1
Key Messages of the Report
The U.S. health care system is characterized by a high degree of fragmentation across many sectors, which raises substantial barriers to providing accessible, quality care at an affordable price. In part, the fragmentation in the system comes from disconnects between public and private services, between providers and patients, between what patients need and how providers are trained, between the health needs of the nation and the services that are offered, and between those with insurance and those without (Stevens, 1999). Communication between providers is difficult, and much care is redundant because there is no way of sharing results.
This report is being published at an opportune time. In 2010, Congress passed and the President signed into law comprehensive health care legislation. These laws, the Patient Protection and Affordable Care Act (Public Law 111-148) and the Health Care and Education Affordability Reconciliation Act (Public Law 111-152), are collectively referred to throughout this report as the Affordable Care Act (ACA). The ACA represents the broadest changes to the health care system since the 1965 creation of the Medicare and Medicaid programs and is expected to provide insurance coverage for an additional 32 million previously uninsured Americans. The need to improve the health care system is becoming increasingly evident as challenges related to both the quality and costs of care persist.
As discussed in the preface, this study was undertaken to explore how the nursing profession can be transformed to help exploit these opportunities and contribute to building a health care system that will meet the demand for safe, quality, patient-centered, accessible, and affordable care. This chapter presents the key messages that emerged from the study committee’s deliberations. It begins by describing a vision for a transformed system that can meet the health
needs of the U.S. population in the 21st century. The chapter then delineates the roles of nurses in realizing this vision. The third section explains why a fundamental transformation of the nursing profession will be required if nurses are to assume these roles. The final section presents conclusions.
A VISION FOR HEALTH CARE
During the course of its work, the Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine developed a vision for a transformed health care system, while recognizing the demands and limitations of the current health care system outlined above. The committee envisions a future system that makes quality care accessible to the diverse populations of the United States, intentionally promotes wellness and disease prevention, reliably improves health outcomes, and provides compassionate care across the lifespan. In this envisioned future, primary care and prevention are central drivers of the health care system. Interprofessional collaboration and coordination are the norm. Payment for health care services rewards value, not volume of services, and quality care is provided at a price that is affordable for both individuals and society. The rate of growth of health care expenditures slows. In all these areas, the health care system consistently demonstrates that it is responsive to individuals’ needs and desires through the delivery of truly patient-centered care. Annex 1-1 lists the committee’s definitions for three core terms related to its vision: health, health care, and the health care system.
THE ROLE OF NURSES IN REALIZING THIS VISION
The ACA provides a call to action for nurses, and several sections of the legislation are directly relevant to their work.1 For example, sections 5501 through 5509 are aimed at substantially strengthening the provision of primary care—a need generally recognized by health professionals and policy experts; section 2717 calls for “ensuring the quality of care”; and section 2718 emphasizes “bringing down the cost of health care coverage.” Enactment of the ACA offers a myriad of opportunities for the nursing profession to facilitate improvements to the health care system and the mechanisms by which care is delivered across various settings. Systemwide changes are needed that capture the full economic value of nurses and take into account the growing body of evidence that links nursing practice to improvements in the safety and quality of care. Advanced practice registered nurses (APRNs) should be called upon to fulfill and expand their potential as primary care providers across practice settings based on their
|
1 |
For a list of nursing-related provisions included in the ACA, see http://championnursing.org/sites/default/files/nursingandhealthreformlawable.pdf. |
education and competency. Nursing initiatives and programs should be scaled up to help bridge the gap between insurance coverage and access to care.
The nursing profession has the potential capacity to implement wide-reaching changes in the health care system. With more than 3 million members, the profession has nearly doubled since 1980 and represents the largest segment of the U.S. health care workforce (HRSA, 2010; U.S. Census Bureau, 2009). By virtue of their regular, close proximity to patients and their scientific understanding of care processes across the continuum of care, nurses have a considerable opportunity to act as full partners with other health professionals and to lead in the improvement and redesign of the health care system and its practice environment.
Nurses practice in many settings, including hospitals, schools, homes, retail health clinics, long-term care facilities, battlefields, and community and public health centers. They have varying levels of education and competencies—from licensed practical nurses, who greatly contribute to direct patient care in nursing homes, to nurse scientists, who research and evaluate more effective ways of caring for patients and promoting health. As described in Annex 1-1 at the end of this chapter, most nurses are registered nurses (RNs), who “complete a program of study at a community college, diploma school of nursing, or a four-year college or university and are required to pass a nationally standardized licensing exam in the state in which they begin practice” (AARP, 2010). Figure 1-1 shows that of the many settings where RNs practice, the majority practice in hospitals; Figure 1-2 shows the employment settings of nurses by highest nursing or nursing-related education. More than a quarter of a million nurses are APRNs (HRSA, 2010), who hold master’s or doctoral degrees and pass national certification exams. APRNs deliver primary and other types of health care services. For example, they teach and counsel patients to understand their health problems and what they can do to get better, they coordinate care and advocate for patients in the complex health care system, and they refer patients to physicians and other health care providers. APRNs include nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, and certified nurse midwives (see Table 1-1). Annex 1-1 provides more detailed descriptions of the preparation and roles of nurses, pathways in nursing education, and numbers of nurses.
Nursing practice covers a broad continuum from health promotion, to disease prevention, to coordination of care, to cure—when possible—and to palliative care when cure is not possible. This continuum of practice is well matched to the current and future needs of the American population (see Chapter 2). Nurses have a direct effect on patient care. They provide the majority of patient assessments, evaluations, and care in hospitals, nursing homes, clinics, schools, workplaces, and ambulatory settings. They are at the front lines in ensuring that care is delivered safely, effectively, and compassionately. Additionally, nurses attend to patients and their families in a holistic way that often goes beyond physical health needs to recognize and respond to social, mental, and spiritual needs. Given their education, experience, and unique perspectives and the centrality of their role in
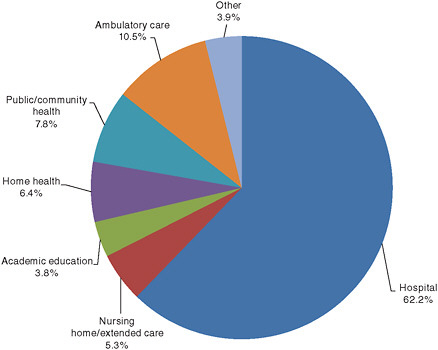
FIGURE 1-1 Employment settings of registered nurses.
NOTES: The totals may not add to 100 percent because of the effect of rounding. Only RNs for whom information on setting was available are included in the calculations used for this chart. Public/community health includes school and occupational health. Ambulatory care includes medical/physician practices, health centers and clinics, and other types of nonhospital clinical settings. Other includes insurance, benefits, and utilization review.
SOURCE: HRSA, 2010.
providing care, nurses will play a significant role in the transformation of the health care system. Likewise, while changes in the health care system will have profound effects on all providers, this will be undoubtedly true for nurses.
Traditional nursing competencies such as care management and coordination, patient education, public health intervention, and transitional care are likely to dominate in a reformed health care system as it inevitably moves toward an emphasis on prevention and management rather than acute care (O’Neil, 2009). Nurses have also begun developing new competencies for the future to help bridge the gap between coverage and access, to coordinate increasingly complex care for a wide range of patients, to fulfill their potential as primary care providers to the full extent of their education and training, to implement systemwide changes that take into account the growing body of evidence linking nursing practice to
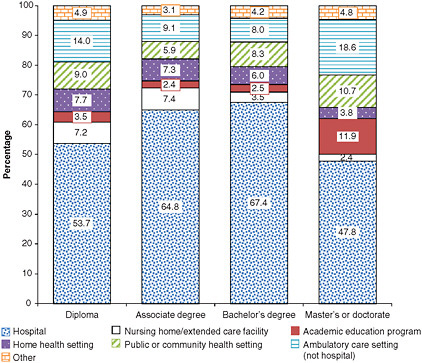
FIGURE 1-2 Employment settings of RNs, by highest nursing or nursing-related education.
NOTES: The total percent by setting may not equal the estimated total of all registered nurses due to incomplete information provided by respondents and the effect of rounding.
SOURCE: HRSA, 2010.
fundamental improvements in the safety and quality of care, and to capture the full economic value of their contributions across practice settings.
At the same time, the nursing profession has its challenges. While there are concerns regarding the number of nurses available to meet the demands of the health care system and the needs of patients, and there is reason to view as a priority replacing at least 900,000 nurses over the age of 50 (BLS, 2009), the composition of the workforce is turning out to be an even greater challenge for the future of the profession. The workforce is generally not as diverse as it needs to be—with respect to race and ethnicity (just 16.8 percent of the workforce is non-white), gender (approximately 7 percent of employed nurses are male), or age (the median age of nurses is 46, compared to 38 in 1988)—to provide culturally relevant care to all populations (HRSA, 2010). Many members of the profession lack the education and preparation necessary to adapt to new roles quickly in response to rapidly changing health care settings and an evolving health care sys-
TABLE 1-1 Types of Advanced Practice Registered Nurses (APRNs)
|
Who Are They? |
How Many in United States? |
What Do They Do? |
|
Nurse Practitioners (NPs) |
153,348 |
Take health histories and provide complete physical exams; diagnose and treat acute and chronic illnesses; provide immunizations; prescribe and manage medications and other therapies; order and interpret lab tests and x-rays; provide health teaching and supportive counseling. |
|
Clinical Nurse Specialists (CNSs) |
59,242* |
Provide advanced nursing care in hospitals and other clinical sites; provide acute and chronic care management; develop quality improvement programs; serve as mentors, educators, researchers, and consultants. |
|
Certified Registered Nurse Anesthetists (CRNAs) |
34,821 |
Administer anesthesia and provide related care before and after surgical, therapeutic, diagnostic, and obstetrical procedures, as well as pain management. Settings include operating rooms, outpatient surgical centers, and dental offices. CRNAs deliver more than 65% of all anesthetics to patients in the United States. |
|
Certified Nurse Midwives (CNMs) |
18,492 |
Provide primary care to women, including gynecological exams, family planning advice, prenatal care, management of low-risk labor and delivery, and neonatal care. Practice settings include hospitals, birthing centers, community clinics, and patient homes. |
|
*APRNs are identified by their responses to the National Sample Survey of Registered Nurses, and this number may not reflect the true population of CNSs. SOURCE: AARP, 2010. Courtesy of AARP. All rights reserved. |
||
tem. Restrictions on scope of practice and professional tensions have undermined the nursing profession’s ability to provide and improve both general and advanced care. Producing a health care system that delivers the right care—quality care that is patient centered, accessible, evidence based, and sustainable—at the right time will require transforming the work environment, scope of practice, education, and numbers and composition of America’s nurses. The remainder of this section examines the role of the nursing profession in health care reform according to the same three parameters by which all other health care reform initiatives are evaluated—quality, access, and value.
Nurses and Quality
Although it is difficult to prove causation, an emerging body of literature suggests that quality of care depends to a large degree on nurses (Kane et al., 2007; Lacey and Cox, 2009; Landon et al., 2006; Sales et al., 2008). The Joint Commission, the leading independent accrediting body for health care organizations, believes that “the future state of nursing is inextricably linked to the strides
in patient care quality and safety that are critical to the success of America’s health care system, today and tomorrow” (Joint Commission, 2010). While quality measures have historically focused on conditions or diseases, many of the quality measures used over the past few years address how well nurses are able to do their jobs (Kurtzman and Buerhaus, 2008).
In 2004, the National Quality Forum (NQF) endorsed the first set of nationally standardized performance measures, the National Voluntary Consensus Standards for Nursing-Sensitive Care, initially designed to assess the quality of care provided by nurses who work in hospitals (National Quality Forum, 2004). The NQF measures include prevalence of pressure ulcers and falls; nursing-centered interventions, such as smoking cessation counseling; and system-centered measures, such as voluntary turnover and nursing care hours per patient day. These measures have helped nurses and the organizations where they work identify targets for improvements in care delivery.
Another important vehicle for tracking and improving quality is the National Database of Nursing Quality Indicators, the nation’s largest nursing registry. This database, which meets the new reporting requirement by the Centers for Medicare and Medicaid Services for nursing-sensitive care, is supported by the American Nurses Association.2 More than 25 percent of hospitals participate in the database, which documents more than 21 measures of hospital performance linked to the availability and quality of nursing services in acute care settings. Participating facilities are able to obtain unit-level comparative data, including patient and staffing outcomes, to use for quality improvement purposes. Comparison data are publicly reported, which provides an incentive to improve the quality of care on a continuous basis. This database is now maintained at the University of Kansas School of Nursing and is available to researchers interested in improving health care quality.
Nurses and Access
Evidence suggests that access to quality care can be greatly expanded by increasing the use of RNs and APRNs in primary, chronic, and transitional care (Bodenheimer et al., 2005; Craven and Ober, 2009; Naylor et al., 2004; Rendell, 2007). For example, nurses serving in special roles created to increase access to care, such as care coordinators and primary care clinicians, have led to significant reductions in hospitalization and rehospitalization rates for elderly patients (Kane et al., 2003; Naylor et al., 2004). It stands to reason that one way to improve access to patient-centered care would be to allow nurses to make more care decisions at the point of care. Yet in many cases, outdated regulations, biases, and policies prevent nurses, particularly APRNs, from practicing to the full extent
of their education, skills, and competencies (Hansen-Turton et al., 2008; Ritter and Hansen-Turton, 2008; Safriet, 2010). Chapter 3 examines these barriers in greater depth.
Nurses also make significant contributions to access by delivering care where people live, work, and play. Examples include school nurses, occupational health nurses, public health nurses, and those working at so-called retail clinics in busy shopping centers. Nurses also work in migrant health clinics and nurse-managed health centers, organizations known for serving the most underserved populations. Additionally, nurses are often at the front lines serving as primary providers for individuals and families affected by natural or man-made disasters, delivering care in homes and designated community shelters.
Nurses and Value
“Value in health care is expressed as the physical health and sense of well-being achieved relative to the cost” (IOM Roundtable on Evidence-Based Medicine, 2008). Compared with support for the role of nurses in improving quality and access, there is somewhat less evidence that expanding the care provided by nurses will result in cost savings to society at large while also improving outcomes and ensuring quality. However, the evidence base in favor of such a conclusion is growing. Compared with other models of prenatal care, for example, pregnant women who receive care led by certified nurse midwives are less likely to experience antenatal hospitalization, and their babies are more likely to have a shorter hospital stay (Hatem et al., 2008) (see Chapter 2 for a case study of care provided by certified nurse midwives at the Family Health and Birth Center in Washington, DC). Another study examining the impact of nurse staffing on value suggests that increasing the proportion of nursing hours provided by RNs without increasing total nursing hours was associated with 1.5 million fewer hospital days, nearly 60,000 fewer inpatient complications, and a 0.5 percent net reduction in costs (Needleman et al., 2006). Chapter 2 includes a case study of the Nurse–Family Partnership Program, in which front-line RNs make home visits to high-risk young mothers over a 2.5-year period. This program has demonstrated significant value, resulting in a net savings of $34,148 per family served. The program has also reduced pregnancy-induced hypertension by 32 percent, child abuse and neglect by 50 percent, emergency room visits by 35 percent, and language-related delays by 50 percent (AAN, 2010).
THE NEED FOR A FUNDAMENTAL TRANSFORMATION OF THE NURSING PROFESSION
Given the crucial role of nurses with respect to the quality, accessibility, and value of care, the nursing profession itself must undergo a fundamental transformation if the committee’s vision for health care is to be realized. As this report
argues, the ways in which nurses were educated and practiced during the 20th century are no longer adequate for dealing with the realities of health care in the 21st century. Outdated regulations, attitudes, policies, and habits continue to restrict the innovations the nursing profession can bring to health care at a time of tremendous complexity and change.
In the course of its deliberations, the committee formulated four key messages that inform the discussion in Chapters 3–6 and structure its recommendations for transforming the nursing profession:
-
Nurses should practice to the full extent of their education and training.
-
Nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression.
-
Nurses should be full partners, with physicians and other health professionals, in redesigning health care in the United States.
-
Effective workforce planning and policy making require better data collection and an improved information infrastructure.
These key messages speak to the need to transform the nursing profession in three crucial areas—practice, education, and leadership—as well as to collect better data on the health care workforce to inform planning for the necessary changes to the nursing profession and the overall health care system.
The Need to Transform Practice
Key Message #1: Nurses should practice to the full extent of their education and training.
To ensure that all Americans have access to needed health care services and that nurses’ unique contributions to the health care team are maximized, federal and state actions are required to update and standardize scope-of-practice regulations to take advantage of the full capacity and education of APRNs. States and insurance companies must follow through with specific regulatory, policy, and financial changes that give patients the freedom to choose from a range of providers, including APRNs, to best meet their health needs. Removing regulatory, policy, and financial barriers to promote patient choice and patient-centered care should be foundational in the building of a reformed health care system.
Additionally, to the extent that the nursing profession envisions its future as confined to acute care settings, such as inpatient hospitals, its ability to help shape the future U.S. health care system will be greatly limited. As noted earlier, care in the future is likely to shift from the hospital to the community setting (O’Neil, 2009). Yet the majority of nurses still work in acute care settings; according to
recent findings from the 2008 National Sample Survey of Registered Nurses, just over 62 percent of working RNs were employed in hospitals in 2008—up from approximately 57 percent in 2004 (HRSA, 2010). Nurses must create, serve in, and disseminate reconceptualized roles to bridge whatever gaps remain between coverage and access to care. More must become health coaches, care coordinators, informaticians, primary care providers, and health team leaders in a greater variety of settings, including primary care medical homes and accountable care organizations. In some respects, such a transformation would return the nursing profession to its roots in the public health movement of the early 20th century.
At the same time, new systems and technologies appear to be pushing nurses ever farther away from patients. This appears to be especially true in the acute care setting. Studies show that nurses on medical–surgical units spend only 31 to 44 percent of their time in direct patient activities (Tucker and Spear, 2006). A separate study of medical–surgical nurses found they walked nearly a mile longer while on than off duty in obtaining the supplies and equipment needed to perform their tasks. In general, less than 20 percent of nursing practice time was devoted specifically to patient care activities, the majority being consumed by documentation, medication administration, and communication regarding the patient (Hendrich et al., 2008). Several health care organizations, professional organizations, and consumer groups have endorsed a Proclamation for Change aimed at redressing inefficiencies in hospital design, organization, and technology infrastructure through a focus on patient-centered design; the implementation of systemwide, integrated technology; the creation of seamless workplace environments; and the promotion of vendor partnerships (Hendrich et al., 2009). Realizing the vision presented earlier in this chapter will require a practice environment that is fundamentally transformed so that nurses are efficiently employed—whether in the hospital or in the community—to the full extent of their education, skills, and competencies.
Chapter 3 examines these issues in greater depth.
The Need to Transform Education
Key Message #2: Nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression.
Major changes in the U.S. health care system and practice environment will require equally profound changes in the education of nurses both before and after they receive their licenses. An improved education system is necessary to ensure that the current and future generations of nurses can deliver safe, quality, patient-centered care across all settings, especially in such areas as primary care and community and public health.
Interest in the nursing profession has grown rapidly in recent years, in part as
a result of the economic downturn and the relative stability the health care sector offers. The number of applications to entry-level baccalaureate programs increased by more than 70 percent in just 5 years—from 122,000 applications in 2004 to 208,000 applications in 2009 (AACN, 2010). While nursing schools across the country have responded to this influx of interest, there are constraints, such as insufficient numbers of nurse faculty and clinical placements, that limit the capacity of nursing schools to accommodate all the qualified applicants. Thus, thousands of qualified students are turned away each year (Kovner and Djukic, 2009).
A variety of challenges limit the ability to ensure a well-educated nurse workforce. As noted, there is a shortage of faculty to teach nurses at all levels (Allan and Aldebron, 2008). Also, the ways in which nurses during the 20th century taught each other to care for people and learned to practice and make clinical decisions are no longer adequate for delivering care in the 21st century. Many nursing schools have dealt with the explosion of research and knowledge needed to provide health care in an increasingly complex system by adding layers of content that requires more instruction (Ironside, 2004). A fundamental rethinking of this approach is needed (Benner et al., 2009; Erickson, 2002; IOM, 2003, 2009; Lasater and Nielsen, 2009; Mitchell et al., 2006; Orsolini-Hain and Waters, 2009; Tanner et al., 2008). Additionally, nurses at all levels have few incentives to pursue further education, and face active disincentives to advanced education. Nurses and physicians—not to mention pharmacists and social workers—typically are not educated together, yet they are increasingly required to cooperate and collaborate more closely in the delivery of care.
The education system should provide nurses with the tools needed to evaluate and improve standards of patient care and the quality and safety of care while preserving fundamental elements of nursing education, such as ethics and integrity and holistic, compassionate approaches to care. The system should ensure nurses’ ability to adapt and be flexible in response to changes in science, technology, and population demographics that shape the delivery of care. Nursing education at all levels needs to impart a better understanding of ways to work in the context of and lead change within health care delivery systems, methods for quality improvement and system redesign, methods for designing effective care delivery models and reducing patient risk, and care management and other roles involving expanded authority and responsibility. The nursing profession must adopt a framework of continuous, lifelong learning that includes basic education, residency programs, and continuing competence. More nurses must receive a solid education in how to manage complex conditions and coordinate care with multiple health professionals. They must demonstrate new competencies in systems thinking, quality improvement, and care management and a basic understanding of health policy and research. Graduate-level nurses must develop even greater competencies and deeper understanding in all of these areas. Innovative new programs to attract nurse faculty and provide a wider range of clinical education placements must clear long-standing bottlenecks in
nursing education. Accrediting and certifying organizations must mandate demonstrated mastery of clinical skills, managerial competencies, and professional development at all levels to complement the completion of degree programs and written board examinations. Milestones for mandated skills, competencies, and professional development must be updated more frequently to keep pace with the rapidly changing demands of health care. And all health professionals should receive more of their education in concert with students from other disciplines. Interprofessional team training of nurses, physicians, and other health care providers should begin when they are students and proceed throughout their careers. Successful interprofessional education can be achieved only through committed partnerships across professions.
Nurses should move seamlessly through the education system to higher levels of education, including graduate degrees. Nurses with graduate degrees will be able to replenish the nurse faculty pool; advance nursing science and contribute to the knowledge base on how nurses can provide up-to-date, safe patient care; participate in health care decisions; and provide the leadership needed to establish nurses as full partners in health care redesign efforts (see the section on leadership below).
The Need to Transform Leadership
Key Message #3: Nurses should be full partners, with physicians and other health professionals, in redesigning health care in the United States.
Not all nurses begin their career with thoughts of becoming a leader. Yet strong leadership will be required to transform the U.S. health care system. A transformed system will need nurses with the adaptive capacity to take on reconceptualized roles in new settings, educating and reeducating themselves along the way—indispensible characteristics of effective leadership.
Whether on the front lines, in education, or in administrative positions and health policy roles, nurses have the well-grounded knowledge base, experience, and perspective needed to serve as full partners in health care redesign. Nurses’ unique perspectives are derived from their experiences in providing direct, handson patient care; communicating with patients and their families about health status, medications, and care plans; and ensuring the linkage between a prescribed course of treatment and the desired outcome. In care environments, being a full partner involves taking responsibility for identifying problems and areas of waste, devising and implementing a plan for improvement, tracking improvement over time, and making necessary adjustments to realize established goals.
Being a full partner translates more broadly to the health policy arena. To be effective in reconceptualized roles, nurses must see policy as something they can shape rather than something that happens to them. Nurses should have a
voice in health policy decision making, as well as being engaged in implementation efforts related to health care reform. Nurses also should serve actively on advisory committees, commissions, and boards where policy decisions are made to advance health systems to improve patient care. Yet a number of barriers prevent nurses from serving as full partners. Examples that are discussed later in the report include laws and regulations (Chapter 3), professional resistance and bias (Chapter 3), a lack of foundational competence (Chapter 5), and exclusion from decision-making bodies and boards (Chapter 5). If nurses are to serve as full partners, a culture change will be needed whereby health professionals hold each other accountable for improving care and setting health policy in a context of mutual respect and collaboration.
Finally, the health care system is widely understood to be a complex system, one in which responses to internal and external actions are sometimes predictable and sometimes not. Health care experts repeatedly encourage health professionals to understand the system’s dynamics so they can be more effective in their individual jobs and help shape the larger system’s ability to adapt successfully to changes and improve outcomes. In a field as intensively knowledge driven as health care, however, no one individual, group, or discipline can have all the answers. A growing body of research has begun to highlight the potential for collaboration among teams of diverse individuals to generate successful solutions in complex, knowledge-driven systems (Paulus and Nijstad, 2003; Pisano and Verganti, 2008; Singh and Fleming, 2010; Wuchty et al., 2007). Nurses must cultivate new allies in health care, government, and business and develop new partnerships with other clinicians, business owners, and philanthropists to help realize the vision of a transformed health care system. Many nurses have heard this call to develop new partnerships in a culture of collaboration and cooperation. However, the committee found no evidence that these initiatives have achieved the scale necessary to have an impact throughout the health care system. More intentional, large-scale initiatives of this sort are needed. These efforts must be supported by research that addresses such questions as what new models of leadership are needed for the increasingly knowledge-intensive health care environment and when collaboration is most appropriate (Singh and Fleming, 2010).
Chapter 5 further examines the need for expanded leadership opportunities in the nursing workforce.
The Need for Better Data on the Health Care Workforce
Key Message #4: Effective workforce planning and policy making require better data collection and an improved information infrastructure.
Key messages 1, 2, and 3 speak to the need to transform the nursing profession to achieve the vision of health care set forth at the beginning of this chapter.
At the same time, nurses do not function in a vacuum, but in the context of the skills and perspectives of physicians and other health professionals. Planning for the fundamental changes required to achieve a reformed health care system cannot be accomplished without a clear understanding of the necessary contributions of these various professionals and the numbers and composition of the health care workforce. That understanding in turn cannot be obtained without reliable, sufficiently granular data on the current workforce and projections of future workforce needs. Yet major gaps exist in the currently available workforce data. These gaps hamper the ability to identify and implement the necessary changes to the preparation and practice of nurses and to the overall health care system. Chapter 6 explores these issues in greater detail.
CONCLUSION
Most of the near-term challenges identified in the ACA speak to traditional and current strengths of the nursing profession in care coordination, health promotion, and quality improvement, among other things. Nurses are committed to improving the care they deliver by responding to health care challenges. If their full potential is to be realized, however, the nursing profession itself will have to undergo a fundamental transformation in the areas of practice, education, and leadership. During the course of this study, the committee formulated four key messages it believes must guide that transformation: (1) nurses should practice to the full extent of their education and training; (2) nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression; (3) nurses should be full partners, with physicians and other health professionals, in redesigning health care in the United States; and (4) effective workforce planning and policy making require better data collection and an improved information infrastructure.
At the same time, the power to deliver better care—quality care that is accessible and sustainable—does not rest solely with nurses, regardless of how ably led or educated they are; it also lies with other health professionals, consumers, governments, businesses, health care institutions, professional organizations, and the insurance industry. The recommendations presented in Chapter 7 target individual policy makers; national, state, and local government leaders; payers; and health care researchers, executives, and professionals—including nurses and others—as well as larger groups such as licensing bodies, educational institutions, and philanthropic and advocacy and consumer organizations. Together, these groups have the power to transform the health care system to achieve the vision set forth at the beginning of this chapter.
REFERENCES
AACN (American Association of Colleges of Nursing). 2010. Completed applications to entry-level baccalaureate nursing programs in the U.S.: 2004-2009. http://www.aacn.nche.edu/Media/pdf/apps.pdf (accessed September 10, 2010).
AAN (American Academy of Nursing). 2010. Edge Runner directory: Nurse-family partnership. http://www.aannet.org/i4a/pages/index.cfm?pageid=3303 (accessed August 27, 2010).
AARP. 2010. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed August 17, 2010).
Allan, J. D., and J. Aldebron. 2008. A systematic assessment of strategies to address the nursing faculty shortage, U.S. Nursing Outlook 56(6):286-297.
Benner, P., M. Sutphen, V. Leonard, and L. Day. 2009. Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass.
BLS (Bureau of Labor Statistics). 2009. Employment projections: Replacement needs. http://www.bls.gov/emp/ep_table_110.htm (accessed September 10, 2010).
Bodenheimer, T., K. MacGregor, and N. Stothart. 2005. Nurses as leaders in chronic care. BMJ 330(7492):612-613.
Craven, G., and S. Ober. 2009. Massachusetts nurse practitioners step up as one solution to the primary care access problem: A political success story. Policy, Politics, & Nursing Practice 10(2):94-100.
Erickson, H. L. 2002. Concept-based curriculum and instruction: Teaching beyond the facts. Thousand Oaks, CA: Corwin Press.
Hansen-Turton, T., A. Ritter, and R. Torgan. 2008. Insurers’ contracting policies on nurse practitioners as primary care providers: Two years later. Policy, Politics, & Nursing Practice 9(4):241-248.
Hatem, M., J. Sandall, D. Devane, H. Soltani, and S. Gates. 2008. Midwife-led versus other models of care for childbearing women. Cochrane Database of Systematic Reviews (4):CD004667.
Hendrich, A., M. P. Chow, B. A. Skierczynski, and Z. Lu. 2008. A time and motion study: How do medical-surgical nurses spend their time? The Permanente Journal 12(3):37-46.
Hendrich, A., M. P. Chow, and W. S. Goshert. 2009. A proclamation for change: Transforming the hospital patient care environment. Journal of Nursing Administration 39(6):266-275.
HRSA (Health Resources and Services Administration). 2010. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. Rockville, MD: HRSA.
IOM (Institute of Medicine). 2003. Health professions education: A bridge to quality. Washington, DC: The National Academies Press.
IOM. 2009. Redesigning continuing education in the health professions. Washington, DC: The National Academies Press.
IOM Roundtable on Evidence-Based Medicine. 2008. Learning healthcare system concepts, v. 2008. Washington, DC: The National Academies Press.
Ironside, P. M. 2004. “Covering content” and teaching thinking: Deconstructing the additive curriculum. Journal of Nursing Education 43(1):5-12.
Joint Commission. 2010. Testimony submitted to inform the Forum on the Future of Nursing: Education. Houston, TX, February 22.
Kane, R. L., G. Keckhafer, S. Flood, B. Bershadsky, and M. S. Siadaty. 2003. The effect of Evercare on hospital use. Journal of the American Geriatric Society 51(10):1427-1434.
Kane, R. L., T. A. Shamliyan, C. Mueller, S. Duval, and T. J. Wilt. 2007. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med Care 45(12):1195-1204.
Kovner, C. T., and M. Djukic. 2009. The nursing career process from application through the first 2 years of employment. Journal of Professional Nursing 25(4):197-203.
Kurtzman, E. T., and P. I. Buerhaus. 2008. New Medicare payment rules: Danger or opportunity for nursing? American Journal of Nursing 108(6):30-35.
Lacey, S. R., and K. S. Cox. 2009. Nursing: Key to quality improvement. Pediatric Clinics of North America 56(4):975-985.
Landon, B. E., S. L. Normand, A. Lessler, A. J. O’Malley, S. Schmaltz, J. M. Loeb, and B. J. McNeil. 2006. Quality of care for the treatment of acute medical conditions in U.S. hospitals. Archives of Internal Medicine 166(22):2511-2517.
Lasater, K., and A. Nielsen. 2009. The influence of concept-based learning activities on students’ clinical judgment development Journal of Nursing Education 48(8):441-446.
Mitchell, P. H., B. Belza, D. C. Schaad, L. S. Robins, F. J. Gianola, P. S. Odegard, D. Kartin, and R. A. Ballweg. 2006. Working across the boundaries of health professions disciplines in education, research, and service: The University of Washington experience. Academic Medicine 81(10):891-896.
National Quality Forum. 2004. National voluntary consensus standards for nursing-sensitive care. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=22094 (accessed September 2, 2010).
Naylor, M. D., D. A. Brooten, R. L. Campbell, G. Maislin, K. M. McCauley, and J. S. Schwartz. 2004. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatric Society 52(5):675-684.
Needleman, J., P. I. Buerhaus, M. Stewart, K. Zelevinsky, and S. Mattke. 2006. Nurse staffing in hospitals: Is there a business case for quality? Health Affairs 25(1):204-211.
O’Neil, E. 2009. Four factors that guarantee health care change. Journal of Professional Nursing 25(6):317-321
Orsolini-Hain, L., and V. Waters. 2009. Education evolution: A historical perspective of associate degree nursing. Journal of Nursing Education 48(5):266-271.
Paulus, P. B., and B. A. Nijstad, eds. 2003. Group creativity: Innovation through collaboration. New York: Oxford University Press.
Pisano, G. P., and R. Verganti. 2008. Which kind of collaboration is right for you? Harvard Business Review 86(12):78-86.
Rendell, E. G. 2007. Prescription for Pennsylvania: Right state, right plan, right now. Harrisburg, PA: Office of the Governor.
Ritter, A., and T. Hansen-Turton. 2008. The primary care paradigm shift: An overview of the statelevel legal framework governing nurse practitioner practice. Health Lawyer 20(4):21-28.
Safriet, B. J. 2010. Federal options for maximizing the value of advanced practice nurses in providing quality, cost-effective health care. Paper commissioned by the Committee on the RWJF Initiative on the Future of Nursing, at the IOM (see Appendix H on CD-ROM).
Sales, A., N. Sharp, Y. F. Li, E. Lowy, G. Greiner, C. F. Liu, A. Alt-White, C. Rick, J. Sochalski, P. H. Mitchell, G. Rosenthal, C. Stetler, P. Cournoyer, and J. Needleman. 2008. The association between nursing factors and patient mortality in the Veterans Health Administration: The view from the nursing unit level. Medical Care 46(9):938-945.
Singh, J., and L. Fleming. 2010. Lone inventors as sources of breakthroughs: Myth or reality? Management Science 56(1):41-56.
Stevens, R. 1999. In sickness and wealth, American hospitals in the twentieth century. Baltimore, MD: The Johns Hopkins University Press.
Tanner, C. A., P. Gubrud-Howe, and L. Shores. 2008. The Oregon Consortium for Nursing Education: A response to the nursing shortage. Policy, Politics & Nursing Practice 9(3):203-209.
Tucker, A. L., and S. J. Spear. 2006. Operational failures and interruptions in hospital nursing. Health Services Research 41(3 Pt 1):643-662.
U.S. Census Bureau. 2009. Table 603. Employed civilians by occupation, sex, race, and Hispanic origin: 2008. In Statistical abstract of the United States: 2010. 129th ed. Washington, DC: U.S. Census Bureau.
Wuchty, S., B. F. Jones, and B. Uzzi. 2007. The increasing dominance of teams in production of knowledge. Science 316(5827):1036-1039.
ANNEX 1-1
KEY TERMS AND FACTS ABOUT THE NURSING WORKFORCE
DEFINITIONS FOR CORE TERMS
Throughout the report, the committee uses three terms—health, health care, and health care system—that are used routinely by policy makers, legislators, health care organizations, health professionals, the media, and the public. While these terms are commonly used, the definitions can vary and are often nuanced. In this section, the committee offers its definitions for these three core terms. In addition to the terms discussed below, other important terms are defined throughout the report in conjunction with relevant discussion. For example, value and primary care are defined and discussed in Chapter 2.
Health
In a previous Institute of Medicine (IOM) report, “health” is defined as “a state of well-being and the capability to function in the face of changing circumstances.” It is “a positive concept emphasizing social and personal resources as well as physical capabilities” (IOM, 1997). Improving health is a shared responsibility of society, communities, health care providers, family, and individuals. Certain social determinants of health—such as income, education, family, and community—play a greater role than mere access to biomedical care in improving health outcomes for large populations (Commission on Social Determinants of Health, 2008; IOM, 1997). However, access to primary care, in contrast to specialty care, is associated with better population health outcomes (Starfield et al., 2005).
Health Care
“Health care” can be defined as the prevention, diagnosis, treatment, and management of disease and illness through a wide range of services provided by health professionals. These services are supplemented by the efforts of private individuals (patients), their families, and communities to achieve optimal mental and physical health and wellness throughout life. The committee considers the full range of services to be encompassed by the term “health care,” including prevention and health promotion, mental and behavioral health, and primary care services; public health; acute care; chronic disease management; transitional care; long-term care; palliative care; end-of-life care; and other specialty health care services.
Health Care System
The term “health care system” refers to the organization, financing, payment, and delivery of health care. As described in greater detail in the IOM report Crossing the Quality Chasm: A New Health System for the 21st Century (IOM, 2001), the U.S. health care system is a complex, adaptive system (as opposed to a simple mechanical system). As a result, its many parts (including human beings and organizations) have the “freedom and ability to respond to stimuli in many different and fundamentally unpredictable ways.” In addition, the system has many linkages so that changes in one part of the system often change the context for other parts (IOM, 2001). Throughout this report, the committee highlights what it believes to be one of the strongest linkages that has emerged within the U.S. health care system: that between health reform and the future of nursing. As the report emphasizes, the future of nursing—how it is shaped and the directions it takes—will have a major impact on the future of health care reform in the United States.
PREPARATION AND ROLES OF NURSING CARE PROVIDERS IN AMERICA3
The range of nursing care providers described below work in a variety of settings including ambulatory care, hospitals, community health centers, public health agencies, long-term care facilities, mental health facilities, war zones, prisons, and schools of nursing, as well as patients’ homes, schools, places of worship, and workplaces. Basically anywhere there are health care needs, nurses can usually be found. Types of nursing care providers include
Nursing Assistants/Certified Nursing Assistants (NA/CNAs) provide basic patient care under the direction of licensed nurses: they feed, bathe, dress, groom, and move patients, change linens and may assume other delegated responsibilities. The greatest prevalence of these providers is in home care and in long-term care facilities. Training time varies from on-the-job training to 75 hours of state approved training for certification (CNA).
Licensed Practical/Licensed Vocational Nurses (LPN/LVNs) provide basic nursing care including monitoring vital signs, performing dressing changes and other ordered treatments, and dispense medications in most states. LPNs work under the supervision of a physician or registered nurse. While there is declining demand for LPNs in hospitals, demand is high in
long-term care facilities and to a lesser degree in out-patient settings, such as physicians’ offices. They complete a 12–18 month education program at a vocational/technical school or community college and are required to pass a nationally standardized licensing exam in the state in which they begin practice. LPNs may become RNs by bridging into an Associate Degree or in some cases, Baccalaureate Nursing Program.
Registered Nurses (RNs) typically complete a program of study at a community college, diploma school of nursing or a four-year college or university and are required to pass a nationally standardized licensing exam in the state in which they begin practice. The essential core of their nursing practice is to deliver holistic, patient-centered care that includes assessment and monitoring, administering a variety of treatments and medications, patient and family education and serving as a member of an interdisciplinary team. Nurses care for individuals and families in all phases of the health and wellness continuum as well as provide leadership in health care delivery systems and in academic settings. There are over 57 RN specialty associations in nursing and others newly emerging. Many RNs practice in medical-surgical areas; some other common specialties among registered nurses, many of which offer specialty certification options, include:
Critical Care Nurses provide care to patients with serious, complex, and acute illnesses or injuries that require very close monitoring and extensive medication protocols and therapies. Critical care nurses most often work in intensive care units of hospitals; however, nurses also provide highly acute and complex care in emergency rooms.
Public Health Nurses work to promote and protect the health of populations based on knowledge from nursing, social, and public health sciences. Public Health Nurses most often work in municipal and State Health Departments.
Home Health/Hospice Nurses provide a variety of nursing services for both acute, but stable and chronically ill patients and their caregivers in the home, including end-of-life care.
Occupational/Employee Health Nurses provide health screening, wellness programs and other health teaching, minor treatments, and disease/medication management services to people in the workplace. The focus is on promotion and restoration of health, prevention of illness and injury, and protection from work related and environmental hazards.
Oncology Nurses care for patients with various types of cancer, administering chemotherapy, and providing follow-up care, teaching and monitoring. Oncology nurses work in hospitals, out-patient clinics and patients’ homes.
Perioperative/Operating Room Nurses provide preoperative and postoperative care to patients undergoing anesthesia, or assist with surgical procedures by selecting and handling instruments, controlling bleeding, and suturing incisions. These nurses work in hospitals and out-patient surgical centers.
Rehabilitation Nurses care for patients with temporary and permanent disabilities within institutions and out-patient settings such as clinics and home health care.
Psychiatric/Mental Health Nurses specialize in the prevention of mental and behavioral health problems and the nursing care of persons with psychiatric disorders. Psychiatric nurses work in hospitals, out-patient clinics, and private offices.
School Nurses provide health assessment, intervention, and follow-up to maintain school compliance with healthcare policies and ensure the health and safety of staff and students. They refer students for additional services when hearing, vision, obesity, and other issues become inhibitors to successful learning.
Other common specialty areas are derived from a life span approach across healthcare settings and include maternal-child, neonatal, pediatric, and gerontological nursing.
There are several entry points as well as progression points for registered nurses:
Associate Degree in Nursing (ADN) or Diploma in Nursing prepared RNs provide direct patient care in various health care settings. The two to three years of education required is received primarily in community colleges and hospital-based nursing schools and graduates may bridge into a baccalaureate or higher degree program.
Baccalaureate Degree in Nursing (BSN) prepared RNs provide an additional focus on leadership, translating research for nursing practice, and population health; they practice across all healthcare settings. A BSN is often required for military nursing, case management, public health nursing, and school-based nursing services. Four-year BSN programs are offered primar-
ily in a university setting. The BSN is the most common entry point into graduate education.
Master’s Degrees in Nursing (MSN/Other) prepare RNs primarily for roles in nursing administration and clinical leadership, faculty, and for advanced practice in a nursing specialty area. The up to two years of education typically occurs in a university setting. Advanced Practice Registered Nurses (APRNs) receive advanced clinical preparation (generally a Master’s degree and/or post Master’s Certificate, although the Doctor of Nursing Practice degree is increasingly being granted). Specific titles and credentials vary by state approval processes, formal recognition and scope of practice as well as by board certification. APRNs fall into four broad categories: Nurse Practitioner, Clinical Nurse Specialist, Nurse Anesthetist, and Nurse Midwife:
Nurse Practitioners (NPs) are Advanced Practice RNs who provide a wide range of healthcare services across healthcare settings. NPs take health histories and provide complete physical examinations; diagnose and treat many common acute and chronic problems; interpret laboratory results and X-rays; prescribe and manage medications and other therapies; provide health teaching and supportive counseling with an emphasis on prevention of illness and health maintenance; and refer patients to other health professionals as needed. Broad NP specialty areas include: Acute Care, Adult Health, Family Health, Geriatrics, Neonatal, Pediatric, Psychiatric/Mental Health, School Health, and Women’s Health.
Clinical Nurse Specialists (CNS) practice in a variety of health care environments and participate in mentoring other nurses, case management, research, designing and conducting quality improvement programs, and serving as educators and consultants. Specialty areas include but are not limited to: Adult Health, Community Health, Geriatrics, Home Health, Pediatrics, Psychiatric/Mental Health, School Health and Women’s Health. There are also many sub-specialties.
Certified Registered Nurse Anesthetists (CRNAs) administer anesthesia and related care before and after surgical, therapeutic, diagnostic and obstetrical procedures, as well as pain management and emergency services, such as airway management. Practice settings include operating rooms, dental offices and outpatient surgical centers. CRNAs deliver more than 65 percent of all anesthetics to patients in the United States.
Certified Nurse Midwives (CNMs) provide primary care to women, including gynecological exams, family planning advice, prenatal care,
management of low risk labor and delivery, and neonatal care. Practice settings include hospitals, birthing centers, community clinics and patient homes.
Doctoral Degrees in Nursing include the Doctor of Philosophy in Nursing (PhD)4 and the Doctor of Nursing Practice (DNP). PhD-prepared nurses typically teach in a university setting and conduct research, but are also employed increasingly in clinical settings. DNP programs prepare graduates for advanced practice and clinical leadership roles. A number of DNPs are employed in academic settings as well.
TABLE 1-A1 Providers of Nursing Care: Numbers, Preparation/Training, and Roles
|
Type of Nursing Care Provider |
Type of Degree |
Preparation Time |
Roles and Responsibilities |
Salaries |
|
Registered Nurses |
Doctor of Philosophy (PhD) or Doctor of Nursing Practice (DNP) Degrees |
4 to 6 years beyond baccalaureate degree |
Serve as health system executives, educators, deans, clinical experts/Advanced Practice Registered Nurses (APRNs), researchers, and senior policy analysts. |
Mean faculty salaries range from $58,051.00 to $96,021.00 Administrators’ and other non-faculty salaries not available but are generally higher |
|
|
Master’s Degree (MSN/MS) |
Typically up to 2 years beyond baccalaureate degree |
Serve as educators, clinical leaders, administrators or APRNs certified as a Nurse Practitioner (NP), Clinical Nurse Specialist (CNS), Certified Nurse Midwife (CNM), or Certified Registered Nurse Anesthetist (CRNA). |
Median salaries for APRNs range from $81,708.00 to $144,174.00 Mean Master’s prepared instructor salary $54,426.00 |
|
|
Baccalaureate Degree (BSN) |
4 years |
Provide direct patient care, nursing leadership, and translating research into nursing practice across all health care settings. |
Mean salary $66,316 |
|
|
Associate Degree (ADN) or a Diploma in Nursing |
2 to 3 years |
Provide direct patient care in various health care settings. |
ADN mean salary $60,890 Diploma mean salary $65,349 |
|
Other Nursing Care Providers |
Licensed Practical Nurse/Licensed Vocational Nurse (LPN/LVN) |
12 to 18 months |
Provide basic nursing care primarily in long-term-care or ambulatory settings under the supervision of the Registered Nurse or Physician. |
Mean salary $40,110.00 |
|
|
Nursing Assistant (NA) |
Up to 75 hours training |
Provide basic care to patients most commonly in nursing care facilities and patient homes. |
Mean salary $26,110.00 |
|
SOURCE: Adapted from AARP, 2010c. Courtesy of AARP. All rights reserved. Original data provided by the American Association of Colleges of Nursing, the Bureau of Labor Statistics, the Health Resource and Service Administration, and the National League for Nursing. |
||||
TABLE 1-A2 Pathways in Nursing Education
|
Type of Degree |
Description of Program |
|
Doctor of Philosophy in Nursing (PhD) and Doctor of Nursing Practice (DNP) |
PhD programs are research-focused, and graduates typically teach and conduct research, although roles are expanding. DNP programs are practice-focused and graduates typically serve in Advanced Practice Registered Nurse (APRN) roles and other advanced positions, including faculty positions. Time to completion: 3–5 years. BSN or MSN to nursing doctorate options available. |
|
Masters Degree in Nursing (MSN/MS) |
Prepares Advanced Practice Registered Nurses (APRNs), Nurse Practitioners, Clinical Nurse Specialists, Nurse-Midwives, and Nurse Anesthetists, as well as Clinical Nurse Leaders, nurse educators and administrators. Time to completion: 18–24 months. Three years for ADN to MSN option. |
|
Accelerated BSN or Masters Degree in Nursing |
Designed for students with baccalaureate degree in another field. Time to completion: 12–8 months for BSN and three years for MSN depending on prerequisite requirements. |
|
Bachelor of Science in Nursing (BSN) Registered Nurse (RN) |
Educates nurses to practice the full scope of professional nursing responsibilities across all health care settings. Curriculum provides additional content in physical and social sciences, leadership, research and public health. Time to completion: Four years or up to two years for ADN/Diploma RNs and three years for LPNs depending on prerequisite requirements. |
|
Associate Degree (ADN) in Nursing (RN) and Diploma in Nursing (RN) |
Prepares nurses to provide direct patient care and practice within the legal scope of professional nursing responsibilities in a variety of health care settings. Offered through community colleges and hospitals. Time to completion: Two to three years for ADN (less in the case of LPN-entry) and three years for diploma (all hospital-based training programs) depending on prerequisite requirements. |
|
Licensed Practical Nurse (LPN)/Licensed Vocational Nurse (LVN) |
Trains nurses to provide basic care, e.g. take vital signs, administer medications, monitor catheters and apply dressings. LPN/LVNs work under the supervision of physicians and registered nurses. Offered by technical/vocational schools and community colleges. Time to completion: 12–8 months. |
|
SOURCE: AARP, 2010a. Courtesy of AARP. All rights reserved. |
|
REFERENCES
AARP. 2010a. Pathways in nursing education. http://championnursing.org/resources/pathways-nursing-education (accessed August 27, 2010).
AARP. 2010b. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed August 17, 2010).
AARP. 2010c. Providers of nursing care: Numbers, preparation/training and roles: A fact sheet. http://championnursing.org/resources/providers-nursing-fact-sheet (accessed August 26, 2010).
Commission on Social Determinants of Health. 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. Final report of the commission on social determinants of health. Geneva, Switzerland: World Health Organization.
IOM (Institute of Medicine). 1997. Improving health in the community: A role for performance monitoring. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
Starfield, B., L. Shi, and J. Macinko. 2005. Contribution of primary care to health systems and health. The Milbank Quarterly 83(3):457-502.


























