The Institute of Medicine (IOM), in response to a request from the White House Office of National AIDS Policy (ONAP), convened a committee in 2009 to plan and conduct a series of three workshops and data gathering activities to evaluate barriers to expanded HIV testing and treatment programs. The committee’s first report focused on the extent to which federal and state laws and policies, private health insurance policies, and other factors inhibit or promote expanded HIV testing (IOM, 2010). This second report prepared by the committee examines how federal and state laws and policies and private health insurance policies and practices affect entry into clinical care and the provision of continuous and sustained care for people with HIV. The committee’s forthcoming third report will examine the current capacity of the health care system to administer a greater number of HIV tests and to accommodate new HIV diagnoses (see Box 1).
As part of its charge for this report, the Committee was asked to consider the following specific questions:
• How can federal and state agencies provide more integrated HIV care services?
• What policies promote/inhibit clinical care services among agencies at the federal level, at the state level, or between state and federal agencies?
• What are federal and state agency policies in funding HIV medication adherence programs? What HIV medication adherence programs work?
1. What is the extent to which federal, state, and private health insurance policies pose a barrier to expanded HIV testing? Issues for the committee to consider include
a. What are the current federal and state laws, private health coverage policies, or other policies that impede HIV testing?
b. What effective HIV testing methods and/or policies should be implemented by federal, state, or local agencies, federal programs, or private insurance companies that can be used to reach populations with a high HIV prevalence and/or high prevalence of undiagnosed HIV infection?
c. What has been the impact of opt-out HIV testing?
2. What federal and state policies and private insurance policies/practices (such as pharmaceutical coverage limits) inhibit entry into clinical care for individuals who test HIV-positive or inhibit the provision of continuous and sustained clinical care for HIV-positive persons? Issues for the committee to consider include
a. How can federal and state agencies provide more integrated HIV care services?
b. What policies promote/inhibit clinical care services among agencies at the federal level, at the state level, or between state and federal agencies?
c. What are federal and state agency policies in funding HIV medication adherence programs? What HIV medication adherence programs work?
d. Will insurance companies and other payors pay for the treatment of an HIV-infected person who tests positive in this theoretical new, expanded testing program, but whose CD4+ T cell count and/or viral load does not fall within the “official guidelines” of starting antiretroviral therapies?
e. What can be done to promote access to HIV treatment for HIV-positive individuals with CD4+T cell counts greater than “official guidelines”?
3. What is the current capacity of the health care system to administer a greater number of HIV tests and to accommodate new HIV diagnoses? Issues for the committee to consider include system, workforce, and private sector issues:
a. Where do HIV-positive patients currently get care?
b. What is the HIV-related training or experience of most HIV care providers (medical doctor, nurse practitioner, physician’s assistant, registered nurse)?
c. What manpower or training/experience improvements are needed to absorb more newly diagnosed HIV-positives from expanded HIV testing services?
d. Is the age profile of providers compatible with sustainability of the HIV care delivery system? That is, are younger clinicians and/or students receiving adequate training/experience to meet future needs?
e. What are the impediments to professionals entering into, or continuing to provide, AIDS care?
f. What policies inhibit or enhance the movement of health care professionals into HIV/AIDS specialties?
g. Are there adequate financial or professional incentives to promote HIV/AIDS as a specialty among the health care professions?
• Will insurance companies and other payors pay for the treatment of an HIV-infected person who tests positive for HIV, but whose CD4+ T cell count and/or viral load does not fall within the “official guidelines” of starting antiretroviral therapies?
• What can be done to promote access to HIV treatment for HIV-positive individuals with CD4+T cell counts greater than “official guidelines”?
The 15-member Committee on HIV Screening and Access to Care is composed of experts in the areas of HIV testing and care policy, HIV/AIDS ethics, epidemiology and biostatistics, HIV/AIDS clinical care, HIV/AIDS care services research, HIV care financing, state HIV/AIDS service programming and implementation, and the behavioral sciences (see Appendix A). The committee held its second public workshop, to explore the second part of its study charge, June 21–22, 2010, in Washington, DC. Invited experts discussed barriers and facilitators to HIV/AIDS care during the following five workshop sessions: (1) overview of clinical care and social service needs of persons with HIV/AIDS; (2) entry into and sustained HIV/AIDS care: the role of federal and state and private health insurance policies; (3) payment for treatment of earlier stage HIV infection; (4) the role of federal and state agencies in supporting integrated HIV care services; and (5) the impact of housing, mental health, and immigration policies on HIV/AIDS care access and retention (see agenda and biographical sketches of invited experts in Appendixes B and C, respectively).
This report is structured in response to the committee’s charge and includes a review of the evidence, where available, from policy documents and the research literature on federal, state, and private health insurance policies as potential barriers or facilitators to improved access to HIV/AIDS care. The committee addresses the question of how federal and state agencies can provide more integrated HIV care services (question 2a) following what it felt was the broader question about policies that promote or inhibit clinical care services among agencies at the federal level, state level, or between state and federal agencies (question 2b).
The committee has attempted to provide evidence supporting the assertions made by workshop speakers, but in some instances there is no research addressing these issues. Testimony provided by workshop speakers should be interpreted as opinion by knowledgeable individuals, unless supported by relevant studies.
HIV infection has been transformed from an unvaryingly fatal disease into a chronic disease. In high-income countries, survival for persons with HIV has improved in part due to improvements in therapy. For instance, the average survival time after HIV diagnosis based on surveillance data from 25 U.S. states increased from 10.5 years to 22.5 years from 1996 to 2005 (Harrison et al., 2010).1 Among HIV-positive persons on antiretroviral therapy (ART) in high-income countries, there have been notable declines in mortality rates and potential years of life lost between 1996–1999 and 2003–2005 (see Table 1) (Antiretroviral Therapy Cohort Collaboration, 2008).
In many settings, the success of antiretroviral therapy in significantly decreasing morbidity and mortality has been possible because of the provision of a comprehensive set of services to meet the particular needs of persons with HIV disease. The care of HIV-infected patients is complex, and subgroups of this population disproportionately face tremendous psychosocial problems, substance abuse, comorbid medical conditions, and poverty. Merrill Singer, University of Connecticut, defined a construct that he referred to as syndemics or “the concentration and deleterious interaction of two or more diseases or other health conditions in a population especially as a consequence of social conditions that promote disease clustering.” Singer emphasized the need to consider HIV/AIDS in the context of other diseases, mental health issues, social structures and environments, housing, and immigration status, especially for the disadvantaged and marginalized populations disproportionately affected by HIV/AIDS. A comprehensive, multidisciplinary approach to HIV/AIDS services is needed due to the complexity of issues implicated in the health of individuals with HIV/AIDS. Despite the improvements in health for people with HIV who are in care and on treatment, many people with HIV in the United States enter medical care with advanced disease, have inconsistent adherence, or discontinue therapy prematurely (Losina et al., 2010). Singer noted the importance of using a syndemics approach to find hidden populations of people with health and social burdens implicated in increased vulnerability for HIV, to help facilitate linkage to and retention in care, and to help reduce health disparities.
There is a lack of reliable, recent estimates of how many individuals who have been diagnosed with HIV/AIDS are receiving care (e.g., have a medical provider, are on antiretroviral therapy, or are receiving psychosocial and support services). One recent study that involved meta-analyses
__________________
1 Despite improvement in survival overall, disparities in survival time after HIV diagnosis persist. Estimated survival time after diagnosis for black males, for example, is about 20 years, compared with 26 years for white males (Harrison et al., 2010).
TABLE 1 Health Indicators for Overall (20 years or older) Population by Period of Follow Up
| Period of therapy initiation | 1996–1999 | 2000–2002 | 2003–2005 | ||||||
| Mortality rates (per 1,000 person-years) | |||||||||
| Overall | 16.3 (14.9-17.8) | 12.4 (11.5-13.2) | 10 (9.3-10.8) | ||||||
| Between the ages of 20 and 44 years | 13.1 (11.7-14.7) | 10.3 (9.4-11.2) | 7.5 (6.8-8.3) | ||||||
| Potential years of life lost before age 65 (per 1,000 person years) | |||||||||
| 20-64 years | 365.9 | 260.4 | 189.4 | ||||||
| Life expectancy (years; adjusted) | |||||||||
| At exact age 20 years | 36.1 (SE 0.60) | 41.2 (SE 0.52) | 49.4 (SE 0.54) | ||||||
| At exact age 35 years | 25 (SE 0.42) | 30.1 (SE 0.31) | 37.3 (SE 0.37) | ||||||
| Percent surviving from 20 to 44 years | 75.5% | 79.5% | 85.7% | ||||||
SOURCE: Adapted from Antiretroviral Therapy Cohort Collaboration, 2008.
of 28 studies involving 53,323 individuals looked at entry into care and retention in care (having multiple HIV medical visits) among individuals in the United States who were diagnosed with HIV. According to the study, 69 percent of those diagnosed with HIV entered HIV medical care averaged across the time intervals in the studies. Seventy-two percent had entered care within 4 months of diagnosis. With regard to retention in care, 59 percent had multiple HIV medical care visits during intervals from 6 months to 5 years (Marks et al., 2010). Another study found that, in 2003, only 55 percent of HIV-infected persons age 15 to 49 in the United States who were eligible to receive ART were in fact receiving ART (Teshale et al., 2005).
In addition to assessing how many infected individuals do not enter care, there is a need to consider the various points along the care continuum where individuals may fall out of care and the potential barriers and facilitators to care linkage and retention. If the goals of expanded HIV testing are to be met, it is important to ensure the availability of, and access to, care and treatment, as well as the continuity of care for those already linked in.
The focus of this report is policy-related barriers to entry into and sustained clinical care for individuals with HIV. A 2005 IOM report identified
Current public financing strategies for HIV care have provided care to and extended the lives of many low-income individuals. However, significant disparities remain in assuring access to the standard of care for HIV across geographic and demographic populations.
The current federal–state partnership for financing HIV care is unresponsive to the fact that HIV/AIDS is a national epidemic with consequences that spill across state borders. State Medicaid programs that provide a significant proportion of coverage for HIV care are dependent upon widely varying resources and priorities that produce an uneven and therefore ineffective approach to managing the epidemic.
Under the current patchwork of public programs that finance HIV care, many HIV-infected individuals have no access or limited access to the standard of care for HIV. Fragmentation of coverage, multiple funding sources with different eligibility requirements that cause many people to shift in and out of eligibility, and significant variations in the type of HIV services offered in each state prevent comprehensive and sustained access to quality HIV care.
Low provider reimbursement in Medicaid and managed care delivery systems has the potential to discourage experienced physicians from treating patients with HIV infection and to undermine the quality of HIV care.
SOURCE: IOM, 2005.
many policy-related barriers to access to the standard of care for HIV in the United States (IOM, 2005) (Box 2). The IOM committee faulted the public response to HIV and described a patchwork of public programs offering fragmented care and health care providers inadequately reimbursed for their services. Most of the barriers to care identified in the 2005 IOM report are still present today.
Jennifer Kates, Kaiser Family Foundation, noted that the health care financing and delivery system in the United States has gaps in access to care that vary by state. Problems in accessing care can be acute for the general population, but they are particularly onerous for individuals with HIV/AIDS who, as a group, are more likely to be poor and disadvantaged. On
March 23, 2010, President Obama signed into law the Patient Protection and Affordable Care Act (ACA) that extensively changes the way in which health care is financed and provided in the United States (P.L. 111-148). This section of the report provides an overview of federal and state programs and policies that affect access to HIV/AIDS care and how these programs may be affected by the recent health care reform.
Health Insurance Policies
Having health coverage is critical to gaining access to HIV/AIDSrelated care due to the high expense involved in medical management of the disease. Care for people with HIV may be covered through federal programs such as Medicaid, Medicare, the Ryan White program, and the Department of Veterans Affairs (VA); community health centers (CHCs); private health insurance; or a combination of programs.
There are no recent national estimates of health coverage of individuals with HIV. The HIV Cost and Service Utilization Study (HCSUS), for example, the only nationally representative study of people with HIV/AIDS in care, was conducted from 1994 to 2000.2 A recent analysis of data from a convenience sample involving 12 medical sites located in urban cities throughout the United States showed that the majority of patients were covered under Medicaid (42 percent, including those dually eligible for Medicare) and the Ryan White program (24 percent) (Table 2).3 These data likely do not represent the national picture of health coverage of individuals with HIV, however, such as those in non-urban areas.
__________________
2 HCSUS estimated that of the estimated 231,400 HIV-infected adults living in the contiguous United States at the time, 32 percent had private health insurance, 29 percent had Medicaid alone, and 20 percent had no insurance. Nineteen percent of patients had Medicare with or without other health insurance (Bozzette et al., 1998)
3 Data are from medical sites located in Baltimore, Maryland; Tampa, Florida; Dallas, Texas; New York City, New York (3 sites); Rochester, New York; Philadelphia, Pennsylvania; Detroit, Michigan; San Diego, California; Oakland, California; and Portland, Oregon.
|
|
|
| Insurance | Number of Patients (%) |
|
|
|
| Private | 2,585 (13) |
| Medicaid | 7,009 (36) |
| Medicare | 2,348 (12) |
| Medicaid & Medicare | 1,091 (6) |
| Ryan White/Uninsured | 4,580 (24) |
| Missing | 1,622 (8) |
| Total Number of Patients | 19,235 |
|
|
|
SOURCE: Analysis of data from K. Gebo and J. Fleishman, November 2010.
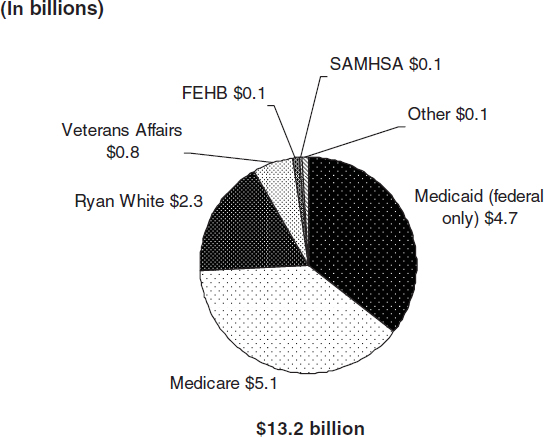
FIGURE 1 Federal funding for HIV/AIDS care by program, FY 2010 (in billions).
SOURCE: KFF, 2010f.
TABLE 3 Potential Eligibility Criteria for People with HIV/AIDS, by Major Payor/Source
| Medicaid | Medicare | Private | |||||||
| Employer | Individual | Ryan White | |||||||
| Who | Must be both low income and categorically eligible | Seniors or under 65 disabled | Job-based | Individual market-based | Low income and uninsured or underinsured | ||||
| Income/asset test | Yes | No | N/A—but costs involved | N/A—but costs involved | Yes | ||||
| U.S. citizen | Yes | Yes | Not necessarily | Not necessarily | No | ||||
| Preexisting condition limit | No | No | Some limits | Yes, in most states | No | ||||
| State variation | Yes | No | Yes | Yes | Yes | ||||
| Capped funding | No | No | Yes | Yes | Yes | ||||
| HIV-specific program | No | No | No | No | Yes | ||||
SOURCE: KFF, 2010e.
Federal and State Health Insurance Programs4
Medicaid Medicaid is the nation’s principal safety-net health insurance program and represents the largest expenditure on health coverage for people with HIV/AIDS when federal and state expenditures are combined. The program is a federal-state partnership, with each state and territory operating its own Medicaid program under broad, federal guidelines. Medicaid is a guaranteed entitlement to U.S. residents and documented immigrants, and federal funding is provided to match state funds for those eligible for coverage. In 2009, 47.8 million people were covered by Medicaid (DeNavas-Walt et al., 2010). An estimated 200,000–240,000 individuals with HIV/AIDS receive care through the Medicaid program (KFF, 2009a). Federal spending on Medicaid in FY 2010 is estimated at $275.4 billion,5 with an estimated $4.7 billion going to HIV care (KFF, 2009b), and additional state spending on HIV care is estimated at close to $4 billion (CMS, personal communication, September 2010).
Minimum eligibility requirements for Medicaid are set by federal law. To be eligible for Medicaid, an individual must be both low income and “categorically” eligible. There are several pathways to Medicaid coverage (Table 4). The large majority of persons with HIV on Medicaid qualify on the basis of being both low income and disabled, as determined by their eligibility for Supplemental Security Income (SSI) benefits. Because states have discretion in designing and administering Medicaid programs, there is considerable variation by state in eligibility, benefits, and other aspects of program. In addition to the mandatory groups that all states must cover to receive federal matching funds, there are optional eligibility groups that states can choose to cover and receive federal matching funds. For instance states have the option to offer eligibility for individuals with income above the threshold for the state (Table 4) (KFF, 2009a).
Income eligibility requirements for Medicaid vary greatly by state, and are often very restrictive. For instance, in 34 states, low-income parents must have incomes less than the federal poverty level (FPL) to be Medicaid eligible; in 17 states, incomes must be less than 50 percent of the FPL (KFF, 2009c).6 Programs and benefits also vary. For example, only 33 states and the District of Columbia have a program for individuals who are medically needy to serve people who have incomes that are too high to qualify for Medicaid but who are otherwise eligible (this is an optional program
__________________
4 This section is based primarily on the presentations of Jennifer Kates, Deborah Parham Hopson, Heather Hauck, and Andrea Weddle.
5 See http://origin.www.gpo.gov/fdsys/pkg/BUDGET-2011-TAB/xls/BUDGET-2011-TAB-16-1.xls.
6 The FPL is an income threshold that is used as a measure to determine eligibility for assistance through several federal programs.
TABLE 4 Medicaid Eligibility Pathways for People Living with HIV/AIDS
|
|
||
| Category | Criteria | Mandatory/Optional |
|
|
||
| SSI beneficiaries | Severely disabled and low income (standard 74% of FPL, varies by state) | Mandatory (11 “209B” states can have more restrictive eligibility) |
| Parents, children, pregnant women | Low income; income and asset criteria vary by category and state | Mandatory; states may offer higher income thresholds |
| Medically needy | Severely disabled and low income, after subtracting incurred medical expenses; income and asset criteria vary by state but generally well below SSI levels | Optional (33 states and the District of Columbia use this option for people with disabilities) |
| Workers with disabilities | Severely disabled; low income; for persons returning to workforce | Optional |
| Poverty-level expansion | Allows for income above SSI levels up to FPL | Optional |
| State supplementary payment | Allows for coverage of those receiving SSP | Optional |
|
|
||
SOURCE: KFF, 2009a.
under Medicaid) (KFF, 2009b), and 19 states have prescription drug limits (e.g., monthly or annual limits on the number of prescriptions) within their Medicaid programs (KFF, 2008).
Heather Hauck, Maryland Department of Health and Mental Hygiene, discussed how some but not all states have Medicaid expansion programs allowing coverage for non-disabled individuals. In addition, there is limited coverage for nonmedical services, such as case management and housing, under Medicaid. Medicaid data system limitations may restrict the ability of administrators to assess who is in care and the appropriateness and outcomes associated with that care.
Other barriers to access to Medicaid coverage include the onerous application process in some states; a restrictive definition of disability that excludes persons with HIV who do not have an AIDS diagnosis and who are capable of engaging in “substantial gainful activity” (although this will be alleviated with changes to categorical eligibility criteria that will no longer require an AIDS diagnosis/disability under the ACA); and limited beneficiary autonomy in choosing a care provider (Rawlings and Hopson, 2009).
Andrea Weddle, HIV Medicine Association (HIVMA), indicated that Medicaid reimbursement rates are a barrier to HIV clinic sustainability. According to recent estimates, Medicaid rates for primary care average 66 percent of Medicare rates and range from 47 percent (California) to 140 percent (Alaska) (Zuckerman et al., 2009).7 In general, the rates increased by 15.1 percent from 2003 to 2008; however, the consumer price index increased by 20.3 percent during this period. Weddle mentioned that states that have greater coverage of benefits tend to have lower provider payment rates. Low provider reimbursement rates have been shown to hinder access to care for Medicaid beneficiaries in particular (IOM, 2005).
Medicaid coverage of HIV testing is discussed in the committee’s first report (IOM, 2010). States must cover all medically indicated/physician ordered HIV tests, but states have the option to cover routine HIV screening.
Medicare Medicare is the federal health insurance program for individuals who are age 65 and older and individuals under age 65 who are disabled. Medicare provides coverage to 47 million Americans (KFF, 2010c), including an estimated 100,000 people with HIV/AIDS (KFF, 2009b). Medicare spending in FY 2010 is estimated at $515 billion with $5.1 billion in expenditures for HIV/AIDS (KFF, 2009e). The program has four parts:
1. Part A covers hospital stays, skilled nursing care, facility stays, home health care, and hospice care (automatically provided if eligible);
2. Part B covers physician payments, outpatient services, preventive services, and home health care (those eligible for Part A may enroll);
3. Part C covers Medicare Advantage (voluntary enrollment in private health plans, such as a health maintenance organization); and
4. Part D covers prescription drugs and low income subsidies (voluntary enrollment).
Most individuals with HIV who qualify for Medicare do so because they are disabled (see Table 5 for Medicare eligibility criteria). Medicare beneficiaries may choose to purchase coverage from a selection of competing private plans to cover prescription drugs under Medicare Part D. The cost sharing under Medicare Part D can be problematic for individuals with HIV who qualify on the basis of disability and are receiving Social Security Disability Insurance (SSDI) assistance. Cost-sharing may put pressure on AIDS Drug Assistance Programs (ADAPs), state-run programs funded
__________________
7 However, there have been recent reductions in provider reimbursement rates under Medicare.
TABLE 5 Medicare Eligibility Pathways for People Living with HIV/AIDS
|
|
|
| Category | Criteria |
|
|
|
| Individuals age 65 and over | Sufficient number of work credits to qualify for Social Security payments |
| Individuals under age 65 with permanent disability | Sufficient number of work credits to qualify for SSDI payments due to disability; eligible for Medicare after receiving SSDI payments for 24 months |
| Individuals with end-stage renal disease or Lou Gehrig’s disease of any age | Sufficient number of work credits to qualify for SSDI; eligible for Medicare as soon as they start receiving SSDI payments (no waiting period) |
|
|
|
SOURCE: KFF, 2009b.
through Ryan White that provide access to medications for low-income and under or uninsured individuals with HIV who cannot afford out-of-pocket expenses for prescription drugs under Medicare Part D (Rawlings and Hopson, 2009).
In addition to the limitations on drug coverage, individuals under age 65 must wait 24 months following their disability determination and the initiation of receipt of SSDI before Medicare coverage begins. Also, Medicare benefits are based on income history, which may not reflect current need (Rawlings and Hopson, 2009). Furthermore, many HIV patients do no have sufficient work history, nor have they accumulated sufficient work credits to qualify for needed benefits. On the other hand, provider reimbursement tends to be higher under Medicare than Medicaid (IOM, 2005), resulting in more providers being willing to provide care for patients eligible for Medicare or dually eligible patients, than for patients who only have Medicaid. Coverage of HIV testing through Medicare is discussed in the committee’s first report (IOM, 2010). A new policy for annual voluntary HIV screening for those at increased risk for HIV, as well as voluntary screening for pregnant women during the third trimester of pregnancy and at labor, was issued in December 2009. Persons who request an HIV test despite reporting no individual risk factors could also be tested under the policy, since this group is likely to include individuals not willing to disclose high-risk behaviors.8
The Ryan White Program The Ryan White program is the only federal grant program designed specifically for people with HIV/AIDS. The pro-
__________________
8 See CMS decision memo CAG-00409N.
gram is estimated to support services for approximately 530,000 HIV-infected people each year (GAO, 2009b). Federal spending on Ryan White is estimated at $2.3 billion in FY 2010 (KFF, 2009e). The program has several parts:
1. Part A provides funding to cities (Eligible Metropolitan Areas [EMAs] and Transitional Grant Areas [TGAs]);
2. Part B provides funding to states, including an ADAP earmark;
3. Part C provides funding to public/private organizations for the provision of health services;
4. Part D provides family-centered care involving outpatient or ambulatory care for women, infants, children, and youth with HIV/AIDS; and
5. Part F provides funds for several programs such as Special Projects of National Significance (SPNS), AIDS Education & Training Centers (AETCs), dental programs, and the Minority AIDS Initiative (MAI).
Ryan White is considered the payor of last resort for individuals with HIV/AIDS. Most clients are low income; more than 70 percent have annual household incomes at or below the poverty level. Most clients are uninsured or underinsured and are people of color (KFF, 2009d). Ryan White is a discretionary program dependent on annual federal, and in some cases state and local, appropriations. Funding is provided, based on formulas, to Part A, B, C, and D grantees, with most of the funding going to states and cities. The program often serves as a wrap-around program to pay for medications and services (e.g., case management, transportation) that are not covered by other funding sources. As such, it is considered a lifeline in terms of providing needed services for people with HIV/AIDS. Ryan White services are tailored to the needs of local communities, and therefore there is considerable variation in services that are available across jurisdictions (Rawlings and Hopson, 2009). A constant amidst the variation is that Ryan White programs are limited to HIV-related outpatient services. Inpatient hospital stays and emergency department visits are not covered. Also, there is only a limited panel of covered specialist providers, and coverage for their services extends only to HIV-related issues. In addition to lack of coverage for inpatient or emergent services, one consequence of these limitations is the need for primary care providers to serve also as default cardiologists, nephrologists, hepatologists, and the like, for their Ryan White funded patients.
Hauck noted that additional resources for Ryan White Part B (ADAPs) and Part D (family-centered care) are needed to expand clinical services. The restrictions on uses of Ryan White funding for core medical services
versus support services9 reduces local flexibility to address client needs. In addition, Hauck stated that federal guidance is lacking on criteria for states to receive supplemental (Part B) Ryan White funding.
Several workshop participants expressed concern about the unmet need for ART medications through the Ryan White ADAP program. As of December 9, 2010, there were 4,543 individuals on ADAP waiting lists in 9 states. An additional 18 states have implemented cost-containment measures (e.g., reduced formularies, lowered financial eligibility, capped enrollment, and implementation of cost sharing) (NASTAD, 2010). Hauck described the problem of state ADAP formularies that are missing critical classes of drugs for mental health, cardiovascular, and gastrointestinal conditions and the various distribution methods for ADAP medications (e.g., direct order, clinic pick up, ADAP pharmacy only, any pharmacy), some of which pose barriers to clients.
Ryan White funds are limited due to the discretionary nature of the program and often are not sufficient to support the care needs of HIV-infected individuals. In some areas (e.g. suburban, rural) there may be very few or no resources available to people with HIV through the Ryan White program. The complexity and burden of the application process for a Ryan White grant, as well as award conditions that carry administrative requirements related to issues such as quality management, may make it easier for large organizations with more resources to obtain funding (Rawlings and Hopson, 2009).
Weddle highlighted the importance of medical case management in client entry into and retention in care. Medical case management facilitates entry into care for those who are newly diagnosed, especially when colocated or integrated with the HIV medical care team. Case management is a key strategy for coordinating care and assisting patients with meeting a range of medical, psychosocial, and basic living needs. Ryan White currently is the principle source of funding for case management for people with HIV/AIDS, but other sources of support are needed. Estimates indicate that case management for people with HIV is covered by approximately 25 percent of Medicaid programs (HRSA, 2004).
Ryan White funds can be used to support diagnostic and laboratory HIV tests. Testing must be considered “integral to the treatment of HIV infection and related complications.”10
__________________
9 Ryan White grantees receiving funds under Parts A, B, and C must spend at least 75 percent of funds on “core medical services,” such as outpatient and ambulatory health services, pharmaceutical assistance, substance abuse outpatient services, oral health, and other services. Remaining funds may be spent on support services such as outreach, medical transportation, language services, respite care for persons caring for people with HIV/AIDS, and referrals for health care and other support services (HRSA, 2010a).
10 See HAB policy notice 07-02: ftp://ftp.hrsa.gov/hab/PN07-02.pdf.
Department of Veterans Affairs The Department of Veterans Affairs, Veterans Health Administration (VHA) is the largest single provider of HIV care in the United States. Federal spending on veteran’s medical care in FY 2010 is estimated at $46.2 billion,11 with an estimated $0.8 billion going to HIV care (KFF, 2010f).To date, nearly 64,000 veterans with HIV have received care in the VHA system. In 2008, more than 23,000 veterans with HIV were served, representing about 1 of every 250 veterans in care. The number of veterans with HIV in care has been relatively stable over the past several years (VA, 2009a).
The VHA provides comprehensive care to a population with complex care needs and prevalent comorbidities, including heart disease, diabetes, cancers, depression, hypertension, and hepatitis C. Veterans who meet certain criteria for character at discharge and length of military service can apply for care through the VHA, which is available for free to those who qualify (VA, 2009b). Veterans with service-connected disabilities (disabilities that arose while in service) including HIV are eligible for compensation benefits through the Veterans Benefits Administration and are entitled to VHA care and other benefits such as preference in federal/state employment and job retention rights.
As of August 2009, the VHA’s policy on HIV testing includes HIV testing as part of routine medical care. Verbal informed consent for testing is considered sufficient, and pre- and post-test counseling are no longer required.12
Federally Qualified Health Centers Federally Qualified Health Centers (FQHCs) are located in or serve a high need community (designated as a Medically Underserved Area (MSA) or population). They provide comprehensive primary health care services as well as supportive services (e.g., education, translation, and transportation that promote access to health care). FQHC services can be used by anyone, with fees adjusted based on ability to pay. FQHCs include CHCs, Migrant Health Centers, Healthcare for the Homeless, and Public Housing Primary Care Programs.13
In 2009, there were 427,797 encounters in CHCs, representing 94,972 patients with HIV/AIDS. CHCs are important testing sites. In 2008, they administered 753,801 HIV tests (HRSA, 2009).
__________________
11 See http://origin.www.gpo.gov/fdsys/pkg/BUDGET-2011-TAB/xls/BUDGET-2011-TAB-16-1.xls.
12 See VHA Directive 2009-036: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=2056.
13 There are also FQHC look-alikes that have been identified by the Health Resources and Services Administration (HRSA) and certified by CMS as meeting the definition of “health center” under Section 330 of the Public Health Service Act, although they do not receive grant funding under Section 330.
Hauck pointed out that state grantees receiving support from the Health Resources and Services Administration (HRSA) through both the Ryan White program and the FQHC program serve many of the same populations, but there is little coordination at the federal level, aside from that among CHCs that are also Ryan White Part C or Part B funded programs. Not all CHCs provide HIV testing and HIV/AIDS care, and Hauck pointed out that in high HIV and viral hepatitis incidence areas, comprehensive HIV and viral hepatitis testing and care should be provided by CHCs in coordination with state HIV/AIDS programs. This has led some to call for the need for a Policy Information Notice (PIN) from HRSA to provide guidance to these CHCs to expand access to HIV testing and care. In September 2010, HRSA issued such a notice to FQHC program grantees specific to HIV testing in health care settings to provide information on the Centers for Disease Control and Prevention’s (CDC) Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings (CDC, 2006) and resources for training and technical assistance to help health centers follow the revised recommendations.14 A similar notice has not been issued on care for persons with HIV.
High Risk Insurance Pools For some individuals, an insurer of last resort is a state-run, high-risk insurance pool that provides health insurance coverage for individuals who are otherwise uninsurable, for example, because they have a preexisting condition such as HIV. Many states have a high-risk insurance pool (NASCHIP, 2010). However, state high-risk insurance pool policies and practices may pose barriers for those without insurance coverage from other sources. Monthly premiums within such pools can be prohibitively expensive, and although Ryan White funds may be used to pay for premiums, this arrangement can be difficult to make.
Private Health Insurance
Fewer than one in five individuals with HIV (17 percent) are estimated to be covered by private health insurance (HHS, 2010). Coverage for care under private insurance varies depending on state insurance laws. Kates stated that 18 states impose rating limits on insurers providing coverage to individuals. In states without such limits, insurers can vary premiums according to an individual’s health status or other attributes. Health insurance sold in the individual market on a “guaranteed issue” basis cannot exclude applicants based on health or risk status. Only 6 states require insurers to offer individuals coverage on a guaranteed issue basis for all products (7 other states have this requirement for selected products).
__________________
14 For further information see http://bphc.hrsa.gov/policy/pal1013/pal1013.pdf.
For individual health insurance policies, there may be a pre-screening application that may exclude coverage for preexisting conditions like HIV disease, although the preexisting condition insurance plan recently implemented under the ACA has already begun to eliminate this exclusion until the broader coverage provisions take effect in January 2014. Caps on benefits, cost sharing for prescription drugs, and co-payments for visits with providers under private health insurance may require that individuals with HIV resort to other programs to supplement payment for their HIV care (IOM, 2005).
Forty-six percent of insured individuals with below average incomes went without needed care (Schoen et al., 2010). Insured individuals may struggle or be unable to cover the costs associated with premiums, co-pays, deductibles, and costs of services, such as vision and dental, that are not covered by their plans (Perry et al., 2009). Private insurance policies often have limits on services needed by those with HIV/AIDS (e.g. substance abuse treatment, mental health treatment, case management, specialty care).
Insurance Policies and Access to Expert HIV Care Providers
Evidence indicates that care provided to HIV-infected individuals by medical providers who specialize or have significant experience in HIV care is better than care provided by non-specialists or providers with limited exposure to HIV patients. Although further research is needed, studies conducted in the 1990s and early 2000s demonstrated that patients cared for by physicians, nurses, and other providers who are experienced in the care of individuals with HIV are more likely to have positive treatment outcomes, be prescribed antiretroviral therapy appropriately, and receive more cost effective care (Bozzette et al., 2001; Kitahata et al., 1996; Landon et al., 2003; Wilson et al., 2005).
A requirement that federal payors include HIV medical clinicians in their provider networks would improve access to such clinicians and improve outcomes according to Weddle. This could be accomplished through having contracts with HIV providers or allowing “any willing provider” into the networks.
In general, insurance plans could allow HIV providers to serve as primary care providers. In California, plans can create a standing referral to an HIV provider (State of California Department of Managed Care, 2010). Another way to facilitate care by an HIV specialist is to allow beneficiaries to have direct access to HIV specialists (i.e., eliminate gatekeepers).
Weddle discussed the importance of having access to other specialists as well. She described how insurers ideally would support robust, coordinated, and integrated provider networks to treat the full range of issues affecting people with HIV. Available specialists might include endocrinolo-
gists, psychiatrists and other mental health professionals, gynecologists, gastroenterologists, cardiologists, nephrologists, hematologists/oncologists, dermatologists, and hepatologists. A number of factors can limit access to these and other specialists: reimbursement, including limited access to specialist care under Ryan White funding; specialist availability; and the provider’s level of knowledge and comfort with treating HIV disease.
Health Care Reform and Access to Health Insurance for Persons with HIV/AIDS
Kates discussed how the ACA will expand access to care for millions of Americans who are currently uninsured, including people with HIV/AIDS. According to a recent Kaiser Family Foundation study, Medicaid expansion will significantly increase the number of people covered by the program and markedly reduce the number of uninsured individuals in states across the country, with the federal government picking up the majority of cost (KFF, 2010b). States with large uninsured populations today are expected to see the biggest increases in Medicaid coverage.
Medicaid will be expanded to all individuals under age 65 with incomes up to 133 percent of the FPL as of 2014 (there is a state option to begin enrollment as of April 1, 2010). There will be a uniform minimum Medicaid eligibility threshold across states. The categorical eligibility criteria that have prohibited most low-income adults, including those with HIV/AIDS without dependent children, from enrolling in the program will be eliminated. As is the case under current law, undocumented immigrants still will not be eligible for Medicaid coverage under the ACA (KFF, 2010a). Uninsured individuals with incomes greater than 133 percent of FPL will be able to obtain coverage through newly created state health insurance exchanges.
The Medicare program provides coverage for the elderly and individuals under the age 65 who are disabled. Under the ACA, there will be an end to the Medicare Part D drug benefit coverage gap (referred to as the “doughnut hole”) by 2019. ADAP payments will count toward the true out-of-pocket threshold used to determine eligibility for catastrophic coverage under Part D. Kates highlighted the improvement in coverage of prevention benefits under Medicare. As of 2011, there will be no coinsurance or deductibles charged in traditional Medicare for preventive services that are rated A or B by the U.S. Preventive Services Task Force (USPSTF).15
Kates mentioned that private health insurance eligibility and coverage will change under health care reform. The ACA requires guaranteed issue and renewability of policies. This means that health insurers will be prohibited from denying coverage for any reason, including health status, and
__________________
15 The USPSTF has assigned a rating of C to routine HIV screening.
also from charging people more for their policies based on health status and gender. Until these reforms are in place, a temporary (from 2010 to 2014) national high-risk pool has been established to meet the needs of those with preexisting conditions. As of 2010, young adults are able to remain on their parent’s health insurance plan up to age 26.
In terms of coverage, Kates described how the ACA will end annual and lifetime limits for those with private insurance coverage. Insurers offering individual or group plans will also have to provide coverage and may not impose any cost sharing requirements for evidence-based preventive services (e.g., those rated A or B by USPSTF).
As part of health care reform, a Prevention and Public Health Fund was established, with an initial appropriation in 2010, to expand and sustain funding for prevention and public health programs. The fund includes support for federal, state, and community initiatives to use evidence-based interventions to address HIV-related health disparities.
Although the ACA will expand access to health insurance and provide new protections for individuals with private coverage, some individuals still will not gain access, such as undocumented immigrants, who will continue to be excluded from Medicaid coverage (KFF, 2010a). There will be a host of implementation challenges, and until the reforms are in place, the coordination of existing programs will be critical. Of concern is the possibility that routine HIV screening will not be covered under the ACA, which runs counter to the recent efforts to expand HIV testing in the United States. The ACA relies on the recommendations of the USPSTF, which do not currently recommend routine HIV screening. Uncertain also is the role of the Ryan White program following implementation of health care reform.
Under the ACA, there are opportunities to expand access to providers experienced in the care of individuals with HIV. Weddle described how health plans operating in state-based exchanges beginning in 2014 will be required to contract with essential community providers, such as those eligible for reduced drug pricing under section 340B of the Public Heatlh Service Act,16 including FQHCs, FQHC look-alikes, and HRSA grantees, such as Ryan White programs.17 It is not yet known whether plans will proactively contract with Ryan White providers and whether the Ryan White programs will be prepared to negotiate contracts and then have the capacity to bill and respond to administrative requirements of private plans (e.g., stricter utilization management requirements). Weddle expressed the concerns of HIVMA over the way in which the health care reform increases Medicaid payments to primary care physicians for 2013 and 2014, but
__________________
16 Public Health Service Act §340B; 42 U.S.C. §256b.
17 The Patient Protection and Affordable Care Act. SEC. 1311: Affordable choices of health benefit plans.
TABLE 6 Odds of Recent Needle Use Among Persons Living with HIV
| Housing Status | NYC Cohort | National Sample | |||||||
| Rate (%) | Adjusted Odds Ratioa | Ratioa Rate (%) | Adjusted Odds Ratioa | ||||||
| Stable housing | 4 | — | 4 | — | |||||
| Unstable housing | 12 | 2.87 | 13 | 2.51 | |||||
| Homeless | 17 | 4.74 | 27 | 4.65 | |||||
aOdds of needle use in the past 6 months by current housing status controlling for demographic characteristics, economic factors, risk group, health status, mental health, and receipt of health and supportive services
All relationships statistically significant; p < .01
SOURCE: Aidala et al., 2003, 2005.
leaves out those HIV physicians who are infectious disease specialists but also provide primary care to their patients.18
Housing Policies
David Holtgrave, Johns Hopkins Bloomberg School of Public Health, described a large body of evidence on the relationship between homelessness and HIV infection. Studies conducted among persons who were homeless or unstably housed in New York City, Philadelphia, and San Francisco, for instance, have shown HIV seroprevalence rates several times higher than that seen in the general population (Culhane et al., 2001; Kerker et al., 2005; Robertson et al., 2004). Housing status is also associated with greater prevalence of HIV-related risk behaviors such as injection drug use and unsafe sex among HIV-infected individuals (Aidala et al., 2005, 2006; Kidder et al., 2007). For example, Table 6 shows the increased odds of recent needle use among HIV-infected individuals in New York City and in a national sample who were either stably or unstably housed or were homeless.
Stably-housed individuals with HIV also may be better able to attend to their health than those who are homeless or unstably housed. A systematic review of studies found a significant positive association between stable housing and improved health care and social service use and adherence to antiretroviral medications. Stable housing also correlated with significant benefits in terms of improved health status and a reduction in HIV risk behaviors (Leaver et al., 2007). Stable housing appears to improve the
__________________
18 Health Care Education and Reconciliation Act of 2010 (P. L. 111-152). www.gpo.gov/fdsys/pkg/PLAW-111publ152/content-detail.html.
survival of people living with HIV/AIDS. Short-term mortality was associated (adjusted hazard ratio 2.92, CI 1.32, 6.44) with recent homelessness, according to one longitudinal study conducted from 1996 to 2005 among 595 individuals living with HIV and alcohol challenge (Walley et al., 2008).
The Housing Opportunity for People with AIDS (HOPWA) program in the Department of Housing and Urban Development provides states and localities with funding to support housing assistance and related services for people living with HIV/AIDS (HUD, 2010b). Ninety percent of HOPWA funding is distributed through a program that uses a statutory formula that relies on AIDS statistics (cumulative AIDS cases and area incidence) from CDC, and 10 percent of HOPWA funds are awarded as grants under a competitive selection of projects proposed by state, city, and local governments or by nonprofit organizations (HUD, 2010b). Holtgrave discussed increased appropriations in 2010 from 2008 levels ($335 million vs. $300 million) for HOPWA (HUD, 2010a), and the proposed funding for 2011 is $340 million (White House, 2010). HOPWA projects that provide permanent supportive housing exceeded the goal that 85 percent of those receiving housing assistance would achieve housing stability in FY 2009 (HUD, 2010b).19 Yet it is estimated that more than 125,000 households have an unmet need for AIDS housing services (NAHC, 2010). Holtgrave asserted that expanded access to HUD and other housing supports for people living with HIV are among the actions needed to meet the National HIV/AIDS Strategy (NHAS) objective to increase access to care and improve health outcomes for people living with HIV (ONAP, 2010).
Holtgrave mentioned the value of the National AIDS Housing Coalition as a source of data on the effectiveness of housing programs in addressing HIV/AIDS. He testified that the evidence indicates that there are many negative consequences of homelessness, including high medical care costs. People who are homeless have many barriers to health care generally, but use acute care services (e.g., emergency rooms) at high rates (Larimer et al., 2009). “Housing First” policies, where the housing needs of individuals are met before attempts are made to address other service needs, such as substance abuse treatment and mental health care, may help to offset costs of care for homeless individuals (Gilmer et al., 2009; Larimer et al., 2009; Sadowski et al., 2009).
Despite the persistent correlation between housing status and better health care access and health outcomes, there have been few randomized clinical trials to study whether housing is causally linked to improvements in health and health outcomes (Kidder et al., 2007). Holtgrave reviewed
__________________
19 This assessment was made for the 23,862 households that benefited from HOPWA permanent housing projects (HUD, 2010a).
the results of a recent randomized clinical trial, the Chicago Housing for Health Partnership (CHHP) study, that followed 407 homeless individuals who were chronically ill with HIV/AIDS or other conditions for 18 months following discharge from the hospital. The immediate provision of supportive housing following hospital discharge (in contrast to usual care, that is, a piecemeal system of emergency shelters, family, and recovery programs) resulted in significant cost savings (Sadowski et al., 2009). For every 100 persons housed, there were 49 fewer hospitalizations, 270 fewer hospital days, and 116 fewer emergency department visits. Reductions in avoidable health care utilization translated into cost savings for the housed participants, even after taking into account the cost of the supportive housing.
A sub-study of the CHHP involving 94 participants with HIV examined the impact of supportive housing on HIV disease progression. Compared with 34 percent of participants with HIV who were randomized to usual care (discharge planning usually provided to homeless individuals during a hospital stay), 55 percent of participants who received permanent housing with intense case management were alive and had “intact immunity” (CD4 ≥ 200 and viral load <100,000) after one year. In addition, the participants randomized to housing and case management were much more likely to have an undetectable viral load (36 percent) compared with those who did not receive these services (19 percent) (Buchanan et al., 2009).
A second randomized trial, the Housing and Health Study, was designed to study the causal effects of providing rental housing to homeless or unstably housed individuals with HIV on physical health, access to medical care, treatment adherence, HIV risk behaviors, and mental health status, using data gathered at baseline and 6, 12, and 18 months (Kidder et al., 2007). The 630 participants were randomized into two groups: the treatment group received immediate HOPWA rental housing assistance with case management and the control group received “customary housing services with case management.” The researchers hypothesized that the “treatment” group, which received immediate rental housing, would demonstrate improvement in all areas, as well as a decrease in HIV risk behaviors, over the control group (Wolitski et al., 2010). Results of the study were complicated by the fact that at 18 months 51 percent of the control group had acquired stable housing, which limited the significance of the results. In an effort to offset this occurrence, data for individuals who had experienced 1 or more nights of homelessness during the study period were compared with those for individuals who had not (Wolitski et al., 2010).
Despite the challenges encountered by the study, the results did show that participants’ mental health, especially perceived stress, was positively affected by housing stability. The findings pertaining to the effect of stable housing on physical health were less consistent, although the results of the as-treated analyses showed that individuals who experienced homelessness
during the study period were more likely to report one or more emergency department visits in the past 6 months (49 percent vs. 29 percent) and more likely to have a detectable viral load (79 percent vs. 61 percent). There was no difference found between the two groups in terms of HIV risk behaviors (Wolitski et al., 2010). Additional longitudinal studies are needed to assess more definitively the direct and indirect effects of housing stability on the physical health of HIV-infected individuals.
On May 20, 2009, President Obama signed into law the Homeless Emergency and Rapid Transition to Housing (HEARTH) Act. The act includes a number of measures to improve efforts to reduce homelessness and housing insecurity that are likely to benefit persons with HIV, including a change in HUD’s definition of homelessness and chronic homelessness and the establishment of a Rural Housing Stability Program.20
Policies Affecting Immigrants
Undocumented immigrants tend to have poor access to health care, and there are very low rates of testing for HIV/AIDS among immigrants who have not yet acculturated to the United States. Catalina Sol, Chief Programs Officer of La Clínica del Pueblo in Washington, DC, described a number of the barriers to HIV/AIDS care experienced by immigrants. These include
• a lack of linguistically and culturally appropriate, geographically accessible services, especially mental health services;
• a lack of access to health care;
• culturally mediated health beliefs and attitudes related to knowledge of disease;
• stigma associated with HIV/AIDS and identification as an immigrant;
• conflicts between work status and medical care (many immigrants have more than one job);
• instability/lack of availability of housing (ineligibility for federal housing programs);
• transient residence, often related to fluctuations in the regional job market; and
• a lack of family/support structures.
Sol described how being an undocumented immigrant could diminish access to care for HIV-infected individuals. An increasing focus on legal immigration status has created difficulties for immigrants as they try to interact with police, law enforcement, and state/government entities. In
__________________
20 For more information see http://www.hudhre.info/documents/S896_HEARTHAct.pdf.
many jurisdictions, undocumented immigrants may not be able to obtain the basic documents (e.g., social security number) necessary to gain employment, obtain a driver’s license, open a bank account, rent or purchase a home, or access safety net services. Due to reduced ability for legal recourse, undocumented immigrants are also vulnerable to unfair practices in the workplace, such as underpayment and unsafe working conditions. Many immigrants have a work permit, which is a legal document that helps with identification, but it is temporary, often misunderstood, and confers no benefits.
With some exceptions, “non-qualified” immigrants (i.e., those who do not meet certain eligibility requirements, including those who are undocumented) are prohibited from enrolling in federal public benefit programs, such as Medicaid (except for emergency care), Medicare, Temporary Assistance for Needy Families, and the like (1996 Welfare law, 8 U.S.C. 1613).21 Legal immigrants (green card holders) who entered the United States on or after the date the Welfare law was enacted also generally are not eligible for public benefits until they have been in residence in the United States for 5 years, at which time they can apply for U.S. citizenship or naturalization.22 States have attempted to fill in some of these coverage gaps. About half of states spend their own money to cover at least some immigrants who are ineligible for federal services, and some states or counties provide health coverage to children and/or pregnant women regardless of their immigration status (Broder and Blazer, 2010).
A 22-year ban on entry into the United States of HIV-infected individuals was lifted in January 2010. Until then, HIV testing was necessary to initiate the application for legal resident status. Sol stated that even without the ban, immigration policy poses multiple barriers to “entry” for low-income immigrants living with HIV. Immigrants must have family-based sponsorship, meet certain employment criteria, or be considered under provisions for asylum or refugee status. Considerations of whether an individual will be a public charge or burden to society are taken into account. In addition to barriers imposed by federal policies, some states have imposed restrictions on access to services for immigrants.
Sol stated that although immigrants with HIV, including those who are undocumented, may be eligible for the Ryan White program, the process for determining eligibility for Ryan White services can be difficult. Eligibil-
__________________
21 The qualified immigrant category includes lawful permanent residents (persons with green cards); refugees, persons granted asylum or withholding of deportation/removal, and conditional entrants; persons granted parole by the Department of Homeland Security for a period of at least 1 year; Cuban and Haitian entrants; certain abused immigrants, their children, and/or their parents; and certain victims of trafficking (Broder and Blazer, 2010).
22 This period is shortened to 3 years if the individual is married to a U.S. citizen or 4 years if permanent residency was received through asylum.
ity workers are not immigration experts and may be confused about legal access to care. The perception among immigrants that they are not eligible for any services may keep them from seeking care. In some communities there is a growing hostility toward immigrants, which in some cases is reinforced by public policies. Service providers are often confused, fearful, and unsure of how to proceed lawfully. In addition, the geographic movement of many immigrant workers in response to fluctuations in the regional job market may hinder their ability to apply for and receive services.
Legislation focusing on immigration reform might address some of these barriers to care. Service providers could: (1) inform their immigrant clients of the availability of Ryan White services; (2) examine how their organizations or facilities may be discouraging or excluding immigrants unnecessarily; (3) limit questions about immigration status to those necessary to determine eligibility; (4) assuage the fears of immigrant patients; and (5) make alliances with community-based organizations that work with immigration issues and inform them of the special needs of HIV-positive patients.
Undocumented immigrants will continue to be excluded from Medicaid under the ACA, but implementation of this exclusionary policy will be very difficult. The immigration status of individuals within a single family may be very different. A father may have a green card, a mother may be undocumented, and a child born in the United States could have citizenship. Eligibility workers will have a difficult time determining who can gain access to Medicaid and who may purchase health insurance on the exchanges that will be set up. From a human rights and a public health perspective, such exclusionary policies are ill advised. With many immigrants being excluded from coverage under the ACA, the preservation of the Ryan White program is essential because it provides a safety net for individuals with HIV/AIDS regardless of their immigration status.
Correctional System Policies
Given that 1.5 percent of prison inmates are HIV positive or have confirmed AIDS diagnoses (Bureau of Justice Statistics, 2009) and an estimated 15 percent of HIV-infected individuals have contact with the correctional system (Hammett, 2009; Hammett et al., 2002), the provision of HIV/AIDS care within the U.S. correctional system is important. Individuals who are incarcerated in jails and prisons are eligible for health care, but HIV/AIDS care is often absent, incomplete, or not coordinated with care that the inmate received prior to admission to the correctional system or that is available upon release. Becky White, University of North Carolina, Chapel Hill, described how sources of health care coverage are discontinued or suspended upon entry into jail or prison. Model programs have shown that
individuals can be routinely tested for HIV at entry into the correctional system, cared for during incarceration, and linked to follow-up care post release. To succeed in providing comprehensive care, funding is necessary, bureaucratic obstacles must be overcome, and collaboration must be forged between correctional and community-based care systems. It is also crucial to ensure that confidentiality and nondiscrimination policies are in place to protect the well-being of individuals diagnosed or treated in a correctional facility (Seal et al., 2010).
White stated that jails and prisons represent the only sector of society where health care is a constitutionally guaranteed right. However, this right often is not fully exercised because the provision of health care is not the primary goal of the correctional system. Furthermore, even when it is a priority, health care delivery is compromised by inadequate funding and staffing, as well as by policies or practices that may deter inmates from seeking care.
Figure 2 shows the cycle of incarceration and release (and sometimes reincarceration) in relation to jail health care, prison health care, and community health care. Some individuals with short sentences only serve time in jails and then are released, while others with longer sentences may transition through the prison health care system before being released. Release from prison is associated with a significant increase in the risk of death, especially during the first 2 weeks following release, when, in one study, the adjusted risk of death among recently released Washington state inmates
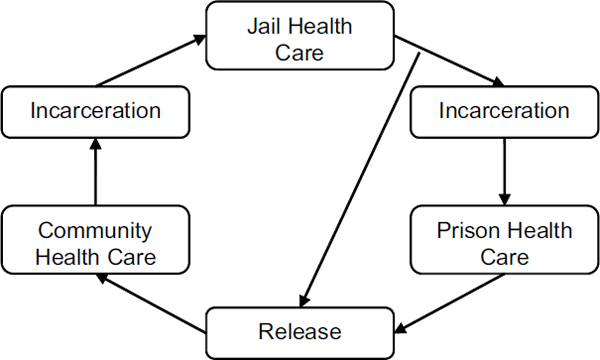
FIGURE 2 Cycle of incarceration and release and relation to health care.
SOURCE: Adapted from Zaller et al., 2009.
was 3.5 times that among other state residents, due in part to renewed substance abuse (Binswanger et al., 2007). A comprehensive approach to correctional health transitions is important, making maximum use of the links to community-based health care and public health systems.
White described several barriers to entry into care that individuals may face as they leave the general community to enter jail. There may be no policy for routine screening for HIV or other infectious diseases, especially in smaller jails with limited resources. Inmates may refuse testing because of concerns about disclosure and a general distrust of the correctional health care system. Jails are characteristically understaffed and must contend with a high turnover of inmates (half of inmates are released within 72 hours). Some jails have no, or very limited, HIV screening/testing policies. These difficulties may not be experienced in very large jails. For example, jails in Los Angeles County, California, and Cook County, Chicago, Illinois, have a medical director available to oversee jail health care. Many states, however, have a jail in almost every county and limited access to medical resources.
Even for individuals identified as HIV positive at entry into jail there are several barriers to receiving HIV care, such as understaffing, poor HIV-related knowledge among staff, and short jail stays. Upon entry into the correctional system, other sources of health care coverage are discontinued or suspended, including Medicare, Medicaid, ADAPs, the VA, and private insurance. The correctional health care system follows a “sick-call” model of care, designed to address prisoners’ acute care needs during specified hours. To further complicate matters, HIV care sites may be located far from jails, making it logistically difficult to transport prisoners to care. Also, prisoners may fear discriminatory treatment or loss of confidentiality.
Inmates with longer sentences generally are sent to prison where the barriers to entry into care are similar to those seen in jails (e.g., disclosure issues, understaffing, lack of HIV screening). There are additional logistical issues to address in prisons because inmates are often moved from prison to prison, which necessitates them having to re-establish relationships with nurses, providers, and a new prison system.
White stated that there are approximately 70 prisons in North Carolina, and prisoners are moved an average of four times during their sentence. Most counties in North Carolina have a jail, which is under the jurisdiction of the county sheriff whose primary duties do not include health care. To overcome barriers in the correctional system, the state has put in place a system to identify HIV-positive individuals at entry, facilitate entry into care during incarceration, and promote follow up for HIV care post release. To accomplish these goals, the state correctional system has instituted a medical/social intake process that includes routine HIV testing and has employed 11 nurse case managers to engage inmates in care.
Some facilitators of continuity of care in prisons include
• availability of specialized staff, such as HIV nurse case managers, HIV specialists (e.g., academic, public health, private, correctional staff), and HIV pharmacists;
• policies in place for treatment according to guidelines;
• effective non-discrimination and confidentiality policies; and
• financial resources to ensure access to ART.
Continuity of care following release can be compromised because often the application processes for Supplemental Security Income, Medicaid and/or ADAP may not be started until close to the time of release. White described how notification of benefit determination may occur after release, making it difficult to link clients to medical care. In many instances, there is limited access to inmates by community-based organizations that could assist with discharge planning and linkages to care. The consequences of discontinuity of care are evident from a study in North Carolina of 15 individuals who left jail, but were later incarcerated. Most of the recidivists had markedly increased viral loads at readmission to jail (Stephenson et al., 2005).
When HIV-infected individuals are released from prison, there is generally no easily accessible system of care for them. Consequently, these individuals often rely on emergency departments for care. White stated that an important means of facilitating continuity of care at release from jail or prison is collaboration between the community and correctional facilities. The case managers hired by the North Carolina corrections department also provide discharge planning upon release (with 30 days of ART) and address issues related to homelessness, mental health, and substance abuse. There is considerable variability in continuity of antiretroviral therapy and HIV care following release from prison or jail (i.e., care within 30 days of release) according to the research literature. Recent studies of persons with HIV released from Texas prisons found major interruptions in treatment following release, with only 30 percent of prisoners filling a prescription for ART within 60 days (Baillargeon et al., 2009) and only 28 percent enrolling in an HIV clinic within 90 days (Baillargeon et al., 2010). The SPNS Project Bridge program provided 18 months of intensive case management to ex-offenders in Rhode Island. More than 90 percent of prisoners in the program received medical care within 6 months of release from prison (Zaller et al., 2008). In another study, 65.1 percent of ex-offenders with HIV who received intensive case management after release attended a routine medical appointment within 4 weeks of release, compared with 54.4 percent of ex-offenders who had standard of care prison-administered discharge planning (Wohl et al., 2010). These projects demonstrate that successful
collaborations can be forged between correctional and community-based care services.
Policies Affecting Care for Mental Health Problems and Substance Abuse
The prevalence of certain mental illnesses and substance abuse is disproportionately high among persons with HIV (Bing et al., 2001). As Evelyn Tomaszewski, Senior Policy Advisor, National Association of Social Workers, discussed, ample evidence exists to support the need for psychosocial services for individuals with HIV/AIDS:
• 26 percent of clients living with HIV experience some form of anxiety disorder within a 12-month period (Gaynes et al., 2008);
• More than 12 percent of adults with HIV screened positive for drug dependence in the previous year (Bing et al., 2001); and
• 13 percent of adults with HIV have co-occurring substance abuse and mental illness (Beckett et al., 2007).
Many people living with HIV are likely to benefit from interventions to assist them in coping with the emotional and cognitive impact of HIV/AIDS (Lutgendorf et al., 1998). In addition, persons living with HIV/AIDS often must contend with psychological and/or physical abuse, poverty, and domestic violence.
Programs and funding are needed that promote cross-disciplinary models and parity between medical and mental health interventions. There is a great need to build provider capacity and capability. The perception of who constitutes the health workforce must be reframed and broadened to include behavioral and mental health care providers. Opportunities are needed for behavioral and mental health professionals and allied health professionals to develop skills that view and address HIV through a health and behavioral health lens. Comprehensive health services are necessary, including behavioral health screening and treatment, with a focus on community-based interventions. In particular, client education and outreach are essential.
There are large gaps in coverage for mental health and substance abuse treatment for persons with HIV/AIDS. Both private and public mental health coverage are generally inadequate. Two-thirds of primary care providers report they are unable to get outpatient mental health care for patients (Cunningham, 2009). Likewise, coverage of substance abuse treatment is generally poor. This likely will improve, however, following the implementation of the new mental health parity law and the ACA. Mental health and substance abuse treatment will be part of the “essential benefits” package for plans operating in the state-based exchanges in 2014. Medicaid
coverage of supportive community-based services is generally better than coverage from private plans.
Providers may lack clear understanding of the definitions of “medical” services employed among various agencies. There can be confusion about whether mental health and substance abuse services, or assessment and early intervention services, are considered medical services under some programs. Tomaszewski stated that some service providers, for example, do not understand what a “core” medical service is under the Ryan White program. It may be the case that although the definitions are clear, the education of providers regarding what is, and is not, reimbursable has not been adequate. Funding, such as that provided under SAMHSA’s National MAI, primarily supports mental health, while less support is used to fund substance abuse treatment and prevention.
Federal and State Policies and Procedures That Facilitate Care Linkage and Retention
Federal and state agencies have implemented a number of initiatives that address structural barriers within the health care system as well as other barriers to connecting persons with HIV to care. For instance, as part of the SPNS, HRSA has developed initiatives to evaluate the effectiveness of focused interventions to improve timely entry into and retention in care for underserved populations and women of color. HRSA also has produced “Connecting to Care” workbooks for HIV service providers that highlight successful methods that organizations are using to connect or re-connect HIV-positive individuals to care. HRSA provides grants under Part C of the Ryan White Act to public and private nonprofit organizations to help connect individuals with HIV to care. State and local health departments also have implemented programs that allow case managers to assist with making care appointments, linking with ADAPs, and locating assistance for housing and substance abuse treatment (GAO, 2009a).
CDC, HRSA, and several states have implemented successful programs to assist HIV-positive persons in their transition from prison and jails back to the community, including continued care and treatment (GAO, 2009a). Using CARE Act or state funds, several state health departments have established programs to partner with their state department of corrections to help prisoners transition back to the community (GAO, 2009a). These include the nationally recognized “Project Bridge,” which has been extremely successful in linking prisoners to medical care upon release (97 percent of participants received medical care during the first month of their release from prison). Inadequate funding, state budget cuts, and availability of housing are among the threats to the continuation of these programs (GAO, 2009a).
HOW FEDERAL AND STATE AGENCIES CAN PROVIDE MORE INTEGRATED HIV CARE SERVICES
As discussed throughout the report, persons with HIV/AIDS often have a variety of medical and social service needs that require the use of support and ancillary services to provide comprehensive care, optimize health outcomes, and prevent HIV transmission. Individuals with HIV often must navigate a confusing set of programs to access care and, once in care, face numerous barriers to staying in care. For low-income individuals especially, gaining access to care can take time and result in treatment delays. Since the HIV epidemic has evolved and the clinical needs of the population have changed, questions have arisen on how best to structure programs.
Stewart Landers, John Snow, Inc., described levels of systems integration for HIV/AIDS services that may be facilitated by federal and state agencies, including
• integration with services for other closely related infectious conditions, such as sexually transmitted infections (STIs), viral hepatitis, and tuberculosis;
• integration with case management, mental health and substance abuse treatment, transportation, translation services, and dental care;
• integration with “upstream” services that impact social determinants of health, such as housing, education, job training, legal services, and refugee and immigrant services; and
• integration into mainstream health care, in particular, the chronic care model.
In terms of federal support for network development, Landers described how the Ryan White program has adopted a model that supports care through networks, for example through Part A EMAs and their planning councils. A study of 42 Part A EMAs found perceived quality and availability of services to be high for primary care and case management, but lower for other services (i.e., mental health, substance abuse, transportation, housing, dental, translation/interpretation) (Hirshhorn et al., 2009). Both primary care providers and case managers reported high levels of contact with each other, but grantee (county and city governments) support for communication between them was not rated highly (Hirshhorn et al., 2009). Patient navigators are effective in maintaining patients in care and increasing the number of contacts that clients have with both medical and support service providers (Bradford et al., 2007).
Categorical vs. Flexible Funding Mechanisms
Categorical grants can be spent for specifically defined purposes. Categorical federal funding programs have been developed for HIV/AIDS, in part, because of the history and origins of the epidemic. A targeted response occurred with the emergence of HIV/AIDS as a new infectious disease in the early 1980s. Now that the epidemic is more than 30 years old, questions have arisen about whether the model of care that has emerged should be maintained and protected in the post-health-care-reform era, or whether HIV/AIDS care should be integrated into the general health care system.
There is much to be said for the current model. In many ways, health care for HIV/AIDS, with its focus on the provision of associated psychosocial services, may be an appropriate model of care not only for individuals who are poor and disadvantaged, but also for those who are otherwise marginalized or stigmatized and have other health disparities. It could be argued that the care models that have evolved, largely as a result of Ryan White funding, should be maintained for HIV-infected individuals and expanded so that they are available for patients with other complex chronic conditions.
The success of this model of comprehensive HIV/AIDS care can be observed in encouraging findings from New York City, where nearly 90 percent of HIV-infected individuals are estimated to be seen at least once annually (personal communication, Michael Horberg to Judy Aberg, New York University, as reported to New York City Department of Health and Mental Hygiene, December 2009). The successes in New York City can be traced to the labor intensive, “hands on” approach applied there.
Kevin Lindamood, Healthcare for the Homeless, stated that disadvantages of disease-specific funding include fragmentation and the potential for creating disparities in care between those with and without the disease. HIV-specific funding could foster two standards of care, one for those who are HIV-infected and one for those who are not, despite the fact that both groups may suffer the same set of comorbidities and psychosocial problems. For example, two individuals, both disadvantaged, could be treated differently in a clinical setting based on their HIV-infection status. The HIV-infected individual could be eligible for a bus token through a HIV/AIDS-supported program, while the other individual would not be eligible. Health departments, when they have attempted to integrate services, have coordinated HIV/AIDS programs with those addressing STIs, hepatitis C, and tuberculosis. From an outreach, prevention, and screening perspective, the integration works well. However, integration is made difficult because of the two-tiered elements of care available for those eligible or not eligible for nonmedical support services through Ryan White funding.
In the face of inefficiencies and fragmentation within the health care
system, providing states with uncategorical funding to design their own systems might make sense. A 2005 IOM report addressed this question, and experience suggests that there are advantages and disadvantages to such a “block grant” approach (IOM, 2005). To overcome the problems associated with categorical funding streams, consideration could be given to having explicit language in notices of grant awards allowing and encouraging flexibility in their use. By federal law, 75 percent of parts A, B, and C of Ryan White funding must be used for core medical care services, including outpatient and ambulatory health services; pharmaceutical assistance; substance abuse outpatient services; oral health; medical nutritional therapy; health insurance premium assistance; home health care; hospice services; mental health services; early intervention services; and medical case management, including treatment adherence services (HRSA, 2010a). The remaining 25 percent of funding may be used for supportive services, defined as “services needed to achieve outcomes that affect the HIV-related clinical status of a person with HIV/AIDS,” including outreach; medical transportation; language services; respite care for persons caring for individuals with HIV/AIDS; and referrals for health care and other support services (HRSA, 2010a). This restriction limits providers’ flexibility to address client needs. Once the ACA is implemented and more clients are covered by Medicaid, Ryan White funds may be more appropriately directed to the provision of supportive services. There is concern that if the “75 percent” rule remains in place, providers will not have the flexibility to use resources where they are most needed.
There currently is wide variation in coverage within state Medicaid programs, although there will be less variation after implementation of the ACA when the national floor for income eligibility will be set above that currently employed by many states. Ryan White funds will be essential for filling in gaps in Medicaid coverage where variation continues to exist after this change, and for those who still have incomes too high to qualify for Medicaid.
As noted previously, there is interest in evaluating the integration of HIV care with that for STIs, viral hepatitis, and tuberculosis. Landers cited a model to integrate HIV and hepatitis C care being studied at the University of California, San Francisco. Reductions in state funding may force disease-specific programs to integrate. Health care reform in Massachusetts reduced/eliminated stand-alone STI and tuberculosis clinics and has integrated them into HIV counseling and testing programs. Landers described how pilot programs supported by the federal government could encourage service integration. Such programs could integrate services for individuals with related infectious diseases (e.g., HIV, STI, hepatitis C, tuberculosis), or certain risk groups or populations (e.g., gay/bisexual/MSM; incarcerated population; refugees/immigrants).
Factors Affecting Providers’ Ability to Provide Comprehensive, Integrated HIV/AIDS Care
Reimbursement23
Clinicians The number of clinicians interested in providing HIV/AIDS care is declining due to economic disincentives and the aging of the HIV/AIDS workforce (HRSA, 2010b). Increased emphasis on and better training opportunities in HIV medicine, and perhaps appropriate financial incentives, are needed to encourage and better prepare younger physicians, nurses, and physician assistants to practice HIV medicine, whether as specialists or as primary care providers.24 Some states have developed reimbursement policies that better support HIV/AIDS care. New York’s Medicaid program, for example, has enhanced reimbursement rates for HIV care under fee-for-service plans and has developed special HIV capitated rates under managed care programs, with additional payments available for mental health care, substance abuse treatment, and other related services.
Under the ACA, Medicaid payment rates to primary care physicians (family medicine, general internal medicine, or pediatric medicine) for furnishing primary care services in 2013 and 2014 will be at least 100 percent of Medicare payment rates under both fee-for-service plans and managed care plans (H.R. 4872, Sec 1202), but infectious disease specialists who provide primary care to HIV/AIDS patients will not be able to benefit from these advantageous primary care provider reimbursement policies.
There are reimbursement policies that better support HIV care. Those available within fee-for-service plans include cost-based reimbursement (as in FQHCs); payments for providing a coordinated, comprehensive “medical home”; and enhanced rates for HIV care (e.g., as in New York’s Medicaid program). Under managed care, risk-adjusted capitation rates or special HIV rates can provide adequate reimbursement. In New York’s Medicaid Managed Care’s Special Needs Plan, there is an HIV rate of $1,328 per member per month (base rate). Payments above the base rate may be generated through the creation of “carve outs,” in which certain services, such as prescription drugs, laboratory monitoring, and mental health and substance abuse programs, are paid for separately.
New York developed a prospective payment system for its Medicaid managed care program using an Ambulatory Patient Group (APG) methodology. APG assignment is based on standard claims information. Separate payments have been created for: chemotherapy drugs and certain other
__________________
23 This section of the report is based, in part, on the presentation of Andrea Weddle.
24 Issues surrounding the capacity of the HIV/AIDS workforce to expand HIV/AIDS care services are addressed in detail in the forthcoming third report of the Committee on HIV Screening and Access to Care.
injectable medications; HIV counseling and testing; therapeutic visits for designated AIDS centers; HIV resistance testing; and other services (e.g., laboratory testing for blood factors).
Community Health Centers CHCs have experienced flat Ryan White payments at the same time as they have experienced increased patient volume following expansions of HIV screening programs. There are concerns related to the limited number of infectious disease providers available and also clinic capacity to effectively maintain access to care. In one Maryland county, there is a 6-week wait before an HIV-infected individual can be seen in a CHC. Increases in federal funding of HIV care through the Ryan White Act are used to purchase HIV medications. Medications are necessary, but represent just one component of the complex of care needed by HIV-infected individuals. Under the ACA, CHCs will receive $11 billion over 5 years.
It is of some concern that not all CHCs are providing HIV testing and HIV/AIDS care. Although a Policy Information Notice from HRSA recently was provided to CHCs on the issue of HIV testing, one is still needed regarding expanding access to HIV/AIDS care services. In high HIV and viral hepatitis incidence areas, comprehensive HIV and viral hepatitis testing and care could be provided by CHCs in coordination with state HIV/AIDS programs.
Reporting Requirements
Representatives of community-based organizations often report to health departments, and they also must meet the reporting requirements of HRSA, SAMHSA, CDC, and other sources of support. Several workshop participants noted that the reports required by different funding agencies are often substantial. Although greater emphasis could be placed on the reporting of clinical outcomes such as CD4 counts and viral load, the reporting burden associated with state and federal funding programs is often related to processes of care (e.g., use of ancillary providers, dietary interventions, psychological services, etc.) that may have minimal value in isolation or not lead to changes in clinical endpoints. In addition, the substantial staff and equipment requirements often needed to submit detailed reports to funding programs may be particularly burdensome to low volume clinics that are relatively understaffed and may not have the computer resources, staff expertise, or Internet connectivity required.
Even within agencies, there can be disparate data collection and dissemination requirements. These reporting issues may reflect a lack of program integration. State grantees receive support from HRSA’s HIV/AIDS
Bureau and the Bureau of Primary Health Care to serve many of the same populations, but there is little coordination between bureaus, other than that between CHCs that are also Ryan White Part C or Part B funded programs. Harmonizing reporting requirements and streamlining the data collection and dissemination requirements across agencies, especially HRSA, CDC, and SAMHSA would reduce the reporting burden for clients, clinics, health departments, and community-based organizations.
Other reporting issues arise due to confusion regarding the meaning of certain terms. There are requirements from both CDC and HRSA, for example, for health departments to provide evidence that linkages to care are being enhanced. However, the ways in which linkages to care are defined and measured differ by agency, and funding streams within individual federal agencies, making reporting on this metric difficult.
Although reporting requirements may be burdensome, there is recognition that data on people with HIV disease and their care need to be current and of high quality. In the present data environment, there are few good estimates of how many HIV-infected individuals are in care, and if in care, are on antiretroviral treatment.
In terms of federal support for data collection, Landers stated that support for information technology (IT) by local government grantees is limited. According to one survey, slightly more than 70 percent of medical directors and case management directors thought there was adequate support for integrated IT. Less than half of these respondents said that common intake forms are supported by grantees (Hirschhorn et al., 2009). This lack of coordination leads to duplicative and redundant reporting. Investments in electronic medical record systems would help to facilitate the reporting of processes of care and outcomes to funding programs.
Training
Workshop participants discussed the need for clinician education on the role of state health departments in identifying individuals with HIV/AIDS and linking them to care to help bridge communication gaps that may exist between clinical and public health providers. Federally sponsored professional training programs, such as AETCs, including those at HRSA, SAMHSA, and CDC, further providers’ understanding of the role of health departments in surveillance, control of HIV-related infectious diseases (e.g., STIs, hepatitis, tuberculosis), and community-based health education and prevention. Additional public health content could be included in training programs. The benefits of cooperation and coordination between primary care providers and health departments in routine testing for HIV and linkage to care could be highlighted.
Health Care Reform
Under the ACA and health care reform there may be opportunities to provide more comprehensive systems of care. States will be able to experiment with pilot programs and models for medical homes. Landers stated that emphases likely will be placed on the use of interdisciplinary teams, case managers, patient navigators, and other nonclinical providers. In addition, the prospect of investments in electronic medical record systems could facilitate the systematic inclusion of treatment protocols into care. With the influx of more individuals into the care system, concerns regarding the implementation of health care reform include the potential for reductions in safety net services, such as those offered through the Ryan White program. Landers pointed out that in Massachusetts, with the perception of “full coverage” under its version of health care reform, lawmakers reduced funding for services directed to STIs, tuberculosis, family planning, sexual assault, and health promotion. Other barriers to HIV care and HIV care integration under health care reform may include co-pays, deductibles, premiums, and other out-of-pocket costs; shortages of primary care providers; lack of support for case managers, interpreters, and patient navigators (newly insured individuals may have particular difficulties navigating the system) (Fairchild, 2009); and equity for ethnic minorities, non-English speaking individuals, immigrants (documented and undocumented), and persons/families with low incomes.
HIV MEDICATION ADHERENCE PROGRAMS
Failure to adhere to a recommended medication regimen, including medication for HIV, can have negative consequences for patients, providers, and society. Promoting HIV medication adherence maximizes the benefits of treatment for HIV-positive persons and probably reduces viral load at the population level. The consequences of poor adherence include faster disease progression, greater potential to infect other persons through risk behaviors such as unprotected sex and intravenous drug use, and the possibility of drug resistance and elimination of a drug for future use.
In the United States, published reviews of studies on overall medication adherence estimate that 20 percent to 80 percent of patients do not adhere to medical therapies, including medication regimens, with the range in estimates reflecting inconsistency in definitions, methods, and aspects of adherence studied (Gellad et al., 2009). Adherence with ART for HIV has become somewhat easier over time given the advent of drugs that are better tolerated and easier to take. One meta-analysis of studies reporting adherence to prescribed medical treatment showed a mean adherence rate of 88 percent for HIV disease, compared with 68 percent for diabetes and 77 percent
for cardiovascular disease, although the number of studies on adherence to treatment for HIV disease was low relative to studies on adherence to treatment for other conditions (DiMatteo, 2004). Differences in adherence can be accounted for by expected or factual efficacy or regimen complexity (DiMatteo, 2004), among other factors. Compared with other chronic conditions, individuals with HIV disproportionately face challenges such as drug addiction, poverty, physical and psychiatric comorbidities, stigma, and the like, that may make it more difficult for them to adhere to medication.
Several workshop participants described the many barriers to adherence to HIV medication and how those barriers can differentially impact rates of adherence among subpopulations. In addition to policy and financial factors, it is important to note that barriers to adherence may be clinical in nature (e.g., side effects), social (e.g., non-disclosure of HIV status, lack of social support, unstable housing, language barriers, illiteracy), or psychological (e.g., denial, depression, stress) (Applebaum et al., 2009; Gellad et al., 2009; Mills et al., 2006; Royal et al., 2009). Some studies have described an association between stigma and low levels of ART adherence (Rintamaki et al., 2006; Vanable et al., 2006).
Federal and State Agency Policies in Funding HIV Medication Adherence Programs
Deborah Parham Hopson, Health Resources and Services Administration, described federal funding for HIV medication adherence programs through the Ryan White program. HRSA supports treatment adherence services through funding for “core medical services” offered under Ryan White Parts A and B. In 2009, slightly more than $104 million of Part A Ryan White support and slightly more than $60 million of Part B Ryan White support were directed to medical case management, which includes treatment adherence. Nearly $405,000 of Part A MAI25 allocations went to treatment adherence counseling. HRSA also provides funding to ADAP programs (another core service under Ryan White Parts A and B), which provide free medications to individuals with HIV who cannot afford to pay for them. Parham Hopson noted that ADAP support can be used to increase access to medication, improve adherence, and monitor progress on therapy, although certain requirements must be met in order to use ADAP support for these purposes. Some states have met these requirements and $15.7 million of ADAP support in 2009 was directed to adherence-related
__________________
25 The Minority AIDS Initiative is part of the Ryan White HIV/AIDS Program (Parts A and B) and provides funding for activities to evaluate and address the disproportionate impact of HIV/AIDS on racial and ethnic minorities.
services. In addition, nearly $7 million of MAI Part B dollars went toward increasing access and adherence to medications.
Wayne Duffus, South Carolina Department of Health and Environmental Control, described the Public Health Service Act, section 2615 (HAB Policy Notice 07-13), which stipulates that no more than 5 percent of a state’s ADAP funding (or 10 percent under extraordinary circumstances, for example, meeting the needs of homeless individuals and substance abusers) can be used for services to
• enable access to medications;
• support adherence to the medication regimen; and/or monitor progress in taking medications.
• monitor progress in taking medications.
In order to use ADAP dollars for these purposes, states must provide comprehensive coverage of ART and medications for opportunistic infections. In addition, they cannot limit access to ADAP (i.e., no client waiting list or limits on enrollment; no restrictions or limitation on HIV medications; ongoing administrative support). Many states have waiting lists and have had to prioritize providing basic access to medications rather than using limited resources for adherence programs. As of December 2010, nine states had ADAP waiting lists and a number of other states had implemented cost containment measures (NASTAD, 2010).
The structure of state ADAP programs also can influence the feasibility of providing adherence services. Based on an informal survey of ADAP programs in nine states and consultation with the National Alliance of State and Territorial AIDS Directors (NASTAD), Duffus described factors that may facilitate robust state adherence programs. These include co-location of HIV/AIDS clinics and pharmacies, good communication between health departments and pharmacies, client-centered pharmacies (e.g., option for mail order filling of prescriptions), electronic medical record systems to track patients and alert providers of episodes of noncompliance (e.g., failure to pick up a prescription), and the availability of staff to monitor adherence and provide adherence counseling and interventions. In addition, some states have used their surveillance systems to provide information on adherence (e.g., CD4 counts, viral load). States that have Board of Pharmacy rules that do not restrict who within a state can perform duties related to medication monitoring give programs flexibility in staffing adherence positions.
Duffus stated there are no state policies and no Board of Pharmacy rules that prohibit the implementation of an adherence program. However, Board of Pharmacy rules may limit who can perform duties related to medication monitoring. Treatment adherence services vary widely across state and Ryan White programs. From a system perspective, Duffus mentioned
financial issues, including limitations on the use of Ryan White resources (Part B only vs. Part A and Part B) and ADAP waiting lists and other cost containment measures. When contract pharmacies are used to distribute medication, including adherence monitoring as part of service delivery can be too costly for states. In the face of limited financial resources, Duffus said that states are put in the position of having to choose between providing medications and providing services.
Duffus called for additional funding to implement and sustain adherence programs. He indicated that adherence models are needed for states, for individual providers, and for case managers. Adherence monitoring at the patient-provider level needs to be distinguished from that at the health department, population level. The dissemination of best practice guidelines would be beneficial in this regard. States also could benefit from clear advice and direction on how best to use the data that are collected. ADAP integration with HIV surveillance could provide lab data (e.g., CD4, viral load, genotypes) that could be helpful in adherence monitoring. Consideration also could be given to the use of other measures of adherence, for example, mortality, community viral load, and community resistance.
Committee member Beth Scalco discussed how the Louisiana Department of Health uses surveillance data to monitor adherence. Viral load and CD4 counts are reported, and if there is an interruption in care lasting more than a year, a disease intervention specialist contacts the individual. In addition, if a client with a lengthy interruption in care enters a public hospital, a flag is raised in their system. Scalco commented that there are issues regarding intrusiveness and overstepping patient’s rights. She mentioned the dilemma of out-of-care patients refusing interventions and the difficulties in defining the ongoing responsibility of the health department in such situations.
Andrea Weddle outlined a series of prescription drug policies that represent challenges to adherence, including the existence in some state Medicaid programs of monthly drug limits, preferred drug lists or formularies, and requirements for prior authorization (Table 7).
Cost Sharing and Adherence
Weddle noted that 14.9 percent of Americans reported in 2007 that they had not seen a doctor in the past year due to cost (KFF, 2010d). Although not HIV specific, systematic reviews of cost-related non-adherence in the United States have found that increased prescription drug cost sharing is associated with lower levels of initiation of prescriptions, poorer adherence, and more frequent discontinuation of medication (Gibson et al., 2005; Goldman et al., 2007). Consumer cost sharing impacts recipients both of private and of public health coverage. Increased co-payments and/or
TABLE 7 Prescription Drug Policies: Challenges to Adherence
|
|
||
| Policy | Examples | How to Improve It |
|
|
||
| Monthly drug limit | Mississippi Medicaid-5 drug limit, 2 brand name limit | - Exemptions for special populations, such as people with HIV -Exemptions authorized by clinician |
| Preferred drug list or formularies | Medicare Part D Most Medicaid programs Most private plans | - Carve out or exempt certain drug classes -Exemptions authorized by clinicians - Require coverage of all drugs in certain classes, e.g., Medicare Part D’s 6 protected classes requirement |
| Prior authorization | Medicare Part D | -Simplify and standardize process - Extended authorization, e.g., approve for 1 year - Strict and enforced response time requirements |
|
|
||
decreased income may influence patients’ ability to pay for medications and thus their adherence to treatment regimens. One review estimated that drug spending decreased by 2 to 6 percent for each 10 percent increase in cost sharing by patients, although for some chronic conditions (e.g., diabetes, lipid disorders, schizophrenia) cost sharing was associated with increased use of medical services (Goldman et al., 2007). Little is known about the influence of increased cost sharing on ART use or clinical outcomes in HIV-infected patients in the United States specifically. One study of the impact of implementation of the Medicare Part D prescription drug benefit, which required increased consumer cost sharing, found that ART interruptions were six times higher among homeless and marginally housed individuals (N = 125) with Part D coverage. Most participants who reported treatment interruptions cited an aspect of the Medicare Part D prescription drug program as a reason for the interruption (Das-Douglas et al., 2009). International studies that have looked specifically at patient payment for prescription drugs for HIV have found an adverse impact on follow up and adherence (e.g., Zachariah et al., 2008).
Medication Adherence Interventions to Improve HIV Treatment Outcomes
David Bangsberg, Harvard University, described some very simple interventions that can improve medication adherence. Pillbox organizers, for example, have been shown to improve adherence and reduce viral
load. In one study, the use of a pillbox improved adherence by 4.1 to 4.5 percent and was associated with a decrease in viral load (0.34–0.37 log10 copies/mL) and a 14.2 percent to 15.7 percent higher probability of achieving a viral load ≤400 copies/mL (odds ratio, 1.8–1.9). At less than $5.00 per pillbox per month, the intervention is considered to be extremely cost-effective and a standard of care (Petersen et al., 2007). A similar intervention is the “bubble pack” packaging provided by some pharmacies; each pack contains the pills required for each dose. Although likely to be less cost-effective than a pillbox, bubble packaging may be better suited to some populations. Other research conducted among homeless and marginally housed individuals, a population expected to have adherence problems, indicates that a single (versus multiple) tablet regimen leads to much better adherence and viral suppression (Bangsberg and Deeks, 2010).
Bangsberg described three meta-analyses/systematic reviews of randomized clinical trials (RCT) that have evaluated the effectiveness of adherence interventions (Amico et al., 2006; Simoni et al., 2006, 2010). The overall effects of the interventions are significant, with an odds ratio of 1.5 (CI 1.16-1.94) in favor of the intervention in terms of achieving a 95 percent level of adherence (Simoni et al., 2006). These reviews indicate that the most effective adherence interventions are interactive, open-ended, and multidisciplinary (e.g., involving a pharmacist, case manager, physician, family/partner). In addition, the most successful interventions include multiple sessions and focus on education, use behavioral skill development, target motivation/cognition/expectations, and include reminders. Interventions tend to have the greatest effect on those who are least adherent at the beginning of an intervention. Bangsberg stated that a challenge for adherence interventions is that their effects do not last much beyond the intervention. Sustaining behavioral change is difficult. Case managers and adherence nurses are effective in building relationships that foster adherence. The effect of more recent interventions may be less likely to show a beneficial effect on patient viral load because of the use of more potent therapies that more effectively reduce viral loads.
Table 8 highlights findings from five RCTs examining the effectiveness of interventions to improve ART adherence. These studies were included in the meta-analyses/systematic reviews previously mentioned.
Directly administered antiretroviral therapy (DAART), where a health care provider witnesses a patient swallowing his or her pills, has received attention as a strategy to improve adherence with ART. Although available evidence does not support the use of DAART for the general population (Ford et al., 2009; Wohl et al., 2006), it has been found to be effective for active drug users and those subject to methadone maintenance who are at higher risk for non-adherence (Altice et al., 2007; Lucas et al., 2004; Macalino et al., 2007). The effects of DAART do not appear to last much
| Author | Subjects | Intervention | Findings | ||||||
| Weber et al., 2004 | 60 HIV-positive individuals | Cognitive behavior intervention on adherence to ARV | No improvement in adherence, but effective in preventing a decline in adherence | ||||||
| Remien et al., 2005 | 215 Serodiscordant MEMS couples (eligible if percent adherent) | Four structured discussion/education sessions about adherence, problem solving to overcome barriers to adherence, and couple communication exercises to optimize partner support | Focus on partners improved HIV medication adherence in terms of medication behaviors and viral load over a 6-month period | ||||||
| Reynolds et al., 2008 (ACTG 731 study) | 109 HIV-positive individuals | Weekly telephone calls by nurses to elicit patient perspectives and address each individual’s biological, social, and cultural situation | Improved adherence and worked particularly well for those with lower levels of literacy; utilized nurses who are well trained and widely available in different clinic settings | ||||||
| Williams et al., 2006 | 171 HIV-positive individuals | 24 home visits by nurses over 12 months to identify concerns and barriers to adherence | Intervention very effective, but expensive | ||||||
| Safren et al., 2009 | 45 subjects with depression | 10-12 sessions of cognitive behavioral therapy, adherence support vs. single session of adherence counseling | Improvements in adherence among depressed subjects at 3 months, with gains maintained at 6 and 12 months | ||||||
beyond the cessation of the intervention and preventing relapse remains a challenge.
There is evidence that many adherence interventions are cost effective. For some of the more costly interventions (e.g., DAART interventions costing $1,000 per person per month), there needs to be about a 35 percent improvement in viral suppression before the intervention can be considered cost effective (Goldie et al., 2003). However, less expensive, albeit somewhat less effective, interventions (e.g., use of weekly telephone calls, reminders, simple counseling) can be cost effective and could be implemented on a broad basis.
Bangsberg described how one limitation of the available evidence on adherence to antiretroviral therapy is that most intervention trials have lasted no longer than 24 months, so concerns related to decades of ongoing adherence have not been addressed. Fatigue can interfere with adherence. The need to be on drugs for decades can lead patients to just get tired of taking pills. Clinicians need education on how to manage this issue with their patients. Providers can inform patients of the problem of fatigue and suggest ways to combat it.
Some new technologies and devices may define the future of adherence monitoring, allowing providers to monitor drug adherence in real time (e.g., with the use of pill dispensers with electronic sensors in the cap, cell phones). Such monitoring is important because evidence suggests that although treatment interruptions of a few days can be tolerated, the probability of virologic rebound increases with longer interruptions. For example, Bangsberg described a study that found longer treatment interruptions to be associated with greater probability of virologic rebound, with a treatment interruption of 15 days being associated with a 50 percent probability of virologic rebound (Parienti et al., 2008). If a non-adherent individual could be identified early, active intervention by telephone or a home visit (e.g., directly observed therapy) could be used to re-engage the client. The type of intervention could be targeted to the needs of the individual (e.g., home visits would be reserved for individuals with the greatest adherence difficulties).
Committee member Ron Bayer, Columbia University, raised consent and privacy issues when discussing the use of technology to monitor medication adherence. A patient likely would need to provide informed consent before having information about medication adherence sent to his or her clinician or health department. Bayer suggested that careful use of language is needed regarding surveillance of HIV/AIDS medication adherence to ensure that privacy and consent issues are addressed.
In terms of federal monitoring of Ryan White grantees, Parham Hopson described how some of HRSA’s performance measures are related to medication adherence. For example, one of the core clinical performance mea-
sures for adults and adolescents is the percentage of HIV-infected clients on ART who are assessed and counseled about adherence two or more times in the measurement year (HRSA, 2008). Through its National Quality Center, HRSA offers a number of online resources and tools for Ryan White Care Act grantees to improve patient adherence to HIV treatment medication.26
Lessons from Successes in Other Chronic Conditions
The committee was asked to consider how successes in promoting adherence to therapy for other chronic conditions may inform approaches to improve adherence with ART and, hence, to improve medical outcomes for people with HIV. Persons with HIV experience unique barriers to maintaining adherence to medication, in addition to the barriers faced by individuals with more common chronic conditions such as hypertension and diabetes (Gellad et al., 2009). Physical and psychiatric comorbidities are common among individuals with HIV, some of which may increase risk for non-adherence. Just as ART can be used to manage HIV, medications can be used successfully in the self management of diabetes. Mann and colleagues (2009) found that in a sample of poor adherers, the major predictors of poor adherence related to patient beliefs about the disease (for example, believing that one only has diabetes when one’s blood sugar is high) and patient beliefs about the medication (for example, not understanding when it is appropriate to take the medication). The lesson for HIV medication adherence is that the provider must ensure that the patient understands both the medical course of HIV and AIDS as well as the critical importance of remaining compliant with the medication regimen.
Much research in the adherence field has focused on smoking cessation. Although this is a different aspect of adherence, there are important lessons to be learned from this literature. For example, depression is a major influence on adherence to smoking cessation programs, with depressed smokers reporting a significantly lower quit rate than nondepressed smokers (Glassman et al., 1990). Rohrer and colleagues (2010) conclude that the critical variables to ensure adherence to quitting smoking include physician recommendation, availability of telephone counseling, pharmacotherapy, targeted print materials, and information about self-help.
Social support is another important component of successful smoking cessation. For example, support from a spouse or a friend can improve adherence. It may be that the lesson is to involve family members (whether biological family or chosen family) in the adherence regimen in order to improve adherence to therapy. Advice from health care providers can play
__________________
an important role in adherence to smoking cessation as well (Stead et al., 2008).
In short, the available data on successful smoking cessation programs indicate multiple components must be incorporated. Such a multicomponent approach must be taken to improve HIV medication adherence in the future.
A final area of relevant research involves the role of illicit drug use in non-adherence. Studies have shown that substance abuse is an important factor in medication non-adherence (Gilmer et al., 2004; Janssen et al., 2006). In considering HIV drug regimens, then, health care providers must take into account the substance abuse patterns of their patients, as this may help them to anticipate patients’ likelihood of adhering to the medication regimen.
Taken together, research from other chronic conditions such as diabetes, smoking, and substance abuse provides important clues to increasing successful adherence to an ART regimen. Health care providers must take care to understand patients’ own understanding of the disease and of the medication. They also should assess whether their patients exhibit symptoms of depression and whether they have social support. Finally, patients’ history of substance abuse should be taken into account when designing the treatment regimen. Taking these factors into account can help improve adherence to ART regimens.
PAYMENT FOR TREATMENT OF EARLIER STAGE HIV INFECTION
As part of its charge, the committee was asked whether insurance companies and other payors will pay for treatment of HIV-infected persons whose CD4 counts and/or viral load does not fall within the “official guidelines” for starting treatment. The committee also was asked what might be done to promote access to treatment for these individuals.
The dramatic effect of ART on viral load has led to discussion of the potential benefit of initiating ART at earlier stages of HIV infection.27 The committee’s charge does not specify which treatment guidelines might be considered “official”; however, the primary U.S. and international guidelines are good candidates. In the United States, the U.S. Department of Health and Human Services (HHS) has issued treatment guidelines at the federal level (HHS, 2009). The HHS guidelines are reviewed continually
__________________
27 For example, in a 2009 study using data from South Africa, World Health Organization researchers concluded that a program of annual universal voluntary testing of all individuals older than 15 and immediate initiation of ART after diagnosis (a “test-and-treat” strategy) could, within 10 years of implementation, reduce HIV incidence and mortality to less than 1 case per 1,000 people per year (Granich et al., 2009).
and updated as needed and seem to offer a reasonable guide for developing policy. Currently, the HHS guidelines and those issued by the International AIDS Society-USA (IAS-USA) recommend that ART be initiated for patients with CD4 counts at or below 500 and regardless of CD4 count for patients with a history of AIDS-defining illness, who are pregnant, or who have HIV-associated nephropathy or hepatitis B virus (HBV) coinfection when treatment of HBV is indicated (for HHS) or those who are symptomatic (for IAS) (see Box 3). IAS-USA, as well as the World Health Organization (WHO), updated their treatment guidelines in 2010, citing new evidence on the timing of treatment, lower toxicity of newer drugs, and the role of ART in the prevention of HIV infection (IAS-USA, 2010; WHO, 2010). Changes
BOX 3
HIV Treatment Guidelines
U.S. Department of Health and Human Services, Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents, 2009
Antiretroviral therapy should be initiated in all patients with a history of an AIDS-defining illness or with a CD4 count <350, as well as those who are pregnant, have HIV-associated nephropathy, or have Hepatitis B virus coinfection, when HBV treatment is indicated. Therapy is also recommended for patients with CD4 counts between 350 and 500. For patients with CD4 counts >500, the HHS panel was evenly divided, with 50 percent favoring starting antiretroviral therapy at this stage and 50 percent viewing initiating therapy at this stage as optional (HHS, 2009).
International AIDS Society-USA, Antiretroviral Treatment of Adult HIV Infection, 2010
Therapy should be initiated for symptomatic patients with established disease regardless of CD4 count, and for asymptomatic individuals with CD4 counts less than or equal to 500. Treatment should be considered for asymptomatic individuals with CD4 counts greater than 500 (IAS-USA, 2010).
World Health Organization, Antiretroviral Therapy for HIV Infection in Adults and Adolescents, 2010
It is recommended to treat all patients with CD4 counts of ≤350. It is recommended that all patients with WHO clinical stage 1 and 2 (less advanced disease) should have access to CD4 testing to decide when to initiate treatment. It is recommended to treat all patients with WHO clinical stage 3 and 4 irrespective of CD4 count (WHO, 2010; see reference for details on WHO clinical staging).
were in the direction of initiation of therapy in patients with higher CD4 counts, which is suggestive of an earlier stage of disease.28
The strength of the evidence supporting initiation of therapy increases as CD4 count decreases, with evidence currently being stronger for initiation of therapy at CD4 counts less than 350 than for CD4 counts between 351 and 500 (When to Start Consortium, 2009; IAS-USA, 2010). Methods used to suggest that a reduction in mortality will result if therapy is started at CD4 counts above 500 (Kitahata et al., 2009) have been deemed problematic by the some researchers (Hernán and Robins, 2009).
Earlier initiation of treatment is associated with better clinical outcomes, yet there is some concern that earlier treatment could result in late effects of treatment, such as the potential for premature aging. There is also the possibility that newer drugs over time will show side effects following long-term use (Katz, 2010; Volberding and Deeks, 2010).
Private Health Insurance
The committee did not survey the various health insurers on their provision of coverage for treatment of individuals with HIV disease less advanced than current guidelines indicate for starting treatment. Private insurers often use evidence-based clinical guidelines to inform decisions about what services to cover.
Michael Horberg, Director HIV/AIDS at Kaiser Permanente (KP), a private insurer, described KP’s aggressive approach to care linkage and retention.29 Most (88.6 percent in 2007) of newly identified HIV-positive individuals (either transfers into KP or new diagnoses) are in care within 90 days (i.e., visit to specialist and laboratory services). The vast majority (86.8 percent in 2007) of patients with CD4 counts below 350 are prescribed ART. Treatment decisions are not governed by CD4 counts alone. Decisions are made on an individual basis between providers and patients, but in general, treatment is initiated when CD4 counts are below 350, as per previous HHS guidelines. Horberg noted, however, that increasingly clinicians are treating patients with higher CD4 counts. In general, all pregnant HIV-infected women are prescribed ART. Adherence to ART is high within KP (median adherence 93.8 percent using 2007 data). This leads to a high proportion of patients with maximal viral control (92.9 percent in 2007). The cost of care is considerable. The current mean estimate of cost for
__________________
28 For instance, IAS-USA previously recommended treatment for patients with symptoms or CD4 counts lower than 350 and that therapy should be considered for individuals with CD4 counts above 350 (IAS-USA, 2008).
29 According to Horberg, KP represents the largest civilian integrated provider of HIV care in the United States, serving more than 19,000 individuals in 2009. KP is second only to the VHA in terms of the number of persons under treatment for HIV/AIDS.
HIV-positive patients on their first and second ART regimens is $24,600 per person per year and $36,300 for later regimens (personal communication with Horberg, October 2010).
Horberg identified several challenges to earlier treatment within KP. First, although there is likely a sufficient supply of providers currently, there are concerns about the future supply, especially the supply of support staff, keeping pace with demand (Zywiak, 2010). As mentioned previously, the first generation of HIV providers are aging and retiring. Consequently, efforts are needed to improve training in HIV care for physicians and other health and allied health providers. As HIV has evolved into a complex, chronic condition, primary care providers in internal medicine, pediatrics, and family medicine increasingly will be overseeing the care of individuals with HIV/AIDS. In addition, the role of nurses, physician assistants, social workers, and other health and allied health providers in caring for such patients will increase as well. As will be discussed in detail in the committee’s third report, current training in HIV medicine in professional schools, post-graduate training, and continuing medical education is insufficient to prepare future providers to meet the increased demand for providers competent in HIV care. The implementation of screening guidelines and health care reform will bring additional HIV-positive patients into the KP system, raising challenges in terms of maintaining KP’s successes to date.
Horberg reported on his inquiries about insurance companies’ policies for payment of HIV/AIDS care.30 According to his communications with representatives of Kaiser Permanente, Aetna, and a professional organization representing health plans (America’s Health Insurance Plans [AHIP]), payments for treatment claims are not based on CD4 counts and treatment decisions are usually left to clinicians. However, specialist care may not be covered or required, so patients may have less access to clinicians who are experienced in the provision of HIV care. The insurance representatives mentioned several issues that may serve as barriers to care: inadequate system capacity; lack of payments for case identification and adherence support; limited drug formularies (i.e., not all antiretroviral drugs may be included); and patients with plans that offer no prescription drug coverage.
As described previously, preexisting condition exclusions may bar some individuals from coverage for care for HIV through private insurance. However, health care reform measures already are being taken to prohibit exclusions by health insurance plans based on preexisting conditions. Reforms also will increase the scope of coverage through a new mandatory benefits package that includes prescription drugs, mental health and sub-
__________________
30 Personal communication between Michael Horberg and Andrew Baskin of Aetna and Bob Rehm of AHIP, June 2010.
stance abuse treatment, preventive care, and chronic disease management (TAEP, 2010).
Medicaid and Medicare
Medicaid is a major source of coverage for people living with HIV/AIDS. Currently, many persons with HIV are not eligible for coverage through Medicaid until they meet criteria for advanced disease (disability), which would be suggestive of symptoms, lower CD4 counts, and higher viral loads.31 An Early Treatment for HIV Act (ETHA) (H.R. 1616, 2009) was reintroduced before Congress in early 2009 to amend the Social Security Act to give states the option of coverage for low-income persons with HIV before they develop HIV-related symptoms or disabling complications, but the act has not been passed. A few states have used demonstration waivers and grants through the Ticket to Work/Work Incentives Improvement Act of 1999 to address this gap (KFF, 2009b). Health care reform under the ACA expands Medicaid income eligibility requirements to include many more individuals who did not qualify previously by raising the floor of eligibility to 133 percent of the FPL. Persons with HIV who meet the new income threshold will no longer have to qualify on the basis of disability (HHS, 2010). It is not clear the full extent to which individuals with nondisabling HIV will be covered due to this expansion (i.e., people with nondisabling HIV who are low income or uninsured, but have incomes above the 133 percent FPL). An evaluation of ETHA conducted after it was first introduced in 2003 projected that, over 10 years, it would reduce by 50 percent the death rate for persons with HIV on Medicaid, result in 35,000 more individuals having CD4 levels above 500, and save more than $30 million (PricewaterhouseCoopers, 2003).
The large majority (>90 percent) of people with HIV on Medicare are under age 65 and qualify because they are disabled and receive Social Security Disability Insurance payments (suggesting more advanced disease). The Medicare Part D prescription drug benefit offers subsidized prescription drug coverage. Part D plans cover approved antiretroviral drugs, but do not have to offer non-antiretroviral drugs (KFF, 2009b).
Expansion of Medicaid and Medicare to follow HHS guidelines on when to begin ART may help to address the concern about waiting until patients are disabled before initiating treatment.
__________________
31 Disabled is defined as having a physical or mental impairment that prevents one from working for a year or more or that is expected to result in death (KFF, 2009b).
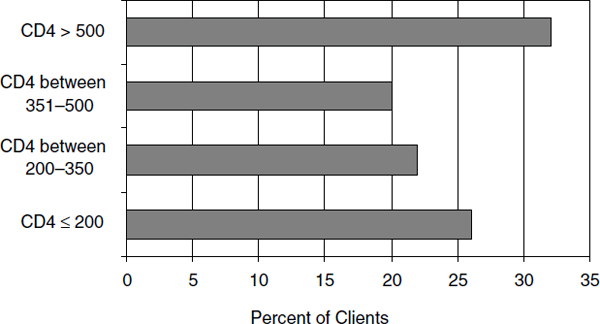
FIGURE 3 ADAP clients by CD4 count, enrolled during 12-month period, June 2009.
SOURCE: NASTAD/KFF, 2010.
The Ryan White Program
The data concerning ADAP coverage of people with early stage HIV infection are incomplete. The Ryan White ADAP program provides prescription drugs to low-income people with HIV/AIDS who have limited or no prescription drug coverage. Each state administers its own ADAP and is given flexibility in designing aspects of its program, including client eligibility guidelines. According to the National ADAP Monitoring Project’s Annual Report (NASTAD/KFF, 2010), all ADAPs require documentation of HIV status and eight reported use of additional eligibility criteria, including specific CD4 counts or viral load ranges. Of 34 ADAPs with clients whose CD4 was reported, almost half (48 percent) had CD4 counts of 350 or below at time of enrollment or at recertification (Figure 3). Thirty-two percent of clients had CD4 counts above 500 (NASTAD/KFF, 2010), but it is unclear whether these individuals had other indicators of more advanced disease (e.g., history of AIDS-related illness).
Offering Antiretroviral Treatment to All HIV-Infected Persons in San Francisco
Grant Colfax, Director of HIV Prevention and Research at the San Francisco Department of Public Health, described how, in early 2010, the
San Francisco Department of Health issued city guidelines recommending ART treatment of HIV-positive individuals as soon as they learn of their infection. Treatment is offered to HIV-positive residents of San Francisco (SF) unless there is a reason not to do so. The decision to start ART is made by the patient in conjunction with the provider. Individuals who opt for treatment but who cannot pay for the medications are assisted in gaining access to programs (e.g., ADAP, Medicaid) that will cover the costs. The implementation of this guideline works in concert with the “Healthy San Francisco” program that provides health care to under- and uninsured SF residents.32 Healthy SF is not an insurance program, but rather a system of clinics throughout the city where residents can receive care.
The SF Department of Public Health recommendations were issued in response to very high HIV prevalence rates, comparable to those seen in Sub-Saharan Africa (El-Sadr et al., 2010). According to data from the Department of Public Health, as of September 2010, an estimated 15,200 of San Francisco’s 815,000 residents are HIV positive. About 85 percent of HIV infections in SF are among men who have sex with men (MSM) and MSM who inject drugs (SFDPH, 2010). There is an HIV epidemic among SF’s MSM population, with the prevalence of infection at 23 percent (Charlebois et al., 2010). The homeless population in SF is underserved as indicated by estimates of the circulating viral loads within that community (SFDPH, 2009).
Colfax explained some of the rationale for SF’s early intervention approach. Policy makers considered an observational study showing evidence that earlier treatment (CD4 > 500) is associated with improved survival (Kitahata et al., 2009). He also cited findings from a sub-analysis of the Strategies for Management of Antiretroviral Therapy (SMART) study that included 254 randomized individuals who either were not on treatment or had been off of treatment for 6 months or more at the beginning of the study. Morbidity and mortality, both AIDS- and non-AIDS-related, was significantly lower in those who immediately initiated ART compared with those who deferred ART (Emery et al., 2008). HIV replication may lead to liver, cardiac, and renal disease and is associated with an increased risk for malignancies and declines in neurocognitive function. ART is associated with reduced risk of these complications. Colfax regarded viral replication as more damaging than the side effects of ART. He also cited evidence regarding a secondary benefit of early treatment, the potential to reduce new infections (Cohen and Gay, 2010; Donnell et al., 2010).33
__________________
32 See http://www.healthysanfrancisco.org/ for more information.
33 According to theoretical models looking at the implications for infection reduction in SF among MSM with full implementation of the “test-and-treat” model, there potentially could be an 81 percent reduction in new infections within this population by 2029 (about 12,000 infections averted [Charlebois et al., 2010]).
According to 2008 data from SF, an estimated 15 to 20 percent of HIV-infected individuals in SF do not know their infection status. Among those who have been identified as HIV positive, 88 percent are engaged in care and 72 percent have virologic suppression (Das et al., 2010). This later statistic can be attributed to the availability of simpler and more potent medications and more aggressive management on the part of providers. SF has adopted the “test-and-treat” model. Even before the new guidelines were implemented in 2009, close to half of persons living with HIV (non AIDS) with CD4 counts above 500 were on ART. Approximately 90 percent of persons living with AIDS and 70 percent of people living with non-AIDS HIV are on ART (Das et al., 2010).34
A “Fast Team” links individuals with care. Routine testing has been implemented in the emergency department of SF General Hospital. A team member links those who are HIV positive to care. According to Colfax, their linkage rate is 96 percent. Targeted testing is also taking place in clinics serving MSM.
Colfax described methods used to monitor the “test-and-treat” program. An electronic medical record captures medication prescribing, medication switches, and laboratory response to treatment (CD4 and viral load). In addition, an annual patient satisfaction survey is conducted. Monitoring takes place to identify patients lost to follow up or who have dropped out of care. Some individuals are referred to the outreach team for support and engagement. There is active surveillance for resistance in collaboration with the University of California, SF virology lab.
There are almost 4,500 individuals in SF who are enrolled in ADAP with an average annual expenditure of about $7,820 per client (Personal communication between Grant Colfax and California State Office of AIDS, June 14, 2010).35 Colfax estimated that additional funding will be needed to support availability of ART for HIV-infected individuals in SF with full implementation of the “test-and-treat” program. The city is currently facing a fiscal deficit and the public health clinic is laying off staff, so implementation may be difficult until the economy recovers.
Colfax described the need for changing provider behavior in terms of adherence to the new guidelines, but acknowledged the difficulties in doing so. There has been general community support of the new guidelines; however, there has been some misunderstanding regarding the primary intent of the program (i.e., treatment vs. prevention). Colfax indicated that a “test-and-treat” strategy alone will not eliminate the HIV/AIDS epidemic. He emphasized the importance of public health approaches that address the many important nonmedical determinants of health and prevention.
__________________
34 These statistics refer to individuals who have been reported to the health department.
35 This estimate does not include the rebate (an average of 46 percent).
Although the vast majority of SF’s HIV-infected population are MSM, the city’s program applies to all HIV-infected individuals and is a model that could be duplicated in other cities or regions with different demographics.
Advances in treatment have led to significant improvements in survival and quality of life for HIV-infected individuals who are identified early and linked to care. In part due to insurer and federal and state policies and practices, the benefits of early intervention and linkage to care, however, have not reached a sizable group of those who are HIV infected.
Policies That Promote or Inhibit Clinical Care Services Among Agencies at the Federal Level, State Level, or Between Federal and State Agencies
Status of Health Care Coverage
Fragmentation of coverage and multiple funding sources with different eligibility requirements cause many people to shift in and out of eligibility for care. Furthermore, there are substantial regional variations in the availability of coverage. Medicaid, in particular, is characterized by wide variation by state, in terms of eligibility and benefit coverage. The Ryan White program has been a lifeline with regard to paying for medications and other services, filling in the gaps left by other funding sources. It also is credited with allowing providers to create “medical homes” for their HIV/AIDS patients. At the same time, unlike Medicaid, the Ryan White program is a discretionary grant program that depends on annual appropriations from Congress, and its funding does not necessarily match the need for or the costs of care, creating gaps in access in several states and cities.
The Affordable Care Act will address several shortcomings in the current financing and delivery systems, with millions of low-income individuals, including people with HIV/AIDS, gaining access to Medicaid and benefiting from the removal of current barriers to accessing private insurance, but there are concerns that not all of the benefits that are currently available through the Ryan White program (e.g., medications, adherence support, case management) will continue to be supported. An integrated approach to HIV/AIDS care may depend on the continuation of the Ryan White program. Furthermore, services provided through the Ryan White program are, and will continue to be, essential for groups of individuals, such as undocumented immigrants, who will remain without access to Medicaid under the ACA.
Several policies could be considered to reduce financial barriers to care, including
• bringing eligibility criteria for public and private coverage into line with HHS guidelines for initiating ART;
• provision of cost sharing assistance or subsidies for lower income populations (as in Medicare Part D);
• imposition of monthly and annual capitations on overall out-of-pocket expenses;
• disallowing the practice of denying coverage for failure to pay for services; and
• elimination of annual or lifetime coverage limits (as proposed in the ACA).
Access to HIV/AIDS Expertise
Current reimbursement policies, particularly under Medicaid, restrict access to providers with HIV/AIDS expertise. Even under the ACA, infectious disease physicians who provide primary care to HIV/AIDS patients may not be able to benefit from advantageous primary care provider reimbursement policies under Medicaid. Federal and/or state policies or other programs could be enacted
• to require health plans to include HIV/AIDS medical providers in their provider networks;
• to change reimbursement policies that restrict access to HIV providers;
• to ensure that infectious disease providers who provide primary care to HIV/AIDS patients will be reimbursed in a manner comparable to other primary care providers; and
• to offer appropriate training and incentives to encourage providers to practice HIV medicine or to become competent to provide HIV care within their primary care practices.
Access to Medications
Restrictive eligibility criteria and cost-sharing requirements for health coverage limit access to medications for many individuals with HIV/AIDS. Federal support for antiretroviral and other essential medications through the Ryan White ADAP program is essential to HIV/AIDS patients, but several states are experiencing waiting lists, and others are exercising other cost containment strategies. Some state ADAP formularies do not cover all antiretroviral drugs and some are missing critical classes of drugs. States facing funding shortfalls must triage care, treating those with the lowest CD4 counts or those who are symptomatic. The lack of programs in several
states to serve individuals who are disabled (but have incomes too high to be eligible for Medicaid), as well as the existence of prescription drug limits in some states, also pose barriers to receipt of care for individuals with HIV/AIDS who are in need of treatment.
To help ensure that all HIV-positive individuals have access to needed medications, consideration might be given to
• providing sufficient Ryan White funding to eliminate ADAP waiting lists and other cost containment and triage strategies;
• extending ADAP coverage to all antiretroviral and other classes of drugs, for example, for mental health, cardiovascular, and gastrointestinal conditions;
• providing programs in all states to serve individuals who are medically needy but have incomes too high to be eligible for Medicaid; and
• eliminating prescription drug limits in all states.
Unstable Housing and Associated Polices
Homelessness is a risk factor for HIV infection and poorer outcomes among HIV-infected individuals. The provision of stable housing is associated with a reduction of risk behaviors, increased health care and social service use, adherence to ART medications, and improvement in the survival and health status of HIV-infected individuals. More longitudinal clinical trials are needed to determine whether, in which areas, and the extent to which housing status is causally related to a decrease in risk behaviors and improvements in health care and health outcomes for HIV-infected individuals. “Housing First” and “one-stop” service housing models have proven cost effective in linking vulnerable individuals into care and improving health outcomes by addressing housing needs first while making service needs easily accessible. Currently, the demand for the Housing Opportunity for People with AIDS program administered by the Department of Housing and Urban Development is much greater than can be met. It is important to ensure adequate, stable housing for HIV-infected individuals through sufficient funding for HOPWA and other programs that support housing.
Policies Affecting Immigrants
Immigrants, and especially undocumented immigrants, face numerous barriers to HIV/AIDS care including a general lack of access to health insurance, the absence of linguistically and culturally appropriate care, stigma, unstable housing, and lack of family support. The ACA, although
beneficial to many, does not include coverage of undocumented immigrants under Medicaid. The Ryan White program, as a federal program that does not make exclusions on the basis of immigration status, continues to be an essential source of care for immigrants with HIV/AIDS.
Possible means to reduce/remove the barriers to care faced by immigrants, and especially undocumented immigrants, include
• providing access to linguistically and culturally appropriate care; and
• preservation of the Ryan White program to provide coverage to individuals regardless of their immigration status.
Policies Affecting Individuals Within the Correctional System
Individuals who are incarcerated in jails and prisons are eligible for health care, but too often HIV/AIDS care is absent, incomplete, or not coordinated with care that the inmate received prior to admission to the correctional system or that is available upon release. Sources of health care coverage are discontinued or suspended upon entry into jail or prison. Model federal and state programs have shown that individuals can be routinely tested for HIV at entry into the correctional system, cared for during incarceration, and linked to follow-up care following release. To succeed in providing comprehensive care, bureaucratic obstacles must be overcome and collaboration must be forged between the correctional and community-based care systems. Provision and continuity of care for incarcerated individuals can be promoted through
• implementation and sufficient funding of programs that provide routine HIV testing to individuals at entry into the correctional system, care for HIV-infected individuals during incarceration, and linkage to follow-up care after release;
• removal of bureaucratic obstacles to such programs; and
• increased collaboration between the correctional and community-based care systems.
Considerations of confidentiality and nondiscrimination are important to protect the well-being of individuals diagnosed or treated in correctional facilities. Establishment of an effective program for testing and treating the groups of individuals who pass through the correctional system is a monumental task but would help to extend interventions to otherwise difficult to reach populations.
Policies Affecting Mentally Ill Individuals and Substance Abusers
Many people living with HIV/AIDS experience mental illness and would benefit from mental health services to help them cope with the emotional and cognitive impact of their condition. In addition, a substantial number of individuals with HIV/AIDS are dependent on substances of abuse. There are large gaps in coverage for mental health and substance abuse treatment for persons with HIV/AIDS. When available, private and public mental health and substance abuse treatment coverage is generally inadequate. Implementation of the Mental Health Parity and Addiction Equity Act of 2008 (P.L. 110-343, Subtitle B, § 511-512) and the ACA will improve coverage. These services will be essential benefits for plans operating in the state-based exchanges in 2014.
How Federal and State Agencies Can Provide More Integrated HIV Care Services
Systems Integration for HIV/AIDS Care
As infection with HIV has evolved into a chronic condition with the advent of HAART, the clinical and social needs of those infected have changed, and questions have arisen about how best to structure programs to meet those needs. Various levels of systems integration for HIV/AIDS services may help individuals receive comprehensive care, optimize their health outcomes, and reduce HIV transmission to others. Federal and state agencies might facilitate integration of HIV care with closely related infectious conditions including STIs, viral hepatitis, and tuberculosis; integration with case management, mental health and substance abuse treatment, transportation, translation services, and dental care; integration with “upstream” services that impact social determinants of health, such as housing, education, job training, legal services, and refugee and immigrant services; and integration into mainstream health care, in particular, the chronic care model.
Filling Gaps Created by Categorical Funding
After the ACA is implemented and more clients are covered by Medicaid, a portion of the Ryan White funds currently dedicated to core medical services may be available for support services (e.g., outreach, medical transportation, referrals for health care and other support, language services, respite care for individuals caring for persons with HIV). To overcome the problems associated with categorical funding, consideration could be
given to having explicit language in notices of grant awards that allows and encourages flexibility in use of the support.
Increasing the Role of Community Health Centers
One provision of the current plan for health care reform under the ACA is increased funding for CHCs to augment the nation’s capacity to meet the health care needs of individuals who are under- and uninsured. It is of concern that not all CHCs are providing HIV testing and HIV/AIDS care. A Policy Information Notice from HRSA could provide guidance to these CHCs to expand access to HIV/AIDS care services. In high HIV incidence areas, comprehensive HIV testing and care could be provided by CHCs in coordination with state HIV/AIDS programs.
Reducing Reporting Burdens
Improved data collection and coordination and reduced reporting burden on the part of clients, clinics, health departments, and community-based organizations could be facilitated by
• streamlining the disparate and redundant data collection and dissemination requirements across agencies; and
• harmonizing reporting requirements across federal agencies (e.g., HRSA, CDC, SAMHSA).
Clinician Training
Educating clinicians about the role of state health departments in identifying individuals with HIV/AIDS and linking them to care can help bridge communication gaps that may exist between clinical and public health providers. It is important to ensure the continuation of federally sponsored and other professional training programs, including AETCs and others at HRSA, SAMHSA, and CDC, to further providers’ understanding of health department programs, such as community-based health education and prevention activities, surveillance, and HIV-related infectious disease programs (e.g., STIs, hepatitis, tuberculosis).
HIV Medication Adherence Programs
Policies in Funding HIV Medication Adherence Programs
The federal Ryan White program, in addition to paying for antiretroviral therapy through the ADAP program, supports adherence interventions.
Some ADAP support can be used to increase access to medication, improve adherence, and monitor progress on therapy. Certain requirements must be met, however, in order to use ADAP support for these purposes. Adherence support through ADAPs is limited by a federal policy that stipulates that no more than 5 percent of a state’s ADAP funding can be used for services related to adherence. Furthermore, in order for states to be able to use ADAP funding for adherence purposes, they must have no client waiting list or limits on enrollment and no restrictions or limitations on HIV medications. States with waiting lists and other restrictions on the program have had to prioritize providing basic access to medications instead of using limited resources for adherence programs.
Improving Adherence
Ensuring that patients adhere to their treatment regimens is necessary to maximize their health outcomes. Interventions to improve adherence to HIV/AIDS medication regimens can be cost effective. They have been shown to both improve adherence and prevent a decline in adherence. Means to improve patient adherence include
• ensuring that the federal rules and funding for Ryan White programs maximize the ability of states to use the funds to support adherence interventions;
• structuring state ADAP programs to maximize the provision adherence services through co-location of HIV/AIDS clinics and pharmacies, client-centered pharmacies (e.g., mail order filling of prescriptions), and electronic record systems to track patient adherence and alert providers of episodes of noncompliance;
• minimizing structures that contribute to adherence problems, such as delays in communication between health departments and pharmacies (necessitating that a client potentially make multiple trips to a pharmacy to get a prescription filled) and rules that may limit who within a state can perform duties related to medication monitoring; and
• implementing adherence interventions that have been demonstrated to be the most effective, such as those involving the use of devices (e.g., pillboxes, bubble packs) that can help to remind patients of when to take their medications, and those that are interactive, open-ended, and multidisciplinary and that include multiple sessions, use behavioral skill development, target motivation/cognition/expectations, and provide periodic reminders.
Access to Treatment of Earlier Stage HIV Infection
The San Francisco “test-and-treat” program that emphasizes detection (through routine and targeted testing programs) and early treatment of HIV-infected individuals might serve as a model for increasing access to treatment in other jurisdictions. Expanded testing, as discussed in the committee’s first report (IOM, 2010), will help to increase the number of individuals diagnosed with HIV, and identification is the first step in increasing individuals’ access to care at earlier stages of infection. The second step is linking newly diagnosed individuals to care and then retaining them in care once linked. The means by which newly diagnosed individuals are linked to care varies depending on the venue where the testing takes place. In general terms, newly diagnosed individuals receive at least basic information and counseling, as well as concrete provisions for follow-up care and treatment. Various methods for improving treatment adherence and retaining individuals in care already have been outlined. Following diagnosis, one of the primary factors affecting access to care specifically for individuals with CD4 counts greater than 500 is treatment coverage.
Decisions by insurers regarding services to cover are often informed by clinical guidelines. Although there is general agreement among professional organizations and government bodies about initiating antiretroviral therapy when the CD4 count is below 500, there is less certainty regarding treatment at CD4 counts above 500. Evidence is mounting to support earlier treatment. Early intervention has been associated with improved clinical outcomes (e.g., reduction in inflammation), reduced viral loads, and lower rates of transmission. Although newer treatments have lesser short-term adverse effects, there is concern that longer-term treatment could have adverse impacts on health, such as accelerated aging.
Insurers may allow clinicians some discretion in making treatment decisions and may pay claims for HIV/AIDS treatments irrespective of CD4 count. However, specialist care may not be covered and so the expertise of clinicians providing care may be at issue. Eligibility for coverage for people with HIV/AIDS under Medicaid and Medicare often requires meeting criteria for disability, which tend to be suggestive of more advanced disease, although under the ACA, persons with HIV who meet the new income threshold will no longer have to qualify on the basis of disability.
Provision of maximal (early) care for HIV-infected individuals with CD4 counts and viral loads that do not fall within the current clinical guidelines may be promoted by
• insurers considering coverage of claims for HIV/AIDS treatments, irrespective of CD4 count;
• Medicaid and Medicare providing coverage for all persons with HIV who meet the income threshold, without requiring them to qualify on the basis of disability, as intended under the ACA;
• funding of ADAP and other programs at levels sufficient to eliminate the need for programs or providers to prioritize provision of treatment based on, for example, CD4 counts;
• the organizations that issue clinical guidelines making their purposes clear and their methodology transparent, so that policy makers can better understand the source of any discrepancies; and
• the federal agencies and professional societies that issue guidelines keeping them updated to reflect the latest scientific evidence, as HHS does on a regular basis.
Taken collectively, improvements in these areas will help to promote both early treatment, with minimal interruption, and the provision of psychosocial and support services for HIV-infected individuals, leading to better health outcomes.
































































