9
The Health Status and Health Behaviors of Hispanics
José J. Escarce, Leo S. Morales, and Rubén G. Rumbaut
The rapid growth in the Hispanic population, and especially in the number of Hispanic youth, represents one of the most dramatic and important demographic trends affecting the United States. Contemporary working-age Hispanic adults will age to become the first sizable wave of Hispanic seniors. More consequential, the large number of contemporary Hispanic children and adolescents will age to swell the ranks of Hispanic young and middle-aged adults within a decade or two. The health status and health behaviors of today’s Hispanic youth will play a central role in shaping the long-term health and health care needs not only of Hispanics in the United States but also of all Americans.
Efforts to provide a detailed and comprehensive description of the health and health behaviors of Hispanics are complicated by a variety of factors. Hispanics living in the United States represent an increasing diversity of national-origin groups. Relatively new groups, including Dominicans, Salvadorans, Guatemalans, and Colombians, have grown rapidly, adding their numbers to well-established populations of Mexican, Puerto Rican, and Cuban origin. The available information suggests that health status differs across national-origin groups. In addition, the health of U.S. Hispanics differs by generational status. On numerous dimensions, foreign-born Hispanics—i.e., immigrants to the United States—have better health indicators than their U.S.-born counterparts. Among the foreign-born, moreover, health status and health behaviors may differ by degree of acculturation to American culture.
In this context, the gaps in the available data on the health and health
behaviors of Hispanics impose serious limitations. One frequent and noteworthy problem is the lack of detailed data for subgroups of Hispanics defined by national origin and generation in the United States. Most studies group Hispanics into a single category or focus on Hispanics of Mexican origin, who are by far the most numerous. Another problem is the relative lack of detailed epidemiological data on the incidence and prevalence of common and important diseases, such as cardiovascular disease. Moreover, for many conditions, data are unavailable to assess incidence or prevalence according to immigrant status or, among the foreign-born, by length of residence in the United States and degree of acculturation.
Despite these limitations, researchers have learned a great deal about the health status and health behaviors of Hispanics over the past 25 years. The story that has emerged is a complex one, with some findings that warrant optimism and others that merit serious concern. The picture of both advantage and disadvantage that has surfaced must be appreciated and understood in order to develop interventions and design policies to improve Hispanic health.
In this chapter, we provide an overview of the health status and health behaviors of Hispanics in the United States. The chapter is divided into sections, as follows. The next section discusses mortality rates among Hispanics and compares them with rates for non-Hispanic whites and non-Hispanic blacks. This section also illustrates the variation in mortality across Hispanic national-origin groups. The three sections that follow cover, in order, the health status and health behaviors of Hispanic adults, the health status and health behaviors of Hispanic children and adolescents, and birth outcomes. The sixth section discusses the so-called epidemiological paradox, one of the most fascinating findings regarding the health of Hispanics and a source of controversy since it was first described. Finally, we conclude with a summary of our findings and what they mean for the health and health care needs of future generations of Hispanics in the United States.
Our objective is not to be comprehensive. Rather, our goal is to summarize research findings that have an especially strong bearing on future trends in Hispanic health. Accordingly, a major portion of the chapter is devoted to reviewing selected aspects of the health and health behaviors of Hispanic children and adolescents. We have chosen today’s Hispanic youth as a major focus because their health has enormous implications for the future health and health care needs of all Americans.
MORTALITY
As Table 9-1 shows, Hispanics in the United States have lower age-adjusted mortality rates than both non-Hispanic whites and non-Hispanic
TABLE 9-1 Mortality Rates per 100,000 Persons for Non-Hispanic Whites, Non-Hispanic Blacks, and Hispanics, and for Hispanic National-Origin Groups, by Age and Gender, 2001
|
Males |
Non-Hispanic Whites |
Non-Hispanic Blacks |
All Hispanics |
Mexicans |
Puerto Ricans |
Cubans |
Other Hispanics |
|
All ages, age adjusted |
1012.8 |
1393.7 |
802.5 |
779.0 |
1029.1 |
— |
747.6 |
|
Under 1 year |
611.6 |
1484.2 |
624.4 |
50.0 |
— |
— |
865.5 |
|
1–4 years |
33.8 |
55.1 |
33.8 |
33.7 |
— |
— |
35.3 |
|
5–14 years |
18.6 |
28.6 |
16.6 |
16.5 |
20.3 |
— |
5.8 |
|
15–24 years |
105.1 |
186.2 |
111.5 |
115.2 |
127.0 |
58.6 |
99.0 |
|
25–34 years |
131.5 |
267.9 |
118.0 |
111.4 |
183.4 |
94.7 |
122.9 |
|
35–44 years |
241.6 |
456.3 |
208.5 |
189.0 |
373.2 |
199.7 |
202.2 |
|
45–54 years |
502.6 |
1014.6 |
443.9 |
396.6 |
767.3 |
428.0 |
440.4 |
|
55–64 years |
1136.3 |
2055.4 |
923.9 |
882.1 |
1424.5 |
1010.4 |
763.4 |
|
65–74 years |
2869.4 |
4218.9 |
2242.6 |
2228.9 |
2671.7 |
1849.0 |
2333.0 |
|
75–84 years |
6851.5 |
8426.8 |
5258.0 |
5262.6 |
— |
— |
— |
|
85 years and over |
17055.3 |
16576.2 |
12888.3 |
— |
— |
— |
— |
|
Females |
|||||||
|
All ages, age adjusted |
713.5 |
925.5 |
544.2 |
536.2 |
667.6 |
450.6 |
649.6 |
|
Under 1 year |
496.4 |
1217.8 |
518.9 |
490.5 |
— |
— |
584.0 |
|
1–4 years |
26.3 |
43.6 |
27.2 |
27.6 |
— |
— |
27.6 |
|
5–14 years |
13.9 |
19.3 |
12.7 |
13.4 |
12.4 |
— |
10.6 |
|
15–24 years |
41.9 |
56.8 |
33.7 |
32.2 |
40.7 |
— |
36.1 |
|
25–34 years |
60.9 |
122.4 |
45.2 |
39.0 |
80.7 |
— |
49.9 |
|
35–44 years |
134.9 |
285.7 |
97.0 |
88.9 |
170.0 |
100.3 |
87.2 |
|
45–54 years |
291.0 |
591.5 |
226.7 |
214.2 |
317.0 |
08.7 |
216.2 |
|
55–64 years |
723.5 |
1238.2 |
543.0 |
538.3 |
45.9 |
427.3 |
494.4 |
|
65–74 years |
1864.1 |
2653.0 |
1408.0 |
1550.1 |
1345.2 |
1140.9 |
1274.3 |
|
75–84 years |
4777.3 |
5645.1 |
3589.8 |
3759.9 |
— |
3047.2 |
3112.5 |
|
85 years and over |
14670.6 |
13951.4 |
11300.5 |
9989.8 |
— |
— |
— |
|
SOURCE: Arias et al. (2003). |
|||||||
blacks (Arias, Anderson, Hsiang-Ching, Murphy, and Kochanek, 2003). In 2001, the age-adjusted death rate for Hispanic men was 802.5 per 100,000 persons, compared with 1012.8 for white men and 1393.7 for black men. The age-adjusted death rate for Hispanic women was 544.2 per 100,000, compared with 713.5 for white women and 925.5 for black women. The mortality advantage of Hispanics in comparison with whites is present
throughout most of the age range, although the advantage grows at older ages. However, Hispanic infants and men ages 15 to 24 have slightly higher death rates than their white counterparts. It is worth noting that vital statistics data may understate mortality for Hispanics due to underidentification of Hispanic ethnicity on death certificates (Rosenberg et al., 1999). We discuss this in greater detail later in the chapter.
Mortality rates differ among Hispanic groups defined by national origin (Table 9-1). Men of Mexican origin and other Hispanic men have lower death rates than men of Puerto Rican origin. (An age-adjusted death rate was unavailable for Cuban men.) Women of Cuban origin have the lowest death rates, followed by Puerto Rican and other Hispanic women; women of Mexican origin have the highest death rates. Notably, all Hispanic groups except Puerto Rican men have lower age-adjusted death rates than non-Hispanic whites. For certain national-origin groups, death rates also differ by nativity, with the foreign-born having lower rates than the U.S.-born.
The two leading causes of death are heart disease and cancer among Hispanics, non-Hispanic whites, and non-Hispanic blacks (Table 9-2). Beyond the top two causes, however, the leading causes of death differ. In particular, homicide, chronic liver disease and cirrhosis, and conditions originating in the perinatal period are among the 10 leading causes of death for Hispanics, but not for whites. The age-adjusted death rate from homicide among Hispanic men was 11.8 per 100,000 persons in 2000, more than three times the rate of 3.6 for non-Hispanic white men (National Center for Health Statistics, 2003). In fact, homicide is responsible for the higher death rate among Hispanic men ages 15 to 24. Both alcohol use and chronic hepatitis infection contribute to the high death rates from chronic liver disease and cirrhosis among Hispanics (Caetano and Galvan, 2001; Vong and Bell, 2004).
The finding that age-adjusted mortality is lower for Hispanics than for non-Hispanic whites, despite the fact that Hispanics have lower socioeconomic status, is at the core of the “epidemiological paradox.” This phenomenon, and its relationship to the finding of a mortality advantage for Hispanic immigrants from certain countries relative to their U.S.-born peers, is discussed in detail later in the chapter.
THE HEALTH AND HEALTH BEHAVIORS OF HISPANIC ADULTS
We begin with a discussion of the health status and health behaviors of Hispanic adults. We review data on common chronic conditions, including diabetes, hypertension, cardiovascular disease, and cancer; on activity limitations caused by chronic conditions; and on biological risk factors for chronic disease, including lipid levels and obesity. We also summarize the available information concerning mental health as well as relevant research
TABLE 9-2 Leading Causes of Death for Non-Hispanic Whites, Non-Hispanic Blacks, and Hispanics, by Sex, 2000
|
Racial or Ethnic Groups/Sex/Cause of Death |
Number of Deaths |
|
Non-Hispanic whites |
|
|
Men |
|
|
All causes |
1,007,191 |
|
Diseases of heart |
301,551 |
|
Malignant neoplasms |
247,403 |
|
Cerebrovascular diseases |
54,938 |
|
Chronic lower respiratory diseases |
54,816 |
|
Unintentional injuries |
53,329 |
|
Diabetes mellitus |
26,009 |
|
Influenza and pneumonia |
25,002 |
|
Suicide |
21,293 |
|
Chronic liver disease and cirrhosis |
15,002 |
|
Nephritis, nephrotic syndrome and nephrosis |
14,385 |
|
Women |
|
|
All causes |
1,064,096 |
|
Diseases of heart |
320,168 |
|
Malignant neoplasms |
232,608 |
|
Cerebrovascular diseases |
89,642 |
|
Chronic lower respiratory diseases |
58,024 |
|
Alzheimer’s disease |
32,936 |
|
Influenza and pneumonia |
32,912 |
|
Diabetes mellitus |
29,552 |
|
Unintentional injuries |
29,263 |
|
Nephritis, nephrotic syndrome and nephrosis |
15,213 |
|
Septicemia |
14,088 |
|
Non-Hispanic blacks |
|
|
Men |
|
|
All causes |
145,184 |
|
Diseases of heart |
36,740 |
|
Malignant neoplasms |
32,817 |
|
Unintentional injuries |
8,531 |
|
Cerebrovascular diseases |
8,026 |
|
Homicide |
6,482 |
|
Human immunodeficiency virus (HIV) disease |
5,400 |
|
Diabetes mellitus |
4,771 |
|
Chronic lower respiratory diseases |
4,238 |
|
Nephritis, nephrotic syndrome and nephrosis |
3,074 |
|
Influenza and pneumonia |
2,915 |
|
Women |
|
|
All causes |
140,642 |
|
Diseases of heart |
40,783 |
|
Malignant neoplasms |
29,128 |
|
Cerebrovascular diseases |
11,195 |
|
Diabetes mellitus |
7,250 |
|
Racial or Ethnic Groups/Sex/Cause of Death |
Number of Deaths |
|
Nephritis, nephrotic syndrome and nephrosis |
3,837 |
|
Unintentional injuries |
3,746 |
|
Chronic lower respiratory diseases |
3,369 |
|
Septicemia |
3,341 |
|
Influenza and pneumonia |
3,075 |
|
HIV disease |
2,448 |
|
Hispanics |
|
|
Men |
|
|
All causes |
60,172 |
|
Diseases of heart |
13,566 |
|
Malignant neoplasms |
11,138 |
|
Unintentional injuries |
6,696 |
|
Cerebrovascular diseases |
2,865 |
|
Diabetes mellitus |
2,507 |
|
Homicide |
2,431 |
|
Chronic liver disease and cirrhosis |
2,312 |
|
Suicide |
1,525 |
|
HIV disease |
1,493 |
|
Chronic lower respiratory diseases |
1,451 |
|
Women |
|
|
All causes |
47,082 |
|
Diseases of heart |
12,253 |
|
Malignant neoplasms |
10,022 |
|
Cerebrovascular diseases |
3,322 |
|
Diabetes mellitus |
2,821 |
|
Unintentional injuries |
2,134 |
|
Influenza and pneumonia |
1,322 |
|
Chronic lower respiratory diseases |
1,238 |
|
Certain conditions originating in the perinatal period |
951 |
|
Chronic liver disease and cirrhosis |
875 |
|
Nephritis, nephrotic syndrome and nephrosis |
841 |
|
SOURCE: National Center for Health Statistics (2003). |
|
findings on health behaviors, including diet, cigarette smoking, alcohol consumption, and illicit drug use. Our focus on chronic conditions and biological and behavioral risk factors for chronic disease stems from our goal of assessing the dimensions of health status and health behaviors that have the greatest implications for the long-term health of Hispanics in the United States. For comparative purposes, the available data on Hispanics is contrasted principally with non-Hispanic whites and whenever possible among the major Hispanic national-origin groups and between foreign-born and U.S.-born Hispanics. We will also highlight the role of acculturation when the data allow.
Chronic Conditions
Diabetes Mellitus
The term “diabetes” refers to a group of diseases characterized by abnormal metabolism of glucose (sugar) and elevated blood glucose levels. Diabetes is one of the most common chronic conditions in the United States, and its prevalence is increasing (Harris, 1998). There are two types of diabetes. Type 1 diabetes is caused by an absolute deficiency of insulin and usually begins in childhood or early adulthood. Type 2 diabetes is caused by either reduced or increased insulin secretion coupled with insulin resistance and accounts for 90 to 95 percent of all cases of diabetes.
Compared with non-Hispanic whites, Hispanics have higher rates of Type 2 diabetes and other manifestations of abnormal glucose metabolism. For example, using data from the Hispanic Health and Nutrition Examination Survey (HHANES, 1982–1984), Flegal et al. (1991) found that 3.8 percent of Hispanics of Mexican origin who were 20 to 44 years old and 23.9 percent of Hispanics of Mexican origin who were 45 to 74 years old had diabetes, compared with 2.4 percent and 15.8 percent of Hispanics of Cuban origin and 4.1 percent and 26.1 percent of Puerto Ricans, respectively. The prevalence of diabetes for non-Hispanic whites was 1.6 percent for 20- to 44-year-olds and 12.0 percent for 45- to 74-year-olds.
Using more recent data from the Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994), Harris et al. (1998a) found that the age-adjusted rate of diabetes was 13.8 percent for adults of Mexican origin and 7.3 percent for non-Hispanic white adults. Diabetes prevalence was higher for Mexicans than for non-Hispanic whites throughout the age range. Hispanics of Mexican origin also had higher rates than whites of impaired fasting glucose and impaired glucose tolerance, both of which indicate abnormal glucose metabolism and are frequent precursors of diabetes (Harris et al., 1998a).
Complications of diabetes include heart disease, blindness, kidney disease, and peripheral nervous system damage. Studies to assess the risk of developing diabetes complications among Hispanics have yielded conflicting results. For example, Harris et al. (1998b) found that people of Mexican origin with diabetes were more likely than non-Hispanic whites to develop diabetic retinopathy, which can lead to blindness, whereas other investigators have concluded that Hispanics are no different from other ethnic groups with regard to their risk of diabetic complications (Luchsinger, 2001). Notably, Harris et al. (1999) found worse glycemic control (i.e., control of blood sugar levels) among Hispanic adults with Type 2 diabetes compared with non-Hispanic whites.
Due to the higher prevalence of diabetes in Hispanics, the burden of
complications attributable to diabetes is greater for Hispanics than for other groups. The health consequences of diabetes for Hispanics are also reflected in data on cause-specific mortality. Thus, in 2000 the age-adjusted rate of death from diabetes for Hispanics was 36.9 per 100,000 people, compared with 21.8 for non-Hispanic whites (National Center for Health Statistics, 2003). The number of years of potential life lost before age 75 per 100,000 people was 215.6 for Hispanics and 150.2 for non-Hispanic whites (National Center for Health Statistics, 2003). (The number of years of potential life lost is calculated by assuming that everyone would live to age 75.)
Hypertension
Hypertension, or chronic elevation of arterial blood pressure, is a major risk factor for heart disease and stroke. Previous reviews have concluded that the prevalence of hypertension in Hispanics is no greater than among non-Hispanic whites and may be lower (Pérez-Stable, Juarbe, and Moreno, 2001; Ramírez, 1996). However, data from the National Health and Nutrition Examination Surveys suggest that, while rates of hypertension were once lower among Hispanics than among non-Hispanic whites, these rates are now similar.
Using the HHANES (1982–1984) and NHANES II (1976–1980), Pappas, Gergen, and Carroll (1990) found lower age-adjusted rates of hypertension among Hispanic adults who were younger than 75 years old than among non-Hispanic whites. Specifically, age-adjusted rates of hypertension were 22.9 percent, 19.7 percent, and 20.5 percent for men of Mexican, Puerto Rican, and Cuban origin, respectively, compared with 32.6 percent for non-Hispanic white men. Similarly, age-adjusted rates of hypertension were 19.7 percent, 18.0 percent, and 13.8 percent for Mexican, Puerto Rican, and Cuban women compared with 25.3 percent for non-Hispanic white women. By contrast, NHANES III (1988–1994) and NHANES IV (1999–2000) found similar rates of hypertension among people of Mexican origin and non-Hispanic whites. The most recent data from NHANES IV found age-adjusted rates of hypertension of 30.6 percent and 25.0 percent, respectively, for adult men and women of Mexican origin who were less than 75 years old. The corresponding rates for non-Hispanic white men and women were 28.8 percent and 24.5 percent, respectively (National Center for Health Statistics, 2003). Hypertension is also common among elderly Hispanics. For example, analyses of the 1994 Hispanic Established Populations for the Epidemiologic Study of the Elderly investigation found that 61 percent seniors of Mexican origin had hypertension (Stroup-Benham, Markides, Espino, and Goodwin, 1999). The growing prevalence of hypertension in Hispanics—especially Hispan-
ics of Mexican origin—could be due to the obesity epidemic that disproportionately affects this population, as we discuss later in the chapter.
Several studies have documented undertreatment of hypertension and poor blood pressure control in hypertensive Hispanics compared with non-Hispanic whites (Pappas et al., 1990; Satish, Stroup-Benham, Espino, Markides, Goodwin, 1998; Sudano and Baker, 2001). Adequate control of hypertension reduces the risk of stroke, coronary artery disease, congestive heart failure, and cardiovascular death.
Cardiovascular Disease
Cardiovascular disease, including ischemic heart disease and cerebrovascular disease, is the leading cause of death for all ethnic groups in the United States. The main risk factors include diabetes, hypertension, obesity, elevated low-density lipoprotein (LDL) cholesterol, low levels of high-density lipoprotein (HDL) cholesterol, and smoking. As discussed in earlier sections of this chapter, Hispanics have higher rates of diabetes and obesity than non-Hispanic whites. However, Hispanics have similar rates of hypertension and similar cholesterol profiles when compared with non-Hispanic whites, although Hispanics are less likely than whites to have their blood pressure controlled. Hispanics also have lower rates of smoking than non-Hispanic whites, as we discuss later on.
Few data are available on the epidemiology of ischemic heart disease among Hispanics. Studies have found both higher and lower prevalence and incidence of acute myocardial infarction among Hispanics of Mexican origin compared with non-Hispanic whites (Goff et al., 1997; Mitchell, Hazuda, Haffner, Patterson, and Stern, 1991; Rewers et al., 1993). Analyses of death certificate data suggest that mortality rates from heart disease are lower for Hispanics than for non-Hispanic whites (e.g., Liao et al., 1997; Sorlie, Backlund, Johnson, and Rogot, 1993). For example, vital statistics data for 2000 indicate that the age-adjusted death rate from heart disease among Hispanics was 196.0 per 100,000 people, compared with 255.5 per 100,000 people among non-Hispanic whites, while the age-adjusted death rate from ischemic heart disease among Hispanics was 153.2 per 100,000 people, compared with 186.6 per 100,000 people among non-Hispanic whites (National Center for Health Statistics, 2003). However, mortality rates based on vital statistics data have several limitations, including incomplete ascertainment of deaths and misclassification of cause of death or ethnicity (Pandey, Labarthe, Goff, Chan, and Nichaman, 2001). Studies that have validated the cause of death have yielded conflicting findings. Analyses of data from the Corpus Christi Heart Project found higher ischemic heart disease mortality in Hispanics of Mexican origin than in whites, especially among women (Pandy et al., 2001). A study based on
data from the San Luis Valley Diabetics Study found similar ischemic heart disease mortality in both ethnic groups (Swenson et al., 2002). The controversy about how heart disease mortality in Hispanics compares with that in whites remains unsettled, and data from regional studies may not be generalizable.
Data on the incidence and prevalence of stroke in Hispanics also are scarce. In the Northern Manhattan Stroke Study, a population-based incidence study in the New York City area, the rates of stroke for Hispanics of all ages were twice as high as the rates for non-Hispanic whites (Jacobs, Boden-Albala, Lin, and Sacco, 2002; Sacco et al. 1998). (In this study, most of the Hispanics were presumably Puerto Ricans and Dominicans.) Several studies have found that Hispanics, including Hispanics in New York and in New Mexico, have a higher incidence than non-Hispanic whites of intracerebral hemorrhage (Bruno, Carter, Qualls, and Nolte, 1996; Frey, Jahnke, and Bulfinch, 1998; Sacco et al., 1998), suggesting an important role for uncontrolled hypertension. However, Hispanics and non-Hispanic whites have similar death rates after both ischemic and hemorrhagic stroke (Ayala et al., 2001).
In 2000, the age-adjusted death rates from strokes was 46.4 per 100,000 people for Hispanics and 59.0 per 100,000 people for non-Hispanic whites (National Center for Health Statistics, 2003). Interestingly, relative mortality rates from cerebrovascular disease vary by age. For people under age 65, Hispanics have higher mortality than non-Hispanic whites, whereas Hispanics older than age 65 have lower mortality than non-Hispanic whites in the same age group (Gillum, 1995; National Center for Health Statistics, 2003). Hispanics lost 207.8 potential years of life before age 75 from stroke, compared with 183.0 years for non-Hispanic whites.
Cancer
Cancer is a leading cause of death in all racial and ethnic groups. Registry data indicate that Hispanics experience overall lower cancer incidence rates than do non-Hispanic whites. Incidence rates are also lower among Hispanics for several major cancers, including cancer of the breast, lung, prostate, and colon and rectum. However, Hispanics have higher rates than non-Hispanic whites of certain cancers, including cervical and stomach cancer (Ramírez and Suárez, 2001).
Cancer mortality reflects differences in cancer incidence rates. In 2000, the age-adjusted death rate from cancer was 134.9 per 100,000 people among Hispanics, compared with 200.6 per 100,000 people among non-Hispanic whites. Hispanics also had lower mortality rates than non-Hispanic whites from cancers of the lung, breast, prostate, and colon and rectum. In addition, Hispanics lost fewer potential years of life before age
75 from cancer than non-Hispanic whites (1,098.2 versus 1,668.4 years of life lost per 100,000 people) (National Center for Health Statistics, 2003).
Activity Limitations from Chronic Conditions
Hispanics in general are less likely than non-Hispanic whites and non-Hispanic blacks to report activity limitations caused by chronic conditions. In 2001, the age-adjusted proportion of Hispanics reporting an activity limitation was 10.6 percent, compared with 12.1 percent for whites and 15.5 percent for blacks (National Center for Health Statistics, 2003). However, Hispanic seniors age 65 or older have higher rates of activity limitations and disability than their white counterparts (e.g., Markides and Rudkin, 1995).
Biological Risk Factors for Chronic Disease
Cholesterol Levels
Cholesterol levels are associated with the development of cardiovascular disease. Regional data from the 1980s indicate that Hispanics of Mexican origin had less favorable lipid profiles than non-Hispanic whites (e.g., Haffner, Stern, Hazuda, Rosenthal, and Knapp, 1986; Mitchell, Stern, Haffner, Hazuda, and Patterson, 1990). However, more recent data suggest that cholesterol levels for Hispanics are generally similar to those for non-Hispanic whites.
Pérez-Stable et al. (2001) summarized several studies based on the HHANES data. These studies found that total cholesterol levels were similar for men and women of Mexican, Puerto Rican, and Cuban origin, and that the levels for Hispanics compared favorably with those for non-Hispanic whites. More recent data from NHANES III and NHANES IV show similar or more favorable total cholesterol levels for men and women of Mexican origin compared with non-Hispanic whites. For instance, in NHANES IV the age-adjusted total cholesterol level for adult Mexican men less than 75 years old was 207 mg/dl, compared with 204 mg/dl for non-Hispanic white men. The age-adjusted total cholesterol level for Mexican women was 198 mg/dl, compared with 206 mg/dl for non-Hispanic white women (National Center for Health Statistics, 2003).
Lipoprotein fractions are generally similar for Hispanics of Mexican origin and non-Hispanic whites, although there are a few differences. Using NHANES III, Sundquist, Winkleby, and Pudaric (2001) found that the prevalence of high non-DL cholesterol (> 155 mg/dl) was 69 percent in Mexican-origin Hispanics age 65 or older, identical to the prevalence of 70
percent in whites. The prevalence of low-HDL cholesterol (< 40 mg/dl) was similar in Mexican-origin and white men of all ages. However, nearly one-half of Mexican-origin women between ages 20 and 64 had low HDL cholesterol levels, compared with less than 40 percent of white women (Park et al., 2003). Earlier data from HHANES found that Puerto Ricans were more likely than Mexicans or Cubans to have high-LDL and low-HDL cholesterol (Pérez-Stable et al., 2001).
Obesity
Overweight, defined as a body mass index (BMI) of 25 or more, and obesity, defined as a BMI of 30 or more, have reached epidemic proportions in the United States. The age-adjusted prevalence of obesity in the U.S. population rose from 22.9 percent in the early 1990s to 30.5 percent in 2000 (Flegal, Carroll, Ogden, and Johnson, 2002). Obesity increases the risk of diabetes, hypertension, cardiovascular disease, and premature mortality.
The rates of overweight and obesity have increased among Hispanics as well, and they remain higher in Hispanics than in non-Hispanic whites. For example, in NHANES III, 20.6 percent of adult men and 33.3 percent of adult women of Mexican origin were obese, compared with 19.9 percent and 22.7 percent of non-Hispanic white men and women, respectively. In the early waves of data from NHANES IV, 29.3 percent of men and 37.9 percent of women of Mexican origin were obese, compared with 27.2 percent and 30.3 percent of non-Hispanic white men and women (National Center for Health Statistics, 2003). Men and women of Mexican origin are also more likely than whites to be overweight.
Self-reported height and weight are less accurate than the actual measures obtained in NHANES. Nonetheless, self-reports from the 1997–2002 National Health Interview Survey (NHIS) allow us to compare rates of overweight and obesity across Hispanic national-origin groups. The data in Table 9-3 for Hispanics of Mexican origin and for non-Hispanic whites are consistent with the patterns observed in NHANES III and NHANES IV. The table also shows that rates of obesity are higher among Hispanics of Mexican or Puerto Rican origin than among Hispanics of Cuban origin and other Hispanics. In fact, the rates of obesity (BMI > 30) are similar for Cubans, other Hispanics, and whites, although the rates of overweight (BMI 25 to 30) are higher among Cubans and other Hispanics than among whites.
Table 9-4 reports data from 1997–2002 NHIS on rates of overweight and obesity among working-age Hispanics by sex, national origin, and nativity. For Hispanic men and women of Mexican origin and for other
TABLE 9-3 Body Mass Index by National Origin and Age
|
National Origin and Age (years) |
Body Mass Index |
||
|
< 25 (%) |
25–30 (%) |
> 30 (%) |
|
|
All Hispanics |
|||
|
18–44 |
41 |
38 |
21 |
|
45–64 |
28 |
44 |
29 |
|
> 64 |
36 |
44 |
20 |
|
Mexican |
|||
|
18–44 |
37 |
40 |
23 |
|
45–64 |
23 |
45 |
33 |
|
> 64 |
33 |
45 |
22 |
|
Puerto Rican |
|||
|
18–44 |
40 |
35 |
25 |
|
45–64 |
29 |
41 |
30 |
|
> 64 |
34 |
43 |
23 |
|
Cuban |
|||
|
18–44 |
49 |
37 |
14 |
|
45–64 |
29 |
47 |
24 |
|
> 64 |
42 |
40 |
18 |
|
Other Hispanics |
|||
|
18–44 |
47 |
37 |
16 |
|
45–64 |
35 |
43 |
22 |
|
> 64 |
40 |
44 |
16 |
|
Non-Hispanic whites |
|||
|
18–44 |
51 |
32 |
16 |
|
45–64 |
37 |
40 |
24 |
|
> 64 |
44 |
38 |
18 |
|
SOURCE: 1997–2002 NHIS. |
|||
Hispanics, rates of obesity are higher for the U.S.-born than for the foreign-born. However, the findings for Hispanics of Cuban and Puerto Rican origin do not follow this pattern.
Recently, abdominal obesity, defined as a waist circumference of 102 centimeters (39.8 inches) or greater in men and 88 centimeters (34.3 inches) or greater in women, has been recognized as a risk factor for hypertension and abnormalities in glucose metabolism and lipid levels (Okosun, Liao, Rotimi, Prewitt, and Cooper, 2000; Okosun, Prewitt, and Cooper, 1999). In NHANES IV, men of Mexican origin had lower rates than non-Hispanic white men of abdominal obesity (35.5 versus 39.3 percent), whereas women of Mexican origin had higher rates of abdominal obesity than non-Hispanic white women (62.1 versus 53.6 percent). Nonetheless, temporal trends in abdominal obesity are ominous, especially for Mexican men. Between 1988 and 2000, the rate of abdominal obesity increased by 5.5 percentage points
TABLE 9-4 Body Mass Index for Hispanic Working-Age Adults By Sex, National Origin, and Nativity
|
National Origin and Nativity |
Body Mass Index |
|||||
|
Men |
Women |
|||||
|
< 25 (%) |
25–30 (%) |
± > 30 (%) |
< 25 (%) |
25–30 (%) |
± > 30 (%) |
|
|
All Hispanics |
||||||
|
Foreign-born |
31 |
51 |
18 |
44 |
35 |
21 |
|
U.S.-born |
29 |
46 |
26 |
44 |
31 |
26 |
|
Mexican |
||||||
|
Foreign-born |
30 |
51 |
19 |
40 |
37 |
23 |
|
U.S.-born |
26 |
46 |
28 |
39 |
32 |
29 |
|
Puerto Rican |
||||||
|
Foreign-born |
29 |
44 |
27 |
39 |
35 |
27 |
|
U.S.-born |
29 |
44 |
27 |
45 |
29 |
26 |
|
Cuban |
||||||
|
Foreign-born |
29 |
50 |
21 |
41 |
41 |
18 |
|
U.S.-born |
43 |
43 |
14 |
58 |
24 |
18 |
|
Other Hispanics |
||||||
|
Foreign-born |
34 |
51 |
15 |
53 |
32 |
16 |
|
U.S.-born |
32 |
47 |
21 |
51 |
30 |
19 |
|
SOURCE: 1997–2002 NHIS. |
||||||
among men of Mexican origin, while it declined slightly among Mexican women (Okosun et al., 2003).
Abdominal obesity is also a component of the “metabolic syndrome,” which is a strong risk factor for cardiovascular disease and includes impaired glucose tolerance, elevated blood pressure, elevated triglyceride levels, elevated levels of LDL cholesterol, and low levels of HDL cholesterol in addition to abdominal obesity. Using NHANES III, Ford, Giles, and Dietz (2002) found that Hispanics of Mexican origin had the highest age-adjusted prevalence of the metabolic syndrome (31.9 percent) of any racial or ethnic group. Mexican-origin women are more likely than non-Hispanic white or black women to have the metabolic syndrome, even after controlling for predisposing factors such as BMI, alcohol consumption, physical activity, and carbohydrate intake (Park et al., 2003).
Mental Health
Studies conducted since the 1980s have provided valuable information regarding the mental health of Hispanics in the United States. Early studies
relied on standardized survey instruments to measure psychiatric symptoms and estimate “caseness” rates, defined as the proportion of persons with sufficient symptoms to indicate a need for treatment. The results of these studies were inconsistent (Vega and Alegría, 2001). However, a potential problem with these studies was that symptom scales measure transient or acute psychological distress rather than chronic psychiatric disorders using formal diagnostic criteria.
Later studies conducted in the 1980s were population studies that attempted to estimate the prevalence of psychiatric disorders, such as major depression, using diagnostic criteria derived from the Diagnostic and Statistical Manual of Mental Disorders (DSM). Three studies used the Diagnostic Interview Schedule: HHANES (Moscicki, Rae, Regier, and Locke, 1987), the Epidemiological Catchment Area study in Los Angeles (LAECA) (Burnam, Hough, Karno, Escobar, and Telles, 1987; Karno and Hough, 1987), and a study in Puerto Rico (Canino et al., 1987). These studies found that the rates of lifetime major depression among Mexicans in the Southwest (4.2 percent) and in Los Angeles (4.9 percent), Puerto Ricans on the island (4.6 percent), and Cubans in Miami (3.9 percent) were lower than those among non-Hispanic whites in Los Angeles (8.4 percent) or Puerto Ricans in the Northeast (8.9 percent). Moreover, in Los Angeles the rate for lifetime major depression among Mexican immigrants (3.3 percent) was about half the rate for the U.S.-born of Mexican origin (6.3 percent). Other psychiatric disorders were also more prevalent among U.S.-born Hispanics of Mexican origin and mainland-born Puerto Ricans than among Mexican immigrants and Puerto Ricans on the island.
Similarly, a 1995–1996 survey of adults of Mexican origin ages 18 to 59 in Fresno County, California, used the World Health Organization’s Composite International Diagnostic Interview to estimate the rates of psychiatric disorders, permitting comparisons of rates of found in California with both the general U.S. population (as estimated by the National Comorbidity Study) and with survey results in Mexico City (Alderete, Vega, Kolody, and Aguilar-Gaxiola, 2000). The Fresno study reported lower rates of psychiatric disorders for immigrants than for U.S.-born Hispanics of Mexican origin; moreover, immigrants with fewer years in the United States had lower rates than those with longer duration of residence. In turn, the lower rates for recent immigrants were similar to those reported in Mexico City, whereas U.S.-born persons of Mexican origin had similar total lifetime rates as the general U.S. population.
The findings of these studies have raised intriguing questions about the role of acculturation in mental health among Hispanic adults in the United States. Vega and Alegría (2001) have interpreted the data to suggest that some Hispanics, such as Mexicans, Puerto Ricans, and Cubans, generally migrate to the United States with better mental health status than the U.S.
population as a whole. As they spend time in the United States, however, they develop an increased risk of mental health problems.
Health Behaviors
Diet
Studies of dietary intake patterns among non-Hispanic white and Hispanic adults have yielded a variety of interesting and sometimes conflicting findings. Data from NHANES III show that total energy intake was similar for non-Hispanic whites and Hispanics of Mexican origin. Total fat intake was higher among white men than among men of Mexican origin, but similar for white and Mexican-origin women. Dietary cholesterol intake was lower among white adults than among adults of Mexican origin (McDowell et al., 1994). In a community-based study of low-income adults and children, Winkleby, Albright, Howard-Pitney, Lin, and Fortmann (1994) found that, compared with non-Hispanic white adults, Hispanic adults consumed diets with less total fat, less saturated fat, more carbohydrates, and similar amounts of protein. By contrast, the San Antonio Heart Study found that men of Mexican origin consumed more saturated fat than white men. It is difficult to formulate valid generalizations regarding diet owing to the variety of complex, possibly regional influences on food preferences and on the ability to secure different types of food (e.g., Horowitz, Colson, Hebert, and Lancaster, 2004).
There is little research comparing dietary habits among Hispanic national-origin groups. In one study using HHANES data, Hispanics of Mexican origin had higher total fat and saturated fat intake than did Puerto Ricans or Cubans (Loria et al., 1995). Older Puerto Rican and Cuban adults met population guidelines for reducing chronic disease risk more often than any other group.
Multiple studies have shown that acculturation affects the dietary intake of Hispanics. Using data from the NHANES III, Dixon, Sundquist, and Winkleby (2000) found that Mexican immigrants met the recommended dietary guidelines or nutrient intakes more often than Hispanics of Mexican origin born in the United States. Winkleby et al. (1994) reported a graded relationship between acculturation and the intake of foods high in fat, including red meat, cheese, cured meats, and fried foods. In a study of Hispanics in rural Washington state, Neuhouser, Thompson, Coronado, and Solomon (2004) found that less acculturated Hispanics ate more fruits and vegetables and less fat than highly acculturated Hispanics and non-Hispanic whites.
Smoking
Hispanics have one of the lowest rates of cigarette smoking among racial and ethnic groups in the United States, and smoking prevalence has decreased during the past 10 to 15 years for most Hispanic subgroups (Marin, 2001). Moreover, the available data suggest that Hispanics smokers smoke fewer cigarettes per day than do non-Hispanic whites (Marin, 2001).
As shown in Table 9-5, data from the 1997–2002 NHIS are consistent with these patterns, although there are marked variations among Hispanic national-origin groups. The table shows that working-age Hispanics of Mexican origin and other Hispanics smoke at considerably lower rates than whites. Young adults (adults ages 18 to 44) of Cuban origin also have lower smoking rates than whites, whereas Puerto Ricans of all ages smoke at rates similar to those of whites. Consistent with these findings, Guendelman and
TABLE 9-5 Current Smoking by National Origin and Age
|
National Origin and Age (years) |
% Current Smokers |
|
All Hispanics |
|
|
18–44 |
20.2 |
|
45–64 |
20.2 |
|
> 64 |
9.9 |
|
Mexican |
|
|
18–44 |
18.5 |
|
45–64 |
19.4 |
|
> 64 |
9.9 |
|
Puerto Rican |
|
|
18–44 |
31.9 |
|
45–64 |
25.0 |
|
> 64 |
10.4 |
|
Cuban |
|
|
18–44 |
23.5 |
|
45–64 |
23.5 |
|
> 64 |
10.7 |
|
Other Hispanics |
|
|
18–44 |
18.6 |
|
45–64 |
18.4 |
|
> 64 |
9.2 |
|
Non-Hispanic whites |
|
|
18–44 |
30.8 |
|
45–64 |
25.1 |
|
> 64 |
10.6 |
|
SOURCE: 1997–2002 NHIS. |
|
TABLE 9-6 Current Smoking by Hispanic Working-Age Adults, By Sex, National Origin, and Nativity
|
National Origin and Nativity |
% Current Smokers |
|
|
Men |
Women |
|
|
All Hispanics |
||
|
Foreign-born |
24 |
10 |
|
U.S.-born |
29 |
19 |
|
Mexican |
||
|
Foreign-born |
23 |
8 |
|
U.S.-born |
27 |
16 |
|
Puerto Rican |
||
|
Foreign-born |
29 |
21 |
|
U.S.-born |
39 |
28 |
|
Cuban |
||
|
Foreign-born |
32 |
19 |
|
U.S.-born |
26 |
17 |
|
Other Hispanics |
||
|
Foreign-born |
21 |
9 |
|
U.S.-born |
26 |
22 |
|
SOURCE: 1997–2002 NHIS. |
||
Abrams (1994) reported that, among women of childbearing age, those of Mexican origin were less likely than white women to smoke.
Table 9-6 presents data on smoking by sex, national origin, and nativity from the 1997–2002 NHIS. The table shows that men and women born in Mexico, Puerto Rico, or other Hispanic countries are less likely than their U.S.-born counterparts to smoke. The difference in smoking rates between the foreign-born and the U.S.-born is especially marked among women of Mexican origin and other Hispanic women. In fact, smoking rates for foreign-born men of Mexican or other Hispanic origin are more than twice as high as the rates for their female counterparts, whereas the sex gap is much smaller for the U.S.-born in these national-origin groups. This pattern is not found among Hispanics of Cuban origin.
Other Health Behaviors
Hispanic men and women are less likely to drink alcohol than their non-Hispanic white counterparts. For example, in 2001, 61 percent of adult Hispanic men and 39 percent of Hispanic women reported being
current drinkers, compared with 72 percent and 64 percent of white men and women, respectively (National Center for Health Statistics, 2003). Similar, Hispanics are slightly less likely than whites to use illicit drugs (National Center for Health Statistics, 2003).
Studies have shown a link between increasing acculturation and alcohol and drug use (e.g., Amaro, Whitaker, Coffman, and Heeren, 1990; Vega and Amaro, 1994). For example, in HHANES, marijuana use was five to eight times higher among highly acculturated Hispanics of Mexican origin and Puerto Ricans than among those who were not acculturated, controlling for other demographic factors. Other studies have documented adverse effects of acculturation among Hispanic groups with respect to cocaine use and alcohol consumption. The LAECA study in the 1980s found higher prevalence rates of drug abuse or dependence among U.S.-born Hispanics of Mexican origin than among Mexican immigrants, and among the latter, prevalence rates increased with longer residence in the United States (Burnam et al., 1987).
Studies have also reported adverse effects of acculturation among Hispanics of Mexican origin with respect to alcohol consumption (Gilbert, 1989; Markides, Krause, and Mendes de León, 1998), with the most pronounced effects found in women. Recently immigrated Mexican women have very low rates of alcohol abuse or dependence, but the prevalence of any alcohol abuse or dependence among U.S.-born women of Mexican origin is approximately five times greater than for immigrant women. Among men, the prevalence rate is approximately two times greater for the U.S.-born than for immigrants. Whereas in the general U.S. population heavy drinking and alcohol-related social problems tend to peak at ages 18 to 29 and to decline thereafter, these problems continue among Mexican-origin men in the United States at older ages.
Recent research has focused on the co-occurrence of alcohol, drug, and psychiatric disorders not related to substance use meeting DSM diagnostic criteria for mood disorder, anxiety disorder, or antisocial personality disorder. One study with a sample of Mexican-origin adults in central California (Vega, Sribney, and Achara-Abrahams, 2003) found that the prevalence of substance use disorders, consisting of alcohol or drug abuse or dependence, was highest among U.S.-born males (36 percent), followed by U.S.-born females (18 percent), immigrant males (17 percent), and immigrant females (2 percent). The prevalence of mood disorders ranged from a high of 22 percent among U.S.-born Mexican-origin women, to 15 percent for U.S.-born men, 9 percent for immigrant women, and a low of 7 percent for immigrant men. The study found co-occurring lifetime rates of alcohol or other drug disorder with nonsubstance-use psychiatric disorders of 12 percent for the U.S.-born and 3 percent for immigrants.
THE HEALTH AND HEALTH BEHAVIORS OF HISPANIC YOUTH
As discussed in the introduction to this chapter, Hispanic children and adolescents represent the largest and most rapidly growing minority group of youth in the United States. Youth of Mexican origin are by far the largest single national-origin group of Hispanic youth, numbering about 8 million and accounting for 62 percent of all Hispanic children and adolescents. Youth of Puerto Rican origin number nearly 1 million, accounting for 8 percent of Hispanic youth, while youth of Cuban origin number approximately 270,000 and account for 2 percent of Hispanic children and adolescents. Taken together, youth of Dominican, Central American, and South American origin number 1.5 million and account for 12 percent of Hispanic children and adolescents.
In this section, we review the data on the health status and health behaviors of Hispanic children and adolescents. We begin by summarizing the available information on two important chronic conditions—asthma and diabetes—and several other disorders that affect the well-being of Hispanic youth. We then discuss risk factors for chronic disease, including overweight, which is occurring in epidemic proportions among Hispanic youth and poses an enormous threat to the long-term health of Hispanics in the United States. Finally, we review the available data on the mental health of Hispanic youth.
Health Conditions
Diabetes
Type 1 diabetes accounts for the vast majority of cases of diabetes in childhood. The available information on the incidence of Type 1 diabetes among Hispanic youth is based on reports from individual cities. Puerto Rican children in Philadelphia have been reported to have higher incidence rates than non-Hispanic whites (Lipman, 1993; Lipman, Chang, and Murphy, 2003), whereas Hispanic children of Mexican origin in Southern California have been reported to have lower rates than whites (Gay et al., 1989; Lorenzi, Cagliero, and Schmidt, 1985). Hispanics in Chicago have been reported to have higher death rates from Type 1 diabetes than whites (Lipton, Good, Mikhailov, Freels, and Donoghue, 1999).
Historically, Type 2 diabetes has been exceedingly infrequent in childhood. However, although national data are lacking, several case reports point to the rising prevalence of Type 2 diabetes among Hispanic children. A research group in California reported that among low-income diabetic Hispanic children treated between 1990 and 1994, 31 percent had Type 2 diabetes (Neufeld, Raffel, Landon, Chen, and Vadheim, 1998). A pediatric research group in Florida reported that the proportion of patients with
Type 2 diabetes among all newly diagnosed cases of diabetes increased from 9.4 to 20 percent between 1994 and 1998. Hispanic ethnicity was an important risk factor for Type 2 diabetes in this cohort (Macaluso et al., 2002). Another study reported an annual average increase of 9 percent per year in the prevalence of early Type 2 diabetes among Hispanic and non-Hispanic black children between 1985 and 1994 (Keenan et al., 2000). The rising prevalence of Type 2 diabetes in minority children has been a topic of several recently published literature reviews (Dabelea, Pettitt, Lee Jones, and Arslanian, 1999; Fagot-Campagna, 2000; Rosenbloom, Joe, Young, and Winter, 1999). Lower levels of physical activity combined with unhealthy diets have been identified as important underlying causes for rising rates of overweight and diabetes in Hispanic children and adolescents (Gordon-Larsen, Adair, and Popkin, 2002; Gordon-Larsen, Harris, Ward, and Popkin, 2003).
Asthma
Asthma affects a disproportionate number of Hispanic children. In one large study of East Coast families, the percentage of families with at least one asthmatic child was 25 percent for Hispanics (mainly Puerto Rican), 18 percent for non-Hispanic blacks, and 10 percent for non-Hispanic whites (Beckett, Belanger, Gent, Holford, and Leaderer, 1996). Asthma affects different national-origin groups of Hispanic children unequally. Nearly two-thirds of the half million Hispanic children with asthma are Puerto Rican, and Puerto Rican children have the highest prevalence of asthma (11 percent) of any racial or ethnic group in the United States (Carter-Pokras and Gergen, 1993). By contrast, only 3 percent of children of Mexican origin and 5 percent of children of Cuban origin have asthma (Carter-Pokras and Gergen, 1993). In a study of asthma in New York City, Puerto Rican children had a significantly higher prevalence of asthma than Dominicans or other Hispanics living in the same buildings (Ledogar, Penchaszadeth, Iglesias Garden, and Garden Acosta, 2000). The reasons for such dramatic differences in asthma prevalence across national-origin groups remain unclear. On one hand, it has been suggested that Puerto Rican children may have a genetic predisposition to asthma not shared by other racial and ethnic groups in the United States (Flores and Zambrana, 2001); on the other hand, the social context of Puerto Ricans in the United States differs in multiple ways from that of other Hispanic groups.
Oral Health
Poor oral health is associated with a variety of adverse health outcomes in children and adolescents, including lower quality of life, poor nutritional
status, and worse educational outcomes (Mouradian, Wehr, and Crall, 2000). In NHANES III, 34.9 percent of 2- to 5-year-olds and 37.2 percent of 6- to 17-year-old youth of Mexican origin had untreated caries, compared with 14.4 and 18.9 percent of non-Hispanic white youth, respectively (National Center for Health Statistics, 1999). Migrant and rural Hispanic children are at especially high risk for poor oral health and low rates of restored teeth. Among migrant Hispanic children ages 5 to 14, the mean proportion of teeth with carious surfaces is 65 percent compared with 17 percent for schoolchildren in the United States, and only 20 percent of Hispanic children in rural areas have restored dental surfaces compared with 76 percent of schoolchildren nationwide (National Institute of Dental Research, 1989). There is little information available about oral health in Hispanic children other than those of Mexican origin.
Lead Poisoning
Lead poisoning is the most common environmental health problem among children in the United States (Flores and Zambrana, 2001). High blood lead levels are associated with learning disabilities and impaired cognitive development. Lead exposure is a serious problem among Hispanic children living in the United States. Using NHANES III data, Morales, Gutierrez, and Escarce (2005) found that 6, 4, and 2 percent of youth of Mexican origin ages 1 to 4, 5 to 11, and 12 to 17, respectively, had blood lead levels exceeding 10 μg/dL, the current threshold for intervention. In addition, 29, 19, and 12 percent of these age groups, respectively, had blood lead levels exceeding 5 μg/dL, which is being considered by the Centers for Disease Control and Prevention as a new threshold based on recent data on the neuropsychiatric effects of low lead levels. A study using data from Florida found that the prevalence of elevated blood lead levels, defined as exceeding 10 μg/dL, was nearly three times higher among Hispanic than among non-Hispanic 2-year-olds (Hopkins, Quimbo, and Watkins, 1995). A potential source of lead exposure is traditional remedies used by immigrant parents (Flores and Zambrana, 2001).
Risk Factors for Chronic Disease
Risk of Overweight and Overweight
Risk of overweight and overweight have become major health problems for Hispanic youth in the United States. Data from three NHANES surveys since the mid-1970s indicate that the prevalence of overweight (defined as BMI > 95th percentile for age and sex) among youth of Mexican origin has grown dramatically over the last 25 years (Figure 9-1). Between
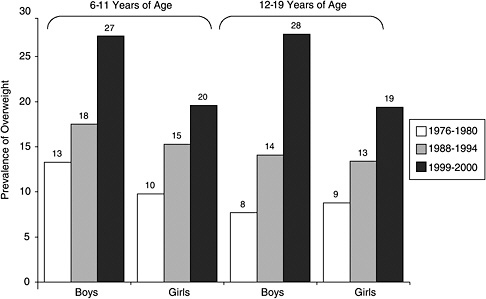
FIGURE 9-1 Time trends in overweight among children and adolescents of Mexican origin, 1976 to 2000.
SOURCE: National Center for Health Statistics (2003).
1976–1980 and 1999–2000 the prevalence of overweight in Mexican-origin youth rose from 13 to 27 percent for boys ages 6 to 11, from 10 to 20 percent for girls ages 6 to 11, from 8 to 28 percent for boys ages 12 to 19, and from 9 to 19 percent for girls ages 12 to 19 (National Center for Health Statistics, 2003). Current rates of overweight for girls of Mexican origin are nearly twice as high as rates for non-Hispanic white girls, and rates for Mexican-origin boys are more than twice as high as rates for white boys (National Center for Health Statistics, 2003). Strauss and Pollack (2001) confirmed the rapid rise in overweight among Hispanic youth using data from the National Longitudinal Survey of Youth. Using data from NHANES IV, Ogden, Flegal, Carroll, and Johnson (2002) found that 39 percent of boys and girls of Mexican origin ages 6 to 11 and 44 percent of boys and girls ages 12 to 19 were at risk of overweight (defined as BMI > 85th percentile). The same study found that only 26 percent of white boys and girls ages 6 to 11 and 27 percent of white boys and girls ages 12 to 19 were at risk of overweight.
Previous studies have found that nativity is associated with risk of overweight and overweight among Hispanic children and adolescents. For example, in an analysis of data from the National Longitudinal Study of Adolescent Health (Add-Health), which includes a nationally representa-
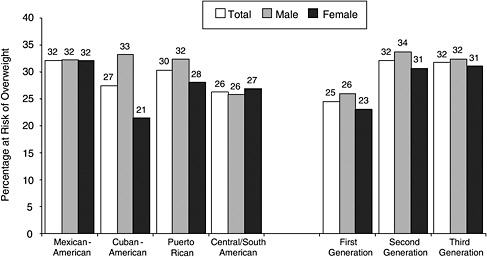
FIGURE 9-2 Risk of overweight among Hispanic adolescents by national-origin group and generational status.
SOURCE: Popkin and Udry (1998).
tive sample of adolescents in grades 7 to 12, Popkin and Udry (1998) found that second- and third-generation Hispanic adolescents were more likely to be at risk of overweight (defined as BMI > 85th percentile) than their first-generation counterparts. And 26 percent of first-generation adolescent boys and 23 percent of first-generation adolescent girls were at risk of overweight, compared with 33 percent of second- and third-generation boys and 31 percent of second- and third-generation girls (Figure 9-2). They also found significant differences across Hispanic national-origin groups. Thus adolescents of Mexican and Puerto Rican origin were the most likely to be at risk of overweight, while Cuban girls and boys and girls of Central American or South American origin had lower rates (Figure 9-2).
Gordon-Larsen et al. (2003) used the Add-Health data to analyze the association between measures of acculturation, such as language spoken at home, duration of residence in the United States, and the proportion of foreign-born neighbors, on one hand, and overweight and overweight-related behaviors, on the other. They found that acculturation was associated with rates of overweight among first-generation adolescents of Mexican, Puerto Rican, and Cuban origin. However, acculturation was unassociated with rates of overweight in second-generation Hispanic adolescents. Gordon-Larsen et al. (2003) also found rapid acculturation of overweight-related behaviors, such as diet and physical inactivity. Taken together, the studies by Popkin and Udry (1998) and Gordon-Larsen et al. (2003) suggest that measures of acculturation, such as language spoken at
home and length of residence in the United States, capture the critical dimensions of acculturation that affect weight among first-generation Hispanic youth. Among second- and third-generation youth, however, generation per se is a better indicator than other acculturation measures of the behaviors that influence weight.
Childhood obesity has important health consequences in childhood and adulthood. Several studies have found that of childhood obesity persists into adulthood (Rolland-Cachera et al., 1987; Serdula et al., 1993; Siervogel, Roche, Guo, Mukherjee, and Chumlea, 1991), and that the likelihood of obesity in adulthood is greater for obese adolescents (Guo, Roche, Chumlea, Gardner, and Siervogel, 1994). Childhood obesity in Hispanic children is also associated with abnormal glucose metabolism, as manifested by resistance to the glucose-lowering effects of insulin and impaired glucose tolerance (Cruz et al., 2004; Sinha et al., 2002). Insulin resistance and impaired glucose tolerance are intermediate stages in the natural history of Type 2 diabetes (Polonsky, Sturis, and Bell, 1996) and predict the risk of developing diabetes (Edelstein et al., 1997) and cardiovascular disease (Haffner, Stern, Hazuda, Mitchell, and Patterson, 1990). In one study, 28 percent of overweight Hispanic children with a family history of diabetes were found to have impaired glucose tolerance (Goran et al., 2004). Obesity is also associated with other risk factors for atherosclerosis.
Risk Factors for Atherosclerosis
A number of recent studies have documented high levels of risk factors for atherosclerosis and cardiovascular disease among Hispanic youth, and especially among youth of Mexican origin. The risk factors that have been studied include blood pressure, fasting insulin levels, insulin resistance, and lipid levels.
Studies comparing blood pressure in Hispanic and non-Hispanic white children and adolescents have yielded conflicting results. However, several recent reports have found higher average blood pressure in youth of Mexican origin than in white youth. Using NHANES IV, Muntner, He, Cutler, Wildman, and Whelton (2004) found that mean age-adjusted systolic blood pressure was 2.7 mm Hg higher among Mexican-origin boys ages 8 to 17 than among their white peers. Other studies based on small regional samples have similarly found higher blood pressures in children and adolescents of Mexican origin than in white youth (Menard, Park, and Yuan, 1999; Sorof, Lai, Turner, Poffenbarger, and Portman, 2004; Tortolero et al., 1997). Muntner et al. (2004) also found that blood pressure in children and adolescents had increased over the last decade, and that the increase was partially attributable to the rising prevalence of overweight.
Recent studies have documented higher fasting insulin levels and more
frequent indicators of insulin resistance and glucose intolerance among Hispanic than white children and adolescents (Reaven, Nader, Berry, and Hoy, 1998; Shea et al., 2003; Tortolero et al., 1997; Winkleby, Robinson, Sundquist, and Kraemer, 1999). In addition, several researchers have reported that Hispanic youth have higher triglyceride levels and lower levels of HDL cholesterol than white youth (e.g., Reaven et al., 1998; Tortolero et al., 1997). Reaven et al. (1998) found that multiple risk factors for atherosclerosis are more likely to occur together in children of Mexican origin than in white children. The available evidence suggests that the differences between Hispanic and white youth in the prevalence of these risk factors for atherosclerosis are at least partly explained by differences in BMI.
Health Behaviors
Physical Activity
Lower levels of physical activity combined with unhealthy diets have been identified as important underlying causes for rising rates of obesity and diabetes in Hispanic children and adolescents (Gordon-Larsen et al., 2002, 2003). In Add-Health, Hispanic adolescent boys were less likely than white boys to engage in low-intensity bouts of physical activity, and Hispanic adolescent girls were less likely than white girls to engage in both low-intensity and high-intensity physical activity. Hispanic adolescent girls also spent more time than white girls engaged in sedentary activities, such as television watching (Gordon-Larsen et al., 2002).
National health surveys have also found differences between Hispanic and non-Hispanic white children and adolescents in levels of physical activity. Based on data from the 1992 National Health Interview Survey-Youth Risk Behavior Survey, 49 percent of Hispanics ages 12 to 21, compared with 55 percent of non-Hispanic whites, reported vigorous or moderate physical activity lasting at least 20 minutes on at least 3 of 7 days during the preceding week (Surgeon General’s Report on Physical Activity and Health, 1996). Similarly, results from a national school-based survey of students in grades 9 to 12 indicate that 57 percent of Hispanic youth, compared with 67 percent of non-Hispanic white youth, participated in vigorous or moderate physical activity on 3 of 7 days in the preceding week (Surgeon General’s Report on Physical Activity and Health, 1996).
Diet
The existing research suggests that acculturation is associated with worse dietary habits among Hispanics of all ages (Dixon et al., 2000; Guendelman and Abrams, 1995; Schaffer, Velie, Shaw, and Todoroff, 1998;
Siega-Riz and Popkin, 2001). Although few studies have focused on the dietary habits of Hispanic children and adolescents, they tend to show that immigrant children have better dietary habits that their U.S.-born counterparts. For example, in Add-Health, foreign-born adolescents of Mexican origin reported higher intake of rice, beans, fruits, and vegetables and lower intake of fast foods and cheese than their U.S.-born counterparts (Gordon-Larsen et al., 2003). Gordon-Larsen et al. (2003) also found that island-born Puerto Rican adolescents had higher intake of fruits and milk than their mainland-born counterparts, while foreign-born Cuban adolescents had higher fruit intake than their U.S.-born peers.
In a study based on older HHANES data, there were no significant differences in daily intake between foreign-born and U.S.-born Hispanic children ages 2 to 5 (Mendoza and Dixon, 1999). However, among 6- to 11-year-olds, foreign-born children of Mexican origin consumed more bread, vegetables, and fruits and fewer servings of added fat than their U.S.-born peers; no differences were seen between mainland- and island-born Puerto Rican school-age children or between U.S.-born and foreign-born Cuban children (Mendoza and Dixon, 1999). Among adolescents, foreign-born Mexicans consumed more bread, vegetables, and fruits and less added fat than their U.S.-born counterparts; island-born Puerto Rican adolescents consumed less milk and added fat than their U.S.-born counterparts; and foreign-born Cuban adolescents consumed more fruits and vegetables than their U.S.-born peers (Mendoza and Dixon, 1999).
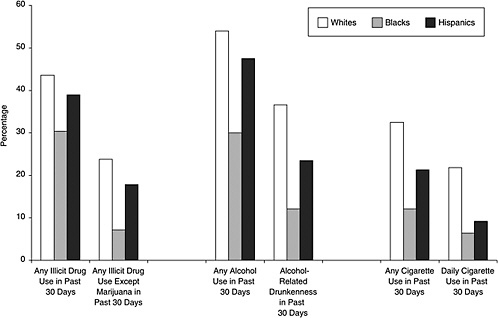
Smoking, Alcohol, and Drugs
Multiple studies have shown high rates of tobacco use, alcohol consumption, and illicit drug among Hispanic adolescents. For example, the Monitoring the Future study found that, in 2002, 39 percent of Hispanic adolescents in twelfth grade reported use of any illicit drug in the past 12 months, 48 percent reported consumption of alcohol in the past 30 days, and 21 percent reported smoking at least one cigarette in the past 30 days (Johnston, O’Malley, and Bachman, 2003). Rates of drug use and alcohol consumption for Hispanics were comparable to those for non-Hispanic whites but higher than for non-Hispanic blacks; smoking rates for Hispanics were lower than for whites but higher than for blacks (Figure 9-3). In an earlier analysis, 25 percent of Hispanic tenth-graders reported heavy drinking and drug use in the last 30 days, a proportion comparable to whites (Johnston, O’Malley, and Bachman, 1998).
In analyses of data for a nationally representative sample of high school seniors, youth of Cuban origin and whites were found to have the highest levels of tobacco, alcohol, and illicit drug use, followed by youth of Mexican origin and youth of Puerto Rican origin. Hispanic youth from
other Latin American countries had low levels of drug use (Wallace et al., 2002). Specifically, 33 percent of Cuban-origin youth reported any illicit drug use in the past 30 days, compared with 26 percent of youth of Mexican or Puerto Rican origin and 19 percent of other Hispanics. And 57 percent of Cuban-origin youth reported smoking in the past 30 days, compared with 51 percent of Mexican-origin youth, 45 percent of Puerto Ricans, and 48 percent of other Hispanics. And 30 percent of Cuban-origin youth reported having a drink in the past 30 days, compared with 26 percent of Mexican-origin youth, 30 percent of Puerto Ricans, and 25 percent of other Hispanics.
Acculturation is associated with higher rates of cigarette smoking, particularly among Hispanic girls (e.g., Casas et al., 1998; Epstein, Botvin, and Díaz, 1998; Gordon-Larsen et al., 2003; Landrine, Richardson, Klonoff, and Flay, 1994), and greater drug use among Hispanic boys and girls (e.g., Blake, Ledsky, Goodenow, and O’Donnell, 2001; Epstein, Botvin, and Díaz, 2001; Gfroerer and Tan, 2003; Kulis, Marsiglia, and Hurdle, 2003). However, the handful of studies that address acculturation and alcohol consumption among Hispanic adolescents have not found a consistent relationship. In some studies acculturation was unassociated with alcohol consumption (Elder et al., 2000), in others more acculturated adolescents were more likely to drink (Brindis, Wolfe, McCarter, Ball, and Starbuck-Morales, 1995; Polednak, 1997), and in still others more acculturated adolescents were less likely to drink (Nielsen and Ford, 2001).
Teenage Childbearing
Hispanic girls have higher rates of teenage childbearing than non-Hispanic white girls. In 2001, 5.8 percent of live births to Hispanic women were to girls younger than age 18, compared with 2.3 percent of births to white women (Martin et al., 2002). Puerto Ricans had the highest proportion of births to girls younger than age 18 (7.4 percent), followed by Mexicans (6.2 percent), Central and South Americans (3.1 percent), and Cubans (2.7 percent). Foreign-born Hispanic mothers from all national-origin groups are much less likely to be teenagers than their U.S.-born peers (Martin et al., 2002).
Mental Health
Studies suggest that Hispanic youth, and especially youth of Mexican origin, have the highest prevalence of depression of any ethnic group (Doi, Roberts, Takeuchi, and Suzuki, 2001; Knight, Virdin, Ocampo, and Roosa, 1994; Roberts and Chen, 1995). A study in Texas found that 31 percent of adolescent girls of Mexican origin had depressive symptoms, compared
with 16 percent of non-Hispanic white girls (Emslie, Weinberg, Rush, Adams, and Rintelmann, 1990). In 1999, 26 percent of Hispanic adolescent girls reported considering suicide, compared with 23 percent of non-Hispanic white adolescent girls (National Center for Health Statistics, 2000), and 20 percent of Hispanic adolescent girls attempted suicide, compared with 9 percent of white adolescent girls (National Center for Health Statistics, 2000). Although injurious suicide attempts were also higher among Hispanic adolescent girls (5 percent) than non-Hispanic whites (2 percent) (National Center for Health Statistics, 2000), Hispanic adolescents complete suicide at lower rates than youth of other ethnic groups (Canino and Roberts, 2000).
Among Hispanics, foreign-born youth experience lower self-esteem and higher levels of suicidal thoughts than U.S.-born youth (e.g., Portes and Rumbaut, 2001). However, U.S.-born Hispanic youth exhibit more serious health risk behaviors and conduct problems than foreign-born youth.
BIRTH OUTCOMES
Hispanic women have higher fertility rates than non-Hispanic white and non-Hispanic black women (Giachello, 2001). For example, in 2001 Hispanics had 96.0 births per 1,000 women ages 15 to 44, compared with 57.7 births for white women and 69.1 births for black women (National Center for Health Statistics, 2003). However, there is enormous variation in fertility across Hispanic national-origin groups. Thus women of Mexican origin have the highest fertility rates of all ethnic groups in the United States, whereas women of Cuban origin have the lowest rates (Giachello, 2001).
Hispanics generally have excellent birth outcomes. In 2001, 6.47 percent of live births to Hispanic mothers were low birthweight (< 2,500 grams) and 1.14 percent were very low birthweight (< 1,500 grams), compared with 6.76 and 1.17 percent, respectively, of live births to non-Hispanic white mothers and 13.07 and 3.08 percent, respectively, of live births to non-Hispanic black mothers. Of the Hispanic national-origin groups, mothers of Mexican origin have the lowest rates of low-birthweight and very-low-birthweight infants and Puerto Rican mothers have the highest rates.
Infant mortality rates are also lower for Hispanic women than for non-Hispanic whites and non-Hispanic blacks (Table 9-7). As with fertility rates and low birthweight births, there is considerable variation in infant mortality rates across Hispanic national-origin groups. Hispanics of Cuban origin have among the lowest infant mortality rates in the United States, and Hispanics of Mexican and Central American or South American origin have low rates as well. By contrast, infants of Puerto Rican mothers have
TABLE 9-7 Infant, Neonatal, and Postneonatal Mortality Rates for Non-Hispanic White, Non-Hispanic Black, and Hispanic Mothers, 2000
relatively high death rates (Table 9-7). The low infant mortality rates for Mexican and Central American women, and especially for immigrant women from these countries, have attracted a great deal of attention because they are unexpected in the context of these women’s low socioeconomic status. These findings are discussed in greater detail in the next section.
THE EPIDEMIOLOGICAL PARADOX
The term “epidemiological paradox” refers to a consistent finding in the research literature that, on certain measures of health, Hispanics in the United States have more favorable indicators than non-Hispanic whites. This finding is considered paradoxical because, as discussed earlier in this volume, Hispanics in the United States have much less favorable socioeconomic profiles than whites. A large body of research has demonstrated a positive, graded relationship between socioeconomic status and health (Adler and Ostrove, 1999; Feinstein, 1993).
There have been numerous studies to confirm and attempt to understand the causes of the epidemiological paradox since it was first described. In this section, we review the evidence for the epidemiological paradox in two main indicators of health: adult mortality and birth outcomes. We also discuss proposed explanations for the epidemiological paradox and how they might apply to adult mortality and birth outcomes.
Adult Mortality
Studies that have compared the mortality experience of Hispanic adults, in the aggregate, and non-Hispanic white adults have consistently found that Hispanics have similar or lower mortality rates after adjusting for age and sex differences in the populations (e.g., Elo and Preston, 1997; Liao et al., 1998; Singh and Siahpush, 2001; Sorlie et al., 1993). These studies also indicate that the Hispanic mortality advantage widens with age. For example, using data from the National Longitudinal Mortality Study (NLMS), Sorlie et al. (1993) found that age-adjusted mortality rates for Hispanic men and women age 45 or older were 18 to 28 percent lower than the rates for their white counterparts; mortality rates were similar for Hispanics and whites ages 25 to 44. Using NLMS data, Elo and Preston (1997) also documented that Hispanic mortality advantage widens after controlling for socioeconomic status. This is unsurprising given the established inverse relationship between socioeconomic status and mortality.
Several studies have attempted to further understanding of the epidemiological paradox by examining mortality differences between Hispanics and non-Hispanic whites by national-origin group or nativity or both (e.g., Abraido-Lanza, Dohrenwend, Ng-Mak, and Turner, 1999; Hummer, Rogers, Amir, Forbes, and Frisbie, 2000; Palloni and Arias, 2004; Singh and Siahpush, 2001; Sorlie et al., 1993). Although the precise findings of these studies differ, in general they suggest that the evidence of an epidemiological paradox in mortality is much stronger for some groups of Hispanics than for others. For instance, Hummer et al. (2000) used the National Health Interview Survey-Multiple Cause of Death (NHIS-MCD) linked data file to examine mortality differences between non-Hispanic whites, on one hand, and Hispanics of Mexican, Puerto Rican, Cuban, Central American or South American, and other Hispanic origin, on the other. They found a sizable mortality advantage for Hispanics of Mexican, Central American or South American, and other Hispanic origin in analyses that controlled for age, sex, and socioeconomic status, but not for Puerto Ricans or Cubans. In addition, they found lower mortality among foreign-born compared with U.S.-born Hispanics. Using the NLMS, Abraido-Lanza et al. (1999) found that Hispanics of Mexican, Puerto Rican, Cuban, and other Hispanic origin all had lower mortality than whites after controlling for age, sex, and socioeconomic status. Among Hispanics of Mexican or other Hispanic origin, moreover, the mortality advantage extended to both the foreign-born and the U.S.-born.
Palloni and Arias (2004) recently published the most detailed analysis to date of mortality differences between Hispanic and non-Hispanic white adults. Using the NHIS-MCD linked data file, these investigators examined mortality over a nine-year period for adults age 35 and older. They found that, controlling for demographic characteristics and socioeconomic status,
only foreign-born men and women of Mexican and other Hispanic origin experienced a mortality advantage when compared with non-Hispanic whites. There were no significant differences in mortality between non-Hispanic whites, on one hand, and either U.S.-born Mexicans, U.S.-born other Hispanics, foreign-born or U.S.-born Puerto Ricans, or foreign-born or U.S.-born Cubans, on the other.
Three explanations have been proposed for the epidemiological paradox in adult mortality. The first explanation attributes the findings to data artifacts. Vital statistics data, in particular, may understate mortality for Hispanics. Mortality rates based on vital statistics data are drawn from two distinct sources. The denominator for the rates is drawn from census data in which individuals self-identify their race and ethnicity; the numerator, by contrast, is drawn from death certificates on which proxy respondents identify the race and ethnicity of decedents. Previous research has shown that Hispanics are underidentified on death certificates, resulting in under-reporting of Hispanic deaths (Rosenberg et al., 1999). Of note, this explanation may apply to both foreign-born and U.S.-born Hispanics. However, it does not affect the NMLS or NHIS-MCD data, in which individuals self-identified their race and ethnicity at baseline and this information was subsequently linked with death certificates.
The second explanation attributes the epidemiological paradox to selective migration in and out of the United States. Proponents of the selective migration explanation have termed selective in- and out-migration the “healthy-migrant effect” and the “salmon-bias effect,” respectively (Abraido-Lanza et al., 1999). The healthy-migrant effect posits that Hispanic migrants are selected from their native populations based on certain traits, including better physical and mental health (Abraido-Lanza et al., 1999; Palloni and Morenoff, 2001). The salmon-bias effect posits that some foreign-born Hispanic subgroups may have a propensity to return to their country of origin following periods of unemployment or poor health (Abraido-Lanza et al., 1999). The net impact of the healthy-migrant and salmon-bias effects is to produce a foreign-born Hispanic population in the United States with a more favorable health profile than non-Hispanic whites. The healthy-migrant and salmon-bias effects may apply to foreign-born Hispanics but not to the U.S.-born. Moreover, the salmon-bias effect is expected to be a factor mainly for immigrants from countries of origin to which return migration is feasible and easy, especially Mexico (Palloni and Arias, 2004).
The third explanation attributes the epidemiological paradox to social and cultural characteristics that differentiate Hispanics from whites, rather than to selection. According to this explanation, Hispanics benefit from protective social and cultural characteristics that operate by positively influencing individual health and lifestyle behaviors, family structure, and
social networks (e.g., Abraido-Lanza et al., 1999; Sorlie et al., 1993). Drawing on this perspective, acculturation research has sought to examine the effects of cultural assimilation on the health of Hispanics as the behavioral and social norms typical of their home culture are replaced by those more typical of the United States. In general, the literature suggests that the effects of acculturation on health behaviors are negative, although these effects depend on the specific behavior and study population under investigation. Protective social and cultural characteristics are expected to exert a stronger effect on the health of foreign-born than U.S.-born Hispanics, since these characteristics are lost with acculturation.
To date, a definitive explanation for the epidemiological paradox in adult mortality remains elusive. In their recent study, Palloni and Arias (2004) claimed to find indirect evidence of a salmon-bias effect to account for the mortality advantage of Mexican immigrants relative to whites, but they could not account for the mortality advantage experienced by the foreign-born of other Hispanic origin. Furthermore, using a variety of indirect tests, they found no evidence of healthy-migrant or acculturation effects. By contrast, Abraido-Lanza et al. (1999) interpreted the results of their mortality analyses as providing no evidence of either a healthy-migrant effect or a salmon-bias effect. Instead, they emphasized the possibility that their findings were due to protective effects of cultural factors. Finally, Jasso, Massey, Rosenzweig, and Smith (2004) interpreted data on health status and life expectancy from a variety of sources as offering strong evidence of a healthy-migrant effect among Hispanic immigrants to the United States.
Birth Outcomes
The epidemiological paradox is also manifested in birth outcomes, including rates of low birthweight and infant mortality. Overall, birth outcomes for Hispanic women are much better than expected given their socioeconomic status. For instance, in 2001 the infant mortality rate (IMR) for Hispanics was 5.4 per 1,000 live births, compared with 5.7 for non-Hispanic whites and 13.5 for non-Hispanic blacks (Mathews, Menacker, and MacDorman, 2003). Among Hispanic national-origin groups, Cubans (4.2) and Central/South Americans (5.0) had the lowest IMRs followed by Mexicans (5.2) and Puerto Ricans (8.5), who were the only group with an IMR above that for whites. Previous studies using regional and national data have consistently found similar results (e.g., Landale, Oropesa, and Gorman, 1999; Williams, Binkin, and Clingman, 1986).
Notably, Hispanic immigrant women have lower IMRs than their U.S.-born peers, despite having lower incomes and educational attainment (Mathews et al., 2003). For example, in 2001, the IMRs for foreign-born and U.S.-born women of Mexican origin were 4.7 and 5.9, respectively.
The IMRs for island-born and mainland-born Puerto Rican women were 7.8 and 8.8, respectively; the IMRs for foreign-born and U.S.-born women of Cuban origin were 3.8 and 4.7, respectively; and the IMRs foreign-born and U.S.-born women of Central American or South American origin were 4.9 and 5.3, respectively.
As with the findings for adult mortality, the main explanations that have been posited for the favorable birth outcomes among Hispanic women include selective migration and protective effects of cultural and social characteristics. To assess the role of selective migration, Weeks, Rumbaut, and Ojeda (1999) compared the pregnancy outcomes of Mexican immigrant women who delivered in San Diego; Mexican women who delivered just across the border in Tijuana, Mexico; U.S.-born women of Mexican origin who delivered in San Diego; and non-Hispanic whites. They found that Mexican women who delivered in Tijuana had the lowest rate of low-birthweight births, and they interpreted this finding as evidence against selective migration to the United States by healthier women or return migration to Mexico by women with poor outcomes.
Evidence for the protective effects of cultural characteristics comes from studies suggesting that acculturation has negative effects on birth outcomes and on behaviors associated with favorable birth outcomes. For example, Guendelman and Abrams (1995) found that immigrant Mexican women of childbearing age had a lower risk of eating a poor diet than U.S.-born women of Mexican origin, whose nutrient intake resembled that of non-Hispanic whites. Using data from the Fragile Families and Child Wellbeing Study, Kimbro, Lynch, and McLanahan (2004) found that nearly 90 percent of immigrant Mexican mothers breastfed their infants, compared with two-thirds of second-generation and just over half of third-generation women of Mexican origin. Additional analyses found that as acculturation (measured using a 7-item scale) increased, the probability of breastfeeding declined. Other studies have found that, compared with Mexican-born women, U.S.-born women are significantly more likely to have diets lower in fruits and cereals and higher in fats and milk products, to smoke, and to abuse drugs and alcohol (Rumbaut and Weeks, 1996, 1998).
CONCLUSIONS
This review of the health and health behaviors of Hispanics in the United States has uncovered several major themes. To begin, the Hispanic population is far from monolithic with respect to these outcomes. Research has documented important differences in health and health behaviors by national origin, nativity and generation, and measures of acculturation. Hispanics of Puerto Rican origin tend to have worse health status indicators than other national-origin groups, including higher mortality and less
favorable birth outcomes. Conversely, Hispanics of Mexican and Central American or South American origin often exhibit favorable health indicators despite low socioeconomic status. Studies have found lower mortality, better birth outcomes, healthier diets, lower rates of overweight and obesity, and other favorable outcomes among foreign-born compared with U.S.-born Hispanics from most national-origin groups.
Within this variation, our review has documented a number of optimistic findings regarding the health and health behaviors of Hispanics. With the exception of Puerto Ricans, Hispanics have lower age-adjusted mortality than non-Hispanic whites. In the context of Hispanics’ low socioeconomic status, this finding is considered so remarkable that it has been called the epidemiological paradox. Research on the epidemiological paradox suggests that the mortality advantage of Hispanics is concentrated among foreign-born Mexicans, Central Americans, and South Americans, and that at least part of the advantage is due to selective migration. Nonetheless, these studies have also found that mortality rates for most U.S.-born Hispanics, in whom selective migration is much less likely to play a role, are at least as favorable as those for non-Hispanic whites.
The other main manifestation of the epidemiological paradox is in birth outcomes. Hispanic women have similar or more favorable birth outcomes, including lower rates of low birthweight and infant mortality, than non-Hispanic white women, again with the exception of Puerto Ricans. As with mortality, the Hispanic advantage in birth outcomes is greater among the foreign-born, but even U.S.-born Hispanic women experience birth outcomes that rival those of whites. Protective cultural and social characteristics of Hispanic immigrants have been invoked to explain the excellent birth outcomes of foreign-born women, but relatively favorable outcomes persist even as these characteristics are lost in the second generation. Although recent studies have furthered our understanding of patterns of mortality and birth outcomes among Hispanics, a full and widely accepted explanation for the epidemiological paradox remains elusive.
Other optimistic findings regarding the health and health behaviors of Hispanic adults include lower incidence rates than whites for several major cancers, relatively low rates of activity limitations (except for seniors), mental health profiles that resemble those of whites, and lower smoking rates than whites. Hispanic adolescents also smoke at lower rates than white adolescents. And with the exception of Puerto Ricans, Hispanic children have low rates of asthma, the major chronic disease of childhood.
Our review has also uncovered a number of worrisome findings regarding the health and health behaviors of Hispanics. Several of these concern Hispanic adults. By far the most ominous findings, however, pertain to Hispanic children and adolescents. In fact, our findings regarding trends in overweight among Hispanic youth raise the possibility of a marked deterio-
ration in the health of the Hispanic population of the United States over the next several decades.
The epidemic of overweight and obesity in the United States has affected all racial and ethnic groups, but Hispanics have been especially hard hit. According to the most recent NHANES data, nearly one-third of adult men and two-fifths of adult women of Mexican origin in the United States are obese. These rates easily surpass the rates for non-Hispanic whites, especially in the case of women, and adult Hispanics are also more likely than whites to be overweight. The rising prevalence of overweight and obesity among Hispanic adults are likely to lead to higher rates of diabetes, hypertension, and cardiovascular disease. Diabetes is nearly twice as frequent among Hispanics of Mexican origin as among whites, and Hispanics bear a higher burden than whites of diabetic complications. The available data suggest that Hispanics of Mexican origin and whites have a similar prevalence of hypertension, but even this is a change from the pattern 25 years ago, when hypertension was considerably less common among Hispanics. Current trends in overweight and obesity raise the likelihood of an aging Hispanic population burdened by much higher rates of cardiovascular disease, stroke, kidney disease, blindness, and other complications of obesity, diabetes, and hypertension. These developments would have major implications for rates of disability and mortality among Hispanics.
Recent changes in the distribution of BMI among Hispanic youth pose an even greater threat to the future health of the Hispanic population of the United States. Hispanic children and adolescents are much more likely than non-Hispanic white children and adolescents to be at risk of overweight or overweight. Moreover, the rate of overweight has been increasing much more rapidly for Hispanic youth than for whites. The most recent data indicate that two-fifths of children of Mexican origin ages 6 to 11 and nearly half of adolescents ages 12 to 19 are at risk of overweight, while more than one-fourth of Mexican-origin boys of all ages and one-fifth of girls are overweight. Although foreign-born Hispanic children and adolescents have lower rates than their U.S.-born peers of risk of overweight and overweight, the rates for foreign-born youth are nonetheless very high.
The health consequences of current trends in BMI for Hispanic youth are already evident. The rising prevalence of Type 2 diabetes among Hispanic children is unprecedented, and portends the future development of diabetic complications in Hispanic adults in much larger numbers and at much younger ages than historical norms. Other consequences of the epidemic in risk of overweight and overweight among Hispanic youth include increasing blood pressure and high rates of insulin resistance, glucose intolerance, and lipid abnormalities. It seems inevitable that the Hispanic population of the United States will experience much higher rates of cardiovas-
cular disease and other manifestations of atherosclerosis as today’s Hispanic youth moves into adulthood.
Unhealthy diets combined with low levels of physical activity are important underlying causes of the rising rates of overweight in Hispanic children and adolescents. In this context, our review has raised serious concerns about the future dietary habits of Hispanics. The available evidence suggests that acculturation is associated with less healthy diets among Hispanics of all ages, and that second-generation Hispanic youth have worse dietary habits than immigrant youth. The process of acculturation is likely to lead today’s immigrant youth to adopt less healthy diets that put them at higher risk of overweight. The second-generation offspring of today’s immigrant adults are likely to be at high risk for unhealthy diets and excessive weight as well.
The other data we have reviewed on the health and health behaviors of Hispanic youth are less worrisome than the data on obesity and its complications. Nonetheless, we uncovered several findings of concern with regard to the well-being of Hispanic youth and especially to their educational performance. Health conditions and behaviors that affect educational performance are noteworthy, because the educational outcomes and attainment of today’s Hispanic youth have important implications for the future economic trajectory of Hispanics in the United States.
Hispanic children and adolescents have considerably worse oral health than their non-Hispanic white peers. Poor oral health is associated with a variety of adverse outcomes among youth, including lower quality of life and worse educational outcomes. Hispanic children also have higher blood lead levels than white children and, consequently, are at much higher risk for the adverse effects of lead poisoning on cognitive development. The Centers for Disease Control and Prevention are currently considering lowering the threshold blood lead level for intervention from 10 μg/dL to 5 μg/dL. More than one-fourth of preschool-age children and one-fifth of elementary schoolchildren of Mexican origin have blood lead levels that would meet the revised threshold. Other threats to the well-being and educational performance of Hispanic youth, and in particular, of adolescent girls, include relatively high rates of depression and teenage childbearing. Finally, the available evidence suggests that the process of acculturation is associated with higher rates of smoking and illicit drug use among Hispanic youth, implying that these may become more salient problems among the second-generation offspring of today’s immigrant adults.
Our review suggests that addressing the rising prevalence of overweight and obesity among Hispanics must be a priority for public health. Hispanic youth, in particular, should be targeted by public health and community-based efforts to prevent overweight before it has a chance to develop. The available data on the relationship between acculturation and both over-
weight and diet suggest that interventions to help Hispanic families preserve the dietary habits that they bring with them from their countries of origin could have an important role to play. However, although Hispanics have been disproportionately affected by the epidemic of overweight and obesity in the United States, no racial or ethnic group is unscathed. Hispanics must be included in broader societal initiatives to address this epidemic.
Other health problems that disproportionately affect Hispanic youth and that may be amenable to public health and community-based interventions include poor oral health, high blood lead levels, and teenage childbearing. Interventions designed to preserve and build on salutary elements of Hispanic culture may be helpful in dealing with smoking, drug use, and teenage childbearing among Hispanic youth and in promoting favorable birth outcomes among Hispanic women. More research is needed on how acculturation to American culture affects the health and health behaviors of Hispanics and on how interventions that exploit the beneficial elements of Hispanic culture can be designed.
Finally, if present trends continue, the U.S. health care system of the future will be faced with much larger numbers of Hispanic patients suffering from such chronic conditions as diabetes, hypertension, and cardiovascular disease as well as from the consequences of these conditions. Hispanics currently face numerous barriers to receiving timely, appropriate, and high quality health care. These barriers, and what must be done to address them, are discussed in detail in the next chapter.
REFERENCES
Abraido-Lanza, A.F., Dohrenwend, B.P., Ng-Mak, D.S., and Turner, J.B. (1999). The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health, 89(10), 1748–1751.
Adler, N.E., and Ostrove, J.M. (1999). Socioeconomic status and health: What we know and what we don’t. In N.E. Adler, M. Marmot, B.S. McEwen, and J. Stewart (Eds.), Socioeconomic status and health in industrial nations: Social, psychological and biological pathways (pp. 3–16). New York: New York Academy of Sciences.
Alderete, E., Vega, W.A., Kolody, B., and Aguilar-Gaxiola, S. (2000). Lifetime prevalence of and risk factors for psychiatric disorders among Mexican farm workers in California. American Journal of Public Health, 90(4), 608–614.
Amaro, H., Whitaker, R., Coffman, J., and Heeren, T. (1990). Acculturation and marijuana and cocaine use: Findings from HHANES 1982–84. American Journal of Public Health, 80(suppl.), 54–60.
Arias, E., Anderson, R.N., Hsiang-Ching, K., Murphy, S.L., and Kochanek, K.D. (2003). Deaths: Final data for 2001. (National Vital Statistics Reports; Vol. 52, No. 3.) Hyattsville, MD: National Center for Health Statistics.
Ayala, C., Greenlund, K., Croft, J.B., Keenan, N.L., Donehoo, R.S., Giles, W.H., Kittner, S.J., and Marks, J.S. (2001). Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. American Journal of Epidemiology, 154(11), 1057–1063.
Beckett, W.S., Belanger, K., Gent, J.F., Holford, T.R., and Leaderer, B.P. (1996). Asthma among Puerto Rican Hispanics: A multiethnic comparison study of risk factors. American Journal of Respiratory and Critical Care Medicine, 154(4 Pt 1), 894–899.
Blake, S., Ledsky, R., Goodenow, C., and O’Donnell, L. (2001). Recency of immigration, substance use, and sexual behavior among Massachusetts adolescents. American Journal of Public Health, 91, 794–798.
Brindis, C., Wolfe, A.L., McCarter, V., Ball, S., and Starbuck-Morales, S. (1995). The associations between immigrant status and risk-behavior patterns in Latino adolescents. Journal of Adolescent Health, 17(2), 99–105.
Bruno, A., Carter, S., Qualls, C., and Nolte, K.B. (1996). Incidence of spontaneous intracerebral hemorrhage among Hispanics and non-Hispanic whites in New Mexico. Neurology, 47(2), 405–408.
Burnam, M.A., Hough, R.L., Karno, M., Escobar, J.I., and Telles, C.A. (1987). Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health and Social Behavior, 28(March), 89–102.
Caetano, R., and Galvan, F.H. (2001). Alcohol use and alcohol-related problems among Latinos in the United States. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 383–412). San Francisco, CA: Jossey-Bass.
Canino, G., and Roberts, R.E. (2000). Suicidal behavior among Latino youth. In L. Davidson and U. Loso (Eds.), Suicide prevention now: Linking research to practice (pp. 66–78). Atlanta: Centers for Disease Control.
Canino, G.J., Bird, H.R., Shrout, P.E., Rubio-Stipec, M., Bravo, M., Martinez, R., Sesman, M., and Guevara, L.M. (1987). The prevalence of specific psychiatric disorders in Puerto Rico. Archives of General Psychiatry, 44(8), 727–735.
Carter-Pokras, O.D., and Gergen, P.J. (1993). Reported asthma among Puerto Rican, Mexican-American, and Cuban children, 1982 through 1984. American Journal of Public Health, 83(4), 580–582.
Casas, J.M., Bimbela, A., Corral, C.V., Yanez, I., Swaim, R.C., Wayman, J.C., and Bates, S. (1998). Cigarette and smokeless tobacco use among migrant and nonmigrant Mexican American youth. Hispanic Journal of Behavioral Science, 20(1), 102–121.
Cruz, M.L., Weigensberg, M.J., Huang, T.T., Ball, G., Shaibi, G.Q., and Goran, M.I. (2004). The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. Journal of Clinical Endocrinology and Metabolism, 89(1), 108–113.
Dabelea, D., Pettitt, D.J., Lee Jones, K., and Arslanian, S.A. (1999). Type 2 diabetes mellitus in minority children and adolescents: An emerging problem. Journal of Clinical Endocrinology and Metabolism, 28(4), 709–729.
Dixon, L.B., Sundquist, J., and Winkleby, M. (2000). Differences in energy, nutrient, and food intakes in a U.S. sample of Mexican-American women and men: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Epidemiology, 152(6), 548–557.
Doi, Y., Roberts, R.E., Takeuchi, K., and Suzuki, S. (2001). Multiethnic comparison of adolescent major depression based on the DSM-IV criteria in a U.S.-Japan study. Journal of the American Academy of Child and Adolescent Psychiatry, 40(11), 1308–1315.
Edelstein, S.L., Knowler, W.C., Bain, R.P., Andres, R., Barrett-Connor, E.L., Dowse, G.K., Haffner, S.M., Pettitt, D.J., Sorkin, J.D., Muller, D.C., Collins, V.R., and Hamman, R.F. (1997). Predictors of progression from impaired glucose tolerance to NIDDM: An analysis of six prospective studies. Diabetes, 46(4), 701–710.
Elder, J.P., Campbell, N.R., Litrownik, A.J., Ayala, G.X., Slymen, D.J., Parra-Medina, D., and Lovato, C.Y. (2000). Predictors of cigarette and alcohol susceptibility and use among Hispanic migrant adolescents. Preventive Medicine, 31(2 Pt 1), 115–123.
Elo, I.T., and Preston, S.H. (1997). Racial and ethnic differences in mortality at older ages. In National Research Council, Racial and ethnic differences in the health of older Americans (pp. 10–42). Committee on Population, L. G. Martin and B. J. Soldo (Eds.). Washington, DC: National Academy Press.
Emslie, G.J., Weinberg, W.A., Rush, A.J., Adams, R.M., and Rintelmann, J.W. (1990). Depressive symptoms by self-report in adolescence: Phase I of the development of a questionnaire for depression by self-report. Journal of Child Neurology, 5(2), 114–121.
Epstein, J.A., Botvin, G.J., and Díaz, T. (1998). Linguistic acculturation and gender effects on smoking among Hispanic youth. Preventive Medicine, 27, 583–589.
Epstein, J.A., Botvin, G.J., and Díaz, T. (2001). Linguistic acculturation associated with higher marijuana and polydrug use among Hispanic adolescents. Substance Use and Misuse, 36(4), 477–499.
Fagot-Campagna, A. (2000), Emergence of type 2 diabetes mellitus in children: Epidemiological evidence. Journal of Pediatric Endocrinology and Metabolism, 13(Suppl. 6), 1395–1402.
Feinstein, J.S. (1993). The relationship between socioeconomic status and health: A review of the literature. Milbank Quarterly, 71(2), 279–322.
Flegal, K.M., Carroll, M.D., Ogden, C.L., and Johnson, C.L. (2002). Prevalence and trends in obesity among U.S. adults, 1999–2000. Journal of the American Medical Association, 288(14), 1772–1773.
Flegal, K.M., Ezzati, T.M., Harris, M.I., Haynes, S.G., Juarez, R.Z., Knowler, W.C., Pérez-Stable, E.J., and Stern, M.P. (1991). Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care, 14(7), 628–638.
Flores, G., and Zambrana, R.E. (2001). The early years: The health of children and youth. In C.W. Molina, M. Aguirre-Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 77–106). San Francisco, CA: Jossey-Bass.
Ford, E.S., Giles, W.H., and Dietz, W.H. (2002). Prevalence of the metabolic syndrome among U.S. adults: Findings from the third National Health and Nutrition Examination Survey. Journal of the American Medical Association, 287(3), 356–359.
Frey, J.L., Jahnke, H.K., and Bulfinch, E.W. (1998). Differences in stroke between white, Hispanic, and Native American patients: The Barrow Neurological Institute stroke database. Stroke, 29(1), 29–33.
Gay, E.C., Hamman, R.F., Carosone-Link, P.J., Lezotte, D.C., Cook, M., Stroheker, R., Klingensmith, G., and Chase, H.P. (1989). Colorado IDDM Registry: Lower incidence of IDDM in Hispanics. Comparison of disease characteristics and care patterns in biethnic populations. Diabetes Care, 12(10), 701–708.
Giachello, A.L. (2001). The reproductive years: The health of Latinas. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 107–156). San Francisco, CA: Jossey-Bass.
Gilbert, M. (1989). Alcohol consumption patterns in immigrant and later generation Mexican American women. Hispanic Journal of Behavioral Science, 9, 299–313.
Gillum, R.F. (1995). Epidemiology of stroke in Hispanic Americans. Stroke, 26(9), 1707–1712.
Gfroerer, J.C., and Tan, L.L. (2003). Substance use among foreign-born youths in the United States: Does the length of residence matter? American Journal of Public Health, 93(11), 1892–1895.
Goff, D.C., Nichaman, M.Z., Chan, W., Ramsey, D.J., Labarthe, D.R., and Ortiz, C. (1997). Greater incidence of hospitalized myocardial infarction among Mexican Americans than non-Hispanic whites. The Corpus Christi Heart Project, 1988–1992. Circulation, 95(6), 1433–1440.
Goran, M.I., Bergman, R.N., Avila, Q., Watkins, M., Ball, G.D., Shaibi, G.Q., Weigensberg, M.J., and Cruz, M.L. (2004). Impaired glucose tolerance and reduced beta-cell function in overweight Latino children with a positive family history for type 2 diabetes. Journal of Clinical Endocrinology and Metabolism, 89(1), 207–212.
Gordon-Larsen, P., Adair, L.S., and Popkin, B.M. (2002). Ethnic differences in physical activity and inactivity patterns and overweight status. Obesity Research, 10(3), 141–149.
Gordon-Larsen, P., Harris, K.M., Ward, D.S., and Popkin, B.M. (2003). Acculturation and overweight-related behaviors among Hispanic immigrants to the U.S.: The National Longitudinal Study of Adolescent Health. Social Science and Medicine, 57, 2023–2034.
Guendelman, S., and Abrams, B. (1994). Dietary, alcohol, and tobacco intake among Mexican-American women of childbearing age: Results from HANES data. American Journal of Health Promotion, 8(5), 363–372.
Guendelman, S., and Abrams, B. (1995). Dietary intake among Mexican American women: Generational differences and a comparison with white non-Hispanic women. American Journal of Public Health, 85(1), 20–25.
Guo, S.S., Roche, A.F., Chumlea, W.C., Gardner, J.D., and Siervogel, R.M. (1994). The predictive value of childhood body mass index values for overweight at age 35. American Journal of Clinical Nutrition, 59(4), 810–819.
Haffner, S.M., Stern, M.P., Hazuda, H.P., Rosenthal, M., and Knapp, J.A. (1986, May). The role of behavioral variables and fat patterning in explaining ethnic differences in serum lipids and lipoproteins. American Journal of Epidemiology, 123(5), 830–839.
Haffner, S.M., Stern, M.P., Hazuda, H.P., Mitchell, B.D., and Patterson, J.K. (1990). Cardiovascular risk factors in confirmed prediabetic individuals: Does the clock for coronary heart disease start ticking before the onset of clinical diabetes? Journal of the American Medical Association, 263(21), 2893–2898.
Harris, M.I. (1998). Diabetes in America: Epidemiology and scope of the problem. Diabetes Care, 21(Suppl 3), C11–C14.
Harris, M.I., Flegal, K.M., Cowie, C.C., Eberhardt, M.S., Goldstein, D.E., Little, R.R., Wiedmeyer, H.M., and Byrd-Holt, D.D. (1998a). Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care, 21(4), 518–524.
Harris, M.I., Klein, R., Cowie, C.C., Rowland, M., and Byrd-Holt, D.D. (1998b). Is the risk of diabetic retinopathy greater in non-Hispanic blacks and Mexican Americans than in non-Hispanic whites with type 2 diabetes? A U.S. population study. Diabetes Care, 21(8), 1230–1235.
Harris, M.I., Eastman, R.C., Cowie, C.C., Flegal, K.M., and Eberhardt, M.S. (1999). Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care, 22(3), 403–408.
Hopkins, R.S., Quimbo, R., and Watkins, S.M. (1995). Elevated blood lead prevalence in Florida two-year-olds. Journal of Florida Medical Association, 82, 193–197.
Horowitz, C.R., Colson, K.A., Hebert, P.L., and Lancaster, K. (2004). Barriers to buying healthy foods for people with diabetes: Evidence of environmental disparities. American Journal of Public Health, 94(9), 1549–1554.
Hummer, R.A., Rogers, R.G., Amir, S.H., Forbes, D., and Frisbie, W.P. (2000). Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Social Science Quarterly, 81(1), 459–476.
Jacobs, B.S., Boden-Albala, B., Lin, I.F., and Sacco, R.L. (2002). Stroke in the young in the Northern Manhattan Stroke Study. Stroke, 33, 2789–2790.
Jasso, G., Massey, D.S., Rosenzweig, M.R., and Smith, J.P. (2004). Immigrant health: Selectivity and acculturation. In National Research Council, Critical perspectives on racial and ethnic differences in health in late life (pp. 227–266). Committee on Population,
N.B. Anderson, R.A. Bulatao, and B. Cohen (Eds.). Washington, DC: The National Academies Press.
Johnston, L.D., O’Malley, P.M., and Bachman, J.G. (1998). National survey results on drug use from the Monitoring the Future study, 1975–1997. (NIH Publication No. 98-4345.) Bethesda, MD: National Institute on Drug Abuse.
Johnston, L.D., O’Malley, P.M., and Bachman, J.G. (2003). Monitoring the Future national survey results on adolescent drug use: Overview of key findings, 2002. (NIH Publication No. 03-537). Bethesda, MD: National Institute on Drug Abuse.
Karno, M., and Hough, R.L. (1987). Lifetime prevalence of specific psychiatric disorders among Mexican Americans and non-Hispanic whites in Los Angeles. Archives of General Psychiatry, 44(August), 695–701.
Keenan, H., el Deirawi, K., Walsh, M., Grover, V.V., Alva, E., Onyemere, K., and Lipton, R. (2000). Are trends in diabetes incidence changing for minority children? Annuals of Epidemiology, 10(7), 459.
Kimbro, R.T., Lynch, S.M., and McLanahan, S. (2004). The Hispanic paradox and breastfeeding: Does acculturation matter? Evidence from the fragile families study. (Center for Research on Child Wellbeing Working Paper #04-01.) Princeton, NJ: Princeton University.
Knight, G.P., Virdin, L.M., Ocampo, K.A., and Roosa, M. (1994). An examination of the cross-ethnic equivalence of measures of negative life events and mental health among Hispanic and Anglo-American children. American Journal of Community Psychology, 22(6), 767–783.
Kulis, S., Marsiglia, F.F., and Hurdle, D. (2003). Gender identity, ethnicity, acculturation, and drug use: Exploring differences among adolescents in the Southwest. Journal of Community Psychology, 31(2), 167–188.
Landale, N.S., Oropesa, R.S., and Gorman, B.K. (1999). Immigration and infant health: Birth outcomes of immigrant and native women. In National Research Council and Institute of Medicine, Children of immigrants: Health, adjustment, and public assistance (pp. 244–285). Board on Children, Youth, and Families, D.J. Hernández (Ed.). Washington, DC: National Academy Press.
Landrine, H., Richardson, J.L., Klonoff, E.A., and Flay, B. (1994). Cultural diversity in the predictors of adolescent cigarette smoking: The relative influence of peers. Journal of Behavioral Medicine, 17(3), 331–346.
Ledogar, R.J., Penchaszadeth, A., Iglesias Garden, C.C., and Garden Acosta, L. (2000). Asthma and Latino cultures: Different prevalence reported among groups sharing the same environment. American Journal of Public Health, 90(6), 929–935.
Liao, Y., Cooper, R.S., Cao, G., Kaufman, J.S., Long, A.E., and McGee, D.L. (1997). Mortality from coronary heart disease and cardiovascular disease among adult U.S. Hispanics: Findings from the National Health Interview Survey (1986 to 1994). Journal of the American College of Cardiology, 30(5), 1200–1205.
Liao, Y., Cooper, R.S., Cao, G., Durazo-Arvizu, R., Kaufman, J.S., Luke, A., and McGee, D.L. (1998). Mortality patterns among adult Hispanics: Findings from the NHIS 1986 to 1990. American Journal of Public Health, 88(2), 227–232.
Lipman, T.H. (1993). The epidemiology of type I diabetes in children 0–14 year of age in Philadelphia. Diabetes Care, 16(6), 922–925.
Lipman, T.H., Chang, Y., and Murphy, K.M. (2003). The epidemiology of type 1 diabetes in children in Philadelphia 1990–1994: Evidence of an epidemic. Diabetes Care, 26(1), 260.
Lipton, R., Good, G., Mikhailov, T., Freels, S., and Donoghue, E. (1999). Ethnic differences in mortality from insulin-dependent diabetes mellitus among people less than 25 years of age. Pediatrics, 103(5 Pt 1), 952–956.
Lorenzi, M., Cagliero, E., and Schmidt, N.J. (1985). Racial differences in incidence of juvenile-onset type 1 diabetes: Epidemiologic studies in southern California. Diabetologia, 28(10), 734–738.
Loria, C.M., Bush, T.L., Carroll, M.D., Looker, A.C., McDowell, M.A., Johnson, C.L., and Sempos, C.T. (1995). Macronutrient intakes among adult Hispanics: A comparison of Mexican Americans, Cuban Americans, and mainland Puerto Ricans. American Journal of Public Health, 85(5), 684–689.
Luchsinger, J.A. (2001). Diabetes. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 277–300). San Francisco, CA: Jossey-Bass.
Maculuso, C.J., Bauer, U.E., Deeb, L.C., Malone, L.C., Chaudhari, M., Silverstein, J., Eidson, M., Goldberg, R.B., Gaughan-Bailey, B., Brooks, R.G., and Rosenbloom, A.L. (2002). Type 2 diabetes mellitus among Florida children and adolescents, 1994 through 1998. Public Health Reports, 117(4), 373–379.
Marin, G. (2001). Tobacco use among Latinos. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 413–434). San Francisco, CA: Jossey-Bass.
Markides, K.S., and Rudkin, I. (1995). Health status of Hispanic elderly in the United States. Galveston: University of Texas Medical Branch.
Markides, K.S., Krause, N., and Mendes de León, C.F. (1998). Acculturation and alcohol consumption among Mexican Americans. American Journal of Public Health, 78, 1178–1181.
Martin, J.A., Hamilton, B.E., Ventura, S.J., Menacker, F., Park, M.M., and Sutton, P.D. (2002). Births: Final data for 2001. National Vital Statistics Report, 51(2).
Mathews, T.J., Menacker, F., and MacDorman, M.F. (2003). Infant mortality statistics from the 2001 period linked birth/infant death data set. National Vital Statistics Report, 52(2), 1–28.
McDowell, M.A., Briefel, R.R., Alaimo, K., Bischof, A.M., Caughman, C.R., Carroll, M.D., Loria, C.M., and Johnson, C.L. (1994). Energy and macronutrient intakes of persons ages 2 months and over in the United States: Third National Health and Nutrition Examination Survey, Phase 1, 1988–91. Advance Data (255), 1–24.
Menard, S.W., Park, M.K., and Yuan, C.H. (1999). The San Antonio Biethnic Children’s Blood Pressure Study: Auscultatory findings. Journal of Pediatric Health Care, 13(5), 237–244.
Mendoza, F.S., and Dixon, L.B. (1999). The health and nutritional status of immigrant Hispanic children: Analyses of the Hispanic Health and Nutrition Examination Survey. In National Research Council and Institute of Medicine, Children of immigrants: Health, adjustment, and public assistance (pp. 187–243). Board on Children, Youth, and Families, D.J. Hernández (Ed.). Washington, DC: National Academy Press.
Mitchell, B.D., Stern, M.P., Haffner, S.M., Hazuda, H.P., and Patterson, J.K. (1990). Risk factors for cardiovascular mortality in Mexican Americans and non-Hispanic whites. San Antonio Heart Study. American Journal of Epidemiology, 131(3), 423–433.
Mitchell, B.D., Hazuda, H.P., Haffner, S.M., Patterson, J.K., and Stern, M.P. (1991). Myocardial infarction in Mexican-Americans and non-Hispanic whites. The San Antonio Heart Study. Circulation, 83(1), 45–51.
Morales, L.S., Gutierrez, P., and Escarce, J.J. (2005). Demographic and socioeconomic factors associated with blood lead levels among Mexican-American children and adolescents in the United States. Public Health Reports, 120(4), 448-454.
Moscicki, E.K., Rae, D., Regier, D.A., and Locke, B. (1987). The Hispanic health and nutrition examination survey: Depression among Mexican-Americans, Cuban-Americans, and Puerto Ricans. In M. Gavitia and J.D. Arana (Eds.), Health and behavior: Research
agenda for Hispanics (pp. 145–159). Simon Bolívar Research Monograph Series 1. Chicago: University of Illinois Press.
Mouradian, W.E., Wehr, E., and Crall, J.J. (2000). Disparities in children’s oral health and access to dental care. Journal of the American Medical Association, 284(20), 2625–2631.
Muntner, P., He, J., Cutler, J.A., Wildman, R.P., and Whelton, P.K. (2004). Trends in blood pressure among children and adolescents. Journal of the American Medical Association, 291(17), 2107–2113.
National Center for Health Statistics (NCHS). (1999). Health, United States, 1999, with Health and Aging Chartbook. (Department of Health and Human Services, DHHS Publication No. 1999–1232.) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
National Center for Health Statistics (NCHS). (2000). Health, United States, 2000, with Adolescent Health Chartbook. (Department of Health and Human Services, DHHS Publication No. 2000-1232-1.) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
National Center for Health Statistics (NCHS). (2003). Health, United States, 2003. (Department of Health and Human Services, DHHS Publication No. 2003-1232.) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
National Institute of Dental Research. (1989). Oral health of United States children, the national survey of dental caries in U.S. school children, 1986–87: National and regional findings. (DHHS Publication No. (NIH) 89-2247.) Bethesda, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health.
Neufeld, N.D., Raffel, L.J., Landon, C., Chen, Y.D., and Vadheim, C.M. (1998). Early presentation of type 2 diabetes in Mexican-American youth. Diabetes Care, 21(1), 80–86.
Neuhouser, M.L., Thompson, B., Coronado, G.D., and Solomon, C.C. (2004). Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington state. Journal of the American Diet Association, 104(1), 51–57.
Nielsen, A.L., and Ford, J.A. (2001). Drinking patterns among Hispanic adolescents: Results from a national household survey. Journal of Studies on Alcohol, 62(4), 448–456.
Ogden, C.L., Flegal, K.M., Carroll, M.D., and Johnson, C.L. (2002). Prevalence and trends in overweight among US children and adolescents, 1999–2000. Journal of the American Medical Association, 288(14), 1728–1732.
Okosun, I.S., Prewitt, T.E., and Cooper, R.S. (1999). Abdominal obesity in the United States: Prevalence and attributable risk of hypertension. Journal of Human Hypertension, 13(7), 425–430.
Okosun, I.S., Liao, Y., Rotimi, C.N., Prewitt, T.E., and Cooper, R.S. (2000). Abdominal adiposity and clustering of multiple metabolic syndrome in white, black, and Hispanic Americans. Annuals of Epidemiology, 10(5), 263–270.
Okosun, I.S., Choi, S.T., Boltri, J.M., Parish, D.C., Chandra, K.M., Dever, G.E., and Lucas, A. (2003). Trends of abdominal adiposity in white, black, and Mexican-American adults, 1988 to 2000. Obesity Research, 11(8), 1010–1017.
Palloni, A., and Arias, E. (2004). Paradox lost: Explaining the Hispanic adult mortality advantage. Demography, 41(3), 385–415.
Palloni, A., and Morenoff, J. (2001). Interpreting the paradoxical in the Hispanic paradox: Demographic and epidemiological approaches. Annals of the New York Academy of Sciences, 954, 140–174.
Pandey, D.K., Labarthe, D.R., Goff, D.C., Chan, W., and Nichaman, M.Z. (2001). Community-wide coronary heart disease mortality in Mexican Americans equals or exceeds that
in non-Hispanic whites: The Corpus Christi Heart Project. American Journal of Medicine, 110(2), 81–87.
Pappas, G., Gergen, P.J., and Carroll, M. (1990). Hypertension prevalence and the status of awareness, treatment, and control in the Hispanic Health and Nutrition Examination Survey (HHANES), 1982–84. American Journal of Public Health, 80(12), 1431–1436.
Park, Y.W., Zhu, S., Palaniappan, L., Heshka, S., Carnethon, M.R., and Heymsfield, S.B. (2003). The metabolic syndrome: Prevalence and associated risk factor findings in the U.S. population from the Third National Health and Nutrition Examination Survey, 1988–1994. Archives of Internal Medicine, 163(4), 427–436.
Pérez-Stable, E., Juarbe, T., and Moreno-John, G. (2001). Cardiovascular disease. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Heath issues in the Latino community (pp. 245–276). San Francisco, CA: Jossey-Bass.
Polednak, A.P. (1997). Gender and acculturation in relation to alcohol use among Hispanic (Latino) adults in two areas of the northeastern United States. Substance Use and Misuse, 32(11), 1513–1524.
Polonsky, K.S., Sturis, J., and Bell, G.I. (1996). Seminars in medicine of the Beth Israel Hospital, Boston. Non-insulin-dependent diabetes mellitus: A genetically programmed failure of the beta cell to compensate for insulin resistance. New England Journal of Medicine, 334(12), 777–783.
Popkin, B.M., and Udry, J.R. (1998). Adolescent obesity increases significantly in second and third generation U.S. immigrants. Journal of Nutrition, 128(4), 701–706.
Portes, A., and Rumbaut, R.G. (2001). Legacies: The story of the immigrant second generation. Berkeley and New York: University of California Press and Russell Sage Foundation.
Ramírez, A.G. (1996). Hypertension in Hispanic Americans: Overview of the population. Public Health Reports, 3(Suppl 2), 25–26.
Ramírez, A.G., and Suárez, L. (2001). The impact of cancer on Latino populations. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 211–224). San Francisco: Jossey-Boss.
Reaven, P., Nader, P.R., Berry, C., and Hoy, T. (1998). Cardiovascular disease insulin risk in Mexican-American and Anglo-American children and mothers. Pediatrics, 101(4), 12–18.
Rewers, M., Shetterly, S.M., Hoag, S., Baxter, J., Marshall, J., and Hamman, R.F. (1993). Is the risk of coronary heart disease lower in Hispanics than in non-Hispanic whites? The San Luis Valley Diabetes Study. Ethnic Disparities, 3(1), 44–54.
Roberts, R.E., and Chen, Y.W. (1995). Depressive symptoms and suicidal ideation among Mexican-origin and Anglo adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 34(1), 81–90.
Rolland-Cachera, M.F., Deheeger, M., Guilloud-Bataille, M., Avons, P., Patois, E., and Sempe, M. (1987). Tracking the development of adiposity from one month of age to adulthood. Annals of Human Biology, 14(3), 219–229.
Rosenberg, H.M., Maurer, J.D., Sorlie, P.D., Johnson, N.J., MacDorman, M.F., Hoyert, D.L., Spitler, J.F., and Scott, C. (1999). Quality of death rates by race and Hispanic origin: A summary of current research, 1999. Vital Health Statistics, Series, 2(128). Hyattsville, MD: National Center for Health Statistics.
Rosenbloom, A.L., Joe, J.R., Young, R.S., and Winter, W.E. (1999). Emerging epidemic of type 2 diabetes in youth. Diabetes Care, 22(2), 345–354.
Rumbaut, R.G., and Weeks, J.R. (1996). Unraveling a public health enigma: Why do immigrants experience superior perinatal health outcomes? Research in the Sociology of Health Care, 13, 335–388.
Rumbaut, R.G., and Weeks, J.R. (1998). Children of immigrants: Is Americanization hazardous to infant health? In H.E. Fitzgerald, B.M. Lester, and B. Zuckerman (Eds.), Children of color: Research, health, and public policy issues (pp. 159–183). New York: Garland.
Sacco, R.L., Boden-Albala, B., Gan, R., Chen, X., Kargman, D.E., Shea, S., Paik, M.C., and Hauser, W.A. (1998). Stroke incidence among white, black, and Hispanic residents of an urban community: The Northern Manhattan Stroke Study. American Journal of Epidemiology, 147(3), 259–268.
Satish, S., Stroup-Benham, C.A., Espino, D.V., Markides, K.S., and Goodwin, J.S. (1998). Undertreatment of hypertension in older Mexican Americans. Journal of the American Geriatric Society, 46(4), 405–410.
Schaffer, D.M., Velie, E.M., Shaw, G.M., and Todoroff, K.P. (1998). Energy and nutrient intakes and health practices of Latinas and white non-Latinas in the 3 months before pregnancy. Journal of the American Dietary Association, 98(8), 876–884.
Serdula, M.K., Ivery, D., Coates, R.J., Freedman, D.S., Williamson, D.F., and Byers, T. (1993). Do obese children become obese adults? A review of the literature. Preventive Medicine, 22(2), 167–177.
Shea, S., Aymong, E., Zybert, P., Shamoon, H., Tracy, R.P., Deckelbaum, R.J., and Basch, C.E. (2003). Obesity, fasting plasma insulin, and c-reactive protein levels in healthy children. Obesity Research, 11, 95–103.
Siega-Riz, A.M., and Popkin, B.M. (2001). Dietary trends among low socioeconomic status women of childbearing age in the United States from 1977 to 1996: A comparison among ethnic groups. Journal of American Medical Women’s Association, 56(2), 44–48, 72.
Siervogel, R.M., Roche, A.F., Guo, S.M., Mukherjee, D., and Chumlea, W.C. (1991). Patterns of change in weight/stature from 2 to 18 years: Findings from long-term serial data for children in the Fels longitudinal growth study. International Journal of Obesity, 15(7), 479–485.
Singh, G.K., and Siahpush, M. (2001). All-cause and cause-specific mortality of immigrants and native born in the United States. American Journal of Public Health, 91(3), 392–399.
Sinha, R., Fisch, G., Teague, B., Tamborlane, W.V., Banyas, B., Allen, K., Savoye, M., Rieger, V., Taksali, S., Barbetta, G., Sherwin, R.S., and Caprio, S. (2002). Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. New England Journal of Medicine, 346(11), 802–810.
Sorlie, P.D., Backlund, E., Johnson, N.J., and Rogot, E. (1993). Mortality by Hispanic status in the United States. Journal of American Medical Association, 270(20), 2464–2468.
Sorof, J.M., Lai, D., Turner, J., Poffenbarger, T., and Portman, R.J. (2004). Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics, 113(3 Pt 1), 475–482.
Strauss, R.S., and Pollack, H.A. (2001). Epidemic increase in childhood overweight, 1986–1998. Journal of American Medical Association, 286(22), 2845–2848.
Stroup-Benham, C.A., Markides, K.S., Espino, D.V., and Goodwin, J.S. (1999). Changes in blood pressure and risk factors for cardiovascular disease among older Mexican-Americans from 1982–1984 to 1993–1994. Journal of American Geriatric Society, 47(7), 804–810.
Sudano, J.J., Jr., and Baker, D.W. (2001). Antihypertensive medication use in Hispanic adults: A comparison with black adults and white adults. Medical Care, 39(6), 575–587.
Sundquist, J., Winkleby, M.A., and Pudaric, S. (2001). Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: An analysis of NHANES III, 1988–1994. Third National Health and Nutrition Examination Survey. Journal of American Geriatric Society, 49(2), 109–116.
Surgeon General’s Report on Physical Activity and Health. (1996). Available: http://www.cdc.gov/nccdphp/sgr/sgr.htm [accessed March 29, 2004].
Swenson, C.J., Trepka, M.J., Rewers, M.J., Scarbro, S., Hiatt, W.R., and Hamman, R.F. (2002). Cardiovascular disease mortality in Hispanics and non-Hispanic whites. American Journal of Epidemiology, 156(10), 919–928.
Tortolero, S.R., Goff, D.C., Nichaman, M.Z., Labarthe, D.R., Grunbaum, J.A., and Hanis, C.L. (1997). Cardiovascular risk factors in Mexican-American and non-Hispanic white children. Circulation, 96, 418–423.
Vega, W.A., and Alegría, M. (2001). Latino mental health and treatment in the United States. In M. Aguirre-Molina, C.W. Molina, and R.E. Zambrana (Eds.), Health issues in the Latino community (pp. 179–208). San Francisco, CA: Jossey-Bass.
Vega, W.A., and Amaro, H. (1994). Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health, 15, 39–67.
Vega, W.A., Sribney, W., and Achara-Abrahams, I. (2003). Co-occurring alcohol, drug, and other psychiatric disorders among Mexican-origin people in the United States. American Journal of Public Health, 93(7), 1057–1064.
Vong, S., and Bell, B.P. (2004). Chronic liver disease mortality in the United States, 1990–1998. Hepatology, 39(2), 476–483.
Wallace, J.M., Jr., Bachman, J.G., O’Malley, P.M., Johnston, L.D., Schulenberg, J.E., and Cooper, S.M. (2002). Tobacco, alcohol, and illicit drug use: Racial and ethnic differences among U.S. high school seniors, 1976–2000. Public Health Reports, 117(Suppl 1), S67–S75.
Weeks, J.R., Rumbaut, R.G., and Ojeda, N. (1999). Reproductive outcomes among Mexican-origin women in San Diego and Tijuana: Testing the migration selectivity hypothesis. Journal of Immigrant Health, 1(2), 77–90.
Williams, R.L., Binkin, N.J., and Clingman, E.J. (1986). Pregnancy outcomes among Spanish-surname women in California. American Journal of Public Health, 76, 387–391.
Winkleby, M.A., Albright, C.L., Howard-Pitney, B., Lin, J., and Fortmann, S.P. (1994). Hispanic/white differences in dietary fat intake among low educated adults and children. Preventive Medicine, 23(4), 465–473.