Improving Food Safety, Nutrition, and Health
The problems have grown all too familiar. Too many Americans are overweight or obese. Too many children do not eat healthy meals at school. Many people consume too much of some foods or nutrients, or too little of others. Information overload confounds some nutritional claims. The nation’s food supply, though generally safe, periodically suffers outbreaks of contamination that cause food-borne illnesses.
All told, the nation has considerable room for improvement in ensuring that the foods available to consumers are safe, that people eat enough of what they should to be healthy, and that they minimize or eliminate their intake of potentially harmful foods. To help meet these goals, the Institute of Medicine (IOM) regularly examines the nation’s nutritional well-being and offers measures for improvement.
Improving food programs
In February 2010, as part of the launch of Let’s Move!, First Lady Michelle Obama’s program to reduce childhood obesity, the secretary of the U.S. Department of Agriculture (USDA), Tom Vilsack, spoke of his department’s commitment to have all schools offer nutritious meals to their students. He said this stand is based in part on the IOM report School Meals: Building Blocks for Healthy Children (2010), which “sounded an alarm about the nutritional value of school meals,” and added that his department “is working as aggressively as possible” to build on the report’s findings. In 2011, the USDA issued new interim rules for its
school breakfast and lunch programs that incorporate many of the IOM’s recommendations.
In 2011, the USDA issued new interim rules for its school breakfast and lunch programs that incorporate many of the IOM’s recommendations.
The report referenced by the secretary was written at the request of the USDA. The agency asked the IOM to review the food and nutritional needs of school-aged children in the United States and offer guidance on updating the regulations, which had been established in 1995. The National School Lunch Program and the School Breakfast Program provide nutritionally balanced, low-cost or free meals each school day. The lunch program served more than 31 million children in 2009. In its report, the IOM offers recommendations that focus clearly on providing meals that are consistent with the Dietary Guidelines for Americans, the foundation of the government’s nutrition policies. The report calls on the USDA’s Food and Nutrition Service to adopt standards for menu planning that increase
Key Recommended Changes in School Lunch Requirements
| Type of Specification | Current Specification | Recommendations |
| Fruits | Considered together as a fruit and vegetable group. No specifications for the type of vegetable. | Required daily amount increased |
| Vegetables | Two servings required daily, amount increased. Must include dark green, bright orange, legumes, starchy, and other vegetables each week | |
| Grains/breads | No requirement for whole grains | At least half must be whole grain rich |
| Milk | Whole, reduced-fat, low-fat, fat-free milks (plain or flavored) | Fat-free (plain or flavored) and plain low-fat milk only |
| Calories | Must meet minimum level | Must be within minimum and maximum level |
| Sodium | None (decreased level recommended) | Gradually but markedly decrease sodium to the specified level by 2020 |
The committee recommends a single approach to menu planning—one that includes a meal pattern plus specifications for minimum and maximum calorie levels, maximum saturated fat content, and maximum sodium content.
SOURCE: School Meals: Building Blocks for Healthy Children.
the amount and variety of fruits, vegetables, and whole grains; set a minimum and maximum level of calories; and place greater focus on reducing the amounts of saturated fat and sodium provided. Other recommendations are intended to ensure not only that schools offer nutritious meals but that students select healthful foods from the menu.
The IOM report generated a response not just by government but also from the business community. In February 2010, several major food services companies that provide students with breakfasts and lunches at schools nationwide announced that they would meet the IOM’s recommended school meal standards for fat, sugar, and whole grains over the next 5 years, and meet the standards for sodium over the next 10 years. The companies—ARAMARK, Sodexo, and Chartwells—also agreed to include more fruit, vegetables, and low-fat and fat-free milk in their school meals. Specifically, they pledged to work to double the amount of produce offered over the next 10 years.
In another study of federal food and nutrition initiatives, the IOM examined USDA’s Child and Adult Care Food Program (CACFP), which supports the nutrition and health of the nation’s most vulnerable individuals—more than 3 million infants and children and more than 114,000 impaired or older adults, primarily from low-income households. To receive federal reimbursement, CACFP meals and snacks must meet regulations designed to ensure that participants receive high-quality, nutritious foods. But the current standards, called Meal Requirements, are based in part on nutrition and health information from 1989. For assistance in updating the program, the Food and Drug Administration (FDA) asked the IOM to review and assess the nutritional needs of the populations served by the CACFP and to provide recommendations to revise its Meal Requirements.
The IOM examined USDA’s Child and Adult Care Food Program, which supports the nutrition and health of the nation’s most vulnerable individuals—more than 3 million infants and children and more than 114,000 impaired or older adults, primarily from low-income households.
In Child and Adult Care Food Program: Aligning Dietary Guidance for All (2010), an IOM committee provided recommendations that cover all age groups and could be implemented by a variety of providers, including those in family homes and large centers. The recommendations are based on current dietary guidance, including the Dietary Guidelines for Ameri-
cans, and take into account such practical considerations as the need for appealing menus, the capabilities of the providers, and cost.
The recommendations target three age groups—infants, children, and adults 19 years and older. (The first two groups are broken down into several subgroups, based on age.) For each group, the committee recommended new Meal Requirements, including both revised daily and weekly meal patterns and additional food specifications. The meal patterns are the types and amounts of foods that are to be offered for breakfast, lunch/ supper, and snacks. The requirements will promote intakes of healthy foods from five food groups: fruits, vegetables, milk, grains/ bread, and lean meats or meat alternates, and seek consistency with the Dietary Guidelines for Americans.
Today, almost 10 percent of infants and toddlers carry excess weight for their length, and slightly more than 20 percent of children between the ages of 2 and 5 years are already overweight or obese.
The effectiveness of the Meal Requirements will be determined in large part by the manner in which they are implemented and monitored for compliance. Key implementation strategies should include engaging families, food industry stakeholders, and community members; providing nutritional education to participants; and training state agency staff and program providers. To aid in implementation, the committee recommended that the USDA offer extensive technical assistance to CACFP providers and work with stakeholders to develop an effective system for monitoring and reimbursing CACFP meals.
Combating the obesity epidemic
Improving school lunches and meals served by child care providers will be one tool in reducing obesity among Americans. The hope is that by learning and practicing good nutritional habits early, children can avoid becoming overweight or obese later in life. And these behaviors must begin among even the youngest of children. Because early obesity can track into adulthood, efforts to prevent obesity should begin long before a child enters school. Today, almost 10 percent of infants and toddlers carry excess weight for their length, and slightly more than 20 percent of children between the ages of 2 and 5 years are already overweight or obese.
In 2010, the IOM appointed a committee to review factors related to overweight and obesity from birth to age 5, with a focus on nutrition, physi-
cal activity, and sedentary behavior. In its report, Early Childhood Obesity Prevention Policies (2011), the committee recommends actions that healthcare professionals, caregivers, and policy makers can take to prevent obesity in children 5 years old and younger.
Parents see pediatricians, primary care physicians, and other healthcare professionals as child care authorities. Thus, these professionals have an important opportunity to increase parents’ awareness about healthy weight early on to allow time for prevention or intervention. The IOM recommends that healthcare professionals measure weight and height or length in a standardized way, as well as pay attention to obesity risk factors, such as rate of weight gain and parental weight, at routine pediatric visits. In addition, the IOM recommends that parents and child care providers keep children active throughout the day and provide them with diets rich in fruits, vegetables, and whole grains, and low in energy-dense, nutrient-poor foods. Caregivers also should limit young children’s screen time and ensure that children sleep an adequate amount each day.
Finally, the committee recommends that the USDA and the Department of Health and Human Services (HHS) establish dietary guidelines for children from birth to age 2. Currently, the Dietary Guidelines for Americans do not include recommendations for children under the age of 2. Such guidelines are necessary for setting nutrition recommendations for public and federal programs.
Another IOM study committee looked at options outside of school for helping children and adolescents avoid weight problems. In Local Government Actions to Prevent Childhood Obesity (2009), the committee identified numerous actions that show potential for use by local governments. Of course, parents and other adult caregivers play a fundamental role in teaching children about healthy behaviors, in modeling those behaviors, and in making decisions for children when needed. But those positive efforts can be undermined by local environments that are poorly suited to supporting healthy behaviors—and may even promote unhealthy behaviors.
Local governments have many opportunities to promote children’s health. Given their jurisdiction over aspects of land use, food marketing, community planning, transportation, health and nutrition programs, and
other community concerns, local governments also are ideally positioned to promote behaviors that will help children and adolescents reach and maintain healthy weights.
As a blueprint for action, the IOM committee recommended nine healthy eating strategies and six physical activity strategies for local government officials to consider in planning, implementing, and refining childhood obesity prevention efforts. The committee also recommended a number of specific action steps for each strategy and highlighted 12 steps overall judged to have the most promise. One general message is clear: Promoting children’s healthy eating and activity will require the involvement of an array of government officials, including mayors and commissioners or other leaders of counties, cities, or townships. Many departments, including those responsible for public health, education, public works, transportation, parks and recreation, public safety, planning, economic development, and housing, also need to be involved.
In addition, community involvement and evaluation are vital to childhood obesity prevention efforts. It is critical for local government officials and staff to involve constituents in determining local needs and identifying top priorities. Engaging community members in the process will help identify local assets, focus resources, and improve implementation plans. And, as obesity prevention actions are implemented, such actions need to be evaluated in order to provide important information on what does and does not work.
The IOM also has dealt with the obesity epidemic across broader society. Approximately 68 percent of adults in the United States aged 20 years or older are either overweight or obese. Among children and adolescents aged 2 through 19 the rate is nearly 32 percent. To respond most effectively, policy makers, public health professionals, and other decision makers need relevant and useful evidence on promising obesity prevention actions for the populations they serve.
Promoting children’s healthy eating and activity will require the involvement of an array of government officials, including mayors and commissioners or other leaders of counties, cities, or townships.
In 2008, Kaiser Permanente asked the IOM to develop a practical,
action-oriented framework to guide the use of evidence in decision making about obesity prevention policies and programs and to guide the generation of new and relevant evidence. The IOM convened a committee that sought the answers to two fundamental questions:
• How can evidence that is currently available and potentially relevant to decisions about obesity prevention be identified, evaluated, and compiled in ways that will best inform decisions?
• How can more evidence be developed that is of high quality and framed to be directly relevant to decision making on obesity prevention?
The committee developed the L.E.A.D. framework process—short for Locate evidence, Evaluate it, Assemble it, and inform Decisions—to help in answering these questions. Presented in the committee’s report, Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making (2010), the framework encourages decision makers and researchers to look at obesity from a systems perspective in order to under-
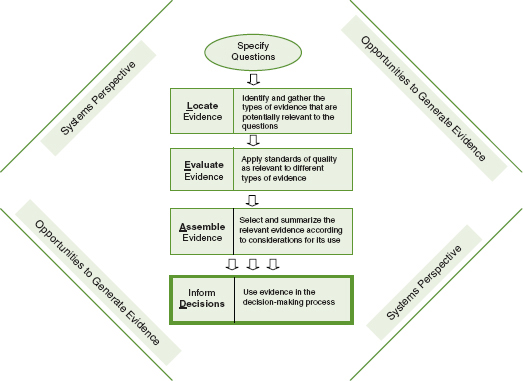
The L.E.A.D. framework.
SOURCE: Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making, p. 5.
stand it as a complex, population-based health problem. The framework provides guidelines for assembling and compiling evidence in an open and transparent way, placing it in a real context in order to inform decisions. It offers opportunities to generate useful, high-quality evidence for decision making at every step, and encourages learning from a variety of sources, including ongoing policies and practices and alternatives to randomized experiments. It also provides a way for assessing how well research results can be applied to other individuals, settings, contexts, and time frames.
The (L.E.A.D.) framework provides guidelines for assembling and compiling evidence in an open and transparent way, placing it in a real context in order to inform decisions.
The IOM continues to tackle the obesity epidemic through many different avenues. Its Standing Committee on Childhood Obesity Prevention, sponsored by the Robert Wood Johnson Foundation, serves as a focal point for national and state-level policy discussions about obesity prevention, and it has guided the development of previous and upcoming studies on various aspects of obesity prevention, among them the legal strategies that have an effect on obesity. The standing committee hosted a workshop to highlight current and potential legal strategies and other public health initiatives in October 2010.
In addition, the IOM recently partnered with HBO Documentary Films on The Weight of the Nation, a project that will incorporate multiple documentary films, publications, and a web component. More about this project can be found in the chapter on collaboration.
Strengthening food safety
Approximately 76 million food-borne illnesses—caused by a variety of bacteria, viruses, parasites, or chemical residues—occur each year in the United States, resulting in more than 300,000 hospitalizations and 5,000 deaths. While food safety is regulated by several agencies, the FDA oversees approximately 80 percent of the nation’s food supply, including all produce, seafood, and cheeses. But experts and the public have criticized the FDA’s food safety system and questioned whether it properly safeguards the public from food-borne diseases. In response, Congress asked the IOM to examine the gaps in the current food safety system under the
purview of the FDA and to identify the tools needed to improve food safety.
In Enhancing Food Safety: The Role of the Food and Drug Administration (2010), the IOM study committee concludes that the FDA lacks a comprehensive vision for food safety and should change its approach in order to properly protect the nation’s food. The agency should use a risk-based approach to evaluate food safety problems rather than its current reactive approach, which addresses problems only on a case-by-case basis and may fail to account for all the factors involved in making a decision. Adopting a risk-based approach will enable decision makers to evaluate the food safety system in a comprehensive way and follow a systematic process for addressing and preventing problems. Components of a risk-based food safety system include conducting strategic planning; ranking public health risks; targeting information gathering efforts, such as surveillance, on identified risks; analyzing and selecting interventions; designing an intervention plan; and monitoring and reviewing implementation efforts.
Approximately 76 million food-borne illnesses—caused by a variety of bacteria, viruses, parasites, or chemical residues—occur each year in the United States, resulting in more than 300,000 hospitalizations and 5,000 deaths.
The committee outlines a set of actions that are needed to implement a risk-based food safety system. For example, the FDA should hire or train additional staff with expertise in risk management and analysis; develop a comprehensive strategic plan that identifies public health goals and metrics to measure success; and define the roles of all parties in the food system, including suppliers, farmers, retailers, consumers, and government agencies, among others. The agency also should lead efforts to integrate federal, state, and local safety programs so they work in a seamless manner; improve food safety inspections; and expand and sharpen communications programs to inform the public of risks in a timely and useful manner.
Finally, the committee called on Congress to help, by considering legislative action to provide the FDA with the authority it needs to fulfill its food safety mission. In November 2010, the Senate passed legislation that aligned with many of the IOM’s recommendations, and in January 2011, President Obama signed into law the FDA Food Safety Modernization Act, which is aimed at ensuring the U.S. food supply is safe by shifting the focus of federal regulators from responding to contamination to preventing it.
Fostering good nutrition
Consumers need sound information about food and nutrition in order to make choices that promote and protect their health and well-being. The IOM has helped by developing and disseminating Dietary Reference Intakes (DRIs) that specify how much of a given nutrient should be consumed for good nutrition and how much is unsafe or unwarranted, with the levels specified according to an individual’s age, gender, and life stage. Now available for more than 40 nutrient sources, the DRIs are intended to serve as a guide for good nutrition and provide the basis for the development of nutrient guidelines in both the United States and Canada.
The IOM has compiled these DRIs into a single listing for easy viewing. A summary guide to the DRIs also is available, along with a number of focused, in-depth publications to help users understand the important considerations in applying the values for planning and assessing diets. Through these and other avenues, the DRIs are used by a range of health professionals and policy makers, including federal nutrition officials who develop policies and programs, dietitians and health practitioners who counsel individuals and groups, and researchers who are working to advance the state of nutrition knowledge.
Dietary Reference Intakes for Calcium and Vitamin D (2010) is the most recent report in the IOM series. These two nutrients have long been known for their role in bone health. Over the past 10 years, however, the public has heard conflicting messages about other benefits of these nutrients—especially vitamin D—and about how much of the nutrients must be consumed for good health. The new DRIs are based on much more information and higher-quality studies than were available when the reference values were first set in 1997.

The report’s authoring committee concluded that a strong body of evidence from rigorous testing substantiates the importance of vitamin D and calcium in promoting bone health. The evidence for other health benefits, however, is mixed and inconclusive, and targeted research is needed to assess these possible health benefits. The committee also found that consuming vitamin D and calcium at levels higher than recommended does not confer greater benefits. In fact, elevated consump-
Dietary Reference Intakes for Calcium and Vitamin D
| Life Stage Group | Calcium | Vitamin D | ||||
| Estimated Average Requirement (mg/day) | Recommended Dietary Allowance (mg/day) | Upper Level Intake (mg/day) | Estimated Average Requirement (IU/day) | Recommended Dietary Allowance (IU/day) | Upper Level Intake (IU/day) | |
| Infants 0 to 6 months | * | * | 1,000 | ** | ** | 1,000 |
| Infants 6 to 12 months | * | * | 1,500 | ** | ** | 1,500 |
| 1–3 years old | 500 | 700 | 2,500 | 400 | 600 | 2,500 |
| 4–8 years old | 800 | 1,000 | 2,500 | 400 | 600 | 3,000 |
| 9–13 years old | 1,100 | 1,300 | 3,000 | 400 | 600 | 4,000 |
| 14–18 years old | 1,100 | 1,300 | 3,000 | 400 | 600 | 4,000 |
| 19–30 years old | 800 | 1,000 | 2,500 | 400 | 600 | 4,000 |
| 31–50 years old | 800 | 1,000 | 2,500 | 400 | 600 | 4,000 |
| 51–70 year old males | 800 | 1,000 | 2,000 | 400 | 600 | 4,000 |
| 51–70 year old females | 1,000 | 1,200 | 2,000 | 400 | 600 | 4,000 |
| >70 years old | 1,000 | 1,200 | 2,000 | 400 | 600 | 4,000 |
| 14–18 years old, pregnant/ lactating | 1,100 | 1,300 | 3,000 | 400 | 600 | 4,000 |
| 19–50 years old, pregnant/ lactating | 800 | 1,000 | 2,500 | 400 | 600 | 4,000 |
*For infants, Adequate Intake is 200 mg/day for 0 to 6 months of age and 260 mg/day for 6 to 12 months of age.
**For infants, Adequate Intake is 400 IU/day for 0 to 6 months of age and 400 IU/day for 6 to 12 months of age.
SOURCE: Dietary Reference Intakes for Calcium and Vitamin D.
tion has been linked to various health problems, such as kidney stones caused by excessive calcium intake—challenging the concept that “more is better.” These findings may raise important concerns as North Americans take more supplements and eat more foods that have been fortified with vitamin D and calcium, increasing their risk of consuming far too much of these otherwise important nutrients.
In another study, the IOM looked at a common food ingredient that can cause health problems: sodium. Americans consume unhealthy amounts of sodium in their food, increasing their risk for high blood pressure, a serious health condition that can lead to a variety of diseases. While numerous stakeholders have initiated voluntary efforts to reduce sodium consumption during the past 40 years, they have not succeeded. Challenges arise because salt—the primary source of sodium in the diet—and other sodium-containing compounds are widely used in the food industry, including restaurants, to enhance the flavor of foods.
Consuming vitamin D and calcium at levels higher than recommended does not confer greater benefits.
To help in meeting this concern, Congress asked the IOM to recommend strategies for reducing sodium intake to levels recommended in the Dietary Guidelines for Americans—currently no more than 2,300 milligrams per day for persons 2 or more years of age. This amounts to about a teaspoon of salt per day, while the average person consumes about 50 percent more than that. In Strategies to Reduce Sodium Intake in the United States (2010), the authoring study committee concluded that a new, coordinated approach is needed to reduce sodium content in food, requiring new government standards for the acceptable level of sodium.

Manufacturers, restaurants, and other food-service operators should be required to meet these standards so all sources in the food supply are involved and so consumers’ taste preferences can be changed over time to the lower amounts of salt in food. The goal is to slowly, over time, reduce the sodium content of the food supply in a way that goes unnoticed by most consumers as individuals’ taste sensors adjust to the lower levels of sodium.
A range of stakeholders will need to cooperate in this effort. HHS should act in cooperation with other government and private groups to design and implement a nationwide campaign to reduce sodium intake and should set a timeline for achieving recommended sodium intake levels. Consumers have an important role to play by making healthy food choices and selecting lower-sodium foods. In addition, government agencies, public health and consumer organizations, health professionals, the health insurance industry, the food industry, and public-private partnerships should support the implementation of the sodium standards for foods and also support consumers in reducing their sodium intake. Finally, better monitoring of sodium intake and of the progress toward changing salt taste preference are essential so the reduction efforts can be tracked and evaluated, and improvements can be made as needed.
In response to the IOM report, some companies in the food industry have begun to act. And Walmart, which sells more food than any other grocery store chain in the nation, announced in January 2011 that it would work with its suppliers to provide healthier food choices and make those foods more affordable to consumers. The company referred to the IOM in making its announcement. Walmart plans to reformulate many of its packaged foods to reduce sodium—as well as added sugars and trans fats—by
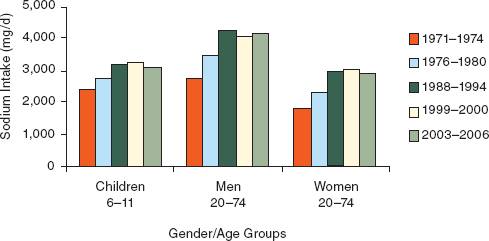
Gender/Age Groups
Trends in mean sodium intake from food for three gender/age groups, 1971–1974 to 2003–2006.
NOTES: Analyzed using 1-day mean intake data for the National Health and Nutrition Examination Survey (NHANES) 2003–2006 to be consistent with earlier analyses and age-adjusted to the 2000 Census; includes salt used in cooking and food preparation, but not salt added to food at the table. d = day; mg = milligram.
SOURCE: Briefel and Johnson (2004) for 1971–2000 data; NHANES for 2003–2006 data.
SOURCE: Strategies to Reduce Sodium Intake in the United States, p. 5.
2015. The company said it also intends to ask its suppliers to reduce sodium by 25 percent in some foods and to report on their progress.
Meeting the needs of an aging population
The nation’s population is increasingly an older population, and IOM’s Food Forum held a workshop in October 2009 to discuss food safety and nutrition in older adults. One general concept that emerged was that there is no single “elder” population. Rather, there are many different aging populations defined by age range as well as by such factors as race, socioeconomic status, level of family support, disability, and chronic health conditions. Meeting the differing needs of these groups rapidly becomes a complex task. Workshop participants from government, academia, industry, and other sectors discussed the variety of ways that different stakeholders are embracing the challenge of improving food safety and nutrition in aging populations.
There is no single “elder” population. Rather, there are many different aging populations defined by age range as well as by such factors as race, socioeconomic status, level of family support, disability, and chronic health conditions.
This challenge is made more difficult by a lack of information in many key areas. For example, although high-quality diets and nutrient optimization are understood to be necessary for maintaining good health in older adults, several questions remain about exactly what constitutes a high-quality diet and what types of obstacles, such as poor oral health and loss of appetite, keep people from obtaining optimal diets. Another challenge in differentiating among multiple aging populations is the lack of health-monitoring data and the consequent inability to generate enough statistical power to make conclusions about the health conditions and needs of those varied populations. Also, although industry has developed new food-processing techniques and novel packaging that minimize many food safety problems, there are still important unanswered questions about how food processing, formulation, and packaging can be improved to better meet the needs of older adults.
In October 2011, the IOM held another workshop to explore nutritional interventions and services for older people staying in community settings. This workshop outlined the scope of nutrition needs; the importance, strengths, and weaknesses of nutrition services; and future research needs related to nutrition and healthy aging in the community.














