1
Introduction and Historical Background
INTRODUCTION
The first outbreak of a waterborne disease to be scientifically documented in modern Western society occurred in London, England, in 1854. This early epidemiology study by John Snow, a prominent local physician, determined that the consumption of water from a sewage-contaminated public well led to cholera (Snow, 1854a,b). This connection, decades before the germ theory of disease would be hypothesized and proven, was the first step to understanding that water contaminated with human sewage could harbor microorganisms that threaten public health. Since then, epidemiology has been the major scientific discipline used to study the transmission of infectious diseases through water (NRC, 1999a).
In the late nineteenth century and throughout the twentieth century, sanitary practices were established in the UnhÚed States regarding the handling and disposal of sewage, while filtration and chlorination systems were increasingly used to disinfect drinking water. Through these historical efforts and owing to ongoing advances in water and wastewater treatment and source water protection, the United States has secured and maintains one of the cleanest and safest supplies of drinking water in the world. Starting in 1920, national statistics on waterborne disease outbreaks caused by microorganisms, chemicals, or of unknown etiology have been collected by a variety of researchers and federal agencies (Lee et al., 2002). These data demonstrate that several outbreaks still occur every year in this country. Moreover, epidemiologists generally agree that these reported outbreaks represent only a fraction of the total that actually occur because many go undetected or unreported (NRC, 1999a). Thus, continued vigilance to protect the public from waterborne disease remains a necessity.
For more than 100 years, U.S. public health personnel have relied extensively on an indicator organism approach to assess the microbiological quality of drinking water. These bacterial indicator microorganisms (particularly “coliforms,” described later) are typically used to detect the possible presence of microbial contamination of drinking water by human waste. More specifically, fecal indicator bacteria provide an estimation of the amount of feces, and indirectly, the presence and quantity of fecal pathogens in the water. Over the long history of their development and use, coliform test methods have been standardized, they are relatively easy and inexpensive to use, and enumeration of coliforms has proven to be a useful method for assessing sewage contamination of drinking water. In conjunction with chlorination to reduce coliform levels, this practice has led to a dramatic decrease in waterborne diseases such as cholera and typhoid fever. Furthermore, the use of bacterial indicators has been extended to U.S. “ambient” waters in recent decades—especially freshwater and marine-estuarine waters used for recreation. However, an increased understanding of the diversity of waterborne pathogens, their sources, physiology, and ecology has resulted in a growing understanding that the current indicator approach may not be as universally protective as was once thought. In this regard, several limitations of bacterial indicators for waterborne pathogens have been reported and are discussed throughout this report.
To protect public health, it is important to have accurate, reliable, and scientifically defensible methods for determining when water is contaminated by pathogens and to what extent. Furthermore, recent and forecasted advances in microbiology, biology, and analytical chemistry make it timely to assess the current paradigm of relying predominantly or exclusively on traditional bacterial indicators for waterborne pathogens in order to make judgments concerning the microbiological quality of water to be used for recreation or as a source for drinking water supply.
Committee and Report
This report was prepared by the National Research Council (NRC) Committee on Indicators for Waterborne Pathogens—jointly overseen by the NRC’s Board on Life Sciences and Water Science and Technology Board. The committee consists of 12 volunteer experts in microbiology, waterborne pathogens (bacteriology, virology, parasitology), aquatic microbial ecology, microbial risk assessment, water quality standards and regulations, environmental engineering, biochemistry and molecular biology, detection methods, and epidemiology and public health. The report’s conclusions and recommendations are based on a review of relevant technical literature, information gathered at four committee meetings, a public workshop on indicators for waterborne pathogens (held on September 4, 2002), and the collective expertise of committee members.
The committee was formed in early 2002 at the request of the U.S. Environ-
mental Protection Agency (EPA) Office of Water to report on candidate indicators and/or indicator approaches (including detection technologies) for microbial pathogen contamination in U.S. recreational waters (excluding coastal marine water and marine-estuarine water) and source water (including groundwater) for drinking water.1 It is important to note that the committee’s charge, as outlined in its statement of task (see Box ES-1), was slightly but substantively altered after its first meeting and subsequent discussions with EPA, most notably to include coastal and marine-estuarine recreational waters that were originally excluded. As a result, it was agreed that the committee’s report would give less space and emphasis to the importance and public health impacts of waterborne pathogens; place less emphasis on defining currently known waterborne pathogen classes and anticipating those emerging waterborne pathogens that are likely to be of public health concern (although Appendix A provides a brief summary discussion and table of new and [re]emerging waterborne pathogens); exclude consideration of blue-green algae and their toxins; and not specifically consider how the use of candidate indicators might allow for determination of an appropriate level of water treatment needed to protect public health. It is also important to state that although an assessment of suitable indicators for shellfish waters is beyond the scope of this report, some discussion of shellfish experience is included because of the (especially historical) interrelatedness of the various microbial indicator standards and their development. Lastly, this report does not address public swimming and wading pools that are regulated by state and local health departments whose disinfection practices vary widely from place to place.
This chapter provides an introduction to the public health importance of waterborne pathogens; a brief summary of key federal laws, regulations, and programs concerning microbial water quality monitoring and especially the use of indicator organisms; the historical development and current use of microbial indicators for waterborne pathogens; and the current status of waterborne disease outbreaks and endemic disease. The chapter ends with a summary of its contents and conclusions. Chapter 2 provides an overview of health effects assessment as related to the current and future use of indicators of waterborne pathogens to help protect public heath. Chapter 3 focuses on the ecology and evolution of waterborne pathogens and indicator organisms by major classes (i.e., viruses, bacteria, protozoa). Chapter 4 assesses the development and uses of indicators and indicator approaches according to their applications and attributes, while Chapter 5 reviews some emerging and innovative approaches for measuring indicator organisms and waterborne pathogens. Lastly, Chapter 6 provides a recommended
|
1 |
For the purposes of this report, surface water sources for drinking water and recreational waters can be considered a subset of U.S. “ambient waters” and “waters of the United States” (see footnote 2). As such and per the statement of task, unless noted otherwise all discussion of “water” in this report refers to source water for drinking water (including groundwater) and freshwater, coastal, and marine-estuarine recreational waters. |
phased monitoring framework for selection and use of indicators, along with examples of how to use such a framework.
Relevant Laws and Regulations
It is beyond the scope of this report to systematically review and discuss all federal, state, or local laws, regulations, and programs that concern the microbiological quality of source water for drinking water and ambient recreational waters. Regarding the latter, state and local governments have primary authority for maintaining the quality and safety of recreational waters (both freshwater and marine). However, given their nationwide application, importance to this report, and direct relevance to the committee’s charge, a brief discussion of the Safe Drinking Water Act (SDWA), Clean Water Act (CWA), Beaches Environmental Assessment and Coastal Health (BEACH) Act of 2000, and several related regulations and programs follows (see also Tables 1-1 and 1-2).
Safe Drinking Water Act
The SDWA, enacted in 1974 and administered by EPA, is the most important and comprehensive law designed to protect the public from man-made or naturally occurring contaminants in drinking water. It has been amended regularly, including significant changes in 1986 and 1996. Prior to passage of the
TABLE 1-1 Microbiological and Other Indicators Used Under EPA’s Drinking Water Regulationsa,b
|
Rule or Program |
Indicator |
Use |
URLs and Notes |
|
Total Coliform Rule |
Total coliforms (TC) |
Determine treatment efficiency and distribution system integrity |
|
|
|
Fecal coliforms (FC) Escherichia coli |
Determine or verify presence of fecal contamination if PWSs obtain sample(s) positive for TC |
|
|
Surface Water Treatment Rule (SWTR), as amended by the following rules |
Turbidity |
Measure of filter efficiency and source water quality |
|
|
Disinfectant residual |
Nondetection of a disinfectant residual indicates a distribution system problem |
|
|
Rule or Program |
Indicator |
Use |
URLs and Notes |
|
Interim Enhanced SWTR |
Heterotrophic plate count |
Measure of drinking water quality in distribution system |
|
|
Long-Term 1 ESWTR |
TC FC |
Measure of source water quality (for unfiltered PWSs) |
|
|
Information Collection Rule (1996-1998) |
Cryptosporidium Giardia Total culturable viruses TC FC |
Results provided information to facilitate development of the Long-Term 2 ESWTR |
http://www.epa.gov/safewater/icr.html Applicable for PWSs serving ≥ 100,000 persons to provide treatment data and monitor disinfection by-products and source water quality parameters |
|
Long-Term 2 ESWTR (proposed rule) |
Cryptosporidium E. coli |
Determine minimum treatment level needed by surface water system |
|
|
Groundwater Rule (final rule expected in late 2004) |
E. coli Enterococci Coliphage |
Determine presence of fecal contamination in source groundwater |
http://www.epa.gov/safewater/gwr/gwrprop.pdf GWR does not apply to privately owned wells that serve <25 person (e.g., household wells) |
|
Drinking Water Contaminant Candidate List (CCL) |
Virulence-factor activity relationships (under consideration) |
Assess potential pathogenicity (virulence) of waterborne pathogens as recommended in Classifying Drinking Water Contaminants for Regulatory Consideration (NRC, 2001) |
www.epa.gov/safewater/ccl/ccl_fr.html www.epa.gov/safewater/ndwac/mem_ccl_cp.html First CCL published in 1998 as required by the SDWA Amendments of 1996, includes 10 pathogens and groups of related pathogens (EPA,1998a) |
|
aAs of August 11, 2003. bRefer to actual rules (URLs) for a description of the monitoring requirements. SOURCES: EPA, 2002d; Lee et al., 2002. |
|||
TABLE 1-2 Microbiological and Other Indicators Used Under Select CWA Regulations and Related Programs
|
Activity or Program |
Indicator |
Use |
URLs and Notes |
|
Ambient Water Quality Criteria for Bacteria |
Freshwater: Escherichia coli Enterococci Marine water: Enterococci |
Determine presence of fecal contamination in ambient and recreational waters |
|
|
Beaches Environmental Assessment and Coastal Health Act of 2000 |
E. coli Enterococci Proposed rapid methods such as Bioluminometer Fiber optics System flow cytometry |
Rapidly determine presence of fecal contamination in freshwater and marine recreational waters |
|
|
Shellfish Program |
Total coliforms (TC) Fecal coliforms (FC) E. coli |
Help ensure shellfish waters are adequately protected from microbial contamination |
|
|
Biosolids (Treated Sewage Sludge) Program |
FC Salmonella Enteric viruses Viable helminth ova |
Adequacy of sludge treatment practices to protect human and environmental health |
http://www.epa.gov/owmitnet/mtb/biosolids/ See also (NRC, 2002) http://cfpub.epa.gov/npdes/ |
|
National Pollutant Discharge Elimination System (NPDES Permitting Program) |
TC FC Fecal streptococci |
Ensure ambient water quality standards are maintained despite pollutant discharges |
|
|
305(b) Water Quality Assessment Report Program |
Varies by state |
Determine if waters meet state-determined ambient water quality standards |
http://www.epa.gov/owow/monitoring/guidelines.html http://www.epa.gov/owow/tmdl/2002wqma.html See also Table 1-3 |
|
303(d) Impaired Waters List and Total Maximum Daily Load (TMDL) Program |
Varies by state |
Determine if waters meet state-determined ambient water quality standards |
http://www.epa.gov/owow/tmdl/pathogen_all.pdf |
|
SOURCE: EPA, 2002d. |
|||
SDWA, the only enforceable federal drinking water standards were for waterborne pathogens in water supplies used by interstate carriers such as buses and trains. Interested readers should refer to Safe Water from Every Tap: Improving Water Service to Small Communities (NRC, 1997) for an overview of the development of drinking water supply regulations in the United States to include the SDWA, or to Pontius and Clark (1999) for a more thorough discussion of the SDWA and its subsequent amendments.
Under the SDWA, microbial contamination is regulated primarily under the Total Coliform Rule (TCR) and the Surface Water Treatment Rule (SWTR), both originally promulgated in 1989 (EPA, 1989a,b, 1990). Under the TCR, all public water systems (PWSs) are required to routinely collect total coliform samples at sites that are considered representative of water throughout the distribution system. The SWTR covers all drinking water systems using surface water or groundwater systems that rely on surface water, requiring them to disinfect their water, while most must also filter (unless they meet EPA-stipulated filter avoidance criteria). The SWTR is intended to protect the public from exposure to the intestinal protozoan parasite Giardia lamblia and viruses through a combination of removal (filtration) and inactivation (disinfection) (EPA, 1989a).
In 1998, EPA promulgated the Interim Enhanced Surface Water Treatment Rule (IESWTR; EPA, 1998c), which builds on the SWTR and includes more stringent requirements related to the performance of filters used in drinking water treatment to protect against the protozoan parasite Cryptosporidium and other pathogens for systems that serve more than 10,000 persons. Similarly, EPA promulgated and finalized the Long-Term 1 Enhanced Surface Water Treatment Rule (LT1ESWTR) requiring PWSs that serve less than 10,000 persons (EPA, 2002a) to meet more stringent filtration requirements. In addition, EPA recently proposed a Long-Term 2 Enhanced Surface Water Treatment Rule (LT2ESWTR) that will provide additional protection against Cryptosporidium and will apply to all systems using surface water or groundwater under the influence of surface water (EPA, 2003b). All PWSs will be assigned to a water treatment category (“bin”) based on Cryptosporidium concentrations in their source water; the category determines how much additional treatment is required. In 2000, EPA proposed the Ground Water Rule (GWR) in response to the SDWA Amendments of 1996 that mandate the development of regulations for the disinfection of groundwater systems as necessary to protect public health (EPA, 2000b). The GWR had not yet been finalized as this report neared publication in early 2004. Table 1-1 summarizes these and other existing and proposed rules and programs concerning the use of pathogens under the auspices of the SDWA and EPA.
Clean Water Act
Growing public awareness of and concern for controlling water pollution nationwide led to enactment of the Federal Water Pollution Control Act (FWPCA;
originally enacted in 1948) Amendments of 1972. Together with the Clean Water Act of 1977 and the Water Quality Act of 1987—both of which amended and reauthorized the FWPCA—it provides the foundation for protecting the nation’s surface waters. Collectively, they are referred to as the Clean Water Act, and that usage is maintained throughout this report. The CWA is of central importance to this report in that it is a comprehensive statute intended to restore and maintain the chemical, physical, and biological integrity of the waters of the United States.2 To accomplish this, the CWA sought to attain a level of water quality that “provides for the protection and propagation of fish, shellfish, and wildlife, and provides for recreation in and on the water” by 1983 and to eliminate the discharge of pollutants into navigable waters by 1985. Primary authority for implementation and enforcement of the CWA rests with the EPA. In addition to measures authorized before 1972, the CWA authorizes water quality programs; requires federal effluent limitations for wastewater discharges to surface waters and publicly owned treatment works (i.e., municipal sewage treatment plants) and ambient water quality standards;3 requires permits for discharge of pollutants4 into waters of the United States; provides enforcement mechanisms; and authorizes funding for wastewater treatment works construction grants and state revolving loan programs, as well as funding to states and tribes for their water quality programs. Provisions have also been added to address water quality problems in specific regions and specific waterways, and the CWA has been amended almost yearly since its inception. Due consideration must be given to the improvements necessary to conserve these waters for the protection and propagation of fish and
|
2 |
As defined in the CWA, “waters of the United States” applies only to surface waters, rivers, lakes, estuaries, coastal waters, and wetlands. However, not all surface waters are legally waters of the United States, and the exact division between waters of the United States and other waters can be difficult to determine. In addition, it is important to note that the CWA does not deal directly with groundwater or water quantity issues; see http://www.epa.gov/r5water/cwa.htm or http://www.epa.gov/watertrain/cwa/ for further information about the CWA. |
|
3 |
Ambient water quality standards (AWQSs) are determined by each state (collectively includes territories, American Indian tribes, the District of Columbia, and interstate commissions of the United States) and consist of (1) designated beneficial uses (e.g., aquatic life support, drinking water supply, primary contact recreation); (2) narrative and numeric criteria (ambient water quality criteria, or AWQC; discussed later) for biological, chemical, and physical parameters to meet designated use(s); (3) antidegradation policies to protect existing uses; and (4) general policies addressing implementation issues (e.g., low flows, variances). State water quality standards have become the centerpiece around which most surface water quality programs revolve; for example, they serve as the benchmark for which monitoring data are compared to assess the health of waters and to list impaired waters under CWA Section 303(d) (discussed later). |
|
4 |
As authorized by the CWA (Section 402), the National Pollutant Discharge Elimination System (NPDES) Permitting Program controls water pollution by regulating point sources (e.g., discrete conveyances such as pipes or man-made ditches) that discharge pollutants into waters of the United States. |
aquatic life and wildlife, recreational purposes, and the withdrawal of water for public water supply, agricultural, industrial, and other purposes. Not surprisingly, EPA conducts a wide variety of programs and activities related to the monitoring of indicators for waterborne pathogens under the CWA as summarized in Table 1-2. It is important to note, however, that many of these listed programs and activities lie outside the committee’s charge.
Regarding the attainment of water quality standards, Section 305(b) of the CWA requires states and other jurisdictions (e.g., American Indian tribes, District of Columbia) to assess and submit to EPA the health of their waters and the extent to which their water quality standards are being met every two years. In 2002, EPA released the 2000 National Water Quality Inventory (NWQI; EPA, 2002c)—the thirteenth installment in a series that began in 1975. These NWQI reports (commonly called “305(b) reports”), as the biannual culmination of the 305(b) process, are considered by EPA to be the primary vehicle for informing Congress and the public about general water quality conditions in the United States5 (EPA, 1997). As such, the reports characterize water quality, identify widespread water quality problems of national significance, and describe various programs implemented to restore and protect U.S. waters. Notably, states use bacterial indicators—although specific indicators, methods, and sampling practices vary from state-to-state—to determine whether waters are safe for swimming and drinking (i.e., support designated beneficial uses). Table 1-3 summarizes select findings from the 2000 NWQI report (EPA, 2002c) related to the identification of surface waters impaired by pathogens (predominantly bacteria).
In addition to establishing water quality standards, and similar to Section 305(b) of the CWA, Section 303(s) of the CWA requires states to identify waters not meeting ambient water quality standards and include them on their 303(d) list of impaired waters. Section 303(d) also requires states to define the pollutants and sources responsible for the degradation of each listed water, establish total maximum daily loads (TMDLs6) necessary to attain those standards, and allocate responsibility to sources for reducing their pollutant releases. The CWA further requires that water quality standards be maintained once obtained and that EPA must approve or disapprove all lists of impaired waters and TMDLs established by states (NRC, 2001). If a state submission is inadequate, EPA must establish the list or the TMDL.
Consistent with the latest NWQI report (EPA, 2002c), in 2000 EPA released
TABLE 1-3 Selected Findings and Results from the 2002 National Water Quality Inventory
|
Waterbody Type |
Total Sizea |
Amountb Assessed (% of Total) |
|
Coastal resources: Ocean shoreline waters |
58,618 miles |
3,221 miles (6%) |
|
Rivers and streams |
3,692,830 miles |
699,946 miles (19%) |
|
Coastal resources: Estuaries |
87,369 sq. miles |
31,072 sq. miles (36%) |
|
Coastal resources: Great Lakes shoreline |
5,521 miles |
5,066 miles (92%) |
|
Lakes, reservoirs, and ponds |
40,603,893 acres |
17,339,080 acres (43%) |
|
aUnits are miles for rivers and streams; acres for lakes, reservoirs, and ponds; and square miles for coastal resources (estuaries, Great Lakes shoreline, and ocean shoreline waters). bIncludes waterbodies assessed as not attainable for one or more designated uses (i.e., total number of waterbody units assessed as good and impaired do not necessarily add up to total assessed). |
||
Atlas of America’s Polluted Waters (EPA, 2000a), which states that about 21,000 river segments, lakes, and estuaries encompassing more than 300,000 river and shore miles and 5 million lake acres have been reported as impaired by states and that the second leading cause of impairments (behind sedimentation or siltation) is “pathogens.”7 As for the 305(b) reports, states rely primarily on bacterial indi-
|
Impairedc (% of Assessed) |
Impaired by Pathogens (Bacteria; % of Impaired) |
Top Five Leading Pollutants and Causes of Impairmentd |
|
434 miles (14%) |
384 miles (88.5%) |
Pathogens (bacteria) Oxygen-depleting substances Turbidity Suspended solids Oil and grease |
|
269,258 miles (39%) |
93,431 miles (34.7%) |
Pathogens (bacteria) Siltation Habitat alteration Oxygen-depleting substances Nutrients |
|
15,676 sq. miles (51%) |
4,754 sq. miles (30%) |
Metals Pesticides Oxygen-depleting substances Pathogens (bacteria) Priority toxic organic chemicals |
|
3,955 miles (78%) |
102 miles (9.3%) |
Priority toxic organic chemicals Nutrients Pathogens (bacteria) Sedimentation or siltation |
|
7,702,370 acres (45%) |
Not reported |
Nutrients Metals Siltation Total dissolved solids Oxygen-depleting substances |
|
cPartially or not supporting one or more designated uses. dFor states and jurisdictions that report this type of information (i.e., often a subset of the total number of states and jurisdictions that assess and report on various waterbodies; see EPA, 2002e for further information). SOURCE: Adapted from EPA, 2002c. |
||
cators rather than specific pathogens to assess whether waters are achieving their standards and to develop TMDLs. Indeed, EPA estimates that from 3,800 to 4,000 TMDLs will have to be completed per year to meet typical 8- to 13-year dead-lines imposed on the process (NRC, 2001). It is beyond the scope of this report to discuss the 303(d) TMDL process in any detail. Rather, please refer to the 2001 NRC report Assessing the TMDL Approach to Water Quality Management, which reviews the program at the request of Congress and provides many recommendations for its comprehensive improvement. For example, based on that report, EPA
recently provided states with guidance for integrating the development and submission of 2002 305(b) water quality reports and Section 303(d) lists of impaired waters. More specifically, the guidance recommends that states, territories, and authorized tribes submit a 2002 Integrated Water Quality Monitoring and Assessment Report that will satisfy CWA requirements for both Section 305(b) water quality reports and Section 303(d) impaired water lists.8
As noted previously, regulation of recreational water (both freshwater and marine waters) is the responsibility of state and local governments. As a result, local monitoring and management programs for recreational waters vary widely, resulting in different standards and levels of protection across the nation. To help address these and related issues, in 1999 EPA issued Action Plan for Beaches and Recreational Waters (Beach Action Plan), a multiyear strategy to improve the monitoring of recreational water quality and the communication of public health risks associated with pathogen-contaminated recreational rivers, lakes, and ocean beaches (EPA, 1999). The Beach Action Plan describes activities of EPA’s Office of Water (OW) and Office of Research and Development (ORD) to accomplish two primary objectives: (1) enable consistent management of recreational water quality programs and (2) improve the science that supports recreational water monitoring programs.
Furthermore, in October 2000, the Beaches Environmental Assessment and Coastal Health Act of 2000 was signed into effect. The BEACH Act requires coastal states to monitor beach water quality and warn the public when these waters contain dangerously high levels of disease-causing microorganisms. More specifically, it amends the CWA to require ocean, bay, and Great Lakes states to adopt minimum, health-based criteria for water quality, comprehensively test recreational beach waters for indicators of waterborne pathogens, and notify the public when contamination levels make beach water unsafe for recreation. Under the BEACH Act, EPA is required to work with states to ensure that they use the latest science to sample and test beach waters to protect the public’s health. Besides requiring consistency by bringing all states up to EPA criteria, the law also requires EPA to upgrade these criteria and to develop new criteria, based on the most recent scientific studies. As a starting point, and in response to the Beach Action Plan and the BEACH Act, EPA recently published for public comment Implementation Guidance for Ambient Water Quality Criteria (EPA, 2002b), which builds on the seminal report Ambient Water Quality Guidance for Bacteria − 1986 (EPA, 1986; see Table 1-2 and later discussion). When finalized, this document will help guide state, territorial, and authorized tribal water quality programs in adopting and implementing bacteriological water quality criteria to protect ambient waters designated for recreation.
|
8 |
See http://www.epa.gov/owow/tmdl/2002wqma.pdf for further information. |
Integrating the SDWA and the CWA
On August 6, 2001, EPA released the draft Strategy for Waterborne Microbial Disease (EPA, 2001), which describes a multiyear strategy for reducing the adverse impacts of microbial contamination in U.S. waters through improved water quality programs, scientific advancements, and risk communication. Moreover, it is an initial effort by EPA to begin to integrate the traditionally separate microbial assessment regulations, programs, and use of differing indicators of waterborne pathogens (see Tables 1-1 and 1-2) under the SDWA and CWA. Specifically, EPA’s draft strategy report identifies the “top four approaches” to water protection, which include limiting both water contamination and exposure: (1) develop an integrated, risk-based approach to setting ambient water quality criteria and related guidance (see footnote 3) based on exposure and the application of a common set of fecal indicators across various uses of water, rather than different indicators for specific uses; (2) manage contamination sources; (3) establish monitoring and treatment standards or discharge criteria for reused water and currently unregulated industrial wastes; and (4) develop an EPA-generated microbial risk assessment paradigm. Notably, several aspects of the first approach are of particular relevance to this report and are discussed in later chapters (especially Chapters 4 and 6). The strategy report is not expected to be finalized and released until sometime in 2004 (Lisa Almodovor, EPA, personal communication, 2003).
REPORTS ON PUBLIC HEALTH IMPACTS OF, AND INDICATORS FOR, WATERBORNE PATHOGENS
Although this is the first NRC study to focus specifically on indicators for waterborne pathogens, issues surrounding their use have been discussed in several recent and historical NRC reports, as summarized in chronological order in Appendix B. Many of these reports review the public health importance of waterborne pathogens, which is discussed briefly in this chapter and in much greater detail in Chapter 2. In addition to the NRC, many federal, state, local government, and nongovernmental organizations, including the water industry and academia, have addressed the issue of the microbiological quality of drinking water and recreational water and its association with various adverse human health effects such as gastroenteritis, ear and eye infections, dermatitis, and respiratory disease. Thus, Appendix B also includes summaries of some key reports that have been conducted and published addressing these concerns.
A recurring theme of many of the reports listed in Appendix B is the need for scientifically defensible, innovative, reliable, rapid, and inexpensive approaches and methods for indicating and detecting the presence of waterborne pathogens, given their clear public health importance. Indeed, identifying, assessing, and recommending ways to help EPA address this need form the core of this report.
HISTORICAL BACKGROUND
In the United States, the principal indicators for waterborne pathogens presently in use are total coliform, fecal coliform, Escherichia coli, and enterococci. The coliform group (described below) is used widely as an indicator of fecal contamination of drinking water, recreational waters, and shellfishing waters, and as a measure of water treatment effectiveness. Enterococci are typically used as indicators of fecal contamination of recreational waters (EPA, 1986, 2002b). Some understanding of the historical development and application of these indicators is useful to help understand their current uses and limitations and to put this report into context.
Evolution of the Use of the Coliform Group
As noted previously, for a period of approximately 100 years following the ground-breaking work of John Snow, the public health community concentrated on preventing the transmission of waterborne bacterial disease through the fecal-to-oral route, particularly the diseases caused by Vibrio cholerae and Salmonella spp. Using methods available during that time, directly monitoring for the presence or absence of these bacteria in drinking water would not provide satisfactory or reliable protection of public health. Consequently, efforts were made to develop a more sensitive way to discern fecal contaminated water (i.e., a fecal contamination index.)
The index developed was based on Escherichia coli, a small bacillus first discovered by professor Theodor Escherich of Germany while he was attempting to identify the cause of cholera (Escherich, 1885). This bacterium is present at extremely high levels in the feces of warm-blooded animals. Near the end of the nineteenth century, Theobold Smith of the State of New York Department of Health developed a presumptive test for E. coli using a lactose-based fermentation tube test (Smith, 1891). Smith’s classic fermentation tube test responds to a group of bacteria called the coliform group, of which E. coli is the most important member. As a result, it is commonly referred to as the coliform test. Shortly after Smith’s work, the State of New York employed the coliform test to demonstrate that sewage contamination of the Mohawk River, a tributary of the Hudson River, had caused typhoid fever in persons drinking water from the Hudson downstream of the confluence of the two rivers (Mason, 1891).
In 1897, the American Public Health Association (APHA) adopted standard procedures for the coliform test, and in 1909 these procedures were published in the first edition of Standard Methods for the Examination of Water and Wastewater (Wolfe, 1972). In 1914, the U.S. Public Health Service (USPHS) set a standard requiring that drinking waters not show evidence of the coliform organism (U.S. Treasury Department, 1914). Technically speaking, as noted earlier, the USPHS standard applied only to waters transported across state boundaries, but it was not long before the test became a standard across the United States (APHA,
1965). Around the beginning of World War II, work done at the USPHS research center in Cincinnati demonstrated that E. coli measurements could be used to estimate the concentration of Salmonella typhi (the cause of typhoid fever) in sewage (Kerr and Butterfield, 1943) and that E. coli are more resistant to disinfection and environmental exposure than several other important bacterial pathogens (Wattie and Butterfield, 1944). This work historically solidified coliform measurement (1) as a means of confirming that a drinking water source was microbiologically safe and (2) for determining whether water treatment had been successful.
Method Refinement
As soon as the coliform test came into widespread acceptance, complications with its use and interpretation began to emerge. One concern was the discovery that a variety of microorganisms that read positive in the coliform test were not of fecal origin. As a result, the test method has evolved continually to become more specific. Some of the more significant developments were the so-called fecal coliform test9 (Geldreich, 1966)—which selects for coliforms of fecal origin by using a higher incubation temperature—and, later on, the MUG test specifically identifies E. coli based on the action of β-glucuronidase10 (Edberg et al., 1988).
Questions have also surfaced concerning the suitability of E. coli as a bacterial indicator of sewage-contaminated water in certain climates, especially tropical and subtropical climates where E. coli is sometimes indigenous (Bermudez and Hazen, 1988; Fujioka, 2001; Fujioka et al., 1999, Hardina and Fujioka, 1991; Hazen et al., 1987; Rivera et al., 1988). As a result, studies using a number of alternative microorganisms to coliforms or E. coli began to appear, particularly enterococci (Slanetz et al., 1955) and Clostridium perfringens (Fujioka and Shizumura, 1985; Fujioka et al., 1997). Enterococci and their taxonomically broader predecessor group, the so-called fecal streptococci, as well as Clostridium perfringens and its broader predecessor group the sulfite-reducing clostridia, have a long history of use and refinement as bacterial indicators of fecal contamination, as summarized below. The development and use of these alternative indicators has continued since the late 1800s because of ongoing concerns about the validity of coliforms as fecal indicators and because of certain properties that made them attractive alternatives to coliforms. Such efforts were necessary to help preserve the validity of using bacterial indicator tests as a sign of fecal contamination.
Fecal Streptococci and Enterococci
The prototypical enterococci, or what were previously called “fecal streptococci,” were first discovered and reported in the late 1880s by several researchers. Enterococcus faecalis was previously named “Micrococcus ovalis” by Escherich (1887), before being called Enterococcus faecalis by Andrewes and Horder (1906). The genus name Enterococcus was first used by Thiercelin (1899) and Thiercelin and Jouhaud in 1903. Enterococcus faecium was first recognized in 1899 and further characterized by Orla-Jensen (1919). By 1900, these bacteria were recognized as being of fecal origin and were proposed as fecal indicators. Several other species of enterococci and streptococci of fecal origin were identified over time. Dible (1921) proposed the name Streptococcus faecalis for what was previously called Enterococcus faecalis. Sherman (1937) proposed that the fecal enterococcal bacterial species of intestinal origin be classified in the genus Streptococcus, which led to widespread use of the term “fecal streptococci” for these bacteria. All of these bacteria are Gram-positive, catalase-negative, non-spore forming, facultative anaerobes with a coccoid shape and belong to the Lancefield Group D streptococci.11 Based on molecular and immunological evidence however, the two species considered of likely fecal origin, faecalis and faecium, along with most other species belonging to the Lancefield Group D, such as S. durans and S. avium were reclassified from the streptococci to the enterococci in 1984. Only a few species in Lancefield Group D were left in the Streptococcus genus, notably the fecal bacteria Streptococcus bovis and S. equinus. There are currently at least 26 documented species of enterococci (Klein, 2003). The streptococci are phenotypically distinguishable from the enterococci by their inability to grow in 6.5 percent NaCl and at 10oC.
Fecal streptococci and enterococci were further evaluated as fecal indicators of water quality in the 1940s and 1950s by several groups. Efforts were made to improve the medium for their detection, with the goal of detecting those microorganisms of primarily fecal origin (Burman, 1961; Kenner et al., 1961; Litsky et al., 1955; Mallmann and Seligman, 1950; Slanetz and Bartley, 1957). Initial efforts also were made to compare these bacteria to coliforms as water quality indicators (Burton, 1949; Ostrolenk et al., 1947). In the 1970s, Cabelli and colleagues of the EPA developed a membrane filter method to detect enterococci, specifically E. faecalis and E. faecium, in water and found that these bacteria were reliable predictors of gastrointestinal illness from primary contact recreation in marine waters (Levin et al., 1975). Subsequent studies have shown that the medium of this method detects at least some other enterococci species that were formerly considered fecal streptococci (Hagedorn et al., 2003).
Clostridium perfringens and Sulfite-Reducing Clostridia
Clostridium perfringens, an anaerobic, Gram-positive, spore-forming, rod-shaped bacterium, was first reported by Welch and Nuttall in 1892 as the cause of the disease gas gangrene. It was first called Clostridium welchii and later C. perfringens by Veillon and Zuber (1898). The potential value of C. perfringens as a fecal indicator of water contamination was reported as early as 1899 by the city of London (Klein and Houston, 1899; as cited by Bonde, 1963). Wilson and Blair (1925) also supported the use of sulfite-reducing clostridia (primarily C. perfringens) as fecal indicators for water. In Europe, C. perfringens has been used in conjunction with other sulfite reducing clostridia to detect fecal contamination in water since the 1960s (Ashbolt et al., 2001; Bonde, 1963; HMSO, 1969).
The source of C. perfringens and especially the spores in environmental samples has been a disputed topic. Some consider the organism to be of exclusively fecal origin but others consider the spores to be ubiquitous in soils, sediments, and other environmental media. Because the spores can survive for decades, their presence in environmental media can be difficult to interpret in the absence of a known source of fecal contamination. That is, they could either be natural environmental inhabitants or represent an historical source of fecal contamination. Uncertainties about the feces specificity of C. perfringens and sulfite-reducing clostridia and their extraordinary persistence in the environment are considered deficiencies in their use as fecal indicator organisms (Ashbolt et al., 2001; Cabelli, 1978). Despite these uncertainties, identification of C. perfringens spores became of increased interest in the 1980s and 1990s due to growing concerns about the pathogenic protozoa Giardia lamblia and Cryptosporidium parvum in water. The persistence of C. perfringens spores in the environment and their relative resistance to conventional water treatment suggest that they are potentially useful indicators of these highly resistant protozoa in drinking water systems and estuarine waters (Ferguson et al., 1996; Payment and Franco, 1993; Venczel et al., 1997). In addition, their apparent absence in unpolluted environmental waters in Hawaii supported their use as a fecal indicator of water quality in this tropical region (Fujioka, 2001).
Extension of the Coliform Indicator to Recreational and Shellfish Waters
Once it was widely understood that water could play an important role in the transmission of disease, it was only natural that this concern would extend from drinking water to recreational and shellfish waters. Shortly after the development of the first drinking water standards, the USPHS pursued concurrent investigations of the role of recreational and shellfish waters in enteric disease transmission by compiling data on outbreaks (Frost, 1925; Stokes, 1927a,b). Stokes (1927a,b) reported that a 1921 epidemic of typhoid fever at a boy’s camp was “unquestionably attributed to bathing in polluted waters.”
Around 1950, several proposed guidelines for recreational waters appeared (APHA, 1949; Cox, 1951; Scott, 1951; Streeter, 1951). In the late 1940s and early 1950s, the USPHS conducted a series of studies at bathing beaches on Lake Michigan, along the Ohio River, and on Long Island Sound (Stevenson, 1953). By the mid 1950s, a variety of bacterial indicator standards had appeared. In 1956, the City of Los Angeles conducted a survey of standards for recreational waters in 13 jurisdictions (Garber, 1956).12 The State of Illinois used enterococci,13 while the remaining jurisdictions used total coliforms. Statistical reporting varied over a wide range: eight jurisdictions used either a geometric mean or a median for total coliforms, three used an arithmetic mean, four used a percentage that could not be exceeded, and three used absolute maximums. The most common standard was a requirement that total coliforms not exceed 1,000 per 100 mL (see Chapter 2 for further information).
A recent review summarized current standards and proposed recreational criteria in all 50 states and various territories and tribes within the 10 EPA Regions (EPA, 2003a) and is compared to Garber’s (1956) survey in Table 1-4. The EPA survey revealed the use of four different bacterial indicators (total coliform, fecal coliform, E. coli, and enteroccoci) either alone or in various combinations. As in the 1950s, this recent survey showed a wide variety of approaches being used. The most common of these was a fecal coliform limit of 200 per 100 mL (geometric mean of 5 samples taken over 30 days). Particularly notable was California, where a total of 10 different standards were being used in various jurisdictions.
Introduction of Fecal Coliform to Recreational Water Criteria
In 1968, the National Technical Advisory Committee (NTAC) convened by the U.S. Federal Water Pollution Control Administration (predecessor to the EPA) was charged with proposing microbiological criteria for recreational waters. It was NTAC’s opinion that a fecal coliform measurement should be used rather than a total coliform measurement because the fecal coliform measurement is more specific.14 Using studies showing that about 18 percent of the total coliforms detected at the Ohio River sample locations used in earlier studies were also positive in the fecal coliform test (Cabelli, 1983), the NTAC converted the total
TABLE 1-4 Number of Jurisdictionsa Using an Indicator or Combination of Indicators for Recreational Waters: Mid-1950s Versus 2002
coliform density of 1,000 per 100 mL, already a common standard, to an estimated fecal coliform density of 200 per 100 mL (i.e., used a total-to-fecal coliform ratio of five-to-one). Thus, the NTAC (1968) recommended the following criteria for recreational waters: geometric mean <200 fecal coliforms per 100 mL; 90 percent of samples <400 fecal coliforms per 100 mL. These criteria were later adopted officially by EPA (1976).
Introduction of E. coli and Enterococci to Recreational Water Criteria
The recreational water criteria proposed by the NTAC in 1968 immediately became the subject of significant criticism (see discussion in Chapter 2). Beginning in 1972, EPA launched several epidemiologic studies designed to address the weaknesses of the previous ones. These included studies at freshwater recreational sites in Lake Erie, near Erie, Pennsylvania and Keystone Lake, near Tulsa, Oklahoma (Dufour, 1984). Similarly, marine studies were conducted at beaches in New York, Boston, and Lake Pontchartrain, Louisiana (Cabelli, 1983). These studies showed poor correlation between both total coliform and fecal coliform and reports of gastrointestinal disease. In contrast, the freshwater studies showed that both E. coli and enterococci were strongly correlated with gastroenteritis among swimmers, while the marine studies showed that enterococci were strongly
correlated in the same way. Following these studies, EPA promulgated new recreational water criteria designed to correspond to the health risks implicated in the earlier rules (EPA, 1986). For freshwater, these criteria specified geometric means of 126 per 100 mL and 33 per 100 mL for E. coli and enterococci, respectively. For marine recreational waters, a geometric mean of 35 per 100 mL was specified for enterococci. Interestingly, enterococci had been proposed for this purpose much earlier (Slanetz et al., 1955) but methods available at that time were problematic.
Detection methods have continued to evolve over the last several decades for the bacteria variously referred to as fecal streptococci, enterococci, and intestinal enterococci in recreational waters (e.g., Messer and Dufour, 1998). These developments, however, have been complicated by periodic changes in the taxonomy of these related groups of bacteria and the identification of new species. Recently, efforts have been made to harmonize both the terminology used to define these bacteria as well as the methods to detect them. In this regard, the European Union and the World Health Organization have come to use the term “intestinal enterococci” to define the group of bacteria that was previously called fecal streptococci and that are now collectively called enterococci in the United States. However, it is generally believed that the different terminologies such as fecal streptococci, enterococci, and intestinal enterococci, all refer to the same group of related bacteria species and that the various methods available to detect them provide generally comparable detection (Bartram and Rees, 2000).
Appearance of Viral Pathogens
Soon after the germ theory of disease became widely accepted and scientists began to use light microscopes routinely to identify disease-causing bacteria, it became evident that certain diseases were caused by microorganisms that were not visible with the best light microscope (i.e., viruses). For example, it had long been recognized that poliomyelitis was transmitted via the fecal-oral route. In the 1940s, several investigators confirmed that the virus responsible for this disease could be found in sewage (Melnick, 1947; Paul et al., 1940; Trask and Paul, 1942). As early as 1945, an epidemic of infectious hepatitis was connected to contaminated drinking water (Neefe and Stokes, 1945). The epidemiologic evidence for a connection between infectious hepatitis and drinking water was further substantiated by a massive outbreak in New Delhi, India in 1954 that was subsequently shown to be caused by hepatitis E virus instead of hepatitis A virus (Melnick, 1957; Viswanathan, 1957; Wong et al., 1980).
Although the proposition of waterborne viral diseases was not widely accepted at first, it gradually gained acceptance, and by the mid-1960s a review cited 50 outbreaks of infectious hepatitis and 8 outbreaks of polio that were waterborne from 1946 through 1960 (Weibel et al., 1964). At about that same time, it also became evident that outside of the host, viruses are not free-living organisms
and do not have metabolic requirements. This important finding supported earlier observations that under certain conditions, viruses can survive in the environment much longer than the coliform indicators (Neefe and Stokes, 1945). The superior environmental survival of important waterborne viral agents raised serious questions about the suitability of the coliform group as an indicator. Thus, while the presence of coliforms could still be taken as a sign of fecal contamination, the absence of coliforms could no longer be taken as assurance that water was uncontaminated.
Expansion Beyond Indicators for Human Fecal Contamination: Zoonoses and Protozoan Pathogens
Most, but not all, pathogens of concern in drinking water are spread by the fecal-to-oral route. In 1854, John Snow demonstrated that cholera could be transmitted through the contamination of drinking water by human feces (Snow, 1854a,b). Two years later, William Budd demonstrated that typhoid fever can be spread through the same route (Budd, 1856). Approximately 30 years later, Robert Koch and Karl Eberth isolated the specific microorganisms responsible for both of these diseases, further demonstrating the connection between disease and drinking water contaminated with human feces (Koch, 1883). As a result of these and other discoveries, by the middle of the nineteenth century, public health practitioners and researchers began to focus almost exclusively on preventing the contamination of water supplies by sewage.
This focus is particularly appropriate because a sewage-to-water connection contributes to facilitating the transmission and distribution of a waterborne pathogen by the fecal-to-oral route. Such widespread transmission can also affect the evolution of the disease organism itself in that unfettered waterborne transmission enables the continued evolution of a disease that might fatally immobilize the victim. Ordinarily, when a disease evolves to the point at which it causes such dire health effects, it loses access to future hosts because the infected host is too immobilized to expose others. On the other hand, with ready access to a public water supply, the victim’s caregiver can effectively spread the disease by merely washing out the bedpan of a bedridden person (Ewald et al., 1998).
Nevertheless, for a long time it has been understood that certain diseases are zoonoses, that is, they are common to both animals and humans. Some well-known zoonotic diseases include rabies, ringworm, and plague. In fact, some researchers have suggested that many of the epidemic diseases associated with early civilization may be of zoonotic origin (Diamond, 1999). It was not a big step, then, to presume that some of the microorganisms present in animal feces could be an important source of waterborne zoonoses as well. In the 1980s, giardiasis and cryptosporiodosis became widely recognized as zoonoses transmitted by the fecal-to-oral route. Furthermore, a large-scale and well-publicized outbreak of cryptosporiodosis occurred in Milwaukee, Wisconsin in 1993 in a public
water system that met SDWA microbiological water quality standards (Edwards, 1993). It is likely that many other microorganisms found in the feces of animals are the etiological agents for zoonoses as well. For example, in June 2000, the bacteria E. coli O157:H7 and Campylobacter jejuni originating from the feces of agricultural animals were found to be the cause of a well-documented waterborne disease outbreak in Walkerton, Ontario (Bruce-Grey-Owen Sound Health Unit, 2000). Finally, the intensive use of antibiotics in animal feedlots raises the specter that feces from such sources could be the source of zoonotic pathogens that possess significant antibiotic resistance (NRC, 1999b; see also Chapter 3 for further discussion).
However, human and animal feces are not the only source of enteric pathogens; microorganisms responsible for waterborne disease have also been connected to other environments (see Chapter 3 for further information). For example, Huq et al. (1983) isolated Vibrio cholerae from copepods found in marine waters. Fortunately, simple filtration to remove these copepods from freshwater has proven to be an effective treatment to reduce infection from drinking water (Huq et al., 1996).
As a result, whereas it made sense in the late nineteenth century to develop and use bacterial indicators to identify the presence of sewage of human origin, modern indices of microbial contamination face a much more complex and challenging task.
CURRENT STATUS OF WATERBORNE OUTBREAKS AND ENDEMIC DISEASE
Even though the association between water quality and disease has been recognized for more than a hundred years, the transmission of waterborne diseases is still a major public health concern in developed nations. In the United States, national statistics on outbreaks associated with drinking water have been collected since 1920 (Craun, 1986). Since 1971, the Centers for Disease Control and Prevention (CDC), EPA, and the Council of State and Territorial Epidemiologists (CSTE) have maintained a collaborative surveillance system of waterborne disease outbreaks (WBDOs). Currently, CDC publishes summary information on the occurrence and causes of WBDOs every two years.
In contrast, the occurrence of endemic waterborne disease has only recently become a focus of the federal government. The 1996 amendments to the SDWA (Section 1458(d)(1)) require CDC’s director and EPA’s administrator to jointly conduct pilot waterborne disease occurrence studies for at least five major communities or public water systems, prepare a report on the findings, and develop a national estimate of endemic waterborne disease occurrence. Furthermore, as noted previously (see also Table 1-2), the federal government has also turned its attention to recreational waters and public health by enacting the BEACH Act of 2000 to improve the quality of coastal recreational waters.
An overview of the current status of waterborne disease outbreaks and endemic disease in U.S. drinking and recreational waters is provided in the following sections. A more detailed description of the National Waterborne Diseases Outbreak Surveillance System (WBDOSS) and of the various epidemiologic studies of endemic disease associated with drinking and recreational waters is provided in Chapter 2.
Waterborne Disease Outbreaks
The United States is one of a few countries to have a national surveillance system for waterborne disease outbreaks. Surprisingly, most European countries do not yet have an adequate surveillance system for waterborne disease (the United Kingdom being a notable exception), while the situation in developing countries is even worse.
The WBDO and the foodborne disease outbreak surveillance systems at CDC are unique in that the unit of analysis is an outbreak rather than an individual case of disease, and these cases are linked to an identified exposure. In contrast, other surveillance systems typically focus on a specific disease (e.g., cryptosporidiosis, legionellosis) and collect standard epidemiologic data (e.g., person, place, and time), but do not obtain any information regarding the mode of transmission such as person-to-person contact versus waterborne or foodborne transmission for cases of cryptosporidiosis.
State, territorial, and local public health agencies are responsible for detecting and investigating WBDOs while CDC, as a federal agency, participates in outbreak investigations only by invitation or when an outbreak involves multiple states. States and territories report their outbreaks on a standard form annually and CDC then compiles, analyzes, and publishes the data every two years as a Morbidity and Mortality Weekly Report (MMWR) Surveillance Summary (in chronological order: Levine and Craun, 1990; Herwaldt et al., 1991; Moore et al., 1993; Kramer et al., 1996; Levy et al., 1998; Barwick et al., 2000; Lee et al., 2002). Reporting is voluntary and passive, and varies by state and territory.
Current data for drinking water and recreational water outbreaks (excluding recreational water outbreaks associated with treated waterbodies such as public swimming and wading pools) are summarized in Figures 1-1 through 1-3. Figure 1-1 provides an overview of the total number of reported WBDOs associated with drinking water by etiologic agent from the time the surveillance system was developed at CDC in 1971 through 2000. Outbreaks peaked in the early 1980s with a steady decline in numbers, except for 1992, until the 1997-1998 reporting period where the trend reversed and continued to increase through 2000. The decline in numbers of outbreaks through the 1980s and 1990s could be a result of implementation of water treatment regulations such as the SWTR; increased efforts by water utilities to produce drinking water that exceeds EPA standards; and widespread efforts by federal, state, and local public health officials to improve
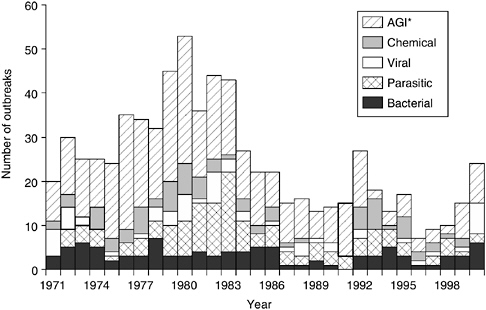
FIGURE 1-1 Number of waterborne disease outbreaks associated with drinking water by year and etiologic agent for the United States: 1971-2000 (n = 730). *AGI denotes acute gastrointestinal illness of unknown etiology. SOURCE: Adapted from Lee et al., 2002.
drinking water quality. Although the significance of the recent increase in reported outbreaks is not clear at this time, as noted previously, not all outbreaks are recognized and investigated and multiple factors can affect whether an outbreak is identified and investigated (see Chapter 2 for further information).
While the number of reported outbreaks increased from 1997 through 2000, the number of persons affected remained comparable to previous years. In this regard, changes in surveillance and reporting of WBDOs might have led to improvements in the detection of outbreaks in small systems, which tend to affect smaller numbers of individuals. In addition, better detection methods in clinical specimens as well as in water samples have increased the identification of outbreaks associated with viral pathogens. This improvement can be seen in the increase in reported viral outbreaks in 2000. Despite these improvements, however, the etiologic agent remains unknown for a large percentage of outbreaks, making the development, selection, and use of indicators for waterborne pathogens very complex.
Figure 1-2 provides an overview of the number of outbreaks by type of water, including waters that are specifically within this committee’s charge; that is, surface and groundwater sources for drinking water and ambient recreational
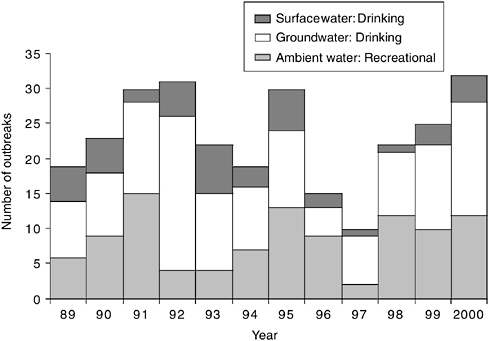
FIGURE 1-2 Number of waterborne disease outbreaks by year and water type for the United States: 1989-2000 (n = 278). SOURCE: Outbreak data through 2000 from the CDC’s National Waterborne Diseases Outbreak Surveillance System.
waters (freshwater, and coastal marine and marine-estuarine waters). It is important to note that the reported time frame for Figure 1-2 begins in 1989 (rather than 1971 as for Figure 1-1) for consistency in classification of water type because the responsibility for the surveillance system moved within CDC divisions at that time.
No clear trend emerges in the total number of reported outbreaks during the period; however, the histogram clearly shows that groundwater outbreaks are most common (7 out of 12 years for 58 percent) followed by ambient recreational water outbreaks (4 out of 12 years for 33 percent). The two categories had the same number of outbreaks in 1990. Figure 1-2 also emphasizes the relatively few number of reported surface water outbreaks in this period, which again might be a reflection of EPA’s regulations targeted at surface water systems and the ability of large water utilities to meet or exceed EPA standards. Small water utilities, often using groundwater sources, have fewer resources and are more likely to have difficulties meeting increasingly stringent water quality standards (NRC, 1997).
Figure 1-3 provides an overview of the number of reported WBDOs by illness and water type. As might be expected, acute gastrointestinal illnesses of
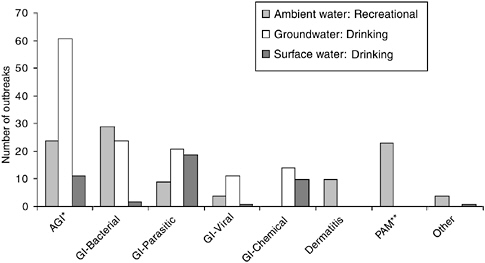
FIGURE 1-3 Number of waterborne disease outbreaks by illness and water type in the United States: 1989-2000 (n = 278). *AGI denotes acute gastrointestinal illness of unknown etiology. **PAM denotes primary amoebic meningoencephalitis (see Chapter 3 for further information). SOURCE: Outbreak data through 2000 from the CDC’s National Waterborne Diseases Outbreak Surveillance System.
unknown etiology are most likely to be associated with groundwater sources because these outbreaks are widely thought to be caused predominantly by viruses, which are difficult to identify in clinical specimens and even more so in water samples (NRC, 1999a). Gastrointestinal outbreaks of known viral etiology were also more likely to occur in groundwater systems. Surprisingly, gastrointestinal illnesses of parasitic origin also were somewhat more likely to be associated with groundwater systems, probably because some of these systems are actually groundwater under the influence of surface water. Gastrointestinal outbreaks of drinking water supplies from bacteria and viruses were rare in surface water systems since these microorganisms are readily killed by conventional treatment practices. While gastrointestinal outbreaks associated with bacteria were most commonly reported in ambient recreational waters, outbreaks of dermatitis and cases of primary amoebic meningoencephalitis were associated only with recreational water. The “other” illness category includes one outbreak each of leptospirosis, legionellosis, and keratitis in ambient waters and one outbreak associated with algae in a surface water system.
The outbreak data summarized in Figures 1-1 through 1-3 demonstrate that the association between various pathogens and human health effects differs depending on the type of water system involved. If indicators for waterborne patho-
gens are to be used to predict the likelihood of water contamination with potential ensuing health effects, it is unlikely that a single indicator will suffice for these different routes of exposure. For these and other reasons, epidemiologic studies are needed to establish the causal link between the presence and density of an indicator and the associated health effects under a variety of environmental conditions. Surveillance for waterborne disease outbreaks and epidemiologic study designs are discussed further in Chapter 2.
Endemic Waterborne Disease
In 1991, Payment and colleagues reported the results of the first randomized intervention trial (i.e., in which investigators control the conditions of exposure) to evaluate whether the consumption of tap water that met current Canadian microbiological standards was associated with an increased risk of gastrointestinal disease. They compared illness rates in households drinking tap water and households drinking reverse osmosis-filtered water, which were considered pathogen free (Payment et al., 1991). The trial estimated that 35 percent of the reported gastrointestinal illness among persons drinking tap water was associated with its consumption. In 1997, Payment and colleagues conducted a follow-up intervention trial to confirm the previous results and to attempt to determine the source(s) of the illnesses (Payment et al., 1997). This second study attributed 14-40 percent of gastrointestinal illness to consumption of tap water meeting current Canadian water treatment standards. These two studies are described in more detail in Chapter 2.
Researchers’ interest in the possible contribution of drinking water that met current treatment standards to the incidence of gastrointestinal illness was heightened as a result of the Payment studies and the continuing occurrence of waterborne disease outbreaks in the United States and elsewhere. As noted previously, Congress responded with new mandates in the 1996 SDWA amendments, and CDC and EPA entered into an interagency agreement in 1997 in response to the congressional mandate to conduct studies and develop a national estimate of endemic waterborne disease. The SDWA amendments were interpreted to mean that the focus of efforts should be directed at municipal drinking water. The amendments did not specify which waterborne diseases were to be studied, and after conducting several workshops, the two agencies determined that the health outcome that would be studied in this initial effort would be gastrointestinal disease.
Based on this interagency agreement, CDC has funded cooperative agreements with academic institutions to conduct two pilot intervention trials of home water treatment in households and one full-scale intervention trial along with several related “nested” epidemiology studies to help maximize the benefit of the large-scale trial. Each of these studies is reviewed in Chapter 2 along with related (including three community intervention trials conducted by EPA) studies of en-
demic waterborne disease. In addition, questions regarding water consumption patterns and usage behavior were added to CDC’s yearly cross-sectional survey for FoodNet (CDC, 1996; see Chapter 2 for further information) beginning with the 1998-1999 cycle.
As part of the BEACH Program, EPA will be conducting new epidemiologic studies intended to correlate water quality with human health effects. The health outcomes will include gastrointestinal disease as well nongastrointestinal health outcomes in eyes, ears, skin, and the respiratory system (Rebecca Calderon, EPA, personal communication, 2002). Beach site selection criteria will include point source contamination, range of exposures, population size, geographic variety, and historical microbial testing. A pilot study was conducted during summer 2002 at one freshwater recreational beach (Indiana Dunes National Lakeshore). The current projected time line includes full-scale studies at three beaches each summer from 2003 to 2005 for a total of nine beaches. Data analysis and report preparation are expected to be completed in 2006 (see Chapter 2 for further information).
All of the aforementioned studies focus on health effects associated with water of varying quality. This water quality is measured using many methods and parameters. Because pathogens are difficult to detect in water, surrogates or indicators are often used in their stead. The following section describes the indicators for waterborne pathogens that are currently in use and provides an overview of the issues associated with the selection of appropriate indicators for waterborne pathogens.
CURRENT INDICATORS FOR WATERBORNE PATHOGENS
In the United States, predominantly bacterial indicators are used to determine (1) if drinking water sources are microbiologically safe, (2) if treatment of drinking water has been adequate, (3) if drinking water in the distribution system continues to be protected, and (4) if recreational and shellfish waters are microbiologically safe (see also Tables 1-1 and 1-2). Each of these test objectives has different requirements, and it is not likely that any one indicator or system of indicators can adequately meet all of these needs. For example, for recreational waters, shellfish waters, and source waters for drinking water, the question being addressed is the same, namely: Has this water been exposed to significant microbiological contamination? However, complexities of several kinds come into play.
First, it is important to know something about the type and source of contamination, particularly if the contamination is of fecal or nonfecal origin. At the time the coliform index was conceived, contamination by human feces was clearly the central public health issue to be addressed. Since that time it has become clear that although contamination with human fecal matter is clearly of profound and continuing public health significance, human pathogens occur in other environ-
ments as well. For example, based on the preceding discussion it is clear that animal fecal matter can be of particular significance and that the widespread use of antibiotics for animal growth promotion, as well as for control of animal diseases, may constitute an important source of antibiotic-resistant pathogens (NRC, 1999b). Finally, some enteric waterborne pathogens have natural reservoirs in the environment where they can proliferate (see Chapter 3 for further discussion of these issues). Moreover, some nonenteric waterborne pathogens are capable of proliferating in waters under the right conditions, and human exposure to the high concentrations resulting from this proliferation can create human health risks. An example is Legionella pneumophila, which proliferates in warm waters containing sediments and nutrients (e.g., institutional hot water systems) and causes respiratory disease through inhalation of aerosolized water (Kaufman et al., 1981).
The specific application and geographic location can also have an impact on selection of the most important indicator candidates. For example, some indicators will be more useful in temperate zones than in the subtropics, some will be more effective in surface water than in groundwater sources of drinking water, and some will be more useful in freshwaters than in marine recreational waters. Finally, a different set of indicator attributes will come into play when the effectiveness of treatment or the integrity of a drinking water distribution system is at issue (though the latter are excluded from explicit consideration in the committee’s charge). These and related issues are discussed and illustrated at length in this report, especially in Chapters 4 and 6.
The timeliness of the indicator system is also more important in some applications than in others. For example, in the case of recreational waters, the results of current bacterial indicator tests are often tied directly and immediately to a decision to allow or restrict public access (see Chapter 4 for further information). It is essential that indicator systems used in such applications provide timely results because swimmers may be exposed to unacceptable levels of pathogens while the analysis is being conducted. Furthermore, beach contamination is often episodic and of short duration and a long turnaround on an indicator test runs the risk that the public is allowed access to unsafe waters, but denied access when the episode has already past (Boehm et al., 2002).
Drinking water supplies generally face different requirements for indicators for waterborne pathogens. It is sometimes possible to use indicator measurements alone to divert or avoid a water supply during a contamination episode. However, it is more common to use indicators in conjunction with other measures (e.g., sanitary surveys) to assess the overall microbiological risk associated with a given water supply source and to address that contamination by removing its source and/or installing (additional) treatment systems to serve as a protective barrier. For assessments of this sort, the accuracy and specificity of the indicator system are more important than the timeliness of the result.
SUMMARY AND CONCLUSIONS
To protect public health, and as mandated in the SDWA and CWA, it is important to have accurate, reliable, and scientifically defensible methods for determining whether source waters for drinking water and recreational waters are contaminated by pathogens and to what extent. In this regard, the development and use of bacterial indicators for waterborne pathogens began more than a century ago, when contamination of drinking waters by enteric bacterial pathogens originating from human waste constituted a major public health threat. The use of bacterial indicators (predominantly coliforms) was later expanded and adopted for use in ambient, recreational, and shellfish waters and continues to focus on identification of fecal contamination, principally of human origin. As such, the current indicator approaches have become standardized; are relatively easy and inexpensive to use; and constitute a cornerstone of local, state, and federal monitoring and regulatory programs. Although these approaches have been extremely effective in reducing waterborne disease outbreaks caused by human enteric bacteria, it is now widely understood that bacteria are not the only pathogens of public health concern; fecal contamination is not the only significant potential source of waterborne microbial pathogens; and many human pathogens and indicator organisms occur in other environments.
The number of reported disease outbreaks associated with drinking water peaked in the early 1980s, declined for more than 10 years, and increased from 1997 through 2000, although the number of persons affected has remained comparable to previous years. Recreational water outbreaks associated with ambient water did not show a specific trend. Better detection methods in clinical specimens as well as in water samples have increased the identification of pathogens, most notably viruses. Despite these improvements, the etiologic agent remains unknown for a large percentage of drinking water and recreational water outbreaks, making the selection and use of indicators for waterborne pathogens very complex.
An increased understanding of the diversity of waterborne pathogens, their sources, physiology, and ecology has resulted in a growing understanding that the use of bacterial indicators may not be as universally protective as once thought. For example, the superior environmental survival of important waterborne viruses and protozoa raised serious questions about the suitability of relying on relatively short-lived coliforms as indicators of the microbiological quality of water. That is, while the presence of coliforms could still be taken as a sign of fecal contamination, the absence of coliforms could no longer be taken as assurance that water was uncontaminated. Thus, existing bacterial indicators and indicator approaches do not in all circumstances identify all potential waterborne pathogens. Indeed, the committee concludes that no single indicator organism or small set of indicators can successfully identify or predict the presence, let alone the source, of all classes of potential pathogens—especially emerging microor-
ganisms. Furthermore, recent and forecasted advances in microbiology, molecular biology, and analytical chemistry make it timely to assess the current paradigm of relying predominantly or exclusively on traditional bacterial indicators for waterborne pathogens to make judgments concerning the microbiological quality of source waters for drinking water and recreational waters. Nonetheless, indicator approaches will still be required for the foreseeable future since it is not practical or feasible to monitor for the complete spectrum of microorganisms that may occur in source waters for drinking water and recreational waters, and many known pathogens are difficult to detect directly and reliably in water samples.
Lastly, improvements in the timeliness of indicator analysis (i.e., rapidity of results) are needed if exposure to pathogen-contaminated water is to be prevented or controlled in a timely manner that protects public health.
REFERENCES
Andrewes, F.W., and T.J. Horder. 1906. A study of the streptococci pathogenic for man. Lancet 2: 708-713.
APHA (American Public Health Association). 1949. Standard Methods for the Examination of Water and Wastewater, 10th Edition. Washington, D.C.
APHA. 1965. Standard Methods for the Examination of Water and Wastewater, 12th Edition. Washington, D.C.
APHA. 1998. Method 9221(3) or Method 9222 (d) in Standard Methods for the Examination of Water and Wastewater, L. Clesceri, A. Greenberg, and A. Eaton, eds., 20th Edition. Washington, D.C.
Ashbolt, N.J., W.O.K. Grabow, and M. Snozzi. 2001. Indicators of microbial water quality. Chapter 13 in Water Quality—Guidelines, Standards and Health: Assessment of Risk and Risk Management for Water-Releated Infectious Disease, L. Fewtrell and J. Bartram, eds., London: World Health Organization and IWA Publishing.
Bartram, J., and G. Rees. 2000. Monitoring Bathing Waters: A Practical Guide to the Design and Implementation of Assessments and Monitoring Programmes. Geneva: World Health Organization.
Barwick, R.S., D.A. Levy, G.F. Craun, M.J. Beach, and R.L. Calderon. 2000. Surveillance for waterborne-disease outbreaks—United States, 1997-1998. MMWR 49 (No. SS-4): 1-35.
Bermudez, M., and T.C. Hazen. 1988. Phenotypic and genotypic comparison of Escherichia coli from pristine tropical waters. Applied and Environmental Microbiology 54: 979-983.
Boehm, A., S. Grant, J. Kim, S. Mowbray, C. McGee, C. Clark, D. Foley, and D. Wellman. 2002. Decadal and shorter period variability of surf zone water quality at Huntington Beach, CA. Environmental Science and Technology 36(18): 3885-3892.
Bonde, G.J. 1963. Bacteria indicators of water pollution. Teknisk Forlag, Copenhagen 221-226.
Bonde, G.J. 1966. Bacteriological methods for the estimation of water pollution. Health Laboratory Science 3: 124.
Bonde, G.J. 1975. Bacteria indicators of sewage pollution. Pp. 37-47 in Discharge of Sewage from Sea Outfalls: Proceedings of an International Symposium, A.L.H. Gameson, ed. New York: Pergamon Press.
Bruce-Grey-Owen Sound Health Unit. 2000. The Investigative Report of the Walkerton Outbreak of Waterborne Gastroenteritis May-June, 2000. Ontario Ministry of Health. Owen Sound, Ontario.
Budd, W. 1856. Outbreak of fever at clergy orphanage. Lancet: 15 November.
Burman, N.P. 1961. Some observations on coli-aerogenes bacteria and streptococci in water. Journal of Applied Bacteriology 24: 368.
Burton, M.C. 1949. Comparison of coliform and Enterococcus organisms as indices of pollution in frozen foods. Food Research 14: 434-448.
Cabelli, V. 1978. Obligate anaerobic bacterial indicators. Pp. 171-200 in: Indicators of Viruses in Water and Food, G. Berg, ed., Ann Arbor Science, Ann Arbor, MI.
Cabelli, V. 1983. Health Effects Criteria for Marine Recreational Waters. Cincinnati, Ohio. EPA-600-1-80-031.
CDC (Centers for Disease Control and Prevention). 1996. FoodNet. [On-line]. Available: http://www.cdc.gov/foodnet/. Accessed October 15, 2002.
Cox. 1951. Acceptable standards for natural waters used for bathing. Proceedings American Society of Civil Engineers 77: 74.
Craun, G.F., ed. 1986. Waterborne Diseases in the United States. Boca Raton, Florida: CRC Press, Inc.
Diamond, J. 1999. Guns, Germs and Steel: The Fates of Human Societies. New York: W. Norton & Co.
Dible, H. 1921. The Enterococcus and the faecal streptococci: Their properties and relations. Journal of Pathology and Bacteriology 24: 3-12.
Dufour, A. 1984. Health Effects Criteria for Fresh Recreational Waters. Cincinnati, Ohio: EPA 600/ 1-84-004.
Edberg, S.C., M.J. Allen, and D.B. Smith. 1988. National field evaluation of a defined substrate method for the simultaneous enumeration of total coliforms and Escherichia coli from drinking water: Comparison with the standard multiple tube fermentation method. Applied and Environmental Microbiology 54(6): 1595-1601.
Edwards, D. 1993. Troubled waters in Milwaukee. ASM News 59(7): 342-345.
EPA (U.S. Environmental Protection Agency). 1976. Quality Criteria for Water. Washington, D.C.: EPA 440-9-76-023.
EPA. 1986. Ambient Water Quality Criteria for Bacteria - 1986. Washington, D.C.: Office of Water. EPA 440-5-84-002.
EPA. 1989a. Drinking Water; National Primary Drinking Water Regulations; Filtration, Disinfection; Turbidity; Giardia lamblia, Viruses, Legionella, and Heterotrophic Bacteria; Final Rule. Federal Register 54: 27486-27541.
EPA. 1989b. Drinking Water; National Primary Drinking Water Regulations; Total Coliforms (Including Fecal Coliforms and E. coli); Final Rule. Federal Register 54: 27544-27568.
EPA. 1990. Drinking Water; National Primary Drinking Water Regulations; Total Coliforms; Corrections and Technical Amendments; Final Rule. Federal Register 55: 25064-25065.
EPA. 1997. Guidelines for Preparation of the Comprehensive State Water Quality Assessments (305(b) Reports) and Electronic Updates. Washington, D.C.: Office of Water. EPA-841-B-97-002A.
EPA. 1998a. Bacterial Water Quality Standards for Recreational Waters (Freshwater and Marine Waters). Washington, D.C.: Office of Water. EPA-823-R-98-003.
EPA. 1998b. Announcement of the Drinking Water Contaminant Candidate List; Notice. Federal Register. 64: 10274-10287.
EPA. 1998c. National Primary Drinking Water Regulations: Interim Enhanced Surface Water Treatment; Final Rule. Federal Register 64: 69477-69521.
EPA. 1999. EPA Action Plan for Beaches and Recreational Waters. Washington, D.C.: Office of Water and Office of Research and Development. EPA-600-R-98-079.
EPA. 2000a. Atlas of America’s Polluted Waters. Washington, D.C.: Office of Water. EPA-840-B00-002.
EPA. 2000b. National Primary Drinking Water Regulations: Ground Water Rule; Proposed Rule. Federal Register 65(91): 30193-30274.
EPA. 2000c. Stage 2 M-DBP Agreement in Principle. Microbial/Disinfection Byproducts (M-DBP) Federal Advisory Committee. Washington, D.C.: Office of Water.
EPA. 2000d. National Primary Drinking Water Regulations: Long Term 1 Enhanced Surface Water Treatment and Filter Backwash Rule; Proposed Rule. Federal Register 65: 19046-19150.
EPA. 2000e. Beaches Environmental Assessment and Coastal Health Act of 2000. Washington, D.C.: Office of Science and Technology. [On-line]. Available: http://www.epa.gov/ost/beaches/beachbill.pdf.
EPA. 2001. Strategy for Waterborne Microbial Disease (Discussion Draft). Washington, D.C.: Office of Science and Technology and Office of Water.
EPA. 2002a. National Primary Drinking Water Regulations: Long Term 1 Enhanced Surface Water Treatment Rule; Final Rule. Federal Register 67: 1811-1844.
EPA. 2002b. Implementation Guidance for Ambient Water Quality Criteria for Bacteria (Draft). Washington, D.C.: Office of Water. EPA-823-B-02-003.
EPA. 2002c. 2000 National Water Quality Inventory. Washington, D.C.: Office of Water. EPA-841-R-2-001.
EPA. 2002d. Management Briefing. Washington, D.C.: Office of Water Microbial Indicator Cross Office Team. Presentation slides received December 19, 2002.
EPA. 2003a. Bacterial Water Quality Standards for Recreational Waters (Freshwater and Marine Waters). Status Report Washington, D.C.: Office of Water. EPA-823-R-98-003.
EPA. 2003b. National Primary Drinking Water Regulations: Longterm 2 Enhanced Surface Water Treatment Rule; Proposed Rule. Federal Register 68: 47640-47795.
Escherich, T. 1885. Die Darmbakterien des Säuglings und ihre Beziehungen zur Physiologie der Verdauung. Stuttgart, Germany.
Escherich, T. 1887. Ueber Darmbakterien im allgemeinen und diejenige der Säuglinge im Besonderen, sowie der Beziehungen der letzteren zur Aetiologie der Darmerkrankungen. Centralblatt für Bakteriologie 1: 705-713.
Ewald, P., J. Sussman, M. Distler, C. Libel, W. Chammas, V. Dirita, C. Salles, A. Vicente, I. Heitmann, and F. Cabello. 1998. Evolutionary control of infectious disease: prospects for vectorborne and waterborne pathogens. Memorial Institute Oswaldo Cruz, Rio de Janeiro 93(5): 567-576.
Ferguson, C.M., B.G. Coote, N.J. Ashbolt, and I.M. Stevenson. 1996. Relationships between indicators, pathogens and water quality in an estuarine system. Water Research 30: 2045-2054.
Frost, W.H. 1925. Report of committee on sanitary control of the shellfish industry in the United States. Public Health Reports Supplement 53: 1-17.
Fujioka, R.S., and L.K. Shizumura. 1985. Clostridium perfringens, a reliable indicator of stream water quality. Journal of Water Pollution Control Federation 57(10): 986-992.
Fujioka, R.S., B. Roll, and M. Byappanahalli. 1997. Appropriate recreational water quality standards for Hawaii and other tropical regions based on concentrations of Clostridium perfringens. Proccedings of the Water Environment Federation 4: 405-411.
Fujioka, R.S., C. Stan-Denton, M. Borja, J. Castro, and K. Morphew. 1999. Soil, the environmental source of Escherichia coli and enterococci in Guam’s streams. Journal of Applied Microbiology Symposium Supplement 85: 83S-89S.
Fujioka, R.S. 2001. Monitoring coastal marine waters for spore-forming bacteria of faecal and soil origin to determine point from non-point source pollution. Water Science and Technology 44(7): 181-188.
Garber, W.F. 1956. Bacteriological standards for bathing waters. Sewage & Industrial Wastes 28(6): 795-807.
Geldreich, E. 1966. Sanitary Significance of Fecal Coliforms in the Environment. Water Pollution Control Research Series. Publ. WP-2-3, FWPCA. Cincinnati, Ohio: U.S. Department of Interior.
Hagedorn, C., J.B. Crozier, K.A. Mentz, A.M. Booth, A.K. Graves, N.J. Nelson and R.B. Reneau, Jr. 2003. Carbon source utilization profiles as a method to identify sources of faecal pollution in water. Journal of Applied Microbiology 94: 792-799.
Hardina, C.M., and R.S. Fujioka. 1991. Soil, the environmental source of E. coli and enterococci in Hawaii’s streams. Environmental Toxicology 6: 185-195.
Hazen, T.C., J. Santiago-Mercado, G.A. Toranzos, and M. Bermudez. 1987. What does the presence of fecal coliforms indicate in the waters of Puerto Rico? A review. Bol. Puerto Rico Medical Association 79: 189-193.
Herwaldt, B.L., G.F. Craun, S.L. Stokes, and D.D. Juranek. 1991. Waterborne-disease outbreaks, 1989-1990. MMWR 40 (No. SS-3): 1-21.
HMSO (Her Majesty’s Stationary Office). 1969. The Bacteriological Examination of Water Supplies. Reports on Public Health and Medical Subjects, 4th edition, No. 71. London.
Huq, A., E.B. Small, P.A. West, M.I. Huq, R. Rahman, and R.R. Colwell. 1983. Ecology of Vibrio cholerae with special reference to planktonic crustacean copepods. Applied and Environmental Microbiology 45: 275-283.
Huq, A., B. Xu, M.A.R. Chowdhury, M.S. Islam, R. Mantilla, and R.R. Colwell. 1996. A simple filtration method for removal of Vibrio cholerae associated with planktonic copepods. Applied and Environmental Microbiology 62: 2508-2512.
Kaufman, A.F., J.E. McDade, C.M. Patton, J.V. Bennett, P. Skaliy, J.C. Feeley, D.C. Anderson, M.E. Potter, V.F. Newhouse, M.B. Gregg, and P.S. Brachman. 1981.Pontiac fever, isolation of the etiological agent (Legionella pneumophila) and demonstration of its mode of transportation. American Journal of Epidemiology 114(3): 337-347.
Kenner, B.A., H.F. Clark, and P.W. Kabler. 1961. Cultivation and enumeration of streptococci in surface water. Applied Microbiology 9: 15.
Kerr, R., and C. Butterfield. 1943. Notes on the relations between coliform organisms and pathogens. Public Health Reports 58(15): 589-607.
Klein, E., and A.C. Houston. 1899. Further report on bacteriological evidence of recent and therefore dangerous sewage pollution of elsewise potable waters. Supplement to 28th Annual Report of the Local Government Board Containing the Report of the Medical Officer for 1898-1899, London City Council, London.
Klein, G. 2003. Taxonomy, ecology and antibiotic resistance of enterococci from food and the gastrointestinal tract. International Journal of Food Microbiology 88: 123-131.
Koch, R. 1883. Bericht uber die Thatigkeit der deutschen Cholera-komission in Aegpytten and Ostindien. Wien Med Wochenschr 33: 1548-1551.
Kramer, M.H., B.L. Herwaldt, G.F. Craun, R.L. Calderon, and D.D. Juranek. 1996. Surveillance for waterborne-disease outbreaks—United States, 1993-1994. MMWR 45 (No. SS-1): 1-33.
Lee, S.H., D.A. Levy, G.F. Craun, M.J. Beach, and R.L. Calderon. 2002. Surveillance for waterborne-disease outbreaks—United States, 1999-2000. MMWR 51 (No. SS-8): 1-47.
Levin, M.A., J.R. Fischer, and V.J. Cabelli. 1975. Membrane filter technique for enumeration of enterococci in marine waters. Applied and Environmental Microbiology 30(1): 66-71.
Levine, W.C., and G.F. Craun. 1990. Waterborne disease outbreaks, 1986-1988. MMWR 39 (No. SS-1): 1-13.
Levy, D.A., M.S. Bens, G.F. Craun, R.L. Calderon, and B.L. Herwaldt. 1998. Surveillance for waterborne-disease outbreaks - United States, 1995-1996. MMWR 47 (No. SS-5): 1-33.
Litsky, W., W.L. Mallman, and C.W. Fifield. 1955. Comparison of the most probable numbers of E. coli and enterococci in river water. American Journal of Public Health 45: 1049.
Mallmann, W.L., and E.B. Seligman. 1950. A comparison study of media for the detection of streptococci in water and sewage. American Journal of Public Health 40: 286.
Mason, W. 1891. Notes on some cases of drinking water and disease. Journal of the Franklin Institute (Nov.): 1-10.
Melnick, J.L. 1947. Poliomyelitis virus in urban sewage in epidemic and nonepidemic times. American Journal of Hygiene: 240-253.
Melnick, J.L. 1957. A waterborne urban epidemic of hepatitis. Pp. 211-225 in Hepatitis Frontiers, F.W. Hartman, ed. Boston: Little Brown and Co.
Messer, J.W. and A.P. Dufour. 1998. A rapid, specific membrane filtration procedure for enumeration of enterococci in recreational water. Applied and Environmental Microbiology 64(2): 678-680.
Moore, A.C., B.L. Herwaldt, G.F. Craun, R.L. Calderon, A.K. Highsmith, and D.D. Juranek. 1993. Surveillance for waterborne-disease outbreaks - United States, 1991-1992. MMWR 42 (No. SS-5): 1-22.
Neefe, J., and J. Stokes. 1945. An epidemic of infectious hepatitis, apparently due to a waterborne agent. Journal of the American Medical Association 128: 1063-1075.
NRC (National Research Council). 1997. Safe Water From Every Tap: Improving Water Service to Small Communities. Washington, D.C.: National Academy Press.
NRC. 1999a. Setting Priorities for Drinking Water Contaminants. Washington, D.C.: National Academy Press.
NRC. 1999b. The Use of Drugs in Food Animals. Washington, D.C.: National Academy Press.
NRC. 2001. Assessing the TMDL Approach to Water Quality Management. Washington, D.C.: National Academy Press.
NRC. 2002. Biosolids Applied to Land: Advancing Standards and Practices. Washington, D.C.: National Academy Press.
NTAC (National Technical Advisory Committee). 1968. National Technical Advisory Committee (NTAC) Report of the Committee on Water Quality Criteria. Washington, D.C.
Orla-Jensen, S. 1919. The Lactic Acid Bacteria. Copenhagen: A. F. Host and Son Co.
Ostrolenk, M., N. Kramer, and R.C. Clerverdon. 1947. Comparative studies of enterococci and Escherichia coli as indices of pollution. Journal of Bacteriology 53: 197-203.
Paul, J.R., J.D. Trask, and S. Gard. 1940. Poliomyelitis virus in urban sewage. Journal of Experimental Medicine 71: 765-777.
Payment, P., L. Richardson, J. Siemiatycki, R. Dewar, M. Edwardes, and E. Franco. 1991. A randomized trial to evaluate the risk of gastrointestinal disease due to consumption of drinking water meeting current microbiological standards. American Journal of Public Health 81: 703-708.
Payment, P., and E. Franco. 1993. Clostridium perfringens and somatic coliphages as indicators of the efficiency of drinking water treatment for viruses and protozoan cysts. Applied and Environmental Microbiology 59: 2418-2424.
Payment, P., J. Siemiatycki, L. Richardson, G. Renaud, E. Franco, and M. Prevost. 1997. A prospective epidemiological study of gastrointestinal health effects due to the consumption of drinking water. International Journal of Environmental Health Research 7: 5-31.
Pontius, F.W., and S.W. Clark. 1999. Drinking water quality standards, regulations and goals. Chapter 1 in Water Quality and Treatment: A Handbook of Community Water Supplies, 5th Edition. New York: McGraw-Hill.
Rivera, S., T.C. Hazen, and G.A. Toranzos. 1988. Isolation of fecal coliforms from pristine water in a tropical rain forest. Applied and Environmental Microbiology 54: 513-517.
Scott, W. 1951. Sanitary study of shore bathing water. Bulletin of Hygiene 33: 353.
Sherman, J.M. 1937. The streptococci. Bacteriological Reviews 1: 3-97.
Slanetz, L., D. Bent, and C. Bartley. 1955. Use of the membrane filter technique to enumerate enterococci in water. Public Health Reports 70(1): 67.
Slanetz, L.W., and C.H. Bartley. 1957. Numbers of enterococci in water, sewage and feces determined by the membrane filter technique with improved medium. Journal of Bacteriology 74: 591.
Smith, T. 1891. A New Method for Determining Quantitatively the Pollution of Water by Fecal Bacteria. 13th Annual Report of the New York State Board of Health. Albany, New York.
Snow, J. 1854a. On cholera. In The Sourcebook of Medical History, L. Clendening, ed. 1942. New York: Paul B. Hoeber, Inc.
Snow, J. 1854b. On the Mode of Communication of Cholera. Self-published by Dr. John Snow of Sackville Street, Picadilly (republished by Delta Omega, the U.S. National Honorary Public Health Society).
Stevenson, A. 1953. Studies of bathing water quality and health. American Journal of Public Health 43: 529-538.
Stokes, W.R. 1927a. Report of the committee on bathing places. American Journal of Public Health 17: 121
Stokes, W.R. 1927b. A search for pathogenic bacteria in swimming pools. American Journal of Public Health 17: 334
Streeter, H.W. 1951. Bacterial Quality Objectives for the Ohio River: A Guide for the Evaluation of Sanitary Condition of Waters Used for Potable Supplies and Recreational Uses. Cincinnati, Ohio: Ohio River Valley Water Sanitation Commission.
Thiercelin, M.E. 1899. Sur un diplocoque saprophyte de l’intestin susceptible de devenir pathogene. CR Soc. Biol. 5: 269-271.
Thiercelin, M.E., and L. Jouhaud. 1903. Reproduction de l’enterocoque; taches centrales; graduations periferiques et microblastes. CRS Soc. Biol. Fil. 55: 686-688.
Trask, J., and J. Paul. 1942. Periodic examination of sewage for the virus of poliomyelitis. Journal of Experimental Medicine 75: 2-6.
U.S. Treasury Department. 1914. Bacterial standard for drinking water. Public Health Report 29: 2959-2966.
Veillon, A., and A. Zuber. 1898. Recherches sur quelques microbes strictement anaérobies et leur rôle en pathologie Arch. Med. Exp. Anat. Pathol. 10: 517-545.
Venczel, L.V., M. Arrowood, M. Hurd, and M.D. Sobsey. 1997. Inactivation Cryptosporidium parvum oocysts and Clostridium perfringens spores by a mixed-oxidant disinfectant and by free chlorine. Applied and Environmental Microbiology 63(4): 1598-1601.
Viswanathan, R. 1957. Infectious hepatitis in Delhi (1955-56), a critical study: Epidemiology. Indian Journal of Medical Research 45(suppl.): 1-29.
Wattie, E., and C. Butterfield. 1944. Relative resistance of Escherichia coli and Eberthella typhosa to chlorine and chloramines. Public Health Reports 59(52): 1661-1671.
Weibel, S.R., F.R. Dixon, B.B. Weidner, and L.J. McCabe. 1964. Waterborne-disease outbreaks, 1946-1960. Journal of the American Water Works Association 56: 947-958.
Welch, W.H., and G.H.F. Nuttall. 1892. A gas-producing bacillus (Bacillus aeorgenes capsulatus, Nov. Spec.) capable of rapid development in the body after death. Johns Hopkins Hospital Bulletin 3: 81.
Wilson, W.J., and E.M.M. Blair. 1925. Correlation of the sulfite reduction test with other tests in the bacteriological examination of water. Journal of Hygiene, Cambridge 24: 111.
Wolfe, H. 1972. The coliform count as a measure of water quality. Pp. 333-346 in Water Pollution Microbiology, R. Mitchell, ed. New York: Wiley-Interscience.
Wong, D. C., R.H. Purcell, S.R. Prasad, M.A. Sreenivasan, and K.M. Pavri. 1980. Epidemic and endemic hepatitis in India: evidence for non-B hepatitis virus aetiology. Lancet 2: 876-879.




































