The Persistence of Chronic Diseases
Chronic diseases are among the most common of all health problems in the United States. They cause about 70 percent of deaths and account for an estimated 75 percent of healthcare costs each year. Although they are more common among older adults, chronic diseases affect people of all ages.
Even as they are so damaging to health, chronic diseases often are among the most preventable health problems. But in many cases, prevention has proved difficult. Effective steps often require fundamental changes in people’s lifestyles and behaviors. Structural factors across society, including within government and the health system, also create barriers. Facing such obstacles, the federal government and various private organizations frequently call on the Institute of Medicine (IOM) for advice on how to better understand and manage a range of chronic diseases.
Combating cardiovascular disorders
Hypertension is one of the nation’s most common chronic conditions—and one of the most vexing. Nearly one-third of adults have hypertension, more commonly known as high blood pressure. Chronic hypertension is a key risk factor for stroke, heart attack, and heart failure, among other health problems, and it accounts for about one in six adult deaths annually. Yet hypertension is relatively easy to prevent, simple to diagnose, and inexpensive to treat.
To help guide nationwide efforts to reduce the impact of hypertension, the Centers for Disease Control and Prevention (CDC), through its
Division for Heart Disease and Stroke Prevention (DHDSP), developed a strategic plan that identified a broad array of action areas and goals. At the CDC’s request, the IOM convened an expert committee to assess the plan and identify a smaller set of high-priority areas on which the DHDSP and other public and private groups should focus in the near term.
Nearly one-third of adults have hypertension, more commonly known as high blood pressure. Chronic hypertension is a key risk factor for stroke, heart attack, and heart failure, among other health problems, and it accounts for about one in six adult deaths annually.
In A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension (2010), the committee reports that in today’s era of tightening budgets, the DHDSP should shift the balance of its hypertension efforts from healthcare interventions directed at individuals to population-based strategies and systems approaches that can reach large numbers of people and improve the well-being of entire communities—at the lowest possible costs. This shift should extend as well to state and local health departments and to various other organizations and providers across the health enterprise.
Under this operational umbrella, the DHDSP should collaborate with state and local public health jurisdictions on a variety of behavioral and lifestyle interventions that target risk factors known to contribute substantially to hypertension. These risk factors include eating an unhealthful diet, consuming too much salt and too little potassium, being overweight or obese, and engaging in too little physical activity. Public health jurisdictions should integrate hypertension prevention and control interventions into their policies and programs in ways that will support healthy eating, active living, and obesity prevention across their respective communities. Jurisdictions also should align their efforts with populations most likely to be affected by hypertension, such as older populations, which often are not the target of these programs.
It also will be necessary to improve how physicians serve their patients. Today, many physicians do not provide treatment for hypertension that is consistent with generally accepted practice guidelines. The DHDSP should conduct research to understand the reasons behind their poor performance, and then lead in developing strategies to increase the likelihood that primary providers will screen for and treat hypertension appropriately.
| Prevalence of Hypertension (averaged measures), Overweight, Obesity, and Average Intake of Dietary Sodium per 1,000 Adults, 1960-2006 | ||||||||
| 1960-1962 | 1971-1974 | 1976-1980 | 1988-1994 | 1999-2000 | 1999-2002 | 2001-2004 | 2003-2006 | |
| Hypertension | 38.1* | 39.8* | 40.4* | 25.5 | 32.8 | 30.0 | 30.9 | 31.3 |
| Overweighta | 44.8* | 44.7* | 47.4* | 56.0 | 64.5 | 65.1 | 66.0 | 66.7 |
| Obesity | 13.3* | 14.3* | 15.1* | 22.9 | 30.5 | 30.4 | 31.4 | 33.4 |
| Sodium (mg/day)b | 2,200* | 2,900* | 3,600* | 3,500* | ||||
a Includes obesity.
b Sodium intake estimates are based on the average of salt intake from 24-hour recalls for men and women from NHANES data. Data from NHANES 1971-1974 include naturally occurring sodium in foods and that added by processors. Data for NHANES 1999-2000 includes naturally occurring sodium in foods and that added by processors and discretionary salt usage.
* For ages 20-74, other data for ages 20 and over.
SOURCES: Briefel and Johnson, 2004; NCHS, 2003, 2009, 2010.
SOURCE: A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension, p. 69.
To effectively carry out current and recommended programs, the DHDSP will need additional federal support. The hypertension program is underfunded, relative to the preventable burden of hypertension. In today’s climate of healthcare reform and the increasing attention being directed to prevention, there is no better time to rise to the challenge. The committee therefore calls on Congress to provide the DHDSP with adequate resources for implementing a broad suite of population-based policy and system approaches at the federal, state, and local levels that have the greatest promise to prevent, treat, and control hypertension.
One important—and widespread—risk factor for cardiovascular disorders is smoking. There also is evidence that exposure to secondhand smoke—that is, smoke from burning cigarettes, cigars, and pipe tobacco, as well as smoke exhaled by smokers—can be damaging to nonsmokers. At the CDC’s request, the IOM convened a committee to assess the evidence on the relationship between exposure to secondhand smoke and effects on the heart, as well as the evidence on how smoking bans affect rates of heart attacks.
In Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence (2009), the committee reports that the bulk of studies
supports the current consensus that exposure to secondhand smoke increases the risk of coronary heart disease among both men and women. The evidence is not sufficient, however, for determining the precise magnitude of the increased risk—that is, the number of cases of disease that are attributable to secondhand-smoke exposure.
The committee also finds that numerous studies support an association between smoking bans and a decrease in the incidence of heart attacks, with observed decreases ranging from 6 percent to 47 percent. However, none of the studies included information on how long or how often individuals were exposed to secondhand smoke before or after implementa-
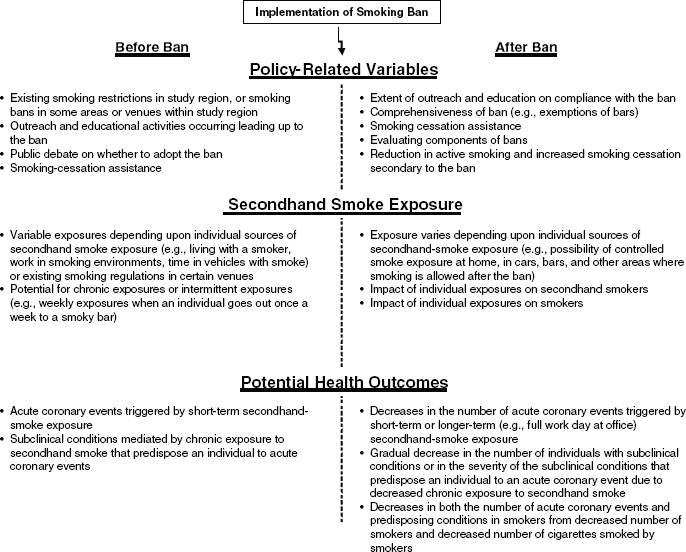
NOTE: Factors that can affect the impact of smoking bans on cardiovascular outcomes. A number of policy-related variables can differ among locations and affect the impact of a smoking ban. The concentration of secondhand smoke can also differ among locations both before and after a ban is implemented. Outcome-related factors can differ and affect study results.
SOURCE: Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence, p. 23.
tion of smoking bans. For example, it is not known whether individuals were exposed to high concentrations sporadically for short periods, to low concentrations more consistently, or both. Without this information, the committee could not determine whether heart attacks were triggered by acute exposures, whether they were the eventual result of chronic exposures that caused chronic damage, or both.
In light of current knowledge gaps, the committee calls for additional research and outlines priority needs. Studies on smoking bans, for example, should examine the time between an intervention and observed health effects, measure the magnitude of the effects, and take various social factors into account. They also should include direct observations on individuals—including their history of cardiac disease, exposure to other environmental chemicals, and other risk factors for cardiac events—to assess the impact of those factors on study results. Further, assessment of smoking status is needed to distinguish between the effects of secondhand smoke in nonsmokers and the effects of a ban that reduces cigarette consumption or supports smoking cessation in smokers.
The bulk of studies supports the current consensus that exposure to secondhand smoke increases the risk of coronary heart disease among both men and women.
In addition, the committee finds only sparse data on the prevalence and incidence of cardiovascular disease and heart attacks at the national level in general, compared with other health endpoints, such as cancer, for which there are central data registries and surveillance of all events. A large prospective cohort study could be very helpful in more accurately estimating the magnitude of the risk of cardiovascular disease and heart attacks posed by exposure to secondhand smoke.
Shaping a national HIV/AIDS plan
HIV/AIDS only recently joined the list of chronic diseases on the national stage. In the early decades of the epidemic, HIV infection was considered to be ultimately fatal. But new, advanced methods of care, including anti-
retroviral therapies, have transformed HIV/AIDS into a chronic—and manageable—condition that people can live with for many years. Ensuring that people know their HIV status and receive adequate care—starting early and continuing for life—can improve clinical outcomes, extend lives significantly, and reduce the transmission of HIV.
In July 2010, the White House Office of National AIDS Policy, which coordinates government efforts to stem the HIV epidemic, released its National HIV/AIDS Strategy. To help guide implementation, the office asked the IOM to appoint a committee to evaluate the extent to which federal, state, and private health insurance policies and practices pose barriers to expanding HIV testing and treatment; examine the current capacity of the healthcare system to administer more HIV tests and accommodate new HIV diagnoses; and identify options for overcoming existing barriers and ensuring adequate system care capacity.


Over the course of its study, the committee issued three reports:
1. HIV Screening and Access to Care: Exploring Barriers and Facilitators to Expanded HIV Testing (2010)
2. HIV Screening and Access to Care: Exploring the Impact of Policies on Access to and Provision of HIV Care (2011)
3. HIV Screening and Access to Care: Health Care System Capacity for Increased HIV Testing and Provision of Care (2011)
Among barriers to expanded HIV testing, the committee identified conflicting federal agency guidelines on who should be tested, low federal and private insurance reimbursement rates that can discourage providers from conducting tests, restrictive laws in some states on how HIV tests should be conducted and who can do the testing, and a widespread lack of programs to combat the stigma and discrimination that often is associated with HIV and that can discourage people from being tested.
Expanding programs to notify partners of HIV-positive individuals, linking HIV testing with other healthcare and social services, and mounting media and social network outreach efforts all could help to promote testing. Expanding the use of “rapid” HIV tests
may help as well. Unlike conventional tests that take days to yield results, rapid tests provide results immediately and thus may reduce the number of people who fail to receive their test results. Streamlining the administration of HIV tests also may make them easier to administer in busy clinics, and it may be possible to simplify and expand HIV testing in prisons and other correctional facilities, where HIV often is prevalent.
Among barriers to care, many patients lack access to a provider with expertise in treating HIV, or they cannot afford treatment, even with insurance. Problems also arise from the lack of integration of state and federal government programs meeting the complex needs of HIV-positive individuals and the intertwined medical and social problems often associated with HIV. Such fragmentation, coupled with multiple funding sources with different eligibility requirements, causes many individuals to shift in and out of eligibility for HIV care.
New, advanced methods of care, including antiretroviral therapies, have transformed HIV/AIDS into a chronic—and manageable—condition that people can live with for many years.
To overcome such barriers, strategies may include making eligibility criteria for public and private coverage consistent with the guidelines issued by HHS for initiating antiretroviral therapies, providing cost-sharing assistance for lower-income populations, imposing monthly and annual caps on a patient’s overall out-of-pocket expenses, ending the practice of denying coverage for failure to pay for services, and eliminating annual or lifetime coverage limits for treatment.
Developing and promoting coordinated care and integrated delivery systems also can help. Healthcare providers and public health officials will need to be increasingly flexible and willing to employ a variety of approaches to meet the needs of HIV-positive individuals, especially given the financial and capacity strains facing the healthcare system. Providers likely will need to collaborate on care of patients and often divide tasks among providers to the extent permitted by state regulations. Approaches to expanding HIV testing and treatment should take account of the setting in which they are being implemented, so as to fit as seamlessly as possible into the workflow.
As an underlying problem, the United States lacks enough providers skilled in HIV/AIDS care, as well as primary care providers more generally, to handle the number of people who need to be tested and treated. To meet
workforce demands, all health professionals, both during their training and through continuing education programs, should be exposed to outpatient HIV care. It also may be desirable to provide better financial and other incentives to encourage more health professionals to enter and remain in HIV care. There is a need as well to reach beyond the primary care physicians and infectious disease specialists who now provide most HIV care. Registered nurses, physician assistants, dentists, pharmacists, and social workers are among those who can help in providing quality HIV care in a variety of settings.
Viral hepatitis: A silent epidemic
Affecting even more people than HIV/AIDS, chronic viral hepatitis—hepatitis B and hepatitis C—causes significant health problems in the United States and is responsible for about 15,000 deaths each year. Yet because viral hepatitis typically causes few if any obvious symptoms, many people do not know they are infected until they develop liver cancer or liver disease many years later. Few among the populations most at risk—including immigrants from Asia and the Pacific islands, where hepatitis B is endemic, and their U.S.-born children, as well as injection-drug users—seek testing or information on how to protect themselves from infection.
Affecting even more people than HIV/AIDS, chronic viral hepatitis—hepatitis B and hepatitis C—causes significant health problems in the United States and is responsible for about 15,000 deaths each year.
With support from several government and private sponsors, including the CDC, the IOM convened a committee to assess current prevention and control activities for hepatitis B and C and identify ways to reduce new cases of infections and lower illnesses and deaths from them. In Hepatitis and Liver Cancer: A National Strategy for Prevention and Control of Hepatitis B and C (2010) the committee identified several priority action areas.
Steps are needed, for example, to develop and provide more comprehensive services for viral hepatitis. Services should have five core components: outreach and awareness, prevention of new
infections, identification of infected people, social and peer support, and medical management of chronically infected people. Stakeholders also should work together to better coordinate their services, which currently are sparse and fragmented among providers and organizations, leading to missed opportunities to prevent the spread of infection and lessen the impact of chronic infections.
New public awareness initiatives are needed along the lines of those that succeeded in increasing recognition, prevention, and treatment of HIV/AIDS. Toward this end, the CDC can work with stakeholders to develop and evaluate innovative hepatitis B and C educational programs for healthcare and social service providers, the general public, and specific populations at higher risk of contracting viral hepatitis.
Stepped-up vaccination efforts are needed for hepatitis B. (There is no vaccine for hepatitis C as yet.) All full-term newborns whose mothers test positive for hepatitis B should receive the vaccine before leaving the delivery room, rather than up to 12 hours after birth as is currently recommended.
| Burden of Selected Serious Chronic Viral Infections in the United States | ||||||
| Virus | Prevalencea,b | Percentage of Population Unaware of Infection Statusc,d,e | Deaths in 2006 Related to Infectiona,b | Vaccine-Preventable | Transmission Routes | Percentage of CDC NCHHSTP FY 2008 Budgetf |
| HBV | 0.8–1.4 million | About 65% | 3,000 | Yes | Birth, blood, sex | 2% combined |
| HCV | 2.7–3.9 million | About 75% | 12,000 | No | Birth, blood, sex | |
| HIV/ AIDS | 1.1 million | About 21% | 14,016 | No | Birth, blood, sex | 69% (domestic activities) |
Abbreviations: CDC NCHHSTP, Centers for Disease Control and Prevention National Center for HIV/AIDS, Viral Hepatitis, Sexually Transmitted Disease, and Tuberculosis Prevention; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV/AIDS, human immunodeficiency virus/acquired immunodeficiency syndrome.
SOURCES: aCDC, 2009b; bCDC, 2009d; cLin et al., 2007; dHagan et al., 2006; eCDC, 2008b; fWard, 2008a.
SOURCE: Hepatitis and Liver Cancer: A National Strategy for Prevention and Control of Hepatitis B and C, p. 26.
In addition, all states should make hepatitis B vaccination a requirement for school attendance, and health plans should fully cover the costs.
Improved surveillance of viral hepatitis is needed because current data do not provide accurate estimates of the disease burden and are insufficient for program planning and evaluation. Among recommended steps, the CDC should develop agreements with state and territorial health departments to support core surveillance for hepatitis B and C, along with targeted surveillance to monitor incidence and prevalence of the diseases in at-risk populations not fully captured by core surveillance.
The IOM’s report set off a cascade of responses. The CDC launched a new website—www.KnowHepatitis.org—to provide frontline community healthcare providers with current and accurate information, with a featured session focused on the report’s recommendations. In addition, HHS organized the Viral Hepatitis Interagency Working Group, which released a blueprint of priorities, called Combating the Silent Epidemic of Viral Hepatitis, for HHS agencies and other government and private partners. Announced in May 2011, the plan is organized by topics that map directly to the IOM recommendations. Finally, in his budget request to Congress for fiscal year 2012, President Obama recommended a $5.2 million increase for the prevention of viral hepatitis in the United States.
Evaluating biomarkers for use in foods
Statements about the healthfulness of foods are commonplace in the media and the marketplace; statements tout various health benefits, including reducing the risk of a variety of chronic diseases. It is well established that diet can raise or lower the risk of developing chronic diseases such as diabetes and heart disease, and food manufacturers want consumers to know when their foods may lower those risks.
It is well established that diet can raise or lower the risk of developing chronic diseases such as diabetes and heart disease, and food manufacturers want consumers to know when their foods may lower those risks.
The FDA regulates statements about health and nutrition on food labels. As part of this process, the FDA often must assess manufacturers’ data on how the food or ingredient affects so-called biomarkers, which are characteristics that indicate biological processes. For example, low-density lipoprotein (LDL) cholesterol level is a widely used biomarker in cardiovascular disease. Some bio-
markers, called surrogate endpoints, are used as substitutes for actual clinical outcomes, such as incidence of disease or death. Surrogate endpoints are intended to predict benefit or harm based on scientific evidence, and they are used in practice when it is difficult to collect data based on clinical endpoints.
As the gatekeeper for entry of foods, drugs, and many other products into the marketplace, the FDA examines data and makes decisions about whether biomarkers or surrogate endpoints can be used for regulatory reviews. In recent years, the FDA’s Center for Food Safety and Applied Nutrition found that it was reviewing significant numbers of applications for food health claims based on stated effects on biomarkers, and the FDA asked the IOM to convene a committee to study the evaluation process for biomarkers, focusing on biomarkers and surrogate endpoints in chronic disease.

In Evaluation of Biomarkers and Surrogate Endpoints in Chronic Disease (2010), the committee recommends that the FDA adopt a consistent framework for biomarker evaluation in order to achieve a rigorous and transparent process for all stakeholders. The proposed framework consists of three steps, involving validating the performance of the biomarker test (analytical validation), assessing the strength of the evidence supporting the link between the biomarker test and the disease (qualification), and considering the purposes for which they will be used (utilization). These steps often will be interrelated, and conclusions in one step may require revisions or additional work in other steps.
For biomarkers with regulatory impact, the IOM committee suggests the FDA go further, convening expert panels to evaluate biomarkers and biomarker tests. Initial evaluation of analytical validation and qualification should be conducted separately from a particular context of use. In addition, the expert panels should reevaluate analytical validation, qualification, and utilization on a continual and a case-by-case basis.
In its regulatory operations, the FDA should use the same degree of scientific rigor for evaluating biomarker use in foods and dietary supplements as it does across other regulatory areas, including drugs and medical devices. Currently, when the FDA reviews drugs, it considers the safety and efficacy of the entire product. But when the agency reviews foods, it con-
siders the safety of individual ingredients rather than the food as a whole. Despite the common perception that foods present fewer risks to consumers than drugs, foods and food ingredients may pose even greater risks because the reach of food is so vast. Even minor risks become clinically consequential when the majority of the population is exposed to them.
In pursuit of chronic disease
Chronic disease continues to be an area of interest for health experts and policy makers, particularly in light of budget constraints. In the spring of 2010, the IOM held a meeting to review the state of research and clinical practice associated with chronic disease illnesses such as cancer, brain tumors, sickle cell disease, epilepsy, diabetes, and congenital heart disease in children. An IOM report on one of the world’s most deadly chronic diseases, cardiovascular disease (CVD) was issued in March 2010. That report, Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health, discussed the worldwide threat, and it is discussed in more detail in the chapter on global health.
In a report sponsored by the CDC, HHS, and the Arthritis Foundation, the IOM is examining the burden of chronic disease. In its report, expected to be released in fall 2011, the IOM will recommend which chronic diseases should be the focus of public health efforts, which populations should be the focus of interventions, and which interventions can help achieve outcomes that maintain or improve quality of life, functioning, and disability.












