Appendix K
Sources of Health and Exposure Data for Veterans
APPENDIX K-1
BIBLIOGRAPHY OF DEPARTMENT OF VETERANS AFFAIRS EPIDEMIOLOGIC STUDIES OF VETERANS
Publication/VHA Environmental Epidemiology Service1
Gulf War Veterans
Blanchard, M. S., S. A. Eisen, R. Alpern, J. Karlinsky, R. Toomey, D. J. Reda, F. M. Murphy, L. W. Jackson, and H. K. Kang. 2006. Chronic multisymptom illness complex in Gulf War I veterans 10 years later. American Journal of Epidemiology 163(1):66-75.
Bullman, T. A., C. M. Mahan, H. K. Kang, and W. F. Page. 2005. Mortality in U.S. Army Gulf War veterans exposed to 1991 Khamisiyah chemical munitions destruction. American Journal of Public Health 95(8):1382-1388.
Davis, L. E., S. A. Eisen, F. M. Murphy, R. Alpern, B. J. Parks, M. Blanchard, D. J. Reda, M. K. King, F. A. Mithen, and H. K. Kang. 2004. Clinical and laboratory assessment of distal peripheral nerves in Gulf War veterans and spouses. Neurology 63(6):1070-1077.
Eisen, S. A., H. K. Kang, F. M. Murphy, M. S. Blanchard, D. J. Reda, W. G. Henderson, R. Toomey, L. W. Jackson, R. Alpern, B. J. Parks, N. Klimas, C. Hall, H. S. Pak, J. Hunter, J. Karlinsky, M. J. Battistone, M. J. Lyons, and the Gulf War Study Participating Investigators. 2005. Gulf War veterans’ health: Medical evaluation of a U.S. cohort. Annals of Internal Medicine 142(11):881-890.
Eisen, S. A., J. Karlinsky, L. W. Jackson, M. Blanchard, H. K. Kang, F. M. Murphy, R. Alpern, R. J. Domenic, R. Toomey, M. J. Battistone, B. J. Parks, N. Klimas, H. S. Pak, J. Hunter, M. J. Lyons, and W. G. Henderson. 2006. Spouses of Gulf War I veterans: Medical evaluation of a U.S. cohort. Military Medicine 171(7):613-618.
Gackstetter, G. D., T. I. Hooper, S. F. DeBakey, A. Johnson, B. E. Nagaraj, J. M. Heller, and H. K. Kang. 2006. Fatal motor vehicle crashes among veterans of the 1991 Gulf War and exposure to munitions
demolitions at Khamisiyah: A nested case control study. American Journal of Industrial Medicine 49(4):261-270.
Gray, G. C., and H. K. Kang. 2006. Healthcare utilization and mortality among veterans of the Gulf War. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences 361(1468):553-569.
Gray, G. C., B. D. Coates, C. M. Anderson, H. K. Kang, S. W. Berg, F. S. Wignall, J. D. Knoke, and E. Barrett-Connor. 1996. The postwar hospitalization experience of U.S. veterans of the Persian Gulf War. New England Journal of Medicine 335(20):1505-1513.
Gray, G. C., A. W. Hawksworth, T. C. Smith, H. K. Kang, J. D. Knoke, and G. D. Gackstetter. 1998. Gulf War veterans’ health registries. Who is most likely to seek evaluation? American Journal of Epidemiology 148(4):343-349.
Gray, G. C., T. C. Smith, H. K. Kang, and J. D. Knoke. 2000. Are Gulf War veterans suffering warrelated illnesses? Federal and civilian hospitalizations examined, June 1991 to December 1994. American Journal of Epidemiology 151(1):63-71.
Gray, G. C., G. D. Gackstetter, H. K. Kang, J. T. Graham, and K. C. Scott. 2004. After more than 10 years of Gulf War veteran medical evaluation, what have we learned? American Journal of Preventive Medicine 26(5):443-452.
Hallman, W. K., H. M. Kipen, M. Diefenbach, K. Boyd, H. Kang, H. Leventhal, and D. Wartenberg. 2003. Symptom patterns among Gulf War Registry veterans. American Journal of Public Health 93(4):624-630.
Hooper, T. I., S. F. DeBakey, A. Lincoln, H. K. Kang, D. N. Cowan, and G. D. Gackstetter. 2005. Leveraging existing databases to study vehicle crashes in combat occupational cohort: Epidemiologic methods. American Journal of Industrial Medicine 48(2):118-127.
Hooper, T. I., S. F. DeBakey, K. S. Bellis, H. K. Kang, D. N. Cowan, A. Lincoln, and G. D. Gackstetter. 2006. Understanding the effect of deployment on the risk of fatal motor vehicle crashes: A nested case-control study of fatalities in Gulf War era veterans, 1991-1995. Accident; Analysis and Prevention 38(3):518-525.
Kang, H. K., and T. A. Bullman. 1996. Mortality among U.S. veterans of the Persian Gulf War. New England Journal of Medicine 335(20):1498-1504.
Kang, H. K., and T. A. Bullman. 1998. Counterpoint: Negligible “healthy-warrior effect” on Gulf War veterans’ mortality. American Journal of Epidemiology 148(4):324-325.
Kang, H. K., and T. A. Bullman. 2001. Mortality among U.S. veterans of the Persian Gulf War: 7-year follow-up. American Journal of Epidemiology 154(5):399-405.
Kang, H. K., and K. C. Hyams. 2005. Mental health care needs among recent war veterans. New England Journal of Medicine 352(13):1289.
Kang, H. K., C. M. Mahan, K. Y. Lee, C. A. Magee, and F. M. Murphy. 2000. Illnesses among United States veterans of Gulf War: A population-based survey of 30,000 veterans. Journal of Occupational and Environmental Medicine 42(5):491-501.
Kang, H. K., C. M. Mahan, K. Y. Lee, F. M. Murphy, S. J. Simmens, H. A. Young, and P. H. Levine. 2002a. Evidence for a deployment related Gulf War syndrome by factor analysis. Archives of Environmental Health 57(1):61-68.
Kang, H. K., T. A. Bullman, G. J. Macfarlane, and G. C. Gray. 2002b. Mortality among U.S. and UK veterans of the Persian Gulf War: A review. Occupational and Environmental Medicine 59(12): 794-799.
Kang, H. K., B. H. Natelson, C. M. Mahan, K. Y. Lee, and F. M. Murphy. 2003. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population based survey of 30,000 veterans. American Journal of Epidemiology 157(2):141-148.
Karlinsky, J. B., M. Blanchard, R. Alpern, S. A. Eisen, H. K. Kang, F. M. Murphy, and D. Reda. 2004. Late prevalence of respiratory symptoms and pulmonary function abnormalities in Gulf War 1 veterans. Archives of Internal Medicine 164(22):2488-2491.
Kipen, H. M., W. Hallman, H. K. Kang, N. Fiedler, and B. H. Natelson. 1999. Prevalence of chronic fatigue and chemical sensitivities in Gulf Registry veterans. Archives of Environmental Health 54(5):313-318.
Levine, P. H., H. A. Young, S. J. Simmens, D. Rentz, V. E. Kofie, C. M. Mahan, and H. K. Kang. 2004. Is testicular cancer related to Gulf War deployment? Evidence from a pilot population-based study of Gulf War era veterans and cancer registries. Military Medicine 170(2):149-153.
Lincoln, A. E., T. I. Hooper, H. K. Kang, S. F. Debakey, D. N. Cowan, and G. D. Gackstetter. 2006. Motor vehicle fatalities among Gulf War era veterans: Characteristics, mechanisms and circumstances. Traffic Injury Prevention 7(1):31-37.
Mahan, C. M., H. K. Kang, N. A. Dalager, and J. M. Heller. 2004. Anthrax vaccination and self-reported symptoms, functional status, and medical conditions in the National Health Survey of Gulf War Era Veterans and Their Families. Annals of Epidemiology 14(2):81-88.
Miller, R. N., D. J. Costigan, H. A. Young, H. K. Kang, N. Dalager, R. W. Mathes, H. C. Crawford, W. F. Page, and S. Thaul. 2006. Patterns of health care seeking of Persian Gulf War Registry members prior to deployment. Military Medicine 171(5):370-375.
Murphy, F. M., H. K. Kang, N. A. Dalager, K. Y. Lee, R. E. Allen, S. H. Mather, and K. W. Kizer. 1999. The health status of Gulf War veterans: Lessons learned from the Department of Veterans Affairs Health Registry. Military Medicine 164(5):327-331.
Page, W. F., C. M. Mahan, H. K. Kang, and T. A. Bullman. 2005a. Health effects in Army Gulf War veterans possibly exposed to chemical munitions destruction at Khamisiyah, Iraq: Part II. Morbidity associated with notification of potential exposure. Military Medicine 170(11):945-951.
Page, W. F., C. M. Mahan, T. A. Bullman, and H. K. Kang. 2005b. Health effects in Army Gulf War veterans possibly exposed to chemical munitions destruction at Khamisiyah, Iraq: Part I. Morbidity associated with potential exposure. Military Medicine 170(11):935-944.
Persian Gulf Veterans Coordinating Board. 1995. Unexplained illnesses among Desert Storm veterans: A search for causes, treatment, and cooperation. Archives of Internal Medicine 155(3):262-268.
Smith, T. C., B. Smith, M. A. Ryan, G. C. Gray, T. I. Hooper, J. M. Heller, N. A. Dalager, H. K. Kang, and G. D. Gackstetter. 2002. Ten years and 100,000 participants later: Occupational and other factors influencing participation in U.S. Gulf War health registries. Journal of Occupational and Environmental Medicine 44(8):758-768.
Smith, T. C., D. L. Jimenez, B. Smith, G. C. Gray, T. I. Hooper, G. D. Gackstetter, J. M. Heller, N. A. Dalager, H. K. Kang, K. C. Hyams, and M. A. Ryan. 2004. The postwar hospitalization experience of Gulf War veterans participating in U.S. health registries. Journal of Occupational and Environmental Medicine 46(4):386-397.
Young, H. A., S. J. Simmens, H. K. Kang, C. M. Mahan, and P. H. Levine. 2003. Factor analysis of fatiguing syndrome in Gulf War era veterans: Implications for etiology and pathogenesis. Journal of Occupational and Environmental Medicine 45(12):1268-1273.
Women Veterans
Dalager, N. A., H. K. Kang, and T. L. Thomas. 1995. Cancer mortality patterns among women who served in the military: The Vietnam experience. Journal of Occupational Medicine 37(3):298-305.
Kang, H. K., C. M. Mahan, K. Y. Lee, C. A. Magee, and S. Selvin. 2000a. Prevalence of gynecological cancers among women Vietnam veterans. Journal of Occupational and Environmental Medicine 42(11):1121-1127.
Kang, H. K., C. M. Mahan, K. Y. Lee, C. A. Magee, S. H. Mather, and G. Matanoski. 2000b. Pregnancy outcomes among U.S. women Vietnam veterans. American Journal of Industrial Medicine 38(4):447-454.
Kang, H. K., C. Magee, C. Mahan, K. Lee, F. Murphy, L. Jackson, and G. Matanoski. 2001. Pregnancy outcomes among U.S. Gulf War veterans: A population-based survey of 30,000 veterans. Annals of Epidemiology 11(7):504-511.
Kang, H. K., N. A. Dalager, C. M. Mahan, and E. Ishii. 2005. The role of sexual assault on the risk of PTSD among Gulf War veterans. Annals of Epidemiology 15(3):191-195.
Thomas, T. L., H. K. Kang, and N. A. Dalager. 1991. Mortality among women Vietnam veterans, 19731987. American Journal of Epidemiology 134(9):973-980.
Atomic Veterans and Radiation Exposure
Dalager, N. A., H. K. Kang, and C. M. Mahan. 2000. Cancer mortality among the highest exposed U.S. atmospheric nuclear test participants. Journal of Occupational and Environmental Medicine 42(8):798-805.
Kang, H. K. 1996. Feasibility of an epidemiologic study of submariners who received radium irradiation treatment. Otolaryngology-Head and Neck Surgery 115(5):433-437.
Kang, H. K., T. A. Bullman, and C. M. Mahan. 2000. A mortality follow-up study of WWII submariners who received nasopharyngeal radium irradiation treatment. American Journal of Industrial Medicine 38(4):441-446.
Watanabe, K. K., H. K. Kang, and N. A. Dalager. Cancer mortality risk among military participants of a 1958 atmospheric nuclear weapons test. American Journal of Public Health 85(4):523-527.
Others (POWs, Mustard Gas)
Bullman, T. A., and H. K. Kang. 1994. The effects of mustard gas, ionizing radiation, herbicides, trauma, and oil smoke on U.S. military personnel: The results of veterans studies. Annual Review of Public Health 15:69-90.
Bullman, T. A., and H. K. Kang. 2000. A fifty year mortality follow-up study of veterans exposed to low level chemical warfare agent, mustard gas. Annals of Epidemiology 10(5):333-338.
Kang, H. K. 1991. Resources for epidemiologic research in Vietnam era veteran populations within the Department of Veterans Affairs. in Epidemiology in military and veteran populations: Proceedings of the second biennial conference, March 7, 1990, edited by W. F. Page. Washington, DC: National Academy Press. Pp. 97-103.
Kang, H. K., and P. P. Breslin. 1986. Effects of military draft on mortality. New England Journal of Medicine 315:454.
Kang, H. K., and T. L. Thomas. 1990. Comment. National sources of vital status information: Extent of coverage and possible selectivity in reporting. American Journal of Epidemiology 132(6):1196-1197.
Kang, H. K., T. A. Bullman, and J. W. Taylor. 2006. Risk of selected cardiovascular diseases and posttraumatic stress disorder among former World War II prisoners of war. Annals of Epidemiology 16(5):381-386.
Page, W. F., C. M. Mahan, and H. K. Kang. 1996. Vital status ascertainment through the files of the Department of Veterans Affairs and the Social Security Administration. Annals of Epidemiology 6(2):102-109.
Schneiderman, A. I., A. E. Lincoln, B. A. Curbow, and H. K. Kang. 2004. Racial variations in health communication needs of combat veterans. American Journal of Public Health 94(12):2074-2076.
Vietnam Veterans
Breslin, P., H. K. Kang, Y. Lee, V. Burt, and B. M. Shepard. 1988. Proportionate mortality study of Army and Marine Corps veterans of the Vietnam War. Journal of Occupational Medicine 30(5):412-419.
Bullman, T. A., and H. K. Kang. 1994. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. Journal of Nervous and Mental Disorder 182(11):604-610.
Bullman, T. A., and H. K. Kang. 1995. A study of suicide among Vietnam veterans. Federal Practitioner 12:9-13.
Bullman, T. A., and H. K. Kang. 1996. Risk of suicide among wounded Vietnam veterans. American Journal of Public Health 86(5):662-667.
Bullman, T. A., and H. K. Kang. 1997. Posttraumatic stress disorder and the risk of traumatic death among Vietnam veterans. In Posttraumatic stress disorder: Acute and long-term responses to trauma and disaster, edited by C. S. Fullerton and R. J. Ursano. Washington, DC: American Psychiatric Press, Inc. Pp. 175-190.
Bullman, T. A., H. K. Kang, and K. K. Watanabe. 1990. Proportionate mortality among U.S. Army Vietnam veterans who served in military region I. American Journal of Epidemiology 132(4): 670-674.
Bullman, T. A., H. K. Kang, and T. L. Thomas. 1991. Posttraumatic stress disorder among Vietnam veterans on the Agent Orange Registry: A case-control analysis. Annals of Epidemiology 1(6): 505-512.
Bullman, T. A., K. K. Watanabe, and H. K. Kang. 1994. Risk of testicular cancer associated with surrogate measures of Agent Orange exposure among Vietnam veterans on the Agent Orange Registry. Annals of Epidemiology 4(1):11-16.
Dalager, N. A., H. K. Kang, V. L. Burt, and L. Weatherbee. 1991. Non-Hodgkin’s lymphoma among Vietnam veterans. Journal of Occupational Medicine 33(7):774-779.
Dalager, N. A., H. K. Kang, V. L. Burt, and L. Weatherbee. 1995. Hodgkin’s disease and Vietnam service. Annals of Epidemiology 5(5):400-406.
Dalager, N. A., and H. K. Kang. 1997. Mortality among Army Chemical Corps Vietnam Veterans. American Journal of Industrial Medicine 31(6):719-726.
Farberow, N. L., H. K. Kang, and T. A. Bullman. 1990. Combat experience and postservice psychosocial status as predictor of suicide in Vietnam veterans. Journal of Nervous and Mental Disease 178:32-37.
Kang, H. K., L. Weatherbee, P. P. Breslin, Y. Lee, and B. M. Shepard. 1986. Soft tissue sarcoma and military service in Vietnam: A case comparison group analysis of hospital patients. Journal of Occupational Medicine 28(12):1215-1218.
Kang, H. K., F. Enzinger, P. Breslin, M. Feil, Y. Lee, and B. Shepard. 1987. Soft tissue sarcoma and military service in Vietnam: A case-control study. Journal of the National Cancer Institute 79(4): 693-699.
Kang, H. K., K. K. Watanabe, J. Breen, J. Remmers, M. G. Conomos, J. Stanley, and M. Flicker. 1991. Dioxins and dibenzofurans in adipose tissue of U.S. Vietnam veterans and controls. American Journal of Public Health 81(3):344-349.
Kang, H. K., N. A. Dalager, L. L. Needham, D. G. Patterson, G. M. Matanoski, S. Kanchanaraksa, and P. S. Lees. 2001. U.S. Army Chemical Corps Vietnam veterans health study: Preliminary results. Chemosphere 43(4-7):943-949.
Kang, H. K., N. A. Dalager, L. L. Needham, D. G. Patterson, P. S. Lees, K. Yates, and G. M. Matanoski. 2006. Health status of Army Chemical Corps Vietnam veterans who sprayed defoliant in Vietnam. American Journal of Industrial Medicine 49(11):975-884.
Mahan, C. M., T. A. Bullman, H. K. Kang, and S. Selvin. 1997. A case-control study of lung cancer among Vietnam veterans. Journal of Occupational and Environmental Medicine 39(8):740-747.
Thomas, T. L., and H. K. Kang. Mortality and morbidity among Army Chemical Corps Vietnam veterans: A preliminary report. American Journal of Industrial Medicine 18(6):665-673.
Watanabe, K. K., and H. K. Kang. 1995. Military service in Vietnam and the risk of death from trauma and selected cancer. Annals of Epidemiology 5(5):407-412.
Watanabe, K. K., and H. K. Kang. 1996. Mortality patterns among Vietnam veterans: 24-year retrospective analysis. Journal of Occupational and Environmental Medicine 38(3):272-278.
Watanabe, K. K., H. K. Kang, and T. L. Thomas. 1991. Mortality among Vietnam veterans: With methodological considerations. Journal of Occupational Medicine 33(7):780-785.
Young, A. L., H. K. Kang, and A. L. Shepard. 1983. Chlorinated dioxins as herbicide contaminants. Environmental Science and Technology 17:530A-540A.
APPENDIX K-2
SELECTED NATIONAL ACADEMIES REPORTS ON U.S. VETERANS’ HEALTH2 (IN CHRONOLOGICAL ORDER)
NRC (National Research Council). 1982. Possible long-term health effects of short-term exposure to chemical agents: Anticholinesterases and anticholingergics. Vol. 1. Washington, DC: National Academy Press.
NRC. 1984. Possible long-term health effects of short-term exposure to chemical agents: Cholinesterase reactivators, psychochemicals and irritants and vesicants. Vol. 2. Washington, DC: National Academy Press.
NRC. 1985. Possible long-term health effects of short-term exposure to chemical agents. Volume 3. Final report. Current health status of test subjects. Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1991. Epidemiology in military and veteran populations: Proceedings of the 2nd biennial conference, March 7, 1990. Washington, DC: National Academy Press.
IOM. 1995. Recommendations for research on the health of military women: Bibliographies. Washington, DC: National Academy Press.
IOM. 1996. Interactions of drugs, biologics, and chemicals in U.S. military forces. Washington, DC: National Academy Press.
IOM. 1996. Military nursing research: Bibliographies. Washington, DC: National Academy Press.
IOM. 1997. Adequacy of the Comprehensive Clinical Evaluation Program: A focused assessment. Washington, DC: National Academy Press.
IOM. 1997. An evaluation of radiation exposure guidance for military operations: Interim report. Washington, DC: National Academy Press.
IOM. 1998. Assessing readiness in military women: The relationship of body, composition, nutrition, and health. Washington, DC: National Academy Press.
IOM. 1999. National Center for Military Deployment Health Research. Washington, DC: National Academy Press.
IOM. 1999. Potential radiation exposure in military operations: Protecting the soldier before, during, and after. Washington, DC: National Academy Press.
IOM. 2000. Protecting those who serve: Strategies to protect the health of deployed U.S. forces. Washington, DC: National Academy Press.
IOM. 2005. Noise and military service: Implications for hearing loss and tinnitus. Washington, DC: The National Academies Press.
IOM. 2006. Amyotrophic lateral sclerosis in veterans: Review of the scientific literature. Washington, DC: The National Academies Press.
IOM. 2006. Disposition of the Air Force Health Study. Washington, DC: The National Academies Press.
APPENDIX K-3
VIETNAM EXPERIENCE STUDY AND OTHER CDC STUDIES ON VIETNAM VETERANS AND GULF WAR VETERANS
Vietnam Experience Study
Background
Conducted by the Centers for Disease Control and Prevention (CDC), the Vietnam Experience Study compared the morbidity and mortality among Vietnam veterans and non-Vietnam veterans.
|
2 |
Not intended to be a comprehensive list. See www.nap.edu for additional reports. |
Vietnam veterans were concerned that their service in Vietnam adversely affected their health, and the health of their families. However, data did not exist comparing those who served in Vietnam and those who served during the Vietnam War in other countries. In 1979 President Jimmy Carter signed the Veterans Health Programs Extension and Improvement Act of 1979 that called for the Veterans Administration (VA) to “conduct an epidemiological study of persons who, while serving in the Armed Forces of the United States during the period of the Vietnam conflict, were exposed to any of the class of chemicals known as ‘the dioxins’ produced during the manufacture of the various phenoxy herbicides (including the herbicide known as ‘Agent Orange’) to determine if there may be long-term adverse health effects in such persons from such experiences” (Veterans Health Programs Extension and Improvement Act of 1979. Public Law 96-151. 96th Cong., 1st Sess.; as referenced in CDC VES, 1989b, pp. 4-5).
In 1981 an amendment was passed to the law above to include “an evaluation of any long-term adverse health effects in humans of such [military] service as such health effects may result from other factors involved in such [military] service, including exposure to other herbicides, chemicals, medications, or environmental hazards or conditions” (Veterans’ Health Care, Training, and Small Business Loan Act of 1981. Public Law 97-72. 97th Cong., 1st Sess.; as referenced in CDC VES, 1989b, p. 5).
The responsibility of designing, conducting, and analyzing such an investigation was originally bestowed upon VA and then transferred, by an Interagency Agreement, to the CDC. The CDC was then authorized to conduct three studies: the Agent Orange Exposure Study, the Selected Cancers Study, and the Vietnam Experience Study (CDC VES, 1989a, p. 3). This section will focus on the Vietnam Experience Study (VES).
VES Main Objectives
Is there an excess risk of postservice mortality for the Vietnam group? (If so, due to what causes?)
-
Is there an excess risk of specific illnesses (including psychological) or groups of postservice illnesses for the Vietnam group?
-
Is there an excess of adverse reproductive outcomes or childhood illnesses among children of the Vietnam group?
(CDC VES, 1989a, p. 4)
VES Cohort
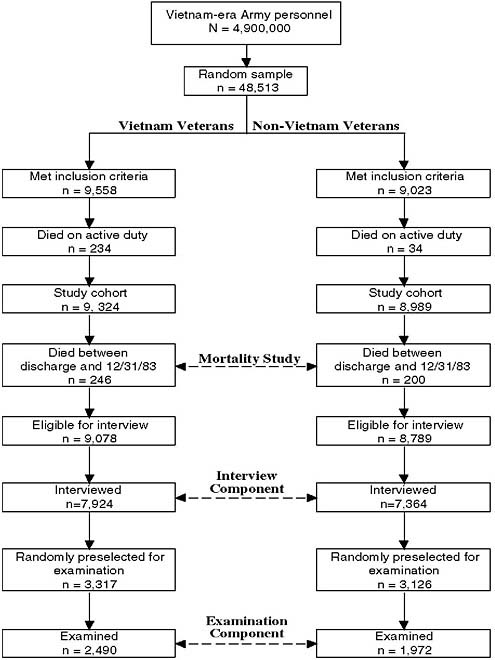
The VES cohort included a random sample of male Vietnam and non-Vietnam veterans (limited to those who served in the United States, Germany, or Korea). The random selection process was based on “a computerized list of accession numbers taken from military personnel files of Army veterans discharged during the relevant time period” (CDC VES, 1987a). Sample sizes are given in Figure K-1. The inclusion criteria for this study were
-
Army veterans (Marine, Air Force, and Navy personnel were not included);
-
military occupational specialty (MOS) other than “duty soldier” and “trainee”;
-
single term of enlistment;
-
minimum of 16 weeks of active duty time;
-
pay grade E-1 (Private) to E-5 (Sergeant-Specialist 5);
Demographics3
-
Vietnam veterans were more likely than non-Vietnam veterans to have
-
lower General Technical (GT) test scores;
-
entered the Army before 1969;
-
been volunteers;
-
had a tactical operation primary MOS;
-
been in a combat unit;
-
honorable discharges;
-
been discharged at pay grades >E3;
-
lower educational attainment at time of interview;
-
more unemployment at time of interview;
-
lower income in year immediately preceding the interview;
-
used drugs (marijuana only, or hard drugs) at least once/week in past year;
-
received therapy for drug, alcohol, or emotional problems in past year; and
-
drank, on average, ≥90 drinks per month (CDC VES, 1989a, Tables 2-4).
-
-
Vietnam veterans were significantly less likely than non-Vietnam veterans to have an executive/managerial professional specialty (OR = 0.9, 95% CI 0.8-0.9) (CDC VES, 1989b, p. 44).
-
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to
-
region of birth, region of residence at time of interview;
-
year of birth, age at interview;
-
race;
-
mean age at enlistment;
-
percent with some AWOL or confinement time;
-
current martial status; and
-
cigarette smoking.
-
Components of the VES
The VES included a mortality study, a telephone interview, an examination (medical, psychological, and laboratory), and a reproductive outcomes and child health component.
Primary potential confounders The primary potential confounders adjusted for in all analyses listed below are as follows:
-
Race = white (referent), black, other
-
Age at entry into the Army = <20 years (referent), ≥20 years
-
Year of entry into Army = 1965-1966 (referent), 1967-1969, 1970-1971
-
Primary MOS = tactical, other (referent)
-
Enlistment status = drafted (referent), volunteered
-
GT test score = 40-89, 90-109 (referent), 110-129, 130-160 (CDC VES, 1989b, p. 23, Table 4)
For this summary on the VES analytical results, if the significance levels are not reported here, they were not reported in the documentation obtained from the CDC. Also, the VES full documentation presents both models: (1) the model only adjusting for the primary potential confounds listed above and (2) a multivariable model that adjusts for further potential confounders as appropriate. However, since the two models offer similar results, this summary only lists the results from the first model.
The Mortality Study: Postservice mortality among Vietnam veterans Mortality among the Vietnam veterans (n = 9,324) was compared to that of the non-Vietnam veterans (n = 8,989), based on information from personal physicians as well as hospital records, autopsy reports, and coroner and law enforcement files. The data showed that, over the entire follow-up period, total mortality in the Vietnam veterans was 17 percent higher than for the non-Vietnam veterans (http://www.cdc.gov/nceh/veterans/default1a.htm; CDC VES, 1987a,b). “The excess in postservice mortality due to external causes among Vietnam veterans is similar to that found among men returning from combat areas after World War II and the Korean War” (CDC VES, 1987b). Selected findings on mortality are given in Table K-1. Other findings on mortality included the following:
-
When all drug-related deaths were analyzed together, “the rate ratio between Vietnam and non-Vietnam veterans appeared to increase with the number of years since discharge.” This difference was found “almost exclusively among draftees; those assigned to tactical military occupational specialties; and those serving in Vietnam during 1968 or 1969, the years of heaviest combat activity.”
-
Alcohol did not seem to account for the difference in motor vehicle crashes between the Vietnam veterans and the non-Vietnam veterans.
-
Vietnam veterans were significantly less likely than non-Vietnam veterans to die from circulatory system diseases (OR = 0.5, 95% CI 0.25-0.99).
TABLE K-1 Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Die from the Following Conditions
|
Condition |
Risk Ratio (RR) |
95% Confidence Interval (CI) |
|
Mortalitya within 5 years of discharge |
1.45 |
1.08-1.96 |
|
Suicides within 5 years of discharge |
2.56 |
1.11-5.87 |
|
Motor vehicle crashes |
1.48 |
1.04-2.09 |
|
aMortality mostly due to motor vehicle accidents, suicide, homicide, and accidental poisonings. SOURCE: CDC VES, 1987a,b. |
||
-
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to mortality from unintentional poisonings, most of which were due to the use of illicit drugs.
-
After the initial 5 years after discharge, there were no significant differences in mortality among the Vietnam veterans and the non-Vietnam veterans, except that drug-related deaths continued to be elevated in the Vietnam veterans.
The telephone interview Under contract with the CDC, Research Triangle Institute (RTI) located, contacted, and interviewed the veterans with the help of Equifax, Inc. which provided multilevel locating and contacting services. To locate veterans these companies used the permanent addresses provided by the veterans at the time of discharge, the names and addresses of family members provided by the veterans upon entry into the service, the address on the veterans’ most recent tax return, and the address provided by the veterans when filing for benefits (CDC VES, 1989a, pp. 7-8; CDC VES, 1989b, p. 9).
Eventually, 9,078 Vietnam veterans and 8,789 non-Vietnam veterans were found to be eligible for the interview (i.e., those not known to have died before December 31, 1983). Of these, veterans were not interviewed if they could not be located, refused to be interviewed, were unable to contact, were incarcerated, died after December 31, 1983, or were mentally or physically incapable of being interviewed. Thus, 7,924 Vietnam veterans and 7,364 non-Vietnam veterans were ultimately interviewed (CDC VES, 1989a, p. 7, Figure 1; CDC VES, 1989b, p. 31, Table 6).
It is important to note that there were differences between those interviewed and those not interviewed. On average, compared to those interviewed (Vietnam and non-Vietnam veterans combined, unless otherwise stated), those not interviewed (Vietnam and non-Vietnam veterans combined, unless otherwise stated) were more often nonwhite (21.5 percent vs. 11.6 percent), younger at enlistment (56.2 percent <20 years vs. 48.8 percent <20 years), volunteers (41.0 percent vs. 34.2 percent), having lower scores on the GT test (mean score about 100.0 vs. 105.2), and more likely received non-honorable discharges (8.0 percent for Vietnam veterans and 21.2 percent for non-Vietnam veterans vs. 1.8 percent for Vietnam veterans and 6.2 percent for non-Vietnam veterans) and discharged at lower pay grades (23.7 percent for Vietnam veterans and 40.1 percent for non-Vietnam veterans vs. 9.3 percent for Vietnam veterans and 15.9 percent for non-Vietnam veterans) (CDC VES, 1989b, pp. 31-33, Table 8). However, significance levels for these differences were not reported in the documents.
Although the unlocatable subset of the non-respondent group appears to be very different from respondents with respect to demographic and military characteristics, about the same degree of divergence is seen for both Vietnam and non-Vietnam veterans. Thus, absence of interview data from the lost-to-follow-up group should not adversely affect the findings presented here.
(CDC VES, 1989b, p. 33)
Selected findings from the telephone interviews are shown in Tables K-2, K-3, K-4, and K-5.
TABLE K-2 Current Health Status: Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Have the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Perceived fair/poor health |
1.8 |
1.7-2.0 |
|
Higher mean BMI |
BMI = geometric mean 25.7 vs. 25.5 |
p = 0.004 |
|
Limitations in activities |
1.3 |
1.2-1.4 |
|
≥3 prescribed medications |
1.3 |
1.1-1.6 |
|
General symptoms |
2.5 |
1.7-3.6 |
|
SOURCE: CDC VES, 1989b, Tables 18, 19, 20, 22, 102. |
||
TABLE K-3 Health Status Between Discharge and Time of Interview: Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Have Experienced/Suffered from the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
≥1 hospitalization |
1.1 |
p <0.05 |
|
Hypertension |
1.3 |
1.2-1.4 |
|
Benign growths |
1.2 |
1.1-1.3 |
|
Chloracne |
3.9 |
2.5-6.2 |
|
Excessive hair growth |
1.9 |
1.6-2.3 |
|
Other skin conditions |
1.8 |
1.7-2.0 |
|
Gastrointestinal ulcers |
1.2 |
1.1-1.3 |
|
≥4 Neurologic symptoms |
2.0 |
1.8-2.3 |
|
Hepatitis B |
1.5 |
1.3-1.8 |
|
Other liver conditions |
1.4 |
1.1-1.8 |
|
Urinary tract problems |
1.2 |
1.1-1.3 |
|
Fertility difficulties |
1.3 |
1.2-1.5 |
|
SOURCE: CDC VES, 1989a, p. 18, Table 5; 1989b, pp. 100, 371-373, Table 73, Table I-I. |
||
TABLE K-4 Reported Medical Care: Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Report Medical Care While in the Army for the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Intestinal infections |
2.7 |
2.1-3.5 |
|
Malaria |
104.0 |
33.3-324.4 |
|
Sexually transmitted disease |
2.0 |
1.7-2.4 |
|
Mycoses |
6.5 |
4.8-9.0 |
|
Ear disorders |
1.7 |
1.4-2.0 |
|
Hepatitis B |
1.8 |
1.3-2.5 |
|
Skin infections |
2.1 |
1.7-2.7 |
|
Other skin disease |
1.3 |
1.1-1.6 |
|
Rash |
3.3 |
2.5-4.3 |
|
Fever |
2.3 |
1.7-3.0 |
|
Open wounds |
3.5 |
3.1-4.0 |
|
Superficial injuries |
1.6 |
1.1-2.1 |
|
Burns |
1.8 |
1.2-2.5 |
|
SOURCE: CDC VES, 1989b, pp. 37-39, Table 12. |
||
TABLE K-5 Vietnam Veterans Were Significantly Less Likely Than Non-Vietnam Veterans to Report Medical Care While in the Army for the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Strep infections |
0.6 |
0.5-0.8 |
|
Acute respiratory infection |
0.8 |
0.7-0.9 |
|
Other upper respiratory disease |
0.6 |
0.4-0.8 |
|
Influenza |
0.8 |
0.7-0.9 |
|
Osteopathy |
0.7 |
0.5-0.9 |
|
SOURCE: CDC VES, 1989b, pp. 37-39, Table 12. |
||
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to postdischarge cancer, diabetes, and cirrhosis (CDC VES, 1989a, p. 18, Table 5).
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to viral exanthemas; neoplasms; endocrine, nutritional, and metabolic disease; mental disorders; disease of the nervous system; eye disorders; circulatory disease; pneumonia; digestive diseases (except for hepatitis B); genitourinary disease; dermatitis; musculoskeletal disease (except for osteopathy); head and neck symptoms; cardiorespiratory symptoms; fractures, dislocations, sprains and strains, intracranial injuries, contusions, other and unspecified injuries; and poisoning (CDC VES, 1989b).
The examination At the end of the telephone interview, veterans were told if they were preselected by RTI to be examined. The preselection process was done randomly by RTI and names and information were then transferred to the Lovelace Medical Foundation (LMF) in Albuquerque, New Mexico. LMF was under contract with the CDC to schedule the examination appointments which were conducted at LMF, arrange the veterans’ round-trip travel to Albuquerque, and provide food and lodging during the examination period (CDC VES, 1989c, p. 16). Over 3,300 Vietnam veterans and over 3,100 non-Vietnam veterans were invited for the examination. However, veterans were not examined if they could not be contacted, refused to be examined, were incarcerated, died after December 31, 1983, were mentally or physically incapable of being examined, or were in a mental institution. Ultimately 2,490 Vietnam veterans and 1,972 non-Vietnam veterans were examined (CDC VES, 1989c, pp. 31, 32). See the demographics section above for differences between the Vietnam and non-Vietnam veterans.
It is important to note that there were also some differences between those examined and those not examined. Higher participation rates were observed among blacks compared to whites, those in the youngest age group compared to those in the older age groups, those with higher levels of education, those in the lowest income category, and those not married compared to those currently married. However, the documentation did not present significance levels (CDC VES, 1989c, pp. 33-34).
For the 3 days before the examination, the veterans were instructed not to eat red meat, pork, or sweets; drink any alcohol or use any mouthwash; take any multivitamins or vitamin C supplements; take any nonprescription drugs; or start a new exercise program. However, participants could continue current prescription medications and exercise programs. From 7pm the night before the first day of examinations, the participants were asked to fast, permitting only water, and during the night they began a 12-hour urine sample (CDC VES, 1989c, p. 17).
Participants were in Albuquerque for 4 days. The first day included an orientation session. The next day started with a morning blood draw, followed by a medical examination (including a medical history questionnaire and general physical, dermatologic and neurological clinical tests), special medical tests (chest roentgenogram, electrocardiogram, pulmonary function, Doppler evaluation of peripheral vasculature, hypersensitivity skin test, nerve conduction velocities, vibratory sensation, audiometry, visual acuity), and laboratory tests (hematologic assays, serum analytes, hepatitis B, endocrine, immunology, urinalysis, 12-hour urine, semen analysis, erythrocyte sedimentation rate, prothrombin time, rapid plasma regain test, stool occult blood, melioidosis antibody titer, breath alcohol level). The third day focused on psychological and neurological tests conducted in a special center at their hotel. On the fourth day the veterans met with an internist and a psychologist to discuss their individual results (CDC VES, 1989c, p. 17). Selected results from the examinations are shown in Tables K-6, K-7, K-8, K-9, and K-10.
TABLE K-6 Current Health Status: Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Currently Have the Following Conditions
|
Condition |
Odds Ratio (OR) |
p-value |
|
Perceived fair/poor health |
1.9 |
p <0.05 |
|
Somatic symptoms |
1.7 |
p <0.05 |
|
SOURCE: CDC VES, 1988a,b; 1989a, p. 18, Table 5. |
||
TABLE K-7 Postdischarge Health Status: Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Vetetrans to Have Experienced/Suffered form the Following Conditions Postdischarge
|
Condition |
Odds Ratio (OR) |
p-Value |
|
Hypertension |
1.2 |
p <0.05 |
|
Chloracne |
7.3 |
p <0.05 |
|
Other skin conditions |
1.7 |
p <0.05 |
|
Other liver conditions |
1.7 |
p <0.05 |
|
Fertility difficulties |
1.5 |
p <0.05 |
|
SOURCE: CDC VES, 1989a, p. 18, Table 5. |
||
TABLE K-8 Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Have Experienced the Following Conditions
|
Conditiona |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Alcohol abuse or dependence |
1.5 |
1.2-1.8 |
|
Generalized anxiety |
1.5 |
1.1-2.1 |
|
Depression |
2.0 |
1.4-2.9 |
|
≥1 of the above conditions |
1.5 |
1.3-1.8 |
|
≥2 of the above conditions |
1.9 |
1.2-2.8 |
|
aBased on the Diagnostic Interview Schedule. SOURCE: CDC VES, 1989a, pp. 24-26, Tables 13-15. |
||
TABLE K-9 Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Have Elevated Levels on the Minnesota Multiphasic Personality Inventory Clinical Scales
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Scale 1 (Hypocondriasis) |
1.7 |
1.4-2.1 |
|
Scale 2 (Depression) |
1.6 |
1.3-1.8 |
|
Scale 3 (Hysteria) |
1.5 |
1.2-2.0 |
|
Scale 7 (Obsessive-compulsive syndrome) |
1.6 |
1.3-1.9 |
|
Scale 8 (Schizophrenia) |
2.0 |
1.6-2.4 |
|
≥1 or more scales elevated |
1.3 |
1.2-1.5 |
|
≥2 or more scales elevated |
1.5 |
1.2-1.7 |
TABLE K-10 Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Experience the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
High-frequency hearing loss |
|
|
|
Right ear |
1.4 |
1.2-1.7 |
|
Left ear |
1.4 |
1.2-1.6 |
|
Both ears |
1.4 |
1.1-1.8 |
|
Peripheral nervous system abnormalities—leg absent pinprick (distal dorsal) |
1.6 |
1.1-2.4 |
|
SOURCE: CDC VES, 1989a, pp. 20-21, Tables 8-9; 1989c, pp. 110, 113, Tables 7.9, 7.12. |
||
Medical history questionnaire
-
These results are somewhat different than those from the telephone interview.
-
Vietnam veterans reported more current health problems than non-Vietnam veterans, particularly for mental disorders; diseases of the nervous system; diseases of the skin; symptoms, signs, and ill-defined conditions. However, significance levels were not reported in the document.
-
Vietnam veterans reported more physician-diagnosed alcohol-related liver damage, hepatitis B, gastritis, and stomach or duodenal ulcer, and less physician-diagnosed cirrhosis than non-Vietnam veterans. However, significance levels were not reported in the document.
-
There were no significant differences between Vietnam veterans and non-Vietnam veterans with respect to current limitation in activities or prescribed medications. These results are different than those from the telephone interview listed above.
-
There were no significant differences between Vietnam veterans and non-Vietnam veterans with respect to post-discharge hospitalization, cancer, benign growth, diabetes, gastrointestinal ulcers, hepatitis B, cirrhosis, and urinary tract problems. These results are somewhat different than those from the telephone interview listed above.
Cardiac tests There were no significant differences between the Vietnam and non-Vietnam veterans with respect to hypertension, altered peripheral arterial hemodynamics, electrocardiogram findings (ischemia, left ventricular hypertrophy, any finding), chest roentgenogram findings (pulmonary, cardiac, any finding), or pulmonary function parameters (CDC VES, 1989a, p. 19, Table 7).
Dermatologic examinations There were no significant differences between the Vietnam and non-Vietnam veterans with respect to chloracne-like lesions, acneiform lesions, hyperpigmentation, skin cancer, infections, and postinflammatory scars. These results are somewhat difference than those from the telephone interview (CDC VES, 1989a, p. 19, Table 6; CDC VES, 1989b, pp. 56-58).
Psychiatric examinations
-
There was no significant difference between the Vietnam veterans and the non-Vietnam veterans with respect to drug abuse or dependence.
-
Combat-related PTSD analysis was restricted to Vietnam veterans since non-Vietnam veterans had a low likelihood of experiencing combat. Almost 15 percent Vietnam veteran had experienced PTSD prior to examination while over 2 percent experienced PTSD the month before the examination.
-
There were no significant differences between the Vietnam veterans and non-Vietnam veterans with respect to MMPI scale 4 (psychopathic personality disorders), scale 5 (male sexual inversion), scale 6 (Paranoia), scale 9 (hypomania), or scale 0 (uneasiness in social situations or dealing with others).
Neurological examinations/tests
-
Vietnam veterans had a significantly lower mean score on the Army Classification Battery (ACB) General Technical Test at examination, Rey-Osterreith Test (RO) Complex Figure-Copy, Wechsler Adult Intelligence Scale-Revised (WAIS-R) block design subset (p <0.05), and a significantly higher average number of cards per sort on the Wisconsin Card Sorting Test (p <0.05).
-
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to peripheral neuropathy.
-
There were no significant differences between the Vietnam veterans and non-Vietnam veterans with respect to a mean score on the California Verbal Learning Tests, Grooved Pegboard, Paced Auditory Serial Addition Test, short-delay recall and long-delay recall
-
on the RO Complex Figure, the information subset of the WAIS-R, and Word List Generation.
Hematological/laboratory tests (CDC VES, 1989c, pp. 174, 176, 187, 190, Tables 11.5, 11.8, 12.6, 12.8)
-
Vietnam veterans had significantly higher fasting serum glucose (difference = 0.9mg/dl, 95% CI 0.2-1.6) and thyroid-stimulating hormone (difference = 4.3mIU/L, 95% CI 0.5-8.2).
-
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to
-
mean red cell count, hemoglobin, hematocrit, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, white cell count, segmented neutrophil, band neutrophil, lymphocyte, monocyte, eosinophil, basophil, platelet count and prothrombin time;
-
free thyroxine index, cortisol, dehydroepiandrosterone, testosterone, follicle-stimulating hormone, or luteinizing hormone;
-
blood urea nitrogen or serum creatinine; and
-
diabetes or hypothyroidism.
-
Semen tests (CDC VES, 1989c, pp. 208-209, Tables 13.5, 13.6)
-
Vietnam veterans had significantly lower sperm concentrations (mean difference = −20.2 million cells/mL, 95% CI −34.5 to −2.8) and a lower percent of normal cell morphology (mean difference = −3.8 percent, 95% CI −6.6 to −0.9) compared to non-Vietnam veterans.
-
There were no significant differences between the Vietnam veterans and the non-Vietnam veterans with respect to movement characteristics (percent motile cells, mean linear velocity, mean straight line velocity, mean linearity, mean amplitude lateral head displacement, mean beat/cross frequency).
Reproductive outcomes and child health During the interview, data on the following topics were collected:
-
Basic data for all veterans’ biological children, including month and year of birth, sex of child, live-born or stillborn status
-
Birth defects of malformations diagnosed by a physicians—up to two per child
-
Physician-diagnosed major health problems or impairments occurring in the first 5 years of life, not including normal childhood diseases and injuries—up to three per child
-
Leukemia and other types of cancer
-
Infant and child mortality
-
Pregnancies fathered by the veteran that ended early, including miscarrages, induces abortions, and tubal pregnancies
(CDC VES, 1989d, p. 9)
Selected results from the interview are as follows are shown in Tables K-11, K-12, and K-13.
TABLE K-11 The Offspring of Vietnam Veterans Were Significantly More Likely Than Those of Non-Vietnam Veterans to Have the Following Conditions
|
Condition |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Been miscarried |
1.3 |
1.2-1.4 |
|
Anomalies (total) |
1.3 |
1.2-1.4 |
|
Anemia |
1.9 |
1.1-3.2 |
|
Diseases of the ear |
1.3 |
1.1-1.6 |
|
Diseases of the skin |
1.5 |
1.1-2.0 |
|
Symptoms and signs |
1.5 |
1.2-1.8 |
|
Injuries and poisoningsa |
1.6 |
1.2-2.1 |
|
aStandardized for race. SOURCE: CDC VES, 1989d, pp. 22-28, Tables 10, 11, 14, 15, 16, 17, 19, 21, 23. |
||
TABLE K-12 Vietnam Veterans Were Significantly More Likely Than Non-Vietnam Veterans to Father Children with Birth Defects of These Organ Systems
|
Organ System |
No. of Children |
Odds Ratio(OR)a |
95% Confidence Interval (CI) |
|
|
Vietnam |
Non-Vietnam |
|||
|
Total anomalies |
826 |
590 |
1.3 |
1.2-1.4 |
|
Nervous |
33 |
13 |
2.3 |
1.2-4.5 |
|
Hydrocephalus |
11 |
2 |
5.1b |
1.1-23.1 |
|
Musculoskeletal |
426 |
309 |
1.2 |
1.1-1.5 |
|
Integument |
41 |
17 |
2.2 |
1.2-4.0 |
|
aAdjusted for primary potential confounders listed above, as well as years between entry into Army and birth of the child. bCrude OR because the number of cases is not sufficient for multivariable modeling. SOURCE: CDC VES, 1989d, pp. 22-28, Tables 10, 11, 14, 15, 16, 17, 19, 21, 23. |
||||
TABLE K-13 Vietnam Veterans Were Significantly More Likely Than NonVietnam Veterans to Report the Following Birth Defects
|
Birth Defect |
Odds Ratio (OR) |
95% Confidence Interval (CI) |
|
Children with 1 birth defect |
1.3 |
1.1-1.4 |
|
Children with >1 birth defect |
1.6 |
1.1-2.5 |
|
1 child with 1 birth defect |
1.2 |
1.1-1.4 |
|
SOURCE: CDC VES, 1989d, pp. 22-28, Tables 10, 11, 14, 15, 16, 17, 19, 21, 23. |
||
-
There were no significant differences between the Vietnan veterans and the non-Vietnam veterans with respect to induced abortions, and tubal pregnancies, stillbirths, and childhood cancer among the offspring.
-
There were no significant differences between the offspring of the Vietnam veterans and the non-Vietnam veterans with respect to infectious and parasitic diseases, benign and unspecified neoplasms, endocrine disease, mental disorders, nervous system diseases (except for diseases of the ear), circulatory system diseases, respiratory system diseases,
-
digestive system diseases, genitourinary system diseases, urinary tract infection, musculoskeletal disease, perinatal conditions, and supplementary classifications.
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to total serious health problems, infant mortality or child mortality.
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to birth defects of the eye; ear, face, and neck; circulatory system; respiratory system; digestive system; genitals; urinary system; or other unspecified systems.
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to veterans reporting more than one child with a birth defect.
The General Birth Defects Sub-Study
The General Birth Defects (GBD) Sub-Study was designed to compare the rates of birth defects, as presented in hospital birth records, among offspring of Vietnam veterans and those among non-Vietnam veterans. This comparison was also used to validate the data from the telephone interview (see data above). Selected results from this substudy are as follows:
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to major, minor, or suspected birth defects.
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to defects of the ear, face, and neck; digestive system; genitals; musculoskeletal system; or integument system.
-
There were no significant differences between the offspring of the Vietnam veterans and those of the non-Vietnam veterans with respect to having a child with low birth weight or perinatal deaths. (CDC VES, 1989d, p. 46, Tables 16, 19, 21, 23, 24)
The Cerebrospinal Malformations Sub-Study
The Cerebrospinal Malformations (CSMs) Sub-Study also used hospital birth records to identify all children with possible cerebrospinal malformations (i.e., a reported CSM, a reported condition that suggested a possible CSM, and all children reported as stillborn) (CDC VES, 1989d, p. 46). Selected results from this sub-study are as follows:
-
Among reported stillbirths, 5 CSMs in the offspring of Vietnam veterans and 6 CSMs in the offspring of non-Vietnam veterans were found; 10 of which were not reported during the time of the interview.
-
Among reported live births, 21 CSMs in the offspring of Vietnam veterans and 6 CSMs in the offspring of non-Vietnam veterans were found.
-
The CSMs observed in Vietnam veterans were anencephaly (n = 10), spina bifida (n = 9), and hyrocephalus (n = 7).
-
The CSMs observed in non-Vietnam veterans were anencephaly (n = 7), spina bifida (n = 2), and hyrocephalus (n = 3). (CDC VES, 1988c)
“Because record retrieval rates varied considerably by cohort status and because negative responses were not verified, we did not calculate or compare rates of CSM cases in the two cohorts; the results are expressed as numbers of verified cases” (CDC VES, 1988c).
Strengths of the VES
As listed in the VES documentation (CDC VES, 1989a, p. 32), the major strengths of the VES are as follows:
-
The random sampling method used to identify large representative samples of Vietnam and non-Vietnam veterans
-
The measures used to assure good comparability of the two cohorts
-
The rigorous vital status ascertainment and cause of death classification methods
-
The high participation rates in the interview component
-
The comparability of the examined cohorts (in the face of differential participation rates)
-
The attempt at independent validation of certain interview outcomes
-
The meticulous data control and bias-avoidance methods used in all components of the study
Limitations of the VES
As listed in the VES documentation (CDC VES, 1989a, p. 32), the major limitations of the VES are as follows:
-
The long time that has elapsed since the end of the Vietnam conflict
-
The differential participation rates in the examined cohorts
-
The lack of any reliable indirect estimate of the Agent Orange exposure (the study was not designed to focus on Agent Orange exposure)
-
The fact that the VES “exposure,” the Vietnam experience, represents a large variety of individual experiences (e.g., combat exposure) that are probably not homogeneous
Selected Cancers Study
Background
Vietnam veterans are concerned that exposure to Agent Orange and especially its TCDD contaminant may negatively impact their health. in response to this concern and to the Veterans Health Programs Extension and Improvement Act of 1979 (Public Law 96-151. 96th Cong., 1st Sess.) and the Veterans’ Health Care, Training, and Small Business Loan Act of 1981 (Public Law 97-72. 97th Cong., 1st Sess.), the CDC conducted the Vietnam Experience Study (see above) and the Selected Cancers Study (CDC VES, 1989a, p. 3).
The Selected Cancers Study is a case-control study of veterans’ risk to six rare cancers (non-Hodgkin’s lymphoma, Hodgkin’s disease, soft-tissue and other sarcomas, nasal cancer, nasopharyngeal cancer, and primary liver cancer among Vietnam veterans) thought to be associated with TCDD exposure based on published literature (see http://www.cdc.gov/nceh/veterans/default1d.htm). This study “focuses on the risk of cancer after service in Vietnam in general. We only indirectly examine any possible association with
herbicide exposure through investigation of service characteristics such as military branch, region of service in Vietnam, calendar years of service, and specific duties that involved the handling of herbicides” (Selected Cancers Cooperative Study Group, 1990b, p. 2474).
Methodology
The three investigations within this study follow the same methodology and control series. The study includes a consensus diagnosis from three experts to confirm the cases (only these are included in the analysis), a standardized telephone interview, and microscopic slides or tissue blocks for 97 percent of lymphoma cases interviewed from pathology department where diagnosis was given (Selected Cancers Cooperative Study Group, 1990a, pp. 1, 12; Selected Cancers Cooperative Study Group, 1990b, p. 2474). The Environmental Support Group also reviewed the medical records of those stationed in Vietnam, when permission was granted (Selected Cancers Cooperative Study Group, 1990b).
The cases and controls were randomly assigned to interviewers so each interviewer had a similar number of cases and control (see Table K-14). The telephone interviews took about 50 minutes to complete, and were conducted in English, Spanish, and Cantonese by fluent speakers. Those who served in Vietnam were asked about dates of tour, branch of service, rank, unit, location in Vietnam, job duties, and self-perceived exposure to herbicides while in Vietnam. They were also asked to name the specific herbicides that they used on crops, in landscaping, in right-of-way maintenance along power lines, rail lines, and in forestry. in this study “stationed in Vietnam” includes those stationed off the coast. The U.S. Army and Joint Services Environmental Support Group then classified veterans’ units into those likely to be combat, combat support, or support based on information provided during the interview (they were not aware of the veterans’ control and case status) (Selected Cancers Cooperative Study Group, 1990a, pp. 16, 18-19; Selected Cancers Cooperative Study Group, 1990b, p. 2475).
TABLE K-14 Sample Size for the Cases and Controls in the Selected Cancers Study
|
|
Controls |
Cases |
|||||
|
NonHodgkin’s Disease |
Soft-Tissue and Other Sarcomas |
Hodgkin’s Disease |
Nasal Cancer |
Nasopharyngeal Cancer |
Liver Cancer |
||
|
Controls Selected or Cases Identified |
2299 |
2354 |
612 |
2354 |
89 |
0131 |
310 |
|
Interviewed |
1910 |
2073 |
521 |
2073 |
80 |
115 |
263 |
|
Specimen Obtained |
N/Aa |
2004 |
511 |
2004 |
78 |
113 |
233 |
|
Diagnosis Confirmed |
N/A |
1511 |
386 |
343 |
70 |
113 |
168 |
|
Excluded from Analysis |
|
|
|
|
|
|
|
|
Military/Vietnam service status unknown |
7 |
5 |
4 |
0 |
0 |
1 |
2 |
|
In/off coasts of Vietnam but not stationed there |
27 |
13 |
8 |
1 |
1 |
1 |
2 |
|
AIDS or related condition |
1 |
290 |
3 |
17 |
3 |
1 |
0 |
Regression models Three models were used for the analysis (Selected Cancers Cooperative Study Group, 1990a,b,c,d) and they are as follows:
-
Model 1 = registry and age in 1968
-
Model 2 = registry, age in 1968, race/ethnicity, educational achievement
-
Model 3 = registry, age in 1968, race/ethnicity, educational achievement, spraying or mixing any herbicide other than in Vietnam, occupational contact with phenoxyherbicide other than in Vietnam, occupational contact with chlorophenols or dioxin other than in Vietnam, medical irradiation, having been raised in the Jewish religion, marital status, cigarette smoking, reported immunodeficiency disease other than AIDS, rheumatoid arthritis, systemic lupus erythematosus, use of immunosuppressive drugs, and use of phenytoin or related compounds, and other relevant potential confounders of Agent Orange exposure
Study Strengths
The strengths of this investigation are that the participation rates were high, only 7.5 percent of controls selected actually reported serving in Vietnam, and the fact that the same study design and control group was used for all six cancers proves against a general selection bias (Selected Cancers Cooperative Study Group, 1990b, p. 2481).
Study Limitations
The limitations of this investigation are that the researchers “could not measure serum TCDD levels in men recently diagnosed to have cancer because of the large quanitity of blood required” and like in any case-control study there is possible bias, residual confounding, and possible misclassification of the exposure or disease (Selected Cancers Cooperative Study Group, 1990b, pp. 2481-2482).
Cases and Controls
Part I: Non-Hodgkin’s lymphoma (NHL) This part of The Selected Cancers Study investigates the association between military service in Vietnam and exposure to phenoxyherbicides and NHL.
Cases and Controls The inclusion criterion for the cases includes
-
had an initial diagnosis of NHL, Hodgkin’s disease, or “lymphoma, not otherwise specified”;
-
men first diagnosed with NHL between December 1, 1984, and November 30, 1988;
-
lived in geographic location areas covered by the population-based cancer registries for five metropolitan areas (Atlanta, GA; Detroit, MI; San Francisco, CA; Seattle, WA; Miami, FL) and three states (Connecticut, Iowa, and Kansas); and
-
born between 1929 and 1953. (Selected Cancers Cooperative Study Group, 1990a, p. 28, 1990b, pp. 2474-2475)
The exclusion criterion includes
-
unknown military or Vietnam service status;
-
been in or off the coast of Vietnam but not stationed there;
-
have AIDS or AIDS-related illness; and
-
not residents of the United States before 1969 and were thus unlikely to have been eligible for U.S. military service in Vietnam. (Selected Cancers Cooperative Study Group, 1990a, p. 28, 1990b, pp. 2474-2475)
The controls were selected based on random digit dialing and frequency-matched to lymphoma cases by geographic areas (registries) and age in 1968, and were the same controls for the other cancers investigated.
Part II: Soft-tissue and other sarcomas This part of the Selected Cancers Study investigates the association between military service in Vietnam and exposure to phenoxyherbicides and softtissue and other sarcomas.
Cases and controls The inclusion criterion for the cases includes
-
men first diagnosed with sarcoma between December 1, 1984, and November 30, 1988;
-
lived in geographic location areas covered by the population-based cancer registries for 5 metropolitan areas (Atlanta, GA; Detroit, MI; San Francisco, CA; Seattle, WA; Miami, FL) and three states (Connecticut, Iowa, and Kansas); and
-
born between 1929 and 1953. (Selected Cancers Cooperative Study Group, 1990a, p. 42, 1990c, p. 2486)
The exclusion criterion includes
-
diagnosis of Kaposi’s sarcoma or mesothelioma;
-
unknown military or Vietnam service status;
-
been in or off the coast of Vietnam but not stationed there;
-
had AIDS or AIDS-related illness;
-
not residents of the United States before 1969 and were thus, unlikely to have been eligible for U.S. military service in Vietnam; and
-
reported a history of von Recklinghausen’s neurofibromatosis or a possible postirradiation osteosarcoma. (Selected Cancers Cooperative Study Group, 1990a, p. 42, 1990c, p. 2486)
The controls were selected based on random digit dialing and frequency-matched to lymphoma cases by geographic areas (registries) and age in 1968, and were the same controls for the other cancers investigated.
Part III: Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, and primary liver cancer This part of the Selected Cancers Study investigates the association between military service in Vietnam and exposure to phenoxyherbicides and the following cancers: Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, and primary liver cancer.
Cases and controls The inclusion criterion for the cases includes
-
men first diagnosed with Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, or liver cancer between December 1, 1984, and November 30, 1988;
-
lived in geographic location areas covered by the population-based cancer registries for 5 metropolitan areas (Atlanta, GA; Detroit, MI; San Francisco, CA; Seattle, WA; Miami, FL) and three states (Connecticut, Iowa, and Kansas); and
-
born between 1929 and 1953. (Selected Cancers Cooperative Study Group, 1990a, pp. 53, 63, 70, 76-77, 1990d, pp. 2496-2497)
The exclusion criterion includes
-
unknown military or Vietnam service status;
-
been in or off the coast of Vietnam but not stationed there;
-
had AIDS or AIDS-related illness;
-
not residents of the United States before 1969 and were thus, unlikely to have been eligible for U.S. military service in Vietnam; and
-
reported a history of von Recklinghausen’s neurofibromatosis or a possible postirradiation osteosarcoma. (Selected Cancers Cooperative Study Group, 1990a, pp. 53, 63, 70, 76-77, 1990d, pp. 2496-2497)
The controls were selected based on random digit dialing and frequency-matched to lymphoma cases by geographic areas (registries) and age in 1968, and were the same controls for the other cancers investigated.
Results
Part I: Non-Hodgkin’s lymphoma (NHL)
Demographics Compared to the controls, NHL cases were distributed differently among the 8 registries, were significantly older, had significantly less formal education, smoked more cigarettes, were more likely to be never married, had systemic lupus erythematosus, took more
immunosuppressive drugs following an organ transplant and intravenous drugs not prescribed by a physician (p <0.05) (Selected Cancers Cooperative Study Group, 1990a, pp. 29-30, 1990b).
There were no significant differences between the cases and controls with respect to being stationed in or off the coast of Vietnam, racial/ethnic group, sprayed or mixed any herbicide on a farm or ranch, sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or forestry work, occupational exposure to phenoxyherbicides, occupational exposure to chlorophenols, raised in the Jewish religion, exposure to medical radiation ≥5 years before the date of diagnosis, diagnosed with rheumatoid arthritis, had an immune disease other than AIDS ≥3 years before the data of diagnosis, had malaria, took medication to treat or prevention malaria, or took phenytoin or related compounds for epilepsy of seizures (Selected Cancers Cooperative Study Group, 1990b).
Part II: Soft-tissue and other sarcomas
Demographics Compared to controls, cases were distributed differently among the 8 registries and were significantly less likely to be white non-Hispanic, more likely to have occupational exposure to chlorophenols and more likely to work in a meat packing or processing plant (p <0.05) (Selected Cancers Cooperative Study Group, 1990a, p. 42, 1990c).
There were no significant differences between the cases and controls with respect to age in 1968, being stationed in or off the coast of Vietnam, highest level of education completed, regular smoking of cigarettes, sprayed or mixed any herbicide on a farm or ranch, sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or forestry work, occupational exposure to phenoxyherbicides, had an immune disease other than AIDS ≥3 years before date of diagnosis, took drugs to suppress the immune system, had Gardner’s syndrome, or took clofibrate or a related compound (Selected Cancers Cooperative Study Group, 1990c).
Part III: Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, and primary liver cancer
Demographics Compared to controls, cases of Hodgkin’s disease were significantly younger, had less formal education, and were more likely to have reported ever having smoked cigarettes regularly (p <0.05). However, there were no significant differences between the cases of Hodgkin’s disease and the controls with respect to the distribution within the 8 registries, being stationed in Vietnam or off the coast of Vietnam, race/ethnicity, reported having sprayed or mixed any herbicide on a farm or ranch, reported having sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or forestry work, reported occupational exposure to phenoxyherbicides, reported occupational exposure to chlorophenols, raised in the Jewish religion, number of siblings lived with while growing up, raised in an urban setting, exposure to medical radiation ≥5 years before the date of diagnosis, had chemotherapy ≥5 years before the date of diagnosis, had mononucleosis, had a tonsillectomy, or had an appendectomy (Selected Cancers Cooperative Study Group, 1990a, p. 54, 1990d).
Compared to controls, cases of nasal cancer were significantly older, had less formal education, and were more likely to have reported ever having smoked cigarettes regularly (p <0.05). However, there were no significant differences between the cases of nasal cancer with respect to the distribution within the 8 registries, being stationed in Vietnam or off the coast of Vietnam, race/ethnicity, reported having sprayed or mixed any herbicide on a farm or ranch, reported having sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or
forestry work, reported occupational exposure to phenoxyherbicides, reported occupational exposure to chlorophenols, working in a pulp, saw or planning mill, worked around wood dust, worked with or around plywood, worked in metal planting, working with or around nickel, worked with or around chromium, or worked with wood as a hobby (Selected Cancers Cooperative Study Group, 1990a, p. 64, 1990d).
Compared to controls, cases of nasopharyngeal cancer were significantly older, were less likely to be white non-Hispanic, had less formal education, were more likely to have reported ever having smoked cigarettes regularly, and more likely to have reported occupational exposure to chlorophenols (p <0.05). However, there were no significant differences between the cases of nasopharyngeal cancer with respect to the distribution within the 8 registries, being stationed in Vietnam or off the coast of Vietnam, reported having sprayed or mixed any herbicide on a farm or ranch, reported having sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or forestry work, reported occupational exposure to phenoxyherbicides, nasopharyngeal cancer in blood relatives, or had an infectious mononucleosis ≥5 years before the date of diagnosis (Selected Cancers Cooperative Study Group, 1990a, p. 71, 1990d).
Compared to controls, cases of liver cancer were distributed within the 8 registries differently and were significantly older, less likely to be white non-Hispanic, have less formal education, more likely to have reported ever having smoked cigarettes regularly, less likely to have reported having sprayed or mixed any herbicide on a farm or ranch, less likely to have occupational exposure to phenoxyherbicides, more likely to have had hepatitis ≥3 years before the date of diagnosis, more likely to had had cirrhosis ≥3 years before the date of diagnosis, and less likely to have worked with chemical solvents (p <0.05). However, there were no significant differences between the cases of liver cancer and the controls with respect to being stationed in Vietnam or off the coast of Vietnam, reported having sprayed or mixed any herbicide for right-of-way maintenance, lawn care, or forestry work, reported occupational exposure to chlorophenols, reported ever drinking alcohol regularly, taking androgenic steroids, or working in a dry-cleaning plant (Selected Cancers Cooperative Study Group, 1990a, p. 77, 1990d).
All investigations (Part I, II, III)
Association between military service in Vietnam and cancer There was a significant association between military service in Vietnam and NHL in the Selected Cancers Study based on Model 1, Model 2, and Model 3 (see above for covariate in each model) (Table K-15). However, there were no significant associations found between military service in Vietnam and soft-tissue and other sarcomas, Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, or liver cancer (see Tables K-15, K-16, K-17, and K-18 for the results for various associations) (Selected Cancers Cooperative Study Group, 1990a,b,c,d).
Histological Classification There was no significant differences between men with NHL stationed in or off the coast of Vietnam and those not stationed in or off the coast of Vietnam with regards to histological classification of the malignant neoplasms (i.e., low grade, intermediate grade, high grade [p = 0.73]) (Selected Cancers Cooperative Study Group, 1990b, p. 2478).
There were no significant differences between men with soft-tissue and other sarcomas stationed in or off the coast of Vietnam and those not stationed in or off the coast of Vietnam with regards to histological classification of the malignant neoplasms (i.e., fibromatous,
TABLE K-15 Association Between Military Service in Vietnam and Cancer
TABLE K-16 Risk of Cancer Among Vietnam Veterans Compared to the Risk Among Four Unexposed Referent Groups
TABLE K-17 Association Between Branch of Military Service and Cancera for Non-Vietnam and Vietnam Veterans
TABLE K-18 Association Between Self-Reported Agent Orange Contact and Cancera Among Those Who Reported the Exposure and Served in Vietnam Compared to Those Who Did Not Report the Exposure but Who Served in Vietnam
TABLE K-19 Association Between Selected Characteristics of Military Service in Vietnam and Cancera
|
Characteristics |
Non-Hodgkin’s Disease OR (95% CI) |
Soft-Tissue and Other Sarcomas OR (95% CI) |
Hodgkin’s Disease OR (95% CI) |
|
Military service in Vietnam |
1.47 (1.09-1.97) |
1.00 (0.63-1.58) |
1.14 (0.71-1.83) |
|
Duration of service in Vietnam (years) |
|
|
|
|
<1 |
1.05 (0.70-1.57) |
0.77 (0.41-1.47) |
0.86 (0.45-1.65) |
|
1-1.4 |
1.98 (1.00-3.94) |
1.28 (0.45-3.66) |
2.43 (0.98-5.99) |
|
1.5-1.9 |
2.99 (1.41-6.31) |
0.92 (0.20-4.26) |
1.14 (0.30-4.37) |
|
≥2 |
1.54 (0.79-3.01) |
1.24 (0.44-3.45) |
1.11 (0.36-3.45) |
|
|
p for trend = 0.06 |
p for trend = 0.80 |
p for trend = 0.33 |
|
Calendar years stationed in Vietnam |
|
|
|
|
Before 1966 |
1.38 (0.54-3.55) |
0.46 (0.05-3.93) |
0.41 (0.05-3.44) |
|
1966-1969 |
1.41 (1.01-1.98) |
0.95 (0.56-1.62) |
1.11 (0.64-1.93) |
|
After 1969 |
1.64 (0.79-3.39) |
1.30 (0.45-3.69) |
1.63 (0.66-4.02) |
|
|
p for trend = 0.93 |
p for trend = 0.66 |
p for trend = 0.42 |
|
Age at beginning of first tour in Vietnam (years) |
|
|
|
|
<21 |
1.73 (1.11-2.70) |
0.97 (0.47-2.01) |
1.15 (0.61-2.18) |
|
21-25 |
1.20 (0.74-1.94) |
1.34 (0.68-2.66) |
1.06 (0.49-2.29) |
|
≥26 |
1.45 (0.81-2.60) |
0.44 (0.13-1.52) |
1.31 (0.42-4.10) |
|
|
p for trend = 0.52 |
p for trend = 0.26 |
p for trend = 0.95 |
|
Rank at end of last tour in Vietnam |
|
|
|
|
E1-E3 |
1.29 (0.61-2.72) |
0.67 (0.19-2.35) |
1.07 (0.37-3.04) |
|
E4-E9 |
1.44 (1.02-2.03) |
1.11 (0.65-1.89) |
1.19 (0.70-2.04) |
|
Officer |
1.78 (0.80-3.96) |
0.69 (0.15-3.22) |
1.33 (0.28-6.26) |
|
|
p for trend = 0.84 |
p for trend = 0.66 |
p for trend = 0.97 |
|
Type of unit in Vietnam |
|
|
|
|
Support |
1.50 (1.02-2.21) |
0.76 (0.37-1.53) |
1.58 (0.90-2.77) |
|
Combat support |
1.18 (0.65-2.15) |
1.03 (0.44-2.41) |
0.50 (0.14-1.76) |
|
Combat |
1.25 (0.63-2.45) |
0.76 (0.25-2.28) |
0.94 (0.34-2.59) |
|
|
p for trend = 0.76 |
p for trend = 0.85 |
p for trend = 0.17 |
|
Corps in Vietnam |
|
|
|
|
I |
2.25 (1.21-4.18) |
1.61 (0.69-3.76) |
1.67 (0.67-4.18) |
|
II |
1.22 (0.66-2.26) |
0.74 (0.25-2.18) |
0.52 (0.15-1.81) |
|
III |
0.89 (0.50-1.58) |
0.50 (0.17-1.44) |
1.25 (0.57-2.75) |
|
IV |
0.90 (0.15-5.41) |
N/A |
0.93 (0.09-9.82) |
|
Blue-water Navy |
2.17 (1.22-3.86) |
0.64 (0.18-2.21) |
1.39 (0.56-3.46) |
|
|
p for trend = 0.11 |
p for trend = 0.33 |
p for trend = 0.59 |
|
Ever in III Corps in Vietnam |
|
|
|
|
No |
1.70 (1.07-2.71) |
1.15 (0.57-2.32) |
1.27 (0.60-2.67) |
|
Yes |
0.96 (0.59-1.57) |
0.67 (0.30-1.54) |
1.12 (0.55-2.27) |
|
Blue-water Navy |
2.18 (1.23-3.88) |
0.63 (0.18-2.20) |
1.42 (0.57-3.52) |
|
|
p for trend = 0.06 |
p for trend = 0.73 |
p for trend = 0.92 |
lipomatous, myomatous, and other soft-tissue sarcomas [p = 0.82]) (Selected Cancers Cooperative Study Group, 1990c, p. 2488).
Conclusions
Part I: Non-Hodgkin’s lymphoma (NHL) “Compared with the other malignant neoplasms under investigation in the Selected Cancer Study, previous studies of Vietnam veterans more strongly support an association with NHL.” “Results of this study strongly suggest that Vietnam veterans have a roughly 50 percent increased risk of developing NHL approximately 15 to 25 years after military service in Vietnam (OR = 1.47, 95% CI 1.09-1.97). The results do not show a similar increased risk among veterans who served in other locations during the Vietnam ear, suggestions that this association is specific to Vietnam service rather than military service in general.” “Although we could not test such hypotheses and we cannot completely rule out the role of chance or unrecognized bias, our results strongly suggest that Vietnam veterans are at increased risk of NHL and that this increased is not due to Agent Orange exposure” (Selected Cancers Cooperative Study Group, 1990b, pp. 2479-2480, 2482).
Part II: Soft-tissue and other sarcomas “The results of this study do not indicate that the risk of sarcoma is increased among men who served in the U.S. military in Vietnam.” “The military service characteristics of men with sarcoma did not suggest that Vietnam veterans who might have been exposed to Agent Orange are at higher risk for the development of sarcoma.” “Our results are in agreement with those of most other studies and suggest that Vietnam veterans are not at increased risk for the development of sarcoma 15 to 25 years after service. We also failed to identify any subgroup of Vietnam veterans at higher risk or any subtype of soft-tissue sarcoma with greater risk for Vietnam veterans” (Selected Cancers Cooperative Study Group, 1990c, pp. 2489, 2491-2492).
Part III: Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, and primary liver cancer “Our results provide no evidence of higher risk of Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, or primary liver cancer among Vietnam veterans.” “Except for Hodgkin’s disease, the malignant neoplasms described in this report have not received extensive attention in other studies of Vietnam veterans.” “Because most of the Vietnam veterans in this study were probably not (or were only minimally) exposed to Agent Orange, the results should not be considered an adequate test of the hypothesis that exposure to Agent Orange of TCDD is
associated with the development of these malignant neoplasms” (Selected Cancers Cooperative Study Group, 1990d, pp. 2503-2504).
Agent Orange Validation Study
Background
The CDC conducted the two studies above (the VES and the Selected Cancer Study) in response to veterans’ concern that their service in Vietnam adversely affected their health. To study Agent Orange more directly, and to “determine if exposure scores based on military records of troop locations and spray locations can identify a large number of men exposed to Agent Orange, as would be needed for a large cohort study,” the CDC also conducted the Agent Orange Validation Study (CDC, 1988, p. 1253; see http://www.cdc.gov/nceh/veterans/default1b.htm).
Agent Orange Validation Study Cohort
The sample size of the study is given in Figure K-2. The Agent Orange Validation Study cohort included Vietnam veterans with the following inclusion criteria:
-
U.S. Army combat battalions
-
Single term of enlistment
-
Minimum or 16 week of active duty time
-
Served 18 months or more in the III Corps military region (includes Saigon) during 1967-1968 (heavy spraying in this year during these years)
-
Military occupational specialty (MOS) other than “duty soldier” or “trainee”
-
Discharged at pay grade E-5 or lower
-
No deceased veterans (CDC, 1988, p. 1250)
The Agent Orange Validation Study cohort included the following non-Vietnam veterans:
-
All who entered the U.S. Army between 1965 and 1971
-
Sample of men interviewed near the end of the Vietnam Experience Study, but were not invited for the medical examination (see description above)
-
Served in the continental United States or Germany
Three hundred and sixty-seven non-Vietnam veterans met the criteria above and were frequency-matched by race and age to the Vietnam veterans originally selected. Two hundred non-Vietnam veterans were invited to participate in both the telephone interview and the medical examination (CDC, 1988, p. 1250).
Demographics
The demographics (mean age, race, region of residence, smoking, alcohol use, mean BMI, and mean total serum lipid level) of the Vietnam veterans were not significantly different than those of the non-Vietnam veterans.
Many more Vietnam veterans self-reported direct herbicide exposure (25 percent) than non-Vietnam veterans (6 percent) and indirect herbicide exposure (71 percent and 6 percent,
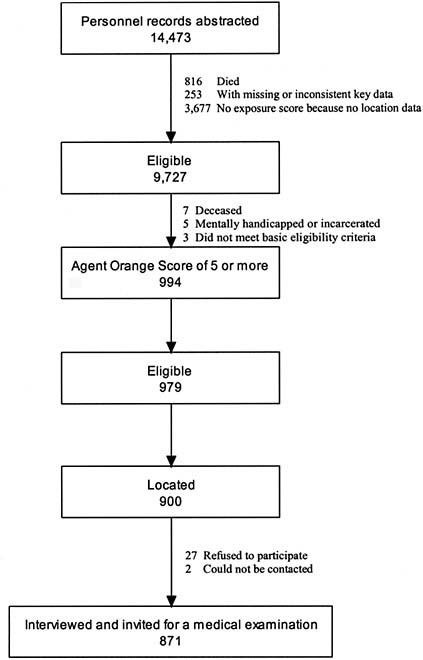
FIGURE K-2 Sample size of the Vietnam veterans in the Agent Orange Validation Study.
SOURCE: CDC, 1988, pp. 1250-1251.
respectively). However, fewer Vietnam veterans self-reported any civilian occupation or home use exposure to herbicides compared to non-Vietnam veterans (20 vs. 33 percent and 33 vs. 44 percent, respectively) (CDC, 1988).
Data from the Agent Orange Validation Study
Potential confounders A priori potential confounders are age, race, body mass index, and self-reported civilian occupational and home exposures to herbicides. Preliminary data analysis showed that smoking history, alcohol consumption, and region of residence are also potential confounders (CDC, 1988, p. 1251).
General methods The methods followed in this study are similar to those of the VES (see above). Briefly, RTI (and Equifax Inc, its subcontractor) located veterans and performed telephone interviews and the medical examinations were performed at the Lovelace Medical Foundation. The data were then abstracted by the U.S. Army and Joint Services Environmental Support Group (CDC, 1988, pp. 1249-1250).
Exposure data Dates and locations of herbicide sprays in South Vietnam for Operation Ranch Hand missions and other sprays were abstracted from military records. Military unit locations were abstracted from military and personnel records. These data were then used to access the herbicide locations of the exposed compared to the unexposed (CDC, 1988, p. 1249).
Exposure score The exposure score was calculated for each day of the study and for each company in 50 of the 65 battalions with abstractable data. The exposure score was calculated by 5 methods (CDC, 1988, p. 1250) as follows:
-
Agent Orange intermediate score
-
“Weighted number of days on which at least one location for a company was within 2 km of a recorded Agent Orange spray within 6 days after the spray” (where the weight is the number of different sprays within 2 km of a company location)
-
Unknown intermediate scores are also calculated since some unknown agents are actually Agent Orange
-
-
Agent Orange slow score
-
“Weighted number of days a company was within 2km of an Agent Orange spray after any earlier spray” (where the weight is the 5-year half life of Agent Orange)
-
Unknown slow scores are also calculated since some unknown agents are actually Agent Orange
-
-
Number of days a company was in one of the five large, heavily sprayed regions
-
Number of days of self-reported direct exposure during military service(spraying herbicide or being present during spraying, handling herbicide, getting herbicide on skin or clothing)
-
Number of days of indirect exposure to herbicides during military service (walking through or clearing vegetation in a previously sprayed area) (from interviews)
Telephone interview Eight-hundred and seventy-one Vietnam veterans completed the interview. Men were asked about exposure to herbicides during military service, civilian work, and at home. Only 5 percent of Vietnam veterans reported spraying herbicides or handling spray equipment during military service (CDC, 1988, pp. 1251, 1254).
There were no significant differences in median current serum TCDD levels in the Vietnam veterans among those with low, medium, and high exposure scores, based on self-reported
indirect exposure (p = 0.08). However, there was a borderline significant difference based on self-reported direct exposure (p = 0.05) (CDC, 1988).
Medical examination The medical examination includes serum samples for TCDD measurements. Each participant fasted overnight; ate a low-fat, low-cholesterol breakfast; and the blood samples were collected 2 hours later. Current TCDD levels of Vietnam veterans are then compared to those of non-Vietnam veterans.
Six-hundred and sixty-five Vietnam veterans and 103 non-Vietnam veterans gave blood samples, and 646 of the samples in Vietnam veterans and 97 samples in non-Vietnam veterans had TCDD results that met laboratory quality control criteria.
Service in Vietnam was not associated with TCDD level after adjusting for age, race, region or residence, body mass index, smoking history, alcohol consumption, and reported civilian herbicide exposure (p = 0.23) (CDC, 1988, p. 1251).
Conclusions
“It seems … that most U.S. Army ground combat troops who did not handle or spray herbicides were not heavily exposed to TCDD in Vietnam” (CDC, 1988, p. 1254). “This study is consistent with other studies and suggests that most U.S. Army ground troops who served in Vietnam were not heavily exposed to TCDD, except perhaps men whose jobs involved handling herbicides” (CDC, 1988).
Strengths of the Agent Orange Validation Study are that there are
-
no indications of selection bias or confounding; and
-
participation rates were modest at 66 percent for Vietnam veterans and 48 percent for non-Vietnam veterans, but they were “unlikely to cause bias.”
Limitations of the Agent Orange Validation Study are that it
-
cannot be generalized to other Vietnam veterans since sample was not random;
-
did not include veterans from the chemical corps, a relatively small group with a high potential for exposure; and
-
military records could not only be used since “records may be unavailable for many of the herbicide applications most likely to have exposed troops” (CDC, 1988, pp. 1253, 1249).
Studies on Gulf War Veterans
For the purposes of this report, short summaries of CDC studies on Gulf War veterans were taken directly from the CDC website (http://www.cdc.gov/nceh/veterans/default2.htm) and provided below.
Health Effects of Exposure to Smoke from Oil Well Fires
Researchers from the Centers for Disease Control and Prevention (CDC) and several other federal agencies conducted surveys of workers in Kuwait City in May 1991, and of firefighters in the oil fields in October 1991. Blood samples were tested for 31 volatile organic compounds (VOCs) and were compared with samples from a group of people
living in the United States. The samples from people living in the United States were collected as part of the Third National Health and Nutrition Examination Survey (NHANES III), a national survey of the health of Americans. The median concentration of VOCs among the firefighters was quite elevated. However, among the non-firefighting personnel, VOC con-centrations were equal to or lower than the levels found among the people living in the United States.
(http://www.cdc.gov/nceh/veterans/default2a.htm)
NCEH also collaborated with the U.S. Department of Defense on a study of 30 members of an Army unit located in Germany. Blood from these military personnel was tested for VOCs at three points in time: before, during, and after their deployment to Kuwait. Tetrachloroethylene, a compound found in degreas-ing agents used to clean equipment, was the only VOC found to be elevated.
(http://www.cdc.gov/nceh/veterans/default2a.htm)
Birth Defects
In 1994, CDC collaborated with the Mississippi Department of Health and the U.S. Department of Veterans Affairs to investigate reports of adverse birth out-comes among members of two Mississippi National Guard Units that served in the Gulf War. This investigation found no increase above expected rates in the total number of birth defects or in the frequency of premature births and low birth-weight babies. The frequency of other health problems, such as respiratory infections, gastroenteritis, and skin diseases among children born to these veterans also did not appear to be elevated.
(http://www.cdc.gov/nceh/veterans/default2b.htm)
(See also Penman et al., 1996)
In 1995, the Naval Health Research Center asked CDC to assist in a study of Goldenhar syndrome. Goldenhar syndrome is characterized by abnormal prenatal development of facial structures. Two clinicians from CDC reviewed birth records of 75,414 infants conceived after the Gulf War and born in military treatment facilities (34,069 infants born to Gulf War veterans and 41,345 born to nondeployed veterans). They identified five infants with Goldenhar syndrome who were born to Gulf War veterans and two infants born to nondeployed veterans. Because of the small number of cases found by the study, the statistical power of the study was low. It was not possible to conclude solely from this study whether there is a higher or lower risk for Goldenhar syndrome among infants born to Gulf War veterans.
(http://www.cdc.gov/nceh/veterans/default2b.htm)
(See also Araneta et al., 1997)
Air Force Study
Various members of a Pennsylvania Air National Guard unit reported illnesses potentially associated with their previous deployment to the Gulf War. in November 1994, the Pennsylvania State Health Department, the U.S. Department of Veteran Affairs, and the U.S. Department of Defense requested that CDC conduct an independent investigation of those illnesses. The investigation, carried out by CDC’s National Center for Infectious Diseases, involved three phases:
-
Interviews with and examination of ill Gulf War veterans from the Air National Guard unit (the index unit) and review of medical records to verify and characterize illness
-
A survey of 3,723 military personnel from four Air Force units, including veterans who were and were not deployed to the Gulf War, to determine the relative prevalence of symptoms and to develop a working case definition of illness
-
A clinical evaluation of 158 Gulf War veterans from the index unit to further clinically characterize illness and to identify risk factors (by examination and laboratory tests)
(http://www.cdc.gov/nceh/veterans/default2c.htm)
A case was defined as a person having one or more chronic symptoms from at least two of three symptom categories (fatigue, mood-cognition, and musculoskeletal). A case was further classified as severe if each case-defining symptom was rated as severe; otherwise, the case was classified as mild-to-moderate. Cases were more likely to demonstrate poorer functioning, depression, and post-traumatic stress disorder. However, no consistent abnormalities were found by physical examination, routine laboratory tests, or tests for several infectious agents endemic to the Middle East. The prevalence of mild-to-moderate and severe cases was 39 percent and 6 percent, respectively, among Gulf War veterans versus 14 percent and 0.7 percent among nondeployed veterans. Fifty-nine (37 percent) clinically evaluated Gulf War veterans did not qualify as cases, 86 (54 percent) were mild-to-moderate cases, and 13 (8 percent) were severe cases. The investigators identified a chronic multisystem condition that was significantly associated with deployment to the Gulf War, but was not associated with specific Gulf War exposures, and that also affected nondeployed personnel.
(http://www.cdc.gov/nceh/veterans/default2c.htm)
(See also CDC, 1995; Fukuda et al., 1998; Nisenbaum et al., 2000)
Health Assessment of Gulf War Veterans from Iowa
In April 1994, Senator Tom Harkin of Iowa requested that CDC conduct a health assessment of Gulf War veterans his state. The study was initiated in December 1994 and was conducted through a cooperative agreement between the Iowa Department of Public Health and CDC’s National Center for Environmental Health. The Iowa Department of Public Health contracted with investigators at the University of Iowa who took the lead in designing and conducting the study. From September 1995 through May 1996, a telephone survey was administered to 1,896 Gulf War veterans and to 1,799 military personnel who were not deployed to the Persian Gulf.
(http://www.cdc.gov/nceh/veterans/default2d.htm)
This was one of the first population-based epidemiologic studies to document that Gulf War veterans are reporting more medical and psychiatric conditions than their military peers.
(http://www.cdc.gov/nceh/veterans/default2d.htm)
The study identified several conditions that need to be studied in more detail, including cognitive dysfunction, depression, chronic fatigue, post-traumatic stress disorder, and respiratory illness (asthma and bronchitis). The conditions identified in this study appear to have measurably affected the functional activity and daily lives of these Gulf War veterans. However, these conditions may not be unique to Gulf War veterans and may be similar to the experience of veterans in other wars. Among Gulf War veterans, minimal
differences were observed between the National Guard or Reserve troops and the regular military personnel.
(http://www.cdc.gov/nceh/veterans/default2d.htm)
(See also Barrett et al., 2002; Black et al., 1999, 2000; Doebbeling et al., 2000, 2002; Iowa Persian Gulf Study Group, 1997; Zwerling et al., 2000)
Iowa Asthma Follow-Up Study
The original Iowa study was extended to collect physical examination data on a subset of the telephone survey participants to validate the self-report of asthma. Data were collected on 32 Gulf War veterans who reported asthma during the telephone survey, 42 Gulf War veterans who reported no illnesses during the tele-phone survey, and 20 non-Gulf War veterans who reported asthma during the telephone survey. The two groups of subjects with reported asthma were similar in symptoms, baseline pulmonary function tests, and bronchial hyperreactivity. The Gulf War veterans who reported asthma had significantly more current symptoms compared with the Gulf War veterans who reported no illness during the telephone survey. They also had comparatively lower baseline spirometry (a measure of how well the lungs exhale) and increased bronchial hyperreactivity. No differences in smoking history were found between the two groups with asthma. However, Gulf War veterans who reported asthma were more likely to be current and past smokers than the Gulf War veterans who did not report illness.
(http://www.cdc.gov/nceh/veterans/default2e.htm)
Cognitive Function and Symptom Patterns in Gulf War Veterans
In November 1997, CDC funded a study by the Boston University School of Public Health to examine potential reasons for the memory and thinking problems reported by Gulf War veterans. in one component of this study, functional magnetic resonance imaging (fMRI) was used to examine possible differences in brain activation patterns within specific areas of the brain. Gulf War veterans and their nondeployed peers with differing levels of symptoms were compared. in another component of this study, Danish armed forces personnel were tested to determine whether they are experiencing the same types of memory and thinking problems reported by U.S. troops who participated in the Gulf War. The Danish troops were also asked about any symptoms that they may be experiencing. Both Danish troops who participated in the Gulf War and troops who were not deployed to the Gulf War were tested. The results will be compared with results from a group of U.S. Gulf War veterans that the Boston University School of Public Health and the Boston VA Medical Center have been following since they returned from the Gulf War. Findings have been published regarding the neuropsychological functioning of the Danish Gulf War troops. No significant differences in neuropsychological test performances were found between the Gulf War-deployed and non-Gulf War-deployed groups. Danish troops deployed to the Gulf War reported significantly more mood complaints (i.e., fatigue and confusion) than their nondeployed counterparts. Publications are still pending for the fMRI component of this study.
(http://www.cdc.gov/nceh/veterans/default2f.htm)
(See also Proctor et al., 2003)
Defining Gulf War Illness
In November 1997, CDC funded a study to characterize and compare different approaches for defining the medically unexplained illnesses of Gulf War veterans. This study by the University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School compared the symptoms of two groups of Gulf War veterans at two points in time. The study subjects included Gulf War veterans from the Department of Veterans Affairs’ Gulf War Registry who had participated in a previous study conducted by the New Jersey researchers, and veterans who had participated in the CDC Air Force study. Data-driven case definitions for illness previously derived from these two groups of Gulf War veterans were compared with standard or existing case definitions for unexplained multi-symptom illnesses (such as chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivity) to determine which definition best characterized Gulf War veterans’ unexplained illnesses. The study also tried to determine how well the derived and existing case definitions could be generalized in a new random sample of deployed and nondeployed Gulf War era veterans and active duty soldiers. The investigators are preparing manuscripts for publication which are expected by the end of 2005.
(http://www.cdc.gov/nceh/veterans/default2g.htm)
Assessing the Potential Health Impact of the Gulf War on Saudi Arabia National Guard Members
This study, initiated in 1999, involved a collaborative effort of health researchers from the United States (U.S. Department of Defense and CDC) and Saudi Arabia. The team examined hospitalization data for 15,612 Saudi Arabia National Guard (SANG) troops. The goal of this study was to compare hospitalization rates and health outcomes among a group of SANG soldiers who were stationed in a combat area in January 1991 (Al Khafji) with soldiers who were stationed in a non-combat area (Riyadh). The investigators identified 148 SANG soldiers who had at least one hospitalization between 1991 and 1999. The adjusted rate of hospitalization was higher in the combat-exposed group (risk ratio = 1.80, 95% confidence interval = 1.25-2.59). No unusual patterns of diagnoses were found. Because the overall number of hospitalizations was low, the absolute difference in risk was found to be very small.
(http://www.cdc.gov/nceh/veterans/default2h.htm)
(See also Gackstetter et al., 2005; Hooper et al., 2005)
Epidemiologic Study of the Occurrence of Amyotrophic Lateral Sclerosis (ALS) Among Gulf War Veterans
In June 1999, the Department of Veterans Affairs and U.S. Department of Defense requested that CDC assist in a study of amyotrophic lateral sclerosis (ALS) among Gulf War veterans. ALS is a fatal neurodegenerative disease that destroys the brain and spinal cord nerve cells that control muscle movement. As the brain and spinal cord nerve cells die, muscles weaken and shrink, and rapid severe paralysis occurs. Neither a cause nor a cure for ALS is known at this time. This investigation of ALS was initiated to determine if there is a higher than expected incidence of ALS among veterans of the 1991 Gulf War and to examine possible risk factors for the disease. CDC’s Environmental Health Laboratory conducted laboratory analyses of blood and urine specimens to look for signs of exposure to heavy metals. Initial results found military personnel who were deployed to the Gulf region during the 1991 Gulf War experienced a greater post-war risk of ALS
than those who were not deployed to the Gulf. Among approximately 2.5 million eligible military personnel, 107 confirmed cases of ALS were identified (an overall occurrence of 0.43 per 100,000 persons per year). Overall, the attributable risk associated with deployment was 18 percent (95% CI = 4.9 to 29.4%). Findings regarding exposure to heavy metals are pending.
(http://www.cdc.gov/nceh/veterans/default2i.htm)
(See also Horner et al., 2003)
Deployment to the Gulf War and Subsequent Development of Cancer
In 2002, George Washington University School of Public Health and Health Services began a study to determine if cancer patterns among veterans of the 1991 Gulf War veterans differ from the patterns found among Gulf War era veterans not deployed to the Persian Gulf. CDC and the Association of Schools of Public Health funded the study. Initial work by the study investigators using data from the District of Columbia and the New Jersey Cancer Registries found a statistically significant excess of testicular cancer in Gulf War deployed veterans compared to non-Gulf War veterans. The current study is focusing on extending the analysis to include cancer data from additional states. These states include Texas, California, Florida, New York, Maryland, and Illinois. This study is expected to continue through July 2005.
(http://www.cdc.gov/nceh/veterans/default2j.htm)
(See also Levine et al., 2005)
Gulf War Research Planning Conference
In early 1999, CDC helped sponsor The Health Impact of Chemical Exposures During the Gulf War: A Research Planning Conference. The U.S. Department of Health and Human Services’ Office of Public Health and Science, the National Institutes of Health, and the Agency for Toxic Substances and Disease Registry cosponsored the conference with CDC. The intent was to obtain broad public input into the development of a multiyear research plan for investigating the relationship between chemical exposures during the Gulf War and illnesses affecting Gulf War veterans. Concurrent workgroups developed research recommendations in the following areas:
-
Pathophysiology/etiology of illnesses among Gulf War veterans
-
The most appropriate methods for assessing and diagnosing the health effects of chemical exposures
-
The most appropriate treatment approaches
-
Ways to prevent similar illnesses in future military deployments
(http://www.cdc.gov/nceh/veterans/default2k.htm)
A final report summarizing conference recommendations was released in March 2000 and is accessible at http://www.cdc.gov/nceh/publications/gulfwar/report.pdf. The background document prepared for the conference that reviews Gulf War-related research conducted before 1999 is accessible at http://www.cdc.gov/nceh/publications/gulfwar/bdgw65.pdf.
Web Based Central Library (Medsearch)
CDC, the U.S. Department of Defense’s Deployment Health Support Directorate, and the Department of Veterans Affairs collaborated to create a centralized Internet site, known
as Medsearch. Veterans and members of the armed forces can visit the site to find information on Gulf War-related medical research developed by or for government agencies. The idea for the online medical library came from a recommendation at a CDC conference in 1999. The conference participants called for a central location where both veterans and researchers could access the latest research on illnesses among Gulf War veterans. The Internet site developers worked with veterans and researchers to ensure that Medsearch is easy to use. Many of the documents available on Medsearch are written in nontechnical language. Medsearch can be accessed at http://www.gulflink.osd.mil/medsearch.
(http://www.cdc.gov/nceh/veterans/default2l.htm)
References
Araneta, M. R., C. A. Moore, R. S. Olney, L. D. Edmonds, J. A. Karcher, C. McDonough, K. M. Hilippoulos, K. M. Schlangen, and G. C. Gray. 1997. Goldenhar syndrome among infants born in military hospitals to Gulf War veterans. Teratology 56(4):244-251.
Barrett, D. H., B. Doebbeling, M. D. Voelker, C. C. Doebbeling, K. Falter, R. Woolson, and D. A. Schwartz. 2002. Post-traumatic stress disorder and physical health status among military personnel service during the Gulf War period. Psychosomatics 43(3):195-205.
Black, D. W., B. N. Doebbeling, M. D. Voelker, W. R. Clarke, R. F. Woolson, D. H. Barrett, and D. A. Schwartz. 1999. Quality of life and health-services utilization in a population-based sample of military personnel reporting multiple chemical sensitivities. Journal of Occupational and Environmental Medicine 41(10):928-933.
Black, D. W., B. N. Doebbeling, M. D. Voelker, W. R. Clarke, R. F. Woolson, D. H. Barrett, and D. A. Schwartz. 2000. Multiple chemical sensitivity syndrome: Symptom prevalence and risk factors in a military population. Archives of Internal Medicine 160(8):1169-1176.
CDC (Centers for Disease Control and Prevention). Agent Orange Validation Study. http://www.cdc.gov/nceh/veterans/default1b.htm (accessed April 24, 2007).
CDC. Air Force Study. http://www.cdc.gov/nceh/veterans/default2c.htm (accessed April 24, 2007).
CDC. Assessing the potential health impact of the Gulf War on Saudi Arabia National Guard members. http://www.cdc.gov/nceh/veterans/default2h.htm (accessed April 24, 2007).
CDC. Birth defects. http://www.cdc.gov/nceh/veterans/default2b.htm (accessed April 24, 2007).
CDC. Cognitive function and symptom patterns in Gulf War veterans. http://www.cdc.gov/nceh/veterans/default2f.htm (accessed April 24, 2007).
CDC. Defining Gulf War illness. http://www.cdc.gov/nceh/veterans/default2g.htm (accessed April 24, 2007).
CDC. Deployment to the Gulf War and subsequent development of cancer. http://www.cdc.gov/nceh/veterans/default2j.htm (accessed April 24, 2007).
CDC. Epidemiologic study of the occurrence of amyotrophic lateral sclerosis (ALS) among Gulf War veterans. http://www.cdc.gov/nceh/veterans/default2i.htm (accessed April 24, 2007).
CDC. Gulf War Research Planning Conference. http://www.cdc.gov/nceh/veterans/default2k.htm (accessed April 24, 2007).
CDC. Gulf War studies. http://www.cdc.gov/nceh/veterans/default2.htm (accessed April 24, 2007).
CDC. Health assessment of Gulf War veterans from Iowa. http://www.cdc.gov/nceh/veterans/default2d.htm (accessed April 24, 2007).
CDC. Health effects of exposures to smoke from oil well fires. http://www.cdc.gov/nceh/veterans/default2a.htm (accessed April 24, 2007).
CDC. Iowa Asthma Follow-Up Study. http://www.cdc.gov/nceh/veterans/default2e.htm (accessed April 24, 2007).
CDC. Postservice mortality among Vietnam veterans. http://www.cdc.gov/nceh/veterans/default1a.htm (accessed April 24, 2007).
CDC. Selected cancer study. http://www.cdc.gov/nceh/veterans/default1d.htm (accessed April 24, 2007).
CDC. Web-based central library (Medsearch). http://www.cdc.gov/nceh/veterans/default2l.htm (accessed April 24, 2007).
CDC. 1988. Serum 2,3,7,8-tetrachlorodibenzo-p-dioxin levels in U.S. Army Vietnam-era veterans. Journal of the American Medical Association 260(9):1249-1254.
CDC. 1995. Unexplained illness among Persian Gulf War veterans in an Air National Guard unit: August 1990-March 1995. Morbidity and Mortality Weekly Report 44(23):443-447.
CDC VES (Centers for Disease Control Vietnam Experience Study). 1987a. Current trends postservice mortality among Vietnam veterans. Morbidity and Mortality Weekly Report 36(5):61-64. http://www.cdc.gov/mmwr/preview/mmwrhtml/00000865.htm (accessed April 16, 2007).
CDC VES. 1987b. Post service mortality among Vietnam veterans. Journal of the American Medical Association 257(6):790-795.
CDC VES. 1988a. Health status of Vietnam veterans: I. Psychosocial characteristics. Journal of the American Medical Association 259(18):2701-2707.
CDC VES. 1988b. Health status of Vietnam veterans: II. Physical health. Journal of the American Medical Association 259(18):2708-2714.
CDC VES. 1988c. Health status of Vietnam veterans: III. Reproductive outcomes and child health. Journal of the American Medical Association 259(18):2715-2719.
CDC VES. 1989a. Health status of Vietnam veterans. Synopsis. Vol. 1. Atlanta, GA: CDC. http://www.cdc.gov/nceh/veterans/default1c.htm (accessed April 16, 2007).
CDC VES. 1989b. Health status of Vietnam veterans. Telephone interview. Vol. 2. Atlanta, GA: CDC. http://www.cdc.gov/nceh/veterans/default1c.htm (accessed April 16, 2007).
CDC VES. 1989c. Health status of Vietnam veterans. Medical examination. Vol. 3. Atlanta, GA: CDC. http://www.cdc.gov/nceh/veterans/default1c.htm (accessed April 16, 2007).
CDC VES. 1989d. Health status of Vietnam veterans. Reproductive outcomes and child health. Vol. 5. Atlanta, GA: Centers for Disease Control. http://www.cdc.gov/nceh/veterans/default1c.htm (accessed April 16, 2007).
Doebbeling, B. N., W. R. Clarke, D. Watson, J. C. Torner, R. F. Woolson, M. D. Voelker, D. H. Barrett, and D. A. Schwartz. 2000. Is there a Persian Gulf War syndrome? Evidence from a large population-based survey of veterans and nondeployed controls. American Journal of Medicine 108(9):695-704.
Doebbeling, B. N., M. F. Jones, D. B. Hall, W. R. Clarke, R. F. Woolson, J. C. Torner, L. F. Burmeister, T. Snyders-Crumley, D. H. Barrett, K. H. Falter, J. A. Merchant, S. Nusser, D. Anderson, and D. A. Schwartz. 2002. Methodologic issues in a population-based health survey of Gulf War veterans. Journal of Clinical Epidemiology 55(5):477-487.
Fukuda, K., R. Nisenbaum, G. Stewart, W. W. Thompson, L. Robin, R. M. Washko, D. L. Noah, D. H. Barrett, B. Randall, B. L. Herwaldt, A. C. Mawle, and W. C. Reeves. 1998. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. Journal of the American Medical Association 280(11):981-988.
Gackstetter, D. G., T. I. Hooper, M. S. Al Qahtani, T. C. Smith, Z. A. Memish, K. M. Schlangen, D. F. Cruess, D. H. Barrett, M. A. K. Ryan, and G. C. Gray. 2005. Assessing the potential health impact of the 1991 Gulf War on Saudi Arabian National Guard soldiers. International Journal of Epidemiology 34(4):801-808.
Hooper, T. I., T. C. Smith, G. C. Gray, M. S. Al Qahtani, Z. A. Memish, D. H. Barrett, K. M. Schlangen, D. F. Cruess, M. A. K. Ryan, and G. D. Gackstetter. 2005. Saudi-United States collaboration in health research: An approach for success. American Journal of Infection Control 33(3):192-196.
Horner, R. D., K. G. Kamins, J. R. Feussner, S. C. Grambow, J. Hoff-Lindquist, Y. Harati, H. Mitsumoto, R. Pascuzzi, P. S. Spencer, R. Tim, D. Howard, T. C. Smith, M. A. K. Ryan, C. J. Coffman, and E. J. Kasarskis. 2003. Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology 61(6):742-749.
Iowa Persian Gulf Study Group. 1997. Self-reported illness and health status among Gulf War veterans: A population-based study. Journal of the American Medical Association 277(3):238-245.
Levine, P. H., H. A. Young, S. J. Simmens, D. Rentz, V. E. Kofie, C. M. Mahan, and H. K. Kang. 2005. Is testicular cancer related to Gulf War deployment? Evidence from a population-based study of Gulf War era veterans and cancer registries. Military Medicine 170(2):149-153.
Nisenbaum, R., D. H. Barrett, M. Reyes, and W. C. Reeves. 2000. Deployment stressors and a chronic multisymptom illness among Gulf War veterans. Journal of Nervous and Mental Disorders 188(5):259-266.
Penman, A., R. S. Tarver, and M. M. Currier. 1996. No evidence of increase in birth defects and health problems among children born to Persian Gulf War Veterans in Mississippi. Military Medicine 161(1):1-6.
Proctor, S. P., R. F. White, T. Heeren, F. Debes, B. Gloerfelt-Tarp, M. Appleyard, T. Ishoy, B. Guldager, P. Suadicani, F. Gyntelberg, and D. Ozonoff. 2003. Neuropsychological functioning in Danish Gulf War veterans. Journal of Psychopathology and Behavioral Assessment 25(2):85-94.
Selected Cancers Cooperative Study Group. 1990a. The association of selected cancers with service in the U.S. military in Vietnam. Final Report. Altanta, GA: CDC. http://www.cdc.gov/nceh/veterans/default1d.htm (accessed April 19, 2007).
Selected Cancers Cooperative Study Group. 1990b. The association of selected cancers with service in the U.S. military in Vietnam: I. Non-Hodgkin’s lymphoma. Archives of Internal Medicine 150(12):2473-2483.
Selected Cancers Cooperative Study Group. 1990c. The association of selected cancers with service in the U.S. military in Vietnam: II. Soft-tissue and other sarcomas. Archives of Internal Medicine 150(12): 2485-2492.
Selected Cancers Cooperative Study Group. 1990d. The association of selected cancers with service in the U.S. military in Vietnam: III. Hodgkin’s disease, nasal cancer, nasopharyngeal cancer, and primary liver cancer. Archives of Internal Medicine 150(12):2495-2505.
Zwerling, C., J. C. Torner, W. R. Clarke, M. D. Voelker, B. N. Doebbeling, D. H. Barrett, J. A. Merchant, R. F. Woolson, and D. A. Schwartz. 2000. Self-reported postwar injuries among Gulf War veterans. Public Health Reports 115(4):346-349.
APPENDIX K-4
SELECTED STUDIES ON VETERANS FROM THE CRISP DATABASE4
(Table follows.)
|
4 |
Not intended to be a comprehensive list. See http://crisp.cit.nih.gov for additional projects. |
|
Primary Investigator |
Project Name |
Grant Number |
Start Date |
End Date |
|
Beebe, G |
Hepatitis B Virus and Liver Cancer in Army Veterans of WW II |
1Z01CP005329-11 |
|
|
|
Doebbeling, Bradley |
Illness Among Persian Gulf War Veterans: Case Validation |
5M01RR000059-411069 |
|
|
|
Dohrenwend, Bruce |
Social Status and PTSD in U.S. Vietnam Veterans |
5R01MH059309-03 |
9/28/1999 |
12/1/2003 |
|
Giardina, Charles |
Mustard Gas Exposure and Carcinogenesis of the Lung |
1R21ES013775-01 |
|
|
|
Golier, Julia |
Psychobiologic Alterations in Persian Gulf War VeteransWith/Without PTSD |
5M01RR000071-400470 |
6/22/1905 |
|
|
Haley, Robert |
Pathophysiologic Studies of Ill Gulf War Veterans and Controls |
5M01RR000633-310606 |
6/21/1905 |
|
|
Hrubec, Zdenek |
Resource Support of Medical Studies on Veteran Twins |
5R01MH018820-04 |
4/1/1970 |
3/31/1974 |
|
Jablon, Seymour |
Epidemiologic Studies in Etiology of Cancer in Veterans |
3N01CP04333600174 |
6/28/1974 |
|
|
Jerskey, Beth |
Combat Trauma and Mid-Life Marital Outcomes: A Twin Study |
5F31MH071017-02 |
3/1/2004 |
6/30/2005 |
|
King, Daniel |
PTSD and Its Etiology: A Quintet of Inquiries |
1R01MH049168-01 |
6/1/1992 |
5/31/1995 |
|
Laufer, Robert |
A Study of Veterans: Impact of The Vietnam War |
3R01MH026832-06S1 |
9/1/1980 |
12/31/1984 |
|
Lee, Chulhee |
Exposure to Disease During Growing Ages and War Service |
5P01AG010120-100001 |
|
|
|
Linet, M |
Studies of Radiation Related Cancer |
1Z01CP010102-01 |
|
|
|
McCaffery, Jeanne |
SES, Health Behaviors and CVD Among Vietnam-Era-Twins |
5R01HL072819-02 |
6/1/2004 |
5/31/2007 |
|
Murphy, Ronald |
Combat Exposure, Early Trauma, and Alcohol Problems |
1R03AA010027-01 |
5/1/1994 |
4/30/1996 |
|
Primary Investigator |
Project Name |
Grant Number |
Start Date |
End Date |
|
Norman, James |
Hepatitis “B” Virus and Liver Cancer in Veterans |
5N01CP031021-00783 |
6/30/1983 |
|
|
Page, William |
Cancer in Navy Korean War Microwave (Radar) Workers |
3N01CP040536-00694 |
9/15/1994 |
10/31/1997 |
|
Page, William |
Studies of Cancer in Veteran Twin Registry |
5N01CP015690-00591 |
3/15/1991 |
3/14/1994 |
|
Pitman, Roger |
Twin Study of Biologic Markers for PTSD |
5R01MH054636-09 |
9/30/1995 |
5/31/2007 |
|
Robinette, C |
Studies of Cancer in Veteran Twin Registry |
3N01CP015690-00191 |
3/15/1991 |
|
|
Rose, Kathryn |
Combat Stress and Cardiovascular Risk Among Aging Men |
1R21HL080422-01A1 |
9/31/2006 |
11/30/2007 |
|
Schmidt, Silke |
Genetic Epidemiology of ALS in Veterans |
5R01ES013244-03 |
8/19/2004 |
6/30/2009 |
|
Schwartz, David |
Iowa Persian Gulf Research Project: Follow-Up Study on Asthma |
5M01RR000059-411045 |
12/1/2001 |
11/30/2002 |
|
Scrimshaw, Nevin |
Exposure toDisease During Growing Ages and War Service |
3P01AG010120-08S20001 |
|
|
|
Tanner, Caroline |
Genes, Environment and Parkinson’s Disease: Studies in Four Unique Cohorts |
1U54ES012077-010001 |
8/26/2002 |
7/31/2007 |
|
Vaccarino, L |
Posttraumatic Stress Disorder and Cardiovascular |
5R01AG026255-03 |
|
|
|
Vandenborne, Krista |
Evaluation of Muscle Function in Persian Gulf Veterans |
5M01RR000040-420711 |
12/1/2001 |
11/30/2002 |
|
Vernon, Sally |
A Cancer Study Among Female Veterans in Texas, 1979-2001 |
5R03CA103512-02 |
9/30/2004 |
8/31/2006 |
|
Yehuda, Rachel |
Psychobiological Alterations in Aging Combat Veterans w/PTSD |
5M01RR000071-400427 |
|
|
|
SOURCE: Crisp Database, http://crisp.cit.nih.gov/. |
||||