Summary of Recommendations
C1 Build the capacity of community members and organizations.
C2 Instill health and safety considerations into land use and planning decisions.
C3 Improve safety and accessibility of public transportation, walking, and bicycling.
C4 Enhance opportunities for physical activity.
C6 Support healthy food systems and the health and well-being of farmers and farm workers.
C7 Increase housing quality, affordability, stability, and proximity to resources.
C8 Improve air, water, and soil quality.
C9 Prevent violence using a public health framework.
C10 Provide arts and culture opportunities in the community.
Health Care Services Recommendations
HC1 Provide high-quality, affordable health coverage for all.
HC4 Take advantage of emerging technology to support patient care.
HC5 Provide health care resources in the heart of the community.
HC6 Promote a Medical Home model.
HC8 Ensure participation by patients and the community in health care related decision.
HC10 Provide outspoken support for environmental policy change and resources for prevention.
S1 Enhance leadership and strategy development to reduce inequities in health and safety outcomes.
S2 Enhance information about the problem and solutions at the state and local levels.
S3 Establish sustainable funding mechanisms to support community health and prevention.
S6 Expand community mapping and indicators.
02 Provide Federal Resources to support state and local community-based prevention strategies.
04 Improve access to quality education and improve educational outcomes.
Equitable Health:
A Four-Pronged Solution
In Alameda County, where we live and work, an African American child born today in Oakland’s flatlands will live an average of 15 years less than a White child born in the Oakland hills neighborhood.1 Further, for every $12,500 in income difference between families, people in the lower-income family can expect to die a year sooner. Tragically, public health data confirms this same jarring reality all across American cities, suburbs, and rural areas.
Good health is precious. It enables us to enjoy our lives and focus on what is important to us—our families, friends, and communities. It fosters productivity and learning, and it allows us to capitalize on opportunities. However, good health is not experienced evenly across society; heart disease, cancer, diabetes, stroke, injury, and violence occur in higher frequency, earlier, and with greater severity among low-income people and communities of color—especially African Americans, Native Americans, Native Hawaiians, certain Asian groups, and Latinos. (See Appendix A: Inequitable Rates of Morbidity and Mortality.)
Health inequity is related both to a legacy of overt discriminatory actions on the part of government and the larger society, as well as to present day practices and policies of public and private institutions that continue to perpetuate a system of diminished opportunity for certain populations. Poverty, racism, and lack of educational and economic opportunities are among the fundamental determinants of poor health, lack of safety, and health inequities, contributing to chronic stress and building upon one another to create a weathering effect, whereby health greatly reflects cumulative experience rather than chronological age.2 Further, continued exposure to racism and discrimination may in and of itself exert a great toll on both physical and mental health.3 Inequities in the distribution of a core set of health-protective resources also perpetuate patterns of poor health.
Historically, African Americans, Native Americans, Alaska Natives, and Native Hawaiians, in particular, have to varying extents had their culture, traditions, and land forcibly taken from them. It is not a mere coincidence that these populations suffer from the most profound health disparities and shortened life expectancies. In many of the low-income and racially segregated places where health disparities abound, a collective sense of hopelessness is pervasive, and social isolation is rampant. This individual- and community-level despair fuels chronic stress, encourages short-term decision making, and increases the inclination towards immediate gratification, which may include tobacco use, substance abuse, poor diet, and physical inactivity.
To date, our collective national response has focused on what happens after people get sick or injured. Improving the health care system by increasing access and quality remains an integral component of addressing health inequities. At the same time, recent data indicates we must do more. Despite our decades-long investment in launching clinically focused initiatives to reduce health disparities, we have made virtually no significant progress in this domain in the United States.45
Health equity is everyone’s issue, and finding solutions will significantly benefit everyone. As the US population becomes increasingly diverse, achieving a healthy, productive nation will depend even more on keeping all Americans healthy. An equitable system can drastically lower the cost of health care for all, increase productivity, and reduce the spread of infectious diseases, thus improving everyone’s well-being. Last—and most importantly—the idea of equity is based on core American values of fairness and justice. Everyone deserves an equal opportunity to prosper and achieve his or her full potential, and it is our moral imperative to accomplish this.
We can remedy the problem of disparities in health and safety outcomes by creating a new paradigm addressing the needs that are critical to achieving health equity, and the specific challenges that affect integrating solutions into practice and policy. (See Appendix B: Definitions of Health Disparities and Health Inequities.) The first need is for a coherent, sustainable health care system that adequately meets the requirements of the entire US population and of racial and ethnic minorities in particular. The second need is for adequate community prevention strategies that target the factors underpinning why people get sick and injured in the first place. These should be integrated to form a unified system for achieving health, safety, and health equity in the US.
In this paper, we propose a set of solutions that are achievable within the local arena. By local, we mean state, regional, and community levels. These solutions not only address the critical needs but also bridge traditional health promotion, disease management, and health care solutions with more upstream work that focuses on preventing illness and injury in the first place. We will outline a composite of community and health care factors that affect health, safety, and mental health and that—most importantly—provide the framework for accomplishing our four-pronged solution:
- Strengthen communities where people live, work, play, socialize, and learn
- Enhance opportunities within underserved communities to access high-quality, culturally competent health care with an emphasis on community-oriented and preventive services
- Strengthen the infrastructure of our health system to reduce inequities and enhance the contributions from public health and health care systems
- Support local efforts through leadership, overarching policies, and through local, state, and national strategy
Policy and institutional practices are the key levers tor change. Institutional practices along with public and private policy helped create the inequitable conditions and outcomes confronting us today. Consequently, we need to focus on these areas—in community, business/labor, and government—in order to “unmake” inequitable neighborhood conditions and improve health and safety outcomes. Policies and organizational practices significantly influence the well-being of the community; they affect equitable distribution of its services; and they help shape norms, which, in turn, influence behavior.
POLICY PRINCIPLES
The following policy principles* provide guidance for taking on the challenge of addressing health inequities:
- Understanding and accounting for the historical forces that have left a legacy of racism and segregation is key to moving forward with the structural changes needed. A component of addressing these historical forces should consider policy and reform related to immigrant groups—notably Latinos, Asians, and Arab Americans.
- Acknowledging the cumulative impact of stressful experiences and environments is crucial. For some families, poverty lasts a lifetime and is perpetuated to next generations, leaving its family members with few opportunities to make healthful decisions.
- Meaningful public participation is needed with attention to outreach, follow-through, language, inclusion, and cultural understanding. Government and private funding agencies should actively support efforts to build resident capacity to engage.
- Because of the cumulative impact of multiple stressors, our overall approach should shift toward changing community conditions and away from blaming individuals or groups for their disadvantaged status.
- The social fabric of neighborhoods needs to be strengthened. Residents need to be connected and supported and feel that they hold power to improve the safety and well-being of their families. All residents need to have a sense of belonging, dignity, and hope.
- While low-income people and people of color face age-old survival issues, equity solutions can and should simultaneously respond to the global economy, climate change, and US foreign policy.
- The developmental needs and transitions of all age groups should be addressed. While infants, children, youth, adults, and elderly require age-appropriate strategies, the largest investments should be in early life because important foundations of adult health are laid in early childhood.
- Working across multiple sectors of government and society is key to making the necessary structural changes. Such work should be in partnership with community advocacy groups that continue to pursue a more equitable society.
- Measuring and monitoring the impact of social policy on health to ensure gains in equity is essential. This will include instituting systems to track governmental spending by neighborhood, and tracking changes in measurements of health equity over time and place to help identify the impact of adverse policies and practices.
- Groups that are the most impacted by inequities must have a voice in identifying policies that will make a difference as well as in holding government accountable for implementing these policies.
- Eliminating inequities is a huge opportunity to invest in community. Inequity among us is not acceptable, and we all stand to gain by eliminating it.
*ADAPTED FROM: Life and Death From Unnatural Causes: Health & Social Inequity in Alameda County. Alameda County Public Health Department September 2008
Critical Needs for Achieving Equitable Health in the United States: A Health System
We need a coherent, sustainable health care system that adequately meets the health requirements of the entire US population and of racial and ethnic minorities in particular
When we talk about fixing the health care system in the United States, we assume there is a system that can be improved. The underlying problem, however, is that we have no coherent system in the first place. While there are some elements in place, they are inaccessible to a vast number of people, especially the disenfranchised. The last time the World Health Organization published data on international health ranking in their World Health Report 2000—Health systems: Improving Performance, the United States ranked number one in health expenditure per capita but only ranked 37th in overall health system performance.6 Among industrialized countries, the United States came in 25th out of 30 on infant mortality and 23rd out of 30 on life expectancy.7 The fact that a growing number of people lack health insurance or adequate health insurance has been well documented.8 Furthermore, even for those with adequate access to health care, the system is flawed. For example, medical practitioners’ job dissatisfaction rates are growing, and major shortages in nursing and allied health professions are projected.9
America’s health care system is neither healthy, caring, nor a system.
WALTER CRONKITE
In a time of financial crisis, we may focus exclusively on reforming the areas of greatest expense in the economy, narrowing in on the cost of specific items as we try to reduce that cost or at least slow its increase. Studies have revealed that the dramatic rise in the prevalence of chronic disease is a major factor responsible for growth in US health care spending.10,11,12 This is a cost that can be reduced through prevention.13 (See Appendix C: The Economics of Prevention.) Further, our current health care system and its reimbursement structure are not designed to incentivize the necessary community-based prevention and management of chronic disease; thus the system is not meeting the needs of communities across our nation, and health care costs will continue to grow.
As we reform and redesign the health care system, we need to explicitly take the issue of equity into account, since anything done to reformulate how care is delivered can either mitigate or exacerbate the problem of inequity. Therefore, quality improvements to any health care component (e.g., prevention, access, and quality) have to embrace principles of cultural competency, diversity, and equity.
We need to create a coherent, comprehensive, and sustainable health care system that is culturally and linguistically appropriate, affordable, effective, and equally accessible to all people—especially disenfranchised populations. The overall health system should start with community strategies—reducing the likelihood that people will get sick or injured in the first place and helping to maintain the well-being of those who are already sick and injured. The overall system should also offer a full set of services (e.g., medical, dental, mental health, and vision), including screening, diagnostic, and disease management services, within the communities where people live.
We need adequate community prevention strategies that target the factors underpinning why people get sick and injured in the first place
Health care is vital but alone it is not enough. The health care system has great strength in its committed providers and in its ever-improving diagnosis, procedures, and medicines. Many formerly fatal diseases are now treatable and even curable. Yet, as important as it is to improve the quality of health care services, it is only part of the solution to improving health and reducing health inequities. Patterns of disease and injury that follow the socioeconomic status gradient would still remain.14 While health care is vital, there are three reasons why addressing access to and quality of health care services alone will not significantly reduce disparities: 1) Health care is not the primary determinant of health; 2) Health care treats one person at a time; 3) Health care intervention often comes late. (See Appendix D: Reasons why addressing access to and quality of health care alone will not significantly reduce inequities.)
If is unreasonable to assume that people will change their behavior easily when so many forces in the social, cultural and political environment conspire against such change.
INSTITUTE OF MEDICINE
In order to successfully address inequities in health and safety, we must pose the following questions: Why are people getting sick and injured in the first place? What impedes their ability to recuperate? Are their neighborhoods conducive to good health? What products are sold and promoted? Is it easy to get around safely? Is the air and water clean? Are there effective schools and work opportunities? Are there persistent stressors in the environment, and what is the long-term impact of this stress on health?
People’s health is strongly influenced by the overall life odds of the neighborhood where they live. Indeed, place matters. In many low-income urban and rural communities, whole populations are consigned to shortened, sicker lives. While residential segregation has declined overall since 1960, people of color are increasingly likely to live in high-poverty communities.15 Racially and economically segregated communities are more likely to have limited economic opportunities, a lack of healthy options for food and physical activity, increased presence of environmental hazards, substandard housing, lower performing schools, higher rates of crime and incarceration, and higher costs for common goods and services (the so-called “poverty tax”).16
Conversely, people are healthier when their environments are healthier. For example, in African American census tracts, fruit and vegetable consumption increases by 32% for each supermarket.17 When states moved to require infant car seats, the impact of policy far exceeded that of education in changing norms and thus behavior: usage for infants went from 25% maximum to nearly universal, and death and injury from car crashes decreased.18
Taking a step back from a specific disease or injury reveals the behavior (e.g., eating, physical activity, and violence) or exposure (e.g., stressors and air quality) that increases the likelihood of the injury or disease. Through an analysis of the factors contributing to medical conditions that cause people to seek care, researchers have identified a set of nine behaviors and exposures strongly linked to the major causes of death: tobacco, diet and activity patterns, alcohol, microbial agents, toxic agents, firearms, sexual behavior, motor vehicles, and inappropriate drug use.19 Limiting unhealthy exposures and behaviors enhances health and reduces the likelihood and severity of disease and injury. In fact, these behaviors and exposures are linked to multiple medical diagnoses, and addressing them can improve health broadly. If we take a second step back from the medical conditions, we see that specific elements of the environments in which people live are major determinants of our exposures and behaviors and thus of our illnesses and injuries. (For a more
in-depth understanding of this model, please go to Appendix E: A Health Equity Framework:—Taking Two Steps Back to the Determinants of Health.)
Therefore, improving the environments in which people live, work, play, socialize, and learn presents a tremendous opportunity to reduce health inequities by preventing illness and injury before their onset. THRIVE (Tool for Health and Resilience in Vulnerable Environments), a research- based framework created by Prevention Institute, offers a way to understand determinants of health at the community level.20 THRIVE includes a set of three interrelated clusters: equitable opportunity, people, and place. Within these clusters are highlighted key factors that influence health and safety outcomes directly via exposures (e.g., air, water, and soil quality; stressors such as racism) and/or indirectly via behaviors that in turn affect health and safety outcomes (e.g., the availability of healthy food affects nutrition). In addition, the environment also has an influence on people’s opportunity to access quality medical services, and these are included as a fourth cluster. On the following page, Table 1: Community Factors Affecting Health, Safety, and Mental Health, presents these four clusters.
Clearly, local solutions to health and safety inequities are central to success. Local work complements broader national change, and local solutions often help shape profound, long-lasting federal changes. Altering community conditions, particularly in low-income communities of color where the memory and legacy of dispossession remains, requires the consent and participation of a critical mass of community residents. Thus strategies that reconnect people to their culture, decrease racism, reduce chronic stress, and offer meaningful opportunities are ultimately health policies. Effective change is highly dependent upon relationships of trust between community members and local institutions. The process of inclusion and engaging communities in decision making is as important as the outcomes, which should directly meet the needs of the local population. Strategies such as democratizing health institutions, as was envisioned with the creation of community health centers, foster increased civic participation and serve as a health improvement strategy.
A quality health care system and community prevention are mutually supportive and constitute a health system
While health care and community prevention are often thought of as separate domains and operate independently, they actually are synergistic. Health care institutions have critical roles to play in ensuring an emphasis on health within communities as a key part of the solution. Health services must recognize that the community locale is an essential place for service provision, for example, by expanding community clinics, providing school health services, and giving immunizations in supermarkets. An effective health care institution will also provide broad preventive services, such as screening and disease management, that address populations at-risk and those that already have illnesses.
Health care also has a role to play in improving community environments. It is one of the nation’s largest industries and is often the largest employer in a low-income community. As such, health care institutions can support pipeline development to recruit, train, and hire people from the community, especially from underserved sectors. They can also advocate for community changes that will positively impact disease management, such as healthier eating and increased activity; improve the local economy by purchasing local products; create a farm-to-institution program to incorporate fresh, local produce and other foods into cafeteria or patient meals; reduce waste and close incinerators to reduce local pollution; and enhance staff and community access to fresh produce
TABLE 1. Community Factors Affecting Health, Safety, and Mental Health
EQUITABLE OPPORTUNITY
- Racial justice, characterized by policies and organizational practices that foster equitable opportunities and services for all; positive relations among people of different races and ethnic backgrounds
- Jobs & local ownership, characterized by local ownership of assets, including homes and businesses; access to investment opportunities, job availability, and the ability to make a living wage
- Education, characterized by high-quality and available education and literacy development across the lifespan
THE PEOPLE
- Social networks & trust, characterized by strong social ties among persons and positions, built upon mutual obligations; opportunities to exchange information; the ability to enforce standards and administer sanctions
- Community engagement & efficacy, characterized by local/indigenous leadership; involvement in community or social organizations; participation in the political process; willingness to intervene on behalf of the common good
- Norms/acceptable behaviors & attitudes, characterized by regularities in behavior with which people generally conform; standards of behavior that foster disapproval of deviance; the way in which the environment tells people what is okay and not okay
THE PLACE
- What’s sold & how it’s promoted, characterized by the availability and promotion of safe, healthy, affordable, culturally appropriate products and services (e.g., food, books and school supplies, sports equipment, arts and crafts supplies, and other recreational items); limited promotion and availability, or lack, of potentially harmful products and services (e.g., tobacco, firearms, alcohol, and other drugs)
- Look, feel & safety, characterized by a well-maintained, appealing, clean, and culturally relevant visual and auditory environment; actual and perceived safety
- Parks & open space, characterized by safe, clean, accessible parks; parks that appeal to interests and activities across the lifespan; green space; outdoor space that is accessible to the community; natural/open space that is preserved through the planning process
- Getting around, characterized by availability of safe, reliable, accessible and affordable methods for moving people around, including public transit, walking, and biking
- Housing, characterized by availability of safe, affordable, and available housing
- Air, water & soil, characterized by safe and non-toxic water, soil, indoor and outdoor air, and building materials
- Arts & culture, characterized by abundant opportunities within the community for cultural and artistic expression and participation and for cultural values to be expressed through the arts
HEALTH CARE SERVICES
- Preventive services, characterized by a strong system of primary, preventive health services that are responsive to community needs
- Cultural competence, characterized by patient-centered care that is understanding of and sensitive to different cultures, languages and needs
- Access, characterized by a comprehensive system of health coverage that is simple, affordable and available
- Treatment quality, disease management, in-patient services, and alternative medicine, characterized by effective, timely, and appropriate in-patient and out-patient care including for dental, mental health, and vision
- Emergency response, characterized by timely and appropriate responses in crisis situations that stabilize the situation and link those in need with appropriate follow-up care
by establishing accessible farmers’ markets or farm-stand programs. For example, Kaiser Permanente, the nation’s largest HMO, has instituted farmers’ markets in some of the communities it serves, providing healthy options tor the residents, offering a needed place to purchase quality food, and strengthening the nearby local farms.
Equally, community prevention efforts should be a part of the strategy to foster health and reduce health disparities by improving the success of treatment and injury/disease management even after people get sick or injured. Illnesses such as diabetes, cardiovascular disease, HIV/AIDS, and cancer require patients to do what the medical practitioner requests, such as eat healthy foods and be more active. It is important for health care institutions to recognize the ways in which poverty and other social structures impede a patient’s ability to follow a doctor’s recommendations. Disenfranchised people usually don’t have safe places to walk or healthful food to eat. Overwhelmed with the requirements of work and daily life and coping with transportation and childcare issues, poor people can have more obstacles to keeping medical appointments as well. With community prevention efforts bolstering neighborhood environments and support structures, disease management strategies will be more effective.
Challenges to Achieving Health Equity through Practice & Policy
Achieving equitable outcomes is challenging and will take concerted attention, leadership, and investment. Building on interviews with local health officers conducted to inform the development of a Health Equity Toolkit funded by the Robert Wood Johnson Foundation as part of the project Advancing Public Health Αdvocacy to Eliminate Health Disparities, we have identified challenges that officials and communities face. This identification is key to shaping responsive solutions.
1. We haven’t embraced the problem of health inequities at its roots
We need to recognize that health inequities are rooted in historical policies and practices and are entrenched in social structures that create barriers to opportunity. This legacy remains invisible to many health care practitioners, policy makers, and the public. Practitioners and community spokespersons need to talk about race and social justice in new ways and often need guidance to do so effectively.
2. We don’t have a good playbook for how to do this
The people and institutions working tor reform need more guidance and information in order to identify and realize the most effective, sustainable changes. They often lack standardized, comparative data; documented examples of success; protocols tor adaptation, with attention to fidelity of core elements; a set of best practices; a framework to measure outcomes and successes; and clear goals tor the community.
The roles of different players are not well-defined. Many health issues can be traced to determinants that cross over into other public sectors, such as housing. Public health practitioners have indicated a need tor guidance on strategies where public health can take the lead.21 Further, they don’t always know how to coordinate with leadership in other sectors such as housing. In most
cases, the charge to address health equity will require public health practitioners to step outside of the contemporary bounds of public health, but this will mean establishing effective communication channels, navigating turf issues, and clarifying shared goals and objectives.
Also, the role of other institutions needs clarification as part of a coherent effort. Banks, businesses, multiple government sectors, schools, and community groups all have a major influence on health equity outcomes, even though they may not realize it or consider it in their decision-making processes. “While these players may not see themselves as having an active role, none should be taking actions that are detrimental to health outcomes.
3. A siloed system leads to a fragmented approach at best
Even if there were a shared understanding of the root of health inequities, sectors are siloed without a mechanism to work collaboratively to provide a coherent, effective set of solutions. By and large, there is a lack of coordination and cross-fertilization across sectors, efforts, and disciplines.22 This is critical to address, because reducing health inequities cannot be achieved by any one organization or sector, let alone any single department or division within public health.
Not only are sectors siloed, but the health system itself is siloed. Even within public health departments, opportunities to create meaningful collaboration across divisions, sections, or departments are limited. Categorical funding—important because it provides dedicated resources to deliver essential programs and services—can reinforce siloed approaches. There is even a divide between public health and health care; the two don’t work together systematically and strategically to catalyze, advocate for, and launch the kinds of solutions that can make a fundamental difference. Finally, community members are not consistently included in prioritizing problems or in shaping solutions.
4. Community-based, family-centered primary care is not a medical emphasis
Medical reimbursement, prestige, and medical education norms can all favor specialization over community-based, family-centered primary care. Furthermore, there is a lack of value and incentive placed on allied health professionals, promotoras (i.e., community health workers), and patient navigators. We also need to incentivize preventive services and better train medical providers in prevention.
5. Disparities in health care are not an organizational priority for many US hospitals
Many hospitals consider disparities in care as a function of conditions beyond their control. They may be reluctant to openly address “disparities” collaboratively, because this might be viewed as an admission of inequitable care.23 Often providers assume they administer equal care since it is their mission. Stratifying their publicly reported quality measures by patient race and ethnicity would be one way to confirm their assumption or identify areas for quality improvement work.
6. Health equity isn’t embedded in most people’s job descriptions; there are many competing demands
Research and practice in equitable outcomes tend to occur either as a small part of one’s job or as a specialty focus of a small group of experts within an organization. The challenge here is how to embed health equity into research and practice across and within organizations, bringing these efforts to scale, infusing them into the broader organizational culture, and propelling them to center stage.
RECOMMENDATIONS
Local Solutions for Advancing Equity in Health and Safety
Strengthen communities where people live, work, play, socialize, and learn
C1 Build the capacity of community members and organizations. Capacity building enables the residents and grassroots groups affected by poor health outcomes to better solve the community problems undermining health and safety. Strategies include:
- Train public sector staff to encourage local capacity building and to empower residents to take action in partnership with city and county governments and community-based organizations to improve their neighborhood conditions.
- Invest in both established and developing community organizations. Encourage and strengthen the capacity of these and other institutions and of individuals via financial support, technical assistance, and sharing best practices.
- Foster structured community planning and prioritization efforts to implement neighborhood- level strategies to address unfavorable social conditions.
C2 Instill health and safety considerations into land use and planning decisions. Land use, transportation, and community design (the built environment) influence health, including physical activity, nutrition, substance abuse, injuries, mental health, violence, and environmental quality. Strategies include:
- Ensure that health, safety, and health equity are accounted for in General Plans, Master Plans, or Specific Plans; zoning codes, development projects, and land-use policies.
- Engage community residents in developing zoning laws and general plans to integrate health and equity goals and criteria into community design efforts.
- Train public health and health care practitioners to understand land use and planning and to advocate for policies that support health and safety.
Integrating a community health and wellness element into general plans
The city of Richmond, California, is one of the first cities in the country to develop a comprehensive general plan element that addresses the link between public health and community design. Nearly 40% of Richmond’s residents live in poverty and over 60% are African American and Latino.24 This element addresses health impacts of community design decisions, such as zoning, on all Richmond residents as well as the historic impacts on low-income communities and communities of color, which share a disproportionately higher burden of negative health impacts. The General Plan considers factors such as physical activity, nutrition, non-motorized travelers’ safety, hazardous materials and contamination, air and water quality, housing quality, preventive medical care, homelessness, and violence, among others.
General plans are mandated for every city and county in California and typically cover a 20- to 30-year time period. Local authorities, either the Planning Commission and City Council for cities, or the Board of Supervisors for counties, must adopt a general plan. In practice, most local authorities appoint committees of residents to inform the process. In California, the Governor’s Office of Planning and Research outlines guidance for development of these plans, including the various elements that must be involved. Other states have similar requirements (and often refer to these plans as “Master Plans”). To date, elements directly addressing the health and justice implications of community design have never been included in the guidance but they are gaining attention.
C3 Improve safety and accessibility of public transportation, walking, and bicycling. Transportation is the means to accessing key destinations such as schools, workplaces, hospitals, and retail venues. Shifting the dominant mode of transportation from driving to greater public transportation use, walking and/or bicycling is a key step to increasing physical activity, reducing traffic injuries, and reducing developmental and respiratory illnesses from poor air quality. Strategies include:
- Implement land-use strategies such as high density, mixed-use zoning, transit-oriented development and interconnected streets that promote walking and bicycling as a means of transportation.
- Adopt complete streets policies in state and local transportation departments to ensure that roads are designed for the safety of all travelers including pedestrians, bicyclists, wheelchairs, and motor vehicles.
- Ensure that public transportation options are safe, easily accessible, reliable, and affordable.
- Design public transit routes to connect community residents to grocery stores, health care, and other essential services.
- Prioritize federal transit funding towards biking, walking, and public transportation.
New Jersey Safe Routes to School improvements in vulnerable communities
Safe Routes to School (SRTS) Federal funding gives states and localities a resource for programs that make walking and bicycling conditions safer, more accessible, and more convenient for children and their families. New Jersey Department of Transportation (NJDOT) is carrying out an Urban Demonstration Project in Newark, Trenton, and Camden to identify barriers to applying for and implementing SRTS programs in urban communities. NJDOT engaged students, school officials, and neighborhood partners to develop a needs assessment and a transportation plan that prioritized safe walking and bicycling. Through the community assessment process, NJDOT identified violence and crime, blighted buildings, and traffic safety as key concerns they will now address in the final package of infrastructure and programming improvements, using SRTS resources.
Congress created a $612 million federal SRTS program in the 2005 federal transportation bill to launch efforts from 2005 to 2009. The pending authorization of a new federal transportation bill can be an opportunity to substantially expand the SRTS program.
C4 Enhance opportunities for physical activity. Home, school, and community environments can either promote or inhibit physical activity. Physical activity is essential to preventing chronic illnesses and promoting physical and mental health. It is imperative to establish a foundation of activity behaviors from an early age and to provide environments with access to parks, open space, and recreational facilities that support people in attaining the daily recommended levels of physical activity.25 Strategies include:
- Develop and promote safe venues and programming for active recreation. Ensure parks, playgrounds, and playing fields are equitably distributed throughout the community.
- Facilitate after-hour (joint) use of school grounds and gyms to improve community access to physical activity facilities.
- Require recess and adopt physical education policies to ensure all students engage in develop- mentally appropriate moderate-to-vigorous physical activity on a daily basis.
- Establish state licensing and accreditation requirements/health codes and support implementation of minimum daily minutes of physical activity in after-school programs and childcare settings.
C5 Enhance availability of healthy products and reduce exposure to unhealthy products in underserved communities. The food retail environment of a neighborhood—the presence of grocery stores, small markets, street vendors, local restaurants, and farmers’ markets—plays a key role in determining access to healthy foods. Communities of color and low-wealth neighborhoods are most often affected by poor access to healthful foods.26 Research suggests that the scarcity of healthy foods makes it more difficult for residents of low-income neighborhoods to follow a good diet compared with people in wealthier communities.27 Strategies include:
- Invest in Fresh rood Financing Initiatives to provide grants, low-interest loans, training, and technical assistance to improve or establish grocery stores, small stores, and farmers’ markets in underserved areas.
- Encourage neighborhood stores to carry healthy products and reduce shelf space for unhealthy foods through local tax incentives, streamlined permitting, and zoning variances.
- Ensure grocery stores, small stores and farmers’ markets are equipped to accept Supplemental Nutrition Assistance Program (SNAP) (formally known as the Food Stamp Program) and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) benefits.
- Establish and enforce regulations to restrict the number of liquor stores and their hours of operation.
Fresh food financing to enhance the availability of healthy products in underserved communities
In 2004, the Food Trust in Philadelphia, PA, in partnership with The Reinvestment Fund and the Greater Philadelphia Urban Affairs Coalition, identified a strong need for government investment to finance supermarkets, grocery stores, and other healthy food retailers in underserved communities. This led to the first statewide fresh food financing initiative. The Philadelphia Legislature allocated $10 million in its annual appropriations in 2004, with additional funds allocated in 2005 and 2006, to establish a grant and loan program to encourage supermarket development in underserved areas. The Reinvestment Fund leveraged the investment to create a $120 million initiative composed of state dollars, federal tax credit dollars, and private investments. To date, the initiative has provided $63.3 million in grants and loans for healthy retail projects, resulting in the creation of and improvements to 68 stores that offer fresh foods. These projects have generating 3,734 jobs and 1.44 million square feet of floor space.28 It is now seen as a model and is being replicated in other US communities.
For more information, visit: www.thefoodtrust.org/
C6 Support healthy food systems and the health and well-being of farmers and farm workers. What farms grow, how they grow it, and how it gets to the consumer have a profound impact on what we eat, on our health, and on our environment. US farm policy and agricultural research and education have contributed to the proliferation of industrial farms that grow grains, oil seeds, corn, meat, and poultry that serve as raw ingredients for cheap soda, fast food burgers, and other highly processed products. These industrial farms pollute the air, water, and soil while harming our nutritional health. Small- and mid-size farmers are struggling to make a living under the current system. Farmers of color face discrimination in access to loans. Farm workers are exposed to hazardous levels of pesticides,29 dangerous working conditions, and poor wages and living conditions. Strategies include:
- Support small- and mid-sized farmers, particularly farmers of color, immigrants, and women through grants, technical assistance, and help with land acquisition, marketing, and distribution.
- Establish incentives and resources for growers to produce healthy products, including fruits, vegetables, and foods produced without pesticides, hormones, or non-therapeutic antibiotics.
- Establish policies that support the health and well-being of farm workers, including enforcing occupational safety and health laws and regulations as well as banning pesticides that may pose health risks. Government entities can also facilitate wage increases for farm workers by providing grants and incentives for growers to engage in labor-sharing strategies with other growers.
Linking green renovation standards and health outcomes
The National Center for Healthy Housing in Columbia, Maryland, is using support from the Blue Cross and Blue Shield of Minnesota Foundation to demonstrate how green building principles can improve health. The center is tracking the health impact of the green renovation of an affordable 60-unit apartment complex in Worthington, Minnesota. Residents are primarily low-income minority families employed in the food processing industry.
Results of this project can inform local zoning decisions and building codes. This is the first time the effect of green building principles will be measured against health outcomes over time. Early results include a majority of adults and children reporting improved health in just one year post-renovation. The adults made large, statistically significant improvements in general health, chronic bronchitis, hay fever, sinusitis, hypertension, and asthma. The children made great strides in general health, respiratory allergies, and ear infections. Overall, there were improvements in comfort, safety, and ease of housecleaning.
For more information, visit: www.nchh.org
C7 Increase housing quality, affordability, stability, and proximity to resources. High-quality, affordable, stable housing located close to resources leads to reduced exposure to toxins and stress, stronger relationships and willingness to act collectively among neighbors, greater economic security for families, and increased access to services (including health care) and resources (such as parks and supermarkets) that influence health. Strategies include:
- Support transit-oriented development and other policies and zoning practices that incentivize density, mixed-use, and mixed-income development.
- Ensure that housing standards; building permits for new buildings and rehabilitation; and housing inspections include safety and health considerations regarding design, the use of materials, and construction requirements.
- Protect affordable housing stock via rent control laws and condominium conversion policies, increase funding for emergency housing assistance, and maintain single room occupancy hotels.
- Support home ownership by creating community land trusts, increasing funds for and utilization of first-time home buyer programs, and establishing inclusionary zoning ordinances.
C8 Improve air, water, and soil quality. Environmental toxins present in air, water, soil, and building materials, including lead in soil and buildings, air pollution from motor vehicle traffic, and water pollutants, such as oil and human waste, have a substantial effect on health. Strategies include:
- Minimize diesel trucks in residential neighborhoods to reduce exposure to diesel particulates.
- Expand monitoring of air and water quality for impact on low-income and vulnerable populations.
- Enforce national water quality standards.
- Strengthen penalties for industrial and agricultural polluters.
- Replicate effective local lead abatement programs.
- Require public health input on air and water pollution impacts in local land use planning and development decisions.
Reducing toxic pollution in West Oakland
For two years, West Oakland residents and community partners worked to research and identify seventeen indicators to monitor environmental, health, and social conditions for their neighborhood. Residents then used the data in the indicators report to issue a formal request that the Bay Area Air Quality Management District (BAAQMD) develop stronger regulations requiring the Red Star Yeast factory (the area’s second leading source of toxic emissions) to reduce both pollution and noxious odors. The evidence in the report was also used to build media advocacy, testify at public hearings, and to garner letters demanding regulation and enforcement from the Department of Public Health and local elected officials. The combination of evidence and pressure led BAAQMD to remove the exemptions that had grandfathered Red Star Yeast into antiquated emissions standards.
For more information, visit: www.pacinst.org/reports/environmental_indicators/neighborhood_knowledge_for_change.pdf
C9 Prevent violence using a public health framework. Violence contributes to pre- mature morbidity and mortality and is a barrier to health-promoting activities, such as physical activity, and to economic development. Strategies include:
- Invest in citywide, cross-sector planning and implementation with an emphasis on coordinating services,30 programming, and capacity building in the most highly impacted neighborhoods, drawing on such tools as the UNITY RoadMap.*
- Support local intervention models to reduce the immediate threat of violence, such as the Chicago CeaseFire model.31
- Institute changes in clinical and organizational practices in health care settings to support and reinforce community efforts to prevent intimate partner violence, which results in injury and trauma from abuse, contributes to a number of chronic health problems,32 and disproportionately impacts immigrant women.33 (See Appendix F: The Role of Health Care Providers in Reducing IPV.)
______________
*The UNITY RoadMap is a resource for cities that maps out effective and sustainable solutions to prevent violence before it occurs. The UNITY RoadMap is informed by the findings from a literature review and interviews with violence prevention practitioners, vetted by city representatives and refined based on cities’ input. More information on both is available at: www.preventioninstitute.org/UNITY.html
Blueprint for Action: Preventing Youth Violence in Minneapolis
Recognizing that youth violence is a public health issue, the City of Minneapolis developed the Blueprint for Action: Preventing Youth Violence in Minneapolis. Using a comprehensive, holistic approach, the Blueprint aims to address the root causes of violence and significantly reduce and prevent youth violence using a combination of public health and law enforcement strategies. Under the leadership of Mayor JT Rybak, the Blueprint is the result of an 8-month collaborative process between the city and diverse community stakeholders. The four goals of the Blueprint are to:
- Connect every youth with a trusted adult;
- Intervene at the first sign that youth are at risk for violence;
- Restore youth who have gone down the wrong path; and
- Unlearn the culture of violence in the community.
Since the implementation of the Blueprint, juvenile-related violent crime citywide declined 37% since 2006 and 29% since 2007.34 In four of the five targeted neighborhoods, rates declined 43% in 2006 and 39% since 2007.35 Additionally, the City of Minneapolis has provided over twelve community organizations with grants to support youth employment, academic enrichment, and other community-based programs. Currently, the city has developed a youth violence prevention legislative agenda, which calls for a statewide policy that defines youth violence as a public health issue. It is a member of the UNITY City Network, a public health initiative funded by the US Centers for Disease Control and Prevention.
For more information, please see: www.ci.minneapolis.mn.us/dhfs/yv.asp for Blueprint for Action: Preventing Youth Violence in Minneapolis and http://preventioninstitute.org/UNITY.html for UNITY: Urban Networks to Increase Thriving Youth.
C10 Provide arts and culture opportunities in the community. Artistic and cultural institutions have been linked with lower delinquency and truancy rates in several urban communities,36 and participation in the arts has been associated with academic achievement, election to class office, school attendance,37 appropriate expression of anger, effective communication, increased ability to work on tasks, less engagement in delinquent behavior, fewer court referrals, improved attitudes and self-esteem, greater self-efficacy, and greater resistance to peer pressure.38 Strategies include:
- Support community art centers and other opportunities for creativity in the community.
- Integrate art and creative opportunities into existing programs and businesses.
- House art commissions within state or city government.
- Work with large art institutions, local policy makers, and residents to bring “Big Art” (e.g., museums and orchestras) to low- and middle-income communities.
- Implement a policy to receive a portion of every ticket sold in the community for movies, sporting events, etc. as an alternate source of funding for arts and culture. Another funding mechanism involves redirecting a portion of hotel and car rental taxes, since art contributes to enhancing the community.
Philadelphia’s Mural Arts Project
The Mural Arts Project (MAP) in Philadelphia has created 2,500 murals citywide. These murals have transformed otherwise depressed and blight-filled neighborhoods throughout Philadelphia into public art displays that cultivate neighborhood pride and reflect the culture, history, and vision of the communities in which they were created.
MAP is an offshoot of the Anti-Graffiti Network, an already existing program intended to provide alternatives to young people engaged in graffiti and other crime. Launched by former Philadelphia Mayor Wilson Goode in 1984, MAP became institutionalized within the city’s Department of Recreation more than ten years ago, and in this role it has created new partnerships among government agencies, educational institutions, corporations, and philanthropic foundations to bring murals to fruition. This program trains thousands of youth every year and provides them with the skills to contribute to the aesthetic of their own neighborhoods. It offers an alternative to gangs and a place to receive mentorship from working artists. More recently, in addition to working with youth, The Mural Arts Program began offering a wide array of mural-making programs for adult men and women at correctional facilities in Pennsylvania’s State Correctional Institution (SCI) and several sites within the Philadelphia Prison System.
In 1971, Seattle, Washington, established an Arts Commission by ordinance and issued a subsequent ordinance requiring all infrastructure projects to set aside 1% of their project costs for public art. Seattle is a national leader in providing residents and visitors with experiences in public art.
Enhance opportunities within underserved communities to access high-quality; culturally competent health care with an emphasis on community-oriented and preventive services
HC1 Provide high-quality, affordable health coverage for all. Everyone, including the most vulnerable populations, should have equal access to health care, including medical, dental, vision, and mental health services. There are a disproportionate number of racial and ethnic minorities who either do not have any health insurance or are enrolled in “lower-end” health plans.39 Strategies include:
- Equalize access to high-quality health plans to limit fragmentation of health care services. For example, Medicaid beneficiaries should be able to access the same health services as privately insured patients.40
- Ensure that all eligible children and families enroll in and access the State Children’s Health Insurance Program (SCHIP).
- Support safety net hospitals through state insurance coverage and state and local subsidies.41
- Ensure equitable support for dental and mental health services.
- Improve access through equitable and fair sharing of health care costs; streamline public health insurance enrollment and increase affordability of services within existing public programs, such as Medicaid; evaluate outreach to and enrollment of underserved populations; and support state and local legislative proposals for universal access to quality health care.
Health care coverage in Massachusetts42
Massachusetts’s Chapter 58 of the Acts of 2006 provides near-universal health insurance coverage and aims to ensure that all state residents have health insurance options that provide “minimal creditable coverage.” The law also has several key provisions that directly and indirectly address disparities in health care. Provisions include:
- Subsidizing health premiums for residents whose incomes fall below 300% of the Federal Poverty Level;
- Charging a new state entity, the Connector, to negotiate with health plans to increase the affordability of unsubsidized coverage and maximize the enrollment of low-income uninsured residents;
- Promoting the diversity and cultural and linguistic competence of health care professionals by establishing a Health Disparities Council in the Office of Minority Health;
Strengthening the data collection and monitoring of disparities through a Health Care Quality and Cost Council within the State Office of Health and Human Services charged with reducing racial and ethnic health disparities and publicly reporting disparities data.
HC2 Institute culturally and linguistically appropriate screening, counseling, and health care treatment. Culture shapes beliefs, behavior, and expectations surrounding health and health care. Physicians and other health care providers should deliver quality services in a culturally competent and sensitive manner. This approach can increase patient satisfaction, patient adherence to treatment plans, and the probability of improved health outcomes. Strategies include:
- Adopt standards of practice that are sensitive to the language and cultural needs of all patients.
- Provide training for providers to conduct screening, counseling, and treatment in both a culturally appropriate and sensitive manner.
- Promote culturally and linguistically appropriate screening programs for specific populations, such as Asian women for cervical cancer and other targeted groups for breast and cervical cancer.
- Ensure an effective communication strategy that takes into account the patients health literacy and preferred language.
- Ensure patient-system concordance (i.e., a setting of care delivery that optimizes patient adherence and a sense of security and safety).
California’s Health Care Language Assistance Act43
The first of its kind in the country, SB853 holds health plans accountable for the provision of linguistically appropriate services and requires the California Department of Managed Health Care to develop standards for interpreter services, translation of materials, and the collection of race, ethnicity, and language data. The bill was sponsored by the California Pan Ethnic Health Network. The law went into full effect on January 1, 2009.
Summary of SB 853 and its regulations:
- Health plans must conduct a needs assessment to calculate threshold languages and collect race, ethnicity, and language data of their enrol lees.
- Health plans must provide quality, accessible, and timely access to interpreters at all points of contact and at no cost to the enrol lee.
- Health plans must translate vital documents into threshold languages.
- Health plans must ensure interpreters are trained and competent and that translated materials are of high quality.
- Health plans must notify their enrollees of the availability of no cost interpreter and translation services.
- Health plans must train staff on language access policies and procedures and on working with interpreters and limited English proficiency patients.
Non-traditional approaches to improving immigrant mental health and social adjustment
This concerns how well both immigrants and their receiving communities are able to draw on their strengths and overcome the challenges affecting the health and vitality of entire communities. Recognizing that social capital/connectedness is a determinant of health, the Blue Cross and Blue Shield of Minnesota Foundation created Healthy Together: Creating Community with New Americans, a statewide grantmaking initiative to reduce health disparities for immigrants and refugees, supporting more than 140 projects since 2005. This effort can serve as a model for institutions and governments across the nation. Some promising strategies include:
- Helping new immigrants forge social connections and rebuild the sense of community they may have lost by connecting them to others facing similar issues and creating social gatherings through “Talking Circles.”
- Providing information and education and pursuing other means to “normalize” and remove stigma and misconceptions from mental health issues and treatment.
- Building on client’s strengths, helping them to reframe their experiences as survivors rather than as victims and to create their own solutions.
- Building cultural competence of providers to recognize mind/body connections and focus on symptoms. The report is available online at www.bcbsmnfoundation.org
HC3 Monitor health care models/procedures that are effective in reducing inequities in health and data documenting racial and ethnic differences in care outcomes. Detailed documentation of health care models/procedures will delineate the key elements of success. Currently, hospital practices for data collection vary widely as do the racial and ethnic classifications used. Strategies include:
- Standardize data: Collect race and ethnicity data in all health institutions. Coordinate state standards for data collection on race and ethnicity with federal standards to track the health of minorities.44 Although it may be difficult to use data to compare institution-to-institution, hospitals can use it to identify existing disparities in care and track trends for different patient populations within a hospital.
- Coordinate data collection and data systems beyond individual institutions and the health care system: Multiple partners from various sectors should be involved in outreach to different populations. For example, when addressing asthma management, school systems would be able to reach out to a broad range of school-aged children. Public health can play a key role in coordinating data collection at the community level and comparing it across systems.
- Disaggregate the data: Ensure that data reflects differences within the broad categories of race and ethnicity (particularly among Latino and Asian/Pacific Islander populations), as well as income levels, and duration of residence in the United States. Adopt uniform patient classifications in health information technology to make quality analysis easier and quicker. Analysis should be included in quality improvement initiatives.
- Incorporate new accreditation standards and mandates that account for equitable health care.
- Apply emerging data practices to better determine what medical procedures are most effective for different populations. (One size does not necessarily fit all.) Explore the Expecting Success disparities collaborative as one such example. Upon submission of their LOI, although the majority (97%) of the 122 hospitals were collecting patient race and ethnicity data, almost none reported using the data for quality improvement purposes at that time. Currently, they are among the most likely to have begun using quality data to reduce inequities in care.45
HC4 Take advantage of emerging technology to support patient care. Recent advances in health care technology can strengthen medical treatment. To the extent that technology is used as an element of quality medical care, it’s important to ensure that these advances fully benefit everyone. Cell phones are one area where there is a high degree of market penetration among all groups and so we should capture their potential to support medical treatment so as not to exacerbate disparities. When technology is not equally available (e.g., computers in every home), alternatives should be provided that are efficacious. Strategies include:
- Institute electronic health records that protect privacy but ensure caregivers have all needed information.
- Use telephone and email reminders to increase frequency of appointments and testing compliance, reduce failure to take pills, and encourage following procedures.
- Make tailored health information easily accessible and responsive.
Automated Telephone Self-Management Support System (ATSM)46
The Improving Diabetes Efforts across Language and Literacy (IDEALL) Project, run out of the California Diabetes Prevention and Control Program, is successfully utilizing health information technology as an efficient patient-centered approach to diabetes management for underserved populations with communication barriers such as limited literacy and limited English proficiency.47
IDEALL compared the effectiveness of two diabetes self-management support interventions (ATSM system and group medical visit support system) against the standard diabetes management approach. More than half of the participants had limited English proficiency, more than half had limited literacy, and half were uninsured. Participants in the ATSM group had the highest levels of participation and showed better communication with providers as compared to usual care and group medical visits. The ATSM participants also demonstrated significant increases in physical activity, exhibited the greatest improvements in carrying out daily activities, and spent fewer days in bed due to illness. Tailored to individual language and literacy need, the ATSM is a cost-effective intervention with great potential for underserved diabetes patients with low literacy and English proficiency levels.48
For more information, contact Dean Schil linger, MD, dschillinger@medsfgh.ucsf.edu
HC5 Provide health care resources in the heart of the community. Strengthening the presence of health care services located in communities of high need reinforces the connection between health care and community and can remove pervasive access barriers such as inadequate transportation options or not being able to seek health care during traditional working hours. Strategies include:
- Support community-based clinics. Clinics have an essential role in improving community health and providing services for uninsured and underserved populations. Clinics should establish organizational practices to increase access to equitable health care.
- Expand availability of school-based health clinics.
- Provide support groups that enhance self-efficacy in engaging in healthy behaviors.
- Provide culturally appropriate care such as translation services, disease prevention counseling, advocacy for quality health care, and other services to patients directly in the community, not just in health care settings.
- Expand the use of community health workers. Reforming reimbursement is essential, including state grants and seed funding as resources.49
- Change the available work hours and locations to meet the needs of patients.
Project Brotherhood in Chicago, Illinois
Supported by seed money from the Cook County Hospital, Project Brotherhood opened its doors as a health and human services provider to African American men in Chicago in 1998. With support from the Cook County Bureau of Health Services Health Center, Project Brotherhood provides services for men on a drop-in basis. Its explicit mission is to address the physical and mental health needs of a neglected population of Black men in a culturally relevant manner. There is no need for an appointment for physicals or lab tests, which are often needed in order to gain employment. Both primary and specialty health care are provided for free, allowing the low-income men that Project Brotherhood primarily serves to access high-quality, culturally appropriate health care that has historically been inaccessible. To increase levels of initial trust, the majority of staff is both African American and male, services are delivered in a less formal environment by offering weekly casual evenings where doctors, staff, and clients participate in informal support group discussions, and a barber provides free haircuts and counseling.
Project Brotherhood continues to grow the number of patients it is reaching with its services:50
- In 1999, Project Brotherhood averaged 4 medical visits and 8 group participants a week.
- By 2005, they averaged 27 medical visits and 35 group participants a week—and 14 haircuts per clinic session.
- No show rates of Project Brotherhood medical visits average 30% per clinic session compared to 41 % at the main health clinic.
- By 2007, Project Brotherhood provided services to more than 13,000 Black men.
On Lok Senior Health Services
With support from the City of San Francisco, in 1983, On Lok Senior Health Services obtained waivers from Medicare and Medicaid to test a new financing method for long-term care. In exchange for fixed monthly payments from Medicare and Medicaid for each enrollee, On Lok was responsible for delivering the full range of healthcare services. This model served as a prototype for a national initiative passed in the Balanced Budget Act of 1997—the Program of All-Inclusive Care for the Elderly (PACE), which receives funding from both Medicare and Medicaid and provides an alternative to the traditional nursing home model for elder care. As a certified PACE program, On Lok seniors who are both Medicare and Medi-Cal (Medicaid in California) beneficiaries receive comprehensive health and health-related services with no premiums or co-payments. Supplemental Security Income Program (SSI) benefits can also be contributed to the cost of On Lok services. For seniors who are only Medicare beneficiaries, the cost of services not covered by Medicare are paid for out-of-pocket and are determined by personal income and assets. Its main goal is to keep seniors at home living in their communities for as long as possible. On Lok’s services encompass full medical care, prescription drugs, home care, adult day health, transportation, and more. On Lok, means “peaceful, happy home” in Cantonese, the language spoken by most of its elderly participants. Although it is rooted in Chinese cultural traditions of reverence for elders, the program long ago branched out to serve other ethnic and racial groups.51 In expanding its services to various neighborhoods, a paramount consideration is the culture of the community it is serving.
HC6 Promote a medical home model. Having a designated health provider for every patient and, ideally, every family has enormous benefits. Primary care becomes more accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective. Patient-centered care is given within a community and cultural context. In 2007, the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, and American Osteopathic Association released the Joint Principles of the Patient-Centered Medical Home. Far fewer people of color have a medical home, which is strongly associated with prevention, screening, and specialty care referral.52 Strategies include:
- Design interventions to incorporate detection, prevention, and management of chronic disease with full deployment of multi- disciplinary teams that are family and patient centered.
HC7 Strengthen the diversity of the health care workforce to ensure that it is reflective and inclusive of the communities it is serving. The diversity of health care professionals is associated with increased access to and satisfaction of care among patients of color. States can adopt strategies such as loan repayment programs and service grants, health profession pipeline programs, and other incentives for service.53 Strategies include:
- Train clinic providers to conduct culturally appropriate outreach and services.
- Address the imbalance of health care providers by offering incentives to work in underserved communities.54 States could provide incentives that include funding graduate medical programs focusing on underserved populations, tuition reimbursement, and loan forgiveness programs that require service in Health Professional Shortage Areas (HPSAs).
- Expand use of Community Health Workers (CHWs) as a means of diversification. By acting as health connectors for populations that have traditionally lacked access to adequate health care, CHWs meet the ever-changing health needs of a growing and diverse population. Their unique ties to the communities where they work allow CHWs to understand cultural and linguistic needs and provide a resource for populations that are not necessarily connected or trusting of the medical system.
Invest in community health workers
The State of Kentucky dedicates $2 million annually for Kentucky Homeplace, an initiative that relies substantially on approximately 40 trained Community Health Workers (CHWs)* to deliver services to rural, underserved populations in 58 counties. Similarly, the City of Fort Worth, Texas, has permanently budgeted for 12 community health worker positions within their Department of Public Health. These particular CHWs are based in neighborhood police stations and work on teams with nurses and social workers responding to non-urgent health and social issues from the community at large. The City also supports the CHWs with training and with addressing issues of health disparities.
For nearly a decade, the Blue Cross and Blue Shield of Minnesota Foundation has served as a catalyst to promote the training and use of CHWs. The foundation’s support has led to:
- Sustainable financing—Minnesota is the only state, other than Alaska, to obtain Medicaid reimbursement for CHW services.
- An 11 -credit CHW certificate program based in the community college system.
- Peer learning and professional development through the Minnesota CHW Peer Network.
- A workforce development partnership through the Minnesota CHW Policy Council.
- Awareness building through a public television program and accompanying DVD.
- CHW models with a current focus on mental health.
- Health plan uptake at Blue Cross and Blue Shield of Minnesota through a CHW internship.
For further information on certain CHW services, visit www.mnchwinstitute.org/MN_Legislation.asp
* CHWs are also known as Lay Health Workers, Promotoras de Salud, Outreach Workers, or Community Health Advocates.
HC8 Ensure participation by patients and the community in health care related decisions. Research suggests that the consistency and stability of the relationship between patient and doctor is an important determinant of patient satisfaction and access to care. However, people of color are less likely to have a consistent relationship with a provider, even when insured at the same levels as White patients.55 Strategies include:
- Develop and strengthen patient education programs to help patients navigate the health care system.56
- Promote community health planning, which actively involves community residents in planning, evaluation, and implementation of health care efforts.57
Senior Injury Prevention Partnership (SIPP)
The population over age 60 will more than double nationally in the next 20 years. In 2005, people age 65 and older represented a little more than 10% of the population of Alameda County but accounted for more than 45% of all hospitalizations and deaths due to unintentional injury.58 Traditionally, injury prevention programs have focused primarily on children. The Senior Injury Prevention Partnership (SIPP), formed more than 10 years ago by the Alameda County Public Health Department and a diverse array of partner organizations, addresses the needs of the older population in our county. SIPP promotes a muIti-factoriaI fall-prevention program that includes: physical activity, home safety, education, and medication management. SIPP got its start with state and foundation grant funding. Following its initial success and advocacy by seniors, local government funding was also allocated. SIPP trains clinicians working with adults age 65 and over. Their program goes beyond the typical boundaries of the traditional medical model by putting peerled physical activity programs into place, which have proven to be as or more effective than programs led by clinicians.59 SIPP is currently hosting trainings for physical activity “lay leaders”—who are often older adults themselves—at senior centers, residential facilities, and other independent senior living locations. By bringing physical activity programs to seniors (rather than the other way around), SIPP increases the likelihood of participation and helps make the healthy choice the easy choice.
HC9 Enhance quality of care by improving availability and affordability of critical prevention services. Access to culturally competent, accessible clinical preventative services is a key ingredient to keeping people healthy. Examples include:
- Immunizations of children, adults and seniors.
- Regular monitoring of children’s growth.
- Assessment of prevention and safety behaviors (e.g., alcohol, tobacco, gun use; vehicle safety devices; family violence; risks including guns, STD’s).
- Medical testing and screening.
- Patient education, counseling, and referrals (e.g., smoking cessation, dietary counseling, and physical activity programs).
- Oral health, a key element of medical care that is too often overlooked.
A community-driven project to reduce STDs in Minneapolis60
Based in Minneapolis, MN, Seen on da Streets is a collaborative sexual health program targeting young African American males age 15 to 24 to reduce the prevalence of sexually transmitted diseases (STDs). The Seen on da Streets project is supported by a 5-year research grant from the US Department of Health and Human Services, Office of Population Affairs/Office of Family Planning. The federal support for the project totals $1,406,500 (97.7% of total costs) and the City of Minneapolis’ Department of Health and Family Support in-kind contribution totals $33,075 (2.3% of total costs). Additionally, Seen on da Streets received a $12,500 grant from the Community Capitol Alliance to add outreach services to young Latino men. Young adults, people of color, and low-income residents in Minneapolis are disproportionately impacted by STDs and unintended pregnancies, and young adult men in particular are far less likely to receive routine STD screening. Collaborating with two local clinics, the Minneapolis Department of Health hires young people of color from the most impacted communities to provide STD prevention education, risk assessment, and specimen collection for testing. By focusing the outreach on places where young men of color naturally congregate—including city parks, churches, barber shops, street corners, and job training centers—Seen on da Streets has over five years reached over 11,000 young people who would otherwise not have sought care. Over the course of the project, Chlamydia rates have only risen by only 2% in Minneapolis compared to 33% in other parts of Minnesota.
HC10 Provide outspoken support for environmental policy change and resources for prevention. In order to reduce racial and ethnic disparities, public policies and practices must address factors beyond medical care that impact health outcomes and disparities, specifically the community recommendations in this document. Strategies include:
- Advocate for community changes that will improve health outcomes and support disease management by speaking up in the media, community, and political environments and within health care institutions and associations and the broader health care community.
- Support pipeline development to recruit, train, and hire people from the community, especially from underserved sectors.
- Reduce waste and close incinerators to reduce local pollution.
- Purchase products and services from local businesses and organizations, such as food from nearby farms.
- Be attentive to community impact (e.g., reducing noise and emphasizing public transportation).
Strengthen the health system infrastructure to reduce inequities and enhance the contributions from public health and health care systems
S1 Enhance leadership and strategy development to reduce inequities in health and safety outcomes. High level leadership at state and local levels and clear strategic direction are essential to achieving equitable health outcomes. Strategies include:
- Engage civic leadership at the highest levels (e.g., mayors and governors) to coalesce influential partners, establish the priority of reducing inequities, ensure accountability, and use the bully pulpit to elevate the problem and solutions.
- Develop local and state plans that clarify what prioritized actions will be taken in order to achieve health equity.
Mayor’s Task Force Blueprint—A plan to eliminate racial and ethnic disparities in health
Boston Mayor Menino convened a blue ribbon task force, composed of leaders from academic institutions, community coalitions, health care, and insurance providers, to develop a blueprint of strategies that address social determinants and health factors that contribute to health disparities. The Boston Blueprint is divided into two sections: 1) Health Care and Public Health and 2) Environmental and Societal Factors. Each section includes specific recommendations and short-term and intermediate action steps.61 The Boston Health Commission issues progress reports that include a review of successes, lessons learned, and next steps. According to the Year One report, “Large numbers of Bostonians became educated about and involved in the issue of racial and ethnic health disparities. A platform for understanding and engagement has been set. Numerous health and social service agencies trained staff and mounted programs that paved the way for improved services to help reduce disparities in health status. There are notable outcomes from those efforts, including standardized disparities-related data collection in hospital settings, expanded health care quality improvement activities, enhanced patient navigation models, and innovative workforce development efforts.”62
S2 Enhance information about the problem and solutions at the state and local levels. A central challenge of 21st century American health policy is to characterize the powerful relationship between social inequities and health inequities and to identify comprehensive multi-disciplinary community-level interventions that systematically reduce social inequity. Strategies include:
- Develop, test, and disseminate new tools such as Connecticut’s Health Equity Index, BARHII’s social gradient analyses, San Francisco’s Healthy Development Measurement Tool, and other innovative tools that integrate information from varied domains to illuminate relationships between social measures and health status.
- Invest in better communicating the problem so that the general public and potential partners understand the underlying contributors to disparities and can evaluate the broader elements and potential solutions (e.g., the PBS documentary series, Unnatural Causes—Is Inequality Making Us Sick?)
Faith-based organizing for health equity
ISAIAH, a faith-based organization committed to racial and economic justice within 100 congregations in Minneapolis, St. Paul, and St. Cloud, Minnesota, is a vehicle for people of faith to work towards creating racially and economically just communities. This work requires that community members have the power to affect the underlying conditions that have an impact on the health of their communities.
Since 2008, ISAIAH has used the PBS series, Unnatural Causes—Is Inequality Making Us Sick?—in facilitated screenings. Twenty-seven ISAIAH congregations viewed the series with a guide adapted to include faith reflections and then held conversations with their local officials and 48 state legislators to create a new and uncommon conversation about health. The chair of the Senate Health Policy Committee hosted a viewing of the series, and the Service Employees International Union (SEIU) showed the series to health care workers.
Jewish Community Action and ISAIAH partnered to have an interfaith event with a synagogue, a catholic church, and a Unitarian church with the Senate Finance Committee Chair to introduce the Minnesota Healthy Communities Act, which was co-created by ISAIAH, SEIU, and the Minnesota Public Health Association. The Act includes a community-driven health impact assessment component.
S3 Establish sustainable funding mechanisms to support community health and prevention. Prevention rarely rises to the level of urgency that would support adequate funding, because public budgets remain in crisis mode and the pay off from prevention comes two or five or ten years down the road. Strategies include:
- Educate the broad public about the cost savings of health care and government investments in prevention.
- Create a wellness trust to collect, manage, and expend prevention funding, including indexing prevention to health care costs.
- Reinvest prevention savings in further prevention efforts.
S4 Build the capacity of state and local health agencies to understand and lead population-based health equity work. Having a public health workforce that is equipped to address issues of health equity and to convene key partners is a critical component of success. Public health practitioners have expressed an eagerness to address health equity and social justice along with an awareness that organizational support and staff capacity are crucial to moving this forward.63 Strategies include:
- Build the capacity of health departments to address issues of equity, including retraining and re- pooling of all staff working in public health and health service to have a solid grounding in the social determinants of health, health equity, and how to work with diverse sectors.
- Recruit and build a diverse health workforce reflective of underserved communities: Institute health equity studies in public health graduate programs; emphasize community-based equity work as a core public health competency and hiring criteria; build a diverse leadership team that includes people most affected; and develop pathways and pipelines for public health professionals to move from community-based equity work into leadership positions.
- Bolster Offices of Minority Health to support multiple sectors/efforts by serving as convener and coordinator of work that spans multiple departments and agencies; providing data sets that help inform and track progress; providing information on most effective practices and solutions;
developing policy solutions to be implemented by multiple sectors; and providing training and capacity building to support communities, public health, and other sectors to reduce inequities in health.
S5 Collaborate with multiple fields to ensure that health, safety, and health equity are considered in every relevant decision, action, and policy. Ensuring health in every policy will be essential in significantly improving health and safety outcomes and achieving health equity. Strategies include:
- Engage and coordinate the efforts of multiple sectors and diverse government agencies (e.g., business, labor, educators, public health, housing, transportation, environmental protection, and planning) to establish policies and efforts in support of health equity, including reducing barriers and improving incentives.
- Establish health and health equity impact/analyses: Evaluate proposed policies and funding streams with a “health lens” to determine impact on health, safety, and equity and ensure that consideration of health equity runs through all practices and policies within health institutions and beyond.
Washington State’s health care expansion laws address health disparities64
In 2006, the legislature in the state of Washington passed four bills addressing the health needs of communities of color, including the establishment of a Governor’s Interagency Coordinating Council on Health Disparities, biennial surveys on the diversity of the health care workforce, and review of the health disparities impact of pending laws. The council’s charge includes planning for the elimination of disparities in health and collaborating on health impact reviews. In 2007, the legislature took further steps by passing a package of three bills that move the state closer to universal health coverage and also address the health needs of communities of color by:
- Aligning the state’s health care resources with community needs, including a particular focus on community and migrant health clinics; and
- Requiring a “statewide health resources strategy” to survey state demographics, inventory health facilities, and assess health care needs geographically.
S6 Expand community mapping and indicators. Community mapping and indicators are emerging techniques that provide the opportunity to have collective community dialogues, to define the elements that comprise a healthy community, to translate community priorities into data that can be monitored over time, and to aggregate inexpensive, compelling, easy- to-use evidence for community advocacy. Strategies include:
- Develop and provide necessary data sets.
- Provide technical assistance on the technology and advocacy potential of maps and in support of local indicator projects.
- Establish standards and guidance for indicators and indicator reports to track improvements in inequities (i.e., the community characteristics and the health outcomes).
- Enhance state and local public health departments’ ability to access electronic health records and data to facilitate timely public health surveillance, trend and outbreak detection, and geographical analysis to link environmental determinants to patterns of disease distribution.
- Link the mapping of medical conditions and community conditions to better assess their interplay and develop effective environmental solutions that reduce the incidence of these conditions (e.g., compare traffic injury data to neighborhoods or diabetes rates to supermarket locations).
Jacksonville, Florida Quality of Life Progress Report
In 1985, the Jacksonville Community Council Inc. (JCCI) developed the nation’s first community-based quality-of-life indicators assessment. The assessment, published annually as the Quality of Life Progress Report, uses indicators to measure and monitor factors that encompass the social determinants of health in Jacksonville and surrounding communities in northeast Florida. In 2002, race relations and disparities in health and social circumstances based on race in Jacksonville were selected as a topic for deep community-led study The resulting study, guided by community participation, documented that racial disparities were prevalent locally in six areas: education, income and employment, housing, health, criminal justice, and the political process. Following completion of the study, JCCI produced a report outlining 27 recommendations to improve race relations in Jacksonville and eliminate racial disparities.
One of the primary recommendations stated that JCCI should convene citizens to create and distribute an annual report card on race relations in Jacksonville, modeled after the Quality of Life Progress Report. In 2005, JCCI released the first Race Relations Progress Report measuring race-based disparities as well as perceptions of racism and discrimination in the community. The report guides policy decisions and community work and measures progress toward an inclusive community free of race-based disparities or discrimination. It has since become an annual report card and review of its findings has become institutionalized in local government. Some of the policy changes that have resulted from the Progress Report’s findings include:
- Establishment of The Jacksonville Re-entry Center, a one-stop shop for ex-offenders looking for housing, employment, substance abuse treatment, legal assistance, and counseling.
- The Mayor embarked on a comprehensive literacy campaign.
- A Mayoral Proclamation and City Council Resolution supporting public policy that promotes equity and justice in Jacksonville.
- The City Council approved spending $900,000 to help supplement the JaxCare Program to reduce racial inequities.
- Provide access to tools and resources to assess and address the elements that can maximize health (e.g., indicators and report cards, maps, and community assessment tools).
- Provide access to high-quality, culturally appropriate technical assistance and training in planning, implementing, and evaluating.
Community planning using THRIVE
THRIVE (Tool for Health and Resilience in Vulnerable Environments) is a community resilience assessment tool that provides a framework for community members, coalitions, public health practitioners, and local decision makers to identify factors associated with poor health outcomes in communities of color, engage relevant stakeholders, and take action to remedy the disparities. Grounded in research, it has demonstrated utility in urban, rural, and suburban settings. Within months of piloting, several communities had initiated farmers’ markets and youth programs.65 One began to take health and safety considerations into account in planning decisions. At the community level, the THRIVE tool contributed to a broad vision about community health, confirmed the value of upstream approaches, challenged traditional thinking about health promotion, organized difficult concepts, enabled systematic planning, and proved to be a good tool for strategic planning at community and organizational levels.
For more information on THRIVE, visit: http://preventioninstitute.org/thrive/index.php.
Support local efforts through leadership, overarching policies, and through local, state, and national strategy
01 Develop a national strategy to promote health equity across racial, ethnic, and socioeconomic lines, with specific attention to preventing injury and illness in the first place. A national strategy could provide an overall framework and direction and set a clear expectation that reducing health inequities is a national priority. Although this paper is about local efforts, there is a critical interplay of the local, state, and national and thus we identify some of the national steps that must be taken in support of local approaches. Components of a national strategy should include:
- Establishing high-level leadership at the White House and the department level to serve as a focal point for strategy on health equity and to ensure collaboration among government agencies.
- Building the capacity of federal, state, and local health agencies to lead health equity work.
- Expanding funding for community-based initiatives.
- Providing technical assistance and tools to support community-level efforts to address determinants of health, improve health care outcomes, and reduce disparities.
- Supporting the development of national, state, and local data systems to inform community efforts, foster accountability, and build a stronger understanding of what it takes to achieve health equity.
- Furthering research on and significantly expanding the amount and proportion of federal research dollars for population-based prevention and health equity, with an emphasis on translating the findings into targeted, community-specific strategies.
- Fostering new leadership to advance health equity work and ensure that attention to achieving health equity is embedded into the priorities, practices, and policies of government entities, private organizations, the health care system, and communities.
World Health Organization’s Commission on Social Determinants of Health: Overarching Recommendations, 200866
- Improve the conditions of daily life—the circumstances in which people are born, grow, live, work, and age.
- Tackle the inequitable distribution of power, money, and resources—the structural drivers of those conditions of daily life—globally, nationally, and locally.
- Measure the problem, evaluate action, expand the knowledge base, develop a workforce that is trained in the social determinants of health, and raise public awareness about the social determinants of health.
02 Provide federal resources to support state and local community-based prevention strategies. Strategies for federal health agencies (such as Health and Human Services, the Centers for Disease Control and Prevention, Health Resources Services Administration, and the National Institutes of Health) include:
- Fund local public health agencies to craft local, flexibly designed community prevention strategies that are relevant to local conditions.
- Align existing strategies and policies with those of other federal agencies such as the Department of Education, Environmental Protection Agency, United States Department of Agriculture, Housing and Urban Development, and Department of Transportation so that states and local communities can leverage resources and efforts.
- Grant regulatory waivers to states seeking to create financial incentives for community-based prevention efforts that reduce medical care costs.
- Reimburse such strategies as fall-prevention for seniors, nurse home visitation for high risk infants, asthma environmental risk reduction initiatives, diabetes peer counseling, promotoras programs, and other proven and promising community-based prevention efforts must be reimbursed.
New York City Center for Economic Opportunity
The New York City Center for Economic Opportunity (CEO), established by Mayor Michael Bloomberg in December 2006, provides an innovative model for implementing, monitoring, and evaluating a successful urban anti-poverty agenda. Through its emphasis on strategies that achieve immediate results and longer-term investments focused on results-based policy and programmatic interventions, the CEO’s early successes and promising initiatives include:
- Developing an alternative to the outdated 40-year old federal poverty measure that more accurately captures the number of people living in poverty Congressman Jim McDermott (D-WA) and Senator Christopher Dodd (D-CT) have since introduced legislation to revise the federal poverty measure.
- Using pre-populated Earned Income Tax Credits (EITC) forms to help eligible low-income New Yorkers receive almost $14 million in EITC.
- Placing 2,166 low-income job seekers from high poverty areas in jobs in 2009.
- Providing financial and academic assistance to low-income students to attend City University of New York Accelerated Associate’s Program increasing anticipated
- 2-year graduation rates from 12.5% to 30%.
- Providing a Child Care Tax Credit for low- to moderate-income working families that provided $30 million in assistance to over 50,000 eligible families in the first year alone.
Building on the local success of CEO, New York City has recently put forth a proposal for a Federal Urban Innovation Fund to be administered by the White House to help support a national urban poverty agenda by dissolving the existing government silos that have hampered success.
For more information about the Center for Economic Opportunity, visit: www.nyc.gov/ceo
03 Tackle the inequitable distribution of power, money, and resources—the structural drivers of the conditions of daily life that contribute to inequitable health and safety outcomes—and especially address race, racism, and discrimination in institutions and polices; racial and socioeconomic segregation; and socioeconomic conditions. Poverty, racism, and lack of educational and economic opportunities are among the fundamental determinants of poor health, lack of safety, and health inequities. Strategies include:
- Assess institutional policies and practices for race, racism, and discrimination—including holding discussions about race and racism within institutions—and modify practices and policies accordingly.
- Conduct a comprehensive review of policies and practices that contribute to racial and socioeconomic segregation, delineate recommended policies to reverse segregation, and include attention to demonstrated promising strategies to reverse residential segregation.
- Improve socioeconomic conditions by 1) raising incomes of the poor, especially those with children (increase enrollment in income support programs; raise the state minimum wage; implement local living wage ordinances); 2) assisting poor people in accumulating assets (provide education and financial counseling to increase access to savings accounts and investment programs; expand home ownership and micro-enterprise opportunities);and 3) supporting job creation and workforce development (negotiate community benefits agreements; preserve industrial land for well-paid jobs; expand local green collar jobs; increase access to education, training, and career ladders; fund job readiness and skill-building programs).
- Reform criminal justice laws to address disproportionate incarceration rates for African Americans, Latinos, and low-income people such as by decriminalizing addiction and implementing community programs for drug offenders in lieu of prison; supporting mental health treatment for those in need, including those with Post Traumatic Stress Disorder; and supporting effective re-entry programs.
“It is not possible to eliminate health disparities without simultaneously reducing disparities in educational achievement. By bringing together programs to improve health and school achievement and by making reducing school dropout rates a public health, educational, and human rights priority, public health professionals have the opportunity to make a lasting contribution to promoting population health and social justice.”
REFRAMING SCHOOL DROPOUT AS A PUBLIC HEALTH ISSUE, CDC ARTICLE, OCT. 2007
04 Improve access to quality education and improve educational outcomes. Educational attainment is one of the strongest predictors of income, and there is a strong relationship between income and health.67,68 Even independent from income, education is associated with improved health outcomes: each additional year in school correlates to increased life expectancy and better health.69 Strategies include:
- Reform school funding to equalize access to quality education in K—12, including providing equal access to technology to develop job readiness for 21st century jobs.
- Invest in recruiting, training, and retaining teachers, particularly to work in disadvantaged schools, and create incentives for teachers to remain in these schools.
- Provide need-based supports to schools, students, and parents—including positive interventions for at-risk middle and high school students and creating greater support for low-income parents of color to participate in their child’s education.
Library cards for all
A simple yet innovative change in practice resulted in more young people reading, engaging in meaningful opportunities, having a safe place to gather, and connecting with their community. In Salinas, California, the library and schools partnered to provide all students with library cards, free of charge and application-free. Further, the library eliminated fines and fees for the first year to enable students to learn about using the library. Since the change, the library has seen a significant increase in library usage by young people and their families. Moreover, the community feels the importance of libraries in their lives, a constituency for libraries has been built, and more young people and their families are reading and spending time together.
05 Invest in early childhood. During the first five years of life, every encounter a child has or lacks is formative. For healthy development, young children need a range of supports, social and emotional care, and nurturing.70 Strategies include:
- Provide high quality and affordable child care and preschools; ensure equitable distribution of and access to preschools and provide subsidies.
- Invest in home visiting initiatives such as the Nurse Family Partnership.
- Invest in recruiting, training, and retaining child care providers.
Consistent investment in Nurse Family Partnership (NFP) initiatives
NFP is a child abuse prevention and mental health treatment program in which trained public health nurses make regular home visits to low-income, first-time mothers. Designed by Dr. David Olds of Colorado, the program reduces the child’s risk for antisocial behavior by improving maternal and child health and reducing the risk of child abuse. Visits from nurses during pregnancy and through the first two years of a child’s life help parents promote healthy emotional development, establish a positive relationship with their child, and build self-efficacy as an adult and parent.
The program has been successfully implemented in rural, urban, and various ethnic communities. It has reduced child abuse by 80% in the first two years of the child’s life and had significant long-term benefits. Fifteen years after services ended, participants had one-third as many arrests and their children were half as likely to be delinquent compared to mothers and children without services. Women in the program also spent less time on welfare, smoked fewer cigarettes, and consumed less alcohol than families in control groups.71
States have utilized a number of mechanisms to secure ongoing funding: tobacco settlement dollars (Colorado, as defined by the Colorado Nurse Home Visitor Act), Medicaid Reimbursement and Block Grants (Louisiana), state appropriation (Oklahoma), and Temporary Assistance for Needy Families (Pennsylvania).
Conclusion:
A Time of Opportunity
As interviews with public health leaders confirm, this is a time of opportunity. (For more detailed information, please see Appendix G: Opportunities.) Nationally, health and health care have emerged as major economic issues and as top priorities of the new Administration and Congress. There is growing understanding of the importance of healthy communities, the influence of their underlying health determinants, and of the role of culturally appropriate, family-centered primary care in accomplishing health equity.
Over the past several decades, there has been a general shift towards moving social programs from federal to state governments—a “devolution of authority.” Although federal initiatives provided the catalyst for health disparities to emerge as a public health issue, states are now poised to build on this opportunity and take the lead in sponsoring policies and social programs that help reduce inequities. States are seen as a key place for health reform.72 Numerous health departments are engaging in efforts to advance health equity in communities large and small, urban and rural.73
Focusing equity efforts at the state and local levels is promising because many of the social and economic health determinants can be acted upon at these levels. There is a strong national trend toward using community-level health indicators and indicator data to monitor change over time, increase accountability among policy makers, and engage communities in a dialogue about local priorities.
What’s good for our health is good for our overall well-being. For example, the mounting concern over environmental degradation and the increased focus on prioritizing solutions, have introduced an opportunity to align issues of health and health equity with those of the environment and improve both simultaneously. Health is not only a major issue in and of itself, but it aligns with many of the other major concerns of our society.
In real estate, there are only three things that matter—location, location, location. Our conclusion as authors is that policy is vital and changing our organizational practices is critical; and it all must be done in service of people, where they live, work, play, socialize, and learn. In other words—community, community, community.
Acknowledgments
The authors would like to acknowledge the IOM Roundtable on Health Disparities for their commitment to addressing this important issue and tor the opportunity to write this background paper. This report was produced in part with core support funding from Kaiser Permanente.
This paper builds on previous work of the Institute of Medicine, the authors, and many others who have contributed to better understanding and addressing health inequities. This paper synthesizes various bodies of work and input from many individuals. We apologize for any oversights and omissions, which are unintentional. We would like to thank the many people who provided input during the development of this paper. Their insight has been invaluable. They are:
Manal Aboelata, Prevention Institute Karen Anderson, Institute of Medicine
Laurie Andress, Andress & Associates, LLC, Bridging the Health Gap
Judith Bell, PolicyLink
Georges Benjamin, American Public Health Association
Clement Bezold, Institute of Alternative Futures
Paula Braveman, University of California San Francisco
Colleen Campbell, Alameda County Department of Public Health
Joan Cleary, Blue Cross and Blue Shield of Minnesota Foundation
Ellen Clement, Washtenaw County Public Health Department
Sue Egerter, University of California San Francisco
Barbara Ferrer, Boston Public Health Commission
Jonathon Fielding, Los Angeles Public Health Department
Lark Galloway-Gilliam, Health Equity Coalition
Randall Henry, Veteran Affairs Greater Los Angeles Healthcare System
David Johnson, Minneapolis Department of Health and Family Support
Jim Krieger, Public Health - Seattle and King County
Julie Lee, Blue Cross and Blue Shield of Minnesota Foundation
Caya Lewis, Senate HELP Committee
Nicole Lurie, RAND
James Marks, Robert Wood Johnson Foundation
Steve Marks, Jewish Family and Children Services of Southern Arizona, Inc.
Leslie Mikkelsen, Prevention Institute
Edward O’Neil, University of California San Francisco
Bob Prentice, Bay Area Regional Health Inequities Initiative
Sara Rosenbaum, George Washington University
Anja Rudiger, National Economic and Social Rights Initiative/National Health Law Program
Linda Rudolf, Center for Chronic Disease Prevention and Health Promotion California
Department of Public Health
Eduardo Sanchez, Blue Cross Blue Shield of Texas
Dean Schillinger, UCSF Center for Vulnerable Populations
Bruce Siegel, George Washington University School of Public Health and Health Services
Brian Smedley, The Joint Center for Political and Economic Studies
Hal Strelnick, Albert Einstein College of Medicine, Montefiore Medical Center
Mildred Thompson, PolicyLink
Robin Weinick, RAND
Winston Wong, Disparities Improvement and Quality Initiatives Kaiser Permanente
Michael Woods, Project Brotherhood
Ellen Wu, California Pan-Ethnic Health Network
The authors would also like to acknowledge their skilled editor, Anne Paniagua, who worked tirelessly to make the paper as clear and concise as possible and their graphic designer, Susan Lock- wood of lockwood design, who worked quickly to turn around the final report.
Health Equity Toolkit Key Informants
Additionally, Prevention Institute conducted a set of key informant interviews with public health practitioners during Spring 2008, with funding from the Robert Wood Johnson Foundation, to inform the development of a Health Equity Toolkit. Prevention Institute synthesized interview findings and highlighted core themes from these interviews which are reflected in the challenges and opportunities sections of the paper and informed our thinking for the paper in general. Key informant interviews were conducted with:
Jayne Andreen, Alaska Department of Health and Social Services
Bobbi Berkowitz, University of Washington — School of Nursing, Department of Psychosocial & Community Health
James Bloyd, Cook County Department of Public Health
Andrew Goodman, New York City Department of Health and Mental Hygiene
Heidi Hataway, Alabama Department of Health
Richard Hofrichter, National Association of County and City Health Officials Frances Kaplan, Arizona Department of Health Services Vincent Lafronza, CommonHealth Action
Gwen Lipscomb, Alabama Department of Public Health, Minority Health Office
Zipatly Mendoza, Arizona Department of Health Services
Ngozi Oleru, Seattle & King County Department of Public Health
JT Petherick, Cherokee Nation
Paul Simon, Los Angeles County Department of Public Health
Adewale Troutman, Louisville Metro Public Health and Wellness, Center for Health Equity
Sandra Witt, Alameda County Public Health Department
Appendix A
Inequitable Rates of Morbidity & Mortality
Racial and ethnic minorities continue to experience higher rates of morbidity and mortality than non-minorities.74 Low-income populations and people of color do not experience different injuries and illnesses than the rest of the population; they suffer from the same injuries and illnesses, only more frequently and severely. For example:
- Compared to Whites, American Indians and Alaska Natives are 2.3 times more likely to have diagnosed diabetes, African Americans are 2.2 times more likely, and Latinos are 1.6 times more likely.75
- Among African Americans between the ages of 10 and 24, homicide is the leading cause of death. In the same age range, homicide is the second leading cause of death for Hispanics, and the third leading cause of death for American Indians, Alaska Natives, and Asian/Pacific Islanders.76 Homicide rates among non-Hispanic, African American males 10 to 24 years of age (58.3 per 100,000) exceed those of Hispanic males (20.9 per 100,000) and non-Hispanic, White males in the same age group (3.3 per 100,000).77
- Native Americans have a motor vehicle death rate that is more than 1.5 times greater than Whites, Latinos, Asian/Pacific Islanders, and African Americans.78,79
- Poverty is associated with risk factors for chronic health conditions, and low-income adults report multiple serious health conditions more often than those with higher incomes.80
- The average annual incidence of end-stage kidney disease in minority zip codes was nearly twice as high as in non-minority zip codes.81
- Premature death rates from cardiovascular disease (i.e., between the ages of 5 and 64) were substantially higher in minority zip codes than in non-minority zip codes.82
- Education correlates strongly with health. Among adults over age 25, 5.8% of college graduates, 11% of those with some college, 13.9% of high school graduates, and 25.7% of those with less than a high school education report being in poor or fair health.83
Appendix B
Definitions of Health Disparities and Health Inequities
The National Institutes of Health defines health disparities as “differences in the incidence, prevalence, mortality, and burden of diseases and other adverse health conditions that exist among specific population groups in the United States.”84
Health inequities are “differences in health which are not only unnecessary and avoidable but, in addition, are considered unfair and unjust.”85
Thus, equity and inequity are based on core American values of fairness and justice whereas “disparity” is a narrow descriptive term that refers to measurable differences but does not imply whether this disparity arises from an unjust root cause.
For the purposes of this paper, the term “inequity” is used when the referenced differences in health outcomes have been produced by historic and systemic social injustices, or the unintended or indirect consequences of social policies.
Appendix C
The Economics of Prevention—Reducing Health Care Costs through Prevention
Currently, health care spending is growing at an unsustainable rate86 (see Figure 1) driven by both rising costs and a growing burden of disease. In addition to straining public resources, the costs are bankrupting families and small businesses, and putting corporations and industry at a competitive disadvantage. How do we remedy this? The long-term solution must involve both cost containment and reduced demand for services. Currently, our nation spends over two trillion dollars each year on health expenditures and approximately 96% of this is expended on medical services—treatment after the onset of illnesses and injuries.87 Nevertheless, access to health care only accounts for 10% of the variation in morbidity and mortality; other factors that determine health include environments and behaviors.88
A vital strategy for creating a sustainable health care system is to improve health status through prevention- reducing demand not by denying service but by reducing the need for service. A review of the literature89 shows the following:
- A majority of the most costly health conditions are preventable.
- Health-related resources are not invested in the areas that most influence health.
- A 5% reduction in preventable illnesses and injuries could lead to substantial savings.
- Savings have been demonstrated and forecasted for specific prevention initiatives.
- Prevention has the potential to reduce end-of-life care costs.
- Savings from prevention accrue beyond the health care sector.
- Prevention could help improve productivity and competitiveness.
- New economic models predict potential cost savings from prevention.
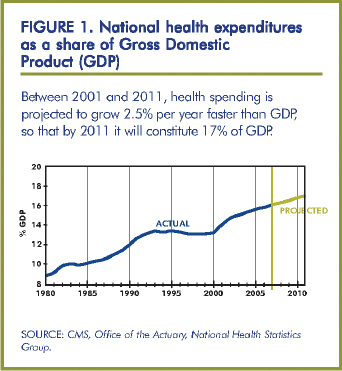
Further, an economic analysis revealed that investing even the modest amount of $10 per person in community level initiatives aimed at reducing tobacco consumption, improving nutrition, and increasing physical activity results in a return on investment within two years and an estimated annual savings of over $15 billion nationally within five years.90 Each year thereafter, the 5 to 1 return on investment is projected to continue. The savings from an investment in prevention in disenfranchised communities should be even greater because they experience the greatest burden of ill health. In addition to this chronic disease analysis, studies reveal that other health-related investments also yield a significant return. For instance, $1 invested in breastfeeding support by employers results in $3 in reduced absenteeism and health care costs for mothers and babies and improved productivity; $1 invested in lead abatement in public housing returns $2 in reduced medical and special education costs and increased productivity; and $1 invested in workplace safety measures returns $4 to $6 in reduced illnesses, injuries, and fatalities.91,92
Appendix D
Reasons why addressing access to and quality of health care alone will not significantly reduce inequities
1. Health care is not the primary determinant of health. Of the 30-year increase in life expectancy since the turn of the century, only about five years of this increase are attributed to medical care interventions.93 Even in countries with universal access to care, people with lower socioeconomic status have poorer health outcomes.94
2. Health care treats one person at a time. By focusing on the individual and specific illnesses as they arise, medical treatment does not reduce the incidence or severity of disease among groups of people because others become afflicted even as others are cured.95
3. Health intervention often comes late. Medical care and intervention play important restorative or ameliorating roles after disease occurs. Further many of today’s most common chronic health conditions, such as heart disease, diabetes, asthma, and HIV/AIDS, are never cured. It is extremely important to prevent them from occurring in the first place and, when they occur, their ongoing prognosis will depend on a number of factors in addition to medical care.
Appendix E
A Health Equity Framework: Taking Two Steps Back to the Determinants of Health
The frequency and severity of injury and illness are not inevitable. Τhe Two Steps Back framework was developed as a tool for analyzing the underlying causes of illness and injury and health inequities and identifying the key opportunities for intervention and prevention. Two Steps Back presents a systematic way of looking at needed medical services and then traveling back to the exposures and behaviors that affect illness and injury and then back to the underlying community conditions that shape patterns of exposure and behavior.

STARTING WITH MEDICAL CARE
Medical care aims to improve health outcomes by focusing on identifying and treating specific medical conditions (e.g., heart disease, diabetes and infections) with medical services. High-quality medical care can prevent the onset of some medical conditions, diagnose problems early, reduce the severity of symptoms, and slow the progression of secondary conditions. The Institute of Medicine’s Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care identified three primary ways to intervene to reduce health inequities through medical care:96
- Increase access to care: Within our current system, lack of insurance and under-insurance, major barriers to accessing medical care, are not borne equally across racial and ethnic lines.
- Improve quality of care (diagnosis and treatment):Unequal Treatment documents that “evidence of racial and ethnic disparities in healthcare is, with few exceptions, remarkably consistent across a range of illnesses and healthcare services.” Unequal Treatment reveals that differences in diagnosis, quality of care, and treatment methods lead to consistently poorer health outcomes among people of color.
- Implement culturally and linguistically appropriate care: A culturally competent system of care is measured both by achieving the desired health outcome and patient satisfaction with medical encounters.97
TAKING A STEP BACK:
From Medical Care to Exposures and Behaviors
Medical care alone cannot eliminate health disparities. The first step back is from medical care to exposures and behaviors. Limiting unhealthy exposures and behaviors enhances health and reduces the likelihood and severity of disease. Through an analysis of the factors contributing to medical conditions that cause people to seek care, researchers have identified a set of nine behaviors and exposures strongly linked to the major causes of death: tobacco, diet and activity patterns, alcohol, microbial agents, toxic agents, firearms, sexual behavior, motor vehicles, and inappropriate drug use.98 These behaviors and exposures are linked to multiple medical diagnoses sand addressing them can improve health broadly. For example, tobacco is associated with a number of health problems including
lung cancer, asthma, emphysema, and heart disease. Diet and activity patterns are associated with cardiovascular and heart disease, certain cancers, and diabetes, among other illnesses.
As a result, reducing exposures and unhealthy behaviors decreases the risk of multiple injuries and illnesses. It is also important to include analysis of exposure to the stressors of poverty, racism, lack of opportunity, etc. Exposure to these stressors affects low-income communities and people of color disproportionately, and similar to the nine listed above are contributing factors in multiple health conditions and opportunities for intervention.
THE SECOND STEP BACK:
From Exposures and Behaviors to the Environment
Exposures and behaviors are determined or shaped by the environments in which they are present, defined as anything external to individuals and shared by members of a community. Exposures, of course, are shaped by what in the environment one is exposed to, and behaviors are shaped (encouraged or discouraged) by what is available in communities and the norms that communities help shape. Taking the second step back from exposures and behaviors to the environment, presents a tremendous opportunity to reduce health inequities by preventing illness and injury before their onset. The environment includes root factors (e.g., poverty, racism, and other forms of oppression), institutions, and community factors. THRIVE (Tool for Health and Resilience in Vulnerable Environments), a research-based framework created by Prevention Institute, offers a way to understand the community factors.99 THRIVE includes 13 community health factors grouped into three clusters: people, place, and equitable opportunity. Similar work by other researchers confirms this overall approach. For example, in 2002 Policy Link published very similar findings and factors in the report, Reducing Health Disparities Through a Focus on Communities.100
The 13 community factors are organized into 3 interrelated clusters: equitable opportunity, people, and place (see Table 1: Community Factors Affecting Health, Safety, and Mental Health) and either directly influence health and safety outcomes via exposures (e.g., air, water, soil quality; stressors) or indirectly via behaviors that in turn affect health and safety outcomes (e.g., the availability of healthy food affects nutrition). In addition, the environment also influences people’s opportunity to access quality medical services, and these are included as a 4th cluster. The clusters are described here:
EQUITABLE OPPORTUNITY: This cluster refers to the level and equitable distribution of opportunity and resources. Root factors, including poverty, racism, and lack of educational and economic opportunities are among the fundamental determinants of poor health, lack of safety, and health inequities. They each contribute to chronic stress and can build upon one another to create a weathering effect, whereby health greatly reflects cumulative experience rather than chronological or developmental age.101 Chronic stress increases risk for coronary artery disease, stroke, cognitive impairment, substance abuse, anxiety, depression, mood disorders, and accelerated aging and cancer.102 Further, economic and racial segregation is one of the most powerful forces shaping health in the US. The availability of jobs with living wages, absence of discrimination and racism, and quality education all affect health and safety.103,104 This segregation is not inevitable; it has been established and maintained through government policy and investment and the practices of institutions and organizations.105 Examples include redlining (wherein low- income neighborhoods and neighborhoods with primarily people of color are identified for discriminatory investment by banks and other lenders, historically by drawing a red line on a map); discriminatory application of GI Bill housing benefits; unequal investment in schools and transportation (leaving low-income communities at an educational and geographic disadvantage, which restricts social and economic mobility and development leading to further concentration of poverty); and judicial rulings such as the Supreme Courts recent ruling (Parents Involved in Community Schools v. Seattle School District) that reverses much of Brown v. Board of Education, which ruled that separate was not equal.)
PEOPLE: This cluster refers to the relationships between people, the level of engagement, and norms, all of which influence health and safety outcomes. For instance, strong social networks and connections correspond with significant increases in physical and mental health, academic achievement, and local economic development, as well as lower rates of homicide, suicide, and alcohol and drug abuse;106,107 children have been found to be mentally and physically healthier in neighborhoods where adults talk to each other.108 Social connections also contribute to a community’s willingness to take action for the common good which is associated with lower rates of violence,109 and improved food access.110
PLACE: This cluster refers to the physical environment in which people live, work, play, and go to school. Decisions about place have multiple direct and indirect effects on health and safety. For example, physical activity levels are influenced by conditions such as enjoyable scenery,111 the proximity of recreational facilities, street and neighborhood design,112 and transportation design;113 each supermarket in an African American census tract, fruit and vegetable intake has been show to increase by 32%;114 and the presence of alcohol distributors in a community is correlated with per capita consumption.115
HEALTH CARE SERVICES: Over the course of our lives we also all want and need health care, including good medical, mental health, and dental services. As a starting point, people need to be able to obtain quality medical and dental care, which means people need adequate and affordable health insurance. To help maintain health, people need preventive care and chronic disease management. In crisis situations, we need reliable, immediate, and qualified emergency medical responses. When we suffer from acute or chronic conditions, we hope for quality medical care to treat or cure our conditions, or help us manage them. For all of these services, culturally and linguistically appropriate patient care is critical for communicating with patients and addressing health concerns within the cultural context of the patient.
Appendix F
The Role of Health Care Providers in Reducing Intimate Partner Violence (IPV)
Health care providers are at the intersection of health, violence, and community. They can use their tremendous influence and credibility to help tip the balance and more systematically prevent IPV.
Clinical Practice
As sources of credibility and regular interaction, health care providers play an important role in the primary prevention of IPV.116,117 Major clinical practices that support IPV prevention include engaging women in an empowering way,118 promoting healthy relationships and sexuality, and dialoguing with parents and parents-to-be. Examples include:119-122
- Examining own personal attitudes that may serve to contribute to prevalent social norms that allow for abuse (i.e., blaming the victim). “Why won’t she leave?” needs to be replaced with “What will make him stop?”123-125
- Using a longitudinal, age-specific approach to engage women and girls developmentally to help reinforce messages throughout a woman’s life stages.126
- Engaging patients as active participants during regular examinations through dialogue and a restructuring of the examination room.
- Dialoguing with parents and parents-to-be, such as encouraging parents to promote flexible sex role socialization of their children by broadening the views of parents regarding behaviors considered “natural” for either gender.127, 128
- Promoting and modeling healthy relationships.
Organizational Practices
Since institutions shape and reinforce norms, it is critical that healthcare settings and professional associations establish and promulgate regulations, practices, and cultures that contribute to IPV reduction. Areas of focus include training and policies, as well as reflecting an egalitarian culture and intolerance of violence and patriarchy. Examples include:
- Establish work place policies that are in alignment with ending IPV (e.g., anti-harassment policies and training on and modeling egalitarian relationships and appropriate ways of handling conflict.)
- Establish policies to enable healthcare practitioners to teach about IPV in the community.
- Provide information and resources to patients, such as in waiting rooms and clinics, about healthy relationships and to raise clients’ consciousness of sexist attitudes in the media that promote sex and violence.129-131
- Encourage ongoing professional development and continuing education on preventing IPV that includes promoting healthy relationships and sexuality.
Spokesperson/Advocate
Health care institutions and providers can be powerful advocates for prevention. Providers must speak up in their clinical practices, in their organizations and associations, and broadly to the public, the media, and policymakers. By speaking up in public meetings, serving as experts to the media and testifying to legislators, health care providers can shape issues, influence the debate, and challenge public and political discourse. Examples include:
- Advocating for decreases in the portrayal of violence in the media,
- Supporting state and national legislative efforts, and
- Petitioning for legal remedies designed to protect women.132
Appendix G
Opportunities
Building on interviews with local health officers conducted to inform the development of a Health Equity Toolkit funded by the Robert Wood Johnson Foundation as part of the project Advancing Public Health Advocacy to Eliminate Health Disparities, we have identified opportunities to advance health equity work.
1. The time has come for health reform
Nationally, health and health care have emerged as major economic issues and as top priorities of the new Administration and Congress. When we consider health reform it is critical that we highlight underlying determinants of health. We have made the case for the economics of community-oriented prevention.133,134 With a growing awareness of community conditions tor health, of tools that help make the case for addressing the underlying causes of health inequities (e.g., the PBS documentary series, Unnatural Causes: Is Inequality Making Us Sick?), and of the role of culturally appropriate, family-centered primary care, the pieces are in place to inform a more equitable, health-producing health system that is sustainable for all. To reduce inequities in health and safety, health reform will need to draw upon community-level prevention to decrease the number of people getting sick and injured; reimburse for medical services, including preventive medical services that are delivered in communities; and assure that system redesign enables the delivery of high-quality, culturally appropriate health care services for all.
2. It makes a lot of sense to focus at the state and local levels to address inequities
Over the past several decades, there has been a general shift towards moving social programs from federal to state governments—a “devolution of authority.” Although federal initiatives provided the catalyst for health disparities to emerge as a public health issue, states are now poised to build on this opportunity and take the lead in sponsoring social programs that help reduce inequities. States are seen as a key place for health reform.135 Numerous health departments are engaging in efforts to advance health equity in communities large and small, urban and rural.136 In some cases, departments are deeply engaged in equity-tocused work and are creating organizational structures and processes to focus specifically on health equity. In other cases, departments are engaged in supportive ways, sharing resources and information with community-based organizations that are providing more of the leadership and energy behind equity efforts. Many health departments are in an exploratory phase, examining internal interest and opportunities for addressing health equity.
Focusing equity efforts at the state and local levels is promising because many of the social and economic health determinants can be acted upon at these levels. For example, a local health department seeking to ensure quality affordable housing can work with the local community development and housing agency to discuss proposed projects, provide data about their potential health impacts, and work with local residents to explore their needs and concerns. Commitment and optimism about health equity becoming a centerpiece of the public heath agenda remains high within health departments as they strive to make the internal and external changes neces-
sary to take on an equity-related focus. There remains a need to further coalesce and project a stronger community voice, though partnerships with community organizations and policy makers have proven successful.137
3. Our ability to map, measure and track is improving significantly
Emerging technologies, coupled with new and expanding sources of data, are providing significant support in reducing health inequities. For instance, community-based organizations and public agencies are increasingly using maps to support social and economic change on a community level. Mapping is a powerful tool in two ways: (1) it makes patterns based on place much easier to identify and analyze and (2) it provides a visual way of communicating those patterns to a broad audience, quickly and dramatically.138 Projects such as Healthy City in Los Angeles allow users with minimal technical skill to create a variety of maps that highlight patterns of community resources, community conditions (e.g., income level or air quality), and health and social outcomes (e.g., disease rates or high school graduation rates). These maps provide stark illustration of community issues and can be used as the focus of community decision making and organizing and as important evidence during advocacy campaigns.
There is a strong national trend toward using community-level health indicators and indicator data to monitor change over time, increase accountability among policy makers, and engage communities in a dialog about local priorities. This movement is being supported by national institutions and resources, such as the Community Health Status Indicators Project, and implemented at regional and local levels. Well-selected community health indicators provide comparative data over time and are a step toward ensuring that actions are aligned with health interests, that the social determinants of health are monitored and acted upon, and that there is accountability for improving community conditions. The process of selecting indicators and collecting data—in essence selecting what will be measured—is in itself valuable as a venue for developing community capacity, building partnerships, and engaging community members, along with representatives from the public and private sectors, in identifying, prioritizing, and setting benchmarks related to health and well-being. Prevention Institute conducted a review of more than 90 indicator reports and report cards for the study Good Health Counts: A 21st Century Approach to Community Health.139 This review revealed that success was achieved through both a carefully developed set of indicators that reflect the determinants of health within the community and a well-orchestrated, transparent process.
Movement toward the use of electronic medical records and shared data among hospitals also holds promise for examining differences in access and equity in hospitals and clinics. As hospitals and clinics move toward electronic systems, the capacity to analyze differences by race and ethnicity increases as does the potential to address issues of high rates of missing race/ethnicity data—a key parameter for establishing the presence of disparities. Taking appropriate steps to protect privacy, we can link this data to GIS mapping to yield powerful information about the impact of community environment on health.
4. What’s good for our natural environment is good for our health
The mounting concern over environmental degradation and the increased focus on prioritizing solutions, have introduced an opportunity to align issues of health and health equity with those of the environment and improve both simultaneously. For instance, greenhouse gas emissions are bad for the environment generally, accelerate climate change, and also have direct repercussion on health (e.g., asthma rates). In our efforts to solve these challenges, we can build powerful partnerships and address health issues that might otherwise be diminished. Strategically improving the physical environment could reduce the number of people getting sick and injured in the first place as well as the severity of those diseases. In effect this could reduce the demand for medical services and the burden on the health care system. It could potentially increase the accessibility and affordability of quality health care and reduce the ecological footprint of our health care institutions.
Shifting towards a more sustainable food system and altering our transportation systems to support public transportation, walking, and biking, are among the initiatives that hold multiple environmental and health benefits by virtue of reducing greenhouse gases and our dependence on fossil fuels while improving air quality and increasing physical activity. There is potential to engage in strategies that simultaneously improve environmental conditions and support the health of vulnerable populations. Policies and practices are needed to improve the environmental and health conditions of communities—including ensuring clean air and water; preserving agricultural lands; reducing exposure to toxins; and providing economic opportunity, quality housing, and safe streets. However, such work must be done cautiously. For instance, rises in gas prices without simultaneous expansion of public transportation may have a positive impact in terms of greenhouse gases but can have disastrous effects on low-income people who live in communities that have been designed around automobile travel and where access to employment and resources such as healthy food are contingent on driving. As another example, popular “cap and trade” policies need to be implemented with safeguards against high polluters moving into communities with limited political capital to oppose such moves.
5. Internal organizational diversity helps to move along an equity-focused health agenda
Achieving greater diversity within the health professions has been identified as a key strategy for ensuring a culturally competent workforce. Greater diversity across all levels of an organization can seed new and creative strategies for tackling health inequities. A number of health organizations are currently at the forefront of efforts to address health equity, and all these organizations—including health departments, health care organizations, and community-based organizations—have the opportunity to increase the diversity of their staffs. Diversity goes beyond racial and ethnic diversity to include factors such as age, gender, socioeconomic status, sexual preference, and professional skills. Ways to build and sustain diverse leadership include proactive efforts to recruit, hire, train, and retain staff that will contribute to diversity.140 Many organizations explicitly looking to address health equity have found that workforce development strategies can build the capacities of current staff and attract skilled and committed individuals to partake in the mission to achieve health equity. Organizations, as a result, seed new and creative ideas for tackling health inequities.
Endnotes
1. Life and Death From Unnatural Causes: Health & Social Inequity in Alameda County. Alameda County Public Health Department September 2008.
2. Geronimus AT. Understanding and eliminating racial inequalities in women’s health in the United States: the role of the weathering conceptual framework. J Am Med Womens Assoc. 2001; 56: 133-6, 149-50.
3. U.S. Department of Health and Human Services. (1999). Mental Health: A report of the Surgeon General. Rockville, MD, Supplement: Mental Health: Culture, Race, And Ethnicity
4. Decades of Work to Reduce Disparities in Health Care Produce Limited Success. Rebecca Voelker. JAMA. 2008;299(12):1411-1413
5. House J.S., & Williams D.R. (2000). Understanding and reducing socioeconomic and racial/ethnic disparities in health. In B. Smedley, & S. Syme (Eds.), Promoting health: intervention strategies from social and behavioral research. Washington, D.C.: National Academy Press.
6. The World health report 2000: health systems: improving performance. Geneva, Switzerland: World Health Organization.
7. OECD Health Data 2007.
8. Schoen C, Osborn R, How S, Doty M, Peugh J. In Chronic Condition: Experiences of Patients with Complex Health Care Needs, In Eight Countries, 2008. Health Affairs. Web Exclusive. November 2008.
9. Nursing Shortage Fact Sheet, American Association of Colleges of Nursing, Updated April 2009. Retrieved at www.aacn.nche.edu/Media/FactSheets/NursingShortage.htm. Accessed April 15, 2009.
10. Kenneth E. Thorpe, David H. Howard and Katya Galactionova. Differences In Disease Prevalence As A Source Of The U.S.-European Health Care Spending Gap. Health Affairs, 26, no. 6 (2007): w678-w686
11. Thorpe K, Factors accounting for the rise in health care spending in the United States: the role of rising disease prevalence and treatment intensity. Public Health. 2006 Nov;120(11): 1002-7. Epub 2006 Oct 9
12. Kenneth Thorpe et al, The Rising Prevalence of Treated Disease: Effects on private Health Insurance Spending. Health Affairs. Volume 24, Supplement 1. 23 June 2005
13. Prevention for a Healthier America: Investments in Disease Prevention Yield Significant Savings, Stronger Communities. Trust for America’s Health, Prevention Institute, Urban Institute. 2008.
14. Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2002; 21(2): 60-76.
15. Poverty and Race Research Action Council analysis of U.S. Census Bureau data, with the assistance of Nancy A. Denton and Bridget J. Anderson, 2005.
16. Smedley B, Jeffries M, Adelman L, Cheng J. Race, Racial Inequity and Health Inequities: Separating Myth from Fact. 2008. Available at: www.unnaturalcauses.org/assets/uploads/file/Race_Racial_lnequality_Health.pdf
17. Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine. 2002; 22:23-9.
18. National Highway Traffic Safety Administration. (2004, June). Sixth report to Congress, fourth report to the president: The national initiative for increasing safety belt use. Washington, DC: Author.
19. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004; 291:1238-1245.
20. Davis R, Cook D, Cohen L. A community resilience approach to reducing ethnic and racial disparities in health. Am J Public Health. 2005;95:2168-73
21. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
22. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished,
23. Siegel Β, Bretsch J, Sears Y, Regenstein M, Wilson M. Assumed Equity: Early Observations from the First Hospital Disparities Collaborative. Journal for Healthcare Qualify 2007; Vol. 29, No. 5, pp 11-15.
24. U.S. Census Bureau. State & County QuickFacts. Richmond, California, Available at: http://quickfacts.census.gov/qfd/states/06/0660020.html Accessed on April 3, 2009.
25. Active Living Research. Robert Wood Johnson Foundation. Investigating policies and environments to support active communities. Active Living Research. Available at: www.activelivingresearch.org/files/briefing0305.pdf. Published March 2005. Accessed 15 April 2009.
26. Larson N, Story M, Nelson M. Neighborhood Environments Disparities in Access to Healthy Foods in the U.S. American Journal of Preventive Medicine 2009; 36(1): 74-81.
27. Sloane DC, Diamant AL, Lewis LB, et al. (2003). Improving the nutritional resource environment for healthy living through community-based participatory research. Journal of General Internal Medicine, 18, 568-575.
28. Pennsylvania Fresh Food Financing Initiative. Providing Healthy Food Choices to Pennsylvania’s Communities. www.thefoodtrust.org/pdf/2009FFFI.pdf Accessed on May 1, 2009.
29. M. Reeves, A. Katten, and M. Guzman, Pesticide Action Network and Californians for Pesticide Reform, “Fields of poison 2002: California farm workers and pesticides,” 2002, Available at: www.panna.org/resources/gpc/gpc_200304.13.1.07.dv.html Accessed September 11, 2007.
30. Weiss, Billie. An Assessment of Youth Violence Prevention Activities in USA Cities. Urban Networks to Increase Thriving Youth (UNITY) through Violence Prevention. Southern California Injury Prevention Research Center UCLA School of Public Health. June 2008.
31. CeaseFire is an evidence-based public health approach to reducing violence, www.ceasefirechicago.org/ Accessed April 15, 2009.
32. Family Violence Prevention Fund. The Facts on Health Care and Domestic Violence. http://endabuse.org/userfiles/file/Children_and_Families/HealthCare.pdf accessed on 4/11/09
33. Family Violence Prevention Fund. The Facts on Immigrant Women and Domestic Violence. http://end-abuse.org/userfiles/file/Children_and_Families/lmmigrant.pdf Accessed 4/11/09
34. City of Minneapolis, BLUEPRINT FOR ACTION: Quarterly Report. October-December 2008 February 2009. Available at: www.ci.minneapolis.mn.us/dhfs/YVP-Quarterly-Report-Fourth-Quarter-2008.pdf. Accessed May 1, 2009.
35. City of Minneapolis, BLUEPRINT FOR ACTION: Quarterly Report. October-December 2008 February 2009. Available at: www.ci.minneapolis.mn.us/dhfs/YVP-Quarterly-Report-Fourth-Quarter-2008.pdf. Accessed May 1, 2009.
36. Stern MJ, Seifert SC. Working Paper #13- Cultural participation and communities: The role of individual and neighborhood effects. Social Impact of the Arts Project, University of Pennsylvania: 2000.
37. Brice Heath, S., Soep, Ε. & Roach, A. (1998). Living the Arts Through Language and Learning: A Report on Community-based Youth Organizations. In Americans for the Arts MONOGRAPHS, V2(7).
38. Catterall, J.S. Involvement in the Arts and Success in Secondary School. In Americans for the Arts MONOGRAPHS, V1 (10).
39. Smedley B, Stith A, Nelson A eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academies Press; 2003: 5
40. Smedley B, Stith A, Nelson A eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academies Press; 2003: 5.
41. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455.
42. Smedley B, Alvarez B., Panares R, Fish-Parcham C, Adland S. Identifying and Evaluating Equity Provisions in State Health Care Reform. April 2008. Available at: www.commonwealthfund.org.
43. California Pan-Ethnic Health Network. A Blueprint for Success: Bringing Language Access to Millions of Californians. Available at: www.c.pehn.org/pdfs/Sb853briefScreen.pdf. Accessed on April 3, 2009.
44. Trivedi A, Gibbs B, Nsiah-Jefferson L, Ayanian JZ, Prothrom-Stith D. Creating A State Minority Health Policy Report Card. Health Affairs March/April 2005. Vol 24, no. 2; pp388-396.
45. Siegel B, Bretsch J, Sears V, Regenstein M, Wilson M. Assumed Equity: Early Observations from the First Hospital Disparities Collaborative. Journal for Healthcare Quality 2007; Vol. 29, No. 5, pp 11 -15.
46. Findings from UCSF IDEALL Study: How Can Public Health Systems Best Support People with Diabetes? 2009.
47. Effects of Self-Management Support on Structure, Process and Outcomes Among Vulnerable Patients with Diabetes: A3-Arm Practical Clinical Trial. Diabetes Care. 2009; 32(4):559-566.
48. Handley, M-, Shumway, Μ., & Schillinger D. Cost-Effectiveness of Automates Telephone Self-Management Support with Nurse Care Management Among Patients with Diabetes. Annals of Family Medicine. 2008; 6(5): 1-7.
49. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455.
50. Brennan Ramirez LK, Baker EA, Metzier M. Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health. Atlanta: US Department of Health and Human Services, Center for Disease Control and Prevention. 2008.
51. Russell S, Senior care innovator retiring: On Lok’s alternative to nursing homes got its start in Chinatown, September 21, 2004. San Francisco Chronicle., B-1. Accessed on April 23, 2009 at www.sfgate.com/cgi-bin/article.cgi?file=/chronicle/archive/2004/09/21/BAGI48SA051.DTL. Accessed May 1, 2009.
52. Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K, Closing the Divide: How Medical Homes Promote Equity in Health Care: Results From The Commonwealth Fund 2006 Health Care Quality Survey, The Commonwealth Fund, June 2007.
53. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455.
54. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455.
55. Smedley B, Stith A, Nelson A eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academies Press; 2003: 5.
56. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455
57. Smedley Bo. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455
58. State of California, Department of Finance, 2000-2005. Sacramento, CA July 2007
59. Journal of the American academy of nurse practitioners, volume 21, issue 2, pages 116-122. published online: 2/12/09
60. Minneapolis Department of Health and Family Support, Program Description: Seen on da Streets.
61. Boston Public Health Commission, Mayor’s Task Force Blueprint A plan to eliminate racial and ethnic disparities in health. June 2005. Available at: www.bphc.org/programs/healthequitysocialjustice/toolsandreports/Forms%20%20Documents/Center%20Reports%20and%20Tools/BPHCOHEBlueprint.pdf on April 15, 2009. Accessed on April 3, 2009.
62. Boston Public Health Commission. Boston works to end racial and ethnic disparities in health Year One Report. Available at: www.bphc.org/programs/healthequitysocialjustice/toolsandreports/Forms%20%20Documents/Center%20Reports%20and%20Tools/BΡHCOHEdisp_year1report.pdf pg. 38 Accessed on April 15, 2009.
63. Prevention Institute, Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
64. Smedley B., Alvarez B., Pañares R., Fish-Parcham C., Adland S., April 2008. Identifying and Evaluating Equity Provisions in State Health Care Reform. The Commonwealth Fund, pub. no. 1124.
65. Davis R, Cook C, Cohen L. A Community Resilience Approach to Reducing Ethnic and Racial Disparities in Health, The American Journal of Public Health. December 2005 (Vol. 95, No. 12).
66. World Health Organization Commission on Social Determinants of Health, 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health.
67. Freudenber N, Rugis J. Reframing School Dropout as a Public Health Issue. Preventing Chronic Disease. Center for Disease Control and Prevention. 2007;4(4): 1-11. Available at: www.cdc.gov/pcd/issues/2007/oct/07_0063.htm. Accessed March 2008.
68. Ross CE, and Mirowsky J. Refining the Association between Education and Health: The Effects of Quantity, Credential, and Selectivity. Demography. 1999;36(4): 445-460.
69. Lleras-Muney A. The Relationship Between Education and Adult Mortality in the United States. Review of Economics Studies. 2005;72:189-221.
70. The Consultative Group on Early Childhood Care and Development. What is ECCD? Available at: www.ecdgroup.com/what_is_ECCD.asp. Accessed March 11, 2002.
71. Olds D, Henderson CR Jr, Cole R, et al. Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized trial. JAMA. 1998; 280;1238-1244.
72. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455
73. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
74. Institute of Medicine (2003). Smedley B, Stith A, Nelson A eds., Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academies Press; 2003.
75. Centers for Disease Control and Prevention. Health United States, 2007. Table 55. 2007. Available at: www.cdc.gov/nchs/data/hus/hus07.pdf
76. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Webbased Injury Statistics Query and Reporting System (WISQARS). Feb 2006. Available at: www.cdc.gov/ncipc/wisqars.
77. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Youth Violence. Available at: www.cdc.gov/ncipc/dvp/YV_DataSheet.pdf
78. United States Department of Transportation. National Highway Traffic Safety Administration. Race and Ethnicity in Fatal Motor Vehicle Traffic Crashes 1999 - 2004. May 2006. Available at: www.watchtheroad.org/809956.pdf. Accessed on April 3, 2009.
79. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Webbased Injury Statistics Query and Reporting System (WISQARS). Available at: www.cdc.gov/ncipc/wisqars. Accessed on April 3, 2009.
80. National Center for Health Statistics. Health, United States, 2007 with Chartbook on Trends in the Health of Americans. Hyattsville, MD: U.S. Department of Health and Human Services; 2007.
81. National Minority Health Month Foundation. Study of Vital Statistics by ZIP Code Shows Health Disparities Affecting Minorities in the Treatment of Kidney and Cardiovascular Diseases. March 2007. Available at: www.rwjf.org/publichealth/product.jsp?id= 18669-Accessed on April 3, 2009.
82. National Minority Health Month Foundation. Study of Vital Statistics by ZIP Code Shows Health Disparities Affecting Minorities in the Treatment of Kidney and Cardiovascular Diseases. March 2007. Available at: www.rwjf.org/publichealth/product.jsp?id=18669. Accessed on April 3, 2009.
83. National Health Interview Survey 2001-2005, available at www.cdc.gov/nchs/nhis.htm
84. National Institutes of Health. (2002). NIH’s strategic research plan and budget to reduce and ultimately eliminate health disparities (Vol. I). Available at: http://ncmhd.nih.gov/our_programs/strategic/pubs/Volumel_031003EDrev.pdf. Accessed on June 26, 2008.
85. Whitehead, M. The Concepts and Principles of Equity and Health. Copenhagen: WHO Regional Office for Europe. 1990. Available at: http://whqlibdoc.who.int/euro/-1993/EUR_ICP_RPD_414.pdf. Accessed on May 1, 2009.
86. Center for Medicare and Medicaid Services. Office of the Actuary, National Health Statistics Group.
87. Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group. 2006 National Health Care Expenditures Data. January 2008. Available at: www.cms.hhs.gov/nationalhealthexpenddata/01 _overview.asp
88. Lee Ρ and Paxman D, Reinventing Public Health. Annual Review of Public Health, 1997; Vol. 18: 1-35.
89. Prevention for a Healthier America: Investments in Disease Prevention Yield Significant Savings, Stronger Communities. Trust for America’s Health, Prevention Institute, Urban Institute. 2008.
90. United States Breastfeeding Committee. Workplace breastfeeding support. Raleigh, NC: United States Breastfeeding Committee; 2002.
91. Brown MJ. Costs and benefits of enforcing housing policies to prevent childhood lead poisoning. Medical Decision Making. 2002;22:482-492.
92. Peters RM. The Negative Effect of the Clinical Model of “Health”: Implications for Health Care Policy. Journal of Health Care Finance. 1998; 25:78-92.
93. Pincus T, Esther R, DeWalt DA, Callahan LF. Social Conditions and Self Management are more Powerful Determinants of Health than Access to Care. Annals of Internal Medicine. 1998; 129:406-411.
94. Institute of Medicine (2000). A social environmental approach to health and health interventions. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies from Sacial and Behavioral Research. Washington, DC: National Academy of Sciences.
95. Smedley B, Stith A, Nelson A eds., UnequaI Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C.: The National Academies Press; 2003: 5
96. The Commonwealth Fund. Medicaid Managed Care and Cultural Diversity in California. February 1999. Avaliable at: www.cmwf.org/programs/minority/coye_culturaldiversity_311,asp#repfoot16. Accessed October 29, 2003.
97. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004; 291:1238-1245.
98. Davis R, Cook D, Cohen L. A community resilience approach to reducing ethnic and racial disparities in health. American Journal of Public Health. 2005;95:2168-73.
99. Policytink Health Disparities Team. Reducing Health Disparities Through a Focus on Communities, PolicyLink. November 2002.
100. Geronimus AT. Understanding and eliminating racial inequalities in women’s health in the United States: the role of the weathering conceptual framework. J Am Med Womens Assoc. 2001; 56:133-6, 149-50.
101. Mays VM, Cochran SD, Barnes NW. Race, Race-Based Discrimination, and Health Outcomes Among African Americans. Annu Rev Psychol. 2007; 58: 201-225.
102. Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2002; 21(2): 60-76.
103. Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality.JAMA. 1998; 279(21):1703-1708.
104. Smedley B, Jeffries Μ, Adelman L, Cheng J, Race, Racial Inequity and Health Inequities: Separating Myth from Fact. 2008. Available at: www.unnaturalcauses.org/assets/uploads/file/Race_Racial_lnequality_Health.pdf. Accessed on April 3, 2009.
105. Wandersman A, Nation M. Urban neighborhoods and mental health: psychological contributions to understanding toxicity, resilience, and interventions. American Psychologist. 1998;43:647-656.
106. Buka S. Results from the project on human development in Chicago neighborhoods. Presented at: 13th Annual California Conference on Childhood Injury Control; October 25-27, 1999; San Diego, CA.
107. Wilkenson R. Income inequality, social cohesion, and health: clarifying the theory - a reply to Muntaner and Lynch. International Journal of Health Services. 1999;29:525-545
108. Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. The American Association for the Advancement of Science. 1997;277(5328:15)918-924.
109. Pothukuchi K. Attracting Supermarkets to Inner-City Neighborhoods: Economic Development Outside the Box. Economic Development Quarterly. 2005; 19: 232-244.
110. Jackson RJ. Creating a Healthy Environment: The Impact of the Built Environment on Public Health. [Center for Disease Control and Prevention Website. Available at www.sprawlwatch.org. Accessed June 2000.
111. Centers for Disease Control and Prevention Public Health Practice Program Office. Principles of Community Engagement. Atlanta, GÁ, 1997.
112. Hancock, Trevor. “Healthy Communities must also be Sustainability Communities.” Public Health Reports. Volume 115, March/April & May/June 2000.
113. Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. AJPH. 2002;92(11): 1761-1 768.
114. Schmid TL, Pratt M, Howze E. Policy as intervention: environmental and policy approaches to the prevention of cardiovascular disease. AJPH. 1995;85(9): 1207-1211.
115. Coker A. Opportunities for Prevention: Addressing IPV in the Health Care Setting. Family Violence Prevention and Health Practice. 2005:1.
116. Sampselle M. The Role of Nursing in Preventing Violence against Women. Journal Obstet Gynecol Neonatal Nurs. 1991. 20: 281-7.
117. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journal of Preventive Medicine. 1991. 7(6): 262-373.
118. Coker A. Opportunities for Prevention: Addressing IPV in the Health Care Setting. Family Violence Prevention and Health Practice. 2005:1.
119. King MC. Changing Women’s Lives: The Primary Prevention of Violence Against Women. AWHONN’s Clinical Issues. 1993; 4 no 3.
120. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journal of Preventive Medicine. 1991. 7(6): 262-373.
121. Sampselle Μ. The Role of Nursing in Preventing Violence against Women. Journal Obstet Gyrtecol Neonatal Nurs. 1991. 20: 281-7.
122. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journal of Preventive Medicine. 1991. 7(6): 262-373.
123. King MC. Changing Women’s Lives: The Primary Prevention of Violence Against Women. AWHONN’s Clinical Issues. 1993; 4 no 3.
124. Sampselle M. The Role of Nursing in Preventing Violence against Women. Journal Obstet Gynecol Neonata/Nurs. 1991. 20: 281-7.
125. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journai of Preventive Medicine. 1991. 7(6): 262-373.
126. Sampselle M. The Role of Nursing in Preventing Violence against Women. Journal Obstet Gynecol Neonata/Nurs. 1991. 20: 281-7.
127. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journal of Preventive Medicine. 1991. 7(6): 262-373.
128. Schwartz IL. Sexual Violence against Women: Prevalence, Consequences, Societal Factors, and Prevention. American Journal of Preventive Medicine. 1991. 7(6): 262-373.
129. Sampselle M. The Role of Nursing in Preventing Violence against Women. Journal Obstet Gynecol Neonatal Nurs. 1991. 20: 281-7.
130. King MC. Changing Women’s Lives: The Primary Prevention of Violence Against Women. AWHONN’s Clinical Issues. 1993; 4 no 3.
131. King MC. Changing Women’s Lives: The Primary Prevention of Violence Against Women. AWHONN’s Clinical Issues. 1993; 4 no 3.
132. Prevention Institute. Reducing Healthcare Costs through Prevention. August 20071
132. Prevention for a Healthier America: Investments in Disease Prevention Yield Significant Savings, Stronger Communities. Trust for America’s Health, Prevention Institute, Urban Institute. 2008.
134. Smedley B. Moving Beyond Access: Achieving Equity In State Health Care Reform. Health Affairs, March/April 2008. Vol 27, No. 2, pp 447-455
135. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
136. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
137. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008. Unpublished.
138. Policy-Link. Available at: www.policylink.org/EDTK/Mapping/. Accessed on April 3, 2009
139. Prevention Institute. Good Health Counts: A 21st Century Approach to Health and Community in California. November 2007
140. Prevention Institute. Health Equity Toolkit Key Informants Interview Synthesis document. 2008, Unpublished.