3
Costs and Financing of Health Professions Education
The costs associated with health professions education pose a considerable barrier for many underrepresented minority (URM) students, whose economic resources are, on average, more limited compared to their majority counterparts. URM students, in particular, may be discouraged from entering health professions training programs when faced with the prospect of high debt. Some health professions leaders have therefore called for a reexamination of the costs and financing of health professions training to significantly reduce or eliminate many training costs, particularly for those students whose service in the public sector is likely to increase access to care for medically underserved populations.
While URM students are more likely than non-URM students to come from low-income families, most low-income students are white. Policies that solely target financial support to low-income students may or may not successfully help URM students to access and succeed in health professions training programs. Therefore, it is important for financial strategies to be implemented in conjunction with other “race-conscious” interventions targeting, for example, admissions and accreditation policies.
A number of public and private initiatives have been established to assist URM students finance the costs of their education and training. Some provide direct financial assistance to students and others indirectly support URM students through funding provided to institutions for diversity activities. All, however, provide support to increase URM participation in health professions and reduce financial barriers, directly or indirectly, for students who experience difficulty financing their training. This chapter will provide
an overview of the financial status of URM families, assess the costs of training, and show the negative impact of these costs on URM students’ pursuit of education. In addition, the chapter will assess the role of private and public sources of funding for health professions students, and examine issues regarding the financing of education. For a detailed review of publicly funded health professions programs that support URM students, the reader is referred to the commissioned paper, Public Financing of the Health Professions: Levers for Change, prepared by Karen Matherlee, which appears as an appendix of this report.
For purposes of this report, the study committee defines health professions educational costs as a formulation involving total educational and living expenses: including tuition and fees (which vary considerably across institutions, particularly between public and private health professions education institutions [HPEIs]); other educational expenses (including books, equipment, supplies, etc.); the number of years to degree completion; living costs (including rent, utilities, and other living expenses); and the costs of any specialized, prerequisite post-high school or post-baccalaureate preparation. The other side of this equation—financing of health professions training—can be described as a student’s financial resources (both personally and nonpersonally derived), as well as scholarships, loans, and other forms of financial assistance. Unmet financial need is therefore total health professions educational costs, minus student financial resources. This chapter attempts to describe educational costs, sources of financing of training, and unmet financial need, and how these factors affect URM participation in health professions education. This analysis is severely limited, however, by a lack of data regarding these factors, particularly in disciplines other than medical education, where financing issues are more thoroughly documented. This absence of data prevents a comparison of financing issues across health professions disciplines, because the factors identified above, such as tuition, fees, number of years to degree completion, and sources of financial aid, vary considerably across disciplines. The most useful perspective is therefore to examine the financial obstacles within each profession, rather than across professions.
FINANCIAL STATUS OF UNDERREPRESENTED MINORITY FAMILIES
Census figures indicate a large disparity in family income among various racial and ethnic groups in the United States (Figure 3-1) (U.S. Census Bureau, 2002a). Households headed by black and Hispanic individuals earn significantly less than either white non-Hispanic or Asian and Pacific Islander householders. In 2001, the median income for black and Hispanic families was approximately $34,000 and $35,000, respectively. In com-
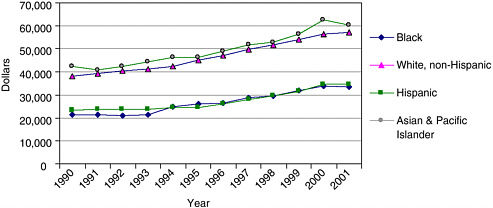
FIGURE 3-1 Race and Hispanic origin of householder: families by median income, 1990–2001.
SOURCE. U.S. Census Bureau, Historical Income Tables—Families, 2002.
parison, white families had a median income of $57,000 and Asian/Pacific Islander families had a median income of $60,000. American Indian and Alaska Native families were not included in these census figures; however other census data indicate that the three-year average median income for 1999–2001 was $32,116 for American Indian and Alaska Native households, which was higher than the median income of black households and similar to the median income of Hispanic households during this time period (U.S. Census Bureau, 2002b). Thus, as URM students prepare for higher education, they are more likely to face difficulties financing their education.
In addition to disparities in household income, data indicate large racial and ethnic differences in wealth (Figure 3-2). On average, white families are wealthier than black or Hispanic households, even after controlling for income and demographic variables (Choudhury, 2002). Housing equity is fairly equally distributed across racial and ethnic groups, although rates of homeownership are greater for whites. Nonhousing equity (e.g., liquid assets, stocks, bonds, IRAs, vehicle and business equity) varies more widely between racial and ethnic groups as income increases, with whites holding larger sums of nonhousing equity.
COSTS OF UNDERGRADUATE EDUCATION: EFFECTS ON ACCESS AND COMPLETION
Much of the available data regarding the impact of the high costs of education relates to college access and degree attainment. These findings have implications for health professions education and strategies that may be employed to reduce financial barriers for URM students entering these fields.
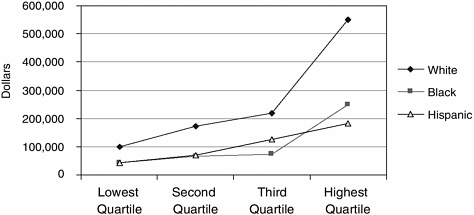
FIGURE 3-2 Mean net worth for households by race, ethnicity, and income quar-tile.
NOTE: Cutoff points for income quartiles, in 1992 dollars: $23,460; $41,900; $66,900.
SOURCE: Health and Retirement Study Wave 1 (1992) as cited in Choudhury, 2002.
The Advisory Committee on Student Financial Assistance reports that “… financial barriers to a college education have risen sharply due to shifts in policies and priorities at the federal, state, and institutional levels, resulting in a shortage of student aid, and in particular need-based grant aid, as well as rising college tuition” (Advisory Committee on Student Financial Assistance, 2002, p. v). The Advisory Committee estimated that these financial barriers prohibit 48 percent of low-income students who are academically qualified for college from attending a four-year institution. The lowest achieving, highest socioeconomic status (SES) students attend college at approximately the same rate as the highest achieving, lowest SES students, at 77 percent and 78 percent, respectively (Advisory Committee on Student Financial Assistance, 2002). Because URM families earn less, on average, than their white or Asian/Pacific Islander counterparts, they may face greater difficulty in financing their children’s undergraduate education. Estimates from the 1999–2000 academic year indicate that among full-time undergraduate students who were financially dependant on their families, black, Hispanic, Asian, and those students who indicated more than one race were more likely to be from low-income families (Figure 3-3; U.S. Department of Education, 2003b). White, Pacific Islander, and American Indian students were more likely to come from high-income families.
While rates of tuition have climbed steadily, sources of grant aid have
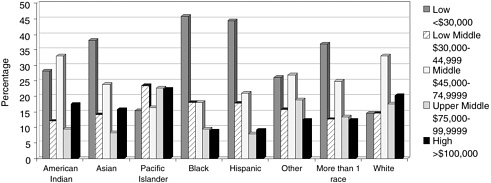
FIGURE 3-3 Percentage distribution of full-time, full-year dependent undergraduates according to family income, 1999–2000, by race and ethnicity.
SOURCE: U.S. Department of Education, National Center for Education Statistics, 2003b.
decreased. At the federal level, the maximum awards provided by Pell grants, awarded to help low-income students attend college, have decreased significantly relative to the cost of attendance. The maximum award decreased from 84 percent of public 4-year costs during the 1975–1976 academic year to 39 percent of costs during the 1999–2000 academic year (College Board, 2000, and U.S. Department of Education, 2000b, as cited in Advisory Committee on Student Financial Assistance, 2001). At the state level, more new grants are merit-based rather than need-based. In 1982, 9.6 percent of grants were merit-based compared to 18.6 percent in 1998 (Heller, in press, as cited in Advisory Committee on Student Financial Assistance, 2001). Similarly, higher education institutions are increasing merit-based awards. At private institutions, grants for middle-income students have exceeded grants for low-income students (McPherson and Shapiro, in press, as cited in Advisory Committee on Student Financial Assistance, 2001).
Increased tuition costs and decreased need-based aid have resulted in higher levels of unmet need for lower income students (Figure 3-4). Unmet financial need is calculated as the total cost of education minus expected family contribution minus aid (U.S. Department of Education, 2003a). In 1995–1996, students from the lowest income families faced $3,800 in unmet need for a public 4-year college and $6,200 for private 4-year colleges. For middle-income students, whose family income was between $25,000 and $49,000, average unmet need was $3,000 for public and $4,900 for private college. In comparison, those students from the highest SES level faced $400 in need for public college and $3,000 for private institutions (U.S.
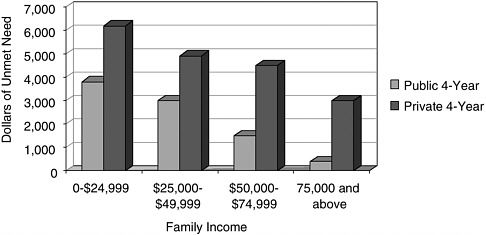
FIGURE 3-4 Average annual unmet need of high school graduates, by family income and type of institution.
SOURCE: Advisory Committee on Student Financial Assistance, 2002.
Department of Education, 1999). Between 1992 and 1999, average annual borrowing by low-income students with high unmet need increased from $1,812 to $2,982 at public 4-year colleges (Advisory Committee on Student Financial Assistance, 2002). At private colleges borrowing increased from $2,935 to $4,130 (Advisory Committee on Student Financial Assistance, 2002). Thus, a 4-year baccalaureate degree can result in over $16,000 of debt for low-income students.
The impact of high unmet need can be considerable on low-income students, even those who are academically prepared for the challenges of higher education. Low-income students with high unmet need are significantly less likely than high-income students with low unmet need to expect to finish college; plan to attend a 4-year college after graduating from high school; take entrance exams; and apply, enroll, and persist to degree completion (Figure 3-5) (Advisory Committee on Student Financial Assistance, 2002). Students who have sufficient funds for college enjoy enhanced academic performance and social integration on campus and are more likely to persist to graduation (Nora and Cabrera, 1996).
In an investigation of the influence of race and gender on the awarding of financial aid, Heller (2000), using data from the National Postsecondary Student Aid Studies, found that while there were variations in financial aid by geographic region and type of institution, in general, African American students were more likely to receive nonneed grants (based on merit or other circumstance not related to financial need, such as academic, artistic, or athletic merit), particularly those students attending public institutions. Hispanic students were less likely to receive nonneed grants. The author
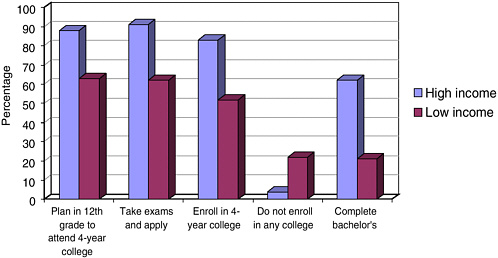
FIGURE 3-5 College access process for high- and low-income college-qualified high school graduates.
SOURCE: Advisory Committee on Student Financial Assistance, 2002.
speculates that since academic achievement and other institutional and student characteristics served as controls, the effect of race on receiving nonneed aid was the result of institutional financial aid policies and that African American students were specifically targeted for financial aid compared with white students (Heller, 2000).
Several studies have examined the impact of financial barriers and the effect of financial aid on student enrollment. An investigation of racial differences in high school students’ access to postsecondary education found that low-income, black, and Hispanic high school graduates were less likely to be academically prepared for a 4-year college and that among those who were prepared, low-income and Hispanic students were less likely to take entrance exams and apply for admissions (U.S. Department of Education, 1997). However, differences in enrollment rates between college-qualified low- and middle-income students were eliminated among those students who took college entrance exams and completed the admissions application. Similarly, differences in enrollment between college-qualified students of varying race and ethnicity (black, Hispanic, Asian, and white) were also eliminated among those who took entrance exams and completed an application. This study also found that “the more sources of information they had obtained, and the more people with whom they had discussed financial aid, the more likely college-qualified low- and middle-income, black, and Hispanic students were to take college entrance exams and apply for admis-
sion to a four-year college” (U.S. Department of Education, 1997, p. 60). However, a causal relationship between college attendance and information-seeking could not be established. It may be that students who intended to attend sought more information.
The type of aid received by students also may influence college attendance. In a review of evidence of financial aid’s impact on college entry and retention, Grumbach et al. (2002) reported that grants had a large effect on increasing attendance for students in the lowest income category. In contrast, loans were not associated with enrollment rates for this group of students. For middle-income students, both grants and loans were associated with increased attendance (St. John, 1994; Grumbach et al., 2002).
Grumbach and colleagues also noted that differences in how far low-income students advance in their education are not only a function of the ability to pay. Low socioeconomic status is associated with a range of factors that may affect college access and success, including attendance at primary and secondary schools with few resources and having few family members who have attended college (and therefore know what the experience is like and can help navigate the application process). As mentioned in the outset of this chapter, providing financial aid alone is unlikely to remove all barriers to higher education for URM students.
In light of trends in tuition costs, educational organizations have called for changes in policies for the provision of financial aid to low-income students. Recently, the College Board urged the government to raise the maximum awards for Pell Grants to cover the average cost of tuition, fees, room, and board, which was estimated to be $9,000 for the 2002–2003 academic year, and to expand loan forgiveness for students who enter and stay in occupations that serve high-need areas (College Board, 2003). In addition, the Board urged the federal government to partner with states, colleges, universities, and the private sector and to take the lead in developing programs to encourage investment in need-based aid. Specific recommendations included:
-
“… Loan forgiveness for students who enter and remain in certain key occupations and those who serve in high-need areas should be supported and expanded…” (College Board, 2003, p. 6).
-
“… The federal government should also increase its level of support directly to institutions that serve large percentages of high-need students…” (College Board, 2003, p. 7).
-
“… Colleges and universities should reaffirm their commitment to need-based aid, striving to enroll larger numbers of students from low-income and underrepresented backgrounds” (College Board, 2003, p. 7).
-
“The federal government and the states should explore ways of more closely linking increases in tuition to increases in need-based aid, to insulate
-
financially needy student from effects of economic downturns…” (College Board, 2003, p. 8).
In summary, the financial burdens imposed by undergraduate education are a significant factor for low-income students who wish to attend college. A student’s ability or academic readiness does not make them immune to these difficulties. These impediments may continue for those who continue their studies at the graduate level.
COSTS OF HEALTH PROFESSIONS EDUCATION: TUITION AND STUDENT DEBT
By the time students with high unmet need complete college, they may have debts of $10,000 to $15,000 or more. As students consider obtaining degrees in one of the health professions, they must contemplate the even higher costs of these degrees. There is some evidence to suggest that low-income students who graduate from college are less likely than their higher income peers to continue on to graduate education (Grumbach et al., 2002). This section will review trends in costs of health professions education and debt incurred by students.
Dental Education
In 1999, the average first-year resident tuition for dentistry schools was $15,653 (Figure 3-6), compared to $7,086 in 1985 (Valachovic et al., 2001). The fees at public schools were $9,354 while private school tuition and fees totaled $30,208, resulting in costs ranging from $37,000 to $120,000 at the end of four years. Moreover, the average debt of dental students has significantly increased in the past 20 years (see Figure 3-7) (Hardigan, 1999). The average rate of increase for all schools between 1991–1992 and 1997–1998 was 84.6 percent. The increase was greatest at public schools (94.5 percent).
Medical Education
For medical students, average tuition and debt are similarly high. During the 2001–2002 academic year, mean tuition and fees for residents at public medical schools were $12,970. Fees for nonresidents were more than double this figure (Figure 3-8) (AAMC, 2003).
In 2001, approximately 75 percent of URM graduates had received scholarships during medical school, with average scholarship awards of $46,383 for private school graduates and $25,184 for public school graduates (AAMC, 2002). By comparison, nearly 50 percent of non-URM stu-
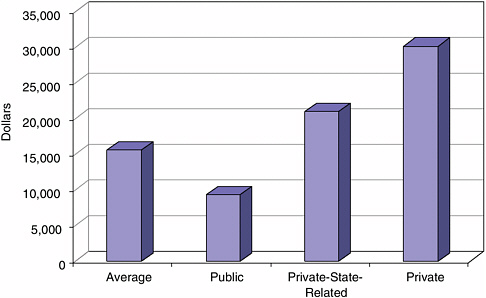
FIGURE 3-7 Average debt of senior dental students, 1991–1992, 1997–1998.
SOURCE: Hardigan, 1999. Reprinted, with permission, from the American Dental Education Association, 2004. Copyright 2004 by ADEA.
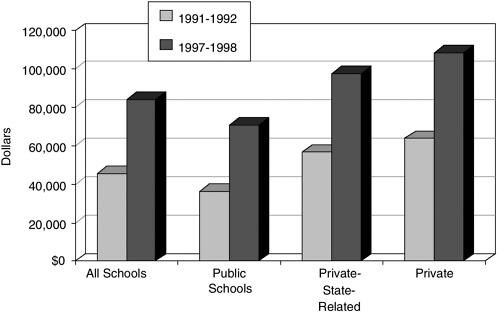
FIGURE 3-6 Average first year resident tuition and fees at U.S. dental schools, 1999.
SOURCE: Valachovic et al., 2001. Reprinted, with permission, from the American Dental Education Association, 2004. Copyright 2004 by ADEA.
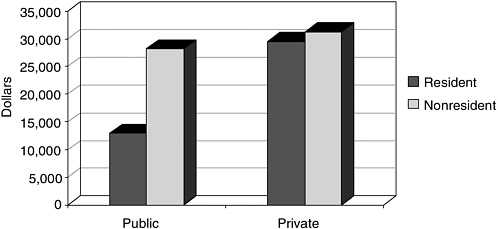
FIGURE 3-8 Tuition and fees for first year students at U.S. medical schools, 2001–2002.
SOURCE: AAMC, 2003.
dents received scholarship aid, averaging $40,197 for private school graduates and $18,134 for public school graduates.
Like dental students, medical graduates face high levels of debt, which have increased six-fold in the past 20 years. Among students who incur debt, URM and non-URM students face similar levels of total debt. However, URM graduates are twice as likely to carry some educational debt. Among 2001 private school graduates, 20.3 percent of non-URMs had no debt, as compared to 8.1 percent of URMs (AAMC, 2002). For public school graduates, 16.8 percent of non-URM students completed with no educational debt, while only 8.4 percent of URM student graduated debt free. However, for those that had debt, approximately 50 percent of all students owed more than $100,000 (AAMC, 2002).
Professional Psychology Education
The average cost of education for students in schools of psychology is less, on average, than for students in other health professions. However, these students tend to earn less once in practice than some other health professionals. During the 2001–2002 academic year, the average cost of tuition at public institutions offering graduate degree programs in psychology was $3,380 for state residents and $8,858 for state nonresidents (Figure 3-9; APA, 2003). Tuition at private institutions was approximately $17,000.
Debt for clinical and other psychology health-service areas has, like other health professions, increased in recent years (Murray, 1999). A larger
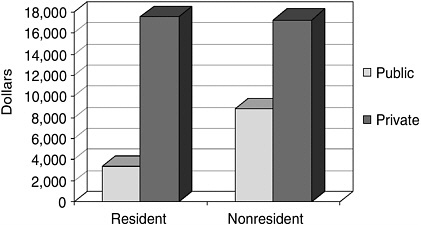
FIGURE 3-9 Median tuition in U.S. graduate departments of psychology by type of institution, 2001–2002.
SOURCE: Graduate Study in Psychology, Compiled by APA Research Office, 2003. 2001–2002 Tuition in Graduate Departments of Psychology. Adapted with permission from the American Psychological Association. Copyright 2004 by APA.
percentage of psychology Ph.D. recipients reported debt in excess of $30,000 than Ph.D. recipients in other science and engineering fields (NSF, 2000). The proportion of students in health-service provider fields with loan debt of more than $30,000 has increased from less than 20 percent in 1989 to more than 40 percent in 1996 (Murray, 1999). Thirty percent of those with Ph.D.s in clinical psychology (1993–1997) had debt exceeding $30,000 (Figure 3-10) (NSF, 2000). Of those with doctoral degrees in counseling, family and marriage, and school psychology, 17 percent carried more that $30,000 in debt. For graduates with Psy.D. degrees (whose programs focus on training for clinical practice), 55 percent had debt in excess of $30,000 (NSF, 2000).
Nursing Education
National-level data on the costs of nursing education, average levels of debt incurred by nursing students, and sources of financial aid for nursing education are not routinely collected and are therefore not as readily available as are data from other health professions. To obtain this information, the study committee contacted several major nursing organizations (e.g., National League of Nursing, the American Association of Colleges of Nurses). National-level statistics for tuition were obtained for basic registered nursing (RN) programs (Figure 3-11), but tuition data for other types
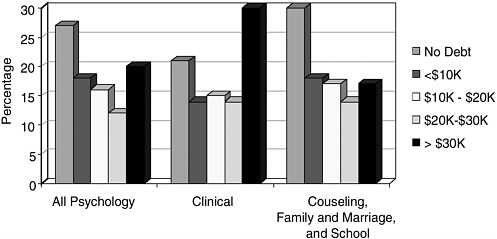
FIGURE 3-10 Percent of debt of 1993–1997 psychology Ph.D.s by field.
SOURCE: National Science Foundation, 2000.
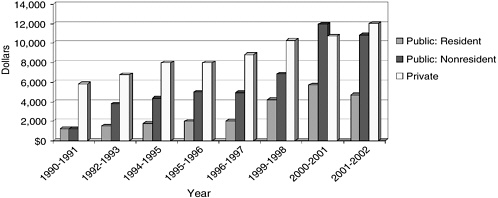
FIGURE 3-11 Estimate of mean annual tuition of full-time students in public or private basic RN programs (preliminary and unpublished data).
NOTE: Tuition data is not a required field in the annual survey.
SOURCE: National League for Nursing. Figure included with the permission of the National League for Nursing, New York, NY.
of nursing programs were not available. Data from the National League for Nursing reveal a steady increase in tuition costs for public and private RN programs from the 1990–1991 to 2001–2002 academic years. In this latter year, tuition for resident at public programs decreased by approximately $1,000.
National level data regarding debt for nursing students were not avail-
able. However, anecdotal reports suggest that nursing students experience large debt loads, as do students in other health professions. For example, at the University of Colorado Health Sciences Center, a public institution, average debt among nursing students (accumulated while attending the university) receiving degrees in 2003 ranged from $19,258 for B.S.N. students to $72,940 for N.D. students, for a total of $31,765 in debt for students receiving degrees in the school of nursing (includes B.S.N., M.S., Ph.D., N.D.) (personal communication, Marlaine Smith, professor and associate dean for academic affairs, University of Colorado Health Sciences Center School of Nursing). These figures, however, may represent a slight overestimate of debt due to a high proportion of N.D. students attending 1.5 to 2 years at N.D. degree-granting institutions and receiving graduate level loans, then transferring to B.S.N. programs (causing the B.S.N. average to be larger than if the student attended only as a B.S.N.). In addition, in many cases students receiving M.S. and or Ph.D. degrees at the school of nursing also receive other degrees at the university.
At Vanderbilt University, a private institution, master’s and baccalaureate nursing students graduated with an average debt burden of $80,000 (personal communication, Colleen Conway-Welch, dean and professor, Vanderbilt University School of Nursing). While 90 percent of students at Vanderbilt qualified for financial assistance as determined by the Free Application for Federal Student Aid (FAFSA), the average scholarship was $4,000, which met 15 percent of the FAFSA need. These examples are taken from private and selective institutions and may not generalize to the educational experiences of other nursing students.
COSTS OF HEALTH PROFESSIONS EDUCATION: BEYOND TUITION
While much of the literature on costs is focused on tuition, it is important to note that the total costs of a health professions education are often far greater than tuition costs alone. Other costs—such as room and board, books and professional supplies and equipment, and other educational expenses—are often difficult to quantify but can be significant depending on the geographic location of the educational institution, institutional requirements for equipment and supplies, and other factors.
In addition to expenses directly related to education, other costs such as consumer debt may cause considerable burden. For example, among 2001 medical graduates, 63 percent of URM students carried consumer debt (for example, credit cards and/or auto loans), compared to 37 percent of non-URM students. However, among those with consumer debt, non-URM graduates carried an average level of $20,783 compared to $12,803 for URM graduates (AAMC, 2002).
As will be discussed in Chapter 5 (“Transforming the Institutional Climate to Enhance Diversity in Health Professions”), to the extent that students must repeat a year of training, tuition and other costs will increase accordingly. These costs, as noted above, disproportionately burden URM students, who have fewer resources, on average, than non-URM students. More research is needed to assess these costs, the impact of educational and noneducational costs on URM students’ decisions to pursue health professions careers, the availability of financial resources (both scholarship and loan) to address unmet financial need, and the impact of these factors on URM student completion of training, graduation rates, and choice of practice location and specialty.
IMPACT OF COSTS AND DEBT
The impact of education costs and debt on students can be quite substantial, affecting persistence, career choices, job satisfaction, and lifestyle. The 2002 National Student Loan Survey (of Nellie Mae subsidized or unsubsidized Stafford or SLS borrowers) examined the impact of debt repayment on students paying back loans in 2002 (Baum and O’Malley, 2003). The analysis included undergraduate as well as graduate borrowers. Students from low-income families (defined as those receiving Pell Grants) reported more feelings of burden about their debt compared to other students. This is reported as a change from previous surveys where there was no significant difference in feeling of burden between low-income students and those not receiving Pell Grants. In addition, African American, Asian American, and Hispanic borrowers reported more burden than white borrowers, after controlling for other factors. The association was strongest for Hispanics, but also significant for African American borrowers. The authors suggest that “socioeconomic and racial background are correlated with perceptions of debt burden, with low-income and minority students perceiving greater hardship than other borrowers with given amounts of debt and current income levels” (Baum and O’Malley, 2003, p. 22).
In a study of debt and persistence among dental students, an analysis of the 1993 National Postsecondary Student Aid Study (DeAngelis, 2000) revealed that receiving financial aid of any type promoted within-year persistence. However, when taking tuition, financial aid received, and debt into account, debt was the only variable found to significantly influence persistence. For every $1,000 in debt, students were 5.76 percentage points less likely to persist to their next semester. The authors conclude that while financial aid meets immediate needs, the accumulation of debt may significantly and negatively affect persistence and that there may be a limit to the amount of debt students are willing to amass.
Most evidence of the effect of debt on career choice is found in the
medical literature. There have been two hypotheses regarding the effect of debt on physicians’ choice of primary care practice versus other specialties (Colquitt et al., 1996). One is that students with high levels of debt chose primary care careers because the training period is shorter and they can begin earning a physician’s salary sooner. The other posits that students with high debt choose specialty fields other than primary care because the salaries are higher and therefore allow them to pay off debt sooner. Several studies have examined the effect of debt on career choice (Baker and Barker, 1997; Brotherton, 1995; Colquitt et al., 1996; Rosenthal et al., 1996). While some evidence suggests that debt has little influence on choice of general or specialty careers (Brotherton, 1995), others have suggested that debt does, in fact, independently contribute to the selection of career specialty. Rosenthal and colleagues (1996) found that debt above a certain threshold (at least $75,000) was an independent predictor of career choice away from family practice. Colquitt and colleagues (1996) suggest that the relationship between debt and career choice is a complex one and that it is important to assess the context, particular groups of students, which specialties are being considered, and how the impact of debt changes over time. In their study, the effect of debt on preferences for family medicine, general internal medicine, and general pediatrics varied, for example, by how much income medical school graduates expected to earn, the level of debt they incurred, how much debt was from subsidized loans, and in which geographic location graduates expected to practice. The researchers concluded that debt was an important factor in specialty choice, driven by a variety of issues. Rico and Stagnaro-Green (1997) reported similar results in a study examining the relationship between debt and career choice in URM and non-URM students placed in residencies at Mount Sinai School of Medicine. While mean debt levels were similar for URM and non-URM graduates, half of URMs had debt in excess of $75,000 compared to 37 percent of non-URMs. Overall, fewer URM graduates chose primary care fields (37.5 percent vs. 46.6 percent). When examining career choices by level of debt, the investigators found that among students with more than $75,000 of debt, 31 percent of URM chose primary care fields, compared to 49 percent of non-URMs. However, among those with debt levels under $75,000, choices for primary care were similar (40 percent URM, 48 percent non-URM). The authors conclude from their preliminary findings that high debt may influence choices for URM students.
The relationship between debt and career satisfaction has also been investigated. Results from a study of nearly 5,000 physicians that examined characteristics of those having second thoughts about their decision to pursue a career in medicine suggests that financial debt may contribute to feelings of dissatisfaction (Hadley et al., 1992). Results revealed that those most likely to have second thoughts were white women, blacks, and His-
panics, all of whom reported lower incomes, higher debt, and higher patient loads. The authors suggest a reexamination of the reliance of medical students, particularly minorities, on loans to finance their education.
Another important impact of student debt that may be overlooked is the effect on graduates’ lifestyle once they are in the workforce. Repayment is made with after-tax dollars and graduates must earn more than what is owed. While debt levels have grown, resident salaries have remained relatively stable (American Medical News, as cited in Johnson, 2002b). Based on the average house staff salary (1999–2000) of $36,928 in the northeast United States, a URM medical student with $105,136 in school debt would have only $737 per month left to cover living and other expenses after making the monthly loan payment. Six years post graduation with an annual salary of $43,045, a URM student with the same level of debt would have $1,079.25 left after making the monthly payment. Consolidating and extending payments 20 years would leave $1,490.78 (Johnson, 2002b). It is important to note that women, who constitute half of the physician workforce, make less, on average, than men. In 1998 the median net earnings for women was $123,390 compared to $171,800 for men (Johnson, 2002b). Thus, women may have more difficulty managing debt.
Students in other disciplines, such as dentistry, face similar circumstances. For example, in 1995 the average student loan debt of dental students (from private and public institutions) was $67,772. If these were all Federal Stafford Loans with relatively low interest rate of 7.66 percent (at that time), students would need an annual income of $121,554 to manage this debt (Myers and Zwemer, 1998). While debt has increased at a rate greater than the growth of the economy, income of dental practitioners has increased at a level lower than the growth of the economy (Myers and Zwemer, 1998). The authors suggest that students will need to have successful practices early on to manage their repayment and that debt can make it difficult for students to consider careers in education because of the salaries of starting faculty.
It has been reported that many students do not think about or plan for debt management (Johnson, 2002b; Lofton, 2002; Zeigler, 2003). Students are encouraged to adjust their lifestyles to help ensure that they can manage their debt once they enter practice. Strategies include keeping spending at a minimum, understanding the consequences of delinquent payments and default, understanding terms of grace periods and methods for deferment, understanding choices for repayment, keeping good financial records, seeking professional financial help if needed, and maintaining a good credit report (Johnson, 2002a). The impact of debt can be quite substantial in the short and long term. Students should be encouraged to plan carefully when financing their education and to consider a range of options that are available for paying these sizeable costs.
SOURCES OF FINANCIAL ASSISTANCE FOR STUDENTS PURSUING EDUCATION BEYOND COLLEGE
Like students entering college, most students who pursue education beyond the college level rely on grants and loans to finance their education. Among students making choices about attending graduate school, URM students were more likely to have borrowed to finance their undergraduate education (Heller, 2001) and to face unpaid debts related to undergraduate education while in graduate school. Nettles (1990) estimated that 46 percent of African American and 43 percent of Hispanic graduate students had unpaid undergraduate student loans compared to 36 percent of white students.
Millet and MacKenzie (1995) investigated the role of financial aid in the education of minority doctoral students using a subset of the 1989–1990 National Postsecondary Student Aid Survey. Results indicate that minority students were more likely to take out loans and receive fellowships than nonminority students. However, minorities were less likely to receive administrative assistantships. This latter finding is a significant area of concern, as Nettles (1990) and others suggested that assistantships may be particularly important for student integration, socialization, and persistence.
National-level data indicate that students who pursue their education beyond the college level tend to rely heavily on loans. Data from the 1999–2000 National Postsecondary Student Aid Study report on the financing used by 2.7 million masters, doctoral (Ph.D., Ed.D., Doctor of Business Administration [D.B.A.], Doctor of Public Administration [D.P.A.], and Doctor of Fine Arts [D.F.A.]), and professional (allopathic medicine, osteopathic medicine, dentistry, law, optometry, pharmacy, podiatry, veterinary medicine, chiropractic, theology) students across the country. Among the 2.7 million students, 12 percent were full-time professional students (of these, 27 percent were in medicine, and 29 percent were in dentistry and other health fields) and 13 percent were enrolled full-time in doctoral programs (U.S. Department of Education, 2002). Figures indicate that among full-time, full-year doctoral students, African American and Hispanic students were slightly more likely to receive any source of aid (Figure 3-12). Hispanic students received more grants and African American students took out more loans than students of other races or ethnicities. Figures were not available for American Indian, Alaska Native, Native Hawaiian, and other Pacific Islander populations.
Among professional students in the U.S. Department of Education survey (2002), African American, Hispanics, and those indicating their race as “other” received more loans, on average, than students of other racial and ethnic groups (Figure 3-13). Hispanic and those indicating “other race”
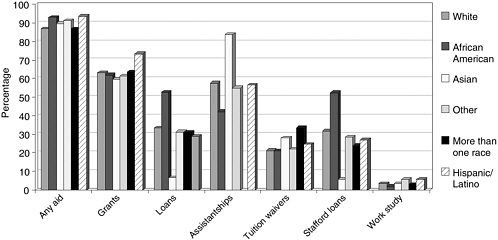
FIGURE 3-12 Percent of full-time, full-year doctoral students who received financial aid, by type of aid, race, and ethnicity.
SOURCE: Student Financing of Graduate and First-Professional Education, 1999-2000. U.S. Department of Education, 2002.
were also more likely to receive grants. Only a minority of all students received assistantships, tuition waivers, and work study.
FINANCING OF HEALTH PROFESSION EDUCATION
Financial Assistance for URM Students
Low-income URM individuals considering health professions education face increasing tuition and other costs, on top of the undergraduate debt they have likely accrued. The thought of accumulating debt in excess of $100,000 can be daunting and serve as a barrier for prospective students. There are several programs that provide financial assistance for students indirectly by giving funds to institutions to recruit URM students. A handful of programs provide assistance directly to students through scholarships, loans, or loan repayment programs.
Financial assistance for health professions students is provided by the federal government, states, and private sources. The paper prepared by Matherlee (this volume) provides a more detailed review of many of these federal and state programs. This section discusses a sample of public and private initiatives that seek to improve the representation of URM students in health professions education through the provision of financial assistance. This section is not meant to represent a comprehensive inventory of
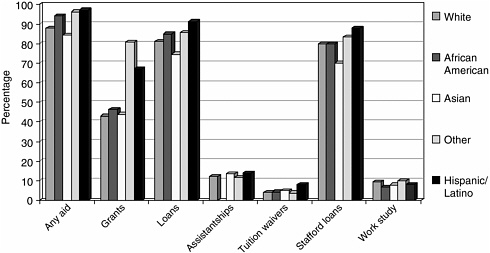
FIGURE 3-13 Percent of full-time, full-year first-professional students who received financial aid, by type of aid, race, and ethnicity.
SOURCE: Student Financing of Graduate and First-Professional Education, 1999–2000. U.S. Department of Education, 2002.
these mechanisms; rather, it highlights some prominent examples of efforts to provide financial aid.
Federal Sources of Financial Assistance
Table 3-1 lists some of the largest federal health professions training programs that focus on increasing racial and ethnic diversity. At the federal level, the Health Resources and Services Administration (HRSA) is the primary funder for health professions programs that either target or predominantly include URM students, practitioners, and/or faculty. HRSA is charged with administering Title VII and Title VIII of the Public Health Service Act. These titles authorize funding, through a variety of programs for students and institutions, in order to increase the quality of the education and training of the primary care provider workforce, including the geographic, racial and ethnic diversity of the United States health-care workforce. Title VII applies to medicine and dentistry (and in many cases mental health), while Title VIII pertains to nursing.
Within HRSA’s Bureau of Health Professionals (BHPr), the Division of Health Careers Diversity and Development administers Title VII programs. The Health Careers Opportunities Program (HCOP) (http://bhpr.hrsa.gov/diversity/hcop/default.htm) is the most extensive of the division’s programs.
TABLE 3-1 Examples of Federal Funding for Health Professions Programs with the Goal of Increasing Diversity
|
Agency |
Division |
Program |
Funding provided to: |
|
HRSA, BHPr |
Division of Health Professions Diversity |
Centers of Excellence (COE) |
Institutions |
|
|
|
Health Careers Opportunities Program (HCOP) |
Institutions |
|
|
|
Minority Faculty Fellowship Program |
Institutions |
|
|
Division of Nursing |
Nursing Workforce Diversity Program |
Institutions |
|
|
Division of Health Careers Diversity and Development |
Scholarships for Disadvantaged Students |
Institutions |
|
|
|
Loans for Disadvantaged Students |
Institutions |
|
|
|
Disadvantaged Faculty Loan Repayment |
Individuals |
|
|
National Health Service Corps (NHSC) |
Scholarship |
Individuals |
|
|
|
Loan repayment program |
Individuals |
|
Indian Health Service |
|
Health Professions Scholarship Program |
Individuals |
|
NIMH & SAMHSA |
|
Minority Fellowship Program |
Institutions |
|
Purpose |
Disciplines included |
Funding |
|
Improve ability of schools to train URM students |
Medicine, Dentistry, Psychology, among others |
$32.7 mil (2002) |
|
Increase number of professionals from disadvantaged backgrounds to meet needs of the underserved |
Psychology, Dentistry, Medicine, among others |
$34.6 mil (2002) |
|
Matching funds to award fellowships to URM faculty |
Dentistry, Medicine, among others |
$280,857 (2002) |
|
Academic preparation activities, retention efforts, student stipends |
Nursing |
$6.2 mil (2002) |
|
Scholarship awarded to students based on financial need |
Nursing, Dentistry, Medicine, Psychology, among others |
$46.2 mil (2002) |
|
Loans awarded to students based on financial need |
Medicine, Dentistry, among others |
$16.2 mil (2002) |
|
Faculty serve at eligible health professions programs in exchange for loan repayment |
Psychology, Dentistry, Nursing, Medicine, among others |
$1.3 mil (2002) |
|
Students compete for educational scholarships and in return for this support they must agree to practice in high-need communities |
Dentistry, Nursing, Medicine, Psychology, among others |
$46.2 mil (2002) |
|
Professionals with qualifying educational loans compete for repayment. Clinicians also receive salary and some tax relief benefits |
Nursing, Medicine, Psychology, Dentistry, among others |
|
|
Scholarship support in exchange for service after graduation |
Medicine, Dentistry, Psychology, Nursing, among others |
$9.75 mil (grants) (2002) |
|
Scholarship awarded to students |
Psychology, Nursing, Medicine (psychiatry), among others |
$3 mil (2001) |
Its purpose is to increase the number of health and allied health professionals from disadvantaged backgrounds. Medicine, dentistry, and clinical psychology are among the many professions targeted. Institutions receiving funds recruit individuals; provide counseling, mentoring, and other services to help retain students; publicize financial aid information; and engage in pipeline initiatives. The Centers of Excellence (COE) (http://bhpr.hrsa.gov/diversity/coe/default.htm) awards are designed to improve health professions schools’ ability to train underrepresented minority students. These grants provide funds to health professions schools with URM enrollments above the national average. Schools of dentistry, psychology, and medicine are included among eligible disciplines. Activities include minority faculty development, information resources, faculty and student research, and additional support for students in the form of stipends. The COE institutions also engage in a number of pipeline efforts. Another of the Division’s programs is the Minority Faculty Fellowships Program (http://bhpr.hrsa.gov/diversity/mffp/default.htm), whose goal is to increase the number of URM faculty at awardee institutions. The program awards 50 percent of salary funds, with the institution matching funds. Fellows are prepared to assume tenured faculty positions at the institution and also provide services in underserved areas.
Under Title VIII, The Division of Nursing, Nursing Workforce Diversity Program (http://bhpr.hrsa.gov/nursing) awards grants to institutions to increase the number of nurses from disadvantaged groups. Eligible institutions receive funds to support a variety of activities. In addition to pipeline efforts (for example, pre-entry preparations), activities include scholarships and retention activities, such as counseling, mentoring, and licensure preparation.
The BHPr also administers the National Health Service Corps (NHSC) (http://nhsc.bhpr.hrsa.gov), whose mission is to improve health care for medically underserved communities. NHSC has supported more than 2,700 clinicians and health care professionals who provide primary health care in medically underserved communities. The NHSC recruits nurse practitioners, certified nurse-midwives, dentists, mental and behavioral health providers, and primary care physicians, among others. A portion of HRSA’s funding is reserved to recruit professionals from disadvantaged backgrounds into the corps. Both scholarship and loan repayment programs are offered.
Other HRSA programs that provide funding include three within the Division of Health Careers Diversity and Development, Student Assistance Programs, which provide loans and scholarships to individuals from disadvantaged backgrounds. HRSA funds a variety of other programs, such as the Area Health Education Centers, Health Education and Training Centers, and Kids into Health Careers, that primarily target students before they reach health professions institutions.
The Indian Health Service (IHS) offers Scholarships for Health Professions Students (http://www.ihs.gov/JobsCareerDevelop/DHPS/Scholarships/Section_104.asp). Priority is given to graduate students and junior and senior students who are no more than four years away from completing their degree. Among the list of eligible disciplines, psychology, nursing, dentistry, and medicine are included. In exchange for scholarship awards, recipients are required to pay back one year of service for each year of support received. Service is provided to the IHS or in other designated communities and areas of need.
The National Institutes of Health and Substance Abuse and Mental Health Services Administration sponsor the Minority Fellowship Program, which supports the training and research of minority students in psychology and other disciplines. The primary goal of the program is to identify, select, and support the training of doctoral-level ethnic minority students and postdoctoral trainees in psychology, nursing, social work, and psychiatry who will make significant contributions to the mental health needs of ethnic and racial minorities. Psychology fellowships are administered by the American Psychological Association. (http://www.apa.org/mfp/pprograms.html). Programs are sponsored by the National Institutes of Mental Health (NIMH), National Institute on Aging (NIA), National Institute of Drug Abuse (NIDA), and the Substance Abuse and Mental Health Services Administration (SAMSHA). The program provides stipend support, ancillary training experiences, mentoring and career guidance, and access to a network of professional contacts. The amount of support varies, depending on federal allocations to the program and on cost-sharing arrangements that the program negotiates with universities.
Private Sources of Financial Assistance
Most funding available to URM students pursuing health professions education is provided by federal sources. A small amount comes from state, local, and private entities. This section reviews a sample of private sources providing funds to students, organizations, and institutions to increase the number of minorities in a variety of health professions (see Table 3-2). It was beyond the scope of the committee’s charge to provide an exhaustive list of private sources of student financial aid. Rather, several examples of these initiatives are presented here.
National Medical Fellowships, Inc. (NMF) (http://www.nmf-online.org) is a nonprofit organization dedicated to improving the health of underserved communities. They seek to increase the representation of minority physicians, educators, researchers, and policy makers in the United States and to train URM minority medical students to address the special needs of their
TABLE 3-2 Examples of Private Funding for Health Professions Programs with the Goal of Increasing Diversity
|
Source |
Program |
Funds provided to: |
Purpose/ Activities |
Disciplines Included |
|
National Medical Fellowships, Inc. |
|
Students |
Scholarships provided on a need-basis |
Medicine |
|
California Endowment |
Administered by Health Professions Education Foundation |
Students |
Scholarships and loan repayment |
Unspecified health professions |
|
California Wellness Foundation |
|
Organizations |
Scholarships, mentoring to support minorities |
Unspecified health professions |
|
W.K. Kellogg Foundation |
Administered by the American Dental Education Association |
Institutions |
Scholarships and financial aid; postdoctoral and fellowship support; faculty, student, and campus development |
Dentistry |
|
Ford Foundation |
Administered by the National Research Council Ford Foundation Fellowships for Minorities |
Students |
Stipends for predoctoral fellows and dissertation fellows |
Psychology |
communities. NMF provides funding to students in the form of need-based scholarships to first- and second-year medical students. Fellowship programs provide training opportunities in substance abuse research and treatment, HIV/AIDS care, violence prevention, biomedical research, community-based primary care, and health services research. A recent initiative, the NMF Fellows Academy, open to current NMF Scholars, provides programs to develop leadership skills, prepare for residency and careers, and expose fellows to role models and mentors who help guide their professional development.
The California Endowment (http://www.calendow.org), a statewide health foundation, awards grants to organizations that engage in activities
directly benefiting the health and well-being of the people of California. The mission of the California Endowment is to expand access to affordable, quality health care for underserved individuals and communities, and to promote fundamental improvements in the health status of all Californians. The Endowment recently provided a 3-year $500,000 grant to the Health Professions Education Foundation (http://www.healthprofessions.ca.gov), a nonprofit public benefit corporation established to provide financial assistance to health professional students throughout California who are willing to practice in medically underserved areas. The Foundation oversees the administration of two funds established by state legislation, the Health Professions Education Fund and the Registered Nurse Education Fund, and closely coordinates its programs with the Office of Statewide Health Planning and Development and its health professional education programs.
The funding received from the California Endowment will support up to 20 scholarships and loan repayment grants annually to underrepresented and economically disadvantaged health professions students who will practice in underserved areas of California. The Foundation offers a variety of other financial assistance programs, including the Associate Degree Nursing Pilot Scholarship Program (ADN), Registered Nurse Education Scholarship Program (BSN), and Registered Nurse Education Loan Repayment Program (LRP). Over the last nine years, the Foundation has given out scholarship and loan repayment awards totaling nearly $4.9 million dollars. The awards have helped approximately 1,100 economically disadvantaged and demographically underrepresented students pursue a career in the health professions.
The California Wellness Foundation (http://www.tcwf.org) has established as its mission to improve the health of the people of California by making grants for health promotion, wellness education, and disease prevention. Through its grants, the Foundation addresses the health needs of traditionally underserved populations, including low-income individuals, people of color, youth, and residents of rural areas.
Grants are provided that address diversity in the health professions workforce. Awards are commonly given to organizations that provide fellowships to support pipeline programs, scholarships, mentoring programs, internships and fellowships that support and advance career opportunities for people of color in the health professions, including allied health and public health professions. Organizations that support URM students in the health professions through strategic partnerships, leadership development, continuing education, and networking activities are also eligible for funding. In addition, the Foundation funds organizations that educate policy makers about public and institutional policies that promote diversity in the health professions. The Foundation’s Diversity in the Health Professions Priority Area Grants provide academic enhancement, financial support,
professional opportunities, and psychosocial support for those in nonspecified health professions.
The W.K. Kellogg Foundation (http://www.wkkf.org), a nonprofit organization whose mission is to apply knowledge to solve the problems of people, provides grants in several areas including health, higher education and efforts to capitalize on diversity. In 2001, the Foundation awarded a $1 million grant to the American Dental Education Association (ADEA) to help increase the number of minority students and faculty in the country’s dental schools. The ADEA awards grants to schools that distribute funds to students and faculty in the form of scholarships and financial aid, postdoctoral and fellowship support, or faculty, student, and campus development. Students may receive up to $5,000 per academic year.
The National Research Council Ford Foundation Pre-doctoral and Dissertation Fellowships for Minorities (http://www7.nationalacademies.org/fellowships/fordpredoc.html) seeks to increase the presence of underrepresented minorities on college and university faculties. The program is funded by the Ford Foundation and administered by the National Research Council of the National Academy of Sciences. The predoctoral fellowship provides support for 3 years in research-based programs in social and behavioral sciences, among other disciplines. Fellows receive stipend and funding toward tuition and fees. Dissertation fellows receive stipends. In 2002, the program made awards to 60 beginning graduate students, 41 students writing dissertations, and 29 recent Ph.D. recipients.
Broader Public Funding of Health Professions Training and Education
The federal health professions training programs described above are funded via discretionary funds and are therefore subject to annual appropriations struggles. One of the primary financing mechanisms for health professions education and training, funded via nondiscretionary funds, is Medicare Graduate Medical Education (GME), which is administered by the Center for Medicare and Medicaid Services (CMS) within the Department of Health and Human Services. Because educational activities enhance the quality of patient care, they are considered a part of the cost of patient care and are paid for, in part, by insurance programs. Medicare GME provides a significant source of funding for the costs of educating physicians and other health professionals. The large majority of this funding goes to hospitals for the training of physicians, with training of nursing diploma program graduates, dental professionals, and allied health professionals constituting a relatively minor role. Payments are made by commercial insurance and managed care companies, government programs such as Medicare and Medicaid, and other state and local appropriations (Knapp, 2002). Funds are paid to over 1,000 teaching hospitals. Direct GME funds
provide medical and dental resident salaries and benefits, hospital overhead related to training, and salaries and benefits of faculty who supervise residents. Indirect payments refer to those costs that are incurred by teaching hospitals as a result of teaching activities and are calculated through statistical analysis. Teaching hospitals receive an additional payment for each Medicare inpatient treated. In the past several years, issues regarding the needs of the workforce and the role of Medicare GME have been the subject of discussion by the Council on Graduate Medical Education (COGME) among others.
In contrast to medical education, dental schools and graduate programs in psychology are largely responsible for financing their clinical programs. As discussed in the previous section, tuition rates have increased substantially in the past 10 to 20 years as federal and state support for education has declined. For example, in 1973, the federal government provided support for 30 percent of dental education. However by 1997, the government supported only 0.9 percent of the dental enterprise (Hardigan, 1999). Expenses of running these programs have continued to exceed revenues. In order to compensate for these losses, dental schools have increased clinic income and tuition (Myers and Zwemer, 1998).
Do These Programs Increase URM Participation in Health Professions Education?
The critical question regarding these targeted public and private programs is whether they are, in fact, successful at significantly increasing the numbers of URMs in the health professions workforce. Does financial assistance provided to students allow them to succeed in completing their education and training? Evidence from college financial aid strategies suggests that the receipt of financial aid is important in determining whether low-income students will attend school. High college costs may reduce the retention of lower-income students, and those who are offered aid may be more likely to apply to college. Some evidence suggests that aid, particularly the receipt of grants, is an important predictor of attendance for students in the lowest income groups. While these issues have not been extensively examined among health professions students, recently researchers have attempted to evaluate components of public programs.
Two studies are cited by Grumbach and colleagues (2002) that attempted to evaluate BHPr programs. The first, an assessment of minority and disadvantaged programs, was conducted in 1994 by Houston Associates. Data collected by HCOP grantees, however, was inconsistent across programs, incomplete, or not able to be used, so that a useful assessment could not be made. The authors of this review offer several recommendations regarding effective ways to collect data so that the program’s activities
could be monitored and evaluated. Subsequently, an evaluation of COE awardees between 1993 and 1999 was conducted by Carline and colleagues (1999). Again, a meaningful assessment was not possible because of inconsistent data collection. To address this deficiency, Carline and colleagues developed a data collection system, including narrative and other objective evidence, such as number of applicants, enrollees, and graduates; demographic characteristics of students; sponsored faculty; amount and dispersment of funding; and research and other activities and experiences of COE faculty and students. While a rigorous evaluation was prohibited by the lack of baseline data and comparison groups, results suggested that many of the COE objectives had been met.
While this chapter has focused on HRSA programs that target minority and disadvantaged students, HRSA’s Title VII, Section 747 programs, which focus on the education and training of the primary care provider workforce more generally, have increased the number of graduates who practice in underserved communities and who are members of racial and ethnic minority groups (Advisory Committee on Training in Primary Care Medicine and Dentistry, 2001). In a report to the Department of Health and Human Services (HHS) and Congress, the Advisory Committee reported that graduates of these programs (in family medicine residency, general dentistry, physician assistant, and general internal medicine/pediatric residency programs) are three to ten times more likely to practice in medically underserved communities. In addition, these programs graduate two to five times the number of minority and disadvantaged students than other programs.
The BHPr also employs funding factors that increase the likelihood that its grants will be awarded to programs that enroll significant numbers of students from minority and disadvantaged backgrounds. While these are not direct strategies to increase diversity, they may indirectly achieve this goal. As with other BHPr activities, it is difficult to assess the impact of such strategies. Grumbach and colleagues (2002) speculate that these strategies may be less effective for increasing the overall pool of URMs in health professions when employed for funding of residency training, since these programs are competing for a finite pool of URM students already enrolled in schools. Rather, funding factors may be more effective for predoctoral education, but the authors note that the amount of funding is not large enough to make a substantial change. It has also been suggested that while requirements for BHPr programs to collect data on race and ethnicity of students and trainees are important in measuring efforts to increase diversity, there is no evidence that collecting this data encourages institutions to improve recruitment efforts (Matherlee, this volume).
The General Accounting Office (GAO) provided an assessment of Titles VII and VIII programs and provided testimony for congressional reauthori-
zation of the programs in 1997 (GAO, 1997). The office concurred with other assessments that the effectiveness of these programs is difficult to evaluate. The GAO found that Titles VII and VIII supported a wide range of objectives without common goals, outcome measures, and reporting requirements and noted that HHS was not required to evaluate their programs. Furthermore, GAO noted that the programs were not linked to improvements in the supply, distribution, and minority of health professionals. Evaluations of some of the programs measured outcomes for particular institutions as opposed to the national impact. Some institutions receiving grants reported on program process as opposed to outcomes (for example, a report was provided on how the institution established recruitment strategies and not the number of students recruited through the activity). The GAO report concluded by stating that “if these programs are to specifically improve supply, distribution, and minority representation for health professionals, federal efforts need to be directed to activities that clearly support those goals and whose results can be measured and reported in terms of those goals…. [O]nce goals are defined, performance measures and targets are critical to determine when federal intervention is no longer required, or when federal strategies are not successful and should be redirected” (GAO, 1997, pp. 6–7).
Another concern critics have raised regarding some of the BHPr’s programs is that program payback requirements often “track” students into specialty areas without the flexibility to expand or change these areas. This may dissuade some students from participating in these programs. It may be beneficial to explore potential options for increasing flexibility of HRSA programs to allow students to explore more specialty options.
In summary, little is known about the efficacy of financial aid programs in increasing URM participation in health professions. Evidence suggests that components of BHPr activities may meet program goals. However, comparisons of programs and knowledge of best practices are lacking. Policy makers have a substantial need to obtain data to evaluate how well various programs that provide financial assistance to students succeed in recruiting and retaining URM students. The National Center for Health Workforce Analysis and its regional centers, which collect and analyze health profession data and evaluate health professions training programs, among other efforts, have made a significant step toward collecting data at the state level (Matherlee, this volume).
Recommendation 3-1: HRSA’s health professions programs should be evaluated to assess their effectiveness in increasing numbers of URM students enrolling and graduating from HPEIs to ensure that they maximize URM participation.
THREATS TO HEALTH PROFESSIONS FINANCING
In the current environment of federal, state, and local budget deficits and reduced endowments of many foundations, programs that support URM access to and success in health professions education programs may be threatened. Matherlee (this volume) cites seven factors that may impede public efforts to increase diversity in the workforce via financing of training and education at the institutional and policy level:
-
Much of the emphasis of programs and funding of educational efforts is on increasing the pipeline of URM students, rather than supporting students in higher education.
-
Most federal health professions training funds rely on discretionary funding, making them vulnerable to cuts.
-
Discretionary funds are “siloed” in various agencies and division within the government, making coordination of funding and communication about the shared goal more difficult. This may also reduce the ability of students to become familiar with career options and paths across disciplines and limit student awareness of varied funding opportunities.
-
The Medicare GME program lacks workforce goals regarding URM participation.
-
There is considerable variation among states in the use of funds to increase URM participation in the workforce.
-
High debt incurred by health professions students may disproportionately hurt URM participation.
-
Policy makers are reluctant to fund new URM initiatives because of federal and state budget deficits.
Several avenues have been discussed for using financial incentives to increase URM participation in health professions education, including the collection of data on various programs and efforts, the use of Medicare GME to develop new policy approaches, and expansion of the NHSC. Evidence from undergraduate education suggests that students may benefit from increased knowledge about the various sources of financial assistance and the provision of grant-based aid rather than loans.
Recommendation 3-2: Congress should increase levels of funding for diversity programs and strategies shown to be effective in ensuring diversity within the National Health Service Corps and Titles VII and VIII of the Public Health Service Act. Furthermore, Congress should develop other financial mechanisms to enhance the diversity of the health-care workforce. This may include exploring changes in Medicare GME to increase URM participation in medicine, psychology, dentistry, and nursing.
RETHINKING THE FINANCING OF HEALTH PROFESSION EDUCATION
The large variety and scope of public and private efforts for funding URM students in health profession education programs make it difficult to assess if and how well funding programs work together and complement one another to expand opportunities for URM participation. While there are many programs targeting URM students who are entering graduate education, many of these same programs as well as a host of others also engage in pipeline enhancement efforts. Grumbach and colleagues note that the result of this compilation of programs is “a discontinuity of interventions across regions and across stages of the educational pipeline, making it difficult to sustain gains from one educational stage to the next” (Grumbach et al., 2002, p. 71). They conclude that coordination and communication among various programs will assist funders to better plan their own efforts and determine additional needs, and that the formation of coalitions of funders may facilitate these goals.
Another area of need identified by Grumbach et al. (2002) is the relative amounts of funding for various health professions disciplines. For example, in FY 2003, Title VII programs received $308.4 million and Title VIII programs received $112.8 million. As discussed in Chapter 1, the nursing profession has reached a critical shortage in its workforce.
An area in need of further exploration in terms of URM student participation in health profession education is the impact of institutional funding programs, policies, and perspectives dealing with URM access. At the institutional level, many students are funded based on need alone and many URM students are funded based on need and ethnicity. The effect of these funding policies on URM student access is an important area that should be investigated further.
While there are barriers for financial aid programs due to larger scale funding or political priorities, some public and private entities have developed innovative ways of using financing as a lever to increase the number of URMs in health professions programs. One new model for education funding is through a unique public–private partnership. The University of Colorado Health Sciences School of Dentistry has partnered with the Orthodontic Education Company (OEC) to establish a new dental center that they hope will address the shortage of orthodontists and provide low-cost care to children in underserved areas (see Box 3-1). The OEC provides scholarships and stipends in exchange for service in OEC private or group practices following graduation. The University of Colorado will establish and administer the program, which will involve the investment of almost $100 million by the OEC. This type of partnership may be an innovative way to deal with an anticipated shortage of orthodontists as well as a variety of
other health professionals in the next decade and finance education while reducing the burden on taxpayers, students, and parents.
A second program at the University of Colorado, legislated by the state, provides community-based learning experiences for students. The Advanced Clinical Training and Service Program, treats the oral health needs of disadvantaged citizens of Colorado (Box 3-2). The program may help to increase diversity by not only generating, among youth served, interest in dental careers, but drawing prospective health professions students through the availability of community-based learning.
As an example from the field of pharmacy, CVS provides a Scholarship of Excellence, a program in which CVS interns apply to receive $5,000 per academic year for a maximum of 4 years. For each year the scholarship is received, students commit to work full-time for 1 year as a CVS registered pharmacist.
In other efforts, New York State has initiated the Minority Participation in Medical Education Grant Program, which provides funds to institutions to enhance minority recruitment and retention, develop minority student mentoring programs, develop medical career pathways for minority
|
BOX 3-1 In January 2003, the School of Dentistry at the University of Colorado and the Orthodontic Education Company (OEC) initiated a 30-year business partnership with a $3 million gift and $92.7 million commitment from OEC to build the Lazzara Center for Oral–Facial Health and establish a training program in orthodontia. The partnership will help to address the anticipated shortage of orthodontists and help to provide low-cost care for low-income, minority, and underserved children in the state of Colorado. It is hoped that qualified students from diverse and economically disadvantaged backgrounds, for whom costs of dental education may be prohibitive, will consider dental specialties as a result of the scholarships. It is also hoped the program will have an indirect benefit of increasing diversity in dentistry by exposing underserved children to the profession through the program’s services. Each year, the OEC will sponsor 12 of the 16 students that the Center will train. These students will receive a $30,000 salary, benefits, malpractice insurance, tuition, and additional funds for instruments and computers. In exchange for sponsorship the students will commit to practice for 7 years postgraduation at OEC sites throughout the country, earning a salary of $150,000 per year. The school will establish admission criteria, curriculum, and academic standards for graduation. Selected residents will have to meet criteria established by the admissions and chair of orthodontics. In addition, the school will follow accreditation procedures set for by the Commission on Dental Accreditation for a specialty program in orthodontics (Landesman, 2003). |
|
BOX 3-2 The Advanced Clinical Training and Service (ACTS) program at the University of Colorado School of Dentistry is a community-based service learning program. This program was legislated by the state of Colorado. Students perform the equivalent of one academic year of direct service, under supervision, to underserved communities in Colorado. Training sites include community health clinics, hospital-based practices, and private practices. Supervision is provided by community dentists who are also faculty members (Landesman, 2003). There are two required rotations for the program. The first, Integrated Care Clinics, provides treatment for older adults and those with HIV or who are mentally and physically challenged. The second rotation involves service provision in rural dental practices. Students choose other rotations in clinics for underserved populations across the state (University of Colorado School of Dentistry, 2003). These experiences in underserved communities help students to increase self-confidence in their clinical skills, promote greater independence, and enhance students’ sense of personal responsibility. As with the university’s business partnership with OEC, it is hoped that ACTS will help to promote diversity in the health professions by drawing students who are interested in serving disadvantaged populations and exposing those who receive the services to the field of dentistry. |
students, and develop minority faculty role models (New York State Office of the Governor, 2002; Stoll, 2003). Funds were provided to seven institutions across the state. There have been no published reports assessing the program’s results or whether certain approaches have been successful in recruiting and retaining minority students. However, the state announced in 2002 that over 155 minority students participated in medical school and residency programs sponsored by the programs in the previous year.
Programs such as the ones outlined in this section may serve as models for ways to use public and private funds to increase diversity of the healthcare workforce. While much of the funding for health profession education is from public sources, private sources can also contribute and have much to gain by investing in diversity. Joint investments made by business, states, the federal government, foundations, and institutions will be crucial in this effort.
Recommendation 3-3: State and local entities, working where appropriate with HPEIs, should increase support for diversity efforts. This may be accomplished via a variety of mechanisms in programs committed to diversity, such as loan forgiveness, tuition reimbursement, loan repayment, GME, and supportive affiliations with community-based providers.
Recommendation 3-4: Private entities should be encouraged to collaborate through business partnerships and other entrepreneurial relationships with HPEIs to support the common goal of developing a more diverse health-care workforce.
SUMMARY
URM students may face sizeable financial barriers as they consider health professions education. The disparity between URM and non-URM family incomes is significant, leaving minority students with fewer financial resources to attend college and health profession schools. The costs of both college and health professions education have increased sharply, while the availability of sufficient need-based aid has decreased, leaving students with higher unmet need and record levels of debt. College tuition trends have prompted the College Board to call for colleges and universities to reaffirm their commitment to need-based aid and for the federal government to increase support to institutions that serve large percentages of high-need students.
While the impact of financial barriers has not been well studied among health professions students, evidence from undergraduate education reveals that low-income students and some URM students may be less likely to apply to college and that aid, particularly grants, may be associated with increased attendance for low-income students.
There are a variety of public and private sources of financial assistance for health professions students, through the provision of scholarships, loans, and loan repayment programs. Most provide funds to institutions that, in turn, make awards to students. The distribution of these funds vary across disciplines, with nursing Title VIII programs receiving significantly less funding than Title VII programs. In addition, these federal programs are funded via discretionary funding and are vulnerable to cuts. It is difficult to assess the impact of these programs on increasing diversity in the health professions workforce, as the scopes of the programs are broad, outcome measures are not clearly specified, and evaluation is not required. The primary source of funding, provided for with mandatory funds, is Medicare Graduate Medical Education (GME). GME dollars have not been tied to efforts to increase the representation of URMs in the health-care workforce.
The high debt incurred by health professions students, reliance on discretionary funding for minority programs, lack of coordination and communication among funding sources, and lack of workforce goals in Medicare GME are among the barriers for the use of financing to increase diversity in the health professions workforce. In addition to a reexamination of existing programs, new and innovative strategies are necessary. Recent efforts have included, for example, partnerships between institu-
tions and private business, which reduce the burden on taxpayers and families. Reexamining the structure of financing programs, systematically measuring outcomes, and exploring new ways to help URM students finance their education will be crucial in increasing diversity in the health professions workforce.
REFERENCES
Advisory Committee on Student Financial Assistance. 2001. Access Denied: Restoring the Nation’s Commitment to Equal Educational Opportunity. Washington, DC: Advisory Committee on Student Financial Assistance.
Advisory Committee on Student Financial Assistance. 2002. Empty Promises: The Myth of College Access in America. Washington, DC: Advisory Committee on Student Financial Assistance.
Advisory Committee on Training in Primary Care Medicine and Dentistry. 2001. Comprehensive Review and Recommendations: Title VII, Section 747 of the Public Health Service Act. Report to Secretary of the U.S. Department of Health and Human Services and Congress. [Online]. Available: http://bhpr.hrsa.gov/medicine-dentistry/actpcmd1.htm [accessed October 1, 2002].
American Psychological Association (APA) Research Office. 2001. Analysis of Data from Graduate Study in Psychology: 1999–2000. By WE Pate II. [Online]. Available: http://research.apa.org/grad00contents.html [accessed August 5, 2003].
Association of American Medical Colleges (AAMC). 2002. Minority Students in Medical Education: Facts and Figures XII. Washington, DC: Association of American Medical Colleges Division of Community and Minority Programs.
Association of American Medical Colleges (AAMC). 2003. Tuition and Student Fees Reports. [Online]. Available: https://services.aamc.org/tsf/TSF_Report/report_intro.cfm [accessed August 5, 2003].
Baker LC, Barker DC. 1997. Factors associated with the perception that debt influences physician’s specialty choices. Academic Medicine 72(12):1088–1096.
Baum S, O’Malley M. 2002. College on Credit: How Borrowers Perceive Their Education Debt. Results of the 2002 National Student Loan Survey. Braintree, MA: Nellie Mae Corporation.
Brotherton SE. 1995. The relationship of indebtedness, race, and gender to the choice of general or subspecialty pediatrics. Academic Medicine 70(2):149–151.
Carline JD, Patterson D, Mandel L. 1999. Methodology Development and Assessment of the Impact of the Centers of Excellence Program. Prepared for the Division of Disadvantaged Assistance, Bureau of Health Professions, Health Resources and Services Administration, Public Health Service, HRSA 240-91-0045.
Choudhury S. 2002. Racial and Ethnic Differences in Wealth and Asset Choices. Social Security Bulletin 64(4). [Online]. Available: http://www.ssa.gov/policy/docs/ssb/v64n4/v64n4p1.pdf [accessed October 2, 2003].
College Board. 2000. Trends in College Pricing. Washington, DC: College Board.
College Board. 2003. Challenging Times, Clear Choices: An Action Agenda for College Access and Success. Investing More Equitably and Efficiently in Higher Education, Creating Value for America. Washington, DC: College Board.
Colquitt WL, Zeh MC, Killian CD, Cultice JM. 1996. Effect of debt on U.S. medical school graduates’ preferences for family medicine, general internal medicine, and general pediatrics. Academic Medicine 71(4):400–411.
DeAngelis SL. 2000. Tuition, financial aid, debt, and dental student attrition. Journal of Student Financial Aid 30(2):7–21.
General Accounting Office (GAO). 1997. Health Professions Education: Clarifying the Role of Title VII and VIII Programs Could Improve Accountability. Testimony by Bernice Steinhardt, Director Health Services Quality and Public Health Issues Health, Education, and Human Services Division before the Subcommittee on Public Health and Safety, Committee on Labor and Human Resources, U.S. Senate. GAO/T-HEHS-97-117. [Online]. Available: http://www.gao.gov/archive/1997/he97117t.pdf [accessed September 5, 2003].
Georges A. 1999. Keeping what we’ve got: The impact of financial aid on minority retention in engineering. National Action Council for Minorities in Engineering Research Letter 9(1):1–20.
Grumbach K, Coffman J, Muñoz C, Rosenoff E, Gándara P, Sepulveda E. 2002. Strategies for Improving the Diversity of the Health Professions. University of California, San Francisco: Center for California Health Workforce Studies.
Hadley J, Cantor JC, Willke RJ, Feder J, Cohen AB. 1992. Young physicians most and least likely to have second thoughts about a career in medicine. Academic Medicine 67(3):180–190.
Hardigan, J. 1999. The costs and financing of dental education. Journal of Dental Education 63(12):873–881.
Heller D. 2000. The Role of Race and Gender in the Awarding of Institutional Financial Aid. Paper presented at the Annual Meeting of the American Educational Research Association. New Orleans.
Heller D. 2001. Debts and decisions: Student loans and their relationship to graduate school and career choice. Lumina Foundation for Education. New Agenda Series 3(4):2–50.
Heller DE. In press. State Student Aid. The Condition of Access. Washington, DC: Advisory Committee on Student Financial Assistance.
Houston Associates. 1994. Evaluation of the Health Careers Opportunity Program Summer Programs Final Report. Silver Spring, MD: Health Resources and Services Administration, Division of Disadvantaged Assistance.
Johnson L. 2002a. Financial planning for residency: Part 2. Journal for Minority Medical Students 14(3):17–20.
Johnson L. 2002b. Planning for residency: First do no harm. Journal for Minority Medical Students 14(2):40–46.
Knapp RM. 2002. Complexity and uncertainty in financing graduate medical education. Academic Medicine 77(11):1076–1083.
Landesman HM. 2003. Potential of Three Colorado Programs to Increase Access to and Interest in Dental Careers among Underrepresented Minorities. Presentation to Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Health Care Workforce, June 30, Washington, DC.
Lofton K. 2002. How med students’ indebtedness influences career choices. Journal for Minority Medical Students 14(2):47–48.
McPherson MS, Schapiro MO. In press. Institutional Student Aid: The Condition of Access. Washington, DC: Advisory Committee on Student Financial Assistance.
Millet C, MacKenzie S. 1995. An Exploratory Study of the Role of Financial Aid in Minority Doctoral Education. Paper presented at the Annual Meeting of the Association for the Study of Higher Education, Orlando, FL.
Mullan F. 1997. The National Health Service Corps and inner-city hospitals. Health Affairs 336(22):1601–1603.
Murray B. 1999. Some clinical psychology students’ growing debt burden triggers response from training programs. American Psychological Association Monitor Online 30(2). [Online]. Available: http://www.apa.org/monitor/feb99/debt.html [accessed August 18, 2003].
Myers DR, Zwemer JD. 1998. Cost of dental education and student debt. Journal of Dental Education 62(5):354–360.
National Science Foundation (NSF). 2000. Psychology Doctorate Recipients: How Much Financial Debt at Graduation? By AI Rapoport, J Kohout, M Wicherski. [Online]. Available: http://www.nsf.gov/sbe/srs/issuebrf/sib00321.htm [accessed August 18, 2003].
Nettles M. 1990. Black, Hispanic, and White Doctoral Students: Before, During and After Enrolling in Graduate School. Princeton, NJ: Educational Testing Service.
New York State Office of the Governor. 2002. Nearly $1 Million to Boost Minority Physician Training. Press Release April 19, 2002. [Online]. Available: http://www.state.ny.us/governor/press/year02/april19_1_02.htm [accessed January 16, 2004].
Nora A, Cabrera AF. 1996. The role of perceptions in prejudice and discrimination and the adjustment of minority students to college. Journal of Higher Education 67(2):119–148.
Rico M, Stagnaro-Green A. 1997. Debt and career choices of underrepresented minorities. Academic Medicine 72(8):657–658.
Rosenthal MP, Marquette PA, Diamond JJ. 1996. Trends along the debt-income axis: Implications for medical students’ selections of family practice careers. Academic Medicine 71(6):675–677.
St. John EP. 1994. Prices, productivity, and investment: Assessing financial strategies in higher education. ERIC Digest. EDO-HE-94-3.
Stoll B. 2003. Overview of the New York State Council on Graduate Medical Education. Boston, MA: Community Catalyst.
University of Colorado School of Dentistry. 2003. Advanced Clinical Training and Service Program. [Online]. Available: http://www.uchsc.edu/sd/sd/advanced.html [accessed September 5, 2003].
U.S. Census Bureau. 2002a. Historical Income Tables—Families. [Online]. Available: http://www.census.gov/hhes/income/histinc/f05.html [accessed August 14, 2003].
U.S. Census Bureau. 2002b. Money Income in the United States: 2001. Current Population Reports, P60-218. Washington, DC: U.S. Government Printing Office. [Online]. Available: http://www.census.gov/prod/2002pubs/p60-218.pdf [accessed September 3, 2001].
U.S. Department of Education. National Center for Education Statistics. 1997. Access to Postsecondary Education for the 1992 High School Graduates. NCES 98-105. By L Berkner, L Chavez. Project Officer CD Carroll. Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 1999. College Access and Affordability. Findings from The Condition of Education 1998. NCES 1999-108. Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 2000a. 1999–2000 National Postsecondary Student Aid Study (NPSAS: 2000). Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 2000b. Digest of Education Statistics, 1999. NCES 2000-031. Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 2002. Student Financing of Graduate and First-Professional Education, 1999–2000. Profiles of Students in Selected Degree Programs and Their Use of Assistantships. NCES 2002-166. By SP Choy, S Geis. Project Officer: AG Malizio. Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 2003a. Characteristics of Undergraduate Borrowers: 1999–2000. NCES 2003-155. By ME Clinedinst, AF Cunningham, JP Merisotis. Project Officer: CD Carroll. Washington, DC: U.S. Department of Education.
U.S. Department of Education, National Center for Education Statistics. 2003b. How Families of Low-and Middle-Income Undergraduates Pay for College: Full-Time Dependent Students in 1999–2000. NCES 2003-162. By SP Choy, AM Berker. Project Officer: CD Carroll. Washington, DC: U.S. Department of Education.
Valachovic RW, Weaver RG, Sinkford JC, Haden NK. 2001. Trends in dentistry and dental education. Journal of Dental Education 65(6):539–561.
Zeigler J. 2003. As tuitions rise, medical students struggle with excessive loans. New Physician 52(6):15–23.







































