Patient-Centered Cancer Treatment Planning: Improving the Quality of Oncology Care
A National Coalition for Cancer Survivorship and Institute of Medicine Workshop
Each year about 1.5 million people are diagnosed with cancer in the United States (ACS, 2010), and must then decide on a course of care. Cancer treatment often involves multiple options and specialties; it can be toxic, costly, intense, and protracted and may involve serious long-term complications. In addition, responses to cancer treatments are quite variable, so predicting the potential risks and benefits of various treatment options for individual patients is often difficult. Because of the complexity of treatment choices, coupled with the life-threatening nature of cancer and its emotional repercussions, it is often difficult for people with cancer to make decisions about their care. The fragmented nature of the cancer care system (IOM, 1999) also presents challenges that may impede coordinated care and the development of comprehensive treatment plans.
Recognizing these challenges, the National Coalition for Cancer Survivorship (NCCS)and the National Cancer Policy Forum (NCPF) of the Institute of Medicine hosted a public workshop in Washington, DC, on February 28 and March 1, 2011, titled Patient-Centered Cancer Treatment Planning: Improving the Quality of Oncology Care. The workshop agenda, which includes speakers and their affiliations, can be found in the appendix. This document is a summary of the workshop. The views expressed in this summary are those of the speakers and discussants, as attributed to them,
and are not the consensus views of the workshop participants or members of the National Cancer Policy Forum.
The workshop included an overview of patient-centered care and cancer treatment planning, as well as sessions on shared decision making, communication in the cancer care setting, and patient experiences with cancer treatment. Best practices, models of treatment planning, and tools to facilitate their use were also discussed, as well as policy changes that may promote patient-centeredness by enhancing patients’ understanding of and commitment to the goals of treatment through a shared decision-making process with their healthcare team from the moment of diagnosis onward. While previous Institute of Medicine (IOM) work has focused on the challenges of cancer care planning for individuals who have completed their treatment (sometimes referred to as follow-up or survivorship care planning), this workshop focused on treatment planning for patients with cancer at the time of diagnosis.
Patient-centered care has been defined as “providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions” (IOM, 2001). A primary goal of patient-centered treatment planning is to engage patients and their families in meaningful and thorough interactions with their healthcare providers to develop an accurate, well-conceived treatment plan, using all available medical information appropriately while also considering the medical, social, and cultural needs and desires of the patient and family. A treatment plan may entail a prognostic and therapeutic plan at the time of initial diagnosis, which can be updated with changes during the course of treatment, as well as a prognostic and palliative care plan near the end of life.
Participants at the workshop identified numerous obstacles to achieving patient-centered care planning in practice, including variable and often suboptimal communication between the patient and healthcare provider that may not be culturally or personally appropriate, and information overload for the patient and family, without appropriate written documentation of treatment plans, options, and expectations that the patient and family might refer to after a visit. Many participants also lamented the frequent lack of involvement of primary care physicians and provider teams who might know patient and family better. Numerous factors that might contribute to that lack of involvement were noted, including poor coordination of care or inappropriate exclusion by the oncology team, the inability of primary care physicians to devote the time needed to keep up with myriad complex and rapidly changing cancer treatment regimens, and the lack of
availability of primary care physicians due to workforce shortages. Other obstacles to care planning identified by workshop participants included the increasingly complex medical data that healthcare providers need to consider when making treatment decisions, and a lack of decision support for healthcare providers (for example, in electronic health records) to aid in managing the complexity of medical information. In addition, the current reimbursement system for health care does not compensate providers for the time it takes to develop, discuss, and document a treatment plan.
Workshop participants also suggested a variety of mitigation strategies to address these many obstacles, including improved training of physicians, nurses, and other healthcare providers in the components of optimal communication with patients and families, and improved education of patients and families about how to be more proactive and assertive to optimize interactions with healthcare providers. Many participants advocated for greater use of support services, such as mental health services, social work, and nutrition counseling, as well as greater involvement of patient navigators who can help coordinate cancer care and foster communication among providers. However, others argued that the need for patient navigators is a symptom of a broken system, and strongly advocated for more structural, systemic reforms in cancer care. For example, many participants emphasized a need to change the reimbursement and financial incentives in the system to encourage and support more patient-centered care. They also stressed that greater use of quality improvement programs and accountable care systems could have a positive impact on the care provided to patients with cancer. A variety of tools and online resources were also cited as potential means to improve care planning, such as electronic health records that can organize all important medical information, share it with all members of the healthcare team, utilize decision support to better ensure optimal treatment recommendations for patients, and facilitate electronic input from patients into their healthcare records.
WHY PATIENT-CENTERED PLANNING FOR CANCER?
Cancer takes patients on a journey most have never taken before, whose outcomes are unknown. This creates uncertainty and anxiety, especially given the potential life-threatening nature of the disease, as several patients and providers noted at the workshop. Mr. Richard Boyajian, a cancer survivor and clinical director and primary nurse practitioner of the Adult Survivorship Program at Dana-Farber Cancer Institute, said that fear of the
unknown was a major issue for him when he was a leukemia patient and that a cancer treatment plan helped alleviate that fear. “The idea of having some sense of the roadmap, of where this journey is going to take you, is really important,” added Mr. Mark Gorman, a cancer survivor and director of Survivorship Policy at NCCS. “It’s critical to manage uncertainty.”
A cancer treatment plan can provide that roadmap, even in the final stages of cancer when treatment might only be palliative (to address symptoms), stressed Dr. Patricia Ganz, professor of health services and medicine at the University of California, Los Angeles, and director of the Division of Cancer Prevention and Control Research at the Jonsson Comprehensive Cancer Center. “Patients want to know what’s going to happen to them. That’s why we have to do this,” she said. Ms. Alison Smith, vice president for strategic initiatives at C-Change, added that “pilots don’t take off without a flight pattern, and architects don’t break ground without a blueprint. Patients diagnosed with cancer are taking the journey of their life, literally, so the role of the cancer treatment plan in starting a conversation, in promoting comprehension and retention, in managing expectations and anxiety, and providing continuity across settings and episodes is so important.”
Cancer care also has a number of unique attributes that make treatment planning vital. Dr. Ganz noted that cancer treatments can be complex, toxic, intense, expensive, disruptive, life-threatening, and protracted, with the possibility of cancer recurrence or late complications, and thus requiring lifelong surveillance. In addition, patients often have to choose between several treatment options, each with its own set of potential risks and benefits. Cancer care also usually involves multiple practitioners and can occur in isolation from primary healthcare delivery, with physicians whom patients usually have not known for long.
Given the complexity of cancer care, a written cancer treatment plan is critical, noted Dr. Karen Sepucha, director of the Health Decision Sciences Center at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School. “It is unfathomable the lack of documentation and what’s supposed to be kept in your head versus the limits of cognition. There is an approach in human factors engineering in which you design your system so that humans can work in it and not fail. We haven’t really translated that well into health care, so we’re setting ourselves up for failure all the time, for missing the handoffs,” she said. Dr. Lawrence Shulman, chief medical officer, senior vice president for medical affairs, and chief of the Division of General Oncology at Dana-Farber Cancer Institute, added that cancer treatment plans are likely to become
increasingly important as the growing complexity of cancer care becomes a challenge for providers.
Cancer treatment planning is especially important because a patient’s survival can hinge on making the correct treatment decision. “When you are making these important decisions, if [a doctor makes] the wrong decision, the next day the doctor gets to try again with a new patient,” said Ms. Anne Willis, cancer survivor and director of Survivorship Programs for NCCS. “The patient doesn’t have that option. [Patients]only have one chance to get it right.”
The 2001 IOM consensus report Crossing the Quality Chasm: A New Health System for the 21st Century defines patient-centered care as “providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions” (IOM, 2001). Most speakers at the workshop indicated that when patient-centered care is given, there is a partnership between a patient and his or her providers. To enable this partnership, communication must be sensitive to the needs and capabilities of the patient so that the patient is informed about his or her treatment options and encouraged to share in the decision making about care.
Patient-centered care may also involve patient navigators, social workers, or other personnel to help patients coordinate their care and relieve their health-related burdens, including psychosocial issues such as anxiety or financial stress. As one patient who spoke at the workshop summarized it, patient-centered care is having the health system organized around the patient rather than the patient having to organize his or her life around the system.
The key components of patient-centered care stressed at the workshop were the following:
- Patient education and empowerment
- Patient-centered communication, involving the patient, family, and friends, that explains treatment options and includes patients in treatment decisions to reflect patients’ values, preferences, and needs
- Coordination and integration of care
- Provision of emotional support as needed, such as relieving fear and anxiety and addressing mental health issues
Oncologists and other cancer healthcare providers typically provide some information to their patients about their diagnosis, stage, and treatment options. Yet, as several speakers at the workshop noted, patients also want to know the likely outcomes and side effects of each potential treatment, including long-term outcomes and risks of cancer recurrence, if known. They also want to know the signs of recurrence so that they don’t worry unnecessarily. Many cancer treatments may also reduce fertility; thus, ways to preserve fertility should also be discussed with patients in advance of treatment when appropriate, several speakers said.
Research on breast and colon cancer patients and survivors by Dr. Deborah Mayer, associate professor at the University of North Carolina School of Nursing, suggested that patients want both print- and Web-based information, and they want information about their diagnosis at the time they are diagnosed and a treatment plan when they first start their treatment. Examples of Web-based tools that can help patients learn more about their diagnosis and treatments options are described in the section on Tools and Resources (p. 29). Cancer patients also would like information on local resources, including support groups, dieticians, physical and mental health therapists, and exercise and health promotion programs.
There is variability in the amount of information that patients want to receive about their cancer, several speakers noted. Because of the stress of being diagnosed with cancer, patients may have difficulty processing excessive amounts of information, especially complex technical information. Mr. Boyajian suggested providing patients with just the “Cliff Notes”—a concise summary of the most important pieces of information about diagnosis and treatment—and then referring them to other sources if they want additional information. However, Dr. Ganz stressed the importance of discussing all care options and having both verbal and written communication of those options and of the treatment plan. Several participants suggested recording the consultation a patient has with his or her oncologist in which this information is discussed, so that it can be reviewed later by the patient and family members. Some patients also find it helpful to have a companion present who can take notes during this discussion and help with post-visit translation of care plans and rationale for treatment.
It is also helpful if providers put the potential risks and benefits of various treatment options in a context that patients can understand, pointed out Dr. Sherrie Kaplan, Assistant Vice Chancellor for Healthcare Measure-
ment and Evaluation and professor of medicine at the University of California, Irvine. For example, the risk of a rare complication can be given as equivalent to the likelihood of other rare events occurring, such as being struck by lightning, hit by a car, or winning the state lottery.
Both patients and providers at the workshop noted that people with cancer are expected to take an active role in their care and share in decision making, but few people have experience and training in what Dr. Kaplan termed “planned patienthood.” Although we are much more likely to be patients at some point during our lifetimes than to be in a fire, she pointed out, we are trained for the latter and not the former. Consequently, the average patient asks five or fewer questions during a 15-minute doctor’s office visit, with a high proportion asking no questions (reviewed by IOM,2008), suggesting that patients generally are not taking an active role in their care. According to the IOM consensus report Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs (2008), poor communication and lack of patient involvement are particularly worrisome because a substantial literature has linked effective patient-clinician communication to positive health outcomes. Thus, Dr. Kaplan stressed that “we need to prepare people on how to be patients.”
Patient advocate Mr. Robert Erwin, president of the Marti Nelson Cancer Foundation, concurred that patients often need to be encouraged to take a more active role in their care. He suggested patients learn to see themselves more as clients, which has more active connotations than the term patients. Along those lines, Dr. Ganz added that patients should be aware that they can always “fire” their doctors if they are not doing a good job of taking care of them. Dr. Elizabeth Clark, executive director of the National Association of Social Workers, added that patients’ self-advocacy gives them a better sense of being in control over their own lives, which is important after being given a life-threatening diagnosis, such as cancer. “Self-advocacy can improve quality of life, and it may be the difference that turns feeling hopeless and helpless into feeling hopeful,” she said.
Dr. Kaplan noted that effective patient skills include asking focused questions, understanding that options exist, and eliciting all options and their potential risks and benefits. Dr. Kaplan stressed that patients should also be assertive about stating personal preferences and relevant life circumstances that affect treatment options and should negotiate conflicts with the
preferences of their physicians when these arise. Empowered patients can actively participate in shared decision making, an important component of patient-centered care. She defined shared decision making as “the process of negotiation by which physicians and patients arrive at a specific course of action, based on a common understanding of the goals of treatment, the risks and benefits of the chosen treatment versus reasonable alternatives, and each other’s values and preferences” (adapted from Sheridan et al., 2004).
Dr. Jessie Gruman, cancer survivor and president of the Center for Advancing Health, pointed out that the National Cancer Institute (NCI) has a monograph that specifies six functions of patient-centered communication (Epstein and Street, 2007):
- Fostering healing relationships
- Exchanging information
- Responding to emotions
- Managing uncertainty
- Making decisions
- Enabling patient self-empowerment
Other participants added that patient-centered communication should be sensitive to patients’
- vulnerability;
- degree of education and ability to understand medical terms, concepts, risks, and benefits;
- possible reluctance to assert preferences and ask questions;
- preferences related to treatment; and
- cultural and spiritual outlook.
Several speakers stressed that provider communication should be simple, concise, and free of acronyms and jargon, which one participant called “oncobabble.” Such communication should be specific to avoid medication errors or inattention to symptoms. For example, Dr. Linda Burhansstipanov, grants director and founder of the Native American Cancer Research Corporation and president of Native American Cancer Initiatives, Inc., pointed out that many patients are told to contact their
doctors when they experience excessive bleeding, but they do not know how much is considered excessive. Dr. Carolyn Clancy, director of the Agency for Healthcare Research and Quality (AHRQ), added that patients may overdose on their medications if their doctor tells them to take two a day, without specifying if it is two pills or 2 milligrams they should be taking daily. “You need to translate across different levels of education and literacy, cultural context, age, gender, and many other individual differences,” said Dr. Jeffrey Peppercorn, associate professor of medicine at Duke University and faculty associate of the Trent Center for Bioethics.
To ensure that patients understand the information given to them, several participants suggested that they be asked to repeat what they heard, rather than just be asked if they understand. Dr. Clancy recalled an evaluation of a diabetes education program led by nurses at an academic medical center primary care clinic that found that although patients would nod politely to indicate they understood the information, questions asked of them a few days later revealed there was little retention of such information. Dr. Burhansstipanov also suggested repeating the key points of the treatment plan to improve patient retention of the information. Those key points could be repeated in different ways, or given in different formats, she suggested.
It is important for providers to solicit patient preferences and not make assumptions about which treatment option and associated side effects patients are more likely to prefer or feel is best for them. Dr. Sepucha pointed out that many providers assume that women with early-stage breast cancer, for whom mastectomy or lumpectomy followed by radiation is equally effective, would prefer not to lose their breast. Yet in a study of breast cancer patients who were provided with comprehensive information about the risks and benefits of mastectomy and lumpectomy, one-third of these informed women chose mastectomy (Collins et al., 2009). “We can’t make assumptions that everybody is going to feel the way that we do, so you have to ask the patient,” she said. Dr. Clancy added that some patients with laryngeal cancer likely prefer having radiation therapy over surgery because although they will not live as long with this treatment, it will preserve their ability to speak and that is more important to them than the length of their life.
Providers also have to be sensitive to what patients are saying. “You need to have competencies on both sides,” said Willis. “It’s not enough for me to go to my doctor and communicate my needs. My doctor needs to be able to listen to what I’m saying.” Dr. Anthony Back, professor of medicine
at the University of Washington and director of the Program in Cancer Communication at the Seattle Cancer Care Alliance and Fred Hutchinson Cancer Research Center, noted that one meta-analysis (Venetis et al., 2009) found that when patients are encouraged to participate in conversations with providers and these providers show empathy, the patients are more likely to report being satisfied with their care than when there is more “instrumental talk,” in which the providers merely indicated the tests and treatments they would be having. Dr. Nancy Keating, associate professor of medicine and healthcare policy at Harvard Medical School and general internist at Brigham and Women’s Hospital, conducted a study that found patients with breast cancer who received the degree of input they wanted into decision making about their treatment were more likely to report being satisfied with their treatment choice than those who did not (Keating et al., 2002).
Dr. Burhansstipanov, who is part Cherokee and advocates for Native Americans, stressed the importance of being culturally sensitive when communicating with patients of differing ethnicities and cultures. She said misunderstandings often occur when doctors inform their Native American patients that their biopsy is “positive” because the patient often assumes this is good news, otherwise the doctor would not consider it to be positive. Gay and lesbian couples, she added, should not be asked if they have a spouse, but rather if they have a lifetime partner who should be informed of the patient’s medical condition.
She also noted that many Native Americans view spirituality as being intertwined with healing and seek traditional healers or spiritual advisers while being treated medically. Physicians need to be sensitive to other religious traditions, as well as the role spirituality plays in healing, Dr. Burhansstipanov said. She added that doctors also have to be cognizant that in some Native American tribes, the mother is the decision maker for her children, even grown children, and thus must be consulted when devising cancer treatment plans.
Other speakers stressed the importance of communication with the family or caregivers of the patient as well as with the patient, and recognition that their informational needs are different. For example, family members need to know how to care for a patient during cancer treatment, how to plan for practical and financial concerns, and how to talk with children about a parent with cancer, Dr. Marie Bakitas, associate professor of anesthesiology at Dartmouth Medical School, pointed out. Studies show it is also helpful to have family members or other companions with patients at
doctor visits to make sure that patient needs, preferences, and questions are conveyed and that the information is being understood. As Dr. Ganz noted, because of the stress of a cancer diagnosis and treatment, a patient may not be able to ask questions and take in what the doctor is saying and a family member or a companion may be more able to do so. One study found that when a companion was present with a patient, significantly more questions were asked than when the patient was alone (Eggly et al., 2006). Dr. Back suggested that physicians should endorse having patients be accompanied by someone other than a family member or friend. This person could take notes, ask questions, and hopefully retain more of what is said than would a family member or friend who is emotionally attached to the patient.
Communication with Patients with Advanced Cancer
Communication about advanced cancer can be especially challenging. Dr. Peppercorn referred to a statement from the American Society of Clinical Oncology (ASCO) on care for patients who have advanced cancer, and thus a poor prognosis (Peppercorn et al., 2011), specifying that when discussing cancer treatment options with patients, they should be told the relevant pessimistic information as well as optimistic information to best inform their decision making. The policy statement also argues that patients should be told not just the likelihood of a response, but the nature of that response (i.e., whether it will improve symptoms, shrink the cancer, or slow its progression), as well as its costs and toxicity.
Although it can be difficult to convey a poor prognosis, some speakers stressed the importance of being honest when communicating with patients. Dr. Thomas Smith, professor of medicine and palliative care at the Virginia Commonwealth University Massey Cancer Center, said his studies show that patients expect their physicians to be honest with them and informing patients that they have a fatal illness does not quash their hope or make them depressed. However, Mr. Erwin noted that patients like to hear, and physicians like to give, hopeful information, even when it is false hope. This often leads to an overpromotion of various types of treatments that are not likely to be effective in late-stage cancer. “It’s almost as though we no longer give people permission to die,” he said, “so the end-of-life aspect of cancer care can get lost.”
Dr. Smith stressed the importance of conveying to patients in the final stages of cancer that although there may no longer be any effective treatment against their cancer, there are still treatments that can improve their
quality of life for the time remaining. “We don’t want to tell patients there is nothing more we can do,” he said. Dr. Back added that studies suggest patients want guidance after being given a poor prognosis and suggested addressing patients “now what do I do” concerns with an action plan when conveying bad news (see Box 1 on advanced care planning).
Advanced cancer is cancer that cannot be cured. It is sometimes referred to as end-stage or terminal cancer. Advanced care planning entails working with cancer care teams to help patients and their families discuss the diagnosis and prognosis, and identify the best, individualized treatment plan for each patient, including care options at the end of life. One aspect of advanced care planning may entail creating or updating an advance directive. An advance directive is a legally binding set of instructions that explains the kind of medical treatment a person wants or does not want if he or she becomes unable to make those decisions.
Types of advance directives
Living will. This is a written set of instructions outlining a person’s wishes about types of medical care that could be used to sustain life in situations when the person has a life-limiting illness and can no longer communicate his or her wishes about medical care. A living will includes statements about:
- Whether you want the medical team to use cardiopulmonary resuscitation (CPR) and/or artificial life support, such as mechanical respirators, if your breathing or heart stops.
- Whether you want to receive a feeding tube (artificial nutrition and hydration)if you cannot be fed otherwise.
- Whether you want certain procedures, such as kidney dialysis, performed.
Durable power of attorney for health care. This type of advance directive designates a person who will make medical decisions for you if you become unable to make them yourself.
SOURCE: ASCO, 2011.
Advanced care planning is an important component of cancer treatment planning. As Ms. Ellen Stovall, senior health policy adviser at the National Coalition for Cancer Survivorship, noted, “Cancer represents perhaps the diagnosis for which for the first time people could see where or how their life might end, hopefully giving them some time to really think about their preferences for how they would want to live and die, in light of this diagnosis.”
Such planning, however, frequently happens too late or not all, according to Dr. Smith. He noted a study that found many oncologists delay having a discussion with their cancer patients about advance directives until patients show symptoms or there are no longer any chemotherapy options for them (Keating et al., 2010b). This study found that 44 and 26 percent of oncologists discuss do-not-resuscitate (DNR) status and hospice care, respectively, when first meeting with their patients. In addition, only 21 percent discuss the patients’ preferred site of death in those initial patient visits. Another study found that 2 months before death, as many as half of all non-small-cell lung cancer patients had not discussed hospice with any of their doctors (Huskamp et al., 2009). In Dr. Smith’s study of 75 patients admitted to a cancer center, most of whom had recurrent acute leukemia or lymphoma, 41 percent had an advance directive that no one knew about, only five patients had discussed advance directives with their oncologist, and for only two of these five did the oncologist initiate the discussion (Dow et al., 2010).
These findings are contrary to national guidelines that recommend advanced care planning for patients with terminal illness and life expectancy less than or equal to 1 year (NCCN, 2005) and the many studies that document the benefits of such planning. Studies show advance directives have never been associated with shortened survival in any study and are actually linked to better survival (Chung et al., 2009; Ganti et al., 2007). Being overly optimistic about survival is not associated with better survival but is associated with worse end-of-life care (Weeks et al., 1998). In addition, having end-of-life discussions was linked to lower rates of ventilation, resuscitation, and admission to an intensive care unit (Wright et al., 2008). This study also found that earlier hospice enrollment and longer hospice stays were associated with a better quality of life for the patients as well as better caregiver quality of life at follow-up. Another study found that patients who reported having an end-of-life care discussion had on average $1,041 lower health care costs in the last week of life, compared to those who did not have this discussion, with higher costs associated with worse quality life in the last
week of life (Zhang et al., 2009). This study estimates that if discussions of end-of-life care were increased so that half of all individuals who die from cancer in the United States each year report an end-of-life care discussion, there would be a cost difference of $76 million between individuals who have end-of-life discussions compared to those who do not.“This is important as we look to find resources to cover more people and new drugs that work,” Dr. Smith noted.
The frequent lack of discussion about advanced care is apparently not due to reluctance on the part of patients to discuss it. Dr. Smith’s study found that 86 percent of the patients were willing to discuss advance directives with the admitting doctor and 95 percent thought it was important. When given a choice by their doctors, about half of the patients said they would prefer to discuss advance directives with their oncologists, and about one-third wished to discuss them with their primary care providers. Studies also find that the vast majority of terminally ill patients said they wanted their oncologists to be realistic and that they associated honesty about their prognosis with compassion and caring (Matsuyama et al., 2006).
Dr. Smith suggested that discussions about advanced care planning with cancer patients happens too little or too late because of reluctance on the part of oncologists to bring up advance directives. He said one of the main reasons oncologists are so reluctant to have these important conversations is because they think it will depress their patients, but one study of terminally ill patients found that end-of-life discussions were not associated with higher rates of a major depressive disorder or more worry (Wright et al., 2008). This study also found that more aggressive medical care was associated with worse patient quality of life and a higher risk of a major depressive disorder in bereaved caregivers.
Another frequent reason oncologists give for not having end-of-life discussions with their patients is that it will take away their hope, according to Dr. Smith, but he found this not to be true in his study of cancer patients (Smith et al., 2010). He found that hope is maintained even with truthful discussions that teach patients their chance of cure, relapse, progression-free survival and overall survival, and about transitions. “Being truthful for people actually improves their hope. It doesn’t squash it,” he said.
A third reason oncologists frequently give for not discussing advance care directives, such as hospice, is that hospice or palliative care will reduce survival, Dr. Smith said. Yet hospice care was found to increase the survival of patients with various types of cancers (Connor, 2007; Temel et al., 2010). He added that another main reason oncologists frequently neglect discus-
sions of advance directives is because they depress the oncologist, which one study supports (Panagopoulou et al., 2008).
All of these findings suggest that patients benefit from having advanced care planning and doctors are wrong in assuming patients will get depressed or experience poorer care or outcomes due to such discussions, Dr. Smith asserted. To aid these discussions he suggested asking a patient’s permission to have them through such questions as
- My general approach is to be as honest as I can in discussing the future—is that OK with you?
- What do you want to know about your illness?
- What do you know about your illness?
- What are you expecting to happen in the future?
- What do you want to do with the time you have?
Dr. Smith concluded his presentation by stressing the importance of oncologists asking their patients to share their advance directives and then documenting them in the medical record. “Advanced care planning is important to maximize the time people have left for important tasks. We are essentially making a survivorship care plan when the time is short,” Dr. Smith said.
Dr. Clark added the need to “foster a community of hope for our patients that accepts all visions of hope, not just the therapeutic vision that most of us are trained in.” She ended her talk with a quote about hope by Ellen Stovall: “With communication comes understanding and clarity. With understanding, fear diminishes. In the absence of fear, hope emerges, and in the presence of hope, anything is possible.”
Many participants emphasized that cancer care is often fragmented among several different providers, including oncologists, radiologists, surgeons, and primary care providers, and often at several different locations. Many workshop speakers, including cancer survivors, said that coordinating care can be a burden for patients, and problems can arise if all the providers are not on the same page and aware of what treatments the patient is undergoing and how the patient has responded to that care. Although electronic medical records could help to address this problem, as noted by
Dr. Shulman, physicians at different locations may not have access to the records generated by all the providers involved in a patient’s care.
In addition, some speakers stressed that patients need to know who is responsible for each aspect of their care and whom to contact if they develop a serious adverse reaction to their chemotherapy or other complication. Another coordination issue that generated a lot of discussion was the role of the primary care physician in cancer treatment (see also Box 2). Even physicians on a cancer treatment team may not be fully aware of who is responsible for each aspect of care and its repercussions. “There is no set of shared expectations about ‘this is my piece. Then I’m passing this off to you, but you will let me know what happens next.’ This is not beyond our capabilities, but we can’t get to patient-centered care unless that’s a vital part of it. It has to be a team sport,” Dr. Clancy stressed.
As Dr. Ganz noted, 80 percent of oncology care happens in community practices where oncologists, surgeons, and radiation therapists are not all in the same facility and may not even be working at the same hospital. “It’s very important for the patient to know that his or her doctors are talking to each other, that they are working together, that they know what’s going on,” she said, but added that such communication rarely occurs. A comprehensive written cancer treatment plan can aid that coordination by ensuring that all providers are on the same page. Patient navigators can also help coordinate cancer care and foster communication between providers.
Addressing Mental Health Issues
Many speakers noted that a critical part of patient-centered cancer care is monitoring mental health issues such as anxiety and depression. The stress of a cancer diagnosis and treatment makes cancer patients more vulnerable to these mental health illnesses, especially if they have a history of such conditions. Several patients at the conference, including one who had a history of psychiatric hospitalization at the time of cancer diagnosis, pointed out that they were never evaluated for mental health issues or given support for the anxiety and depression they experienced during cancer treatment. As Ms. Willis noted, “Being 15 is very hard, but being 15 with cancer is even harder. Nobody asked me how I was doing.”
A cancer treatment plan can also address and coordinate the psychosocial services that cancer patients need. Dr. Ganz stressed that the IOM consensus report Cancer Care for the Whole Patient (2008) found that there is a paucity of coordination of such services for patients with cancer, despite
the fact that these services are often available. A cancer treatment plan could facilitate better psychosocial care delivery, she said, pointing to the psychosocial services model of care delivery recommended in that IOM report (Figure 1). Mr. Boyajian also noted the importance of attending to the mental health issues of cancer patients. “I have had many side effects from my cancer treatment, including many late effects, but it was the psychological impact that was much more difficult to overcome,” he said.
Patient-Centered Cancer Treatment Plan
The cancer treatment plan is a document that is given to the patient, family, and other treating physicians that serves to keep everyone on the treatment team informed of the path of care, and identifies who is responsible for each portion of that care.
Many speakers noted that a cancer treatment plan should inform patients of their diagnosis, prognosis, and options for care, as well as the potential risks, benefits, and side effects of each, using available evidence from randomized controlled clinical trials, meta-analyses, and clinical guidelines.
Typically a cancer treatment plan will have the following:
- Specific tissue diagnosis and stage, including relevant biomarkers
- Initial treatment plan and proposed duration
- Expected common and rare toxicities during treatment and their management
- Expected long-term effects of treatment
- Who will take responsibility for specific aspects of treatment and their side effects
- Psychosocial and supportive care plans
- Vocational, disability, or financial concerns and their management
- Advance care directives and preferences
As noted by Ms. Angelina Esparza, director of the Patient Navigator Program & Cancer Resource Centers at the American Cancer Society, the plan provides personalized information, including the strategies for addressing a patient’s specific psychosocial and biomedical care needs and the resources to address the specific needs of the patient’s family and caregivers. A cancer treatment plan could also include clinical trial options available to a patient, suggested Dr. Martin Murphy, chief executive officer of the CEO Roundta-
BOX 2
Role of the Primary Care Physician in Cancer Treatment Planning
The first healthcare practitioner that patients usually see when they show signs or develop symptoms of cancer is their primary care physician. Because a patient’s cancer diagnosis is often delivered by that provider, the starting point for cancer treatment occurs in the primary care setting, pointed out Dr. Larissa Nekhlyudov, assistant professor at Harvard Medical School and general internist at Harvard Vanguard Medical Associates. Consequently, she suggested giving primary care providers more information about cancer diagnoses and some guidance as to where referrals should be made for their patients. “A prostate cancer patient we can refer to a urologist, and that decision is made. We can also refer him to an oncologist, and that decision might also be made. So we need to really think about starting in the primary care setting and providing some recommendations for how primary care physicians should refer—which kinds of patients should be referred to a cancer center or to a local oncologist or surgeon,” she said.
Often internists and family doctors know their patients longer and better than the oncologists that patients first meet when they are diagnosed with cancer. Yet the role that the primary care physician plays in the cancer treatment planning of their patients is nebulous and often minimal. “It’s a challenge in developing the treatment plan—knowing who might have a better sense of those patients’ preferences and what they might want to do,” Dr. Ganz said. She pointed out that most cancer patients are over 65 and at diagnosis usually have other chronic conditions for which they are being treated. “Maybe the person who has been taking care of that individual and his or her diabetes or other chronic conditions may have a better sense of what this person’s life view is,” she said. “But once they get this cancer diagnosis, they are not in touch with their internist because of the busyness and complexity of the cancer care delivery system. This is a missed opportunity to actually engage physicians and nurses and other providers who might have known the patient for 20years before that cancer diagnosis,” Dr. Ganz stressed.
Other participants noted that primary care physicians need to be kept abreast of their patients’ cancer treatments because it influences how they care for the patients’ concurrent illnesses and conditions. Such care should be out of the sphere of the oncologist, said Dr. Ira Parker, associate clinical professor of medicine at the University of California,
San Diego; instead, primary care practitioners should be empowered to better serve their patients who have been diagnosed with cancer or who are survivors of cancer, he said.
Dr. Parker also called for primary care physicians (PCPs) to take a more active role throughout their patients’ journey with cancer. “PCPs still have a role in this, especially in regards to advance directives and family meetings. We have to open up our eyes to the PCPs,” he said.
Dr. Mayer noted that her surveys found primary care physicians have great interest in being involved in their patients’ cancer care, especially if they are long-standing patients, but they lack preparation and knowledge in that regard. “One family physician told me, ‘I know I am supposed to play a role, I just don’t know what it is,’” she noted. Another participant added that surveys by Eva Grunfeld show that primary care providers are interested in providing care to their cancer patients if they are given the tools they need to care for those patients (Del Giudice et al., 2009).
Among the tools that aid primary care providers are cancer treatment plans and summaries. “We have found that primary care physicians who receive these treatment summaries and care plans prefer to refer back to those oncologists because they now know how to follow those patients,” Dr. Ganz said. However as Dr. Partridge pointed out, “Primary care providers have different needs than the patients do around these tools” and may require a different version of a cancer treatment plan or summary than that given to patients. Mr. Boyajian concurred and pointed out that primary care physicians do not have the time to wade through all the extensive details involved in a patient’s cancer care. These physicians prefer a more condensed version of a cancer treatment plan or summary, he said.
Mr. Boyajian also stressed providing more guidance for the primary care physician about cancer care. “When I went back to my primary care physician, it was like shock and awe—it was outside his realm of expertise,” he said.
In summary, many participants favored more involvement of primary care physicians in the care of cancer patients, but there are numerous obstacles to achieving that goal in practice, including a lack of sufficient time to adequately participate in the process and to stay abreast of the complex and rapidly changing nature of cancer treatment, poor coordination of care generally, and the growing shortage of primary care physicians.
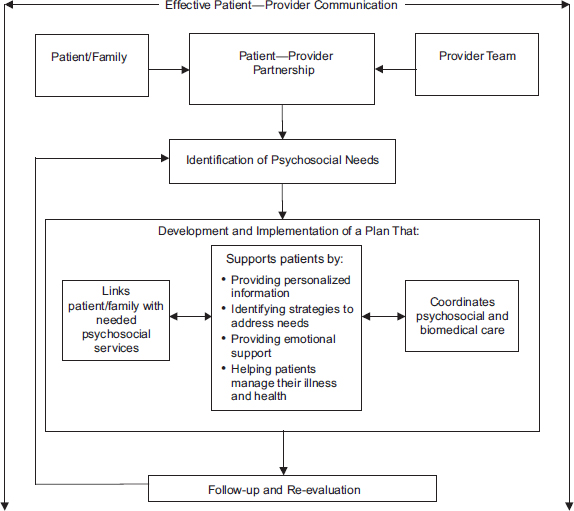
FIGURE 1 Model of psychosocial care. SOURCE: IOM, 2008.
ble on Cancer. Drs. Ganz and Clancy agreed that this could be an important addition that could help increase the number of patients that participate in clinical trials and thus speed progress in improving cancer treatments.
Several speakers stressed that a cancer treatment plan should not just be handed to patients, but instead must be conveyed verbally as well, to facilitate better communication between patients and their providers. “The whole point of a care plan is not just to have a document, but to have a conversation. I think we will have failed if we do nothing but generate treatment plans and that dialogue hasn’t occurred,” said Dr. Julia Rowland, director of the Office of Cancer Survivorship at the National Cancer Institute.
A cancer treatment plan is altered when new information, such as a change in treatment response or in patient preference for treatment, dic-
tates the need for treatment changes. A new treatment plan must then be devised and shared with the patient and his or her providers. “It gives the patient the opportunity to bring up new information,” Dr. Ganz said, such as feeling the need to take a break from chemotherapy or the development of new side effects.
Dr. Ganz pointed out that with the exception of leukemias, lymphomas, and other fast-growing tumors, most common epithelial cancers grow relatively slowly, so patients should not feel pressured to make treatment decisions immediately upon being diagnosed and can take the time to consider all their options and acquire second opinions. “It’s important for us during the treatment planning process to not rush patients to make a decision, and instead to develop a treatment plan by consulting all of the people and professionals who are relevant,” Dr. Ganz said. However Ms. Smith noted that patients may feel otherwise. “When you have an alien living in you, you want it out now,” she said. Dr. Sharon Murphy, scholar in residence at the Institute of Medicine, added that most pediatric tumors tend to be embryonal, not epithelial, and consequently grow much more quickly and require immediate treatment. “You do not have a lot of time. It is sometimes an acute emergency and there is not that leisure to just go home and think about it,” she said.
PATIENT-CENTERED CANCER TREATMENT PLANNING IN PRACTICE: ARE WE THERE YET?
Several recent studies to assess whether patient-centered cancer treatment planning is being put into clinical practice suggest there is much room for improvement in patient education, communication, attention to patients’ emotional and family needs, and coordination of care. Dr. Ed Wagner, director of the MacColl Institute and senior investigator at Group Health Research Institute, reported that in a study of colorectal cancer patients, 29 percent of patients reported not receiving enough information about cancer treatments, 48 percent reported problems in getting health information, and 25 percent said they were not involved in decisions as much as they desired (Ayanian et al., 2005). He also noted that recent research is suggesting that many problems in cancer care can be traced back to failures in communication. Inadequate communication, including failure to provide information on treatment options and failure of providers to listen to patients, may contribute to patient-reported harms, including physical or psychological harm, life disruptions, or unnecessary financial costs.
Breast cancer care is often used as a model for assessing whether patient-centered cancer planning is occurring because for many women with early stages of the cancer, there are two equally effective options: mastectomy or lumpectomy followed by radiation. Consequently, patient preferences and input must be solicited when making treatment decisions.
In a study of breast cancer patients (Lee et al., 2009a), Dr. Sepucha noted that only a little more than half of patients reported hearing about both mastectomy and breast conserving surgery options, and patients reported that the pros and cons of each option were thoroughly discussed only 41 and 18 percent of the time, respectively. Only about half the time did patients report that their doctor asked them which treatment they wanted.
In another study of breast cancer patients (Keating et al., 2003), about 60 percent of patients and surgeons agreed that the surgeon discussed both lumpectomy and mastectomy treatment options, and about 7 percent agreed that they discussed only one or the other. Yet 22 percent of the time, the surgeon said that he or she had discussed both options, but the patients only reported hearing one option. Dr. Keating suggested that this most likely was due to doctors conveying information that patients are not hearing or understanding. “It’s really important that we recognize that this mismatch exists,” she said. “We really need to take a lot of extra care in making sure that all of our patients understand what’s going on.”
Another study found that after meeting with their doctors, only about half of early-stage breast cancer patients knew survival was the same with mastectomy and lumpectomy (Fagerlin et al., 2006). Other studies have found that only 11 percent of breast cancer patients could answer three basic questions about reconstruction correctly (Morrow et al., 2005) and that they vastly overestimated the benefit of chemotherapy (Ravdin et al., 1998) and the risk of dying from ductal carcinoma in situ (Rakovitch et al., 2003). “There are some huge knowledge gaps here,” Dr. Sepucha concluded. “We are not doing a great job of informing patients.”
Dr. Clark added that many patients feel their practitioners are speaking a different language when they relate their diagnosis and treatment options. “The language we use is very important,” she said. In a study that audiotaped patients with hematologic malignancies having a consult with their physicians, “it sounded like you were listening to an ASCO abstract,” said Dr. Back. “One of the patients said it was like being in ‘Bone Marrow 101’.” The median number of recommendations physicians made was nine
per consultation, and only 1 percent concerned how patients could play a role in their care (Alexander et al., 2011).
Dr. Bakitas concurred that often there is information overload as well as presentation at a higher level than patients can comprehend. She observed this in a focus group study of nurses presenting information about cancer treatment to patients, in which patients had poor retention of the information presented (Skalla et al., 2004).
Shared decision making also does not appear to be occurring as frequently as it should, speakers suggested. Dr. Wagner said that cancer patients often say that they did not have enough information to be active participants, while providers felt patients were passive. In Dr. Keating’s study of breast cancer patients, 9 percent reported that their physician decided what treatment they should have, and 18 percent reported their physician presented his or her recommendations for them to accept or reject; 33 percent reported that their doctor discussed alternatives with them and they decided together how to proceed; and about 40 percent said their doctor presented all the available options and allowed the patient to decide (Keating et al., 2002). In her study of lung and colorectal cancer patients, 17 percent of the patients reported they had a more physician-controlled discussion about their treatment, 39 percent reported there was shared control, and 44 percent reported it was a patient-controlled discussion (Keating et al., 2010a).
However Dr. Keating also pointed out that not all patients want to have an active role in deciding their treatment. In her studies, 12 percent of breast cancer patients reported that they preferred to have their physician either decide or recommend their treatment, and 10 percent of lung and colorectal cancer patients preferred such treatment discussions to be physician-controlled. The decision-making role that patients wanted matched the role they received only about half the time in both studies. “About half the time, doctors are actually engaging patients in the way that the patients want to be engaged. It’s probably something we can do a little bit better,” Dr. Keating said.
Similarly, a meta-analysis of 22 studies of cancer patients cited by Dr. Wagner found that the level of participation patients wanted in deciding upon their treatment often did not correlate with the way decision making was shared with their physicians: 44 percent of patients reported that they
wanted shared decision making, but this occurred for only 18 percent of patients, and of the 34 percent of those patients who preferred to be passive in the decision-making process, only 59 percent reported that they actually were passive (Tariman et al., 2010). Dr. Sepucha added that in her studies of breast cancer patients, she found that 18 percent of women who preferred mastectomy had a lumpectomy, about 20 percent who preferred reconstruction did not receive it, and 16 percent who preferred to have chemotherapy did not receive it (Lee et al., 2009a,b, 2010). “So there’s a significant minority of women to whom we are giving the wrong treatment,” she said. “We need to figure out how to make sure we are actually matching the right person with the right treatment every time.”
Perhaps one of the more striking findings in regard to whether cancer patients’ preferences are being solicited or met, according to Dr. Bakitas, is the fact that a large percentage of cancer patients receive chemotherapy during the last two weeks of life. “I’m sure none of them planned on receiving chemotherapy in their last two weeks of life. Clearly, all of us have our work ahead to do a better job laying forth a treatment plan that will result in letting patients decide how they want to live the remainder of their lives,” Dr. Bakitas said. Dr. Smith added, “Most patients are not being asked by their oncologists to share their advance medical directive decisions, even if they have them.”
Sensitivity to patients’ emotional and family needs also seems to be insufficient. In one study (Ayanian et al., 2005), 41 percent reported that their providers did not make them feel better emotionally, and 16 percent felt that their family was not involved enough. In his own cancer patient focus groups, Dr. Wagner found inadequate emotional and social support for patients and families. Dr. Back discussed another study of 400 taped conversations between oncologists and patients that showed that oncologists provided an empathetic response in only 22 percent of encounters that afforded this opportunity (Pollak et al., 2007). In addition, coordination of care is frequently a problem. Dr. Wagner mentioned a study (Ayanian et al., 2005) which found that 25 percent of cancer patients reported problems in how well their providers worked together.
CHALLENGES TO PATIENT-CENTERED CARE
Workshop participants cited several challenges in providing patient-centered care. Some of these challenges stem from the patient and include patients’ lack of assertiveness, health literacy and numeracy, and their
emotional state and concurrent illnesses. Others were due to physician limitations, such as a lack of time to explain complex information and insensitivity to patients’ emotions and cultural perspectives. In addition, a number of system challenges were cited, including fragmentation of the healthcare system, lack of accountable care, and a lack of financial incentives for providers to devote the time and effort required for patient-centered care planning.
A major challenge noted by both providers and patients at the workshop was the high level of stress experienced by a person who has recently been given a cancer diagnosis. The life-threatening nature of this diagnosis often induces a great deal of anxiety, a sense of vulnerability and lack of control, fear of the unknown, and a sense of isolation. This can hamper patients’ ability to take in information presented to them and prevent them from taking an active role in their health care and advocating for their needs and preferences. “We know from all the psychological literature that patients shut down and are not able to hear what we have to say,” Dr. Ganz said, and Dr. Clark concurred that “cancer is a crisis that causes us to go into a state of cognitive confusion. We give all that information when someone is first diagnosed, and it just goes right over their heads.”
Patients’ ability to make good decisions may also be impaired by their emotions, Dr. Gruman added. “When we have to make major health decisions, many of us are deeply anxious and frightened, or our minds are clouded by drugs or by pain, and that may interfere with rational decision making,” she said.
Many patients’ response to such stress is to rely on their doctors to make the proper decisions and to take a more passive stance than they would have otherwise, thus hampering the assertiveness they need for shared decision making about their treatment. “Many patients do prefer a passive to an active role, particularly if they are older or have more serious illness,” said Dr. Keating. Some patients are also hesitant to seek out second opinions for fear of angering their doctor, noted Mr. Mark Smith, principal at the Liberty Partners Group.
It can be challenging to assess how much information patients are capable of taking in, as well as how much they want to know. As Dr. Bakitas noted, “Some patients want to prepare for every possible outcome, while others are in denial and want to avoid every possible piece of information.”
Dr. Mayer added, “Some people want the headlines, while some people want the source material. One size does not fit all. We need to have a variety of options if it is truly going to be patient-centered. Otherwise we are [cancer] center-centered and not patient-centered.”
Lack of Health Literacy and Numeracy
Dr. Clark noted that another major barrier in communicating to patients about their cancer diagnosis and treatment is a lack of health literacy, with the average person having had his or her last health course in high school. Dr. Clancy concurred and added that “people don’t get instructions. Often there are communication errors about fairly basic things.” Dr. Ganz also stressed that cancer and how it is diagnosed, staged, and treated constitute an extremely complex topic to cover in an office visit, especially since the physician is likely to be under time pressure. Conveying all relevant genetic details in a concise fashion to primary care physicians and other practitioners involved in a patient’s care is also challenging, especially since this information is continually being updated in the medical literature.
Both doctors and patients also need to better understand the potential risks and benefits of cancer treatments, some participants suggested. This information has to be presented in a clinically relevant way, such as the number of patients that need to be treated to achieve a positive benefit for one patient (known as the “number needed to treat”1), Dr. Sheldon Greenfield, professor of medicine at the University of California, Irvine, pointed out. There is also room for improvement in basic math skills. “A huge percentage of people can’t figure out what 10 percent for a tip is or understand even pie charts,” Dr. Russell Glasgow, deputy director of dissemination and implementation science at the NCI Division of Cancer Control and Population Sciences, noted. Dr. Kaplan added, “I don’t think we are there yet, even on the physician side, never mind on the patient side. I teach statistics to doctors and the number needed to treat is still elusory to many practicing physicians.”
___________________
1The number needed to treat (NNT) is an epidemiological measure used in assessing the effectiveness of a healthcare intervention, typically a treatment with medication. The NNT is the number of patients who need to be treated to prevent one additional bad outcome (i.e., the number of patients that need to be treated for one to benefit compared with a control in a clinical trial). The ideal NNT is 1, where everyone improves with treatment and no one improves with control. The higher the NNT, the less effective is the treatment.
Patients can also misinterpret health information presented to them because of their biases. They may not appreciate the benefits of chemotherapy because they view it as a poison and may not understand how a poison can be helpful, Dr. Sepucha noted. Patients from disenfranchised communities may also distrust the healthcare system as a whole, and this can be a major impediment to their receiving the care they need, pointed out Ms. Esparza. Dr. Ganz added that fear of treatment toxicity may hamper decisions. “Often what poisons the well for people is if they have seen a loved one experience toxicity from cancer treatment, or get treatment and die anyway,” she said.
Also challenging are conflicts between what the patient would like to have as a treatment and what his or her family members would like. “Most of the time I see this when the family wants more aggressive care than the patient. But it’s our job not to just say ‘it is patient autonomy and they get to make the decision,’ but to help guide everybody through a process that everyone can hopefully feel good about in the end,” said Dr. Peppercorn. Family dynamics can also complicate planning cancer care, Dr. Clark noted, because there are no guarantees that family members can give good social support, and families frequently undergo caregiver burnout. Dr. Bakitas added, “When we are thinking about communicating cancer treatment planning needs, we are thinking about not just the patient, but the family members, and recognizing that they might have different needs.”
There can also be conflicts between the type of treatment a patient wants and the type of treatment a doctor thinks is best for the patient. Sometimes a patient may want to pursue a treatment the doctor considers dangerous. For example, a patient diagnosed with a node-positive and aggressive subtype of breast cancer may decide to forgo surgery after having a good response to neoadjuvant therapy. “It can be challenging to have a patient who has a preference for something with no evidence of benefit or even evidence of harm. This does happen in practice and as we talk about shared decision making, we need to at least think about how we are going to deal with those issues,” Dr. Peppercorn said.
Some of the challenges in providing patient-centered cancer treatment planning are due to shortcomings in the current healthcare system in the United States. These challenges include fragmentation that hampers coordination of care involving a number of specialists per patient, with treatments across time and space at various outpatient, inpatient, and specialized treatment facilities or private physician practices, Dr. Ganz noted. Fragmentation of the healthcare system may also make it difficult to deal with comorbidities that patients frequently have in addition to cancer, including heart disease and diabetes. Dr. Bakitas noted that it often is not clear which provider is responsible for which disorders and suggested being more explicit about how care is divided among providers. “If you have a playbook and everyone knows what their job is, there are more chances of success of that process,” she said.
Dr. Gruman added that due to the decentralized medical care most patients receive in this country, some patients may choose the treatment they want for their cancer and then choose the physician who can administer that treatment, which may preclude shared patient-doctor decision making and selection of a cancer treatment plan. It also is challenging to determine who should be responsible for devising such a plan—often the first physicians that patients see as they embark on their cancer journey are their primary care physician and a surgeon, but they may not be best suited for devising a comprehensive cancer treatment plan, Dr. Ganz noted.
Dr. Ganz added that a lack of accountability and accountable care entities also hinders patient-centered treatment plans’ becoming standard of care. She deplored the lack of financial incentives to reward physicians for taking the time needed to foster shared decision making, coordinated care, and the other components of patient-centered care. Currently, physicians are not paid for these types of activities, she said. There also is a lack of financial resources to pay for patient advocates, navigators, and social workers, who can help coordinate patient care and ensure that psychosocial needs are addressed, Dr. Clark stressed.
In addition, a lack of accountability can impede care, when more than one insurance policy or federal agency, such as the Indian Health Service, is involved, and it is not clear which policy or agency will pay for or provide what service. A shortage of providers and services, and inadequate and untimely reimbursement for healthcare and related services, can create delays in delivering cancer care and impede the development of a cancer
treatment plan that can be followed, pointed out Dr. Burhansstipanov. Dr. Wagner concurred that his research has found there is unequal access to care. “We found places in this country where uninsured patients could not get symptoms of cancer properly followed up and diagnosed. We found that the reimbursement system by everyone’s account was a major barrier to the provision of patient-centered care,” he said.
Providers also often find it difficult to conduct patient-centered cancer planning because of a dearth of patient-focused information. “We have the studies that look at survival or disease-free survival, but don’t address such questions as, ‘How am I going to feel?’ or ‘How long before I can get back to work?’” said Dr. Sepucha. She suggested systematically collecting this information from patients currently receiving cancer care so that the information is available for newly diagnosed patients.
TOOLS, PERSONNEL, AND PROGRAMS TO OVERCOME BARRIERS
Participants at the workshop offered several strategies for overcoming or lessening the current barriers to providing patient-centered cancer care, including tools and resources, personnel that can fill gaps in care and help coordinate care, enhanced training, and model care programs.
Several resources are available that can improve patient-centered cancer treatment planning, including those provided by the National Transitions of Care Coalition. On its website, the coalition provides tools called “My Medicines,”2 for listing important information about a patient’s medications, and “Taking Care of My Healthcare,”3 a guide for patients and their caregivers to be better prepared when they see a healthcare professional, including suggestions of questions they can ask. In addition, NCCS’ Cancer Survival Toolbox4 equips patients to better meet and understand the challenges of their illness. This free audio-based resource, developed by leading cancer organizations, helps individuals build important skills that can be beneficial in navigating a cancer diagnosis, including how to communicate,
________________________
2See http://www.ntocc.org/Portals/0/My_Medicine_List.pdf.
3See http://www.ntocc.org/Portals/0/Taking_Care_Of_My_Health_Care.pdf.
find information, make decisions, and negotiate and stand up for one’s rights as a patient.
AHRQ provides a number of patient guides for people with various types of cancer that help empower patients, including a list of questions patients should ask their providers, said Dr. Clancy. Some oncology practices and centers provide one-page forms patients can bring to their doctor visits that suggest information they should discuss with their doctor, including diagnosis, stage, and treatment goals. Dr. Back said he routinely sends patients a letter or e-mail that specifically invites them to bring questions and someone who can advocate on their behalf when they come to see him. Giving patients permission to ask questions is “hugely important,” he said, and noted an Australian study in which physician endorsement of patient questions positively correlated with the number of questions patients asked (Clayton et al., 2007). Dr. Clancy agreed about the importance of encouraging patients to ask questions and giving them a sense of the types of questions they should ask. The American Cancer Society also offers a number of online tools, including their “Cancer Profiler”5 treatment decision support tool that helps patients understand how their diagnosis, test results, and medical history affect treatment options.
The American Society for Clinical Oncology recently released a guide to help patients with advanced cancer broach difficult conversations about their prognosis, treatment, and palliative care options with their physicians (ASCO, 2011). Dr. Smith, a palliative care physician, gives his patients with metastatic cancer information forms specific for their stage of cancer that present written information along with graphic representations to show their chances of a treatment working, and how long they are likely to live with or without treatment. At the end of this form, patients are asked their advance medical directives in simple language, such as “If you couldn’t speak for yourself, who would want to make decisions about your care?” Dr. Smith said most patients reported this information was helpful and did not exhibit any undue distress when they read it (Smith et al., 2011).
It is also helpful to patients if doctors provide a written summary of their consultation, Dr. Back suggested. Such summaries improve patient satisfaction and understanding, he said. He writes a one-page summary for each patient during the consultation visit. This summary provides a record of the visit and points to future action. The patient is given a copy of the
________________________
summary, which is also placed in the patient’s chart. “The patients bring these back, so it’s clear to me that they are reading them,” he said.
Patient and physician reminders and prompts for suggesting a palliative care consult or asking patients about their advance medical directives, or other information, can also be helpful, Dr. Smith reported. He noted one study that found when prompts about such directives were given to primary care physicians in conjunction with mailing patients advance directive forms and educational literature about them, more patients completed their advance directive forms (Heiman et al., 2004). However, the physician reminders alone did not appear to have an effect.
Sometimes verbal descriptions are not sufficient in describing the options available to patients, and videos may be more effective, said Dr. Smith. In one randomized study, patients with malignant glioma either were shown a video depicting three levels of medical care or received a verbal narrative of these options. The three levels of medical care included (1) life-prolonging care, including the administration of cardiopulmonary resuscitation (CPR) and ventilation; (2) basic care, including hospitalization without CPR; and (3) comfort care, such as symptom relief. Investigators found that patients who watched the video were much more likely to choose comfort care or basic medical care and not life-prolonging care compared to patients who received only verbal descriptions of the care options (El-Jawahr et al., 2010).
A number of technologies can aid patient-centered cancer care and planning, including electronic medical records (see Box 3) and telephone counseling and follow-up by nurses to save patients the trouble of traveling to an outpatient clinic. Dr. Russell Hoverman, vice president of Quality Programs at Texas Oncology and medical director of managed care and disease management at US Oncology,6 noted that at US Oncology, oncology-certified nurses call patients before they receive chemotherapy to discuss their advance directives and other information.
Interactive voice response or automated telephone systems that elicit patients’ symptoms may also be useful. One study found that such automated systems led to faster symptom response times and referrals than those using a cognitive behavioral phone interview with a nurse (Given et al., 2008), and another study found that patients had an increased discussion of symptoms and quality of life with their providers when they used
________________________
6US Oncology is the largest community-based cancer care and research network in the nation, with nearly 550 affiliated sites of care and 1,400 physicians.
BOX 3
Electronic Medical Records
An important tool that may have a positive impact in furthering patient-centered cancer treatment planning is electronic medical records (EMRs). As Dr. Shulman pointed out, EMRs can facilitate safe and high-quality care by the following means:
- Creating a crucial checklist of key components in a treatment plan, including addressing psychosocial issues.
- Providing auto-fill options with drop-down menus that avoid errors of omission and transcription, thereby making care more efficient and making it easier to fill out a cancer treatment plan.
- Coordinating care by automatically sending a cancer treatment plan and any changes made to it to all involved providers and patients.
- Directing providers to follow treatment guidelines by preventing physicians from ordering chemotherapy without having a treatment plan and following its dictates.
- Tracking behavior and providing feedback—the American Society of Clinical Oncology and the National Cancer Institute petitioned the Certification Commission for Health Information Technology to develop oncology-specific criteria to include in EMRs. Work is now under way, with ASCO members included in the workgroup.
- Auto-generating patient teaching sheets related to drugs in a treatment plan, as well as patient consent forms—the National Library of Medicine is linking EMRs to ICD-9s (International Classification of Diseases, 9th Revision) for both provider and patient educational materials.
computer-based patient symptom reporting (Berry et al., 2011), Dr. Bakitas noted. “We need to expand the use of interactive, phone, and Web-based strategies in treatment preparation and symptom management,” she said.
There are also tools and technologies to assess patients’ psychosocial needs and help address those needs. Ms. Ivy Ahmed of the Cancer Support Community described an iPhone application her organization developed called Cancer Help. This application tracks users’ moods and identifies psychosocial resources in their area.
- Generating information about how specific treatments are likely to affect specific subgroups of patients. For example, US Oncology used patient data collected in its healthcare system to determine the comparative effectiveness of Avastin in different age groups for various tumor types. Data standards, interoperability, and curation are needed for this information to be generated.
Dr. Wagner concurred, saying his research indicated that although EMRs were not widely used, when they were available, they seemed to help with planning treatment, preventing errors, and coordinating care. Dr. Shulman also stressed that EMRs can change physician care patterns much more so than standard means. “You can send physicians an e-mail saying ‘starting tomorrow everybody is going to do X or Y’ and hope they do it. But at least in my institution, 50 to 60 percent of the doctors delete all of my e-mails giving them instructions. But if every time they go into the patient record, it will remind them to do X or Y, that is a much more effective way to change behavior,” he said.
Dr. Hoverman suggested that patient-reported outcomes be built into EMRs. Dr. Shulman noted that pain scores and other such patient-reported outcomes are great monitoring tools when they are incorporated into EMRs.
Although EMRs can save money by reducing the time it takes to access patient charts and data, many community practices cannot afford electronic medical records, several participants pointed out. Dr. Shulman countered that although “there is a large initial investment in implementing EMRs, it will pay off in spades in the long run. But it is very hard to show that, and it has been one of the obstacles for adoption because people see the initial bill and it is hard for them to see what the downstream savings are.”
Dr. Ganz noted other screening tools, such as the distress thermometer, that doctors can use to detect depression in their patients or to aid with symptom management. Many of these newer tools are electronic, she said. She noted that physicians generally do a poor job detecting depression or a past history of mental illness in their patients. She uses the Patient Health Questionnaire (PHQ-9) survey for her patients who are cancer survivors. She suggested that screening for mental health issues be part of the cancer treatment planning process.
There was some discussion of the role the Internet can play in educating patients. There seemed to be agreement among participants that the Internet can be a valuable complementary resource and that doctors should direct patients to reliable and accurate websites to find information about their particular cancer and its treatment. “We need to give them the trusted Internet sources because we are not going to be able to provide all that information in that one consultation or even in that treatment plan,” said Dr. Ganz. Dr. Back added that “people come in having read a fair amount of stuff and my job is to help them sort through it and endorse the stuff that I think is really accurate and put in a caution about the stuff that isn’t accurate.” Dr. Kaplan added that the Web can also offer patient empowerment tools so they are more active participants in their care.
Many workshop participants suggested that there be better training for physicians and other providers about patient-centered cancer care planning. There currently are a few programs for such training, including a program at Georgetown University that pairs up first-year medical students with patients, Dr. Rowland reported. Patients tell the students their medical histories; then the students attend all of the patients’ medical appointments. “The student’s job is to learn what it is like to be on the receiving end,” she said. The University of California at San Francisco (UCSF) also has interns available to accompany patients on their office visits. This program teaches doctors-in-training to be more sensitive to patients’ needs, while at the same time providing patient navigation to improve patient care.
Dr. Back also suggested that we train physicians better so they respond well to active and assertive patients, instead of defensively viewing them as difficult. He and Drs. Ganz and Peppercorn suggested providing better role modeling for physicians in training, as well as feedback on their performance in real time, but Dr. Back added that this training must continue after medical school. “I don’t think you can rely on what happens [to someone] as a medical student to continue to serve them when they turn out to be an oncologist. There’s a new level of reintegration they need to do,” Dr. Back said.
Dr. Bakitas suggested training nurses on how to have end-of-life conversations with their patients. Dr. Ira Parker, associate clinical professor of medicine at the University of California, San Diego, suggested there be
more training for geriatric oncologists and oncology nurses so that cancer patients’ comorbidities are effectively treated.
Ms. Brenda Nevidjon, clinical professor and specialty director of nursing and healthcare leadership at Duke University School of Nursing, proposed that there be more dissemination of the best practices from both community care private practices and academic centers. Dr. Partridge concurred, adding, “As we figure out the best ways and tools, we absolutely also need to think forwardly about how to train people to implement them.”
Many speakers at the workshop advocated for greater use of patient navigators, nurse oncologists, and social workers to provide more patient-centered cancer care.
There was a lot of discussion at the workshop about patient navigation and how or even whether to make more use of patient advocates or navigators, as well as how to develop a new business model to support them. During her presentation, Ms. Esparza cited C-Change’s definition of patient navigation, which is “individualized assistance offered to patients, families, and caregivers to help overcome healthcare system barriers and facilitate timely access to quality medical and psychosocial care from pre-diagnosis through all phases of the cancer experience” (C-Change, 2005). This definition asserts that navigation services and programs should be provided by culturally competent professionals or nonprofessionals in a variety of medical, organizational, advocacy, or community settings.
In addition, the type of navigation services will depend on the particular type, severity, and complexity of the identified barriers, which explains why both professional and nonprofessional navigators can help provide these services, Ms. Esparza pointed out. Patient navigators who once were patients themselves can serve another important role, Mr. Boyajian noted, in helping relieve patients’ isolation and show them that favorable outcomes are possible. “I wanted to see someone who had lived through what I was going to go through,” said Mr. Boyajian. “That made more of a difference than anything the people in the white coats told me.” Dr. Mayer concurred and added that patient surveys on survivorship care plans showed that patients wanted peer navigators. “The professional navigator is a Band-Aid
on a broken system, someone who helps patients figure out how to get from point A to point B. But a peer navigator is somebody who can show them the journey, and that they are a few steps ahead of them and are doing relatively well, and can talk to them peer to peer,” she said.
Navigators have many responsibilities, as can be seen in Figure 2. “Navigators should be viewed as clinical extenders,” said Ms. Esparza. “They are not necessarily doing the work of anybody else who is already in the system, but rather, enhance that work by doing the triaging. They are understanding where the best place is for this patient to go to seek information or to seek resources.”
The first patient navigation program was developed for medically underserved patients at Harlem Hospital and was shown to foster earlier diagnosis of breast cancer and to increase the number of patients who had colorectal cancer screening, Ms. Esparza reported. Since then, she said, several studies have shown numerous benefits of patient navigation, including the following (Bayard et al., 1997; Gabram et al., 2008; Gittell et al., 2000; Lasser et al., 2009; Oluwole et al., 2003; Stille et al., 2005):
- Improvements of adherence to screening, diagnostics, and treatment regimens
- Improvements in completion of treatments and reported levels of increased psychosocial support
- Increased enrollment and retention in clinical trials
- Increased patient-reported quality of life
Ms. Esparza reported that the patient navigation services offered by the American Cancer Society (ACS) served more than 83,000 patients and caregivers in 2010. A recent internal evaluation found that the more patients met with their navigators, the more they experienced an increase in self-efficacy and understanding. They also were better able to cope with their disease. The navigators also improved communication between the patient and the healthcare provider, decreased barriers to care, and reduced the degree of fear and anxiety patients reported when initially interacting with healthcare providers. Ms. Esparza asserted that patient navigation should ultimately save patients’ lives by helping eliminate all the nonmedical issues that can impede a patients’ best chance for optimal use of the system.
Dr. Ganz pointed out that with the current complexity of health care, especially for cancer patients, it is not just the patients who are traditionally underserved that require patient navigation, but all patients. “When the
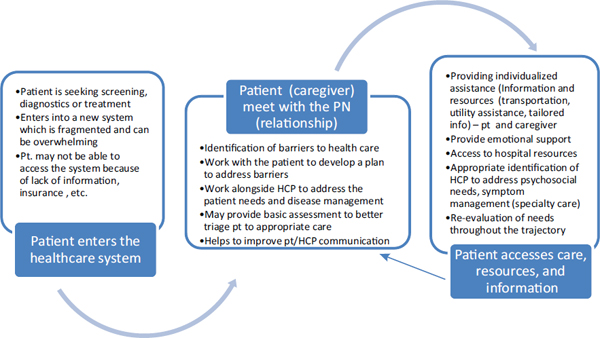
FIGURE 2 The roles of patient navigators includes facilitating patients’ entry into the healthcare system, establishing a relationship to assess and address patient needs, and providing access to resources and care. NOTE: HCP = health care professional; PN = patient navigator; pt = patient. SOURCE: Esparza presentation (February 28, 2011).
average person coming to get medical care needs some kind of navigator, I think we’re in big trouble,” she said, and argued that instead there should be some sort of structural, systemic reform so patient navigators are not needed. “We have to put the care back into caring for patients with cancer,” Dr. Ganz stressed. Others also questioned using patient navigators as Band-Aids to an ailing healthcare system and instead called for healthcare reform. “We need to rebuild the cancer care system, not shuffle the chairs on the deck of the Titanic,” said Dr. Ferrell.
However, Ms. Esparza stressed that health disparities still exist, so some patients need navigation more than others and that navigation improves outcomes the most in those subpopulations. “Let’s not throw the baby out with the bath water, and instead let’s refine where the system needs improvement,” she said.
Patient navigation has now become more integrated in Canada as a means to improve care and increase efficiency, Ms. Esparza reported, and an ACS survey7 found that there are more than 1,000 individual groups claiming to provide some type of patient navigation. More than half of the patient navigators had been caregivers to people who had severe disease, and their average age was 59 years. Many navigators were nurses or social workers as well as other health professionals. The lay patient navigators tended to work more closely with community groups and with minority and medically underserved populations. Most navigators were paid around $40,000 annually, although this figure varied depending on their educational background and on the part of the country in which they were working.
Dr. Burhansstipanov noted that the Native American patient navigators she works with are lay navigators who are paid between $11 and $13.50 an hour depending on their level of education and training. Prior to paying these navigators competitive wages, Dr. Burhansstipanov had a problem with high turnover. “We had to have competitive salaries not to lose them, and now we videotape all our training so that if there is turnover, we can handle it,” Dr. Burhansstipanov said. Now, they only lose about one patient navigator every five years.
Dr. John Mendelsohn, president of M.D. Anderson Cancer Center, suggested that patient navigation be more integrated into the healthcare system rather than being a “cottage industry” dependent on grants and philanthropy. Yet he also pointed out that given the current economy and high costs of medical care, it is hard to imagine how the additional costs of
________________________
supporting patient navigation will be borne. Dr. Kaplan suggested thinking outside the box to make a business case for patient navigation because it is likely to reduce healthcare costs by preventing readmissions, costly errors, and other medical expenses. “To put a new player on the ground, you are going to have to save somewhere, and continuity of care and systems that are organized to realize those cost savings aren’t out there right now,” Dr. Mendelsohn said. Ms. Esparza added that patient navigators improve the efficiency and effectiveness of medical services by fostering low no-show rates and patients’ adherence to treatment regimens, as well as encouraging treatment on a timely basis before major health complications develop. “If we continue to collect the data that show this, we can make the business case,” she said, and suggested that the new Center for Medicare and Medicaid Innovation8 collect such data.
Ms. Esparza noted that much still needs to be defined within the burgeoning field of patient navigation, such as how patient navigators are trained and what competencies they should have. She pointed out that the American College of Surgeons’ Commission on Cancer9 is expected to provide a new standard on patient navigation in 2011.
Ms. Esparza also stressed the need for common outcome measures to assess the impact of patient navigation. ACS has developed a supplement that provides navigation measures across the care continuum. Dr. Mendelsohn suggested including improved survival and cure rates as outcome measures for patient navigation.
However, as previously noted by speakers, a major challenge of patient navigation is how to integrate it into the current healthcare system, and who will pay for this service. “There are hospitals that are asking for this to be part of their system, and there are individuals who want to fund it as well as some federal money being spent on this. The interest and support is there, but now we have to make sure that the policy follows,” Ms. Esparza said.
________________________
8See http://innovations.cms.gov/news/media-center/cms-introduces-new-center-formedicare-and-medicaid-innovation/.
9The Commission on Cancer (CoC) is a consortium of professional organizations dedicated to improving survival and quality of life for cancer patients through standard-setting, prevention, research, education, and the monitoring of comprehensive quality care. See http://www.facs.org/cancer/coc/cocar.html.
Oncology Nurses and Social Workers
Dr. Bakitas focused her remarks on the underutilization of nurse oncologists as communication resources during cancer treatment planning. These health professionals have several assets that can aid the communication process, including being trusted by and accessible to patients, she said. A 2010 Gallup poll found that the American public judged nursing as the most trusted, honest, and ethical profession (Gallup, 2010), Dr. Bakitas said. She added that board-certified oncology nurses also have more contact with cancer patients and their families than any other discipline, with one study documenting that nurses spend one to two hours in patient communication during each cancer treatment (De Raad et al., 2010). In addition, a systematic review of 46 studies found that the nurses’ role as information providers for cancer patients is prominent, especially after the initiation of treatment, and that nurses are effective in providing information (Koutsopoulous et al., 2010). There is also some evidence, Dr. Bakitas said, that patients may prefer nurses as information providers at specific times in their treatment, especially with regard to symptom management.
Dr. Bakitas cited several studies that showed the benefits of using oncology nurses, including a study of newly diagnosed patients with solid tumors who were discharged after surgery (McCorkle et al., 2000). Those who received a standardized nursing protocol, including comprehensive clinical assessments, monitoring, and teaching, had better 2-year survival rates than a control group. Another study (Northouse et al., 2010) found that nurse communication with family members reduced caregiver burden and improved the caregiver’s ability to cope, increased self-efficacy, and improved quality of life. In addition, another study found that communication about palliative care at the initiation of cancer treatment can influence quality of life and mood through the end of life and might improve survival outcomes (Bakitas et al., 2009).
Despite the benefits of using oncology nurses in cancer treatment planning, the IOM consensus report The Future of Nursing: Leading Change, Advancing Health found that these health professionals are underutilized in many areas of health care (IOM, 2010), Dr. Bakitas noted. She called for making the communication role of the oncology nurse explicit through cancer treatment planning guidelines.
Social workers are also communication specialists that should be used more in cancer treatment planning, according to Dr. Clark. She added that the report Imperatives for Quality Cancer Care (NCCS, 1996) specified that
psychosocial services must be safeguarded and promoted. She called for social workers to advocate for individual patients both in the healthcare system and in the policy arena, so their profession becomes an integral part of cancer treatment planning.
A number of model programs have attempted to make cancer treatment planning and other aspects of health care more patient-centered. These models include patient coaching programs, centers for shared decision making, enhanced discharge planning programs, accountable care systems, and self-help support groups.
Dr. Kaplan has been studying programs in which patients are coached prior to seeing their physicians for care for a variety of conditions, including breast cancer, diabetes, hypertension, and rheumatoid arthritis. Such coaching involves showing patients their medical records and explaining how to use their medical information to ask their providers questions and participate in decision making about their treatment. Dr. Kaplan’s randomized, controlled studies show that coached care improved glycemic control in diabetes patients and led to a 25 percent reduction in symptoms and a 30 percent improvement in functional status. Compared to controls, patients receiving coached care asked three times more questions, were two times more effective in information seeking, and took more control of the conversations they had with their physicians (Greenfield et al., 1988).
To further patient-centered decision making, the Hitchcock Breast Center at Dartmouth has a Center for Shared Decision Making to whom all patients with breast cancer are referred when they are first diagnosed. At this center, patients fill out online surveys, including those that capture their medical and family history, and ask how important it is to them to keep their breasts, avoid radiation, and other treatment-related preferences. Patients also watch a video with a decision aid that is appropriate for their situation. Patients are then asked what treatment they are leaning toward and how certain they are about the choice. In addition, they are asked if they
understand survival and recurrence rates for the various treatment options. All of this information from patients is placed into a clinical decision support system, which triggers different actions depending on what the patient responses were. “It’s a way to bring the patient’s goals and concerns into the visit right away, so we can try to make sure that we are really tailoring things to what the patients want,” said Dr. Sepucha.
To assess the value of this center, patients were asked questions related to their knowledge of breast cancer treatment options after a visit with their doctor, including the likelihood of the treatment options to affect survival and recurrence, and how much time they could take to decide on a treatment option. Ninety-two percent of patients answered these questions correctly, Dr. Sepucha reported (Collins et al., 2009). “So when you have this decision support in place, you can consistently get people very well informed,” she said. “Shared decision making, supported by decision aids and other tools, works,” she concluded.
The University of California, San Francisco’s Carol Franc Buck Breast Care Center offers a Decision Services program, which provides decision aids to patients in advance of their doctor’s visit, along with an information packet they are encouraged to review. In addition, interns offer each patient consultation planning over the phone or in person, which results in a prioritized list of questions for the provider that is written down and sent to both the patient and the provider. These interns are also available to accompany patients on their doctor visits, during which they record the discussion and write down the answers the doctor gives to the patient’s questions. These answers are reviewed by the doctor, put in the medical chart, and also sent home with the patient, along with an audiotape of the visit. When Dr. Sepucha surveyed patients who had been through this process, 95 percent said they heard about all treatment options from their doctor, with most also responding that both the pros and the cons of those options were discussed. About two-thirds reported that the doctor asked them what their treatment preferences were (Belkora et al., 2011).
US Oncology has implemented a number of programs to help ensure that its care is more efficient and patient-centered. The basis for its patient-centered delivery system is a comprehensive, evidence-based suite of recommended regimens and routine assessments of whether physicians are following those regimens, as well as performing well on the patient-centered
metrics of ASCO’s Quality Oncology Practice Initiative (QOPI).10 These metrics include having a discussion with the patient about the intent of chemotherapy and providing the patient with a chemotherapy treatment plan, assessing patient emotional well-being and pain levels, and providing appropriate hospice enrollment.
Patient education and self-management build on this template, Dr. Hoverman reported. US Oncology’s Innovent initiative provides a standard information packet to patients. This packet includes a section on advanced care planning discussions and on questions to ask the physician. Patients’ symptoms are also color coded for severity, such that different colors trigger different actions on the part of the healthcare team. If a patient has a severe symptom, for example, this would automatically trigger immediate care. In addition, US Oncology’s Practice Quality and Efficiency initiative reengineered physician, lab, and infusion processes to enhance ideal patient flow and decrease patient wait times.
US Oncology is currently exploring how to incentivize its programs and reward physicians and other healthcare providers who meet its quality metrics. One issue that Dr. Hoverman and others in his organization have been wrestling with is the minimum number of metrics needed to determine whether quality, patient-centered care is being provided. “We have to do more research into parsimony in metrics,” he said.
Several participants pointed out the value of programs that measured outcomes and used those measures to provide feedback to physicians so they can improve their patient care. Dr. Smith cited a study (Blayney et al., 2009) showing that within just a few months of instituting QOPI and informing doctors of their scores on the QOPI metrics, the percentage of patients receiving chemotherapy during the last two weeks of life dropped from 50 percent to 20 percent. Mr. Gorman suggested collecting measures of patient experience and making them publicly available to spur improvements in patient care. “In a world of accountable systems, patient information [such as the main reasons patients are admitted to the hospital] could be collected and fed back to the systems so that they know how well their planning pro-
________________________
10ASCO’s Quality Oncology Practice Initiative (QOPI®) is an oncologist-led, practice-based quality improvement program. QOPI’s goal is to promote excellence in cancer care by helping practices create a culture of self-examination and improvement. The process employed for improving cancer care includes measurement, feedback, and improvement tools for hematology-oncology practices. See http://qopi.asco.org/program (accessed May 17, 2011).
cess is actually working by how well their patients are having these effects managed. That kind of information should then be publicly available,” he said. Dr. Wagner added that “the absence of widespread quality measurement contributes to a relative dearth of quality improvement activity.”
Some insurance companies are trying to address shortcomings in patient-centered care by contacting their participants directly. Dr. Smith reported that Aetna’s Compassionate Care Program has computer programs that recognize when someone is being treated for terminal cancer. These patients are flagged to receive calls from nurses trained in palliative care. In those phone calls, patients are offered visits from representatives from hospice and palliative care programs. Few patients denied these visits, and the program led to a doubling in the amount of time patients received hospice care. The program dramatically reduced the number of inpatient days from about 4,000 down to 1,500 and reduced the number of days patients spent in the intensive care unit (ICU) from about 10,000 to 1,100. This also resulted in a cost savings of about $32million per 1,000 members in inpatient costs and $30 million per 1,000 members in ICU costs. No changes were seen in how long the patients in the Compassionate Care Program lived compared to patients who were not in the program (Spettell et al., 2009).
Inpatient care is also being reduced by Rush University Medical Center’s enhanced discharge planning program, which is run by social workers, Dr. Clark reported. These social workers ask patients, after they have been discharged repeatedly from the hospital within a short period of time, whether they are able to acquire and afford their medicines and other questions aimed at assessing what might be interfering with the patients’ care. This program has reduced the number of patients being readmitted within 30 days, according to Dr. Clark.
She also pointed out that the Cancer Support Community offers professionally facilitated support groups and other programs and services to enable cancer patients and their families to manage their treatment and recovery as effectively as possible. One participant suggested creating survivorship advisory committees that can bring feedback and programmatic needs to the attention of hospitals and community practices.
Several participants pointed out that it will be challenging to implement, at the community practice level, model programs that work in
academic cancer centers. “The bottom line is that most people are not in academic medical centers. We need to come up with a way that works in reality and not in academic fantasyland,” said Mr. Boyajian. Innovative programs developed in small community care settings may also be difficult to scale up for large cancer centers, Dr. Smith noted.
Dr. Partridge reported on her experience with the ASCO Breast Cancer Registry Pilot. This pilot assessed the usefulness of an ASCO-developed template for breast cancer treatment plans in improving communication and care coordination and the feasibility of implementing it in the oncology ambulatory community practice. Practices were asked to enter data about their patients with breast cancer into a Web-based registry, which then generated in real time a treatment plan and summary. The computerized system also gave practice reports based on QOPI breast cancer measures of quality from the registry.
Practice staff or nurses entered data from more than 2,000 patients into the registry by the time the pilot was concluded in December 2010. Dr. Partridge’s survey of participants in the pilot found that 73 percent of practice respondents were satisfied with the registry, and 90 percent of those who had been involved in creating or communicating the treatment plans or summaries found them useful to improve communication between the medical oncologist and the patient. Among practitioners, 93 percent thought the registry had improved the quality of their practice, but 31 percent expressed concern about the amount of time required to accomplish at least one aspect of the pilot, and 52 percent indicated the practice incurred additional costs to meet the requirements of the registry.
Patient respondents also found the pilot beneficial, with 94 percent of those surveyed responding that it improved communication with their doctors and 82 percent reporting that it improved communication between the doctors on their treatment team. Although some people have expressed concern that the treatment plans and summaries might boost patients’ anxiety levels, 72 percent of the patients surveyed said it gave them greater peace of mind and only 1 percent said it gave them less peace of mind; 97 percent felt the breast cancer treatment plan and summary was useful, and 62 percent had given the form to another doctor, or planned to do so. All patients surveyed recommended that the practice continue to provide the cancer treatment plans and summaries to patients.
“The challenge now is dissemination and implementation of the breast cancer registry more widely, but first we need to figure out how to minimize the burden of it,” Dr. Partridge said. She added, “Projects like this that have a back door registry where we can provide feedback to practices in real time are a great opportunity for point-of-care quality improvement, improved care communication, and coordination and they also enable us to do health services research to learn about the quality of care.”
Survivorship Planning as a Model for Treatment Planning
Dr. Mayer reported on her study of implementing survivorship care planning for early-stage colon cancer patients funded by the Centers for Disease Control and Prevention. In this study, either the surgical or the medical oncology nurse practitioner delivers pre-prepared survivorship care plans to patients within six weeks of completing their cancer treatment. Dr. Mayer and her colleagues used five templates for the survivorship plan: three provided by Journey Forward, Lance Armstrong OncoLife, or the American Cancer Society; a version of the Journey Forward template tailored to North Carolina; and an abbreviated “Cliff Notes” version of the Journey Forward plan.
Survivor focus groups found that patients prefer the Journey Forward format, but many patients were confused about which practitioner to call when various health issues arise. One aspect the patients found lacking in the survivorship plans was how they can promote their health and nutrition. “When their treatment ends and patients perceive their safety net is gone, they want to know what they can do to promote their health, and nobody is addressing that as a concern or issue,” said Dr. Mayer. Most patients found the survivorship plan to be very helpful and said they would use it in discussions with their healthcare providers, family, and friends. As one patient who was interviewed pointed out, the survivorship plan “will tell you things you don’t remember, dates that you don’t remember.” Patients also saw the plan as a useful tool for “providers to talk to each other so they could all be on the same page,” Dr. Mayer said.
Dr. Mayer’s research team also completed focus groups with primary care providers in family practices or internal medicine. In these in-depth interviews, five such physicians described communication with their patients’ oncology teams based on what their prior relationship was with the providers (for example, whether they knew them from attending medical school, or whether they were part of the same electronic medical records system). If primary care providers said that they did not have an ongoing
relationship with the oncology providers or were not in the same electronic records system, doctors relied on their patients to fill them in on the care they received, which, as Dr. Mayer noted, “is a real burden for the patient.”
Primary care physicians preferred the scaled-down version of the Journey Forward template. “They wanted information about the diagnosis and a treatment overview summary that didn’t get into oncobabble, with numerous acronyms of genetic details, Dr. Mayer said. They also wanted to know what signs and symptoms could indicate recurrence or late side effects of treatment and what to do about them. They wanted resources and references as a single citation, link, or PDF they could put in a patient’s file, not a long laundry list of sources.
Dr. Mayer used this information to improve the Journey Forward survivorship care plan, which is now being distributed to colon cancer patients. So far, the research team has found that delivery of the care plans is not taking much longer than a normal surveillance visit after treatment, but the plans provide more structure to the visit and serve as reminders of what needs to be covered, which patients seem to appreciate, Dr. Mayer said. She is just starting to do the follow-up calls with participating providers and patients for a more formal evaluation of the plans.
Dr. Mayer is also providing breast cancer patients with a survivorship care plan during their transition or first survivorship visit. She documents how much time is spent delivering and explaining the survivorship care plan, what questions patients raise about it, and other information that will help evaluate the plan’s costs and benefits. She encouraged collecting and evaluating these data to assess the value of treatment plans for patients and whether they are worth the extra time they may take to complete and convey to patients.
Dr. Mayer concluded her presentation by listing the lessons learned from her evaluations of survivorship care plans. She stressed the need to get buy-in from all providers. “The teams I work with all think it is a great idea, they just don’t want to be the ones doing it,” she said. Automated reminders are also needed so that practitioners remember to create and deliver the care plan, as well as an ability to tailor templates to better meet the needs of particular patients. “We need to have menus to personalize the templates,” Dr. Mayer said, so they include local resources and are well suited to patients’ reading levels and desire for information. “We should speak plain English and not use our oncospeak as we develop these kinds of things. Patients don’t understand medical lingo, and a lot of primary care providers [are also unfamiliar with oncology terminology],” she said.
Dr. Mayer added that until information technology issues such as privacy and compatibility are addressed, the creation of survivorship care plans will require a laborious effort. “We need to take advantage of the health information technology efforts that are going on in healthcare reform now to create these interfaces that will make doing these things a bit easier,” she said. To ensure the value of survivorship care plans before they are fully implemented, Dr. Mayer suggested identifying and measuring outcomes when the plans are put into practice. “While this is not an evidence-based intervention currently, there is no reason why it can’t be over time,” she said.
POLICY OPTIONS TO PROMOTE PATIENT-CENTERED CANCER TREATMENT PLANNING
Participants suggested several policy options to promote patient-centered cancer treatment planning, including standards for training, licensure, and practice of providers, financial incentives, research, and healthcare reform.
Standards for Training, Licensure, and Practice
Several speakers suggested setting standards of care for oncology that include patient-centered treatment planning and communication, and making these standards part of physician training and licensure. Mr. Boyajian also suggested that standard cancer treatment plan templates be developed on a national level and made freely available to institutions and practices.
Dr. Ganz suggested that one standard of care for the initial cancer treatment planning process should be for a multidisciplinary team that uses the best available evidence. The treatment planning process should include the patient and family in decision making, encourage second opinions to validate the initial provider’s recommendations and diagnosis, and organize treatment decisions with a written treatment plan that is communicated to all parties, she added.
Dr. Bakitas suggested developing cancer treatment planning guidelines that make oncology nurse education sessions about cancer treatment explicit and mandatory. Attending to patients’ psychosocial concerns should also be made a standard of patient-centered care, and there should be policies, funding, and training that supports this, stressed Drs. Clark, Partridge, and Hoverman and Ms. Esparza. Currently social workers are not reimbursed for many of their services to cancer patients, Dr. Smith pointed out.
Mr. Gorman added that viewing good physician communication with patients as a skill that can be learned, rather than a trait that is inherited, has led some state medical licensing boards to start to require adequate physician communication in their certification process, especially for internal medicine and its subspecialties.
Financial incentives are also needed to spur implementation of patient-centered cancer treatment planning, according Dr. Ganz. As Dr. Keating noted, “The visit-based reimbursement system that we have in health care doesn’t help us at all because doctors’ schedules are packed, and they don’t have a lot of time.”
Dr. Ganz suggested that insurers could incentivize patient-centered care by reimbursing physicians only if they provide the documentation that is involved in creating a patient-centered cancer treatment plan. As she pointed out, insurers already require documentation on a number of items for reimbursement. Dr. Shulman added that one of Massachusetts Blue Cross’s pay-for-performance metrics is the creation of treatment plans. The reasoning for this, he said, is that encouraging more documentation of care can ensure that proper care is being given (for example, obtaining KRAS11 status before administering cetuximab to colon cancer patients). The documentation also enables insurers to be proactive, such as providing nurse navigators when needed to reduce emergency room visits and hospital stays.
In an initiative led by the NCCS, patient advocates have lobbied for legislation that would require the Centers for Medicare and Medicaid Services (CMS) to cover cancer care planning as part of its Medicare program, Ms. Elizabeth Goss, partner at Turner & Goss, LLP, reported. She said there were plans to reintroduce the legislation, called the Comprehensive Cancer Care Improvement Act, to Congress again in 2011. Mr. Erwin also suggested that CMS could pay for a patient-centered care program as part of its coverage with evidence development program.12
________________________
11Kirsten ras, a type of oncogene in which activating mutations play a key role in the progression of some cancers, such as colon cancer.
12On July 12, 2006, CMS released a guidance document titled National Coverage Determinations with Data Collection as a Condition of Coverage: Coverage with Evidence Development (CED); see https://www.cms.gov/CoverageGenInfo/03_CED.asp (accessed May 12, 2011).
Many participants said that an integral component to providing more patient-centered cancer treatment planning is the collection of more data on patient-centered outcomes such as how various cancer treatments affect patients’ quality of life and daily functioning. “If we are going to have good decisions, we have to have good evidence,” said Dr. Sharon Murphy. Dr. Mayer added, “We need to create the evidence as we go along and think about the evidence we want to collect.” Dr. Greenfield also stressed the need to do more comparative effectiveness research to provide information that patients and their doctors need when deciding on the most appropriate care.
To facilitate patient-centered care, AHRQ has conducted surveys through the Consumer Assessment of Healthcare Providers and Systems (CAHPS) program. These surveys are designed to bring the patient’s voice into assessments of healthcare quality and the results will be used for quality improvement and consumer choice. AHRQ is currently working with the NCI to develop a cancer-focused CAHPS, Dr. Clancy said. The agency also conducts research aimed at addressing questions that are particularly important to cancer patients, such as what the long-term consequences of various cancer treatment options are.
Dr. Claire Snyder, associate professor of medicine at Johns Hopkins University, pointed out the usefulness of the Patient Reported Outcomes Measurement Information System (PROMIS) developed by the National Institutes of Health (NIH). This system is designed to collect a wide array of outcomes, not just those relevant to cancer, and provides short forms as well as computer-adaptive tests to ensure that the questions asked are relevant to the patients in a specific population. It also enables comparisons across studies. She added that cancer patients can log on and enter information about their quality of life at patientviewpoint.org, which is then fed into the patients’ electronic medical record. Dr. Glasgow noted that PROMIS could also advance performance measurement by creating a common core set of patient reported measures that can be widely used in patient care.
Other tools are also available to measure patients’ quality of life, including the Memorial Symptom Assessment Scale, Dr. Mayer reported, as well as the PACIC (Patient Assessment of Chronic Illness Care) that was developed by Dr. Glasgow and measures patient experiences with a chronic disease. Dr. John Ayanian developed a survey instrument based on
the Picker patient-centered principles,13 Dr. Wagner reported, and he has found it useful in measuring problems that patients are experiencing in their cancer care. Dr. Wagner cautioned against using generic patient satisfaction surveys because he said they lull providers and organizations into thinking they are measuring patient experience when they are not doing so effectively. Dr. Smith also stressed the need to verify patient-reported outcomes, because some may be based on false hopes or other misconceptions of what can be achieved with treatment.
Supporting the endeavor to conduct research whose findings will aid cancer treatment planning are the millions of dollars AHRQ recently received via the American Recovery and Reinvestment Act of 2009 to support patient-centered outcomes research, as well as the establishment of the Patient-Centered Outcomes Research Institute (PCORI), which was called for in the Patient Protection and Affordable Care Act of 2010. This institute is supported by federal funds, including taxes on insurers that will amount to about $600 million a year, Dr. Clancy reported. PCORI is governed by stakeholders and has a 21-member board that includes the directors of AHRQ and NIH, industry representatives, clinicians, insurers, and consumers. She said that PCORI will be unique in giving researchers the capacity to do long-term follow-up of cancer patients and to acquire patients’ perspectives on the care they received and how it affected them. “The only way you can find out if care is patient-centered is to ask the patients themselves. Clinical aspirations to get to patient-centered care aren’t enough. We are going to need to get there by constantly checking to see how we’re doing,” Dr. Clancy said.
Several participants suggested policies to enhance systematic healthcare reform that promotes patient-centered cancer treatment, including more accountable care organizations that coordinate care under a single institution and have quality metrics and incentives to ensure that patient-centered care is being provided. Dr. Wagner noted that “cancer patients need a clinical home that takes responsibility and is accountable for the quality of care through all the handoffs.” Dr. Wagner emphasized this need in his figure of the chronic care model, adapted specifically for oncology (Figure 3).
Dr. Hoverman added that such model cancer treatment centers will
________________________
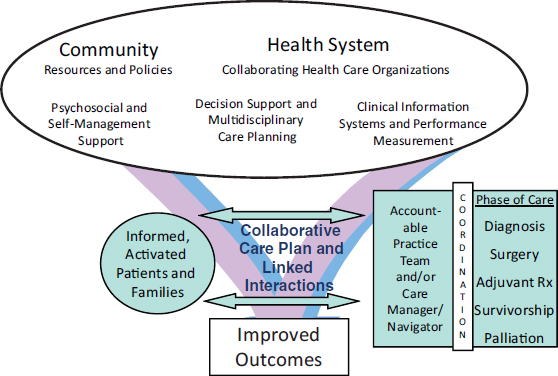
FIGURE 3 The model of quality cancer care developed by Dr. Ed Wagner emphasizes the need for an accountable practice team or navigator to ensure that cancer care is coordinated among the different phases and modalities of care. SOURCE: Wagner presentation (March 1, 2011). Reprinted, with permission, from Ed Wagner.
work only if they can be shown to save money, and he encouraged an exploration of how resources can be redirected within the healthcare system. Dr. Ganz suggested addressing the inefficiency and waste in the current healthcare system and said that the resources saved in this effort could be put to use providing better, more comprehensive, and more coordinated care to patients. Dr. Smith noted that abundant resources can be saved by providing cancer patients with appropriate end-of-life care. Mr. Smith suggested involving health economists in healthcare reform efforts and conducting studies that address the financial concerns of the Congressional Budget Office.
Other powerful tools for change are videos of patients telling their own stories, several participants suggested. Mr. Erwin added, “You ultimately have to have the facts to have good legislation, but if you don’t have the story and the emotion and the sound bite, the facts themselves don’t sell very easily.” He noted that having people convey their personal experiences with breast cancer was instrumental in getting state cigarette taxes allocated to breast cancer research in California. Ms. Smith added that “engaging
patients in solving the barriers is really important,” and Mr. Gorman suggested that patients be taught advocacy skills so they can tell their stories powerfully and succinctly.
According to many workshop speakers, cancer patients often are not receiving patient-centered cancer treatment planning, and many speakers suggested that there needs to be more promotion of such planning via accreditation standards, guidelines, financial incentives, training, and policy. Speakers also suggested that research on patient-centered cancer treatment outcomes and the value of cancer treatment plans is needed. However, several people also pleaded to avoid letting “the great be the enemy of the good” but rather to take concrete steps now, based on existing knowledge and evidence, to foster patient-centered cancer treatment planning. “We have enough trends to show that this is going in a very positive direction,” noted Ms. Esparza. “Don’t use evidence-based practice as an excuse not to do anything.” Mr. Boyajian added, “Develop some consensus, go forward from that, and look for the evidence afterwards. I don’t want to be a patient that is left behind while you are waiting for the gold standard. I want you to give us your best guess, and we’ll start looking at that.”
ACS (American Cancer Society). 2010. Cancer facts and figures 2010. Atlanta, GA: American Cancer Society.
Alexander, S. C., A. M. Sullivan, A. L. Back, J. A. Tulsky, R. E. Goldman, S. D. Block, S. K. Stewart, M. Wilson-Genderson, and S. L. Lee. 2011. Information giving and receiving in hematological malignancy consultations. Psycho-Oncology 20(5):10.
ASCO (American Society of Clinical Oncology). 2011. Advanced care planning. http://www.cancercarolinas.com/default/assets/File/Advanced_Cancer_Care_Planning.pdf (accessed May 12, 2011).
Ayanian, J. Z., A. M. Zalavsky, E. Guadagnoli, C. S. Fuchs, K. J. Yost, C. M. Creech, R. D. Cress, L. C. O’Connor, D. W. West, and W. E. Wright. 2005. Patients’ perceptions of quality care for colorectal cancer by race, ethnicity, and language. Journal of Clinical Oncology 23(27):6576-6586.
Bakitas, M., K. D. Lyons, M. T. Hegel, S. Balan, F. C. Brokaw, J. Seville, J. G. Hull, Z. Li, T. D. Tosteson, I. R. Byock, and T. A. Ahles. 2009. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized controlled trial. Journal of the American Medical Association302(7):741-749.
Bayard, J. M., C. Calianno, and C. L. Mee. 1997. Care coordinator-blending roles to improve patient outcomes. Nursing Management 28(8):49-51.
Belkora, J. K., A. Teng, S. Volz, M. K. Loth, and L. J. Esserman. 2011. Expanding the reach of decision and communication aids in a breast care center: A quality improvement study. Patient Education and Counseling 83(2):234-239.
Berry, D. L., B. A. Blumenstein, B. Halpenny, S. Wolpin, J. R. Fann, M. Austin-Seymour, N. Bush, B. T. Karras, W. B. Lober, and R. McCorkle. 2011. Enhancing patient-provider communication with the electronic self-report assessment for cancer: A randomized trial. Journal of Clinical Oncology 29(8):1029-1035.
Blayney, D. W., K. McNiff, D. Hanauer, G. Meila, D. Markstrom, and M. Neuss. 2009. Implementation of the Quality Oncology Practice Initiative at a university comprehensive cancer center. Journal of Clinical Oncology 27(23):3802-3807.
C-Change. 2005. Cancer patient navigation. http://www.cancerpatientnavigation.org/resources.html (accessed April 24, 2011).
Chung, H. M., L. Lyckholm, and T. J. Smith. 2009. Palliative care in BMT. Bone Marrow Transplantation 43(4):265-273.
Clayton, J. M., P. N. Butow, M. H. Tattersall, R. J. Devine, J. M. Simpson, G. Aggarwal, K. J. Clark, D. C. Currow, L. M. Elliott, J. Lacey, P. G. Lee, and M. A. Noel. 2007. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. Journal of Clinical Oncology 25(6):715-723.
Collins, E. D., C. P. Moore, K. F. Clay, S. A. Kearing, A. M. O’Connor, H. A. Llewellyn-Thomas, R. J. Barth, Jr., and K. R. Sepucha. 2009. Can women with early-stage breast cancer make an informed decision for mastectomy? Journal of Clinical Oncology 27(4):519-525.
Connor, S. R. 2007. U.S. hospice benefits. Journal of Pain Symptom Management 33(3):238-246.
De Raad, J., K. van Gool, M. Haas, P. Haywood, M. Faedo, G. Gallego, S. Pearson, and R. Ward. 2010. Nursing takes time: Workload associated with administering cancer protocols. Clinical Journal of Oncology Nursing 14(6):735-741.
Del Giudice, M. E., E. Grunfeld, B. J. Harvey, E. Piliotis, and S. Verma. 2009. Primary care physicians’ views of routine follow-up care of cancer survivors. Journal of Clinical Oncology 10;27(20):3338-3345.
Dow, L., L. Kuhn, V. Vramakrishnan, R. Matsuyama, E. Lamont, and T. J. Smith. 2010. Paradoxes in advance care planning: The complex relationship of oncology patients, their physicians, and advance medical directives. Journal of Clinical Oncology 28(2):299-304.
Eggly, S., L. A. Penner, M. Greene, F. W. K. Harper, J. C. Ruckdeschel, and T. L. Albrecht. 2006. Information seeking during “bad news” oncology interactions: Question asking by patients and their companions. Social Science & Medicine 63(11):2974-2985.
El-Jawahr, A., L. M. Podgurski, A. F. Eichler, S. R. Plotkin, J. S. Temel, S. L. Mitchell, Y. Chang, M. J. Barry, and A. E. Volandes. 2010. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. Journal of Clinical Oncology 28(2):301-310.
Epstein, R. M., and R. L. Street, Jr. 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute.
Fagerlin, A., I. Lakhani, P. M. Lantz, N. K. Janz, M. Morrow, K. Schwartz, D. Deapen, B. Salem, L. Liu, and S. J. Katz. 2006. An informed decision? Breast cancer patients and their knowledge about treatment. Patient Education and Counseling 64(1-3):303-312.
Gabram, S. G., M. J. Lund, J. Gardner, N. Hatchett, H. L. Bumpers, J. Okoli, M Rizzo, B. J. Johnson, G. B. Kirkpatrick, and O.W. Brawley. 2008. Effects of an outreach and internal navigation program on breast cancer diagnosis in an urban cancer center with a large African-American population. Cancer 113(3):602-607.
Gallup. 2010. Nurses top honesty and ethics for 11th year. http://www.gallup.com/poll/145043/Nurses-Top-Honesty-Ethics-List-11-Year.aspx (accessed April 24, 2011).
Ganti, A. K., S. J. Lee, J. M. Vose, M. P. Devetten, R. G. Bociek, J. O. Armitage, P. J. Bierman, L. J. Maness, E. C. Reed, and F. R. Loberiza, Jr. 2007. Outcomes after hematopoietic stem-cell transplantation for hematologic malignancies in patients with or without advance care planning. Journal of Clinical Oncology 25(35):5643-5648.
Gittell, J. H., K. M. Fairfield, B. Bierbaum, W. Head, R. Jackson, M. Kelly, R. Laskin, S. Lipson, J. Siliski, T. Thornhill, and J. Zuckerman. 2000. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: A nine-hospital study of surgical patients. Medical Care 38(8):807-819.
Given, C. W., A. Sikorskii, D. Tamkus, B. Given, M. You, R. McCorkle, V. Champion, and D. Decker. 2008. Managing symptoms among patients with breast cancer during chemotherapy: Results of a two-arm behavioral trial. Journal of Clinical Oncology 26(36):5855-5862.
Greenfield S., S. H. Kaplan, J. E. Ware Jr., E. M. Yano, H. J. Frank. 1988. Patients’ participation in medical care: Effects on blood sugar control and quality of life in diabetes. Journal of General Internal Medicine 3(5):448-457.
Heiman, H., D. W. Bates, D. Fairchild, S. Shaykevich, and L. S. Lehmann. 2004. Improving completion of advance directives in the primary care setting: A randomized controlled trial. American Journal of Medicine 117(5):318-324.
Huskamp, H. A., N. L. Keating, J. L. Malin, A. M. Zaslavsky, J. C. Weeks, C. C. Earle, J. M. Teno, B. A. Virnig, K. L. Kahn, Y. He, and J. Z. Ayanian. 2009. Discussions with physicians about hospice among patients with metastatic lung cancer. Archives of Internal Medicine 169(10):954-962.
IOM (Institute of Medicine). 1999. Ensuring quality cancer care. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century.Washington, DC: National Academy Press.
IOM. 2008. Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press.
IOM. 2010. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
Keating, N. L., E. Guadagnoli, M. B. Landrum, C. Borbas, and J. C. Weeks. 2002. Treatment decision making in early-stage breast cancer: Should surgeons match patients’ desired level of involvement? Journal of Clinical Oncology 20(6):1473-1479.
Keating, N. L., J. C. Weeks, C. Borbas, and E. Guadagnoli. 2003. Treatment of early stage breast cancer: Do surgeons and patients agree regarding whether treatment alternatives were discussed? Breast Cancer Research and Treatment 79(2):225-231.
Keating, N. L., M. B. Landrum, N. K. Arora, J. L. Malin, P. A. Ganz, M. van Ryn, and J. C. Weeks. 2010a. Cancer patients’ roles in treatment decisions: Do characteristics of the decision influence roles? Journal of Clinical Oncology 28(28):4364-4370.
Keating, N. L., M. B. Landrum, S. O. Rogers, Jr., S. K. Baum, B. A. Virnig, H. A. Huskamp, C. C. Earle, and K. L. Kahn. 2010b. Physician factors associated with discussions about end-of-life care. Cancer 116(4):998-1006.
Koutsopoulous, S., E. D. Papthanassoglou, M. C. Katapodi, and E. I. Patiraki. 2010. A critical review of the evidence for nurses as information providers to cancer patients. Journal of Clinical Nursing 19(5-6):749-765.
Lasser, K. E., J. Murillo, E. Medlin , S. Lisboa, L. Valley-Shah, R. H. Fletcher, K. M. Emmons, and J. Z. Ayanian. 2009. A multilevel intervention to promote colorectal cancer screening among community health center patients: Results of a pilot study. BMC Family Practice, 2009 May 29;10:37.
Lee, C., J. K. Belkora, Y. Chang, C. Cosenza, C. A. Levin, B. Moy, A. Partridge, and K. R. Sepucha. 2009a. The quality of decisions about breast cancer surgery. Presented at the 31st Annual Meeting of the Society for Medical Decision Making, October 2009, Hollywood, CA.
Lee, C., J. Belkora, M. Wetschler, Y. Chang, S. Feibelmann, B. Moy, A. Partridge, and K. Sepucha. 2009b. The quality of decisions about adjuvant chemotherapy for early stage breast cancer. Presented at the San Antonio Breast Cancer Symposium, December 2009, San Antonio, TX.
Lee, C. N., R. Dominik, C. A. Levin, M.J. Barry, C. Cosenza, A. M. O’Connor, A. G. Mulley Jr., K. R. Sepucha. 2010. Development of instruments to measure the quality of breast cancer treatment decisions. Health Expectations (3):258-72.
Matsuyama, R., S. Reddy, and T. J. Smith. 2006. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. Journal of Clinical Oncology 24(21):3490-3496.
McCorkle, R., N. E. Strumpf, I. F. Nuamah, D. C. Adler, M. E. Cooley, C. Jepson, E. J. Lusk, and M. Torosian. 2000. A specialized home care intervention improves survival among older post-surgical cancer patients. Journal of the American Geriatric Society 48(12):1701-1713.
Morrow, M., M. Mujahid, P. M. Lantz, N. K. Janz, A. Fagerlin, K. Schwartz, L. Liu, D. Deapen, B. Salem, I. Lakhani, and S. J. Katz. 2005. Correlates of breast reconstruction: Results from a population-based study. Cancer 104(11):2340-2346.
NCCN (National Comprehensive Cancer Network). 2005. Practice guidelines in oncology. Palliative care. Pittsburgh, PA: National Comprehensive Cancer Network.
NCCS (National Coalition for Cancer Survivorship). 1996. Imperatives for quality cancer care: Access, advocacy, action, and accountability. Washington, DC: National Coalition for Cancer Survivorship.
Northouse, L. L., M. C. Katapodi, L. Song, L. Zhang, and D. W. Mood. 2010. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians 60(5):317-339.
Oluwole, S. F., A. O. Ali, A. Adu, B. P. Blane, B. Barlow, R. Oropeza, and H. P. Freeman 2003. Impact of a cancer screening program on breast cancer stage at diagnosis in a medically underserved urban community. Journal of the American College Surgery. 196(2):180-188.
Panagopoulou, E., G. Mintziori, A. Montgomery, D. Kapoukranidou, and A. Benos. 2008. Concealment of information in clinical practice: Is lying less stressful than telling the truth? Journal of Clinical Oncology 26(7):1175-1177.
Peppercorn, J. M., T. J. Smith, P. R. Helft, D. J. DeBono, S. R. Berry, D. S. Wollins, D. M. Hayes, J. H. von Roenn, and L. E. Schnipper. 2011. American Society of Clinical Oncology statement: Toward individualized care for patients with advanced cancer. Journal of Clinical Oncology 29(6):755-760.
Pollak, K. I., R. M. Arnold, A. S. Jeffreys, S. C. Alexander, M. K. Olsen, A. P. Abernethy, C. Sugg Skinner, K. L. Rodriguez, and J. A. Tulsky. 2007. Oncologist communication about emotion during visits with patients with advanced cancer. Journal of Clinical Oncology 25(36):5748-5752.
Rakovitch, E., E. Franssen, J. Kim, I. Ackerman, J. P. Pignol, L. Paszat, K. I. Pritchard, C. Ho, and D. A. Redelmeier. 2003. A comparison of risk perception and psychological morbidity in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Research and Treatment 77(3):285-293.
Ravdin, P. M., I. A. Siminoff, and J. A. Harvey. 1998. Survey of breast cancer patients concerning their knowledge and expectations of adjuvant therapy. Journal of Clinical Oncology 16(2):515-521.
Sheridan, S. L., R. P. Harris, and S. H. Woolf. 2004. Shared decision making about screening and chemoprevention: A suggested approach from the U.S. Preventive Services Task Force. American Journal of Preventive Medicine 26(1):56-66.
Skalla, K. A., M. Bakitas, C. T. Furstenberg, T. Ahles, and J. V. Henderson. 2004. Patients’ need for information about cancer therapy. Oncology Nursing Forum 31(2):313-319.
Smith, T. J., L. A. Dow, E. Virago, J. Khatcheressian, L. Lyckholm, and R. Matsuyama. 2010. Giving honest information to patients with advanced cancer maintains hope. Oncology 24(6):521-525.
Smith, T. J., L. A. Dow, E. A. Virago, J. Khatcheressian, R. Matsuyama, and L. J. Lyckholm. 2011. A pilot trial of decision aids to give truthful prognostic and treatment information to chemotherapy patients with advanced cancer. Journal of Supportive Oncology 9(2): 79-86.
Spettell, C. M., W. S. Rawlins, R. Krakauer, J. Fernandes, M. E. Breton, W. Gowdy, S. Brodeur, M. MacCoy, and T. A. Brennan. 2009. A comprehensive case management program to improve palliative care. Journal of Palliative Medicine 12(9):827-832.
Stille, C. J., A. Jerant, D. Bell, D. Meltzer, and J. G. Elmore. 2005. Coordinating care across diseases, settings, and clinicians: A key role for the generalist in practice. Annals of Internal Medicine 142(8):700-708.
Tariman, J. D., D. L. Berry, B. Cochrane, A. Doorenbos, and K. Schepp. 2010. Preferred and actual participation roles during health care decision making in persons with cancer: A systematic review. Annals of Oncology 21(6):1145-1151.
Temel, J. S., J. A. Greer, A. Muzikansky, E. R. Gallagher, S. Admane, V. A. Jackson, C. M. Dahlin, C. D. Blinderman, J. Jacobsen, W. F. Pirl, J. A. Billings, and T. J. Lynch. 2010. Early palliative care for patients with metastatic nonsmall-cell lung cancer. New England Journal of Medicine 363(8):733-742.
Venetis, M. K., J. D. Robinson, K. L. Turkiewiczc, and M. Allen. 2009. An evidence base for patient-centered cancer care: A meta-analysis of studies of observed communication between cancer specialists and their patients. Patient Education and Counseling 77(3):379-383.
Weeks, J. C., E. F. Cook, S. J. O’Day, L. M. Peterson, N. Wenger, D. Reding, F. E. Harrell, P. Kussin, N. V. Dawson, A. F. Connors, Jr., J. Lynn, and R. S. Phillips. 1998. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. Journal of the American Medical Association 279(21):1709-1714.
Wright, A. A., B. Zhang, A. Ray, J. W. Mack, E. Trice, T. Balboni, S. L. Mitchell, V. A. Jackson, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2008. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Journal of the American Medical Association300(14):1665-1667.
Zhang, B., A. A. Wright, H. A. Huskamp, M. E. Nilsson, M. L. Maciejewski, C. C. Earle, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2009. Health care costs in the last week of life: Associations with end-of-life conversations. Archives of Internal Medicine 169(5): 480-488.


























































