Debate over America’s place at the top of economic superpowers aside, it is clear that it is not a superpower in health. In fact, this Institute of Medicine (IOM) Committee on Public Health Strategies to Improve Health asserts that merely reaching the average of comparable high-income countries in health status would require considerable national effort.
Despite spending far more on medical care than any other nation, and despite having seen a century of unparalleled improvement in population health and longevity, the United States is now falling behind many of its global counterparts and competitors in such health outcomes as overall life expectancy and the incidence of preventable diseases and injuries. A fundamental but often overlooked driver of the imbalance between spending and outcomes is the nation’s inadequate investment in strategies that promote health and prevent disease and injury population-wide. Strategies that are often summarized by the set of Essential Public Health Services1 include monitoring and reporting on community health status; investigating and controlling disease outbreaks; educating the public about health risks and prevention strategies; implementing community-wide health improvement initiatives (including the social and physical environment); developing and enforcing laws and regulations to protect health; and assuring the safety and quality of water, food, air, and other resources necessary for health. All of these services require coordinated action at the local, state, and national
______________
1The committee’s previous two reports (IOM, 2011a,b) listed the 10 Essential Public Health Services, a list that serves as a cornerstone to descriptions of the work of public health departments and their community partners.
levels, and public health departments have essential roles in informing and mobilizing public- and private-sector efforts.
The U.S. public health infrastructure—the constellation that includes federal, state, and local public health agencies, laboratories, and information technology and surveillance networks—is fragmented and lacks the resources necessary to carry out its roles effectively and ensure a basic level of health protection for all Americans. Historically, public health responsibilities emerged as primarily locally- and state-based, with the federal government intervening in the course of some epidemics. At the federal level, the Department of Health and Human Services (HHS) came together in piecemeal fashion in the 20th century, as discussed in more detail in the 2003 IOM report on the future of the public’s health. Today, this highly complex infrastructure is supported by diminishing resources, and that poses grave threats to and the loss of important opportunities for the nation’s health. Over 52,200 combined state and local public health jobs have been lost since 2008 (17 percent of the state and territorial public health workforce and 22 percent of the local public health workforce [ASTHO, 2012]).
The underinvestment in public health has ramifications for the nation’s overall health status, for its financially-strained health care delivery system, and, the committee argues, for its economic vitality and global competitiveness. Although 2012 is a challenging time in national and world economic history, the nation’s portfolio of investments in health must be reconsidered and rebalanced to lead the way toward an invigorated “health system,” economy, and society. In referring to the nation’s health system,2 the committee means not only the component that delivers medical care, but the intersectoral system that was first introduced in the 2003 report The Future of the Public’s Health in the 21st Century (IOM, 2003) and that comprises the governmental public health agencies and various partners, including communities, the health care delivery system, employers and businesses, the mass media, and the education sector.
At a time when expenditures on medical care are limiting its ability to make crucial investments in other arenas that are critical for the quality of life and economic health of Americans, the committee believes that a strong governmental public health infrastructure can mobilize strategies that reduce the occurrence of disease and injury, offset the need for ever-
______________
2In its report on measurement, the system was redefined by the committee as simply “the health system” because “the modifiers public and population are poorly understood by most people other than public health professionals and may have made it easier to misinterpret or overlook the collective influence and responsibility that all sectors have for creating and sustaining the conditions necessary for health. In describing and using the term the health system, the committee [sought] to reinstate the proper and evidence-based understanding of health as not merely the result of medical or clinical care but the result of the sum of what we do as a society to create the conditions in which people can be healthy (IOM, 1988)” (IOM, 2011b).
more costly medical interventions, and foster the productivity and wellbeing of the nation. Fulfilling that promise requires strategic expenditures to ensure capable and well-equipped public health agencies in all regions and greater attention to health promotion and disease prevention in all sectors of American society.
In previous two reports the committee summarized salient evidence on the social determinants of health (IOM, 2011a,b). There is substantial support for the links between health outcomes and factors related to where people live, learn, work, and play. However, there are gaps in the evidence on population-based interventions, that is, on what strategies are most effective in addressing the factors that contribute to poor health outcomes. The gaps in evidence are in large measure due to failures to invest in building the knowledge base on population health, including not only research on population-based interventions but on public health infrastructure, financing and functioning. Research and experience have demonstrated the effectiveness of some approaches, but the knowledge has not been operationalized for reasons that include lack of funding, insufficient political will, and the requirement to change societal norms. In this report, the committee offers a vision for a revitalized governmental public health enterprise, and discusses the financial resources that are needed to ensure an effective public health infrastructure in all communities.
The committee was given the following charge:
Develop recommendations for funding state and local public health systems that support the needs of the public after health care reform. Recommendations should be evidence based and implementable. In developing their recommendations the committee will:
• Review current funding structures for public health
• Assess opportunities for use of funds to improve health outcomes
• Review the impact of fluctuations in funding for public health
• Assess innovative policies and mechanisms for funding public health services and community-based interventions and suggest possible options for sustainable funding
The committee’s starting challenge was to explain the boundaries of governmental public health in its study. The committee began with the recognition, described in the committee’s previous report on law, that public health has historically identified health problems, their causes, and potential solutions without necessarily bearing or assuming the responsibility for addressing them. In many cases, other government agencies came to be
charged with responsibilities over aspects of sanitation, safe water, safe food, and housing, among others (IOM, 2011a, p. 21). Moreover, other areas of government action and societal investment such as education, housing, transportation, and urban planning, are also determinants of health whose links to population health have been documented in existing research. For the purposes of the present study, the committee acknowledged the breadth of influences on health and the wide range of societal actors engaged in acting on the health of the population—public health writ large—but it did not attempt to review the myriad public- and private-sector funding streams involved. For reasons first of committee composition and expertise, and second of data and time limitations, the committee provides little discussion on private-sector funding for population health, or societal investments in areas beyond health that may have ramifications for national health status. In the report, the term “public health” is used to denote the governmental public health enterprise. At times, however, the report refers to the broader understanding of public health as the multitude of strategies and actors that contribute to improving population health, and that is explained in the text.
The report is comprised of four chapters. After the introduction, the second chapter is devoted to examining how governmental public health activity (in state and local public health departments) is funded and the requirements placed on public health spending. The third chapter discusses the administrative changes needed to support the uniform collection and reporting of public health financial information (revenues and expenditures), and the research needed to inform the most efficient and effective use of public health funding. The fourth and final chapter describes contemporary public health funding, provides some estimates of need, and discusses options for generating revenues to ensure stable, sustainable, and adequate funding for public health defined in this context somewhat narrowly to encompass only the state and local public health departments.
The health of a nation’s population is determined by the conditions that it creates for living, the equity in opportunity that it affords, and the access to and quality of its medical care delivery system.3 Health in the United States advanced during the last century, adding approximately 30 years to life expectancy between 1900 and 1999 (CDC, 1999b). More
______________
3The United States entered the 21st century with glaring inadequacies in health and health care delivery system experiences for vulnerable subsets of the U.S. population due in large measure to socioeconomic and attendant environmental risks, as well as to inadequate access to care and variations in clinical practice (Braveman et al., 2011a; de la Plata et al., 2007; Haider et al., 2008; Lucas et al., 2006; Shafi et al., 2007).
than two-thirds of that increase was related to public health strategies that resulted in improvements in conditions for living such as nutrition, water and workplace safety, and prevention and control of communicable diseases with immunizations, antibiotics, and outbreak control (Bunker et al., 1994; CDC, 1999b). Despite its unrivaled wealth, the United States nonetheless ended the century lagging behind many developed countries in health status as reflected in indicators of mortality, morbidity, and loss of potential productivity. Table 1-1 shows U.S. rankings on life expectancy, infant mortality, and maternal mortality according to three different sources: the Organisation for Economic Co-operation and Development (OECD),4 which has 34 member countries, including “many of the world’s most advanced countries but also emerging countries like Mexico, Chile and Turkey” (OECD, 2012); the United Nations (UN), which provides data on up to 196 countries;5 and the Central Intelligence Agency (CIA), which provides data on 221 countries (CIA, 2011).
Medical Costs
Non-communicable, preventable chronic conditions are consuming increasing and extraordinary amounts of national spending on health, accounting for more than 75 percent of the $2.6 trillion spent each year on medical care (KFF, 2012). In 2007 and 2008, 23 percent of U.S. adults reported having one chronic medical condition, and an additional 31 percent reported having two or more (KFF, 2012; Soni, 2011). Chronic medical conditions associated with modifiable risk factors (smoking, nutrition, weight, and physical activity) represented 6 of the 10 costliest medical conditions6 in the United States with a combined medical care expenditure of $338 billion in 2008 (Soni, 2011). Those same six largely preventable conditions accounted for 29 percent of the total increase in U.S. medical care spending during the 1987-2000 period (Thorpe et al., 2004b, 2010).
The indirect costs associated with preventable chronic diseases—costs related to diminished labor supply and worker productivity and the resulting fiscal drag on the nation’s economic output—have been estimated at over $1 trillion a year (DeVol and Bedroussian, 2007). The nation’s poor health status and the expense of its medical care delivery system place an enormous burden on the still-weak U.S. economy, the deficit-burdened federal
______________
4The OECD mission is “to promote policies that will improve the economic and social well-being of people around the world” (OECD, 2012).
5The UN data from World Population Prospects, The 2008 Revision includes data for 196 countries (“[o]nly countries or areas with 100,000 persons or more in 2009”), although its multi-year data and estimates (2005-2010) includes only 146 countries (UN, 2009).
6The 10 are heart disease, cancer, mental disorders, trauma-related disorders, osteoarthritis, asthma, hypertension, diabetes, back problems, and hyperlipidemia (Soni, 2011).
TABLE 1-1 U.S. Health Rankings
| Source | U.S. Ranking (U.S./Total) | ||
| Life Expectancy | Infant Mortality | Maternal Mortality | |
| UN | 28/146 | 32/146 | n/a |
| (2005-2010 data) | (2005-2010 data) | ||
| OECD | 26/34 | 31/34 | 25/34 |
| (2007 data) | (2007 data) | (2007 data) | |
| CIA | 50/221 | 174/222 | 121/172 |
| (2011 estimated data; in 2010 data, U.S. ranked 49th) | (2011 estimated data) | (2011 estimated data) | |
NOTE: n/a = not available.
SOURCES: CIA, 2011; NRC, 2011; OECD, 2011; United Nations, 2009.
budget, and the financial security of many individual households. National health expenditures in 2010 reached $2.57 trillion, 17.3 percent of gross domestic product (GDP). Spending is projected to increase to $4.48 trillion, 19.3 percent of GDP, by 2019 (Truffer et al., 2010). Most of that increase will be due to federal spending on major medical care programs—including Medicare, Medicaid, the Children’s Health Insurance Program, and subsidies for eligible individuals who are expected to gain health insurance coverage under the federal Affordable Care Act (ACA).
The last decade’s growth in health care cost has dramatically affected household budgets, consuming nearly all the gains in income that were realized by the average U.S. family in the decade. Increased insurance premiums, out-of-pocket costs, and taxes devoted to health care consumed all but $95 of the increase in average monthly income from 1999 to 2009 (Auerbach and Kellermann, 2011). Family premiums for a typical insurance plan are estimated to rise 94 percent from 2008 to 2020, from $12,298 to $23,842 (Schoen et al., 2009). During the 10-year period 2009-2019, individual out-of-pocket expenses are expected to increase by 64 percent (from $284 billion to $466 billion), an average annual increase of 6.3 percent, which is more than twice the rate of increase in 2009 (CMS, 2010).
The financial impact of increasing health care costs is seen in bankruptcy trends and other signs of household financial insecurity. In two separate surveys, Himmelstein et al. (2009) reported that the rate of medical bankruptcies increased 50 percent from 2001 to 2007. The “medical debtors” were largely insured (75 percent), well-educated, and owners of homes, and made up 62 percent of the national random sample of 2,314 bankruptcies (Himmelstein et al., 2009). The impact of high medical care costs was reported in the 2011 Employee Benefits Research Institute’s consumer health confidence survey of adult Americans which found decreased
savings for retirement (29 percent of respondents); decreased non-retirement savings (56 percent); increased credit card use (19 percent); delay in going to the doctor (44 percent); and skipping of medication doses or not filling prescriptions altogether (26 percent) (Fronstin, 2011).
The high cost associated with the poor health of Americans poses global competitive disadvantages for the nation in employer and national costs. Current OECD data show that per capita U.S. health expenditures are more than two times the OECD average ($7,960 vs. $3,223 in 2009), and 2-3 times greater than those of such rapidly advancing economies as Czech Republic, Korea, Poland, and Turkey (OECD, 2010b). Obesity alone accounts for up to 20 percent of the rise in medical care spending over the past decade, and obese adults present medical care costs 37 percent greater than those of their normal-weight counterparts because of their risks of diabetes, high blood pressure, and related chronic conditions (Thorpe et al., 2004a). Preventable diseases and injuries are important components of the labor costs that saddle U.S. employers. It has been estimated that the cost of treating obese adults was about $147 billion in 2008, that the annual excess health care cost to private payers per obese adult was $1,140 in 2006 (Finkelstein et al., 2009), and that obese working-age adults (18-65 years) incurred 37 percent higher annual health care costs than their normal-weight counterparts (Sturm, 2002). Health risk factors that are highly amenable to population-based preventive strategies (i.e., smoking, cholesterol, physical inactivity, and obesity) have strong influences on annual health care costs. Workers who had medium risk (three or four risk factors) were shown to incur $1,261 more in annual health care costs than workers who had low health risk (two or fewer risk factors), and those who had high risk (five or more risk factors) $3,321 more (Edington, 2001). The economic burden of excess chronic disease morbidity on employers also includes substantial adverse effects on productivity due to lost work time (“absenteeism”) and diminished performance at work because of illness (“presenteeism”) (Collins et al., 2005; Kessler et al., 2001; Wang et al., 2003). The medical care delivery system is expensive today; if it stays on its current course, it will be unsustainable in the future (CBO, 2011).
Putting Prevention at the Center of National Strategies
An estimated 80 percent of cases of heart disease and of type 2 diabetes and 40 percent of cases of cancer could be prevented by exercising more (which might be made possible by, for example, improving green spaces and increasing neighborhood safety), eating better (made possible by, for example, increasing affordability and availability of fresh foods), and avoiding tobacco (made possible by, for example, sponsoring programs for smoking prevention and cessation) (see Brownson et al., 2006; CDC, 2011d; Ewing,
2005; Mokdad et al., 2004; Ver Ploeg et al., 2009; WHO, 2012a; WHO Commission on Social Determinants of Health, 2008). But the United States is not making substantial progress in advancing the prevention strategies needed to support these changes. One-fifth of adults still smoke and half of adults—and nearly 20 percent of children—are overweight or obese (Cory et al., 2010). Without system-wide changes, one-third of American adults will develop diabetes by 2050 (up from one-tenth today) (Boyle et al., 2010). The current generation of children and young adults in the United States could become the first generation to experience shorter life spans and fewer healthy years of life than those of their parents (Olshansky et al., 2005).
Despite the knowledge that most cases of those costly chronic conditions are preventable, the national strategy to address the health crisis is directed predominantly downstream at the medical care delivery system. Strategic interventions are aimed at improving coordination of transitions of care (acute hospitals and step down institutions or home care), strengthening primary care, reforming payments and financial incentives, modernizing the information system infrastructure, and improving management of persons with chronic conditions. The Affordable Care Act includes several provisions that aim to advance population health, and is a legislative precedent worth building on. However, upstream causes (such as low educational attainment) of health problems continue to generate large volumes of new cases that require additional attention and adequate resources. Success in improving population health and reducing the volume of cases of non-communicable disease entering the medical delivery system will require a major strategic focus and aggressive action on root causes. Homer and Hirsch (2006), among others, have illustrated the system dynamics (beginning with social and behavioral risks) that ultimately lead to increased demand for medical care.7
The committee finds that poor U.S. health status and costly medical care consumption reflect a failure of the nation’s health system as a whole—medical care, governmental public health, and other actors—to support strategies that advance population health. Solutions will require more than reforms of the delivery and payment systems for medical care. They will also require greater health system efficiency and more balanced investment in health, especially in the use of population-level interventions. Better public health efforts can reduce the rising prevalence of chronic diseases and influence other high-priority outcomes, such as injuries, mental illness, and substance abuse—and simultaneously attenuate the downstream medical care costs associated with them. Improving the effectiveness of the nation’s governmental public health infrastructure can contribute to offsetting medical costs in three ways:
______________
7See Figure 4 in Homer and Hirsch (2006, p. 457).
1. Population-based public health strategies (such as policies to control tobacco, reduce motor vehicle injuries, require immunization, and reshape the social determinants of health) mobilized by this infrastructure can decrease numbers of cases of disease and injury (Halpin et al., 2010; see Box 1-1).
2. Public health agencies can use their data surveillance, analysis, and reporting capabilities to assist the medical care delivery system in identifying ineffective or inappropriate clinical care and in creating opportunities to advance population health in the clinical setting.
3. Public health agencies can convene or join partnerships aimed at creating environments in which people can be healthy.
A growing body of evidence indicates that effective prevention strategies can substantially improve health with little or no additional lifetime medical spending (i.e., from more potential years of medical care use). A recent study modeled various scenarios to estimate the potential benefits of effective interventions to reduce risk factors of adults in mid-life. It found that those exposed to successful clinical prevention interventions for obesity, hypertension, and diabetes experienced reduced lifetime medical spending and lived longer (Goldman et al., 2009). For example, as the population ages, diabetes prevalence is predicted to rise, peaking at about 34 percent at the age of 79 years. In the predicted scenarios where interventions had success rates of 10, 20, or 50 percent, the predicted diabetes prevalence was lowered to about 30, 25, and 16 percent, respectively (Goldman et al., 2009). Preventive efforts that decrease the prevalence of risk factors through non-clinical approaches can be expected to reduce costs further, because population-based strategies are typically less expensive than clinical ones. A recent American Heart Association literature review and policy statement, characterized primordial prevention as a key approach to obtaining value from decreasing the burden of cardiovascular disease (Weintraub et al., 2011). In terms of broader economic impact, one study estimates a net gain in economic growth of $1.2 trillion in real GDP over 20 years because of the effects of increases in chronic disease prevention efforts on labor productivity (DeVol and Bedroussian, 2007).
Collaboration Between Public Health and Clinical Care
As shown above, public health prevention strategies can help to contain medical care costs: they require relatively modest investments; they attack problems largely by addressing root causes of disease and injuries and thereby reduce the need for advanced, costly medical care; and they operate at the level of the population rather than through one-on-one clinical interventions. At a time when there is little agreement on the most appro-
BOX 1-1
Public Health Action and Tobacco Control
The history of tobacco control and smoking prevention illustrates how properly funded and researched public health prevention programs can address 21st century challenges population health. Tobacco has long been a public health scourge responsible for illness and death in both smokers and those around them, and tobacco control efforts have decreased rates of smoking-related disease and death (CDC, 2004, 2005, 2008; IOM, 2009). “Between 1965 and 2005, the percentage of adults who once smoked and who had quit more than doubled from 24.3 to 50.8 percent and the percentage of adults who have never smoked more than 100 lifetime cigarettes increased by approximately 23 percent from 1965 to 2005” (IOM, 2007). Those reductions are due largely to public health prevention efforts that began after the surgeon general’s report was published (IOM, 2007).
State and local smoking prevention programs were paid for through a combination of excise taxes on the sale of cigarettes, federal funds (for comprehensive prevention programs), and contributions by philanthropic organizations (IOM, 2007). In 1999, the Centers for Disease Control and Prevention (CDC) replaced two large programs with one program that provided funds to all 50 states and the District of Columbia. State programs contained various initiatives (such as public education, counter advertising, smoke-free workplaces, and increased taxes on cigarettes). The programs were based on evidence that showed that interventions focused on individual behavior were “not likely to result in large-scale declines in smoking prevalence.” Hence the new focus on altering social and environmental influences (IOM, 2007).
The level of state funding for tobacco control correlates with the success of smoking prevention programs (Farrelly et al., 2003). Tauras and colleagues (2005)
priate strategies for constraining the growth in medical cost—particularly strategies that raise concerns about limiting access to services or restraining innovation and discovery in medical science—cost-effective population-based approaches offer considerable appeal. That suggests that an essential component of health care cost control strategies is to attack the occurrence of disease and injury through population-based strategies, on which a solid knowledge base and successful track record are available, even as the search for medical care delivery reforms continues.
Other approaches to cost containment that use public health skills and competencies would rely on an improved governmental public health infrastructure to accelerate the movement toward more effective and more efficient strategies for medical care delivery. For example, some public health departments are uniquely positioned (although not many have the capacity) to assess the appropriateness and effectiveness of medical care services that
studied state expenditures on tobacco control and found evidence that tobacco control funding was inversely related to the percentage of young people who smoked and “the average number of cigarettes smoked by young smokers.” States with the most comprehensive (and thus resource-intensive) smoking prevention programs saw a greater decline in smoking rates than the national average (Tauras et al., 2005). Aggressive state campaigns aimed at adults in the late 1990s also contributed to a decrease in the prevalence of smoking by adults (IOM, 2007). The California Tobacco Control Program,a a program with stable funding, was associated with almost twice the reduction of smoking prevalence from 1989 and 1993 compared with the rest of the United States (Gilpin et al., 2001).
CDC has recommended minimum state spending levels needed for successful tobacco use prevention and cessation (CDC, 2004). However, most states do not meet that minimum and since 2002 states have needed to cut funding to their tobacco prevention programs (IOM, 2007). In 2008, Farrelly and colleagues looked at state tobacco use prevention funding levels from 1995 to 2003 and found that states that had larger declines in adult smoking spent more on those programs (they controlled for other factors such as increased tobacco prices) (Farrelly et al., 2008). Overall, research shows that implementation of comprehensive state tobacco prevention and cessation programs that are also adequately funded has a substantial effect on tobacco use in a state (Campaign for Tobacco-Free Kids, 2011; CDC, 1996; Dilley et al., 2011; Farrelly et al., 2003, 2008; Pierce et al., 2011, also see California Department of Public Health Tobacco Control Program, 2009, 2011; Oregon Health Authority, 2011).
aThe Tobacco Tax and Health Protection Act (Proposition 99) started a 25-cent tax on each package of cigarettes sold in California and led to the creation of the California Tobacco Control Program which allowed California to be the first state to fund a comprehensive tobacco control program (California Department of Public Health, 2009).
can have considerable effects on population health (see example in Box 1-2). By coupling analytic capabilities with an expanded information system, public health departments can provide leadership in measuring, monitoring, and reporting the performance of medical care delivery systems, and enhancing the transparency of their costs, quality, and outcomes. Similarly, public health can play an important role in advancing health literacy, consumer knowledge, and protections and in furthering standard and rigorous processes for generating the best community and preventive service recommendations throughout the various agencies of federal and state governments.
The committee’s report on measurement (IOM, 2011b) recommended collaboration between the public health and clinical care worlds to draw on the expertise of public health to improve aspects of clinical care both to advance the health of populations, and to familiarize Americans with the meaning of high-value (evidence-based, efficient, and appropriate) care,
BOX 1-2
Improving Quality and Offsetting Medical Care Costs:
A Pilot Project for the New York State Department of Health
Percutaneous coronary intervention (PCI) is effective in evolving heart attacks, but its value compared with that of medical management has not been demonstrated in patients who have no history of recent heart attack or unstable angina. In addition, PCI carries a greater risk of procedure-related heart attacks than does medical management. A 2010 New York State Department of Health (NYSDOH) review of the care of people who underwent PCI revealed that a substantial number of procedures performed in New York hospitals did not meet the American College of Cardiology and American Heart Association 2009 criteria for appropriateness. Initially, the department will alert the medical care delivery system when there has been a departure from the criteria. The Basic Benefits Review Work Group of the NYSDOH has recommended that Medicaid coverage of PCI be eliminated when criteria for PCI have not been met. The department anticipates that savings associated with avoidance of unnecessary procedures will directly support a cardiac services registry to continue evaluations of appropriateness and quality of care and that additional savings will accrue directly to the Medicaid program.
SOURCE: Medicaid Redesign Team, 2011.
in the form of local aggregated performance reports on the appropriateness, quality, safety, and efficiency of clinical care services delivered in the community. Because data analysis and surveillance are fundamental tasks of public health, public health agencies in collaboration with medical care delivery systems are well positioned to develop mechanisms for tracking and analyzing inputs into and outputs of the medical care delivery system that allow the identification and early resolution of system problems. Some jurisdictions that serve smaller populations may never achieve local capacity of this kind—in some states or territories, it may require a more centralized function—but governmental public health should be able to provide information to the medical care delivery system, and to the public it serves, on the effectiveness and efficiency of the latter’s operation. In addition to interaction or integration between the public health and clinical care systems described above, some current examples are: reports of outlier rates of hospitalization for selected diseases and of the degree of consistency between procedure use per population consistent with predicted prevalence of need in a population. New York State provides a useful example of the role that a state public health agency could play in improving aspects of clinical care delivery while lowering cost (see Box 1-2).
Environments in Which People Can Be Healthy
Public health has special skills and a knowledge base to help society to understand the factors that are contributing most to poor population health outcomes, and how to alter them. This includes a wide array of potential activities that may or may not reside within governmental public health’s immediate sphere of influence. For example, some of the underlying determinants of disease and death such as educational attainment, early childhood development, and aspects of the built environment (Wilkinson and Marmot, 2003). Others are risk factors more proximate to the outcomes, such as behaviors including poor eating habits and inactivity, and yet others pertain to the availability, quality, and appropriateness of clinical care services. Public health has contributions to make in changing many of the factors described, implementing strategies that seek to prevent poor outcomes at multiple levels, from the most distal (facilitating societal attention to broad-based factors that influence population health) to the more proximal (population-based action on the conditions that influence health behaviors) (IOM, 2011b).
The United States seems to lag behind most high-income nations in the deployment of socially protective strategies that appear to correlate with better population health (NRC, 2011; OECD, 2009, 2010b). Excessive allocation of national spending on medical care services poses major societal opportunity costs and restricts funding opportunities for other essential sectors such as education, energy, water, transportation, agriculture, and employment (Anderson and Frogner, 2008; Darzi et al., 2011). For example, the rise of medical care costs and the recent recession have contributed to a decline in state appropriations for public higher education (Kane and Orszag, 2003; Orszag, 2010). In 2008, some 43 states cut financing for colleges and universities or increased tuition (Johnson et al., 2011). The decrease in state subsidizing of public higher education has left public colleges and universities less competitive in salaries and spending on students than private colleges and universities and has decreased the quality of public higher education in the United States. Educational achievement has been found to be a more powerful predictor of health status than access to medical care, thereby raising the question of how the nation considers its priorities for resource allocation if disinvestments in education predictably lead to a less educated populace, with poorer health status (Cutler and Lleras-Muney, 2006; Woolf et al., 2007).
A World Economic Forum report noted that “as the economic burden of chronic disease grows, it could crowd out monies needed to improve other critical issues as well as to meet basic needs such as education and infrastructure” (World Economic Forum, 2008, p. 5). Indeed, national investments in other social services and infrastructure are key to health and health
system performance and to sustained economic development. An analysis of data on 30 OECD countries that examined the relationship between five population health outcomes (life expectancy, maternal mortality, infant mortality, low birth weight, and productive life years lost) and health care or non–health care social spending showed that spending allocation in the United States is the reverse of that in other OECD countries (Bradley et al., 2011). The ratio of non–health care social spending to health care social spending was 2.0 in the OECD countries compared to 0.83 in the United States (see Figure 1-1).
Bradley and colleagues reported improved population health outcomes both in association with health care social spending (measured by life expectancy and maternal mortality) and for non–health care social spending (measured by life expectancy, infant mortality, and potential years of life lost), demonstrating the favorable health effects of other social domains on health (Bradley et al., 2011). In other studies of social spending influences on health, Eikemo and colleagues (2008) and Muntaner et al. (2011) have grouped European countries according to well-established political typologies that reflect a variety of social programs (health and non–health related social spending) and characteristics. Both sets of researchers found evidence of a relationship between national health status and national investment in social programs such as social transfers (for example, social security and unemployment benefits) and policies that support full employment and income protection. Scandinavian countries topped the ranking. Eastern and southern European nations had the lowest levels of social spending and the poorest health outcomes. It is important to note that there are considerable social and political differences among these nations and between them and the United States. However, there is no doubt that when a high proportion of social spending goes for medical care, as is the case in the United States, there is less money available for other important contributors to health (such as early childhood development and education) (see Box 1-3). Smeeding (2005) and Garfinkel et al. (2005) found that the vast majority of U.S. social spending goes toward medical care, and a far smaller fraction remains available for other social programs. OECD data from the last several years shows that the United States invests far less than its peers in several dimensions of child well-being. It was beyond the committee’s ability to ascertain the implications of such differences and the opportunity cost of the nation’s social spending, but an upcoming report from a joint National Research Council–Institute of Medicine committee will consider the effect of national attention to such factors on health differences among high-income nations (NRC and IOM, 2012).
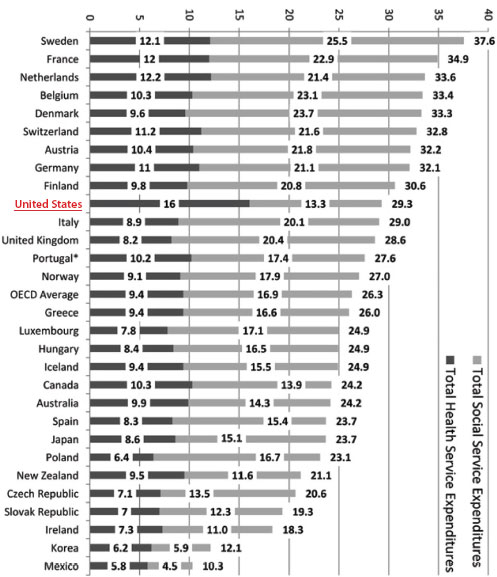
FIGURE 1-1 Average social-service expenditures versus average health-services expenditures as percentages of gross domestic product (GDP) from 1995 to 2005 by country.
SOURCE: Bradley et al., 2011, p. 3.
Spending More Prudently
In the United States, public health and prevention strategies are financed through a complex and often ad hoc patchwork of funding streams with federal, state, local, and private sources that vary widely among communities and exhibit considerable instability (this is discussed in detail in Chapter 2). Funding levels and targets are rarely based on objective measures of
BOX 1-3
An Example of the Opportunity Costs of
Runaway Medical Care Spending
The nation’s excessive medical care expenditures present opportunity costs. For example, the United States underinvests in infant and early childhood development, and investments in education are uneven, leaving some populations disadvantaged (Barnett et al., 2010; Epstein and Barnett, 2010). There is compelling evidence of the significance of education for numerous health outcomes including infant mortality (maternal education) (Matthews et al., 2008), life expectancy (Census Bureau, 2010), and adult health behaviors and health status (Cutler and Lleras-Muney, 2006). An “education gradient” exists that demonstrates increased health benefits with greater levels of education and is consistent in men, women, blacks, and whites (Cutler and Lleras-Muney, 2006). Infants’ and children’s social and economic environments have profound and potentially lifelong impacts on health through brain, cognitive, and behavior development (Garner et al., 2012). Associations have been shown between early childhood brain developmental experiences and numerous chronic conditions which account for much of adult morbidity, mortality, and health care cost including hypertension, cardiovascular disease, stroke, obesity, depression, and diabetes (Cubbin et al., 2008).
preventable disease burden and risk but rather are driven by the confluence of historical precedent, government fiscal capacities, political dynamics, and agency entrepreneurship. The results are large gaps between population health needs and available resources in many communities and large inequities in health protection and risk reduction among communities and population groups.
The current U.S. level of support for the governmental public health infrastructure is inadequate to deliver the health and economic benefits of prevention. Although more than 75 percent of health care costs is attributable to preventable conditions, estimates consistently indicate that as little as 3 percent of U.S. health spending is devoted to public health and prevention activities (CMS, 2011; Mays and Smith, 2011; Miller et al., 2008). Although public health writ large commands additional resources through other government agencies and programs that foster the health of the public (such as highway safety or food security) (Grogan, 2012) these contributions are not included in the CMS calculation. Nor does this report consider them in any detail, given the committee’s charge to examine funding streams that support governmental public health infrastructure. (The committee elaborates further on this in Chapter 4.) Several sources attest to the inadequacy of that spending level, including recent National Association
of County and City Health Officials and Association of State and Territorial Health Officials reports of program cuts and deep staff reductions, Trust for America’s Health assessments of health department preparedness for public health emergencies, and various reports showing how state or local public health departments struggle to make ends meet while fulfilling their statutory duties to their communities (ASTHO, 2012; NACCHO, 2012; TFAH, 2012). In fact, the nation spends several times as much on administrative overhead for medical care and health insurance as it does on public health activities (CMS, 2011; Mays and Smith, 2011). Turnock (2009) notes that 2 percent of HHS funding goes to the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration, the primary federal funding sources for local public health activities. The bulk of HHS funding goes to publicly funded clinical care (through Medicaid and Medicare) and to the National Institutes of Health, largely for basic research, little of it for primary prevention and even less for population-based interventions.
Medicine’s lack of success in countering the rise in obesity demonstrates the limited reach of clinical interventions. The available evidence suggests that population-based efforts are needed to modify the social, environmental, and policy contexts that encourage poor eating and inactivity (Candib, 2007; Kumanyika et al., 2002; TRB and IOM, 2005). Considerable evidence links obesity to environmental factors that are clearly out of the reach of clinical interventions: for example, children’s eating habits and nutritional preferences are affected by advertising, and those early influences affect life-long behaviors (McGinnis et al., 2006; Wilcox et al., 2004). Leverage from outside the clinical care sector, such as urban design and food policy shifts to address obesity for population health improvements is also important. Consequently, solutions to complex population-level problems like obesity require the ability to design and mobilize coordinated, multi-pronged initiatives that support changes at multiple points on the web of causation [for an example, see CDC, 2011b,c, describing the effect of an array of community-based obesity prevention programs on the prevalence of childhood obesity in New York City (Jilcott Pitts et al., 2012; Ohri-Vachaspati, 2012)].
The modern history of governmental public health has demonstrated its capacity in the not-so-distant past to mobilize large-scale, multi-faceted solutions related to such issues as tobacco control, vaccine preventable diseases, and lead poisoning prevention (CDC, 2011b). If that capacity were similarly mobilized for obesity prevention on a population-wide basis, the resulting health and economic impact would be substantial. For example, reducing the prevalence of adult obesity by 50 percent—roughly the same relative reduction as was achieved through public health’s multi-faceted attack on smoking prevalence during the latter decades of the 20th century—could produce a $58 billion reduction in annual U.S. medical care
expenditures, according to estimates from a recent simulation study (Dall et al., 2009). That reduction would be sufficient to offset 50-65 percent of the total expected growth in medical care expenditures in a typical year, not to mention additional reductions in the indirect costs of obesity through gains in worker productivity. Achieving the necessary reduction in obesity prevalence would be challenging but feasible through a combination of behavioral, policy, and environmental changes that would see the average overweight adult reducing daily caloric intake or increasing daily caloric expenditure by a modest 100 calories per day over 4 years, equivalent to one less serving of sugar-sweetened beverages per day or an additional mile of walking per day. History demonstrates that such large-scale, high-impact changes in population health are possible through deliberately targeted and sufficiently resourced public health efforts.
SETTING A NATIONAL TARGET FOR IMPROVED HEALTH
There is a broad consensus among labor, business, and government that the U.S. health status and the health system are in urgent need of improvement. Improving U.S. health system performance requires clear overall system objectives, discrete quantifiable targets, effective and sustained leadership, and clear and unambiguous accountability for achieving targets and overall system performance. The locus of responsibility for U.S. health system performance is the office of the Secretary of Health and Human Services. The secretary of HHS is well-positioned to set national health performance targets for several reasons. HHS is responsible for some of the key guiding documents for the nation’s health, such as the Healthy People initiatives. Also, because the National Prevention, Health Promotion and Public Health Council is convened under the aegis of the surgeon general of the U.S. Public Health Service, the committee believes that there is a greater likelihood than previously that at least the federal government will be able to coordinate its policies (in areas not limited to health) in ways that could benefit population health. The committee’s report For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges provided examples of such “health in all policies” approaches, including the Department of Housing and Urban Development–Department of Transportation–Environmental Protection Agency Partnership for Sustainable Communities initiative (IOM, 2011a).
There is a need to consolidate the abundant health and health system targets to simplify and focus national efforts on the most essential health and health system outcomes (IOM, 2011b). The committee believes that measures of healthful longevity and per capita health expenditure are appropriate to address this need. In the absence of such clear health system performance targets, national efforts to remedy our health system preparedness
to address the major contemporary national health threats will be diluted, inefficient, and incremental.
Health-adjusted life expectancy (HALEs) as an aggregate measure of health system performance were discussed in the committee’s first report, For the Public’s Health: The Role of Measurement in Action and Accountability (IOM, 2011b) and described as the best instrument for describing and monitoring population health. A consensus measure is still undergoing testing through the National Center for Health Statistics, and the committee found that an interim measure of aggregate health will continue to be required until a national approach is established (IOM, 2011b). The committee endorses using life expectancy as this interim measure. The measure is imperfect, but it has a demonstrated association with spending on healthcare and is used by other nations for this purpose (see Figure 1-2) (OECD, 2010a).8Figure 1-2 shows life expectancy vs. total expenditures on health in OECD countries. The lower left side of the curve shows largely middle-income nations, while the cluster near the center shows largely higher income nations, and the United States is the outlier at far right.
The committee reviewed evidence that other high income countries that have sophisticated medical care achieve better value for their health investments. This is shown in research and analyses of the OECD that built on a body of work involving multiple international organizations—including the World Bank, the World Health Organization, and the World Economic Forum—that measured system cost-effectiveness or assessed value per dollar spent by comparing health spending with life expectancy (see, for example, Anderson, 2008; Cutler and Lleras-Muney, 2006; Darzi et al., 2011; Murray and Frenk, 2010; Poullier et al., 2002; WHO, 2010).
Research suggests that one-third of all medical expenditures (which, given the insignificant spending on non-clinical health activities, this proportion, synonymous with one-third of all health expenditures) is wasted and thus does not lead to improvements in health outcomes (Bentley et al., 2008; Fineberg, 2012; IOM, 2010, 2011c; Joumard et al., 2010). In cases of misuse and overuse, such inefficient spending is actually harmful, and finding ways to remedy it could help the United States realize greater value for its investment. In sum, the solutions to achieving better value include
______________
8In addition to summary measures of population health, the committee’s report on measurement also recommended the development and implementation of measures of community health, to reflect not merely rates of death or disease in a community, but attributes of the community that contribute to or detract from its ability to promote health. Such measures could include metrics of a community’s walkability and other aspects of the built environment, the food environment, and other features.
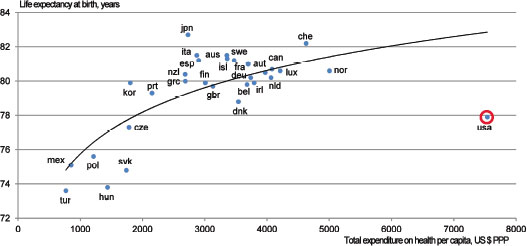
FIGURE 1-2 Health spending and life expectancy (2008* data).
NOTE: aus = Australia; aut = Austria; bel = Belgium; can = Canada; che = Switzerland; cze = Czech Republic; deu = Germany; dnk = Denmark; esp = Spain; fin = Finland; fra = France; gbr = United Kingdom; grc = Greece; hun = Hungary; irl = Ireland; isl = Iceland; ita = Italy; jpn = Japan; kor = Korea; lux = Luxembourg; mex = Mexico; nld = Netherlands; nor = Norway; nzl = New Zealand; pol = Poland; prt = Portugal; svk = Slovak Republic; tur = Turkey; swe = Sweden; usa = United States.
SOURCE: OECD Health Data, 2010.
1. controlling administrative waste;
2. eliminating sources of excess cost and other inefficiencies in clinical care, while improving quality;
3. achieving universal coverage (this involves increased cost for basic services, but also savings by intervening earlier and broadening coverage); and
4. implementing population-based health improvement strategies (including acting on non-health factors that are known to influence health outcomes).
The first three solutions have been discussed in detail by prior IOM committees, the IOM Roundtable on Value & Science-Driven Health Care, and many others (Berwick et al., 2003; CBO, 2011; CDC, 2011b,c; IOM, 2000, 2011c). The present committee has examined the fourth solution, although focusing mostly on the governmental public health enterprise and its contributions to population health. The evidence on the effectiveness of population-based interventions includes several pieces of information, beginning with a growing body of systematic reviews and recommendations (for example, from the CDC Community Preventive Services Task Force). Two-thirds of the increases in life expectancy observed in the United States
in the 20th century predate 1950 and the major expansion in biomedical science and technology, and are attributed to basic public health strategies (clean water, sanitation, and infectious disease control) (CDC, 1999b). Moreover, the main causes of poor health (such as substance use, motor vehicle crashes, homicide, suicide, and cardiovascular disease) are not primarily solvable by clinical care but are amenable to population-based approaches. Finally, what could differentiate the United States from comparable nations falls outside the medical realm, and includes shortfalls in educational achievement, and lack of investment in and policy attention to other social factors known to have favorable effects on health (see, for example, Bradley and Taylor, 2011).
Comparing life expectancy and health spending sheds some light on value per dollar spent, but it has limitations. Life expectancy is only one of many measures of health status, and spending outside the health sector also influences health (Anderson, 2008). However, life expectancy has been shown to correlate with other indicators of health status (OECD, 2010a,b), and the fact that non-health spending can also influence health outcomes is itself informative. Recognizing this suggests the diminishing returns and opportunity costs of the high U.S. spending on medical care (Anderson, 2008; Darzi et al., 2011; WHO, 2010). The experience of many other high-income nations indicates that it is possible to achieve greater value, to obtain better results while spending less on health. The United States can move in that direction by implementing the four solutions outlined above, and its progress can be measured against benchmarks in cost savings, and in health outcomes. This leads to the following proposal of a two-part goal for the nation.
Recommendation 1: The Secretary of HHS should adopt an interim explicit life expectancy target, establish data systems for a permanent health-adjusted life expectancy target, and establish a specific per capita health expenditure target to be achieved by 2030. Reaching these targets should engage all health system stakeholders in actions intended to achieve parity with averages among comparable nations on healthy life expectancy and per capita health expenditures.
The committee proposes a modest level of health improvement. According to the data in NRC, 2011 (Table 1-1), the 2006 life expectancy for U.S. women at the age of 50 years was 33.0 years. The mean in OECD countries was 34.5 years (standard deviation [SD],9 1.56 years; range, Denmark 31.9 years, to Japan 37.1 years). Assuming no additional secular improvements in
______________
9SDs were derived from NRC, 2011.
life expectancy the goal would require that the United States add an average of about 1.5 years to the life expectancy of 50-year-old women. Reaching the top ranking would require the far more ambitious addition of 4.1 years. The 2006 life expectancy for U.S. men at the age of 50 years was 29.2 years. The mean in OECD countries was 30.0 (SD, 0.95 years; range, Denmark, 28.2 years, to Australia, 31.5 years), and reaching that would require that the United States add 0.8 years to the life expectancy of 50-year-old men. Reaching the top-ranking nation would require a gain of 2.3 years. Those estimates, however, do not reflect the fact that comparable countries will continue to make gains; thus, the committee recognizes that the current gap in life expectancy that needs to be closed is less than the increase that will be needed to bring U.S. life expectancy to a level comparable with the average of its peers.
THE CENTRALITY OF PUBLIC HEALTH IN
ACHIEVING HEALTH SYSTEM IMPROVEMENT
Governmental public health plays pivotal roles in a health system that comprises of multiple societal subsystems whose dynamic interactions create living conditions that determine health (“social determinants”) (Braveman et al., 2011b; Marmot et al., 2008; WHO Commission on Social Determinants of Health, 2008; Wilkinson and Marmot, 2003). Public health is an essential component of a focused national strategy for improving health and health system performance. Its capabilities have been deployed against some past major health challenges that were complex and multi-sectoral, for example, lead toxicity, drinking water fluoridation, motor vehicle safety, and cigarette smoking. The reduction in lead toxicity in children and households during the last three decades is due largely to public health leadership in removing lead from paint and gasoline, screening children and remediating homes, surveillance, and engagement of the private sector and the medical care delivery system (Gold et al., 1994). In the case of motor vehicle and road safety, interventions affecting numerous reinforcing system sectors were undertaken. The interventions involved families, communities, schools, workplaces, governments, law enforcement, motor vehicle manufacturers, and transportation system designers. The systems approach precipitously reduced motor vehicle fatalities despite dramatic increases in motor vehicle density and vehicle miles traveled throughout the 20th century (CDC, 1999a). A third example of public health deployment on a major health challenge is cigarette smoking. Since the 1964 Surgeon General’s Report on smoking, millions of productive lives have been saved as the prevalence of smoking among adults has declined (Gold et al., 1994). As in the case of motor vehicle safety, multi-sectoral interventions involving the mass media, legislation, employers, schools, health care providers and non-profit orga-
nizations have been used to accomplish the reduction (CDC, 1996; Florida Department of Health, 2012).
Over the last century, governmental public health has been charged, organized and funded to convene, collaborate and act to control major health threats from infectious diseases; unsafe water, sanitation, housing, and transportation; occupation disease and injury; and smoking (CDC, 1999b). Current major health threats are the result of health system dynamics that have changed during the last 30 years, altered living conditions and led to a new constellation of population health challenges in the 21st century (Wahdan, 1996; WHO, 2012a). Chronic physical and behavioral health conditions are now the major health impediments to active living and personal fulfillment and to national economic competitiveness and productivity (Thorpe et al., 2010; WHO, 2012b). Those non-communicable conditions are downstream effects of social and physical environments and the personal behaviors that they influence (Candib, 2007; Gibson et al., 2011; McGinnis and Foege, 1993; Mokdad et al., 2004). These conditions are of particular consequence to people of lower income and low educational achievement. The well-known inequalities that class differences confer are important obstacles to achieving healthy life expectancy comparable with that of other wealthy nations.
Creating health more efficiently throughout the population will require both addressing the social and environmental determinants of health and taking a more systematic and concerted look at the clinical care delivery system’s effectiveness in creating health through the services that it delivers. In contrast with the pivotal role occupied by the public health field in leading interventions directed at the major population health challenges of the last century, governmental public health departments have not been adequately funded to take on the complex tasks of designing and implementing strategies that can limit the burden of non-communicable diseases in the United States. Public health has also not been called on to exercise its data capacity and analytic skills to assist the medical care delivery system in evaluating the appropriateness (with respect to underuse and overuse of services) and success of the care that it furnishes. More rapid change is needed.
The committee views governmental public health as a key health system force in improving health outcomes and mitigating health expenditures. It will require a fundamental transformation of its mission (see Chapter 2) and organization and, adequate and stable funding for deploying public health experience and skill to meet pressing population health challenges (Bar-Yam, 2006; Lurie, 2002).
The urgency of a comprehensive national approach to the remediation of the “upstream” causes of non-communicable diseases, injuries and other contemporary health challenges, and the urgency of improving the functioning of the clinical care system could not be more pronounced. The nation’s
expenditures on medical care are grossly disproportionate to the quality, efficiency, and equity with which they being delivered (AHRQ, 2007; Commonwealth Fund Commision on a High Performance Health System, 2008, 2009; IOM, 2000, 2001; Leape and Berwick, 2000).
The Affordable Care Act was enacted to address this crisis in health and in health care costs. It seeks to provide access to care for 32 million uninsured Americans and to establish a framework of centers and authorities charged to improve quality and control costs by reducing variation in practice, implementing new models for care, and changing payment mechanisms and spending by Medicare (Patient Protection and Affordable Care Act, Public Law 111-148). The legislation recognizes the importance of public health and provides investments in population health initiatives, including the grants for community transformation and the prevention and public health trust fund (HHS, 2010a,b, 2011). However, the investment is small (and has already been substantially reduced) (Benjamin, 2012) compared with medical care interventions and no changes to federal incentives to states are made to reform the priorities, organization or funding of the public health infrastructure. The national strategy to address the health crisis is directed predominantly downstream at the locus of care delivery and only weakly upstream at the causes of poor health that continue to generate large volumes of new cases in the medical care delivery system.
Beginning with its first report (IOM, 2011b), the present committee has discussed the evidence that some of the most powerful interventions to improve America’s poor health performance are multi-sectoral public health interventions and other population-based approaches to health improvement. Such approaches are informed by high-quality population health and care delivery performance indicators as discussed in For the Public’s Health: The Role of Measurement in Action and Accountability (IOM, 2011b). They will be facilitated by the use of powerful tools of law and public policy to transform conditions for living (such as education and the physical and social environment) that impact health, as discussed in the committee’s second report, For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges (IOM, 2011a).
In this, its third report, the committee offers guidance for rebalancing the nation’s portfolio of health investments by revitalizing governmental public health and, giving it the resources necessary to reign in preventable diseases, injuries, and their associated costs on a broad national scale. Public health funding for new mission support, re-organization, and information management will be essential for improving population health.
AHRQ (Agency for Healthcare Research and Quality). 2007. National Healthcare Disparities Report. Rockville, MD: HHS.
Anderson, G. F., and B. K. Frogner. 2008. Health spending in OECD countries: Obtaining value per dollar. Health Affairs 27(6):1718-1727.
Anderson, P. 2008. Reducing overweight and obesity: Closing the gap between primary care and public health. Family Practice 25(Suppl 1):10-16.
ASTHO (Association of State and Territorial Health Officials). 2012. Budget Cuts Continue to Affect the Health of Americans: Update March 2012. Arlington, VA: ASTHO.
Auerbach, D. I., and A. L. Kellermann. 2011. A decade of health care cost growth has wiped out real income gains for an average US family. Health Affairs 30(9):1630-1636.
Barnett, W. S., D. J. Epstein, M. E. Carolan, J. Fitzgerald, D. J. Ackerman, and A. H. Friedman. 2010. The State of Preschool 2010. New Brunswick, NJ: The National Institute for Early Education Research.
Bar-Yam, Y. 2006. Improving the effectiveness of health care and public health: A multiscale complex systems analysis. American Journal of Public Health 96(3):459-466.
Benjamin, G. 2012. Prevention Funding: One Step Forward, Two Steps Back. http://healthaffairs.org/blog/2012/03/01/prevention-funding-one-step-forward-two-steps-back/ (March 5, 2012).
Bentley, T. G. K., R. M. Effros, K. Palar, and E. B. Keeler. 2008. Waste in the U.S. health care system: A conceptual framework. Milbank Quarterly 86(4):629-659.
Berwick, D. M., N. A. DeParle, D. M. Eddy, P. M. Ellwood, A. C. Enthoven, G. C. Halvorson, K. W. Kizer, E. A. McGlynn, U. E. Reinhardt, R. D. Reischauer, W. L. Roper, J. W. Rowe, L. D. Schaeffer, J. E. Wennberg, and G. R. Wilensky. 2003. Paying for performance: Medicare should lead. Health Affairs 22(6):8-10.
Boyle, J., T. Thompson, E. Gregg, L. Barker, and D. Williamson. 2010. Projection of the year 2050 burden of diabetes in the US adult population: Dynamic modeling of incidence, mortality, and prediabetes prevalence. Population Health Metrics 8(1):29.
Bradley, E. H., and L. Taylor. 2011. To Fix Health, Help the Poor. The New York Times. http://www.nytimes.com/2011/12/09/opinion/to-fix-health-care-help-the-poor.html (December 12, 2011).
Bradley, E. H., B. R. Elkins, J. Herrin, and B. Elbel. 2011. Health and social services expenditures: Associations with health outcomes. BMJ Quality & Safety 20(10):826-831.
Braveman, P., S. Egerter, and D. R. Williams. 2011a. The social determinants of health: Coming of age. Annual Review of Public Health 32:381-398.
Braveman, P. A., S. A. Egerter, and R. E. Mockenhaupt. 2011b. Broadening the focus: The need to address the social determinants of health. American Journal of Preventive Medicine 40(1 Suppl 1):S4-S18.
Brownson, R. C., D. Haire-Joshu, and D. A. Luke. 2006. Shaping the context of health: A review of environmental and policy approaches in the prevention of chronic diseases. Annual Review of Public Health 27(1):341-370.
Bunker, J. P., H. S. Frazier, and F. Mosteller. 1994. Improving Health: Measuring Effects of Medical Care. The Milbank Quarterly 72(2).
California Department of Public Health. 2011. California Smoking Rate Reaches Historic Low (Press Release). http://www.cdph.ca.gov/Pages/NR11-031.aspx (July 13, 2011).
California Department of Public Health Tobacco Control Program. 2009. California Tobacco Control Update 2009. 20 Years of Tobacco Control in California. Sacramento: California Department of Public Health.
Campaign for Tobacco-Free Kids. 2011. Comprehensive Tobacco Prevention and Cessation Programs Effectively Reduce Tobacco Use. Washington, DC: Campaign for Tobacco-Free Kids.
Candib, L. M. 2007. Obesity and diabetes in vulnerable populations: Reflection on proximal and distal causes. The Annals of Family Medicine 5(6):547-556.
CBO (Congressional Budget Office). 2011. CBO’s 2011 Long-term Budget Outlook. Washington, DC: CBO.
CDC (Centers for Disease Control and Prevention). 1996. State Tobacco Control Highlights—1996 (Publication No. 099-4895). Atlanta, GA: CDC, National Center for Chronic Disease Prevention and Health Promotion, and Office on Smoking and Health.
CDC. 1999a. Achievements in public health 1900-1999. Motor-Vehicle safety: A 20th century public health achievement. Morbidity and Mortality Weekly Report 48(12):369-374.
CDC. 1999b. Ten great public health achievements—United States, 1900-1999. Morbidity and Mortality Weekly Report 48(12):241-243.
CDC. 2004. Sustaining State Funding for Tobacco Control: The Facts. Atlanta, GA: CDC.
CDC. 2005. Annual Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 1997–2001. Morbidity and Mortality Weekly Report 54(25):625-628.
CDC. 2008. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000-2004. Morbidity and Mortality Weekly Report 57(45):1226-1228.
CDC. 2011a. Chronic Disease Prevention and Health Promotion. Preventive Health and Health Services Block Grant. A Critical Public Health Resource at a Glance 2011. http://www.cdc.gov/chronicdisease/resources/publications/AAG/blockgrant.htm (January 3, 2012).
CDC. 2011b. Obesity in K-8 students—New York City, 2006-07 to 2010-11 School Years. Morbidity and Mortality Weekly Report 60:1673-1678.
CDC. 2011c. Overweight and Obesity: Program Highlights. http://www.cdc.gov/obesity/stateprograms/highlights.html (March 30, 2012).
CDC. 2011d. Rising Health Care Costs are Unsustainable. http://www.cdc.gov/workplacehealthpromotion/businesscase/reasons/rising.html (January 27, 2012).
CDC. 2011e. Ten great public health achievements—United States, 2001-2010. Morbidity and Mortality Weekly Report 60(19):619-623.
CDC. 2011f. Vital signs: Current cigarette smoking among adults aged ≥18 Years—United States, 2005-2010. Morbidity and Mortality Weekly Report 60(35):1207-1212.
Census Bureau. 2010. National Longitudinal Mortality Study. http://www.census.gov/did/www/nlms/publications/public.html.
CIA (Central Intelligence Agency). 2011. World Factbook. Washington, DC: CIA.
CMS (Centers for Medicare and Medicaid Services). 2010. National Health Expenditure Projections 2009-2019. Forecast Summary. Baltimore, MD: HHS.
CMS. 2011. National Health Expenditures. https://www.cms.gov/NationalHealthExpendData/downloads/tables.pdf (December 19, 2011).
Collins, J. J., C. M. Baase, C. E. Sharda, R. J. Ozminkowski, S. Nicholson, G. M. Billotti, R. S. Turpin, M. Olson, and M. L. Berger. 2005. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. Journal of Occupational and Environmental Medicine 47(6):547-557.
Commonwealth Fund Commision on a High Performance Health System. 2008. Why Not the Best? Results from the National Score Card on U.S. Health System Performance, 2008. NY, New York: The Commonwealth Fund.
Commonwealth Fund Commision on a High Performance Health System. 2009. The Path to a High Performance U.S. Health System: A 2020 Vision and the Policies to Pave the Way. Washington, DC: The Commonwealth Fund.
Cory, S., A. Ussery-Hall, S. Griffin-Blake, A. Easton, J. Vigeant, L. Balluz, W. Garvin, and K. Greenlund. 2010. Prevalence of selected risk behaviors and chronic diseases and conditions-steps communities, United States, 2006-2007. Morbidity and Mortality Weekly Report. Surveillance Summaries 59(8):1-37.
Cubbin, C., V. Pedregon, S. Egerter, and P. Braveman. 2008. Where We Live Matters for Our Health: Neighborhoods and Health. Princeton, NJ: Robert Wood Johnson Foundation.
Cutler, D. M., and A. Lleras-Muney. 2006. Education and Health: Evaluating Theories and Evidence. NBER Working Paper Series (Working Paper 12352). Cambridge, MA: National Bureau of Economic Research.
Dall, T. M., V. L. Fulgoni, Y. Zhang, K. J. Reimers, P. T. Packard, and J. D. Astwood. 2009. Potential health benefits and medical cost savings from calorie, sodium, and saturated fat reductions in the American diet. American Journal of Health Promotion 23(6):412-422.
Darzi, A., S. Beales, M. Hallsworth, D. King, M. Macdonnell, and I. Vlaev. 2011. The Five Bad Habits of Healthcare. How New Thinking About Behaviour Could Reduce Health Spending. Geneva, Switzerland: World Economic Forum and Imperial College.
de la Plata, C. M., M. Hewlitt, A. de Oliveira, A. Hudak, C. Harper, S. Shafi, and R. Diaz-Arrastia. 2007. Ethnic differences in rehabilitation placement and outcome after TBI. The Journal of Head Trauma Rehabilitation 22(2):113-121.
DeVol, R., and A. Bedroussian. 2007. An Unhealthy America: The Economic Burden of Chronic Disease. Charting a New Course to Save Lives and Increase Productivity and Econmic Growth. Executive Summary and Research Findings. Santa Monica, CA: Milken Institute.
Dilley, J. A., J. R. Harris, M. J. Boysun, and T. R. Reid. 2011. Program, policy, and price interventions for tobacco control: Quantifying the return on investment of a state tobacco control program. American Journal of Public Health 102(2):22-28.
Edington, D. W. 2001. Emerging research: A view from one research center. American Journal of Health Promotion 15(5):341-349.
Eikemo, T. A., C. Bambra, K. Judge, and K. Ringdal. 2008. Welfare state regimes and differences in self-perceived health in Europe: A multilevel analysis. Social Science & Medicine 66(11):2281-2295.
Epstein, D. J., and W. S. Barnett. 2010. Early education in the United States: Programs and access. In Handbook of Early Childhood Education edited by R. C. Pianta, W. S. Barnett, L. M. Justice, and S. M. Sheridan. New York: The Guilford Press.
Ewing, R. 2005. Can the physical environment determine physical activity levels? Exercise and Sport Sciences Reviews 33(2):69-75.
Farrelly, M. C., T. F. Pechacek, and F. J. Chaloupka. 2003. The impact of tobacco control program expenditures on aggregate cigarette sales: 1981-2000. Journal of Health Economics 22(5):843-859.
Farrelly, M. C., T. F. Pechacek, K. Y. Thomas, and D. Nelson. 2008. The impact of tobacco control programs on adult smoking. American Journal of Public Health 98(2):304-309.
Fineberg, H. V. 2012. A successful and sustainable health system—how to get there from here. New England Journal of Medicine 366(11):1020-1027.
Finkelstein, E. A., J. G. Trogdon, J. W. Cohen, and W. Dietz. 2009. Annual medical spending attributable to obesity: Payer and service specific estimates. Health Affairs 28(5):822-831.
Florida Department of Health. 2012. Tobacco Free Florida. http://www.doh.state.fl.us/tobacco/tobacco_home.html (January 6, 2012).
Fronstin, P. 2011. 2011 Health confidence survey: Most Americans unfamiliar with key aspect of health reform. Employee Benefit Research Institute 32(9):2-12.
Garfinkel, I., T. M. Smeeding, and L. Rainwater. 2005. Welfare State Expenditures and the Redistribution of Well-being: Children, Elders, and Others in Comparative Perspective. Working Paper. Luxembourg: Luxembourg Income Study (LIS).
Garner, A. S., J. P. Shonkoff, B. S. Siegel, M. I. Dobbins, M. F. Earls, L. McGuinn, J. Pascoe, and D. L. Wood. 2012. Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics 129(1):224-231.
Gibson, M., M. Petticrew, C. Bambra, A. J. Sowden, K. E. Wright, and Whithead. 2011. Housing and health inequalities: A synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health & Place 17(1):175-184.
Gilpin, E. A., S. L. Emery, A. J. Farkas, J. M. Distefan, M. M. White, J. P. Pierce. 2001. The California Tobacco Control Program: A Decade of Progress, Results from the California Tobacco Surveys, 1990-1998. La Jolla: University of California, San Diego.
Gold, M. R., S. Teutsch, K. McCoy, P. Shaffer, J. Siegel, P. Johnson, B. R. Luce, R. E. Brown, M. O. Butler, G. Lissovoy, M. T. Halpern, M. L. Hare, E. Hatziandreu, J. Hersey, R. P. Hertz, P. McMenamin, B. Rader, M. Rothman, and J. J. Stein. 1994. For a Healthy Nation: Returns on Investment in Public Health. Washington, DC: HHS, Office of Disease Prevention and Health Promotion, CDC, and Centers for Public Health Research and Evaluation.
Goldman, D. P., Y. Zheng, F. Girosi, P. C. Michaud, S. J. Olshansky, D. Cutler, and J. W. Rowe. 2009. The benefits of risk factor prevention in Americans aged 51 years and older. American Journal of Public Health 99(11):2096-2101.
Grogan, C. M. 2012. Behind the jargon: Prevention spending. Journal of Health Politics, Policy and Law 37(2):229-342.
Haider, A. H., D. C. Chang, D. T. Efron, E. R. Haut, M. Crandall, and E. E. Cornwell, III. 2008. Race and insurance status as risk factors for trauma mortality. Archive of Surgery 143(10):945-949.
Halpin, H. A., M. M. Morales-Suarez-Varela, and J. M. Martin-Moreno. 2010. Chronic disease prevention and the new public health. Public Health Reviews 32(1):120-154.
HHS (Department of Health and Human Services). 2010a. HHS Awards $16.8 Million to Train Public Health Workforce: Grants Awarded to 27 Public Health Training Centers (News Release). http://www.hhs.gov/news/press/2010pres/09/20100913a.html (November 12, 2010).
HHS. 2010b. Sebelius Announces New $250 Million Investment to Lay Foundation for Prevention and Public Health (News Release). http://www.hhs.gov/news/press/2010pres/06/20100618g.html (June 22, 2010).
HHS. 2011. Affordable Care Act Funds to Help Create Healthier U.S. Communities. http://www.hhs.gov/news/press/2011pres/06/20110616b.html (June 20, 2011).
Himmelstein, D. U., D. Thorne, E. Warren, and S. Woolhandler. 2009. Medical bankruptcy in the United States, 2007: Results of a national study. American Journal of Medicine 122(8):741-746.
Homer, J. B., and G. B. Hirsch. 2006. System dynamics modeling for public health: Background and opportunities. American Journal of Public Health 96(3):452-458.
IOM (Intitute of Medicine). 1988. The Future of Public Health. Washington, DC: National Academy Press.
IOM. 2000. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press.
IOM. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2003. The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press.
IOM. 2007. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: The National Academies Press.
IOM. 2009. Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence. Washington, DC: The National Academies Press.
IOM. 2010. Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: The National Academies Press.
IOM. 2011a. For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges. Washington, DC: The National Academies Press.
IOM. 2011b. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: The National Academies Press.
IOM. 2011c. The Healthcare Imperative: Lowering Costs and Improving Outcomes—Workshop Series Summary. Washington, DC: The National Academies Press.
Jilcott Pitts, J. S. B., L. M. Whetstone, J. R. Wilkerson, T. W. Smith, A. S. Ammerman. 2012. A Community-Driven Approach to Identifying “Winnable” Policies Using the Centers for Disease Control and Prevention’s Common Community Measures for Obesity Prevention. http://www.cdc.gov/pcd/issues/2012/11_0195.htm (March 30, 2012). Johnso
Johnson, N., P. Oliff, and E. Williams. 2011. An Update on State Budget Cuts. At Least 46 States Have Imposed Cuts That Hurt Vulnerable Residents and Cause Job Loss. Washingon, DC: Center on Budget and Policy Priorities.
Joumard, I., C. Andre, and C. Nicq. 2010. Health Care Systems: Efficiency and Institutions, OECD Economics Department (Working Papers, No. 769). Paris, France: OECD.
Kane, T. J., and P. R. Orszag. 2003. Higher Education Spending: The Role of Medicaid and the Business Cycle. The Brookings Institution Policy Brief, Vol. 24. Washington, DC: The Brookings Institution.
Kessler, R. C., P. E. Greenberg, K. D. Mickelson, L. M. Meneades, and P. S. Wang. 2001. The effects of chronic medical conditions on work loss and work cutback. Journal of Occupational and Environmental Medicine 43(3):218-225.
KFF (The Henry J. Kaiser Family Foundation). 2012. U.S. Health Care Cost. http://www.kaiseredu.org/Issue-Modules/US-Health-Care-Costs/Background-Brief.aspx#footnote7 (February 24, 2012).
Kumanyika, S., R. W. Jeffery, A. Morabia, C. Ritenbaugh, V. J. Antipatis, and P. W. Grp. 2002. Obesity prevention: The case for action. International Journal of Obesity 26(3):425-436.
Leape, L. L., and D. M. Berwick. 2000. Safe health care: Are we up to it? British Medical Journal 320(7237):725-726.
Lucas, F. L., T. A. Stukel, A. Morris, A. E. Siewers, and J. D. Birkmeyer. 2006. Race and surgical mortality in the United States. Annals of Surgery 243(2):281-286.
Lurie, N. 2002. The public helath infrastructure: Rebuild or redesign? Health Affairs 21(6): 28-30.
Marmot, M., S. Friel, R. Bell, T. A. J. Houweling, and S. Taylor. 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet 372(9650):1661-1669.
Matthews, T. J., M. F. MacDorman, and Division of Vital Statistics. 2008. Infant mortality statistics from the 2005 period linked birth/infant death data set. National Vital Statistics Reports 57(2):1-32.
Mays, G. P., and S. A. Smith. 2011. Evidence links increases in public health spending to declines in preventable deaths. Health Affairs 30(8):1585-1893.
McGinnis, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. Journal of the American Medical Association 270(18):2007-2012.
McGinnis, J. M., J. A. Gootman, and V. I. Kraak, eds. 2006. Food Marketing to Children and Youth: Threat or Opportunity. Washington, DC: The National Academies Press.
Medicaid Redesign Team. 2011. Basic Benefit Review Work Group. Final Recommendations on Redesigning the Medicaid Program. New York: New York State Department of Health.
Miller, G., C. Roehrig, P. Hughes-Cromwick, and C. Lake. 2008. Quantifying national spending on wellness and prevention. In Beyond Health Insurance: Public Policy to Improve Health Advances in Health Economics and Health Services Research. Vol. 19: 1-24.
Mokdad, A. H., J. S. Marks, D. F. Stroup, and J. L. Gerberding. 2004. Actual causes of death in the United States, 2000. Journal of the American Medical Association 291(10):1238-1245.
Muntaner, C., C. Borrell, E. Ng, H. Chung, A. Espelt, M. Rodriguez-Sanz, J. Benach, and P. O’Campo. 2011. Politics, welfare regimes, and population health: Controversies and evidence. Sociology of Health & Illness 33(6):946-964.
Murray, C. J., and J. Frenk. 2010. Ranking 37th—measuring the performance of the U.S. health care system. New England Journal of Medicine 362(2):98-99.
NACCHO (National Association of County and City Health Officials). 2011. Local Health Department Job Losses and Program Cuts: Findings from January 2011 Survey and 2010 National Profile Study (Research Brief). Washington, DC: NACCHO.
NACCHO. 2012. Local Health Department Job Losses and Program Cuts: Findings from January 2012 Survey. Washington, DC. NACCHO.
NRC (National Research Council). 2011. International Differences in Mortality at Older Ages: Dimensions and Sources. Washington, DC: The National Academies Press.
NRC and IOM. 2012. Panel on Understanding International Health Differences in High-Income Countries: Patterns, Puzzles, Paradoxes, and Public Health Opportunities. http://www7.nationalacademies.org/cpop/Intl%20Health%20Differences%20Project.html (January 3, 2012).
OECD (Organisation for Economic Co-operation and Development). 2009. Disparities in Health Expenditures Across OECD Countries: Why Does the United States Spend so Much More Than Other Countries? A written statement to Senate Special Committee on Aging. Washington, DC: OECD.
OECD. 2010a. Health Care Systems: Getting More Value for Money, OECD Economics Department Policy Notes No. 2. Paris, France: OECD.
OECD. 2010b. OECD health data 2010: How does the United States compare? In OECD Health Data 2010: Statistics and Indicators. Paris, France: OECD.
OECD. 2011. Child outcomes. CO1.1: Infant mortality. In OECD Family Database. Paris, France: OECD.
OECD. 2012. Members and Partners. http://www.oecd.org/pages/0,3417,en_36734052_36761800_1_1_1_1_1,00.html (March 18, 2012).
Ohri-Vachaspati, P., L. Leviton, P. Bors, L. Brennan, R.C. Brownson, S. Strunk. 2012. Strategies proposed by Healthy Kids, Healthy Communities partnerships to prevent childhood obesity. Preventing Chronic Disease 9:100292, http://www.cdc.gov/pcd/-issues/2012/10_0292.htm (March 30, 2012).
Olsha nsky, S. J., D. J. Passaro, R. C. Hershow, J. Layden, B. A. Carnes, J. Brody, L. Hayflick, R. N. Butler, D. B. Allison, and D. S. Ludwig. 2005. A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine 352(11):1138-1145.
Oregon Health Authority. 2011. Successes of Tobacco Control in Oregon: The 2009-2011 Tobacco Prevention and Education Program Report. Portland, OR: Oregon Health Authority.
Orszag, P. 2010. A Health Care Plan for Colleges. The New York Times. http://www.nytimes.com/2010/09/19/opinion/19orszag.html?_r=2&ref=peter_orszag&pag (September 18).
Pierce, J. P., K. Messer, M. M. White, D. W. Cowling, and D. P. Thomas. 2011. Prevalence of heavy smoking in California and the United States, 1965-2007. The Journal of the American Medical Association 305(11):1106-1112.
Poullier, J., P. Hernandez, K. Kawabata, and W. D. Savedoff. 2002. Patterns of Global Health Expenditures: Results for 191 Countries. EIP/HFS/FAR Discussion Paper No. 51. Geneva, Switzerland: WHO.
Schoen, C., J. L. Nicholson, and S. Rustgi. 2009. Paying the Price: How Health Insurance Premiums are Eating Up Middle-Class Incomes—State Health Insurance Premium Trends and the Potential of National Reform. New York: The Commonwealth Fund.
Smeeding, T. 2005. Government Programs and Social Outcomes: The United States in Comparative Perspective. Luxembourg: Luxembourg Income Study.
Soni, A. 2011. Top 10 Most Costly Conditions among Men and Women, 2008: Estimates for the U.S. Civilian Noninstitutionalized Adult Population, Age 18 and Older. Statistical Brief # 331. Washington, DC: HHS.
Sturm, R. 2002. The effects of obesity, smoking, and drinking on medical problems and costs. Health Affairs 21(2):245-253.
Tauras, J. A., F. J. Chaloupka, M. C. Farrelly, G. A. Giovino, M. Wakefield, L. D. Johnston, P. M. O’Malley, D. D. Kloska, and T. F. Pechacek. 2005. State tobacco control spending and youth smoking. American Journal of Public Health 95(2):338-334.
TFAH (Trust for America’s Health). 2012. A State-by-State Look at Public Health Funding and Key Health Facts. Washington, DC: TFAH.
Thorpe, K. E., C. S. Florence, D. H. Howard, and P. Joski. 2004a. The impact of obesity on rising medical spending. Health Affairs (Suppl Web Exclusives):480-486.
Thorpe, K. E., C. S. Florence, and P. Joski. 2004b. Which medical conditions account for the rise in medical care spending? Health Affairs Web Exclusive:437-445, http://content.healthaffairs.org/cgi/content/abstract/hlthaff.w4.437v1 (August 25, 2004).
Thorpe, K. E., L. L. Ogden, and K. Galactionova. 2010. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Affairs 29(4):1-7.
TRB (Transportation Research Board) and IOM. 2005. Does the Built Environment Influence Physical Activity? Examining the Evidence—Special Report 282. Washington, DC: The National Academies Press.
Truffer, C. J., S. Keehan, S. Smith, J. Cylus, A. Sisko, and J. A. Poisal. 2010. Health spending projections through 2019. The recession’s impact continues. Health Affairs 29(3):522-529.
Turnock, B. J. 2009. Public Health: What It Is and How It Works. Sudbury, MA: Jones and Bartlett Publishers.
UN (United Nations), Department of Economic and Social Affairs, Population Division. 2009. World Population Prospects: The 2008 Revision, Highlights. Working Paper No. ESA/P/WP.210. Geneva, Switzerland: UN.
Ver Ploeg, M., V. Breneman, T. Farrigan, K. Hamrick, D. Hopkins, P. Kaufman, B. H. Lin, M. Nord, T. Smith, R. Williams, K. Kinnson, C. Olander, A. Singh, and E. Tuckermanty. 2009. Access to Affordable Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences—Report to Congress. Washington, DC: Department of Agriculture.
Wahdan, M. H. 1996. The epidemiological transition. Eastern Mediterranean Health Journal 2(1):8-20.
Wang, P. S., A. Beck, P. Berglund, J. A. Leutzinger, N. Pronk, D. Richling, T. W. Schenk, G. Simon, P. Stang, T. B. Ustun, and R. C. Kessler. 2003. Chronic medical conditions and work performance in the health and work performance questionnaire calibration surveys. Journal of Occupational and Environmental Medicine 45(12):1303-1311.
Weintraub, W. S., S. R. Daniels, L. E. Burke, B. A. Franklin, D. C. Goff, L. L. Hayman, D. Lloyd-Jones, D. K. Pandey, E. J. Sanchez, A. P. Schram, and L. P. Whitsel. 2011. Value of primordial and primary prevention for cardiovascular disease. Circulation 124(8):967-990.
WHO (World Health Organization). 2010. Adelaide Statement on Health in All Policies. Geneva, Switzerland: WHO.
WHO. 2012a. Trade, Foreign Policy, Diplomacy, and Health: Health Transition. http://www.who.int/trade/glossary/story050/en/index.html (January 30, 2012).
WHO. 2012b. WHO NCD Surveillance Strategy. http://www.who.int/ncd_surveillance/strategy/en/index.html (March 24, 2012).
WHO Commission on Social Determinants of Health. 2008. Closing the Gap in a Generation. Geneva, Switzerland: WHO.
Wilcox, B. L., D. Kunkel, J. Cantor, P. Dowrick, S. Linn, and E. Palmer. 2004. Report of the APA Task Force on Advertising and Children. Washington, DC: American Psychological Association.
Wilkinson, R., and M. Marmot, eds. 2003. Social Determinants of Health: The Solid Facts. 2 ed. Copenhagen, Denmark: WHO, Regional Office for Europe.
Woolf, S. H., R. E. Johnson, R. L. Phillips, Jr., and M. Philipsen. 2007. Giving everyone the health of the educated: An examination of whether social change would save more lives than medical advances. American Journal of Public Health 97(4):679-683.
World Economic Forum. 2008. Working Towards Wellness: The Business Rationale. Geneva, Switzerland: World Economic Forum.
































