F
Health Care System Reform and the Nursing Workforce: Matching Nursing Practice and Skills to Future Needs, Not Past Demands1
Julie Sochalski, Ph.D., R.N., FAAN
University of Pennsylvania School of Nursing
Jonathan Weiner, Dr.P.H.
Johns Hopkins University Bloomberg School of Public Health
INTRODUCTION
The Robert Wood Johnson Foundation’s Initiative on the Future of Nursing is founded on a major study, undertaken in collaboration with the Institute of Medicine, that will “examine the capacity of the nursing workforce to meet the demands of a reformed health care and public health system.” A report pursuing such a goal is propitious, and path-breaking from the legion of nursing workforce reports produced over the past half-century by departing from “what is” and focusing on “what should be.” This paper seeks to aid that effort through a detailed examination of how health reform may alter the demand for the registered nurses (RN), and the degree to which the RN workforce measures up to this anticipated demand.
A thoughtful examination of the capacity of the RN workforce to support health reform is important for several reasons. The health reform legislation signed by President Obama on March 23, 2010, and the American Recovery and Reinvestment Act of 2009 which proceeded it, include a range of initiatives that seek to redesign the organization, financing, and delivery of health care. A number of these programs—for example, primary care medical homes and accountable care organizations (ACOs)—rely on interventions that fall squarely within the scope of practice of RNs (e.g., care coordination, transitional care). Furthermore, expanding the reach of insurance coverage will place greater demands on the primary care system, as witnessed in Massachusetts (Long, 2008; Long and
Masi, 2009), and consequently on RNs and nurse practitioners to practice in these settings (Craven and Ober, 2009). In addition, investment in the expansion of interoperable health information technology (HIT) platforms that are critical to the implementation of these system reforms will spur the growth of community-wide information exchange that has the potential to change the distribution, skill-mix, and scope of practice of nurses in profound ways.
So what does a reformed health care delivery system foretell for the future nursing workforce? Will the demand for services provided by RNs change, as the provisions in the legislation suggest, and if so is the nursing workforce positioned to effectively respond? What role will the nursing workforce play in a post-reform environment? This paper examines these questions. We assess the composition, skill set, and scope of practice needed from a future RN workforce to support the health care delivery and coverage reforms that will emerge from the reform legislation and related initiatives. We describe the future demand for RNs under these reforms, how that demand comports with the current and anticipated future supply of RNs, the challenges in meeting the workforce demands of a reformed health care delivery system, and recommendations for future RN workforce planning.
THE IMPACT OF HEALTH CARE DELIVERY REFORMS ON DEMAND FOR HEALTH CARE SERVICES OF NURSES
What will be the demand for the health care services of RNs under the proposed health care delivery reforms? An examination of the health reform legislation and other related policy initiatives reveals a number of programs and provisions that call for reorganization of health care services and the workforce responsible for delivering them. Their implementation could have a significant effect on the future roles of and requirements for RNs.
Advancing Care Management Models
“Care management” comprises a broad and evolving range of strategies to effectively intervene and improve the care for primarily chronically ill individuals—those whose care spans multiple providers and requires continuous, long-term management. Disease management (DM) programs—diagnosis-specific programs targeting chronic illnesses responsible for the largest share of health care spending—have been the dominant form of care management programs for the past 15 years. DM programs target patients with specific chronic illnesses (e.g., heart failure, chronic obstructive pulmonary disease, diabetes), offer providers tools to improve their clinical management, promote outreach and support strategies to improve patient adherence to treatment plans, and provide feedback systems to monitor patient outcomes (Krumholz et al., 2006). Out of DM programs came case management and care coordination strategies that target persons with multimorbidity chronic illnesses and complex care needs in addition
to one or more significant chronic illnesses. These programs rely on rigorous care coordination and well-managed interdisciplinary clinical management to achieve quality outcomes (Anderson, 2005; Bodenheimer, 2008).
Provisions in the Medicare Prescription Drug Improvement Modernization Act of 2003 launched a series of population-based care coordination pilot programs to test the applicability of these strategies for Medicare beneficiaries and to assess the quality improvement outcomes and cost savings that could be achieved (Anderson, 2005; Foote, 2003). The evaluations revealed that while these programs yielded a variety of important quality outcomes, cost savings remained largely elusive (Ayanian, 2009; Peikes et al., 2009). These findings echoed those in an earlier report from the Congressional Budget Office for the U.S. Senate Budget Committee that noted the promise but lack of evidence of cost savings from these programs (CBO, 2004).
Further analyses, however, revealed that cost savings—principally by reducing avoidable hospital admissions—in addition to quality outcomes have been achieved by some care management programs (Bodenheimer and Berry-Millett, 2009; Bott et al., 2009; Sochalski et al., 2009). Programs that have been successful share several important features: care management strategies directed by nurses who were integral to the physician’s practice, who coordinated care and communication between the patient and all members of the interdisciplinary team serving the patient, and who directly provided health care services via in-person and telephonic/electronic methods. Increasing evidence is showing that enhanced and integral involvement of nurses in both the coordination and delivery of care, particularly for patients enduring multiple chronic illnesses and complex care regimens, and in care management is critical to achieving cost and quality targets (Fisher et al., 2009).
Several programs and initiatives included in the health reform legislation involve interdisciplinary and cross-setting care coordination and care management services of RNs.
Patient-Centered Medical Homes (PCMH)
Health reform raised the profile of strategies seeking to eliminate fragmentation in care and its costly and poor quality consequences. A recent report from the Institute of Medicine’s Roundtable on Evidence-Based Medicine (2009) estimated potential annual savings of $271 billion that could accrue by 2014 by facilitating care coordination which would reduce these discontinuities in care. One such strategy is the patient-centered medical home, an enhanced model of primary care through which care teams attend to the multifaceted needs of patients and provide whole person comprehensive and coordinated patient-centered care (Kaye and Takach, 2009).
Health reform’s version of the PCMH is an outgrowth of both structural and care delivery innovations over the past several decades. The structure derives from the pediatric medical home model developed to mainstream care for special
needs children, and expanded to embrace the consensus view of primary care as first-contact, comprehensive, continuous, coordinated care for all populations (IOM, 1996; Starfield and Shi, 2004). This model is joined by key elements of Wagner’s Chronic Care Model (Wagner et al., 1996), several system redesign features (e.g., interdisciplinary collaboration and fully integrated HIT), and a new payment structure that recognizes the broad set of services comprising the patient-centered medical home (Berenson et al., 2008). The PCMH is intended to address critical deficiencies in the current primary care system: (1) making the “patient” the focus of and place for care—redesigning practice so that it is truly “centered” on patient and caregivers; (2) meeting the growing challenge of managing chronic illnesses in primary care settings; and (3) providing necessary resources and payment for care management and coordination activities required for an effective PCMH (Berenson et al., 2008; Chokshi, 2009; Rittenhouse et al., 2009).
A fully functional PCMH is founded on patient and caregiver engagement in care that meets patient preferences; information and education that promotes self-management; care coordination that monitors, reviews, and follows up on all services needed and provided across settings; secure transitions across health care settings; and effective information flow across all providers and services to assure integrated care delivery (Davis et al., 2005; Gerteis et al., 1993). This PCMH model is envisioned to result in lower costs through reductions in emergency room visits and hospital admissions (Hussey et al., 2009; Eibner et al., 2009). Patient self-management, care coordination, and transitional care—services at the core of the PCMH and shown to result in lower hospital and ER use—are directed and provided by nurses.
The Guided Care Program offers an example of a successful PCMH model, one that has improved patient outcomes and quality and reduced health care costs through nursing services (Boult et al., 2008; Boyd et al., 2007, 2008; Leff et al., 2009; Sylvia et al., 2008). The Guided Care (GC) model is a PCMH program using an interdisciplinary team approach to coordinate care for older adults with complex chronic conditions. Based in primary care physician practices, GC nurses coordinate care among health care providers; complete standardized comprehensive home assessments; and collaborate with physicians, patients, and caregivers to create and execute evidence-based care guides and actions plans. GC nurses work on a long-term basis with clients, provide transitional care, and assist patients with self-management skills and accessing necessary community-based services (Boult et al., 2008). Early findings from a cluster randomized trial of this program reveal a 24 percent reduction in inpatient days, 15 percent reduction emergency room visits, and a net Medicare savings of $75,000 per GC nurse in the programs (Leff et al., 2009).
The Intermountain Healthcare Medical Group in Utah (Dorr et al., 2008) and the Geriatric Resources for Assessment and Care for Elders (GRACE) program in Indiana (Counsell et al., 2007) are PCMH models that have targeted high risk older adults for rigorously coordinated care provided by nurses embedded in
primary care practices, in the case of Intermountain, and nurse practitioner/social worker teams in the case of the GRACE program. Each have achieved a significant reduction of hospitalizations and lower costs. Similar gains were also found for high-risk children in PCMH programs. Community Care of North Carolina (McCarthy and Mueller, 2009; Steiner et al., 2008) had nurses provide case management and care coordination services to high-risk Medicaid and SCHIP enrollees, resulting in a 40 percent reduction in hospitalizations for asthma and a 16 percent reduction in emergency room visits and yielding total annual savings of $154–170 million
The Tax Relief and Health Care Act of 2006 directed the Centers for Medicare and Medicaid Services (CMS) to undertake a demonstration program to test the effectiveness of PCMH models for Medicare enrollees and the capacity to achieve both quality outcomes and lower health care spending through such approaches to organize primary care. Provisions in the health reform legislation complement Medicare’s demonstration program, testing different PCMH models and creating a new CMS Innovation Center to support testing new approaches to organizing, delivering and paying for health care services (Chokshi, 2009). Their capacity to achieve real savings, some argue, will depend on the breadth of providers (e.g., primary care, specialists, hospitals) linked to the medical home and the depth of interdisciplinary collaboration and care coordination among them (Fisher, 2008), underscoring the focal role that nursing will play in achieving these outcomes.
Transitional Care
Other innovations in care management also call upon the scope of practice of RNs. Various current and proposed reforms would financially penalize hospitals whose Medicare readmission rates exceeded an established threshold. These provisions come on the heels of a recent study which found that one in five hospitalized Medicare beneficiaries are readmitted within 30 days of discharge, nearly half of whom return without having seen a physician or other health care practitioner in the intervening period (Jencks et al., 2009). Of the $103 billion spent by Medicare on hospital care in the study year, 17 percent was spent on readmissions that were unplanned and potentially avoidable. These findings raise serious questions about the coordination of care and hospital discharge protocols in place where these patients sought care (Epstein, 2009). The financial penalty is intended to serve as a significant incentive to hospitals to adopt evidence-based strategies that will reduce avoidable readmissions.
Co-incident with the release of the readmission study, CMS announced the 14 sites for its newly funded Care Transitions Project. This nationwide pilot program supports partnerships between Medicare’s Quality Improvement Organizations and local providers to develop and implement strategies to manage the transitions of Medicare patients from acute care to post-acute care settings, whether it’s the patient’s home or another health care setting. Transitions between
settings—e.g., hospital to home, hospital to nursing home—are points of great vulnerability for patients, and poorly managed transitions are a chief culprit in hospital readmissions (Coleman et al., 2006; Naylor et al., 1999, 2004). Two prominent evidence-based models of care for managing transitions between settings are founded on nursing services: Coleman’s Care Transitions Model and Naylor’s Transitional Care Model. The Coleman model employs advanced practice nurses as “transition coaches” to manage chronically ill patients and their care needs as they transition between settings and to encourage these patients and their caregivers to assume more active roles in managing their care. The Naylor model targets complex chronically ill patients—those with multiple chronic illnesses and other complicating conditions—and uses specially trained transitional care nurses to provide, manage, and coordinate the full complement of clinical care and transitional care services during, between, and after the hospital stay. Both the Coleman and Naylor models have demonstrated significant reductions in hospital readmissions and health care costs. The health reform legislation includes provisions for a startup program of transitional care that is modeled directly on these two evidence-based models.
Accountable Care Organizations (ACOs)
ACOs received noteworthy attention within influential legislative circles during the debate on health reform that led to their inclusion in the final legislation as a pilot program. ACOs, modeled in large part after successful integrated delivery systems like Kaiser Permanente and Geisinger Health System, have been advanced by the Dartmouth Institute for Health Policy and Clinical Practice and Engelberg Center for Health Reform at the Brookings Institution. Their structure grew out of the seminal work on the geographic patterns of health care use and spending from the Dartmouth Institute (Fisher et al., 2009; Goldsmith, 2009; McKethan and McClellan, 2009). Taking advantage of the natural clustering of health care services around hospitals which the analyses on regional patterns of service use revealed, ACOs are envisioned as locally integrated groups of hospitals, physicians, and other providers that are responsible for the health service needs of a defined population of patients (Crosson, 2009a). Their structure draws from the current Medicare Physician Group Practice demonstration program and the prior decade’s Physician Hospital Organization program (Crosson, 2009b).
ACOs offer a pathway to cost control through payment reform, by establishing collaborations of providers that enter agreements with payers to be financially accountable for the provision of health care services to a defined population. These provider collaborations can take a variety of configurations to accommodate and build upon existing local relationships among providers. The payment methods that have been proposed embody a variety of provider incentives to meet cost targets including shared savings, shared risk, partial capitation, and beneficiary incentives such as differential co-pays. Performance measurement
is an integral component of ACOs to provide quality and cost benchmarks and progress, and to ensure that cost control is not achieved through by limiting necessary or appropriate care.
ACOs will depend on several structural and organizational features in order to meet their cost and quality targets. Fully integrated electronic health records (EHRs) and other types of HIT would be required for timely and meaningful information sharing across the entire range of providers. Regular feedback on performance and benchmarks will need to be shared with all providers, services and enrollees in the ACOs. Moreover, ACOs will be supported and strengthened by adopting rigorous, evidence-based care management practices that are the foundation of many complementary system reforms, e.g., PCMHs and transitional care, to manage and guide the care of fully functioning teams of providers and to coordinate communication within and across teams, organizations, and disciplinary lines.
The care management and coordination strategies adopted by ACOs and other types of integrated delivery systems require an RN workforce that is linked to the patient, can readily transition with the patient across time and care settings and is ultimately accountable for outcomes that transcend time and place. RNs working in this context would be employed by the ACO, one of its practices or contracting care coordination organizations and would be responsible for care management for the most complexly ill patients in the group and for their care transitions. These transitions would include from hospital to home or other postacute setting, from home to hospital, or from ongoing primary care to intensive outpatient secondary care.
Expanding Primary Care Capacity
The demand to build the primary care nursing workforce—both RNs and advanced practice nurses—will grow as accessibility to coverage, service settings, and services increases. The Massachusetts experience provides evidence of this growth in demand: passage of health reform in 2006 led to a substantial increase in demand for primary care services only some of which could be met with the existing reservoir of primary care resources (Long, 2008; Long and Masi, 2009). Moreover, today the number of nurse practitioners (NPs) and physician assistants (PAs) rivals the number of family physicians delivering primary care; thus a substantial share of the growth in demand for primary care services that will follow the expansion in health coverage will by design fall on the shoulders of nurses (Green et al., 2004).
The growth in health centers during the prior decade provides some parameters for quantifying the growth in the demand for the primary care RN workforce. Between 2000 and 2006 the number of patients served by the nation’s health centers grew 67 percent, to 16 million. To meet the concomitant increase in demand for care, the number of primary care physicians at health centers grew by
57 percent, advanced practice clinicians (i.e., NPs, PAs, and certified nurse midwives [CNMs]) by 64 percent, and RNs by 38 percent. Yet despite that growth, according to the National Association for Community Health Centers (NACHC et al., 2008), health centers fell short by 1,843 primary care providers, including physicians, NPs, PAs, and CNMs, and by 1,384 RNs.
NACHC estimates that 56 million people lack access to a primary care medical provider (NACHC, 2007). For health centers to increase the number of patients served (for medical visits) from 16 million to 30 million, an additional 15,600 to 19,400 primary care providers are estimated to be needed. Using the current skill mix of clinicians, 36 percent of these additional providers—from 5,600 to 7,000—would be NPs/CNMs/PAs. In addition, health centers would require another 11,600–14,400 RNs. Assuming that 75 percent of the advanced practice clinicians would be NPs or CNMs, an additional 16,000–20,000 RNs would be required to meet this demand.
National statistics on the RN workforce in primary care suggest that nursing is not growing to meet this demand (Box F-1). The percent of RNs employed in ambulatory care, e.g., clinics, physicians’ offices, health centers remained virtually unchanged between 2004 and 2008, at just over 12 percent. This seemingly steady employment rate masks the gradual decline in the ambulatory care nursing workforce in a number of states. For example, the RN ambulatory care workforce in Florida grew an appreciably decelerating rate over this period: 25 percent from 2004–2006, 12 percent from 2006–2008, and virtually no change from 2008–2009. In 2007 amulatory care settings employed 7.8 percent of RNs in Pennsylvania, down from 8.4 percent 2 years earlier. In 2006 6.3 percent of RNs in California worked in ambulatory care, down from 8.3 percent only 2 years earlier (UCSF School of Nursing and CHWS, 2007). Statistics from the 2004 National Sample Survey of Registered Nurses indicate that between 17,000 and 20,000 RNs were working in health center settings. Meeting the demand for primary care services at community health centers estimated by NACHC would require a doubling of the RN workforce in health centers today, an unlikely circumstance given the prevailing trends in ambulatory care employment of RNs. Furthermore, community health centers represent only one primary care setting that will demand additional RNs. Other services and settings offering access to primary care and preventive health services and receiving enhanced support from the health reform legislation and consequently will place additional demand on RNs include workplace wellness programs, home-based primary care (e.g., Independence at Home program), nurse home visitation services, nurse-managed health centers, and community health teams.
Adoption of Health Care Support Technologies
Within the first few months in office President Obama signed economic stimulus legislation that included a significant investment to expand the HIT
|
BOX F-1 RN Ambulatory Care Workforce U.S. RN ambulatory care workforce:
Florida RN ambulatory care workforce:
Pennsylvania RN ambulatory care workforce:
California RN ambulatory care workforce:
|
infrastructure for the nation (Blumenthal, 2009). This investment is intended to nourish the seeds of digital health care that are well rooted though not widespread. Today only 15–20 percent of hospital RNs practice within a minimally functional HIT infrastructure and well under 5 percent practice within a fully wired context (DesRoches et al., 2008). However, a full array of HIT is expected to diffuse rapidly over the coming decade, with significant implications for future training, staffing models, and workforce policies for RNs. HIT is anticipated to lead to (1) profound changes in the content and process of clinical practice; (2) a redesign of the roles and skill mix of the health care workforce and the ways in which multidisciplinary teams will work with one another; (3) new paradigms for how time and place will influence the delivery of care; and (4) increased care efficiency and better outcomes.
Changing Clinical Practice
HIT will fundamentally change the ways that RNs plan, deliver, document, and review clinical care. The process of obtaining and reviewing diagnostic information, making clinical decisions, communicating with patients and families, and carrying out clinical interventions will radically depart from how these activities occur today. Moreover, the relative proportion of time RNs spend on various tasks is likely to change appreciably over the coming decades. While arguably HIT will have its greatest influence over how RNs plan and document their care, all facets of care will be mediated increasingly by digital workflow, computerized knowledge management, and decision support.
In the future virtually every facet of nursing practice in each setting where it is rendered will have a significant digital dimension around a core electronic health record. Biometric data collection will increasingly be automated, and diagnostic tests, medications and some therapies will be computer generated, managed and delivered with computer support. Patient histories and examination data will increasing be collected by devices that interface directly with the patient and automatically stream into the EHR. Automated blood pressure cuffs, PDA-based functional status, and patient history surveys are examples of this.
In HIT supported organizations a broader array and higher proportion of services of all types will be provided within the context of computer templates and workflows. Care and its documentation will less frequently be “free-hand.” As routine aspects of care become digitally mediated and increasingly rote, RNs and other clinicians can be expected to shift and expand their focus to more complex and nuanced “high touch” tasks that these technologies can not readily or appropriately accomplish. This would include communication, guidance and support of the patient/consumer and their families. There will likely be greater opportunity for interventions such as counseling, behavior change, and social and emotional support—interventions that lie squarely within the province of nursing practice.
Redesigned Roles and Skill-Mix
The new practice milieu—where much of nursing and medical care is mediated and supported within an interoperable “digital commons”—will support and potentially even require a much more effective integration of multiple disciplines into a collaborative team focused on the patient’s unique set of needs. Furthermore, interoperable EHRs linked with personal health records and shared support systems will influence how these teams work and share clinical activities. It will increasingly be possible for providers to work on digitally linked teams who will collaborate with patients and their families no longer limited by “realtime” contact.
As the knowledge base and decision pathways that previously resided primarily in the clinicians’ brain are transferred to “clinical decision support” (CDSS) and computerized provider order entry (CPOE) modules of advanced HIT systems, some types of care most commonly provided by nurses can readily shift to personnel with less training or to the patient and their families. Similarly, many types of care previously provided by physicians and other highly trained personnel can be effectively provided by advanced practice and other specialty trained RNs. Furthermore, the performance of these fundamentally restructured teams will be monitored through the use of biometric, psychometric, and other types of process and outcomes “e-indicators” extracted from the HIT infrastructure.
Change in Time and Place of Care
Care supported by interoperable digital networks will shift in the importance of time and place. The patient/consumer will need not always be in the same location as the provider and the provider need not always interact with the patient in real time. As EHRs, CPOE systems, labs results, imaging systems, and pharmacies are all linked into the same network, many types of care can be provided without regard to location, as the “care grid” is available anywhere, anytime.
Remote patient monitoring is expanding exponentially. There is an evergrowing array of biometric devices (e.g., indwelling heart or blood sugar monitors) that can collect, monitor, and report information from the patient in real time, either in an institution or the home. Some of these devices can also provide direct digitally mediated care—the automated insulin pump and implantable defibrillators are two extreme examples.
The implications of this for nursing will be considerable and as of yet not fully understood (Abbott and Coenen, 2008). It is not clear how much of nursing care might be “geographically untethered” when HIT is fully implemented but it will likely be a significant subset of care, possibly in the range of 15–35 percent of what nurses do today. In words, for this proportion of care, nurses need not be in the same locale (or even the same nation) as their patients. As new technolo-
gies impact the hospital and other settings for nursing services this phenomenon may increase.
Efficiency and Outcomes
HIT adoption is expected to increase efficiency and effectiveness of clinician interactions with each patient and the target population. EHRs and other HIT should lower the cost per unit of service delivered and/or improve the quality of care as measured by outcomes or achievement of other end points, such as increased adherence to optimal guidelines. HIT will lead to greater efficiency if it takes less time for a clinician to provide the same unit of service or if a lower-cost clinician now practicing with extensive HIT support can now deliver the same type of care as a higher cost non-HIT supported provider. Controlled “time and motion” studies that have compared clinicians doing the same task with and without HIT support have produced mixed findings on time efficiencies gained across clinicians and settings. One area with emerging evidence is hospital nursing time saved in documentation, with studies showing a 23–24 percent reduction in documentation time (Poissant et al., 2005). These efficiency gains may be partially offset by the information demands of quality improvement initiatives and similar programs undertaken by a growing number of institutions (DesRoches et al., 2008).
CHALLENGES AND RECOMMENDATIONS
The composition and distribution of the current RN workforce is diverging increasingly from workforce need to support the implementation of health reform and related initiatives. Reversing a 15-year trend, a growing number of RNs are employed in hospital settings—62 percent of employed RNs in 2008 (U.S. Department of Health and Human Services, 2010) compared with 56 percent in 2004 (U.S. Department of Health and Human Services, 2006). Higher salaries in the acute care sector appear to have drawn RNs to hospitals from other health care settings as well as reentrants into the workforce. Furthermore, only 10–12 percent of RNs work in ambulatory care settings—settings where much of the system innovation is targeted yet where the evidence base for effective clinical nursing practice is underdeveloped. Moreover, current payment policy and employer behavior have produced a nursing practice model (i.e., staffing composition and scope of practice) that is largely setting-defined rather than patient-centered, so coordination of care and managing transitions across settings has not developed as an integral part of nursing care. The recent Carnegie Foundation report on the future of nursing education (Benner et al., 2009) noted that few schools nationwide have clinical curricula that allow students to follow patients and families across time and institutional settings; consequently students clinical experiences focus on acute inpatient care and episodic care in the health care settings. Finally
the RN workforce is reported to be in the grips of a decade-long nursing supply shortage that is poised to worsen with the impending exodus of a substantial number of retiring baby boomers. Looming large among these retirees are nursing faculty whose departure will impede the replenishment of the depleted RN ranks.
Historically, the U.S. health care system has been able to absorb the entire available supply of RNs. The wide geographic availability of nurses, their deep and nimble skill set, and lower wages relative to physicians and other health care professionals have contributed to their employment in every setting where health care services are delivered. Between 2001 and 2008, total RN FTEs rose roughly 25 percent (Buerhaus et al., 2009) while the general population grew only 7 percent, continuing a decades-long pattern of rising RN-to-population ratios (Figure F-1). The behavior of health care institutions—the main employers of nurses—influenced by government and health plan reimbursement policies, appear to be the main driver of RN demand, a demand that appears to be all but inexhaustible. The education sector has responded to that demand, producing nurses well prepared to deliver acute care services largely in acute care settings, with a shallow skill set and thin distribution in other areas such as ambulatory care, home-based and community-based care, and geriatrics and long-term-care services.
If the demand for RNs changes in response to the system changes and incentives embodied in the health reform legislation and related initiatives, what will
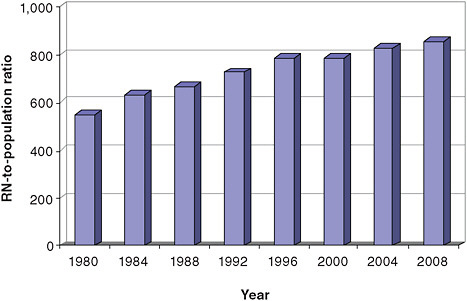
FIGURE F-1 RN-to-population ratio, 1980–2008
SOURCES: HRSA, 1982, 1986, 1990, 1994, 2002, 2006, 2010.
it take for the RN workforce respond in kind, and what are the implications for workforce planning? Viewing the future RN workforce through the lens of health reform would significantly recharacterize the supply shortage and thus redirect policy actions to build, skill, and distribute an RN workforce that can meet the demands of a reformed health care delivery system (Bovbjerg et al., 2009).
Increasing the presence of RNs in settings and positions that will assist the development of care management initiatives will require preparing RNs to direct team-based care management strategies and transitional care from ambulatory care practices, and reassessing the need for a growing share of the nurses to fill staffing vacancies in hospitals. Hospital vacancy rates derive from staffing levels that vary significantly across regions (Figure F-2), and across hospitals within regions, and are largely determined locally based on an estimate of the number of nurses needed to meet some predetermined ideal threshold (Goldfarb et al., 2008). Grumbach and colleagues (2001) remark on the absence of widely accepted standard for what constitutes adequate RN staffing levels in hospitals. A review of the evidence on the outcomes of RN staffing levels in hospitals does not produce a staffing rate or configuration that consistently yields positive outcomes, in spite of substantial cross-sectional associations between the number of RNs and hospital patient outcomes (Kane et al., 2007; Lankshear et al., 2005). Nonetheless, vacancy rates—which are widely accepted as evidence of supply shortages of RNs—continue to be used in workforce planning efforts to estimate the shortfall in hospital RNs and drive policy action and educational system re-
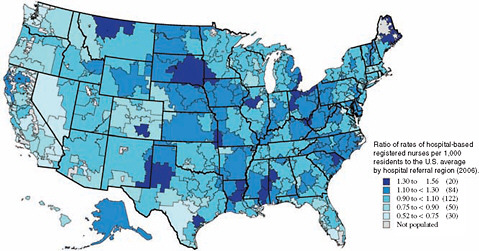
FIGURE F-2 Geographic variation in rates of hospital-based RNs per 1,000 population (2006).
SOURCE: Goodman et al., 2009. Reprinted with permission from the Dartmouth Atlas Project, 2009. Copyright 2009 by the Trustees of Dartmouth College.
sponses that support the diversion of RNs to hospitals and setting-specific models of nursing practice.
Growing RN primary care capacity in response to the anticipated rise in demand for care from increased coverage will require overcoming significant hurdles in the preparation and deploying of RNs to the full array of ambulatory care settings. Retooling nursing education and revamping working conditions and salaries in ambulatory care will be needed to stem the flow of nurses to hospitals, both RN as well as advanced practice nurses. The growing evidence of the influence of prolonged hours of interns and residents on medical errors and adverse events has led to the introduction of regulations limiting their hours. This “shortfall” in medical resident hours has stimulated a demand for, and a gradual migration of, NPs to acute care settings. And while the shortage of primary care capacity would be expected to engender greater demand for all primary care providers including NPs, barriers to practice interfere with their full employment in ambulatory care. Even in states where state practice acts allow NPs to practice fully and independently, the demand for NPs has been constrained by health plan practices (e.g., failure to be credentialed as primary care providers) and reimbursement policies.
Getting the RN workforce required to support health care delivery reform will require a wholesale paradigm shift in the framework and context used to prepare and deploy the RN workforce and to forecast future requirements. This shift will be predicated on the degree to which the implementation of the health reform legislation “recalibrates” the demand for RNs. Payment reform that rewards effective coordination of care over inefficient use of acute inpatient services will demand RNs with skills in care management particularly for the complexly chronically ill, transitional care and community-based services. Payment reform that promotes the creation of medical homes will demand the production of RNs who can provide and direct interdisciplinary teams in the provision of primary care services. Accountable care organizations that are responsible for the full range of health needs of defined populations will demand RNs whose skills span from primary care to end-of-life care and who practice follows the patient and family/caregivers across the full range of settings including the home. And all of these innovations will require fully integrated, interoperable HIT that will support health care teams in ways that are likely affect the effective use of all of their members.
The challenges to achieving this RN workforce in the future are grouped in three general categories. The first challenge lies in the health care marketplace. Currently nurses are hired by employers to fill vacant positions rather than to provide specific skills, perpetuating an employment pattern that is insensitive to different and potentially more efficient skill mix configurations. The health care marketplace, and payers in particular, have not offered sufficient incentives for health care employers to demand a nursing workforce that aligns the skills of RNs more effectively with needs of patients and the health care system. There
are few integrated delivery systems or ACO-type entities that are responsible for, and explicitly rewarded for, their overall performance across the settings that comprise their system of care rather than a single setting. In the main, financial performance is captured and rewarded at the level of the individual setting (e.g., hospitals) and not at the system level (e.g., ACO), so the behavior of each setting is independent and driven by its own goals. Consequently, hospitals lack the financial incentive to hire and deploy RNs to provide transitional care if the outcome is reduced income in the form of reduced admissions. ACO-type organizations lack the incentive to employ RNs to provide care coordination and team management services if these entities are not rewarded for improved financial performance and quality outcomes that these services produce.
The second challenge lies in the educational sector. As currently designed primary nursing education prepares nurses to function in discrete settings rather than across settings (Benner et al., 2009) and as individual clinical providers rather than team members. Team-based care and care coordination are not meaningfully integrated in primary nursing educational pedagogies. Reorienting nursing education to incorporate these themes will require significant redesign of both classroom and clinical education. Furthermore, primary nursing education is still largely focused on the acute care setting. Preparing RNs, in addition to advanced practice clinicians, to practice in ambulatory care settings where the demand for care is clearly growing will require a substantial shift in classroom education but even a greater shift in the clinical practica for students. Finally, the scope and breadth of nursing education needed to meet the needs of reformed health care delivery will require assessment of whether the current educational modality—where the majority of nurses complete their primary nursing education in associate degree programs—produces the right mix of RNs and skills needed to enact these reforms. Without a change in demand, however, the educational system will continue to produce the RN supply—the numbers and skill composition—that it has in the past.
Finally, workforce planning and forecasting will likewise require a comparable paradigm shift. Forecasting models based on current RN demand will not produce useful estimates to guide future policy, i.e., the capacity of the RN workforce to meet the needs of future models of health care services. The current RN workforce is deficient in a number of dimensions to support health reform. Specifically, there is a shortage of RNs deployed to ambulatory care settings and a shortage of advanced practice nurses delivering primary care services. There is a shortage of RNs trained and working as care managers directing and delivering care coordination for patients in acute and post-acute care systems. There is a shortage of RNs with sufficient training and experience in the full array of clinical practice and team management skills that reorganized care delivery models will require. Estimating these shortages, and developing the pathway to resolving them argues for a wholesale new approach to assessing future nursing requirements and preparing and allocating nursing resources to meet those requirements.
Moreover, without a national, integrated approach to workforce planning, one that includes and obligates the critical stakeholders to the goals of an evidence-based and effectively deployed health care workforce, forecasting efforts will produce estimates that cannot guide future workforce planning. In the absence of interdisciplinary collaboration, health care education and the supply forecasts it feeds will proceed as a decentralized, professionally governed activity that produces estimates of health care workforce requirements that meet individual professional goals that may not serve the nation’s need for an effectively prepared and deployed workforce.
Further challenging these efforts will be incorporating the effects of fully integrated health information support, which available evidence suggests will significantly influence the skill mix needed to deliver health care services. HIT will be a key factor affecting the practice of nursing and medicine over the next generation, and its impact on nursing practice and workforce requirements is still very poorly understood. In the future, a more complex calculus will be needed to assess the overall change in efficiency or cost versus benefit of HIT systems. It will be necessary to provide controlled evidence showing the impact of an entire well calibrated HIT supported system within an ACO or other integrated delivery systems. Rather than a single end point (like RN time spent charting) a full market basket of patient outcomes will need to be included as the end point in this equation. And this assessment would also need to account for the fact that the ACO will likely be able to adjust the skill mix of its HIT-supported workforce in order to deliver the same or higher level of care quality more efficiently. For example, this could be accomplished by substituting a higher percentage of lower salaried professionals who can extend their scope of practice with guidance from computerized clinical support systems.
Recommendations
Recommendation 1: The U.S. Department of Health and Human Services should spearhead an interagency innovations research collaborative with responsibility to test new models for organizing health care services and determine the workforce features critical to achieving desired cost and quality outcomes.
For too long health services research and health workforce studies have not been effectively integrated. Studies testing various models for redesigning health care service delivery have focused primarily on the outcomes achieved by delivery system innovations in contrast to usual care but have not included an explicit assessment of the relative contributions of different configurations and skill sets of health care clinicians to the outcomes achieved. Health care workforce research has largely adopted a human capital approach—i.e., stud-
ies assessing supply and demand for various health care clinicians and factors contributing to recruitment and retention of health care workers—with little time spent on assessing the optimal mix of clinicians and skills to achieve cost and quality outcomes. By failing to integrate these two analytic areas, we produce a health care workforce that is poorly positioned to efficiently and effectively enact delivery system reforms that stand to improve system performance and costs. Demonstration projects that assess the effects of service delivery innovations and encourage a range of skill mix models as well as role differentiation (i.e., who performs which tasks) will grow the evidence base that is sorely needed to inform both health system redesign and workforce planning. Only a concerted and cumulative effort will produce the evidence needed to guide payment policy changes that support delivery system and workforce reforms.
The U.S. Department of Health and Human Services should establish a government-wide interagency innovations research collaborative comprising all agencies/departments engaged in health care service delivery and research, with the goal of testing new models to organize and pay for health care services and determining the workforce features critical to achieving desired cost and quality outcomes from these new models. The Quality Interagency Coordination Task Force (QuIC), established in 1998 harness the federal government’s efforts in health care quality improvement, offers a prototype for such an initiative (AHRQ, 2001). The purpose of the QuIC was “to ensure that all Federal agencies involved in purchasing, providing, studying, or regulating health care services worked in a coordinated manner toward the common goal of improving quality care.” Our proposed innovations research collaborative would span such agencies as the Veterans Health Administration, the Department of Defense, the Agency for Healthcare Research and Quality, the National Institutes of Health, and CMS. The new Center for Medicare and Medicaid Innovation established under health reform would be an integral participant. Dedicated funding from each agency would be set aside to build the pool of funds available to undertake the concerted body of research needed and increase the target populations and workforce configurations studied to further our understanding of how to most effectively structure these innovations. Private-sector partnerships would be encouraged, especially with the payer community, since an appropriately aligned payment policy is the linchpin to adopting new models of care by providers and demanding the workforce needed to enact them. Additional partnerships with organizations engaged in quality and outcomes measurement, such as the National Quality Forum, should likewise be pursued. An independent advisory board should be empanelled to develop recommendations on the innovations research agenda to be pursued by the collaborative.
In addition to determining the skill mix configuration that produces optimal cost and quality outcomes, a full assessment of the methods and processes by which those configurations are achieved will be needed. This assessment would explicate the range of policy and strategic initiatives that could be pursued to
promote such configurations. Such skill mix changes have been of great interest to the UK National Health Services (NHS), who sponsored a systematic review of the literature on the shifting roles of health care providers (Sibbald et al., 2004). In that review, which focused to a considerable degree on nursing, the authors offered a framework that captured the range of processes through which changes in the roles, and thus the skill mix, of health care providers occur (Box F-2). The authors further note certain administrative or policy changes, largely at the interface between settings, that could likewise lead to shifts in roles and skill mix of providers (Box F-2). Dubois and Singh (2009) note that achieving optimal “skill mix” options requires taking a much more dynamic approach to workforce utilization by exploring the full range of skill flexibility and skill development that could lead to newly configured roles and more effectively deployed staff. This process would involve identifying and confronting any institutional and regulatory barriers to achieving the staff configurations needed to meet the cost and quality outcomes of these delivery system innovations.
Recommendation 2: The Health Resources and Services Administration of the U.S. Department of Health and Human Services should (a) create a multistakeholder National Workforce Advisory Group responsible for developing op-
|
BOX F-2 Processes and Policy Initiatives Producing Health Care Workforce Skill Mix Changes Processes producing role changes that influence skill mix:
Policy initiatives producing shifts in roles and skill mix:
|
tions for integrated, skill-based workforce requirements models, and (b) collaborate with the Agency for Healthcare Research and Quality (AHRQ) to provide funding to support the development of analytic approaches to assess skills shortages rather than personnel shortages and for articulating optimal skill-mix configurations to address those skills shortages.
Over the years the federal government has invested considerable resources in analytic efforts to estimate the future supply of and demand for doctors, nurses, and a range of allied health workers. Together the estimates from these activities have been used to estimate the shortfall or surplus in these health occupations. These efforts are flawed in several significant ways that affect their utility for future workforce planning. As discussed earlier the demand-based models are founded on current patterns of demand which we have shown for nurses to poorly conform to evidence-based models for effective nursing use. The supply-based models derive from current patterns of producing nurses that are influenced in part by current demand and by current patterns of education that are not well aligned with the future RN workforce requirements to support delivery system redesign. Finally, these models do not take into account the overlap in the skills and abilities of RNs and other health occupations, e.g., doctors, as well as other nursing personnel categories.
In its 2008 report, Out of Order, Out of Time, the Association of Academic Health Centers (2008) calls for the creation of a national health workforce planning body to provide a coordinated approach to health workforce planning that offers an integrated national strategic vision rather than decentralized multi-stakeholder decision-making. This idea is echoed in provisions in the health reform legislation calling for the creation of a National Health Care Workforce Commission. Our proposed recommendation would support and augment the work of this Commission in two ways: (1) by creating an Advisory Group responsible for developing a range of options for building integrated skill-based workforce requirements models, and (2) by providing funding through AHRQ to explore ways to assess and compare the outcomes of health care services offered under a range of skill-mix configurations derived from these integrated requirements models. These strategies would be founded on a comprehensive review of the literature and related resources illuminating the full range of workforce configurations employed in the delivery of health care services and, where available, associated outcomes.
The reorganization of health care service delivery that will accompany many of the innovations included in health reform has potentially profound implications for RNs, whose broad scope of practice places them at the cross section of virtually all health care settings. Redefining roles and responsibilities of health team members that such innovations will entail could significantly affect the skill mix
of the team and of nursing in particular. For example, HIT or other technological innovations may allow health care workers with less training to move into expanded roles with efficiency gains while maintaining quality, e.g., lab techs rather than nurses recording and monitoring biological responses to treatment changes; simultaneously these innovations may lead to improved care by moving clinicians into previously unmet clinical arenas, e.g., moving RNs into providing care management. In both instances these role redefinitions—lab techs moving into clinical lab monitoring from which nurses exit as they assume new roles in care management—change the roles and skills mix of health team members in significant ways.
This recommendation provides strategies to develop and evaluate a broad range of workforce configurations and assess their implications for health care workforce planning. Moreover, by shifting the focus from personnel shortages to skill shortage we invite a wider and more diverse array of policy options to meet the care delivery needs of the public with more effective skill-mix configurations.
Recommendation 3: Nursing education must become a full partner of health care system redesign through meaningful participation in redesign initiatives, and revamping its educational enterprise to meet the needs of redesigned service delivery.
Health care services redesign and the nursing education enterprise are not well aligned, as noted in highlights from the recent Carnegie Foundation study on nursing education:
A major finding from the study is that today’s nurses are undereducated for the demands of practice. Previous researchers worried about the education-practice gap; that is, the ability of practice settings to adopt and reflect what was being taught in academic institutions. Now, according to the authors, the tables are turned: nurse administrators worry about the practice-education gap, as it becomes harder for nursing education to keep pace with the rapid changes driven by research and new technologies. (Carnegie Foundation for the Advancement of Teaching, 2009)
Delivery system redesign initiatives included in health reform depend upon a set of skills and experiences that nursing education has yet to incorporate demonstrably into its pedagogy. Primary nursing education is still largely located in the acute care domain, with students mastering the care of the acute manifestations of chronic disease rather than care management of complex chronic illness. Care coordination and management are not integral to the classroom and clinical activities of nursing students, and yet it is a role that nurses can and have ably assumed in delivery settings where such skills will be increasingly demanded. Transitional care, which the evidence to date shows is a critical feature in pre-
venting hospital readmissions and other adverse events, lies directly in the scope of nursing practice. Yet clinical education does not afford the opportunity to follow patients across health care settings. Thus transitional care, as well as all other cross-setting models of care, are infrequently practiced and thus even less frequently taught. Despite its increasing recognition as the foundation for effective care into the future, team-based care and multidisciplinary care management remain if anything the province of classroom instruction and rarely connected to the practice setting. Primary care and community-based approaches to care represent a minority share of the nursing curriculum even as the demand for these services is predicted to grow. The consequence is the production of succeeding generations of nurses that are not well positioned—in numbers and skills—to meet the needs of a redesigned delivery system.
Meaningful collaboration between nursing education and health care delivery redesign will encourage the alignment in their goals, which is critical to their joint success. Opportunities to advance such collaboration, and mechanisms for its support, should be actively sought. For example, Medicare-funded pilot studies and demonstration programs testing programs that rely on nursing-led interventions, such as ACOs or transitional care, should include representatives from nursing education—its leadership as well as key stakeholders, such as the regulatory bodies that determine the terms and scope of nursing education and practice—in activities associated with the design, review, implementation, evaluation, and dissemination of these initiatives. In similar form, health professions schools testing models of interprofessional education and other models of team-based care education should include representatives from the clinical directors of medicine and nursing in health systems and other key stakeholders from the clinical practice communities.
In reciprocal fashion, this collaboration should inform nursing education as to where gaps exist in educational offerings and skills development to meet the needs of a redesigned delivery system. Closing the gaps will involve thoughtful appraisal of where and how to integrate these new areas of knowledge and clinical experiences into the current curricular offerings. Faculty expertise will need to be developed in a number of these care models. The premium on clinical placements will require consideration of how simulation learning environments may augment current clinical experiences. HRSA should empanel a Technical Advisory Group whose purpose would be to make recommendations on the role and opportunities for relevant agencies within the federal government to support the development of new programmatic and curricular offerings to build this needed skill set, including a full review of the grants and initiatives within Title VIII and other sources of federal funding for nursing education. The report from the Technical Advisory Group should include a discussion of the role of other critical stakeholders, e.g., state regulatory bodies, health care private foundations, professional associations, etc., in better aligning health professions education with the unfolding reforms from health care reform and related initiatives.
REFERENCES
Abbott, P.A., and A. Coenen. 2008. Globalization and advances in information and communication technologies: The impact on nursing and health. Nursing Outlook 56(5):238–246.
AHRQ (Agency for Health Care Research and Quality). 2001. Quality Interagency Coordination Task Force (QuIC). Fact Sheet, AHRQ Publication No. 00-P027. Rockville, MD: Agency for Healthcare Research and Quality. http://www.ahrq.gov/qual/quicfact.htm (accessed April 2, 2010).
Anderson, G.F. 2005. Medicare and chronic conditions. New England Journal of Medicine 353(3): 305–309.
Association of Academic Health Centers. 2008. Out of order, out of time: the state of the nation’s health workforce. Washington, DC: Association of Academic Health Centers. http://www.aahcdc.org/ (accessed February 25, 2010).
Ayanian, J.Z. 2009. The elusive quest for quality and cost savings in the Medicare program. Journal of the American Medical Association 301(6):668–670.
Benner, P., M. Sutphen, V. Leonard, and L. Day. 2009. Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass.
Berenson, R. A., T. Hammons, D. N. Gans, S. Zuckerman, K. Merrell, W. S. Underwood, and A. F. Williams 2008. A house is not a home: Keeping patients at the center of practice redesign. Health Affairs 27(5):1219–1230.
Blumenthal D. 2009. Stimulating the adoption of health information technology. New England Journal of Medicine 360(15):1477–1479.
Bodenheimer, T. 2008. Coordinating care: A perilous journey through the health care system. New England Journal of Medicine 358(10):1064–1071.
Bodenheimer, T., and R. Berry-Millett. 2009. New England Journal of Medicine 361(16):1521-1523.
Bott, D. M., M. C. Kapp, L. B. Johnson, and L. M. Magno. 2009. Disease management for chronically ill beneficiaries in traditional Medicare. Health Affairs 28(1):86–98.
Boult, C., L. Reider, K. Frey, B. Leff, C. M. Boyd, J. L. Wolff, S. Wegener, J. Marsteller, L. Karm, and D. O. Scharfstein. 2008. The early effects of “guided care” on the quality of health care for multi-morbid older persons: A cluster randomized controlled trial. Journal of Gerontology Series A: Biological Sciences and Medical Sciences 63(3):321–327.
Bovbjerg, R. R., B. A. Ormond, and N. Pindus. 2009. The nursing workforce challenge: Public policy for a dynamic and complex market. Washington, DC: The Urban Institute.
Boyd, C. M., C. Boult, E. Shadmi, B. Leff, R. Brager, L. Dunbar, J. L. Wolff, and S. Wegener. 2007. Guided care for multi-morbid older adults. Gerontologist 47(5):697–704.
Boyd, C. M., E. Shadmi, L. Jackson Conwell, M. Griswold, B. Leff, R. Brager, M. Sylvia, and C. Boult. 2008. A pilot test of the effect of guided care on the quality of primary care experiences for multimorbid older adults. Journal of General Internal Medicine 23(5):536–542.
Buerhaus, P. I., D. I. Auerbach, and D. O. Staiger. 2009. The recent surge in nurse employment: Causes and implications. Health Affairs 28(4):w657–w668.
Carnegie Foundation for the Advancement of Teaching. 2009. Book Highlights from “Educating Nurses: A Call for Radical Transformation.” http://www.carnegiefoundation.org/elibrary/educating-nurses-highlights (accessed February 25, 2010).
CBO (Congressional Budget Office). 2004. An analysis of the literature on disease management programs. http://www.cbo.gov/ftpdocs/59xx/doc5909/10-13-DiseaseMngmnt.pdf (accessed February 25, 2010).
Chokshi, D. A. 2009. Ensuring progress in primary care: What can health care reform realistically accomplish? New England Journal of Medicine 361(20):e43(1)–e43(4).
Coleman, E. A., C. Parry, S. Chalmers, and S. Min. 2006. The care transitions intervention: results of a randomized controlled trial. Archives of Internal Medicine 166(17):1822–1828.
Counsell, S. R., C. M. Callahan, D. O. Clark, W. Tu, A. B. Buttar, T. E. Stump, and G. D. Ricketts. 2007. Geriatric care management for low-income seniors: A randomized controlled trial. Journal of the American Medical Association 298(22):2623–2633.
Craven, G., and S. Ober. 2009. Massachusetts nurse practitioners step up as one solution to the primary care access problem. Policy, Politics & Nursing Practice 10(2):94–100.
Crosson, F. J. 2009a. 21st-century health care: The case for integrated delivery systems. New England Journal of Medicine 361(14):1324–1325.
Crosson, F. J. 2009b. Medicare: the place to start delivery system reform. Health Affairs 28(2): w232–w234.
Davis, K., S. C. Schoenbaum, and A. M. Audet. 2005. A 2020 vision of patient-centered primary care. Journal of General Internal Medicine 20(10):953–957.
DesRoches, C., K. Donelan, P. Buerhaus, and L. Zhonghe. 2008. Registered nurses use of electronic health records: Findings from a national survey, Medscape Journal of Medicine 10(7) 164, July 15 online.
Dorr, D. A., A. B. Wilcox, C. P. Brunker, R. E. Burdon, and S. M. Donnelly. 2008. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. Journal of the American Geriatric Society 56(12):2195–2202. Findings updated for presentation at White House roundtable on Advanced Models of Primary Care, August 10, 2009.
Dubois, C.-A., and D. Singh. 2009. From staff-mix to skill-mix and beyond: Towards a systemic approach to health workforce management. Human Resources for Health 7:87.
Eibner, C., P. Hussey, M. Ridgely, and E. McGlynn. 2009. Controlling health care spending in Massachusetts: An analysis of options. http://www.rand.org/pubs/technical_reports/2009/RAND_TR733.pdf (accessed February, 2010).
Epstein, A. M. 2009. Revisiting readmissions: Changing the incentives for shared accountability. New England Journal of Medicine 360(14):1457–1459.
Fisher, E. S. 2008. Building a medical neighborhood for the medical home. New England Journal of Medicine 359(12):1202–1205.
Fisher, E. S., M. B. McClellan, J. Bertko, S. M. Lieberman, J. J. Lee, J. L. Lewis, and J. S. Skinner. 2009. Fostering accountable health care: Moving forward in Medicare. Health Affairs 28(2): w219–w231.
Foote, S. M. 2003. Population-based disease management under fee-for-service Medicare. Health Affairs web exclusive July 30, 2003:w3-342–w3-356.
Gerteis, M., S. Edgman-Levitan, J. Daley, and T. L. Delbanco. 1993. Through the patient’s eyes: Understanding and promoting patient-centered care. San Francisco, CA: Jossey-Bass.
Goldfarb, M. G., R. S. Goldfarb, and M. C. Long. 2008. Making sense of competing nursing shortage concepts. Policy, Politics, & Nursing Practice 9(3):192–202.
Goldsmith, J. 2009. The accountable care organization: not ready for prime time. Health Affairs Blog August 17, 2009. http://healthaffairs.org/blog/2009/08/ (accessed February 25, 2010).
Goodman, D. C., E. S. Fisher, and K. K. Bronner. 2009. Hospital and physician capacity update: A brief report from the Dartmouth Atlas of Health Care. Hanover, NH: The Dartmouth Atlas Project.
Green, L. A., M. S. Dodoo, G. Ruddy, G. E. Fryer, R. L. Phillips, J. L. McCann, E. H. O’Neil, and L. S. Klein. 2004. The physician workforce of the United States: A family medicine perspective. Washington, DC: Robert Graham Center. http://www.graham-center.org/PreBuilt/physician_ workforce.pdf (accessed February 25, 2010).
Grumbach, K., M. Ash, J. A. Seago, J. Spetz, and J. Coffman. 2001. Measuring shortages of hospital nurses: How do you know a hospital with a nursing shortage when you see one? Medical Care Research & Review 58(4):387–403.
HRSA (Health Resources and Services Administration). 1982. The registered nurse population: An overview from National Sample Survey of Registered Nurses, November 1980. Hyattsville, MD: HRSA.
HRSA. 1986. The registered nurse population: Findings from the National Sample Survey of Registered Nurses, November 1984. Rockville, MD: HRSA.
HRSA. 1990. The registered nurse population: Findings from the National Sample Survey of Registered Nurses, March 1988. Rockville, MD: HRSA.
HRSA. 1994. The registered nurse population: Findings from the National Sample Survey of Registered Nurses, March 1992. Rockville, MD: HRSA.
HRSA. 2002. The registered nurse population, March 2000: Findings from the National Sample Survey of Registered Nurses. Rockville, MD: HRSA.
HRSA. 2006. The registered nurse population: Findings from the March 2004 National Sample Survey of Registered Nurses. Rockville, MD: Health Resources and Services Administration.
HRSA. 2010. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. HRSA.
Hussey, P. S., C. Eibner, M. S. Ridgely, and E. A. McGlynn. 2009. Controlling U.S. health care spending: Separating promising from unpromising approaches. New England Journal of Medicine 361(22):2109–2111.
IOM (Institute of Medicine). 1996. Primary care: America’s health in a new era. Washington, DC: National Academy Press.
IOM. 2009. The healthcare imperative: Lowering costs and improving outcomes. Washington, DC: The National Academies Press.
Jencks, S. F., M. V. Williams, and E. A. Coleman. 2009. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine 360(14):1418–1428.
Kane, R. L., T. A. Shamliyan, C. Mueller, S. Duval, and T. J. Wilt. 2007. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Medical Care 45(12):1195–1204.
Kaye, N., and M. Takach. 2009. Building medical homes in state Medicaid and CHIP programs. Portland, ME: National Academy of State Health Policy.
Krumholz, H. M., P. M. Currie, B. Riegel, C. O. Phillips, E. D. Peterson, R. Smith, C. W. Yancy, and D. P. Faxon. 2006. A taxonomy for disease management: A scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation 114(13):1432–1445.
Lankshear, A. J., T. A. Sheldon, and A. Maynard. 2005. Nurse staffing and healthcare outcomes: A systematic review of the international research evidence. Advances in Nursing Science 28(2): 163–174.
Leff, B., L. Reider, K. D. Frick, D. O. Scharfstein, C. M. Boyd, K. Frey, L. Karm, and C. Boult. 2009. Guided care and the cost of complex healthcare: A preliminary report. American Journal of Managed Care 15(8):555–559.
Long, S. K. 2008. On the road to universal coverage: impacts of reform in Massachusetts at one year. Health Affairs 27(4):w270–w284.
Long, S. K., and P. B. Masi. 2009. Access and affordability: An update on health reform in Massachusetts. Health Affairs 28(4):w578–w587.
McCarthy, D., and K. Mueller. 2009. Community care of North Carolina: Building community systems of care through state and local partnerships. NY: The Commonwealth Fund. http://www.commonwealthfund.org/~/media/Files/Publications/Case%20Study/2009/Jun/1219_McCarthy_CCNC_case_study_624_update.pdf (accessed April 2, 2010).
McKethan, A., and M. McClellan. 2009. Moving from volume-driven medicine toward accountable care. Health Affairs Blog August 20, 2009. http://healthaffairs.org/blog/2009/08/ (accessed February 25, 2010).
NACHC (National Association of Community Health Centers), The George Washington University School of Public Health and Health Services, and The Robert Graham Center. 2008. Access transformed: building a primary care workforce for the 21st century. Washington, DC: National Association of Community Health Centers. http://www.nachc.com/access-reports.cfm (accessed February 25, 2010).
NACHC and The Robert Graham Center. 2007. Access denied: A look at America’s medically disenfranchised. Washington, DC: National Association of Community Health Centers. http://www.nachc.com/access-reports.cfm (accessed February 25, 2010).
Naylor, M. D., D. A. Brooten, R. L. Campbell, G. Maislin, K. M. McCauley, and J. S. Schwartz. 2004. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society 52(5):675–684.
Naylor, M. D., D. Brooten, R. Campbell, B. S. Jacobsen, M. D. Mezey, M. V. Pauly, and J. S. Schwartz. 1999. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized controlled trial. Journal of the American Medical Association 281(7):613–620.
Peikes, D., A. Chen, J. Schore, and R. Brown. 2009. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. Journal of the American Medical Association 301(6):603–618.
Poissant, L., J. Pereira, R. Tamblyn, and Y. Kawasumi. 2005. The impact of electronic health records on time efficiency of physicians and nurses: A systematic review. Journal of the American Medical Informatics Association 12(5):505–516.
Rittenhouse, D. R., S. M. Shortell, and E. S. Fisher. 2009. Primary care and accountable care: Two essential elements of delivery-system reform. New England Journal of Medicine 361(24):2301–2303.
Sibbald, B., J. Shen, and A. McBride. 2004. Changing the skill mix of the health care workforce. Journal of Health Services Research and Policy 9(Suppl 1):S128–S138.
Sochalski, J., T. Jaarsma, H. M. Krumholz, A. Laramee, J. J. V. McMurray, M. D. Naylor, M. W. Rich, B. Riegel, and S. Stewart. 2009. What works in chronic care management? The case of heart failure. Health Affairs 28(1):179–189.
Starfield, B., and L. Shi. 2004. The medical home, access to care, and insurance: A review of evidence. Pediatrics 113(5):1493–14998.
Steiner, B. D., A. C. Denham, E. Ashkin, W. P. Newton, T. Wroth, and L. A. Dobson. 2008. Community Care of North Carolina: Improving care through community health networks. Annals of Family Medicine 6(4):361–367.
Sylvia, M. L., M. Griswold, L. Dunbar, C. Boyd, M. Park, and C. Boult. 2008. Guided care: Cost and utilization outcomes in a pilot study. Disease Management 11(1):29–36.
UCSF (University of California, San Francisco), School of Nursing and CHWS (Center for California Health Workforce Studies). 2007. California Board of Registered Nursing 2006 Survey of Registered Nurses. http://www.rn.ca.gov/pdfs/forms/survey2006.pdf (accessed February 25, 2010).
U.S. Department of Health and Human Services, Health Resources and Services Administration. 2010. The registered nurse population: Initial findings from the March 2008 National Sample Survey of Registered Nurses. Rockville, MD: U.S. Department of Health and Human Services.
U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. 2006. Findings from the March 2004 National Sample Survey of Registered Nurses. Rockville, MD: U.S. Department of Health and Human Services.
Wagner, E. H., B. T. Austin, and M. Von Korff. 1996. Organizing care for patients with chronic illness. Milbank Quarterly 74(4):511–554.


























