4
Effects of Fluoride on Teeth
In this chapter, the committee reviews research on the occurrence of enamel fluorosis at different concentrations of fluoride in drinking water, with emphasis on severe enamel fluorosis and water fluoride concentrations at or near the current maximum contaminant level goal (MCLG) of 4 mg/L and the secondary maximum contaminant level (SMCL) of 2 mg/L. Evidence on dental caries in relation to severe enamel fluorosis, aesthetic and psychological effects of enamel fluorosis, and effects of fluoride on dentin fluorosis and delayed tooth eruption is reviewed as well. Evidence on caries prevention at water concentrations below the SMCL of 2 mg/L is not reviewed. Strengths and limitations of study methods, including issues pertaining to diagnosis and measurement, are considered.
ENAMEL FLUOROSIS
Fluoride has a great affinity for the developing enamel because tooth apatite crystals have the capacity to bind and integrate fluoride ion into the crystal lattice (Robinson et al. 1996). Excessive intake of fluoride during enamel development can lead to enamel fluorosis, a condition of the dental hard tissues in which the enamel covering of the teeth fails to crystallize properly, leading to defects that range from barely discernable markings to brown stains and surface pitting. This section provides an overview of the clinical and histopathological manifestations of enamel fluorosis, diagnostic issues, indexes used to characterize the condition, and possible mechanisms.
Clinical and Histological Features
Enamel fluorosis is a mottling of the tooth surface that is attributed to fluoride exposure during tooth formation. The process of enamel maturation consists of an increase in mineralization within the developing tooth and concurrent loss of early-secreted matrix proteins. Exposure to fluoride during maturation causes a dose-related disruption of enamel mineralization resulting in widening gaps in its crystalline structure, excessive retention of enamel proteins, and increased porosity. These effects are thought to be due to fluoride’s effect on the breakdown rates of matrix proteins and on the rate at which the by-products from that degradation are withdrawn from the maturing enamel (Aoba and Fejerskov 2002).
Clinically, mild forms of enamel fluorosis are evidenced by white horizontal striations on the tooth surface or opaque patches, usually located on the incisal edges of anterior teeth or cusp tips of posterior teeth. Opaque areas are visible in tangential reflected light but not in normal light. These lesions appear histopathologically as hypomineralization of the subsurface covered by a well-mineralized outer enamel surface (Thylstrup and Fejerskov 1978). In mild fluorosis, the enamel is usually smooth to the point of an explorer, but not in moderate and severe cases of the condition (Newbrun 1986). In moderate to severe forms of fluorosis, porosity increases and lesions extend toward the inner enamel. After the tooth erupts, its porous areas may flake off, leaving enamel defects where debris and bacteria can be trapped. The opaque areas can become stained yellow to brown, with more severe structural damage possible, primarily in the form of pitting of the tooth surface.
Enamel in the transitional or early maturation stage of development is the most susceptible to fluorosis (DenBesten and Thariani 1992). For most children, the first 6 to 8 years of life appear to be the critical period of risk. In the Ikeno district of Japan, where a water supply containing fluoride at 7.8 mg/L was inadvertently used for 12 years, no enamel fluorosis was seen in any child who was age 7 years or older at the start of this period or younger than 11 months old at the end of it (Ishii and Suckling 1991). For anterior teeth, which are of the most aesthetic concern, the risk period appears to be the first 3 years of life (Evans and Stamm 1991; Ishii and Suckling 1991; Levy et al. 2002a). Although it is possible for enamel fluorosis to occur when teeth are exposed during enamel maturation alone, it is unclear whether it will occur if fluoride exposure takes place only at the stage of enamel-matrix secretion. Fejerskov et al. (1994) noted that fluoride uptake into mature enamel is possible only as a result of concomitant enamel dissolution, such as caries development. Because the severity of fluorosis is related to the duration, timing, and dose of fluoride intake, cumulative exposure during the entire maturation stage, not merely during critical periods of certain types
of tooth development, is probably the most important exposure measure to consider when assessing the risk of fluorosis (DenBesten 1999).
Mechanisms
Dental enamel is formed by matrix-mediated biomineralization. Crystallites of hydroxyapatite (Ca10(PO4)6(OH)2) form a complex protein matrix that serves as a nucleation site (Newbrun 1986). The matrix consists primarily of amelogenin, proteins synthesized by secretory ameloblasts that have a functional role in establishing and maintaining the spacing between enamel crystallites. Full mineralization of enamel occurs when amelogenin fragments are removed from the extracellular space. The improper mineralization that occurs with enamel fluorosis is thought to be due to inhibition of the matrix proteinases responsible for removing amelogenin fragments. The delay in removal impairs crystal growth and makes the enamel more porous (Bronckers et al. 2002). DenBesten et al. (2002) showed that rats exposed to fluoride in drinking water at 50 or 100 mg/L had lower total proteinase activity per unit of protein than control rats. Fluoride apparently interferes with protease activities by decreasing free Ca2+ concentrations in the mineralizing milieu (Aoba and Fejerskov 2002).
Matsuo et al. (1998) investigated the mechanism of enamel fluorosis in rats administered sodium fluoride (NaF) at 20 mg/kg by subcutaneous injections for 4 days or at 240 mg/L in drinking water for 4 weeks. They found that fluoride alters intracellular transport in the secretory ameloblasts and suggested that G proteins play a role in the transport disturbance. They found different immunoblotting-and-pertussis-toxin-sensitive G proteins on the rough endoplasmic reticulum and Golgi membranes of the germ cells of rats’ incisor teeth.
Health Issues and Clinical Treatment
Whether to consider enamel fluorosis, particularly the moderate to severe forms, an adverse cosmetic effect or an adverse health effect has been the subject of debate for decades. Some early literature suggests that the clinical course of caries could be compromised by untreated severe enamel fluorosis. Smith and Smith (1940, pp.1050-1051) observed, “There is ample evidence that mottled teeth, though they be somewhat more resistant to the onset of decay, are structurally weak, and that unfortunately when decay does set in, the result is often disastrous. Caries once started evidently spreads rapidly. Steps taken to repair the cavities in many cases were unsuccessful, the tooth breaking away when attempts were made to anchor the fillings, so that extraction was the only course.” Gruebbel (1952, p.153) expressed a similar viewpoint: “Severe mottling is as destructive to teeth as
is dental caries. Therefore, when the concentration is excessive, defluorination or a new water supply should be recommended. The need for removing excessive amounts of fluorides calls attention to the peculiar situation in public health practice in which a chemical substance is added to water in some localities to prevent a disease and the same chemical substance is removed in other localities to prevent another disease.” Dean advised that when the average child in a community has mild fluorosis (0.6 on his scale, described in the next section), “… it begins to constitute a public health problem warranting increasing consideration” (Dean 1942, p. 29).
There appears to be general acceptance in today’s dental literature that enamel fluorosis is a toxic effect of fluoride intake that, in its severest forms, can produce adverse effects on dental health, such as tooth function and caries experience. For example:
-
“The most severe forms of fluorosis manifest as heavily stained, pitted, and friable enamel that can result in loss of dental function” (Burt and Eklund 1999).
-
“In more severely fluorosed teeth, the enamel is pitted and discolored and is prone to fracture and wear” (ATSDR 2003, p. 19).
-
“The degree of porosity (hypermineralization) of such teeth results in a diminished physical strength of the enamel, and parts of the superficial enamel may break away … In the most severe forms of dental fluorosis, the extent and degree of porosity within the enamel are so severe that most of the outermost enamel will be chipped off immediately following eruption” (Fejerskov et al. 1990, p. 694).
-
“With increasing severity, the subsurface enamel all along the tooth becomes increasingly porous … the more severe forms are subject to extensive mechanical breakdown of the surface” (Aoba and Fejerskov 2002, p. 159).
-
“With more severe forms of fluorosis, caries risk increases because of pitting and loss of the outer enamel” (Levy 2003, p. 286).
-
“ … the most severe forms of dental fluorosis might be more than a cosmetic defect if enough fluorotic enamel is fractured and lost to cause pain, adversely affect food choices, compromise chewing efficiency, and require complex dental treatment” (NRC 1993, p. 48).
Severe enamel fluorosis is treated to prevent further enamel loss and to address the cosmetic appearance of teeth. Treatments include bleaching, microabrasion, and the application of veneers or crowns. Bleaching and microabrasion are typically used with the mild to moderate forms of enamel fluorosis. Bleaching is the least invasive procedure, but does not eliminate the dark stains associated with severe enamel fluorosis. Microabrasion involves the controlled abrasion of enamel to remove superficial stains.
This technique has been reported to be minimally invasive and successful in treating single-line or patched opacities, but was not effective in treating defects that extend deeper into the enamel (Wong and Winter 2002). Train et al. (1996) found that while microabrasion improved the appearance of all degrees of enamel fluorosis, severely fluorosed teeth exhibited more defective surfaces following treatment. Pits and fissures can be filled with flowable composites. Partial veneers, composite veneers, and crowns provide the best aesthetic results for very severe enamel fluorosis, but are the most invasive treatments. Crowns are usually used as a last resort because they can be a threat to tooth vitality (Christensen 2005). The procedure requires the further removal of tooth enamel to allow for bonding of the crown, and sometimes requires replacement within a few years. The more invasive treatments should be used only in the most severe cases of enamel fluorosis.
Ascertaining Enamel Fluorosis
Enamel Fluorosis Indexes
The three main indexes used to grade enamel fluorosis in research are Dean’s index, the Thylstrup-Fejerskov index (TFI), and the tooth surface index of fluorosis (TSIF). A particularly useful review of the characteristics, strengths, and limitations of these indexes is given by Rozier (1994).
Dean’s index (Table 4-1) uses a 6-point ordinal scale, ranging from normal to severe, to classify individuals with regard to enamel fluorosis (Dean 1942). Scores are assigned on the basis of the two worst-affected teeth and are derived from an assessment of the whole tooth rather than the worst-affected tooth surface. Although Dean’s index is considered adequate for a broad definition of prevalence and trends, it suffers from limited sensitivity for analytical research in several ways. Because a person is assigned to a fluorosis category on the basis of only two severely affected teeth, the score may not discriminate between those individuals who have more affected teeth from those with only a few affected teeth. In addition, as the teeth most frequently affected by enamel fluorosis are posterior teeth and not the aesthetically important anterior teeth, Dean’s index may misclassify individuals with respect to aesthetic effects (Griffin et al. 2002). As a score assigned at the level of the person, Dean’s index enables the computation of prevalence estimates but does not permit an analysis of the effects of changes in exposure during the development of different teeth. Finally, with only one category for severe fluorosis, Dean’s index does not discriminate between staining and pitting or between discrete and confluent pitting. In fact, Dean revised the index in 1942 to create the version in use today, which combines the original “moderately severe” and “severe” categories. Despite its limitations, Dean’s index is by far the most widely used measure of enamel
TABLE 4-1 Clinical Criteria for Dean’s Enamel Fluorosis Index
|
Diagnosis |
Criteria |
|
Normal (0) |
The enamel represents the usually translucent semivitriform type of structure. The surface is smooth, glossy, and usually a pale creamy white color. |
|
Questionable (0.5) |
The enamel discloses slight aberrations from the translucency of normal enamel, ranging from a few white flecks to occasional white spots. This classification is utilized when a definite diagnosis of the mildest form of fluorosis is not warranted and a classification of “normal” is not justified. |
|
Very mild (1) |
Small, opaque, paper white area scattered irregularly over the tooth but not involving as much as approximately 25% of the tooth surface. Frequently included in this classification are teeth showing no more than 1 to 2 mm of white opacity at the tip of the summit of the cusps of the bicuspids or second molars. |
|
Mild (2) |
The white opaque areas in the enamel of the teeth are more extensive but do not involve as much as 50% of the tooth. |
|
Moderate (3) |
All enamel surfaces of the teeth are affected, and surfaces subject to attrition show marked wear. Brown stain is frequently a disfiguring feature. |
|
Severe (4) |
All enamel surfaces are affected and hypoplasia is so marked that the general form of the tooth may be altered. The major diagnostic sign of this classification is the discrete or confluent pitting. Brown stains are widespread and teeth often present a corroded appearance. |
|
SOURCE: Dean 1942. Reprinted with permission; copyright 1942, American Association for the Advancement of Science. |
|
fluorosis in the research literature. As a consequence, any comprehensive review of the literature must rely upon it.
The TFI (Table 4-2), which classifies the facial surface of each tooth on a 10-point scale (0 to 9), provides more criteria and categories for characterizing mild and severe forms of fluorosis than Dean’s index allows (Thylstrup and Fejerskov 1978). At the upper end of the severity scale, the TFI usefully distinguishes among marked discoloration without pitting (score 4); discrete or focal pitting (score 5); and degrees of confluent pitting, enamel loss, and tooth deformation (scores 6-9). The TFI has been shown to be a valid indication of the fluoride content of fluorotic enamel. Most investigators combine TFI scores of 5 and higher, all of which include pitting, to form a category of severe enamel fluorosis.
The TSIF (Table 4-3) ascribes a fluorosis score on an 8-point scale (0 to 7) to each unrestored surface of each tooth (Horowitz et al. 1984). At the higher end of the scale, there is a greater range of criteria for characterization of effects. A TSIF score of 5 is the lowest classification on this scale that involves enamel pitting. Although some researchers combine scores 5-7
TABLE 4-2 Clinical Criteria and Scoring for the Thylstrup and Fejerskov Index (TFI) of Enamel Fluorosis
|
Score |
Criteria |
|
0 |
Normal translucency of enamel remains after prolonged air-drying. |
|
1 |
Narrow white lines corresponding to the perikymata. |
|
2 |
Smooth surfaces: More pronounced lines of opacity that follow the perikymata. Occasionally confluence of adjacent lines. Occlusal surfaces: Scattered areas of opacity < 2 mm in diameter and pronounced opacity of cuspal ridges. |
|
3 |
Smooth surfaces: Merging and irregular cloudy areas of opacity. Accentuated drawing of perikymata often visible between opacities. Occlusal surfaces: Confluent areas of marked opacity. Worn areas appear almost normal but usually circumscribed by a rim of opaque enamel. |
|
4 |
Smooth surfaces: The entire surface exhibits marked opacity or appears chalky white. Parts of surface exposed to attrition appear less affected. Occlusal surfaces: Entire surface exhibits marked opacity. Attrition is often pronounced shortly after eruption. |
|
5 |
Smooth and occlusal surfaces: Entire surface displays marked opacity with focal loss of outermost enamel (pits) < 2 mm in diameter. |
|
6 |
Smooth surfaces: Pits are regularly arranged in horizontal bands < 2 mm in vertical extension. Occlusal surfaces: Confluent areas < 3 mm in diameter exhibit loss of enamel. Marked attrition. |
|
7 |
Smooth surfaces: Loss of outermost enamel in irregular areas involving less than half of entire surface. Occlusal surfaces: Changes in morphology caused by merging pits and marked attrition. |
|
8 |
Smooth and occlusal surfaces: Loss of outermost enamel involving more than half of surface. |
|
9 |
Smooth and occlusal surfaces: Loss of main part of enamel with change in anatomic appearance of surface. Cervical rim of almost unaffected enamel is often noted. |
|
SOURCE: Thylstrup and Fejerskov 1978. Reprinted with permission; copyright 1978, Community Dentistry and Oral Epidemiology. |
|
to classify severe enamel fluorosis, others extend their highest category of severity to include score 4, which includes staining but not pitting.
Other fluorosis indexes, such as those developed by Siddiqui (1955) and Al-Alousi et al. (1975), are used less frequently in research and almost never in the United States. The developmental defects of enamel (DDE) index was designed as a general classification scheme for enamel defects (FDI 1982; Clarkson and O’Mullane 1989). As it emphasizes aesthetic concerns and is not based on etiologic considerations, it is not technically an index of enamel fluorosis. The fluorosis risk index (FRI) was developed specifically for use in case-control studies (Pendrys 1990), very few of which have been conducted.
TABLE 4-3 Clinical Criteria and Scoring for the Tooth Surface Index of Fluorosis (TSIF)
|
Score |
Criteria |
|
0 |
Enamel shows no evidence of fluorosis. |
|
1 |
Enamel shows definite evidence of fluorosis—namely, areas with parchment-white color that total less than one-third of the visible enamel surface. This category includes fluorosis confined only to incisal edges of anterior teeth and cusp tips of posterior teeth (“snowcapping”). |
|
2 |
Parchment-white fluorosis totals at least one-third, but less than two-thirds, of the visible surface. |
|
3 |
Parchment-white fluorosis totals at least two-thirds of the visible surface. |
|
4 |
Enamel shows staining in conjunction with any of the preceding levels of fluorosis. Staining is defined as an area of definite discoloration that may range from light to very dark brown. |
|
5 |
Discrete pitting of the enamel exists, unaccompanied by evidence of staining of intact enamel. A pit is defined as a definite physical defect in the enamel surface with a rough floor that is surrounded by a wall of intact enamel. The pitted area is usually stained or differs in color from the surrounding enamel. |
|
6 |
Both discrete pitting and staining of the intact enamel exist. |
|
7 |
Confluent pitting of the enamel surface exists. Large areas of enamel may be missing and the anatomy of the tooth may be altered. Dark-brown stain is usually present. |
|
SOURCE: Horowitz et al. 1984. Reprinted with permission; copyright 1984, American Dental Association. |
|
A major difference among the three principal enamel fluorosis indexes is the level at which the scores are recorded: the level of the person on Dean’s index, the level of the tooth on the TFI, and the level of the tooth surface on the TSIF. As the tooth-level scores for Dean’s index are usually recorded but not reported, it is impossible to break the reported person-level scores down to the tooth or tooth-surface level. Similarly, the tooth level TFI scores cannot be broken down to the level of the tooth surface. In contrast, it is possible to combine TFI scores up to the person level and to combine TSIF scores up to the tooth or person levels.
Because the person-level Dean’s index is the oldest and still the most widely used enamel fluorosis index, researchers using the TFI or TSIF sometimes, though rarely, aggregate scores on those scales up to the person level for comparability. When this is done, the most severe one or two teeth or tooth surfaces are typically used. As a consequence, the prevalence of a given level of enamel fluorosis severity (other than “normal” or “unaffected”) will tend to be lowest if expressed as a proportion of all tooth surfaces, intermediate in magnitude if expressed as a proportion of all teeth, and highest if expressed as a proportion of all persons in a given sample. Prevalence estimates at the person level are reviewed by the committee later in this chapter. When the interest is in aesthetic concerns about milder forms of fluorosis,
the person level and tooth level have disadvantages, as the affected teeth may be located in the posterior part of the mouth and thus less visible under ordinary (nonclinical) circumstances. For the severest forms, in contrast, the considerations are reversed. It is more informative to know the proportion of a population who have any teeth with dark staining and pitting than the proportion of all teeth or of all tooth surfaces that have these most severe manifestations of enamel fluorosis.
Diagnostic Issues
The 1993 National Research Council (NRC) report found that the accuracy of clinical diagnosis of fluorotic lesions, especially those of the mild form, has been plagued by the fact that not all white or light yellow opacities in dental enamel are caused by fluoride. The ascertainment of severe enamel fluorosis, in contrast, is much more secure. This is especially true in studies of children in communities with relatively high water fluoride concentrations in the United States and similar locales, where there are few if any alternative explanations for dark yellow to brown staining and pitting of the enamel of recently erupted permanent teeth.
Some studies in the international literature have reported severe mottling of the teeth that could not be attributed to fluoride exposure. For example, Whitford (1996) was unable to explain a high prevalence of severe lesions resembling fluorosis in individuals in Morrococha, Peru, on the basis of exposure to fluoride in water, food, or dental products. Yoder et al. (1998) found severe dental mottling in a population in Tanzania with negligible fluoride in the water (<0.2 mg/L). They noted that urinary fluoride concentrations in affected subjects from that area were not consistent with concentrations found in subjects from a high-fluoride area who had severe enamel fluorosis. Mottling unrelated to fluoride has been suggested to be due to malnutrition, metabolic disorders, exposure to certain dietary trace elements, widespread introduction of tea drinking among children at very early ages, or physical trauma to the tooth (Curzon and Spector 1977; Cutress and Suckling 1990).
A genetic condition called amelogeneis imperfecta causes enamel defects that can be mistaken for enamel fluorosis (Seow 1993); the hypoplastic lesions of this condition have a deficiency in the quantity of enamel with grooves and pits on the surface. Hypocalcified lesions have low mineralization, appear pigmented, and have softened and easily detachable enamel. Hypomaturation conditions are evident as opaque and porous enamel. The prevalence of amelogeneis imperfecta ranges from approximately 1 in 700 to 1 in 14,000, depending on the population studied (Seow 1993).
Angmar-Mansson and Whitford (1990) reported that acute and chronic exposures to hypobaric hypoxia that occurs at high altitudes are associated
with bilaterally symmetrical and diffuse disturbances in enamel mineralization that might be mistaken for fluorosis. More recently, Rweneyonyi et al. (1999) reported higher prevalences of severe enamel fluorosis at higher altitudes than at lower altitudes in Ugandan populations with the same water fluoride levels.
Some evidence from animal studies indicates that genetics might contribute to susceptibility to enamel fluorosis (Everett et al. 2002). It has also been proposed that use of the antibiotic amoxicillin during infancy might contribute to the development of enamel fluorosis of the primary teeth (Hong et al. 2004).
A number of review articles evaluate the strengths and deficiencies of the various indexes used to diagnose and characterize the degree of enamel fluorosis (Clarkson 1989; Ellwood et al. 1994; Kingman 1994; Rozier 1994). In general, the following observations may be made:
-
The various indexes use different examination techniques, classification criteria, and ways of reporting data. All indexes are based on subjective assessment, and little information is available on their validity or comparability. Prevalence data obtained from these indexes also can vary considerably because of differences in study protocols and case definitions. Nevertheless, the American Dental Association (2005) considers severe and even moderate fluorosis “typically easy to detect.”
-
Examiner reliability is an important consideration in evaluation studies. Systematic interexaminer variability has been reported (Burt et al. 2003). Rozier (1994) noted that only about half the studies available in 1994 provided evidence that examiner reliability was evaluated. Although almost all of those assessments were conducted in populations in which severe enamel fluorosis was very rare, they showed an acceptable level of agreement.
-
Agreement among examiners tends to be lower when enamel fluorosis is recorded at the level of the tooth or tooth surface than when it is recorded at the person level.
Prevalence of Severe Enamel Fluorosis in Relation to Water Fluoride Concentrations
In many reviews and individual studies, all levels of enamel fluorosis severity are grouped together. This approach is less problematic at comparatively low levels of fluoride intake, where all or almost all of the cases are mild or moderate in severity. At higher intake levels, such as those typically found in communities with water fluoride concentrations at the current MCLG of 4 mg/L or the current SMCL of 2 mg/L, it is more informative to report results for the different levels of fluorosis severity. Those reviews in
which severity distinctions have been drawn, such as NRC (1993) and IOM (1997), have tended to combine moderate and severe fluorosis into a single category. The present report focuses more specifically on the severe forms.
The committee compiled prevalence estimates at the person level for severe enamel fluorosis in relation to water fluoride levels from studies around the world. The starting points were the estimates provided in EPA’s documentation supporting the MCLG (50 Fed. Reg. 20164 [1985]) and Appendix C6 of McDonagh et al. (2000a). To these were added results from 24 additional studies (Venkateswarlu et al. 1952; Forsman 1974; Retief et al. 1979; Rozier and Dudney 1981; Subbareddy and Tewari 1985; Haimanot et al. 1987; Kaur et al. 1987; Mann et al. 1987, 1990; Szpunar and Burt 1988; Thaper et al. 1989; Jackson et al. 1995; Cortes et al. 1996; Akpata et al. 1997; Gopalakrishnan et al. 1999; Kumar and Swango 1999; Menon and Indushekar 1999; Rwenyonyi et al. 1999; Sampaio and Arneberg 1999; Awadia et al. 2000; Alarcón-Herrera et al. 2001; Grobler et al. 2001; Ermisş et al. 2003; Wondwossen et al. 2004). Results were excluded if they were for fluorosis indexes other Dean’s index, the TFI, the TSIF, or modifications thereof (e.g., Goward 1982; Nunn et al. 1992); for all fluorosis or for moderate and severe fluorosis combined (e.g., Warnakulasuriya et al. 1992; Mella et al. 1994; Alonge et al. 2000; Burt et al. 2003); for primary or deciduous teeth as opposed to permanent teeth (e.g., McInnes et al. 1982); for different teeth separately with no results at the person level or for all teeth combined (e.g., Opinya et al. 1991); for unbounded upper categories of water fluoride for which no mean or median value was given (e.g., > 1.2 mg/L in Heller et al. [1997], > 2 mg/L in Ray et al. [1982], > 2.5 mg/L in Angelillo et al. [1999]); for bounded but extremely wide water fluoride ranges (e.g., 0.8 to 4.3 mg/L in Haimanot et al. [1987], 0.7 to 4.0 in Beltran-Aguilar et al. [2002], 0.3 to 2.2 mg/L in Wondwossen et al. [2004]). For narrower bounded categories, the midrange water fluoride level was used. Results from studies of children and teenagers (age 20 years or younger) were tallied separately from results for adults. Severe enamel fluorosis was classified as the “severe” classification in Dean’s index and, depending on the groupings created by the original invesgtigators, TFI scores of 4-9 or 5-9 and TSIF scores of 4-7 or 5-7. Because of the wide variability in methods and populations, and the lack of independence when a given study provided more than one result, the estimates were not subjected to formal statistical analyses. Instead, plots of the prevalence estimates in relation to water fluoride concentration were examined for the presence of any clear and obvious patterns or trends.
Figure 4-1 shows 94 prevalence estimates from studies in the United States. Despite the wide range of research methods, fluorosis indexes, water fluoride measurement methods, and population characteristics in these studies conducted over a period spanning half a century, a clear trend is evident.
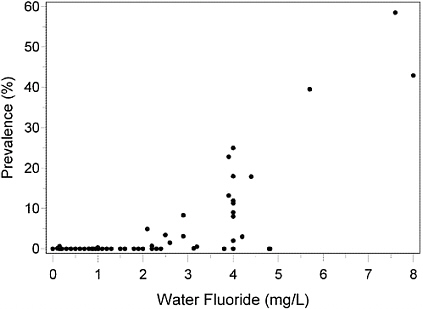
FIGURE 4-1 Prevalence of severe enamel fluorosis at the person level by water fluoride concentration, permanent teeth, age < 20 years, U.S. communities.
The prevalence of severe enamel fluorosis is close to zero in communities at all water fluoride concentrations below 2 mg/L. Above 2 mg/L, the prevalence rises sharply. The shape of this curve differs dramatically from the linear trend observed when all levels of fluorosis severity are combined and related to either the water fluoride concentration (Dean 1942) or the estimated daily dose in milligrams per kilogram (Fejerskov et al. 1990).
Not shown in Figure 4-1 are a prevalence of 54% in a community with a water fluoride concentration of 14 mg/L (50 Fed. Reg. 20164 [1985]) and results from two studies of adults. One, with an age range of 20-44 years, reported prevalences of zero at <0.1 mg/L and 2% at 2.5 mg/L (Russell and Elvove 1951). In the other, with an age range of 27-65 years, the prevalences were zero at 0.7 mg/L and 76% at 3.5 mg/L (Eklund et al. 1987). These results are broadly consistent with those in Figure 4-1.
Strongly supporting evidence comes from a series of surveys conducted by researchers at the National Institute of Dental Health (Selwitz et al. 1995, 1998). In these studies using the TSIF, scores were reported only at the tooth-surface level (Figure 4-2). As with the person-level prevalence estimates (Figure 4-1), an approximate population threshold for severe enamel fluorosis is evident at water concentrations below 2 mg/L.
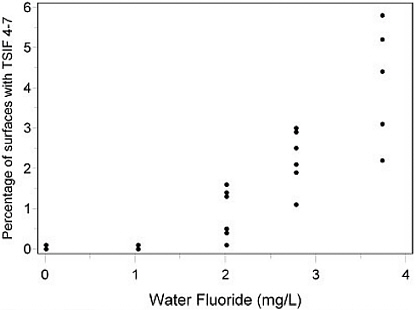
FIGURE 4-2 Percentage of tooth surfaces with severe enamel fluorosis (TSIF scores 4-7) by water fluoride concentration, permanent teeth, ages 8-10 and 13-16 years, U.S. communities, 1980, 1985 and 1990. (Some samples of children at a given water fluoride concentration had identical percentages of tooth surfaces with TSIF scores 4-7.) SOURCE: Selwitz et al. 1995, 1998.
Figure 4-3 shows 143 prevalence estimates from studies of children outside the United States. Not shown are results for three Ethiopian communities with extremely high water fluoride concentrations of 26, 34 and 36 mg/L and prevalences of 18%, 48% and 25%, respectively (Haimanot et al. 1987). Although a positive association may be discernible, it is much less obvious than in the U.S. studies. There is little evidence of an approximate population threshold as in the results in U.S. communities (Figure 4-1). In many regions around the world, water intake among children whose permanent teeth are forming can be much more variable than in the United States, susceptibility may differ more widely, sources of fluoride intake other than the community water supply may be more prevalent, or the ascertainment of severe enamel fluorosis may be more often compromised by other determinants of dental discoloration and pitting.
One question is whether the most severe forms of enamel fluorosis, specifically those involving confluent pitting, occur at water concentrations in the range of the current MCLG of 4 mg/L. This question cannot be an-
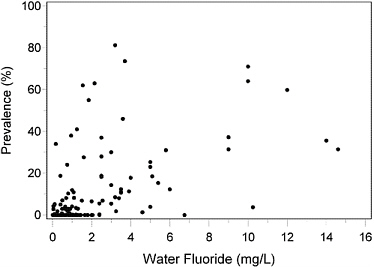
FIGURE 4-3 Prevalence of severe enamel fluorosis at the person level by water fluoride concentration, permanent teeth, age < 20 years, communities outside the United States.
swered by most studies, which use Dean’s 1942 modification of his index combining “moderately severe” and “severe” classifications of his original system (Dean 1934) into a single category (Dean 1942; Rozier 1994). Three studies, however, in U.S. communities with water fluoride concentrations of approximately 4 mg/L have used enamel fluorosis indexes that draw severity distinctions within the “severe” category.
In Lowell, Indiana, with a water fluoride concentration of approximately 4 mg/L, 7% of a 1992 sample and 2% of a 1994 sample of children 7-14 years of age had at least one tooth surface assigned the highest possible TSIF score of 7 (Table 4-4). Expressed as a percentage of all tooth surfaces examined (mean, 32.3 per child), the prevalence of TSIF score 7 in the 1992 sample was substantially lower at 0.5% (Jackson et al. 1995). The lower prevalence using this metric is not surprising, as it includes surfaces on anterior teeth, which are not generally as susceptible to fluorosis as molars and other teeth located farther back in the mouth.
In Bushnell, Illinois, with a mean water fluoride concentration of 3.8 mg/L, samples of children age 8-10 years and 13-15 years were examined in 1980 and 1985 (Heifetz et al. 1988). As shown in Table 4-5, the TSIF score
TABLE 4-4 Maximum TSIF Scores in Two Samples of Children Age 7-14 Years in a U.S. Community with a Water Fluoride Concentration of 4.0 mg/L
|
|
1992 study |
1994 study |
||
|
Maximum TSIF Score |
Number of Children |
Percent |
Number of Children |
Percent |
|
0 |
8 |
7.9 |
1 |
1.0 |
|
1 |
23 |
22.8 |
34 |
32.4 |
|
2 |
17 |
16.8 |
18 |
17.1 |
|
3 |
26 |
25.7 |
31 |
29.5 |
|
4 |
7 |
6.9 |
12 |
11.4 |
|
5 |
10 |
9.9 |
7 |
6.7 |
|
6 |
3 |
3.0 |
0 |
0.0 |
|
7 |
7 |
6.9 |
2 |
1.9 |
|
Total |
101 |
100.0 |
105 |
100.0 |
|
SOURCE: Jackson et al. 1995, 1999; R.D. Jackson (Indiana University-Purdue University Indianapolis, personal commun., December 21, 2005). |
||||
TABLE 4-5 Percentage of Tooth Surfaces Assigned TSIF Scores in Four Samples of Children Age 8-10 Years and 13-15 Years in a U.S. Community with a Water Fluoride Concentration of 3.8 mg/La
of 7 was assigned in all four samples. Detailed TSIF scores from this study are available only on as a percentage of all tooth surfaces examined. These results are consistent with those from the 1992 sample in Lowell, Indiana (Jackson et al. 1995) using the same fluorosis metric.
Confluent enamel pitting must be present for a tooth surface to be assigned a score of 7 on the TSIF scale (Table 4-3). In addition to the usual presence of dark brown staining, large areas of enamel may be missing and gross tooth structure may be altered as well. Thus, it has been sufficiently well documented that the most severe forms of enamel fluorosis for which classifications exist occur in children who reside in communities with water fluoride concentrations at or near the MCLG of 4 mg/L.
A third study, confined to the age range of 27-65 years, included a sample of 192 adults from Lordsburg, New Mexico, with a water fluoride concentration of 3.5 mg/L (Eklund et al. 1987). All members of this sample were native to Lordsburg and long-term residents of that community. The prevalence of severe fluorosis on Dean’s 1942 scale was extremely high in this sample, 76% overall. The investigators modified Dean’s scale specifically to split the “severe” category into ‘severe’ (discrete pitting) and ‘very severe’ (confluent pitting)” (Eklund et al. 1987). About half of those with more than moderate fluorosis were classified in the “very severe” category. These results for New Mexico adults are consistent with the results for children in Indiana and Illinois.
A reduction of all water fluoride concentrations to below 2 mg/L would be expected to make severe enamel fluorosis an extreme rarity in the United States, but would not be expected to eliminate it entirely. Isolated cases could still occur from excessive fluoride exposure from other sources, such as toothpaste swallowing and use of fluoride supplements and rinses. One can never rule out the possible existence of hypersusceptible individuals. Finally, though the ascertainment of severe enamel fluorosis is usually quite accurate in the United States, especially among children, it might be possible for dark yellow or brown staining and enamel pitting from other causes to be misdiagnosed as fluorosis. Such false positives might be particularly common among adults who are long-term users of smoked and smokeless tobacco products, heavy consumers of beverages such as coffee and tea, and perhaps some with special occupational exposures.
Aesthetic and Psychological Consequences of Enamel Fluorosis
Studies show that facial attractiveness is important and that attractive people are judged to be more socially desirable than less attractive people (Berscheid and Walster 1974; Adams and Huston 1975; Adams 1977; Jenny and Proshek 1986). Newton et al. (2003) assessed the impact of modified images of untreated cavities on front teeth on the appraisal of personal characteristics in the United Kingdom. Study participants associated decayed and discolored teeth with lower intelligence and social competence and with poor psychological adjustment. Interestingly, the ratings depended on the facial appearance studied, an indication that the impact of enamel
fluorosis is less noticeable in a more attractive face. Although studies of the attractiveness of teeth are sparse, the orthodontic literature has shown that more than 80% of patients seek care out of concern for aesthetics, rather than health or function (Albino et al. 1981).
The potential for psychological and behavioral problems to develop from the aesthetically displeasing consequences of enamel fluorosis has been a long-standing concern. In 1984, an ad hoc panel of behavioral scientists convened by the U.S. Environmental Protection Agency (EPA) and the National Institute of Mental Health to evaluate the issue concluded that “individuals who have suffered impaired dental appearance as a result of moderate and severe fluorosis are probably at increased risk for psychological and behavioral problems or difficulties” (R.E. Kleck, unpublished report, Nov. 17, 1984, as cited in 50 Fed. Reg. 20164 [1985]). The panel recommended research on the social, emotional, and behavioral effects of enamel fluorosis.
Few studies have assessed the association between the public’s perceived aesthetic problems and degree of enamel fluorosis. Only one of those studies was conducted in the United States. Lalumandier and Rozier (1998) found that parental satisfaction with the color of their children’s teeth decreased as the severity of fluorosis increased. Although 73.9% of parents were satisfied with the color of teeth in the absence of enamel fluorosis, only 24.2% of parents were satisfied with the color of their children’s teeth when the TSIF score was 4 or greater (moderate to severe forms). In a study of dental students’ perceptions, Levy et al. (2002b) observed that fluorosis and nonfluorosis images were consistently rated more favorably by fourth-year students than by the same students in their first year. According to the authors, the results suggested that dentists might regard fluorosis with less concern given that they are exposed to a wide range of oral conditions, whereas those outside the dental profession might view fluorosis with more concern. Griffin et al. (2002) reviewed five published studies of aesthetic perception and enamel fluorosis and estimated that approximately 2% of U.S. schoolchildren might experience perceived aesthetic problems from exposure to fluoride at 0.7-1.2 mg/L. It should be noted that perceived aesthetic problems have also been reported even in the absence of enamel fluorosis because of nonfluorotic enamel opacities and hypoplasia, natural yellowish appearance of teeth, and discoloration due to dental caries. For example, Griffin et al. (2002) also noted that the percentage of respondents with no fluorosis who were not satisfied with the appearance of their teeth ranged from 18% to 41%.
In general, studies conducted in other parts of the world show that the level of satisfaction expressed by parents, children, and dentists with the appearance of enamel fluorosis decreases with increasing severity of enamel fluorosis (Clark et al. 1993; Riordan 1993; Clark 1995; Hawley et al. 1996;
Lalumandier and Rozier 1998; Griffin et al. 2002). In contrast with those studies, Ismail et al. (1993) did not find enamel fluorosis to be an aesthetic problem in Truro, Nova Scotia. The primary reason for disliking the color of front teeth was perceived yellowness unrelated to enamel fluorosis. Similarly, a study conducted in Brazil found that enamel fluorosis had no impact on children’s self-perception of appearance (Peres et al. 2003).
A systematic review of water fluoridation estimated the proportion of the population likely to have aesthetic concerns about enamel fluorosis on the basis of a review of 88 studies (McDonagh et al. 2000a). The authors pointed out that the differences in the proportion of the population having enamel fluorosis of aesthetic concern with low concentrations of fluoride in drinking water and with fluoride at 1.2 mg/L were not statistically significant. However, the estimation of aesthetic concerns was based solely on a study conducted in Great Britain (Hawley et al. 1996) in which 14-year-old children from Manchester were asked to rate the appearance of life-sized pictures of two front teeth with enamel fluorosis (lips cropped off) classified by the TFI. According to the authors, the percentage of subjects who considered the appearance of the teeth unacceptable decreased from 29% for TF scores of 0 to 15% for TF scores of 2 and increased to 85% for TF scores of 4. Using those data, McDonagh et al. (2000a) defined enamel fluorosis of aesthetic concern as a case with a TF score of 3 or more, Dean’s score of “mild” or worse, and a TSIF score of 2 or more. With this definition, McDonagh et al. (2000a) estimated the prevalence of fluorosis of aesthetic concern in the United Kingdom to be 63% at 4 mg/L and 25% at 2 mg/L. For lower water fluoride concentrations, the estimated prevalence ranged from 15% at 1.2 mg/L down to a baseline of 6% at 0.1 mg/L.
The committee judges that this analysis produced an overestimation of the prevalence of fluorosis of actual aesthetic concern for two main reasons. First, McDonagh et al. (2000a) applied the aesthetic concerns expressed by study participants about fluorosis on front teeth to fluorosis prevalence studies that included posterior teeth, which have much less potential to pose aesthetic problems. Second, the analysis did not take into account the observation by Hawley et al. (1996) that a higher percentage of children found teeth with milder forms of enamel fluorosis (TF scores lower than 3) aesthetically preferable to normal teeth; almost one-third of the children rated the photograph of teeth with no fluorosis as unacceptable.
There have been no new studies of the prevalence of moderate enamel fluorosis in U.S. populations since the early 1990s. Previous estimates ranged from 4% to 15% (50 Fed. Reg. 20164 [1985]). These estimates are based on studies that used classification indexes for scoring enamel fluorosis, and are not based on an assessment of aesthetics. None of the available indexes allow for making distinctions between fluorosis on the anterior and posterior teeth, so the percentage of children with moderate enamel fluorosis
of aesthetic concern could not be determined, but the percentage would be lower than 15%.
The committee found only one study (Morgan et al. 1998) that specifically evaluated the psychological and behavioral impacts of enamel fluorosis on children with the condition. A group of 197 pediatric patients of a dental practice between the ages of 7 and 11 were examined for enamel fluorosis. Their parents completed the Child Behavior Checklist (CBCL), a widely used measure of behavioral problems in studies of children. The study found no substantial differences between groups classified by degree of fluorosis in overall CBCL scores or in scores on two subscales: externalizing (aggressive, hyperactive and antisocial behaviors typical of undercontrol or “acting out”) and internalizing (behaviors of social withdrawal, depression and anxiety typical of overcontrol or inhibition). The study was limited by the fact that an aggregate measure of fluoride exposure was unrelated to enamel fluorosis and few if any of the children had severe enamel fluorosis.
Several methodologic issues have hindered the assessment of the aesthetic importance of unattractive teeth in general and enamel fluorosis in particular. First, assessing the perception of aesthetics is by its very nature subjective. Second, it is not clear who should make judgments about the aesthetic appearance of teeth. The perceptions of the affected individual, as a child and in subsequent life, as well as those of parents, friends, teachers, and other acquaintances can all be important. A sizeable proportion of parents and children have expressed dissatisfaction with the color of teeth even in the absence of enamel fluorosis. On the other hand, judgments made by professionals might not reflect the perception of the public. Third, it is difficult to place the condition of enamel fluorosis into the context of an overall aesthetic assessment of a person’s appearance or facial attractiveness. Cultural influences can play a role in how the condition is perceived. It also appears that perceptions of the appearance of teeth can be modified by the attractiveness of other facial features. Fourth, when the public or dental professionals are asked to assess aesthetic acceptability, their perceptions might change during the evaluation session.
From the standpoint of this committee’s charge to consider effects of relatively high levels of water fluoride, the main points to note are that the emphasis of research and discussion on psychological, behavioral, and social effects of enamel fluorosis has been almost entirely on children and on the mild and moderate forms of the condition that are more typical of lower fluoride exposure levels. Research needs to focus specifically on severe enamel fluorosis in those areas in which it occurs with appreciable frequency. In addition, research needs to include not only affected children while they are still children, but after they move into adulthood. Finally, parents might experience psychological and behavioral effects when their children develop
enamel fluorosis, especially in its moderate and severe forms. Unfortunately, research on parental effects is completely lacking.
Dental Caries in Relation to Water Fluoride Concentrations of 2 mg/L and Higher
Many reports have discussed the inverse relationship between dental caries and water fluoride at concentrations considerably lower than the current MCLG of 4 mg/L and SMCL of 2 mg/L (Dean 1942; PHS 1991; McDonagh et al. 2000a; CDC 2001). Fewer studies have been conducted in the United States of overall caries experience in communities with naturally occurring fluoride concentrations higher than those produced by fluoridation. The studies of children are shown in Table 4-6. One study suggested that the overall frequency of caries is reduced at approximately 4 mg/L compared with approximately 1 mg/L (Englander and DePaola 1979). A study of New Mexico adults gave similar results (Eklund et al. 1987). Another study suggested little or no difference (Jackson et al. 1995) and another gave mixed results (Selwitz et al. 1995). The evidence from these studies is not persuasive that caries frequency is appreciably lower at approximately 4 mg/L than at approximately 2 mg/L or 3 mg/L. The evidence from studies conducted in other countries is no more consistent (Binder 1973; Olsson 1979; Kunzel 1980; Chen 1989; Lewis et al. 1992; Warnakulasuriya et al. 1992; Yoder et al. 1998; Angelillo et al. 1999; Grobler et al. 2001).
Dental Caries in Relation to Severe Enamel Fluorosis
As previously noted, it is suspected within the dental research community that the enamel pitting that occurs in severe fluorosis might increase caries risk by reducing the thickness of the protective enamel layer and by allowing food and plaque to become entrapped in enamel defects. The possibility is thus raised that in a community with a water fluoride concentration high enough to produce an appreciable prevalence of severe fluorosis, the specific subset of children who develop this condition might be placed at increased caries risk, independent of the effect of the fluoride itself on the remainder of the population. The population of interest consists of those children who develop severe enamel fluorosis at 4 mg/L. If the water fluoride concentration were reduced to below 2 mg/L, few if any of these children would still develop severe enamel fluorosis. Many of them would develop mild to moderate fluorosis, however, while others might develop no fluorosis. It would be unreasonable, however, to assume that some children would skip all the way down from severe fluorosis to no fluorosis when the water concentration is reduced, while others would have mild to moderate fluorosis at either concentration. As the desired fluorosis severity
TABLE 4-6 Mean Number of Decayed, Missing and Filled Surfaces (DMFS) in Permanent Teeth by Water Fluoride Concentration in Studies of Children in U.S. Communities with Water Fluoride Concentrations at or Near the MCLG of 4 mg/L
|
Reference |
Age (years) |
Year |
Community |
Number of Children |
Approximate Water Fluoride Concentration (mg/L) |
Mean DMFS |
|
Englander and DePaola (1979) |
12-15 |
NA |
Kalamazoo, MI |
315 |
1 |
5.1 |
|
Stickney, IL |
312 |
1 |
4.5 |
|||
|
Charlotte, NC |
213 |
1 |
4.4 |
|||
|
Midland, TX |
311 |
5-7 |
2.4 |
|||
|
Driscoll et al. (1983) |
8-11 |
1980 |
Kewanee, IL |
157 |
1 |
2.0 |
|
Monmouth, IL |
80 |
2 |
1.4 |
|||
|
Abindgon and Elmwood, IL |
110 |
3 |
1.0 |
|||
|
Bushnell, Ipava and Table Grove, IL |
77 |
4 |
1.6 |
|||
|
Driscoll et al. (1983) |
12-16 |
1980 |
Kewanee, IL |
179 |
1 |
4.1 |
|
Monmouth, IL |
63 |
2 |
2.7 |
|||
|
Abindgon and Elmwood, IL |
82 |
3 |
2.0 |
|||
|
Bushnell, Ipava and Table Grove, IL |
59 |
4 |
2.6 |
|||
|
Heifetz et al. (1988) |
8-10 |
1985 |
Kewanee, IL |
156 |
1 |
1.5 |
|
Monmouth, IL |
102 |
2 |
1.1 |
|||
|
Abindgon and Elmwood, IL |
112 |
3 |
0.8 |
|||
|
Bushnell, Ipava and Table Grove, IL |
62 |
4 |
0.8 |
|||
|
Heifetz et al. (1988) |
13-15 |
1985 |
Kewanee, IL |
94 |
1 |
5.1 |
|
Monmouth, IL |
23 |
2 |
2.9 |
|||
|
Abindgon and Elmwood, IL |
47 |
3 |
2.5 |
|||
|
Bushnell, Ipava and Table Grove, IL |
29 |
4 |
3.9 |
|||
|
Selwitz et al. (1995) |
8-10, 14-16 |
1990 |
Kewanee, IL |
258 |
1 |
1.8 |
|
Monmouth, IL |
105 |
2 |
1.4 |
|||
|
Abindgon and Elmwood, IL |
117 |
3 |
1.4 |
|||
|
Bushnell, Ipava and Table Grove, IL |
77 |
4 |
1.8 |
|||
|
Jackson et al. (1995) |
7-14 |
1992 |
Brownsburg, IN |
117 |
1 |
4.4 |
|
Lowell, IN |
101 |
4 |
4.3 |
|||
|
NA: Not available. |
||||||
distribution is inherently unknown, a conservative approach is to compare the children with severe fluorosis at 4 mg/L with children from their own communities with mild to moderate fluorosis.
Results for such comparisons are summarized in Table 4-7 for studies reporting the mean number of decayed, missing and filled tooth surfaces (DMFS), in Table 4-8 for studies reporting the number of decayed, missing and filled teeth (DMFT), and in Table 4-9 for studies reporting the per-
TABLE 4-7 Mean Number of Decayed, Missing, and Filled Permanent Tooth Surfaces (DMFS) among Children with Severe and Mild to Moderate Enamel Fluorosis
|
Country (reference) |
Age (years) |
Number of Children |
Fluorosis Index and Range |
Mean DMFS |
|
United States (Driscoll et al. 1986) |
8-16 |
218 54 |
Dean very mild to moderate Dean severe |
1.6 3.0 |
|
Israel (Mann et al. 1987) |
15-16 |
83 46 |
Dean very mild to moderate Dean severe |
4.4 10.4 |
|
Israel (Mann et al. 1990) |
8-10 |
55 6 |
Dean very mild to moderate Dean severe |
1.2 1.8 |
|
Turkey (Ermisş et al. 2003) |
12-14 |
24 105 |
TSIF 1-3 TSIF 4-7 |
1.7 1.9 |
TABLE 4-8 Mean Numbers of Decayed, Missing, and Filled Permanent Teeth (DMFT) among Children with Severe and Mild to Moderate Enamel Fluorosis
|
Country (reference) |
Age (years) |
Number of Children |
Fluorosis Index and Range |
Mean DMFT |
|
Taiwan (Chen 1989) |
6-16 |
1,290 10 |
Dean very mild to moderate Dean severe |
1.7 2.5 |
|
Sri Lanka (Warnakulasuriya et al. 1992) |
14 |
44 48 |
Dean mild Dean moderate to severe |
3.4 3.3 |
|
Brazil (Cortes et al. 1996) |
6-12 |
42 18 |
TFI 3-4 TFI ≥5 |
1.1 1.3 |
|
Turkey (Ermisş et al. 2003) |
12-14 |
24 105 |
TSIF 1-3 TSIF 4-7 |
1.2 1.3 |
|
Ethiopia (Wondwossen et al. 2004) |
12-15 |
87 89 |
TFI 3-4 TFI 5-7 |
1.5 2.4 |
TABLE 4-9 Percentage of Teeth Scored as Decayed, Missing, Filled, or with Caries among Children and Adults with Severe and Mild-to-Moderate Enamel Fluorosis
|
Country (reference) |
Age (years) |
Teeth |
Number of Persons |
Range of Dean’s Fluorosis Index |
Measure (%) |
|
Ethiopia (Olsson 1979) |
6-7, 13-14 |
All |
|
Mild to moderate Severe |
Cavities 25 9 |
|
United States (Driscoll et al. 1986) |
8-16 |
All |
218 54 |
Very mild to moderate Severe |
Decayed or filled 4 20 |
|
United States (Eklund et al. 1987) |
27-65 |
Molars |
38 125 |
Mild to moderate Severe |
Decayed, missing or filled 43 40 |
|
|
|
Premolars |
38 125 |
Mild to moderate Severe |
11 19 |
|
|
|
Anterior |
38 125 |
Mild to moderate Severe |
3 6 |
centage of decayed, missing and filled teeth. Not all researchers reported P-values for the specific contrasts in these tables. Moreover, the results are not independent, as some researchers studied more than one age group or reported results for more than one caries frequency measure or for more than one type of teeth. Nevertheless, in 11 of the 14 available contrasts, the measure of caries frequency was higher among those with severe fluorosis than among those with mild to moderate forms. In some comparisons, the differences were slight. Descriptively, the most pronounced differences were for all teeth among children age 15-16 years in Israel (Mann et al. 1987, Table 4-7), for all teeth among children age 8-16 years in Illinois (Driscoll et al. 1986, Table 4-9), for premolars among adults age 27-65 in New Mexico (Eklund et al. 1987, Table 4-9), and for all teeth among children ages 6-7 and 13-14 in Ethiopia (Olsson 1979, Table 4-9).
Mixed evidence comes from correlation or regression analyses. In studies in Uganda (Rwenyonyi et al. 2001) and Tanzania (Awadia et al. 2002), statistically significant correlations were not observed (P > 0.05) between severe fluorosis and caries frequency. A study of children in a South African community with a water fluoride concentration of 3 mg/L and a 30% prevalence of severe fluorosis reported a positive correlation (P < 0.05) between fluorosis scores on the Dean index and caries experience (DMFT) (Grobler et al. 2001). In the same study, no correlation between fluorosis and caries
frequency was found in two other communities with water fluoride concentrations of 0.5 and 0.2 mg/L, in which the prevalence of severe fluorosis was 1% and 0%, respectively.
The studies on severe enamel fluorosis and caries are limited by being cross-sectional in design and conducted in a wide range locales. In most of the studies, there was no adjustment for oral hygiene, dental care, or other determinants of caries risk. Moreover, as previously noted, measures of the role of chance (i.e., confidence intervals or P-values) are not available for the specific contrasts of interest to the present report. Nevertheless, the hypothesis of a causal link between severe enamel fluorosis and increased caries risk is plausible and the evidence is mixed but supportive.
OTHER DENTAL EFFECTS
Fluoride may affect tooth dentin as well as enamel. The patterns of change observed in bone with age also occur in dentin, a collagen-based mineralized tissue underlying tooth enamel. Dentin continues to grow in terms of overall mass and mineral density as pulp cells deposit more matrix overall and more mineral in the dentin tubules. Several investigators have observed that, like older bone, older dentin is less resistant to fracture and tends to crack more easily (Arola and Reprogel 2005; Imbeni et al. 2005; Wang 2005). Aged dentin tends to be hypermineralized and sclerotic, where the dentin tubules have been filled with mineral and the apatite crystals are slightly smaller (Kinney et al. 2005), which could be significant because, as dentin ages in the presence of high amounts of fluoride, the highly packed fluoride-rich crystals might alter the mechanical properties of dentin as they do in bone (see Chapter 5). Unlike bone, however, dentin does not undergo turnover. Some preliminary studies show that fluoride in dentin can even exceed concentrations in bone and enamel (Mukai et al. 1994; Cutress et al. 1996; Kato et al. 1997; Sapov et al. 1999; Vieira et al. 2004). Enamel fluorosis, which accompanies elevated intakes of fluoride during periods of tooth development, results not only in enamel changes as discussed above but also in dentin changes. It has now been well established that fluoride is elevated in fluorotic dentin (Mukai et al. 1994; Cutress et al. 1996; Kato et al. 1997; Sapov et al. 1999; Vieira et al. 2004). Whether excess fluoride incorporation in fluorotic teeth increases the risk for dentin fracture remains to be determined, but the possibility cannot be ruled out.
Questions have also been raised about the possibility that fluoride may delay eruption of permanent teeth (Kunzel 1976; Virtanen et al. 1994; Leroy et al. 2003). The hypothesized mechanisms for this effect include prolonged retention of primary teeth due to caries prevention and thickening of the bone around the emerging teeth (Kunzel 1976). However, no systematic studies of tooth eruption have been carried out in communities exposed
to fluoride at 2 to 4 mg/L in drinking water. Delayed tooth eruption could affect caries scoring for different age groups.
FINDINGS
One of the functions of tooth enamel is to protect the dentin and, ultimately, the pulp from decay and infection. Severe enamel fluorosis compromises this health-protective function by causing structural damage to the tooth. The damage to teeth caused by severe enamel fluorosis is a toxic effect that the majority of the committee judged to be consistent with prevailing risk assessment definitions of adverse health effects. This view is consistent with the clinical practice of filling enamel pits in patients with severe enamel fluorosis and restoring the affected teeth.
In previous reports, all forms of enamel fluorosis, including the severest form, have been judged to be aesthetically displeasing but not adverse to health (EPA 1986; PHS 1991; IOM 1997; ADA 2005). This view has been based largely on the absence of direct evidence that severe enamel fluorosis results in tooth loss, loss of tooth function, or psychological, behavioral, or social problems. The majority of the present committee finds the rationale for considering severe enamel fluorosis only a cosmetic effect much weaker for discrete and confluent pitting, which constitutes enamel loss, than it is for the dark yellow to brown staining that is the other criterion symptom of severe fluorosis. Moreover, the plausible hypothesis of elevated caries frequency in persons with severe enamel fluorosis has been accepted by some authorities and has a degree of support that, though not overwhelmingly compelling, is sufficient to warrant concern. The literature on psychological, behavioral, and social effects of enamel fluorosis remains quite meager. None of it focuses specifically on the severe form of the condition or on parents of affected children or on affected persons beyond childhood.
Two of the 12 members of the committee did not agree that severe enamel fluorosis should now be considered an adverse health effect. They agreed that it is an adverse dental effect but found that no new evidence has emerged to suggest a link between severe enamel fluorosis, as experienced in the United States, and a person’s ability to function. They judged that demonstration of enamel defects alone from fluorosis is not sufficient to change the prevailing opinion that severe enamel fluorosis is an adverse cosmetic effect. Despite their disagreement on characterization of the condition, these two members concurred with the committee’s conclusion that the MCLG should prevent the occurrence of this unwanted condition.
Severe enamel fluorosis occurs at an appreciable frequency, approximately 10% on average, among children in U.S. communities with water fluoride concentrations at or near the current MCLG of 4 mg/L. Strong evidence exists of an approximate population threshold in the United States,
such that the prevalence of severe enamel fluorosis would be reduced to nearly zero by bringing the water fluoride levels in these communities down to below 2 mg/L. There is no strong and consistent evidence that an appreciable increase in caries frequency would occur by reducing water fluoride concentrations from 4 mg/L to 2 mg/L or lower. At a fluoride concentration of 2 mg/L, severe enamel fluorosis would be expected to become exceedingly rare, but not be completely eradicated. Occasional cases would still arise for reasons such as excessive fluoride ingestion (e.g., toothpaste swallowing), inadvisable use of fluoride supplements, and misdiagnosis.
Despite the characterization of all forms of enamel fluorosis as cosmetic effects by previous groups, there has been general agreement among them, as well as in the scientific literature, that severe and even moderate enamel fluorosis should be prevented. The present committee’s consensus finding that the MCLG should be set to protect against severe enamel fluorosis is in close agreement with conclusions by the Institute of Medicine (IOM 1997), endorsed recently by the American Dental Association (ADA 2005). As shown in Table 4-10, between 25% and 50% of U.S. children in communities with drinking water containing fluoride at 4 mg/L would be expected to consume more than the age-specific tolerable upper limits of fluoride intake set by IOM. Results from the Iowa Fluoride Study (Levy 2003) indicate that even at water fluoride levels of 2 mg/L and lower, some children’s fluoride intake from water exceeds the IOM’s age-specific tolerable upper limits (Table 4-11).
For all age groups listed in Table 4-10, the IOM’s tolerable upper intake values correspond to a fluoride intake of 0.10 mg/kg/day (based on default body weights for each age group; see Appendix B). Thus, the exposure estimates in Chapter 2 also showed that the IOM limits would be exceeded at 2 mg/L for nonnursing infants at the average water intake level (Table 2-14). Specifically, as described in Chapter 2 (Tables 2-14 and 2-15), nonnursing
TABLE 4-10 Tolerable Upper Fluoride Intakes and Percentiles of the U.S. Water Intake Distribution, by Age Group
|
|
Tolerable Upper Intake (IOM 1997) |
Water Intake, mL/day (EPA 2004) |
||
|
Age Group |
Fluoride, mg/day |
Water, mL/day (at 4 mg/L) |
50th Percentile |
75th Percentile |
|
0-6 months |
0.7 |
175 |
42 |
585 |
|
7-12 months |
0.9 |
225 |
218 |
628 |
|
1-3 years |
1.3 |
325 |
236 |
458 |
|
4-8 years |
2.2 |
550 |
316a |
574a |
|
aAges 4-6 years. For ages 7-10 years, the 50th percentile is 355 mL/day and the 75th percentile is 669 mL/day. |
||||
TABLE 4-11 Comparison of Intakes from Drinking Watera from the Iowa Fluoride Study and IOM’s Upper Tolerable Intakes
infants have an average total fluoride intake (all sources except fluoride supplements) of 0.144 and 0.258 mg/kg/day at 2 and 4 mg/L fluoride in drinking water, respectively. Corresponding values are 0.090 and 0.137 mg/kg/day for children 1-2 years old and 0.082 and 0.126 mg/kg/day for children 3-5 years old. Furthermore, at EPA’s current default drinking water intake rate, the exposure of infants (nursing and non-nursing) and children 1-2 years old would be at or above the IOM limits at a fluoride concentration of 1 mg/L (Table 2-13). For children with certain medical conditions associated with high water intake, estimated fluoride intakes from all sources (excluding fluoride supplements) range from 0.13-0.18 mg/kg/day at 1 mg/L to 0.23-0.33 mg/kg/day at 2 mg/L and 0.43-0.63 mg/kg/day at 4 mg/L.
IOM’s tolerable upper limits were established to reduce the prevalence not only of severe fluorosis, but of moderate fluorosis as well, both of which ADA (2005) describes as unwanted effects. The present committee, in contrast, focuses specifically on severe enamel fluorosis and finds that it would be almost eliminated by a reduction of water fluoride concentrations in the United States to below 2 mg/L. Despite this difference in focus, the committee’s conclusions and recommendations with regard to protecting children from enamel fluorosis are squarely in line with those of IOM and ADA.
The current SMCL of 2 mg/L is based on a determination by EPA that objectionable enamel fluorosis in a significant portion of the population is an adverse cosmetic effect. EPA defined objectionable enamel fluorosis as discoloration and/or pitting of teeth. As noted above, the majority of the committee concludes it is no longer appropriate to characterize enamel pitting as a cosmetic effect. Thus, the basis of the SMCL should be discoloration of tooth surfaces only.
The prevalence of severe enamel fluorosis is very low (near zero) at fluoride concentrations below 2 mg/L. However, from a cosmetic stand-
point, the SMCL does not completely prevent the occurrence of moderate enamel fluorosis. EPA has indicated that the SMCL was intended to reduce the severity and occurrence of the condition to 15% or less of the exposed population. No new studies of the prevalence of moderate enamel fluorosis in U.S. populations are available. Past evidence indicated an incidence range of 4% to 15% (50 Fed. Reg. 20164 [1985]). The prevalence of moderate cases that would be classified as being of aesthetic concern (discoloration of the front teeth) is not known but would be lower than 15%. The degree to which moderate enamel fluorosis might go beyond a cosmetic effect to create an adverse psychological effect or an adverse effect on social functioning is also not known.
RECOMMENDATIONS
-
Additional studies, including longitudinal studies, of the prevalence and severity of enamel fluorosis should be done in U.S. communities with fluoride concentrations higher than 1 mg/L. These studies should focus on moderate and severe enamel fluorosis in relation to caries and in relation to psychological, behavioral, and social effects among affected children, their parents, and affected children after they become adults.
-
Methods should be developed and validated to objectively assess enamel fluorosis. Consideration should be given to distinguishing between staining or mottling of the anterior teeth and of the posterior teeth so that aesthetic consequences can be more easily assessed.
-
More research is needed on the relation between fluoride exposure and dentin fluorosis and delayed tooth eruption patterns.




























