Strengthening the Healthcare Workforce
The workforce of healthcare professionals—the backbone of the nation’s healthcare system—labors under many pressures. Some care providers have difficulty coping with a rapidly evolving healthcare system. Doctors are increasingly challenged to keep up with advances in science and medicine. Global health problems create shared responsibilities for health workers everywhere. New and emerging diseases raise safety concerns for frontline care providers. Rising patient expectations and increasing demand from more widespread insurance coverage will heighten the challenges.
The Institute of Medicine (IOM) has examined many aspects of the healthcare workforce—delineating problems, identifying solutions, and charting paths forward. Government policy makers, healthcare and education leaders, individual care providers, and a range of other stakeholders can draw on this knowledge to ensure that the nation takes full advantage of a skilled, adaptive, and well-protected healthcare workforce.
The future of nursing
With more than 3 million members, the nursing profession is the largest segment of the nation’s healthcare workforce. But even as nurses are the primary professional caregivers for many patients, a number of barriers prevent nurses from being able to keep up with changes in where and how health care is delivered and in the skills required to keep pace with today’s evolving healthcare system.
In 2008, the Robert Wood Johnson Foundation (RWJF) and the IOM launched a 2-year study to respond to nurses’ needs and transform the nursing profession. Called the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine, the project followed a methodical course to ensure comprehensive analysis. Over 2 years, the study committee held three national forums focused on critical aspects of health, including acute care; community health, primary care, and long-term care; and nursing education. The meetings enabled stakeholders to share their knowledge and express their concerns about the roles of nurses in the current healthcare system, and the IOM published summaries of each forum. The committee also held several technical workshops at which members further explored challenges facing the nursing profession.
From these efforts, the committee produced The Future of Nursing: Leading Change, Advancing Health (2010). The report describes the committee’s vision for health care and the essential role of nurses in realizing this vision, concluding that a fundamental transformation of the nursing profession is needed if nurses are to fulfill this role. The report presents a blueprint for action in the form of recommendations and related research priorities. Transformations are needed in three broad areas—nursing practice, education, and leadership—and within this framework, the committee developed four key messages that structure its recommendations.
The report describes the committee’s vision for health care and the essential role of nurses in realizing this vision.
First, nurses should practice to the full extent of their education and training. Because licensing and practice rules vary across states, the regulations regarding scope of practice—that is, the activities that a qualified nurse may perform—have varying effects on different types of nurses in different parts of the country. Consequently, the tasks that nurses are allowed to perform are often determined not by their education and training but by the unique state laws under which they work. The report calls on a variety of stakeholders—from state legislators to the Centers for Medicare and Medicaid Services to the Congress—to ensure
that nurses can practice to the full extent of their education and training. The federal government is particularly well suited to promote reform of states’ scope-of-practice laws by sharing and providing incentives for the adoption of best practices.
Second, nurses should achieve higher levels of education and training through an improved education system that promotes seamless academic progression into higher-degree programs. Patient needs have become more complicated, and nurses need to achieve requisite competencies to deliver high-quality care in a variety of settings and in partnership with teams of health professionals. Needed competencies include system improvement, research and evidence-based practice, and teamwork and collaboration,
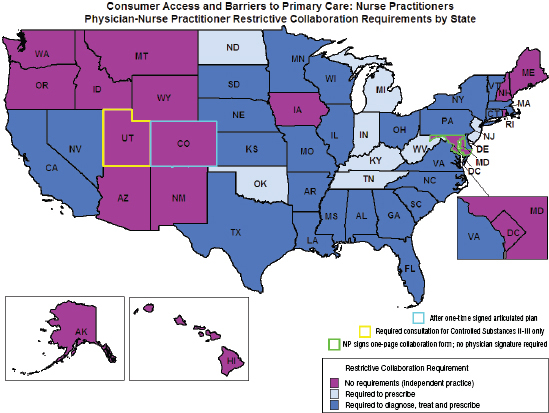
Requirements for physician−nurse collaboration, by state, as a barrier to access to primary care.
NOTE: Collaboration refers to a mutually agreed upon relationship between nurse and physician.
SOURCE: AARP, 2010b. Courtesy of AARP. All rights reserved. This figure combines Map 1, Overview of Diagnosing and Treating Aspects of NP Practice and Map 2, Overview of Prescribing Aspects of NP Practice, both developed by Linda Pearson (2010).
SOURCE: The Future of Nursing: Leading Change, Advancing Health, p. 99.
among others, as well as competencies in specific content areas, including community and public health and geriatrics. Nurses also should be educated with physicians and other health professionals both as students and throughout their careers in lifelong learning opportunities. And to improve the quality of patient care, a greater emphasis must be placed on making the nursing workforce more diverse, particularly in the areas of gender, race, and ethnicity.
Third, nurses should be full partners with physicians and other healthcare professionals in redesigning health care. Being a full partner will involve taking responsibility for identifying problems and areas of system waste, devising and implementing improvement plans, tracking improvement over time, and making necessary adjustments to realize established goals. In the health policy arena, nurses should participate in, and sometimes lead, decision making and be engaged in healthcare reform-related implementation efforts. Nurses also should serve actively on advisory boards on which policy decisions are made to advance health systems and improve patient care. To ensure that nurses are ready to assume leadership roles, nursing education programs need to embed leadership-related competencies throughout training.
Nurses should be full partners with physicians and other healthcare professionals in redesigning health care.
Fourth, planning for fundamental, wide-ranging changes in the education and deployment of the nursing workforce will require comprehensive data on the numbers and types of health professionals—including nurses—currently available and required to meet future needs. Once an improved infrastructure for collecting and analyzing workforce data is in place, systematic assessment and projection of workforce requirements by role, skill mix, region, and demographics will be needed to inform changes in nursing practice and education.
Building on this report, the RWJF and the IOM convened the National Summit on Advancing Health through Nursing. Held in late 2010, it brought together more than 500 stakeholders from multiple sectors to discuss implementing the report’s recommendations. Thousands more participants joined via webcast and more than 120 satellite meetings in 45 states.
At the summit, RWJF, in collaboration with AARP, the advocacy group for older people, announced the launch of the Initiative on the Future
of Nursing Campaign for Action. Using the IOM report as a framework, the campaign works in partnership with numerous healthcare groups and professionals on a variety of activities, such as data collection and dissemination of educational tools, aimed at ensuring that nurses are prepared to meet the demands of the 21st-century health system.
Lifelong learning
Every segment of the healthcare workforce must comprise professionals who provide high-quality health care and assure patient safety. However, the nation lacks a comprehensive, effective system of continuing education in the health professions, and that this gap contributes to knowledge and performance deficiencies at the individual and system levels. Many stakeholders have called for a national interprofessional continuing education institute that would advance the science of continuing education. With support from the Josiah Macy Jr. Foundation, the IOM examined options for bridging the education gap.
The IOM study committee’s report, Redesigning Continuing Education in the Health Professions (2009), described the merits and drawbacks of current programs, explored development of a national continuing education institute, and offered guidance on the establishment and operation of such an institute. To add perspective to its deliberations, the committee evaluated a number of possible alternatives to an institute. They included maintaining the status quo, developing a government program within an existing agency, forming a coalition of continuing education stakeholders and other organizations focused on healthcare quality and patient safety, and creating a new entity drawn from professional societies. The committee judged each alternative to be feasible, but concluded that a public-private institute held the most promise for fostering collaboration among all stakeholders that would improve the nation’s system of continuing education for all health professionals.
There are major flaws in the way continuing education is conducted, financed, regulated, and evaluated, and the science underpinning continuing education for health professionals is fragmented and underdeveloped.
The report identifies a set of key messages that should help guide reforms. Among them, there are major flaws in the way continuing education is conducted, financed, regulated, and evaluated, and the science
Overview of Current Continuing Education Financing in Medicine
| Current System | |
| Industry funding? | Yes, ~58% of total |
| Out-of-pocket cost to physicians | ~42% of total, or $1,200 per physician per year |
| Mode of delivery | Primarily in-person lectures and workshops, with a small amount of simulation training and performance improvement exercises taking hold |
| Educational value, impact on patient care | Unclear |
SOURCE: Redesigning Continuing Education in the Health Professions, p. 67.
underpinning continuing education for health professionals is fragmented and underdeveloped. Continuing education efforts should bring health professionals from various disciplines together in carefully tailored learning environments. And in an overarching shift, the nation should develop a comprehensive new vision of professional development to replace the culture that now envelops continuing education in health care.
The new vision should be based on an approach called continuing professional development, in which learning takes place over a lifetime and stretches beyond the classroom to the point of care. Unlike today’s more structured approach, this holistic approach would incorporate a broad variety of learning methods and theories, and it would be learner driven, allowing learning to be tailored to individuals’ needs.
The nation should develop a comprehensive new vision of professional development to replace the culture that now envelops continuing education in health care.
To help in reaching these goals, the Department of Health and Human Services (HHS) should commission a blue-ribbon panel to oversee the design and implementation of an independent public-private Continuing Professional Development Institute. As a neutral body, not embedded within any agency, the institute could promote and catalyze stakeholder collaboration. The IOM report presents a detailed action plan for the institute. Among other actions, the institute should develop and prioritize a national research agenda in continuing education, work toward harmonizing the complex web of regulations covering continuing education, and explore new financing mechanisms that
will support a broader-based continuing professional development system while avoiding potential conflicts of interest.
Guarding worker safety
Given that professionals across the healthcare workforce grapple regularly with a variety of medical threats, including new and emerging diseases, it is important to protect them where they work. One such risk emerged with the recent outbreak in the United States and other nations of a new type of influenza, called H1N1 influenza A. At the request of the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA), the IOM convened an expert committee to rapidly develop recommendations on how best to provide respiratory protection for healthcare workers who might be exposed to the virus on their jobs.
In Respiratory Protection for Healthcare Workers in the Workplace Against Novel H1N1 Influenza A: A Letter Report (2009), the committee recommends that personnel in hospitals and other care settings who are in close contact with individuals with H1N1 influenza A or influenza-like illnesses use an N95 respirator (or one equally effective) that is adjusted for proper fit. Employers should ensure that the use and fit testing of N95 respirators be conducted in accordance with OSHA regulations, and healthcare workers should use the equipment as required by regulations and employer policies.
The committee also calls for the CDC and other federal agencies, as well as private health groups, to fund or conduct additional research to resolve unanswered questions about the relative contribution of various routes of influenza transmission; explore the effectiveness through randomized clinical trials of personal respiratory protection technologies in a variety of clinical settings; and design and develop the next generation of personal respiratory protection technologies for healthcare workers to enhance safety, comfort, and ability to perform work-related tasks.
While this study answered some particularly pressing health questions raised by the emergence of a new influenza virus, the healthcare community clearly faces broader challenges in dealing with influenza pandemics and other viral diseases. To help in efforts to better protect the healthcare workforce, the National Personal Protective Technology Laboratory at the National Institute for Occupational Safety and Health
(NIOSH) asked the IOM to assess the personal protective equipment (PPE) on which workers rely. PPE may include respirators, face masks, gloves, gowns, eye protection, and face shields. The IOM previously had examined this issue and reported the findings in Preparing for an Influenza Pandemic: Personal Protective Equipment for Healthcare Workers (2008). The new IOM study focused on updating progress in research and identifying future directions for PPE for healthcare personnel.
The healthcare community clearly faces broader challenges in dealing with influenza pandemics and other viral diseases.
In Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Personnel—Update 2010, the committee proposes an integrated approach that embraces the full spectrum of research (from basic research to policy research) and translates research findings into improvements in healthcare practice. Feedback loops will be critical, with adaptations made along the way as new equipment and processes are developed and tested in real-world settings. Such an integrated approach will call for collaboration and discourse among scientists, clinicians, policy makers, and other stakeholders who may not have had previous interactions.
Among research needs, basic questions remain about how the various modes of influenza transmission—droplet spray, aerosol, and direct or indirect contact—contribute to the overall spread of illness. Improvements
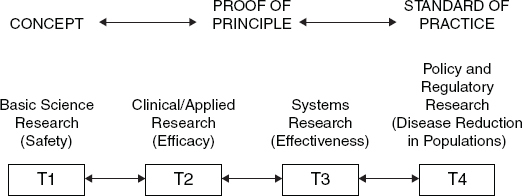
An integrated system moving research into practice, depicting the translation of research from basic science (T1) through policy and regulatory research (T4).
SOURCE: Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Personnel—Update 2010, p. 8.
also are needed in equipment design. For example, safety devices known as filtering facepiece respirators are widely used and much improved in recent years, but new technologies are needed to improve their fit and reduce inward leakage of potentially contaminated air. In addition, better understanding is needed of how safety equipment and processes are used in various types of healthcare settings where a number of factors—the user, the device, the task, and the general work and organizational context—come into play. Paying greater attention to interactions among such contextual factors will better align research on PPE use in health care with other branches of occupational safety and health research.
Better understanding is needed of how safety equipment and processes are used in various types of healthcare settings where a number of factors—the user, the device, the task, and the general work and organizational context—come into play.
But the committee said that even as research continues, enough is known to implement a number of new approaches and technologies immediately, and it recommended a four-pronged strategy. There should be deliberate planning and preparation at the leadership and organizational levels; comprehensive training of personnel, including supervisors and managers; widespread and convenient availability of appropriate PPE devices; and accountability at all levels of the organization. Policies for PPE use by healthcare personnel need to be carefully planned at the organizational and institutional level to ensure a culture of safety, compliance, and buy-in at all levels. Managers and frontline workers alike need to understand and accept their roles and responsibilities, and using PPE needs to be as easy and convenient as possible for all healthcare personnel.
Occupational health nursing (OHN) is one healthcare profession particularly focused on PPE in the workplace. Occupational health nurses (OHNs) work in a variety of workplace environments, including agriculture, construction, health care, manufacturing, and public safety. In these environments, OHNs have a wide range of roles and responsibilities that span management and organization, worker health assessment and direct healthcare services, and prevention and research. In many settings where OHNs work, employees require protective measures to safeguard them from a range of respiratory hazards—for example, respirable dust in construction and chemical sprays in agriculture. As key members of the occupational health and safety workforce, OHNs need adequate education and
training in respiratory protection in order to ensure both their own safety and the safety of America’s workers.
As key members of the occupational health and safety workforce, occupational health nurses need adequate education and training in respiratory protection in order to ensure both their own safety and the safety of America’s workers.
At the request of NIOSH’s National Personal Protective Technology Laboratory, the IOM examined existing respiratory protection curricula in occupational health nursing programs and made recommendations to improve the education and training of OHNs. The IOM identified essential content that should be included in education and training programs for OHNs and the best approaches to teaching that content. The report, Occupational Health Nurses and Respiratory Protection: Improving Education and Training—Letter Report (2011) finds that current respiratory protection education for OHNs receives varying amounts of dedicated time and resources and is taught using a variety of approaches. The report makes several recommendations to occupational health nursing education and training programs and the National Personal Protective Technology Laboratory, such as expansion of respiratory protection information provided across all levels of nursing education and training; consistent integration of essential content into graduate curricula and continuing education programs for OHNs; continued and expanded use of innovative teaching methods, such as online courses, use of simulation and case studies, and field observation and practice; and exploration of the development of core competencies in respiratory protection.
Millions of workers rely on a variety of personal protective technologies to keep them safe.
Millions of workers rely on a variety of personal protective technologies (PPT) to keep them safe. PPT encompass a range of specialized clothing and equipment, including gloves, hearing protection, fall arrest harnesses, respirators, and eye protection. To ensure that PPT will perform as intended, government agencies, manufacturers, testing laboratories, workers, and other stakeholders participate in an array of activities collectively called conformity assessment. Activities include testing to ensure that the product meets specific design or performance criteria, examining the test results to declare conformity to the specifications, inspecting manufacturing sites, and conducting postmarket evaluations.
The National Personal Protective Technology Laboratory asked the IOM to appoint an expert committee to examine PPT conformity assessment issues and recommend improvements. The committee’s report, Certifying Personal Protective Technologies: Improving Worker Safety (2010) concluded that current approaches to evaluating occupational PPT, often by job sector, are fragmented and vary in rigor. The committee recommends as a first step that a comprehensive framework be established for PPT conformity assessment. The framework would categorize products into tiers, based on the degree of risk to the safety and health of the user, while also considering various pragmatic factors, such as the cost or feasibility of developing a new product and the size of the intended target population.
Within the framework, risks would be rated as high, medium, or low, with each category requiring different levels of conformity assessment. When risks are low, manufacturers would need only to attest that their products meet certain standards recognized by the federal government. When risks are medium, products would need to be tested and assessed by an independent testing laboratory and certifying organization to ensure that they meet federal standards. When risks are high, third-party testing and certification would be required, coupled with intensive government involvement at all stages, from design to manufacture and follow-up testing in the workplace.
Numerous stakeholders must participate in developing, implementing, and supporting this new framework. The National Personal Protective Technology Laboratory at NIOSH can play a lead role, and it should work with other federal agencies, certifying and accrediting organizations, manufacturers, and workers who use PPT. Other efforts also will be needed to improve communications between government and employers and workers about the availability and effectiveness of PPT, and to expand federal surveillance programs to monitor the effectiveness of PPT products in the workplace. With such a comprehensive system in place, the government and others will be better able to direct conformity assessment efforts, identify remaining gaps in assessment, and prioritize resources to ensure that workers receive the best protection possible on their jobs.
Fighting HIV/AIDS in Africa
In addition to working to improve the health and well-being of Americans, the U.S. workforce of healthcare professionals, by necessity, tackles international health challenges as well. No challenge is greater than combating HIV/AIDS in sub-Saharan Africa, which in 2009 accounted for 68 percent of cases worldwide and 69 percent of new infections. In a major U.S. effort, the President’s Emergency Plan for AIDS Relief has provided approximately $32 billion to HIV/AIDS-related programs since it was established in 2003. But this and other assistance efforts are being overwhelmed as the epidemic continues to spread.
No challenge is greater than combating HIV/AIDS in sub-Saharan Africa, which in 2009 accounted for 68 percent of cases worldwide and 69 percent of new infections.
In this context, the IOM appointed a committee of experts to recommend affordable, sustainable strategies that both African nations and the United States can implement to reduce the long-term burden of HIV/AIDS. The committee’s report, Preparing for the Future of HIV/AIDS in Africa: A Shared Responsibility (2010), concludes that the burden of morbidity and mortality in Africa cannot be alleviated through treatment alone. Treatment can reach only a fraction of those who need it, and its costs are unsustainable. Greater emphasis must be placed on preventing new infections. The report identifies a number of specific, tailored strategies for building African capacity—including human, scientific, technological, organizational, institutional, and/or resource capabilities—to prevent, treat, and care for HIV/AIDS.
African countries, with the support of international donors, including the United States, should develop and implement methods for measuring the level of and change in new HIV infections to enable better planning and evaluation of prevention programs. The nations also should focus on strengthening their healthcare systems by making the most of existing capacities, such as healthcare workers on the ground and local institutions. Needed actions include making use of management and support staff from outside the clinical health sector to free up time for healthcare providers to perform clinical work; delegating tasks of health professionals, when appropriate, to health workers with less-specialized training; tapping the potential of modern information and communications technology, such as smart phones and distance learning; and forming partnerships between developing countries and creating regional collaborations to exchange technical assistance.
For the United States, strategies should focus on supporting partnerships—particularly institutional partnerships—that can help Africa move forward independently in HIV/AIDS treatment and prevention. Such partnerships can be formed in the public and private sectors and include collaborations among academic institutions, faith-based organizations, and the militaries of the United States and African nations. Among other actions, the White House and the Office of the Global AIDS Coordinator should develop a U.S. roadmap for HIV/AIDS in 2020 that incorporates a model of U.S.-African shared responsibility. This roadmap should give priority to HIV/AIDS prevention and strike an optimal balance between bilateral and multilateral funding mechanisms. Likewise, HIV/AIDS coordinating groups in Africa should develop a 20-year roadmap for combating the epidemic, including sufficient investment in prevention and the development of more efficient models of care and treatment.
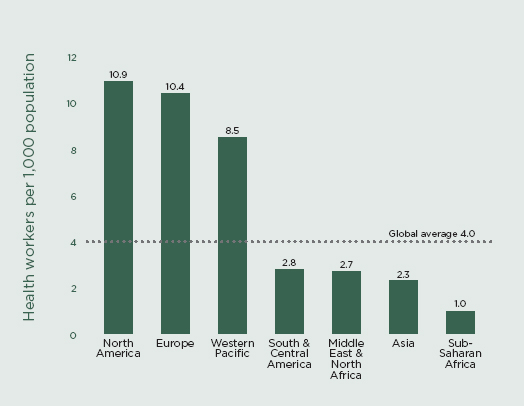
Health worker density by region.
SOURCE: JLI, 2004, compiled from WHO, 2004.
SOURCE: Preparing for the Future of HIV/AIDS in Africa: A Shared Responsibility, p. 108.














