5
The Medical Examination and Disability Rating Process
Processing claims for veterans disability compensation, including determining the ratings, is the responsibility of the Veterans Benefits Administration (VBA), one of the three major organizations within the Department of Veterans Affairs (VA).1 VA established VBA in 1953 (then called the Department of Veterans Benefits) to administer the GI Bill and the compensation and pension program.
VBA’s mission is “to provide benefits and services to the veterans and their families in a responsive, timely, and compassionate manner in recognition of their service to the nation” (VA, 2007e). According to VA’s strategic plan, disability compensation is part of strategic goal 1: “Restore the capability of veterans with disabilities to the greatest extent possible, and improve the quality of their lives and that of their families.” To achieve this goal, VA has set out specific program objectives in its strategic plan. The objective most relevant to the disability compensation program is objective 1.2: “Provide timely and accurate decisions on disability compensation claims to improve the economic status and quality of life of service-disabled veterans” (VA, 2006c).
Chapter 4 addressed the effectiveness of VA’s Schedule for Rating Disabilities (Rating Schedule) in assessing degree of disability for impairment purposes, with a particular focus on whether it is medically up to date and whether it is constructed appropriately to measure severity of impairment, limitation of function, quality of life, or extent of disability. This chapter
addresses the process by which the Rating Schedule is applied, focusing on the timeliness, accuracy, and consistency of decisions on veterans claims.
The key medical aspects of the disability claims process are
-
development of medical evidence, such as information about degree of impairment, functional limitation, and disability, which usually includes a disability examination conducted by a VHA clinician or medical contractor;
-
the rating process, in which the medical evidence is compared with the criteria in the Rating Schedule and a percentage rating is determined; and
-
the appeal process, in which the adequacy and meaning of the medical evidence is often the central question.
ORGANIZATION OF THE VETERANS BENEFITS ADMINISTRATION
VBA is an organization of about 13,000 employees. Staffing in fiscal year (FY) 2006 was 12,810 full-time equivalents (FTEs) and is estimated to be 13,104 FTEs in FY 2007. Approximately half the staff (an estimated 6,425 in FY 2007) is directly devoted to administration of the disability compensation program (VA, 2007b). VBA has 57 regional offices, including at least one in every state in the nation (except Wyoming, which is served by the Denver, Colorado, regional office), as well as offices in Puerto Rico and the Philippines, and additional locations in Korea and Germany.
Within VBA, the Compensation and Pension (C&P) Service administers the disability compensation program. C&P Service also administers the dependency and indemnity compensation, death compensation, disability pension, death pension, burial benefits, automobile allowance/adaptive equipment, clothing allowance, and specially adapted housing programs.2
Each regional office includes a veterans service center (VSC), which is the component that processes disability compensation claims. These centers function under a standardized structure called the claims process improvement (CPI) model, which was recommended in 2001 by the Claims Processing Task Force appointed by the VA secretary to address the growing backlog of claims.3 The model was designed to increase efficiency in
|
2 |
The other program components of VBA are the Vocational Rehabilitation, Education, Loan Guaranty, and Insurance Services. |
|
3 |
These descriptions of the organization and structure of a VSC are based on information provided to the Institute of Medicine (IOM) staff by the Baltimore, Maryland, Regional Office, as well as VA’s Compensation and Pension Adjudication Procedure Manual, M21-1MR, Part III, Subpart I, Chapter 1. http://www.warms.vba.va.gov/admin21/m21_1/mr/part3/subpti/ch01.doc (accessed February 28, 2007). |
processing compensation and pension claims and to reduce the number of errors. The model was fully implemented in 2002, and it established a consistent organizational structure and standard work processes across all regional offices.4 The model
-
requires triage of incoming mail and analysis of incoming claims;
-
emphasizes the importance of complete and accurate development of claims by veterans service representatives (VSRs) specially trained to do the work; and
-
promotes specialization that improves quality and the expeditious handling of claims, while at the same time allowing management the flexibility to adjust resources to meet the demands of changing workload requirements.
Specialized Team Structure
Each VSC uses six separate teams specialized to handle specific steps in the compensation claim process.
Public Contact Team
The public contact team handles personal interviews and telephone inquiries. Team members assist walk-ins, answer telephones, answer routine correspondence (including e-mails), respond to veterans assistance inquiries, and address outreach and fiduciary issues.
VSRs on the public contact team interview veterans and collect as much information as possible to complete a veteran’s claim. If the veteran provides a birth certificate and the master record indicates an award can be prepared immediately, a VSR on the public contact team can prepare the veteran’s award. If additional records are needed, such as from a VA medical center, or if the veteran was recently released from the military and his or her service medical records and separation examination are on record, the public contact team will forward the claim to the triage team.
The public contact team’s regular outreach activities include contacts with veterans service organizations (VSOs), nursing homes, state fairs, stand-downs, and benefit clinics.
Personnel on the public contact team include a
-
coach (GS-13);
-
assistant coach (GS-12);
-
VSR (rotational) (GS-11);
-
public contact and outreach specialist (GS-10);
-
public contact specialist (GS-9);
-
field examiner (GS-10);
-
legal instrument examiner (GS-9); and
-
intake specialist (GS-7).
One of the primary objectives of the public contact team is to promote a bilateral exchange of information with the triage team.
Triage Team
The triage team helps coordinate the work of the other specialized teams. Team members review, control, and process all incoming mail. They also process actions that can be completed with little or no review of the claim folder.
Personnel in the triage team include a
-
coach (GS-13);
-
assistant coach (GS-12);
-
rating VSR (GS-12);
-
senior VSR (GS-12);
-
VSR (GS-11);
-
claims assistant (GS-6);
-
file bank coach (GS-6); and
-
file clerk/program clerk (GS-4).
Predetermination Team
The predetermination team’s primary role is to develop evidence necessary for a rating to be made. This team is responsible for most of the medical development activity in the following cases:
-
original and reopened compensation;
-
compensation claimed due to injury or death caused by VA medical care or evaluation;
-
original and reopened disability pension;
-
original and reopened dependency and indemnity compensation (DIC); and
-
basic eligibility issues requiring a rating decision.
Staff on the team also prepare administrative decisions, including decisions on
-
character of discharge;
-
line of duty;
-
willful misconduct;
-
deemed valid marriage (death claims); and
-
common law marriage (live claims).
Personnel in the predetermination team are the same as in the triage team.
Rating Team5
The rating team makes decisions on claims that require consideration of medical evidence. Rating VSRs (RVSRs) on the rating team rate claims that have been certified by the predetermination team as “ready to rate.” They may prepare a rating for partial grant if there is insufficient evidence to rate all of a veteran’s medical conditions (referred to as issues), but there is sufficient evidence to make an award on one or more issues. In such a case, the rating specialist rates the issue(s) ready to be rated, prepares a separate deferred rating for the unresolved issues, and returns the claims file to the predetermination team for further development.
Personnel on the rating team include a
-
coach (GS-13);
-
assistant coach (GS-12);
-
RVSR (GS-12); and
-
claims assistant (GS-6).
Postdetermination Team
The postdetermination team develops evidence for non-rating issues, processes awards, and notifies claimants of decisions. This team also completes entitlement determinations for issues that do not require a rating, such as
-
accrued benefits;
-
apportionment decisions;
-
competency issues;
-
income changes;
-
original pension;
-
dependency issues;
-
burials;
-
death pension;
-
hospital adjustments;
-
specially adapted housing; and
-
the Civilian Health and Medical Program.
Personnel on the postdetermination team include a
-
coach (GS-13);
-
assistant coach (GS-12);
-
senior VSR (GS-12);
-
VSR (GS-11); and
-
claims assistant (GS-6).
Appeals Team
The appeals team handles decisions with which claimants have formally disagreed (i.e., appealed). The appeals team processes both appeals submitted by veterans and cases returned by the Board of Veterans’ Appeals (BVA) for further development, called remands. The appeals team is also responsible for development of remands, which may involve returning the case to VHA for a medical examination or opinion and for making a decision on the basis of the additional information. If the adjudicator reaffirms the original denial of the case, the case is sent back to BVA for review and decision. The team is intended to increase the level of accountability and maintain control over the appeal workload.
Personnel on the appeals team include a
-
coach (GS-13);
-
decision review officer (GS-13);
-
senior VSR (GS-12);
-
RVSR (GS-12);
-
VSR (GS-11);
-
claims assistant (GS-6); and
-
file clerk/program clerk (GS-4).
Role of the VSR and RVSR
VSRs on the public contact, triage, predetermination, postdetermination, and appeals teams perform a vital role in the compensation claim adjudication process. They conduct interviews, identify issues, gather relevant evidence, adjudicate certain claims, authorize payments, and input data for award generation and notification of the veteran. However, the key staff person in the actual disability rating is the RVSR, who is on the
rating team. The rating team and the disability rating produced by that team is the central component of the veterans disability compensation claims process.6
The RVSR serves as the decision maker for most claims involving rating decisions. He or she analyzes claims, applies the Rating Schedule, and prepares rating decisions that inform the VSR or claimant of the decision and the basis for the decision. There is routine collaboration between the RVSR and the other members of a given team, which includes VSRs and the decision review officer (DRO). The RVSR is also available to discuss claims with VSO representatives. In addition, the RVSR may directly interact with the veteran and his or her representative or advocate.
An RVSR is required to analyze claims to determine
-
if diseases and injuries were incurred or aggravated by military service in the line of duty for purposes of compensation, hospital and outpatient treatment, provision of prosthetics, vocational training, and related employment and compensation benefits;
-
a need for examination, reexamination, and hospitalization for observation of veterans and their dependents and the character of these examinations; and
-
the competency of veterans, their dependents, and beneficiaries, and the permanent incapacity of a veteran’s children or widow or widower for self-support, as well as testamentary capacity for insurance purposes.
As needed, the RVSR may ask the VSR to initiate action to obtain evidence needed to support a veteran’s claim. In some cases, the RVSR monitors the claim to eliminate unnecessary delays.
The RVSR determines
-
service connection;
-
percentage of disability;
-
permanent and total disability;
-
entitlement to compensation, pension, and vocational training;
-
medical and dental treatment;
-
automobiles or other conveyances;
-
insurance;
-
specially adapted housing;
-
dependent education allowances; and
-
other ancillary benefits.
He or she is fully accountable for proper analysis, appropriate development, proper application of the Rating Schedule, and final rating determinations.7
MEDICAL EVALUATION PROCESS
Claims for disability compensation are initiated when a veteran files an application, either online or at a regional office. VA rules require that “[a] specific claim in the form prescribed by the Secretary must be filed in order for benefits to be paid to any individual under the laws administered by VA.”8 However, any communication or action indicating an intent to apply for benefits from a claimant or his or her representative may be considered an informal claim.9
In 1998, VA and the Department of Defense (DoD) established a program called Benefits Delivery at Discharge (BDD) to help servicemembers initiate a disability compensation claim at their military bases prior to being discharged. The program is in effect in 140 locations in the United States, Korea, and Germany. It currently operates under a 2004 memorandum of agreement between VA and DoD to create a cooperative separation medical examination process to ease the transition from service to veteran status. The BDD program “enables separating service members to file disability compensation claims with VA staff at military bases, complete physical exams, and have their claims evaluated before, or closely following, their military separation” (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2007a). In FY 2006, 40,600 claims were filed through the BDD program (about 5 percent of the compensation claims for that year) (VDBC, 2007). BDD sites took in 30,000 claims in FY 2004 and 35,000 in FY 2005 (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2005c). VA reports that the BDD process reduces the average time for an adjudication decision to approximately 60 days (compared with 160–180 days for processing regular claims) (U.S. Congress, Senate, Committee on Veterans’ Affairs, 2007). VA’s goal is to have 65 percent of the original claims made by veterans within the first year after release from active duty filed at a BDD site (the actual percentage in FY 2006 was 50 percent) (VA, 2006). In 2005, VBA consolidated the rating of BDD claims in two regional offices to “bring greater consistency of decisions on claims filed by newly separated veterans” (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2005a).
In addition to BDD, which is not available to wounded or injured servicemembers being considered for separation for inability to perform their duties, DoD provides VA a monthly list of servicemembers referred to a physical evaluation board by a medical evaluation board.10 The list enables VA to contact servicemembers likely to be separated while they are still in the service to facilitate their transfer to VA health care and benefits when they separate. In spinal cord injury cases, DoD and VA have a memorandum of understanding under which active duty servicemembers can be treated in VHA’s specialized spinal cord injury centers. More recently, a similar arrangement was made for treatment of traumatic brain injury (TBI) and polytrauma cases in VHA’s TBI and polytrauma centers. As of the end of FY 2006, DoD had sent VA contact information for 13,622 individuals (U.S. Congress, Senate, Committee on Veterans’ Affairs, 2007).
On receipt of a “substantially complete application” (which includes the claimant’s name, his or her relationship to the veteran, sufficient service information for VA to verify the veteran’s service and claimed medical condition or conditions), VA will begin to process the claim. In accordance with the Veterans Claims Assistance Act (VCAA) of 2000, VA has a “duty to assist” the claimant. VA must give the claimant written notification of the evidence necessary to substantiate the claim. It must also tell the claimant whether VA or the claimant is responsible for obtaining that evidence. VA must make reasonable efforts to obtain relevant records not in the custody of the federal government, and it must make as many requests as necessary to obtain relevant records within the custody of federal departments or agencies, including the veteran’s service medical records and VA records of examination or treatment. However, VA encourages applicants to submit copies of their own medical records to expedite the claim (Box 5-1).
The evidence development phase of disability claims processing is often the most time-consuming part of the entire process. Multiple requests may be necessary to obtain needed information. This phase of the claims process is managed by the predetermination team in the VSC. The team sets diaries (deadline dates) for receipt of requested information, then determines the need for a VA medical examination to assess the current level of disability or to provide a medical opinion about whether the current disability is related to the veteran’s military service (referred to as “medical nexus”).
|
BOX 5-1 Excerpt from VA Publication: Understanding the Disability Claim Process What VA Does After It Receives Your Claim After VA receives your Application for Compensation, it sends you a letter. The letter explains what VA needs in order to help grant your claim. It states how VA assists in getting records to support your claim. The letter may include forms for you to complete, such as medical releases. They help VA obtain pertinent medical records from your doctor or hospital. You should try to complete and return all forms VA sends within a month. Your claim can often be processed more quickly if you send a copy of your own medical records. What Records VA Obtains to Support Your Claim VA then attempts to get all the records relevant to your claimed medical conditions from the military, private hospitals or doctors, or any other place you tell us. The person who decides your claim (called a Rating Veterans Service Representative) may order a medical examination. This examination is free of charge. It is extremely important that you report for your examination at the scheduled time to avoid delaying your claim. SOURCE: VA (2007f). |
Compensation and Pension Examinations
According to VA, “The purpose of C&P examinations is to provide the medical information needed to reach a legal decision about a veteran’s entitlement to VA monetary benefits based on disability” (Brown, 2003). Obtaining a C&P medical examination is part of VA’s duty to assist the applicant. An examination is required
-
when a veteran files a claim for service connection and submits evidence of disability;
-
when a service-connected veteran asserts a worsened condition;
-
to provide medical nexus;
-
to reconcile diagnoses;
-
as directed by BVA; and
-
as required by regulation (Pamperin, 2006).
VA may accept a medical report from a private physician if it is “adequate for rating purposes.”11 However, C&P examinations are ordered in most disability compensation claims for several reasons:
-
to obtain current medical information;
-
to obtain information relevant to disability (such as functional impacts of an impairment) rather than the diagnostic and treatment information sought in a standard medical examination; and
-
to have information from someone more independent than the applicant’s treating physician might be.
In FY 2005 VA obtained more than a half million C&P examinations. VHA performed 84 percent of these examinations in its own medical facilities, and the remaining 16 percent were obtained from a contract examination provider (QTC, 2006). Examinations from VHA generally take about 35 days to complete, and those from the contract provider take about 38 days (Pamperin, 2006).
Generally, the predetermination team in the regional office’s VSC determines the kind of examination needed based on the available medical records and uses one or more of 58 examination worksheets (referred to as AMIE worksheets, after the Automated Medical Information Exchange system for which they were originally developed in 1997) to describe for the examiner the specific requirements of the examination. There are separate worksheets for specific diagnoses (e.g., diabetes mellitus, hypertension, cold injury, posttraumatic stress disorder [PTSD]) and for certain body systems (e.g., eye, genitourinary, dental and oral, mental, hemic disorders). There is one sheet for a general medical examination. Although there are 58 different examination worksheets, the 10 most frequently requested examinations account for 67 percent of C&P exams (Brown, 2006b) (Table 5-1).
The first 57 examination worksheets were last thoroughly revised (by a workgroup with representation from VHA, VBA, and BVA) when they were incorporated in the AMIE system in 1997. Using the AMIE system, they can now be downloaded by examiners in the VA medical centers. The 58th worksheet, for social and industrial assessments surveys, was added in 2004, and the diabetes mellitus worksheet was updated the same year. In 2005, the worksheets for eating disorders; initial evaluation of PTSD; review examination for PTSD; joints; mental disorders except PTSD and eating disorders; nose, sinus, larynx, and pharynx; prisoner of war (POW) protocol examinations; and spine were updated (VA, 2007d).
In 2002, another VHA/VBA/BVA workgroup developed the C&P Service Clinician’s Guide (VA, 2002a). The guide includes the worksheets and
TABLE 5-1 The 10 Most Requested Medical Examinations
|
Examination Worksheet |
Percent of Exams |
|
|
1 |
General medical examination |
18.9 |
|
2 |
Joints (shoulder, elbow, wrist, hip, knee, and ankle) |
11.7 |
|
3 |
Audio |
8.7 |
|
4 |
Spine (cervical, thoracic, and lumbar) |
8.4 |
|
5 |
Mental disorders (except initial PTSD and eating disorders) |
5.7 |
|
6 |
Eye |
3.5 |
|
7 |
Initial evaluation for PTSD |
2.8 |
|
8 |
Feet |
2.7 |
|
9 |
Review examination for PTSD |
2.7 |
|
10 |
Skin diseases (other than scars) |
2.7 |
|
Cumulative total |
67.2 |
|
|
SOURCE: Brown (2006b). |
||
additional information on conducting each kind of examination. VA has also developed two more detailed guides for particular examinations: Best Practice Manual for Posttraumatic Stress Disorder (PTSD) Compensation and Pension Examinations (VA, 2001b) and Handbook of Standard Procedures and Best Practices for Audiology Compensation and Pension Examinations (VA, 2004b).
In 2004, VA began fielding online examination templates for each of the AMIE worksheets in graphical user interface format. These “intelligent,” point-and-click templates are designed to structure the information gathering and reporting process, thus increasing completeness, consistency, and timeliness of examination reports. As of April 2005, a version of each of the automated templates was installed in all examination sites (U.S. Congress, House of Representatives, Veterans’ Affairs Committee, 2005b). The templates had been used 290,000 times as of the end of February 2007 and accounted for about 28 percent (21,125 of 75,000) of the C&P examinations performed by VHA that month. Of 102 sites using the templates, 59 completed more than 1,000 in January 2007. According to the director of the Compensation and Pension Examination Program (CPEP), VA is committed to mandating template use, and key stakeholder feedback and refinement activities are underway prior to taking that step (Brown, 2007).
The regional office requesting an examination is responsible for specifying the type of examination required and any special reports or studies needed. The VHA health-care facility decides who will perform the examination and where and how the examination will be conducted. The regional office may request specific specialist examinations, but the physician examiner may also decide if a specialist examination is necessary on a
case-by-case basis (VA, 2006b). If the examination is being conducted on a remanded case, BVA usually requires the examiner to review the entire claims file, including service records, medical records, and previous C&P examination reports.
In addition to medical information, such as the results of tests or examinations, the examiner may be asked to provide an expert opinion on such questions as whether a condition is related to a specific event during service in the military, or a preexisting condition was aggravated in service, or a condition may be a secondary manifestation or consequence of a condition that previously was service connected. In these cases, the examiner is asked to use the following terminology:
-
is due to (100% sure);
-
more likely than not (greater than 50%);
-
at least as likely as not (equal to or greater than 50%); and
-
not at least as likely as not (less than 50%) (VA, 2002a).
The VSC uses the Compensation and Pension Record Exchange (CAPRI) system (the successor to AMIE) to order C&P examinations from VHA. This system still relies on the AMIE worksheets for examination specifications. CAPRI allows more efficient communication between VBA and VHA by directly linking their information systems and thereby providing VBA with direct, online access to VHA medical data (VA, 2005a).
VHA C&P examiners are supposed to conduct the examination in accordance with the format of the AMIE worksheets and the C&P Service Clinician’s Guide (VA, 2002a), but they are not required to use the worksheets to report the examination, as long as they provide
-
an up-to-date, brief medical and industrial history from the date of discharge or the last examination;
-
a record of subjective complaints;
-
a complete description of objective findings stated in concrete terms;
-
a diagnosis of all described conditions;
-
answers to any questions specifically requested in the examination request;
-
opinions specifically requested in the examination request;
-
a diagnosis or notation that a chronic disease or disability was ruled out for each disability, complaint, or symptom listed on the examination request; and
-
the clinical findings required by the rating schedule for the evaluation of the specific disability being claimed (VA, 2006b).
The VSC orders examinations from the contract examination provider, QTC, using the Veterans Examination Request Information System (VERIS). The VSR or other authorized employee enters examination requests on a daily basis. An encrypted file is transferred to QTC. After the examination is complete, the VSR or other authorized employee logs directly into QTC’s secure website to download the completed examinations in batches (Pamperin, 2006). QTC examiners are provided with a template for online reporting but are not required to use it as long as they provide the required information.
If an examination report does not include sufficiently detailed information to support the diagnoses or about the effects of diagnosed conditions on functioning, the RVSR is instructed to return the report as inadequate for rating purposes.
VHA Examiner Qualifications, Training, and Quality Assurance
Training and qualifications of examiners who perform C&P examinations in VHA are monitored by CPEP, a joint initiative between VHA and VBA established in 2001 to improve the C&P examination process. CPEP focuses on the 10 most frequently requested examinations.12 It first establishes baseline performance for examiners, then develops performance improvement initiatives, monitors performance, and provides feedback. It relies on a quality indicator approach, focusing on selected important and representative elements (rather than a comprehensive audit of all possible elements). Core quality indicators apply to all examination types, but there are additional examination-specific quality indicators as well. CPEP has produced regular reports of the top 10 examination types since 2003, based on data collected starting in 2001 (Brown, 2006a,b).
In May 2006, VA’s under secretary for health and under secretary for benefits initiated a mandatory certification procedure for clinicians who perform C&P examinations, directing CPEP to
provide every clinician who performs C&P exams for VHA, whether employee or contractor, the necessary training to have a full understanding of the requirements of the process…. Individuals who meet the training requirements for certification will be tracked, and this data will be made available to the credentialing and privileging authority for their respective healthcare facility.
Although this certification program is still under development, the program will consist of educational content, videotape and web-based training, and testing (Brown, 2006a,b, 2007).
For most examinations, VHA decides on a case-by-case basis the appropriate level of training the examiner must have. However, for initial mental disorder examinations (including PTSD examinations) the examination must be conducted by a board-certified or board-eligible psychiatrist or licensed doctorate-level psychologist or, under their close supervision, by a psychiatry resident, doctorate-level mental health provider, or clinical/ counseling psychologist with a completed one-year internship or residency (VA, 2006e). Auditory examinations must be performed by licensed audiologists.
QTC Examiner Qualifications, Training, and Quality Assurance
QTC Medical Group, Inc. currently provides C&P examinations for 10 VA regional offices and 26 BDD sites, using a network of approximately 1,600 contracted private practitioners. QTC also has clinics in California, Texas, and Virginia, in which examiners are QTC employees. Examiners who perform C&P examinations for QTC must be
-
graduates of an accredited medical school (M.D. or D.O.);
-
licensed to practice medicine in the location(s) where they conduct examinations;
-
board certified or board eligible;
-
clear of Medicare, Medicaid, and any other federal exclusions; and
-
covered by malpractice insurance.
QTC trains its examiners and monitors performance in an internal quality assurance program, which includes a probationary period with review and quality feedback. QTC has full-time quality assurance personnel who review all reports for quality before they are released, ensuring that they adhere to AMIE worksheet requirements. Quality assurance personnel also identify any negative trends, and retrain or dismiss problematic providers (QTC, 2006). The 150 contract psychiatrists who perform PTSD examinations are given additional training (Shahani, 2005).
QTC developed a training manual for its examiners, which was approved by the VBA medical director. It trains examiners either in person or during several conference calls. QTC’s policy is to monitor examiners’ work closely for the first three months. If the work is not satisfactory (that is, examination reports do not meet AMIE worksheet requirements), he or she is released. QTC has a quality control person on each administrative
team who works with examiners to scrutinize each report before it goes to VA .13 As noted above, reports of new examiners are analyzed in detail for the first three months and feedback is provided. To ensure QTC examination quality, the C&P Services’ medical director reviews a random sample of 384 reports each quarter. At least 92 percent of the reports must be complete, and there are financial penalties for failing to meet, and incentives for exceeding, that figure.14
According to the VA inspector general, “There is little difference between the quality of contractor-produced C&P examinations and VA [VHA] examinations and their impact on the degrees of disability that are eventually awarded to the veterans.” This finding was based on a comparison of a set of examination reports from each organization and the results of a survey of raters (VA, 2005b).
THE DISABILITY RATING PROCESS
After all development actions are complete, the VSC predetermination team refers the claim to the rating team for a rating. The rating team reviews all the evidence associated with the claim, makes decisions on issues raised by the claimant, and identifies any inferred issues that should be addressed. The team documents the rating decision in a standard format, using an automated rating preparation system called Rating Board Automation (RBA) 2000. After completing the rating decision, the team routes the claim to the postdetermination team.
The postdetermination team implements the rating decision by preparing either a monetary award or a denial. It also prepares notification letters for the claimant and representative.
When performing a rating evaluation, RVSRs consider all evidence associated with the claim. This includes service medical records, VA medical examination records, clinical summaries from VA medical centers where treatment has been provided to the veteran, and evidence provided from private sources, such as the veteran’s treating physician.
Primary guidance for performing rating evaluations are contained in the Rating Schedule itself, the Compensation and Pension Adjudication Procedures Manual, M21-1MR, and internal program guides. Underlying principles that provide the philosophical base for rating evaluations include (but are not limited to) the following:
-
Each disabling condition shown by a veteran’s service records, or for which he seeks a service connection must be considered on the basis of the places, types and circumstances of his service…. Determinations as to service connection will be based on review of the entire evidence of record, with due consideration to the policy of VA to administer the law under a broad and liberal interpretation consistent with the facts in each individual case (38 CFR 3.303).
-
The veteran will be considered to have been in sound condition when examined, accepted and enrolled for service, except as to defects, infirmities, or disorders noted at entrance in service, or where clear and unmistakable (obvious or manifest) evidence demonstrates that an injury or disease existed prior thereto and was not aggravated by such service. Only such conditions as are recorded in examination reports are to be considered as noted (38 CFR 3.304b).
-
Rating agencies will handle cases affected by change of medical findings or diagnosis, so as to produce the greatest degree of stability of disability evaluations consistent with the laws and VA regulations governing disability compensation and pension. It is essential that the entire record of examinations and the medical-industrial history be reviewed to ascertain whether the recent examination is full and complete, including all special examinations indicated as a result of general examination and the entire case history (38 CFR 3.344).
-
It is the responsibility of the rating specialist to interpret reports of examination in the light of the whole recorded history, reconciling the various reports into a consistent picture so that the current rating may accurately reflect the elements of disability present. Each disability must be considered from the point of view of the veteran working or seeking work (38 CFR 4.2).
-
Every element in any way affecting the probative value to be assigned to the evidence in each individual claim must be thoroughly and conscientiously studied (38 CFR 4.6).
-
Where there is a question as to which of two evaluations shall be applied, the higher evaluation will be assigned if the disability picture more nearly approximates the criteria required for that rating (38 CFR 4.7).
As illustrated by this (partial) list, the RVSR must assess several areas in order to develop a rating decision. All the guiding principles in the Rating Schedule must be considered, as they apply, for each decision component of the rating. These basic decision components include
-
a determination that the veteran has a disabling condition or conditions;
-
a determination as to whether each disability is service-connected;
-
a determination on the evaluation level (10 percent, 20 percent, etc.) to be assigned for each service-connected disability (done through referral to sections 4.71a to 4.150 of the Rating Schedule, where specific disabilities are listed, along with diagnostic criteria and associated evaluation levels); and
-
an effective date for entitlement to payment for each service-connected condition.
RVSRs assign evaluation levels based on the tables, diagnostic codes, and the percentages provided in the Rating Schedule, correlating the medical evidence in the individual case to the criteria and percentages provided in the Rating Schedule.
When multiple conditions have been evaluated, a combined rating evaluation is performed according to a “combined rating table” found in 38 CFR 4.25.
To the extent that the Rating Schedule reflects current medical diagnostic knowledge, assessment of disability, and treatment, the resultant rating evaluation should accurately reflect disability. To the extent that the Rating Schedule is outdated, the resultant rating evaluation will be subject to distortions and imprecision.
The standard rating evaluation decision format contains the following sections: Introduction, Decision, Statement of Evidence, and Reasons and Bases for the Decision. It also includes a section called Coded Conclusion, containing statistical information about the veteran, the specific evaluations, and the combined evaluation. The RVSR signs the completed rating decision.
The discussion above shows that the rating process is complicated and multifaceted. The technicians who execute the ratings are expected to have substantial expertise in VA law and the medical aspects of the Rating Schedule. Rating team personnel are generally grouped together in a section or sections of the VSC. The RVSRs do their evaluations individually, however. They do not have routine access to medical practitioners or legal experts as they conduct their assessments. They have only their training guides and regulations to interpret.
Quality Review Process
VBA’s primary means of assessing the quality of the rating process is a program called Statistical Technical Accuracy Review (STAR). The STAR program was developed in the late 1990s in response to concerns about the accuracy of C&P claims adjudications. In FY 2006, the program was staffed with 18 senior, experienced VSRs and RVSRs from within VBA (VA, 2006). These employees are recruited and managed by the C&P Service.
Most employees are located in Nashville, Tennessee, although some STAR staff work from the VA central office (VACO).
STAR reviews are done based on a standard protocol that asks questions in the following areas:
-
Were all issues in the claim addressed, including inferred issues?
-
Was evidentiary development done properly and thoroughly in accordance with the Veterans Claims Assistance Act?
-
Were decisions on grant or denial, and percentage evaluation assigned, correct?
-
Were payment dates and rates correct?
-
Were decisions properly documented?
-
Were notifications of decisions sent and appropriate?
STAR reviews are conducted by the national staff in Nashville, usually several weeks after the rating decision has been completed.
VA also began a new program, Statistical Individual Performance Assessment, in 2002 to offer immediate feedback on claims processing, including ratings, and to promote accuracy and consistency of claims adjudication. It also was intended to provide performance management results at the individual employee level. The original plan was to have supervisors review 10 cases from each technician every month, correcting errors before decisions were made. The program was absorbed into the employee performance management system.
APPEAL PROCESS15
A veteran (or other applicant, such as a surviving spouse, child, or parent of a veteran) who disagrees with a VA regional office’s decision can file an appeal either to the local regional office (for reconsideration of the original decision) or to BVA. If the veteran chooses to appeal to the regional office, but is still dissatisfied with the decision, he or she may then appeal to BVA. If still dissatisfied, the veteran may file additional appeals (in sequential order) to
-
the U.S. Court of Appeals for Veterans Claims (CAVC);
-
the U.S. Court of Appeals for the Federal Circuit; and
-
the U.S. Supreme Court.
Although a veteran can appeal for any reason, issues frequently appealed include disability compensation, pension, education benefits,
recovery of overpayments, and reimbursement for unauthorized medical services. The two most common appeals are made by veterans who feel that (1) the VA regional office denied them benefits for an impairment (i.e., it was declared not to be service connected) that they believe began while they were in service, and (2) the severity rating assigned to the impairment was too low and an increase in the rating level is warranted (BVA, 2002a).
Appeal Steps
To begin the appeal process, a veteran files a written notice of disagreement (NOD) with the field office from which the disputed decision was issued. For most compensation cases, the appeal must be filed within one year from the date of the decision.
If more than one claim is at issue (e.g., a claim for compensation based on an orthopedic condition and claim for compensation on a respiratory condition), the NOD must be specific about which issue or issues are being appealed. If a veteran is appealing to the local regional office (rather than BVA), he or she may choose to have the case handled in the traditional appellate review process (in which an RVSR handles the appeal) or to have the file be reviewed by a DRO. DROs provide a second review of an appellant’s entire file, and they can hold a personal hearing about an appellant’s claim. DROs are authorized to grant the contested benefits based on the same case record that the local office used to make the initial decision.
After completing any additional development or proceedings, the RVSR or DRO (as appropriate) sends the veteran either a favorable decision on all issues, or a statement of case explaining the reasons for the decision not to allow the appeal, along with VA Form 9, the substantive appeal form, which the veteran may use to ask for a BVA review of the decision. VA Form 9 must be filed within 60 days of the mailing of the statement of case, or within one year from the date VA mailed its decision, whichever is later. (The 60-day period for filing a substantive appeal can be extended for “good cause.”)
On VA Form 9, the veteran states the desired benefit, notes perceived mistakes in the statement of case, and comments on anything with which he or she disagrees. If the veteran submits new evidence or information with the substantive appeal, such as records from recent medical treatments or evaluations, the VA local office prepares a supplemental statement of case, which is similar to the statement of case, but addresses the new information or evidence submitted.
The local VA office sends a letter to the veteran who is appealing when the claims folder is transferred to BVA in Washington, D.C. Generally, the appellant has 90 days (from the date of the letter) or until BVA decides his
or her case, whichever comes first, during which to submit more evidence, request a hearing, or select or change a representative.
At personal hearings, veterans meet with either a DRO at the regional office or a BVA member (at BVA hearings). Personal hearings are informal. Appellants in most areas of the country can choose to hold a BVA hearing, commonly called a travel board hearing, either at the regional office or at the BVA office in Washington, D.C. Some regional offices are also equipped to hold BVA hearings by videoconference with the appellant at his or her regional office and the board member in Washington, D.C., which is considered the most expedient choice. BVA held 2,700 hearings by video-conference in FY 2006, up from 1,300 in FY 2000, and expects this number to continue to rise (BVA, 2006).
After the hearing, a BVA board member will review a transcript of the hearing (if applicable) and the appellant’s file and make a decision either allowing or denying the case. Appeals may be dismissed in certain limited circumstances. However, if BVA cannot make a final decision, it may remand the case (i.e., send the claim back to the regional office) for additional development and a new determination. If after completing the additional development, the local office is again unable to allow the claim, the case is returned to BVA for a final decision.
Board of Veterans’ Appeals
BVA is a quasi-judicial, organizationally independent component of VA that reports directly to the VA secretary and makes final agency decisions with respect to claims for veterans benefits. BVA reviews all appeals for entitlement to veterans benefits on behalf of the VA secretary, including appeals involving claims for service connection, increased disability ratings, individual unemployability, pension, insurance benefits, educational benefits, home loan guaranties, vocational rehabilitation, and dependency and indemnity compensation, and also determinations of duty status, marital status, dependency status, and effective dates of benefits. In FY 2005, 94 percent of the cases were appeals of compensation decisions by regional offices (Terry, 2006a).
The law requires BVA to decide cases on a “first come, first served” basis. To do that, BVA assigns cases a docket number in the order in which cases are received. A veteran may file a motion to advance the case if he or she believes that his or her appeal should be decided sooner than the appeals of others.
BVA decides cases de novo (that is, it makes an entirely new decision, rather than reviewing the prior decision), so it gives no deference to the regional office decision being appealed. Decisions are based only on the law, VA’s regulations, precedent decisions of the courts, and precedent opinions
of VA’s general counsel. BVA performs an analysis of credibility and probative value of evidence and considers all potentially applicable provisions of law and regulations. Final decisions must include
-
findings of fact;
-
conclusions of law;
-
analysis of the reasons and bases for the decision on each material issue of fact and law; and
-
an order granting or denying the appeal (Terry, 2006a).
BVA Organization and Staffing
BVA consists of a chairman, vice chairman, senior deputy vice chairman, 56 veterans law judges (VLJs), 4 of whom are deputy vice chairmen and 8 of whom are chief judges, 248 staff counsel, and other administrative and clerical staff (Terry, 2006a). Staff is organized into four decision teams with jurisdictions covering four geographical regions—the Northeast, Southeast, Midwest, and West (including the Philippines). Each decision team includes
-
1 deputy vice chairman;
-
2 chief judges;
-
11 VLJs;
-
2 senior counsel; and
-
60 counsel and associate counsel.
Each VLJ works with five to six attorneys (counsel and associate counsel) as a small team. The attorneys
review the claims file, research the applicable law, and prepare a comprehensive draft decision or remand document that details the relevant law and evidence. The document and the claims folders are then forwarded to the assigned VLJ for review, approval, revision, and signature (Terry, 2006b).
When an appellant’s docket number is reached, the file is prepared by staff and the decision approved by a VLJ. Each VLJ is expected to complete a minimum of 752 decisions per year as his or her “fair share” of BVA’s total workload and conduct three one-week travel boards to regional offices. Counsel, who draft decisions, are asked to draft at least 156 decisions per year (Terry, 2006b).
BVA Workload
In FY 2006, BVA received 41,802 appeals and issued 39,076 decisions (BVA, 2006). These included 37,295 decisions on compensation cases, of which
-
20 percent involved a grant on at least one issue;
-
46 percent involved a denial of all issues;
-
32 percent involved a remand to the agency of original jurisdiction, meaning the regional office; and
-
2 percent were classified as “other” (BVA, 2006).
Sources of Medical Expertise in BVA
Prior to passage of the Veterans Judicial Review Act of 1988, BVA had always used expert panels to adjudicate claims. Each three-person section of BVA had a physician member “whose medical judgment often controlled the outcome of an appeal” (BVA, 1996b:32).16 BVA physician members acted as adjudicators and as providers of expert advice and medical opinions, and they also helped train BVA’s attorneys (BVA, 1996b).
The 1988 act changed BVA from functioning as a panel of experts to one in which independent judges weigh and consider only the evidence of record. A subsequent series of opinions by the CAVC barred BVA physicians from acting as adjudicators:
In the cases of Gilbert v. Derwinski, Colvin v. Derwinski, and Hatlestad v. Derwinski, the Court held, in essence, that the Board could no longer base its decisions on its own medical expertise, including that of physicians then serving as Board members (BVA, 1996a:18).
Since then, all board members have been lawyers, although there is no requirement that they be lawyers.
In response to the court decisions, BVA converted some of its physicians (two full-time and three part-time) from board members to advisors who provided expert medical opinions on the record when needed to adjudicate a case. They also provided informal advice to attorneys and VLJs, gave educational lectures on medical topics, and reviewed requests for VHA and outside medical advisory opinions “to ensure accuracy in the way in which the evidence is reported and the questions are framed” (BVA, 1997:14). However, using BVA physicians to provide expert opinions was soon barred by court decisions that questioned the fairness and impartiality of BVA’s
own medical advisers (BVA, 2001).17 Because BVA cannot use its own expertise to “fill in the blanks,” it is very reliant on adequate development of medical evidence in the case by the regional office to render a decision, according to BVA’s chairman. It also increases the time BVA attorneys need to analyze the medical evidence in the record, conduct research, and explain the medical principles on which their decisions rely, including citations of independent authority, such as medical treatises, texts, journals, and epidemiological studies (Terry, 2006a).
Currently BVA has a single medical advisor position, filled by a physician:
The medical advisor’s duties are to review draft outside medical opinions for the purpose of advising the originating VLJ as to the proper medical specialist to address the opinion request and whether the questions posed are adequate to elicit a meaningful response from that specialist.
The Medical Advisor also provides training on medical issues to the Board’s VLJs and staff counsel. Additionally, he is available to consult with staff counsel and VLJs to read medical records and provide background information and training on medical issues encountered in review of particular claims. He is not involved in the adjudication of the appeal (Keller, 2007).
BVA also began to obtain expert medical advice from VHA clinicians and, occasionally, the Armed Forces Institute of Pathology (AFIP). It also used its authority to obtain advisory medical opinions from independent experts more frequently:
In an effort to alleviate the need for BVA to remand cases for additional medical information, we established a VHA medical opinion program. The board maintains a list of participating hospitals and their specialty, if any. When a case requires a medical opinion, a hospital is selected according to the particular need, and a specialist prepares an opinion answering the board’s questions. This program cuts the cost and time—sometimes six to nine months—to obtain an independent outside medical opinion (VA, 2000:29).
In FY 2006, for example, BVA requested 643 outside medical opinions (464 from VHA, 4 from AFIP, and 175 from independent medical examiners). This was more than was requested from those sources in 2004 and 2005 (560 and 513, respectively).18
Medical opinions are generally sought for establishing medical nexus, differential diagnosis, unusual or complex issues, and legal issues, such as injury of the veteran being examined by VHA. Medical opinion may be needed to establish service connection when a veteran’s record
-
contains competent evidence of current disability, or persistent or recurrent symptoms of disability;
-
contains supporting evidence of an in-service event, injury, or disease, or presumptive disease or symptoms;
-
indicates claimed disability symptoms may not be associated with service; or
-
does not contain sufficient competent medical evidence to decide the claim (Terry, 2006a).
No specific formula exists to use in weighing medical opinions. BVA may favor the opinion of one competent medical expert over that of another when adequate reasons or bases are provided. Factors weighed include
-
competency of the medical professional or medical evidence provided;
-
use of the correct factual history;
-
adequacy of supporting analysis or basis provided for opinion;
-
consideration of a review of the claims file or a full history of the disability;
-
whether the clinician is the veteran’s treating physician and familiar with his or her medical records and history;
-
level of thoroughness and detail of opinion;
-
equivocality of the opinion;
-
personal interest in the case on the part of the opinion provider;
-
special qualifications or expertise of the opinion provider;
-
contradictory or internally inconsistent statements;
-
differentiation among multiple opinions based on rationale or analyses; and
-
consideration of the benefit of doubt rule if there are multiple conflicting medical opinions (Terry, 2006a).
U.S. Court of Appeals for Veterans Claims
In the event that a claimant is dissatisfied with a final BVA appeals decision, he or she has several options:
-
Accept the decision and take no further action, in which case the decision becomes final;
-
Go back to the regional office and try to reopen the claim;
-
File a motion for reconsideration or to vacate (i.e., an attempt to have the same court withdraw or modify its decision) with BVA;
-
Ask for a rereview of the case because there was a clear and unmistakable error in the BVA decision; or
-
File an appeal with the U.S. Court of Appeals for Veterans Claims.
If BVA denies requested benefits, or it grants less than the maximum benefit available under the law, and the veteran decides to appeal to the CAVC, he or she must file the appeal within 120 days after BVA mailed its decision. Unlike BVA, the court may not receive new evidence. It considers only
-
the BVA decision;
-
briefs submitted by the veteran and VA;
-
oral arguments, if any; and
-
the case record that VA considered and BVA had available.
In cases decided on merit (cases not dismissed on procedural grounds), the court may (1) reverse the BVA decision (i.e., grant contested benefits); (2) affirm the BVA decision (i.e., deny contested benefits); or (3) remand the case back to BVA for rework.
U.S. Court of Appeals for the Federal Circuit and the U.S. Supreme Court
Under certain circumstances, a veteran who disagrees with a decision of the CAVC may appeal to the Federal Circuit Court of Appeals and then to the U.S. Supreme Court.
The court reviews the same record that was considered by BVA; that is, the court does not receive new evidence nor does it hold a trial. Appellants themselves or their lawyers or approved agents may serve as representatives before the court; however, the court directs whether oral argument is held. Either party may appeal a decision made by the CAVC to the Federal Circuit Court of Appeals, and may seek further review in the U.S. Supreme Court.
BVA Quality Assurance and Training
BVA’s Office of Quality Review, headed by the senior deputy vice chairman, oversees a formal quality review (QR) program. The quantitative program began in 1998 with the collection of baseline data, and an ongoing QR process started at the beginning of 1999. Staffing of the QR
unit was increased and the positions made permanent in 2002, including a permanent full-time training coordinator position.
The program reviews every 20th original VLJ decision and every 10th VLJ decision on cases remanded by the CAVC to BVA. This sample size, chosen to achieve a confidence level of 95 percent with a margin of error ±5 percent, is reviewed on an ongoing basis. The review evaluates decisions in five areas:
-
identification of issues;
-
findings of fact;
-
conclusions of law;
-
reasons and bases for decisions; and
-
due process.
A deficiency or error in any of the five areas constitutes a failure. The standard is whether a deficiency or error exists that would be expected to result in a reversal by or remand from the CAVC or a change in the outcome (Terry, 2006a).19
The results of the QR program are the basis for training activities:
-
quarterly “Grand Rounds” training sessions for all VLJs and staff counsel to stay current with changes in the law;
-
training on specific legal issues, conducted by the full-time training coordinator, usually twice a month;
-
periodic “Quality Review Tips,” provided to legal staff;
-
detailed monthly QR statistics for managers;
-
referral of QR errors back to the originating VLJ; and
-
a variety of team-level mentoring and training programs and online indexes and legal research tools for staff (Terry, 2006a).
Medical training occurs on an ongoing basis, and the BVA medical advisor is available for consultation and informal training. BVA training sessions held during the past two years on medical and legal topics involving medical matters included
-
introduction to medical terminology;
-
secondary service connection/Allen cases;
-
presumption of service connection and applying rating criteria when there has been a change in the law;
-
radiation claims;
-
presumption of soundness;
-
POW claims adjudication and medical matters;
-
Agent Orange/herbicide exposure;
-
rating spine disabilities;
-
education and vocational rehabilitation;
-
rating musculoskeletal disabilities—functional limitation and pain (DeLuca criteria);
-
rating disabilities involving injuries to multiple muscle groups (gunshot and shrapnel wounds);
-
multiple opinions—assigning credibility and weight of the evidence when reviewing;
-
special monthly compensation and adaptive equipment;
-
respiratory disorders;
-
rating knee disabilities;
-
total disability ratings based on individual unemployability; and
-
hearing loss and tinnitus.
DISABILITY CLAIMS PROCESS ISSUES: TIMELINESS, ACCURACY, AND CONSISTENCY
Veterans deserve a claims process that is efficient and fair. They should not have to wait long for decisions on disability compensation and other benefits. The decisions should accurately determine eligibility to minimize the number of false negatives (veterans incorrectly denied benefits) and false positives (veterans granted benefits for which they are not eligible). Veterans with similar levels of disability should be treated the same even if they are dealing with different regional offices. And if they appeal, they should receive an accurate decision within a reasonable amount of time.
The VA claims process has long struggled with timeliness, accuracy, and consistency. The importance of adequate medical examinations in achieving timeliness, accuracy, and consistency has been recognized since the early 1990s. But, the most important factor affecting VA’s ability to produce timely, accurate, and consistent decisions is the disability claim workload.
Medical Examination Quality
In 1996, BVA reported that about 70 percent of the cases remanded by BVA to the regional offices included a request for a C&P examination to obtain incomplete or missing medical information (BVA, 1996b). This followed a 1994 VA inspector general’s report critical of C&P medical examinations services, and VBA and VHA were already working to improve the adequacy of medical examinations (VA, 1994). The VA Office of Inspector
General (OIG) reported that 24 percent (95,000 of 405,000) of the C&P examinations had been incomplete in FY 1993, a percentage that had not improved much in FY 1996, when 22 percent were incomplete (VA, 1997b). A C&P examination task force, on which BVA was represented, led to a 2001 memorandum of agreement between VBA and VHA on C&P examination standards and procedures to improve quality, expedite decisions, and reduce remands. The memorandum also established the CPEP program.
CPEP has monitored the quality of C&P examinations performed by VHA clinicians on a monthly basis since October 2003. Earlier, CPEP had identified the 10 most commonly requested C&P examinations and developed quality indicators, some applying to all examinations, some specific to each examination. The indicators were used to assess 110 randomly selected examinations of each type that had been performed in the last quarter of FY 2001. The resulting quality indicator score was 85 percent, but it varied across examination types from 72 percent for joint examinations to 94 percent for mental disorder examinations (VA, 2002c). Overall, 59 percent of the examinations scored 90 percent or better (met or exceeded 90 percent of the quality indicators) and 37 percent scored 100 percent. Most of the errors were omissions of specific data elements, whereas some were omissions of entire worksheets (Brown, 2003). CPEP then analyzed examinations by using the Veterans Integrated Service Network (VISN), finding differences in the percentage of A-level examinations, defined as those that meet 90 percent or more of the quality indicators, which are discussed in the next section, on “consistency.” As a group, the percentage of A-level examination in this first, baseline study was 53.5 percent (Brown, 2006b).
Since 2001, CPEP has led a number of initiatives to improve the percentage of A-level examinations. The initiatives include onsite training sessions, video and computer-based training on the examinations, establishment of the percentage of A-level examinations as a performance goal for the directors of each VISN, and the development of online examination templates with structured data input. In 2006, CPEP was directed to establish a training and certification program for C&P examiners, which is currently under development. Web-based training modules have been developed for some body systems (musculoskeletal, mental, PTSD). Certification tests are in final testing, and audio and eye training modules are next to be developed (Brown, 2007). Deployment of the training and certification program is scheduled for FY 2008.20
In FY 2004 and FY 2005, the VISN performance target for A-level examinations was 64 percent. The average score across VISNs was 82 per-
cent in February 2006, compared with 77 percent in February 2005 and 58 percent in February 2004. All 21 VISNs met the performance target for A-level exams in September 2005, up from 18 in September 2004 (up from 1 in October 2003) (Brown, 2006b). When the target for A-level exams was increased from 64 percent to 83 percent for FY 2006, the number of VISNs meeting the target initially dropped to 9 but improved to 21 in December 2006. The average score across VISNs was 86 percent in January 2007, although the consistently high scoring audio examination had been replaced by the lower scoring diabetes examination among the 10 examinations being scored in October 2006 (Table 5-2) (Brown, 2007). Accuracy of examination reports is a performance measure for VISN directors (VA, 2006d).
CPEP randomly samples 1,470 examination reports each month—7 reports from each of the 10 examination types from each of the 21 VISNs. The sample size is set to produce statistically valid error rates for each VISN on a quarterly basis (VA, 2006d).
CPEP is also addressing the adequacy of regional office requests for C&P examinations. It has been conducting monthly reviews of these requests since early 2004, finding that many were incomplete or inaccurate, as noted in a 2005 GAO report:
For example, of the spine exams requested during the second quarter of fiscal year 2005, 32 percent of the exam requests had at least one error such as:
-
not identifying the pertinent condition;
-
not requesting the appropriate exam;
TABLE 5-2 Rates of A-Level Compensation and Pensions Examinations, by Type of Examination, January 2007
|
Examination Type |
Percent of A-Level Exams |
|
|
1 |
Initial PTSD |
97 |
|
2 |
Eye |
95 |
|
3 |
Mental disorders |
94 |
|
4 |
Diabetes |
89 |
|
5 |
General medical |
88 |
|
6 |
Skin |
85 |
|
7 |
Review PTSD |
82 |
|
8 |
Feet |
79 |
|
9 |
Joints |
78 |
|
10 |
Spine |
71 |
|
|
All 10 examinations |
86 |
|
SOURCE: Brown (2007). |
||
-
not providing clear or useful information in the remarks section of the request;
-
not identifying the specific joint or part to be examined; or
-
not explaining instances in which the exam request contained no telephone number for the veteran who was to be examined (GAO, 2005b).
In August 2005, CPEP revised the set of indicators of examination request quality to focus on content accuracy and exclude non-substantive process errors. It planned to track them for six months to establish a baseline, then provide the regional offices with the results (Mansfield, 2005).
Disability Claims Workload and Timeliness
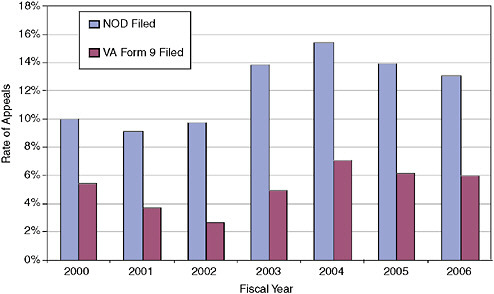
In FY 2006, VA received 806,000 disability-related claims. Most of these (654,000) were from veterans for compensation for service-connected injuries and diseases.21 Compared with the FY 2000 workload, this was a 38 percent increase in disability-related claims and a 56 percent increase in compensation claims (VA, 2006). In addition, the number of claims involving eight or more issues (i.e., medical conditions), each of which must be evaluated separately, has more than doubled, from about 21,000 (20 percent of the original claims) in 2000 to about 51,000 (22 percent of original claims) in 2006 (Figure 5-1). This means that the number of rating decisions that must be made was a multiple of the 654,000 disability compensation claims filed in FY 2006.
VBA has been unable to track total number of issues adjudicated until recently, with the advent of the current tracking system, RBA 2000. According to data provided to the committee by VBA, adjudicators made more than 1.8 million rating decisions on compensation for disabilities during calendar year 2006, while adjudicating 628,000 disability compensation claims, indicating that the average number of issues (disabilities) per claim was just under three.
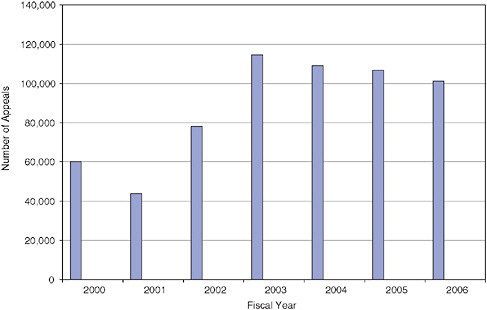
As the annual number of rating-related claims filed has increased, so have the number of decisions on rating-related claims (Figure 5-2).
However, new claim receipts continue to exceed case dispositions, resulting in an increasing backlog of pending claims. Nearly 380,000 rating-related claims were pending at the end of FY 2006, compared with 228,000 at the end of FY 2000 (Figure 5-3).
From the point of view of the veteran, the average length of time a claim is pending action by a regional office has been about four months in recent years (down from six months in FY 2001–FY 2002). Subsequent
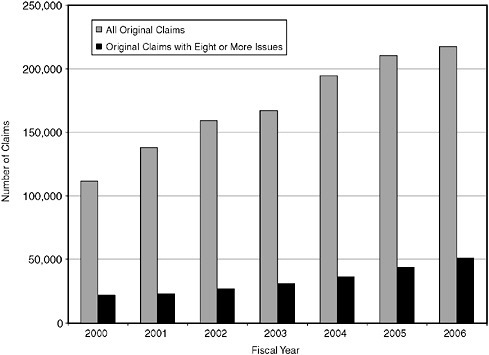
FIGURE 5-1 Number of original compensation claims from veterans and number of original compensation claims from veterans containing eight or more issues, end of fiscal years 2000–2006.
SOURCE: VA (2007b:6B-7, 6B-18).
processing by the regional office has averaged just under six months since FY 2000, except in FY 2002, when it was eight months (GAO, 2007). Accordingly, a veteran can expect to wait an average of about 10 months to receive a decision on his or her claim. This is two and one-half months more than the time period VA is trying to achieve. VA’s current performance target for average days pending of rating-related actions on compensation claims is 100 days. Its target to process rating-related claims is 125 days on average (VA, 2007b:6B-24).
In 1993, the deputy under secretary for benefits appointed a blue ribbon panel on claims processing to find ways to decide disability decisions more quickly. GAO issued a series of reports on problems with claims processing at VA between 1992 and 1996. VA’s Office of Inspector General also issued a series of reports on claims timeliness and accuracy during the
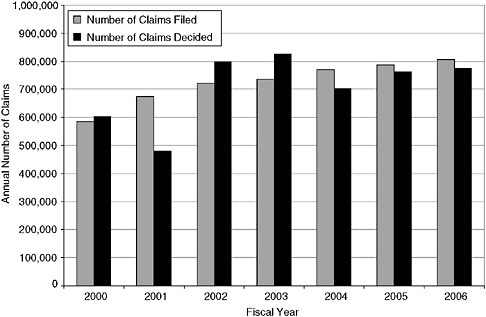
FIGURE 5-2 Number of rating-related claims filed and decided, FY 2000–FY 2006.
SOURCES: VA (2000, 2001a, 2002b, 2003, 2004c, 2005c, 2006a, 2007b).
1990s.22 Congress established the Veterans’ Claims Adjudication Commission, which reported in 1996, and the Senate Appropriations Committee mandated a study of VBA by the National Academy of Public Administration (NAPA), which reported in 1997.23
VBA regional offices were reorganized along case management lines, to ensure that someone was accountable for each case as it went through the decision-making process, and a major effort to improve the timeliness and quality of C&P examinations was launched (discussed earlier). Implementation of the case management model reduced production in the short run, however, while the number of claims increased substantially because of legislation (e.g., VCAA of 2000), court decisions, and regulatory changes (e.g., VA decision to make diabetes mellitus presumptive for Vietnam vet-
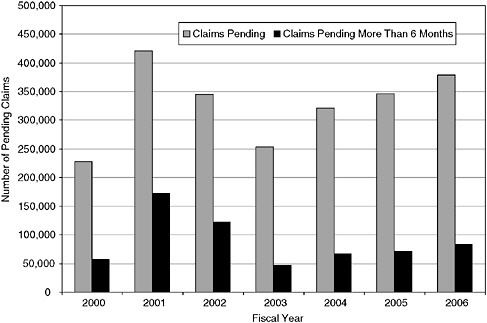
FIGURE 5-3 Number of rating-related claims pending and number pending more than six months, end of FY 2000–FY 2006.
SOURCES: VA (2000, 2001a, 2002b, 2003, 2004c, 2005c, 2006a, 2007b).
erans and to expand the list of radiation-related diseases with presumptive service connection).24
In 2001, the VA secretary appointed the Claims Processing Task Force. The task force not only recommended the major changes in the organization of the field offices described earlier (i.e., establishment of veterans service centers with staff units specializing in different parts of the claims process), but also a number of other steps to reduce the backlog of pending claims. These included
-
creation of “tiger teams” in the Cleveland regional office and establishment of nine resource centers to focus on processing cases of claimants over age 70, and then claims older than a year;
-
establishment of appeals claims processing teams in all regional offices;
-
faster record recovery from the VA Records Management Center;
-
better training;
-
updated performance standards for VSRs, RVSRs, DROs, and regional office directors;
-
consolidation of pension maintenance processing in three centers;
-
temporary shifting of staff from the Education Service to work on compensation claims; and
-
shifting of cases among regional offices to even out the workload.
VBA succeeded in substantially reducing the backlog by the end of FY 2003; after that, however, it began to climb again. The number of pending cases increased from 254,000 to 378,000 at the end of FY 2006, the number of cases pending more than 6 months increased from 47,000 to 83,000 (Figures 5-3), and the average number of days a case was pending increased from 111 to 127 (VA, 2006a).
VA points to several trends that affect the disability claims workload in terms of the number of claims and effort required to evaluate them. These include a larger share of claims with eight or more issues, more reopened claims submitted by veterans with chronic progressive conditions, additional claims submitted by the aging veteran population, and the claims submitted by veterans of Operation Iraqi Freedom (OIF) in Iraq and Operation Enduring Freedom (OEF) in and around Afghanistan.
In addition to the increasing number of disabilities claimed, VA reports that the nature of the disabilities has become more complex. VA cites PTSD, complex combat injuries, diabetes and related conditions, and environmental diseases as examples (VA, 2007b).
Another factor in timeliness is the adequacy of VA’s capacity to process the claims. In its FY 2008 budget submission, VA is asking for 475 more FTEs for direct compensation work in FY 2008 than in FY 2006, because “current staffing levels do not enable VA to reduce the pending claims inventory and provide timely service to veterans” (VA, 2007b:6B-4).25
Cases remanded by BVA also add to the workload and increase claim processing time. The inventory of remanded cases was 21,200 at the end of FY 2006 (VA, 2007b). Remands are discussed more fully below.
Appeal Workload and Timeliness
As discussed earlier, veterans dissatisfied with the decision made by the regional office may file an appeal by submitting an NOD contesting the denial of service connection, rating level given, or effective date of the grant. According to BVA, the appeal rate on disability determinations has historically been about 7 percent. More recently that rate has climbed from about
11 to 14 percent. In FY 2006, the appeal rate was about 13 percent—down from a high of 16 percent in FY 2004, but still well above historical averages. During the same period, the rate of formal appeals (based on number of VA Form 9s filed after the veteran receives the statement of the case from VBA) was 6 percent in FY 2006, down from 7 percent in FY 2004, but more than double the rate in FY 2002 (Figure 5-4).
As a result of this increasing workload, BVA has struggled to process appeals within a reasonable time period. The annual number of NODs, the first step in the appeal process, nearly doubled from FY 2000 to FY 2003, from 60,000 to 115,000. This increase was caused in part by the increased number of cases decided that could be appealed, but it is also caused by the greater propensity of veterans to appeal.26 The number of NODs has decreased since FY 2003, but was still 101,000 in FY 2006 (Figure 5-5). If current trends hold, VA is expecting between 90,000 and 110,000 appeals (NODs) a year in FY 2007 and FY 2008 (VA, 2007b:6B-14).
Many NODs are resolved by the regional office or when the veteran does not pursue the appeal, but the number of formal appeals was still higher in FY 2006 than in FY 2000. Veterans filed 46,100 formal appeals in FY 2006 by submitting VA Form 9, compared with 32,600 formal appeals in FY 2000. The annual number of BVA decisions, however, has not increased. As a result, the number of cases pending at BVA at the end of FY 2006—40,265—was almost double the number at the end of FY 2000. This does not include the substantial number of appeals being worked on by the appeals teams in regional offices and the Appeals Management Center, which was established by VBA in 2003 to consolidate expertise in processing remands from BVA (Figure 5-6).
The average number of days it took to resolve appeals, either by VBA or BVA, was 657 in FY 2006. This continued a steady increase since FY 2003, but was an improvement from the 731 days it took in FY 2002 (Figure 5-7).
Most appeals (72 percent in FY 2006) are resolved without a hearing before BVA. In FY 2006, 22,000 cases were resolved at the field office level after the NOD was received but before a formal appeal was filed on VA Form 9. In 42,200 cases, the veteran decided not to appeal further after reading the field office’s statement of the case. Another 11,000 were resolved at the field office level after VA Form 9 was submitted. That left 29,000 appeals, of which BVA resolved 25,000 and remanded 4,000 to the field offices for further development (VA, 2007b:6B-15).
BVA decided 39,100 cases involving disability compensation specifically in FY 2006. It upheld the field office denials 46 percent of the time,
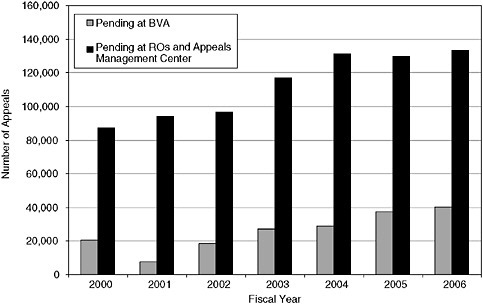
FIGURE 5-6 Number of appeals pending at BVA and at regional offices and the Appeals Management Center, FY 2000–FY 2006.
SOURCES: BVA (2001, 2003, 2004, 2006), cases ending at BVA; and VA (2007c), total appeals requiring adjudication.
reversed the field office decision on one or more of the issues 20 percent of the time, and remanded the case to the originating field office 32 percent of the time for further development of one or more issues (VA, 2006a:19).
The number of appeals to the CAVC averaged between 2,000 and 2,500 a year before FY 2005, when it jumped to 3,500 (Figure 5-8). The court received 3,700 appeals in FY 2006. It affirmed the BVA decision in full or in part in 11 percent of the cases in FY 2004, 16 percent in FY 2005, and 25 percent in FY 2006. During the same three years, the same court reversed the BVA decision or remanded the case for further development 50–60 percent of the time (U.S. Court of Appeals for Veterans Claims, 2006).27
There were 382 appeals to the federal circuit court in FY 2006, the highest since FY 2002, when 410 appeals were filed (Figure 5-8).
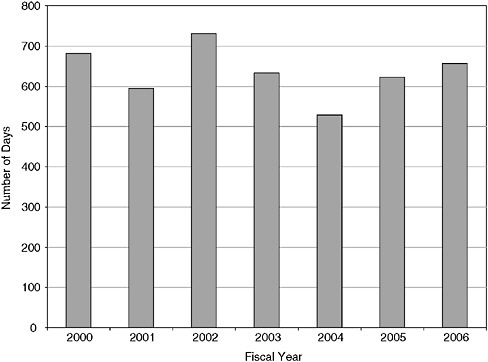
FIGURE 5-7 Average number of days to resolve appeals (i.e., appeals resolution time), FY 2000–FY 2006.
NOTE: Appeals resolution time is a joint BVA-VBA measure of time from receipt of an NOD by VBA to a final decision by VBA or BVA. Remands are not considered to be final decisions in this measure. Also not included are cases returned as a result of a remand by the CAVC.
SOURCES: VA (2000, 2001a, 2002b, 2003, 2004c, 2005c, 2006a).
Remands and Timeliness
Remands are of concern because not only do they increase the time it takes for a decision on the individual veteran’s claim by at least a year, but they also increase the overall workload and slow the resolution of appeals of other veterans (VA, 2000:29). By law, BVA must decide on appeals in the order in which they were entered on the docket. If BVA remands a case to the regional office, and that case is subsequently returned to BVA for a decision, which happens about 75 percent of the time (Terry, 2006b), the returned case takes precedence over appeals currently before BVA. During FY 2006, BVA remanded 32 percent (12,500) of the cases it decided. At the end of FY 2006, 16 percent (21,200 of 133,600) of the rating-related claims pending at regional offices and the VBA Appeals Management Cen-
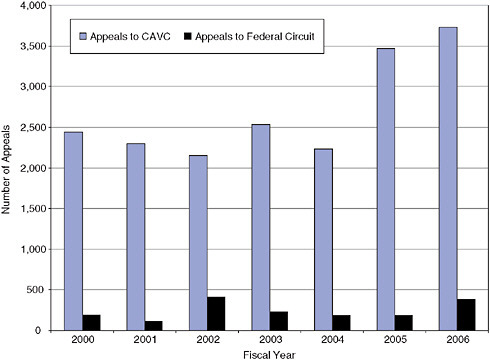
FIGURE 5-8 Annual number of appeals of BVA disability decisions to the courts, FY 2000–FY 2006.
SOURCE: U.S. Court of Appeals for Veterans Claims (2006).
ter were remands. If, as expected, 75 percent of the remands are returned to BVA after further development, they will constitute 30–40 percent of the 35,000–40,000 cases decided by BVA each year (in FY 2006, for example, BVA received 14,400 remands returned by the Appeals Management Center and regional offices for decision, equal to 37 percent of BVA decisions that year) (VA, 2007a:7C-4).
The percentage of BVA dispositions remanded jumped from 30 percent in FY 2000 to 49 percent in FY 2001. In 2002, in response to a recommendation of the 2001 Claims Processing Task Force, BVA established an evidence development unit to develop evidence needed to make a final decision or correct a procedural error in cases that otherwise would have to be remanded. The remand rate fell to about 15 percent “within a matter of months” (BVA, 2004:2).
When evidence development by BVA was barred by the CAVC, VBA created the Appeals Management Center in July 2003 to specialize in devel-
oping the cases that have been remanded by BVA and to review regional office decisions (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2005d).
The remand rate began to increase again, from 19 percent in FY 2002 to 43 percent the next year to 57 percent in FY 2004. In 2004, the VA deputy secretary charged the under secretary for benefits and the chairman of BVA with developing a comprehensive plan to reduce the number of avoidable remands. As part of that effort, a joint working group analyzed a representative sample of explanations for past remands and began to track them prospectively. The reasons given were separated into “before certification” and “after certification,” on the grounds that the causes of avoidable remands that happened before they were certified and transferred by regional offices to BVA should be in the control of, and therefore could be prevented by, regional offices. The initial analysis of 200 remand cases identified 379 precertification reasons for the remands. About a quarter of these (99) were for deficiencies involving C&P medical examinations and opinions; 9 percent (34) were for lack of an initial request for service medical records, VA medical records, or private medical records; and 6 percent (24) were for lack of an additional request for VA medical records or private medical records. Deficiencies in C&P examinations included lack of an examination, lack of a required medical opinion or an inadequate opinion, incomplete examination findings, and lack of current findings (VA, 2004a).
The remand rate dropped from 57 percent in FY 2004 to 32 percent in FY 2006 (BVA, 2006:20).28 The number of remands involving precertification problems with C&P examinations and other medical evidence also fell (Figure 5-9). Missing and inadequate C&P examinations and opinions constituted a third of the remand reasons in all three years, and failures to obtain other medical records remained at about 19 percent of the remand reasons.
In addition to efforts by BVA and VBA to reduce avoidable remands, primarily by training, and to improve the adequacy of C&P examinations, BVA is trying to address the backlog of appeals by increasing productivity. These steps include
-
having VLJs and counsel write shorter, more concise decisions;
-
having VLJs draft some decisions;
-
increasing the use of travel boards to decide cases and provide regional office training;
-
expanding employee incentive, mentoring, and training programs;
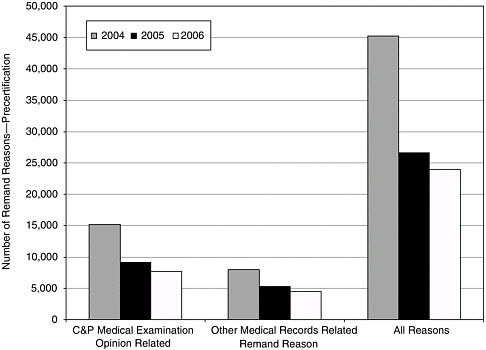
FIGURE 5-9 Number of remands by reason, FY 2004–FY 2006.
NOTE: Other medical records include military service, VA, and private medical records that should have been requested but were not, or if requested but not forthcoming, were not followed up. Nonmedical reasons for remands have to do with duty to notify (lack of, incorrect, or inadequate notices to appellants), duty to assist (not obtaining nonmedical service and other records), and due process (not following procedural rules).
SOURCE: Keller (2007).
-
increasing paralegal assistance;
-
increasing use of overtime;
-
providing improved online legal and medical research tools; and
-
focusing training on problems revealed through the quality assurance process (Terry, 2007).
Accuracy
VA has made accuracy of disability benefit decisions one of the key measures in its annual performance and accountability plans. As noted previously, VA has used the STAR process to measure technical accuracy since 1998. STAR review of a rating-related case determines if the benefit
entitlement decision process addresses all issues claimed (including inferred issues), provides assistance in obtaining evidence as required by the Veterans Claims Assistance Act, and results in correct decisions, including correctness of the decision to grant or deny benefits, percentage rating, payment rate, and effective dates. If the adjudication of the case fails any of these standards, it is classified as incorrect in the accuracy rate calculation. STAR review also determines if there is adequate and correct decision documentation and proper notification of the decision, although these scores are not in the performance and accountability plan.
During the year ending May 31, 2006, VBA reviewed 6,458 rating cases and found the national benefit entitlement accuracy rate to be 88 percent and the decision documentation and notification rate to be 90 percent (VA, 2006a:172). The entitlement accuracy rate was less than 60 percent in FY 2000. It improved steadily to 87 percent in FY 2004, leveling off at approximately the same rate in FY 2005 (84 percent) and FY 2006 (88 percent) (Figure 5-10).
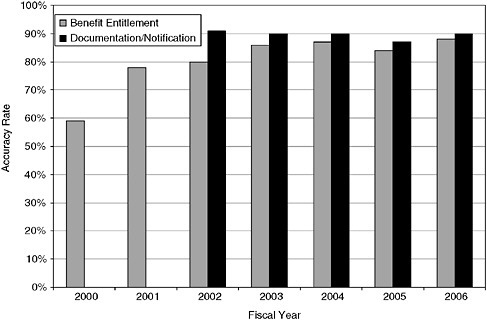
FIGURE 5-10 Accuracy of compensation and pension entitlement decisions, FY 2000–FY 2006.
NOTE: Documentation and notification were included in the entitlement accuracy rate until FY 2002. The 2001 Claims Processing Task Force recommended that VBA measure them separately so that the benefit entitlement accuracy rate would only include items that, if inadequate, could result in remand from BVA.
SOURCES: VA (2000, 2001a, 2002b, 2003, 2004c, 2005c, 2006a).
The STAR program began to determine annual accuracy rates for each regional office in FY 2002, which required a larger sample size and more staff (GAO, 2001). The original plan was to review approximately 10,000 cases annually in order to achieve a confidence level of 95 percent with a margin of error range of ±6 percent for best performing regional offices and ±9 percent for regional offices with the lowest performance rates. The actual number of cases reviewed has been less—6,458 in FY 2006. VBA randomly samples 120 rating cases per regional office each year, except it conducts 240 annual rating reviews for the four largest regional offices and the six regional offices with the lowest overall accuracy (VA, 2006d).
VBA requires regional offices to certify that appropriate action was taken on errors found in the STAR process. Offices with low accuracy rates are required to implement corrective action plans. Trends in error types are used to design national training programs and to identify needed regional office-specific training, which is offered during site visits (VA, 2007a).
Another indicator of accuracy problems is the percentage of initial decisions that are either reversed or remanded by BVA. In FY 2006, BVA reversed the initial regional office denial decision on at least one issue claimed by the appellant in 19 percent of cases and remanded another 32 percent of the cases, suggesting problems with just over half the cases reviewed. Although this is lower than the historical rate of about 60 percent, it still represents a substantial portion of the decisions (BVA, 2006).
BVA also has a quality assurance program that analyzes a sample of its own decisions to determine the percentage that have substantive or procedural deficiencies that would be expected to result in a reversal or a remand by the court. Deficiencies are identified in five areas: issues, findings of fact, conclusions of law, reasons and bases, and due process. BVA also uses the results to determine areas of training emphasis.
BVA’s deficiency-free decision rate improved from 86 percent in FY 2000 to 93 percent in FY 2004. It fell to 89 percent in FY 2005, but increased again to 93 percent in FY 2006 (Figure 5-11).
Consistency
VA has only recently undertaken an effort to assess consistency of decision making across regional offices and adjudicators. It is not a new issue. In a 1997 report on VA claims processing (mentioned earlier), NAPA concluded that consistency would be difficult, at best, to achieve across 58 field offices.29 NAPA recommended increasing consistency by reducing the number of regional offices. It also found that the quality assurance process did not address consistency:
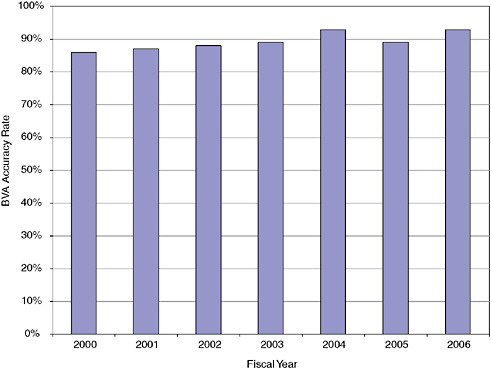
FIGURE 5-11 BVA accuracy rate, FY 2000–FY 2006.
NOTE: As recommended by the 2001 Claims Processing Task Force, BVA excluded deficiencies that would not be considered by the court, such as incorrect formatting, beginning in FY 2002.
SOURCES: VA (2003, 2006).
There is no current measure of decision consistency within the system, and on data collected to inform management regarding to what extent consistency may be a problem. Given the differing types of medical issues and cases within the system which in many cases require subjectivity (such as psychiatric cases as compared with orthopedic cases), there is need to bound types of medical issues and the degree of subjectivity, set consistency standards, measure this as part of a QR process (or through blind testing of a control case by several regions), and accumulate data (NAPA, 1997:128).
The 2001 VA Claims Processing Task Force recommended that VBA evaluate and address inconsistencies among regional offices. The task force noted the large disparities in average compensation payments across states, differences in appeal rates and results of appeals in terms of reversal and
remand rates from state to state, and lack of uniform guidance on interpretation of court decisions, any or all of which might indicate inconsistent decision making. GAO identified lack of consistency as a problem in a series of reports:
Even though available evidence provides indications that variations in decision making may occur across all levels of VA adjudication, VA does not conduct systematic assessments to determine the degree of variation that occurs for specific impairments and to provide a basis for determining ways, if considered necessary, to reduce such variation (GAO, 2002a:2).
VA’s disability decision quality review program—known as Systematic Technical Accuracy Review (STAR)—assesses the overall accuracy of all disability decisions, but not the consistency of decisions overall or for specific impairments (GAO, 2005a:6).
… variation is an inherent factor in the decision-making process. This makes it crucial that VA have a system for routinely identifying variations among its 57 regional offices so that such variations can be studied to determine if they are within the bounds of reasonableness and, if not, how to correct the problem. Also … VA must deal with issues involving not only its regional offices but also its 157 medical centers that conduct most of the disability examinations that regional offices rely on to provide the medical information they need to make disability decisions (GAO, 2006:2).
In 2005, VA’s Office of Inspector General investigated the differences in average compensation payments from state to state, which ranged from $7,000 in Illinois to $12,000 in New Mexico in FY 2004 (VA, 2005b). The report also looked at the differences in the percentages of veterans receiving compensation across states, which ranged from 6.9 to 19.2 percent. The inspector general examined a number of explanations for the variation in payments besides inconsistencies in disability ratings among regional offices, including demographic differences (such as the percentage of veterans in a state’s population, their period of service, and their average age) and process factors (such as percentage of claimants with representation, percentage of raters with more than two years of experience, and appeal rates). The inspector general could not analyze variations in grant rates, however, because VBA did not track them at that time. The report looked at correlations of explanatory factors with average payments one by one; a multivariate analysis was not done with average payment as the dependent variable or with other dependent variables of interest, such as percentage of veteran population receiving compensation or average combined rating degree. The report concluded that
VBA should develop a comprehensive and systematic method for collecting data on factors impacting variance in payments that will enable VA to model the compensation claims process and predict outcomes. Such
information would help program managers evaluate issues such as variances in disability ratings or payment patterns (VA, 2005b:34).
In the course of the study, the inspector general collected information on state differences in the average number of service-connected disabilities per veteran, average combined degree of disability, average ratings for each of the 14 body systems, percentage of veterans service connected for PTSD, percentage of veterans with ratings of 100 percent and with individual unemployability, and STAR error rates, each of which shows substantial state-to-state variability. The average number of service-connected disabilities, for example, ranges from 2.1 to 3.4 across states. The average combined rating degree ranged from 33 to 45 percent across the states. The rate of service connection for PTSD also varies by state, ranging from 4.1 per thousand resident veterans to 25.5 per thousand resident veterans. The results for individual unemployability (IU) were similar to those for PTSD. The number of veterans service connected for IU ranged from 2.5 to 28.2 per thousand resident veterans in FY 2004. Overall STAR accuracy rates varied from 76 to 96 percent, while the median rate was 88 percent (see Figure 5-12).
BVA data for FY 2006 also shows wide geographical variation in appeal reversal and remand rates. Depending on the regional office from which cases originate, BVA remanded appeals between 22 and 65 percent of the time. Appeal allowance rates by region varied from 7 to 34 percent. BVA upheld the original denial in 63 percent of appeals from one office but in only 15 percent of appeals from another office (BVA, 2007).
Concerns with consistency are not limited to geographic variations. BVA’s disposition of appeals also varies depending on the specific medical condition involved. Regional office decisions on some conditions are much more likely to be reversed or remanded on appeal than are others. Data for the first eight months of FY 2006 show that BVA was much more likely to either reverse (i.e., allow) or remand cases for individuals with certain medical conditions, and much more likely to deny cases for others. Table 5-3 lists the diagnostic codes present in cases that VLJs were most likely to reverse or remand, and those diagnostic codes present in cases that they were least likely to reverse or remand.30
Differences in judgment are inevitable in evaluating impairment and functional capacity, more for some conditions than others, depending on how subjective are the criteria; therefore, some degree of variation is inevitable. However, wide variation may be an indicator of inconsistent decision making. In addition, high reversal or remand rates may also indicate that the evaluation criteria are not as clear or appropriate as they should be.
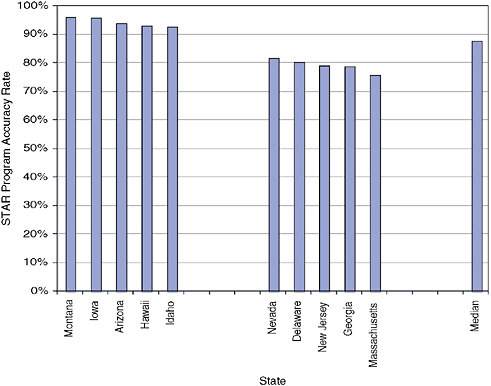
FIGURE 5-12 STAR program accuracy rates, 5 highest and 5 lowest states, FY 2004.
SOURCE: VA (2005b).
Another area of variability is C&P examination quality, which is critical to the accuracy of the rating process. Overall C&P examination quality was discussed earlier, but it also varies from region to region. For example, according to GAO, CPEP reported that only 78 percent of joint and spine examinations in FY 2004 included examiner discussions of pain now required due to the 1995 court case, DeLuca v. Brown. However, the extent to which examinations complied with these requirements varied considerably across VHA’s 21 VISNs, ranging from 57 to 92 percent compliance (Figure 5-13) (GAO, 2005b).
In 1997, NAPA pointed out that the large number of regional offices was a source of inconsistency and inefficiency. In 1999, the Congressional Commission on Servicemembers and Veterans Transition Assistance suggested that consolidation of claims adjudication in fewer offices should be part of an effort to modernize VBA’s benefits delivery processes (Congressional Commission, 1999). The 1991 Claims Processing Task Force
TABLE 5-3 Medical Conditions Most and Least Likely to Be Allowed or Remanded on Appeal by BVA (Minimum of 100 Appeals), October 1, 2005–May 31, 2006
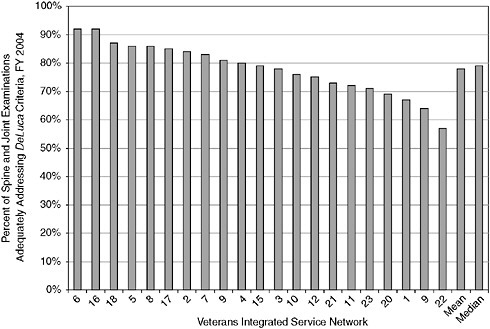
FIGURE 5-13 Percentage of spine and joint examinations adequately addressing DeLuca criteria, by VISN, FY 2004.
SOURCE: GAO (2005b).
reported that apparent inconsistencies in claims decisions from state to state should be addressed.
In 1995, a VBA task force on field office restructuring recommended some consolidations of compensation and pension functions, citing the following advantages:
-
allowing VBA to assign the most experienced and productive adjudication officers and directors to the consolidated offices;
-
facilitating increased specialization and as-needed expert consultation in deciding complex cases;
-
improving the completeness of claims development, the accuracy and consistency of rating decisions, and the clarity of decision explanations;
-
improving overall adjudication quality by increasing the pool of experience and expertise in critical technical areas; and
-
facilitating consistency in decision making through fewer consolidated claims processing centers (NAPA, 1997).
During the 1990s, VBA consolidated loan guaranty work in four regional centers, education benefits in four regional processing centers, and insurance in one national service center. More recently, VBA consolidated the income and eligibility verification work of the pension program in three regional offices, and is planning to consolidate all pension work in these offices. To deal with the 2001 jump in pending claims, VBA established the tiger team unit at one regional office and established resource centers at nine regional offices to specialize in claims of older veterans. In 2003, as discussed previously, VBA established the Appeals Management Center to help process remands. VBA centralized dependency and indemnity compensation claims by survivors of servicemembers who die on active duty in a casualty assistance unit in the Philadelphia regional office. BDD claims are also handled in a few regional offices. VBA established two “development centers” in Phoenix and Roanoke to assist regional offices in developing all radiation claims and centralized the processing of radiation claims in the Jackson regional office. Just recently, the VA secretary designated the two development centers and three of the nine resource centers as a special tiger team for processing OIF/OEF claims. The two development centers are developing the evidence, and the three resource centers are rating OIF/OEF claims for regional offices with the heaviest workloads (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2007b). Medical examinations for OIF/OEF veterans claims are also being expedited.
Nevertheless, the VSOs do not favor consolidating regional offices because they do not want to lose access to adjudicators or make it more difficult for veterans to appear in person before DROs who are reconsidering initial denials of their claims.
FINDINGS AND RECOMMENDATIONS
The Medical Evaluation Process
The quality and completeness of the medical information needed to apply the criteria in the Rating Schedule are critical to the disability compensation claims process for veterans. Obtaining needed medical information affects the timeliness, accuracy, and consistency of adjudication decisions. It requires the predetermination team to request the correct information needed from the medical examiners, examiners to conduct thorough examinations and report the results completely and accurately, and raters to interpret the medical information in light of the criteria in the Rating Schedule. It also requires VHA to ensure that the expertise of the examiner or examiners is appropriate for the condition or conditions being evaluated, especially for complex conditions such as PTSD, TBI, and polytrauma encountered in veterans of the current wars in Iraq and Afghanistan.
Need for Regular Updating of Examination Worksheets
VA has made a great deal of progress during the past 10 years in upgrading the medical evaluation process. Examination worksheets—two-to three-page outlines of the elements that must be addressed—for the most common conditions encountered in disability claims were developed. They were made available to examiners online to view and download. Currently, VA is developing intelligent interactive examination templates that structure the input needed in each case, which increases completeness and timeliness. VA does not, however, have a regular process for updating the worksheets, most of which date from 1997. Committee members evaluated some of the worksheets in light of the criteria in the Rating Schedule and current medical knowledge and found problems with outdated tests and examinations. Some of the problems stem from outdated criteria in the Rating Schedule. For example, rating of intervertebral disc syndrome relies on the duration of incapacitating episodes to assign 10 percent (1–2 weeks), 20 percent (2–4 weeks), 40 percent (4–6 weeks), or 60 percent (6 weeks or more). Incapacitating episodes are defined as bed rest prescribed by a physician, although bed rest is not the standard treatment for back problems.
Recommendation 5-1. VA should develop a process for periodic updating of the disability examination worksheets. This process should be part of, or closely linked to, the process recommended above for updating and revising the Schedule for Rating Disabilities. There should be input from the disability advisory committee recommended above (see Recommendation 4-1).
Use of the Examination Templates
VA does not require examiners to use printed-out examination worksheets and, consequently, many examiners do not use them. Although use of the online examination templates has increased rapidly (presumably because of their ease of use), VA also does not require their use—although it is considering such a mandate.
In an October 2005 report on C&P examinations, VA’s inspector general noted progress being made in developing the templates, but expressed concern about their limited use:
While VA, through the development and implementation of CPEP report templates, is making an effort to standardize C&P medical examinations, use of the templates is not yet required of VHA facilities. VBA rating personnel have seen only a limited number of examination reports submitted in the template format. We spoke with personnel at seven VAROs [VA regional offices] and were informed that use of the templates at VHA facilities is not yet common. VSC personnel at five of the seven VAROs indicated that they either have not seen any examination reports completed in the template format or they have only seen a limited number completed by one medical center in their area. Use of the templates was more frequent at medical centers serving the other two VAROs. Rating personnel at two VAROs who have seen the results of C&P examinations presented in the template format stated that they believed the examination reports need to be improved and that it was difficult to locate the information needed for rating purposes. According to VBA management, they are engaged in an effort to review and approve the report templates (VA, 2005b:69).
In the same report, the inspector general went on to recommend that the examination report templates be made mandatory, and that VA needed to ensure that medical and rating staff are familiar with the templates and that they are used consistently. The VA undersecretary for benefits concurred with this recommendation, and stated:
We will continue to work with the Veterans Health Administration to improve the quality of medical examinations performed to support disability compensation evaluations. We will work with the CPEP Office to ensure that all automated examination report templates thoroughly and accurately solicit the medical evidence needed to consistently evaluate the disability. We will also work with VHA to establish a formal approval process for the templates and to obtain agreement on the mandatory use of approved templates (VA, 2005b:189).
By June 2006, more than 128,000 examinations had been completed using the report templates, but they were still not mandatory, despite the fact that early results had shown template examination reports to have
higher quality than dictated reports, often significantly. In addition, template reports were released from 7 to 17 days sooner than dictated reports. “High-level” discussions were still underway within VA about whether to mandate use of the templates (Brown, 2006b,c).
Recommendation 5-2. VA should mandate the use of the online templates that have been developed for conducting and reporting disability examinations.
Assessing and Improving Quality and Consistency of Examinations
As noted previously, VA established CPEP in 2001 to develop and administer a QR program, and it has integrated the QR results into the performance plans of the VISN directors. Improvement in meeting the quality indicators has been rapid since 2002 when the effort began. The percentage of examinations meeting 90 percent of the quality indicators was 86 percent in January 2007, much better than the 58 percent achieved three years earlier. However, this percentage is still too low.
Another concern is that the quality indicators used in the QR process are more procedural rather than substantive. They are measures of the presence or absence of a particular worksheet item in the report, not of whether the examination was good. Independent examinations of a sample of claimants to assess inter-rater reliability are not performed.
Recently, CPEP began to assess the quality of the examination requests, which is critical. Previously, if the examiner provided 100 percent of the information requested, but the request was not correct, the QR system counted it as a quality examination. The next step would be for VA to make the quality of examination requests part of the performance program for predetermination teams and regional office directors.
In addition, the QR program currently does not directly assess consistency among examiners. It relies on improving accuracy to narrow the differences among examiners and VISNs.
Recommendation 5-3. VA should establish a recurring assessment of the substantive quality and consistency, or inter-rater reliability, of examinations performed with the templates, and if the assessment finds problems, take steps to improve quality and consistency, for example, by revising the templates, changing the training, or adjusting the performance standards for examiners.
This substantive assessment should be part of the QR audit and include a mechanism for random sampling. The training program should include examples of well-done and complete reports.
The Rating Process
Quality of Rating Decisions
VBA’s QR program, STAR, was implemented in 1998 and substantially revised and expanded to monitor individual regional office accuracy in 2001. The accuracy rate has improved from 64 percent in 1998 to 80 percent in FY 2002, and to 88 percent in FY 2006. Although this represents substantial improvement, it still shows that one of every nine rating decisions is incorrect, and this leaves considerable room for further improvement.
In addition, the STAR accuracy rate is based on a relatively small sample—only large enough to determine the aggregate accuracy rate of regional offices. It does not assess accuracy at the body system or diagnostic code level, and it does not measure consistency across regional offices. In 2005, in response to findings of inconsistencies by GAO and VA’s Office of Inspector General, VBA announced an effort to identify high rates of variability in claims adjudication by diagnostic code, to be followed by an assessment of decision consistency among and between regional offices for those conditions. The results would be used to identify needs for additional training, better guidance, procedural changes, or regulatory changes (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2005a).31
In 2005, VBA chose three conditions to assess for inconsistency: hearing loss, PTSD, and knee conditions. Ten subject-matter specialists were assigned to review 1,750 regional office decisions, followed by studies of additional conditions. These analyses were not made public.
According to VA’s latest strategic plan
VA will analyze ratings and claims data to track any unusual patterns of variance for further consistency review. Integrated systems and better data sharing will improve the quality of decision making by providing more accurate information to claims adjudicators. We will also develop systems and programs to evaluate employees’ information needs and deliver training to address those needs (VA, 2006c).
There are many sources of variability in decision making that, if not addressed and reduced to the extent possible, make it unlikely that veterans
with similar disabilities are being treated the same. VA should identify conditions subject to a great deal of decision variability, understand the reasons for the variability, and act to reduce that variability. Variability cannot be totally eliminated in evaluating most disabling conditions. There will be cases in which raters with the same information and criteria reach different conclusions, especially conditions with large subjective elements such as mental disorders and back pain. Still, sources of variability that can be controlled, such as training, guidelines, and rater qualifications, should be addressed.
Recommendation 5-4. The rating process should have built-in checks or periodic evaluations to ensure inter-rater reliability as well as the accuracy and validity of rating across impairment categories, ratings, and regions.
For example, VA could have a sample of claims rated by two or more RVSRs and analyze the degree of consistency in the ratings given. Or the same claims could be analyzed by RVSRs using standard procedures and information sources and by raters with access to medical advisers, and the results compared to assess whether having medical advisers for raters improves decision making. A comparison of raters with a medical background, such as nurses and physician assistants, and raters without medical backgrounds would inform decisions about the qualifications of raters. These comparisons could be done using hypothetical or actual cases. BVA might do the same with appeals.
VA could sample claims involving the rating of a particular diagnostic code across field offices and analyze inter-rater and inter-regional differences. Presumably these would be diagnostic codes of conditions that are relatively numerous or costly. A next step could be to determine the degree to which regulations, the adjudication manual, and other forms of guidance could be revised to reduce variability, or training or the QR system could increase consistency.
Another approach to reducing unwanted variability in the rating process is the use of best practices. The adoption of the CPI model by all regional offices in 2001–2002 is an example of this approach, but there is still evidence of considerable variation across regional offices in decision outcomes, such as grant rates, rating levels, and rates of appeals. VA should study these variations and identify best practices for all offices to adopt.
Better Access to Medical Expertise
In some cases, disability evaluators can use an authoritative medical finding, such as a particular test score of a certain degree, to make a rating
decision. In most cases, however, the evidence is less direct, more complex, and perhaps conflicting. The evaluator must understand the medical evidence and use judgment, for example, in weighing conflicting medical opinions. The evaluators are not usually medical professionals themselves. Other major disability programs either involve physicians or other appropriate clinicians in the adjudication decision or have medical experts readily available to review cases, for example, to interpret medical information for disability evaluators or advise on missing information that should be requested (see Appendix D). These are in addition to arrangements for independent medical examinations where needed to provide missing or inconsistent medical information. For example, Social Security disability determinations are generally made by two-person teams, one member of which is a physician or other appropriate medical professional (e.g., audiologist). At DoD, physical evaluation boards—which also use and apply the VA Rating Schedule—have at least one physician among the three members. The Federal Employee Compensation Act program and civil service disability retirement programs have physician consultants on staff. Private disability insurance carriers have a variety of arrangements to provide disability evaluators with advice.
The separation between medical examiners and rating specialists at VA is artificial and based on a misunderstanding of the role of physicians in adjudication. The U.S. Court of Appeals for Veterans Claims barred the participation of physicians in rating decisions on the grounds that they should not substitute their own clinical judgment because they represent the agency. In fact, the role of a physician-adjudicator differs from that of a physician performing a disability examination. They do not examine the claimant. They evaluate the evidence in the claimant’s file to confirm that a diagnosis was made and is adequately documented, weigh conflicting evidence in the medical records, and apply other aspects of the adjudication process. RVSRs can probably adjudicate many or most cases without physician involvement, but physician advice is helpful in complex cases. The Social Security Administration experimented successfully with having disability evaluators decide cases alone and only bring in medical consultants when, in their judgment, they needed the expert advice.
Currently, RVSRs do not have readily available medical consultants. If there is a question, they have to send the case back to VHA, which adds time to the process. VBA should have medical consultants accessible to RVSRs in the regional office VSCs. With modern communications technology, these consultants could be in a national or in regional centers, and have access to the claims file, the C&P examination report, and VA medical records, if any. This would not obviate the need for C&P examinations but would expedite the adjudication decision process.
Recommendation 5-5. VA raters should have ready access to qualified health-care experts who can provide advice on medical and psychological issues that arise during the rating process (e.g., interpreting evidence or assessing the need for additional examinations or diagnostic tests).
These health-care experts could come from VHA or outside contractors, or VBA could hire health-care providers to serve on its own staff. If they were VHA staff, arrangements would have to be made to ensure that the C&P examiner of a veteran was also not the consultant on his or her case, and training on the appropriate adjudication consultant role would have to be provided.
Training of Examiners and Adjudicators
VA is well along in developing a training and certification program for C&P medical examiners, and it is scheduled to be developed during FY 2007 and deployed during FY 2008. It is to be mandatory, although a date by which examiners must be certified has not yet been set.
VBA has also developed an extensive training program for case adjudicators. This is critical because VBA hired approximately 1,180 new VSRs and RVSRs in FY 2006, and plans to hire many more in FY 2007 and FY 2008 to make up for attrition and to meet the increase in caseload (VA, 2006a). A centralized two-week training course is given every quarter to new VSRs. This is followed by a national standardized training 23-week curriculum given at their home regional offices, which includes full lesson plans, handouts, student guides, instructor guides, and slides for classroom instruction. Newly-hired RVSRs are also provided a nationally consistent training program. VBA gives a week-long instructor development course to trainers in the regional offices. A computer-based training program, the Training and Performance Support System, has a set of modules on rating-related topics, including evaluation of disability conditions by body system. BVA also has an extensive training program, part of which is given by an on-staff medical adviser, a physician who also acts as an informal adviser to VLJs and counsel in a role somewhat like the medical consultant role recommended in Recommendation 5-4. The QR programs of both VBA and BVA are used to identify training needs, whether on particular topics or at particular regional offices.
In FY 2006, the VA under secretary for benefits directed regional offices to provide all claims adjudicators with a mandatory 70 hours of job-specific training, increasing to 80 hours in FY 2007 (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2006). VBA is not evaluating the effectiveness of its training programs, however.
VBA has developed a certification program for VSRs and plans to
extend it to RVSRs and DROs. The test was developed and validated for VBA by the Human Resources Research Organization (HumRRO), a national nonprofit organization that specializes in certification testing. As of September 2006, VBA had promoted 633 VSRs to the GS-11 level through the certification testing process. It is working with HumRRO on a test for the GS-12 RVSR position (U.S. Congress, House of Representatives, Committee on Veterans’ Affairs, 2006).
Recommendation 5-6. Educational and training programs for VBA raters and VHA examiners should be developed, mandated, and uniformly implemented across all regional offices with standardized performance objectives and outcomes. These programs should make use of advances in adult education techniques. External consultants should serve as advisors to assist in the development and evaluation of the educational and training programs.
REFERENCES
Brown, S. H. 2003. Presentation on CAPRI C&P worksheet module. VHA eHealth University class #145, May 14. http://www.vehu.med.va.gov/vehu/campcprs2003/ SessionCaptures/Hands-On/145/145_files/frame.htm (accessed March 15, 2007).
Brown, S. H. 2006a. Overview of CPEP and quality assurance improvement initiatives for C&P exams. Presentation to the IOM Committee on Medical Evaluation of Veterans for Disability Compensation, Washington, DC, May 25.
Brown, S. H. 2006b. Compensation and pension examination program overview. Presentation to the Veterans’ Disability Benefits Commission, Washington, DC. http://www.1888932-2946.ws/vetscommission/e-documentmanager/gallery/ Documents/June_2006/CPEPBriefing_June2006.pdf (accessed March 2, 2007).
Brown, S. H. 2006c. Examiner certification and exam templates update. Presentation to the Veterans’ Disability Benefits Commission, Washington, DC. http://www.1888932-2946.ws/vetscommission/e-documentmanager/gallery/Documents/September_2006/CPEP_Presentation_09-15-2006.pdf (accessed March 16, 2007).
Brown, S. H. 2007. Written response to IOM request for most recent information on quality review of compensation and pension examinations, use of online examination templates, and training and certification of examiners, attached to April 9, 2007, e-mail from Steven H. Brown, director, VA Compensation and Pension Examination Program.
BVA (Board of Veterans’ Appeals). 1994. FY 1994 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/ BVA1994AR.pdf (accessed March 16, 2007).
BVA. 1996a. FY 1995 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA1995AR.pdf (accessed March 16, 2007).
BVA. 1996b. FY 1996 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA1996AR.pdf (accessed March 16, 2007).
BVA. 1997. FY 1997 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA1997AR.pdf (accessed March 16, 2007).
BVA. 2000a. Understanding the appeal process. VA Pamphlet 01-00-1. http://www.va.gov/vbs/bva/y2000.pdf (accessed February 28, 2007).
BVA. 2000b. FY 2000 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2000AR.pdf (accessed March 16, 2007).
BVA. 2001. FY 2001 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2001AR.pdf (accessed March 16, 2007).
BVA. 2002a. How do I appeal? VA Pamphlet 01-02-02A. http://www.va.gov/vbs/bva/0102A.pdf (accessed February 28, 2007).
BVA. 2002b. FY 2002 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2002AR.pdf (accessed March 16, 2007).
BVA. 2003. FY 2003 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2003AR.pdf (accessed March 16, 2007).
BVA. 2004. FY 2004 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2004AR.pdf (accessed March 16, 2007).
BVA. 2005. FY 2005 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2005AR.pdf (accessed March 16, 2007).
BVA. 2006. FY 2006 report of the chairman, Board of Veterans’ Appeals. Washington, DC: BVA. http://www.va.gov/Vetapp/ChairRpt/BVA2006AR.pdf (accessed March 16, 2007).
BVA. 2007. Data from the Veterans Appeals Control and Locator System on the disposition of claims by regional office during FY 2005, provided by BVA.
Congressional Commission (Congressional Commission on Servicemembers and Veterans Transition Assistance). 1999. Final report of the Congressional Commission on Servicemembers and Veterans Transition Assistance. http://www.vetbiz.gov/library/Transition%20Commission%20Report.pdf (accessed March 16, 2007).
GAO (General Accounting Office). 2001. Veterans’ benefits: Quality assurance for disability claims processing. GAO-01-930R. http://www.gao.gov/new.items/d01930r.pdf (March 15, 2007).
GAO. 2002a. Veterans’ benefits: Quality assurance for disability claims and appeals processing can be further improved. GAO-02-806. http://www.gao.gov/new.items/d02806.pdf (accessed February 28, 2007).
GAO. 2002b. Veterans’ benefits: Despite recent improvements, meeting claims processing goals will be challenging. GAO-02-645T. http://www.gao.gov/new.items/d02645t.pdf (accessed March 15, 2007).
GAO. 2005a. Veterans benefits: VA needs plan for assessing consistency of decisions. GAO-05-99. http://www.gao.gov/new.items/d0599.pdf (accessed March 15, 2007).
GAO. 2005b. Veterans’ disability benefits: VA could enhance its progress in complying with court decision on disability criteria. GAO-06-46. http://www.gao.gov/new.items/d0646.pdf (accessed March 15, 2007).
GAO. 2005c. VA disability benefits: Board of Veterans’ Appeals has made improvements in quality assurance, but challenges remain for VA in assuring consistency. GAO-05-655T. http://www.gao.gov/new.items/d05655t.pdf (accessed February 28, 2007).
GAO. 2006. VA disability benefits: Routine monitoring of disability decisions could improve consistency. GAO-06-120T. http://www.gao.gov/new.items/d06120t.pdf (accessed March 15, 2007).
GAO. 2007. Veterans’ disability benefits: Long-standing claims processing challenges persist. GAO-07-512T. http://www.gao.gov/new.items/d07512t.pdf (accessed May 28, 2007).
Keller, S. 2007. Written response to IOM request for information on BVA sources of medical expertise and statistics on reasons for remands, attached to March 21, 2007, e-mail from Steve Keller, senior deputy vice chairman, Board of Veterans’ Appeals.
Mansfield, G. H. 2005. Letter to Cynthia A. Bascetta, director, Education, Workforce and Income Security Issues, GAO. GAO-06-46. http://www.gao.gov/new.items/d0646.pdf (accessed March 15, 2007).
NAPA (National Academy of Public Administration). 1997. Management of compensation and pension benefits claim processes for veterans. Washington, DC: NAPA.
Pamperin, T. 2006. Overview of disability compensation and pension examinations. Presentation to Veterans’ Disability Benefits Commission. http://www.1888932-2946.ws/vetscommission/e-documentmanager/gallery/Documents/June_2006/VBAPresentation_6-21-06.pdf (accessed March 2, 2007).
QTC. 2006. QTC exam process and demo. Presentation to the Veterans’ Disability Benefits Commission. http://www.1888932-2946.ws/vetscommission/e-documentmanager/gallery/Documents/June_2006/QTCOverview_June2006.pdf (accessed March 2, 2007).
Shahani, M. 2005. QTC medical services overview. Presentation to VA’s Advisory Committee on Women Veterans. http://www.va.gov/womenvet/docs/ACWV_Nov._05_meeting_web_version.doc (accessed September 5, 2006).
Terry, J. P. 2006a. Briefing for the Institute of Medicine. Presentation to the IOM Committee on Medical Evaluation of Veterans for Disability Compensation, Washington, DC, July 7.
Terry, J. P. 2006b. Prepared statement of James P. Perry, Chairman, Board of Veterans’ Appeals, before the Veterans’ Disability Benefits Commission. Washington, DC, January 20. http://www.1888932-2946.ws/vetscommission/e-documentmanager/gallery/Documents/January_2006/Statement_Terry_BVAChairman_Jan06.pdf (accessed February 28, 2007).
Terry, J. P. 2007. Statement before the Committee on Veterans’ Affairs, U.S. Senate, March 7, 2007. http://veterans.senate.gov/index.cfm?FuseAction=Hearings.CurrentHearings&rID=943&hID=250 (accessed March 15, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2005a. Prepared statement of Ronald R. Aument, Deputy Under Secretary for Benefits, VA. 109th Cong., 1st Sess., December 7. http://veterans.house.gov/hearings/schedule109/dec05/12-7-05/raument.html (accessed March 5, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2005b. Prepared statement of Steven H. Brown, Director, Compensation and Pension Examination Program, VA, on compensation and pension examination variability. 109th Cong., 1st Sess., October 20. http://www.va.gov/OCA/testimony/hvac/sdama/051020SB.asp (accessed March 15, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2005c. Statement of Gordon H. Mansfield, Deputy Secretary, VA. 109th Cong., 1st Sess., September 28. http://veterans.house.gov/hearings/schedule109/sep05/9-28-05/gmansfield.pdf (accessed March 5, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2005d. Testimony of Michael Walcoff, Associate Deputy Under Secretary for Field Operations, Veterans Benefits Administration. 109th Cong., 1st Sess., May 5. http://www.va.gov/OCA/testimony/hvac/sdama/050505MW.asp (accessed May18, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2006. Prepared testimony of Michael Walcoff, Associate Deputy Under Secretary for Field Operations, Veterans Benefits Administration, VA. 109th Cong., 2nd Sess., September 13. http://veterans.house.gov/hearings/schedule109/sep06/9-13-06/MichaelWalcoff.html (accessed May 22, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2007a. Testimony of R. James Nicholson, Secretary of Veterans Affairs. 110th Cong., 1st Sess., February 8. http://veterans.house.gov/hearings/schedule110/feb07/02-08-07/JamesNicholson.html (accessed March 1, 2007).
U.S. Congress, House of Representatives, Committee on Veterans’ Affairs. 2007b. Prepared statement of Ronald R. Aument, Deputy Under Secretary for Benefits, VA. 110th Cong., 1st Sess., March 13. http://veterans.house.gov/hearings/schedule110/mar07/03-13-07/3-13-07aument.shtml (accessed March 5, 2007).
U.S. Congress, Senate, Committee on Veterans’ Affairs. 2007. Prepared statement of David S. C. Chu, Under Secretary of Defense (Personnel and Readiness). 110th Cong., 1st Sess., January 23. http://veterans.senate.gov/index.cfm?FuseAction=Hearings.CurrentHearings&rID=891&hID=234 (accessed March 5, 2007).
U.S. Court of Appeals for Veterans Claims. 2006. Annual reports of the U.S. Court of Appeals for Veterans Claims. http://www.vetapp.uscourts.gov/documents/Annual_Reports.pdf (accessed May 15, 2007).
VA (Department of Veterans Affairs). 1994. Timeliness of C&P medical examination services. Report No. 4R1-A02-092. Washington, DC: Office of Inspector General, VA.
VA. 1997a. Summary report on VA claims processing issues. Report No. 8D2-B01-001. Washington, DC: Office of Inspector General, VA. http://www.va.gov/oig/52/reports/1998/8D2-B01-001.pdf (accessed March 12, 2007).
VA. 1997b. Review of compensation and pension medical examination services. Report No. 7R1-A02-114. Washington, DC: Office of Inspector General, VA. http://www.va.gov/oig/52/reports/1997/7R1-A02-114--C-PEXAM.PDF (accessed March 12, 2007).
VA. 2000. Annual performance report, FY 2000. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2000/PerfRpt2000.pdf (accessed March 16, 2007).
VA. 2001a. Annual performance report, FY 2001. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2001/PerfRpt2001.pdf (accessed March 15, 2007).
VA. 2001b. Best practice manual for posttraumatic stress disorder (PTSD) compensation and pension examinations. http://www.ptsdmanual.com/ptsd.pdf (accessed March 20, 2007).
VA. 2002a. C&P Service clinician’s guide. Version 3.0, edited by L. R. Coulson, VHA. http://www.warms.vba.va.gov/Admin21/GUIDE/Cliniciansguide.doc (accessed March 4, 2007).
VA. 2002b. Fiscal year 2002 performance and accountability report. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2002/Perform_AccountRpt2002.pdf (accessed March 15, 2007).
VA. 2002c. Quality measurement of compensation and pension examinations: National baseline performance, ten most common exam types. Washington, DC: Compensation and Pension Examination Project Office, VA.
VA. 2003. Fiscal year 2003 performance and accountability report. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2003/Perform_AccountRpt2003.pdf (accessed May 20, 2007).
VA. 2004a. Avoidable remands agreement and implementation. VBA Letter 20-04-58. http://www.warms.vba.va.gov/admin20/letters/vba04_58.doc (accessed March 15, 2007).
VA. 2004b. Handbook of standard procedures and best practices for audiology compensation and pension examinations, edited by K. C. Dennis, L. B. Beck, D. W. Chandler, and J. Schafer. Washington, DC: Employee Education System, VA. http://www-nehc.med.navy.mil/downloads/Occmed/HCToolbox/Toolbox_files/VA%20Audiology%20Best%20Practices%20%26%20Procedures.pdf (accessed March 20, 2007).
VA. 2004c. Fiscal year 2004 performance and accountability report. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2004/9208DepVetAff_2004.pdf (accessed March 15, 2007).
VA. 2005a. Department of Veterans Affairs compensation and pension record interchange user guide. http://www.va.gov/vdl/documents/Financial_Admin/CAPRI/ capri_ug_dvba_2.7_91.pdf (accessed March 4, 2007).
VA. 2005b. Department of Veterans Affairs Office of Inspector General review of state variances in VA disability compensation payments. Report No. 05-00765-137. http://www.va.gov/oig/52/reports/2005/VAOIG-05-00765-137.pdf (accessed March 4, 2007).
VA. 2005c. Fiscal year 2005 performance and accountability report. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2005/VA-2005_FULL-WEB.pdf (accessed March 15, 2007).
VA. 2006a. FY 2006 performance and accountability report. Washington, DC: Office of Budget, Office of Management, VA. http://www.va.gov/budget/report/2006FullWeb.pdf (accessed March 16, 2007).
VA. 2006b. VHA handbook 1601E.01, Compensation and pension (C&P) examinations. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=1400 (accessed March 15, 2007).
VA. 2006c. VA strategic plan FY 2006-2011. http://www.va.gov/op3/docs/VA_2006_2011_Strategic_Plan.pdf (accessed March 16, 2007).
VA. 2006d. Accuracy and accountability. Unpublished PowerPoint presentation. Washington, DC: C&P Service, VA.
VA. 2006e. Qualifications for examiners performing compensation and pension (C&P) mental disorder examinations. VBA Fast Letter 06-03, March 15. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=1391 (accessed April 4, 2007).
VA. 2007a. Veterans Administration fiscal year 2008 budget submission. Vol. 4, Summary. http://www.va.gov/budget/summary/VolumeIVSummaryVolume.pdf (accessed February 28, 2007).
VA. 2007b. Veterans Administration fiscal year 2008 budget submission. Vol. 2, National Cemetery Administration, benefit programs, and departmental administration. http://www.va.gov/budget/summary/VolumeIINationalCemeteryAdministrationBenefitsProgramsandDepartmentalAdmin.pdf (accessed February 28, 2007).
VA. 2007c. Monday morning workload reports, end of the fiscal year: 2000–2006. http://www.vba.va.gov/bln/201/reports/mmrindex.htm (accessed May 22, 2007).
VA. 2007d. Index to disability examination worksheets. http://www.vba.va.gov/bln/21/Benefits/exams/index.htm (accessed May 20, 2007).
VA. 2007e. Mission statement of the Veterans Benefits Administration. http://www.vba.va.gov/mission_vision.htm (accessed February 28, 2007).
VA. 2007f. Understanding the disability claims process. http://www.vba.va.gov/bln/21/Topics/claims.htm (accessed May 18, 2007).
VDBC (Veterans’ Disability Benefit Commission). 2007. Transition report. http://www.1888932-2946. ws/vetscommission/e-documentmanager/gallery/Documents/2007_February/TransitionReport_Slides_2-21-2007.pdf (accessed March 3, 2007).