3
Drug-Resistant Tuberculosis
in the Russian Federation
Key Messages
- The breakdown of the Soviet Union exacerbated TB by increasing unemployment, poverty, migration, and social unrest, but the situation has been slowly improving over the past decade.
- On the other hand, the incidence of MDR TB has continued to increase, as has infection with HIV and coinfection with HIV and TB.
In Russia and the former Soviet Union, TB has been an acute problem.1 Today, the official estimate of the incidence of TB is about 82 to 83 per 100,000 population. According to Perelman, not all cases are diagnosed, however, and not all patients are registered as incident cases; thus this estimate is an underestimation of the true burden of disease.2 The estimate of 82 to 83 cases per 100,000 population also is an average that includes an incredibly diverse population and thus is not very revealing. Russia is a vast country, and the incidence of TB differs as much as tenfold among
![]()
1 This introductory text and the following section are based on the presentation of Mikhail Perelman, Moscow Medical Academy.
2 In Russia, estimated TB incidence (new and relapse cases) in 2009, including TB-HIV coinfection, was 106 per 100,000 population (confidence interval 89-125) (WHO, 2010c).
geographic regions. It is higher in the eastern portion of the country, with the highest rates in the Russian Far East adjacent to Mongolia, China, and Japan. Areas in that part of the country have an incidence ten times that of Moscow.
Before the breakdown of the Soviet Union, the prevention and treatment of TB were under stringent federal control. After the breakdown, many events occurred to exacerbate the problem of TB. Dislocations in the economy made the population poorer, and poverty is a risk factor for TB. Unemployment and crime rates worsened considerably, which encouraged the spread of TB in communities and the prison population. High levels of migration into the country also contributed to the spread of TB, as did military conflicts and the overall degradation of the health care system, which loosened previously stringent controls on the level of disease in the population.
Perelman explained that over the last decade, the TB situation in the Russian Federation has slowly improved. The number of new cases is somewhat lower, and both morbidity and mortality have been on the decline.
A HISTORICAL PERSPECTIVE
In 1943−1944, the Soviet Union received its first lot of penicillin, which was used by the military on the front lines. As early as 1944, the chief surgeon of the Red Army wrote about drug resistance after the potency of penicillin had declined substantially. When penicillin was recently reintroduced, however, it was much more effective, said Perelman.
Before drug therapy became available, TB was treated in Russia through surgery, which saved hundreds of thousands of lives. The surgery option also was used extensively in Scandinavia, France, and the United States, as described in journals such as the Annals of Surgery. Today, better diagnostic and surgical capabilities are available, such as surgery using state-of-the-art visual technologies. In Russia, from 12,000 to 14,000 surgical operations for TB are performed per year, and surgical treatment is about 85 percent effective. According to Perelman, however, the need for surgery is at least 25,000 cases, so the number of surgeries needs to double. In addition, surgery is complex and expensive and requires specialized departments and personnel who are aware of the TB problem.3
The proper approach to TB in Russia today, said Perelman, is for every person suspected of having TB to undergo a general medical checkup, including a chest examination. Russia did not accept DOTS
![]()
3 In Russia, surgery is considered a component of treating patients with chronic TB that has been unresponsive to antimicrobial therapy, as well as newly diagnosed TB patients with complications, drug resistance, and/or intolerance to anti-TB drugs (Perelman, 2000).
in its initial version, and Perelman believes this was a good decision. If DOTS had been implemented, he suggested, the medical checkup would have been abandoned. Today about 50 percent of new cases in Russia are reviewed by x-ray, which provides good data with very little irradiation because digital systems are used. Also, treatment of patients under DOTS was supposed to be a short course. Perelman believes that patients left the program undertreated, and this short course was one of the reasons for the broad spread of MDR TB. Perelman stated that MDR TB also can result if treatment is discontinued based on sputum tests without consideration of cavities in lungs. Finally, he suggested that abandoning luminescent microscopy or treatment in sanatoriums would not have been appropriate in Russia.
An integrated approach to TB is important for prevention, said Perelman. If all people had a high standard of living and education on how to maintain their health, TB would be much less likely to spread. At present, complex combination treatment is needed and is most effective.
EPIDEMIOLOGY OF TB IN THE RUSSIAN FEDERATION4
Yakimova observed that TB remains a very serious problem in Russia. Approximately 320 new TB cases appear each day, and 64 deaths are associated with the disease.
The basic reasons for the TB epidemic in Russia are socioeconomic, medical, and biological, Yakimova stated. Socioeconomic causes include such factors as low living standards, unemployment, and migration. Medical causes include late detection, a lack of anti-TB therapy (especially second-line therapy), a shortage of laboratories, and insufficient infection control. Biological causes include the spread of MDR TB and HIV and the continuing adaptation of M.tb. to antibiotics.
International experts estimate that about 50,000 people in Russia have MDR TB. Between 40 and 70 percent of newly detected TB cases occur in socially vulnerable groups, including the homeless, the unemployed, migrants, and people with drug and alcohol dependencies (see Chapter 7). The incidence of TB among the unemployed is 750 per 100,000 unemployed people, compared with 45 per 100,000 employed people. Children from socially vulnerable groups contract TB 10 to 20 times more frequently than other children.
Altogether in Russia, 117,227 cases of TB were detected in 2009, which is equivalent to 82.6 per 100,000 population. This figure represents a decrease of 2.9 percent relative to 2008. The incidence among children
![]()
4 This section is based on the presentation of Marina Yakimova, Central TB Research Institute, Russian Academy of Medical Sciences.
younger than 15 was 14.7 per 100,000, a decrease of 3.9 percent relative to 2008. The incidence among men is 2.8 times higher than that among women (Figure 3-1). Among all cases of TB in Russia, 12 percent occur in people incarcerated by the Ministry of Justice.
The incidence of TB grew markedly in Russia during the 1990s as the economy of the country deteriorated (Figure 3-2). As noted above, however, the incidence of the disease differs markedly across the country, with some Russian territories accounting for a disproportionate number of cases. Therefore, suggested Yakimova, a single approach will not be appropriate for all populations. TB incidence and mortality in Russia’s prisons have fallen dramatically over the past 10 years, from 4,347 cases per 100,000 prisoners and detainees, with 238 deaths, in 1999 to 1,308 per 100,000 prisoners and detainees, with 80 deaths, in 2008. Detection and treatment also have lowered the percentages of people with TB in Russia who suffer the destructive pulmonary form of the disease.
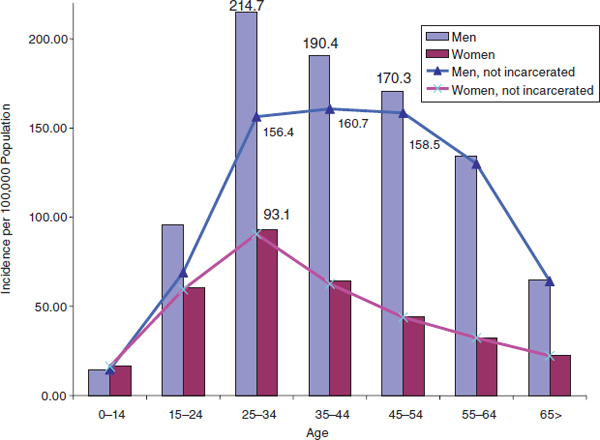
FIGURE 3-1 TB incidence by gender and age rises to a peak between ages 25 and 34.
SOURCE: Yakimova, 2010.
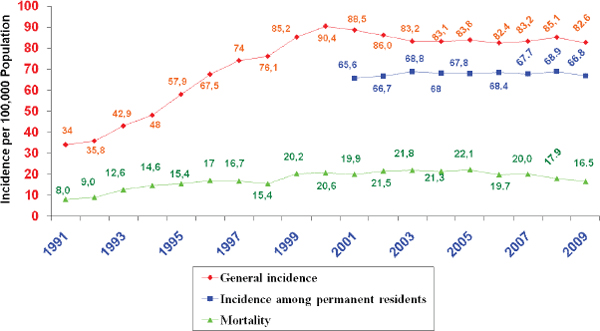
FIGURE 3-2 TB incidence and mortality rose in the 1990s and have declined slightly since.
SOURCE: Yakimova, 2010.
The effectiveness of detection and diagnosis varies among regions within the Russian Federation. Estimated detection rates are below 50 percent overall—“lower than we would like,” said Yakimova. In some regions of the Russian Federation, many cases of TB go undetected. Detection is important because it determines the reservoir of patients who can serve as a source of infection for the general population.
Nevertheless, TB mortality has decreased in the past 5 years in the Russian Federation, as has the proportion of TB cases detected after the subject’s death. An emphasis on TB in national and regional health programs has contributed to this decrease, with a new TB early detection and prevention program starting in 2010. Preventive measures, including infection control and vaccination or prophylactic chemotherapy, must be clearly designed and organized, Yakimova stated. The identification and treatment of TB cases, particularly for people with infectious forms of the disease, are critical to prevention. Other steps Yakimova recommended are:
- creating an integrated system for delivering TB health care, focusing on prevention and early diagnosis;
- designing and implementing initiatives to encourage TB testing among vulnerable groups;
- increasing the vigilance of general practitioners, family doctors, and specialists offering outpatient care;
- implementing directly observed therapy at all stages of TB health care;
- designing and implementing uniform treatment and diagnostic standards in TB health care;
- making improvements in diagnostic methods, combination therapy regimens, and rehabilitation (medical, social, and psychological);
- expanding facilities that offer an alternative to inpatient treatment, such as outpatient, day patient, and home care;
- providing training and retraining for specialists offering prophylactic, therapeutic, and diagnostic services to TB patients as continuing education;
- improving the physical condition and technology of medical facilities offering TB care and equipping them with modern medical and diagnostic equipment;
- guaranteeing the availability of good-quality first- and second-line therapies; and
- increasing the effectiveness of TB prevention initiatives (such as decontamination) in TB centers.
NATIONAL MDR TB SURVEILLANCE SYSTEM5
Full reporting of MDR TB has been ongoing in the Russian Federation since 1999, said Skachkova. This period has seen the gradual development of recording and reporting, epidemiological analysis and research, cohort analysis, legislation, and training. The last annual review of surveillance data was in 2008.
The recording of MDR TB underwent a change at the beginning of 2010. More detailed case records were instituted, and experts were tasked to review data and ensure accuracy. Laboratory documents also were collected and reviewed by the Ministry of Health. New forms are being introduced for recording MDR TB and the effectiveness of MDR TB treatment. Furthermore, a new project is being implemented for continuous tracking of TB patients and risk groups. These changes have enabled much more precise and accurate reporting of not only MDR but also XDR TB cases.
An assessment of MDR TB data that began last year has made it possible to calculate the primary incidence and prevalence of pulmonary MDR TB. Review of these data in turn makes it possible to evaluate the success rates for MDR TB treatment. The guidelines are that a minimum of 85
![]()
5 This section is based on the presentation of Elena Skachkova, Central Research Institute for the Organization and Informatization of Health Care, Russian Federation.
TABLE 3-1 MDR TB Data from the Russian Federation, 2007−2009
|
|
|||
| 2007 | 2008 | 2009 | |
|
|
|||
| Newly detected cases of culture-positive pulmonary TB | 35,449 | 35,573 | 36,679 |
| Relapse cases of culture-positive pulmonary TB | 5,820 | 6,224 | 6,159 |
| Newly detected cases investigated for drug susceptibility | 31,560 | 34,241 | 33,540 |
| Percentage of newly detected cases investigated for drug susceptibility | 89% | 91.1% | 91.4% |
| Relapse cases investigated for drug susceptibility | 5,151 | 5,489 | 5,554 |
| Percentage of relapse cases investigated for drug susceptibility | 88.5% | 88.2% | 90.2% |
| Resistance identified to any drug, newly detected patients | 10,056 (31.9%) |
11,365 (33.2%) |
12,116 (36.1%) |
| Resistance identified to any drug, relapse cases | 2,307 (44.8%) |
2,757 (50.2%) |
3,016 (54.3%) |
| MDR TB identified, newly detected cases | 4,085 (12.9%) |
4,656 (13.6%) |
5,193 (15.5%) |
| MDR TB identified, relapse cases | 1,280 (24.8%) |
1,580 (28.8%) |
1,869 (33.7%) |
|
|
|||
SOURCE: Skachkova, 2010.
percent of culture-positive patients should be investigated. Also, with effective TB prevention, widespread drug susceptibility testing, and widespread treatment, the incidence of pulmonary MDR TB should not exceed 1.5 per 100,000 population, and prevalence should not exceed 9 per 100,000.
More than 90 percent of newly detected culture-positive TB cases are now investigated for drug susceptibility in the Russian Federation (Table 3-1). The percentage of newly detected cases with resistance to any drug has increased in recent years, to 36 percent in 2009, while the resistance to any drug among relapsed cases rose to 54 percent in 2009. MDR TB was identified in 15.5 percent of newly detected cases and in 33.7 percent of relapse cases.
Together, these trends point to an increase in the number of MDR TB cases over the past decade (Figure 3-3). This increase is related to the expansion of drug susceptibility testing and to improved investigation of drug-resistant TB. It is also due in part to an increase in the number of unsuccessfully treated patients and to a lack of directly observed treatment.
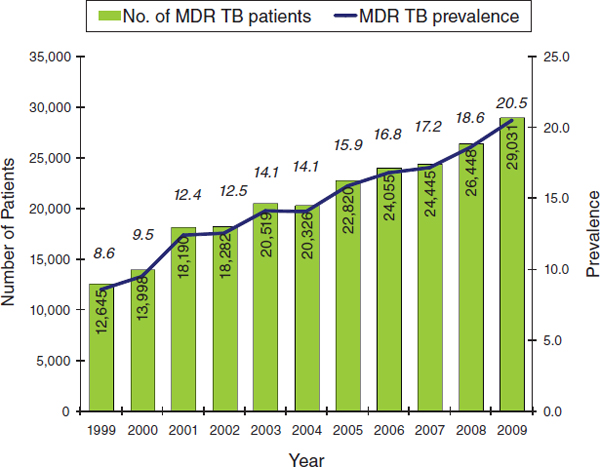
FIGURE 3-3 The number of MDR TB patients has continued to grow in the Russian Federation during the 21st century.
SOURCE: Skachkova, 2010.
Today a culture exam is performed in 97 percent of all patients. However, questions remain about the completeness and reliability of the resulting data since not all of the patients have positive culture results, and the quality of the samples is not 100 percent reliable.
Data from some parts of the Russian Federation also are not very reliable, according to Skachkova, especially where laboratory capacity is lacking. As this capacity is increased, incidence rates will increase as well. And with an overall incidence of MDR TB of 4 per 100,000 population, the rate of new cases remains significantly higher than the national goal of 1.5 per 100,000 population.








