5
Interdisciplinary Collaboration
FOSTERING COLLABORATION AMONG HEALTH CARE PROFESSIONALS
Studies of the context in which health care is delivered date back at least to the reforms instituted by Florence Nightingale in the 1850s, said Dr. Pamela Mitchell, professor of Biobehavioral Nursing and Health Systems at the University of Washington and president of the American Academy of Nursing. Since then, many other studies have looked at issues such as continuous quality improvement, patient safety, and crew resource management as ways to improve interprofessional collaboration.
In a demonstration project conducted in the 1980s by the American Association of Critical-Care Nurses, a positive work environment characterized by interprofessional collaboration and a high level of expertise on the part of both nurses and physicians had lower-than-expected mortality and very high patient satisfaction (Mitchell et al., 1989). As this association was tested in a larger number of critical care units with generally good mortality outcomes, an association between positive work environments and reduced mortality proved to be elusive. Nevertheless, this study, and several others conducted over the years, showed that a positive work environment led to greater retention of registered nurses (RNs) because they developed a sense of having a greater influence over the working environment, more collaboration with physicians and other health care workers, and access to a wider variety of conflict resolution skills. These studies also showed that physicians had better perceptions of the quality of nurses, other physicians, and the unit as a whole, while RNs had better perceptions of overall quality and patient satisfaction
(Ingersoll and Schmitt, 2004; Mitchell et al., 1996). Together, this research contributed to a recommendation made in 2003 at a summit sponsored by the Institute of Medicine that health professions education should focus on core competencies for all health professionals so they can work in interdisciplinary teams, use evidence-based practice, provide patient-centered care, apply quality improvement principles, and use information technologies, as shown in Figure 5-1 (IOM, 2003).
Since World War II numerous attempts have been made to create educational endeavors that bring people together across professions. For example, the rehabilitation of soldiers wounded in World War II required the input of many people in both acute care and rehabilitation. The Great Society of the 1960s brought a resurgence of these educational efforts, augmented by the increased use of technology in intensive care units. In the mid-1970s and 1980s, there was dedicated federal and private funding for interdisciplinary education (Baldwin, 1996). Periods of health care reform tend to produce greater funding for such endeavors, Mitchell said, which means that interprofessional education could again receive greater attention in the years ahead.
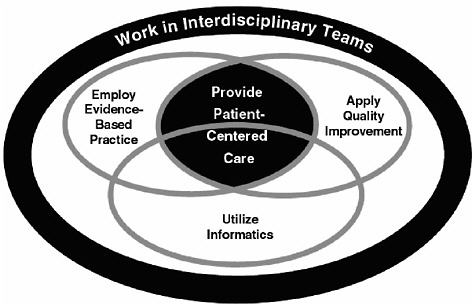
FIGURE 5-1 Relationship among core competencies for health professionals.
SOURCE: IOM (2003).
In recent years, the University of Washington and many other educational institutions have experimented with different forms of interprofessional education. These approaches were grounded in the belief that collaboration requires understanding and respect for others’ expertise as well as competence in one’s own practice discipline. Collaboration also requires understanding the context and complexity of the health of a population, which requires basic group skills such as conflict resolution (Mitchell et al., 2006). However, these approaches to interprofessional collaboration initially underplayed the importance of including the patient, family, and others in the community as part of the care team, Mitchell said. “That is something that I believe needs to be emphasized as we move forward.”
Several years ago, Mitchell served on an IOM committee that produced the report Keeping Patients Safe: Transforming the Work Environment of Nurses (IOM, 2004). The report recommended that hospitals and educational institutions support nursing staff in ongoing acquisition and maintenance of knowledge and skills. It also recommended adopting mechanisms such as interdisciplinary rounds and ongoing education in interdisciplinary collaboration.
Work from Dr. Stephen Shortell and colleagues about successful quality improvement programs forms a useful framework for identifying the components of successful interprofessional education programs (Shortell et al., 1996). Strategically, such programs need institutional leadership and faculty champions. Structurally, they need consistent institutional policies and a physical infrastructure. Technical knowledge and skills need to be combined with a meaningful focus. In addition, a culture of collaboration, strong personal relationships, and time and flexibility are needed to make programs work.
Mitchell offered a single recommendation: Academic institutions and health care organizations need to make a real commitment to interprofessional education that develops and sustains collaborative skills, both before and after licensure. The recommendation is not new, Mitchell said. “But let’s make it real this time.… That means committing money, committing resources, and committing structure.”
DISRUPTIVE BEHAVIOR, NURSING CARE, AND PATIENT SAFETY
In 2000, Dr. Alan Rosenstein, vice president and medical director for VHA West Coast, began to study the effects of disruptive behavior on nursing care and patient safety. Rosenstein defined disruptive behavior as “any inappropriate behavior, confrontation, or conflict ranging from verbal abuse to physical or sexual harassment.” Disruptive behavior in the workplace is a serious concern for those who experience it and witness it, as well as for the patients being cared for in this negative environment. As demonstrated in Figure 5-2, there is relatively little physical abuse, Rosenstein said, but there is “a lot of yelling, a lot of screaming, a lot of condescending, berating behavior, particularly in front of peers.”
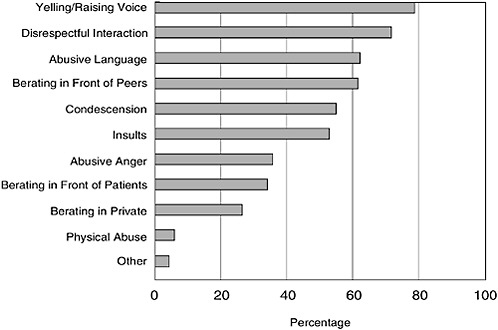
FIGURE 5-2 Types of disruptive behaviors witnessed by respondents. The data represented in this figure are from VHA West Coast surveys received from June 2002 through November 2009. Results shown are from the entire respondent group, including nurses, physicians, administrative executives, and those who listed their title as “other.”
Little if any research had been published on the subject of disruptive behavior before, but an initial survey opened up a “Pandora’s box,” Rosenstein noted. The survey found a high incidence of disruptive behaviors among physicians, with a significant impact on nurse satisfaction and retention (Rosenstein, 2002; Rosenstein et al., 2002). A follow-up survey published in 2005 found that disruptive behavior by both physicians and nurses had a significant impact on clinical outcomes of care (Rosenstein and O’Daniel, 2005). Additional surveys in 2007 and 2008 documented a significant impact of disruptive behavior on clinical outcomes in high-stress areas such as surgery and cardiovascular specialties and on psychological factors (Rosenstein and O’Daniel, 2006, 2008a, 2008b). “Disruptive behavior has tremendous ramifications … and the data are striking,” Rosenstein said.
According to these surveys, 77 percent of hospital personnel have witnessed disruptive behavior from a physician at their hospital and 65 percent have witnessed disruptive behavior from a nurse. Those figures rise to 88 and 73 percent, respectively, for surveys of RNs. Such behavior from physicians tends to be more overt, while among nurses it can be more subtle, “which is probably more disruptive because you don’t know where you are at.” Rosenstein’s research also found that 60 to 70 percent of the adverse events that happen to patients can be traced to problems with communication. Furthermore, 50 percent of physicians are not good communicators, Rosenstein said.
The problem is not new, but bureaucracy, hierarchies, and politics have stymied efforts to deal with it, Rosenstein said. More recently, the effects of disruptive behavior on nurse and patient satisfaction and patient safety have increased focus on the problem. Surveys show that one third of nurses who leave hospitals do so at least in part because of disruptive physicians, which has become a particular concern as nursing shortages have become more pressing. Surveys also show that this disruptive behavior often leads to stress, frustration, loss of concentration, reduced collaboration, reduced information transfer, reduced communication, and impaired nurse–physician relationships.
Furthermore, surveys done by Rosenstein and his collaborators document a link between disruptive behavior and undesirable clinical outcomes, including adverse events, errors, increased mortality, and decreased patient safety, quality of care, and patient satisfaction, as shown in Figure 5-3. Among all personnel surveyed, 18 percent were aware of specific adverse effects that occurred as a result of disruptive behavior.
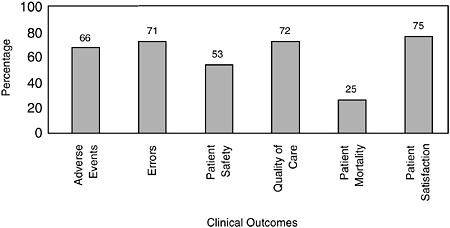
FIGURE 5-3 Linkage of disruptive behavior to undesirable clinical outcomes reported as occurring sometimes, frequently, or constantly. The data represented in this figure are from VHA West Coast surveys received from June 2002 through November 2009. As in Figure 5-2, results shown are from the entire respondent group, including nurses, physicians, administrative executives, and those who listed their title as “other.”
Comments from individuals substantiated this finding, Rosenstein said. As one respondent wrote, “Most nurses are afraid to call Dr. X when they need to, and frequently won’t call. Their patients’ medical safety is always in jeopardy because of this.” Another wrote, “Staff nurses advocated for better patient care, but M.D. [was] not willing to listen to reason. As a result the patient died. The doctor chose to undo all the help that various staff had been working on for weeks to get this patient the help so badly needed.”
Many factors cause people to act and react the way they do in these situations, including age differences, gender, culture, ethnicity, values, experiences, training, and personality styles. Stress, frustration, fatigue, depression, substance abuse, or a lack of emotional intelligence can all contribute to the problem, as can situational factors such as the environment or the mood of the day.
Modifying behaviors can be difficult, but several steps could reduce disruptive behaviors. Organizations need to be committed to changing the culture, with endorsement from leadership. One way to approach the problem is with an internal survey, because staff typically do not want to discuss these issues in public. Education needs to occur across the board, from the senior level to students, including administra-
tors and support staff. Advanced training can focus on the areas of diversity, competence (in both knowledge and communication), and assertiveness. Programs to reduce disruptive behavior need to offer structured training and educational programs, coaching support, endorsement by clinical champions, reinforcement of policies and procedures, a consistent process for reporting and follow-up for disruptive events, and strategies to enforce compliance through means such as intervention and feedback. Early intervention programs have the greatest chance of success (Rosenstein, 2009).
These steps need to be taken to reinforce patient safety initiatives, Rosenstein asserted. “What nurses really want is to feel that they are a part of the process, that they are respected, and that they have some participation in a patient’s care plan.”
REACTIONS AND QUESTIONS
Nancy Chiang remarked on the particular value of collaboration for students. “The willingness of the various disciplines in the hospital to work with students is crucial,” she said. “Clinical time is very limited for us, so in addition to what we get from the nurses, what we get from the other specialties is just as important.”
In response to a question about the best way for interprofessional education to occur, Mitchell cited a program at the University of South-ampton in England in which teams of medical students, nurses, social workers, and pharmacists worked with particular units in the hospital to develop continuous quality improvement projects. Just being around people from other professions is not enough, she said. People need to work through problems together, often with the aid of a coach or facilitator.
In response to a question about whether an age and gender gap between physicians and nurses contributes to a lack of collaboration and whether narrowing that gap will change matters, Rosenstein responded that an “old guard” still exists in health care that has been doing business the same way for many years. “There are still enough of the old people around, and until we can convince them to make the right changes, it is going to be slow to happen.”
Bernice Coleman agreed that bringing colleagues along in efforts to change the culture of health care can be difficult. She reiterated that all advanced-practice nurses should be part of an active interdisciplinary
team during their training. “They are going to need to do that, and they are the clinical leaders, so I think it is a critical part of their education.”
Finally, a viewer of the webcast commented that multidisciplinary education should include not just physicians and nurses, but hospital and health care administrators as well.








