2
Social Security Disability Programs and Procedures
This chapter contains a brief summary of the Social Security Administration’s (SSA’s) disability programs and procedures. Readers familiar with Social Security disability may wish to proceed directly to the next chapter. However, it may be useful to review some key features of the programs that the committee considered and treated as givens in their approach to evaluating and recommending changes in the cardiovascular listings, as follows:
-
The statutory definition of disability used to decide if a claimant should receive disability benefits is strict—essentially, it requires an adult claimant to have a medically determinable impairment or impairments that prevent the ability to work for a continuous period of not less than 12 months or is expected to result in death. An individual with partial or short-term disability is not entitled to Social Security disability benefits. Therefore, many individuals with severe impairments that limit, or even prevent, their ability to perform their usual work will not be entitled.
-
One example of why a claimant with a severe cardiovascular impairment may not be disabled is that the effects of treatment may improve his or her functional status. Treatment may include medical, surgical, or a prescribed program of progressive physical activity, among others. When a claimant with a cardiovascular impairment is on a prescribed treatment program, SSA may defer evaluation of the impairment or impairments for up to 3 months from the beginning of the treatment cycle to gauge net benefit on the individual’s functional status.
-
By law, the disability must result from a “medically determinable impairment,” defined as an impairment that results from anatomical, physiological, or psychological abnormalities that can be shown by medically acceptable clinical and laboratory diagnostic techniques. Therefore, diagnostic techniques and measures of medical severity of cardiovascular impairments in SSA’s Listing of Impairments (the Listings) should be as current as possible.
-
The Listings are the third step in the five-step sequential evaluation process for adults (see Figure 2-1), where they serve as an administrative expedient to quickly identify allowances, that is, cases in which the impairment is considered severe enough to prevent the claimant from doing any work. Thus the Listings help SSA avoid subjecting obviously disabled claimants to a time- and resource-intensive, in-depth assessment of their residual functional capacity and vocational issues that must be performed at later steps of the sequential evaluation process.
-
The use of the Listings as an administrative expedient has declined over time. Currently, nearly half of the allowances made annually are based on the Listings, compared with approximately 70 percent in the 1980s.
-
The adult Listings are based on a standard stricter than the statutory definition of disability, that is, the inability to engage in “any gainful activity” rather than the inability to engage in “any substantial gainful activity.” The Listings standard is stricter because the purpose of the Listings is to describe impairments that are severe enough to prevent an individual from doing any work without even considering his or her age, education, or work experience.
-
Claimants who are not allowed at the Listings step are not necessarily denied. Those with severe impairments may be allowed at Step 5 of the sequential evaluation process based on an assessment of their residual functional capacity and considering their age, education, and work history.
-
SSA has Listings for children under age 18 with criteria that are used to assess a child’s impairment or impairments. If the criteria in the Listings for children do not apply, or if there is no equivalent child listing, SSA may use the criteria in an appropriate adult listing. In addition to meeting or medically equaling a listing, a child may functionally equal the Listings by having “marked and severe functional limitations.”
-
After nonmedical eligibility is confirmed by an SSA field office, the claim is sent to one of the SSA state agencies, usually called disability determination services (DDS), in the state where the claimant lives. DDSs, funded by SSA, are responsible for case de-
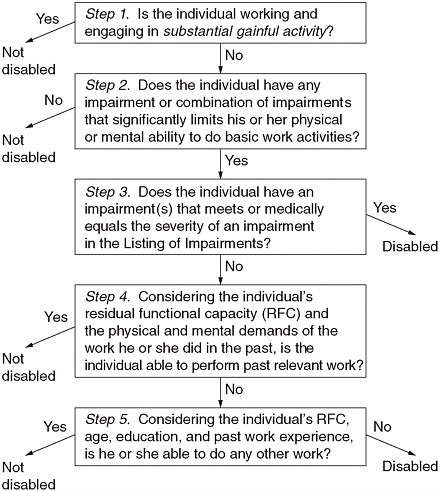
FIGURE 2-1 Five-step sequential evaluation process for adults.
SOURCES: 20 CFR §§ 404.1520 and 416.920.
-
velopment, the initial decision to allow or deny the claim, and the first level of appeal.
-
In most states, the decisions in DDSs are usually made by an adjudicative team composed of a medical consultant (e.g., a licensed physician) or a psychological consultant (a licensed or certified psychologist) and a lay disability examiner. The adjudicative team determines whether a claimant is disabled based on medical and other evidence in the case record, but does not see the claimant in person.
-
Most claims involving cardiovascular impairments involve medical consultants who are generalists (i.e., internists or family practice
-
doctors), except that: (1) claims for children under the Supplemental Security Income (SSI) program must involve a pediatrician or another appropriate specialist, and (2) claims for adults or children in which there is an indication of a mental impairment and that are unfavorable to the claimant must generally involve a psychiatrist or psychologist. Few subspecialists, such as cardiologists, are in the DDSs (IOM, 2007).
-
SSA will not pay for expensive, invasive, or risky procedures that would otherwise be useful in diagnosis and assessing impairment severity, such as coronary angiography. Therefore, some claimants who have not undergone such procedures privately (because, for example, they lack health insurance or geographic access to care) may not be able to show an impairment that meets a listing.
-
SSA prefers that the requirements for meeting a listing rely on tests, examinations, or other kinds of information that are likely to be available in the medical record. If the Listings rely solely or primarily on cutting-edge tests that are better technically, but not generally available in doctors’ offices or health facilities nationally, or that are very expensive, few claimants would be able to show an impairment that meets a listing, which would defeat the purpose of the Listings.
-
By law, SSA cannot interfere with the patient–doctor relationship, so the most it will require, and only to meet some listings, is adherence to “prescribed therapy,” which may or may not be optimum therapy as defined by the latest clinical guidelines. Willful refusal to follow prescribed therapy that is clearly expected to restore the capacity to work may be grounds for denial, but SSA does not require disabled claimants to stop smoking, lose excess weight, or take other evidence-based steps to reduce or end disability.
SSA DISABILITY PROGRAMS
SSA pays disability benefits through two programs: Social Security Disability Insurance (SSDI) and SSI. In 2008, more than 12 million people received Social Security disability benefits (see Table 2-1). SSA expects to receive more than 3.3 million applications for disability benefits in fiscal year 2010, about 300,000 more than in fiscal year 2009 and 700,000 more than in fiscal year 2008 (SSA, 2010).
DEFINITION OF DISABILITY
To be found disabled, a claimant’s impairment or impairments must meet SSA’s statutory definition of disability. Adult disability is based on the
TABLE 2-1 Numbers of Disability Program Beneficiaries and Benefit Amounts, 2008
inability to work. Childhood disability under SSI is based on functional limitations. The definitions are as follows:
-
Adult disability is “the inability to engage in any substantial gainful activity by reason of any medically determinable physical or mental impairment(s) which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months.”
-
A child under the age of 18 is considered disabled if he or she has “a medically determinable physical or mental impairment, which results in marked and severe functional limitations, and which can be expected to result in death or which has lasted or can be expected to last for a continuous period of not less than 12 months.”
DISABILITY EVALUATION DECISION PROCESS
SSA uses a sequential evaluation process to determine whether a claimant is disabled. The evaluation stops at any step in the sequence at which a decision about disability is made. The steps are different for adults and children, although the Listings are applied at the third step in each case.
Adult Disability Decision Process
At Step 1 of the adult evaluation (Figure 2-1), SSA determines whether the claimant is engaging in substantial gainful activity (SGA). If not, the claim is forwarded to the DDS and proceeds to Step 2 to determine whether
the claimant has a severe medically determinable impairment or impairments that significantly limit the claimant’s ability to perform basic work activities (e.g., standing, sitting). If the claimant is found to have a severe impairment, then SSA determines, at Step 3, whether the impairment satisfies the criteria describing a medical condition found in the Listings. The Listings serve as an administrative expedient to quickly identify allowances.
Step 3 is the first point at which the claimant may be found disabled, but if the claimant’s impairment or impairments do not meet or medically equal a listing, the claim is not denied. Rather, adult claims not allowed at the Listings step proceed to Step 4, which consider the claimant’s ability to perform past relevant work, and if necessary, to Step 5, which considers the claimant’s ability to do other work that exists in significant numbers in the national economy. At Step 4, SSA assesses the claimant’s residual functional capacity (RFC), which is the claimant’s remaining ability to do physical and mental work-related activities despite limitations from all of his or her impairment or impairments, including any impairments that are not “severe.” Assessing RFC is a time- and resource-intensive process based on an analysis of all relevant medical and other evidence in the case record and requires a more detailed assessment of functioning than under listings that also include functional criteria.
At Step 4, SSA uses the RFC assessment to determine the claimant’s capacity to do past relevant work (defined in part as jobs held during the previous 15 years). If SSA determines that the claimant is unable to perform past relevant work, the claim progresses to Step 5.
At Step 5, SSA evaluates the claimant’s capacity to adjust to any other kind of work, taking into consideration his or her age, educational attainment, work experience, and RFC. Generally, the greater the age of the individual, the lower his or her educational attainment, and the lower the skill level of previous jobs held, the more likely it will be that SSA will find the claimant disabled. If the claimant is found capable of performing other work, he or she is not considered disabled. If he or she cannot perform other work, he or she is considered disabled based on medical and vocational factors.
Child Disability Determination Process
For children under age 18 applying for SSI benefits, Steps 1 and 2 of the evaluation process are essentially the same (Figure 2-2). At Step 3, the considerations are whether a child’s impairment meets or medically equals a listing, as in the adult evaluation process, or “functionally equals the Listings.” Unlike meets and medical equivalence, functional equivalence is not based on specific listings but on a standard of “listing-level severity”; that is, an impairment or impairments must result in “marked” limitations
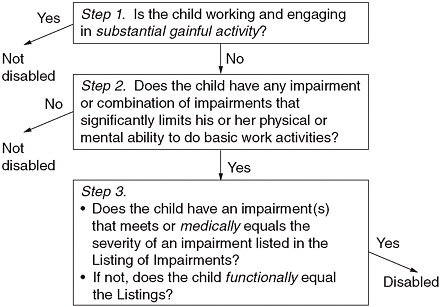
FIGURE 2-2 Disability evaluation process for Supplemental Security Income children.
SOURCE: 20 CFR § 416.924.
in two domains of functioning or an “extreme” limitation in one domain. Domains are broad areas of functioning intended to capture all of what a child can or cannot do in activities at home, at school, and in the community compared with other children of the same age who do not have impairments. The domains are as follows:
-
Acquiring and using information;
-
Attending and completing tasks;
-
Interacting and relating with others;
-
Moving about and manipulating objects;
-
Caring for yourself; and
-
Health and physical well-being.
For each of the first five domains, a “marked” limitation is found when a child’s impairment or impairments interfere seriously with his or her ability to independently initiate, sustain, or complete activities. A “marked” limitation also means one that is “more than moderate” but “less than extreme.” It is the equivalent of the functioning one would expect to find on standardized testing with scores that are at least two, but less than three, standard deviations below the mean.
An “extreme” limitation is found when a child’s impairment or impairments interfere very seriously with his or her ability to independently initi-
ate, sustain, or complete activities. An “extreme” limitation also means a limitation that is “more than marked,” and is the rating given to the worst limitation. It is the equivalent of the functioning one would expect to find on standardized testing with scores that are at least three standard deviations below the mean. Limitation in the sixth domain, “health and physical well-being,” is also assessed on the frequency of impairment-related illnesses or exacerbations that result in significant documented symptoms or signs.
THE LISTING OF IMPAIRMENTS
History and Purpose
SSA has used a listing of impairments to ease the administrative burden of determining the functional capacity of each claimant since the disability freeze program, the immediate predecessor to the SSDI program, began in 1955.1 The Listings were, and are, a set of serious medical conditions used to identify claimants with medical conditions of such severity that they could be considered disabled without further evaluation. SSA updates the Listings periodically. Every adult claim that can be allowed based on the Listings is one that does not have to undergo the lengthy RFC assessment or the vocational analyses required at Steps 4 and 5. Thus, the Listings are an administrative expedient that allows SSA to process many cases more quickly and efficiently, which saves time and resources.
In applying the Listings, SSA’s concern is that the criteria in the Listings describe impairments that are severe enough to prevent an individual from doing any gainful activity, regardless of his or her age, education, or work experience. This Listings severity standard is stricter than the statutory standard for disability in adults because, under the Listings, claimants have to be unable to engage in “any gainful activity” rather than in “any substantial gainful activity” as required by the statute. Although the Listings standard is stricter, SSA also wants a reasonable threshold of severity for the criteria in the Listings in order to allow as many claimants as appropriate under the Listings. Further, SSA wants the criteria in the Listings to be clear and easy to apply so that their adjudicators can allow claims quickly under Listings.
Over time, however, the Listings have become much less effective in expediting allowances. The percentage of claims initially allowed based on the Listings has been declining steadily, from 70 percent in the 1980s to
about 50 percent now (IOM, 2007). At the same time, the percentage of claims allowed initially has remained about the same, raising the question of whether the Listings could be revised to allow more claims at Step 3, thus reducing the number of claims to decide at Steps 4 and 5.
Structure
The Listings consist of Part A (primarily for adults) and Part B (for children only). They are organized into 14 body systems for adults and 15 for children.2 For each body system, the Listings are preceded by a narrative introductory text that defines key concepts, terms, and procedures used in that body system to document the diagnosis and severity of an impairment. For ease of use, the Listings are numbered according to body system and disease or condition. For example, 4.00, the cardiovascular system, has eight separate adult listings, as follows:
-
Chronic heart failure (4.02);
-
Ischemic heart disease (4.04);
-
Recurrent arrhythmias (4.05);
-
Symptomatic congenital heart disease (4.06);
-
Heart transplant (4.09);
-
Aneurysm of aorta or major branches (4.10);
-
Chronic venous insufficiency (4.11); and
-
Peripheral arterial disease (4.12).
Updating the Listings
SSA has periodically revised the Listings since first publishing them as regulations in 1968. The last comprehensive revision was in 1985. Since then, SSA has focused on updates that address single body systems or sometimes specific listings. In recent years, SSA has been systematically updating all the body systems on a continual basis.
Over time, SSA has added steps to the revision process to expand input from knowledgeable sources outside SSA. Rather than beginning the revision process by proposing new or revised rules in a Notice of Proposed Rulemaking (NPRM) in the Federal Register, SSA first issues an Advance Notice of Proposed Rulemaking, which announces its intention to update a
specific body system or a specific listing or listings and asks for suggestions from the public. SSA may also hold one or more outreach meetings at which researchers, clinicians, patients, and patient representatives give presentations commenting on the existing listings and offering suggestions on how to revise them. After these additional steps in the process, SSA drafts proposed rules and publishes an NPRM for public comment before issuing final rules.
INITIAL DECISIONS
Social Security disability claims are initially processed through a network of local SSA field offices and DDSs. Field offices make determinations that claimants are not entitled based on non-disability criteria and generally make the determination when a claimant is doing SGA. In most cases, however, DDSs develop and evaluate medical and other evidence of disability and make the initial disability determination.
The DDS first attempts to obtain evidence from the claimant’s treating physicians and medical sources. If that evidence is unavailable or insufficient to make a determination, the DDS will arrange for a consultative examination (CE) to obtain the necessary additional medical information. The claimant’s treating physician is the preferred source for the CE, but the DDS also may obtain it from an independent source.
Based on all the medical and other information, the DDS makes the initial disability determination. Disability determinations are most often made by an adjudicative team composed of a medical consultant (e.g., a licensed physician) or a psychological consultant (a licensed or certified psychologist) and a lay disability examiner. Reasonable efforts are made to ensure that an appropriate specialist evaluates cases involving mental disorders (e.g., a psychologist or psychiatrist) or those involving children (e.g., a pediatrician or speech-language pathologist). Most claims involving physical impairments are evaluated by medical consultants who are generalists (e.g., internists and family medicine physicians); relatively few subspecialists work for DDSs except in a few large states.
In fiscal year 2009, DDSs adjudicated 2.8 million disability claims in an average time of 101 days (SSA, 2009c).
APPEALS PROCESS
After the initial decision, claimants have the opportunity to appeal the determination. The appeals process generally consists of four levels: the first three are reconsideration, administrative law judge hearing, and appeals council review. If the claimant is still dissatisfied with SSA’s final decision, he or she may ask for judicial review by filing a civil lawsuit in federal district court. The appeals process levels are described below:
-
Reconsideration—If the claimant is dissatisfied with the determination, he or she may request reconsideration. A different adjudicative team in the DDS then makes a new determination, following the same procedures described for initial determinations above. In fiscal year 2009, DDSs conducted 598,000 reconsiderations (SSA, 2009c).
-
Administrative law judge (ALJ) hearing—If the claimant is dissatisfied with the reconsideration determination, he or she may appeal to SSA’s Office of Disability Adjudication and Review for a de novo hearing before an ALJ. Claimants usually appear before the ALJ in person. Most claimants have an attorney or other representative, although representation is not required. The ALJ may ask for testimony from a medical or vocational expert, or both. Most ALJ decisions are based on the claimant’s RFC rather than the first three steps of sequential evaluation, including the Listings. In fiscal year 2009, ALJs held 661,000 hearings (SSA, 2009c).
-
Appeals Council—If the claimant is dissatisfied with the ALJ decision, the claimant may ask for review by SSA’s Appeals Council. The Appeals Council will review the ALJ decision and will not usually make its own decision. Thus, the Appeals Council may deny or dismiss the request for review without making a decision. The Appeals Council may also issue its own decision affirming, modifying, or reversing the ALJ decision or remand the case to an ALJ for more proceedings at the hearing level. There were 89,000 Appeals Council reviews in fiscal year 2009 (SSA, 2009c).
-
Federal court—If the claimant is dissatisfied with the Appeals Council’s action, the claimant may appeal to the federal courts, up to and including the Supreme Court.
REVIEW OF CONTINUING DISABILITY
SSA is required by law to determine if there is continuing disability in every case allowed. At the time of the initial allowance, cases are classified as follows:
-
Medical improvement expected (MIE);
-
Medical improvement possible (MIP); or
-
Medical improvement not expected (MINE).
In MIE cases, a continuing disability review (CDR) is conducted 6 to 18 months after the most recent decision that the individual is disabled. Cases that involve medical interventions, such as bypass surgery, angioplasty, or pacemaker implantation, may be classified as MIE and reviewed after a
year or similar time period.3 For organ transplantation, including heart transplantation, a 1-year period of disability is specified in the applicable listings. After the year, the beneficiary is reevaluated to determine if a residual impairment exists that still prevents SGA.
MIP cases, in which improvement is possible but not predictable, are subject to a CDR at least every 3 years. MINE cases involve extremely severe conditions that SSA expects from experience to remain static or be progressively disabling.4 The law still requires SSA to review them, but they are reviewed every 5 to 7 years.
SSA confirms that many beneficiaries are still disabled through the use of a “mailer”—a form sent to the claimant to determine whether there has been a change in the claimant’s medical or other status. When SSA conducts a full CDR, it develops medical and other evidence on the beneficiary’s current condition, including health status, work status, education and vocational training, and activities of daily living. If the evidence shows that there has been medical improvement in the beneficiary’s impairment or impairments and the person has the ability to engage in SGA, his or her benefits may be terminated. SSA completed 317,000 CDRs in fiscal year 2009 (SSA, 2009c).
DEVELOPMENT OF MEDICAL EVIDENCE
The DDS is responsible for developing a person’s complete medical history for at least the previous 12 months in most claims. “Every reasonable effort” is made to obtain medical reports from the claimant’s treating physician and other medical sources. DDS medical and psychological consultants (hereafter both referred to as medical consultants) are involved in evaluating the medical and other evidence by reviewing information in existing records, assessing it for completeness and consistency, requesting additional information as needed, and clarifying any concerns that the disability examiner may have about the medical and other evidence in the case record. Evidence includes objective medical information (i.e., signs and laboratory findings) and other evidence, including statements or reports from the claimant, the treating or examining physician, psychologist, or other source, and others about the claimant’s medical history, diagnosis, prescribed treatment, daily activities, efforts to work, and any other infor-
mation about the impact of the claimant’s impairment or impairments and related symptoms on the ability to work.
REFERENCES
IOM (Institute of Medicine). 2007. Improving the Social Security disability decision process, edited by J. D. Stobo, M. McGeary, and D. K. Barnes. Washington, DC: The National Academies Press. http://www.nap.edu/catalog.php?record_id=11859 (accessed June 29, 2010).
SSA (Social Security Administration). 2009a. Annual statistical report on the Social Security Disability Insurance Program, 2008. http://www.ssa.gov/policy/docs/statcomps/di_asr/2008/index.html (accessed June 2, 2010).
SSA. 2009b. SSI annual statistical report, 2008. http://www.ssa.gov/policy/docs/statcomps/ssi_asr/index.html (accessed June 2, 2010).
SSA. 2009c. FY2009 performance and accountability report. Baltimore, MD: SSA. http://www.ssa.gov/finance/2009/Full%20FY%202009%20PAR.pdf (accessed June 28, 2010).
SSA. 2010. Social Security helps states with mounting disability claims. http://www.ssa.gov/pressoffice/pr/est-pr.htm (accessed May 10, 2010).














