6
Direct and Indirect Costs of Violence
While no methodology exists to enumerate the full extent of the impact of violence, some costs can be estimated. These costs are roughly divided into direct costs, or those arising immediately or proximally to the violent event, and indirect costs, or those that result as a consequence, externality, or loss of opportunity. Direct costs are more readily quantifiable and tend to fall into traditional categories of medical and nonmedical costs and productivity costs. Indirect costs indicate impact beyond direct victims and perpetrators and also include indirect victims and often society at large. However, some costs can be categorized in either way, suggesting that a definitive line between the two does not truly exist.
The first paper is an overview of the costs of interpersonal violence around the world. This represents a comprehensive survey that includes a large number of data sources. It attempts to place the costs within a context by which comparisons across regions can be made.
The second paper discusses the costs and implications of elder abuse, an often-overlooked type of violence. Elder abuse, which can encompass more than just physical and psychological violence, is poised to have enormous impact as populations around the world age.
The third paper looks at a major risk factor for violence—firearms. The impact of gun-related violence extends beyond the home and immediate victims, but affects the neighborhood and community as well. This paper examines the indirect and more diffuse costs of such violence.
The fourth paper explores a similar concept of social costs by examining the contagious nature of violence. Violence does not occur in a vacuum, and often the undercurrent or environment of violence normalizes violent
response in other settings. As well, witnessing or being a victim of violence can increase the risk of future violence.
The final paper lays out the significant impact of violence at early stages of child development, by examining violence and its effects along the life span. Violence, resulting in traumatic stress, can have psychological and physiological effects on the brain and body, some of which can manifest much later in life. Mitigating these effects requires early intervention.
THE COSTS OF INTERPERSONAL VIOLENCE—
AN INTERNATIONAL REVIEW1
Hugh Richard Waters, Ph.D.
Johns Hopkins Bloomberg School of Public Health
Adnan Ali Hyder, M.D., M.P.H., Ph.D.
Johns Hopkins Bloomberg School of Public Health
Yogesh Rajkoti, Ph.D., M.Sc.
Johns Hopkins Bloomberg School of Public Health
Suprotik Basu, M.H.S.
The World Bank
Alexander Butchart, Ph.D., M.A.
World Health Organization
Abstract
This article reviews evidence of the economic impact of interpersonal violence internationally. In the United States, estimates of the costs of interpersonal violence reach 3.3 percent of the gross domestic product (GDP). The public sector—and thus society in general—bears the majority of these costs. Interpersonal violence is defined to include violence between family members and intimate partners, as well as violence between acquaintances and strangers that is not intended to further the aims of any formally defined group or cause. Although these types of violence disproportionately affect poorer countries, there is a scarcity of studies of their economic impact in those countries. International comparisons are complicated by the calculation of economic losses based on forgone wages and income, thus undervaluing economic losses in poorer countries.
___________________
1 Reprinted from Waters, H. R., A. A. Hyder, Y. Rajkotia, S. Basu, and A. Butchart. 2005. The costs of interpersonal violence—An international review. Health Policy 73(3):303-315.
Introduction and Methods
This article systematically reviews peer-reviewed literature related to the economic consequences of interpersonal violence internationally. Although much of the available literature concerns high-income countries, violence disproportionately affects low- and middle-income countries, where an estimated 90 percent of all violence-related deaths occur (Krug et al., 2002).2 As a result, the economic effects of violence are also likely to be proportionally more severe in poorer countries.
This article defines interpersonal violence as violence between family members and intimates and violence between acquaintances and strangers that is not intended to further the aims of any formally defined group or cause. Self-directed violence, war, state-sponsored violence, and other collective violence are specifically excluded from these definitions.
We conducted a comprehensive literature search to identify published estimates of the cost of interpersonal violence, using electronic databases, governmental and nongovernmental websites, and contacts with knowledgeable individuals working in the fields of violence prevention and economic evaluation. After initial electronic searches, additional sources were identified through the reference lists of collected articles and reports. The details of this search—including keywords used for electronic searching and experts consulted—are provided in the acknowledgments. The search was conducted without restrictions on the language of publication and included publication dates from January 1980 to September 2004.
To categorize studies by type of interpersonal violence, we adapted the definitions of the most prevalent categories of interpersonal violence described in the 2002 World Report on Violence and Health, as shown in Table 6-1.
Studies documenting the economic effects of interpersonal violence have used a broad range of categories of costs. We have divided cost categories broadly into “direct” costs and benefits—those resulting directly from acts of violence or attempts to prevent them—and “indirect” costs and benefits. The most commonly cited direct costs are medical care and the costs of the judicial and penal systems (policing and incarceration). Indirect costs include the long-term effects of acts of violence on perpetrators and victims, such as lost wages and psychological costs, also referred to as pain and suffering (Hornick et al., 2002).
We converted all monetary results to 2003 U.S. dollars to enable comparisons and to adjust for inflation and varying exchange rates. Values
___________________
2 Countries are classified by income level using the following categories from the 2004 World Development Report (World Bank, 2004): low-income = $745 per capita or less; lower middle-income = $746 to $2,975; upper middle-income = $2,976 to $9,205; high-income = $9,206 or more.
TABLE 6-1 Types of Interpersonal Violence
|
Child abuse and neglect |
Child abuse or maltreatment constitutes all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment, or commercial or other exploitation, resulting in actual or potential harm to the child’s health, survival, development, or dignity in the context of a relationship of responsibility, trust, or power |
|
|
Intimate partner violence |
Any behavior within an intimate relationship that causes physical, psychological, or sexual harm to those in the relationship |
|
|
Abuse of the elderly |
Act of commission or of omission, intentional or unintentional, of a physical nature; it may be psychological (involving emotional or verbal aggression), or it may involve financial or other material maltreatment |
|
|
|
Regardless of the type of abuse, it will certainly result in unnecessary suffering, injury, or pain; the loss or violation of human rights; and a decreased quality of life for the older person |
|
|
Sexual violence |
Any sexual act, attempt to obtain a sexual act, unwanted sexual comments or advances, or acts to traffic, or otherwise directed, against a person’s sexuality using coercion, by any persons regardless of their relationship to the victim, in any setting, including but not limited to home and work |
|
|
Youth violence |
Violence committed by or against people between the ages of 10 and 29 years |
|
|
Workplace violence |
Physical or psychological behavior directed against coworkers, including bullying, sexual harassment, threats, and intimidation |
|
| SOURCE: Adapted from Krug et al., 2002. | ||
expressed in other currencies in original documents, and U.S. dollar values from previous years, have been converted to 2003 U.S. dollars using the U.S. consumer price index and applicable international exchange rates from the year of the original estimates. Costs expressed as a percentage of the GDP were calculated using the GDP from the year the costs were reported.
Findings
There are widely varying estimates of the cost of violence internationally, depending on the definitions used, the types of costs included, and the methodologies used. The U.S. Department of Justice (1994) reported estimated direct costs of violent crime to victims resulting from short-term medical expenses and work loss. These estimates were based on responses to the National Crime Victimization Survey (NCVS), an annual survey based on 100,000 interviews with crime victims. These costs amounted to
$1.8 billion, 0.02 percent, of the U.S. GDP in 1994. When indirect costs are included, estimates of the costs of violence in the United States are substantially higher. Miller et al. (1993) estimated an annual cost of intentional injuries of $84.1 billion in the United States for 1987-1990. Throughout the literature on the costs of violence, psychological costs greatly outweighed the direct costs of violence—partially explaining the wide variance in the estimates that are available.
Miller et al. (2001) estimated that lost earnings, psychological costs, and the opportunity cost of victims’ time, in addition to the costs of policing, incarceration, and life insurance in the State of Pennsylvania, equaled $14.2 billion. Separately, Miller et al. (1996) estimate a total annual cost to victims of personal crime in the United States—including domestic violence, sexual assault, rape, and child abuse—of $507 billion. This estimate, which includes psychological costs of pain and suffering, is equivalent to 6.5 percent of GDP, or $1,100 per person in the United States. Brand and Price (2000) estimated total costs from crime of $63.8 billion in England and Wales. Sixty-three percent of this amount was attributable to violence—including homicide, wounding, and sexual assault. This tally includes both direct costs such as police and judicial system costs and indirect costs that included forgone output and physical and emotional costs.
Estimates from other high-income countries are more conservative. The Australian Institute of Criminology (2003) reported national annual costs for assault of $159 million, an estimate that did not include indirect costs and was based largely on the costs of incarcerating offenders. Similarly, the cost of homicide in Australia was calculated at $194 million per year, based on a cost per homicide of $602,000 (Walker, 1997). Fanslow et al. (1997) calculated the economic cost from homicide in New Zealand: when lost earnings, legal fees, incarceration, and policing were included, the cost per homicide was $829,000 for a total of $67.9 million.
There are few documented estimates of the costs of violence in low- and medium-income countries. Additionally, comparisons with high-income countries are complicated by the fact that economic losses related to productivity tended to be undervalued in lower-income countries since these losses were typically based on forgone wages and income. For example, Phillips (1998) calculated the cost of homicides in the Western Cape Metropolitan Area in South Africa. Using a 4 percent rate to discount future productivity and opportunity costs, he calculated a cost averaging $15,319 per homicide, sharply lower than the United States, United Kingdom, Australian, and New Zealand estimates above.
The Inter-American Development Bank (IDB) has spearheaded efforts to systematically document the costs of both interpersonal and collective violence in the Americas. Central America has been particularly affected. In 1995, El Salvador spent 6 percent of the gross national product (GNP) to
TABLE 6-2 Costs of Social Violence in Latin America
| Country | 1997 GDP Lost Due to Social Violence (%) |
| Brazil | 10.5 |
| Colombia | 24.7 |
| El Salvador | 24.9 |
| Mexico | 12.3 |
| Peru | 5.1 |
| Venezuela | 11.8 |
| NOTE: Definition of violence includes collective violence (Buvinic et al., 1999). GDP = gross domestic product. | |
control violence (Buvinic and Morrison, 1999). As part of the IDB’s work, Buvinic et al. (1999) reported estimates of economic losses due to social violence—including collective violence—in a variety of countries (see Table 6-2). These losses ranged from 5.1 percent of GDP in Peru to 24.9 percent in El Salvador, which was still in the throes of guerrilla war in the mid-1990s when the data were generated. The estimates included lost earnings, the opportunity cost of time, policing, incarceration, judicial costs, forgone investments in human capital, and effects on investment.
Child Abuse and Neglect
The extent of child abuse and neglect is difficult to gauge since much if not most of it is unreported. The 2002 World Report on Violence and Health (WHO, 2002) estimates that the rates of homicide of children under 5 years of age were 2.2 per 100,000 for boys and 1.8 per 100,000 for girls in high-income countries. In low- and middle-income countries, the corresponding rates are 6.1 and 5.1 per 100,000, respectively, for boys and girls. In Africa, the rates are 17.9 per 100,000 for boys and 12.7 per 100,000 for girls (Krug et al., 2002). Many of the estimates of the costs of child abuse available in the literature are from the United States (see Table 6-3).
The cost of child abuse ranges widely and depends on the mix of direct and indirect costs used to calculate it. Courtney (1999) calculated a figure of $14 billion for direct costs, including counseling and child welfare services resulting from child abuse in the United States. The U.S. Department of Health and Human Services (2001) calculated the costs of child abuse and maltreatment in Colorado to be $468 million—of which indirect costs represent 53 percent.
There is a considerable range of estimates of individual-level treatment costs for child abuse, depending on the types of costs included. On
TABLE 6-3 Costs of Child Abuse
| Study | Study Location and Population | Cost Categories Included (indirect costs in italics) | Total Annual Costs (2001 US$) |
|
Courtney, 1999 |
United States, maltreated children and their families |
Direct medical (including counseling) |
$14.0 billion |
|
Evasovich et al., 1998 |
United States, Ohio (4 counties), children referred to social services for suspected child abuse (n = 104) |
Direct medical, legal fees (court costs, fines) |
$0.3 million; $2,884 per child |
|
Forjuoh, 2000 |
United States, Pennsylvania, 1995, hospital discharge data (n = 348 children) |
Direct medical |
$6.3 million; $18,103 per child |
|
HHS, 2001 |
United States, Colorado, 1995 |
Direct medical, legal services, incarceration, workers’ productivity, lost earnings, and opportunity cost of lost time |
$17.4 million |
|
Irazuzta et al., 1997 |
United States, West Virginia, 1991-1994, pediatric ICU admissions (n = 13) |
Direct medical |
$0.6 million; $42,518 per child |
|
Libby et al., 2003 |
Head trauma patients from Colorado hospital discharge database, 1993-2000 |
Direct medical |
Mean charges of $4,232 more than those with unintentional head trauma |
|
New and Berliner, 2000 |
United States, Washington State, 1994, mental health treatment costs compensated by crime victims compensation program (n = 608 children) |
Direct medical |
$1.2 million; $1,891 per child |
|
Rovi et al., 2004 |
United States, national sample of inpatients through the healthcare costs and utilization project, 1999 |
Direct medical |
Mean charges of $19,266 compared to $9,513 for other hospitalized children |
|
Summers and Molyneux, 1992 |
United Kingdom, 1990, children hospitalized (n = 181) |
Direct medical examinations only |
1990 GB£63,500 |
|
Yodanis et al., 2000 |
United States, Washington State, randomly selected sample of women (n = 1,225) enrolled in an HMO; 42.8 percent maltreated as children |
Direct medical |
$9.1 million; $17,356 per child |
| NOTE: HMO = health maintenance organization; ICU = intensive care unit. | |||
the high end, Irazuzta et al. (1997) calculated treatment costs per child of $42,518 based on daily hospital charges of $6,317 in a pediatric intensive care unit in Charlestown, West Virginia. Forjuoh (2000), working with discharge data from acute care hospitals in Pennsylvania, calculated a mean hospitalization cost of $18,103 per child abuse victim—comparable to a cost $19,266 per discharge found by Rovi (2004), working from a national survey of inpatients. Plontnick and Deppman (1999) calculated an average cost of $12,028 for hospitalizing an abused child for one week.
Evasovich and Klein (1998) studied the costs of medical care and related legal fees for children admitted to the burns unit at the Children’s Hospital Medical Center in Akron, Ohio, and found costs totaling $13,781 per child. Public funds paid for 65 percent of these costs. New and Berliner (2000) examined claims paid by the Crime Victims Compensation program in Washington State and calculated mental health treatment costs of $2,921 per child, with counseling services costing between $70 and $90 per hour, exclusive of hospitalization or other healthcare costs. There are few estimates available of the cost of child abuse internationally. Mendonca et al. (2002) measured hospital costs due to violence against children and adolescents in Pernambuco State, Brazil. The mean cost of hospitalization for children and adolescents was $184. Violence against children and adolescents in greater metropolitan Recife, the principal city in the state, accounted for 65.1 percent of hospital admissions and 77.9 percent of hospital costs.
Intimate Partner Violence
The true extent of intimate partner violence is unknown. Surveys suggest a wide range in prevalence, but the results are difficult to compare given cultural differences and social taboos in responding to questions (see Table 6-4). In Paraguay and the Philippines, 10 percent of women surveyed reported being assaulted by an intimate partner (Heise et al., 1999), compared to 22 percent in the United States (Tjaden and Thoennes, 2000), 29 percent in Canada, and 34 percent in Egypt (El-Zanaty, 1996). Other studies have shown that 3 percent or less of women in Australia, the United States, and Canada had been assaulted by a partner in the previous 12 months, compared to 27 percent of ever-partnered women in South Korea and 53 percent of currently married women in the West Bank and Gaza (Krug et al., 2002).
There are complex methodological issues involved in measuring the economic impact of intimate partner violence. Many, if not most, incidents of intimate partner violence go unreported, and the effects of such abuse on investments in human capital and productivity inside and outside the home are difficult to estimate (El-Zanaty, 1996). Studies have documented
TABLE 6-4 Costs of Intimate Partner Violence
| Study | Study Location and Population | Cost Categories Included (indirect costs in italics) | Total Annual Costs (2001 US$) |
|
Coker et al., 2004 |
United States, Medicaid-eligible women in Houston |
Direct medical costs (physician, drug, and hospital) |
Mean difference between high-IPV and no-IPV women of $1,064 |
|
Day, 1995 |
Canada, data drawn from surveys |
Direct medical costs (dental costs also), lost earnings and opportunity cost of time, other monetary costs, psychological costs |
$1.2 billion |
|
Mansingh and Ramphal, 1993 |
Jamaica, Kingston public hospital, 1991 |
Costs for treating victims of intimate partner violence, direct medical costs |
$454,000 |
|
New and Berliner, 2000 |
United States, Washington State, 1994, 318 women; victims compensated by the crime victims compensation program |
Direct medical costs (mental health treatment costs) |
$3,087 per patient (median 15 sessions) |
|
Snively, 1994 |
New Zealand |
Direct medical costs, welfare, legal, policing |
$3,087 per patient (median 15 sessions) |
|
Stanko et al., 1998 |
United Kingdom, borough of Hackney, 1996 |
Public services only, policing, legal, medical costs, other monetary costs (housing, refuge, social services) |
$717,000 |
|
Wisner et al., 1999 |
United States, Minnesota, 1992-1994, 126 victims of intimate partner violence in a large health plan |
Direct medical costs |
$4,341 per patient |
| NOTE: IPV = intimate partner violence. | |||
per-case direct treatment costs for intimate partner violence, but this type of study is only possible for those victims who have contact with the healthcare system. New and Berliner (2000) found that women who were compensated through the Crime Victims Compensation Program
in Washington State averaged $3,087 for mental health treatment and counseling costs.
Day (1995) comprehensively calculated the aggregate costs of violence against women in Canada. Including healthcare costs, policing, legal fees, incarceration, lost earnings, and psychological costs, violence against women cost an estimated $1.2 billion. In these calculations, medical and dental visits are assigned a value of $67, a probable underestimate—so the total costs are likely to be higher than reported.
As a percentage of GDP, estimates of the costs of intimate partner violence are considerably higher in low- and middle-income countries than in high-income countries. Morrison and Orlando (1999) calculated the costs of domestic violence against women based on stratified random samples of women in Chile and Nicaragua. Based only on the lost productive capacity of these women, they extrapolated total costs of $1.73 billion in Chile and $32.7 million in Nicaragua—equivalent to 1.6 percent of GDP in Nicaragua and 2 percent of GDP in Chile.
Stanko et al. (1998) counted the costs of public services—including policing, court costs, medical care, and refuge—spent in the year 1996 on responses to domestic violence against women in the borough of Hackney in the United Kingdom. They estimated these costs to be $13.3 million for the borough, averaging $159 per household.
Sexual Violence
As with intimate partner violence, the costs of sexual assault are difficult to document systematically—given that many such assaults go unreported. As a result, most documented calculations are likely to be underestimates. Many of the published studies are based in the United States (see Table 6-5). The estimates vary widely, depending on the cost categories included and methods used. For example, Cohen (1988), using pain and suffering awards from more than 100,000 jury decisions in the United States, calculated that the annual aggregate direct and indirect costs of rape were $14.9 billion—equivalent to 0.2 percent of GDP.
In contrast, the U.S. Department of Justice (1994) calculated the economic losses of rape as $33 million, based on reported direct medical costs and lost earnings, though this estimate did not include psychological costs. For costs at the level of individual rape victims, Miller et al. (1993) used the NCVS to calculate a total cost of $85,000 per rape.
Workplace Violence
Violence at or related to the workplace extracts a significant economic toll (see Table 6-6), but studies of its magnitude are not well developed
TABLE 6-5 Costs of Sexual Violence
| Study | Study Location and Population | Cost Categories Included | Total Annual Costs (2001 US$) |
|
Cohen, 1988 |
United States, pain and suffering data from more than 100,000 jury decisions |
Direct medical costs, lost earnings and opportunity costs of time, psychological costs, other nonmonetary costs |
Cost of rape, $14.9 billion |
|
Miller et al., 1993 |
United States, NCVS, all victims of nonfatal physical and psychological injury, 1987-1990 |
Direct medical costs, life insurance costs, victim compensation costs (jury awards), employment and workers’ productivity, psychological costs, lost earnings, and opportunity costs of time |
Costs per rape, $85,000 |
|
U.S. Department of Justice, 1994 |
United States, NCVS |
Direct medical costs, lost earnings, and opportunity cost of time |
Cost of rape, $33 million |
and are hampered by measurement difficulties and nonstandardized methodologies. McCall and Horwitz (2004) found that in Oregon the rate of reported incidents of workplace violence was 1.86 per 10,000 employees annually, with female workers and those under age 35 experiencing the most violence.
There is a wide range of estimates of how much interpersonal violence-related absenteeism, together with related medical care and productivity losses, costs employers and society in general. Internationally, a non-peer-reviewed report commissioned by the International Labor Organization (ILO) on the costs of violence and stress in work environments estimates that losses from stress and violence at work represent from 1 to 3.5 percent of GDP over a range of countries (Hoel et al., 2001).
Biddle and Hartley (2002) studied the costs of homicides in the workplace in the United States and calculated an annual cost of approximately $970 million. This estimate included the lost earnings of victims extrapolated to the age of 67. Hashemi and Webster (1998) reviewed a random sample of nonfatal workplace violence claims filed with a large workers’ compensation insurance carrier. They calculated $26.5 million in annual costs to the insurer, based on 7,173 compensated claims, or $3,694 per
TABLE 6-6 Costs of Workplace Violence
| Study | Study Location and Population | Cost Categories Included | Total Annual Costs (2001 US$) |
|
Biddle and Hartley, 2002 |
United States, all occupational homicide deaths from national traumatic occupational fatalities (NTOF) surveillance system 1980-1997 |
Direct medical costs, lost earnings, and opportunity costs of time |
Cost of workplace homicides, $970 million |
|
Hashemi and Webster, 1998 |
United States, 600 nonfatal workplace violence claims, randomly selected |
Direct medical costs, lost earnings and opportunity cost of time employment and workers’ productivity psychological costs, other nonmonetary costs |
Costs per workplace compensation claim, $3,694 |
|
McCall and Horwitz, 2004 |
United States, 2,028 workers’ claims of workplace violence in Oregon 1990-1997 |
Direct medical costs, lost earnings and opportunity cost of time, employment and workers’ productivity |
$6,200 average per claim |
claim. McCall and Horwitz (2004) found a cost to insurers of $6,200 average per claim in Oregon.
Youth Violence
Youth violence is defined as violence committed by or against individuals between the ages of 10 and 29. In 2000, an estimated 199,000 youth homicides were committed globally—9.2 per 100,000 people. This rate varied from 0.9 per 100,000 in high-income countries to 17.6 in Africa and 36.4 in Latin America. Based on studies of nonfatal violence, it was further estimated that for every youth homicide there are 20-40 victims of nonfatal youth violence receiving hospital treatment (Krug et al., 2002).
Miller et al. (2001) analyzed violent crimes committed in Pennsylvania in 1993, finding that juvenile violence accounted for 24.7 percent of all violent crimes and 46.6 percent of the total victim costs from violent crime. Juvenile crime resulted in $6.6 billion in costs to victims—including quality-of-life and productivity losses. Cohen (1998) reviewed the costs of crimes committed by juveniles. He estimated that a typical crime committed by a juvenile resulted in $16,600 to $17,700 in costs to the victim, plus $44,000
in costs to the criminal justice system. Adding these costs to the forgone economic contributions of incarcerated criminals, he calculated that the total cost to society of one youth reverting to a life of crime ranged from $1.9 million to $2.6 million—based on 68-80 crimes committed. Interventions to prevent high-risk youth from becoming career criminals are therefore likely to be highly cost-effective (see Table 6-7).
Violence Facilitators: Guns, Alcohol, Drugs, and Gangs
Guns, gangs, alcohol, and drugs all show up in the literature as major facilitators for interpersonal violence. Access to guns is without question a leading facilitating factor. Most estimates of the economic impact of gun violence include suicide. In the United States, there is clear evidence to show that the overall toll of gun violence is very high. More than 30,000 people die annually from firearms injuries in the United States; these injuries are the second leading cause of death for individuals aged 15-34 (Gunderson, 1999).
Max and Rice (1993) calculated the annual costs of firearm injuries in the United States at $27.3 billion, including direct medical care and lost productivity with a 6 percent discount rate; 85 percent of this amount was due to lost productivity. They based their estimates on a variety of sources, including the National Mortality Detail File and the National Medical Care
TABLE 6-7 Costs of Youth Violence
| Study | Study Location and Population | Cost Categories Included | Total Annual Costs (2001 US$) |
|
Cohen, 1998 |
United States, youth criminals (data from other studies) |
Costs of incarceration, direct medical costs, lost earnings and opportunity costs of time, employment and workers’ productivity, psychological costs |
Cost per youth resorting to life of crime, $1.9 million to $2.6 million |
|
Miller et al., 2001 |
United States, violent juvenile crimes committed in Pennsylvania in 1993 (n = 93,000) |
Direct medical costs, lost earnings and opportunity cost of time, employment and workers’ productivity, psychological costs, other nonmonetary costs |
Costs per workplace compensation claim, $3,694 |
Utilization and Expenditure Survey. Miller and Cohen (1997) included psychological costs and the value of quality of life and arrived at a significantly higher estimate for the toll of gun-related violence in the United States—$155 billion, or 2.3 percent of GDP. They also calculated that, on a per capita basis, the costs of gun violence in Canada were 36 percent of the U.S. figure. Using individuals’ expressed willingness to pay for decreases in gun violence, Ludwig and Cook (2000) calculate that gun violence cost $100 billion a year, including indirect costs such as increased security and psychological effects.
Hospital-based studies have also found a heavy economic toll related to gun violence. In a study of 9,562 patients discharged from California acute care hospitals after treatment for firearm-related injuries, Vassar and Kizer (1996) found mean hospital charges of $23,187 per patient; 56 percent of the patients were paid for through publicly financed insurance. Cook et al. (1999) studied 800 cases of gunshot injuries treated in emergency rooms across the United States. Using discharge information they calculated average medical costs of $20,304 per gunshot victim. With a 3 percent discount rate, lifetime medical treatment costs per person amount to $37,000-$42,000.
Mock et al. (1994) studied gunshot wounds at a regional hospital in Seattle, Washington, from 1986 to 1992. They found direct average hospital charges of $17,367 for gunshot victims, compared to $7,699 for stab victims (2001 dollars). They argued that if guns were eliminated—even with the same level of violence occurring through stab wounds—$1.5 million would be saved annually at that hospital alone. Seventy-six percent of these savings would be of public sector funds. There are few estimates of the costs of gun violence outside of the United States and Canada. A study at the Groote Schurr Hospital in Cape Town, South Africa, found that direct medical costs averaged 30,628 rand—$10,308 in 2003 U.S. dollars—per gunshot victim (Peden and Van der Spuy, 1998).
Alcohol and drugs are also leading contributors to violence and its costs. Based on the NCVS and Survey of State Prison Inmates, alcohol use was a factor in 25 percent of assaults for victims hospitalized in Vermont, with average hospital charges of $420—19 percent of which was paid by public sources and 54 percent of which was unpaid. Crime committed under the influence of drugs, or to obtain money to purchase drugs, amounted to $103.6 million, or 25.7 percent of the total for violent crime. The National Crime Prevention Council (1999) estimated that the cost of all drug-related crime, including productivity costs, amounted to $60 billion to $100 billion annually in the United States. Violent crime accounted for approximately 10 percent of this figure.
Gangs are described as significant violence facilitators in several studies of the costs of violence (Tellez et al., 1995). Song et al. (1996) systematically
categorized patients suffering from gang-related violence in the University of California, Los Angeles (UCLA) Medical Center. They found 272 cases of gang-related gunshot injuries over a 29-month period from 1992 to 1994. These injuries resulted in an average of $21,200 in direct medical charges. For 58 percent of these charges, there was no available insurance or third-party reimbursement to pay the bill.
Discussion
Methodological Variation Across Studies
This review shows clearly that a wide range of methodologies is used to calculate the costs of violence and that researchers’ choice of methodologies and approaches can have an important effect on their ultimate results. The most evident methodological difference among studies of the economic effects of interpersonal violence is the broad range of categories of costs employed. Many of the differences in economic estimates are due to the inclusion or exclusion of specific categories of costs, rather than to different approaches toward counting costs.
Another significant difference among studies is the perspective from which costs are calculated. The majority of studies use a societal perspective—in principle including all costs and benefits. Several studies, however, included only costs to the victims, without counting the social costs of prevention, law enforcement, incarceration, and lost productivity. Most of the cost estimates of the aggregate economic losses caused by violence are for a 1-year period, but the time frame used varies across studies, complicating direct comparisons. Nearly all studies that do calculate costs and benefits beyond a 1-year time frame use some kind of discount rate to discount future costs and benefits—based on the principle that humans value consumption and quality of life in the present more than they do an equivalent amount of consumption in the future. The discount rates used in the studies reviewed here range from 2 to 10 percent.3
An important difference across studies lies in the values assigned to human life, lost productive time, and psychological distress. The value of life has been calculated using lost wages, estimates of the quality of life, wage premiums for risky jobs, willingness to pay for safety measures, and individual behaviors related to safety measures. The values used among
___________________
3 The U.S. Panel on Cost-Effectiveness in Health and Medicine has recommended using a real rate of 3 percent for cost evaluations in health care (Gold, 1996). This rate reflects a wide range of studies documenting individuals’ preferences for present consumption compared to future consumption and interest rates for private investment. In theory, both of these factors influence the discount rate for future costs and benefits in the context of financial and health-related gains and losses.
studies based in the United States ranged from $3.1 million to $6.8 million. These estimates are in line with those generally used in the economic evaluation literature.4
Costs Paid by Public Sources
A considerable portion of the costs of violence are paid by public sources and thus represent a cost to society in general. A study at the University of Southern California Medical Center found that 87 percent of the costs of treating gunshot wounds of the trunk were paid with public funds—with average hospital stays of 6.8 days and costs of $10,600 per patient (Payne et al., 1993). Similarly, 80 percent of the direct medical costs for gunshot wounds, stab wounds, and injuries from assault at the San Francisco General Hospital in the mid-1980s were paid for with public funds (Sumner et al., 1987).
Sixty-five percent of the costs of medical care and legal fees for burns suffered by child abuse victims were paid with public funds in a study in Ohio (Evasovich et al., 1998). Clancy et al. (1994) found that 70 percent of hospital charges for patients with assault-related penetrating injuries at a major medical centre in North Carolina were not reimbursed. Gunderson (1999) reported that 85 percent of the costs for medical care of victims of gun violence in the United States were paid from public sources. In low- and middle-income countries, it is also probable that society in general absorbs much of the costs of violence. A study in Jamaica found that 90 percent of the cost of treating victims of violence at the Kingston Public Hospital— including materials, drugs, and doctors’ fees—was paid by the government (Mansingh and Ramphal, 1993).
Conclusion
Given the wide range of methodological differences and extensive gaps in the existing literature on the economics of interpersonal violence, there is a clear need for systematic future research into the costs of violence. Such research should follow rigorous methodological guidelines, include both direct and indirect cost categories, and perhaps most importantly, permit comparisons across countries and settings. There is also a need for standardized research on the indirect costs of violence. Beyond the individual
___________________
4 Miller (1989) reviewed 29 cost-benefit studies and found that the mean value given to a human life in these studies was $4.2 million. Fisher et al. (1989) reviewed 21 studies and found a range of $2.6 million to $13.7 million. Walker used a figure of $1 million Australian dollars (equivalent to US$602,000 in 2001), but this does not include the costs of the judicial system or psychological costs.
consequences of opportunity cost and pain and suffering, interpersonal violence has a series of economic effects at the population level, including reduced foreign investment and lowered confidence in society’s economic, legal, and social structures. There are very few estimates of the extent of these costs, which if quantified are likely to be several times the value of the direct costs of violence.
Likewise, an important future step is to document the costs and benefits of potential interventions to reduce interpersonal violence. This paper shows that an economic approach can demonstrate the magnitude of the damage caused by interpersonal violence—a first step toward a unified agenda to reduce the human toll caused by unnecessary violence.
Acknowledgments
This research was funded by the World Health Organization. The literature search was conducted without restrictions on the language of publication and included publication dates from January 1980 to September 2004. We used the following keywords, representing types of violent behavior and factors associated with violent behavior combined with economic variables:
- Violence: interpersonal violence, family violence, partner violence, domestic violence
- Abuse: child abuse, domestic abuse, partner abuse, girl abuse
- Assault benefits
- Homicide investments
- Injury and intentional injury
- Human capital
- Firearms expenses
- Costs: cost-effectiveness, cost-benefit
- Economics: economic policy
The following databases and websites were searched:
- Australian Institute of Criminology
- CIAO—Columbia International Affairs Online
- CINAHL—Cumulative Index to Nursing and Allied Health Literature
- Cochrane Library
- Contemporary Women’s Issues
- EconLit
- General Sciences database
- Gun Control Alliance (South Africa)
- Health Canada
- Illinois Coalition Against Sexual Assault
- Index to United Nations Documents and Publications
- Inter-American Development Bank
- International Labor Organization
- National Clearinghouse on Child Abuse and Neglect Information
- National Crime Prevention Council (USA)
- New Zealand Ministry of Justice
- PAIS
- Physicians for Social Responsibility
- Popline
- Prevent Child Abuse America—www.preventchildabuse.org
- Pubmed
- Social Sciences Abstracts
- Social Sciences Citation Index
- Sociological Abstracts
- SourceOECD
- U.S. Department of Justice
- Womankind Worldwide
- Women’s Advocates Inc. (USA)
- World Bank
- World Health Organization
After the initial database and Internet literature searches, additional sources were identified through the reference lists of collected articles and through consultation with the following resource experts, gratefully acknowledged below:
- David Ball, Middlesex University, United Kingdom
- David Bishai, Johns Hopkins Bloomberg School of Public Health
- Nancy Cardia, Centre for the Study of Violence, University of São Paulo, Brazil
- Phillip Cook, Duke University
- Phaedro Corso, Centers for Disease Control and Prevention
- Elizabeth Eckermann, Deakin University, Australia
- Rune Elvik, Norwegian Center for Transport Research
- Adam Graycar, Australian Institute of Criminology
- Rodney Hammond, Centers for Disease Control and Prevention
- Patricia Hernandez, World Health Organization
- Michael Koenig, Johns Hopkins Bloomberg School of Public Health
- Daniel Lederman, The World Bank
- Pat Mayhew, Australian Institute of Criminology
- Katherine McKenna, Centre for Women’s Studies and Feminist Research, University of Western Ontario
- James Mercy, Centers for Disease Control and Prevention
- Ted Miller, Pacific Institute for Research and Evaluation
- Andrew Morrison, Inter-American Development Bank
- Gregory Pappas, Macro International
- Ann Dryden Witte, Wellesley College
- Carrie Yodanis, University of Fribourg
CONSEQUENCES OF ELDER ABUSE: THE NEEDS FOR
SOCIAL JUSTICE AND POLICY IMPLICATIONS
XinQi Dong, M.D., M.P.H.
Rush University Medical Center
Introduction
The dramatic growth of the American elderly population has great implications for our healthcare, social welfare, justice, and financial systems. There are approximately 40 million people over the age of 65, and by 2030, there will be more than 72 million older adults, more than twice the number in 2000, of whom those over the age of 85 are the fastest-growing segment of the elderly population (Administration on Aging, 2011). Elder abuse is a substantial global public health and human rights problem. The World Health Organization (2002) has declared that elder abuse is a violation of one of a human being’s most basic fundamental rights, to be safe and free of violence. Elder abuse includes physical abuse, sexual abuse, emotional abuse, neglect (both caregiver and self-neglect), and financial abuse. Available prevalence data suggest that at least 10 percent (or 5 million) of the U.S. elderly persons experience abuse each year, and many of them experience it in multiple forms (Acierno et al., 2010; Beach et al., 2010). In addition, data from U.S. Adult Protective Services Agencies depict an increasing trend in the reporting of elder abuse (Teaster et al., 2004). This trend is particularly alarming as the literature suggests that elder abuse is associated with increased risk of morbidity and mortality (Dong, 2005, 2011; Dong et al., 2009b, 2010, 2011b; Lachs et al., 1997, 1998, 2002).
The notion of “granny-battering” was initially introduced as a letter to the editor in the British Medical Journal in 1975 containing multiple descriptions of elder abuse and neglect perpetrated by family members (Burston, 1975). Despite the accessibility of adult protective services and nursing home regulations in all 50 states, as well as mandatory reporting laws for elder abuse and neglect in most states, an overwhelming number of abused and neglected elderly pass through our healthcare system undetected and untreated. Many cases involve only subtle signs such as poor hygiene or dehydration and can easily be missed. It is estimated that only 1 in 14
cases of elder abuse and neglect comes to the attention of authorities (NRC, 2003). The direct medical costs associated with these violent injuries are estimated to add more than $5.3 billion to the nation’s annual health expenditures (Mouton et al., 2004). Over the last few decades, the child abuse prevention movement has prompted extensive investigation and publicity, but attention to elder abuse and neglect has been relatively lacking across most disciplines. This paper discusses the medical implication of elder abuse as well as policy implication at the national level.
Quality of Life
Functional Impairment and Dependency
Functional status is the foundation of geriatric medicine and has a direct impact on elders’ ability to live successfully within their environment. Older people who have difficulty performing activities of daily living are more often neglected, particularly if their problem involves eating (Homer and Gilleard, 1990; Kleinschmidt, 1997). Demented patients who cannot perform activities of daily living sustain more physical abuse (Coyne et al., 1993). Neglect most commonly affects those who have no one to turn to for help, are in poor health and function, or live alone (Podnieks, 1992). This subsequently creates a vicious cycle of progressive inability to perform daily functions as the result of mistreatment and then increases risk for additional insults of abuse and neglect.
Other studies have suggested that functional impairment leads to dependency and vulnerability in the elderly (Jones et al., 1997). Most people understand that older adults may need some assistance, but being primarily dependent on others over prolonged periods of time is looked upon negatively either by older people themselves or by those who must care for them. Such dependency is often viewed with fear, dread, disrespect, embarrassment, and disapproval. We accept dependency in children because we understand that children need their parents for survival, but children grow up and gradually become less dependent. This is not true for those elderly who become functionally dependent because of physical or mental impairments. These impairments are likely to deteriorate over time, given the nature of chronic illness. The older adult becomes gradually more dependent and therefore more defenseless to the action of abuse and neglect (Steinmetz, 1990). The type of dependencies encountered can include economic dependency, as the individual moves from being a producer to a consumer; physical dependency arising from waning physical strength and energy and diminishing ability to perform activities of daily living; social dependency, accruing if mobility becomes problematic; and emotional dependency, often a corollary of the other forms of dependency (Cantor, 1991).
Self-Rated Health and Helplessness
Poor self-reported health is strongly associated with mortality and adverse health outcomes. The abused and neglected elderly suffer many losses as well as progressively declining health status. From the Missing Voices Series, elderly in eight different countries were surveyed regarding the effect of abuse and neglect (WHO, 2002). The elderly expressed desperation because of the feeling of insecurity, loss of dignity, disrespect, and poor state of health as a result of abuse and neglect. The vulnerable elderly often quoted that “one rude word said to an old man is stronger than stabbing him with a knife” and “respect is better than food and drink.” Given the expansion and modernization of many developing countries, many elderly from this series felt that family bonds are collapsing, in so much as there is less respect and more carelessness toward the elderly and their health is suffering as a result of such abuse.
Frequently the older person reacts to abuse and neglect with denial, resignation, withdrawal, fear, or depression. These reactions can subsequently result in feelings of guilt, shame, helplessness, and worthlessness. Through the multiple losses of power that can come in old age, some elders may come to feel that they are a burden to others. Some older people react by becoming more submissive, which in turn may invite more abuse and neglect by a malicious or unsympathetic caregiver. Many older people come to believe that events are beyond their control, and feelings of impotence take root. The elder, helpless to change the abusive environment, stops trying to do anything and accepts whatever treatment is presented. This phenomenon was described by Seligman (1975), who termed it “learned helplessness.” Seligman postulated that helplessness produces emotional disturbances. The motivation to respond to a situation is exhausted if the elderly feel nothing can be done to affect the outcome. This is also due to an increased inability to perceive success. The elder may do something that does indeed change the situation for the better but may not be aware of the success or may not fully realize that his or her action has made a difference. Hence, even success becomes failure. Such perceived helplessness produces fear as long as the person is uncertain of being able to influence what happens, and then it produces depression.
Fear and Social Isolation
Access to the abused and neglected elderly can be difficult for healthcare providers, in part because the perpetrator may block efforts to intervene and further induce isolation of the victim. As a reaction to the abuse and neglect, most victims will react with anger, disappointment, fear, or grief. At other times, the elderly will not cooperate with the healthcare worker in providing
services to take action toward the alleged abuser because they believe that little can be done to improve their situation and fear further abuse (Bookin and Dunkle, 1985). If elderly people perceive investigation of abuse and neglect as an intrusion into their lives, they will demonstrate this through resistance to the service provided (Longres, 1994). Resistance may be demonstrated thusly: elderly clients will directly or indirectly let the elder abuse investigator know that they are uncomfortable with the service provided and that their discomfort will be reflected in the outcome of the service process. That is, there will be lower rates of substantiation, higher rates of service refusal, and a gap between the service needed and that provided.
Evidence suggests that older adult who were abused and neglected are more likely to be socially isolated (Dong and Simon, 2008, 2010; Lau and Kosberg, 1979). Among a multitude of explanations are fear of retaliation, embarrassment, unwillingness to initiate legal action, trepidation that the solution to the problem will be worse than the problem itself, beliefs that they are being “paid back” for their earlier abusive behaviors, and perceiving their dependence as the cause of the problem. Many older people are concerned about their family privacy and fear public exposure and the embarrassment and humiliation that such exposure will bring. They may worry that they will not be believed, because the alleged abuser may act differently in public. A study of black, white, and Asian subjects showed differences in perception of abuse and neglect and in help-seeking patterns (Moon and Williams, 1993). The study identified differences in formal and informal help-seeking attitudes between groups. In a recent study, Chinese Americans were less likely to seek help and further induce social isolation (Dong et al., 2011a). They did not want to reveal “family shame” to others or create conflict among their relatives, yet they were not able to get any external help in their environment and alleviate the causes of the abuse and neglect. When the alleged abuser is an adult child, the victim may feel disgraced for having raised a child who would betray him or her in any way.
The elderly and their caregivers are often caught together in emotional turmoil that they cannot comprehend and for which there are no easy solutions. There are circumstances in the lives of older persons that make the caregiver role difficult to maintain. Older persons tend to lose their roles, suffer losses that cannot be recovered, and require more services than are available to them. Linked to these feelings of shame and embarrassment is anxiety about what will happen when others find out about the abuse and neglect. They do not want to admit their vulnerabilities, betray loved ones, or report abuse and neglect to the authorities or outsiders. Victims of abuse and neglect may also fear that losing a caregiver will result in institutionalization. Their fear may be true, as reflected in a study in which 60 percent of abused and neglected victims admitted for short-term care remained institutionalized permanently (Faulkner, 1982). The older person may also
realistically fear that if the abuse and neglect is reported, the perpetrator will strike back with additional mistreatment. Alleged abusers may threaten to inflict more severe abuse; destroy property or pets; or even kill their victims, other loved ones, or themselves (Breckman, 1988).
Psychological Distress
Over the last few decades of research, stress and stressful life events have been linked to the onset of illness and other maladaptive behavior at both the individual and the societal levels. Victims of abuse and neglect suffer more than just the debilitating physical or material consequences of the acts. Becoming a victim challenges most people’s basic assumptions about safety and security. Research has demonstrated that elder abuse victims have higher risk for psychological distress (Dong et al., 2008, 2009a, in press) and also begin to question themselves and to see themselves as weak, frightened, out of control, powerless, and lacking a sense of autonomy (Nahmiash, 2002). In a case-control study of elderly patients referred for abuse and neglect to a geriatric assessment clinic, the study found a higher prevalence of depression in victims of mistreatment compared to patients referred for other reasons (Dyer et al., 2000). Victims of elder abuse and neglect tend to blame themselves for abuse and harbor much guilt and low self-esteem (Podnieks, 1992).
Other studies have highlighted the individual’s relative ignorance of psychological abuse in contrast to physical abuse, perhaps in part because of the difficulty in identifying observable consequences of psychological abuse (Childs et al., 2000). Neville et al. (1999) found that the most common reasons for psychiatric admission for such a population were due to behavior problems, self-neglect, psychotic symptoms, and other psychiatric illness. Sensitivity to the psychological states of elder abuse and neglect may be especially important because it may assist in the early and accurate identification of elderly persons at risk. Such persons may be more prone to depression and may engage in suicide and other self-destructive behaviors (McIntosh and Hubbard, 1988).
Morbidity and Mortality
Healthcare System Utilization
Elder abuse and neglect are recently recognized forms of family violence, but much less is known compared to child or spousal abuse, with respect to how elder abuse victims interact with the healthcare system. Mouton and Espino (1999) found that older women who experienced abuse were likely to consult medical practitioners with conditions such as
physical injuries, gynecological complaints, gastrointestinal disorders, fatigue, headache, myalgias, depression, and anxiety. Yet the true underlying abuse and neglect of the elderly remain to be discovered. Those patients often also have frequent nonspecific presentations to the outpatient settings. An effective strategy to address family violence in all its forms in the nonemergency outpatient setting would certainly improve the quality of life for those individuals and perhaps reduce healthcare cost at the same time.
Evidence suggests that abused and neglected community elders recognized through a state elderly protective services program are more likely to come to the emergency room for assessment and treatment (Dong, 2011; Lachs et al., 1997). One-fourth of emergency room visits had ICD-9 (International Classification of Diseases, ninth revision) codes consistent with injury, and 66 percent of the subjects who used emergency services had at least one emergency room visit with injury-related discharge diagnosis or chief complaint. No single injury type or chief complaint emerged as highly prevalent in this population. Jones et al. (1997) retrospectively examined medical records of elder abuse and neglect cases that were identified through the emergency room. In this study, elder neglect presented to the emergency room exceeded physical abuse, bruises, lacerations, and other injuries. Other presentations of abuse and neglect included dehydration, fractures, and failure to thrive (Jones, 1994).
The metaphor of a “frequent flyer” in the emergency room should raise caution to healthcare professionals, especially relating to the magnitude of an elderly patient’s healthcare needs. Becoming aware of those repeated presentations to the emergency room should lead us to explore in greater detail the nature of the elder’s health status and medical management and to express concern about the adequacy of the elder’s healthcare management by caregivers and healthcare professionals. Elderly patients who have recurrent visits to the emergency room should be considered at greater risk for abuse and neglect (Fulmer et al., 2003). The high flow of a busy emergency room should be seen not as an impediment to care but as an opportunity to influence the lives of frail elderly.
Nursing Home Placement
Adult Protective Services (APS) is the official state entity charged with promoting advocacy and protecting victims of elder abuse and neglect. Elderly referred to protective services represent some of the most frail, isolated, and medically and psychiatrically ill older members of society. Nursing home placement is a drastic, restrictive, and costly intervention, and it is one of the most difficult decisions that adult protective services workers and elder abuse field workers face. One of the first papers published on outcomes of elder abuse and neglect appeared in the 1970s. The authors found that by
being referred to adult protective services, the elderly were more likely to be institutionalized (Blenkner et al., 1971). One of the troubling findings of this paper was that a system intended to protect the health and independence of the vulnerable elderly was causing institutionalization. Others have suggested that services utilization rather than adult protective services use may be the reason for increased probability of nursing home placement.
In a community-based cohort of older adults (New Haven Established Population for Epidemiologic Studies in the Elderly [EPESE]), the study team matched data with adult protective services records. The cohort had been previously linked with a long-term care data registry in the State of Connecticut, permitting the certainty of nursing home placement records for all cohort members. This study found that the number of abused and neglected elderly referred to adult protective services is a compelling predictor of nursing home placement, even after adjusting for other variables known to be associated with institutionalization in the older population (Lachs et al., 2002).
Mortality
A 10-year retrospective case review of morbidity and mortality among elders was conducted at a state medical examiner’s office serving a major metropolitan region in Kentucky and Indiana (Shields et al., 2004). The study addressed medical-legal autopsies and the examination of living subjects pursuant to a clinical forensic medicine program. The authors presented 74 postmortem cases, in which 52 deaths were attributed to a homicidal act and 22 deaths were suspicious for neglect. Of the 22 living victims of elder abuse and neglect, 19 cases constituted physical and/or sexual assault and 3 individuals suffered from neglect. Furthermore, 81.8 percent of the neglect cases had physical injuries, including abrasions and contusions; 95.4 percent of the neglect cases revealed decubitus ulcers. Lachs et al. (1998) investigated the independent contribution of reported elder abuse and neglect to all-cause mortality in the EPESE cohort. At the end of the 13-year follow-up, elder abuse victims had poorer survival (9 percent) than either those seen for self-neglect (17 percent) or other non-investigated members (40 percent).
Recent data from Dong et al. (2009c) examined the relationship between elder abuse and mortality (all-cause and cause-specific) of 9,813 participants within the context of a longitudinal population-based cohort: Chicago Health and Aging Project (CHAP). The authors found that elder abuse was associated not only with increased all-cause mortality, but also with increased cardiovascular-related mortality over the 15 years of follow-up (Dong et al., 2009c). In addition, mortality associated with elder abuse was most prominent among those with the lowest levels of cognitive or
physical function and the highest levels of psychological distress and social isolation (Dong et al., 2009b, 2010). Moreover, Dong et al. (2011b) found that black older adults with self-neglect had significant higher mortality risk than white older adults in the same CHAP cohort.
Policy Implication for Elder Abuse
The field of elder abuse is estimated to be 40 years behind the field of child abuse and 20 years behind the field of domestic violence. While there have been strong national policies dealing with child abuse and violence against women, there has been a great paucity of national policy to prevent elder abuse and to protect victims of elder abuse. This paper highlights the existing elder abuse programs through two major federal laws: the Older American Act (OAA) and the Violence Against Women Act (VAWA).
The OAA is responsible for funding the National Center on Elder Abuse to provide grants to states’ elder justice system and state agencies to develop and enhance programs to address elder abuse. The OAA establishes long-term care ombudsman programs to identify, investigate, and resolve complaints related to these institutions; state-based services designed to provide legal assistance and other counseling services; and programs to support locally relevant projects, supportive services, and outreach and advocacy programs. Finally, the OAA designates state agencies and area plans and develops objectives, priorities, policy, and long-term plans for elder abuse prevention and services.
The VAWA authorizes the attorney general to formulate grants to enhance training and services to end violence against and abuse of older women. This program is intended to assist law enforcement, prosecutors, and local courts on the issues of elder abuse. In addition, the VAWA authorizes the attorney general to create grants that provide or enhance services for elder abuse victims, conduct cross-training for organizations serving elder abuse victims, and create or support multidisciplinary collaborative community responses to the victims of elder abuse.
Based on a recent Government Accountability Office (GAO) report to the Department of Health and Human Services, elder abuse-related spending in 2009 included $1.1 million by the National Institutes of Health, $50,000 by the Centers for Disease Control and Prevention, $5.9 million by the Administration on Aging, $0.75 million by the Department of Justice Civic Division, and $1.2 million by the National Institute of Justice. The Office of Victims of Crimes and the Office on Violence Against Women spent $520,000 and $4.9 million, respectively. In 2009, these federal agencies spent $11.9 million for all activities related to elder abuse. This contrasts to the annual funding for violence against women programs ($649 million). Despite the well-intentioned services by these seven federal
agencies, the most basic needs are not met to protect older adults from abuse, neglect, and exploitation.
The Elder Justice Act (EJA) was passed as a part of the Affordable Healthcare Act, and for the first time, the EJA authorizes federal response to the issues of elder abuse through training, services, and demonstration programs. The Administration on Aging is responsible for the implementation of the EJA as well as formation of the Elder Justice Coordinating Council and the National Advisory Board. More specifically, the Elder Justice Coordinating Council will be required to issue reports to describe the activities, accomplishments, and challenges faced, as well as to provide legislative recommendations to congressional committees. The National Advisory Board, which will be required to submit reports and recommendations regarding elder justice activities, has already solicited nominations.
The EJA will also be responsible for issuing human subjects protections guidelines to assist researchers and for establishing elder abuse forensic centers. The EJA will provide grants and incentives for long-term care staffing and electronic medical records technology grants programs and will collect and disseminate annual data related to elder abuse from adult protective services. The EJA will also be responsible for sponsoring and supporting training, services, reporting, and the evaluation of elder justice programs in community and long-term care settings. Regrettably, compared to the previous EJA from the 109th Congress, key elements were dropped in the current bill, which include, but are not limited to, the national data collection effort; the consumer clearinghouse; and grant programs for prevention, detection, assessment, and treatment of, intervention in, investigation of, and prosecution of elder abuse.
The EJA has authorized $777 million funding over four years, and immediate appropriation is particularly important, because APS will garner significant funding to bolster direct services to victims. Recently, a survey in 30 states reported that 60 percent of APS programs have faced budget cuts on average of 14 percent, while two-thirds of the APS reported an average increase of 24 percent in elder abuse reports. A recent letter from the Leadership Council of Aging Organizations strongly urged the Senate and House Subcommittee on Labor, Health and Human Services, and Education to fully appropriate the EJA (Leadership Council of Aging Organizations, 2010).
In March 2011, the Senate Special Committee on Aging held a hearing on elder abuse: “Justice for All: Ending Elder Abuse, Neglect and Exploitation.” Based on the GAO (2011) report, victims and experts highlighted the lack of research, education, training, and prevention strategies. In June 2010, the National Institute on Aging and the National Academy of Sciences hosted a state-of-science conference on elder abuse and highlighted the research progress and gaps and recommended research priorities to advance the field of elder abuse.
National representative longitudinal studies are needed to examine the incidence of elder abuse subtypes and to elucidate risk and protective factors and adverse health outcomes associated with incident cases. Unified national APS data collection could aid in examining the needs, processes, outcomes, and efficacy of the current system. Future research must be innovative, multidisciplinary, collaborative, and cost-effective in order to devise targeted prevention and intervention strategies. With the increasingly diverse U.S. population and the variations in the definition of elder abuse, cultural issues must be addressed (Dong et al., 2011a).
Education and training are critically needed for healthcare professionals, law enforcement, social services, community organizations, and others who have contact with older adults. As child abuse and domestic violence training are mandatory parts of health professional education, so should elder abuse training be. Training and resources for the APS and other frontline workforce will be critical to alleviate factors exacerbating the abusive situation and to prevent elder abuse recidivism of an already vulnerable population. This is especially critical because most APS departments are facing budget cuts and increasing demands in their daily work.
In sum, elder abuse is a pervasive public health and human rights issue, yet there are major gaps in funding, policy, research, education, and training. The full appropriation of the EJA is critically needed. National representative longitudinal research is needed to better define the incident, risk and protective factors, and consequences of elder abuse in diverse racial and ethnic populations. Collective federal, state, and community efforts are needed to support the APS services, training, and education of diverse disciplines dealing with aging issues.
Epilogue: “For years, I suffered silently, unable to muster the courage to seek the help I knew I needed…. I felt trapped, scared, used, and frustrated. And above all, when a man feels helpless, it’s terrible. And I was helpless.” Mr. Mickey Rooney, Elder Abuse Victim, at the Hearing of the Senate Special Committee on Aging, March 2011.
COSTS OF FIREARM VIOLENCE: HOW YOU
MEASURE THINGS MATTERS
David Hemenway, Ph.D.
Harvard School of Public Health
The Centers for Disease Control and Prevention (CDC) estimates that, in 2005, the societal cost for all suicide in the United States was $26 billion, the cost of all unintended poisoning deaths was $23 billion, and the cost of all homicides was $20 billion (CDC, 2011). These cost estimates come from adding together the medical costs and the productivity losses.
These are, of course, only estimates, but they put the societal cost of suicide and poisoning deaths above that of homicide. I believe these estimates are misleading, can lead to bad policy decisions, and illustrate why the way you measure things matters.
There are many ways to categorize costs. One is to divide the cost burden into three components: (1) to the individuals directly involved, (2) to the family and friends, and (3) to the community at large. For a suicide or an unintentional poisoning death, most of the costs fall on the individual who dies and on the family and friends who suffer grief and personal loss. There is some, but not a large, cost to others in the community.
By contrast, consider the cost of a street firearm homicide (most homicides in the United States are firearm homicides that occur outside the home; by contrast, most suicides occur at home).
There are usually direct costs to two individuals and two families rather than one—not only to the victim, but probably also to the shooter, who is often caught, convicted, and incarcerated. In addition, there are the costs to the community associated with criminal law enforcement, including the costs of police, district attorneys, judges, parole officers, and prisons.
There are also large psychological costs caused by street violence. Exposure to violence (e.g., witnessing violence) increases the risk for psychiatric, emotional, behavioral, and health problems. Psychiatric problems include posttraumatic stress disorder (PTSD), depression, anxiety, intrusive thoughts, sleep problems, and personality change. Emotional problems include anger, nervousness, withdrawal, loneliness, and despair. Behavioral problems include low academic performance, risky sexual behavior, substance abuse, delinquency, and violence. Finally, exposure to violence has been linked to such health problems as asthma, heart disease, and low-birth-weight babies.
There are also high community costs of street crime that accrue when people and institutions try to avoid the shootings and protect themselves. Commercial and residential locations can be affected. Businesses do not want to locate in areas of high crime, tourists do not want to go there, and people do not want to live there. This leads to fewer jobs and to flight from the neighborhood of higher-income people who can afford to leave (e.g., “white flight”). The loss of jobs, good stores, community social capital, and positive role models leads to neighborhood deterioration.
To avoid being shot, residents also change their behavior concerning recreation, shopping, leisure, and other activities. Children are not allowed to play outside, residents are less likely to go out at night, and they are less likely to accept evening work. People live behind locked doors. Having fewer people on the street further reduces the safety of being on the street.
When people and institutions cannot avoid danger, they often try to protect themselves from it (e.g., “target hardening”). Schools use metal
detectors and police wear bulletproof vests. To protect themselves, juveniles might obtain guns and join gangs, which further increases the problem of lethal violence.
Indeed, one of the major costs of street gun violence is that it creates “positive-feedback” loops, leading to more street gun violence. Retaliation against street gun violence is common, as victims and their friends retaliate against those they perceive to be the perpetrators. Trauma to bystanders, victims, and even perpetrators increases the likelihood of even more violence, and higher levels of violence can lead to the “normalization” of violence, opening the door to still more violence. Attempts by individuals and institutions to avoid the violence can lead to neighborhood deterioration, creating a setting for additional violence. Finally, attempts by young people to protect themselves by acquiring guns and joining gangs exacerbate the problem.
Using medical costs and productivity losses to estimate the societal cost of injury is a common, if somewhat controversial, economic approach. However, for some injuries, such as street killings, this approach misses more of the total costs than it does for other injuries, such as unintentional poisonings and suicide. When a 24-year-old urban male dies from either a street killing or an unintentional poisoning, the medical and productivity costs may be similar, but the actual costs to society are far different.
If the measured costs of various injuries are going to be used to help target prevention efforts, it is important to get the relative costs correct. The current CDC approach focusing exclusively on medical and productivity losses vastly underestimates the relative costs to society of street violence.
Recommendations
The costs of firearm violence in the United States are enormous. The first step in the public health approach to reducing violence is to create a good surveillance system. The United States has such a system—the National Violent Death Reporting System, but it operates in only 20 states. The National Violent Death Reporting System should be expanded to cover the entire United States.
The second step in the public health approach is to determine the causes and correlates of violence. Unfortunately, funding for scientific studies of firearm violence is miniscule related to the size of the problem. Currently, for example, the CDC provides no funding for this injury issue, and only one foundation provides consistent funding for research on firearm injuries. Funding for research on firearm violence should be expanded.
The scientific knowledge that exists has to be disseminated, and false beliefs need to be corrected. Currently there are few respected and reliable sources providing accurate information about firearm violence and its prevention. The Surgeon General of the United States should issue
periodic reports about what the science tells us about firearm violence and its prevention.
THE CONTAGION OF VIOLENCE:
THE EXTENT, THE PROCESSES, AND THE OUTCOMES
L. Rowell Huesmann, Ph.D.
Institute for Social Research, University of Michigan
One of best-established findings in the psychological literature on aggressive and violent behavior is that violence begets violence. This contagion of violence appears to be a universal phenomenon. The contagion of violence occurs within families. Violence between partners increases the risk of violence directed at children and increases the risk of the children behaving violently themselves. Having one violent individual in a family makes it more likely there will be others. It is true within peer groups. Violence by some peers increases the risk of violence by others. Violence by peers directed outward not only stimulates violence by others that is directed outward, but stimulates violence between peers within the group. This is true in neighborhoods and communities. Violent communities and neighborhoods breed violence in those who join the community or neighborhood. Introducing violence into a community increases the risk of greater violence throughout the community. It even appears to be true within nations and cultures, and it is true across generations. Children “catch” it from their parents, and parents can catch it from their children.
Violence is highly contagious. Not only is it spread from the perpetrators of violence to the victims, but it is spread to onlookers and observers. It is not surprising that violent victimization leads to violent retaliation within and between families, peer groups, schools, communities, ethnic groups, cultures, and countries. What may be more surprising to some is that simply the observation of violence also leads to increased violence within and between all of these groups. Violence can even be spread to faraway people who observe it at a distance. The boundaries of time and space that apply to most biological contagions do not apply to the contagion of violence.
Why is violence so contagious and how does it spread? What psychological processes are involved? How could the spread be halted? These are some of the questions addressed in this paper.
Severe violent behavior is almost always the product of predisposing individual differences and precipitating situational factors (Huesmann, 1998). One important environmental experience that contributes both to predisposing a person to behave more violently in the long run and to precipitating violent behavior in the short run is the observation of violence. Psychological theories that have emerged over the past few decades now
explain the short-term precipitating effects mostly in terms of priming, simple imitation, and excitation transfer. Priming is the neurological process through which seeing violence produces a spreading activation in the neurons of the brain that stimulates all sorts of ideas related to violence, making violence more likely. Imitation of violence in the short run occurs because human beings, from a very young age, have a wired-in tendency to mimic whatever they see. Excitation transfer means that when someone provokes us, we feel more angry if we have recently been aroused and made angry by something we observed, such as violence.
The long-term predisposing effects of observing violence, however, involve more complex processes of observational learning of cognitions and of emotional desensitization. Obviously being victimized always also includes observing violence—part of the mind of the child who is being spanked or the youth who is being beaten up is observing the interaction while another part is suffering from the interaction. Although the emotional reactions to victimization may be more intense and immediate, observation alone also produces both intense emotional and intense cognitive reactions that can have long-term effects on a person’s mental health (e.g., post-traumatic stress disorder [PTSD] symptoms) and behavior problems (e.g., violent behavior). This is diagrammed in Figure 6-1.
Before elaborating on these processes for the contagion of violence in more detail, I want to present an example of the phenomenon of contagion of violence through observation. Probably no children in the world are exposed to more violence on a day-in and day-out basis than those who live in regions of war and ethnic violence. They are regularly exposed to scenes of extreme human violence at rates that would be hard to find even in America’s most violent ghettos. My research team has just finished collecting data on children in one such region—Palestine (West Bank and Gaza) and Israel (Israeli Jewish and Arab communities). We interviewed 600 Palestinian, 450 Arab Israeli, and 450 Jewish Israeli children and their parents individually three times at 1-year intervals from 2007 to 2010. At the start of the interviews the children were either 8, 11, or 14 years old. Each year we asked the children and their parents to report on how much violence they had been exposed to in the past year. For example, we asked, “How often have you seen right in front of you Palestinian (or Israeli for Israeli children) buildings or buses or other property destroyed by Israelis (or Palestinians for Israeli children)?” We asked many questions of this type, including about “seeing a family member die,” “seeing friends die,” “seeing them injured,” “seeing them held hostage or tortured,” etc. The rates of observation in person were very high—for example, 55 percent of Palestinian children had seen a friend die due to the Israelis, 43 percent had seen someone tortured or held hostage, and 63 percent had seen someone crying because someone they knew had died. The rates of seeing
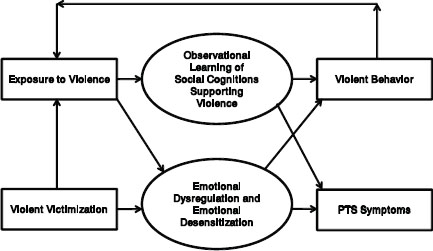
FIGURE 6-1 The psychological processes promoting the contagion of violence. SOURCE: Huesmann, 1988.
such things rose to more than 90 percent for the past year when observing in the mass media was included. The rates for Israeli Jewish children were about half as much and for Israeli Arab children half as much again, but even among them, about 1 out of every 20 children had seen someone killed or be seriously injured in front of them in the past year.
These rates are appallingly high. The question is, Does such exposure to such violence increase the aggressive and violent behavior of the children subsequently? The answer, we discovered, is clearly yes. The violence spreads like a contagious disease among them. For example, as shown in Figure 6-2, Palestinian kids and Israeli Jewish kids who fall in the top 25 percent on the amount of war violence they have seen in 1 year are 15 percent more likely to punch or beat a peer than kids who fall in the lowest 25 percent on violence exposure, and Arab Israeli youth in the highest quartile on exposure are about 30 percent more likely to punch or beat a peer during the year. These youth have not been victimized by their peers; yet they attack their peers. In fact, we found that those who are in the highest 25 percent on exposure are also significantly more likely to go beyond “punching” and to commit very serious acts of violence against their peers, including using knives or guns on them. These results cannot be explained by demographic differences, age differences, or gender differences. Differences in exposure to violence account for more of the individual differences in aggression than any other single factor.
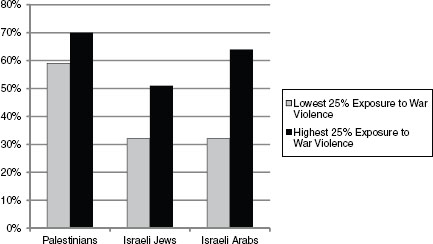
FIGURE 6-2 Children behave more violently as they see more war violence in the Middle East: Percentage that punched or beat another youth in the last year.
Because we collected the data over 3 years, we can also rule out the idea that more violent or aggressive youth expose themselves to more war violence. No, the direction of the effect is clearly that exposure to violence stimulates later increases in aggression even after we control for initial differences in aggression. For example, for 8- and 11-year-olds the causal path coefficients from exposure to violence in year 1 of the study to change in aggression from year 1 to year 3 are about .30, while the causal path coefficients from aggression in wave 1 to increases in exposure to war violence between wave 1 and wave 3 are about 0. For the oldest cohort only is there some evidence that aggression makes later exposure more likely, but it is significantly smaller than the effect that exposure has on later aggression.
What produces this kind of contagion of violence over time? The contagion is promoted by the fact that children grow up in an ecology of nested spheres of influence in which, as Bronfenbrenner (1979) and Sameroff (2010) have pointed out, macro-environments such as war settings influence micro-environments such as the family, which in turn affect the child who in turn affects the micro-environments around him or her. Children are most directly influenced by a micro-system of influences that are close to them—most notably, family and peers. However, family and peers in turn are influenced by the schools and communities in which they reside, and these in turn are influenced by more distal systems such as the ethnopolitical culture, the mass media, and the country. These ecological systems are not independent. Each influences and is influenced by the systems within which
it is nested and by the systems nested within it. Thus, violence or nonviolence in a country influences violence in communities and subcultures, which influences violence in schools and families, which influences violence in youth. This is exactly what we have found in our study of Palestinian and Israeli youth. In regions where more war violence occurs, we found more intracommunity violence and more intrafamily violence. These in turn stimulate more youth violence.
However, this ecological proximity effect does not explain why violence is so contagious that it is spread by observation alone, even if the observation is at some physical distance. The answer to this puzzle is provided by the way in which the human information processing system has evolved to make humans adaptive for survival—in particular, by evolving mechanisms for encoding cognitive scripts to imitate observed behaviors of others (observational learning) and by evolving mechanisms for adaptation to emotionally disturbing environments to reduce the stress they produce (desensitization).
We know that all social behavior is guided by encoded scripts (programs for behavior) that we all have acquired as we grew up. When confronted with a social problem, young people first make attributions about what is going on in the situation and then retrieve from their minds whatever social scripts are most easily recalled and seem most relevant. These generally are scripts that are most strongly primed by the social situation and have been most strongly learned from past experiences. Thus, a boy who has grown up observing violence around him almost every day (whether war violence, neighborhood violence, gang violence, school violence, or family violence) will believe that the world is a hostile place and will be biased toward making hostile attributions about those who annoy him. Such attributions and the repertoire of aggressive scripts the boy will have encoded over time will then make it more likely that he will use an aggressive social script for dealing with such a person. Additionally, he will be more likely to view behaving in such an aggressive manner as normative and acceptable. Equally importantly, repeated exposures to violence will blunt the negative emotional responses (anxiety and fear) that humans normally experience when they see violence or think about violence. What will remain is the angry emotional distress that, through excitation transfer, can exacerbate the young person’s tendency to behave aggressively. Thus, the more a young person is exposed to war violence, the more likely he or she is to behave violently toward others, even though the others may have no connection to the war violence. This process is illustrated in Figure 6-3, which is taken from our recent study of Palestinian and Israeli youth. The numbers in this diagram show the strength we found for the causal effects represented by the arrows. The 14-year-olds in this diagram who have been exposed to the most political conflict or violence in year 1 fantasized more
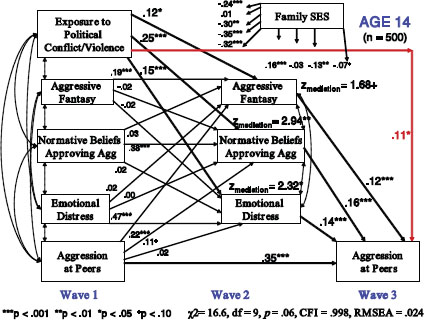
FIGURE 6-3 Exposure to violence stimulates later increases in aggression.
about behaving aggressively in year 2 (that is, they rehearse aggressive scripts more), held stronger beliefs that aggressive behavior toward others is okay in year 2, and showed higher levels of emotional distress in year 2. Each of these effects in turn stimulated them to behave more aggressively toward their peers in year 3.
Summary
Violence is clearly contagious. While being victimized by violence promotes more violence, all that is really required is viewing violence. There are now many other examples in the scientific literature, besides the one discussed above, that demonstrate how habitual observation of violence by young people leads to behaving more aggressively. Violence is contagious in multiple contexts. It is contagious in the short run and in the long run. The contagion is mediated by both changes in emotions and changes in cognitions caused by repeated exposures to violence. These neurological and psychological reactions are “wired-in” and probably evolutionarily adaptive. Consequently, it is difficult to intervene to prevent the contagion of violence other than by preventing the observation of violence. However,
the most promising additional interventions would undoubtedly be those that are directed at counteracting the changes in cognitive and emotional processing that the observation of violence engenders.
HOW PERSISTENT FEAR AND ANXIETY CAN AFFECT YOUNG
CHILDREN’S LEARNING, BEHAVIOR, AND HEALTH5
Nathan A. Fox, Ph.D.
Department of Human Development, University of Maryland6
Jack P. Shonkoff, M.D.
Center on the Developing Child at Harvard University7
Evidence from neuroscience is increasingly helping us to understand exactly how fear and anxiety in childhood—such as that occasioned by exposure to violence in the family—shape the young child’s developing brain, with lasting effects on learning and development. In this article, Professors Nathan A. Fox and Jack P. Shonkoff review the evidence and its implications for public policy.
Ensuring that young children have safe, secure environments in which to grow, learn, and develop healthy brains and bodies not only is good for the children themselves but also builds a strong foundation for a prosperous, just, and sustainable society. That said, science shows that early exposure to violence and other circumstances that produce persistent fear and chronic anxiety can have lifelong consequences by disrupting the developing architecture of the brain. While some of these experiences are one-time events and others may reoccur or persist over time, all of them have the potential to affect how children learn, solve problems, relate to others, and contribute to their community.
All children experience fears during childhood, including fear of the dark, monsters, and strangers. These fears are normal aspects of
___________________
5 Reprinted courtesy of Early Childhood Matters (June 2011), Bernard van Leer Foundation. The authors wish to advise that the article was originally adapted from the following publication: National Scientific Council on the Developing Child (2010). Persistent fear and anxiety can affect young children’s learning and development. Working Paper 9. Cambridge, MA: Center on the Developing Child at Harvard University. Available at http://www.developingchild.net (accessed April 2011).
6 Nathan A. Fox, Ph.D., is distinguished professor at the Institute for Child Study, Department of Human Development, and director of the Child Development Laboratory, University of Maryland.
7 Jack P. Shonkoff, M.D., is the Julius B. Richmond FAMRI Professor of Child Health and Development at the Harvard School of Public Health and Harvard Graduate School of Education; professor of pediatrics at Harvard Medical School and Children’s Hospital Boston; and director of the Center on the Developing Child at Harvard University.
development and are temporary in nature. In contrast, threatening circumstances that persistently elicit fear and anxiety predict significant risk for adverse long-term outcomes from which children do not recover easily. Physical, sexual, or emotional abuse; significant maltreatment of one parent by the other; and the persistent threat of violence in the community are examples of such threatening circumstances.
Unfortunately, many children are exposed to these kinds of experiences. Child maltreatment has been shown to occur most often in families that face excessive levels of stress, such as that associated with community violence, parental drug abuse, or significant social isolation (CDC, 2009). Research also tells us that nearly half of children living in poverty in the United States witness violence or are indirectly victims of violence (Finkelhor et al., 2005). Globally, despite more limited data, the risks are as bad or worse. In 2006, the United Nations Secretary-General’s Study on Violence against Children reported that more than 130 million children have witnessed intimate partner violence in the home, and more than 200 million have suffered some form of sexual abuse. For children living in such circumstances, frequent and repetitive threats create the potential for heightened fear and chronic anxiety.
Behavioral neuroscience research in animals tells us that serious, fear-triggering experiences elicit physiological responses that affect the architecture of the developing brain. Chronic activation of the body’s stress response systems has been shown to disrupt the efficiency of brain circuitry and lead to both immediate and long-term problems in learning, behavior, and physical and mental health. This is especially true when stress system overload occurs during sensitive periods of early brain development. Despite this rapidly increasing knowledge base, however, significant gaps continue to exist in how societies respond to the developmental needs of children who regularly experience serious, fear-inducing events.
The Science of Fear and Anxiety
Some types of fear are normal aspects of development. Infants begin to experience feelings of fear and differentiate them from other emotions between 6 and 12 months of age (Lewis and Michalson, 1983; Nelson and DeHaan, 1996). Over the course of the early childhood period, toddlers and preschoolers typically express fear of a wide variety of events or individuals. Generally speaking, normal preschool fears do not disrupt a child’s life, and they dissipate by age 7 or 8. That is, while children may express these fears at certain times (such as bedtime) or in response to certain events (for example, when confronted by a stranger), their overall behavior does not otherwise suggest that they are generally fearful or distressed.
The emergence and course of typical childhood fears are different from the fears and anxiety elicited by traumatic situations such as physical or sexual abuse or exposure to family violence. While typical fears disappear with age, the fear and anxiety elicited by maltreatment and other threatening circumstances do not. Scientific research provides an explanation for why children outgrow normative fears. Many result from the difficulty young children have in distinguishing between the real and the imaginary. As they get older, children get better at understanding what is real and what it means for something to be “make believe.” They also develop the cognitive and social skills needed to better understand predictability in their environment and, therefore, gain a greater sense of control.
Early exposure to extremely fearful events affects the developing brain, particularly in areas involved in emotions and learning. A large and growing body of research, including animal studies as well as recent neuroimaging studies of human adults, has revealed groundbreaking insights into the brain circuitry that underlies how we learn to be afraid (Delgado et al., 2006; Phelps and LeDoux, 2005) and how we come to associate a specific event or experience with negative outcomes. Two extensively studied structures located deep in the brain—the amygdala and the hippocampus—are involved in fear conditioning. The amygdala detects whether a stimulus, person, or event is threatening and how persistent fear and anxiety can affect young children’s learning, behavior, and health; the hippocampus links the fear response to the context in which the aversive stimulus or threatening event occurred (Kim and Fanselow, 1992; LeDoux, 2000; LeDoux and Phelps, 2008). Studies also show that both the amygdala and the hippocampus play an important role in how the body then responds to this threat. Elevated stress hormones such as cortisol have been shown to affect the growth and performance of the hippocampus and the activity of the amygdala in rodents and nonhuman primates, and early and persistent activation of the stress response system adversely affects brain architecture in these critical regions.
Beyond its impact on these two brain structures, heightened stress has also been shown in animals to impair the development of the prefrontal cortex, the brain region that, in humans, is critical for the emergence of executive functions—a cluster of abilities such as making, following, and altering plans; controlling and focusing attention; inhibiting impulsive behaviors; and developing the ability to remember and incorporate new information in decision making. These skills continue to develop and become increasingly important throughout the school years and into adulthood. Behavioral neuroscience research in animals tells us that the prefrontal cortex is highly sensitive to the detrimental effects of excessive stress exposure and that its developing architecture is vulnerable to the negative effects of chronic fear (Arnsten, 2009).
When young children experience serious fear-triggering events, they learn to associate that fear with the context and conditions that accompanied it. Very young children can actually learn to be fearful through a process called “fear conditioning,” which is strongly connected to the development of later anxiety disorders (Grillon and Morgan, 1999; Pine, 1999). In the typical circumstances of early childhood, fear responses are activated quickly and then dissipate. However, when young children are chronically exposed to perceived or real threat, such as ongoing violence in the family environment, fear system activation can be prolonged. Conditioned fear is apparent when individuals come to experience and express fear within the context in which the learning occurred. For example, a child who is physically abused by an adult may become anxious in response to both the person and the place where the fear learning occurred. Over time, the fear elicited and the consequent anxiety can become generalized, and subsequent fear responses may be elicited by other people and places that bear sometimes only small resemblances to the original conditions of trauma. Consequently, for young children who perceive the world as a threatening place, a wide range of conditions can trigger anxious behaviors that then impair their ability to learn and to interact socially with others. The extent to which these problems affect physical and mental health is influenced by the frequency of the stressful exposure and/or the emotional intensity of the fear-eliciting event.
Unlearning fear is a fundamentally different process from fear learning. The process of unlearning conditioned fear is called “extinction” and actually involves physically separate and distinct areas of the brain’s architecture from those into which fear responses are first incorporated. Generally speaking, the unlearning process involves activity in the prefrontal cortex, which decreases the fear response by regulating the activity of the amygdala (Phelps et al., 2004; Quirk et al., 2006). Research tells us that fears are not just passively forgotten over time, they must be actively unlearned. Studies show that fear learning can occur relatively early in life (Sullivan et al., 2000), whereas fear unlearning is only achieved later, when certain structures in the brain have matured (Carew and Rudy, 1991; Kim and Richardson, 2008). Consequently, the effects of family violence in early childhood can have a significant impact on physical and mental health that can take years to remediate—something that is extremely important to understand in designing interventions for children and families who are experiencing violence.
Chronic and intense fear early in life affects the development of the stress response system and influences the processing of emotional memories (Nemeroff, 2004; Sanchez et al., 2001). When an individual is confronted with a threat, stress systems are activated and elevate the levels of several different stress chemicals that are circulating throughout the body
(McEwen, 2007). An increase in one of those chemicals, cortisol, can have a dramatic impact on how memories are processed and stored (de Kloet et al., 2008). The production of cortisol and adrenaline (as well as noradrena-line) in the brain in a normal stress response leads to memory formation for events and places that signify danger. More specifically, elevated cortisol levels can strengthen the formation of memories of emotional events ( McGaugh et al., 1996), block the ability to unlearn fear memories (Yang et al., 2007), and enhance the formation of memories of the surrounding context in which the fearful event occurred (Brinks et al., 2008). Interestingly, too much cortisol can also have the opposite effect and actually impair memory and learning in nonthreatening contexts (Roozendaal et al., 2009). Thus, the biological response to stress is intimately involved in both fear learning and fear unlearning.
Persistent fear can distort how a child perceives and responds to threat. Fear learning typically takes place in specific contexts and results in those fears’ becoming associated with the places where the learning occurred. Children may also express fear in response to situations that are similar (not identical) to those initially learned or to situations that are similar to the contexts in which the original learning occurred. These are called “generalized” fear responses, and they are thought to underlie the expression of later anxiety disorders, including PTSD (Davis, 2006; Grillon, 2002; Grillon and Morgan, 1999). Indeed, children who have had chronic and intense fearful experiences often lose the capacity to differentiate between threat and safety. This impairs their ability to learn and interact with others, because they frequently perceive threat in familiar social circumstances, such as in their home or neighborhood. These responses inhibit their ability to learn and often lead to serious anxiety disorders (Grillon et al., 1998; Reeb-Sutherland et al., 2009).
Young children who have been exposed to traumatic circumstances also have difficulty identifying and responding to different expressions of emotions and, therefore, have trouble forming healthy relationships (Wismer Fries et al., 2005). These deficits lead to general problems with social interaction, such as understanding others’ facial expressions and emotions. For example, children raised in physically abusive households show heightened sensitivity (compared with nonabused children) to angry faces, which negatively affects their brain function and behavior (Pollak and Kistler, 2002; Pollak et al., 2000). Learning to identify anger—quickly and successfully—in order to avoid being harmed is a highly adaptive and appropriate response to an abusive environment. However, an increased tendency to assume someone is angry when his or her facial expression is ambiguous can be inappropriate and maladaptive in a typical, nonthreaten-ing social setting and even dangerous in unfamiliar social settings (Pollak, 2008). Thus, the extent to which children view the world as a hostile and
threatening place can be viewed as both a logical adaptation to an abusive or violent environment and a potent risk factor for behavior problems in later childhood, adolescence, and adult life.
Early exposure to intense or persistent fear-triggering events affects children’s ability to learn. There is extensive and growing scientific evidence that prolonged and/or excessive exposure to fear and states of anxiety can cause levels of stress that can impair early learning and adversely affect later performance in school, the workplace, and the community. Multiple studies in humans have documented problems in cognitive control and learning as a result of toxic stress (National Scientific Council on the Developing Child, 2005; Shonkoff et al., 2009). These findings have been strengthened by research evidence from nonhuman primates and rodents that is expanding our understanding of the brain mechanisms underlying these difficulties.
The brain region in animals that appears highly vulnerable to adversity in this regard is the prefrontal cortex, which is the critical area for regulating thought, emotions, and actions as well as for keeping information readily accessible during the process of active learning. For example, researchers have found that elevations of brain chemicals such as noradrenaline, an important neurotransmitter, can impair functions that are controlled by the prefrontal region by altering the activity of neurons in that area of the brain. In a related fashion, humans experiencing chronic stress have been shown to perform poorly on tasks related to prefrontal cortex functioning (such as working memory or shifting attention) and their ability to control their emotions is typically impaired (Arnsten, 2009).
Implications for Policy and Practice
Many policy makers, educators, and even medical professionals are unaware of the potentially significant, long-term risks to children of exposure to fear-provoking circumstances—including family violence—and lack information about the prevalence of these situations in their communities. This can lead to widespread misconceptions of how children experience and respond to fear.
The scientific knowledge around fear and anxiety points to three important implications:
- Young children can perceive threat in their environment, but unlike adults, they do not have the cognitive or physical capacities to regulate their psychological response, reduce the threat, or remove themselves from the threatening situation. As a result, serious fear-triggering events such as family violence can have significant and long-lasting impacts on the developing child, beginning in infancy.
- Children do not naturally outgrow early learned fear responses over time. If young children are exposed to persistent fear and excessive threat during particularly sensitive periods in the developmental process, they may not develop healthy patterns of threat or stress regulation. When they occur, these disruptions do not naturally disappear.
- Simply removing a child from a dangerous environment will not by itself undo the serious consequences or reverse the negative impacts of early fear learning. Children who have been traumatized need to be in responsive and secure environments that restore their sense of safety, control, and predictability—and supportive interventions are needed to ensure the provision of these environments.
As a result, it is important for policies and programs to take into account children’s developmental needs, beginning in early infancy, particularly focusing more attention on preventing persistent fear and anxiety.
Children who live in violent homes or communities have been shown to have more behavior problems, greater evidence of PTSD, and increased physical symptoms such as headaches and stomach aches, as well as lower capacity for empathy and diminished self-esteem (Huth-Bocks et al., 2001). Programs focused on the reduction of domestic violence, substance abuse, neighborhood violence, and poverty are examples of the kinds of community-based services whose impacts could be enhanced by incorporating targeted interventions to explicitly address the emotional needs of young children living under these conditions. When delivered effectively, such interventions could have a multiplier effect into the next generation by reducing both the individual and the societal costs of the negative developmental effects of persistent fear, including mental health impairment, antisocial behavior, physical disease, and violent crime.
REFERENCES
Acierno, R., M. A. Hernandez, A. B. Amstadter, H. S. Resnick, K. Steve, W. Muzzy, and D. G. Kilpatrick. 2010. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The national elder mistreatment study. American Journal of Public Health 100(2):292-297.
Administration on Aging. 2011. Aging statistics. http://www.aoa.gov/aoaroot/aging_statistics/index.aspx (accessed July 1, 2011).
Arnsten, A. F. T. 2009. Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience 10(6):410-422.
Australian Institute of Criminology. 2003. Australian crime: Facts and figures. Canberra: The Australian Government.
Bandura, A. 1977. Social learning theory. Englewood Cliffs, NJ: Prentice Hall.
Bargh, J. A., and T. L. Chartrand. 1999. The unbearable automaticity of being. American Psychologist 54(7):462-479.
Beach, S. R., R. Schulz, N. G. Castle, and J. Rosen. 2010. Financial exploitation and psychological mistreatment among older adults: Differences between African Americans and non-African Americans in a population-based survey. Gerontologist 50(6): 744-757.
Berkowitz, L. 1993. Aggression: Its causes, consequences, and control. McGraw-Hill Series in Social Psychology. New York: McGraw-Hill.
Biddle, E., and D. Hartley. 2002. The cost of workplace homicides in the 1990-1997. In Injury prevention and control. U.S. Sixth world conference. Pp. 421-422.
Blenkner, M., M. Bloom, and M. Nielsen. 1971. Research and demonstration project of protective services. Social Casework 52(8):483-499.
Bookin, D., and R. E. Dunkle. 1985. Elder abuse—Issues for the practitioner. Social Casework-Journal of Contemporary Social Work 66(1):3-12.
Brand, S., and R. Price. 2000. The economic and social costs of crime, Home Office Research Study 217. London: Home Office.
Breckman, R. S., and R. D. Adelman 1988. Strategies for helping victims of elder mistreatment. Sage Human Services Guides. Newbury Park, CA: Sage Publications.
Brinks, V., E. R. de Kloet, and M. S. Oitzl. 2008. Strain specific fear behaviour and glucocorticoid response to aversive events: Modelling PTSD in mice. Progress in Brain Research 167:257-261.
Bronfenbrenner, U. 1979. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press.
Burston, G. R. 1975. Granny-battering. British Medical Journal 3(5983):592.
Buvinic, M., and A. R. Morrison. 1999. Violence as an obstacle to development. IDB technical note 4. Washington, DC: Inter-American Development Bank (IDB).
Buvinic, M., A. R. Morrison, and M. Shifter. 1999. Violence in Latin America and the Caribbean: A framework for action. In Too close to home: Domestic violence in the Americas, edited by A. Morrison and B. Orlando. New York: Inter-American Development Bank. Pp. 3-34.
Cantor, M. H. 1991. Family and community—Changing roles in an aging society. Gerontologist 31(3):337-346.
Carew, M. B., and J. W. Rudy. 1991. Multiple functions of context during conditioning— A developmental analysis. Developmental Psychobiology 24(3):191-209.
CDC (Centers for Disease Control and Prevention). 2008. Adverse health conditions and health risk behaviors associated with intimate partner violence. Morbidity and Mortality Weekly Report 57(05):113-117.
CDC. 2009. Understanding child maltreatment. http://www.cdc.gov/violenceprevention/pdf/CM-FactSheet-a.pdf (accessed April 2011).
CDC. 2011. Data & statistics (wisqars): Cost of injury reports. http://wisqars.cdc.gov:8080/costT/ (accessed 2011).
Childs, H. W., B. Hayslip, L. M. Radika, and J. A. Reinberg. 2000. Young and middle-aged adults’ perceptions of elder abuse. Gerontologist 40(1):75-85.
Cialdini, R. B. 2001. Influence: Science and practice. 4th ed. Boston, MA: Allyn and Bacon.
Clancy, T. V., L. N. Misick, and D. Covington. 1994. The financial impact of intentional violence on community hospitals. Journal of Trauma-Injury Infection and Critical Care 37(5):704.
Cohen, M. A. 1988. Pain, suffering, and jury awards—A study of the cost of crime to victims. Law & Society Review 22(3):537-555.
Cohen, M. A. 1998. The monetary value of saving a high-risk youth. Journal of Quantitative Criminology 14(1):5-33.
Coker, A. L., C. E. Reeder, M. K. Fadden, and P. H. Smith. 2004. Physical partner violence and Medicaid utilization and expenditures. Public Health Reports 119(6):557-567.
Cook, P. J., B. A. Lawrence, J. Ludwig, and T. R. Miller. 1999. The medical costs of gunshot injuries in the United States. Journal of the American Medical Association 282(5):447-454.
Courtney, M. E. 1999. The economics. Child Abuse & Neglect 23(10):975-986.
Coyne, A. C., W. E. Reichman, and L. J. Berbig. 1993. The relationship between dementia and elder abuse. American Journal of Psychiatry 150(4):643-646.
Davis, M. 2006. Neural systems involved in fear and anxiety measured with fear-potentiated startle. American Psychologist 61(8):741-756.
Day, T. 1995. The health-related costs of violence against women in Canada: The tip of the iceberg. Centre for Research on Violence Against Women and Children Publication Series. London, Ont.: The University of Western Ontario.
de Kloet, E. R., H. Karst, and M. Joels. 2008. Corticosteroid hormones in the central stress response: Quick-and-slow. Frontiers in Neuroendocrinology 29(2):268-272.
Delgado, M. R., A. Olsson, and E. A. Phelps. 2006. Extending animal models of fear conditioning to humans. Biological Psychology 73(1):39-48.
Dodge, K. A. 1986. A social information-processing model of social competence in children. Minnesota Symposia on Child Psychology 18:77-125.
Dodge, K. A., J. M. Price, J. A. Bachorowski, and J. P. Newman. 1990. Hostile attributional biases in severely aggressive adolescents. Journal of Abnormal Psychology 99(4): 385-392.
Dollard, J., L. W. Doob, N. E. Miller, O. H. Mowrer, and R. R. Sears. 1939. Frustration and aggression. New Haven, CT: Yale University Press.
Dong, X. 2005. Medical implications of elder abuse and neglect. Clinics in Geriatric Medicine 21(2):293.
Dong, X. 2011. Prospective study of the elder self-neglect and emergency department use in a community population. Journal of the American Geriatrics Society 59:S190-S191.
Dong, X., and M. A. Simon. 2008. Is greater social support a protective factor against elder mistreatment? Gerontology 54(6):381-388.
Dong, X., and M. A. Simon. 2010. Gender variations in the levels of social support and risk of elder mistreatment in a Chinese community population. Journal of Applied Gerontology 29(6):720-739.
Dong, X., M. A. Simon, R. Odwazny, and M. Gorbien. 2008. Depression and elder abuse and neglect among a community-dwelling Chinese elderly population. Journal of Elder Abuse & Neglect 20(1):25-41.
Dong, X., T. Beck, and M. A. Simon. 2009a. Loneliness and mistreatment of older Chinese women: Does social support matter? Journal of Women & Aging 21(4):293-302.
Dong, X., M. Simon, C. M. de Leon, T. Fulmer, T. Beck, L. Hebert, C. Dyer, G. Paveza, and D. Evans. 2009b. Elder self-neglect and abuse and mortality risk in a community-dwelling population. Journal of the American Medical Association 302(5):517-526.
Dong, X., M. Simon, C. Mendes de Leon, T. Fulmer, T. Beck, L. Hebert, C. Dyer, G. Paveza, and D. Evans. 2009c. Elder self-neglect and abuse and mortality risk in a community-dwelling population. Journal of the American Medical Association 302(5): 517-526.
Dong, X., M. A. Simon, T. T. Beck, C. Farran, J. J. McCann, C. F. Mendes de Leon, E. Laumann, and D. A. Evans. 2010. Elder abuse and mortality: The role of psychological and social wellbeing. Gerontology.
Dong, X., E. S. Chang, E. Wong, B. Wong, and M. A. Simon. 2011a. How do U.S. Chinese older adults view elder mistreatment? Findings from a community-based participatory research study. Journal of Aging and Health 23(2):289-312.
Dong, X., M. A. Simon, T. Fulmer, C. F. M. de Leon, L. E. Hebert, T. Beck, P. A. Scherr, and D. A. Evans. 2011b. A prospective population-based study of differences in elder self-neglect and mortality between black and white older adults. Journals of Gerontology Series a-Biological Sciences and Medical Sciences 66(6):695-704.
Dong, X., E. S. Chang, E. Wong, B. Wong, and M. A. Simon. In press. Association of depressive symptomology and elder mistreatment in a U.S. Chinese population: Findings from a community-based participatory research study. Journal of Agression, Maltreatment, and Trauma.
Dyer, C. B., V. N. Pavlik, K. P. Murphy, and D. J. Hyman. 2000. The high prevalence of depression and dementia in elder abuse or neglect. Journal of the American Geriatrics Society 48(2):205-208.
El-Zanaty, F. H. 1996. Egypt demographic and health survey, 1995. Cairo, Egypt; National Population Council, Calverton, MD; Macro International.
Evasovich, M., R. Klein, F. Muakkassa, and R. Weekley. 1998. The economic effect of child abuse in the burn unit. International Journal of Burns 24(7):642-645.
Fanslow, J., C. Coggan, B. Miller, and R. Norton. 1997. The economic cost of homicide in New Zealand. Social Science & Medicine 45(7):973-977.
Farrington, D. P. 1997. The relationship between low resting heart rate and violence. In Bio-social bases of violence. Vol. 292, edited by A. Raine, P. Brennan, D. P. Farrington, and S. A. Mednick. New York: Plenum Press. Pp. 89-106.
Faulkner, L. R. 1982. Mandating the reporting of suspected cases of elder abuse—An inappropriate, ineffective and ageist response to the abuse of older adults. Family Law Quarterly 16(1):69-91.
Finkelhor, D., R. Ormrod, H. Turner, and S. L. Hamby. 2005. The victimization of children and youth: A comprehensive, national survey. Child Maltreatment 10(1):5-25.
Fisher, A., L. G. Chestnut, and D. M. Violette. 1989. The value of reducing risks of death: A note on new evidence. Journal of Policy Analysis and Management 8(1):88-100.
Forjuoh, S. N. 2000. Child maltreatment related injuries: Incidence, hospital charges, and correlates of hospitalization. Child Abuse & Neglect 24(8):1019-1025.
Fulmer, T., A. Firpo, L. Guadagno, T. M. Easter, F. Kahan, and B. Paris. 2003. Themes from a grounded theory analysis of elder neglect assessment by experts. Gerontologist 43(5):745-752.
GAO (Government Accountability Office). 2011. Elder justice: Stronger federal leadership could enhance national response to elder abuse. http://aging.senate.gov/events/hr230kb2.pdf (accessed July 1, 2011).
Gold, M. R., J. E. Siegel, L. B. Russell, and M. C. Weinstein. 1996. Cost-effectiveness in health and medicine. New York: Oxford.
Grillon, C. 2002. Startle reactivity and anxiety disorders: Aversive conditioning, context, and neurobiology. Biological Psychiatry 52(10):958-975.
Grillon, C., and C. A. Morgan. 1999. Fear-potentiated startle conditioning to explicit and contextual cues in Gulf War veterans with posttraumatic stress disorder. Journal of Abnormal Psychology 108(1):134-142.
Grillon, C., L. Dierker, and K. R. Merikangas. 1998. Fear-potentiated startle in adolescent offspring of parents with anxiety disorders. Biological Psychiatry 44(10):990-997.
Guerra, N. G., L. R. Huesmann, and A. Spindler. 2003. Community violence exposure, social cognition, and aggression among urban elementary school children. Child Development 74(5):1561-1576.
Gunderson, L. 1999. The financial costs of gun violence. Annals of Internal Medicine 131(6):483-484.
Hashemi, L., and B. S. Webster. 1998. Non-fatal workplace violence workers’ compensation claims (1993-1996). Journal of Occupational and Environmental Medicine 40(6):561-567.
Heise, L., M. Ellsberg, and M. Gottemoeller. 1999. Ending violence against women. Baltimore, MD: Johns Hopkins University School of Public Health, Center for Communications Programs.
HHS (U.S. Department of Health and Human Services). 2001. Prevention pays: The costs of not preventing child abuse and neglect. Fairfax, VA: Caliber Associates (no longer available).
Hoel, H., K. Sparks, and C. Cooper. 2001. The cost of violence/stress at work and the benefits of a violence/stress-free working environment. University of Manchester Institute of Science and Technology. Report commissionned by the International Labor Organization.
Homer, A. C., and C. Gilleard. 1990. Abuse of elderly people by their carers. British Medical Journal 301(6765):1359-1362.
Hornick, J., J. Paetsch, and L. Bertrand. 2002. A manual on conducting economic analysis of crime prevention programs. Ottawa, Canada: National Crime Prevention Centre.
Huesmann, L. R. 1988. An information-processing model for the development of aggression. Aggressive Behavior 14(1):13-24.
Huesmann, L. R. 1998. The role of social information processing and cognitive schemas in the acquisition and maintenance of habitual aggressive behavior. In Human aggression: Theories, research, and implications for social policy, edited by R. G. Geen and E. I. Donnerstein. New York: Academic Press. Pp. 73-109.
Huesmann, L., and N. Guerra. 1997. Children’s normative beliefs about aggression and aggressive behavior. Journal of Personality and Social Psychology 72(2):408-419.
Huth-Bocks, A. C., A. A. Levendosky, and M. A. Semel. 2001. The direct and indirect effects of domestic violence on young children’s intellectual functioning. Journal of Family Violence 16(3):269-290.
Irazuzta, J. E., J. E. McJunkin, K. Danadian, F. Arnold, and J. L. Zhang. 1997. Outcome and cost of child abuse. Child Abuse & Neglect 21(8):751-757.
Jones, J. S. 1994. Elder abuse and neglect—Responding to a national problem. Annals of Emergency Medicine 23(4):845-848.
Jones, J. S., C. Holstege, and H. Holstege. 1997. Elder abuse and neglect: Understanding the causes and potential risk factors. American Journal of Emergency Medicine 15(6):579-583.
Kim, J. H., and R. Richardson. 2008. The effect of temporary amygdala inactivation on extinction and reextinction of fear in the developing rat: Unlearning as a potential mechanism for extinction early in development. Journal of Neuroscience 28(6):1282-1290.
Kim, J. J., and M. S. Fanselow. 1992. Modality-specific retrograde-amnesia of fear. Science 256(5057):675-677.
Kleinschmidt, K. C. 1997. Elder abuse: A review. Annals of Emergency Medicine 30(4): 463-472.
Krug, E., L. Dahlberg, J. Mercy, A. Zwi, and R. Lozano. 2002. World report on violence and health. Geneva: World Health Organization.
Lachs, M. S., C. S. Williams, S. O’Brien, L. Hurst, A. Kossack, A. Siegal, and M. E. T inetti. 1997. ED use by older victims of family violence. Annals of Emergency Medicine 30(4): 448-454.
Lachs, M. S., C. S. Williams, S. O’Brien, K. A. Pillemer, and M. E. Charlson. 1998. The mortality of elder mistreatment. Journal of the American Medical Association 280(5):428-432.
Lachs, M. S., C. S. Williams, S. O’Brien, and K. A. Pillemer. 2002. Adult protective service use and nursing home placement. Gerontologist 42(6):734-739.
Lau, E., and J. Kosberg. 1979. Abuse of the elderly by informal care providers. Aging 299: 10-15.
Leadership Council of Aging Organizations. 2010. Letter to Chairman Harkin and ranking member Cochran-Chairman Obey and ranking member Tiahrt. http://www.nasuad.org/documentation/policy_priorities/signed_onto_letters/elderjusticeact.pdf (accessed 2010).
LeDoux, J. E. 2000. Emotion circuits in the brain. Annual Review of Neuroscience 23: 155-184.
LeDoux, J. E., and E. A. Phelps. 2008. Handbook of emotions. 3rd ed, edited by M. Lewis, J. M. Haviland-Jones, and L. F. Barrett: New York: Guilford Press. Pp. 159-179.
Lewis, M., and L. Michalson. 1983. Children’s emotions and moods: Developmental theory and measurement. New York: Plenum Press.
Libby, A. M., M. R. Sills, M. K. Thurston, and H. D. Orton. 2003. Costs of childhood physical abuse: Comparing inflicted and unintentional traumatic brain injuries. Pediatrics 112(1):58-65.
Longres, J. F. 1994. Self-neglect and social-control—A modest test of an issue. Journal of Gerontological Social Work 22(3-4):3-20.
Ludwig, J., and P. J. Cook. 2000. Homicide and suicide rates associated with implementation of the Brady handgun violence prevention act. Journal of the American Medical Association 284(5):585-591.
Mansingh, A., and P. Ramphal. 1993. The nature of interpersonal violence in Jamaica and its strain on the national-health system. West Indian Medical Journal 42(2):53-56.
Max, W., and D. P. Rice. 1993. Shooting in the dark—Estimating the cost of firearm injuries. Health Affairs 12(4):171-185.
McCall, B. P., and I. B. Horwitz. 2004. Workplace violence in Oregon: An analysis using workers’ compensation claims from 1990-1997. Journal of Occupational and Environmental Medicine 46(4):357-366.
McEwen, B. S. 2007. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews 87(3):873-904.
McGaugh, J. L., L. Cahill, and B. Roozendaal. 1996. Involvement of the amygdala in memory storage: Interaction with other brain systems. Proceedings of the National Academy of Sciences USA 93(24):13508-13514.
McIntosh, J. L., and R. W. Hubbard. 1988. Indirect self-destructive behavior among the elderly—A review with case examples. Journal of Gerontological Social Work 13(1-2): 37-48.
Mendonca, R. N., J. Alves, and J. Cabral Filho. 2002. Hospital costs due to violence against children and adolescents in Pernambuco State, Brazil, during 1999. Cad Saude Publica.
Miller, T. R. 1989. Narrowing the plausible range around the value of life. Washington, DC: The Urban Institute.
Miller, T. R., and M. A. Cohen. 1997. Costs of gunshot and cut/stab wounds in the United States, with some Canadian comparisons. Accident Analysis and Prevention 29(3):329-341.
Miller, T. R., M. A. Cohen, and S. B. Rossman. 1993. Victim costs of violent crime and resulting injuries. Health Affairs 12(4):186-197.
Miller, T. R., M. A. Cohen, and B. Wiersema. 1996. Victim costs and consequences: A new look. National Institute of Justice Research Report, U.S. Department of Justice, Office of Justice Programs.
Miller, T. R., D. A. Fisher, and M. A. Cohen. 2001. Costs of juvenile violence: Policy implications. Pediatrics 107(1):art. no.-e3.
Mock, C., S. Pilcher, and R. Maier. 1994. Comparison of the costs of acute treatment for gunshot and stab wounds—Further evidence of the need for firearms control. Journal of Trauma-Injury Infection and Critical Care 36(4):516-522.
Moon, A., and O. Williams. 1993. Perceptions of elder abuse and help-seeking patterns among African-American, caucasian American, and Korean-American elderly women. Gerontologist 33(3):386-395.
Morrison, A., and M. Orlando. 1999. Social and economic costs of domestic violence: Chile and Nicaragua. In Too close to home: Domestic violence in the Americas, edited by A. Morrison and M. Biehl. New York: Inter-American Development Bank.
Mouton, C. P., and D. V. Espino. 1999. Health screening in older women. American Family Physician 59(7):1835-1842.
Mouton, C. P., R. J. Rodabough, S. L. D. Rovi, J. L. Hunt, M. A. Talamantes, R. G. Brzyski, and S. K. Burge. 2004. Prevalence and 3-year incidence of abuse among postmenopausal women. American Journal of Public Health 94(4):605-612.
Nahmiash, D. 2002. Powerlessness and abuse and neglect of older adults. Journal of Elder Abuse & Neglect 14(1):21-47.
National Crime Prevention Council. 1999. Saving money while stopping crime: A handy reference for prevention advocates. Topics in Crime Prevention. Washington, DC.
National Scientific Council on the Developing Child. 2005. Excessive stress disrupts the architecture of the developing brain: Working paper no. 3. http://developingchild.harvard.edu/index.php/resources/reports_and_working_papers/working_papers/wp3/ (accessed April 2011).
Nelson, C. A., and M. DeHaan. 1996. Neural correlates of infants’ visual responsiveness to facial expressions of emotion. Developmental Psychobiology 29(7):577-595.
Nemeroff, C. B. 2004. Neurobiological consequences of childhood trauma. Journal of Clinical Psychiatry 65(1):18-28.
Neville, P., A. Boyle, and S. Baillon. 1999. A descriptive survey of acute bed usage for dementia care in old age psychiatry. International Journal of Geriatric Psychiatry 14(5):348-354.
New, M., and L. Berliner. 2000. Mental health service utilization by victims of crime. Journal of Traumatic Stress 13(4):693-707.
NRC (National Research Council). 2003. Elder mistreatment: Abuse, neglect, and exploitation in an aging America. Panel to Review Risk and Prevalence of Elder Abuse and Neglect. Edited by R. J. Bonnie and R. B. Wallace. Washington, DC: The National Academies Press.
Payne, J. E., T. V. Berne, R. L. Kaufman, and R. Dubrowskij. 1993. Outcome of treatment of 686 gunshot wounds of the trunk at Los-Angeles-County-USC-Medical-Center— Implications for the community. Journal of Trauma-Injury Infection and Critical Care 34(2):276-281.
Peden, M., and J. Van der Spuy. 1998. The cost of treating firearm victims. Trauma Review 6:4-5.
Phelps, E. A., and J. E. LeDoux. 2005. Contributions of the amygdala to emotion processing: From animal models to human behavior. Neuron 48(2):175-187.
Phelps, E. A., M. R. Delgado, K. I. Nearing, and J. E. LeDoux. 2004. Extinction learning in humans: Role of the amygdala and vmPFC. Neuron 43(6):897-905.
Phillips, R. 1998. The economic cost of homicide to a South African city. University of Cape Town Graduate School of Business, Cape Town.
Pine, D. S. 1999. Pathophysiology of childhood anxiety disorders. Biological Psychiatry 46(11):1555-1566.
Plotnick, R. D., and L. Deppman. 1999. Using benefit-cost analysis to assess child abuse prevention and intervention programs. Child Welfare 78(3):381-407.
Podnieks, E. 1992. National survey on abuse of the elderly in Canada. Journal of Elder Abuse & Neglect 4:5-58.
Pollak, S. D. 2008. Mechanisms linking early experience and the emergence of emotions: Illustrations from the study of maltreated children. Current Directions in Psychological Science 17(6):370-375.
Pollak, S. D., and D. J. Kistler. 2002. Early experience is associated with the development of categorical representations for facial expressions of emotion. Proceedings of the National Academy of Sciences USA 99(13):9072-9076.
Pollak, S. D., D. Cicchetti, K. Hornung, and A. Reed. 2000. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology 36(5):679-688.
Quirk, G. J., R. Garcia, and F. Gonzalez-Lima. 2006. Prefrontal mechanisms in extinction of conditioned fear. Biological Psychiatry 60(4):337-343.
Reeb-Sutherland, B. C., S. M. Helfinstein, K. A. Degnan, K. Perez-Edgar, H. A. Henderson, S. Lissek, A. Chronis-Tuscano, C. Grillon, D. S. Pine, and N. A. Fox. 2009. Startle response in behaviorally inhibited adolescents with a lifetime occurrence of anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry 48(6):610-617.
Roozendaal, B., B. S. McEwen, and S. Chattarji. 2009. Stress, memory and the amygdala. Nature Reviews Neuroscience 10(6):423-433.
Rovi, S., P. H. Chen, and M. S. Johnson. 2004. The economic burden of hospitalizations associated with child abuse and neglect. American Journal of Public Health 94(4):586-590.
Sameroff, A. 2010. A unified theory of development: A dialectic integration of nature and nurture. Child Development 81(1):6-22.
Sanchez, M. M., C. O. Ladd, and P. M. Plotsky. 2001. Early adverse experience as a developmental risk factor for later psychopathology: Evidence from rodent and primate models. Development and Psychopathology 13(3):419-449.
Seligman, M. E. P. 1975. Helplessness: On depression, development, and death. San Francisco, CA: W.H. Freeman.
Shields, L. B. E., D. M. Hunsaker, and J. C. Hunsaker. 2004. Abuse and neglect: A ten-year review of mortality and morbidity in our elders in a large metropolitan area. Journal of Forensic Sciences 49(1):122-127.
Shonkoff, J. P., W. T. Boyce, and B. S. McEwen. 2009. Neuroscience, molecular biology, and the childhood roots of health disparities. Journal of the American Medical Association 301(21):2252-2259.
Snively, S. 1994. The New Zealand economic cost of family violence. Wellington, New Zealand: Family Violence Unit, Department of Social Welfare.
Song, D. H., G. P. Naude, D. A. Gilmore, and F. Bongard. 1996. Gang warfare: The medical repercussions. Journal of Trauma-Injury Infection and Critical Care 40(5):810-815.
Stanko, E. A., C. Hale, and H. Lucraft. 1998. Counting the costs: Estimating the impact of domestic violence in the London borough of Hackney. Crime Concern, funded by Hackney Safer Cities and the Children’s Society with the co-operation of the London Borough of Hackney.
Steinmetz, S. K. 1990. Elder abuse by adult offspring: The relationship of actual vs. perceived dependency. Journal of Health and Human Resources Administration 12(4):434-463.
Sullivan, R. M., M. Landers, B. Yeaman, and D. A. Wilson. 2000. Neurophysiology—Good memories of bad events in infancy. Nature 407(6800):38-39.
Summers, C. L., and E. M. Molyneux. 1992. Suspected child-abuse—Cost in medical time and finance. Archives of Disease in Childhood 67(7):905-910.
Sumner, B. B., E. R. Mintz, and P. L. Brown. 1987. Injuries caused by personal violence. Injury-International Journal of the Care of the Injured 18(4):258-260.
Teaster, P., T. Dugar, M. Moendiondo, E. Abner, K. Cecil, and J. Otto. 2004. The 2004 survey of adult protective services: Abuse of adults 60 years of age and older. www.elderabusecenter.org/pdf/research/apsreport030703.pdf (accessed April 4, 2007).
Tellez, M. G., R. C. Mackersie, D. Morabito, C. Shagoury, and C. Heye. 1995. Risks, costs, and the expected complication of re-injury. American Journal of Surgery 170(6):660-664.
Tjaden, P., and N. Thoennes. 2000. Full report of the prevalence, incidence, and consequences of violence against women: Findings from the National Violence Against Women Survey. Washington, DC: National Institute of Justice, Office of Justice Programs.
U.S. Department of Justice, Bureau of Justice Statistics. 1994. The costs of crime to victims: Crime data brief.
Vassar, M. J., and K. W. Kizer. 1996. Hospitalizations for firearm-related injuries—A population-based study of 9562 patients. Journal of the American Medical Association 275(22):1734-1739.
Walker, J. R. 1997. Estimates of the costs of crime in Australia 1996. Trends & Issues in Crime and Criminal Justice, No. 72. Canberra, Australian Capital Territory: Australian Institute of Criminology.
WHO (World Health Organization). 2002. World report on violence and health. Geneva, Switzerland.
Wismer Fries, A. B., T. E. Ziegler, J. R. Kurian, S. Jacoris, and S. D. Pollak. 2005. Early experience in humans is associated with changes in neuropeptides critical for regulating social behavior. Proceedings of the National Academy of Sciences USA 102(47): 17237-17240.
Wisner, C. L., T. P. Gilmer, L. E. Saltzman, and T. M. Zink. 1999. Intimate partner violence against women—Do victims cost health plans more? Journal of Family Practice 48(6):439-443.
World Bank. 2004. World development report: Making services work for poor people. Washington, DC: The World Bank.
Yang, Y. L., P. K. Chao, L. S. Ro, Y. Y. P. Wo, and K. T. Lu. 2007. Glutamate NMDA receptors within the amygdala participate in the modulatory effect of glucocorticoids on extinction of conditioned fear in rats. Neuropsychopharmacology 32(5):1042-1051.
Yodanis, C. L., A. Godenzi, and E. A. Stanko. 2000. The benefits of studying costs: A review and agenda for studies on the eonomic costs of violence against women. Policy Studies 21(3):263-276.



















































