaccine response. Addiction, 97(8), 985-992.
Reuter, P., and Kleiman, M. (1986). Risks and prices: An economic analysis of drug enforcement. In N. Morris and M. Tonry (Eds.), Crime and justice: An annual review of research, vol. 7 (pp. 289-340). Chicago: University of Chicago Press.
Reuter, P., Crawford, G., and Cave, J. (1988). Sealing the borders: The effects of increased military participation in drug interdiction. Santa Monica, CA: RAND Corporation.
Robinson, T.E., and Berridge, K.C. (2003). Addiction. Annual Review of Psychology, 54, 25-53.
Rose, G. (1992). The strategy of preventive medicine. Oxford, England: Oxford University Press.
Rydell, C.P., and Everingham, S.S. (1994). Controlling cocaine: Supply versus demand programs. Santa Monica, CA: RAND Corpoation.
Saffer, H., and Chaloupka, F. (1995). The demand for illicit drugs. Cambridge, MA: National Bureau of Economic Research.
Schmitz, J.M., Grabowski, J., and Rhoades, H. (1994). The effects of high and low doses of methadone on cigarette smoking. Drug and Alcohol Dependence, 34(3), 237-242.
Shadish W.R., Hu, X., Glaser, R.R., Kownacki, R., and Wong, S. (1998). A method for exploring the effects of attrition in randomized experiments with dichotomous outcomes. Psychological Methods, 3, 3-22.
Shaffer, H.J., and LaSalvia, T.A. (1992). Patterns of substance use among methadone maintenance patients: Indicators of outcome. Journal of Substance Abuse Treatment, 9(2), 143-147.
Shrader-Frechette, K.S. (1991). Risk and rationality. Berkeley and Los Angeles: University of California Press.
Silva de Lima, M., Garcia de Oliveira Soares, B., Pereira Reisser, A.A., and Farrell, M. (2002). Pharmacological treatment of cocaine dependence: A systematic review. Addiction, 97, 931-949.
Simpson, D.D., Joe, G.W., and Brown, B.S. (1997). Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors, 11, 294-307.
Siqueland, L., Crits-Christoph, P., Frank, A., Daley, D., Weiss, R., Chittams, J., Blaine, J., and Luborsky, L. (1998). Predictors of dropout from psychosocial treatment of cocaine dependence. Drug and Alcohol Dependence, 52, 1-13.
Skinner, B.F. (1953). Science and human behavior. New York: Free Press.
Skog, O.-J. (1993). The tail of the alcohol consumption distribution. Addiction, 88, 601-610.
Slovic, P., Fischhoff, B., and Lichtenstein, S. (1979). Rating the risks. Environment, 21, 14-20, 36-39.
Stark, M.J., and Campbell, B.K. (1993). Cigarette smoking and methadone dose levels. American Journal of Drug and Alcohol Abuse, 19(2), 209-217.
Stetzer, A., and Hofman, D.A. (1996). Risk compensation: Implications for safety interventions. Organizational Behavior and Human Decision Processes, 66, 73-88.
Stolte, I.G., Dukers, N.H., de Wit, J.B., Fennema, H., and Coutinho, R.A. (2002). A summary report from Amsterdam: Increase in sexually transmitted diseases and risky sexual behaviour among homosexual men in relation to the introduction of new anti-HIV drugs. Eurosurveillance Monthly Archives, 7(2), 19-22.
Sulzer-Azaroff, B., and Mayer, G.R. (1977). Applying behavior-analysis procedures with children and youth. New York: Holt, Rinehart, and Winston.
Szilagyi, P.G., Bordley, C., Vann, J.C., Chelminski, A., Kraus, R.M., Margolis, P.A., and Rodewald, L.E. (2000). Effect of patient reminder/recall interventions on immunization rates. Journal of the American Medical Association, 284(14), 1820-1827.
Tenner, E. (1996). Why things bite back: Technology and the revenge of unintended consequences. New York: Alfred A. Knopf.
Thompson, T. (2002). The dealers think they’re untouchable now … The Observer, Feb. 24.
Van Horn, D.H.A., and Frank, A.F. (1998). Psychotherapy for cocaine addiction. Psychology of Addictive Behaviors, 12, 47-61.
Vaughan, D. (1996). The Challenger launch decision: Risky technology, culture, and deviance at NASA. Chicago: University of Chicago Press.
Viscusi, W.K. (1992). Fatal tradeoffs: Public and private responsibilities for risk. Oxford, England: Oxford University Press.
Viswesvaran, C., and Schmidt, F.L. (1992). A meta-analytic comparison of the effectiveness of smoking cessation methods. Journal of Applied Psychology, 77, 554-561.
Vuchinich, R., and Heather, N. (Eds.). (2003). Choice, behavioural economics and addiction. Oxford, England: Elsevier Science.
White, J.M., Winn, K.I., and Young, W. (1998). Predictors of attrition from an outpatient chemical dependency program. Substance Abuse, 19, 49-59.
Wilde, G.J.S. (1982). The theory of risk homeostasis: Implications for safety and health. Risk Analysis, 2, 209-255.
Williams, J., Pacula, R.L., Chaloupka, F.J., and Wechsler, H. (2001). Alcohol and marijuana use among college students: Economic complements or substitutes? Cambridge, MA: National Bureau of Economic Research.
World Health Organization. (2001). Advancing knowledge on regulating tobacco products. Geneva: World Health Organization.
Zito, J.M., Craig, T.J., and Wanderling, J. (1991). New York under the Rivers decision: An epidemiologic study of drug treatment refusal. American Journal of Psychiatry, 148(7), 904-909.