3
MDR TB Transmission, HIV Coinfection, and Transmission Control
The spread of drug-resistant TB has been accelerated by several factors, including ineffective and interrupted treatment, coinfection with HIV, and inadequate infection control. Evidence suggests that there are two pathways through which the prevalence of drug-resistant TB increases—acquired resistance, discussed in the preceding chapter, and transmitted resistance, discussed here.
COINFECTION WITH HIV
Friedland expanded on his remarks, summarized in Chapter 2, regarding the progression of the TB epidemic in KwaZulu-Natal, South Africa, and its catastrophic relationship with HIV. The emergence and progression of the HIV/AIDS epidemic have dramatically affected the population in the region. A large percentage of the region’s residents now have compromised immune systems that make them increasingly vulnerable to infection and the progression of disease. The coincidence of TB and HIV has both accelerated drug resistance and contributed to the rapid transmission of HIV. Friedland suggested that the present situation, characterized by recent increases in MDR and XDR TB, illuminates past and current deficiencies in existing knowledge of TB, as well as the practices, programs, and strategies used to combat the disease. Areas with high TB and HIV rates threaten the success of both the Stop TB Partnership and historic antiretroviral rollout programs.
Compounding the problem are the limitations of infection control facilities and practices in health care institutions. Health care institutions
routinely house patients who are HIV positive with patients who have drug-resistant TB, creating opportunities for nosocomial transmission and perhaps tangentially increasing community transmission. Recent efforts are aimed at deinstitutionalizing and decentralizing care by focusing on community-based treatment in people’s homes and huts, thereby reducing the probability of nosocomial transmission.
TREATMENT
Murray discussed the inadequacies of current TB treatment strategies and how these inadequacies lead to increases in drug resistance and transmission. She cited estimates that of the half million MDR TB cases and 40,000 XDR TB cases newly diagnosed in 2006, only a small proportion are being treated through either GLC-approved or non-GLC-approved treatment programs (see Figure 3-1). Even among the small proportion of patients that are being treated, many are not receiving drugs that actually address their drug resistance profile, and therefore their treatment is ineffective. A recent review of treatment outcomes for MDR TB cases across 23 studies in 15 different countries (including high-, moderate-, and low-income countries) found that long-term cure rates ranged between 33 and 83 percent. It was found that MDR TB patients coinfected with HIV had lower cure rates than patients with MDR TB alone. Use of fluoroquinolone and surgical resection were associated with better cure rates. Programs that systematically included fluoroquinolone in treatment protocols tended to have cure rates ranging from 60 to 85 percent (Chan and Iseman, 2008). Murray presented pooled data from Partners In Health in Peru and Russia showing that while no particular second-line drug is absolutely necessary for success, the use of injectables (i.e., kanamycin, capreomycin, or amikacin) and fluoroquinolone is associated with better cure rates.
Murray also presented XDR TB outcome data published over the past year. These data showed that the failure rate for treatment of XDR TB ranges from about 35 percent to about 80percent, mainly in non-HIV-prevalent populations. Murray hypothesized that the failure rates in Africa and in parts of Eastern Europe where HIV is more prevalent would likely be even higher. She noted that XDR TB cases, which are not treatable with fluoroquinolone, usually are not treatable unless a second injectable drug is available. Further, although cycloserine and ethionamide may have some impact, there is a strong potential for treatment to fail if the XDR TB strains are resistant to capreomycin, kanamycin, or amikacin.
The implications of the data presented by Murray for the epidemic potential of MDR and XDR TB are troubling. Without a vaccine and without early, accurate case detection and proper treatment, the MDR/XDR TB epidemic will be driven by transmission.
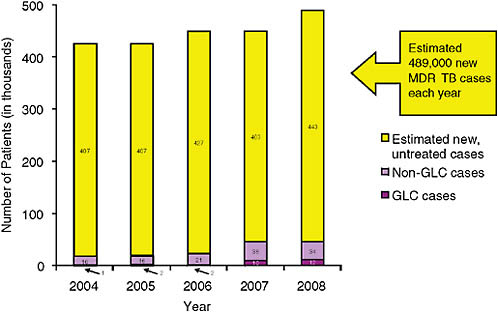
FIGURE 3-1 MDR TB burden and patients in treatment.
NOTES: The bars represent the number of new MDR TB cases in each year. Data for 2007 and 2008 are WHO estimates. The lavender portions indicate the number of patients treated in non-GLC-approved projects; the purple portions indicate the number of patients treated in GLC-approved projects; and the yellow portions represent patients receiving no treatment. GLC = Green Light Committee.
SOURCE: Zintl, 2008 (based on unpublished data from GLC Secretariat, Geneva 2008).
TRANSMISSION OF XDR TB
Jeffrey Drazen of the New England Journal of Medicine noted that drug-resistant strains of other diseases typically are not as resilient as drug-susceptible strains and therefore tend to die out. By contrast, in the MDR TB epidemic that occurred in New York City in the early 1990s, which affected mainly HIV-infected persons, the strains were readily transmissible. The recent experience in Africa and elsewhere provides further evidence of this phenomenon.
Murray discussed a study from the 1950s that exposed animals to laboratory TB strains selected for resistance to isoniazid. The isoniazid-resistant strain was found to be less virulent than susceptible strains in the animals. When the experiment was repeated with clinical strains, however, those strains were observed to be much more heterogeneous in their behavior in animals than were the laboratory strains. The results of these experiments
have been confirmed in recent years by multiple laboratories and are consistent with what is now known about MDR TB drug resistance. It is thought that the setting in which strains are transmitted acts as an “evolutionary” barrier: the less fit mutants are weeded out, and those mutants with greater fitness are selected. It is also likely that compensatory mutations1 take place after an initial drug-resistance mutation. The sequencing of a set of evolved strains is now under way to identify such compensatory mutations.
Edward Nardell of Brigham and Women’s Hospital stated that he and colleagues at the South African Medical Research Council and CDC have been researching the transmission of MDR TB from patients directly to sentinel guinea pigs to replicate and expand upon some of the early research of Richard Riley discussed by Murray. Although Nardell’s group has observed higher rates of transmission than were reported in the past, rates of progression to active disease have been low. Nardell stated that from these studies, it is apparent that although the strains that are transmitted among normal hosts are likely to retain fitness, even attenuated strains likely survive and are transmitted in HIV-infected populations.
Gandhi added that colleagues in Durban have demonstrated that in South Africa over the past 10 years, certain predominant strains have been overrepresented among MDR and XDR TB cases (Pillay and Sturm, 2007). Principal among these are the Beijing strain and the KwaZulu-Natal strain. Until the mid-1990s, the KwaZulu-Natal strain existed in a fully susceptible form, but as drug-resistant forms of this strain emerged, they began and continue to be overrepresented in MDR and XDR TB patients.
Gandhi gave further evidence that XDR TB is being transmitted rather than acquired in Tugela Ferry by expanding on Friedland’s comments regarding the Tugela Ferry epidemic. In 2006, Gandhi’s group recorded the first 53 cases of XDR TB in South Africa. The study received international attention because of two notable factors (Gandhi et al., 2006). First, the XDR TB was highly fatal, with 98 percent of patients dying within a median of just 16 days after sputum collection. (More recent data presented in Chapter 2 indicate that the mortality rate has dropped to 82 percent [Gandhi et al., 2009].) This severe mortality was explained in part by the fact that all the patients were HIV infected (Gandhi et al., 2006). Second, because about half of these patients had never before been treated for TB, and 85 percent had a genetically similar strain, resistance was likely transmitted rather than acquired. The progression of XDR TB from June 2006 to 2007 is depicted in Figure 3-2, which shows facilities within KwaZulu-Natal Province where at least one XDR TB case was described or diagnosed. There were 6 such
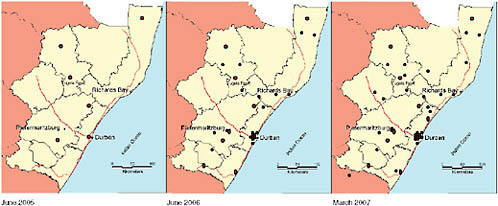
FIGURE 3-2 Facilities in KwaZulu-Natal Province where at least one XDR TB case was described or diagnosed from June 2005 to March 2007.
NOTE: There were 6 such facilities as of June 2005, a figure that had increased to 32 by June 2006 and 42 by March 2007. More than 60 facilities in KwaZulu-Natal have now reported cases of XDR TB.
SOURCE: Moodley et al., 2007.
facilities as of June 2005; by March 2007, that number had increased to 42, and it is now above 60 (Moodley et al., 2007). This situation is not limited to Tugela Ferry or to KwaZulu-Natal Province. In fact, cases of XDR TB have been found throughout South Africa, and prevalence rates have been roughly similar among the various provinces. XDR TB cases have also been reported from all of South Africa’s neighbors.
Gandhi said it is generally thought that selection for drug-resistant strains, usually termed acquired or amplified resistance, occurs in settings where TB treatment is inadequate, patients fail to adhere to proper treatment regimens, or incorrect or non-quality-assured drugs are used for treatment. The other mechanism through which resistance is perpetuated is the direct transmission of drug-resistant strains, called primary or transmitted resistance. Gandhi stated that this latter mechanism has largely been neglected in the development of TB control programs. While acquired or amplified resistance due to inadequate treatment may explain how the very first cases of XDR TB emerged in South Africa and other parts of the world, it is difficult to say that the current magnitude of the epidemic could be attributable to acquired resistance alone. Gandhi reported that at his site in Tugela Ferry, there have been nearly 400 XDR TB cases in the past 3 years (Moll et al., 2007), and it is highly likely that the majority of these cases developed as a result of primary or transmitted resistance. But he hypothesized that even among those who had received prior TB treatment and relapsed (a majority of whom had documentation that their TB had been
cured or that they had completed their treatment course), the vast majority probably represented new infections rather than acquired resistance.
To better understand the role of acquired versus transmitted resistance among relapsed patients with MDR and XDR TB, molecular fingerprinting was used. Seventeen patients were identified for whom both initial susceptible isolates and follow-up MDR or XDR TB isolates were available. The results (shown in Figure 3-3) indicated that all 17 patients who relapsed with MDR or XDR TB had different genotypes in their relapse isolates compared with their initial isolates. Because the initial and relapse isolates differed in genotype, all 17 relapses occurred as a result of new infections and primary transmission, not acquired resistance. Additionally, while there was diversity among the TB strains in the initial isolates, only a few TB strains were seen among the MDR and XDR TB relapses (Andrews et al., 2008). This finding suggests not only that the relapses were due to new infections, but also that common sources of primary transmission are likely. High rates of HIV coinfection and hospitalization probably contributed to the risk for reinfection.
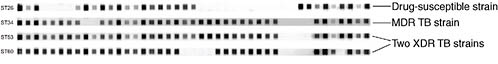
Figure 3-4 shows four different TB strains that were isolated from a single patient. The initial spoligotype pattern at the top is the baseline isolate, which was totally drug susceptible. Seventy days later, a follow-up culture indicated a different TB strain (second row) that was resistant to isoniazid and rifampicin. After second-line therapy was initiated, two additional TB strains were isolated, both of which were XDR TB. Genotyping, however, demonstrated that these two new XDR TB isolates resulted from new infections due to primary transmission, not acquired resistance to second-line therapy.
Gandhi suggested that three important lessons should be learned from these findings:
-
Efforts must focus on creating infection control programs to prevent the further transmission of drug-resistant strains. Currently, most health care and congregate settings worldwide utterly lack infection control facilities.
-
Early diagnosis of MDR and XDR TB cases is critical to facilitate infection control measures. Diagnosis of MDR and XDR TB is currently severely hampered by a lack of laboratory capacity and by the unavailability of a simple rapid diagnostic test that could be used in resource-limited settings (see the discussion in the next chapter).
-
Further studies are needed to better characterize transmission patterns both in hospitals and in communities so that other means of curbing the epidemic can be devised.
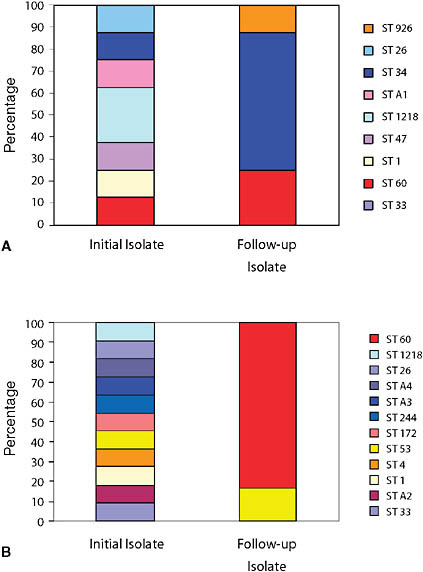
FIGURE 3-3 Genotypes of 17 patients with MDR and XDR TB relapse.
NOTE: Image A shows the genotypes of initial susceptible isolates and the follow-up MDR TB isolates for 7 patients. Image B shows the genotypes of initial susceptible isolates and the follow-up XDR TB isolates for 10 patients. All 17 patients had different genotypes in their relapse isolates compared with their initial isolates. Although there was diversity among the TB strains in the initial isolates, only a few TB strains were seen among the MDR and XDR TB relapses.
SOURCE: Andrews et al., 2008. Copyright 2008 by the Infectious Diseases Society of America. All rights reserved.
PERSPECTIVE FROM RUSSIA
Nardell began his remarks by stressing that because a third of the world’s population is already infected with TB, a static condition, the term “transmission control” is more appropriate than “infection control.” Transmission denotes the process of an organism’s going from one person to another, a dynamic process that needs to be interrupted if the epidemic is to be combated successfully.
Nardell presented his perspective on transmission in Tomsk, Russian Republic, a setting that has different characteristics from those of Africa: the climate in Tomsk is very different from that in Africa, highly effective treatment for MDR TB is available, and HIV infection is not widespread. Despite these differences, however, there is evidence of unrestrained transmission of MDR TB, and its rates are currently rising. To understand why MDR TB case rates were increasing despite the availability of effective treatments, a retrospective study was conducted. The investigators hypothesized that substance abuse was a strong predictor of nonadherence to TB treatment protocols and would therefore be correlated with MDR TB. However, the study results did not support this hypothesis. Instead, hospitalization (either early or later in the course of TB treatment) was correlated with MDR TB. A patient in Tomsk was six times more likely to develop MDR TB if hospitalized for drug-susceptible TB than if not hospitalized (Gelmanova et al., 2007). These results strongly suggest that transmission rather than resistance acquired predominantly by nonadherence is increasingly responsible for the rising MDR TB case rates in Russia and many other places. Nardell stated that the data presented by Nunn showing that the majority of new MDR TB cases occur among previously treated persons do not mean that these cases do not represent transmission and reinfection with a strain that is already drug resistant. Nardell argued that data from both Africa and China support the theory that cases of MDR and XDR TB are increasing because of transmission and reinfection. (Information on the current situation in Shanghai, China, presented by Qian Gao of Shanghai Medical College, is provided in Box 3-1.)
MITIGATING TRANSMISSION
Nardell stated that, given a setting with appropriate resources for transmission control strategies and more effective treatment, it is possible to cure and control the spread of MDR TB. This was convincingly demonstrated during the 1985–1992 resurgence of TB in New York City and Miami. With the infusion of many millions of dollars, MDR TB cases were effectively treated, and institutional spread was sharply decreased through the implementation of effective transmission control measures (this experience is dis-
|
BOX 3-1 Transmission of MDR and XDR TB in Shanghai Each year 1.3 million new cases of TB are diagnosed in China. Based on a nationwide survey conducted in 2000, roughly 18.6 percent of these new cases are drug resistant, and 7.6 percent are MDR (Ministry of Health of the People’s Republic of China, 2000). A more recent survey in Shanghai indicated that about 5.6percent of TB patients had MDR TB; of these, 6.3 percent were XDR TB, and 31.4 percent were considered pre-XDRTB* (Zhao et al., 2009). More than 50 percent of the MDR and XDR TB cases are new, indicating that transmission may be a very important factor. To better understand the cause of drug resistance among treated patients, a prospective study was conducted using genotyping technology. The goal of the study was to determine whether propagation of MDR and XDRTB was through acquired or transmitted resistance. The researchers sought to identify patients having two or more isolates with different drug susceptibility results. From their original patient pool they identified 32 patients that met their criteria. Strains were isolated and genotyped from patients both before and after treatment. Then using MIRU (mycobacterial interspersed repetitive unit) and IS6110 (insertion sequence 6110), the isolates were genotyped. Resistance could be classified as acquired if both isolates from the same patient had identical MIRU or RFLP (restriction fragment length polymorphism) patterns. Among the 32 patients, 84 percent had a pair of isolates with discordant patterns, and 16 percent had a pair of isolates with identical patterns. Thus, the researchers concluded that among treated patients, 84 percent of drug resistance was transmitted and 16 percent acquired. Gao stated that new strategies are needed to block the transmission of MDR and XDRTB.
SOURCE: Gao, 2008. |
cussed in more detail below). However, implementing effective transmission control in resource-limited settings globally presents major challenges:
-
Establishing community-based treatment outside a hospital currently is not feasible in some settings because the tradition and infrastructure for community care do not exist.
-
Transmission control is expensive in many climates. For example, it is expensive to install and maintain ventilation systems in regions where natural ventilation is not sufficient.
-
Technical expertise is often lacking to implement building design and engineering strategies.
-
Health care workers and patients are stigmatized by wearing respirators, and therefore may neglect to do so.
-
In many high-burden countries, health care workers are already infected and fail to see the rationale for transmission control practices.
-
Many TB programs and hospitals do not fully appreciate the magnitude of the MDR TB problem or lack the will (and resources) to address it head-on. For example, some programs were under the impression that directly observed treatment, short course (DOTS)2 alone would prevent the emergence of MDR TB and that MDR TB strains are less virulent than susceptible TB strains.
Nardell commented that, while the need for transmission control appears obvious, as recently as 2006 the current global plan from the Stop TB Partnership,3 a roadmap for global TB control efforts, failed to mention it in any detail. Another factor in transmission control is the underappreciated importance of undiagnosed and unsuspected cases to the spread of disease. While the current focus of TB transmission control is on known cases, unsuspected cases may be responsible for a high proportion of transmission. A survey conducted in a hospital ward in Peru screened female patients that entered the ward for active cases of TB for an entire year. Of the 250 female patients treated in that ward, 40 (16 percent) were positive for TB by culture, 27 (11percent) were positive by smear, and 8 (3 percent) had MDR TB. Thirteen of the 40 culture-positive patients were unsuspected cases, and 6 (46 percent) of those (i.e., the 13 unsuspected cases) actually had MDR TB, compared with 2 (7 percent) of the 27 suspected cases. Of the 8 patients that had MDR TB, 5 were smear positive, meaning they were highly infective (Willingham et al., 2001).
Congregate settings also have an impact on the propagation of MDR TB. As mentioned earlier, between 1985 and 1992 there was a somewhat focal MDR TB epidemic in the United States. Studies showed that MDR TB was being spread in hospitals, jails, prisons, homeless shelters, and residential AIDS facilities, among other congregate settings where both HIV-positive and -negative persons were exposed. In their retrospective review of how the New York City epidemic was brought under control, Frieden and colleagues (1995) credit more effective case finding and treatment and
|
2 |
DOTS is an internationally recommended strategy for TB control. More information about the program and its five components can be found at http://www.who.int/tb/dots/en/. |
|
3 |
The Stop TB Partnership, established in 2000, consists of almost 1,000 organizations from around the world. The primary goal of this alliance is to eliminate TB as a public health problem. More information about the organization can be found at http://www.stoptb.org/. |
effective institutional transmission control. The recent outbreak of XDR TB in KwaZulu-Natal in the absence of any transmission control interventions is reminiscent of these earlier outbreaks, not only in New York City and Miami, but also in Buenos Aires, Italy, and elsewhere in the world. Based on that experience, epidemic control will require interrupting transmission as well as providing effective treatment. Nardell attributed the extent of the epidemics in KwaZulu-Natal and China to ineffective transmission control strategies.
Potential Strategies
Nardell described a number of potential strategies with the potential to reduce the transmission of drug-resistant TB.
Hospital Triage and Separation. Over the past 15 years, Partners In Health has designed and implemented an effective transmission control program in Haiti that may be a useful model for other resource-poor settings. This is a community-based treatment program with relatively few patients requiring hospitalization. When hospitalization is required, however, a baseline triage and separation strategy is implemented. Patients are admitted to either the general medical ward, a TB pavilion, or very basic isolation rooms based on smear results and HIV status (see Figure 3-5). Although this approach is not ideal, Nardell argued that implementing this simple baseline strategy globally would help in combating the TB epidemic. The strategy is imperfect for several reasons: sputum smear-positive patients can transmit their disease, smear-positive patients in the TB pavilion can reinfect one another, and unsuspected cases pose a threat. Compared with current conditions, however, this baseline strategy could be highly effective if adapted and widely implemented in settings where no transmission control currently exists. At the same time, while apparently effective in Haiti, this model might not have the same success in Africa, where in many settings 85–90 percent of individuals infected with MDR TB are coinfected with HIV: It is more difficult to triage patients effectively when HIV infection is so dominant.
Ventilation. The rooms used in Haiti have natural ventilation supplemented by exhaust fans in isolation rooms. Under optimal design and climatic conditions, natural ventilation can be very effective in increasing the number of air changes per hour (ACH). Nardell presented data from KwaZulu-Natal to support this claim. Moll and colleagues (2007) reported at the recent IUATLD meeting in Paris that in a recently renovated ward, the rate of air replacement with windows closed and no ventilation equaled 0.3 ACH; the rate with closed windows plus ventilation equaled 16 ACH; and the rate with windows open and mixer fans on was much greater, equaling 67 ACH.
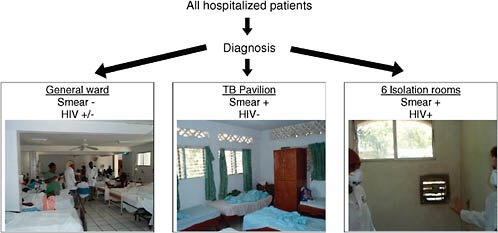
FIGURE 3-5 Partners In Health’s community-based TB treatment triage strategy in Haiti.
NOTE: The general medical ward has natural ventilation and ultraviolet (UV) air disinfection; the TB ward has natural ventilation with fenestrated brick and more UV fixtures to disinfect the air than the general ward has; the six isolation rooms are off a common corridor, and each has a large exhaust fan built into the wall that draws air into the room from the corridor, as well as a UV fixture.
SOURCE: Nardell, 2008.
Respirators. The role of respirators in TB transmission control in resource-poor settings is controversial both because the equipment is costly and because the opportunities for transmission are legion. Respiratory protection is used optimally to reduce industrial risks for filterable airborne hazards—settings where the risky exposure activities are relatively few and can be identified for use of the equipment. In regions with high TB prevalence, exposure to the disease is commonplace, from unsuspected as well as from known sources. Moreover, because properly fitting disposable respirators are costly, they tend to be used for prolonged periods, and protection may deteriorate because of leaky face seals. Better respirators that are cleanable and reusable are needed for the developing world. A new program sponsored by the U.S. Veterans Administration is aimed at developing better respirators for health care workers requiring prolonged protection during a possible influenza pandemic. These nondisposable respirators may also be appropriate for use in resource-limited settings. At present, available nondisposable respirators interfere with speech, among other limitations. At the Partners In Health Lesotho MDR TB hospital, however, nurses and doctors have been using nondisposable respirators despite these limitations with the expectation of better protection at lower cost.
New Resources. New resources have been invested in several programs. The WHO infection control sub-working group (under TB-HIV) was established to provide guidance for and monitoring of transmission control interventions. New funding for TB transmission control has been made available through a number of major global funders, including PEPFAR and the Global Fund for AIDS, Tuberculosis, and Malaria. Multiple organizations, including the TB Control Assistance Program, CDC, and others, have launched training programs to develop the needed expertise. Harvard School of Public Health, for example, recently held a 2-week summer course for engineers and architects on design and engineering aspects of airborne infection control. Despite this infusion of new resources, however, the expertise needed to implement these interventions is lacking.
New Research. New research is under way on several novel interventions to enhance transmission control:
-
Nardell stated that installation of upper-room UV air disinfection in a hospital and TB/HIV ward in Lima has been shown to reduce transmission by 72 percent. Additional experiments with upper-room UV disinfection are being conducted at an MDR TB hospital in South Africa, with sentinel guinea pigs being used to determine whether the intervention is effective in preventing transmission. That study is also showing excellent efficacy.
-
The Harvard-based nonprofit organization Medicine in Need, or MEND, is developing inhaled antibiotics—specifically dry powder inhaled capreomycin that is aimed at improved therapy in the lung but may also provide a new approach to contagion control.
Summary
Farmer closed the discussion of infection control by stating that the apparent magnitude of transmitted MDR and XDR TB has profound implications for infection control, yet attention to this issue throughout the developing world is currently inadequate. Treating drug-resistant TB patients in hospitals is inherently problematic because it is difficult to prevent noninfected patients from being exposed. Rather than managing patients as inpatients in a hospital setting, it is important to establish effective community-based care that offers the potential to deliver higher-quality care, yield better outcomes, and reduce transmission.
IMPLICATIONS FOR HEALTH CARE WORKERS
As discussed earlier in this chapter, during the XDR TB epidemic in Tugela Ferry in 2006, 53 patients were diagnosed with XDR TB. Gandhi elaborated on the impact of that occurrence on health care workers in the region. Among health care workers involved in treating those afflicted by the XDR TB epidemic, there were four in whom XDR TB was suspected; all four were HIV infected, and all four died with a rapid course similar to that of the 53 patients. Since the initial cases were described, additional health care workers have been infected with both MDR and XDR TB. Strategies to protect health care workers have now been implemented, but the risk has not been eliminated. Friedland estimated that, at least in Tugela Ferry, about 75 percent of expected cases in health care workers could be averted if simple measures were instituted. He added that infection in health care workers has consequences for health care systems as well as individuals. The former consequences can be dire beyond those immediately affected, as they can deter other workers from providing care to TB patients or from working in an environment where TB patients are being treated.