Appendix D
Commissioned Paper:
A Cost and Speed Analysis of
Strategies for Prepositioning
Antibiotics for Anthrax1
James Guyton, Principal, PRTM, lead author
Robert Kadlec, Chandresh Harjivan, Shabana Farooqi, Sheana Cavitt, and Joseph Buccina, PRTM, co-writers and contributors
This paper was prepared by PRTM Management Consultants, LLC (PRTM) under a contract with the Institute of Medicine (IOM) and submitted in April 2011. This publication is limited to the approach and analysis described herein and on information available as of April 15, 2011. No representation or warranty (express or implied) is given as to the accuracy or completeness of the information contained in this publication, and to the extent permitted by law, PRTM and its members, employees, and agents do not accept any liability, responsibility, or duty of care for any consequences of the Committee or anyone else acting, or refraining to act, in reliance on the information contained in this publication or for any decision based on it.
INTRODUCTION
Currently, the United States Government (USG) stores the vast majority of its contingency medical countermeasures (MCM) in 12 centralized locations as part of the Centers for Disease Control and Prevention’s (CDC’s) Strategic National Stockpile (SNS); adopting the concept of prepositioning could alter this modus operandi. Prepositioning for public health preparedness is the placement and storage of MCM in caches that are geographically closer to the metropolitan areas and the corresponding populations at
![]()
1This paper was commissioned by the Institute of Medicine (IOM) to provide background for the deliberations of the Committee on Prepositioned Medical Countermeasures for the Public. The responsibility for the content of this paper rests with the authors, and the paper does not necessarily represent the views of the IOM or its committees and convening bodies.
risk. The primary goal of prepositioning is to increase the speed of MCM distribution and dispensing during a high-consequence biological incident.
In the event of an attack with aerosolized Bacillus anthracis (anthrax), administering oral antibiotics immediately following exposure has demonstrated the potential to save lives (Friedlander et al., 1993). Anthrax exists in vegetative and spore forms. The spore is an extremely hardy, dormant form of the bacterium; it can persist for decades in the environment. When a spore enters a live host, it transforms into its vegetative, disease-causing state. Once active, anthrax produces toxins that are lethal. Given its high lethality and potential ease of acquisition, production, and dissemination, the release of aerosolized anthrax is the type of high-consequence biological attack that is of most concern.
The Center for Biosecurity at the University of Pittsburgh Medical Center notes that anthrax is considered one of the most serious bioterrorism threats for the following reasons (UPMC Center for Biosecurity, 2007):
• widespread availability of starter cultures in culture collection banks around the world;
• widespread natural availability in endemic areas;
• wide commercial availability of equipment and techniques for mass production and aerosol dissemination;
• robustness of anthrax spores, making anthrax easier to weaponize for aerosol dissemination than other biological agents of concern;
• high fatality rate in untreated inhalational cases;
• relatively low infectious dose, based on nonhuman primate animal data;
• risk of antibiotic-resistant strains that exist in nature or that may be easily cultivated for use in an intentional release; and
• recent use of anthrax during the 2001 Amerithrax attacks.
During the 2001 Amerithrax attacks, the median incubation time for inhalational anthrax was 4 days (Jernigan et al., 2001). It is estimated that if oral antibiotics are not administered before the onset of clinical symptoms, the mortality rate, even in intensively treated cases, could potentially exceed 90 percent (UPMC Center for Biosecurity, 2007). In the few inhalational anthrax cases treated in 2001, intensive clinical treatment resulted in a mortality rate of 45 percent (Jernigan et al., 2001). Depending on the initial infective dose and when the exposure is detected, the effective window for antibiotic administration may be considerably less than 96 hours. As a matter of USG policy, current requirements have set the objective of delivery of oral antibiotics to potentially exposed individuals within 48 hours of the decision to do so (CDC, 2010a). Prepositioning can enable more rapid dispensing of oral antibiotics following an anthrax attack, thus increasing
the likelihood that a larger proportion of infected individuals will receive antibiotics during the asymptomatic incubation period.
The Institute of Medicine’s (IOM’s) Committee on Prepositioned Medical Countermeasures for the Public commissioned this paper to provide background for its deliberations on prepositioning strategies for anthrax antibiotics. PRTM analyzed three prepositioning strategies:
• caches in hospitals and pharmacies;
• caches in workplaces of different types (e.g., state and local government, private infrastructure, Fortune 50 companies, small businesses), schools, universities, daycare centers, and institutional facilities for older adults (for simplification, the PRTM team categorized these into large and small places of work); and
• approved MedKits (or similar dose packs) stored in individual households and intended for use by occupants.
This paper focuses largely on two variables: the cost of each prepositioning strategy, and the time to antibiotic distribution and dispensing. The paper also examines the implications of these strategies in three different settings: urban, suburban, and rural. PRTM chose the Minneapolis-St. Paul metropolitan statistical area (MSA) as a case study because of the availability of relevant cost and delivery time data and its confluence of urban, suburban, and rural environments. The prepositioning strategies are compared with two scenarios:
• The current approach of SNS to receiving, storage, and staging (RSS) sites to points of dispensing (PODs)—This approach serves as the baseline model.
• The postal distribution model—In 2008, federal health officials announced the beginning of a postal distribution pilot project in the cities of Minneapolis and St. Paul (Roos, 2008). In this model, postal workers deliver antibiotics directly to individuals’ homes in the event of an anthrax attack.
Other approaches also are considered in the section below on alternative dispensing strategies, including a forward-deployed SNS model and vendor-managed inventory. In addition, in the course of this effort, PRTM uncovered several areas for additional consideration, which are highlighted in a later section. Note that detailed data on which the discussion of the various dispensing strategies is based are presented in Appendix D.1.
In conducting research for this paper, PRTM performed an extensive review of open-source literature and interviewed more than 40 subject matter experts. Appendix D.2 provides a list of interviewees.
STRATEGIES FOR PREPOSITIONING
This section provides a brief background on CDC’s current strategy for distribution and dispensing of antibiotics and a description of each prepositioning strategy. The current approach, based on PODs, is the standard, practiced model for delivering MCM, such as oral antibiotics and vaccines, to an impacted locale following a biological attack. This model is the backbone of several MCM dispensing strategies that were reviewed. Whereas the prepositioning strategies are intended to increase the speed with which a 10-day supply of oral antibiotics is delivered, they are intended only as an adjunct to the POD dispensing approach. The SNS-RSS-POD approach serves as the principal means to distribute and dispense the remainder of the full 60-day course of antibiotics, and vaccination as necessary, to all those affected.
Current Approach for Distribution and Dispensing: Points of Dispensing
The current distribution and dispensing model (Figure D-1) is managed by CDC in conjunction with state, local, and tribal health departments. Antibiotics and other MCM are stored in 12 undisclosed locations across the United States in the SNS. The exact amount of antibiotics stored in these caches is not made public, for security reasons. In the event of an attack, CDC guarantees the delivery of a “Push Package” of medical material, including oral antibiotics, to the affected location within 12 hours of a request (CDC, 2010b). A Push Package is a large package of medications and other medical supplies that can be transported quickly from one of the SNS locations. The oral antibiotics (approximately 500,000 doses in the Push Package) are intended to be an initial supply. Additional quantities of oral antibiotics are transported to the area from a larger reserve contained in a vendor-managed inventory, or inventory controlled by the manufacturer that is guaranteed to be available to the federal government upon request.
Once the Push Package has been transported from the SNS, state authorities receive it at a predesignated RSS site. At this point, the MCM are transitioned from federal to state control. The RSS staff unpacks the
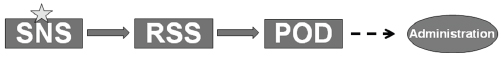
FIGURE D-1
Strategic National Stockpile (SNS) to receiving, storage, and staging (RSS) sites to points of dispensing (POD) model.
NOTE: The star denotes where the antibiotics are stored.
medications and transfers them to trucks, which are bound for individual PODs. The amount of antibiotics delivered to each POD is predetermined by the estimated number of people to be served by each.
Once the antibiotics reach the PODs, they may remain under state control or be turned over to local (county or city) control, depending on the jurisdiction. Although the conceptual approach was developed by CDC, the PODs’ actual operation and staffing are determined by the state or local jurisdiction. At the PODs, public health practitioners screen the public for contraindications to the antibiotics, educate them on the use of the antibiotics, and then dispense a 10-day supply to each person. Different jurisdictions employ a variety of approaches to increase throughput, such as having the head of the household retrieve drugs for everyone in that household, as one interviewee from Tennessee indicated, or having the necessary paperwork completed before a potential event to avoid time spent filling out forms during an emergency, as an interviewee from New York noted.
Caching in Hospitals and Pharmacies
Prepositioning contingency antibiotics in hospitals and pharmacies (Figure D-2) would effectively result in increasing the on-hand antibiotic supply beyond current inventories for routine use in such facilities. Generally, hospitals and pharmacies stock enough antibiotics to meet their immediate daily needs. They rely on distributors to continuously provide “just in time” supplies of antibiotics so they have enough stock to fill their needs, but not so much that they have extra stock on hand. Notable exceptions to this practice are Department of Veterans Affairs (VA) hospitals, Department of Defense (DOD) medical treatment facilities, and some private hospitals that maintain a limited stockpile to provide to their staff and patients in the event of a biological attack.
Expanding this practice to all hospitals, and possibly clinics, would require significant increases in their stock on hand and the costs associated with excess inventory. While they would likely still use the first-in/first-out
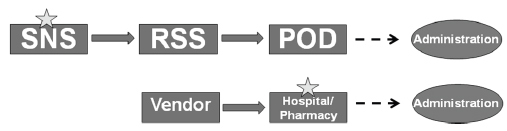
FIGURE D-2
Hospital/pharmacy prepositioning model.
NOTE: The stars denote where the antibiotics are stored.
approach to lessen the impact of expiry, actual costs associated with expiry would depend on the ratio of the size of the cache to the turnover volume of routine use of the antibiotics.
While hospitals, clinics, and pharmacies could maintain contingency antibiotic stockpiles, the manner in which those institutions could dispense such products would be significantly different. Hospitals would serve only as closed PODs. A closed POD is a location that is not open to the general public, but is set up to serve a predefined population. Hospitals would provide prophylactic antibiotics only to patients, staff, and families of staff.
This practice would increase the likelihood that essential hospital workers would report for duty. Limiting dispensing to hospital personnel would be intended to maintain operations for treating current patients and those who needed treatment during the emergency. This dispensing strategy would not accommodate the general public, who, if they sought such treatment, would likely inundate the facility and possibly render it incapable of performing its essential functions.
In contrast, pharmacies and some clinics could serve as open PODs. They would be able to dispense antibiotics to the general public during an emergency. One advantage of this model is that pharmacies and clinics are numerous and have high prevalence in the United States, and people have a general familiarity with the location of their local pharmacy or neighborhood clinic. This approach, however, would require that pharmacies rapidly package antibiotics for swift dispensing, as opposed to routine operations whereby prescriptions are filled on an ad hoc basis.
Hospitals, pharmacies, and some clinics already have some security measures in place for safeguarding medications, so during nonemergencies they likely would not incur an incremental security cost. However, in the event of a biological attack, additional security would likely be necessary to augment existing security activities during dispensing operations. Hospitals, clinics, and pharmacies also would have medical staff on hand who would be licensed to dispense antibiotics and could conduct the necessary prescreening of patients.
Caching in the Workplace
Prepositioning in workplaces (Figure D-3) would effectively create additional closed PODs. In this approach, private companies would stock enough antibiotics to dispense to their employees during an emergency. It would be the company’s decision whether to also provide antibiotics to employee families. The manner by which private companies could participate is two-fold. They could purchase and store antibiotics on site themselves, or they could identify themselves to local public health authorities to serve as a closed POD. In the latter case, the local authorities would provide the
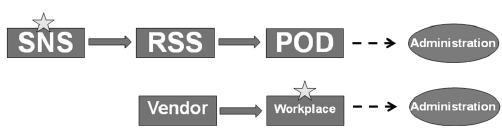
FIGURE D-3
Workplace prepositioning model.
NOTE: The stars denote where the antibiotics are stored.
antibiotics to the workplace by way of the SNS. The former approach, prepositioning on site, would offer the advantage of decreasing the time to dispensing. Serving as a closed POD would not necessarily increase speed over the baseline because no prepositioning would be taking place, and the delivery of antibiotics to the workplace would be contingent on the speed of delivery of the SNS assets.
Caching in workplaces would effectively decrease the percentage of the population that would have to be serviced by public PODs. Employees would benefit from being able to access antibiotics from a familiar place. However, workplaces would likely need to bring in medical personnel for screening and dispensing if they did not already have medically trained personnel on site. Alternatively, the workplace could conduct prescreening of personnel before the event, a practice that was performed in one interviewee’s workplace. This approach might allow the antibiotics to be dispensed by nonmedical personnel following an anthrax incident.
Caching in the Home (MedKits)
Prepositioning antibiotics in the home would entail providing MedKits to a predefined segment of the population within a certain area (Figure D-4). In lieu of a Food and Drug Administration (FDA)–approved MedKit or an over-the-counter product, a prescription would be required for each recipient’s doctor, or recipients would have to be subject to some screening by a health care worker before the MedKits could be issued. This approach would involve screening every person prior to dispensing to determine contraindications, such as allergies, and dosing changes. The appropriate type and numbers of bottles of antibiotics would then be shipped to every household. These bottles would be encased in plastic bags with instructions on storage and use of the antibiotics. Each bag would contain enough antibiotics to cover each person in the household for 10 days. Figure D-5 shows a depiction of a home MedKit.
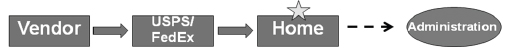
FIGURE D-4
Home MedKit prepositioning model.
NOTE: The star denotes where the antibiotics are stored. USPS = U.S. Postal Service.
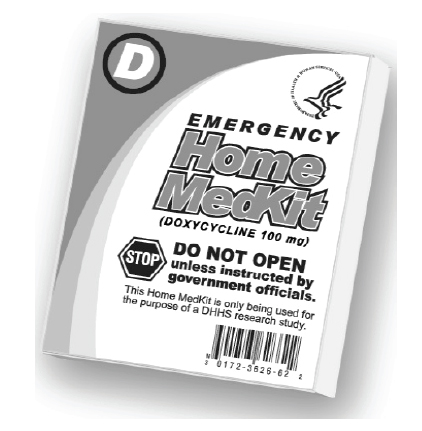
FIGURE D-5
Depiction of a home MedKit.
SOURCE: CDC, 2008.
CDC conducted a study in which it dispensed MedKits to a predefined population in St. Louis to determine how MedKits would be handled and whether people would appropriately follow the instructions provided (CDC, 2008). It was found that the large majority of the population (97 percent) did not use the antibiotics inappropriately and returned the MedKits intact. The study also showed that people had a generally positive response to the MedKits and felt more prepared having one in the home.
The advantage of this model is speed of dispensing in response to an event. The public could be alerted and begin taking the antibiotics immediately without needing to leave their homes. However, many variables could impede the effectiveness of this model. These include little or no medical oversight of prescription medications, loss of the medication, incorrect storage, compliance and tampering, product expiry and returns, and inappropriate usage during other periods of illness. Because of the risk of antibiotic-resistant strains of anthrax, moreover, it could be necessary to have multiple types of antibiotics in the MedKit, which would further complicate the use of this approach.
Postal Distribution Model
One additional model used in this study for comparison is the postal distribution model (Figure D-6). This model is a variation on the standard SNS-RSS-POD model. Rather than the pull approach of that model, the postal distribution model serves to push MCM out to the population. The pilot for this model was sponsored by the Cities Readiness Initiative (CRI) and was employed in the Minneapolis-St. Paul MSA.
In this model, the medications are shipped from the SNS to the RSS, as in the standard model. From there, the medications are delivered to the postal service rather than to PODs. The medications are then delivered to residences in the affected area by postal workers, who agree to deliver the antibiotics on a volunteer basis. In exchange, they are given one MedKit for their home and one for work to cover them and their families. During an emergency, the postal workers would report to the postal service and receive enough MCM to cover approximately two normal routes, as well as a security escort. They would then deliver one bottle of antibiotics to each household on the predetermined routes (Plessas, 2010). As the postal workers cover these routes every day, they are trained to make these deliveries and have done so with efficiency in limited-scope trials in Seattle, Boston, and Philadelphia.
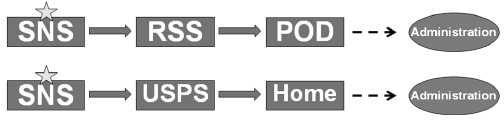
FIGURE D-6
Postal distribution model.
NOTE: The stars denote where the antibiotics are stored. USPS = U.S. Postal Service.
ANALYTICAL FRAMEWORK
PRTM used the analytical framework shown in Figure D-7 to compare the above dispensing models. In conducting the analysis, the PRTM team sought to compare the different prepositioning strategies included within the scope of this paper with the current SNS-RSS-POD baseline. To accomplish this, the team estimated total costs associated with:
• product,
• transport,
• inventory management, and
• dispensing.
For each dispensing strategy, the team examined the time required to dispense antibiotics from the cache to the subset of the population served, as well as the total time required to dispense antibiotics to the general public using a combined SNS-RSS-POD and prepositioned cache strategy. By measuring the SNS-RSS-POD baseline, the team was able to estimate time savings over the baseline, as well as time savings per dollar spent for each prepositioning strategy.
It is important to note that the time savings referenced above apply to the subset of the population served by the various prepositioning strategies. According to a Georgia Institute of Technology study, 20 percent participation by the private sector is a reasonable goal, taking into consideration anticipated reluctance to participate (Lee, 2011). As a result, the team estimated that 20 percent of the population would receive an
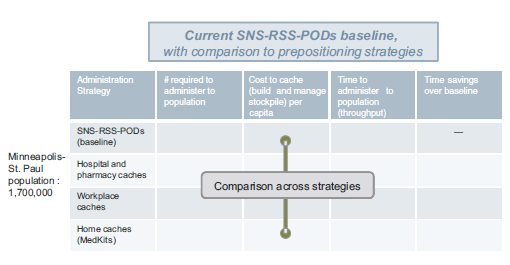
FIGURE D-7
Analytical framework.
initial dose of MCM through prepositioned caches at workplaces or hospitals/pharmacies, while the remaining 80 percent would still need to receive MCM through PODs. For those scenarios, referenced time savings are therefore applicable only to the 20 percent of the population that would receive MCM through the prepositioned caches. In addition to enabling initial time savings, prepositioned caches would help alleviate the burden on PODs by decreasing the total number of individuals that would visit PODs to receive their initial dose of MCM.
To allow for additional analysis and comparison, the team reviewed cost and speed implications associated with employing the postal model in the Minneapolis-St. Paul MSA. To facilitate an accurate comparison, the team assumed the same treatment and dosage as planned for the postal model (consisting of an initial treatment course of 10 days, with two pills per dose), as well as the same target population (the Minneapolis-St. Paul postal plan is intended to serve residents in 20 zip codes, with a combined population of 1.7 million individuals), according to estimates provided by interviewees.
COMPONENTS OF COST AND SPEED FOR DISPENSING STRATEGIES
PRTM assessed each strategy by taking into consideration three key variables: (1) total population served, (2) total cost, and (3) total speed of dispensing. The following sections decompose the general methodology employed by the team, including major assumptions, to derive the estimated population, cost, and speed for each strategy assessed. Additional detail on these calculations can be found in Appendix D.1.
Total Population Served
Both total cost and speed will vary greatly depending on the expectation of the total population to be served by each dispensing location. Table D-1 lists the PRTM team’s assumptions related to estimating the population served.
TABLE D-1
Assumptions Related to Estimating the Population Served Under Each Dispensing Strategy
| Dispensing Strategya | Total Population Assumed Served by Referenced Dispensing Strategy |
| Workplace Cache | The team assumed that a representative large workplace consists of 10,000 employees and a small workplace 300 employees, referencing data from the U.S. Bureau of Labor Statistics.b The team further assumed that each prepositioning cache would include treatment for dependents, estimating an average household size of 2.28 individuals (Minnesota Department of Administration, 2000). |
| Hospital Cache | To arrive at total hospital cache requirements, the team determined the total number of hospital employees, dependents, and patients, assuming that a hospital would act as a closed POD. Dependents were determined assuming 2.28 individuals per household, and patients by determining the total number of hospital beds in the Minneapolis-St. Paul area and assuming a 67 percent average patient occupancy rate. |
| Pharmacy Cache | To determine pharmacy cache requirements, the team assumed that pharmacies would operate as open PODs and would store enough product to cover the remaining population that is assumed to be served by prepositioned caches but that hospitals lack the capacity to handle. The team then divided the total population assumed to obtain MCM through pharmacies by the total number of pharmacies in the Minneapolis-St. Paul area to determine the average number of individuals each pharmacy could expect to serve. |
| MedKit | The team assumed that 100 percent of the population would receive the initial dose of MCM through MedKits. |
aThe team assumed that 20 percent of the total population (1.7 million in this study), would receive the initial 10-day dose of antibiotics through workplace or hospital/pharmacy caches, with the remainder served by PODs.
bSee www.bls.gov.
Total Cost
Total cost can be decomposed into the components listed earlier:
• product,
• transport,
• inventory management, and
• dispensing.
Where possible, the team used empirical data to derive the various cost estimates; where data were not readily available or could not be shared, the team estimated the total cost by using information obtained during its interviews and literature review to develop assumptions and model different dispensing strategies. Note that there are additional costs and considerations that could not be quantified for each strategy, such as security, POD or equivalent worker reliability, or public acceptance of the MCM, although these may be significant issues during a potential biological attack.
Product
Product costs are incurred when prepositioned caches or MedKits in homes are established or replenished. Cost components and key assumptions related to product costs are shown in Table D-2.
Transport
Transport costs are incurred when products are shipped to a hospital, pharmacy, workplace, or household to establish or replenish prepositioned caches or MedKits. Cost components and key assumptions related to transport are shown in Table D-3.
TABLE D-2
Product-Related Cost Components and Key Assumptions
| Product-Related Cost Component | Key Assumptions |
| Product Type | The project team chose to focus its analysis on the dispensing of doxycycline because a 2008 Biomedical Advanced Research and Development Authority (BARDA) Emergency Use Authorization (EUA) application requested that the FDA issue an EUA for the pre-event provision and potential use of doxycycline hyclate tablet emergency kits for inhalational anthrax (Hamburg, 2010). Interviewee feedback supported the idea that doxycycline is the method of treatment preferred by the federal government. |
| Product Cost | The team assumed a total product cost of $0.10 per pill, or $0.20 per daily dose of doxycycline, which is a member of the tetracycline antibiotics family (Medscape Reference, 2010). |
| Product Dose | The team assumed that prepositioned caches, in combination with the baseline POD capability, would carry enough MCM to supply the total population served, including dependents, with a 10day prophylactic course of doxycycline. |
TABLE D-3
Transport-Related Cost Components and Key Assumptions
| Transport-Related Cost Component | Key Assumptions |
| Shipping Mode | Total shipping costs were determined by averaging the rates of commercial shippers, assuming ground shipping and varied shipment weights and distances traveled. |
| Shipping Weight | For each prepositioning scenario, the team estimated total weight by referencing shipping weight data from online sourcesa for one bottle of 100 mg, 20-count doxycycline tablets, and multiplying by the total number of bottles required by each hospital, pharmacy, workplace, or household. |
| Shipment Origin/Destination | To determine transport costs associated with hospital/pharmacy or workplace caches, the team assumed that MCM would be shipped directly from pharmaceutical distributors. The team determined the location of a representative, authorized Pfizerb distributor located within Minnesota for use as an origin zip code. The representative urban and suburban zip codes identified served as the destination zip codes. |
NOTE: The team assumed no additional transportation costs would be incurred post-event, since MCM would already be positioned at PODs. In some cases, additional transport could be required to move product held in a central facility to decentralized PODs. However, these costs generally represent opportunity costs, as organizations would typically use their own assets to move product and would not pay out of pocket for services provided by commercial carriers.
bPfizer is a major manufacturer of Vibramycin.
Inventory Management
Once MCM had been purchased and had arrived at storage facilities, hospitals, pharmacies, and workplaces would incur additional costs related to maintaining inventory, including labor, storage, and inventory replenishment costs. While costs related to labor and storage do not apply to the MedKit dispensing strategy, inventory replenishment costs do. Cost components and key assumptions related to inventory management are shown in Table D-4.
Dispensing
Dispensing costs are incurred post-event and include salaries for administrative staff, supplemental nurses, and security personnel, as well as costs
TABLE D-4
Inventory Management-Related Cost Components and Key Assumptions
| Inventory Management-Related Cost Component | Key Assumptions |
| Labor and Storage Cost/Pallet | To determine labor and storage costs, the team assumed a cost per pallet derived from an average of two estimates provided by interviewees. In the absence of additional data to differentiate further among prepositioning locations, the team held this cost/pallet estimate constant for hospitals/pharmacies and workplaces. |
| Total Pallets Requiring Storage | To estimate total pallet requirements, the team referenced a report on the Cities Readiness Initiative (CRI) in Philadelphia, which indicated that a pallet can hold 10,000 bottles (Baccam, 2007). Assuming total population estimates for each scenario, as described above, the team was able to determine the total pallet requirement associated with holding inventory on site. |
| Product Expiry | For purposes of this analysis, the team assumed a product expiry of 1 year. Since hospitals and pharmacies manage their own supply and distribute doxycycline for other purposes, the team assumed that they could manage their inventory on a first-in/first-out basis, thereby eliminating the need to replenish inventory every year. In the workplace and MedKit scenarios, products would require full replenishment each year. Replenishment includes costs associated with replacing product in full, as well as shipping new product to prepositioning locations. |
associated with training and operations. Note that dispensing costs are applicable to all strategies considered, with the exception of MedKits. Cost components and key assumptions related to dispensing are shown in Table D-5.
Dispensing Speed
Dispensing speed is a factor in the throughput at each dispensing location. To determine the total speed associated with dispensing, the team assumed varying throughput estimates per dispensing strategy employed. Key assumptions are shown in Table D-6.
TABLE D-5
Dispensing-Related Cost Components and Key Assumptions
| Dispensing-Related Cost Component | Key Assumptions |
| Salaries for Administrative Staff | To estimate salaries for administrative staff on the day of dispensing, the team assumed that the number of staff required to implement each dispensing strategy should reflect the same staff-to-patient ratio as that expected for PODs. According to one interviewee, an average POD operates with 300 administrative staff per 24-hour period. Assuming that 20 PODs would serve a total population of 1.7 million and that only one representative from each household would collect MCM, the team derived the total number of patients each POD would be expected to serve. Assuming a constant staff-to-patient ratio, the team estimated total salary costs by determining the staffing requirements for each dispensing strategy, assuming an average hourly wage of $18.64 (Zaric et al., 2008). |
| Supplemental Nurses | The team assumed that workplaces would incur additional costs associated with employing supplemental nurses to aid in dispensing. One study assumes two supplemental nurses on the day of dispensing for a closed POD (Lee, 2011). The team maintained this assumption for large workplaces, but assumed that small workplaces and hospitals/pharmacies would require only one supplemental nurse/shift worked. |
| Additional Security Measures | In assessing costs associated with employing additional security measures, the team assumed that hospitals have sufficient such measures in place and would not incur additional security costs, but that pharmacies might employ a security guard at $29.01 per hour, representing the average hourly wage for a police officer in the Minneapolis- St. Paul area as indicated by the U.S. Bureau of Labor Statistics (BLS, 2010). To determine security requirements for workplaces, the team assumed the same security guard-to-patient ratio as that for PODs, as recommended by Bioterrorism and Epidemic Outbreak Response Model (BERM) (AHRQ, 2011). |
| Nonlabor Costs | As with the Georgia Institute of Technology study, the team assumed additional administrative costs for pharmacies and workplaces of $5,000 per day to cover all other nonlabor costs associated with dispensing MCM (Lee, 2011). The team also referenced study estimates for training of $5,000-$50,000 per site, assuming annual training. The team estimated training at the lower end of this spectrum for small workplaces and on the higher end for large workplaces. No additional training costs were included for hospitals and pharmacies, as the team assumed that their staff already possess requisite skills for dispensing. |
TABLE D-6
Key Assumptions About Throughput for Dispensing Locations
| Dispensing Location | Key Assumptions |
| Large Workplaces and PODs | For large workplaces and PODs, the team estimated a throughput of 1,000 people per hour. This estimate is the gold standard for throughput time, as indicated by interviewees and as identified during the team’s literature review. |
| Small Work-places, Hospitals, and Pharmacies | For smaller workplaces, hospitals, and pharmacies that are less well equipped to dispense MCM, the team assumed a throughput rate of 100 people per hour, as was determined feasible over the course of the interviews. |
OBSERVATIONS FROM STRATEGY COMPARISONS
By leveraging its literature review and interviews, the team constructed a model for estimating the overall cost and dispensing time for each of the antibiotic dispensing strategies. These estimates were calculated for the dispensing of a 10-day prophylactic course to each of the 1.7 million individuals in the Minneapolis-St. Paul MSA. This section presents the data on costs, dispensing times, and the trade-offs between these two variables for all five dispensing options. Figure D-8, D-9, and D-10 illustrate these estimates. Each of the antibiotic dispensing strategies is analyzed in greater depth to determine the sources of variability in cost and dispensing time and provide a brief overview of the strategic implications of these data.
Figure D-8 shows the dispensing time for each of the strategies. While the SNS-RSS-POD baseline is estimated to exceed the CRI target time of 48 hours, all other dispensing strategies fall below the 48-hour ceiling. For the prepositioning strategies, the public POD component has a considerably longer dispensing time than that of hospitals, pharmacies, or workplaces; the same dynamic occurs for the postal model.
Figure D-9 depicts the overall cost for each of the dispensing strategies. The home MedKit strategy costs substantially more than any other option. The hospital/pharmacy model has a slightly lower overall cost than the SNS-RSS-POD option, and these two strategies are easily the two lowest-cost.
Figure D-10 illustrates the trade-offs between cost and dispensing time for each of the strategies. The home MedKit option is the clear outlier, with a very high cost and a negligible dispensing time. The hospital/pharmacy and postal models fare best in terms of balancing cost-efficiency with speed of dispensing.
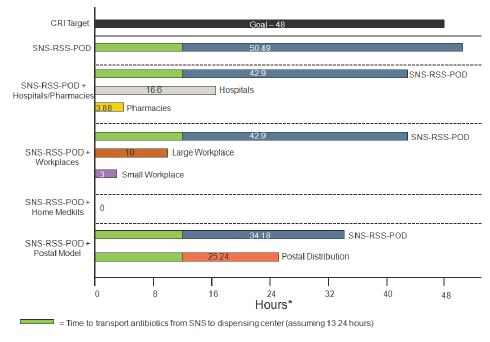
FIGURE D-8
Comparison of times to dispensing of first 10-day supply for prepositioning strategies.
*Distribution speed should include margin of error to accommodate varying throughput estimates.
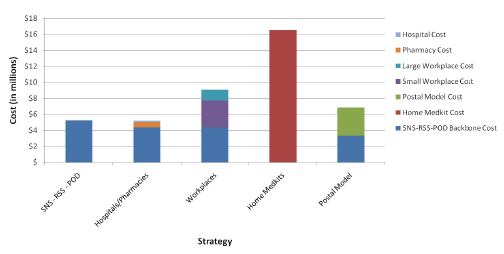
FIGURE D-9
Comparison of overall strategy costs.
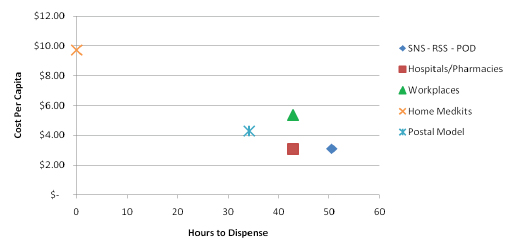
FIGURE D-10
Comparison of per capita costs and dispensing times.
Observations on the SNS-RSS-POD Baseline Scenario
The primary baseline scenario is the traditional SNS to RSS to POD model. In the pre-event stage, antibiotics are stored centrally at the SNS. When an event has been detected and the decision is made to mobilize SNS antibiotics, they are shipped to state-managed RSS sites and then distributed to locally administered PODs. This is the current modus operandi for the majority of U.S. localities in the event of an anthrax attack. Moreover, with the exception of the home MedKits model, each of the other prepositioning strategies includes a component that is served by the SNS-RSS-POD model; these options utilize more than one complementary strategy.
The SNS-RSS-POD model is the second-least costly of the five scenarios. The low cost and low speed of dispensing stem from the same central feature: this strategy utilizes a small number of dispensing sites that can leverage economies of scale to serve large population groups. Interviews indicated that the case study MSA has 20 PODs and a population of 1.7 million; each POD effectively serves 85,000 individuals. Given that a head of household can obtain MCM for his/her immediate family, the average POD will have to process only 37,281 individuals. Interviews and the literature review indicated that the throughput for a POD is 1,000 individuals per hour; only large workplaces, with similar economies of scale,
are assumed to achieve a similarly high throughput. The PODs’ economies of scale also yield benefits in terms of lower overall dispensing, security, and training costs as compared with the smaller-scale hospital/pharmacy and workplace models.
On the other hand, the SNS-RSS-POD model features the longest overall dispensing time. Moreover, the data analysis indicates that the SNS-RSS-POD model’s estimated antibiotic dispensing time of 50.49 hours would exceed the CRI goal of 48 hours by roughly 2.5 hours. Given the throughput, there are simply too many individuals per POD to dispense all of the antibiotics within the 48-hour goal. There are other inherent challenges to the POD-only approach. Because of the potential pressure of time and uncertain psychosocial responses of a population subject to a biological attack, security becomes an essential adjunct to maintain the desired throughput. PODs also are highly dependent on volunteers to staff the process, and there is no guarantee that workers will report for duty in the event of an attack.
To meet the CRI requirements using this strategy, the throughput or number of PODs would have to be increased. Alternatively, complementary strategies could be leveraged to offload a portion of the public from the SNS-RSS-POD model; this option is examined with the hospital/pharmacy cache, workplace cache, and postal distribution models.
Observations on Caching in Hospitals and Pharmacies
The hospital/pharmacy strategy is by far the least expensive prepositioning option, and it is even slightly less costly than the SNS-RSS-POD baseline strategy. Several factors account for the relatively low cost of this option. First, hospitals and pharmacies are staffed by trained medical professionals; unlike the workplace option, this strategy requires no training or supplemental nurses. Second, the security costs of this strategy have the potential to be inherently lower or minimal; hospitals already have a security presence, while one officer can likely provide sufficient security for a pharmacy. In contrast, workplace and POD dispensing options entail moderate security costs, and the postal option entails a large security cost ($1.03 million for the postal component alone). In the event of a biological attack, it is likely that all dispensing approaches and sites would require additional security; for this study, the team estimated the level of security that would be needed.
It is important to note that hospitals and pharmacies can make use of managed inventory, an approach that lowers potential replenishment costs. Under this approach, hospitals and pharmacies rotate antibiotic stock on a first-in/first-out basis that minimizes the costs of replacing the medication. An additional benefit is the ability to routinely track and manage manufacturer recalls for defective batches of antibiotics. Hospitals and
pharmacies could expand the size of their pre-existing antibiotic stocks, which could provide a sufficient quantity of antibiotics in the event of an anthrax attack. The routine hospital or pharmacy utilization of antibiotics, particularly doxycycline, would determine what percentage of the contingency supply would be used in a given year and what amount would need to be replenished.
The hospital and pharmacy dispensing time of 42.9 hours is roughly midway between the postal model (34.18 hours) and the SNS-RSS-POD option (50.49 hours). Under the assumption that 20 percent of the MSA population would receive antibiotics from hospitals and pharmacies, the rate-limiting component of this strategy is the 80 percent of the population that would go to public PODs.
Figures D-11 and D-12 are notional representations of the number of hospitals and pharmacies in the Minneapolis-St. Paul MSA. The MSA has 19 hospitals2 and an estimated 310 pharmacies.3 By utilizing these locations as prepositioning and dispensing sites, this approach would greatly increase the number of antibiotic dispensing sites in the MSA. With a 20 percent population burden, the hospital/pharmacy sites would complete dispensing well before the public PODs. Moreover, offloading 20 percent of the population from the public PODs would decrease their dispensing time by nearly 8 hours. This reduction in dispensing time would place the SNS-RSS-POD strategy 5.1 hours below the CRI recommendation of 48 hours.
Observations on Caching in the Workplace
The workplace prepositioning option entails considerably higher costs than the SNS-RSS-POD model (73 percent higher) or the postal distribution model (25 percent higher). Conceptually, the workplace model is most similar to the hospital/pharmacy model; it is worthwhile to analyze the component costs to uncover why the workplace option is roughly 75 percent more expensive than the hospital/pharmacy option. First, workplaces would require considerable training (the working assumptions are $50,000 per large workplace and $5,000 per small workplace [Lee, 2011]) in properly storing and dispensing antibiotics; hospitals and pharmacies already are properly staffed and equipped for these functions. Second, since the vast majority of workplaces lack trained medical staff, their dispensing labor would have to be augmented by supplemental nurses, whose training to predict or manage associated adverse events would be highly varied. Third, workplace caches would not benefit from routine utilization of the stored antibiotics, which would have to be replaced and replenished at least
![]()
3Derived from National Association of Chain Drug Stores estimate of 56,000 pharmacies throughout the United States.
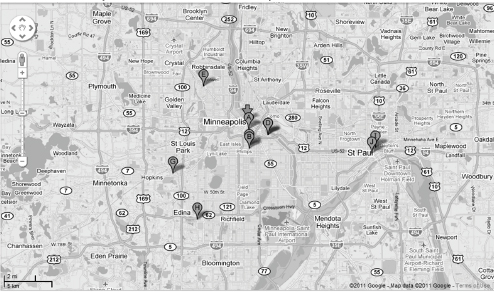
FIGURE D-11
Google map depiction of hospitals in the Minneapolis-St. Paul metropolitan statistical area (MSA).
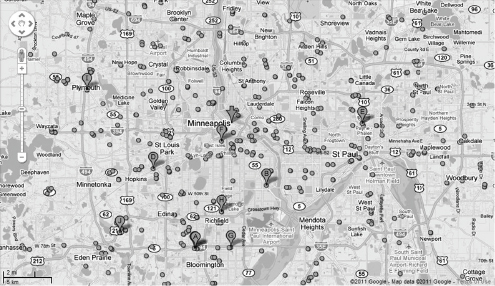
FIGURE D-12
Google map depiction of pharmacies in the Minneapolis-St. Paul metropolitan statistical area (MSA).
yearly under current FDA requirements. Finally, while large workplaces offer significant economies of scale, small workplaces yield a distinct disadvantage in this regard. Assuming 567 small workplaces of 300 individuals each, considerable fixed costs are associated with training, augmenting with supplemental nurses, and shipping MCM for each workplace. Large workplaces offer greater economies of scale than small workplaces; on a per capita basis, small workplaces are roughly 251 percent more costly. This differential suggests that a workplace prepositioning strategy focused more heavily on large workplaces would be more cost-effective.
The dispensing time for the workplace option is 42.9 hours, which is equivalent to that for the pharmacy and hospital prepositioning strategy. The same dynamic comes into play: the public POD component of this strategy is the rate-limiting factor.
The literature review (Lee, 2011) and interviews indicated that 20 percent is a reasonable assumption for the proportion of the population that could be served by prepositioned workplace caches; the team chose the same assumption for the hospital/pharmacy option to allow for an equivalent comparison. An analysis of these two strategies suggests that overall dispensing time for both could be lowered further if a higher proportion of the population could be served by workplaces or hospitals/pharmacies, as opposed to public PODs.
Observations on Caching in the Home (MedKits)
The home MedKit strategy features the highest cost and shortest dispensing time. This strategy yields a dispensing time of essentially zero; the MedKits would be stored pre-event in individual homes, and the team assumed they would not need to be distributed in the event of an anthrax attack. However, home prepositioning carries a significant financial cost. At $16.54 million, this approach is 215 percent more costly than the SNS-RSS-POD baseline scenario and 127 percent more costly than the postal model. It should be noted that the team used an extreme case of this strategy for illustrative purposes, assuming no use of PODs for distributing the initial 10-day prophylactic course of antibiotics.
The high cost of the home MedKit option is due primarily to two factors. First, the cost of the MedKit includes much more expensive packaging than that entailed in any other option. Home MedKits would cost $5.12 per person for a 10-day course of doxycycline, while the equivalent cost for all other options is considerably less. Second, there is a high distribution cost ($5.45 million) for shipping the medication to each individual’s home. With the exception of the postal model, all other options entail antibiotics being shipped in larger quantities to fewer locations. The cost of telephone prescreening for home MedKits is comparable to the labor cost of screen-
ing at public PODs; thus this cost does not represent an additional burden relative to the baseline scenario.4
It is important to note that this option also features the highest replenishment costs ($14.51 million annually). Under current FDA Emergency Use Authorization (EUA) regulations, each home MedKit would have to be replaced annually. Thus, annual replenishment costs would include the full cost of the MedKit itself and the transportation cost; this model assumes that telephone screening would not be necessary on an annual basis, but that some degree of rescreening would be necessary on a semiannual basis.
Observations on the Postal Distribution Model
The prepositioning strategies were also compared with the postal distribution model. This model has been adopted much less widely than the SNS-RSS-POD model. However, there is a standing executive order for the United States to establish a postal MCM dispensing capability, and the Minneapolis-St. Paul MSA is carrying out an ongoing postal distribution pilot project. Thus, it is worthwhile to compare the prepositioning strategies with this postal distribution model.
The postal distribution model ranks third out of five strategies for overall cost. Its cost falls roughly halfway between the SNS-RSS-POD model and the workplace cache option, and is less than half that of the home MedKit model. The postal model does not place a heavy emphasis on screening recipients, and it delivers one 10-day course of doxycycline to each household, regardless of the number of residents. Thus, compared with other models, its dispensing costs are relatively low. On the other hand, the requirement for one police officer paired up with each postal worker yields a higher security cost ($1.03 million) for only a 12-hour operational period.
This model also is notable for its relatively rapid dispensing. The postal model is second only to home MedKits in terms of overall distribution speed. Through the postal model, each household would receive one 10-day course of antibiotics in 25.24 hours: 13.24 hours for transporting the medication from SNS to RSS to post office and 12 hours for postal workers to deliver it. Under the current concept of operations, the remaining doses to complete 10-day courses for the MSA would be provided through the
![]()
4Prescreening for MedKits is not an additional cost relative to public PODs. People at public PODs are screened as well, but that screening takes place the day of the event, rather than beforehand. The team reasons that the screening time, and hence the costs, are fairly similar. In fact, the team based its estimate of prescreening labor and cost for MedKits on the time it would take to screen individuals at a public (or for that matter, closed) POD.
traditional SNS-RSS-POD model. The rate-limiting step in this strategy is the SNS-RSS-POD component, which is estimated to take 34.18 hours.
CASE METROPOLITAN STATISTICAL AREA FOR COMPARISON: MINNEAPOLIS-ST. PAUL
The team assessed the differences associated with employing each dispensing strategy in geographic areas with varying degrees of population density. To conduct this analysis, the team selected representative zip codes that closely reflect the population density of an urban, suburban, and rural setting (see Figure D-13) (Zipskinny, 2000). Representative zip codes provide population and distance assumptions that were used to estimate the cost and speed of distribution to these areas.
The team selected the most densely populated zip code to represent an urban environment and one relatively less dense to reflect a suburban population. Note that among other factors, the U.S. Census Bureau classifies urban areas as densely settled territory consisting of “core census block groups or blocks that have a population density of at least 1,000 people per square mile and surrounding census blocks that have an overall density of at least 500 people per square mile” (U.S. Census Bureau, 2011). Areas
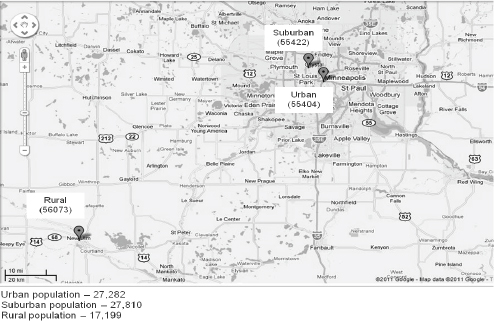
FIGURE D-13
Google map depiction of selected representative urban, suburban, and rural zip codes in Minnesota.
that do not meet this criterion are classified as rural. No specific definition is provided for suburban areas. Since the postal model serves only urban and suburban areas, the team selected an alternative zip code within the vicinity of Minneapolis-St. Paul as representative of a rural area.
When performing the calculations for the populations in each zip code, the team noted no significant quantitative differences among strategies across the different areas. Costs and speed of distribution are virtually the same for the representative zip codes using the data that were collected. It is likely that such variables as number of pharmacies and hospitals or ratio of large to small businesses would differ across zip codes. However, these data were unavailable. In lieu of a quantitative analysis, this section provides a qualitative discussion of how the various strategies would differ across geographic settings.
Urban Area Profile
The high density of urban areas can carry many advantages and disadvantages in terms of antibiotic dispensing. First, a greater number of people would be vying for access to PODs, which could create much longer lines relative to less densely populated areas. However, people would not have to travel as far to get to a POD since there would likely be a greater number of PODs per square mile in an urban area.
Urban areas also are likely to have more hospitals, pharmacies, and workplaces per square mile than suburban and rural areas. This feature of urban areas could provide more POD options to the general public and thus could relieve the pressure on any one POD or strategy. Urban health departments also tend to be larger, with more personnel, than those in suburban and rural areas. They would have more specialized personnel as well (e.g., an urban health department could have an emergency planner, whereas a rural area could not support such a position). Therefore, urban environments would have a greater workforce available to staff PODs.
In addition, many urban areas have a large commuter workforce. It is safe to assume that the population of an urban area is higher during the day than at night, when commuters return to suburban or rural areas. Planning for dispensing would need to account not only for population density, but also for the population that did not necessarily reside in the area but was located there during the workday. Tourism is another factor that could increase the population of an urban area at any given time.
Suburban Area Profile
Suburban areas are the most difficult areas to define. As noted, the U.S. Census Bureau does not even provide a definition for a suburban area.
These areas can have many characteristics of both urban and rural areas, as their population density can vary widely between the two.
One unique characteristic of a suburban area is that most residents have cars. Some locales have run exercises showing that drive-through PODs are a highly effective model for suburban areas. These PODs would function like a drive-through restaurant in that people would not have to leave their cars to receive MCM.
As mentioned above, one also must account for the commuter population. Many suburban residents will have workplaces in the city, so the population of a suburban area will be greater at night and on weekends than during the day on weekdays.
Rural Area Profile
The smaller population density of a rural area means that the population is much more spread out than in urban and suburban areas. If planning accounts for a POD to serve a standard number of people, the number of PODs will be much lower in a rural area. With PODs being more spread out, it is safe to assume that travel times to reach them will be much longer. This could be a disadvantage if it takes a long time to get to a POD; however, it could also be an advantage if arrival times are staggered, which could reduce POD queues. Another factor to consider is the length of time it would take for a POD to receive MCM from the RSS. Rural areas are locations where prepositioning could particularly save time. However, they are likely to have fewer pharmacies, hospitals, and businesses in which prepositioning could occur.
In addition, health departments in rural areas have fewer employees. The employees also are less specialized, so there is likely less manpower devoted to emergency planning. Moreover, fewer public health employees would be available to man PODs.
One interesting model for dispensing MCM in rural areas is what one interviewee referred to as the “school bus” model. This model would involve loading a school bus or equivalent with MCM, basically serving as a mobile POD that would travel to predetermined locations in rural areas to deliver the MCM to the public.
ALTERNATIVE DISPENSING STRATEGIES
For this study, the team identified the alternative MCM dispensing strategies depicted in Figure D-14.
The current strategy for distributing antibiotics relies on the SNS-RSS-POD model, which is a centralized to decentralized model. As noted earlier, the SNS is contained in a set of central storage sites, which is funded by
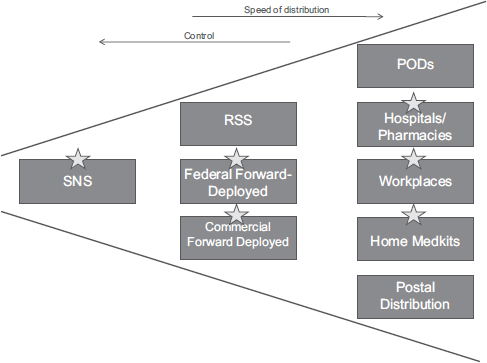
FIGURE D-14
Comparison of alternative dispensing strategies.
NOTE: The stars indicate possible storage locations.
the federal government; these sites also are set up and staffed by the federal government. The RSS sites reside under either state or local control, depending on the locale. These are simply throughput sites used for receiving MCM from the SNS and distributing them to PODs. The PODs themselves are the most decentralized. The number of PODs and their locations are determined by local authorities.
One advantage of the medications being controlled by the federal government is the Shelf Life Extension Program (SLEP). If not controlled by the federal government, MCM must be replaced annually in accordance with prescription laws. The number of years for which MCM can be extended under SLEP is determined by the FDA; in general, however, SLEP could double or triple the shelf life of these medications, which would lead to lower replenishment costs. However, this advantage must be weighed against the fact that tetracyclines can show significant decreases in efficacy and increases in adverse events over short periods of time.
In addition to avoidance of yearly replenishment costs and/or expiry issues, a federally controlled forward-deployed stock would be geographi-
cally closer to areas that might need it than would be the case if those areas had to rely on the central SNS warehouses. Alternatively, CDC has investigated the possibility of decreasing the distribution time from the SNS to PODs by having more regional storage sites. This would, in theory, remove the RSS stage of the process while retaining federal control so SLEP could be applied. CDC expects that this model could decrease the distribution time from the SNS to PODs from around 12 hours to around 6 hours.
Other examples of facilities that could be used for federal forward-deployed stocks are VA or DOD medical storage facilities. The VA is experienced with caching as it currently stores many medications and medical supplies on VA property. Storing MCM in existing warehouses on federal property could greatly reduce storage costs over the use of contracted warehouses. The VA has many central hospitals and other facilities located in major metropolitan areas, as well as clinics and other facilities spread throughout cities. In Minneapolis, the VA hospital is centrally located (see Figure D-15), and the many clinics located around the city could serve as
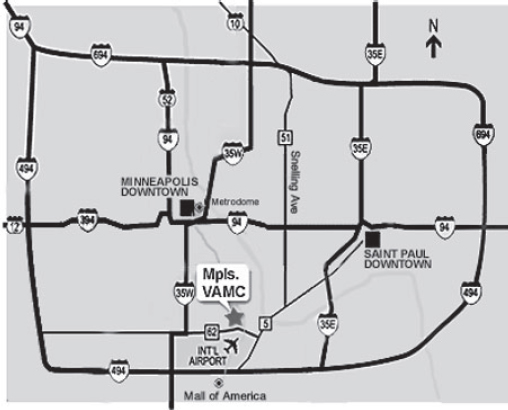
FIGURE D-15
Location of the Department of Veterans Affairs (VA) hospital in Minneapolis.
PODs. The VA also has medical staff on site who could assist with dispensing. Similarly, DOD medical treatment facilities could be used, although they are fewer in number and restricted to areas where they are collocated with military installations.
Another option is a commercially controlled forward-deployed stock. One example is a pharmaceutical distributor, where MCM could serve as vendor-managed inventory. For example, New York City has been working with pharmaceutical distributors to hold extra inventory in their chains. Pharmaceutical distributors have agreed to keep extra stock of antibiotics on hand, and the department of health has agreed to pay the cost difference for storing the extra medication. The cost is pennies on the dollar. This strategy brings the MCM closer to the population because pharmaceutical distributors are usually regionally located. These distributors also are selling these drugs daily for normal medical use, and by using the first in/first out approach could avoid the expiry issue that most caching strategies entail. Also, pharmaceutical distributors store and deliver medications every day and can quickly alter their destination sites over a wide area based on demand. Therefore, they may be better equipped to handle these tasks during an emergency than an entity that does not perform these tasks daily. However, as these resources would be outside of immediate federal control, there may be trade-offs as far as resource prioritization and decision-to-action cycle time.
Through these upstream changes, downstream distribution and dispensing could occur much more rapidly. Any of these forward-deployed stocks could be distributed to traditional public PODs, closed PODs, or alternative dispensing sites. Moving stocks farther downstream pre-event could dramatically reduce overall dispensing time. Many of these mechanisms also could serve to decrease overall costs.
ADDITIONAL CONSIDERATIONS
This section addresses some additional considerations that were high-lighted during the course of the team’s research. These considerations fall into six categories: variability, liability, amount of medication required, efficiency, packaging, and ongoing prophylaxis. These considerations are challenges to the implementation of any prepositioning strategy.
Variability
• State/Local Capability: It is difficult to speak of any of the costs or benefits of alternative dispensing strategies in absolute terms since many variables depend on the state or local capability. For example, many states have a health department run by the state itself,
whereas others have a conglomeration of local or regional health departments. States vary as well in size of population, population density, budget, and storage space. Thus it is difficult to make assumptions that will apply to all locations, although there are issues that apply to all states.
Liability
• Product Approval: Since the medications are being prescribed for use outside of their normal purview, each strategy requires an EUA for an investigational new drug (IND). This is much easier to achieve when the drugs remain under federal control until they are ready for dispensing, but is far more difficult for home MedKits. Doxycycline, like any other prescription medication, carries a high risk of adverse reactions if proper patient assessment by a clinician does not occur. The team’s analysis does not address the time and cost of acquiring an EUA for placing antibiotics in the home, which can be a time-consuming and costly process.
• Return and Disposal of Expired Antibiotics: What will be done with expired home MedKits needs to be considered. If MedKits are to be returned to an official location after expiry, the cost of return shipping must be accounted for. Simply asking the public to throw away their MedKits after expiry poses a substantial risk since doxycycline becomes toxic and can cause kidney damage once it has expired (Drugs.com, 2009).
Amount of Medication Required
• Uncertainty of Household Needs: An additional consideration for the postal distribution model is the number of pills to be handed out. In the home MedKit model, each person receives enough pills to last for 10 days. In the postal model, each household receives 20 pills, regardless of the number of residents. The result could be increased pressure on PODs for those households with large numbers of people.
• Need for More Medication Overall with Prepositioning: Any prepositioning strategy will require medications farther downstream relative to more centralized strategies. Therefore, more antibiotics will have to be purchased overall to acquire enough to fill each cache in each location. If each location requires enough antibiotics to cover its population, those drugs will have to be purchased in addition to what is currently held in the SNS. The cost of all these additional antibiotics must be considered.
• “Double Dippers”: The more prepositioning strategies are employed, the more “double dippers” must be accounted for. If people have access to MCM at a workplace, a POD, and a local pharmacy, what is to prevent them from taking advantage of all three? This possibility must be considered when one is looking at the number of antibiotics provided overall in an affected area, as must tracking mechanisms for those who have received medications and those who have not.
Efficiency
• Reliance on Push Packages: Each prepositioning strategy will require the use of a Push Package to get the medications to a POD or to the postal service as soon as possible. An issue with the Push Package is that it does not contain just antibiotics. The Push Package consists of 130 cargo containers with a combined weight of 50 tons (Baccam, 2007). This means that in addition to the antibiotics needed for an anthrax attack, an RSS would receive material that might not be necessary initially for that emergency. The result would be extra cost for weight and transport, as well as extra time needed to sort through the pack to get to what is really needed. And what is to be done with the remaining materials that are not needed?
• Throughput: The team found that the rate-limiting factor is not speed of transportation but speed of dispensing. Prepositioning closer to the impacted locale can greatly increase speed, but without the manpower to dispense the MCM, that gain in speed becomes moot. Most state and local health authorities speak about throughput goals; however, they all wish for higher throughput. Most mention a goal of 1,000 people per hour, but in large cities with populations in the millions, even this goal could overwhelm the POD system. More effort should be expended on finding ways to increase the rate of dispensing.
Packaging
• Packaging Efficiency: Antibiotics in the Push Package are stored in unit-of-use bottles (20 pills to a bottle). The bottles are spacious for the number of pills they contain. This leads to the need for increased storage space for the antibiotics, which in turn leads to increased storage costs. Also, the pill bottles can be too large for some mail slots in the postal model. A more efficient practice could be the production of smaller unit-of-use pill bottles.
• Scalability of Labor for Breakdown and Packaging: Many strategies involve receiving the MCM in bulk. In fact, all medications coming from the SNS-managed inventory (not the Push Package) are delivered in bulk. Extra costs are entailed for materials and labor to portion out the medications in the appropriate dose. For example, the Minnesota Department of Health portions out antibiotics for the MedKits for postal volunteers. This is no small undertaking. It requires many hours of labor for two trained medical professionals to place the pills into bottles, label the bottles, and ensure that the correct medications are going to each home. Scaling this amount of labor and materials to meet the demand for a larger population would be unwieldy. Also, taking time to portion out medications while PODs are running during an event would increase dispensing time and labor costs.
Ongoing Prophylaxis
• Dispensing Strategy for a 60-Day Courses to Cover the Population: Each prepositioning strategy covers only the initial immediate need for antibiotics. A concrete strategy is needed for providing the rest of the 60-day course to those who are impacted. There will be additional pressure on PODs to provide the rest of the course, as well as adherence issues for the public with respect to finishing the course (see below). In addition, more clinical studies are needed to better determine the long-term safety impact of 60-day therapy with doxycycline in large populations.
• Antibiotic Resistance: One negative effect of failure to complete an antibiotic course is antibiotic resistance. Adherence is a major issue for any dispensing strategy. The development of an antibiotic resistant strain of anthrax following an anthrax attack would be a very unfortunate outcome.
CONCLUSIONS
This study has attempted to estimate the costs and time savings associated with each of the three identified prepositioning strategies, as well as other possible approaches. It is not intended as an exhaustive cost/benefit analysis for use in determining whether any of these prepositioning strategies should be deployed. As events and circumstances frequently do not occur as expected, there may be material differences between the estimates in this paper and actual outcomes.
The analysis does suggest that the strategy of caching in hospitals and pharmacies and the delivery of antibiotics through the U.S. postal system
both could yield significant time savings without a commensurate increase in cost. These approaches could be further enhanced through the use of regional warehousing that would position the antibiotics closer to the impacted population than the current SNS model. Home MedKits, although comparatively expensive, could be appropriate for certain segments of the population for whom immediate availability of antibiotics would be worth the cost, such as essential first responders. In any city or region that chooses to preposition antibiotics, it is likely that a combination of these strategies should be considered.
While PRTM has attempted to add some quantitative dimension to the cost and time of prepositioning strategies through this paper, many uncertainties remain. Access to additional data will clarify some unknowns, as will the continued evolution of federal and state prepositioning policies. Further study of the relative benefits and trade-offs of each of these strategies would be required to provide more concrete recommendations for prepositioning MCM based on quantitative analysis.
REFERENCES
AHRQ (Agency for Healthcare Research and Quality). 2011. The Weill/Cornell Bioterrorism and Epidemic Outbreak Response Model (BERM). http://www.ahrq.gov/research/biomodel3/ (accessed September 8, 2011).
Baccam, S. 2007. Cities Readiness Initiative (CRI) postal plan: Philadelphia operational drill June 23-24, 2007. Research Triangle Park, NC: Innovative Emergency Management.
BLS (U.S. Bureau of Labor Statistics). 2010. Occupational Employment Statistics Query System. Selected “Minneapolis/St. Paul/Bloomington MSA.” http://data.bls.gov/oes/search.jsp?data_tool=OES (accessed September 8, 2011).
CDC (Centers for Disease Control and Prevention). 2008. Emergency MedKit evaluation study. Atlanta, GA: CDC-Office of Science and Public Health Practice.
CDC. 2010a. Cities Readiness Initiative. http://www.bt.cdc.gov/cri/ (accessed September 8, 2011).
CDC. 2010b. Strategic National Stockpile (SNS). Atlanta, GA: CDC-SNS, http://www.bt.cdc.gov/stockpile/ (accessed February 16, 2011).
Drugs.com. 2009. Tetracycline. http://www.drugs.com/tetracycline.html (accessed September 8, 2011).
Friedlander, A. M., S. L. Welkos, M. L. M. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, and W. B. Lawrence. 1993. Postexposure prophylaxis against experimental inhalation anthrax. The Journal of Infectious Diseases 167:1239-1242.
Hamburg, M. 2010 (August 23). Reply to BARDA request for FDA approval of an EUA for doxycycline. http://www.fda.gov/downloads/EmergencyPreparedness/UCM229682.pdf (accessed September 8, 2011).
Jernigan, J. A., D. S. Stephens, D. A. Ashford, C. Omenaca, M. S. Topiel, M. Galbraith, M. Tapper, T. L. Fisk, S. Zaki, T. Popovic, R. F. Meyer, C. P. Quinn, S. A. Harper, S. K. Fridkin, J. J. Sejvar, C. W. Shepard, M. McConnell, J. Guarner, W. J. Shieh, J. M. Malecki, J. L. Gerberding, J. M. Hughes, and B. A. Perkins; Anthrax Bioterrorism Investigation Team. 2001. Bioterrorism-related inhalational anthrax: The first 10 cases reported in the United States. Emerging Infectious Diseases 7(6):933-934.
Lee, E. 2011 (unpublished). Analysis of large-scale medical countermeasure dispensing: Multi-modality and cost-effectiveness. Industrial and Systems Engineering, Georgia Institute of Technology.
Medscape Reference. 2010. Tetracycline. http://reference.medscape.com/drug/tetracycline-342550#90 (accessed September 8, 2011).
Minnesota Department of Administration. 2000. Minnesota household profile of general demographic characteristics from Census 2000. http://www.demography.state.mn.us/Cen2000profiles/cen00profhh.html (accessed September 8, 2011).
Plessas, J. 2010. The postal model. Washington, DC: United States Postal Service, http://www.authorstream.com/Presentation/aSGuest58704-459527-plenary-plessas/ (accessed September 9, 2011).
Roos, R. 2008. To blunt anthrax attack, mail carriers to get antibiotics. CIDRAP News, October 2.
UPMC Center for Biosecurity. 2007 (November 8). Bacillus anthracis (anthrax). Baltimore, MD: UPMC Center for Biosecurity, http://www.upmc-biosecurity.org/website/our_work/biological-threats-and-epidemics/fact_sheets/anthrax.html (accessed September 8, 2011).
U.S. Census Bureau. 2011. Census 2000 urban and rural classification. http://www.census.gov/geo/www/ua/ua_2k.html (accessed September 8, 2011).
Zaric, G. S., D. M. Bravata, J.-E. Cleophas Holty, K. M. McDonald, D. K. Owens, and M. L. Brandeau. 2008. Modeling the logistics of response to anthrax bioterrorism. Medical Decision Making 28(3):332-350.
Zipskinny. 2000. Zipskinny. www.zipskinny.com (accessed September 8, 2011).
This page intentionally left blank.
Appendix D.1
Detailed Data
This appendix provides the calculations that form the basis of the Observations from Strategy Calculations, incorporating the assumptions described in Components of Cost and Speed for Dispensing Strategies. Note that some cells in the following tables have been redacted to protect sensitive information.
TABLE D.1-1
High-Level Overview Data
| Prepositioning Strategy | |||
| 20% Hospitals and Pharmacies; 80% SNS-RSS-POD |
20% Large and Small Workplaces; 80% SNS-RSS-POD |
Home MedKits | |
| Overall Cost | $5,212,761 | $9,096,388 | $16,542,288 |
| Per Capita Cost | $3.07 | $5.35 | $9.73 |
| % Difference in Overall Cost vs. SNS-RSS-POD Baseline | –0.82 | 73.08 | 214.75 |
| % Difference in Overall Cost vs. Postal Model | –28.47 | 24.82 | 127.00 |
| Overall Dispensing Time (hours) | 42.9 | 42.9 | 0 |
| % Difference in Dispensing Time vs. SNS-RSS-POD Baseline | –15.03 | –15.03 | N/A |
| % Difference in Dispensing Time vs. Postal Model | 25.51 | 25.51 | N/A |
| Cost Per Hour Reduction vs. SNS-RSS-POD | –$5,655 | $506,022 | $223,541 |
| Per Capita Cost Per Hour Reduction vs. SNS-RSS-POD | $0.00 | $0.30 | $0.13 |
| Cost Per Hour Reduction vs. Postal Model | N/A | N/A | $270,767 |
| Per Capita Cost Per Hour Reduction vs. Postal Model | N/A | N/A | $0.16 |
| Replenishment Costs (annual) | If vendor-managed inventory is utilized, then replenishment costs are negligible. | $14,154,000 | |
| Replenishment Costs (SLEP) | 0 | ||
| Replenishment Costs (annual + SLEP) | $14,154,000 | ||
| Alternative Strategies | |||
| SNS-RSS-POD | 44% Postal Model; 56% SNS-RSS-POD | ||
| Overall Cost | $5,255,680 | $7,287,466 | |
| Per Capital Cost | $3.09 | $4.29 | |
| Overall Dispensing Time (hours) | 50.49 | 34.18 | |
| Replenishment Costs (annual) | 0 | $42,656 | |
| Replenishment Costs (SLEP) | |||
| Replenishment Costs (annual + SLEP) | |||
NOTE: Due to insufficient information, the SNS-RSS-POD transportation costs have been excluded from our cost calculations.
TABLE D.1-2
SNS-RSS-POD Data
| Costs Description |
Data | Calculations |
| Individuals | 1,700,000 | |
| Households | 745,000 | |
| Product Purchase Price | ||
| Product Purchase Price - Costs per daily dosage- Propylaxis, Doxycycline | ||
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | ||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | ||
| Product Purchase Price - Total Costs for Medication (per household) | ||
| Product Purchase Price - Total Costs for Medication (overall) | ||
| Transportation | ||
| Transportation - SNS to RSS to Postal Office | N/A | not available |
| Transportation Costs (overall) | $0.00 | not available |
| Dispensing | ||
| Dispensing - Labor - Salaries (per POD, per day) | $44,736.00 | 300 staff per POD/day (source: interview with state public health official) x 8 hours/day x $18.64/hr (source: Zaric et al.) |
| Dispensing - Labor - Salaries (20 PODs, per day) | $894,720.00 | Labor per day per POD x 20 PODs |
| Costs Description |
Data | Calculations | |
| Individuals | 1,700,000 | ||
| Dispensing - Labor - Salaries (total) | $1,388,680.00 | 37.25 hours x 1 day/24 hours x $894,720/day | |
| Dispensing - Labor - Training (annual) | $894,720.00 | 300 staff per POD x 8 hours of training/yr x $18.64/hr | |
| Dispensing - Administrative Fees/Operational Costs (daily, per POD) | $5,000.00 | ||
| Dispensing - Administrative Fees/Operational Costs (daily, 20 PODs) | $100,000.00 | $5,000 x 20 PODs | |
| Dispensing - Administrative Fees/Operational Costs (total) | $155,208.33 | 37.25 hours x 1 day/24 hours x $100,000/day | |
| Dispensing - Security (daily, per POD) | $2,784.96 | ||
| Dispensing - Security (daily, 20 PODs) | $55,699.20 | ||
| Dispensing - Security (total) | $86,449.80 | 37.25 hours x 1 day/24hours x $2,784.96/POD per day x 20 PODs | |
| Dispensing - Total Costs | $2,525,058.13 | Labor-salaries (total) + labor-training (total) + security (total) | |
| Inventory Management | |||
| Inventory Management - Labor | |||
| Inventory Management - Cost of Storage/Pallet (yearly) | |||
| Inventory Management - # of Bottles/Pallet | |||
| Inventory Management - # of Pallets Required | |||
| Costs Description |
Data | Calculations |
| Individuals | 1,700,000 | |
| Inventory Management - Storage (total) | ||
| Inventory Management - Total Costs (excluding replenishment costs) | ||
| Inventory Management - Replenishment - Product Purchase (overall) | ||
| Inventory Management - Replenishment - Transportation (overall) | $0 | |
| Inventory Management - Replenishment - Dispensing (overall) | $0.00 | |
| Inventory Management - Replenishment Costs (total, SLEP) | Total costs for product purchase + total costs for dispensing | |
| Total Costs | ||
| Product Purchase Price | ||
| Transportation | $0.00 | |
| Dispensing | $2,525,058.13 | |
| Inventory Management (without replenishment) | ||
| Total Cost (without replenishment) | $5,255,679.73 | |
| Replenishment Costs (SLEP) | ||
| Total Dispensing Time for Strategy | ||
| Costs Description |
Data | Calculations |
| Individuals | 1,700,000 | |
| Dispensing Time - SNS to RSS to POD Transportation (hours) | 13.24 | (source: calculations derived from presentation - Burel, G. An SNS Perspective on Pre-positioning Medical Countermeasures. Centers for Disease Control and Prevention, February 28, 2011. Presented to IOM Committee on Prepositioned Medical Countermeasures for the Public) |
| Dispensing Time - POD Operating Time (hours) | 37.25 | (745,000 households / 20 pods x 1 hr/1,000 households) |
| Dispensing Time for Strategy - Total (hours) | 50.49 | SNS to RSS to POD + POD Operating Time |
TABLE D.1-3
Hospital/Pharmacy Data
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Individuals | 65,758.05 | Population served by hospital derived from calculating patient population and hospital employees from ucomparehealthcare.com | 274,242.95 | (1,700,000 x .20) - (population served by pharmacy) |
| Households | 28,841.25 | 65,758.05 individuals x 1 household/2.28 individuals | 120,282.00 | 274,242.95 individuals x 1 household/2.28 individuals |
| Hospitals/Pharmacies | 19 | Source - ucomparehealthcare.com | 310.1 | 56,000 pharmacies/US (source - National Association of Chain Drug Stores) x US population/307,006,550 individuals (source - U.S. Census Bureau) x 1.7 million in MSA |
| Costs | ||||
| Product Purchase Price | ||||
| Product Purchase Price - Costs per daily dosage - Prophylaxis, Doxycycline | $0.20 | $0.10/pill x 2 pills per day | $0.20 | $0.10/pill x 2 pills per day |
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | $0.01 | $0.01 | ||
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | $0.21 | $0.20 per daily dosage + $0.01 additional medication costs per dosage | $0.21 | $0.20 per daily dosage + $0.01 additional medication costs per dosage |
| Product Purchase Price - Total Costs for Medication (per household) | $2.10 | $0.21/day x 10 days | $2.10 | $0.21/day x 10 days |
| Product Purchase Price - Total Costs for Medication (overall) | $138,092 | (65,758.05 individuals x one 10-day course per individual x $2.10 per 10-day course) | $575,910 | (274,242.95 individuals x one 10-day course per individual x $2.10 per 10-day course) |
| Transportation | ||||
| Transportation - Shipping Medications to Hospitals/ Pharmacies | $353.02 | Source - average estimated shipping cost of USPS and FedEx | $3,310.80 | Source - average estimated shipping cost of USPS and FedEx |
| Transportation (overall) | $353.02 | $3,310.80 | ||
| Dispensing | ||||
| Dispensing - Labor - Salaries (per hospital/pharmacy, per day) | $2,684.16 | 6 staff x 18.64/hr x 8 hr/shift x 3 shifts | $894.72 | 2 staff x $18.64/hr x 8 hr/day x 3 shifts |
| Dispensing - Labor - Salaries (19 pharmacies/310.1 pharmacies, per day) | $50,999.04 | $2,684.16 x 19 hospitals | $277,453 | $894.72 x 566.67 small workplaces |
| Dispensing - Labor - Salaries (total) | $32,256.89 | 15.18 hours x 1 day/24 hours x $266,179.20/day | $44,855 | 3.88 hours x 1 day/24 hours x $507,011/day |
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Dispensing - Labor - Training (annual) | $0.00 | Since hospitals and pharmacies have trained medical staff, assume that no training is necessary (source: Georgia Tech paper) | $0 | Since hospitals and pharmacies have trained medical staff, assume that no training is necessary (source: Georgia Tech paper) |
| Dispensing - Labor - Supplemental Nurses (per hospital/pharmacy, per day) | $0.00 | Since hospitals and pharmacies have trained medical staff, assume that no supplemental nurses are necessary (source: Georgia Tech paper) | $0 | Since hospitals and pharmacies have trained medical staff, assume that no training is necessary (source: Georgia Tech paper) |
| Dispensing - Labor - Supplemental Nurses (19 pharmacies/310.1 pharmacies, per day) | $0.00 | Since hospitals and pharmacies have trained medical staff, assume that no supplemental nurses are necessary (source: Georgia Tech paper) | $0 | Since hospitals and pharmacies have trained medical staff, assume that no training is necessary (source: Georgia Tech paper) |
| Dispensing - Labor - Supplemental Nurses (19 pharmacies/310.1 pharmacies) | $0.00 | Since hospitals and pharmacies have trained medical staff, assume that no supplemental nurses are necessary (source: Georgia Tech paper) | $0 | pharmacies have trained medical staff, assume that no training is necessary (source: Georgia Tech paper) |
| Dispensing - Administrative Fees/Operational Costs (total) | $0.00 | Opportunity cost absorbed by hospital | $0.00 | Opportunity cost absorbed by pharmacy |
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Dispensing - Security (per workplace, per day) | $0.00 | Hospitals already have a security presence | $696.24 | 1 officer x 3 shifts x $29.01/hr x 8 hrs/shift |
| Dispensing - Security (19 pharmacies/310.1 pharmacies, per day) | $0.00 | Hospitals already have a security presence | $215,904.02 | ($696.24 x 310.1 pharmacies) |
| Dispensing - Security (total for 19 pharmacies/310.1 pharmacies) | $0.00 | Hospitals already have a security presence | $34,904.48 | $394,538.32 x 3.88 hours operating time x 1 day/24 hours |
| Dispensing - Total Costs | $32,256.89 | Labor-salaries (total) + labor-training (total) + security (total) | $79,759.33 | Labor-salaries (total) + labor-training (total) + security (total) |
| Inventory Management | ||||
| Inventory Management - Labor | 0 | not available | 0 | not available |
| Inventory Management - Cost of Storage/Pallet per month | $14 | Average of interview data | $14 | Average of interview data |
| Inventory Management - # of Bottles/Pallet | 10,000 | Interview | 10,000 | Interview |
| Inventory Management - # of Pallets Required | 6.58 | 65758.05 bottles x 10,000 bottles/pallet | 27.42 | 274241.95 bottles x 10,000 bottles/pallet |
| Inventory Management - Storage (total/annual) | $1,105 | 6.58 pallets x $14/month x 12 months/1 year | $4,607 | 27.42 pallets x $14/ month x 12 months/ 1 year |
| Inventory Management - Total Costs (annual, excluding replenishment costs) | $1,105 | $4,607 | ||
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Inventory Management - Replenishment - Product Purchase (overall) | $0 | Hospitals and pharmacies can use first-in, first-out managed inventory, which makes replenishment costs negligible. | $0 | Hospitals and pharmacies can use first-in, first-out managed inventory, which makes replenishment costs negligible. |
| Inventory Management - Replenishment - Transportation (overall) | $0 | $0.00 | ||
| Inventory Management - Replenishment - Dispensing (overall) | $0.00 | 0 | ||
| Inventory Management - Replenishment Costs (total, annual) | $0.00 | Total costs for product purchase + total costs for transportation | $0.00 | Total costs for product purchase + total costs for transportation |
| Total Costs | Hospital Component (3.87%, 6,5758.05 individuals) | Pharmacy Component (16.13%, 2,74241.95 individuals) | ||
| Product Purchase Price | $138,091.91 | $575,910.20 | ||
| Transportation | $353.02 | $3,310.80 | ||
| Dispensing | $32,256.89 | $79,759.33 | ||
| Inventory Management (without replenishment) | $1,105 | $4,607 | ||
| Hospital/Pharmacy Component | Hospital | Pharmacy | ||
| Costs Description |
Data | Calculations | Data | Calculations |
| Total Cost (without replenishment) | $171,806.55 | $663,587.61 | ||
| Replenishment Costs (annual) | $0.00 | $0.00 | ||
| Total Costs | Hospitals and Pharmacies Combined (20%, 340,000 individuals) | |||
| Product Purchase Price | $714,002.10 | |||
| Transportation | $3,663.82 | |||
| Dispensing | $112,016.23 | |||
| Inventory Management (without replenishment) | $5,712.02 | |||
| Total Cost (without replenishment) | $835,394.16 | |||
| Replenishment Costs (annual) | $0.00 | |||
| Dispensing Time | Hospitals | Pharmacies | ||
| Dispensing Time - Transportation (hours) | 0 | Caches are prepositioned | 0 | Caches are prepositioned |
| Dispensing Time - Closed POD/ Hospital and Pharmacy Dispensing Time (hours) | 15.18 | 28,841.25 individuals/19 hospitals x 1 hr/100 individuals (throughput) | 3.88 | 120,282 individuals/310.1 pharmacies x 1 hr/100 individuals (throughput) |
| Dispensing Time - Total (hours) | 15.18 | 3.88 | ||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Individuals | 1,360,000 | 1,700,000 - population served by pharmacy/ hospital) | ||
| Households | 596,491 | 1,360,000 individuals x 1 household/2.28 individuals | ||
| Product Purchase Price | ||||
| Product Purchase Price - Costs per daily dosage- Propylaxis, Doxycycline | ||||
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | ||||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | ||||
| Product Purchase Price - Total Costs for Medication (per household) | ||||
| Product Purchase Price - Total Costs for Medication (overall) | ||||
| Transportation | ||||
| Transportation - SNS to RSS to Postal Office | N/A | not available | ||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Transportation Costs (overall) | $0.00 | not available | ||
| Dispensing | ||||
| Dispensing - Labor - Salaries (per POD, per day) | $44,736.00 | 300 staff per POD/day (source: interview with state public health official) x 8 hours/day x $18.64/hr (source: Zaric et. al.) | ||
| Dispensing - Labor - Salaries (20 PODs, per day) | $894,720.00 | Labor per day per POD x 20 PODs | ||
| Dispensing - Labor - Salaries (total) | $1,105,724.80 | 29.66 hours x 1 day/24 hours x $894,720/day | ||
| Dispensing - Labor - Training (annual) | $894,720.00 | 300 staff per POD x 8 hours of training/yr x $18.64/hr | ||
| Dispensing - Administrative Fees/Operational Costs (daily, per POD) | $5,000.00 | |||
| Dispensing - Administrative Fees/Operational Costs (daily, 20 PODs) | $100,000.00 | $5,000 x 20 PODs | ||
| Dispensing - Administrative Fees/Operational Costs (total) | $123,583.33 | 29.66 hours x 1 day/24 hours x $100,000/day | ||
| Dispensing - Security (daily, per POD) | $2,784.96 | |||
| Dispensing - Security (daily, 20 PODs) | $55,699.20 | |||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Dispensing - Security (total) | $68,834.93 | 29.66 hours x 1 day/24 hours x $2,784.96/POD per day x 20 PODs | ||
| Dispensing - Total Costs | $2,192,863.06 | Labor-salaries (total) + labor-training (total) + security (total) | ||
| Inventory Management | ||||
| Inventory Management - Labor | ||||
| Inventory Management - Cost of Storage/Pallet | ||||
| Inventory Management - # of Bottles/Pallet | ||||
| Inventory Management - # of Pallets Required | ||||
| Inventory Management - Storage (total) | ||||
| Inventory Management - Total Costs (excluding replenishment costs) | ||||
| Inventory Management - Replenishment - Product Purchase (overall) | ||||
| Inventory Management - Replenishment - Transportation (overall) | ||||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Inventory Management - Replenishment - Dispensing (overall) | ||||
| Inventory Management - Replenishment Costs (total, SLEP) | ||||
| Dispensing Time | ||||
| Dispensing Time - SNS to RSS to Postal Office Transportation (hours) | 13.24 | (source: calculations derived from presentation - G. Burel. An SNS Perspective on Pre-positioning Medical Countermeasures. Centers for Disease Control and Prevention, February 28, 2011. Presented to IOM Committee on Prepositioned Medical Countermeasures for the Public) | ||
| Dispensing Time - POD Operating Time (hours) | 29.66 | (596,491.23 households / 20 pods x 1 hr/1,000 households) | ||
| Dispensing Time - Total (hours) | 42.9 | SNS to RSS to POD transportation time + POD Operating Time | ||
| Total Costs - POD (80%, 955,000 doses/individuals, 418,859.65 heads of household) | ||||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Product Purchase Price | ||||
| Transportation | $0.00 | |||
| Dispensing | $2,192,863.06 | |||
| Inventory Management (without replenishment) | ||||
| Total Cost (without replenishment) | $4,377,366.46 | |||
| Replenishment Costs (SLEP) | ||||
| Total Costs - Hospital/Pharmacy Component + POD Component | ||||
| Product Purchase Price | ||||
| Transportation | $3,664 | |||
| Dispensing | $2,304,879 | |||
| Inventory Management | ||||
| Total Cost (without replenishment) | $5,212,761 | |||
| Replenishment Costs (annual) | $0.00 | |||
| Replenishment Costs (SLEP) | ||||
| Replenishment Costs (annual + SLEP) | ||||
| Total Dispensing Time for Strategy | ||||
| POD Component | ||||
| Costs Description |
Data | Calculations | ||
| Dispensing Time for Pharmacy Component (hours) | 3.88 | |||
| Dispensing Time for POD Component (hours) | 42.9 | |||
| Rate-Limiting Step (hours) | 42.9 | |||
| Total Dispensing Time for Strategy (hours) | 42.9 | |||
TABLE D.1-4
Workplace Data
| Workplace Component | Large Workplace | Small Workplace | ||
| Description | Data | Calculations | Data | Calculations |
| Individuals | 170,000 | 1,700,000 x .10 | 170,000 | 1,700,000 x .10 |
| Households | 74,561.40 | 170,000 individuals x 2.28 individuals/household | 74,561.40 | 170,000 individuals x 2.28 individuals/household |
| Workplaces | 17 | 170,000 individuals x 1 large workplace/10,000 individuals | 566.67 | 170,000 individuals x 1 small workplace/300 individuals |
| Costs | ||||
| Product Purchase Price | ||||
| Product Purchase Price - Costs per daily dosage - Prophylaxis, Doxycycline | $0.20 | $0.10/pill x 2 pills per day | $0.20 | $0.10/pill x 2 pills per day |
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) |
$0.01 | $0.01 | ||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | $0.21 | $0.20 per daily dosage + $0.01 additional medication costs per dosage | $0.21 | $0.20 per daily dosage + $0.01 additional medication costs per dosage |
| Product Purchase Price - Total Costs for Medication (per household) | $2.10 | $0.21/day x 10 days | $2.10 | $0.21/day x 10 days |
| Product Purchase Price - Total Costs for Medication (overall) | $357,000 | (170,000 individuals x one 10-day course per individual x $2.10 per 10-day course) | $357,000 | (170,000 individuals x one 10-day course per individual x $2.10 per 10-day course) |
| Workplace Component | Large Workplace | Small Workplace | ||
| Description | Data | Calculations | Data | Calculations |
| Transportation | ||||
| Transportation - Shipping Medications to Workplaces | $3,392.18 | Source - average estimated shipping cost of USPS and FedEx | $5,519.37 | Source: average estimated shipping cost of USPS and FedEx |
| Transportation (overall) | $3,392.18 | $5,519.37 | ||
| Dispensing | ||||
| Dispensing - Labor - Salaries (per workplace, per day) | $15,657.60 | 35 staff (source: derivation from public POD labor requirement based on population served per workplace) x 18.64/hr (source: Zaric et al.) x 8 hr/shift x 3 shifts | $894.72 | 2 staff (source: derivation from public POD labor requirement based on population served per workplace) x 18.64/hr (source: Zaric et al.) x 8hr/shift x 3 shifts |
| Dispensing - Labor - Salaries (17 large/566.67 small workplaces, per day) | $266,179.20 | $15,657.60 x 17 large workplaces | $507,011 | $894.72 x 566.67 small workplaces |
| Dispensing - Labor - Salaries (total) | $110,908.00 | 10 hours x 1 day/24 hours x $266,179.20/day | $63,376 | 3 hours x 1 day/24 hours x $507,011/day |
| Dispensing - Labor - Training (annual total for 17 large/566.67 small workplaces) | $850,000.00 | $50,000 training cost per workplace (source: Georgia Tech paper) x 17 large workplaces | $2,833,350 | $5,000 training cost per workplace (source: Georgia Tech paper) x 566.67 small workplaces |
| Dispensing - Labor - Supplemental Nurses (per workplace, per day) | $1,731.36 | 2 nurses x 2 shifts x 12 hours/shift x 36.07/hr | $866 | 1 nurses x 2 shifts x 12 hours/shift x 36.07/hr |
| Dispensing - Labor - Supplemental Nurses (17 large/566.67 small workplaces, per day) | $29,433.12 | $1,731.36 x 17 large workplaces | $490,555 | $1,731.36 x 566.67 small workplaces |
| Dispensing - Labor - Supplemental Nurses (total for 17 large/ 566.67 small workplaces) | $12,263.80 | $29,433.12 cost/day x 10 hours operating time x 1 day/24 hours | $61,319 | $490,555 x 3 hours operating time x 1 day/24 hours |
| Workplace Component | Large Workplace | Small Workplace | ||
| Description | Data | Calculations | Data | Calculations |
| Dispensing - Administrative Fees/ Operational Costs (total) | $0.00 | Opportunity cost absorbed by company | $0.00 | Opportunity cost absorbed by company |
| Dispensing - Security (per workplace, per day) | $1,392.48 | 2 officers/shift x 3 shifts x $29.01/hr x 8 hrs/shift | $696.24 | 1 officer x 3 shifts x $29.01/hr x 8 hrs/shift |
| Dispensing - Security (17 large/566.67 small workplaces, per day) | $23,672.16 | $1,392.48 x17 | $394,538.32 | 696.24 x 566.67 |
| Dispensing - Security (total for 17 large/566.67 small workplaces) | $9,863.40 | $23,672.16 cost/day x 10 hours operating time x 1 day/24 hours | $49,317.29 | $394,538.32 x 3 hours operating time x 1 day/24 hours |
| Dispensing - Total Costs | $983,035.20 | Labor-salaries (total) + labor-training (total) + security (total) | $3,007,363.02 | Labor-salaries (total) + labor-training (total) + security (total) |
| Inventory Management | ||||
| Inventory Management - Labor | 0 | not available | 0 | not available |
| Inventory Management - Cost of Storage/ Pallet per month | $14 | Average of interview data | $14 | Average of interview data |
| Inventory Management - # of Bottles/Pallet | 10,000 | Interview | 10,000 | Interview |
| Inventory Management - # of Pallets Required | 17 | 170,000 bottles x 10,000 bottles/pallet | 17 | 170,000 bottles x 10,000 bottles/pallet |
| Inventory Management - Storage (total/ annual) | $2,856 | 17 pallets x $14/month x 12 months/1 year | $2,856 | 17 pallets x $14/month x 12 months/1 year |
| Inventory Management - Total Costs (excluding replenishment costs) | $2,856 | $2,856 | ||
| Workplace Component | Large Workplace | Small Workplace | ||
| Description | Data | Calculations | Data | Calculations |
| Inventory Management - Replenishment - Product Purchase (overall) | $357,000 | 170,000 individuals x one 10-day course per household x $2.10 per 10-day course | $357,000 | 170,000 individuals x one 10-day course per household x $2.10 per 10-day course |
| Inventory Management - Replenishment - Transportation (overall) | $3,392 | $5,519.37 | ||
| Inventory Management - Replenishment - Dispensing (overall) | $0.00 | 0 | ||
| Inventory Management - Replenishment Costs (total, annual) | $360,392.18 | Total costs for product purchase + total costs for transportation | $365,375.37 | Total costs for product purchase + total costs for transportation |
| Total Costs | Large Workplace Component (10%, 170,000 individuals) | Small Workplace Component (10%, 170,000 individuals) | ||
| Product Purchase Price | $357,000.00 | $357,000.00 | ||
| Transportation | $3,392.18 | $5,519.37 | ||
| Dispensing | $983,035.20 | $3,007,363.02 | ||
| Inventory Management (without replenishment) | $2,856 | $2,856 | ||
| Total Cost (without replenishment) | $1,346,283.38 | $3,372,738.39 | ||
| Replenishment Costs (annual) | $360,392.18 | $365,375.37 | ||
| Total Costs | Large and Small Workplaces Combined (20%, 340,000 individuals) | |||
| Workplace Component | Large Workplace | Small Workplace | ||
| Description | Data | Calculations | Data | Calculations |
| Product Purchase Price | $714,000.00 | |||
| Transportation | $8,911.55 | |||
| Dispensing | $3,990,398.22 | |||
| Inventory Management (without replenishment) | $5,712.00 | |||
| Total Cost (without replenishment) | $4,719,021.77 | |||
| Replenishment Costs (annual) | $725,767.55 | |||
| Dispensing Time | Large Workplaces | Small Workplaces | ||
| Dispensing Time - Transportation (hours) | 0 | Caches are prepositioned | 0 | Caches are prepositioned |
| Dispensing Time - Closed POD/Workplace Dispensing Time (hours) | 10 | 170,000 individuals/component x 10,000 individuals/ large workplace x 17 workplaces x 1,000 individuals/hour | 3 | 170,000 individuals/component x 300 individuals/large workplace x 566.67 workplaces x 100 individuals/hour |
| Dispensing Time - Total (hours) | 10 | 3 | ||
| POD Component | ||||
| Description | Data | Calculations | ||
| Costs | ||||
| Individuals | 1,360,000 | |||
| Households | 596,491 | |||
| Product Purchase Price | ||||
| Product Purchase Price - Costs per daily dosage - Propylaxis, Doxycycline | ||||
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | ||||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | ||||
| Product Purchase Price - Total Costs for Medication (per house-hold) | ||||
| Product Purchase Price - Total Costs for Medication (overall) | ||||
| Transportation | ||||
| Transportation - SNS to RSS to Postal Office | N/A | not available | ||
| Transportation Costs (overall) | $0.00 | not available | ||
| Dispensing | ||||
| Dispensing - Labor - Salaries (per POD, per day) | $44,736.00 | 300 staff per POD/day (source: interview with state public health official) x 8 hours/day x $18.64/hr (source: Zaric et al.) | ||
| Dispensing - Labor - Salaries (20 PODs, per day) | $894,720.00 | Labor per day per POD x 20 PODs | ||
| Dispensing - Labor - Salaries (total) | $1,105,724.80 | 29.66 hours x 1 day/24 hours x $894,720/day | ||
| POD Component | ||||
| Description | Data | Calculations | ||
| Costs | ||||
| Dispensing - Labor - Training (annual) | $894,720.00 | 300 staff per POD x 8 hours of training/ yr x $18.64/hr | ||
| Dispensing - Administrative Fees/Operational Costs (daily, per POD) | $5,000.00 | |||
| Dispensing - Administrative Fees/Operational Costs (daily, 20 PODs) | $100,000.00 | $5,000 x 20 PODs | ||
| Dispensing - Administrative Fees/Operational Costs (total) | $123,583.33 | 29.66 hours x 1 day/24 hours x $100,000/day | ||
| Dispensing - Security (daily, per POD) | $2,784.96 | |||
| Dispensing - Security (daily, 20 PODs) | $55,699.20 | |||
| Dispensing - Security (total) | $68,834.93 | 29.66 hours x 1 day/24hours x $2,784.96/POD per day x 20 PODs | ||
| Dispensing - Total Costs | $2,192,863.06 | Labor-salaries (total) + labor-training (total) + security (total) | ||
| Inventory Management | ||||
| Inventory Management - Labor | ||||
| Inventory Management - Cost of Storage/Pallet | ||||
| Inventory Management - # of Bottles/Pallet | ||||
| Inventory Management - # of Pallets Required | ||||
| Inventory Management - Storage (total) | ||||
| Inventory Management - Total Costs (excluding replenishment costs) | ||||
| POD Component | ||||
| Description | Data | Calculations | ||
| Costs | ||||
| Inventory Management - Replenishment - Product Purchase (overall) | ||||
| Inventory Management - Replenishment - Transportation (overall) | $0 | |||
| Inventory Management - Replenishment - Dispensing (overall) | $0.00 | |||
| Inventory Management - Replenishment Costs (total, SLEP) | ||||
| Dispensing Time | ||||
| Dispensing Time - SNS to RSS to Postal Office Transportation (hours) | 13.24 | (source: calculations derived from pre-sentation - Burel, G. An SNS Perspective on Prepositioning Medical Countermea-sures. Centers for Disease Control and Prevention, February 28, 2011. Presented to IOM Committee on Prepositioned Medical Countermeasures for the Public) | ||
| Dispensing Time - POD Operating Time (hours) | 29.66 | (596491.23 households/20 pods x 1 hr/1,000 households) | ||
| Dispensing Time - Total (hours) | 42.9 | SNS to RSS + POD Operating Time | ||
| Total Costs - POD (80%, 955,000 doses/individuals, 418,859.65 heads of household) | ||||
| Product Purchase Price | ||||
| Transportation | $0.00 | |||
| Dispensing | $2,192,863.06 | |||
| Inventory Management (without replenishment) | ||||
| Total Cost (without replenishment) | $4,377,366.46 | |||
| Replenishment Costs (SLEP) | ||||
| POD Component | ||||
| Description | Data | Calculations | ||
| Costs | ||||
| Total Costs - Workplace Component + POD Component | ||||
| Product Purchase Price | ||||
| Transportation | $8,912 | |||
| Dispensing | $6,183,261 | |||
| Inventory Management | ||||
| Total Cost (without replenishment) | $9,096,388 | |||
| Replenishment Costs (annual) | $725,767.55 | |||
| Replenishment Costs (SLEP) | ||||
| Replenishment Costs (annual + SLEP) | ||||
| Total Dispensing Time for Strategy | ||||
| Dispensing Time for Large Workplace Component (hours) | 10 | 170,000 individuals/component x 10,000 individuals/large workplace x 10 workplaces x 1,000 individuals/hour | ||
| Dispensing Time for Small Workplace Component (hours) | 3 | 170,000 individuals/component x 300 individuals/small workplace x 566.67 workplaces x 100 individuals/hour | ||
| Dispensing Time for POD Component (hours) | 42.9 | |||
| Rate-Limiting Step (hours) | 42.9 | |||
| Total Dispensing Time for Strategy (hours) | 42.9 | |||
TABLE D.1-5
MedKit Data
| Costs Description |
Data | Calculations |
| Individuals | 1,700,000 | |
| Product Purchase Price | ||
| Product Purchase Price - Medication Costs Per MedKit- Prophylaxis, Doxycycline | $4 | Source: interview with state public health official - cost for MedKits for postal workers |
| Product Purchase Price - Additional Costs Per MedKit (packaging, etc,) | $1.12 | Cost derived by comparing cost of packaging for non-doxycycline, commercially available MedKits |
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | $5.12 | Medication costs + Additional Costs |
| Product Purchase Price - Total Costs for Medication (overall) | $8,704,000 | (1,700,000 individuals x $5.12 per MedKit) |
| Transportation | ||
| Transportation - Shipping MedKits - Vendor to Households | $5,450,000.00 | Average of sending 1.7 million MedKits via FedEx and USPS = ($7,300,000 + $3,600,000)/2 |
| Transportation Costs (overall) | $5,450,000 | |
| Dispensing | ||
| Dispensing - Labor - Screening | $2,370,000 | Calculuation derived from POD screening time and labor (according to BERM model) |
| Dispensing - Labor - Hotline | $18,288 | 10 days labor for a hotline |
| Dispensing Costs (overall) | $2,388,288 | |
| Inventory Management | ||
| Inventory Management - Total Costs (excluding replenishment costs) | 0 | Excluding replenishment costs, no inventory management costs for MedKits |
| Costs Description |
Data | Calculations |
| Inventory Management - Replenishment - Product Purchase (overall) | $8,704,000 | 1,700,000 individuals x one 10-day course per individual x $5.12 per 10-day course |
| Inventory Management - Replenishment - Transportation (overall) | $5,450,000 | |
| Inventory Management - Replenishment - Dispensing (overall) | $0.00 | |
| Inventory Management - Replenishment Costs (total, annual) | $14,154,000 | Total costs for product purchase + total costs for transportation + total costs for dispensing |
| Total Costs per Dispensing for 10-day course to population | ||
| Product Purchase Price | $8,704,000 | |
| Transportation | $5,450,000 | |
| Dispensing | $2,388,288 | |
| Inventory Management (without replenishment) | $0 | |
| Total Cost (without replenishment) | $16,542,288 | |
| Replenishment Costs (annual) | $14,154,000 | |
| Total Dispensing Time for Strategy | ||
| Total Dispensing Time for Strategy (hours) | 0 | No dispensing time for MedKits |
TABLE D.1-6
Postal Data
| Postal Component | ||
| Description | Data | Calculations |
| Individuals | 745,000 | |
| Households | 745,000 | |
| Costs | ||
| Product Purchase Price | ||
| Product Purchase Price - Costs per daily dosage- Propylaxis, Doxycycline | ||
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | ||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | ||
| Product Purchase Price - Total Costs for Medication (per household) | ||
| Product Purchase Price - Total Costs for Medication (total postal dispensing) | ||
| Product Purchase Price - Total Costs for Postal Workers’ MedKits | $42,655.74 | [2,540 workers x 2.28 MedKits (for household) x $5.12 per MedKit] + [2,540 workers x 1 MedKit (for work) x 5.12 per MedKit] |
| Product Purchase Price - Total Costs for Medication (overall) | ||
| Transportation | ||
| Transportation - SNS to RSS to Postal Office | N/A | not available |
| Transportation Costs (overall) | $0.00 | not available |
| Postal Component | ||
| Description | Data | Calculations |
| Dispensing | ||
| Dispensing - Labor - Postal workers | $843,483.20 | [(2,540 workers x 8 hours x 23.72/hr) + (2,540 workers x 4 hours OT wage [1.5 regular])] - 332.08 per worker |
| Dispensing - Administrative Fees/Operational Costs | $460,000 | $23,000 per zip x 20 zip codes (source: Interview with federal official) |
| Dispensing - Security (per officer) | $406.16 | 12 hour shift, 8 regular/4OT, for MnSP using BLS rate of $29.01/hr |
| Dispensing - Security needs (# of officers) | 2,540 | 2/3 (volunteer rate) x 3,810 (total USPS carriers in MnSP) - (source: interview with federal official) |
| Dispensing - Security (total) | $1,031,646.40 | 2,540 x $406.16 |
| Dispensing - Total Costs | $2,335,129.60 | (Labor - postal workers) + (Dispensing - Administrative Fees/Operational Costs) + (Dispensing - Security) |
| Inventory Management | ||
| Inventory Management - Labor | ||
| Inventory Management - Cost of Storage/Pallet | ||
| Inventory Management - # of Bottles/Pallet | ||
| Inventory Management - # of Pallets Required | ||
| Inventory Management - Storage (total) | ||
| Inventory Management - Total Costs (excluding replenishment costs) | ||
| Postal Component | ||
| Description | Data | Calculations |
| Inventory Management - Replenishment - Total Costs for Medication (total postal dispensing) | ||
| Inventory Management - Replenishment - Total Costs for Postal Workers’ MedKits | $42,655.74 | [2,540 workers x 2.28 MedKits (for household) x $5.12 per MedKit] + [2,540 workers x 1 MedKit (for work) x 5.12 per MedKit] |
| Inventory Management - Replenishment - Total Costs for Product Purchase (overall) | ||
| Inventory Management - Replenishment - Labor - Postal workers | $0.00 | |
| Inventory Management - Replenishment - Security (total) | $0.00 | |
| Inventory Management - Replenishment - Total Costs for Dispensing | $0.00 | |
| Inventory Management - Replenishment Costs (total) | ||
| Dispensing Time | ||
| Dispensing Time - Postal Dispensing (hours) | 12 | (source: interview with federal employee and Georgia Tech paper) |
| Dispensing Time - SNS to RSS to Postal Office Transportation (hours) | 13.24 | (source: calculations derived from presentation - G. Burel. An SNS Perspective on Pre-positioning Medical Countermeasures. Centers for Disease Control and Prevention, February 28, 2011. Presented to IOM Committee on Prepositioned Medical Countermeasures for the Public) |
| Postal Component | ||
| Description | Data | Calculations |
| Dispensing Time - Total (hours) | 25.24 | Postal Dispensing (hours) + SNS to RSS to Postal Office Transportation (hours) |
| Total Costs - Postal (43.82%, 745,000 doses/households) | ||
| Product Purchase Price | ||
| Transportation | $0.00 | |
| Dispensing | $2,335,129.60 | |
| Inventory Management | ||
| Total Cost (without replenishment) | $3,495,285.34 | |
| Replenishment Costs (annual) | ||
| POD Component | Data | Calculations |
| Costs | ||
| Individuals | 955,000 | |
| Households | 418,859.65 | |
| Product Purchase Price | ||
| Product Purchase Price - Costs per daily dosage - Propylaxis, Doxycycline | ||
| Product Purchase Price - Additional Medication Costs Per Daily Dosage (packaging, etc.) | ||
| Product Purchase Price - Total Costs for Medication Per Daily Dosage | ||
| POD Component | Data | Calculations |
| Costs | ||
| Product Purchase Price - Total Costs for Medication (per household) | ||
| Product Purchase Price - Total Costs for Medication (overall) | ||
| Transportation | ||
| Transportation - SNS to RSS to Postal Office | N/A | not available |
| Transportation Costs (overall) | $0.00 | not available |
| Dispensing | ||
| Dispensing - Labor - Salaries (per POD, per day) | $44,736.00 | 300 staff per POD/day (source: interview with state department of health official) x 8 hours/day x $18.64/hr (source: Zaric et al.) |
| Dispensing - Labor - Salaries (20 PODs, per day) | $894,720.00 | Labor per day per POD x 20 PODs |
| Dispensing - Labor - Salaries (total) | $780,643.20 | 20.94 hours x 1 day/24 hours x $894,720/day |
| Dispensing - Labor - Training (annual) | $894,720.00 | 300 staff per POD x 8 hours of training/yr x $18.64/hr |
| Dispensing - Administrative Fees/Operational Costs (daily, per POD) | $5,000.00 | |
| Dispensing - Administrative Fees/Operational Costs (daily, 20 PODs) | $100,000.00 | $5,000 x 20 PODs |
| Dispensing - Administrative Fees/Operational Costs | $87,250.00 | 20.94 hours x 1 day/24 hours x (total) $100,000/day |
| Dispensing - Security (daily, per POD) | $2,784.96 | |
| Dispensing - Security (daily, 20 PODs) | $55,699.20 | |
| POD Component | Data | Calculations |
| Costs | ||
| Dispensing - Security (total) | $48,597.55 | 20.94 hours x 1 day/24 hours x $2,784.96/POD per day x 20 PODs |
| Dispensing - Total Costs | $1,811,210.75 | Labor-salaries (total) + labor-training (total) + security (total) |
| Inventory Management | ||
| Inventory Management - Labor | ||
| Inventory Management - Cost of Storage/Pallet | ||
| Inventory Management - # of Bottles/Pallet | ||
| Inventory Management - # of Pallets Required | ||
| Inventory Management - Storage (total) | ||
| Inventory Management - Total Costs (excluding replenishment costs) | ||
| Inventory Management - Replenishment - Product Purchase (overall) | ||
| Inventory Management - Replenishment - Transportation (overall) | ||
| Inventory Management - Replenishment - Dispensing (overall) | ||
| Inventory Management - Replenishment Costs (total, SLEP) | ||
| Dispensing Time | ||
| Dispensing Time - SNS to RSS to Postal Office Transportation (hours) | 13.24 | (source: CDC presentation) |
| POD Component | Data | Calculations |
| Costs | ||
| Dispensing Time - POD Operating Time (hours) | 20.94 | 418,859.65 households/20 pods x 1 hr/1,000 households |
| Dispensing Time - Total (hours) | 34.18 | SNS to RSS to Postal Office Transportation + POD Operating Time |
| Total Costs - POD (56.18%, 955,000 doses/individuals, 418,859.65 heads of household) | ||
| Product Purchase Price | ||
| Transportation | $0.00 | |
| Dispensing | $1,811,210.75 | |
| Inventory Management (without replenishment) | ||
| Total Cost (without replenishment) | $3,345,180.35 | |
| Replenishment Costs (SLEP) | ||
| Total Costs - Postal Component + POD Component | ||
| Product Purchase Price | ||
| Transportation | $0.00 | |
| Dispensing | $4,146,340.35 | |
| Inventory Management | ||
| Total Cost (without replenishment) | $6,919,617.69 | |
| Replenishment Costs (annual) | $42,655.74 | |
| Replenishment Costs (SLEP) | ||
| Replenishment Costs (annual + SLEP) | ||
| Total Dispensing Time for Strategy | ||
| POD Component | Data | Calculations |
| Costs | ||
| Dispensing Time for Postal Component (hours) | 25.24 | |
| Dispensing Time for POD Component (hours) | 34.18 | |
| Rate-Limiting Step (hours) | 34.18 | |
| Total Dispensing Time for Strategy (hours) | 34.18 | |
Appendix D.2
Authors, Acknowledgments, and Interviewees
AUTHORS AND ACKNOWLEDGMENTS
James Guyton is the lead author of this paper. The following PRTM employees served as co-writers or contributors to this effort:
• Dr. Robert Kadlec
• Dr. Chandresh Harjivan
• Shabana Farooqi
• Sheana Cavitt
• Joseph Buccina
PRTM enjoyed the privilege of working with the Institute of Medicine (IOM). PRTM would like to thank Clare Stroud, who served as an immensely helpful point of contact. PRTM expresses its gratitude to the Committee on Prepositioned Medical Countermeasures for the Public for the opportunity to contribute to its mission. PRTM would also like to thank Kristin Viswanathan for her assistance with the document review and all IOM employees that contributed to this effort.
PRTM interviewed more than 40 subject matter experts on this topic. The team would like to thank each of them for their time and their keen insights.
INTERVIEWEES
The following is a list of individuals who were interviewed by PRTM for the purposes of this paper. Affiliations listed reflect the individual’s primary association as of the date of the interview.
Sid Baccam, Innovate Emergency Management, Inc.
Mike Berzig, Department of Veterans Affairs
Tara Blackley, Virginia Department of Health
Joseph Canzolino, Department of Veterans Affairs
Norm Coleman, Department of Health and Human Services (HHS), Assistant Secretary for Preparedness and Response (ASPR), Office of Policy and Planning (OPP)
Susan Cooper, Tennessee Department of Health
Victoria Davey, Department of Veterans Affairs
Adele Etheridge, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention (CDC)
Matthew Feltman, Kroger/Giant
Sue Gorman, Office of Public Health Preparedness and Response, CDC
Jayne Griffith, Minnesota Department of Health
Roy Herman, Office of Public Health Preparedness and Response, CDC
Laura Herrera, Department of Veterans Affairs
Jack Herrmann, National Association of County and City Health Officials (NACCHO)
Mary Beth Hill-Harmon, HHS/ASPR/Biomedical Advanced Research and Development Authority (BARDA)
Jeffrey Holmes, PRTM
Nathaniel Hupert, CDC and Weill Medical College, Cornell University
Terrie Kolodziej, HHS/ASPR/BARDA
Lisa Koonin, CDC
George Korch, HHS/ASPR
Joe Larsen, HHS/ASPR/BARDA
Eva Lee, Georgia Tech University
Aggie Leitheiser, Minnesota Department of Health
Rebecca Lipsitz, HHS/ASPR
Rich McNally, HHS/ASPR
Carter Mecher, National Security Staff
Matthew Minson, Texas A&M University
Amanda Fuller Moore, North Carolina Department of Health and Human Services
Stephen Morris, HHS/ASPR/BARDA
Chris Motsek, Office of Public Health Preparedness and Response, CDC
Paul Peterson, Tennessee Department of Health
Jude Plessas, U.S. Postal Service
Ken Rapuano, The MITRE Corporation
Marjorie Sidebottom, University of Virginia
David Starr, Office of Emergency Preparedness and Response, New York City Department of Health and Mental Hygiene
Jason Stear, Office of Public Health Preparedness and Response, CDC
Thomas Tighe, Direct Relief International
Penny Turnbull, Marriott Hotels International
James Turner, American College Health Association Representative, Utility Services Provider
Michael Valentino, Department of Veterans Affairs
This page intentionally left blank.














































































