5
Transforming Leadership
|
Key Message #3: Nurses should be full partners, with physicians and other health professionals, in redesigning health care in the United States. Strong leadership is critical if the vision of a transformed health care system is to be realized. Yet not all nurses begin their career with thoughts of becoming a leader. The nursing profession must produce leaders throughout the health care system, from the bedside to the boardroom, who can serve as full partners with other health professionals and be accountable for their own contributions to delivering high-quality care while working collaboratively with leaders from other health professions. |
In addition to changes in nursing practice and education, discussed in Chapters 3 and 4, respectively, strong leadership will be required to realize the vision of a transformed health care system. Although the public is not used to viewing nurses as leaders, and not all nurses begin their career with thoughts of becoming a leader, all nurses must be leaders in the design, implementation, and evaluation of, as well as advocacy for, the ongoing reforms to the system that will be needed. Additionally, nurses will need leadership skills and competencies to act as full partners with physicians and other health professionals in redesign and
reform efforts across the health care system. Nursing research and practice must continue to identify and develop evidence-based improvements to care, and these improvements must be tested and adopted through policy changes across the health care system. Nursing leaders must translate new research findings to the practice environment and into nursing education and from nursing education into practice and policy.
Being a full partner transcends all levels of the nursing profession and requires leadership skills and competencies that must be applied both within the profession and in collaboration with other health professionals. In care environments, being a full partner involves taking responsibility for identifying problems and areas of waste, devising and implementing a plan for improvement, tracking improvement over time, and making necessary adjustments to realize established goals. Serving as strong patient advocates, nurses must be involved in decision making about how to improve the delivery of care.
Being a full partner translates more broadly to the health policy arena. To be effective in reconceptualized roles and to be seen and accepted as leaders, nurses must see policy as something they can shape and develop rather than something that happens to them, whether at the local organizational level or the national level. They must speak the language of policy and engage in the political process effectively, and work cohesively as a profession. Nurses should have a voice in health policy decision making, as well as being engaged in implementation efforts related to health care reform. Nurses also should serve actively on advisory committees, commissions, and boards where policy decisions are made to advance health systems to improve patient care. Nurses must build new partnerships with other clinicians, business owners, philanthropists, elected officials, and the public to help realize these improvements.
This chapter focuses on key message #3 set forth in Chapter 1: Nurses should be full partners, with physicians and other health professionals, in redesigning health care in the United States. The chapter begins by considering the new style of leadership that is needed. It then issues a call to nurses to respond to the challenge. The third section describes three avenues—leadership programs for nurses, mentorship, and involvement in the policy-making process—through which that call can be answered. The chapter then issues a call for new partnerships to tap the full potential of nurses to serve as leaders in the health care system. The final section presents the committee’s conclusions regarding the need to transform leadership in the nursing profession.
A NEW STYLE OF LEADERSHIP
Those involved in the health care system—nurses, physicians, patients, and others—play increasingly interdependent roles. Problems arise every day that do not have easy or singular solutions. Leaders who merely give directions and expect them to be followed will not succeed in this environment. What is needed is
a style of leadership that involves working with others as full partners in a context of mutual respect and collaboration. This leadership style has been associated with improved patient outcomes, a reduction in medical errors, and less staff turnover (Gardner, 2005; Joint Commission, 2008; Pearson et al., 2007). It may also reduce the amount of workplace bullying and disruptive behavior, which remains a problem in the health care field (Joint Commission, 2008; Olender-Russo, 2009; Rosenstein and O’Daniel, 2008). Yet while the benefits of collaboration among health professionals have repeatedly been documented with respect to improved patient outcomes, reduced lengths of hospital stay, cost savings, increased job satisfaction and retention among nurses, and improved teamwork, interprofessional collaboration frequently is not the norm in the health care field. Changing this culture will not be easy.
The new style of leadership that is needed flows in all directions at all levels. Everyone from the bedside to the boardroom must engage colleagues, subordinates, and executives so that together they can identify and achieve common goals (Bradford and Cohen, 1998). All members of the health care team must share in the collaborative management of their practice. Physicians, nurses, and other health professionals must work together to break down the walls of hierarchal silos and hold each other accountable for improving quality and decreasing preventable adverse events and medication errors. All must display the capacity to adapt to the continually evolving dynamics of the health care system.
Leadership Competencies
Nurses at all levels need strong leadership skills to contribute to patient safety and quality of care. Yet their history as a profession dominated by females can make it easier for policy makers, other health professionals, and the public to view nurses as “functional doers”—those who carry out the instructions of others—rather than “thoughtful strategists”—those who are informed decision makers and whose independent actions are based on education, evidence, and experience. A 2009 Gallup poll of more than 1,500 national opinion leaders,1 “Nursing Leadership from Bedside to Boardroom: Opinion Leaders’ Perceptions,” identified nurses as “one of the most trusted sources of health information” (see Box 5-1) (RWJF, 2010a). The Gallup poll also identified nurses as the health professionals that should have greater influence than they currently do in the critical areas of quality of patient care and safety. The leaders surveyed believed that major obstacles prevent nurses from being more influential in health policy decision making. These findings have crucial implications for front-line nurses,
|
BOX 5-1 Results of Gallup Poll “Nursing Leadership from Bedside to Boardroom: Opinion Leaders’ Perceptions”
SOURCE: RWJF, 2010a. |
who possess critical knowledge and awareness of the patient, family, and community but do not speak up as often as they should.
To be more effective leaders and full partners, nurses need to possess two critical sets of competencies: a common set that can serve as the foundation for any leadership opportunity and a more specific set tailored to a particular context, time, and place. The former set includes, among others, knowledge of the care delivery system, how to work in teams, how to collaborate effectively within and across disciplines, the basic tenets of ethical care, how to be an effective patient advocate, theories of innovation, and the foundations for quality and safety improvement. These competencies also are recommended by the American Association of Colleges of Nursing as essential for baccalaureate programs (AACN, 2008). Leadership competencies recommended by the National League for Nursing and National League for Nursing Accrediting Commission are being revised to reflect similar principles. More specific competencies might include learning how to be a full partner in a health team in which members from various professions hold each other accountable for improving quality and decreasing preventable adverse events and medication errors. Additionally, nurses who are interested in pursuing entrepreneurial and business development opportunities need competencies in such areas as economics and market forces, regulatory frameworks, and financing policy.
Leadership in a Collaborative Environment
As noted in Chapter 1, a growing body of research has begun to highlight the potential for collaboration among teams of diverse individuals from different professions (Paulus and Nijstad, 2003; Pisano and Verganti, 2008; Singh and Fleming, 2010; Wuchty et al., 2007). Practitioners and organizational leaders alike have declared that collaboration is a key strategy for improving problem solving and achieving innovation in health care. Two nursing researchers who have studied collaboration among health professionals define it as
a communication process that fosters innovation and advanced problem solving among people who are of different disciplines, organizational ranks, or institutional settings [and who] band together for advanced problem solving [in order to] discern innovative solutions without regard to discipline, rank, or institutional affiliation [and to] enact change based on a higher standard of care or organizational outcomes. (Kinnaman and Bleich, 2004)
Much of what is called collaboration is more likely cooperation or coordination of care. Katzenbach and Smith (1993) argue that truly collaborative teams differ from high-functioning groups that have a defined leader and a set direction, but in which the dynamics of true teamwork are absent. The case study presented in Box 5-2 illustrates just how important it is for health professionals to work in teams to ensure that care is accessible and patient centered.
Leadership at Every Level
Leadership from nurses is needed at every level and across all settings. Although collaboration is generally a laudable goal, there are many times when nurses, for the sake of delivering exceptional patient and family care, must step into an advocate role with a singular voice. At the same time, effective leadership also requires recognition of situations in which it is more important to mediate, collaborate, or follow others who are acting in leadership roles. Nurses must understand that their leadership is as important to providing quality care as is their technical ability to deliver care at the bedside in a safe and effective manner. They must lead in improving work processes on the front lines; creating new integrated practice models; working with others, from organizational policy makers to state legislators, to craft practice policy and legislation that allows nurses to work to their fullest capacity; leading curriculum changes to prepare the nursing workforce to meet community and patient needs; translating and applying research findings into practice and developing functional models of care; and serving on institutional and policy-making boards where critical decisions affecting patients are made.
Leadership in care delivery is particularly important in community and
|
The AAI’s director, Claudia J. Beverly, PhD, RN, FAAN, said that these two components are funded separately but go hand in hand in practice. New patients usually see a physician for an initial examination. APRNs are responsible for health promotion and disease prevention—mammograms and flu shots, for example—as well as analyses of current drug regimens. For patients with complex conditions, social workers make referrals and work with families on nursing home placement. Almost all older Arkansans can now access interprofessional geriatric care within an hour’s drive of their home. Patients are quite satisfied with their care and with the team approach (Beverly et al., 2007). Unpublished analyses of the areas around the centers show lower rates of emergency room use and hospitalization and higher rates of health care knowledge among elderly patients. Physicians at the eight sites report to Dr. Beverly, who is also director of UAMS’s Hartford Center of Geriatric Nursing Excellence, which provides some funding to the AAI. She has hired a nurse with a doctorate and a geriatrician to act as associate directors. Developing teamwork has been a priority. “This is such a beautiful case study in how nursing and medicine can work together,” she said, “and how, together, we can do good things.” There have been some obstacles: primary care services are dependent upon Medicare funding, and with an annual budget of $2 million to divide among eight sites, additional revenue is needed. There also may not be enough clinicians trained in geriatrics available. And although Dr. Beverly believes that APRNs “should have their own panel of patients,” they see only returning patients at the centers. She said funding has been secured to further evaluate how best to use team members. The model has continued to evolve from the first center in Northwest Arkansas that Dr. Beverly started as a Robert Wood Johnson Executive Nurse Fellow. That site is developing a program for the training of in-home caregivers, including home health aides and family members. And a new telehealth project will allow patients and clinicians to “see” a specialist electronically. “Economically, this is going to provide a huge benefit to patients,” Ms. Overton-McCoy said.  Nurse Amyleigh Overton-McCoy explains to Bonnie Sturgeon how to manage the common health concerns associated with aging. |
home settings where nurses work more autonomously with patients and families than they do in the acute care setting. In community and home settings, nurses provide a direct link connecting patients, their caregivers, and other members of the health care team. Other members of the health care team may not have the time, expertise, or first-hand experience with the patient’s home environment and circumstances to understand and respond to patient and family needs. For example, a neurologist may not be able to help a caregiver of an Alzheimer’s patient understand or curtail excessive spending habits, or a surgeon may not be able to offer advice to a caregiver on ostomy care—roles that nurses are perfectly positioned to assume. Leadership in these situations sometimes requires nurses to be assertive and to have a strong voice in advocating for patients and their families to ensure that their needs are communicated and adequately met.
Box 5-3 describes a nurse who evolved over the course of her career from thinking that being an effective nurse was all about honing her nursing skills and competencies to realize that becoming an agent of change was an equally important part of her job.
A CALL FOR NURSES TO LEAD
Leadership does not occur in a social or political vacuum. As Bennis and Nanus (2003) note, the fast pace of change can be managed only if it is accompanied by leaders who can track the context of the “social architecture” to sustain and implement innovative ideas. Creating innovative care models at the bedside and in the community or taking the opportunity to fill a seat in a policy-making body or boardroom requires nurse leaders to develop ideas; approach management; and courageously make decisions within the political, economic, and social context that will make their solutions real and sustainable. A shift must take place in how nurses view their responsibility to those they care for; they must see themselves as full partners with other health professionals, and practice and education environments must socialize and educate them accordingly.
An important aspect of this socialization is mentoring others along the way. More experienced nurses must take the time to show those who are new and less experienced the most effective ways of being an exceptional nurse at the bedside, in the boardroom, and everywhere between. Technology such as chat rooms, Facebook, and even blogs can be used to support the mentoring role.
A crucial part of working within the social architecture is understanding how leadership and practice produce change over time. The nursing profession’s history includes many examples of the effect of nursing leadership on changes in systems and improvements in patient care. In the late 1940s and early 1950s, nurse Elizabeth Carnegie led the fight for the racial integration of nursing in Florida by example and through her extraordinary character and organizational skills. Her efforts to integrate the nursing profession were based in her sense of social justice not just for the profession, but also for the care of African American
citizens who had little access to a workforce that was highly skilled or provided adequate access to health care services. Also in Florida, in the late 1950s, Dorothy Smith, the first dean of the new University of Florida College of Nursing, developed nursing practice models that brought nursing faculty into the hospital in a joint nursing service. Students thereby had role models in their learning experiences, and staff nurses had the authority to improve patient care. From this system came the patient kardex and the unit manager system that freed nurses from the constant search for supplies that took them away from the bedside. In the 1980s, nursing research by Neville Strumpf and Lois Evans highlighted the danger of using restraints on frail elders (Evans and Strumpf, 1989; Strumpf and Evans, 1988). Their efforts to translate their findings into practice revolutionized nursing practice in nursing homes, hospitals, and other facilities by focusing nursing care on preventing falls and other injuries related to restraint use, and led to state and federal legislation that resulted in reducing the use of restraints on frail elders.
Nurses also have also led efforts to improve health and access to care through entrepreneurial endeavors. For example, Ruth Lubic founded the first free-standing birth center in the country in 1975 in New York City. In 2000, she opened the Family Health and Birth Center in Washington, DC, which provides care to underserved communities (see Box 2-2 in Chapter 2). Her efforts have improved the care of thousands of women over the years. There are many other examples of nurse entrepreneurs, and a nurse entrepreneur network2 exists that provides networking, education and training, and coaching for nurses seeking to enter the marketplace and business.
Will Student Nurses Hear the Call?
Leadership skills must be learned and mastered over time. Nonetheless, it is important to obtain a basic grasp of those skills as early as possible—starting in school (see Chapter 4). Nursing educators must give their students the most relevant knowledge and practice opportunities to equip them for their profession, while instilling in them a desire and expectation for new learning in the years to come. Regardless of the basic degree with which a nurse enters the profession, faculty should feel obligated to show students the way to their first or next career placement, as well as to their next degree and continuous learning opportunities.
Moreover, students should not wait for graduation to exercise their potential for leadership. In Georgia, for example, health students came together in 2001 under the banner “Lead or Be Led” to create a student-led, interprofessional nonprofit organization that “seeks to make being active in the health community a professional habit.” Named Health Students Taking Action Together (Health-STAT), the group continues to offer workshops in political advocacy, media
|
BOX 5-3 Nurse Profile: Connie Hill A Nurse Leader Extends Acute Care Nursing Beyond the Hospital Walls It was at a 2002 meeting at Children’s Memorial Hospital in Chicago that Connie Hill, MSN, RN, reviewed the chart of a child who had been on a ventilator in her unit for 2 years. She asked her colleagues why the child had not been discharged. “It wasn’t because she was not medically stable,” Ms. Hill said recently, “but because there was a lack of community resources to support her.” Inadequate community services existed for a child with special needs in Chicago, the third-largest city in the nation? “I was dumbfounded,” she recalled. “And I said, ‘We need to start a consortium. We need to invite policy makers, state agencies, community leaders.’ And people just looked at me, like, ‘Okay, Connie. How are we going to get that started?’” As director of 9 West, the 30-bed Allergy/Pulmonary/Transitional Care Unit, Ms. Hill persisted, and in 2004 the Consortium for Children with Complex Medical Needs was formed. The 75-member coalition of parents, clinicians, advocates, and representatives of government agencies and insurance companies meets quarterly, with the goal of “networking, education, and advocacy” on behalf of the city’s special-needs children, some of whom may be on ventilators indefinitely. For example, the group identified poor reimbursement of home health care as a serious obstacle, and the hospital established ties to agencies able to tackle the reimbursement issue. Now, some children can go home to receive care.  Connie Hill, MSN, RN Ms. Hill never intended to be a leader. She was working as a staff nurse at the hospital in the mid-1990s when colleagues encouraged |
training, networking, and fundraising. Its annual leadership symposium convenes medical, nursing, public health, and other students statewide to learn about health issues facing the state and work together on developing potential solutions (HealthSTAT, 2010). The National Student Nurses Association (NSNA), initiated in 1998, offers an online Leadership University that allows students to enhance
|
her to apply for a clinical manager position in 9 West. She followed their advice, and in late 2000 when her supervisor failed to return from maternity leave, she proposed a “shared leadership model.” After a year or so during which she and two other nurses shared the directorship, Ms. Hill was asked to become sole director (some staff were uncomfortable with the decentralized authority, despite good clinical outcomes). She did so, with a modest goal: “I wanted to provide a venue for all nurses to have a voice.” With this goal in mind, Ms. Hill decided in 2008 that 9 West would be a good fit for Transforming Care at the Bedside (TCAB), a national initiative of The Robert Wood Johnson Foundation with the Institute for Healthcare Improvement. Communication between nurses and rotating medical residents was targeted in the hospital’s quest to improve the coordination of care (Quisling, 2009). As Ms. Hill said, “It’s disheartening when you receive a patient survey and a family says, ‘The doctor said this, but then the nurse told me that.’” A procedure was created for staff nurses to provide orientations to residents, who rotate monthly among units, to foster better team communication. Residents are now more likely to confer with 9 West nurses during rounds, Ms. Hill said, increasing satisfaction among nurses, residents, patients, and families. As a doctoral student at the University of Wisconsin-Milwaukee College of Nursing, Ms. Hill is examining an often neglected population: teens born with HIV, a majority of whom are African American and Hispanic. Now that many HIV-positive children survive into adulthood, they mature sexually and face the stigma attached to the infection. Ms. Hill’s study uses PhotoVoice, which involves putting cameras into the hands of HIV-positive teens and asking them for a visual answer to the question, “Where do you see yourself in five years?” “They’re writing their own story” in photographs, she said, a story they can use to raise awareness in others and to remind themselves of their own strengths.
Ms. Hill has quite a story herself. As a mother of a grown son, a pediatric nurse who endured many hospitalizations as a child, a researcher whose study is an outgrowth of her advocacy work, and an African American who strives to enhance access to health care for all, she is a woman of both practical ideas and lofty ideals. So when she saw that a child capable of living at home had been in her unit for 2 years, her natural response was to assemble a consortium. Today, that child is doing well at home. |
their capacity for leadership through several avenues, such as earning academic credit for participating in the university’s leadership activities and discussing leadership issues with faculty. Students work in cooperative relationships with other students from various disciplines, faculty, community organizations, and the public (Janetti, 2003). Box 5-4 profiles two student leaders, one of whom eventu-
|
BOX 5-4 Nurse Profile: Kenya D. Haney and Billy A. Caceres Building Diversity in Nursing, One Student at a Time Despite improvements to the demographic make up of the nursing workforce in recent decades, the workforce remains predominantly white, female, and middle aged. Racial and ethnic minorities make up 34 percent of the U.S. population but only 12 percent of the registered nurse (RN) workforce, and just 7 percent of RNs are men (AACN, 2010). And diversity matters to patients: many studies have shown that a more diverse health care workforce results in greater access to care for minority populations (IOM, 2004). Two nurses, an African American woman and a Hispanic man, both under age 35, illustrate the growing diversity of the profession and the importance of offering various educational paths as an entry into nursing. Kenya D. Haney, RN, was a married mother of two in 2004 when she was trying to decide between nursing school and law school. She had taken classes toward a bachelor’s degree in communications and knew she would need a more flexible program. She chose the associate’s degree in nursing program at St. Louis Community College in Missouri: it offered a part-time option and child care at $2 an hour, which her educational grants covered. If the child care had not been available, she would have waited until her children were older, she said, and then “gone back to finish the communications degree and gone on to law school. There’s just not a doubt in my mind.” After graduating, Ms. Haney got a job in intensive care; entered the  Kenya D. Haney, RN bachelor’s of science in nursing (BSN) program for RNs at the University of Missouri, St. Louis; and joined the Breakthrough to Nursing initiative at the National Student Nurses Association (NSNA). The NSNA initiative aims to increase the number of men entering the profession, recruit and retain nurses of diverse ethnic and racial backgrounds, support nursing students with physical disabilities, and increase enrollment of young and nontraditional students. It works toward these goals by making peers available to students in need of support. Ms. Haney became its director in 2008 and NSNA president in 2009. “You know, we’re not the answer to everything,” she said |
|
of Breakthrough to Nursing. “But we’re there for support. Maybe we’ll just say, ‘You can do this. You’re not alone, and you really are needed.’”
Billy A. Caceres, BSN, RN, already had a bachelor’s degree in politics and communications and a job in event planning for a New York City nonprofit when he made the decision to pursue a BSN. As an undergraduate at New York University (NYU), he had volunteered to raise awareness of sexual assault and substance abuse on campus and wanted to learn more about health. He applied and was accepted to NYU’s College of Nursing in its 15-month accelerated program for students with a bachelor’s in another field. Soon he became involved in the Hartford Geriatric Nursing Institute at NYU. As a nurse, Mr. Caceres has encountered bias at times from patients, especially older women, some of whom feel uncomfortable being cared for by a man. “I don’t get offended,” he said. “But sometimes I think, What if nobody else was around? What would you do? I’m just trying to provide care for you.” He has just begun his first job as a hospital staff nurse, in a New York City orthopedics unit, and hopes one day to merge his interests in geriatrics and health policy, he said. Both Ms. Haney and Mr. Caceres intend to pursue graduate degrees,  Billy A. Caceras, BSN, RN perhaps even the doctorate. If so, they will be models for a new generation: only 23 percent of students in research-focused doctoral programs in nursing are from minority backgrounds, and only 7 percent are men (AACN, 2010). Regardless, the two have taken significant steps. As Ms. Haney said, “Sometimes it’s that initial barrier of getting into nursing school that can hurt so many. But the NSNA is a way to bring us together to see that we have one common goal, and that is to be professional nurses. Basically, it’s for the patient.”
|
ally became NSNA president; both represent as well the growing diversity of the nursing profession, a crucial need if the profession is to rise to the challenge of helping to transform the health care system (see Chapter 4).
Looking to the future, nurse leaders will need the skills and knowledge to understand and anticipate population trends. Formal preparation of student nurses may need to go beyond what has traditionally been considered nursing education. To this end, a growing number of schools offer dual undergraduate degrees in partnership with the university’s business or engineering school for nurses interested in starting their own business or developing more useful technology. Graduate programs offering dual degree programs with schools of business, public health, law, design, or communications take this idea one step further to equip students with an interest in administrative, philanthropic, regulatory, or policy-making positions with greater competencies in management, finance, communication, system design, or scope-of-practice regulations from the start of their careers.
Will Front-Line Nurses Hear the Call?
Given their direct and sustained contact with patients, front-line nurses, along with their unit or clinic managers, are uniquely positioned to design new models of care to improve quality, efficiency, and safety. Tapping that potential will require developing a new workplace culture that encourages and supports leaders at the point of care (whether a hospital or the community) and requires all members of a health care team to hold each other accountable for the team’s performance; nurses must also be equipped with the communication, conflict resolution, and negotiating skills necessary to succeed in leadership and partnership roles. For example, one new quality and safety strategy requires checklists to be completed before certain procedures, such as inserting a catheter, are begun. Nurses typically are asked to enforce adherence to the checklist. If another nurse or a physician does not wash his/her hands or contaminates a sterile field, nurses must possess the basic leadership skills to remind their colleague of the protocol and stop the procedure, if necessary, until the checklist is followed. And again, nurses must help and mentor each other in their roles as expert clinicians and patient advocates. No one can build the capabilities of an exceptional and effective nurse like another exceptional and effective nurse.
Will Community Nurses Hear the Call?
Nurses working in the community have long understood that to be effective in contributing to improvements in the entire community’s health, they must assume the role of social change agent. Among other things, community and public health nurses must promote immunization, good nutrition, and physical
activity; detect emergency health threats; and prevent and respond to outbreaks of communicable diseases. In addition, they need to be prepared to assume roles in dealing with public health emergencies, including disaster preparedness, response, and recovery. Recent declines in the numbers of community and public health nurses, however, have made the leadership imperative for these nurses much more challenging.
Community and public health nurses learn to expect the unexpected. For example, a school nurse alerted health authorities to the arrival of the H1N1 influenza virus in New York City in 2009 (RWJF, 2010c). Likewise, an increasing number of nurses are being trained in incident command as part of preparedness for natural disasters and possible terrorist attacks. This entails understanding the roles of and working with community, state, and federal officials to assure the health and safety of the public. For example, when the town of Chehalis, south of Seattle, experienced a 100-year flood in 2007, a public health nurse called the secretary of Washington State’s Department of Health, Mary Selecky, to ask how to “deal with and dispose of dead cows, an unforeseen challenge [for] a public health nurse. The nurse knew she needed [to provide] tetanus shots and portable toilets but had not anticipated other, less common, aspects of the emergency” (IOM, 2010).
The profile in Box 5-5 illustrates how nurses lead efforts that provide critical services for communities. The profile also shows how nurses can also become leaders and social change agents in the broader community by serving on the boards of health-related institutions. The importance of this role is discussed in the next section.
Will Chief Nursing Officers Hear the Call?
Although chief nursing officers (CNOs) typically are part of the hierarchical decision-making structure in that they have authority and responsibility for the nursing staff, they need to move up in the reporting structure of their organizations to increase their ability to contribute to key decisions. Not only is this not happening, however, but CNOs appear to be losing ground. A 2002 survey by the American Organization of Nurse Executives (AONE) showed that 55 percent of CNOs reported directly to their institution’s CEO, compared with 60 percent in 2000. More CNOs described a direct reporting relationship to the chief operating officer instead. Such changes in reporting structure can limit nurse leaders’ involvement in decision making about the most important product of hospitals—patient care. Additionally, the AONE survey showed that most CNOs (70 percent) have seen their responsibilities increase even as they have moved down in the reporting structure (Ballein Search Partners and AONE, 2003). CNOs face growing issues of contending not only with increased responsibilities, but also with budget pressures and difficulties with staffing, retention, and turnover levels during a nursing shortage (Jones et al., 2008).
|
BOX 5-5 Nurse Profile: Mary Ann Christopher Cultivating Neighborhood Nursing at the Visiting Nurse Association of Central Jersey At the Visiting Nurse Association of Central Jersey (VNACJ), president and chief executive officer Mary Ann Christopher, MSN, RN, FAAN, maintains a $100 million annual budget, a 4,000-patient daily census, and a 1,700-person staff. Services available to residents in 10 central New Jersey counties include home care, primary care, wellness services, mental health care, rehabilitation, homeless services, and hospice and palliative care. Yet despite the size and complexity of the 98-year-old organization, Ms. Christopher’s primary objective has remained simple in her 27-year career there. “People need to know that you stand for what you say you stand for,” she said. And what the VNACJ stands for is local communities “driving” the services provided. Ms. Christopher has called it Neighborhood Nursing, a collaborative model in which nurses are assigned to specific neighborhoods so they and community members can respond to what they identify as the most pressing health issues. As an example of the model, she cites a VNACJ nurse who noticed that many residents of a retirement community were exhibiting signs of congestive heart failure. The nurse proposed that the VNACJ set up a  Mary Ann Christopher, MSN, RN, FAAN kiosk that would contain a telehealth monitor. The device would permit residents to check their weight, oxygen saturation, and blood pressure levels and automatically transmit the values to a cardiac nurse. If a patient’s indicators were outside the desired range, the nurse and patient would converse remotely, in real time, and patients needing a medica |
Nurses also are underrepresented on institution and hospital boards, either their own or others. A biennial survey of hospitals and health systems conducted in 2007 by the Governance Institute found that only 0.8 percent of voting board members were CNOs, compared with 5.1 percent who were vice presidents for medical affairs (Governance Institute, 2007). More recently, a 2009 survey of
|
tion adjustment would be visited. The VNACJ funded the idea, and outcomes are being monitored. Ms. Christopher said that the aims of such an initiative are both immediate and long term. In the short run, the VNACJ hopes to reduce rates of emergency room (ER) use and repeated hospitalizations—expensive and inefficient means of managing chronic illness. As for the long-term goal, the VNACJ nurses strive to give individuals as well as entire communities greater control over their health. After the telehealth kiosk was set up, for example, residents began paying attention to one another’s weight and blood pressure levels. Ms. Christopher has secured grants to test a wide range of such ideas. For example, the Mobile Outreach Program has reduced rates of ER use among deinstitutionalized mentally ill and homeless patients; funded in the mid-1980s by The Robert Wood Johnson Foundation and the State of New Jersey, it is now supported by local governments. The Mobile Outreach Program is the VNACJ initiative Ms. Christopher is the most proud of and the one, she said, that may be the most replicable. In 1998 the Balanced Budget Act resulted in a 15 percent reduction in revenues and left the VNACJ with only $100,000 in reserve. Now, even with $24 million in reserve, Ms. Christopher worries about declines in federal, state, and philanthropic funding, especially in light of the recent increases in un- and underinsured patients being seen as a result of the recession. Still, she said that the agency’s focus on providing services the community values, even as those values change, has kept the association fiscally sound.
Not all CEOs of visiting nurse associations are nurses (those in New York City and Boston, for example, are not). Ms. Christopher said she can see why it matters that she is a nurse. First, she knows well what nurses can do. She has cultivated an atmosphere of honoring staff ideas (such as the cardiac monitoring initiative). As a result, the VNACJ has a turnover rate of less than 5 percent for nurses. Second, Ms. Christopher is sought after to serve on governing boards and advisory groups and is the only RN on the board of trustees at the University of Medicine and Dentistry of New Jersey. She believes that her nursing expertise, keen sense of community, and fiscal responsibility give her “legitimacy at any table I’m at…being a guardian for what’s best for patients and communities.” |
community health systems found that nurses made up only 2.3 percent of their boards, compared with 22.6 percent who were physicians (Prybil et al., 2009).3
While most boards focus mainly on finance and business, health care delivery, quality, and responsiveness to the public—areas in which the nature of their work gives nurses particular expertise—also are considered key (Center for Healthcare Governance, 2007). A 2007 survey found that 62 percent of boards included a quality committee (Governance Institute, 2007). A 2006 survey of hospital presidents and CEOs showed the impact of such committees. Those institutions with a quality committee were more likely to adopt various oversight practices; they also experienced lower mortality rates for six common medical conditions measured by the Agency for Healthcare Research and Quality’s (AHRQ’s) Inpatient Quality Indicators and the State Inpatient Databases (Jiang et al., 2008).
The growing attention of hospital boards to quality and safety issues reflects the increased visibility of these issues in recent years. Several states and the Centers for Medicare and Medicaid Services, for example, are increasing their oversight of specific preventable errors (“never events”), and new payment structures in health care reform may be based on patient outcomes and satisfaction (Hassmiller and Bolton, 2009; IOM, 2000; King, 2009; Wachter, 2009). Given their expertise in quality and safety improvement, nurses are more likely than many other board members to understand the issues involved and often can educate other members about these issues (Mastal et al., 2007). This is one area, then, in which nurse board members can have a significant impact. Recognizing this, the 2009 survey of community health systems mentioned above specifically recommended that community health system boards consider appointing expert nursing leaders as voting board members to strengthen clinical input in deliberations and decision-making processes (Prybil et al., 2009).
More CNOs need to prepare themselves and seek out opportunities to serve on the boards of health-related institutions. If decisions are taking place about patient care and a nurse is not at the decision-making table, important perspectives will be missed. CNOs should also promote leadership activities among their staff, encouraging them to secure important decision-making positions on committees and boards, both internal and external to the organization.
Will Nurse Researchers Hear the Call?
Nurse researchers must develop new models of quality care that are evidence based, patient centered, affordable, and accessible to diverse populations. Developing and imparting the science of nursing is also an important contribution to nurses’ ability to deliver high-quality, safe care. Additionally, nurses must serve as advocates and implementers for the program designs they develop. Academic–service partnerships that typically involve nursing schools and nearby, often low-income communities are a first step toward implementation. Given that a nursing school does not exist in every community, however, such partnerships cannot achieve change on the scale needed to transform the health care system. Nurse researchers must become active not only in studying important care deliv-
ery questions but also in translating research findings into practice and developing and setting the policy agendas. Their leadership is vital in ensuring that new state-and federal-level policies are based on evidence and will help increase quality and access while decreasing costs and health care disparities. The Affordable Care Act (ACA) provides opportunities for demonstration projects and pilot programs directed at various elements of nursing. If these projects and programs do not adequately track nursing inputs and intended/unintended outcomes, they cannot hope to achieve their potential.
Nurse researchers should seek funding from the National Institute for Nursing Research and other institutes of the National Institutes of Health, as do scientists from other disciplines, to help increase the evidence base for improved models of care. Funding might also be secured from other government entities, such as AHRQ and the Health Resources and Services Administration (HRSA) and local and national foundations, depending on the research topic. To be competitive in these efforts, nurses should hone their analytical skills with training in such areas as statistics and data analysis, econometrics, biometrics, and other qualitative and quantitative research methods that are appropriate to their research topics. Mark Pauly, codirector of the Robert Wood Johnson Foundation’s Interdisciplinary Nursing Quality Research Initiative, argues that, for nursing research to achieve parity with other health services research in terms of acceptability, it must be managed by interprofessional teams that include both nurse scholars and scholars from methodological and modeling disciplines. For nurse researchers to achieve parity with other health services researchers, they must develop the skills and initiative to take leadership roles in this research.4
Will Nursing Organizations Hear the Call?
The Gallup poll of 1,500 opinion leaders referenced earlier in this chapter also highlighted fragmentation in the leadership of nursing organizations as a challenge. Responding opinion leaders predicted that nurses will have little influence on health care reform over the next 5–10 years (see Figure 5-1). By contrast, they believed that nurses should have more input and impact in areas such as planning, policy development, and management (Figure 5-2) (RWJF, 2010a). No one expects all professional health organizations to coordinate their public agendas, actions, or messaging for every issue. But nursing organizations must continue to collaborate and work hard to develop common messages, including visions and missions, with regard to their ability to offer evidence-based solutions
|
4 |
Personal communication, Mark Pauly, Bendheim Professor, Professor of Health Care Management, Professor of Business and Public Policy, Professor of Insurance and Risk Management, and Professor of Economics, Wharton School of the University of Pennsylvania, and Codirector of the Robert Wood Johnson Foundation’s Interdisciplinary Nursing Quality Research Initiative, June 25, 2010. |
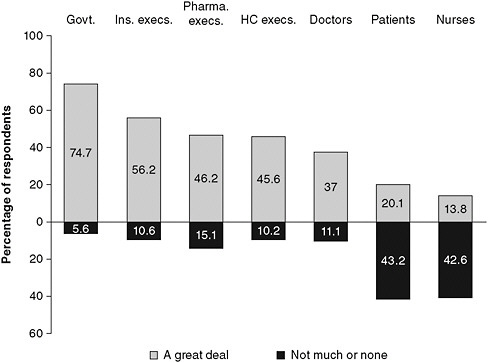
FIGURE 5-1 Opinion leaders’ predictions of the amount of influence nurses will have on health care reform.
NOTE: Govt. = Government; Ins. Execs. = Insurance executives; Pharma. execs. = Pharmaceutical executives; HC execs. = Health care executives.
SOURCE: RWJF, 2010b. Reprinted with permission from Frederick Mann, RWJF.
for improvements in patient care. Once common ground has been established, nursing organizations will need to activate their membership and constituents to work together to take action and support shared goals. When policy makers and other key decision makers know that the largest group of health professionals in the country is in agreement on important issues, they listen and often take action. Conversely, when nursing organizations and their members disagree with one another on important issues, decisions are not made, as the decision makers often are unsure of which side to take.
Quality and safety are important areas in which professional nursing organizations have great potential to serve as leaders. The Nursing Alliance for Quality Care (NAQC)5 is a Robert Wood Johnson Foundation–funded effort with the mission of advancing the quality, safety, and value of patient-centered health care for all individuals, including patients, their families, and the communities where patients live.
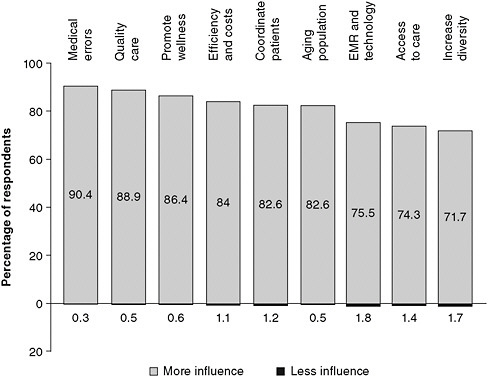
FIGURE 5-2 Opinion leaders’ views on the amount of influence nurses should have on various areas of health care.
SOURCE: RWJF, 2010b. Reprinted with permission from Frederick Mann, RWJF.
Based at the George Washington University School of Nursing, the organization stresses the need for nurses to advocate actively for and be accountable to patients for high-quality and safe care. The establishment of the NAQC “is based on the assumption that only with a stronger, more unified ‘voice’ in nursing policy will dramatic and sustainable achievements in quality and safety be achieved for the American public” (George Washington University Medical Center, 2010).
ANSWERING THE CALL
The call for nurses to assume leadership roles can be answered through leadership programs for nurses; mentorship; and involvement in the policy-making process, including political engagement.
Leadership Programs for Nurses
Leadership is not necessarily innate; many individuals develop into leaders. Sometimes that development comes through experience. For example, nurse
leaders at the executive level historically earned their way to their position through their competence, rather than obtaining formal preparation through a business school. However, development as a leader can also be achieved through more formal education and training programs. The wide range of effective leadership programs now available for nurses is illustrated by the examples described below. The challenge is to better utilize these opportunities to develop a greater number of nursing leaders.
Integrated Nurse Leadership Program
The Integrated Nurse Leadership Program (INLP),6 funded by the Gordon and Betty Moore Foundation, works with hospitals in the San Francisco Bay area that wish to remodel their professional culture and systems of care to improve care while dealing more effectively with continual change. The program develops hospital leaders, offers training and technical assistance, and provides grants to support the program’s implementation. INLP has found that the development of stable, effective leadership in nursing-related care is associated with better-than-expected patient care outcomes and improvements in nurse recruitment and retention. The impact of the program will be evaluated to produce models that can be replicated in other parts of the country.
Fellows Program in Management for Nurse Executives at Wharton7
When the Johnson & Johnson Company and the Wharton School joined in 1983 to offer a senior nurse executive management fellowship, the program concentrated on helping senior nursing leaders manage their departments by providing them, for example, intense training in accounting (Shea, 2005). The Wharton Fellows program has changed in many ways since then in response to the evolving health care environment, according to a 2005 review (Shea, 2005). For example, the program has strengthened senior nursing executives’ ability to argue for quality improvement on the basis of solid evidence, including financial documentation and probabilistic decision making. The program also aims to improve such leadership competencies as systems thinking, negotiation, communications, strategy, analysis, and the development of learning communities. Its offerings will likely undergo yet more changes as hospital chief executive and chief operating officers increasingly come from the ranks of the nursing profession.
Robert Wood Johnson Foundation Executive Nurse Fellows Program
The Robert Wood Johnson Foundation Executive Nurse Fellows Program8 is an advanced leadership program for nurses in senior executive roles who wish to lead improvements in health care from local to national levels. It provides a 3-year in-depth, comprehensive leadership development experience for nurses who are already serving in senior leadership positions. The program is designed to cultivate and expand fellows’ capacity to lead teams and organizations. The fellowship program includes curriculum and program activities that provide opportunities for executive coaching and mentoring, team-based and individual leadership projects, professional development that incorporates best practices in leadership, as well as access to online communities and leadership networks. Through the program, fellows master 20 leadership competencies that cover a broad range of knowledge and skills that can be used when “leading self, leading others, leading the organization and leading in health care” (RWJF Executive Nurse Fellows, 2010).
Best on Board
Best on Board9 is an education, testing, and certification program that helps prepare current and prospective leaders to serve on the governing board of a health care organization. Its CEO, Connie Curran, is a registered nurse (RN) who chaired a hospital nursing department, was the dean of a medical college, and founded her own national management and consulting services firm. A 2010 review cites the growing recognition by blue ribbon panels and management researchers that nurses are an untapped resource for the governing bodies of health care organizations. The authors argue that while nurses have many qualities that make them natural assets to any health care board, they must also “understand the advantages of serving on boards and what it takes to get there” (Curran and Totten, 2010).
Robert Wood Johnson Foundation Health Policy Fellows and Investigator Awards Programs
While not limited to nurses, the Robert Wood Johnson Foundation Health Policy Fellows and Investigator Awards programs10 offer nurses, other health professionals, and behavioral and social scientists “with an interest in health [the opportunity] to participate in health policy processes at the federal level” (RWJF Scholars, Fellows & Leadership Programs, 2010). Fellows work on Capitol Hill with elected officials and congressional staff. The goal is for fellows to use their academic and practice experience to inform the policy process and to improve
the quality of policies enacted. Investigators are funded to complete innovative studies of topics relevant to current and future health policy. Participants in both programs receive intensive training to improve the content and delivery of messages intended to improve health policy and practice. This training is critical, as investigators are often called upon to testify to Congress about the issues they have explored. The health policy fellows bring their more detailed understanding of how policies are formed back to their home organizations. In this way, they are more effective leaders as they strive to bring about policy changes that lead to improvements in patient care.
American Nurses Credentialing Center Magnet Recognition Program
Although not an individual leadership program, the American Nurses Credentialing Center (ANCC) Magnet Recognition Program11 recognizes health care organizations that advance nursing excellence and leadership. In this regard, achieving Magnet status indicates that the nursing workforce within the institution has attained a number of high standards relating to quality and standards of nursing practice. These standards, as designated by the Magnet process, are called “Forces of Magnetism.” According to ANCC, “the full expression of the Forces embodies a professional environment guided by a strong visionary nursing leader who advocates and supports development and excellence in nursing practice. As a natural outcome of this, the program elevates the reputation and standards of the nursing profession” (ANCC, 2010). Some of these Forces include quality of nursing leadership, management style, quality of care, autonomous nursing care, nurses as teachers, interprofessional relationships, and professional development.
Mentorship12
Leadership is also fostered through effective mentorship opportunities with leaders in nursing, other health professions, policy, and business. All nurses have a responsibility to mentor those who come after them, whether by helping a new nurse become oriented or by taking on more formal responsibilities as a teacher of nursing students or a preceptor. Nursing organizations (membership associations) also have a responsibility to provide mentoring and leadership guidance, as well as opportunities to share expertise and best practices, for those who join.
Fortunately, a number of nursing associations have organized networks to support their membership and facilitate such opportunities:
|
11 |
See http://www.nursecredentialing.org/Magnet/ProgramOverview.aspx. |
|
12 |
This section draws on personal communication in 2010 with Susan Gergely, Director of Operations, American Organization of Nurse Executives; Beverly Malone, CEO, National League for Nursing; Robert Rosseter, Chief Communications Officer, American Association of Colleges of Nursing; and Pat Ford Roegner, CEO, American Academy of Nursing. |
-
The American Association of Colleges of Nursing (AACN) conducts an expertise survey that is used to identify subject matter experts across topic areas within its membership; it also maintains a list of nursing education experts. Names of these experts are shared with members on request. These resources also are used to identify experts to serve on boards, respond to media requests, and serve in other capacities. In addition, AACN offers an annual executive leadership development program and a new deans mentoring program to further promote and foster leadership.
-
The National League for Nursing (NLN) has established an Academy of Nurse Educators whose members are available to serve as mentors for NLN members. NLN engages these educators in a variety of mentoring programs, from a National Scholarly Writing Retreat to the Johnson & Johnson mentoring program for new faculty.
-
While AONE does not have a formal mentoring program, it has developed online learning communities where members are encouraged to interact, post questions, and learn from each other. These online communities facilitate collaboration; encourage the sharing of knowledge, best practices, and resources; and help members discover solutions to day-to-day challenges in their work.
-
The American Academy of Nursing keeps a detailed list of nurse “Edge Runners”13 that describes the programs nursing leaders have developed and the outcomes of those programs. Edge Runner names and contact information are prominently displayed so that learning and mentoring can take place freely.14
-
The American Nurses Association just passed a resolution at its 2010 House of Delegates to develop a mentoring program for novice nurses. The program has yet to be developed.
-
Over the years, the National Coalition of Ethnic Minority Nurse Associations (NCEMNA) has offered numerous workshops, webinars, and educational materials to develop its members’ competencies in leadership, policy, and communications. NCEMNA’s highly regarded Scholars program15 promotes the academic and professional development of ethnic minority investigators, in part through a mentoring program. It serves as a model worth emulating throughout the nursing profession.
|
13 |
The Edge Runner program is a component of the American Academy of Nursing’s Raise the Voice campaign, funded by the Robert Wood Johnson Foundation. The Edge Runner designation recognizes nurses who have developed innovative, successful models of care and interventions to address problems in the health care delivery system or unmet health needs in a population. |
|
14 |
See AAN’s Edge Runner Directory, http://www.aannet.org/custom/edgeRunner/index.cfm?pageid=3303&showTitle=1. |
|
15 |
Involvement in Policy Making
Nurses may articulate what they want to happen in health care to make it more truly patient centered and to improve quality, access, and value. They may even have the evidence to support their conclusions. As with any worthy cause, however, they must engage in the policy-making process to ensure that the changes they believe in are realized. To this end, they must be able to envision themselves as leaders in that process and seek out new partners who share their goals.
The challenge now is to motivate all nurses to pursue leadership roles in the policy-making process. Political engagement is one avenue they can take to that end. As Bethany Hall-Long, a nurse who was elected to the Delaware State House of Representatives in 2002 and is now a state senator, writes, “political actions may be as simple as voting in local school board elections or sharing research findings with state officials, or as complex as running for elected office” (Hall-Long, 2009). For example, engaging school board candidates about the fundamental role of school nurses in the management of chronic conditions among students can make a difference at budget time. And if the goal is broader, perhaps to locate more community health clinics within schools, achieving buy-in from the local school board is absolutely vital. As Hall-Long writes, however, “since nurses do not regularly communicate with their elected officials, the elected officials listen to non-nursing individuals” (Hall-Long, 2009).
Political engagement can be a natural outgrowth of nursing experience. When Marilyn Tavenner first started working in an intensive care unit in Virginia, she thought, “If I were the head nurse or the nurse manager, I would make changes. I would try to influence that unit and that unit’s quality and staffing.” After she became a nurse manager, she thought, “I wouldn’t mind doing this for the entire hospital.” After succeeding for several years as a director of nursing, she was encouraged by a group of physicians to apply for the CEO position of her hospital when it became available. Eventually, Timothy Kaine, governor of Virginia from 2006 to 2010, recruited her to be the state’s secretary of health and human resources. In February 2010, Ms. Tavenner was named deputy administrator for the federal Centers for Medicare and Medicaid Services. Like many nurses, she had never envisioned working in government. But she realized that she wanted to have an impact on health care and health care reform. She wanted to help the uninsured find resources and access to care. For her, that meant building on relationships and finding opportunities to work in government.16
Other notable nurses who have answered the call to serve in government include Sheila Burke, who served as chief of staff to former Senate Majority Leader Robert Dole, has been a member of the Medicare Payment Advisory Commission,
and now teaches at Georgetown and Harvard Universities; and Mary Wakefield, who was named administrator of HRSA in 2009 and is the highest-ranking nurse in the Obama Administration. Speaker of the House Nancy Pelosi’s office has had back-to-back nurses from The Robert Wood Johnson Foundation Health Policy Fellows Program as staffers since 2007, providing a significant entry point for the development of new health policy leaders. Additionally, in 1989 Senator Daniel Inouye established the Military Nurse Detailee fellowship program. This 1-year fellowship provides an opportunity for a high-ranking military nurse, who holds a minimum of a master’s degree, to gain health policy leadership experience in Senator Inouye’s office. The fellowship rotates among three branches of service (Army, Navy, and Air Force) annually.17 During the Clinton Administration, Beverly Malone served as deputy assistant secretary for health in the Department of Health and Human Services (HHS). In 2002, Richard Carmona, who began his education with an associate’s degree in nursing from the Bronx Community College in New York, was appointed surgeon general by President George W. Bush. Shirley Chater led the reorganization of the Social Security Administration in the 1990s. Carolyne Davis served as head of the Health Care Finance Administration (predecessor of the Centers for Medicare and Medicaid Services) in the 1980s during the implementation of a new coding system that classifies hospital cases into diagnosis-related groups. From 1979 to 1981, Rhetaugh Dumas was the first nurse, the first woman, and the first African American to serve as a deputy director of the National Institute of Mental Health (Sullivan, 2007). Nurses also have served as regional directors of HHS and as senior advisors on health policy to HHS.
As for elected office, there were three nurse members of the 111th Congress—Eddie Bernice Johnson (D-TX), Lois Capps (D-CA), and Carolyn McCarthy (D-NY)—all of whom had a hand in sponsoring and supporting health care–focused legislation, from AIDS research to gun control. Lois Capps organized and co-chairs the Congressional Nursing Caucus (which also includes members who are not nurses). The group focuses on mobilizing congressional support for health-related issues. Additionally, 105 nurses have served in state legislatures, including Paula Hollinger of Maryland, who sponsored one of the nation’s first stem cell research bills. None of these nurses waited to be asked; they pursued their positions, both elected and appointed, because they knew they had the expertise and experience to make changes in health care.
Very little in politics is accomplished without preparation or allies. Health professionals point with pride to multiple aspects of the Prescription for Pennsylvania initiative, a state health care reform initiative that preceded the ACA and is also described in Box 5-6. As is clear from a detailed 2009 review, success was not achieved overnight; smaller legislative and regulatory victories set the stage
|
BOX 5-6 Case Study: Prescription for Pennsylvania A Governor’s Leadership Improves Access to Care for Residents of a Rural State When Pennsylvania Governor Edward Rendell took office in 2003, one-twelfth of the state’s 12 million residents had no access to health care, 80 percent of health care expenditures went to treating chronic illnesses, and $3 billion was spent annually on avoidable hospitalizations of chronically ill patients. Pennsylvanians were 11 percent more likely than all other Americans to use the emergency room (ER).
On his first day in office, Governor Rendell established the Office of Health Care Reform to begin to address residents’ access to affordable, high-quality health care. In January 2007 he announced a major new blueprint for that reform, Prescription for Pennsylvania (known as Rx for PA, www.rxforpa.com), which would promote access to care for all Pennsylvanians and reduce the state’s skyrocketing health care expenses. In the 3-plus years since, many initiatives have been undertaken, including
|
|
This last strategy has had an impact on access to care, particularly for the uninsured and underinsured. There are now 51 retail clinics that use APRNs in urban, suburban, and rural areas, and they provide care to 60 percent of the state’s uninsured, said Ann S. Torregrossa, Esq., who in 2005 was named deputy director and in 2009 director of the Office of Health Care Reform. Ms. Torregrossa said that of 300,000 visits to such clinics, about half would have been ER visits. Retail clinics have been shown to reduce costs and improve access to care (Mehrotra et al., 2009). Other outcome data after the first year of Rx for PA show an increase in the number of people with diabetes receiving eye and foot examinations and a doubling of the number of children with asthma who have a plan in place for controlling exacerbations (Pennsylvania Governor’s Office, 2009). There are about 250 nurse-managed health centers nationwide and 27 in Pennsylvania; many are affiliated with schools of nursing and provide care at a 10 percent lower cost than other models—including a 15 percent reduction in ER use and a 25 percent reduction in prescription drug costs (according to unpublished data from the National Nursing Centers Consortium [NNCC]). Tine Hansen-Turton, MGA, JD, CEO of the NNCC and vice president of the Public Health Management Corporation, a nonprofit institute, said that nurses involved in Rx for PA have a great deal to teach clinicians and leaders in other states as they grapple with health care reform (Hansen-Turton et al., 2009). The nurse-managed health centers in particular offer a preventive care model that improves access to care. And Pennsylvanians have given high marks to the care they have received from APRNs, Ms. Hansen-Turton said, adding, “It’s all about access.”  Governor Edward Rendell speaks about the important role of nurses in improving access to health care in Pennsylvania. |
starting in the late 1990s. Even some apparent legislative failures built the foundation for future successes because they caused nurses to spend more time meeting face to face with physicians who had organized opposition to various measures. As a result, nursing leaders developed a better sense of where they could achieve compromises with their opponents. They also found a new ally in the Chamber of Commerce to counter opposition from some sections of organized medicine (Hansen-Turton et al., 2009).
Hansen-Turton and colleagues draw three major lessons from this experience. First, nurses must build strong alliances within their own professional community, an important lesson alluded to earlier in this chapter. Pennsylvania’s nurses were able to speak with a unified voice because they first worked out among themselves which issues mattered most to them. Second, nurses must build relationships with key policy makers. Pennsylvania’s nurses developed strong relationships with several legislators from both major political parties and earned the support of two successive sitting governors: Thomas Ridge (Republican) and Edward Rendell (Democrat). Third, nurses must find allies outside the nursing profession, particularly in business and other influential communities. Pennsylvania’s nurses gained a strong ally in the Chamber of Commerce when they were able to demonstrate how expanding regulations to allow nurses to do all they were educated and demonstrably capable of doing would help lower health care costs (Hansen-Turton et al., 2009).
Perhaps the most important lesson to draw from the Pennsylvania experience lies in the way the campaign was framed. The focus of attention was on achieving quality care and cost reductions. A closer examination of the issues showed that achieving those goals required, among other things, expanding the roles and responsibilities of nurses. What drew the greatest amount of political support for the Prescription for Pennsylvania campaign was the shared goal of getting more value out of the health care system—quality care at a sustainable price. The fact that the campaign also expanded nursing practice was secondary. Those expansions are likely to continue as long as the emphasis is on quality care and cost reduction. Similarly, the committee believes that the goal in any transformation of the health care system should be achieving innovative, patient-centered, highvalue care. If all stakeholders—from legislators, to regulators, to hospital executives, to insurance companies—act from a patient-centered point of reference, they will see that many of the solutions they are seeking require a transformation of the nursing profession.
A CALL FOR NEW PARTNERSHIPS
Having enough nurses and having nurses with the right skills and competencies to care for the population is an important societal issue. Having allies
from outside the profession is important to achieving this goal. More nurses need to reach out to new partners in arenas ranging from business, government, and philanthropy to state and national medical associations to consumer groups. Additionally, nurses need to fortify alliances that are made through personal connections and relationships. Just as important, society needs to understand its stake in ensuring that nurses are effective full partners and leaders in the quest to deliver quality, high-value care that is accessible to diverse populations. The full potential of the nursing profession in care, leadership, and research must be tapped to deal with the wide range of health care challenges the nation will face in the coming years.
Eventually, to transform the way health care is delivered in the United States, nurses will have to move not just out of the hospital, but also out of health care organizations entirely. For example, nurses are underrepresented on the boards of private nonprofit and philanthropic organizations, which do not provide health care services but often have a large impact on health care decisions. The Commonwealth Fund and the Kaiser Family Foundation, for instance, have no nurses on their boards, although they do have physicians. Without nurses, vital ground-level perspectives on quality improvement, care coordination, and health promotion are likely missing. On the other hand, AARP provides a positive example. At least two nurses at AARP have served in the top leadership and governance roles (president and chair) in the past 3 years. Nurses serve on the health and long-term services policy committee, and the senior vice president of the Public Policy Institute is also a nurse. AARP’s commitment to nursing is clear through its sponsorship, along with the Robert Wood Johnson Foundation, of the Center to Champion Nursing.
CONCLUSION
Enactment of the ACA will provide unprecedented opportunities for change in the U.S. health care system for the foreseeable future. Strong leadership on the part of nurses, physicians, and others will be required to devise and implement the changes necessary to increase quality, access, and value and deliver patient-centered care. If these efforts are to be successful, all nurses, from students, to bedside and community nurses, to CNOs and members of nursing organizations, to researchers, must develop leadership competencies and serve as full partners with physicians and other health professionals in efforts to improve the health care system and the delivery of care. Nurses must exercise these competencies in a collaborative environment in all settings, including hospitals, communities, schools, boards, and political and business arenas. In doing so, they must not only mentor others along the way, but develop partnerships and gain allies both within and beyond the health care environment.
REFERENCES
AACN (American Association of Colleges of Nursing). 2008. The essentials of baccalaureate education for professional nursing practice. Washington, DC: AACN. Available from http://www.aacn.nche.edu/education/pdf/BaccEssentials08.pdf.
AACN. 2010. Enhancing diversity in the nursing workforce: Fact sheet updated March 2010. http://www.aacn.nche.edu/Media/FactSheets/diversity.htm (accessed July 1, 2010).
ANCC (American Nurses Credentialing Center). 2010. Program overview. http://www.nursecredentialing.org/Magnet/ProgramOverview.aspx (accessed August 25, 2010).
Ballein Search Partners and AONE (American Organization of Nurse Executives). 2003. Why senior nursing officers matter: A national survey of nursing executives. Oak Brook, IL: Ballein Search Partners.
Bennis, W., and B. Nanus. 2003. Leaders: Strategies for taking charge. New York: HarperCollins.
Beverly, C. J., R. E. McAtee, R. Chernoff, G. V. Davis, S. K. Jones, and D. A. Lipschitz. 2007. The Arkansas aging initiative: An innovative approach for addressing the health of older rural Arkansans. Gerontologist 47(2):235-243.
Bradford, D. L., and A. R. Cohen. 1998. Power up: Transforming organizations through shared leadership. Hoboken, NJ: John Wiley & Sons, Inc.
Center for Healthcare Governance. 2007. A seat at the power table: The physician’s role on the hospital board. Chicago, IL: Center for Healthcare Governance.
Curran, C. R., and M. K. Totten. 2010. Expanding the role of nursing in health care governance. Nursing Economic$ 28(1):44-46.
Evans, L. K., and N. E. Strumpf. 1989. Tying down the elderly. A review of the literature on physical restraint. Journal of the American Geriatrics Society 37(1):65-74.
Gardner, D. B. 2005. Ten lessons in collaboration. OJIN: Online Journal of Issues in Nursing 10(1):2.
George Washington University Medical Center. 2010. NAQC: Nursing alliance for quality care. http://www.gwumc.edu/healthsci/departments/nursing/naqc/ (accessed August 25, 2010).
Governance Institute. 2007. Boards x 4: Governance structures and practices. San Diego, CA: Governance Institute.
Hall-Long, B. 2009. Nursing and public policy: A tool for excellence in education, practice, and research. Nursing Outlook 57(2):78-83.
Hansen-Turton, T., A. Ritter, and B. Valdez. 2009. Developing alliances: How advanced practice nurses became part of the prescription for Pennsylvania. Policy, Politics, & Nursing Practice 10(1):7-15.
Hassmiller, S. B., and L. B. Bolton (eds.). 2009. Transforming care at the bedside: Paving the way for change. American Journal of Nursing 109(11):3-80.
HealthSTAT. 2010. About us. http://www.healthstatgeorgia.org/?q=content/about (accessed June 29, 2010).
IOM (Institute of Medicine). 2000. To err is human: Building a safer health system. Washington, DC: National Academy Press.
IOM. 2004. In the nation’s compelling interest: Ensuring diversity in the health care workforce. Washington, DC: The National Academies Press.
IOM. 2010. A summary of the December 2009 Forum on the Future of Nursing: Care in the community. Washington, DC: The National Academies Press.
Janetti, A. 2003. NSNA leadership university: A practicum in shared governance. DEAN’S Notes 25(1).
Jiang, H. J., C. Lockee, K. Bass, and I. Fraser. 2008. Board engagement in quality: Findings of a survey of hospital and system leaders. Journal of Healthcare Management 53(2):121-134; discussion 135.
Joint Commission. 2008. Behaviors that undermine a culture of safety. Sentinel Event Alert (40).
Jones, C. B., D. S. Havens, and P. A. Thompson. 2008. Chief nursing officer retention and turnover: A crisis brewing? Results of a national survey. Journal of Healthcare Management 53(2):89-105; discussion 105-106.
Katzenbach, J. R., and D. K. Smith. 1993. The wisdom of teams: Creating the high-performance organization. Boston, MA: Harvard Business School Press.
King, S. 2009. Channeling grief into action: Creating a culture of safety conference call, February 25, 2009, Hosted by Institute for Healthcare Improvement.
Kinnaman, M. L., and M. R. Bleich. 2004. Collaboration: Aligning resources to create and sustain partnerships. Journal of Professional Nursing 20(5):310-322.
Mastal, M. F., M. Joshi, and K. Schulke. 2007. Nursing leadership: Championing quality and patient safety in the boardroom. Nursing Economic$ 25(6):323-330.
Mehrotra, A., H. Liu, J. L. Adams, M. C. Wang, J. R. Lave, N. M. Thygeson, L. I. Solberg, and E. A. McGlynn. 2009. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Annals of Internal Medicine 151(5):321-328.
Olender-Russo, L. 2009. Creating a culture of regard: An antidote for workplace bullying. Creative Nursing 15(2):75-81.
Paulus, P., and B. Nijstad, eds. 2003. Group creativity: Innovation through collaboration. New York: Oxford University Press.
Pearson, A., H. Laschinger, K. Porritt, Z. Jordan, D. Tucker, and L. Long. 2007. Comprehensive systematic review of evidence on developing and sustaining nursing leadership that fosters a healthy work environment in healthcare. International Journal of Evidence-Based Healthcare 5:208-253.
Pennsylvania Governor’s Office. 2009. Governor Rendell thanks “pioneers” for making Pennsylvania the national leader on chronic care management and creating patient-centered medical homes. http://www.portal.state.pa.us/portal/server.pt?open=512&objID=3053&PageID=431159&mode=2&contentid=http://pubcontent.state.pa.us/publishedcontent/publish/global/news_releases/governor_s_office/news_releases/governor_rendell_thanks__pioneers__for_making_pennsylvania_the_national_leader_on_chronic_care_management_and_creating_patient_centered_medical_homes.html (accessed July 1, 2010).
Pisano, G. P., and R. Verganti. 2008. Which kind of collaboration is right for you? Harvard Business Review 86(12):78-86.
Prybil, L., S. Levey, R. Peterson, D. Heinrich, P. Brezinski, G. Zamba, A. Amendola, J. Price, and W. Roach. 2009. Governance in high-performing community health systems: A report on trustee and CEO views. Chicago, IL: Grant Thornton LLP.
Quisling, K. E. 2009. Resident orientation: Nurses create a program to improve care coordination. American Journal of Nursing 109(11 Suppl):26-28.
Rosenstein, A. H., and M. O’Daniel. 2008. A survey of the impact of disruptive behaviors and communication defects on patient safety. Joint Commission Journal on Quality and Patient Safety 34(8):464-471.
RWJF (Robert Wood Johnson Foundation). 2010a. Nursing leadership from bedside to boardroom: Opinion leaders’ perceptions. http://www.rwjf.org/pr/product.jsp?id=54350 (accessed May 14, 2010).
RWJF. 2010b. Nursing leadership from bedside to boardroom: Opinion leaders’ views. http://www.rwjf.org/pr/product.jsp?id=54491 (accessed August 25, 2010).
RWJF. 2010c. Unlocking the potential of school nursing: Keeping children healthy, in school, and ready to learn. Charting Nursing’s Future July(14):1-8.
RWJF Executive Nurse Fellows. 2010. Overview. http://www.executivenursefellows.org/index.php?option=com_content&view=article&id=1&Itemid=34 (accessed September 28, 2010).
RWJF Scholars, Fellows & Leadership Programs. 2010. Robert Wood Johnson Foundation Health Policy Fellows. http://www.rwjfleaders.org/programs/robert-wood-johnson-foundation-healthpolicy-fellow (accessed September 28, 2010).
Shea, G. 2005. Developing the strategic voice of senior nurse executives. Nursing Administration Quarterly 29(2):133-136.
Singh, J., and L. Fleming. 2010. Lone inventors as sources of breakthroughs: Myth or reality? Management Science 56(1):41-56.
Strumpf, N. E., and L. K. Evans. 1988. Physical restraint of the hospitalized elderly: Perceptions of patients and nurses. Nursing Research 37(3):132-137.
Sullivan, P. 2007. Rhetaugh Dumas, 78; nurse rose to become NIMH deputy director. The Washington Post, July 27.
Wachter, R. M. 2009. Patient safety at ten: Unmistakable progress, troubling gaps. Health Affairs 29(1):165-173.
Wuchty, S., B. Jones, and B. Uzzi. 2007. The increasing dominance of teams in production of knowledge. Science 316(5827):1036-1039.


































