Crossing the Quality Chasm
Janet Corrigan
Institute of Medicine
The Quality of Care in America Project was started about three years ago. The final report, Crossing the Quality Chasm, is a comprehensive review of the overall quality of the health care system, including an assessment of its safety and effectiveness and recommendations for a comprehensive strategy for improvement (IOM, 2001).
The first step in the project was a review of the literature by RAND. About 70 RAND studies have documented serious deficiencies and large gaps between the care people should receive and the care they actually do receive. Deficiencies were observed in all health care settings, in all age groups, and in all geographic areas. In other words, the problems are systemic and permeate the health care industry; problems are just as prevalent in traditional indemnity, or less managed, settings as in managed care settings.
Two factors influence how we approach this problem. The first is the expanding knowledge base, which has clearly overwhelmed physicians and made it all but impossible for an individual physician to provide high quality care on his or her own. A tremendous number of publications now report the results of randomized controlled trials, and the number of new drugs and medical devices and the amount of information flowing into the marketplace has increased exponentially.
The second major factor is the need to care for people with chronic conditions. A very limited number of chronic conditions, 15 or 20, account for the bulk of health care problems. If we targeted those conditions, we could make tremendous progress and affect a sizable proportion of the health care delivery system, as well as of the general population.
The models that are most useful in caring for the chronically ill are very different from our current delivery system models. Providing high-quality care to chronically ill individuals requires well designed care processes focused on information that meets the self-management needs of patients and their families. Patients with chronic illnesses require multidisciplinary care from teams of physicians, nurses, social workers, aides, and others. Team care is essential for high quality care.
Our current health care delivery system, which is organized around professionals and types of institutions, grew out of a need to provide primarily acute care rather than chronic care. This is one kind of chasm we have to cross. The health care delivery system must be reorganized to meet the real needs of patients.
Few clinical programs have the infrastructure to provide a full complement of services to chronically ill patients. Some institutions have well defined programs for particular chronic conditions, but few institutions or systems provide high quality care for the full range of chronic conditions. In addition, we have a problem in “scaling up”—exemplary programs are not replicated throughout the industry.
The lack of standardized performance measures has made it difficult if not impossible to make cross-institutional comparisons. For example, we have no standardized performance or outcome measures that enable us to identify which providers deliver exemplary care for diabetes. This creates two problems. First, we do not know where the best performers are. Second, the best performers are not rewarded for their excellent work. We need much better systems for managing knowledge and for using information technology to help people make decisions, and we need unfettered, timely access to clinical information.
Today, physician groups often operate as “silos” (i.e., in isolation) without benefit of the kind of information, infrastructure, and support they need to provide high quality care. On the one hand, we can no longer deliver health care through a collection of silos. On the other hand, we do not have the organizational support that can, for example, pull together the latest knowledge and make it readily available to providers and patients. If one looks on the Web, one finds 42,000 sites on lupus and 75,000 sites on breast cancer. Individual patients and individual professionals are overloaded with huge amounts of undigestible, disorganized information.
The Committee on Quality of Health Care in America recommended that the redesign process be initiated by focusing on priority areas. Specifically, the Agency for Healthcare Research and Quality should identify 15 priority areas and define them clearly so that everyone involved can work toward the same goals. The committee also recommended that Congress establish a $1 billion innovation fund to seed improvement projects and that purchasers, health care organizations, and professional groups begin to develop action plans immediately for each priority area. The goal should be a 50-percent improvement in quality and safety in the next five years.
Meaningful innovation in the health care delivery system will require some significant changes in the overall health system environment. The Chasm report describes changes in four key areas: (1) the use of information technology; (2) payment policies; (3) the development of best practices, decision support tools, and an accountability system; and (4) professional education and training (IOM, 2001).
We have many examples of how information technology can improve quality. For instance, we know that computerized order entry by physicians can reduce adverse drug events by 50 to 60 percent—an enormous improvement in safety. Reminder systems for physicians or patients and their families have been found to be effective in getting people the right services at the right time. The Institute of Medicine is working on a strategic plan for an information technology initiative that should be ready soon.
Second, current payment policies are complex, contradictory, and often work against improving quality. For example, current payment systems do not reward investments in information technology. Unlike investments in medical technology, investments in information technology do not directly generate billable services under Medicare or third-party-payer, fee-for-service systems. Hence, providers may realize a faster return on investments in a new surgical suite than they will on investments in an automated order entry system. Unfortunately, errors in clinical care contribute to rising health care expenditures because patients injured as a result of errors typically require more services and readmissions.
The problem is compounded because the marketplace typically cannot discern differences in quality. Because we do not have good comparative data for measuring quality and performance in medical care and patient outcomes, health care organizations, medical groups, and hospital systems that have better outcomes do no better in the marketplace than providers with poorer outcomes. We must move very aggressively to address these payment concerns before they stifle the adoption of information technologies critical to improving the safety and quality of care.
Third, we need to translate the evidence base into best practices that can be implemented in care delivery and then communicate this information to health care professionals and patients. In addition, we must develop and implement decision-support tools to assist clinicians and patients in using the clinical knowledge base effectively. Last but not least, the Chasm report calls for “transparency”—an accountability system that emphasizes the release of comparative data.
Fourth, we must make major changes in the medical education system. Currently, many providers are trained in environments that are not “wired.” Students are not exposed to technology and decision-support systems, evidence-based practices are not emphasized, and learning is not focused on multidisciplinary teams. In other words, we are not training individuals to practice or acquire the kinds of skills they will need to be effective in the health care delivery system we are attempting to create. Changing the medical education system will require the active participation of professional associations, educational leaders, and professional licensing and certification groups.
FIVE-PART AGENDA FOR CHANGE
The committee put forward an agenda for changing the U.S. health care system:
-
Commit to a shared agenda for improvement in six areas: safety, effectiveness, patient-centeredness, timeliness, efficiency, and fairness.
-
Adopt “10 rules” (see below) to guide the redesign of care processes.
-
Implement more effective organizational supports.
-
Focus initial efforts on priority areas.
-
Create an environment that fosters and rewards improvement.
TEN RULES FOR REDESIGNING AND IMPROVING CARE
Private and public purchasers, health care organizations, clinicians, and patients should work together to redesign health care processes in accordance with the following rules.
-
Care should be based on continuous healing relationships. Patients should receive care whenever they need it and in many forms, not just through face-to-face visits. The health care system should be responsive at all times (24 hours a day, every day), and access to care should be provided over the Internet, by telephone, and by other means in addition to face-to-face visits.
-
Care should be customized based on the patient’s needs and values. The system of care should be designed to meet the most common needs but should have the flexibility to respond to an individual patient’s choices and preferences.
-
The patient should be in control. Patients should be
-
given necessary information and the opportunity to exercise as much control as they choose over health care decisions that affect them. The health system should be able to accommodate differences in patient preferences and should encourage shared decision making.
-
The system should encourage shared knowledge and the free flow of information. Patients should have unfettered access to their own medical information and to clinical information. Clinicians and patients should communicate effectively and share information.
-
Decision making should be evidence-based. Patients should receive care based on the best available scientific knowledge. Care should not vary illogically from clinician to clinician or from place to place.
-
Safety should be a property of the system. Patients should be safe from injury caused by the care system. Reducing risk and ensuring safety will require systems that help prevent and mitigate errors.
-
The system should be transparent. The health care system should make information available to patients and their families that allows them to make informed decisions when selecting a health plan, a hospital, or a clinical practice or when choosing among alternative treatments. Patients should be informed of the system’s performance on safety, evidence-based practice, and patient satisfaction.
-
The system should anticipate patients’ needs. The health system should be proactive in anticipating a patient’s needs, rather than simply reacting to events.
-
The system should constantly strive to decrease waste. The health system should not waste resources or patients’ time.
-
The system should encourage cooperation among clinicians. Clinicians and institutions should actively collaborate and communicate with each other to ensure that patients receive appropriate care.
REFERENCE
IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
Bridging the Quality Chasm
David Lawrence
Kaiser Foundation Health Plan
This presentation focuses on the management of scientific and technological breakthroughs as they are made available to the health care delivery system—specifically on whether health care has kept pace with innovation by moving them into practice safely and responsibly. There is a substantial amount of overuse, misuse, and underuse of available science and technologies in the health care system—regardless of geography, type of payment, or when and where physicians were trained. To address this problem, the Institute of Medicine (IOM) undertook two studies, To Err Is Human, published in 2000, which focused on safety issues, and Crossing the Quality Chasm, published in 2001, which focused on quality issues. Both reports highlight the symptoms of a broken system. Both reports concluded that there is a mismatch between the rate and quantity of scientific and technological innovations and the ability of the health care system to use them safely and responsibly.
Wide variations in quality were documented as far back as 1975 in a small-area variation analysis by John Wennberg, M.D., and then in a variety of other studies across the country in the last 30 years (O’Connor et al., 1999; Wennberg, 1999). Recent safety studies, primarily but not exclusively studies by Lucien Leape and his colleagues at Harvard, identified a variety of medical errors that result in morbidity and mortality caused not because of physician malfeasance but because of system errors (Brennan et al., 1991; Leape et al., 2002; Thomas et al., 2000). The number of hospital deaths from these errors range from 30,000 to 80,000 per year. At this point, we have no understanding and little documentation of the number of errors in the ambulatory setting. Some early estimates in the United Kingdom and the United States have been published (Bubin, 1999; Fischer et al., 1997; Weingart et al., 2000). The total number of deaths attributable to errors in the health care system we think could be as high as 150,000 or even 200,000 per year.
Another measure was published by Barbara Starfield in an article in Journal of the American Medical Association in 2000. Dr. Starfield looked at the whole question of system-related deaths for all reasons, including errors. She concluded that 200,000 to 250,000 deaths per year were attributable to system-related causes, of which error is the most notable (Starfield, 2000). Starfield also made interesting comparisons between our system and others in terms of a variety of health outcomes. She concluded, as have many others, that although we spend an enormous amount on health care and lead the world in scientific innovation and technology, the results in terms of improved health do not match the level of investment.
There are also other symptoms of poor quality in the health care system. One of them has to do with responsiveness. In the Picker Institute studies of patient assessments of their health care experiences, about three-quarters of those surveyed indicated that their experiences with the health care system had led them to conclude that it was a “nightmare” to navigate (Picker Institute, 2000). They identified duplication, lack of communication, conflicting points of view about what should be done, and lack of understanding about what the science suggested. In short, the system is fragmented, fractured, and not patient-centric.
Finally, there is the cost of poor quality care, which has interesting implications for innovation. Between $.30 and $.40 of every dollar spent on health care is spent on the costs of poor quality. This extraordinary number represents slightly more than a half-trillion dollars a year. A vast amount of money is wasted on overuse, underuse, misuse, duplication, system failures, unnecessary repetition, poor communication, and inefficiency.
In this respect, the experience of General Electric Company and others in more tightly managed and highly organized manufacturing systems may be instructive. Companies often find substantial opportunities for improvement in the cost performance of the system by using quality-
improvement tools. The health care system does not even come close to a well organized, systematically designed system like a production or manufacturing system.
Our experience in Kaiser Permanente suggests that these numbers are not exaggerations. When we look for ways to improve the organization and delivery of care, we often find that substantial improvements can be made in the underlying cost performance of the organization. In fact, the premise on which we compete is that we can drive costs down by improving quality.
There are five major problems with the health care system. The first is that most of the scientific and technological breakthroughs that have occurred since World War II have not simplified the task of taking care of patients. In fact, they have made it more complex. Here are some examples:
-
As we entered the 1950s, there were about 10 to 12 categories of health care professionals in the United States. Today, there are more than 220 categories of health care professionals.
-
Right after World War II, there were about six to eight—depending on how you counted them—specialties in medicine. Today, there are more than a hundred.
-
In 1970, there were approximately 100 published randomized control trials (RCTs) in the American medical literature. In 1999 alone, almost 10,000 RCTs were published. Half of RCTs published in the United States have appeared in the last five years.
Science and technology have certainly contributed to growing complexity in medicine—increasing the number of people involved, increasing the number of categories of people involved, raising expectations about what can be done to treat people, and increasing the amount of science and technology that must be managed. Largely as a result of advances in science and technology, the medical care system is far more complex today in terms of the number of institutions and types of health care practitioners than it was in 1950.
Second, the health care system, or nonsystem, has grown enormously over the last 50 years but has failed to keep the patient and the patient’s family at the center of the enterprise. It is small wonder that people identify the system as a nightmare to navigate. It is not a patient-centered system.
How could the complexity of a system be significantly decreased? First, we could create a highly sophisticated production-design or manufacturing-design process to handle the complexity. Then an investment could be made in an information technology infrastructure. Next, we could create flow systems to manage the support activities required to carry out these processes, retain people, and set new standards of quality.
In medicine, we have done very little of this. Physicians are still trained on the principle of individual, professional autonomy, even though, in reality, they do not work in autonomous situations at all. Production design is a foreign word. In fact, it is considered almost sacrilegious to talk about production design in medicine. To many practitioners medicine is a religion, not a science. Therefore, the tools of production design have not been applied in the units where patients get care.
The third issue is that it is extraordinarily difficult to scale up medical care delivery. There are few examples of integrated care across ambulatory, inpatient, hospice, and home settings. Only a few systems enable us to capture capital and reinvest capital in the delivery system infrastructure. With 80 percent of physicians practicing in groups of fewer than 10, medicine remains largely a single interaction between a patient and a doctor. In reality, although the patient-doctor interaction remains absolutely essential, the enterprise itself now involves a much more complex set of interactions.
Except for the Veterans Health Administration, Kaiser Permanente, which has 10,000 physicians, is the largest health care delivery system. The next largest may be the Mayo Clinic. Most others are small, regional players on the delivery system side. Until there are more scaled-up enterprises, it will be difficult to collect and reinvest enough capital to build and support the production capability essential to the delivery of the science and technology that innovators are creating for us.
Fourth, our public policy environment is structured to inhibit the reshaping of the medical care delivery system. For example, in Wisconsin there are 27 licensed categories of health care professionals, each with its own board of practice. Medicine should be about removing boundaries so that people can flow seamlessly among a variety of practitioners, based on what the technology requires and what the patient needs. Yet regulatory and license-based silos create barriers between professionals. These barriers must be broken down to create teams and to deliver integrated care. This can be done, but only with great effort. The licensing system is designed to protect the interests of particular professional groups in medicine, not to further the delivery of integrated care.
On the reimbursement side, the fee-for-service system is designed to reward individual acts by individual clinicians. Our current reimbursement system does not support integrated delivery capabilities. Crossing the Quality Chasm called for experimenting with a variety of reimbursement approaches to determine which ones would stimulate the creation of integrated delivery capabilities—prepayment, perhaps, or capitation or other approaches. The fact remains that the classic fee-for-service system is a barrier to the development of collaborative medicine.
The final issue identified in Crossing the Quality Chasm is that information technology is not being used in the delivery system the way one would expect for such an information-rich industry. It is estimated that less than 2 percent of total revenues in health care is being invested in information technology infrastructure. Much more is being invested on the health insurance side, but investment on the delivery system
side is much lower than in other industries or in the medical technologies industry. Finding capital, either by aggregating organizations to generate capital or by other means, is a major issue. As the system stands, we cannot make innovations in health care delivery that match the complexity of the science. A physician trying to keep up with 10,000 RCTs in a year cannot practice evidence-based medicine without an information technology decision-support system. It is simply beyond the capacity of the individual to keep up.
Now let’s turn to opportunities for innovation, using the problem areas as the focal points. The first priority for innovation is to improve the ways patients can connect with the medical care delivery system. Innovations in monitoring, diagnosis, and treatment technologies will enable patients to self-manage, or at least communicate on a regular, ongoing basis, with the health care system. It makes no sense to continue to invest heavily in the bricks and mortar of classic delivery systems when there are other vehicles for taking care of patients in a far more responsive, patient-centric way. So giving patients the tools and creating bridges between the patient and the delivery system is one focus for innovation.
For example, one of the many promising innovations is the ability to test whether Coumadin is operating at therapeutic levels; this can be done by the patient using a hand-held testing device. A device for testing blood sugar is another. These and many other devices will substantially improve the connection between the patient and the system and put more capability in the hands of the patient. These innovations will also decrease our dependence on brick and mortar solutions for the delivery system.
The second major area for innovation is translating the tools used in the manufacturing and production of goods and services into a language that applies to health care. I would argue that the delivery of medical care today is the most complex production challenge on the planet. Think about what is involved in running a hospital with about 250 beds—a wide array of diagnoses, a multitude of judgments being made by teams of professionals interacting with patients, and all of the support production that makes this happen hour after hour, 24 hours a day, seven days a week. This is an extraordinarily complex production challenge.
The third area of innovation involves organizational design or scaling. It has proven to be extremely difficult to create sufficient scale systemwide to produce the necessary capital, systems, and training capabilities. Scaling up has been done successfully in certain health care settings, for example, hospitals, nursing homes, laboratories, and pharmacies, but it has proven to be extremely difficult to create any kind of organizational scale for building integrated delivery capabilities.
Last, innovation could come through interventions at the national policy level in regulation, reimbursement, and, possibly, the financing of the information technology infrastructure in medicine. Given the current organization of the health care system, the financing of the information technology infrastructure may exceed the capacity of the private marketplace. Perhaps we will have to create the medical equivalent of the Superfund for environmental cleanup to build the information technology infrastructure for the health care delivery system. This infrastructure involves more than electronic medical records, which simply capture and move information to support decision making. A robust infrastructure would incorporate analytic tools that would enable epidemiological studies of disease. Without this infrastructure, it is extremely difficult to test whether or not microproduction units are working well and whether we are getting anywhere with the larger organizational challenges facing us.
In closing, the message of Crossing the Quality Chasm should be taken to heart. The mismatch between the pace and scope of innovation in medical science and technology and innovation in the delivery system has created a chasm, which is aggravated by shifting demographics and the shifting of the disease burden from acute to chronic care. The complexity that both add to the task of taking care of patients has not been matched by equivalent sophistication in the delivery system.
REFERENCES
Brennan, T.A., L.L. Leape, N.M. Laird, L. Hebert, A.R. Localio, A.G. Lawthers, J.P. Newhouse, P.C. Weiler, and H.H. Hiatt. 1991. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. New England Journal of Medicine 324(3): 370–376.
Bubin, C. 1999. Mistakes happen: improved processes mean fewer mistakes. Ambulatory Outreach (Fall): 23–26.
Fischer, G.F., A.P. Munro, and E.B. Goldman. 1997. Adverse events in primary care identified from a risk-management database. Journal of Family Practice 45(1): 40–46.
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System, L.T. Kohn, J.M. Corrigan, and M.S. Donaldson, eds. Washington, D.C.: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
Leape, L.L., D.M. Berwick, and D.W. Bates. 2002. What practices will most improve safety?: evidence-based medicine meets patient safety. Journal of the American Medical Association 288(4): 501–507.
O’Connor, G.T., H.B. Quinton, N.D. Traven, L.I. Ramunno, T.A. Dodds, T.A. Marciniak, and J.E. Wennberg. 1999. Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. Journal of the American Medical Association 281(7): 627–633.
Picker Institute. 2000. Eye on Patients. A Report by the Picker Institute for the American Hospital Association. Boston, Mass.: Picker Institute.
Starfield, B. 2000. Is U.S. health care really the best in the world? Journal of the American Medical Association 284(4): 483–485.
Thomas, E.J., D.M. Studdert, H.R. Burstin, E.J. Orav, T. Zeena, E.J. Williams, K.M. Howard, P.C. Weiler, and T.A. Brennan. 2000. Incidence and types of adverse events and negligent care in Utah and Colorado. Medical Care 38(3): 261–271.
Weingart, S.N., R.M. Wilson, R.W. Gibberd, and B. Harrison. 2000. Epidemiology of medical error. British Medical Journal 320(7237): 774–777.
Wennberg, J.E. 1999. Understanding geographic variations in health care delivery. New England Journal of Medicine 340(1): 52–53.
Envisioning the Future
Jeff Goldsmith
Health Futures Incorporated
Our health care system is the largest knowledge-based activity in the world. It is one-third larger than the gross domestic product (GDP) of China and four times the size of Africa’s entire economy. The research and development portion of the health care system alone—this year about $50 billion between spending by the National Institutes of Health, venture capital firms, equity markets, and pharmaceutical companies—is as big as the GDP of many Latin American countries. And yet, although we are generating new knowledge at a staggering pace, we are also staggeringly inefficient in assimilating that knowledge and applying it to the delivery of health care services. Even though our health care system is being constantly enriched by new knowledge, we are still using nineteenth-century architectures and sociological constructs for this information.
UNRAVELING THE GENOME AND EXTENDING THE HUMAN LIFE SPAN
The business and mission of the health care system will change with two radical scientific advances. The first is the unraveling of the human genome. There was a tremendous wave of expectation that the mere mapping of the genome would revolutionize medicine and create powerful new tools for intervening definitively in disease processes. My nonscientist’s belief is that the results won’t be felt until we’ve done a couple of generations of really hard work. Eventually, genetic information will produce powerful tools for affecting our health, but it is going to take a while.
The second advance is tinkering with the human life span. At the beginning of the twentieth century, a typical American lived to be 47; by the end of the century, average life expectancy was about 80. Most of the increase was the result of eliminating premature causes of death—such as infant mortality and childhood diseases. In the past, most human biologists believed that there would never be much more improvement because the maximum life span of human beings is hardwired into our genome or into the processes by which cells reproduce.
In 1998, discoveries in the processes of cell biology led to the hope that we were close to understanding one of the mechanisms that limit the viability of our cells and tissues and, therefore, the life span of our organ systems. Many gerontologists became convinced that if we could understand the hardwired limits on the capacity of our cells and tissues to reproduce and begin attacking some of them—declining hormone levels, oxidation, etc.—we could dramatically extend the life span of human beings. There is now serious discussion of people living to be 140 or 150 years old.
The stem cell, the Holy Grail of human biology, is the subject of an enormous political debate in Washington, because the principal source of stem cells is discarded embryos from in vitro fertilization. Buried in the software of a stem cell is the recipe for each tissue type in your body, as well as the assembly instructions for the organ systems that those tissues ultimately form. A lot of people believe that, once we master the instruction sets buried in the stem cells, we will be able to create, on demand, tissues from our own cells that can be used to repair damage to our organ systems from strokes, spinal cord injuries, and other causes. In combination with growth factors that our bodies produce naturally to encourage cells to grow, we will have the power to replace damaged tissues and, eventually, whole organ systems.
As our understanding of human genetics improves, our paradigm of vaccination will also change. Right now we think of a vaccination as something given to children to protect them against infectious diseases. Soon, however, we will be vaccinating people against chronic diseases, such as breast cancer, asthma, and, perhaps, arthritis. We will be able to vaccinate people any time during the course of the development of the disease. Not everyone will be given the same vaccine, however, because the tools of genetic prediction will enable us to distinguish between risks of disease for each individual all the way down to the level of nucleotide
sequences. Instead of building blockbuster drugs to knock out diseases in whole populations of people, the pharmaceutical system will produce highly specific, genetically tailored responses to an individual’s genetic risk. Many of these advances in genetics will not be the result of “wet work” (i.e., laboratory research) but of computer modeling and the manipulation of massive computer databases using high-performance computing.
COMPUTERIZED PATIENT RECORDS AND DECISION-SUPPORT SYSTEMS
The Gartner Group, which studies health care systems, has envisioned a computerized five-generation patient record:
-
Generation 1 is a passive repository of clinical data based on information gathered manually and on paper.
-
Generation 2 is the repository of clinical data plus an electronic version of the paper chart. On this level, passive alerts about drug interactions would be possible. Crude rules built into Generation 2 systems would suggest that doctors reconsider decisions if a deviation from standard practice were observed.
-
Generation 3 combines the repository of clinical data, the electronic version of the paper chart, and orders entered by the physician. A Generation 3 record would be able to track patients across inpatient ambulatory settings and provide a full array of passive care alerts. If the patient’s status changes, the system would send the doctor a “do you want to do X?” type of message, thus providing an undergirding for making clinical decisions.
-
Generation 4 would make the leap from a passive system that mimics a record-keeping system to what might be called “groupware” for clinical decision making. Embedded in the system would be care pathways, work flows, and data on the outcomes of certain courses of action for a particular patient with a particular condition. Creating a Generation 4 record will be very expensive. It will require information based on thousands of hours of structured discussions by physicians regarding what they do and then review of emerging scientific literature on clinical effectiveness and to support clinical decisions. At this level, the patient’s chart would become a living document that guides the care process; the system would become a full partner in the care process.
-
Generation 5 would be an “intelligent” system capable of self-modification that has acquired knowledge of the context of the patient and of the cognitive style and work flow requirements of the physician or clinical team. With a Generation 5 system, physicians would have complete access to the information they need to make better decisions. Thus, the system would become a trusted source of new knowledge that could help physicians make decisions. The system would create enough options and possibilities for physicians to continue learning, thus encouraging the physician’s development, as well as improving patient care.
INTERACTIONS BETWEEN PATIENTS AND THE HEALTH CARE SYSTEM
Changes in the clinical operating system will improve interactions between doctors and patients, who will not have to be in the same room, or even in the same time frame. Enterprise software will provide a patient’s personal health record with information from the person’s entire clinical history. Patients and caregivers will have a “dashboard” that enables them to control their interactions with the rest of the health care system. Thus, patients will be able to acquire knowledge not only from their doctors but also from the system about managing their own health problems. Once patients understand that this is possible, they will insist on being treated in institutions that have these capabilities.
Patients will hire care managers, particularly for the elderly in a household. Care managers will use Web-based tools to navigate knowledge domains to help make better decisions and get better results. For instance, we will have a search engine that will enable us to ask the questions we really want answered. For example, we could ask where the three most promising clinical trials for drugs that affect lupus are being done and for a link so we can find out about participating in a trial.
SUMMARY
Advances in medicine in the last 25 or 30 years—tools from electrical engineering, miniaturization, and less invasive surgery—have moved our understanding and our interventions closer to the origins of disease. In the nineteenth century, the health care system was focused on acute care—intervening in the late stages of disease and salvaging people from life-threatening events. In the twenty-first century, the health care system will focus on predicting a patient’s risk for disease based on genetic screening and powerful clinical chemistry. The system will not only have therapeutic tools but will also have tools to change behavior and disease-management software to modify risk factors and, ideally, eliminate the risk before it progresses into an illness in the first place.
An array of powerful new tools will make our medical care system more humane and more responsive to our needs. But to liberate caregivers and patients from our current cumbersome processes that don’t work very well and cost a staggering, even unconscionable, amount of money, we will have to do a tremendous amount of work to renovate the institutions and cultures of medical care.
Improving Health and Health Care
Lewis G. Sandy
Robert Wood Johnson Foundation
Private foundations like the Robert Wood Johnson Foundation are like venture capitalists for ideas. Today, I’m going to talk about our priorities and strategies for improving the health care system and health care. I will reflect on the challenges we face in implementing our agenda, outline strategic directions, and suggest how engineering and medicine can be linked.
I want to make three points. First, I believe the major problem in health care is not a lack of tools, although we have heard about new tools that could and probably should be developed. The major problem is the way we use existing tools. Second, in thinking about using engineering principles, theory, and knowledge, we must think about health, not just health care. We must think beyond the health care delivery system to using technology to actually improve the health of people. We must think beyond the organization and financing of our current health care system. Third, bringing engineering and medicine together is not predominantly a technical problem; it is a cultural problem.
The Robert Wood Johnson Foundation is one of the largest foundations in the country and the largest foundation devoted to improving health and health care for Americans. We have about $8 billion in assets and award $400 million annually in grants. We use a variety of methods to achieve our goals—such as supporting research projects, demonstrations, training, communications, and workshops. Our work is organized around three goals: (1) ensuring that all Americans have access to care; (2) improving care for people with chronic health conditions; and (3) helping the country deal with substance abuse. General improvement is part of our mission, but the specifics are embodied in our goals. We encourage the health care system to do the right things. In some cases, we support innovations. In addition, we promote the diffusion and adoption of existing best practices.
For example, a program called Improving Chronic Illness Care run by the Group Health Cooperative of Puget Sound focuses on improving care for people with chronic illnesses. Our health care delivery system generally focuses on acute care; the system is geared toward treating infectious diseases and acute traumas. There is a mismatch, however, between that model and the prevalence of disease, predominantly chronic illnesses that require a different model of care with different elements.
A chronic care model of health care delivery includes linkages between the health system and the community, as well as support for self-care and self-management. A health care delivery system organized for chronic care must provide decision-support tools for providers and for patients and families. It must also have a supporting information infrastructure; in addition, the health care delivery team must be redesigned and retrained. The foundation has provided $32 million to support projects, research, and demonstrations and provide technical assistance to promote a health care system configured to treat chronic illnesses.
A program called Smoke Free Families focuses on the dissemination of best practices. The goal of the program is to eliminate, or at least reduce, smoking by pregnant women, one of the most important, modifiable risk factors for premature births. Everyone recognizes that prenatal smoking is a problem, but the adoption of proven, effective interventions has not been successful. We provide instructions for providers to assess the situation and advise women to quit smoking during prenatal visits.
We try to implement and evaluate new models of health care being developed by researchers and idea entrepreneurs. Once a better technology has been developed and demonstrated, the difficulty is in getting individuals to use it. It is even more difficult to create an incentive structure that encourages the entire delivery system to adopt and diffuse innovations. We have tried to increase consumer demand for higher quality care and have worked through vehicles, such as a purchaser institute that brings together public and private purchasers. We know that consumer demand can change systems of care. Consider the changes in obstetrical care,
which has changed from a technological, sterile practice to a more humane, patient-centered, caring, warm experience through birthing centers. These changes are the result of consumer demand for changes in care.
Not enough attention has been paid to improving overall health care. The health care system needs a “Toyota,” someone who can do for health care what Toyota did for the auto industry—engineer the product in a fundamentally different way. No health care delivery system yet has been demonstrated to be better in all respects—in technical quality, interpersonal quality, and so on.
The foundation is providing support to the Institute for Health Care Improvement to develop a demonstration program that would lead to a transformational change in health care. The project, called Pursuing Perfection, is focused on analyzing barriers to improving health care. We want to shake up the current system to show that things can be done in a fundamentally different way. We provide grants and technical assistance for the program, and we are creating a learning network and undertaking a communications campaign. Currently, we are visiting 26 sites to choose awardees for 12 planning grants, some on errors in medication, some on access to care and patient flow, and some on nursing, staffing, and human resource management.
The program has generated a great deal of interest, indicating that there is a pent-up demand among providers for a transformational change in health care. In a recent survey, we found that about 30 percent of physicians think improving care is an important problem and that they personally could affect change (IHI, 2001).
Very little production-process thinking is being used in health care. Even those working on improving quality of care are not using applicable engineering tools. We need to open a bridge between medicine and engineering. People in the engineering community know which tools would be helpful for analyzing problems and effecting improvements.
One of the differences between engineering and medicine is that engineers believe in the theoretical possibility of perfection; doctors do not. Even in highly reliable organizations, adverse events happen all the time. We know from the genome project that human beings are riddled with genetic errors. Doctors understand illness and medical care as part of the human condition and the human tragedy.
But we can make changes through process improvement. Medicine is an ancient story about heroes and tragedies that has only been a high-technology scientific enterprise for the past 50 to 75 years. For the first 3,000 or 4,000 years of the history of medicine, it was considered a calling, a profession that dealt with the inexplicable tragedy of the human condition. This long history is built into the socialization of physicians in a fundamental way.
To bridge the culture gap, engineers who work in health care delivery or operations improvement will need cultural training in some aspects of health care. A good resource is On Doctoring by Reynolds and Stone (1991), which is given to all entering medical students by our foundation to socialize them into the practice and culture of medicine.
Physicians also need to be educated in what I call the “engineering culture.” Some efforts are being made to train physicians in principles of operations and improvement. However, we need to develop a language and concepts for health care practitioners interested in this field. We also need a research agenda, such as the one being developed for medical errors and patient safety. Another critical area for research is human factors engineering. The burden of malpractice suits and litigation can hardly be overestimated, and we need to create safe harbors for reporting on adverse events or near misses. We must also develop a national agenda for improvement.
We must consider health care at the macrosystem level, that is, the health of the population, and not just the health care system. The Web and other technologies can be used to provide consumers with information on healthy living and to promote behavioral change. The major modifiable determinants of health are in the environment in which people live, choices in individual behavior. Think about how we can use technology and engineering principles to influence those choices. In addition, we should be thinking about designing communities that encourage people to walk or otherwise stay physically active because we know that even minimal exercise can have a huge health impact. We can promote behavioral change strategies to help improve people’s diets and help them deal with stress. New organizations and new functions outside the traditional health care delivery system can improve people’s lives.
REFERENCES
IHI (Institute for Healthcare Improvement). 2001. Pursuing Perfection. Press release May 8, 2001.
Reynolds, R., and J. Stone, eds. 1991. On Doctoring: Stories, Poems, Essays. New York: Simon & Schuster.
Engineering and the Health Care System
Richard J. Coffey
University of Michigan Health System
I’ve spent almost 40 years in health care, including 10 years in consulting, which has given me the opportunity to see many different institutions. Today, I will lay out a general format for the issues facing our institution and other institutions across the country.
We can divide health care systems into different levels. Table 1 shows a model with five levels. At the individual patient level (Level 1), the treatment of the patient, we encounter the issue of autonomy. Physicians are trained from the very beginning to work autonomously, to make autonomous decisions. When we try to standardize care, some physicians may feel their autonomy is being challenged. This has made it difficult to standardize equipment, supplies, and pharmaceuticals. Leaders of industrial organizations, for example, often have trouble understanding that health care leaders cannot just order physicians to do something. Academic institutions that have tenured physicians may have the most difficulty resolving this issue. To compound the problem, institutions tend to recruit interns, residents, and physicians with the same attitude toward autonomy. Mayo Clinic tends to recruit people whose cultural orientation is similar to the prevailing orientation at Mayo. Academic institutions tend to recruit strong researchers who are used to having academic autonomy.
The second level is the department/unit level, such as operating rooms and cancer programs. The third level is the individual hospital. The fourth level, multihospital/ multiorganizational systems, try to coordinate operations among multiple sites, multiple kinds of functions, and so forth. These systems have developed largely in the last few years. A few years ago, my colleagues and I wrote a book on a fifth level, virtually integrated health systems, collaborations among multiple organizations to improve health (Coffey et al., 1997).
TABLE 1 A Five-Level Model of a Health Care System
|
Level |
Explanation |
Examples |
|
Patient |
Treatment of individual patient |
|
|
Department/unit |
Specific systems within a program, unit, or department |
|
|
Hospital |
Interacting systems within a hospital |
|
|
Multi-institutional/ |
Interacting systems among institutions multiorganizational systems |
|
|
Virtually integrated health system |
Medical care in the larger context of a community and environment |
|
To begin with, we should correct a common mistake. Most of the current U.S. health care system is not focused on health. The current system is primarily a medical care system focused on diseases and illnesses. Primarily, we treat people who are already sick. Some organizations, such as health maintenance organizations, are focusing more on prevention and health; but in large part, the system deals with medicine, rather than health.
Table 2 describes the concept of a six-dimensional, virtually integrated health system. The first dimension, social and environmental conditions, includes crime violence, the community situation, the family situation, and many other factors that have a much stronger effect on health than much of what we do. A health care system that ignores the environmental dimension has a very narrow focus.
The second dimension, health-related human conditions, is familiar to many. A classification system is necessary so we can standardize or categorize diseases and treatments (e.g., diagnosis-related groups). The third dimension, foci, describes types of activity. The majority of work done by health care organizations currently involves diagnosis and treatment, but very little protection. Occupational Safety and Health Administration standards, Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and other organizations address protection more directly than the traditional health care system.
Settings is the fourth dimension. Most of our work right now is done in ambulatory and inpatient settings, facilities to which patients come. An example of health care in the community setting is a cooperative program by the University of Michigan Health System (UMHS) and St. Joseph Mercy Health System, in Ann Arbor, Michigan. The purpose of the program is to discourage smoking by eighth graders and to raise their health awareness.
Core/key processes, the fifth dimension, categorizes major processes, such as leadership, planning, and human resources. These categories are very similar to those used by JCAHO and other organizations. The final dimension categorizes resources.
As an example of how these levels apply, consider the taxonomy we use to address heart disease. What are we doing environmentally to affect heart disease? How do we categorize heart disease? What functions are we and/or others providing? Are we focusing on treatment? The methods of treatment for heart disease are changing radically—especially surgery versus the new drug-eluting stents, which could threaten the role of cardiac surgeons. Recently, radiologists have been testing whether CT scanners can diagnose heart disease as well as or better than cardiac catheterization. Because CT scans are noninvasive, this research has many potential implications for the way we coordinate and provide care. These changes will affect who provides care, where the money goes, and who controls it; there are substantial dollar differences between medical and surgical admissions. The settings may also change. As we consider engineering applications, we must remain mindful that the health care system is much broader than just work in a hospital. Most of you know there has been a sharp drop in the length of hospital stays in the last decade. Much of that change has been possible because some care is now provided in other settings. Most large health care organizations have home-care services. Today, even if you are on IV therapy, you may not have to be in a hospital. Many patients can be treated in a less costly environment than a hospital.
Dr. James L. Reinertsen contrasts the ideas of “high science” and “low science” (Reinertsen, 2003). High science asks if population A is different from population B (you try to control for all other variables). High science studies involve comparative research or clinical trials that generate “descriptive statistics.” Low science asks how a process will work the next time a patient experiences it, which involves many complex variables. Methods used to answer this question include quality improvement, run and control charts, and modeling. Low science generates “analytic statistics.” Most academic medical and engineering publications do not publish “low science” research.
Academic physicians survive not by the quality of patient care, but by whether or not they get tenure. And tenure is based not on the number of patients seen, but on research and publications. Young professors in engineering colleges are judged in similar fashion. If “low science” is considered substandard, not academically acceptable, young academicians are discouraged from pursuing this type of work in health care. When W. Edwards Deming split from the rest of the statisticians, most academic statisticians advocated theoretical “high science.” Deming advocated using statistics to predict system performance. I think we should support research in predictive science, and what Reinertsen calls “low science.” If we don’t, we will be turning our backs on enormous opportunities to improve systems, health care, and health.
Figure 1 illustrates an example of interacting systems in a hospital. This is not intended to be a flow chart, but it shows some of the interactive processes involved in the care of a patient. Patients come into a clinic or emergency department and may move from there to another area—to the operating room, post-anesthesia care unit, intensive care unit, acute care bed, home care, etc. Physician services and consults are also going on, as well as diagnostic tests. Improved engineering could benefit every one of these processes. There are large variations among patients, which we also need to address. But, most important, we must address the large variations in the way we care for patients. Engineering models could help us address these system variations and minimize their impacts. To reduce health costs, most health care institutions are improving their use of resources, including staff, equipment, and facilities. If systems are not efficient and coordinated, this leads to major bottlenecks,
TABLE 2 Taxonomy for a Virtually Integrated Health System
|
1 |
2 |
3 |
4 |
5 |
6 |
|
Social and Environmental Conditions |
Health-Related Human Conditions |
Foci |
Settings |
Core/Key Processes |
Resources |
|
|
|
|
|
|
|
Source: Coffey et al., 1997. |
|||||
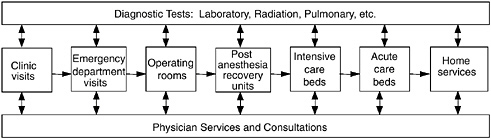
FIGURE 1 Sample of interacting hospital system components.
poor care, delays, lost business, more pain, and so on. This is an illustration of the tremendous opportunities for engineering.
Figure 2 illustrates a breakthrough matrix (Gaucher and Coffey, 2000). Engineering can make major contributions in terms of designing products and processes. We can improve models of customer requirements, interests, and perceptions.
Many kinds of engineering applications (e.g., queuing, operations research, and human factors research) can be applied at all five levels of health care systems (i.e., patient, department, hospital, multi-institutional systems, and virtually integrated health systems). Consider scheduling systems, for example. We have good scheduling systems for individual departments and services, like operating rooms. Where we have failed, as was pointed out in the Institute of Medicine reports, is in “handoffs,” the movement of patients from one area of the system to another (IOM, 2000, 2001). At UMHS, for example, we have a good operating room scheduling system, but it isn’t linked to staffing of the nursing units or the admitting system. Therefore, we have discrepancies in our schedules. The same is true to some degree in virtually all health care organizations.
Another example of a scheduling problem is the result of our aging population. People often show up in emergency rooms at night with cardiac and other serious problems. These visits lead to increased medical admissions, which often delay the operating room cases the next day and cause huge turmoil in the organization. I believe one of the greatest opportunities for engineering is to improve the coordination of systems throughout a hospital or among multiple institutions.
At the patient system level (Level 1 in Table 1), changes should be planned and implemented in collaboration with physicians, nurses, and other caregivers. Engineers don’t deliver care, but they help analyze and model changes, such as comparing the cost effectiveness of different medications. Today, every insurance company and every hospital is doing cost-effectiveness comparisons, but these efforts are not coordinated in any way.
Another frustrating thing is that we do not have a bar coding system throughout the health care industry. Each manufacturer has its own bar code system. Standardized bar codes could improve the quality of care, staffing, speed, and operational effectiveness. Also, we could model and optimize care protocols using decision algorithms and critical pathways. Many protocols have been developed, but few of them are used. I believe this is because individual physicians retain their autonomy rather than deferring to the collective autonomy of a group of physicians to design best-practice protocols. In UMHS, for example, we have a notebook full of critical pathways, but we frequently do not use those protocols.
Don B. Chaffin, professor of industrial and operations engineering at the University of Michigan, is working to improve the handling of patients to reduce back injuries to staff (Chaffin et al., 1999). Although the injury rate for employees in the health care industry is higher than in the construction industry, as an industry, we are not even taking care of our own employees. So there are many opportunities for engineering applications.
At the department level (Level 2 in Table 1), engineering methods (e.g., scheduling systems, inventory control, and staffing models) could improve the quality of care and cost effectiveness. As most of you know, we do not have labor standards in health care. In fact, very few health care managers understand what labor standards are—engineered standards that define a job, measure time, pace-rate the person doing the job, etc. Hospitals don’t even have well defined jobs; every nurse does the job differently. Most hospitals don’t even have labor standards for nonprofessional staff, such as housekeepers. At U of M, an industrial and operations engineering student group is working on standards for environmental services, establishing a standard for how long it takes to clean a patient room, for example. There is a tremendous opportunity for engineering here, which could also provide fantastic opportunities for engineering students. Every term, 40 to 45 students undertake projects and engineering studies in UMHS. But senior people must oversee the students to make sure they understand cross-departmental, interactive issues.
At the hospital system level (Level 3 in Table 1), a great deal of attention has been given to information technology. Linking scheduling systems among departments or elements
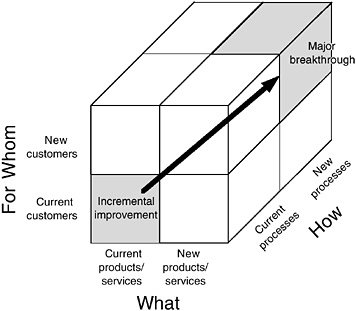
FIGURE 2 Breakthrough matrix. Source: Gaucher and Coffey, 2000.
offers a great opportunity for engineering applications. Computerized physician order entry systems are being strongly promoted by many organizations, including large employer organizations (e.g., the Leapfrog Group), and there are a few really good systems. For example, Intermountain Health has an excellent system that’s been in development for about 30 years. But hospital-wide information systems don’t come about quickly, and they are very expensive. At UMHS, we have spent about $30 to $50 million dollars over the last 10 years, and we still don’t have an order entry system. We do have an excellent result reporting system, called CareWeb, that includes test results, operating room reports, discharge summaries, clinic notes, and other things—all available at any computer terminal in our system. Now we are spending millions to develop a physician order entry system with built-in logic checks for laboratory results, pharmaceuticals, and other factors. As an industry, we have poor hospital-wide information systems.
The multi-institutional system level (Level 4 in Table 1) addresses issues related to multiple facilities or organizations in a single health care system. For example, how are home-care services linked with hospital discharge planning, and how are both of them linked with ambulatory care clinics? Lack of coordination among departments and organizational units is often a serious problem.
At the virtually integrated health system level (Level 5 in Table 1), the engineering opportunity is to develop processes to enable physicians, hospitals, public health departments, employers, schools, houses of worship, and other organizations to work collaboratively to improve health. I think there are tremendous opportunities here for engineering applications, but I’m not sure where the political support, leadership, resources, and financial support will come from. Schools, houses of worship, YMCAs, and other organizations may have more effect on changes in behavior than most physicians. Yet few health care systems include schools and other organizations in the foci dimension (see Table 2). Even UMHS, a leader in health planning and delivery, has barely scratched the surface of becoming a virtually integrated health system.
Right now, the health care system in the United States is characterized by fighting over resources and a lack of coordination. Employers, employees, insurance companies, hospitals, doctors, and other stakeholders are fighting with each other rather than trying to coordinate care to improve health. I think each group is so protective of its autonomy that we are not thinking about the broader good for everyone.
In summary, the United States has an aging population, rapidly developing technologies and medical care capabilities, and increasing expectations for care, which are driving our health care costs out of control. Every organization and individual is impacted by these changes. Small employers are perilously close to not being able to afford insurance for their employees. Health care insurance premiums for small employers have been rising by double digits for the past three to five years.
In my opinion, the recognition that we need engineering assistance is greater now than it has been at any time in the past 40 years. At UMHS, the dean of the medical school, many faculty members, and many hospital administrators now recognize that we need models of how UMHS works and engineering tools to help us manage it better. The question is whether, in an environment of very scarce resources, health care leaders are willing to pay for engineering to improve the health care system. In general the answer is no, at least so far. Engineering professionals must demonstrate the cost effectiveness of their services, because engineering models and solutions at all five levels of health care systems are vitally important.
REFERENCES
Chaffin, D.B., G.B.J. Andersson, and B.J. Martin. 1991. Occupational Biomechanics. 3rd edition. New York: Wiley-Interscience.
Coffey, R.J., K.M. Fenner, and S.L. Stogis. 1997. Virtually Integrated Health Systems: A Guide to Assessing Organizational Readiness and Strategic Partners. San Francisco: Jossey-Bass.
Gaucher, E., and R.J. Coffey. 2000. Breakthrough Performance: Accelerating the Transformation of Healthcare Organizations. San Francisco: Jossey-Bass.
IOM (Institute of Medicine). 2000. To Err Is Human: Building a Safer Health System, L.T. Kohn, J.M. Corrigan, and M.S. Donaldson, eds. Washington, D.C.: National Academies Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C.: National Academy Press.
Reinertsen, J.L. 2003. Science, Art, and Physician Autonomy. The 22nd Annual Donald P. Shiley Visiting Lectureship, Scripps Research Institute, La Jolla, California, March 23, 2003.
Engineering and the Health Care Organization
Vinod K. Sahney
Henry Ford Health System
Even though as an industry the U.S. health care system spends more than $2 trillion every year, a number of barriers at the organizational level have impeded the performance improvements we are all seeking. Certainly, one should not assume that the leaders who run this industry are incompetent; they invest in whatever is in the best interests of their particular institutions. Because of the environment, the payment systems, and the way things are structured, health care leaders have not invested in engineering approaches that could have a positive impact on quality and productivity.
The Henry Ford Health System is a very large integrated health care system with three major components: hospitals, a medical group, and a health plan with 600,000 enrollees. The system has $2.6 billion dollars in annual revenue, six hospitals, and a medical group with 900 physicians and 16,000 employees in the metropolitan Detroit area.
Changing practices in an environment like Henry Ford or the Mayo Clinic or Kaiser Permanente, where the medical staffs are highly motivated, well paid, and academically oriented, is not the same as changing practices in a community hospital system, where physicians come for part of their time and are independent business people. In a community hospital environment, it can be extremely difficult to change clinical practice. It can be all but impossible to get six orthopedic surgeons to standardize the use of supplies (e.g., to agree on which implant they will use). If they are pressured, they can walk out and go to the hospital across the street. So far, most of the work on quality improvement and engineering solutions is being done in a few leading-edge organizations.
Anyone who thinks the problems of the world can be solved by rational discussion among highly educated people has never attended a faculty meeting. The problem is not intelligence, but self-interest. Every organization that tries to introduce change faces cultural issues that work against the implementation of new solutions. For instance, the Institute for Healthcare Improvement has learned that current best practices are not even implemented consistently by single institutions, much less by institutions around the country (Sahney, 2003). An institution may implement best practices in its prostate cancer unit, but other groups in the same institution may completely ignore those practices. Problems occur both within institutions and among multiple institutions.
There are four major barriers to improving quality. The first barrier is a lack of metrics for comparison. What do we mean by improving a system’s performance? Often, large numbers of patients select one delivery system over another based on their specific needs. For instance, if a patient is getting diabetic care in one system and prostate care in another, comparing quality of health care and productivity becomes a difficult issue. It may be possible to determine that, at a microlevel, a system has improved care for a particular disease. But at a macrolevel, comparison is nearly impossible. It is very hard to evaluate whether any innovations make a difference in cost or productivity.
In the United States, the problem is further complicated because the acute-care sector is highly organized, but the chronic-care system is very disorganized, with large numbers of independent physicians providing care. Another aspect of the metrics problem is the indigent-care sector. Fifty percent of the population within a 10-mile radius of Henry Ford Hospital is either underinsured (Medicaid) or uninsured. The hospital must treat all of these patients for free, which puts an enormous burden on the hospital’s services. Before solutions can be proposed for improving organization, it is essential that we agree on the metrics to be used for comparison. As an example of the confusion surrounding rating systems, the ratings issued by U.S. News and World Report, AARP, and Solucient are all based on different criteria; as a result, each has rated a different institution as the best in providing care.
The second barrier is a lack of alignment in the reimbursement system. In general, under the fee-for-service system, institutions are paid for procedures and visits but not for improvements in health status. The Advisory Board, a health
care industry organization in Washington, D.C., subscribed to by almost all of the major institutions in this country, recently recommended that institutions that want to be successful should focus not on caring for medical patients, but on procedural care (The Advisory Board Company, 2001). In other words, if an institution wants to maximize revenue and profitability, it should keep all of the procedural-based patients and send all of the medical-care patients to the hospital across the street. Here’s another problem (or misalignment) in the current system. The reimbursement rate is higher when patients develop complications; this is obviously a perverse incentive. Instead of paying for quality care, the current system pays more generously if patients develop complications.
The third barrier is industry structure. Innovations are made by large hospitals and academic centers, which account for only about 25 percent of total expenditures in health care. A large proportion of care is provided by small community hospitals. For health care to improve nationally, innovations must be implemented in community hospitals. Therefore, improvement protocols should also be tested in these institutions.
A fourth barrier to improvement is that many people, including physicians, think quality health care is synonymous with the use of the latest technology. It is important to understand that there can be enormous gaps between quality of design and quality of conformance. Take an example from the automotive industry. Ford Motor Company spent millions to develop the Jaguar Lemans racing car, a vehicle that will only be used in races. Ford justified the expenditure by claiming the technology developed would also be used in the manufacture of new cars for consumers (e.g., the Ford Focus). But when the Focus was introduced, it was a mess. It was recalled six times in its first year. The engine compartment would catch on fire, the air bag would catch on fire or deploy spontaneously, the car would stall on the freeway, the front suspension would collapse. Otherwise, it was a good car.
In The Machine That Changed the World, the Toyota production system, which is considered the world’s best production system, was described in detail (Womack et al., 1990). But when other companies tried to copy that system, they found that they could not convert their production systems without developing the accompanying organizational culture. This is a problem in health care too. American surgeons can do wonderful things; but can they do them every time, consistently? Can quality care be delivered every time? This is a quality-of-conformance issue and not a quality-of-design issue. Making sure every patient gets the same quality of care every time is a serious issue. There are huge gaps here, major problems of conformance in the health care industry.
Across the country, a huge number of projects have been undertaken to improve the experience of patients at the care-delivery level (the microlevel). But at the macrolevel, little has been done to create an organizational environment that will make an overall impact and enable the transfer of knowledge from one microproject to another. In addition, as I mentioned earlier, the current payment system may not generate the will for senior leaders to improve quality. It’s not that we can’t improve or that we lack ideas—there are plenty of ideas. It’s just that we don’t have the will to work on improvements.
What would generate the will? If there were enough payment incentives, senior leaders would pay attention to what needs to be done. When clinical service chiefs at major institutions were asked how their senior leaders evaluate them, they all said by financial performance. They said they were never asked about the quality of health care they provide. In the prevailing culture, these questions are simply not asked. The will for improvement is not there.
To change this environment, the first thing we must change is the goals for health care delivery; the goals must be in alignment with population health status goals. To begin with, health care systems must define the populations they serve. If a health care system cannot define the population for which it is responsible, it is extremely difficult to set goals for improving people’s health status. If no goals are set, the system cannot be held accountable for failing to meet them.
Next, we should create macro-organizational models to test alternative reimbursement policies for delivery systems. Models that demonstrate the “cost of poor quality” must also be created. A major barrier to investments in quality improvement is the belief on the part of physicians and senior leaders that the investments do not pay back. Models could prove that investing in improvements would actually generate a reasonable rate of return.
Another important step would be to create organizational decision simulators—practical operational tools that would show nurses what to do, if, for instance, the OR or ER is backed up.
And finally, it is important to improve employee and team skills for evidence-based care. It is very difficult to give staff time for training, but it is also important that institutions keep on training care teams. New, cost-effective methods of training must be developed.
In conclusion, major improvements in the health care industry will require not only engineering solutions, but also cultural changes in health care delivery organizations.
REFERENCES
Advisory Board Company. 2001. The New Economics of Care. Washington, D.C.: The Advisory Board Company.
Sahney, V.K. 2003. Generating Management Research on Improving Quality. Accepted for publication in Health Care Management Review.
Womack, J.P., D.T. Jones, and D. Roos. 1990. The Machine That Changed the World. New York: Maxwell MacMillan International.
























