This chapter begins by providing definitions of key terms and essential contextual information. It then presents the committee’s argument for the need for a comprehensive approach to child and adolescent health if measures of child and adolescent health and health care quality are to be improved. The final section offers initial observations that serve as the foundation for the rest of the report. The chapter provides the conceptual basis for addressing the strengths and limitations of current data sets that are used to measure health and health care quality for children and adolescents. It also summarizes the committee’s perspectives regarding the ways in which these measures are derived from the structures, processes, and outcomes of health care services, as well as the social and behavioral determinants of health.
Definitions for several key terms are foundational for this report. These terms include child and adolescent health, functioning, and well-being, defined below. They also include a number of terms related to data collection, defined in Box 2-1.
Children and Adolescents
In this report the terms children and adolescents are used to differentiate critical stages of development rather than precise age ranges. The terms include related terms such as childhood, teenagers, and youth. Adolescents
BOX 2-1
Terms Related to Data Collection
In addition to understanding what is measured, it is important to understand how data on these measures are collected. The terms defined below are used throughout this report; the specific methods of data collection are examined in greater detail in the following chapter.
Measures are specific data collection items within a survey/interview or administrative record system, including scales, numerators, and denominators, that serve to score survey results, medical records data, administrative data, and similar data sources. They involve such questions as: “Would you rate your child’s overall health as excellent, very good, good, fair, or poor?,” “What is the birth weight of U.S. infants?,” “What is the average age, weight, or height of children served?,” “Have you [an adolescent] ever used marijuana?,” “Do you smoke cigarettes?,” “Have you ever engaged in sexual intercourse?,” and “How often do you take aspirin or medications like Tylenol for headache or other physical pain?”
Indicators are a collection of individual quality measures, consisting of a denominator and a numerator, that suggest a trend or pattern of health conditions, behaviors, or influences. Indicators of mental health status, for example, may consist of several individual measures of selected disorders, such as depression, attention-deficit disorder, and mental retardation.
Indexes are composites of indicators that are weighted to reflect assumptions about the relative value of selected indicators. One such example is body mass index (BMI), an index calculated on the basis of an individual’s weight and height (and for children, gender and age) and used in the clinical assessment of obesity and overweight. Another example is the Consumer Price Index (CPI), which represents the total cost of a market basket of goods and services purchased by households at a point in time. Inflation is defined as a change in the CPI and is used by government, business, labor, and private citizens for many purposes. Some scholars have attempted to develop a Child Well-being Index (CWI) as a similar standard for assessing the general status (including health) of children over selected years. The CWI concept is based on a composite of indicators of well-being, including “economic well-being, safe/risky behavior, social relationships, emotional/spiritual well-being, community engagement, educational attainment …. and health” (Land and FCD, 2010, p. 3).
Data systems are the collection of measures (e.g., surveys, indicators, and other reporting tools) that are used to examine the quality of child and adolescent health and health services. A data system may consist of several federally sponsored surveys, such as the National Immunization Survey (NCHS, 2011c), the National Health Interview Survey (NCHS, 2011b), and the Survey of Children with Special Health Care Needs (NCHS, 2009b). Data systems may require the linkage of several indicators or data sets to examine specific questions about the impact of children’s health care quality on selected areas of functioning, such as: “What do we know about the impact of the quality of asthma care on the educational outcomes of school-aged children with asthma?”
are specified in the report because the scope of the task includes health conditions and behaviors that are unique to this age group. The age break in defining adolescent up to age 18 in this report is influenced by the age breaks currently associated with Medicaid data systems. Yet such definitions are frequently arbitrary. An earlier National Research Council (NRC) and Institute of Medicine (IOM) report Adolescent Health Services: Missing Opportunities (IOM and NRC, 2009a) described adolescence as a time of major transitions in which youth develop relational and behavioral skills and patterns that continue into adulthood and that critically impact future life experiences and outcomes. In earlier decades, adolescence was thought to begin with biological processes, namely the onset of puberty (generally around ages 12 or 13) and to end with the assumption of the social roles of an adult, such as the completion of education, the beginning of full-time employment, and the formation of relationships such as marriage and parenthood. In practice, multiple age breaks are used to define adolescence, such as the variations associated with the legal age of driving, underage drinking, military recruitment, voting, and so forth. Most of these eligibility criteria are determined by local customs or federal and state regulations that are not informed by the science of adolescent development.
The 2009 NRC and IOM report observed that adolescence is a theoretical construct that continues to evolve in response to historical events, cultural context, and biological changes. Disagreement persists among health care researchers, experts in adolescent health and development, practitioners, and policy makers on the specific age ranges associated with the terms children and adolescents. The lower range of adolescence has shifted in response to the earlier onset of puberty among boys and girls, calling into question the term that should be used to describe pre-teen children who exhibit signs of adolescent development. The widening delay in time between physical maturity and securing professional employment and independent living has also caused some researchers to designate the late teenage years and early 20s as a period of “emerging adulthood” (Arnett, 2000, 2004).
Before reviewing the current inventory of federally supported population health data systems in the chapters that follow, it is critical to understand what is meant by child and adolescent health. The World Health Organization (WHO) defines health as “not only the absence of infirmity and disease but also a state of physical, mental, and social well-being” (WHO, 1948). However, health involves more than physical wellness—it is affected by mental and emotional states as well. Moreover, those who are concerned with children’s health status want to know about more than the presence or absence of specific health problems in the general child population at a given point in time. They also want to know whether children’s health improved or diminished as compared with other periods. They often want to know as well how children with certain types of characteristics are
faring. And increasingly, they want to know whether children are on track to grow into healthy adults. These multiple interests require an examination of the relationship between certain health conditions or behaviors and other child characteristics (such as age, race or ethnicity, gender, geography, and household income).
A growing literature documents the complex interaction among the genetics, environment, and developmental stages of children and the powerful impact of these factors on children’s overall health. Transition points are also being recognized as key in children’s health and well-being trajectory, including, for example, the transitions between childhood and adolescence and between adolescence and young adulthood (Ben-Shlomo and Kuh, 2002). Two other major factors are being recognized as influential—social determinants of health and life-course impacts.
An earlier IOM and NRC report, Children’s Health, the Nation’s Wealth (IOM and NRC, 2004), endorses an expanded definition of child health:
Children’s health should be defined as the extent to which individual children or groups of children are able or enabled to (a) develop and realize their potential, (b) satisfy their needs, and (c) develop the capacities that allow them to interact successfully with their biological, physical, and social environments…. (p. 4)
The report refers to three domains that are associated with the measurement of children’s health: health conditions, functioning, and health potential (pp. 34–37):
- Health conditions denote disorders or illnesses of body systems.
- Functioning focuses on the manifestations of individual health in daily life.
- Health potential captures the development of health assets that indicate positive aspects—competence, capacity, and developmental potential.
In addition to these domains, that earlier report examines the relationships among a variety of physical, social, and policy influences and health status and outcomes. The IOM committee that developed the report formulated a conceptual model emphasizing the dynamic and developmental nature of children’s health, focusing on the role of biology, the physical environment, and social and behavioral determinants in shaping the health and behaviors of children and youth (see Figure 2-1). While policy and health care services were also seen as key influences, they did not have a central role in that earlier study. The model of health used for Healthy People 2010 offers another approach to describing the interactions among
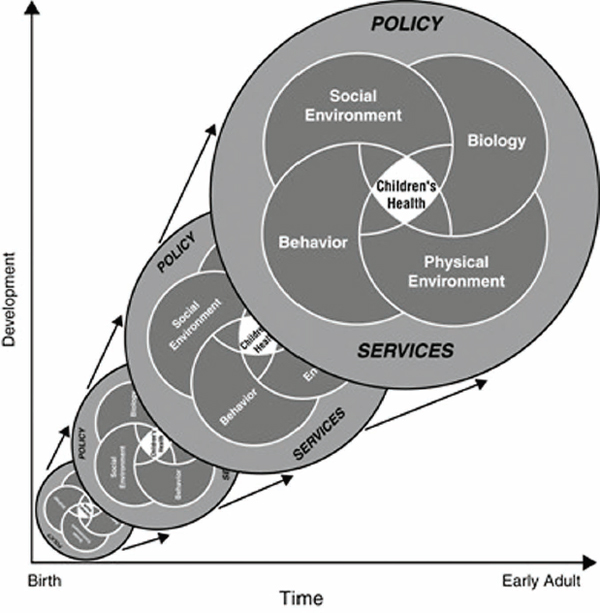
FIGURE 2-1 A model of children’s health and its influences.
SOURCE: IOM and NRC, 2004, p. 42.
environmental factors and the biology and behavior of children and youth (HHS, 2000a).
While this committee endorses an expanded definition of child health, multiple definitions are in use. A number of challenges to current measurement efforts are a consequence of this lack of consensus on the definition of child health.
Different definitions of child health reflect different goals and yield distinct statistics. One systematic review found that the prevalence of chronic conditions among children in the United States ranges from less than 1 percent to as high as 44 percent across different studies, depending on the
definition, sample, and methods used (Van der Lee et al., 2007). Assessment of the scope of selected health conditions through general population surveys is challenging, but it is equally difficult to estimate the prevalence of health disorders based on data from clinical service-based population surveys, such as hospital discharge or medical expense data studies.
In recent years, child and adolescent health indicators have expanded to include measures of overall levels of functioning and well-being—“a state broader than health that incorporates social, psychological, educational, behavioral, and economic dimensions” (IOM and NRC, 2004, p. 20)—especially in comparing the status of children and youth in the United States and in other developed nations. This approach led to a broadening of the concept of child health to include “the ability to realize aspirations, satisfy needs, and change or cope with the environment” (Starfield, 2004, p. 166). One result of this broader perspective is greater recognition of the different developmental stages of children and ways to enhance their successful transitions and navigation between childhood and adulthood, as well as greater appreciation of the importance of childhood antecedents of adult disease (such as the major role childhood obesity can play in cardiovascular disease and cancer, as well as in adult mortality). In addition, a focus on functioning and well-being encompasses interventions to minimize the impact of the experience of illness.
This distinction between the presence of a health problem and factors that lead to dysfunction resulting from that problem is articulated in the IOM report Disability in America: Toward a National Agenda for Prevention (1991). More recently, WHO extended this concept to say that every human being can experience a decrement in health and thereby experience some degree of disability. Disability is not something that only happens to a minority of humanity (WHO, 2010). According to WHO, this disability can reflect both biological and environmental factors. This formulation also emphasizes the dynamism of health as individuals experience and recuperate from health conditions (WHO, 2008). The fundamental shift in the types of morbidities facing children, from infectious to chronic conditions, as well as the impact of injuries on health, further requires a broadening of the definition of where health interventions need to focus, with increasing attention being paid to communities (e.g., neighborhood and housing characteristics), families (e.g., family structure and social support), and schools (e.g., school nutrition and physical education/activities). Considering child and adolescent morbidities within a community context, for example, allows for a more comprehensive examination of the clustering and interaction of risk factors (e.g., substandard housing conditions, poor air and water quality, poor social environment) and/or protective resources (e.g., access to affordable, healthy foods; affordable housing and transportation;
and essential services such as medical care and education) (Fielding et al., 2010; NRC, 2000).
The growing focus on children’s levels of functioning or well-being has drawn attention to the complexity of assessing the nature and direction of interactions among children’s health status, their access to and use of health services, and the impact of their physical and social environments on their health. In recent years, the quality of health care services provided to children in different settings, by different providers, and under different conditions also has been the subject of study.
For example, growing interest has focused on the use of a medical home, which the American Academy of Pediatrics defines as primary care that is “accessible, continuous, comprehensive, family centered, coordinated, compassionate, and culturally effective” (AAP, 2002, p. 184). The medical home concept may be especially useful for children with complex health care needs that require care coordination. Its utility as a measure of quality may be limited, however, in such areas as primary care and preventive services, where the identification of evidence-based and effective practices is still evolving, or in areas where the social or behavioral determinants of health may have greater impact than the use of health care services on health outcomes (such as in the areas of intentional or unintentional injury). The extent to which the medical home concept, by itself, can serve as a measure of the quality of the health care system also is questionable in the absence of more information about the extent to which other care arrangements, or other population health interventions, can effectively improve the health outcomes of children and adolescents.
The overall result of these shifts in focus is increased interest in identifying quality indicators of child and adolescent health and health care that are associated not only with traditional measures of child and adolescent health outcomes but also with broader indicators of well-being, such as school performance, risk behaviors, and childhood antecedents of adult disease. Greater attention also is being paid to the far-reaching costs and implications of childhood disease with respect to the productivity of caregivers, as well as the future productivity of children in whom the precursors of adult disease, such as obesity and smoking, are not addressed. For example, nearly a quarter of parents (23.8 percent) of children with special health care needs reported having to stop work or cut back hours at work because of their children’s needs (HHS, 2008). These changes in employment had direct and significant consequences for family income, especially among lower-income families (HHS, 2008).
In focusing on data systems, the committee endeavored to examine the contributions of existing child health data collection efforts and to assess their relative strengths and limitations (see Chapter 4). The findings resulting from these efforts serve as the basis for changes recommended by
the committee to improve the measurement of the health of children and adolescents and the quality of their health care services, especially in those areas of greatest concern to federal agencies and legislative policy makers. These findings also informed the committee’s assessment of the potential for aggregating, synthesizing, and linking measures of specific health characteristics to reflect the general health status of children and adolescents (see Chapter 4).
As context for the remainder of the report, this section provides a current snapshot of children and youth in the United States, their health status and trends, and their access to and use of health services. It also presents the committee’s argument for a comprehensive approach to child and adolescent health, the importance of measuring health and quality of health care for children and adolescents, and the need for a high-quality data system to collect these measures. Finally, it outlines challenges to creating such a data system.
Current Snapshot of Children and Youth in the United States
Children represent a substantial and growing segment of the U.S. population. In 2009, there were more than 74.2 million children and youth under age 18 in the United States, 1.9 million more than in 2000 (DeNavas-Walt et al., 2010). This number is projected to increase to 82 million in the next decade (FIFCFS, 2009).
Although children make up 25 percent of the total U.S. population, they represent 35 percent of those living in poverty (DeNavas-Walt et al., 2010). Compared with U.S. adults, U.S. children also are disproportionately of nonwhite race/ethnicity. According to the 2009 American Community Survey (ACS):
- In 2009, 55 percent of U.S. children were white, non-Latino; 22 percent were Latino; 15 percent were African American; 4 percent were Asian/Pacific Islander; 1 percent were American Indian/Alaska Native; 5 percent were multiracial; and 7 percent were identified as other race/ethnicity.
- The percentage of Latino children in the U.S. population continues to grow, and it is projected that one in every four children in the United States will be of Latino race/ethnicity by 2021 (FIFCFS, 2009).
Recent studies have focused on measuring disparities in terms of racial or ethnic differences, but disparities can also be measured along other dimensions, such as gender, household income, educational status of the child or parent, insurance type, and medical practice setting (Alessandrini et al., 2001; Merrick et al., 2001; Van Berkestijn et al., 1999; Wood et al., 1992). Some studies probe the importance of knowing more about the primary language spoken by parents and their children, since having English as a primary language frequently influences the success of efforts to navigate access to and use of health care services (Flores et al., 2000). For example, inequities and poor outcomes may be unobserved or understated with health care quality measures that are reported for those of Latino ethnicity without further subdivision by the child’s or family’s primary language.
Research has demonstrated that children in lower-income families have more severe health problems and worse health prognoses than children in higher-income families (IOM and NRC, 2004, p. 112). Yet few opportunities exist to collect data that provide a systematic understanding of differences in the health of children and adolescents based on their socioeconomic status. Several large population health surveys (such as the National Survey of Children’s Health [NSCH] and the National Survey of Children with Special Health Care Needs [NS-CSHCN]) provide opportunities to collect this type of information, but their results cannot be integrated with the administrative data on health care services and expenditures that are routinely collected for Medicaid and Children’s Health Insurance Program (CHIP) populations. Adding more data elements on race/ethnicity, socioeconomic status, special health care needs, primary language spoken at home, and parental English proficiency to administrative data sets for Medicaid and CHIP populations would provide a basis for comparing their health status and the quality of health care services they receive with the health and health care of other populations of children and adolescents.
Poor and minority children have disproportionately high special health care needs compared with their nonpoor and white counterparts, and they are more frequently insured through public health programs such as Medicaid and CHIP (Horn and Beal, 2004) (see Box 2-2 for a description of these programs). Recent estimates suggest that more than 40 percent of African American and one-third of Latino children are estimated to have public insurance (Horn and Beal, 2004). According to the census report on income, poverty, and health insurance coverage in the United States for 2009 (DeNavas-Walt et al., 2010):
- 20.7 percent of all children, or 15.5 million, lived in poverty in 2009 (p. 16);
BOX 2-2
Brief Description of the Medicaid and CHIP Programs
In the past 50 years, the U.S. Congress established two major health plans that extend health services to large groups of disadvantaged children and youth: Medicaid, established in 1965, and the Children’s Health Insurance Program (CHIP) (formerly known as the State Children’s Health Insurance Program, or SCHIP), established in 1997. Both programs were enacted by the Social Security Act (Titles XIX and XXI), which also established the Maternal and Child Health Bureau (MCHB) (Title V). Each of these programs involves substantial public investments by both federal and state governments, in contrast to Medicare and MCHB, which are administered and funded solely by a federal agency.
Medicaid
Medicaid is a joint federal−state program that provides access to affordable and comprehensive health care for targeted low-income people—primarily children, pregnant women, parents, the disabled, and the elderly (Villegas, 2011). Roughly 60 million people receive Medicaid benefits at “some point” during a given year, about half of whom—29 million—are children (Urban Institute and Kaiser Commission, 2010). Medicaid is administered by the states, although the federal government sets minimum eligibility standards and provides at least half of the funding (Villegas, 2011). Medicaid accounts for roughly one-sixth of the nation’s total health care spending (Urban Institute and Kaiser Commission, 2010).
Children represent nearly half of all Medicaid enrollees but account for only 17 percent of total Medicaid expenditures. On the other hand, seniors and people with disabilities represent one-quarter of Medicaid enrollees but account for 70 percent of total Medicaid spending (in part because of the more intensive use of acute and long-term care services by these groups).
CHIP
SCHIP (now CHIP) was established in 1997 to provide a capped amount of federal matching funds to states for coverage of children whose family incomes were too high to qualify for Medicaid but for whom private health insurance was either unavailable or unaffordable. CHIP covers roughly 7 million children in a given year (KFF, 2008).
The Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA) was signed into law in February 2009 (see Box 2-3). CHIPRA extends and expands the original SCHIP program, adding $33 billion in federal funds for children’s coverage over the next 4.5 years. The Congressional Budget Office (CBO) estimates that CHIPRA will provide coverage to an additional 6.5 million children under CHIP and Medicaid in 2013 (CBO, 2003).
In addition to providing significantly higher federal funding for children’s health coverage, CHIPRA restructured the formula that determines how much CHIP funding states receive each year; the new formula bases allotments on actual expenditures and includes an “inflation factor,” which is designed to take into account both the growth in per capita health care expenditures and the growth in the number of children in each state. The enactment of national health care reform in March 2010 extended CHIP funding through 2015 and continues the program through 2019.
- 9.3 percent of all children, or 6.9 million, lived in extreme poverty in 2009 (defined as income below 50 percent of the federal poverty level) (p. 19); and
- from 2000 to 2009, the poverty rate for children younger than 18 increased from 16.2 to 20.7 percent (p. 17).
Moreover, children in low-income families (typically operationalized as families with incomes less than 200 percent of the federal poverty level) share many of the adverse health characteristics and access problems of children in impoverished families. According to the Census Bureau’s Current Population Survey from 1980–2008, 40 percent of children ages 0–17 lived in low-income families and 44 percent of children less than 6 years lived in low-income families (FIFCFS, 2010).
Equity is a feature of the initial health care quality framework set forth in Crossing the Quality Chasm (IOM, 2001a) and is also stressed in recent legislative guidance, as well as the CHIPRA domains for measurement. Previous IOM reports have identified the equitable distribution of health care services as an overarching concern in assessing health care in the United States (IOM, 2006b, 2006c, 2006d). One recent review found that all of the available data sets surveyed included items that could serve as the basis for analysis of patients at risk for poor outcomes in various categories of disparity (Beal et al., 2004). However, the authors noted that studies of equity in children’s health care have relied on only a third of these data sets (Beal et al., 2004). And even these data sets have limitations that could affect their validity and reliability: only four of the survey instruments are available in languages other than English, and only one has undergone cross-cultural validation.
Child and Adolescent Health Status and Trends
Most children and adolescents in the United States are healthy (OECD, 2010b). Advances in medicine and more robust prevention efforts in the last half century have led to declines in infant and child mortality and improvements in overall child health. Dramatic improvements have occurred in survival rates for childhood conditions that previously had high fatality rates. Even in the short interval between 1985 and 1999, for example, mortality from cystic fibrosis fell by 61 percent for children aged 2–5, 70 percent for those aged 6−10, and 45 percent for those aged 11−15 (Kulich et al., 2003). Childhood cancer mortality has also seen substantial improvements. For the years 1975−1995, the reduction in mortality was greater than 50 percent for childhood leukemia (Linet et al., 1999). Overall, children experience lower rates of mortality, chronic illness, and disability compared with adults (Starfield, 2004).
BOX 2-3
Public Law 111-3, Title IV: Strengthening Quality of Care and Health Outcomes
On February 4, 2009, the Congress enacted the Children’s Health Insurance Program Reauthorization Act (CHIPRA) of 2009 (Public Law 111-3). Sections 401–403 call for a number of child health improvement activities for children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP), including the following:
- Development of an initial core set of health care quality measures for children enrolled in Medicaid or CHIP—The Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ) will collaborate to make recommendations for an initial core set of children’s health care quality measures (completed January 1, 2010). The initial core set will be used voluntarily by Medicaid and CHIP.
- Quality Demonstration Grants—CMS will implement a CHIPRA Quality Grant Program to establish and evaluate a national quality system for children’s health care, which encompasses care provided through Medicaid and CHIP. This will be accomplished by awarding 10 demonstration grants to states, funded by CHIPRA. This funding opportunity will result in the establishment and evaluation of a national quality system for children’s health care.
- MACPAC—CHIPRA establishes the Medicaid and CHIP Payment and Access Commission (MACPAC) to review Medicaid and CHIP access and payment policies, and submit reports and recommendations to Congress (KFF, 2008). MACPAC’s purview was expanded in the Affordable Care Act.
The picture is not entirely or uniformly positive, however. For example, several studies document that African American children have the highest prevalence of asthma of any racial/ethnic group, and substantially higher than that of whites. Compared with whites, African Americans also experience substantially higher rates of asthma-related mortality, hospitalization, and emergency department and office visits, and these disparities have widened over time (Flores, 2010).
While children generally experience far less disease and disability than adults, new health indicators pertinent to the health experiences of early childhood, school-aged children, and adolescents are especially concerning:
- The United States has achieved significant improvements in infant mortality—declining from 20.0 to 6.7 deaths per 1,000 live births
- Federal Quality Workgroup of the CHIPRA Steering Committee—The Secretary of Health and Human Services (HHS) created a Federal Quality Workgroup of the CHIPRA Steering Committee to ensure that the expertise of key HHS entities would be brought to bear in efforts to improve quality measurement and quality health care for all children. This workgroup includes members from AHRQ, CMS, HHS’s Office of the Assistant Secretary for Planning and Evaluation, the Centers for Disease Control and Prevention, the Health Resources and Services Administration, the Indian Health Service, the Substance Abuse and Mental Health Services Administration, and the Office of the National Coordinator for Health Information Technology.
- Census activities—CHIPRA includes $20 million for the Census Bureau to improve state-specific estimates of children’s insurance status and requires a federal evaluation of this program.
- Health information technology—AHRQ and CMS will collaborate to develop an electronic health record format for children.
- Development, validation, and improvement of pediatric quality measures—AHRQ will create a program that uses grants and contracts to develop, validate, and improve pediatric quality measures. That program is to be in place by January 1, 2011, and completed by January 1, 2013, in time to produce a final core quality measurement set.
- Technical support—AHRQ will provide technical consultation to CMS as it reports on quality measures and recommendations for legislative changes, provides content for best practices related to the implementation of core measures, and prepares an evaluation of outcomes of demonstration projects aimed at improving the quality of health care for children.
-
from 1970 to 2007; however, the United States still ranks thirty-second in infant mortality worldwide (OECD, 2010a).
- The rising tide of childhood obesity has emerged as a major public health epidemic throughout the nation (IOM, 2005). At least 18 percent of U.S. children and adolescents are obese—an increase from approximately 5 percent in the 1980s (Ogden et al., 2010). Over the past three decades, the proportion of obese children has more than doubled for preschool children aged 2–5 and adolescents aged 12−19, and it has more than tripled for children aged 6−11 (IOM, 2005).
- An estimated 9 percent of children and adolescents have asthma—nearly twice as many as in the 1980s (Akinbami, 2006).
- The number of children and youth in the United States identified as having chronic health conditions has increased considerably in the
-
past four decades (Perrin, 2007). This trend may be the result of environmental changes, better survival rates for certain conditions, increased access to health care through Medicaid expansions and CHIP, or a combination of these factors (Van Cleave et al., 2010).
- More than 12 million U.S. children meet the definition of children with special health care needs—“those who have a chronic physical, development, behavioral, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally” (McPherson et al., 1998, p. 138). This group accounts for roughly 15−18 percent of the child population and uses 80 percent of the health care dollars spent annually for all children (Newacheck et al., 1998a).
- While the number is difficult to estimate, as many as one in five U.S. children may have a mental disorder (Costello et al., 1996). It appears, however, that only about one-fifth of those with a need for mental health services receive a mental health evaluation, leaving as many as 7.5 million children with an unmet need for these services (Kataoka et al., 2002). A recent collaboration between the National Institute of Mental Health (NIMH) and the National Center for Health Statistics (NCHS) has led to the collection of population-based data on selected mental disorders in the National Health and Nutrition Examination Survey (NHANES), an important first step toward a national database on mental health in children and adolescents (Merikangas et al., 2010a).
- Unintentional injuries are the leading cause of morbidity and mortality among children in the United States. Between 2000 and 2006, more than 12,000 children (aged 0−19) died each year in the United States from an unintentional injury. During that same period, an estimated 9.2 million children annually made an initial emergency department visit for an unintentional injury (Borse et al., 2008). Approximately 20 million children and adolescents experience injuries that require medical attention or result in restricted activity each year; medical costs for these injuries exceed $17 billion annually (Danseco et al., 2000).
- Early exposure to smoking can greatly impact disparities in health outcomes (IOM, 2011a). An analysis of the National Health Interview Survey (NHIS) indicated that 30 percent of American children are exposed to secondhand smoke on a regular basis (at least 1 day a week) (Schuster et al., 2002). The amount of environmental tobacco smoke varies according to socioeconomic status, with children in households of lower socioeconomic status being twice as likely to be exposed as those in households of higher socioeconomic status (Mannino et al., 1996). According to the Surgeon
General’s report on unintended health consequences of smoking, moreover, higher levels of cotinine (a biological marker of secondhand smoke exposure) were correlated with increased risk of sudden infant death syndrome (SIDS), lower birth weight, respiratory infections, decreased lung function, and other health problems (HHS, 2006).
The above evidence underscores the need to focus attention on measuring and improving child and adolescent health and the quality of their health care.
Access to and Use of Health Services
Children’s health depends in part on their access to and utilization of health services, including routine physical examinations, preventive care, health education, screening, immunizations, and care for illness or injuries. Children with a usual source of health care—a regular provider to consult for treatment and preventive care—are more likely to receive timely and appropriate care (Hoilette et al., 2009; Newacheck et al., 1996). Chronic conditions are more likely to be identified and treated at early stages of development among children with a usual source of care, thereby preventing the serious consequences associated with hospitalization and emergency room use. Over time as children age, they and their parents also need to learn skills in navigating the health care system, as well as accessing confidential care for sensitive services. Increasingly, achieving access to care means that the usual source of care must be able to provide continuity and coordination of care as captured in the concept of the medical home.
Having health insurance, whether public or private is strongly associated with access to health care and use of health services among children (GAO, 1997; Newacheck et al., 1998a; Olson et al., 2005). According to an earlier IOM report, America’s Uninsured Crisis: Consequences for Health and Health Care (IOM, 2009a, p. 5):
- Children with health insurance coverage are more likely to have access to a usual source of care, immunizations, and well-child care to prevent future illness and monitor developmental milestones; prescription medications; appropriate care for asthma; and basic dental services.
- Serious childhood health problems are identified earlier in children with health insurance.
- Insured children with special health care needs are more likely to have access to specialists.
- Children with health insurance receive more timely diagnoses of serious health conditions, experience fewer avoidable hospitalizations, have improved asthma outcomes, and miss fewer days of school.
The majority of children and adolescents have some form of health insurance coverage. In 2009, the percentage of children nationwide under 18 who lacked health insurance was 10 percent, or 7.5 million children. This figure was down from 11 percent, or 8.1 million, in 2007 and up, by just one-tenth of a percent (from 9.9 percent, or 7.3 million), since 2008, which saw the lowest uninsured rate and number of uninsured children recorded in more than 30 years (since 1987, the first year in which comparable health insurance data were collected) (DeNavas-Walt et al., 2010). Some children receive health insurance through a parent’s employer or through a privately purchased plan; others are enrolled in public programs, such as Medicaid or CHIP. With the passage of the Affordable Care Act of 2010, the number of children and adolescents with health insurance coverage increased as a result of the inclusion of private-sector coverage through age 26, thereby accentuating the need to maintain access, utilization, and quality throughout this early adulthood transition period.
Children who lack health insurance of any kind or have intermittent health care coverage are more likely to be poor or near-poor and of minority race/ethnicity (DeNavas-Walt et al., 2010). Multiple interruptions in health care coverage are correlated with fewer or no well-child visits and increased likelihood of having unmet medical or prescription drug needs (Cassedy et al., 2008).
At the same time, having health care coverage is no guarantee that children will receive medical or dental care or that the care that they receive will adequately meet their needs or be of high quality. For example, the National Survey of Children’s Health (NSCH) assesses the adequacy of children’s health insurance coverage by asking parents about services and costs associated with their children’s health insurance—whether it covers services and access to health care providers that meet their children’s needs and whether the parents consider their out-of-pocket expenses for health care to be reasonable. In 2007, the NSCH found that nearly a quarter—23.5 percent—of currently insured children lacked adequate insurance (HHS et al., 2009).
These facts take on special significance given the strong evidence alluded to above that health status in childhood lays the foundation for health status throughout the life course. For example, if a baby born is too small or too early, then it is more likely to experience cognitive, behavioral, and physical challenges as a child, as well as develop chronic health condi-
tions, including high blood pressure, heart disease, and diabetes as an adult (IOM, 2006c).
Despite the previous trend in increasing birth weight, the percentage of infants born preterm (birth at less than 37 completed weeks of gestation) and the percentage born with low birth weight (less than 2,500 grams, or 5 pounds, 8 ounces) declined slightly in 2007. The percentage of infants born preterm in 2007 was 12.7 percent (down from 12.8 percent in 2006), while the percentage of infants born with low birth weight in 2007 was 8.2 percent (down from 8.3 percent in 2006, the sixth consecutive year of increase and the highest rate recorded in 40 years) (FIFCFS, 2009; HHS et al., 2009). However, there has been no change in the proportion of infants born at greatest risk for adverse outcomes—those born at less than 32 weeks of gestation or of very low birth weight (less than 1,500 grams). Despite the recent declines, moreover, disparities in preterm birth and low birth weight have persisted by race/ethnicity, as well as by the age of the mother and health insurance status.
Another example of a factor influencing health status throughout the life course is childhood obesity. Over the past three decades, obesity has more than doubled among children aged 2–5 and more than tripled among those aged 6−11 and adolescents aged 12−19. The prevalence of obesity among children aged 2–5 increased from 5 percent in 1980 to 10.4 percent in 2008. Among children aged 6−12, obesity increased from 6.5 percent in 1980 to 19.6 percent in 2008. During that same period, obesity increased from 5.0 to 18.1 percent among adolescents aged 12−19 (NCHS, 2004; Ogden et al., 2010). Obese children are more likely to be obese as adults, placing them at risk for serious chronic diseases, including diabetes, heart disease, and stroke (Serdula et al., 1993). An overweight 10-year-old child has a 40–80 percent probability of being overweight at age 35 (Parsons et al., 1999). Moreover, overweight in adolescence is associated with a broad range of adverse health effects in adulthood that are independent of adult weight. Among men, for example, being overweight during adolescence is associated with approximately double the relative risk of mortality both from all causes and from heart disease (Guo and Chumlea, 1999).
Poor health in childhood may set the stage for a broad array of long-term outcomes that include not only future health, but also lower educational attainment, socioeconomic status, and productivity (McCormick et al., 2011). For example, beyond increasing the risk of significant morbidity in the newborn period, premature birth may also increase the probability of health problems such as asthma, or cognitive and behavioral problems that lead to lower school achievement. In recent Scandinavian studies, premature birth was associated with increased rates of hospitalization, work limitations due to disability, and lower rates of family formation (Moster
BOX 2-4
The Role of Health Care, Public Health Interventions, and Clinical Preventive Services in Child Health and Well-Being
The Role of Health Care
Health care comprises services provided by health professionals, including screening and prevention, treatment and disease management, and the maintenance of physical and emotional well-being. Children’s health has improved markedly over the last century in part as a result of advances in health care, as well as in public health (see below).
A critical component of children’s health care is the preventive services encompassed by regular well-child care, particularly as a lack of adequate well-child care visits often correlates with incomplete immunizations (Freed et al., 1999; Kogan et al., 1998). Child Health USA, the Health Resources and Services Administration’s (HRSA’s) annual report on the health status and service needs of America’s children, tracks health care utilization. Highlights from the 2007 report underscore the differential rates of well-child care among children of different ages, household income, and racial and ethnic backgrounds:
- Nearly 26 percent of children under age 18 were reported by their parents not to have had a preventive, or well-child, medical visit in the past year, although this number ranges from 17.3 percent of those aged 4 or younger to 36 percent of those aged 15−17.
- During the past year, 20.2 percent of non-Hispanic black children and 25.9 percent of non-Hispanic white children failed to have a well-child visit. Hispanic children were least likely to have had a well-child visit (31.5 percent).
- In the past year, 25.7 percent of children with family incomes above the poverty threshold ($21,203 for a family of four in 2007) did not have a well-child visit, compared with 29.3 percent of children with family incomes below the poverty threshold (HHS et al., 2009).
The Role of Public Health Interventions
Numerous improvements in the health of the U.S. population have been accomplished through public health measures. The Institute of Medicine report The Future of Public Health established three core functions of public health: as-
et al., 2008; Selling et al., 2008; Swamy et al., 2008). Children with birth weights lower than expected for their gestational age may also be at risk for adult-onset cardiovascular disease and diabetes (Doyle and Anderson, 2010; Evensen et al., 2009; Hack, 2009). Moreover, the vulnerabilities incurred by premature birth reduce the ability to deal with adversity, particularly socioeconomic disadvantage. Absent appropriate intervention, then, the adverse outcomes of premature birth reflect an ongoing interplay
sessment (e.g., conducting surveillance of disease/injuries, monitoring trends, and identifying needs); policy development (e.g., promoting evidence-based decision making and developing comprehensive public health policies); and assurance (e.g., requiring and providing needed services) (IOM, 1988).
Examples of public health achievements that have reduced morbidity and mortality and significantly improved quality of life among children include the control of communicable diseases; improvements in hygiene, sanitation, and food safety; and maternal and child health services. Clean water, for example, is credited with a significant reduction in infant and child mortality in major cities in the 19th and early 20th centuries—a three-quarters reduction in infant mortality and a nearly two-thirds reduction in child mortality (Cutler and Miller, 2004). Fluoridation of drinking water is another public health intervention that improves child health by effectively preventing tooth decay, regardless of socioeconomic status or access to care.
The Role of Clinical Preventive Services
Clinical preventive services also play a significant role in child health and well-being. For example, universal childhood vaccination programs helped control—and in the case of smallpox, eradicate—previously life-threatening illnesses. Dramatic declines in morbidity occurred for the nine vaccine-preventable diseases (smallpox, pertussis, tetanus, poliomyelitis [paralytic], measles, mumps, rubella, congenital rubella, and Haemophilus influenzae type b) (CDC, 1999).
Developmental screenings and mental/behavioral health screenings (e.g., screening for major depressive disorder among adolescents), which may increase the likelihood of early detection and timely intervention (if appropriate treatment is available), provide another critical pathway to improved child health and well-being (Sandler et al., 2001; U.S. Preventive Services Task Force, 2009). Among U.S. children, for example, an estimated 17 percent have a developmental or behavioral disability, such as intellectual disability or attention-deficit/hyperactivity disorder (ADHD). However, fewer than 50 percent of children with such a disability are identified as having the problem before starting school, by which time significant delays may already have occurred and opportunities for treatment missed (CDC, 1999). As a group, adolescents receive limited clinical preventive screening services, although many of their behaviors place them at particular risk, including tobacco and alcohol use and sexual activity (IOM, 2009c). However, receipt of service is not an end unto itself; access to a system that provides poor-quality care will not improve health outcomes (Mangione-Smith et al., 2007).
of a combination of biological and social factors with a cumulative impact on adult functioning.
Chapter 4 addresses in detail the relationship between childhood events and outcomes observed in adulthood, as well as the intergenerational transmission of health and well-being. Box 2-4 summarizes the role of health care, public health interventions, and clinical preventive services in child health and well-being.
NEED FOR A COMPREHENSIVE APPROACH TO CHILD AND ADOLESCENT HEALTH
Taking a life-course perspective and considering the social context in which health develops helps to provide a comprehensive picture of child and adolescent health. In considering how measures of child and adolescent health and health care quality might be improved, the committee concluded that taking such a comprehensive approach is an essential step to that end.
The Life-Course Approach to Health
As noted above, many adult health conditions originate in childhood, and several conditions that occur in childhood impact adult health. A recent IOM report, Leading Health Indicators for Healthy People 2020 (“Leading Health Indicators”) (2011b), offered the following concise description of the life-course approach:
The life-course approach is based on two concepts: first, the impact of specific risk factors and determinants of health varies during the life course; and second, health and disease result from the accumulation of the effects of risk factors and determinants over the life course. The combination of these two components produces a life-course health “trajectory” that represents the cumulative effect of risk factors and determinants at each point in the life course. Typically, the health trajectory “rises” during childhood, adolescence, and early adulthood, plateaus during middle age, and then declines with advancing age. This trajectory can be improved through the reduction of risk factors and the promotion of health through individual and population level (i.e., societal) actions, applied at specific points or during specific stages of the life course, especially during the early years of life (Ben-Shlomo and Kuh, 2002; Halfon and Hochstein, 2002; Halfon et al., 2002; IOM, 1999; Wise, 2009). There is also evidence to suggest that the impact of factors during early life and at other points in the life course is not immutable but can be influenced by other factors later in the life course (Ben-Shlomo and Kuh, 2002; Wise, 2009).
As described above, the life-course approach considers how an individual’s current and future health (or “health trajectory”) may be affected by the dynamic interaction among social, biological, and environmental influences over time. It underscores the importance of multiple risk and protective influences, and considers how the presence or absence of these influences during critical and sensitive stages of development (e.g., the prenatal period, early childhood, and adolescence) may affect the health of individuals or selected populations.
The life-course approach encompasses consideration of interactions among multiple determinants of health over time, including factors op-
erating at the individual, family, community, and societal levels. It provides a basis for interpreting how distal influences, such as the context of individuals, affect current or future health outcomes and contribute to health disparities over time. It also provides a bridge between individual and population health measures, highlighting opportunities for preventive or treatment interventions to have significant effects on the well-being of selected groups. The committee’s use of the life-course perspective provides an appropriate lens through which to view measures of child and adolescent health and health care quality.
While life-course research, particularly in the United States, is in its infancy, the rationale for the life-course approach is well supported in the literature (Ben-Shlomo and Kuh, 2002; Braveman and Barclay, 2009; Guyer et al., 2009; Halfon and Hochstein, 2002; Kuh and Ben-Shlomo, 1997; Shonkoff et al., 2009), and this approach is emerging as an important framework for national health policy goals. For example, the Healthy People 2020 agenda includes an overarching goal to “promote quality of life, healthy development and healthy behaviors across all life stages,” which inherently demands using the life-course approach. Likewise, the MCHB within the HHS has developed a strategic plan that incorporates the life-course perspective as the foundation for MCHB, its grantees, and its partners over the next 5 years.
The life-course approach shaped the seven priority areas recommended by the committee in Chapter 4 as the focus for efforts to measure the health and health care quality of children and adolescents. These cross-cutting priority areas represent selected life stages within childhood and adolescence, as well as the transition to adulthood. Chapters 4 and 5, respectively, describe the limited number of existing measures and data collection efforts related to measuring health and monitoring health care services across the life course.
A recent report, The Foundations of Lifelong Health Are Built in Early Childhood, describes how “personal experiences, environmental conditions and developmental biology work together in early childhood to influence the roots of lifelong physical and mental well-being” (CDCHU, 2010, p. 5). The report notes that “a considerable body of research suggests that adult disease and risk factors for poor health can be biologically embedded in the brain and other organ systems during these sensitive periods, with resulting health impairments appearing years, or even decades, later” (p. 6).
Illustrative Examples
This section presents two illustrative examples of the life-course approach: childhood obesity and adolescent health care. These examples demonstrate how assessing maternal, child, and adolescent health across
the life course provides valuable insights into the multiple points of intervention (e.g., environmental, behavioral, socioeconomic), multiple stages of the life course, and various levels of intervention (e.g., individual, family, community, state, federal) that are salient to improving child and adolescent health trajectories.
The Life-Course Perspective and Childhood Obesity
Childhood obesity, with its associated increased risk for adult obesity and type 2 diabetes, illustrates the value of using the life-course approach. Consider, for example, the biological influences on obesity. The life-course approach to measurement in this area would include assessing relevant exposures (e.g., maternal malnutrition before or during pregnancy, or childhood experiences of food insecurity) across critical or sensitive periods of development from preconception through adolescence. The specificity and sensitivity of selected biological processes that occur during these periods may result in greater risk for obesity from adverse exposures than would be the case at other times. Prior to conception, for example, maternal weight and diet can influence a child’s risk of obesity later in life (Gillman, 2005; IOM and NRC, 2009b; Kitsantas et al., 2010; Ludwig and Currie, 2010). Similarly, gestational weight gain during the prenatal period is associated with childhood obesity and overweight (IOM and NRC, 2009b).
Environmental and behavioral influences offer another example. The life-course approach to measurement would include assessing relevant exposures (e.g., stress, poverty, environmental toxins, or access to appropriate nutrition) across the same critical or sensitive periods of development. Again, the specific biological processes that occur during these periods influence the ways in which adverse environmental and behavioral exposures may produce a significant risk for obesity. For example, certain feeding practices in early childhood are associated with risk for overweight and obesity later in life (Dietz, 1994; Gaillard et al., 2008; Owen et al., 2005a, 2005b). Likewise, increased and cumulative levels of individual, maternal, and family stress in early and middle childhood are associated with increased risk of adolescent overweight and obesity (Garasky et al., 2009; Gundersen et al., 2008; Lohman et al., 2009). Moreover, these effects are amplified among children in low-income households who experience food insecurity (Lohman et al., 2009).
The Life-Course Perspective and Adolescent Health Care
Adolescence is a critical period of transition that includes numerous biological changes (e.g., those associated with puberty and brain development) and the development of important cognitive functions (e.g., formal
operational thought and maturation of higher executive function) that lay the foundation for future health (Arnett, 2006; IOM and NRC, 2009a). As noted in an earlier IOM and NRC report, “the health care system plays an important role in promoting healthful behavior, managing health conditions, and preventing disease in adolescence” (IOM and NRC, 2009a). Behaviors established during adolescence can have a profound influence (either protective or detrimental) not only on current health status but also on the risk of developing chronic diseases in adulthood (Mulye et al., 2009); the quality of adolescent health care therefore may have significant life-course implications.
The health care system can identify and address certain health conditions and risk factors that have particular importance during adolescence and implications for adult health, including sexually transmitted infections, chronic mental health conditions, substance abuse/use, disordered eating, unprotected sexual intercourse, and overweight/obesity, among others. Consider, for example, adolescent pregnancy, which has serious adverse consequences for the mother, including curtailing her educational attainment, which constrains her life chances and predicts worse health in adulthood (AHRQ, 2003). Early childbearing also has been linked to significant negative social, educational, economic, and other outcomes for the child, with ripple effects that impact health care access, educational opportunities, and risk behaviors (Baydar, 1995; IOM, 1995). Although social factors are crucial determinants of adolescent pregnancy (IOM, 1995), health promotion services, access to counseling, or access to affordable and confidential family planning services can help prevent unintended pregnancies (Kirby, 2007). The quality of hospital and postpartum care (e.g., breastfeeding education and support) strongly influences breastfeeding and the subsequent interpregnancy interval (Hack, 2009; Hack et al., 2002; Joyce et al., 2000). All of these services have a multigenerational impact on maternal and child health trajectories (Sable and Herman, 1997).
Policy Implications of the Life-Course Approach
The life-course approach has emerged in the national agenda for improving the health of all Americans, as reflected by the Healthy People 2020 goals and objectives. Similarly, MCHB is engaging states and local health agencies in exploring the applications and implications of the life-course approach for overall efforts to improve the health and well-being of current and future generations of women, children, adolescents, and families. A recent concept paper prepared for MCHB provides an “organizing framework” for using the life-course approach to guide the work of the Bureau and its grantees (Fine and Kotelchuck, 2010). The life-course approach also reflects growing international consensus on the importance of the
behavioral and social determinants of health and their critical influence at different stages of development, including their influence on health disparities (Frieden, 2010; Marmot et al., 2008; Miller et al., 2009; WHO, 2008).
Behavioral choices influence health throughout the life course. Engagement in high-risk or illegal activities, early sexual activity, use of substances (e.g., tobacco, alcohol, illicit drugs), and participation in violent crime contribute to negative health consequences (FIFCFS, 2010a). Early sexual activity can expose children and adolescents to sexually transmitted infections, pregnancy risk, and diminished physical and emotional health (Meier, 2007). According to the National Statistics for Family Growth (NSFG), teen pregnancies were experienced by 70.6 per 1,000 women in 2005; although this was a historic low, pregnancy in this age group is associated with morbidity, mortality, and health care costs (Ventura et al., 2009). Furthermore, one in five births to adolescent mothers are repeat pregnancies (Abma et al., 2004), a statistic that suggests the urgent need for access to and utilization of reproductive services among at-risk individuals.
The social determinants of health, or “the conditions in which people are born, grow, live, work and age, including the health system,” also are critical to understanding child and adolescent health and development (WHO, 2010). A significant and growing body of evidence demonstrates the links and interactions among social structures, environments, economic systems, and health (Braveman et al., 2011; Kawachi and Berkman, 2003; Marmot and Wilkinson, 1999; WHO, 2008). For example, researchers have found that family income and educational attainment are associated with adults’ health status, as well as the health of their children. Specifically, higher educational attainment and higher income are associated with longer life expectancy in adults and lower rates of infant and child mortality (Blumenshine et al., 2010; Braveman et al., 2010), and children of parents with higher educational attainment experience better health (Braveman et al., 2010).
Like income and education, neighborhood conditions are linked to health outcomes. For example, poor neighborhood conditions (e.g., substandard housing and excess community violence) are associated with inferior health status (Diez Roux and Mair, 2010; Miller et al., 2011). Conversely, adequate neighborhood resources (e.g., access to healthy foods and safe, walkable neighborhoods) are associated with positive health behaviors, including healthier diets and increased physical activity (Diez Roux and Mair, 2010; Laraia et al., 2004; Larson et al., 2009; Morland et al., 2002).
Finally, the social environment (the social context and/or social interaction) is associated with health. For example, a poor social environment (e.g., neighborhoods and communities with low levels of social interaction) may have a negative impact on residents’ health; this effect has been ob-
served with asthma (Cagney et al., 2007; Williams et al., 2009) and health risk behaviors, including smoking (Chuang et al., 2005; Pickett and Pearl, 2001) and sexual and reproductive health behaviors (Averett et al., 2002; Lindberg and Orr, 2011). By contrast, a positive social environment (e.g., neighborhoods and communities with high levels of cohesiveness and social order) is associated with better health outcomes (Anderson et al., 2003; Giles-Corti and Donovan, 2002; Story et al., 2008).
Reflecting the above-noted international consensus on the importance of social determinants of health, those determinants are emerging as a central focus in the national agenda for improving the health of all Americans. For example, “social determinants of health” is a new topic area in Healthy People 2020 for which specific objectives are currently under development. Recently, the Centers for Disease Control and Prevention’s (CDC’s) National Center for HIV/AIDS, Viral Hepatitis, STD (sexually transmitted disease), and TB Prevention (NCHHSTP) published a paper outlining its planned activities to reduce health disparities related to these diseases by addressing the social determinants of health (HHS, 2010a). Finally, in fiscal year 2010, HHS’s Office of Minority Health announced more than $16 million in grants aimed at eliminating health disparities, with a special emphasis on the social determinants of health.
Figure 2-2 illustrates the behavioral and social determinants of health across the life course, tying together the important concepts described above.
Measuring Health for Children and Adolescents
Changing demographic trends among America’s children and youth; new health problems in the general population; persistent health disparities; and dynamic interactions among health, health services, health influences, and child functioning all contribute to the need for timely and accurate data systems that can document the health of children and adolescents. Questions have been raised about the capacity of existing data collection efforts to uncover key problem areas and disparities, as well as trends over time and fundamental changes that may contribute to their severity or amelioration. Significant questions also arise regarding the scope, sources, and specificity of data that are available at the national, state, and regional levels to monitor the status of children and youth, especially those at high risk of poor health outcomes.
The measurement of health for children and adolescents requires attention to multiple data sets that collect health information about specific populations, often sorted by age ranges, gender, race, ethnicity, or geography. The information is frequently derived from responses to survey questions from parents or reviews of health records and claims-based data,
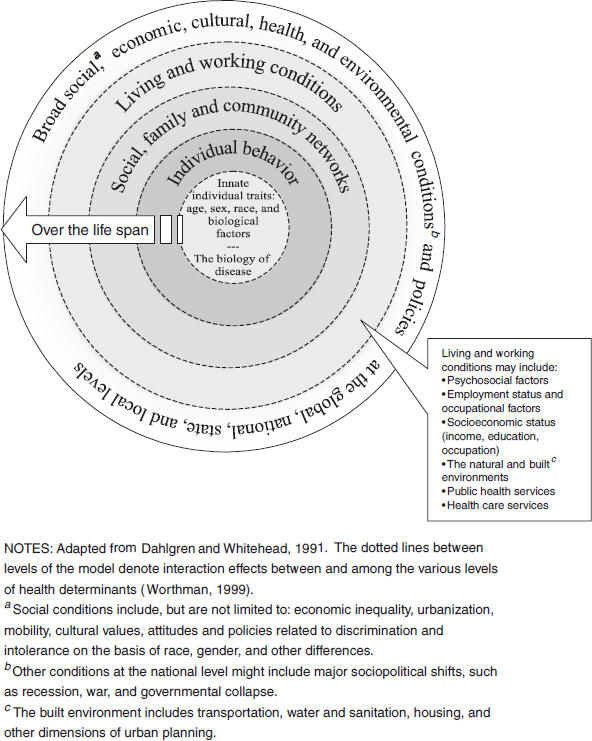
FIGURE 2-2 The determinants of health across the life course.
SOURCE: IOM, 2003a, 2011a.
as discussed in Chapter 3. Many existing health data sets offer useful snapshots of specific conditions and selected populations, such as the number and geographic or age distribution of children with diabetes or asthma, or the ages and gender of adolescents who engage in unhealthy behaviors such as underage drinking, risky driving, or substance abuse.
However, the nation lacks the capacity to identify and monitor sig-
nificant trends in many areas that involve the health status or health outcomes of children and adolescents. This is especially so for underserved populations—such as poor children; racial/ethnic minority children; children in rural settings; children in immigrant families; and children subject to multiple risk factors, such as abuse or neglect, who experience special barriers to care. Many current health and health care data sets are responsive to past concerns instead of providing guidance for questions on current or future needs, such as
- What are the general health and educational outcomes of low-birth-weight or premature infants as they become older?
- How many children or adolescents experience symptoms of mental, emotional, or behavioral disorders?
- How many children with chronic health conditions are able to function effectively in school?
- Do exposures to risk factors in early, middle, and/or late childhood contribute to the onset of adolescent health disorders?
Measuring Health Care Quality for Children and Adolescents
Measuring health care quality involves information about the types of health care services offered to children and adolescents, the settings in which these services are based, and the outcomes associated with the utilization or absence of selected care processes. A classic paradigm for assessing quality is derived from the Donabedian model, which identifies three basic components of the health care system: structure, process, and outcomes (Donabedian, 1988). Measures of the quality of each of these three components are thought to yield measures of the quality of the health care system. While this model is particularly useful in assessing the performance of health care services in meeting the needs of children and adolescents with special health care needs, as well as assessing the value and effectiveness of preventive services offered to general populations of children and adolescents in clinical settings, it may have limited value in determining the level of unmet health or health care needs of selected populations.
Health care quality measures can address such questions as
- Are immunization programs effective in protecting children and adolescents from infectious disease?
- Under what conditions do early preventive intervention services for populations of at-risk children produce better health outcomes than the delivery of treatment services after a chronic condition has been diagnosed?
- Do asthma education programs reduce the number of children with asthma who require emergency care or hospitalization?
- Does the early identification of mental health conditions through routine primary care screening lead to better long-term outcomes?
- Can school dropout rates or juvenile crime rates be reduced through early preventive intervention services for young children or adolescents?
- What interventions can reduce or eliminate significant disparities in health and health care quality?
The measurement of health care quality requires rigorous attention to the settings in which services are provided (structure) and the specific types or sequence of selected services (process) in order to understand the ways in which they influence health outcomes. Health care quality data frequently are collected from administrative or claims records or abstracts from medical records. Such data can also be derived from population health surveys of providers, patients, or their families. While multiple measures of health care quality are currently available, measures that rely heavily on abstraction from medical records are costly and are not feasible for use in large-scale data sets.
Many policy makers and researchers may be particularly interested in selected health outcomes or health trends within the general population of children and adolescents, but it is equally important to have rigorous measures of structures and processes of care in order to acquire greater understanding of the relationship between the utilization and quality of health care and health outcomes. This rigor requires the creation and use of valid, reliable, and well-specified measures that are feasible to implement, generally focusing on specific activities that occur within a selected health care setting or on interactions among health care providers in addressing a specific health condition through treatment or prevention interventions.
Using Population Health Measures for Action and Accountability
A recent IOM report, For the Public’s Health: The Role of Measurement in Action and Accountability, highlights the importance of developing an information enterprise to drive knowledge and to improve the health of the U.S. population. Citing research demonstrating that “clinical care alone is neither responsible for poor health outcomes nor the sole solution to the problem” (IOM, 2011a, p. 35; Lalonde, 1981), the study identifies information needs of the health system and the capacities and limitations of the nation’s population health statistics and information system to address these needs. The basic components of the population health information system include data sources such as vital records systems; surveillance
systems (e.g., for acute conditions such as HIV/AIDS); clinical care data sources, including administrative claims databases; electronic health records data; and federal surveys summarizing population health outcomes (NCVHS, 2010). Key reports and other products associated with these systems include Healthy People 2010 and Healthy People 2020 (HHS, 2010b; Koh, 2010); the annual NCHS report Health, United States, 2009 (NCHS, 2009a); and Health Data Interactive, a web-based site that provides access to multiple population health data sets (NCHS, 2011a).
According to the IOM committee that produced For the Public’s Health:
One of the persistent challenges to measures of health outcomes, and one of the obstacles to any attempt to nurture a level of standardization in the field, is that there are many different phenomena that may be measured, but the field is much more advanced in the area of distal health outcomes (e.g., mortality, cancer incidence) and intermediate outcomes (or individual-level and behavioral determinants of health) such as smoking and overweight, than in developing a knowledge base and valid useful indicators of more upstream determinants of health (social cohesion, social support, the quality of housing, green spaces, stress). (IOM, 2011a, p. 59)
The population health emphasis on intermediate and distal determinants of health, such as those that are influenced by social and economic factors or individual behaviors, is now beginning to shape the types of data that are collected within health care quality data sets as well. But significant challenges exist in striving to integrate health or health care quality data sets that have been designed for different purposes.
Using Metrics to Drive Improvements in Health Outcomes
The U.S. health care system comprises a diverse set of programs, services, policies, and practices that draw on resources and personnel in both the public and private sectors. Within this complex system, there is a growing emphasis on measuring health processes and outcomes and their determinants at both the individual and community levels, drawing largely on population health data sets that can support community-based analyses at the local, state, national, and even international levels. There is also a substantial body of work associated with the development of metrics focused on processes of care that can provide the basis for comparing the health outcomes and quality of services associated with individual providers and care settings, such as hospitals or regional networks of providers. In addition, interest is growing in the development of metrics that can provide a basis for analyzing the health outcomes and quality of care associated with different health plans or levels of public or private investment in health care services. These analyses can help identify whether children and adolescents
who receive care through Medicaid or CHIP plans, for example, achieve health outcomes comparable to those whose clinical services are reimbursed through private health plans.
Each of these initiatives is developing metrics and indicators for different purposes. They draw on different data sources and direct their analytic efforts toward different audiences. Those who are concerned with strengthening the capacity of public health agencies to improve population health outcomes, for example, will often focus on ways in which community-based resources and preventive strategies can contribute to lower rates of obesity or infant mortality (see, for example, IOM, 2011a). Those who want to improve the use of evidence-based care in clinical services and care settings will emphasize the need to identify specific processes and organizational practices that can improve the effectiveness, safety, and efficiency of health care services. And those who want to achieve better health outcomes for patients who depend on public health plans will emphasize the need to monitor the health status and quality of care for groups of patients with similar health conditions in ways that can support analyses and help identify opportunities for interventions at the regional and national levels.
Although each of these efforts draws on different data sources for different objectives, they all share a common interest in using data and indicators to drive improvements in the performance of the health care system. In the public health sector, for example, there is evidence of growing interest in developing common metrics and strategies that “align potentially divergent interests towards a shared goal at local (city and county), state, and national levels” (IOM, 2011a, p. 19). Similarly, the emphasis on improving measurement of the quality of health care in clinical services has stimulated the creation and use of metrics and indicators that can be used to assess the safety, timeliness, effectiveness, and efficiency of care across diverse public and private health care settings.
Despite these common interests, the nation has yet to develop a strategy or framework that can combine the metrics associated with population health efforts with those that are focused more directly on the quality of clinical care. The population health measures advanced in Healthy People 2010 and 2020, for example, are not used by the clinical care delivery system or health insurance plans as outcome sets. One reason for this may be concern about accountability for health outcomes, especially for underserved and vulnerable populations, whose health conditions may be affected by behavioral or social determinants of health as well as the quality of care they receive. The notion of shared or partial accountability of the clinical care setting for achieving community health outcomes is not yet well established, particularly in drawing on a life-course perspective.
In this report, the committee examines specific ways to improve the measurement of health and health care quality through the lens of the
clinical services supported by Medicaid and CHIP. At appropriate times, opportunities to align this work with other measurement improvement efforts, such as those now emerging in population health, are identified.
Need for a High-Quality Data System
Addressing questions such as those listed earlier requires a coordinated and meaningful quality measurement system, one that can capture and monitor key indicators and support analyses of selected population groups on the basis of age, race/ethnicity, gender, education, household income, geographic location, and other characteristics. Given the high—and growing—rates of participation of children in public health insurance programs, it will become increasingly important to know whether and how these plans contribute to the health and well-being of the nation’s children and youth. Furthermore, given the extent of variations in public and private health care plans in terms of benefit designs, eligibility criteria, health care practices, and different types of health care providers seeing and treating children, it is necessary to understand the consequences of differences in health services that result from these variations.
People concerned with the health and well-being of today’s children and youth, as well as their parents, educators, community leaders, future employers, and many others, want to know more about the extent to which existing investments result in improved health and health care outcomes. They also want to know whether the presence or absence of services that are covered by public plans such as Medicaid and CHIP make significant differences in child and adult health outcomes. They are particularly interested in knowing more about the relationship of selected health care structures and processes to child and adolescent health outcomes, such as the relative value of treating children with selected conditions in primary care versus specialty settings, or the outcomes associated with early preventive interventions for large populations of at-risk children compared with treatment services for identified conditions. Within a life-course framework, it is also reasonable to ask whether early prevention services financed by Medicaid or CHIP can reduce long-term Medicare costs by preventing avoidable health conditions in the nation’s aging population.
Certain criteria need to be defined in developing such a high-quality child health data system. For example:
- What are the basic characteristics of healthy development? Healthy children—especially in early childhood—experience rapid cognitive, emotional, social, and physical development. A data collection system needs to reflect the dynamic state of child health across different developmental periods, including transitions between child-
-
hood and adolescence and adolescence and young adulthood, in ways that can be used to examine health status over time. Furthermore, the system needs to have the capacity to identify and monitor important racial/ethnic and gender differences in health status and functioning.
- What are the essential health services that contribute to healthy development? Certain services that are associated with the prevention of infectious disease (such as immunizations) are much easier to monitor and classify than services that contribute to higher levels of functioning or enhance positive development. As traditional threats to child health, such as polio and measles, were successfully addressed, attention began to focus on new health problems that require greater emphasis on interventions in such areas as nutrition, mental health, social behavior, functioning, and self-regulation. As these areas present enormous challenges to standardized measurement and data collection, a broad, longitudinal approach may assist in addressing this question.
- How should preventive services be defined and measured? The dynamic nature of interactions between children and their families, as well as their physical and social environments, presents major challenges to the identification and measurement of risk and protective factors. Formulating quality indicators for preventive services may be especially important for certain periods of development, such as pregnancy, early childhood, and adolescence, when the timing or sequence of such services may interact with certain biological or psychological changes that influence the desired outcomes. It is also important to consider the challenges that may exist in reaching children at critical stages of development. As many early childhood interventions are not identified or initiated until a child enters elementary school, screening and other preventive services may help capture opportunities when such interventions are likely to be most effective (NRC, 2000).
Challenges to Creating a High-Quality Data System for Child and Adolescent Health and Health Care Quality
Evidence indicates that the health care system in the United States is underperforming for children and that, as discussed above, considerable variation exists in access to care, care quality, and health outcomes (Kavanagh et al., 2009; Mangione-Smith et al., 2007; Schuster et al., 2005). A previous study by the President’s Advisory Commission on Consumer Protection and Quality in the Healthcare Industry noted inadequacies in the measurement and monitoring of quality measures for children’s health care (PAC, 1998).
Further study indicated that a failure to properly document both the quantitative and qualitative characteristics of health and health care services for children and adolescents would mean that health care improvement efforts will not lead to anticipated results or may fail to occur at all (Dougherty and Simpson, 2004). Yet several persistent challenges must be met in creating a high-quality data system for child health and health care quality. Below are brief descriptions of the primary challenges, which are addressed in greater depth in the chapters that follow.
Gaps in the Development of Indicators and Measures
While recent efforts have shown progress, the development of key health and health care quality indicators for children and adolescents still falls far short of where it should be. The majority of current indicators are related to routine outpatient care, yet nearly 40 percent of U.S. health care spending for children in 2004 was for inpatient care. This dichotomy points to the importance of developing and using quality indicators for high-cost, low-incidence areas of care, such as neonatal intensive care and treatment of childhood cancers (Hartman et al., 2008), although focusing only on severe and rare conditions will not allow assessment of health care quality for a majority of children. In addition, quality measures ought to focus on high-prevalence issues, such as high-quality preventive services. Moreover, many measures currently in use focus on the process of providing health care, with varying degrees of evidence regarding the linkage to the true health outcomes or functional status of America’s children.
To date, few health indicators exist for important subpopulations of children and youth. One important such subpopulation is children with special health care needs. As a group, children with special health care needs are difficult to define precisely, although a definition was developed by MCHB and adopted by the American Academy of Pediatrics (McPherson et al., 1998). National surveys have estimated that children under 18 with chronic physical, developmental, behavioral, or emotional conditions, the basis for the MCHB definition, make up 13.9 to 16.0 percent of the pediatric population and account for more than one-third of total health care costs (Dietrich et al., 2008; Newacheck and Kim, 2005). The use of the MCHB definition, however, cannot be universal, as defining those children who are at risk for developing a chronic condition is highly dependent upon which criteria are used in identifying at-risk children.
Similarly, there are few well-defined and measurable indicators for child and adolescent mental health. A national inventory of mental health quality measures includes no measures for children and adolescents supported by “good research evidence” and few (eight) supported by “fair research evidence,” as defined by the Agency for Healthcare Research and Quality
(AHRQ) (CQAIMH, 2010). Because of the limitations posed by the availability of evidence, HHS’s initial core set of children’s health care quality measures includes only two measures directly related to mental/behavioral health (i.e., follow-up after hospitalization for mental illness and follow-up care for children prescribed attention-deficit/hyperactivity disorder [ADHD] medication) (CMS, 2010).
Quality indicators focused on educating parents and caregivers of very young children about safety and child development are also in short supply (Kavanagh et al., 2009). Providing this type of education may prevent inappropriate care and accidental injury, as well as allow early identification of potential learning or behavioral problems (Gardner, 2007).
Lack of Parental and Adolescent Perspectives in Identifying Priority Measures
The preferences of parents and especially adolescents are not reflected in the existing array of measures of health and health care quality for children and adolescents. Adolescents’ reports of their own health status, as well as their experiences with health care providers and settings, have been shown to be valid and reliable in reflecting the care they have received (IOM and NRC, 2009a). Parents also have been shown to be reliable informants in describing the extent to which their child’s needs were met—especially when seeking treatment for severe or chronic health problems (IOM and NRC, 2009a).
Lack of Integration/Coordination of Data Gathering Efforts
Although numerous agencies, states, insurers, organizations, and delivery systems are engaged in measuring the quality of health and health care services, they lack a common approach to measurement. Analyses of data also are limited by a lack of comparable data across states or benchmarks from national sources that might be used for performance improvement. Additionally, most systems and agencies lack the ability to access important data from multiple sources. And while integrating multiple administrative data sources is elemental to understanding the complex needs of children and families with multiple issues and those involved with more than one system of care simultaneously, few agencies or jurisdictions are able to accomplish such integration.
Limited Capacity to Monitor Significant Trends Over Time
Most data collection efforts lack the capacity to integrate sets of data or are limited by factors such as the ability to conduct medical record abstrac-
tion on a large scale. Hence, most current measures gauge only whether care is provided/offered and yield little information about the receipt of care, adherence to regimens prescribed or recommended, or the long-term impact of care.
Gaps in Monitoring of Disparities
Several different types of disparities deserve consideration in monitoring health and health care equity issues among children and adolescents. These include differences in socioeconomic factors, such as household income, accumulated wealth, education, and occupation; racial and ethnic disparities; and disparities in English proficiency. Each area requires consistent and precise definitions to make it possible to track trends within and between selected populations, as well as to follow trends across different time periods. Interactions may occur among each of these areas, and all may be affected as well by the powerful role—as mediators and/or moderators—of social conditions within a specific community (Braveman, 2006). Considerable evidence indicates that these conditions and social factors operate through diverse, often complex pathways, including biological mechanisms, pathways involving access to health-promoting or health-damaging resources, and pathways involving psychosocial phenomena.
Scores of studies published in the medical literature over the past several decades document that numerous racial/ethnic disparities in children’s health and health care persist, even after adjusting for all relevant covariates, including socioeconomic status. The 2003 IOM report Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (IOM, 2003a), for example, states that “racial and ethnic minorities tend to receive a lower quality of healthcare than non-minorities, even when access-related factors, such as patients’ insurance status and income, are controlled” (p. 1). Likewise, the American Academy of Pediatrics Committee on Pediatric Research published a technical report in 2010 stating that “racial/ethnic disparities in children’s health and health care are extensive, pervasive, and persistent, and occur across the spectrum of health and health care” (Flores, 2010, p. e1015). The report identifies numerous studies documenting stark racial/ethnic disparities for these populations, after adjusting for socioeconomic status and other relevant covariates.
A substantial body of research also documents a range of deleterious effects that language barriers can have on the health and health care quality of children and adolescents, including inferior medical and oral health status; greater odds of having no medical or dental insurance; a lower likelihood of having a usual source of medical care; and impaired patient understanding of diagnoses, medications, and follow-up (Baker et al., 1996; Burbano O’Leary et al., 2003; Crane, 1997; Flores and Tomany-Korman,
2008; Hu and Covell, 1986; Kirkman-Liff and Mondragon, 1991). For example, language barriers are associated as well with medical errors, injuries, and other patient safety events, including increased risk of serious medical events and physical harm (Cohen et al., 2005; Divi et al., 2007). Available evidence indicates that optimal communication, the highest patient satisfaction, the best outcomes, and the fewest errors of potential clinical consequence occur when patients and families with limited English proficiency have access to trained professional interpreters or bilingual health care providers (Flores, 2005).
An emerging literature points to the value of considering additional variables when assessing disparities in health care quality, access, and outcomes among children and adolescents. These include socioeconomic status, school density and status, parental education, literacy, family structure, and environmental quality at the neighborhood level with respect to safety and other social determinants that impact the health of children and adolescents. As CDC notes in a 2011 report on health disparities, “although the combined effects of changes in the age structure, racial/ethnic diversity, and income inequality on health disparities are difficult to assess, the nation is likely to continue experiencing substantial racial/ethnic and socioeconomic health disparities” (CDC, 2011, p. 3). A greater emphasis on improving precise measures of a broader range of variables may enable clearer causal inferences and intervention points than are possible with current measures of health disparities alone.
Several studies document the adverse effects that racial discrimination can have on the health and health care of racial/ethnic minorities (Williams and Sternthal, 2010). A recent review of the literature reveals that racism can result in racial/ethnic disparities in child health (Pachter and García Coll, 2009). Disparities exist in other areas that have received less attention—from special health care needs to sexual orientation—and share analogous issues of underreporting and insufficient and inconsistent data collection. For example, states collect data on health and health care disparities in a variety of nonstandard ways, which can make it challenging to identify, monitor, and address disparities at the national level.
Challenges in Translating Data into Practice and Action
The limited data that are available today are not well translated into practice and action. This translation requires unique skills and capacity, as well as quality improvement strategies. As the available data reflect a wide set of indicators, communities and providers often must prioritize the health conditions on which to focus, determine how to use the data to improve service delivery, and build the capacity for evidence-based practice. For asthma, for example, while an individual care plan may help ensure that a
child is receiving the most effective treatment regimen, attention must also be focused on addressing factors known to be associated with preventable asthma hospitalizations, including avoidance of known disease triggers, inferior housing conditions, poor air quality, lack of adequate parental education, inadequate access to prescription refills, and lack of follow-up with health care providers (Flores et al., 2005a).
Challenges of Relying on the Appropriate Key Informant
Whereas parents/primary caregivers are clearly the most knowledgeable about their children’s health status, they may encounter a variety of barriers to understanding crucial health care concepts for their children, including low health literacy due to medical jargon, language barriers, low literacy overall, and low educational attainment, as well as pressures related to social acceptability (e.g., respondents may provide answers that they feel are more “appropriate” or “acceptable”). These barriers may create issues of validity and/or reliability for many measures. (See Box 2-5 for a detailed description of low health literacy issues.)
A second issue is that when adolescents seek care for sensitive services, such as mental health issues, drug or alcohol dependency, and sexually transmitted infections and contraceptives, their parents may or may not be aware of these health-seeking behaviors or their children’s health status. This lack of awareness may lead to inaccurate reporting or underreporting of risk behaviors and/or health conditions.
INITIAL OBSERVATIONS ON CURRENT DATA SYSTEMS ADDRESSING CHILD AND ADOLESCENT HEALTH AND HEALTH CARE
The committee recognized from the outset of this study that in efforts to address important issues related to child and adolescent health status, health care access and quality, and outcomes of care, attention must be paid to decades-old problems within the data collection and reporting systems. At present, there is no shortage of child health data, but it is exceedingly difficult to aggregate these data in a form that is optimally useful for either sound policy decisions or health care program management. To address these issues, the committee noted that several steps will need to be taken, some requiring new and increased funding and others requiring intergovernmental coordination that is often considered difficult to accomplish. These steps are captured in the initial observations detailed below.
Initial Observation 1: A general conceptual map of the critical dimensions of child and adolescent health (including health status; health
BOX 2-5
Challenges Posed by Low Health Literacy
Health literacy is integrally linked to social determinants of health and the contexts in which families live. People who lack basic functional health literacy, defined as those who possess insufficient reading and writing skills to function effectively in everyday situations, are more likely to have never attended or completed high school (Nutbeam, 2000), live in poverty, have limited English-language proficiency, and be non-Caucasian (Kutner et al., 2006). Low health literacy affects a large portion of the U.S. population. According to the most recent national assessment of health literacy among those aged 16 and older, 30 million (14 percent of the adult U.S. population) failed to meet standards for basic health literacy (Hawkins et al., 2010).
Low health literacy has important implications for parents who are charged with seeking preventive or treatment services for their children or adhering to prescribed treatments. Although one in five adults reads at the fifth-grade level, most health information is communicated in writing and at the tenth-grade level (Hawkins et al., 2010). Research has shown that low levels of functional health literacy are associated with increased hospitalizations, greater use of emergency services, lower likelihood of obtaining preventive vaccinations, diminished ability to read and comprehend prescription labels and health messages, poorer oral health status, and lower likelihood of enrolling in social welfare programs designed to improve child health and family well-being (AHRQ, 2011; Mejia et al., 2010; Miller et al., 2010; Pati et al., 2010). Consistent with these findings, the estimated excess health care cost associated with low health literacy in the United States is $50–73 billion (Weiss and Palmer, 2004). These findings suggest that even when parents have access to and receive information from pediatric providers, health care quality will likely be compromised by the parents’ inability to use the information effectively, leading to poorer outcomes, greater health disparities, and increased health care costs.
The problem of low health literacy levels may be interpreted by providers as evidence that health education is an ineffective strategy for promoting health. As health information becomes more available to the public through the Internet and other media, however, parents’ capacity to access and understand the information, to decipher its meaning and accuracy, and to feel confident in their ability to use the information effectively has never been more important. Unfortunately, identifying families with low levels of health literacy is a challenge since many individuals with low literacy skills feel ashamed and do not want others to know. Moreover, extant health literacy measures are flawed; a recent review cites numerous weaknesses related to their psychometric quality and problems with wide variations in how relevant aspects of health literacy are defined and measured (Jordan et al., 2010).
Given the challenge of identifying individuals in the health care system with limited health literacy skills and the likelihood that as more immigrant families enter the health care system, more children will be affected, it is imperative that innovative strategies for the delivery of health information be developed. These strategies may include greater use of audio and video recorded messages, pictures, maps, diagrams, and large print with simple words that are easy to understand (Hawkins et al., 2010).
care access, utilization, and quality; and health care outcomes) will need to be developed, widely adopted, and implemented by federal, state, and local health and health care agencies, as well as private-sector organizations.
There is considerable value to be derived from conceptual frameworks presented in a graphically understandable form. One such framework upon which the committee decided to build was developed by the IOM committee that produced Children’s Health, the Nation’s Wealth (IOM and NRC, 2004). This diagram, reproduced earlier as Figure 2-1, offers a perspective on how children’s developmental stages over time have important (and different) health implications for four spheres of influence on child/adolescent health (biological factors; the child’s social environment; the physical environment in which the child lives and matures; and health-relevant behaviors, some of which are health-promoting, while others pose threats to health status and the processes of healthy physical and emotional/mental development).
This committee did not attempt to reconceptualize these important facets of child health and development but used this earlier framework to begin addressing the questions posed by the Congress and the federal agency sponsoring this study (see Chapter 1). In embarking on its charge, however, the committee noted that, despite the focus of the earlier IOM report on child health status and the multidimensional factors that, together, influence health status, the diagram in Figure 2-1 does not illustrate the complexities associated with interactions between health care services and interventions and health outcomes. Thus it fails to address access to and availability of relevant services for children; understanding of the presumptive value of such services by parents or guardians; the actual provision of those services and their quality; and the impact of access to and use of those services on child health outcomes, such as functional health status. The committee determined that it was necessary to complement the conceptualization of children’s health and its influences with an approach that would capture additional facets of health care services, including access, use and quality of services, and impact.
The committee began this discussion with the now axiomatic formulation of the late Avedis Donabedian of the University of Michigan (Donabedian, 1988), who identified structure, process, and outcomes as the key dimensions of health care quality. Using these Donabedian domains, the committee identified three key foci for the collection, analysis, and use of child and adolescent health and health care quality measures: (1) access to care/services; (2) levels of utilization and quality of care/services (including underlying processes); and (3) outcomes of service access, use, and quality (see Figure 2-3). This initial formulation led to an elaboration of the es-
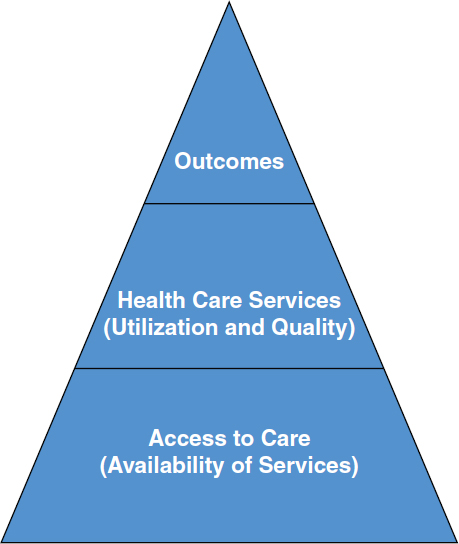
FIGURE 2-3 The pyramid of child health care.
sential content and meaning of each of these three interrelated dimensions (see Figure 2-4).
The committee quickly concluded that a comprehensive attempt to characterize the principal (and priority) components of a national data system to address the key components of child and adolescent health care—including access to and utilization of quality services and the outcomes of such access and use—would be an effort of considerable complexity, beyond the scope of this study. This effort would need to identify not only measures of evidence-based health care services but also the extent to which such services were available or provided in an effective manner to the appropriate populations of children and adolescents, including indicators of overuse and underuse of such services. Including these types of data system components would represent an extension of the four major categories of influence on child and adolescent health depicted in the diagram from the earlier IOM study, Children’s Health, the Nation’s Wealth (Figure 2-1),
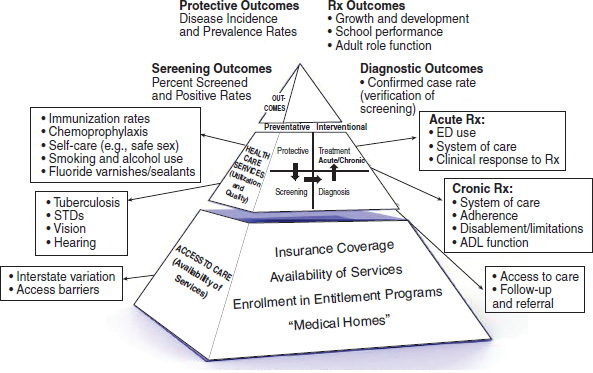
FIGURE 2-4 Changing the structure and emphasis in child and adolescent health care access and quality measures.
NOTE: ADL = activities of daily life; DX = diagnosis; ED = emergency department; STD = sexually transmitted disease.
and introduce even greater complexity, cost, and anticipated difficulties in implementation.
In its deliberations, the committee assumed that an important outcome of its efforts would be the promulgation of one or more conceptual models for a comprehensive data system for child and adolescent health and health care quality. To be successful, such conceptual models would need to be widely accepted and applicable at all levels (federal, state, and local) so as to promote efforts at each level to develop useful child and adolescent health data systems for the future.
Initial Observation 2: The identification of critical dimensions of child and adolescent health and health care services will require consensus around specified goals for this population.
Many of the objectives of such a system, however, are of high priority. A planning process will be necessary to prioritize needs for data on child and adolescent health status, health care needs, service availability and accessibility, utilization and quality of care processes, and outcomes of care that will make it possible to address urgent public policy issues surround-
ing new program initiatives and entitlement expansions for children and adolescents. In this report, therefore, the committee attempts to identify concrete steps that can be taken to meet these needs.
Initial Observation 3: Once consensus is reached on the best and most reliable indicators of key variables in this conceptual map, federal, state, and local health and health care agencies, as well as the private sector, will need guidance on the feasibility of incorporating these indicators and associated measures as requisite data items (i.e., minimum basic data items to be collected on child and adolescent health) in existing health and health care data sets.
An important initial step in enabling immediate progress toward a national approach to child and adolescent health and health care quality data was undertaken by an expert advisory panel convened by AHRQ. This panel, known as the Subcommittee of the National Advisory Committee (SNAC), recommended an initial group of core measures for health and health care quality for children and adolescents. (A detailed review of the SNAC effort is provided in Chapter 5.) The SNAC identified 24 key indicators (referred to as “the initial core set”) of health and health care service utilization that are currently available from federal agency sources and could serve as a useful starting point for a national approach to the development of a child and adolescent health data system.
Initial Observation 4: Standardized, annual (or more frequent) reporting of these standard measures (minimum basic data items) is necessary. In some cases, high-quality measures are already available and being collected in some but not all jurisdictions. In other cases, less than optimal data collection strategies may exist that can be improved through additional funding and collaboration among local, state, and federal agencies.
As the committee began its work, it soon realized that the task before it would involve consideration of additional (and perhaps new) statistical measures of various indicators of child and adolescent health and health care quality that would fill gaps in current federal data sources. Thus it would be important to lay the groundwork for the definition of a minimum basic data set for child and adolescent health and health care quality that would be enabled by the standardized collection, analysis, and reporting of comparable data of high statistical quality from every state. Clearly, the implementation of a new national effort to collect, analyze, and report data on child and adolescent health and health care quality that involves
federal, state, and local collaboration would require time, expertise, and financial support.
A commitment to improving the health and health care of children and adolescents requires careful and thoughtful measurement to gauge progress, existing gaps, and future directions. The increasingly diverse population of the United States necessitates that data be collected routinely; consistently; and with special attention to identifying, monitoring, and addressing racial/ethnic, socioeconomic, linguistic, and special health care disparities. Changing definitions of health, the changing sociodemographic profile of the nation’s next generation, and significant changes in health conditions call for improved measures in the nation’s health care and population-based information systems. The improved measures will need to address the availability of and access to health care services, the utilization and quality of health and health care services and their underlying processes, and the outcomes associated with their use.
Initial observations about the current state of measurement of child and adolescent health and health care quality suggest that conceptual work is necessary to organize data on child and adolescent health and health care quality; to identify priority goals in these areas; to reach consensus on valid and feasible measures for these goals; and to standardize reporting of these measures in federal, state, and local reports. These observations provided the starting point for the committee’s deliberations.












































