M
Secondary Conditions with Spinal Cord Injury
William A. Bauman*
The secondary consequences of spinal cord injury may be medical, neurological, musculoskeletal, or urological. This paper discusses the medical consequences of spinal cord injury and describes a few of the pulmonary, cardiac, body compositional, metabolic, gastrointestinal, and dermatological issues confronting individuals with such injuries. In another paper presented at the IOM workshop, Margaret Turk (Appendix J) listed the secondary medical disabilities that are associated with spinal cord injuries and suggested that they have been accepted into mainstream medical knowledge, which is quite different than what was accepted just a few years ago.
PULMONARY AND CARDIOVASCULAR DISEASES
In the 1940s and 1950s most individuals with spinal cord injuries died of urinary complications soon after their injury, but today their longevity approaches that of the general population. Because individuals with spinal cord injuries are living longer, researchers have the opportunity to appreci-
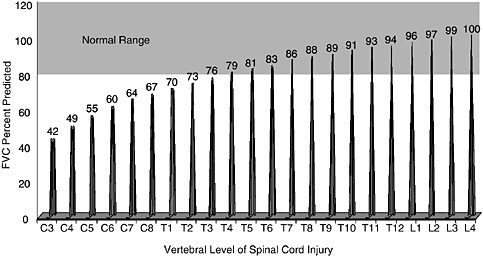
FIGURE M-1 Fitted values for percentage of forced vital capacity (FVC) predicted by level of complete motor lesions. C = cervical; T = thoracic; L = lumbar.
SOURCE: Compiled from data presented by Linn et al. (2001).
ate their secondary disabilities. In individuals with chronic spinal cord injuries, as in the able-bodied population, the common causes of morbidity and mortality are pulmonary and cardiovascular diseases. For example, Gale Whiteneck has found that, similar to the able-bodied population, cardiovascular disease is a leading cause of death in those with spinal cord injuries (Whiteneck et al., 1992). He and his colleagues have reported that among individuals who survive more than 30 years after their injury, 46 percent of all deaths are the result of a fatal cardiovascular event; among those older than 60 years, cardiovascular disease is responsible for 35 percent of all deaths. Heart and lung diseases may not be an immediate cause of death, but they potentially cause further functional impairment and require additional expenditures of resources in those with greater disabilities.
Individuals with spinal cord injuries are classically described as having restrictive ventilatory dysfunction, although in those with higher cord lesions, there is also evidence of airflow obstruction. The higher the spinal cord lesion that an individual has, the greater compromise of the muscles of respiration and the more difficult it is to breathe and cough effectively. If cough is reduced or absent, the clearance of secretions is impaired, which, in turn, can lead to atelectasis and, possibly, pneumonia. Those individuals who have lesions that are at thoracic level 4 or higher have been reported to have an ability to forcibly exhale that falls below the normal range, as evidenced by a forced vital capacity below 80 percent of the levels predicted for able-bodied subjects matched for age, gender, race, and height (Figure M-1).
At present, the clearance of pulmonary secretions for such individuals is accomplished by pharmacological interventions, by the use of pulmonary rehabilitation modalities, or with mechanical devices, including those that produce insufflation-exsufflation and those that electrically stimulate the muscles used for respiration. However, these interventions are often inadequate. As such, therapeutic strategies need to be developed to help those with higher spinal cord lesions to cough more effectively. If such interventions are efficacious, they would be expected to reduce the pulmonary causes of morbidity and mortality.
Individuals with cervical spinal cord injuries have heightened cholinergic airway tone and exhibit nonspecific airway hyperreactivity similar to that found in asthmatic subjects. These individuals also report worsening breathlessness after exposure to cold air, hot air, and secondary smoke. Inhaled bronchodilators are efficacious in improving airflow in those with higher cord lesions, although it has not been determined whether the regular use of these medications is associated with reduced morbidity or mortality. It is also not known whether exposure to common air pollutants, such as sulfur dioxide, causes bronchoconstriction in those with tetraplegia, although these pollutants might be expected to cause airway hyperreactivity. Members of my research unit will address this question in collaboration with Henry Gong, Chief of Environmental Health Service, Rancho Los Amigos National Rehabilitation Center.
METABOLIC SYNDROME
Those with spinal cord injuries have an increased tendency to develop what is now commonly referred to as the “metabolic syndrome.” These individuals become insulin resistant, have associated carbohydrate and lipid abnormalities, and tend to be relatively overweight. Furthermore, those with paraplegia have an increased prevalence of hypertension, a condition not found in individuals with higher cord lesions.
Lipid Abnormalities
The primary lipid abnormality in those with spinal cord injuries is a low serum high-density lipoprotein (HDL) cholesterol (“good” cholesterol) level. The proportion of individuals with spinal cord injuries with normal serum low-density lipoprotein (LDL) cholesterol concentration, a modifiable risk factor for coronary artery disease, is similar to that in the able-bodied population. However, normal LDL levels may lull the health care provider into a sense of complacency that may be ill founded. This possibility is discussed below in greater detail.
The protective effect of serum HDL cholesterol is predominantly by
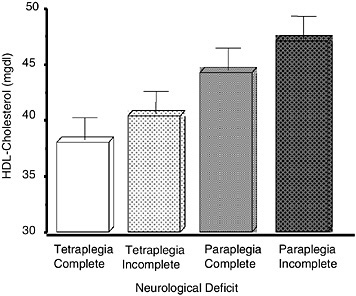
FIGURE M-2 Level of HDL cholesterol by extent of neurological deficit.
SOURCE: Compiled from data presented by Bauman et al. (1998a).
reverse cholesterol transport, which removes cholesterol from the periphery (vessel wall and macrophages) and transports it to the liver. Other beneficial mechanisms of action of serum HDL cholesterol include antioxidant, anti-inflammatory, direct vascular, antiplatelet, and anticoagulant effects. When the serum HDL cholesterol falls below 40 milligrams per deciliter (mg/dL), the morbidity risk ratio rises above unity.
Higher, more complete spinal cord lesions result in greater neurological impairment, which are associated with lower serum HDL cholesterol levels; those who have the least impairment have the highest serum HDL cholesterol levels (Figure M-2). At present, there is no specific recommendation for a therapeutic goal for the serum HDL cholesterol level. However, the Framingham study has shown that for every 1-milligram-per-deciliter (mg/ dL) fall in the serum HDL cholesterol concentration, there is about a 2 to 3 percent increase in the risk of having a cardiac event (Castelli et al., 1986).
Interventions used to raise the serum HDL cholesterol level, as in the able-bodied population, include diet, activity, and drug therapy. A three-center collaborative study (sponsored by the National Institute of Disability and Rehabilitation Research of the U.S. Department of Education) is under way to investigate the effect of Niaspan, a long-acting niacin preparation, on increasing HDL cholesterol levels and reducing the rate of vascular disease among individuals with spinal cord injuries. Smoking cessation is also associated with a rise in serum HDL cholesterol levels.
The conventional risk factors have been shown to account for only about half the total risk of a cardiac event. Thus, it may be worthwhile to touch on other emerging risk factors for coronary artery disease: LDL particle number, the lipoprotein(a) concentration, and the plasma homocysteine level. Evidence indicates that individuals with the metabolic syndrome have smaller, denser, and more atherogenic LDL particles. For the same absolute level of serum LDL cholesterol, if the amount of LDL particles in the circulation is increased, the risk of vascular disease is increased. If the caring physician were to base a therapeutic decision solely on the absolute concentration of serum LDL cholesterol, no treatment may be initiated. However, the risk of coronary artery disease may be elevated if the number of LDL particles is considered, as has recently been shown in several epidemiological studies.
Higher levels of lipoprotein(a) are atherogenic. It had been thought that the level of activity affected the serum lipoprotein(a) concentration. Contrary to expectation, the distribution of lipoprotein(a) levels in individuals with spinal cord injuries was similar to that in an age- and a gender-matched able-bodied population (Bauman et al., 1998b).
Elevated plasma homocysteine levels are vasotoxic. The concentrations of plasma homocysteine have been reported to be higher in those with spinal cord injuries than in a reference able-bodied population (Bauman et al., 2001).
Insulin Resistance
What are the determinants of insulin resistance? Body composition and an individual’s level of activity largely influence insulin sensitivity. Increased adiposity and decreased muscle mass are associated with insulin resistance, as are decreased levels of activity and fitness.
Changes in body composition in individuals with spinal cord injuries occur immediately after the acute injury in a dramatic fashion and continue insidiously for years. There is an obvious and immediate loss of muscle tissue after an acute spinal cord injury, but for decades after the injury there is also a progressive, incremental loss of lean body tissue and a relative gain of adiposity. The mechanisms for this include paralysis and immobilization, as well as a possible reduction in anabolic forces (serum testosterone and growth hormone/insulin-like growth factor levels) and an elevation of catabolic hormone (angiotensin 1 and cortisol) levels. A study performed in conjunction with the Rancho Los Amigos National Rehabilitation Center showed that the percentage of total lean tissue in the body declined more rapidly in individuals with spinal cord injuries of all ages than in a matched able-bodied population (Figure M-3).
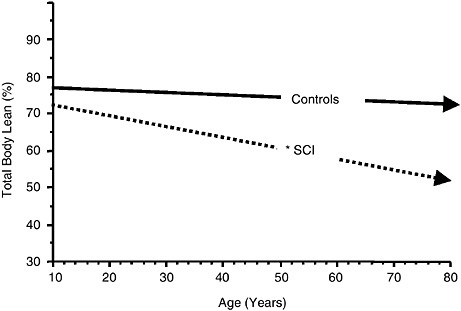
FIGURE M-3 Association between the percentage of total percent lean tissue in the body and age for able-bodied controls (solid arrow; slope = –0.102; r2 = 0.02) compared with that for individuals with spinal cord injuries (SCI) (dashed arrow; slope = –0.275; r2 = 0.10) (*, p < 0.0001).
SOURCE: Compiled from data presented by Spungen et al. (2003).
In the able-bodied population, the body mass index (BMI) is a surrogate measure of adiposity. A person with a spinal cord injury who has a BMI of 25.0 kilograms per meter squared (kg/m2) has 10 to 15 percent more total body fat than an able-bodied individual with the same BMI (Figure M-4). Therefore, this commonly relied upon surrogate measure of adiposity in the able-bodied population grossly underestimates the true level of adiposity in those with spinal cord injuries.
Individuals with the highest and the most complete spinal cord injuries are at the lowest end of the activity spectrum. They have lost the greatest amount of muscle and are relatively fatter than individuals with lower cord lesions. Is there a greater risk of developing insulin resistance and problems with carbohydrate handling in those with the greatest neurological impairment? Those with high and complete spinal cord injuries have a 73 percent chance of having an abnormality in the ability to handle oral carbohydrates, either impaired glucose tolerance or diabetes mellitus, whereas other groups with spinal cord injuries (incomplete tetraplegia, complete paraple-
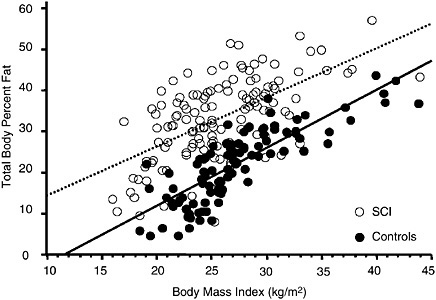
FIGURE M-4 Relationship of percent body fat to BMI for individuals with spinal cord injuries (SCI) compared with that for controls.
SOURCE: Spungen et al. (2003). Used with permission.
gia, and incomplete paraplegia) have significantly lower percentages (Figure M-5). Individuals with higher cord lesions (tetraplegia) have a higher prevalence of hyperinsulinemia than those with lower cord lesions (53 and 37 percent, respectively).
Individuals with spinal cord injuries have a cluster of risk factors for heart disease. What can be done to favorably modify the risk? The use of oral hypoglycemic agents in the general population has been shown to delay the progression from normal glucose tolerance or impaired glucose tolerance to diabetes. Serum HDL cholesterol may be raised by increasing the level of activity. The maintenance of a steady exercise routine is inherently difficult in able-bodied persons, and it is certainly no less difficult in those with spinal cord injuries. It should be noted that evidence suggests that small increases in fitness are associated with favorable metabolic changes, such as increases in serum HDL cholesterol levels. Thus, even modest improvements in the level of activity should be considered and pursued. When indicated, diet or pharmacological interventions, or both, should also be used to increase the serum HDL cholesterol concentration. Smoking cessation should be encouraged as another way to favorably affect the lipid profile.
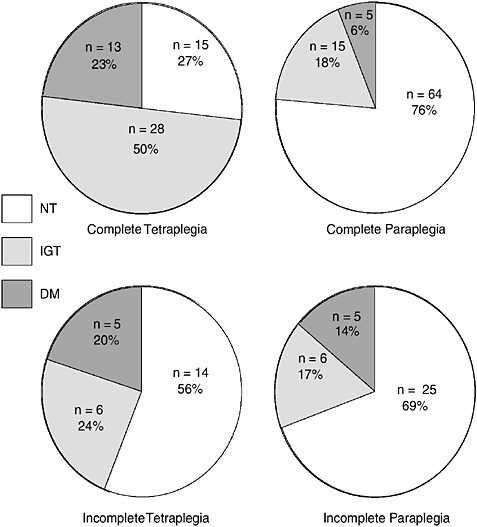
FIGURE M-5 Oral glucose tolerance by level of neurological deficit. NT = normal glucose tolerance; IGT = impaired glucose tolerance; DM = diabetes mellitus.
SOURCE: Compiled from data presented by Bauman et al. (1999).
BOWEL EVACUATION
Individuals with spinal cord injuries often have difficulty with bowel evacuation. Bowel care can be extremely time-consuming and often inadequate, leaving the individual with the potential for accidents. Attendant care may be required as well, causing a loss of independence and privacy. Reduced bowel motility in those with spinal cord injuries is postulated to be due to defective or relatively reduced parasympathetic tone to the gut.
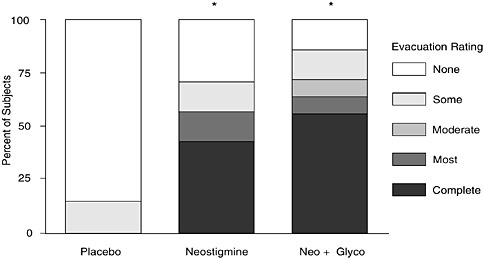
FIGURE M-6 Bowel evacuation after the administration of neostigmine or neostigmine and glycopyrrolate compared with that after administration of a placebo (*, p < 0.01 for both drugs compared with placebo).
SOURCE: Compiled from data presented by Korsten et al. (2005).
Increased gut motility and bowel evacuation after administration of a cholinergic agent have been reported in individuals with spinal cord injuries. Because cholinergic agents are associated with adverse effects on the heart (bradycardia) and lung (bronchoconstriction), glycopyrrolate, a partial cholinergic antagonist or blocker, has successfully been administered in conjunction with neostigmine, a cholinergic medication. Glycopyrrolate successfully blocks the adverse cardiopulmonary effects but preserves the effect of neostigmine on the bowel to produce evacuation (Figure M-6).
OSTEOPOROSIS
Osteoporosis in the appendicular skeleton is a source of morbidity in individuals with spinal cord injuries. Bone loss occurs very rapidly at the time of injury, and although this loss slows, it continues for years after the injury. In a study with identical twins, when an interpair difference score was determined—that is, when the bone mineral density (or bone mineral content) of the twin without a spinal cord injury was subtracted from that of the twin with a spinal cord injury—an estimate of the bone loss in the twin with a spinal cord injury can be generated. It was found that with longer duration of injury, more bone is lost in the lower extremities and pelvis (regions of the skeleton below the level of the lesion).
Bone loses its architectural structure by a loss of trabeculae and intervening struts as early as 1 or 2 years after acute immobilization. Once the normal architecture or connectivity is lost, the quality of bone is severely compromised, and this qualitative loss appears to be irreversible. Thus, bone loss must be prevented at the time of injury. To date, this has not yet been successfully accomplished in a clinically useful manner. The possibility exists that the prevention of bone loss may be feasible by the administration of an antiresorptive agent (e.g., a bisphosphonate) in conjunction with an osteoblastic agent or mechanical stimuli immediately after paralysis.
VITAMIN D DEFICIENCY
Individuals with spinal cord injuries have been shown to be vitamin D deficient. In one study, about one-third of military veterans with spinal cord injuries were vitamin D deficient, as were those at university hospitals and other community medical centers (unpublished findings). In the presence of vitamin D deficiency, parathyroid hormone (PTH) levels are elevated. An increase in the PTH level is often associated with increased bone turnover and bone loss. The Food and Nutrition Board of the Institute of Medicine recommends the consumption of 200 units of vitamin D per day until age 50 years and 400 units per day in those aged 50 years and older. In one study, 800 units of vitamin D per day were provided for 12 months to 40 individuals with spinal cord injuries (Figure M-7). At the baseline, 33
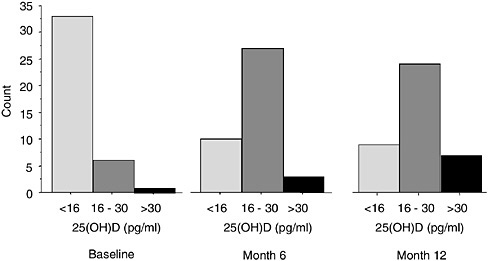
FIGURE M-7 Distribution of serum 25-hydroxyvitamin D [25(OH)D] in 40 individuals with spinal cord injuries who received supplementary vitamin D (800 units per day for 12 months).
SOURCE: Bauman et al. (2005). Used with permission.
subjects (83 percent) had vitamin D levels that were below the absolute lower limit of normal. After 12 months of vitamin D replacement therapy, 9 subjects (23 percent) had levels that remained below the normal range, and after 12 months 23 subjects (58 percent) had levels between 16 to 30 picograms per milliliter (pg/mL). Individuals with vitamin D levels between 16 and 30 pg/mL may be referred to as relatively vitamin D deficient because the plateau is not yet reached for maximum vitamin D-facilitated calcium absorption or for maximum PTH suppression. The significance of preventing osteoporosis would be to improve employment and personal activities, as well as afford psychological benefits.
PRESSURE ULCERS
Pressure ulcers occur in all immobilized individuals and are common in those with spinal cord injuries. They are a tremendous source of morbidity and carry with them a high cost of care. The cost of care rendered for pressure ulcers in hospitals, nursing homes, and home care nationwide has been estimated to be about $8 billion to $10 billion each year. In January 2005, the Cooperative Studies Program of the U.S. Department of Veterans Affairs funded a study to address pressure ulcer care in veterans with spinal cord injuries. The primary objective is to determine if inpatients with spinal cord injuries who have a full-thickness pressure ulcer of the pelvic region and who receive optimized clinical care and an oral anabolic agent for 24 weeks or less have a greater percentage of full healing than those who receive placebo and the same clinical care. The expectation is to learn the percentage of full-thickness ulcers that healed completely; the healing rate; and the effects of nutrition, inflammatory, and endocrine factors on pressure ulcer healing.
CONCLUSION
In summary, most individuals with spinal cord injuries have learned to adapt to being paralyzed. The secondary complications may have a greater impact on quality of life than the loss of ambulation. The knowledge gained from studying the secondary consequences of spinal cord injuries can be transferred, in large measure, to other disabilities or immobilizing conditions. The cost of investigating the problems associated with the medical consequences of spinal cord injuries is slight compared with the cost of care after neglecting them.
REFERENCES
Bauman WA, Spungen AN. Carbohydrate and lipid metabolism in chronic spinal cord injury. Journal of Spinal Cord Medicine 2001; 24:266–277.
Bauman WA, Adkins RH, Spungen AM, Kemp BJ, Waters RL. The effect of residual neurological deficit on serum lipoproteins in individuals with spinal cord injury. Spinal Cord 1998a; 36:13–17.
Bauman WA, Adkins RH, Spungen AM, Herbert R, Schecter C, Smith D, Waters RL. Individuals with extreme inactivity do not have abnormal serum Lp(a) levels. Horm Metab Res 1998b; 30:601–603.
Bauman WA, Adkins RH, Spungen AM, Waters RL. The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord 1999; 37(11):765–771.
Bauman WA, Adkins RH, Spungen AM, Waters RL, Kemp BJ, Herbert V. Levels of plasma homocysteine in a population of persons with spinal cord injury. J Spinal Cord Med 2001; 24:81–86.
Bauman WA, Morrison NG, Spungen AM. Vitamin D replacement therapy in persons with spinal cord injury. Journal of Spinal Cord Medicine 2005; 28:203–207.
Castelli WP, Garrison RJ, Wilson PWF, Abbott RD, Kalousdian S, Kannel WB. Incidence of coronary heart disease and lipoprotein cholesterol levels: the Framingham Study. Journal of the American Medical Association 1986; 256:2835–2838.
Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, Jacobs DR Jr, Bangdiwala S, Tyroler HA. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 1989; 79(1):8–15.
Korsten MA, Rosman AS, Ng A, Cavusoglu E, Spungen AM, Radulovic M, Wecht J, Bauman WA. Infusion of neostigmine-glycopyrrolate for bowel evacuation in persons with spinal cord injury. American Journal of Gastroenterology 2005; 100(7):1560–1565.
Linn WS, Spungen AM, Gong H Jr, Adkins RH, Bauman WA, Waters RL. Forced vital capacity in two large outpatient populations with chronic spinal cord injury . Spinal Cord 2001; 39(5):263–268.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr., Waters RL, Bauman WA. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. Journal of Applied Physiology 2003; 95:2398–2407.
Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA, Krishnan KR, Menter RR, Nuseibeh I, Short DJ, et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992; 30(9):617–630.












