Summary and Assessment1
The emergence of a novel human coronavirus in late 2002 alarmed populations across the globe, elicited a massive public health response, gave rise to a multinational research network, gripped the news media, wreaked political havoc in China, and struck a blow to the tourism and travel industries of several countries. By the time this coronavirus, labeled SCoV, apparently receded from human hosts in July 2003, nearly 10 percent of more than 8,000 individuals who fit the probable case definition had died of the disease now known as severe acute respiratory syndrome (SARS) (World Health Organization [WHO], 2003a). Analyses of this epidemic could lead to improvements in the global community’s preparedness for and response to future global outbreaks of infectious disease.2
For these reasons, the Institute of Medicine’s (IOM’s) Forum on Microbial Threats convened the workshop Learning from SARS: Preparing for the Next
|
1 |
The speed with which the SARS epidemic spread last year was matched by a similar swiftness in the rate at which the understanding of the disease and its effects evolved among scientists, public health officials, and other members of the global health community. For this reason, individual papers within this volume are likely to reflect different stages and perspectives from among the many attempts that have been made to assess the course of the epidemic at different times and places. In some cases, analyses of public health responses or variations in empirical data (such as the number of suspected SARS cases or SARS-related deaths) may reflect the fluid nature of these circumstances. For the most current updates on SARS and recommendations for clinicians and public health officials, readers are referred to the relevant websites of the WHO (http://www.who.int/csr/sars/en/) and the CDC (http://www.cdc.gov/ncidod/sars/). |
|
2 |
This report entered final production before the January 5, 2004, confirmation of the first SARS case since July 2003—explaining the references throughout the report to the uncertainty about the reemergence of the disease. |
Disease Outbreak on September 30 and October 1, 2003. Participants discussed the emergence, detection, spread, and containment of SARS; political responses to the epidemic; its economic consequences; basic research on coronaviruses; preparations for a possible reemergence of SCoV; and lessons learned from the SARS epidemic that could shape responses to future microbial threats.
This workshop summary does not contain consensus recommendations, nor does it represent a consensus opinion of the IOM Forum on Microbial Threats. Rather, it presents the individual perspectives and research of people who made presentations at the IOM workshop on SARS or who participated in workshop discussions.
While the workshop attempted to explore a range of issues that emerged from the SARS outbreak, it is important to recognize that neither the discussions nor this report provide an exhaustive survey of the body of knowledge about SARS. Some important issues not addressed through workshop discussions include analyses of modes of transmission in indoor environments, especially airplanes; consideration of major technological breakthroughs or new fields of inquiry that would significantly advance our ability to prevent and treat infectious diseases; and comparative analyses of actions and outcomes related to the public health responses of different countries.
It should also be noted that considerable effort was made to engage the participation of more Chinese colleagues in the presentations and discussion of the workshop. The short time during which the workshop was organized made it very difficult for Chinese counterparts to obtain the necessary travel visas. Contributions from Chinese participants were important to the workshop as were additional phone and email consultations to the development of this report.
The following text summarizes what transpired during the workshop and assesses how the world’s experience with SARS could potentially guide preparations by the public health community, researchers, and policy makers for future outbreaks of infectious disease.
OVERVIEW OF THE SARS EPIDEMIC
SARS is unremarkable in certain ways among infectious diseases. For example, the transmission rate of SCoV pales in comparison with those of other known microbial threats, such as influenza, but appears to be similar to that of smallpox. Despite nationwide vaccination campaigns against influenza in the United States, an average of 36,000 U.S. residents die annually from influenza infections—nearly 50 times more people than the number killed by SARS worldwide (Centers for Disease Control and Prevention, 2002).
Yet the quality, speed, and effectiveness of the public health response to SARS brilliantly outshone past responses to international outbreaks of infectious disease, validating a decade’s worth of progress in global public health networking. Thus, in several respects, the SARS epidemic reflected fundamental
improvements in how the world responds to an outbreak of infectious disease; and at the same time, highlights the continuing need for investments in a robust response system that is prepared for the next emerging disease—whether naturally occurring or intentionally introduced.
The World Health Organization (WHO) deserves credit for initiating and coordinating much of this response through its Global Outbreak Alert and Response Network (GOARN), as do the partner organizations comprising 115 national health services, academic institutions, technical institutions, and individuals. In the future, this public health network—originally developed to manage outbreaks of influenza and other infectious diseases—ideally will encompass more partners and have the capacity to handle outbreaks of greater magnitude than SARS. Nevertheless, it is clear that multinational, collaborative, and coordinated surveillance, research, and containment measures greatly limited the spread of SCoV.
Despite the low transmission rate of SCoV and the relatively low number of SARS deaths compared to other infectious diseases, SARS had a remarkably powerful and negative psychological impact on many populations worldwide. The relatively high case fatality rate, the identification of superspreaders, the newness of the disease, the speed of its global spread, and public uncertainty about the ability to control its spread may have contributed to the public’s alarm. This alarm, in turn, may have led to behavior that exacerbated the economic blows to the travel and tourism industries of the countries with the highest number of SARS cases.
In addition, the SARS epidemic starkly outlined the benefits and dangers of the impact of globalization on infectious disease. The ease and frequency of international travel facilitated the swift spread of SCoV infections to 5 countries within 24 hours and to more than 30 countries on 6 continents within 6 months (WHO, 2003a). Likewise, the increased migration of workers from rural to urban areas within their home country or into different countries (and continents) has increased the risk that new and previously unrecognized viruses will become established in worldwide human populations.
Yet at the same time, worldwide telecommunications networks facilitated collaborative research among 11 geographically distinct laboratories, helping them to identify this new infectious agent in just 1 month. The news media, individuals, and public health organizations disseminated information about SARS almost in real time, influencing behavior that helped limit the spread of the virus. It was also suggested that this information ultimately created heightened awareness and pressure within the Chinese government and public to take action against the SARS and to engage with the global efforts of research, prevention, and containment.
A complex set of factors underlies the emergence and spread of microbial threats. The extraordinary capacity of microbes to change and adapt, the disruption of human and microbial environments, and the activities that expose humans
November 2002: First case of SARS occurs in Guangdong Province, China.
|
November |
January |
|
2002 |
2004 |
to new microbes all play a role. The convergence of these and other factors lead to the emergence of infectious diseases, as illustrated in Figure S-1.
Emergence of SARS
Such a convergence likely occurred during late 2002 in southern China, where merchants and farmers took small wild mammals from their native environments to local markets and sold both slaughtered and live animals for human consumption. Some of these mammals most likely carried a coronavirus resembling SCoV (Guan et al., 2003). The likelihood of human exposure to the virus is quite high when the crowded and relatively unsanitary conditions of these markets are considered. As a result, SARS emerged in the southern Chinese province of Guangdong in late 2002. The index case, retrospectively identified on November 16, occurred in the city of Foshan; by mid-December, SARS had appeared in two additional cities in the province.
An expert team from the provincial government and the national Ministry of Health went to the city of Zhongshan to investigate one of these outbreaks. The team concluded on January 21, 2003, that the infection was atypical pneumonia probably caused by a viral agent. The team recommended measures for the prevention and treatment of infection and suggested that a case reporting system be established to monitor the disease. The investigative team’s findings were reported to every hospital in the province. Unfortunately, the reporting of these findings coincided with the Chinese New Year holiday. This compounded the challenge for early intervention against the disease in two ways: the report did not receive significant attention from health officials on leave; and the opportunities for disease spread were greatly enhanced by the travel that often accompanies the celebration of the New Year.3 Additionally, as we discuss later in this chapter, the medical community’s understanding of the true etiology of SARS was delayed significantly by a February announcement from a senior scientist at the Chinese Center for Disease Control that he suspected the infectious agent was Chlamydia—a commonly understood bacterial agent that would not have warranted heightened concern or investigation.
January 21, 2003: Guangdong provincial investigators report on “atypical” pneumonia.
January 31, 2003: First super-spreading SARS patient.
|
November |
January |
|
2002 |
2004 |
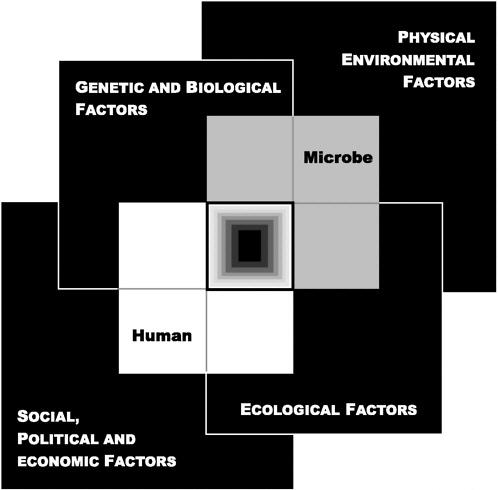
FIGURE S-1 The Convergence Model. This diagram illustrates how four factors that influence the interaction between humans and microbes may converge in such a way that an infectious disease emerges (central box). The interior of the central box is black, representing the unknown influences on emergence, and the lightening to white at the edges of this box represents the known influences.
SOURCE: IOM (2003).
February 11, 2003: Chinese Ministry of health reports to WHO on respiratory disease in Guangdong.
|
November |
January |
|
2002 |
2004 |
On January 31, the first hyperinfective, or superspreading, case of SARS occurred in the city of Guangzhou. The patient was transferred among three hospitals and infected an estimated 200 people, many of them hospital workers.
As these events unfolded, the international public health community began to receive news of the outbreak through e-mails, Internet chat rooms, and local media outlets, whose reports were widely disseminated through electronic reporting systems such as the Global Public Health Intelligence Network (GPHIN) and Pro-MED mail (Eysenbach, 2003). Based on this information, WHO queried the Chinese government on February 10 and received a response the following day describing an outbreak of an acute respiratory syndrome involving 305 cases and five deaths in Guangdong Province (WHO, 2003b).
Some of the most severe SARS symptoms were suffered by residents of the Amoy Gardens apartment towers in Hong Kong during an outbreak in late March that sickened more than 300 people (WHO, 2003c). Rather than its usual route of transmission by respiratory droplets, the virus is thought to have spread via aerosolized fecal matter through the internal sewer system of the apartment complex (WHO, 2003f). Consequently, on March 31, Hong Kong’s health authorities issued an unprecedented quarantine order to halt the spread of SARS on the island, which required some residents of the housing complex to remain in their apartments until midnight of April 9 (10 days later) (WHO, 2003c).
Spread of the SARS Coronavirus Beyond China
Epidemiological investigations revealed that the spread of SCoV outside China began on February 21, 2003, when 12 people staying in the Metropole Hotel in Hong Kong contracted SCoV from an infected, symptomatic physician from Zhongshan University (see Figure S-2). These 12 people subsequently carried the infection with them to Singapore, Vietnam, Canada, Ireland, and the United States—initiating chains of infection in all of these countries except for Ireland. According to WHO estimates, most of the more than 8,000 probable cases of SARS worldwide originated with this superspreader (WHO, 2003a).
Vietnam
Dr. Carlo Urbani, a WHO infectious disease specialist based in Vietnam, reported concerns about a patient in the Hanoi French Hospital with a high
February 18, 2003: Senior microbiologist at Chinese Center for Disease Control announces he suspects the disease is Chlamydia.
|
November |
January |
|
2002 |
2004 |
fever and atypical pneumonia to WHO’s Western Pacific office on February 28 (WHO, 2003c). Responding to Dr. Urbani’s alert and other reports of atypical pneumonia in Vietnam and Hong Kong, WHO sent GOARN teams to Hong Kong and Hanoi to join the investigative and containment efforts already underway. The early detection of SARS in Vietnam, prompt sharing of that information with the international community, and aggressive containment efforts by the Vietnamese government, in partnership with a GOARN team, enabled
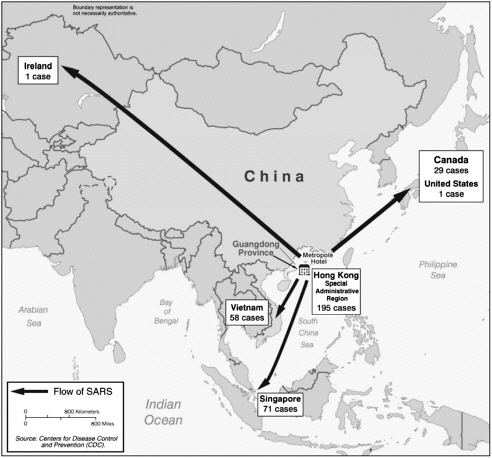
FIGURE S-2 Portrait of a superspreader: spread of SARS from the Metropole Hotel in Hong Kong as of March 28, 2003.
February 21, 2003: Worldwide epidemic begins at Metropole Hotel, Hong Kong.
|
November |
January |
|
2002 |
2004 |
the Vietnamese to eradicate SARS by the end of April. This was accomplished before SARS was contained in either Canada or Singapore, despite Vietnam’s comparatively limited health care resources and lower education levels among its population. (Tragically, Dr. Urbani himself died of SARS.) It was suggested by workshop participants that containment of the disease in Vietnam was, in fact, aided by the absence of more sophisticated medical devices and facilities—such as mechanical ventilation by intubation, bronchoscopy, aerosolized medications, and large hospital facilities that exposed large numbers of individuals to undiagnosed SARS patients awaiting care—which have been identified as factors that promoted SCoV transmission considerably in Singapore and Toronto (Lee et al., 2003).
On March 12, WHO issued a global alert describing outbreaks of the yet-unnamed respiratory disease in Hong Kong and Vietnam and instituted worldwide surveillance (WHO, 2003d). A second alert on March 15 named the condition, listed its symptoms, and advised travelers to have a high level of suspicion of SARS and report to a health worker if they had SARS symptoms and had visited an area where SARS was known to be occurring. Two further alerts provided recommendations for airports to screen passengers and for travelers to avoid areas where SARS had been detected, respectively (WHO, 2003e).
Canada
Canada’s experience with SARS illustrates the importance of identifying and isolating every infected individual in stemming the spread of the disease. There, the index patient returned to Toronto from Hong Kong on February 23, developed a febrile illness that was diagnosed as pneumonia, then died at home on March 5. Her son, who cared for her, subsequently became ill and on March 7 was admitted to a hospital, where he infected many patients and members of the staff. He died there on March 13, one day after WHO issued its first global alert. In this, the first phase of the Toronto epidemic, unrecognized patients who shared rooms with the son went on to infect scores of other patients, family members, and hospital workers. This scenario was repeated in several area hospitals, as well as others around the globe, even after increased infection control measures were undertaken.
Realizing that SARS was not contained within a single hospital, Ontario declared a provincial emergency on March 26 that halted the transfer of patients among hospitals, instituted infection control measures and created SARS units within hospitals, minimized visitor access to hospitals, and established a process
February 28, 2003: Atypical pneumonia reported in Hanoi, Vietnam.
|
November |
January |
|
2002 |
2004 |
to screen all persons entering hospitals for symptoms of SARS. Because the spread of SARS in Toronto was largely restricted to the hospital setting, these precautions were effective in controlling the outbreak. When a second phase of SARS occurred in mid-May, after emergency measures were relaxed, it was quickly brought under control with little spread outside the affected hospital (See D. Low in Chapter 1). A similar lapse in infection control in a Taiwan hospital ignited an outbreak in mid-April (WHO, 2003g). Health authorities responded quickly by increasing surveillance, redoubling infection control measures, and launching a mass education campaign credited with reducing the time between symptom onset and patient isolation.
Singapore
Rapid contact tracing by health authorities in Singapore, where scores of SARS cases had been reported, linked that country’s index case to the Metropole Hotel by April 4. Singaporean authorities imposed strict containment measures, including contact tracing and 10-day quarantine for all contacts of known SARS patients, as well as screening for fever among incoming and outgoing passengers at all airports and seaports. One indication of the effectiveness of these measures is the fact that 80 percent of Singapore’s SARS patients did not infect anyone else (WHO, 2003h; Singapore Government, 2003).
On September 8, an isolated case of SARS was reported in Singapore, and subsequently confirmed by the U.S. Centers for Disease Control and Prevention (CDC) (WHO, 2003l). The patient, a 27-year-old microbiology postdoctoral student, had no history of travel to SARS-affected areas or contact with SARS patients. Rather, he apparently become infected through a laboratory accident stemming from the contamination of samples containing West Nile virus, the subject of the patient’s research, with the SCoV, which was also being studied in the same biosafety level 3 facility.
THE IMPACT OF THE SARS EPIDEMIC
As the SARS coronavirus spread around the globe, so did its political, sociological, and economic repercussions. Workshop participants described the official reaction to the outbreak in China, examined the political and public health implications of how China acknowledged and confronted the full dimensions of the epidemic on national and international levels, and assessed the immediate and long-term economic
March 7, 2003: Son of Toronto index patient enters Scarborough Grace Hospital, initiating outbreak.
|
November |
January |
|
2002 |
2004 |
impact of SARS. Central to these discussions was the recognition of the extreme pressure SARS exerted on both international and local health care systems and the frightening prospect of future outbreaks of greater contagion or virulence.
The multinational effort to contain SARS placed unprecedented demands on affected and unaffected countries to accurately identify and report cases in a timely manner, to cooperate with GOARN expert teams of scientists and medical personnel coordinated by WHO, and to sacrifice immediate economic interests (e.g., travel, trade, tourism). Without international legal obligation to report SARS, most countries did so fully. Yet this extraordinary alliance would have failed without the full cooperation of China, the epicenter of the epidemic.
Politics, Tradition, and the Chinese Response to SARS
Workshop participants asserted that China’s problems in dealing with the SARS epidemic were fundamentally rooted in organizational obstacles. Problems cited during the workshop included impediments to the flow of information through the governmental hierarchy, a lack of coordination among fragmented governmental departments, and a political system in which the value of handling problems internally overrides any recognized value of external assistance. Importantly, workshop participants noted that these systemic failings are not exclusive to China and impede the response to public health and other social problems in a large number of countries around the world.
Uniquely, the Chinese tradition of respect for senior scientists in positions of authority may have substantially influenced the behavior of the Chinese Center for Disease Control and of other Chinese scientists who were researching the epidemic (Enserink, 2003). A highly respected Chinese scientist reportedly claimed that Chlamydia infection caused SARS, based on an examination of only two specimens. This may have led the Chinese Center for Disease Control and other Chinese clinicians and scientists to maintain that Chlamydia was the SARS agent, despite other evidence inside China indicating that the agent was viral. Consequently, virologists in a Beijing laboratory refrained from announcing their discovery in early March of the SARS coronavirus, a decision that set back by weeks research on the disease and a more significant public health response in China (Enserink, 2003).
The SARS epidemic also exposed weaknesses in China’s public health infrastructure, including inadequate state funding, lack of effective surveillance systems, and severe shortages in facilities and medical staff prepared for an epidemic infec-
March 10, 2003: WHO teams arrive in Hong Kong and Hanoi.
March 12, 2003: First WHO global alert issued on yet-unnamed disease.
|
November |
January |
|
2002 |
2004 |
tious disease outbreak. As a forewarning, a workshop participant observed that these same weaknesses are often cited by medical and public health experts when assessing the state of preparedness for infectious disease outbreaks in the United States.4 These statements corresponded with other participants who suggested that, in the case of SARS, the United States was perhaps more lucky than it was prepared.
In response to the deficiencies highlighted by SARS, the Chinese government established a case reporting structure, strengthened its emergency response system, dismissed key officials who mismanaged the crisis during its initial months, and provided funding for the prevention and control of SARS. Chinese workshop participants also credited the SARS experience for increasing the recognition and understanding of government officials and the public about the importance of infectious disease control and prevention in general.5
Economic Impact
While the most immediate and dramatic economic effects of SARS occurred in Asia, every market in today’s global economy was at some point impacted directly or indirectly by the epidemic. Several agencies and experts have attempted to estimate the cost of SARS based on near-term expenditures and losses in key sectors such as medical expenses, travel and related services, consumer confidence, and investment. One model estimated that the short-term global cost of lost economic activity due to SARS was approximately $80 billion.6 Participants agreed, however, that the true economic consequences of SARS remain to be determined, particularly given the possibility of its return.
An economic model presented at the workshop estimated the impact of SARS on several countries—and in aggregate, on the world. It considered two different scenarios: a short-term shock coincident with a one-time epidemic, and long-term effects typical of recurring outbreaks. The model was not intended to
March 15, 2003: Second WHO global alert names SARS; first travel advisory declared.
|
November |
January |
|
2002 |
2004 |
calculate precise monetary effects, but rather to reveal the magnitude of the impact on countries and regions, scaled to their individual economies (see Lee and McKibbin in Chapter 2).
According to this model, the short-term SARS shock disproportionately affected Hong Kong due to its economic dependence on services (e.g., travel, tourism). Significant short-term losses also accrued in China as a result of a sharp decrease in foreign investment, a trend that could be crippling if perpetuated over several years. In the long term, the expectation of continued outbreaks of infectious disease emanating from China could engulf that entire region of Asia in a permanent “disease transmission shock.”
Paradoxically, workshop participants discussed the global cost of SARS associated with lost economic activity—now estimated to have been around $40 billion, and possibly as high as $54 billion if investors remain cautious about the possibility of future outbreaks—as a potential cost of neglecting to invest in public health infrastructure. Several participants warned of a vicious spiral to be avoided: an economic downturn resulting from SARS or another pandemic which squeezes funding for public health, further weakening the world’s ability to prevent or contain subsequent outbreaks. The message here: an ounce of prevention is worth a pound of cure. It was suggested by several participants that further analyses comparing the anticipated costs associated with strengthening both global and national public health systems of surveillance and response with the anticipated costs of another epidemic SARS (or other disease) outbreak might reveal important results to persuade decisionmakers to make priority investments in relevant public health and research areas.
Impact on Global and Local Public Health Systems
Like many of the emergent diseases of the last decade, the challenge of SARS has cast a glaring spotlight on the need for greater investments in public health infrastructure. The outbreak placed a huge burden on international health systems that were already straining to address AIDS, tuberculosis, malaria, and a host of other conditions. With GOARN, WHO had an established structure to coordinate international resources and personnel and thereby muster surge capacity to address such outbreaks. That network was severely tested by SARS, but the successful containment of SARS through national actions supported by international collaboration confirms the value of this approach in addressing future epidemics (see Abdullah et al. in Chapter 1).
March 17, 2003: WHO establishes laboratory network to seek cause of SARS.
|
November |
January |
|
2002 |
2004 |
A key factor underlying the influence of SARS on public health, political, and economic systems was the infection of large numbers of health care workers. Nowhere was the impact of SARS felt more keenly than in the local health care systems of affected areas, where frontline caregivers all too frequently ended up as intensive care patients in need of extended hospital stays or as fatalities. This assault on the well-being of many health care personnel, coupled with the exhausting demands put on those who remained healthy, led Toronto health officials to send out a call to infectious disease professionals in the United States and Europe to come to Canada to bolster their capacity to fight the disease. Additionally, a workshop participant alleged that in Toronto, the closing of outpatient clinics in response to SARS may have caused greater morbidity and mortality than the disease itself. However, other participants argued that without a vaccine or cure for SARS, the isolation of patients and their contacts—including their caregivers—represented the most effective method of containing the epidemic.
THE PUBLIC HEALTH RESPONSE TO SARS
The Global Response
As noted earlier, the WHO response to SARS was spearheaded by GOARN. To extend its capacity for surveillance, reporting, and containment, WHO enlisted the support of public health services from the United States, United Kingdom, Germany, France, and other nations. GOARN recruited more than 60 teams of medical experts to assist with infection control in SARS-affected areas, which included 84 personnel from the U.S. CDC. Ultimately, more than 800 CDC employees were involved in the response to SARS.
Through GOARN, WHO also established a virtual network of 11 leading infectious disease laboratories in 9 countries. Connected by a secure website and daily teleconferences, the laboratories collaborated to identify the causative agent of SARS and to develop a diagnostic test; similar groups were also created to pool clinical knowledge and compare epidemiological data on SARS. By April 16, exactly 1 month after the laboratory network was established, its researchers had conclusively identified SCoV as the causative agent.
When evidence revealed that persons infected with SCoV continued to travel—placing adjacent passengers on airplanes at risk of infection—WHO advised airlines to screen departing passengers (WHO, 2003n). Further WHO advisories to avoid all but essential travel to certain high-risk areas were the
March 20, 2003: United States reports first cases of SARS.
March 26, 2003: Ontario declares provincial emergency.
|
November |
January |
|
2002 |
2004 |
most restrictive in the history of the organization (WHO, 2003c). The U.S. CDC and Health Canada also issued advisories that warned against travel to SARS-affected countries.
Chinese Cooperation
Members of a GOARN mission to China in late March warned that country’s health authorities that if SARS was not brought under control in China, there would be no chance of controlling the global threat of SARS. Within days, the GOARN team announced that Chinese authorities had agreed to join the GOARN collaborative effort to contain the outbreak and prevent further international spread (WHO, 2003i).
At a March 28 meeting with the Chinese Minister of Health, WHO officials determined that the atypical pneumonia in Guangdong was SARS and that the first cases had appeared in mid-November 2002 (WHO, 2003c). Data provided by the Chinese Center for Disease Control suggested an association between exotic food animals and SARS, indicating the possibility of a zoonosis. More than a third of the earliest SARS cases—those that emerged in China before February 2003—occurred among workers who handled, butchered, or sold wild animals in Guangdong’s markets, or who prepared and served them as food. Viruses closely resembling SCoV were eventually isolated from several animal species sold in such markets; however, a natural reservoir for SCoV has yet to be found (Guan et al., 2003).
Although Chinese officials acknowledged that SARS had emerged in their country, they continued to downplay the extent and severity of the outbreak. This led the WHO team in Beijing to take the unusual measure of publicly expressing “strong concern over inadequate reporting” of SARS cases on April 16 (WHO, 2003c).
On April 20, national government leaders declared a “nationwide war on SARS” and removed the mayor of Beijing and the Minister of Health from their posts reportedly for failing to satisfactorily address the epidemic (WHO, 2003c). Thereafter, China increased both its disease control efforts and its cooperation with the international community in the effort to contain SARS. Both the Chinese government and the public took considerable action to halt the epidemic. A workshop participant described how large numbers of government offices, schools, and universities were shut down. Quarantines to prevent public gatherings and travel from cities were imposed to prevent the spread of the disease to
March 27, 2003: WHO instructs airlines to screen passengers in SARS-affected areas.
|
November |
January |
|
2002 |
2004 |
the rural interior of the country, where it was feared that medical resources would be unable to contain or treat the disease. In late June, after more than 5,000 cases had been reported, the disease was contained in China. By this time, Beijing had reported 348 deaths and Hong Kong, 298—the two greatest death tolls due to SARS for any city or region at that time (WHO, 2003c).
When WHO declared on July 5 that all chains of SARS transmission had been broken, the disease was thought to have spread to more than 30 countries, only 8 of which—Canada, China, Hong Kong, the Philippines, Singapore, Taiwan, the United States, and Vietnam—reported more than 10 probable cases.
Assessing the Use of Public Health Tools
The experience of the SARS outbreak and the history of its control hold clues to the origin and spread of the disease—knowledge that will help to prevent or curtail its resurgence. In assessing the public health response to SARS at both the global and local levels, workshop participants focused on the roles of surveillance and containment in limiting the spread of SARS and anticipated the use of these tools against future microbial threats.
Surveillance
Broad international networks of individuals and organizations within and across disciplines were responsible in large part for the successful surveillance of the SARS epidemic. Electronic communication networks such as the Global Public Health Information Network (GPHIN) and ProMED mail reported the early outbreaks. ProMED uses electronic communications to provide up-to-date news on disease outbreaks and is open to all Internet users. GPHIN, established by Health Canada in collaboration with WHO, is an Internet-based application that continuously scans global electronic media (news wires, websites) for information on global public health risks, including infectious disease outbreaks. Although these systems ultimately proved to be critical tools for effective surveillance, workshop participants questioned the ability of the existing system to rapidly identify novel emerging threats, which induce symptoms and behaviors characteristic of other infectious diseases that may not initially promote concern or further investigation. Additionally, the sensitivity of the system was considered inadequate because of its inability to correlate disparate data from multiple
March 28, 2003: Chinese officials share details of first SARS cases.
March 30, 2003: Amoy Gardens, Hong Kong, outbreak announced.
|
November |
January |
|
2002 |
2004 |
surveillance networks that, only when taken as a whole, might surpass a threshold that signals an alarm to public health professionals. Retrospective analyses of the reports on several surveillance networks revealed multiple reports of atypical pneumonia in China between November 2002 and January 2003. However, the lack of collaborative data analysis between multiple reporting systems and the initial absence of clustering allowed the virus to spread unchecked. GOARN identified and verified subsequent outbreaks with the help of the media, nongovernmental organizations, agencies of the United Nations, and public health teams from many countries in addition to those where the outbreaks occurred. GOARN communicated new information to authorities and the public through the WHO website, satellite broadcasts, and news conferences.
The SARS epidemic became a front-page event for the worldwide news media. Daily updates posted on the WHO website for travelers and the public sought to counter rumors with reliable information. The U.S. CDC, which spearheaded the U.S. response to SARS, provided information through its website, satellite broadcasts, and a public response hotline for clinicians and the public.
The vast Emerging Infections Network created by the Asian Pacific Economic Community (APEC) also conducted surveillance for SARS. In addition, it provided an arena for discussions relevant to both biomedical research and disease control, and it monitored the economic impact of SARS in its member countries, which comprise 2.5 billion people and conduct nearly half of the world’s trade (see Kimball et al. in Chapter 5).
Containment
While many aspects of the public health response to SARS benefited from such technological developments as global broadband telecommunications, the containment of the epidemic ultimately depended on the venerable strategies of identifying and isolating persons who fit the case definition and tracing and quarantining their contacts. In countries such as Vietnam and Singapore, where these measures were imposed soon after the identification of index cases, the chain of infection was broken quickly. By contrast, China’s delayed response to the epidemic rendered contact tracing impossible and resulted in the need for broader quarantines.
The U.S. strategy to prevent an outbreak within its borders focused on the early detection of symptom onset and rapid implementation of infection control
March 31, 2003: Hong Kong health authorities issue quarantine order requiring some residents of the Amoy Gardens apartment complex to remain in their homes until April 9.
|
November |
January |
|
2002 |
2004 |
and isolation. Only in high-risk settings such as health care facilities or airline flights carrying passengers exposed to SARS-infected individuals did CDC suggest the use of quarantine (by definition, the isolation of asymptomatic individuals believed to have been exposed to a contagion). In the absence of an outbreak, the agency directed its efforts toward informing the traveling public about high-risk areas, issuing travel advisories, distributing millions of health alert notices in seven languages at airports and U.S.–Canada border crossings, and responding to symptomatic incoming passengers. However, several other countries quarantined travelers arriving from SARS-affected areas.
The relative effectiveness of various strategies applied to SARS containment—the use of standardized case definitions and laboratory testing to identify the infected, the isolation of ill persons, and the quarantine of contacts—remains to be determined. Based on the present understanding that asymptomatic infected individuals transmit SARS at a low rate, if at all (WHO, 2003j), and that transmission occurs primarily through contact with ill individuals, workshop participants suggested that quarantine of contacts was the least effective of these strategies. However, they also recognized that quarantine could facilitate the containment of a SARS-like disease by reducing the number of contacts by infected individuals during the delay between the onset of symptoms and diagnosis. This would be particularly effective when, as in the case of SARS, symptoms are nondescript and difficult to distinguish from those of other illnesses. It was also emphasized that quarantine should not be viewed as an impermeable cordon sanitaire confining those at risk for illness with the known ill, but as a scalable, self-protective measure that can be adapted to local conditions.
Less problematic than quarantine, the isolation of infected individuals clearly played a central role in containing SARS. Although isolating SARS patients within hospitals could be viewed as increasing the risk of infection for health care workers and other hospital staff, evidence from Toronto indicates that hospital personnel can be protected through strict infection-control practices, such as washing hands, wearing masks and gloves, and requiring patients to wear masks. The most effective type of mask remains to be determined, however.
Finally, even if it were known which of the various strategies used to contain SARS were most effective, it is far from certain whether they would continue to be effective should SARS return. For example, although it appears that quarantine helped control SARS in China and Toronto, it did so largely because of the limited contagiousness of the virus. The likelihood that SCoV
April 2, 2003: WHO declares travel advisory for Hong Kong and Guangdong Province.
April 4, 2003: Role of Metropole Hotel in global epidemic identified.
|
November |
January |
|
2002 |
2004 |
could become more easily transmissible cannot be determined without a better understanding of its biology, ecology, and natural history—knowledge that will be essential to mounting a rational response should SARS recur (see Cetron et al. in Chapter 1).
Evaluating SARS Containment Measures
To plan rationally for the containment of a future SARS outbreak, it will be important to know the relative effectiveness of the various measures taken to contain the recent epidemic. In the absence of such information, the strategy for containing SARS should emphasize overall preparedness at the local level in every community and hospital, participants agreed.
Participants discussed techniques and equipment to protect frontline caregivers of SARS patients in the hospital and at home. Simple habits such as frequent handwashing with soap and water are very important to prevent the transmission of any infectious agent. Other measures include wearing a mask that covers the nose and mouth, protective eyewear, gloves, gowns, or a containment suit. Participants noted that masks are effective only if they fit snugly and are not removed when the wearer coughs.
During the discussion of masks, participants debated the relative protectiveness of standard surgical masks compared with N-95 masks (so named because 95 percent of the time, they filter out any particle equal to or greater than 0.3 microns in size). Coronaviruses are smaller than 0.3 microns, so N-95 masks would not capture them; however, because viruses may travel in clumps, N-95 masks theoretically could capture some of the agent (University of California–Berkeley, 2003). Participants discussed a case control study in five Hong Kong hospitals in which wearers of surgical masks and N-95 masks did not contract the SARS coronavirus, while a few wearers of paper masks became infected (Seto et al., 2003). A larger study to validate this finding was proposed.
One workshop presentation described a relatively inexpensive mobile technology that potentially could be used to isolate individual patients during transport to and within hospitals, to protect staff during high-risk procedures such as intubation or bronchoscopy, to decontaminate large areas such as hospital waiting rooms or airplanes, and to create air exchange systems for isolation facilities or areas within hospitals (see Schentag et al. in Chapter 4). These mobile units remove and destroy airborne viral particles and droplets; the latter are widely believed to be the vector for SCoV transmission. Importantly however, it was
April 16, 2003: SARS coronavirus identified; WHO accuses Chinese government of underreporting SARS cases.
|
November |
January |
|
2002 |
2004 |
noted that such technologies must be thoroughly evaluated to determine their suitability for containing SARS in a variety of clinical settings before they are recommended for use.
CORONAVIRUS RESEARCH AND SARS
The SARS coronavirus (SCoV) appears to be zoonotic and to have originated in wild mammals in southern China. A coronavirus comprises single-stranded RNA inside a lipid envelope. Coronaviruses cause a substantial fraction of human colds and a number of common respiratory infections in other animals, including livestock and poultry (Holmes, 2003). Since its emergence, several veterinary and biomedical scientists have been called on to share their considerable knowledge of coronaviruses with a vast new audience and to join the research response to the epidemic. This experience—and the high value evident in available knowledge and understanding of coronavirus biology and molecular biology, gained at a time when coronaviruses were not recognized to be the causative agent of any severe infectious disease—attests to the value of basic research.
Based on their genetic sequences, the 14 previously known coronaviruses have been divided into three major groups. While SCoV has been linked with Group II coronaviruses, whose members include human and bovine respiratory viruses and the mouse hepatitis virus, there is still some debate over whether its genetic features might be sufficiently distinct to warrant classification within a separate, fourth class of coronaviruses.
Although coronaviruses generally cause disease in a single species, it has been demonstrated that some coronaviruses can cross species barriers. Moreover, RNA viruses are more likely to be zoonotic than DNA viruses. These findings lend credence to the hypothesis that SCoV is a zoonosis. Viruses resembling human SCoV reportedly have been detected in wild mammals of southern China that were brought to marketplaces where they were sold as exotic food. Immunological and genetic tests of these SCoV-like viruses suggest that human SCoV may be an animal virus transmitted to humans in the recent past (Guan et al., 2003).
Understanding the Biology and Epidemiology of SARS
As one would expect of a newly characterized disease, much knowledge about the microbiology, pathogenesis, natural history, and epidemiology of SARS
April 20, 2003: Mayor of Beijing and Chinese Minister of Health fired.
|
November |
January |
|
2002 |
2004 |
|
BOX S-1
SOURCES: Breiman presentation; Denison presentation (see Chapters 1 and 3 respectively); WHO, 2003j. |
remains to be discovered. For example, scientists have not yet identified the animal source of the infectious agent and have not determined whether a persistent animal reservoir of the infectious agent exists. It is also unclear whether SARS, like influenza, is a seasonal disease that would have receded on its own. Along the same lines, it remains to be seen whether SARS will reemerge on a seasonal basis, and if so, how virulent future manifestations of SCoV will be. These and other unanswered scientific questions, listed in Box S-1, were a prominent theme of workshop presentations and discussions. Answers to these questions would certainly advance the world’s ability to predict and prepare for a resurgence of SARS.7
April 23, 2003: WHO declares travel advisory for Beijing, Shanxi Province, and Toronto.
|
November |
January |
|
2002 |
2004 |
Considerable effort already has been applied to finding the animal source of SCoV. For example, viral isolates from suspected animal sources were genetically characterized and compared with samples of SCoV (see Guan et al. in Chapter 3). However, recalling previous investigations of outbreaks of Legionnaire’s disease, Schistosomiasis, and E. coli 0157, workshop participants noted the crucial role played by epidemiological “detective work” in developing hypotheses that led ultimately to the source of transmission (Zhong et al., 2003).8To this end, it was suggested at the workshop that a case control study of the first 50 to 100 SARS patients be conducted using epidemiological data collected in Guangdong Province. Such an endeavor may provide direction to further laboratory surveys of animal viruses to reveal the source of SCoV and, perhaps, its animal reservoir.9
SARS researchers benefit from the wealth of literature on coronaviruses in general. Presentations by two coronavirus experts at the workshop summarized the current understanding of coronavirus biology and pathogenesis and suggested promising directions for research on SARS and other emerging zoonoses (see Saif and Denison in Chapter 3).
The pathogeneses of animal coronaviruses conform to a basic model of either intestinal (enteric) or respiratory infection. Enteric coronaviruses can cause fatal infections in young, seronegative animals. Respiratory coronavirus infections in adult animals have shown increased severity in the presence of several factors, including high exposure doses, respiratory coinfections, stress related to shipping or commingling with animals from different farms, and treatment with corticosteroids. It is unknown whether SCoV is a respiratory virus or a pneumoenteric virus. This knowledge gap will stymie efforts to develop a vaccine or drug against SCoV.
Studies of coronavirus replication reveal several mechanisms that account for the repeated, persistent infections typical of coronaviral disease. High rates of mutation and RNA-RNA recombination produce viruses that are extremely adaptable and capable of acquiring or regaining virulence. The relatively large coronavirus genome tolerates deletions, mutations, and substitutions and can recover from deleterious mutations. Molecular biological studies have also identified
April 28, 2003: SARS contained in Vietnam.
April 30, 2003: WHO lifts Toronto travel advisory.
|
November |
January |
|
2002 |
2004 |
several potential targets for antiviral drug discovery, including viral binding and uncoating, replication, protein expression and processing, assembly, and release. Cellular functions on which the virus depends, such as cholesterol synthesis, membrane trafficking, and autophagy, also present opportunities for antiviral design (see Matthews et al. in Chapter 4).
The tendency of coronaviruses to undergo mutation and recombination represents a significant challenge for vaccine development. To date, no vaccine has been produced that can provide highly effective, long-term protection against respiratory coronavirus infections. Genetic approaches represent the best hope of overcoming this propensity for mutability, according to workshop presenters.10 For example, it might be possible to find ways to limit RNA-RNA homologous recombination, or to identify areas in the genome that are more or less prone to survive mutation. Promising approaches to these challenges include the use of reverse molecular genetics to make specific mutations in the virus genome and test their functional effects.
Workshop presenters emphasized that appropriate animal models are needed immediately to advance the development of a SARS vaccine. Participants also noted that studies in existing animal models of coronavirus infection could play a role in the development of antiviral therapies against SARS. Ultimately, a range of natural and transspecies disease models will be critical to understanding the pathogenesis of this and other emerging zoonoses. Coordinated, multidisciplinary research drawing on expertise in veterinary sciences, medicine, molecular biology, and virology will be needed to meet these goals. However, the coronavirus experts who presented at the workshop lamented that there is little encouragement or support for such critical cross-disciplinary research at present.
BUILDING DEFENSES AGAINST A REEMERGENCE OF SARS
Anticipating the Reemergence
Considering the likelihood of a return of SARS under a variety of circumstances is an important first step in planning for a broad range of contingencies
May 3, 2003: Taiwan outbreak grows to 100 cases; WHO sends team.
May 8, 2003: WHO declares travel advisory for Tianjin, Inner Mongolia, and Taipei.
|
November |
January |
|
2002 |
2004 |
and challenges. A trio of plausible scenarios was presented at the workshop (see Monaghan in Chapter 5). The first scenario entailed a resurgence of SARS in China, followed by limited spread to other countries in the region. Heightened surveillance and rapid response could quickly contain such an outbreak, but might also cause SARS to be viewed less as a threat and more as a public nuisance; this attitude could lead to a decline in vigilance, raising the risk of a future epidemic.
In the second scenario, SARS spreads to poor countries in Asia and Africa, where inadequate health systems, preexisting health problems, high population density, and weak government leadership result in high infection rates and mortality. Such an epidemic would prove difficult to contain and create a humanitarian emergency that would place costly demands on international policy makers and institutions as well as developed countries compelled to respond for reasons that were both humane and self-protective.
The final, scenario depicts the resurgence of SARS in key trading centers of Asia and Canada, followed by transmission to the United States, Brazil, India, Japan, and Europe.
And even if this epidemic produced fewer cases of SARS than in 2003, it would be likely to cause major disruptions in trade and investment flows.
In considering further preparations for the reemergence of SARS, workshop participants discussed the development of surveillance and containment strategies in case SARS reappears during the winter of 2004; ongoing efforts to develop diagnostic tools for SARS and other infectious diseases; and long-term prospects for the discovery and development of antiviral drugs and vaccines against this newly emergent disease.
Continued Surveillance for SARS
For a number of reasons, workshop participants agreed that continued vigilance in light of SARS is warranted for a number of reasons. First, it is very likely that an animal reservoir for the virus exists in China. Second, the continued sale of live, small wild mammals in marketplaces and the preparation of these animals as food perpetuates a hypothesized route of SCoV transmission to humans. Third, the possibility that SARS, like influenza, is a seasonal disease means it could reappear during the winter of 2004. Finally, initial low-level transmission of the virus could elude clinical recognition and reporting of the disease.
May 21, 2003: WHO declares travel advisory for all of Taiwan.
May 22, 2003: Second wave of SARS begins in Toronto.
|
November |
January |
|
2002 |
2004 |
It was suggested that in the absence of inexpensive, accurate, and widely available SARS diagnostics, syndromic surveillance—particularly in populations at high risk for reemergence—might be important for spotting nascent outbreaks. This methodological strategy, which involves monitoring groups of signs and symptoms associated with disease activity—unusual spikes in the purchase of commonly available health remedies, for example, or surges in particular symptoms reported among routinely collected information from clinical sources—has shown some promise in the early detection of disease outbreaks in the United States (Institute of Medicine, 2003). However, because SARS symptoms are variable and difficult to distinguish from those of influenza and seasonal human coronavirus infections that emerge in the same populations, it is not clear that such methods would be capable at present of distinguishing the emergence of novel infections such as SARS without careful consideration of the utility, quantity, and specificity of the surveillance data to be collected. Until a specific diagnostic test becomes available, there will continue to be a substantial risk of both missed cases and false alarms, and syndromic surveillance methods should be evaluated as possible complements to rather than replacements for maintaining and strengthening traditional clinical reporting systems.
Development of SARS Diagnostics
A rapid, specific, reliable, and inexpensive clinical diagnostic test for SARS would be a valuable tool for improving surveillance and limiting the transmission of SCoV. First, however, scientists must determine which tissues contain the highest concentrations of virus during the presymptomatic stage of infection. It was also noted that in confirmed cases of SARS, the virus appears to be located deep in the respiratory tract, making specimens difficult to collect.
Available Diagnostics
Absent a clinical diagnostic test, suspected cases of SARS must be confirmed in the laboratory using reverse-transcription polymerase chain reaction (RT-PCR) or much slower methods involving serology or viral culture, isolation, and identification by electron microscopy (Yam et al., 2003).
According to WHO, the laboratory case definition of SARS requires one of the following:
May 23, 2003: SARS linked to masked palm civet and raccoon-dog; Hong Kong and Guangdong travel advisories lifted.
|
November |
January |
|
2002 |
2004 |
-
A positive RT-PCR finding in two or more clinical specimens, sequential samples, or assays using separate RNA extracts from the same sample.
-
Seroconversion or a fourfold increase in titer between the acute and convalescent phases of infection as determined by immunoassay.
-
Isolation of the virus with RT-PCR validation.
Recent incidents have highlighted the critical need for both specificity and sensitivity of laboratory diagnostic procedures. To address these issues, WHO and the CDC continue to work to standardize test protocols, reagents, and controls and to establish procedures for evaluation and quality control throughout the global network of diagnostic laboratories that may handle suspected SARS cases (WHO, 2003m).
Workshop participants considered several platforms that could potentially be adapted for the rapid, clinical diagnosis of early, asymptomatic SCoV infection. For example, workshop participants considered the use of RT-PCR for detecting SCoV nucleic acids. A recent evaluation of two RT-PCR protocols found them to be highly specific for the SARS coronavirus; however, these protocols were insufficiently sensitive to detect the virus reliably in respiratory specimens. Testing two specimens from the same patient increased the probability of an accurate diagnosis (see Yam et al. in Chapter 4).
A different platform discussed at the workshop purportedly can identify the family, and possibly the genus, of known or novel infectious agents (see Sampath and Ecker in Chapter 4; Hogg, 2003). Unlike many RT-PCR techniques, which target nucleic acid sequences unique to a specific organism, this test amplifies strategically chosen, highly conserved sequences from the broadest possible grouping of organisms. The molecular weight of the amplimers is measured by electrospray ionization mass spectrometry. Then the relative amounts of each base (i.e., the percentage of adenine, cytocine, thiamine, and guanine) are deduced. The base-pair composition of the selected genetic sequence serves as a signature to identify and distinguish organisms in a sample.
Originally designed for the environmental surveillance of biowarfare agents, such technology could potentially diagnose SARS directly from a tissue sample, obviating the need for time-consuming viral culture. According to workshop presenters, their method can distinguish between SCoV and other coronaviruses and perhaps even between genetic variants of SCoV. However, it is important to note that the test’s sensitivity has yet to be evaluated using samples of human SARS-infected tissue.
May 31, 2003: SARS contained in Singapore.
|
November |
January |
|
2002 |
2004 |
Antiviral Drugs and Vaccines
As noted earlier, until basic research on the pathogenesis of SARS elucidates whether the infection is respiratory or pneumoenteric, it is unclear which tissues a therapeutic agent should target. That being said, preparing for a reemergence of SARS might include the strategic development of a vaccine and an antiviral drug.
Theoretically, an ideal vaccine would contain an epidemic more effectively than an ideal antiviral drug if a large segment of the population were vaccinated. Yet mathematical models of influenza described at the workshop indicate that an epidemic could be contained effectively by providing an antiviral prophylaxis to close contacts of index cases. Therefore, the parallel development of both a vaccine and a drug for SARS may be an effective course of action.
The perceived urgency of developing SARS therapeutics has led several pharmaceutical and biotechnology companies to pursue the development of countermeasures for SARS. Two advantages these companies enjoy are the panoply of veterinary vaccines against coronaviruses and the ease with which SCoV can be grown in culture.
Previous antiviral discovery efforts by researchers from Pfizer Inc., of New York, focused on the human rhinovirus 3C protease, a functional, genetic, and structural analog to a key SCoV protease named “3C-like” (3CL). This work has proved advantageous in searching for 3CL protease inhibitors. Together with scientists at the National Institute for Allergy and Infectious Diseases and the U.S. Army Medical Research Institute of Infectious Diseases, who had developed an assay to test candidate compounds for their ability to prevent death in SARS-infected monkey kidney cells, Pfizer tested existing compounds that had shown activity against the rhinovirus protease. An X-ray crystallographic atomic-level resolution model of 3C protease of human rhinovirus 14 served as the basis for structural models of the 3CL protease binding site. This structural information enabled the scientists to identify additional compounds that demonstrated significant antiviral activity. The group is currently evaluating the solubility, metabolic stability, and other physicochemical properties of some of these inhibitors in hopes of finding promising compounds for clinical development. Pfizer researchers are also employing structure-based design and combinatorial chemistry as an alternative, complementary strategy to discovering 3CL protease inhibitors (see Matthews et al. in Chapter 4).
Despite the research described earlier in this chapter and the wealth of literature on coronaviruses, it will take more time before a compound designed to
June 13, 2003: SARS contained in China, except Beijing.
|
November |
January |
|
2002 |
2004 |
defeat SCoV reaches clinical trials. SARS vaccine development programs require biosafety level 3 conditions, which make research efforts slower and more expensive than other targets of less contagious microbes. For this reason and others, such as the genetically unstable nature of the virus and the current lack of an appropriate animal model, a vaccine for SARS could well postdate a return of the disease, perhaps by several years, even if such a product were steered through a streamlined development process. If SARS fails to reappear within the next few years, however, it is unlikely that either antiviral or vaccine development will continue, given the cost of these efforts.11
The Food and Drug Administration’s (FDA’s) Center for Biologics Evaluation and Research (CBER) conducts research to facilitate the development of needed biological products, including antiviral drugs and vaccines. Several functions handled by CBER during the SARS epidemic would pertain to future microbial threats. These include ensuring the availability of virus isolates for vaccine stock, recognizing research needs and contingencies in areas such as vaccine testing, and conducting public workshops on needed technologies, such as diagnostics.12
LESSONS FROM SARS FOR FUTURE OUTBREAKS
Recognizing that it would be impossible to address the vast array of potential microbial threats individually, public health policy makers are formulating general strategies to evaluate and respond to outbreaks of all kinds. At the international level, revisions to the International Health Regulations—rules concerning infectious disease that legally bind WHO member nations—have been underway since 1995, and are expected to be completed in 2005. Workshop participants concurred that efforts to address microbial threats should encompass and be enriched by existing strategies for defense against bioterrorism. As one participant noted, authorities do not know until well into an outbreak if it is a naturally occurring or manmade threat—in either case a robust and prepared system will be able to respond rapidly and effectively to contain disease spread.
June 23, 2003: SARS contained in Beijing.
|
November |
January |
|
2002 |
2004 |
The importance of collaboration was a common theme among workshop discussions on research. It was discussed in the context of scientists around the globe who identified the causal agent of SARS, of veterinary and biomedical research communities studying zoonotic pathogens, and of private sector companies working in conjunction with government agencies and academia to develop antiviral drugs and vaccines.
Workshop participants considered what could be learned from the experience of SARS and how that knowledge could improve the public health community’s response to future outbreaks of infectious disease. The principal topics discussed include:
-
the early detection of outbreaks,
-
effective communication to the public in the event of an outbreak,
-
the promotion of research and development,
-
strategies for containment, and
-
multinational collaboration in implementing such strategies.
Importance of Early Detection
The central response to SARS—surveillance and containment, when instituted promptly, rapidly, and effectively—applies to almost any microbial threat. It is clear that the initial delays in not only detecting the novel SCoV, but also alerting national and global health officials to the disease outbreak significantly increased the spread of SARS and its impact on affected countries. However, soon after the global outbreak alerts were issued, the timely recognition of the emergence of SARS in other countries proved to be an important factor in breaking all chains of transmission. The surveillance networks such as GOARN and GPHIN, supported by personnel and laboratories from 115 other partnerships, made this success ultimately possible. Along with these vital resources, workshop participants identified additional surveillance strategies for microbial threats; these include hospital-based surveillance systems capable of recognizing both known and novel diseases, and occupational clustering, with particular attention paid to illness in health care workers. Behavior-based surveillance could identify such phenomena as drug sales, or even such phenomena as the rapid rise in vinegar sales that occurred in response to SARS in Guangdong in January 2003
July 2, 2003: SARS contained in Toronto.
|
November |
January |
|
2002 |
2004 |
(vinegar is commonly used to combat respiratory illness in traditional Chinese medicine).
Drawing on the SARS experience, a recent WHO global consultation focused on strengthening national capacities for surveillance, response, and control of communicable diseases. After SARS, it was noted, “countries increasingly look at the integration of disease surveillance activities as an effective, efficient and sustainable approach to improving national capacities.” Among recommendations issuing from this consultation was the admonition that “member states should review existing legal frameworks to further support strengthening of surveillance including participation of the private sectors and non-governmental organizations” (WHO, 2003k). Several workshop participants observed that more nationally and globally coordinated systems of information-sharing and data analyses among surveillance networks might dramatically improve the world’s ability to contain microbial threats.
While discussing the critical role of laboratories for effective surveillance, concerns about laboratory safety were raised. Accidents in a Singapore clinical laboratory (described earlier in this chapter) and a Taiwan research laboratory have been responsible for SARS infections in workers (Center for Disease Control Taiwan, 2003). These incidents highlight the importance of hospital surveillance procedures and appropriate clinical management and infection control measures in preventing an outbreak. They should also raise the awareness of the research community, particularly given the many laboratories now conducting research on SARS, to the risks inherent in handling all communicable agents and the need for strict adherence to well established laboratory procedures.
Overall, workshop participants observed that surveillance must be backed up with action and reinforced by sufficient laboratory capacity, well-trained personnel, and a legal framework consistent with objectives of transparency, global cooperation, and sensitivity to the balance between public protection and the interests of individual countries and persons. Workshop discussants emphasized that investments made toward this end should capitalize on the existing networks and need not be prohibitively extensive or expensive.
Strategies for Containing Future Threats
An estimated 75 percent of emerging human pathogens and 61 percent of all human pathogens are zoonotic (Taylor et al., 2001). Therefore, many predictions
July 5, 2003: SARS contained in Taiwan; WHO declares containment of worldwide epidemic.
|
November |
January |
|
2002 |
2004 |
about the nature of future novel pathogens anticipate the emergence of zoonoses. Thus, workshop participants considered the strategies for containing known zoonoses—in particular, influenza—as potential models for the containment of SARS and unidentified zoonotic diseases of the future.
Lessons Learned from Influenza
The same trends that ushered SARS into the human population have been apparent during a century of influenza outbreaks. The exponential increase in avian influenza virus infections among humans over the past decade has been associated with a sharp rise in the size and density of chicken and pig farm populations, their proximity to human settlements, and movement of animals through market channels, which in turn parallels the world’s rapidly expanding and mobile population. As with SARS, animal markets provide the breeding ground for recent outbreaks of influenza; laboratory sources also appear to have sparked at least one epidemic. Fortunately, most of the recent influenza outbreaks did not feature the transmission of the virus to humans. However, experts agree that it is only a matter of time until a highly virulent and contagious flu, such as the strain that caused over 20 million and perhaps as many as 40 million deaths during the 1918 influenza epidemic, confronts the world (see Webby and Webster in Chapter 5).13
Vaccines and antiviral therapies play a significant role in containing epidemics of influenza. It is advantageous that the timing of annual outbreaks of influenza and the strain or strains of the virus can, to some extent, be anticipated. However, strategic actions recommended against influenza that could also inform efforts to better prepare for other viral disease outbreaks have yet to be implemented. These strategies include:14
|
13 |
Shortly before the publication of this report in January 2004, the highly pathogenic H5N1 avian influenza virus was implicated in a human outbreak of the disease in Vietnam and Thailand. Sixteen of the 20 individuals so far infected have died. Thousands of birds in eight countries, including Vietnam, The Republic of Korea, Thailand, China, and Japan are suspected to be infected with the virus. See http://www.who.int/en/disease outbreaks for more information. |
|
14 |
Workshop presentation, Robert Webster, St. Jude’s Children’s Research Hospital, October 1, 2003. |
September 8, 2003: Isolated case of SARS occurs in Singapore due to laboratory accident.
|
November |
January |
|
2002 |
2004 |
-
stockpiling of broad-spectrum antiviral drugs,
-
advanced development of pandemic strain vaccines,
-
the establishment of surge capacity for rapid vaccine production, and
-
the development of models to determine the most effective means of delivering therapies during an outbreak.
It is evident from the experience of the late 2003 influenza season that our supply and effectiveness of antiviral drugs, capabilities to accurately predict the best viral strain for annual vaccine production, and mechanisms for surge capacity production remain inadequate (Treanor, 2004; WHO, 2003o). Recognition of these vulnerabilities lead numerous workshop participants to call for greater scientific and financial investments to strengthen our defenses against these certain future threats.
Quarantine
Some emerging infections of the future, like SARS, may be truly novel threats for which the world—including its pharmacopoeia—is inadequately prepared. Lacking other forms of effective interventions, the implementation of quarantine or isolation strategies may prove valuable in such instances. Workshop participants discussed several ways that modeling tools might be used to improve and tailor such measures. Models based on detailed observations from previous epidemics can be used to predict demands on hospital capacity during a hypothetical epidemic and to guide the timing and nature of quarantine measures. Models that can estimate the length and severity of an unfolding epidemic will likely increase public acceptance of quarantine by permitting people to form realistic expectations of their sacrifice and its benefit to the community (see Amirfar et al. in Chapter 5).
Evidence indicates that a modern approach to quarantine encompassing a range of options designed to reduce the frequency of social contact can significantly reduce the spread of infectious disease. Such options include short-term, voluntary home curfew; suspension or cancellation of public activities (such as events, mass transit, or access to public buildings); and “snow day” or sheltering-in-place measures. These measures could be employed individually or in concert. In addition to or in place of these strategies, a program of contact surveillance—the monitoring of asymptomatic persons exposed to an infectious disease—could be undertaken. Modern quarantine and contact surveillance preserve individual liberties and require far less labor and other community re-
December 5, 2003: Taiwanese researcher contracts SARS during experiment.
|
November |
January |
|
2002 |
2004 |
sources than would be required to enforce a mandatory quarantine. Voluntary and other forms of scalable quarantine nevertheless reduce productivity and may result in public perceptions that stigmatize groups of individuals and promote irrational behavior. For example, there is evidence that consumers began to avoid Asian restaurants in the United States and other nonaffected countries during the SARS epidemic even though neither quarantine nor public health messages suggested such action. For any quarantine to be effective, workshop participants noted, a number of needs must be met, including:
-
education to build public trust in health authorities,
-
compensation and job security for quarantined workers, and
-
incentives to health care workers to maintain their morale in the face of increased risk and to pay greater attention to infection control practices.
In the more difficult case of mandatory quarantine, enforcement requires careful planning and a clear understanding of public health law; this is particularly true in the United States, where quarantine is likely to necessitate the coordination of federal, state, and local jurisdictions and legal authorities. For example, if an infectious disease has the potential to spread across state boundaries but has not yet done so, an action by CDC to limit transmission would require the cooperation of appropriate state and local authorities. The presidential executive order adding SARS to a list of other diseases subject to federal quarantine actions eliminated such jurisdictional uncertainties (Executive Order 13295: Revised List of Quarantinable Communicable Diseases, 2003). Additional legal considerations include planning for due process—proper notice, legal representation, court-reviewed decisions, and remote communications to permit a quarantined person to be heard in court—and for practical contingencies, such as the need for law enforcement officials to serve notice of quarantine (see Matthews in Chapter 5).
Workshop participants also discussed the need to develop strategies by which hospitals—and entire communities, in the event of quarantine—can determine when precautions against infection can be scaled back. Some experts have argued that containment measures should be swiftly imposed in response to a perceived infectious disease threat (as occurred when SARS appeared in Vietnam) and reduced only after surveillance determines the absence of a threat. Clearly, the consequences of false alarms in this case must be weighed against the risks of
December 7-10, 2003: Infected researcher attends conference in Singapore.
|
November |
January |
|
2002 |
2004 |
inaction in the early stages of an epidemic, as demonstrated by China’s experience with SARS.
Informing the Public
Although no presentations exclusively addressed the subject of public communication, this topic was identified as important and was widely discussed by workshop participants. Social cohesion and compliance with quarantine in Toronto were attributed in part to a combination of clear communication and practical guidance by public health authorities. The media’s sustained and intensive focus on the epidemic, heavy traffic on informational SARS websites operated by WHO and CDC, and a great volume of calls to CDC’s SARS hotline reflect the public’s hunger for news and information during the public health emergency.
Official travel and health advisories, though deemed necessary, were also linked to consumer avoidance of international travel, international events, and even Asian restaurants. It was suggested that such adverse effects could be mediated in the future by accompanying advisories with educational messages designed to help the public develop a realistic perception of the risks for infection and appropriate responses. Research designed to identify why societies respond dramatically and irrationally to certain types of public health threats might help communicators to develop messages that positively influence the public’s behavior during medical emergencies.
The media’s powerful role in the response to SARS was characterized in both positive and negative terms: as a cause of stigma and discrimination due to sensationalized reporting on the epidemic; as a demystifier of quarantine and other public health measures through exhaustive coverage; and, as a persuasive contributor to China’s decision to cooperate with international efforts to control SARS. The Internet, recognized as a key source of early leads to the outbreak of SARS, was also viewed with concern for its potential to propagate false rumors. It is important to guard against such threats in the event of public health emergencies. Likewise, it will be critical to make use of the media to inform and educate the public on how best to protect themselves and their communities in the event of future outbreaks
December 17, 2003: Singapore authorities quarantine 70 individuals.
|
November |
January |
|
2002 |
2004 |
Surge Capacity
Health Care Personnel
Workshop participants remarked that the strained capacity of the U.S. and global public health infrastructure—attributed to insufficient funding, labor shortages, and a lack of facilities—impedes preparations for SARS and other threats to public health. As described earlier, even some of the highly developed health care systems of Toronto struggled to cope with inadequate numbers of health care personnel (particularly because of the inevitable toll that moderately to highly contagious diseases take on health care personnel) and were ultimately unable to sustain normal levels of care for both SARS and non-SARS patients.
In moving forward, workshop participants suggested that up-to-date information and skills needed for containing epidemic-prone diseases must be better integrated into the training of all health care professionals, not only those specializing in infectious diseases or infection control. In citing Toronto’s call to health care personnel in other regions and countries, a participant recommended the expansion and establishment of formal networks to rapidly identify, transport, and enlist experienced health care personnel in the event of future outbreaks. Such contingencies would be designed for local, regional, national, and international responses and, in particular, would facilitate the mobilization of human and technical resources that are known to have previously tackled certain disease outbreaks. The question was asked, if SARS is to reemerge how will we harness the skills and new knowledge of the thousands of individuals involved with finally containing the disease? While some participants lauded the efforts of GOARN and the CDC in this regard, they questioned if that was enough.
Health Care Facilities
The inability to effectively establish isolation areas and procedures within hospitals and other health care facilities contributed to the spread of SARS in several countries. Inadequate facilities not only promoted the spread of the disease, but also forced the suspension of other vital health care procedures. As previously described, one workshop participant suspected that more patients died during the SARS outbreak in Toronto as a result of the inability to access appropriate care for conditions other than SARS rather than from SARS itself.
January 5, 2004: China and WHO confirm SARS case in Guangdong Province.
|
November |
January |
|
2002 |
2004 |
As such, participants called for preparedness planning that established procedures for rapid identification and use of facilities designated not only for treatment of suspected and confirmed cases of an epidemic disease, but also facilities that could be isolated for the conduct of other critical procedures such as emergency surgeries, trauma care, and organ transplantation. In this regard, several participants credited the rapid construction of “SARS hospitals” in China as a key element in ultimately containing the disease.
Supporting the Research Response
Years of investment in basic research on coronaviruses, largely in the veterinary research fields, helped the scientific community to identify the SARS coronavirus within months of its emergence. Consequently, numerous participants noted that the potential for future outbreaks not only justifies presentday investments in basic research on viruses and microbes, but also argues for greater attention to and investment in research efforts that integrate the direct contributions of zoonotic infectious disease research with biomedical research efforts. As noted earlier (see Box S-1), a number of basic scientific questions about the biology and epidemiology of SARS need to be answered in order to develop diagnostics and therapeutics for the disease, as well as to construct and implement targeted surveillance strategies. Apart from research that is specific to the SARS coronavirus, however, workshop participants discussed a number of broader areas of basic research that might be pursued in order to counter the threat that would arise from either a recurrence of SARS or the emergence of other new infections.
First, now that the more urgent pace of responding to an ongoing epidemic has subsided, researchers should be encouraged to thoroughly and methodically take stock of data that was accumulated over the course of fighting this epidemic. Workshop participants suggested that the public health community should not be complacent about the eventual success that was had in containing last year’s SARS outbreak; there remains a need to understand exactly what strategies were most effective, what strategies were less successful or even counterproductive, and what steps would be most essential for combating the emergence of a new and possibly more virulent or more infectious pathogen. As part of this retrospective evaluation, for example, extant patient and hospital records should be assembled, compared, and analyzed in order to provide as exact an assessment as possible of the effectiveness of each of the many control
measures that were adopted, as well as the points of greatest weakness that allowed the virus to spread. Some of the lessons to be learned will be specific to the profile of SARS, but many of them will also be readily applicable to other new infections in the crucial early stages of an epidemic when less is known about the biology of the disease than about its manner and rate of spread. On the next occasion when scientists and public health officials are confronted by a novel threat, it is important that they have a battery of well-researched studies to fall back on concerning measures that have previously been shown to be effective and feasible in controlling even a disease entity that has not yet been well characterized.
Secondly, this evaluative process should expand beyond those areas encompassed by clinical medicine and emergency care. The SARS epidemic illustrated how rapidly the impacts of a new disease can reverberate through the political and economic structures of successive countries and regions, and the decisions that were made in response to the epidemic ultimately reached into the highest levels of government and international bodies. Just as with the measures that were taken within individual hospitals and clinical settings, the comparative effectiveness of the broader quarantine measures, travel advisories, communications with the general public, and other legal and public health directives that were issued should be gauged relative to their costs and difficulties. Any possible improvements in the measures that were adopted in the case of SARS—or recommendations for flexible options or combinations of options that might be applied in the face of different types of pathogens—may need to be examined within a broad and multidisciplinary discussion framework.
Finally, basic research needs to be conducted into not only the measures that were most effective in containing the last epidemic but also those steps that would best facilitate research on understanding the next one. The uncertainty and confusion that are likely to be present in an epidemic’s early stages may at least be ameliorated if scientists, public health officials, and governmental bodies understand and are well prepared to collect the types of data that have been shown to be most crucial in assessing the nature and magnitude of a novel threat. A number of workshop participants commented on the need to look into better standards for data capture and coordination during the course of an epidemic, as well as the need to have better models on hand for evaluating the effects of possible intervention strategies as early as possible. Likewise, while carefully controlled therapeutic trials are often impractical (or at best extremely difficult) during the first stages of a disease outbreak, some workshop participants lamented the fact that relatively little progress was made toward developing a standard treatment algorithm for SARS patients during last year’s epidemic, and there remains significant controversy over the effectiveness of certain treatments that were applied. It was suggested that in the case of any future epidemics, better pooling of data from scattered clinical treatment
centers could at least initiate the process of assessing the efficacy of different treatment strategies and provide groundwork for more reliable clinical advisories until the time and means are available for more thorough studies.
Engaging the Private Sector
Several presentations and considerable discussion concentrated on mechanisms that could potentially engage the private sector—specifically, pharmaceutical and biotechnology companies—in the research and development of products targeted at the greatest threats to public health, including infectious diseases.
For pharmaceutical researchers, streamlining the development process is crucial to productive engagement in strategic research. Means of streamlining this process include the clear identification of patient and physician needs, access to detailed biological studies of the pathogen of interest, and technologies such as computational and combinatorial chemistry that speed target selection and lead generation. Workshop presenters described the need for technology to improve predictions of the safety of drug candidates so unsafe compounds could be weeded out at an early and less expensive stage of the development process.
Promotion of International Cooperation and Collaboration
If SARS never returns, the 2003 epidemic will nonetheless be remembered as a watershed event in the history of public health because of the degree of multinational cooperation to contain the disease. As the world becomes more conscious of microbial threats to health, countries are increasingly compelled to report infectious outbreaks and join international efforts to contain them. Recognizing that such transparency often comes at a price to a nation’s economy, particularly in developing countries, workshop participants attempted to identify incentives to encourage nations and individuals to act for the common good.
Some participants offered specific ideas for incentives, including cooperative grants to support disease-monitoring efforts by academic researchers in developing countries and high-profile awards from bodies such as the Institute of Medicine or World Health Organization to countries or individuals who make important sacrifices for the health of world.
Networking can also play a vital role in local and regional preparedness for infectious disease threats. Tabletop exercises, in which detailed outbreak scenarios are presented to officials who develop a response based on the tools and resources at their disposal, encourage preparedness and provide a forum for building collaborations among the many individuals and sectors essential to an effective, coordinated response. From such exercises, the real-time compilation of epidemiological, clinical, and laboratory data that could be made available to the international community through WHO could also stimulate cooperation and collaboration. When implemented via the Internet or other communication net-
works, these exercises can be used to develop systems of communication, as well as working relationships, in advance of an outbreak or other emergency.
Some countries are increasingly cognizant of the fact that the health of the global public affects the individual security of all nations, especially those that are most enmeshed in global networks of trade, tourism, and investment. Nevertheless, many governments continue to allocate inadequate resources to their health care systems and lack the political will to improve the quality of their public health systems and the integration of those systems nationally and internationally. This observation highlights an additional lesson offered by SARS, one that echoes what we have learned from HIV/AIDS, influenza, Ebola, malaria, and a host of other infectious diseases: the desperate state of public health infrastructure in much of the world, and especially in those countries where microbial threats are likeliest to emerge and take hold. If such lessons are to be heeded, global strategies to enhance the prevention and control capabilities of all nations will be important as the world prepares for future outbreaks of infectious disease.
Adel A.F. Mahmoud, M.D., Ph.D.
Chair, Forum on Microbial Threats
Stanley M. Lemon, M.D.
Vice-Chair, Forum on Microbial Threats
REFERENCES
Center for Disease Control Taiwan. A report on the laboratory-acquired SARS in Taiwan. [Online] Available: http://www.cdc.gov.tw/sarsen/ [accessed January 19, 2004].
Centers for Disease Control and Prevention. Public health and aging: influenza vaccination coverage among adults aged >50 years and pneumococcal vaccination coverage among adults aged >65 years—United States, 2002. MMWR 52(41):987-92.
Enserink M. 2003. SARS in China. China’s missed chance. Science 301(5631):294-6.
Eysenbach G. 2003. SARS and population health technology. Journal of Medical Internet Research 5(2):e14.
General Accounting Office. 2001. Challenges in Improving Infectious Disease Surveillance Systems. GAO-01-722. Washington, DC: GAO.
Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CLLSW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KLCKW, Lim W, Shortridge KF, et al. 2003. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science 302(5643):276-8.
Hogg C. 2003. Test for early detection of SARS. BBC News.
Holmes KV. 2003. SARS coronavirus: a new challenge for prevention and therapy. Journal of Clinical Investigation 111(11):1605-9.
Institute of Medicine. 2003. Microbial Threats to Health: Emergence, Detection, and Response. Washington, DC: The National Academies Press.
Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, Ahuja A, Yung MY, Leung CB, To KF, Lui SF, Szeto CC, Chung S, Sung JJ. 2003. A major outbreak of severe acute respiratory syndrome in Hong Kong. New England Journal of Medicine 348(20):1986-94.
National Intelligence Council. 2000. National Intelligence Estimate: The Global Infectious Disease Threat and Its Implications for the United States. NIE 99–17D. Washington, DC: NIC.
Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, Ho LM, Peiris JS. 2003. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet 361(9368):1519-20.
Singapore Government. 2003. Singapore government SARS website. [Online] Available: http://www.sars.gov.sg/ [accessed January 18, 2004].
Taylor LH, Latham SM, Woolhouse ME. 2001. Risk factors for human disease emergence. Philosophical Transactions of the Royal Society of London-Series B: Biological Sciences 356(1411):983-9.
Treanor J. 2004. Influenza vaccine—outmaneuvering antigenic shift and drift. New England Journal of Medicine 350(3):218-20.
University of California–Berkeley. 2003. Will a mask protect you? UC Berkeley Wellness Letter. [Online] Available: http://wellnessletter.com/html/wl/2003/wlFeatured0703.html.
World Health Organization (WHO). 2003a. Summary of probable SARS cases with onset of illness from November 2, 2002 to July 42, 2003. [Online] Available: http://www.who.int/csr/sars/country/table2003_09_23/en/ [accessed December 17, 2003].
WHO. 2003b. Acute respiratory syndrome in China—Update. [Online] Available: http://www.who.int/csr/don/2003_2_20/en/ [accessed December 17, 2003].
WHO. 2003c. Update 95—SARS: chronology of a serial killer. [Online] Available: http://www.who.int/csr/don/2003_07_04/en/.
WHO. 2003d. WHO issues a global alert about cases of atypical pneumonia. [Online] Available: http://www.who.int/csr/sars/archive/2003_03_12/en/.
WHO. 2003e. World Health Organization issues emergency travel advisory. [Online] Available: http://www.who.int/csr/sars/archive/2003_03_15/en/.
WHO. 2003f. Update 47—Studies of SARS virus survival, situation in China. [Online] Available: http://www.who.int/csr/sars/archive/2003_05_05/en/print.html.
WHO. 2003g. Update 96—Taiwan, China: SARS transmission interrupted in last outbreak area. [Online] Available: http://www.who.int/csr/don/2003_07_05/en/print.html.
WHO. 2003h. Update 70—Singapore removed from list of areas with local SARS transmission. [Online] Available: http://www.who.int/csr/don/2003_05_30a/en/print.html.
WHO. 2003i. Severe Acute Respiratory Syndrome (SARS)-multi-country outbreak-Update 13: China joins WHO collaborative network. [Online] Available: http://www.who.int/csr/don/2003_03_28/en/.
WHO. 2003j. WHO issues consensus document on the epidemiology of SARS. [Online] Available: http://www.who.int/csr/sars/archive/epiconsensus/en/print.html.
WHO. 2003k. Revision process of the International Health Regulations (IHR). [Online] Available: http://www.who.int/csr/ihr/revision/en/print.html.
WHO. 2003l; Severe acute respiratory syndrome (SARS) in Singapore—update 2: SARS case in Singapore linked to accidental laboratory contamination. [Online] Available: http://www.who.int/csr/don/2003_09_24/en/ [accessed January 18, 2004].
WHO. 2003m. Summary of the discussions and recommendations of the SARS laboratory workshop, October 22, 2003. [Online] Available: http://www.who.int/csr/sars/guidelines/en/SARSLabmeeting.pdf [accessed January 14, 2004].
WHO. 2003n. Update 11—WHO recommends new measures to prevent travel-related spread of SARS. [Online] Available: http://www.who.int/csr/sars/archive/2003_03_27/en/ [accessed January 20, 2004].
WHO. 2003o. Avian influenza (“bird flu”) and the significance of its transmission to humans. [Online] Available: http://www.who.int/csr/don/2004_01_15/en/ [accessed January 26 2003].
Yam WC, Chan KH, Poon LLM, Guan Y, Yuen KY, Seto WH, Peiris JSM. 2003. Evaluation of reverse transcription-PCR assays for rapid diagnosis of severe acute respiratory syndrome associated with a novel coronavirus. Journal of Clinical Microbiology 41(10):4521-4.
Zhong NS, Zheng BJ, Li YM, Poon, Xie ZH, Chan KH, Li PH, Tan SY, Chang Q, Xie JP, Liu XQ, Xu J, Li DX, Yuen KY, Peiris, Guan Y. 2003. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People’s Republic of China, in February 2003. Lancet 362(9393):1353-8.








































