Reforming Public Health
and Its Financing
The strategies necessary to reach the national health target recommended by the committee in Chapter 11 depend on the implementation of population-based prevention and wellness initiatives. However, the vast majority of government health spending in the United States is for individual illness care and treatment for disease; a far smaller and inadequate proportion is provided, ineffectively, to support governmental public health’s efforts to improve population health.2 The current financing system for health in the United States is profoundly misaligned. The nation is not buying what is needed to produce the health outcomes that it seeks.3 In this chapter, the committee examines the financing misalignment in more detail, focusing on the public health department capabilities that are needed for all or most programs (for example, in communication, information systems, and policy
______________
1Recommendation 1: The secretary of health and human services should adopt an interim explicit life expectancy target, establish data systems for a permanent health-adjusted life expectancy target, and establish a specific per capita health expenditure target to be achieved by 2030. Reaching these targets should engage all health system stakeholders in actions intended to achieve parity with averages among comparable nations on healthy life expectancy and per capita health expenditures.
2As noted in Chapter 1, the committee has previously described a multisectoral health system that goes beyond governmental public health and targets a wide array of determinants of health (IOM, 2011a,b). But in the context of the current report, the committee found it challenging and nearly impossible to attempt a broader examination of the funding aspects of the system as a whole—both because of its great complexity and because of the extreme scarcity of data on system contributors other than governmental public health.
3As noted in Chapter 1, this refers only to spending that is specifically for health, not to spending on education, housing, or other social determinants of health.
analysis) and reviewing limitations imposed on the current system that interfere with the efficient use of existing resources.
The national health target recommended in Chapter 1 is an ambitious one, but the committee believes that it is achievable because much of the current morbidity and mortality is preventable—half the deaths in the United States and more than half the morbidity (perhaps three-fourths) (CDC, 2005; Danaei et al., 2009; IOM, 2008; Woolf et al., 2007, 2010). The cost of the preventable disease burden makes it crucially important to seek, find, and implement solutions. According to federal estimates, “one year’s worth of injuries has an estimated lifetime cost of $406 billion in medical expenses and lost productivity” (Foreman, 2009). In 2004, total Medicaid smoking-attributable expenditures amounted to $22 billion (Armour et al., 2009).
The core mission and unique competence of the governmental public health agencies (public health departments) are informed by their focus on wellness and prevention rather than illness care and treatment. Public health departments are statutorily charged with protecting and promoting population health, and they are uniquely positioned and qualified (through the science, tools, and skills of public health, including epidemiology and health planning) to take or support evidence-based action on many of the risk factors that lead to poor health. Although some clinical care interventions can help to prevent a disease process in an individual, they cannot be used efficiently throughout a population to address pressing community health challenges. Those challenges, such as growing rates of obesity and diabetes, increase health care costs, diminish American productivity and competitiveness, and probably limit the opportunities available to the next generation of Americans because of increasingly poor health. Taking action as early and at the level of population, long before diabetes is diagnosed in one obese person, or chronic bronchitis4 is diagnosed in one smoker, is the most efficient and effective route to disease prevention.
The nation needs to rely on public health departments to lead the effort to reduce the burden of preventable morbidity and mortality. It is important to consider why public health has not already done more in this regard. A large part of the answer is that only a small proportion of current public health financing targets the major causes of preventable morbidity and mortality in the 21st century. Partly as a result of the historic successes of public health against infectious diseases, today’s preventable disease burden is primarily the result of chronic disease, injury, and upstream social determinants. Although it is essential to ensure that funding continues to sustain hard-won public health achievements in maternal and child health, environmental sanitation and hygiene, and the prevention of infectious diseases, public health investments are needed to address the full array of high-
______________
4A precursor of and part of chronic obstructive pulmonary disease.
priority population health challenges, beginning with those most responsible for today’s and tomorrow’s preventable burden of disease.
The Centers for Disease Control and Prevention (CDC) has analyzed its spending on the preventable burden of disease (Curry et al., 2006) and has found, for example, that although cardiovascular disease was the leading disease category, only 1.9 percent of CDC’s budget (allocated by Congress by specific categories) was spent on it. Table 2-1 illustrates the most recently available information on the misalignment between spending and disease burden.
Although there has been some improvement in funding for chronic disease prevention, there remain large categories of relative underfunding (for example, for injuries, environmental health, and mental health). Given Congress’s budget compromise that removed $5 billion from the prevention and public health fund (Haberkorn, 2012) and the further reductions expected in authorizations, there is little hope that the funding problems will be resolved soon. An update of the work of Curry and colleagues would be an important contribution to ascertaining the extent to which public health funding (in CDC and preferably at all levels of government) is aligned with population health needs.
A survey of 17 of the largest metropolitan health departments in the United States conducted by Georgeson and colleagues (2005) found that although “[c]hronic diseases account for 70% of all deaths nationwide on average,… the health departments surveyed allocated an average of 1.85% of their budgets to chronic disease” (2005, p. 183). Frieden and colleagues found “a gross mismatch between funding levels for different categories of diseases and the number of premature deaths caused by those diseases”
TABLE 2-1 Funding Versus Preventable Burden of Disease, Ranked by Medical Cost
| Disease Category | Rank (by cost |
Fraction of CDC 2003 Budget, % | Amount in CDC 2003 Budget, $ |
Cardiovascular, circulatory |
1 | 1.89 | ~81.5 million |
Cancer |
2 | 9.88 | ~426.7 million |
Injury |
3 | 4.95 | ~213.9 million |
Mental health |
4 | 0.19 | ~8.4 million |
Endocrine and metabolic disorders (such as diabetes) |
5 | 4.77 | ~206.3 million |
Disability |
6 | 3.04 | ~131.2 million |
Chronic lung disease |
7 | 1.50 | ~64.8 million |
Infectious disease |
8 | 70.48 | ~3.0 billion |
aMedical cost (see Cohen and Krauss, 2003).
SOURCE: 1997 and 2003 budget data from Curry et al., 2006.
(2008, p. 974) in New York City. For example, emergency preparedness, tuberculosis, HIV, sexually transmitted infections, and vaccine-preventable diseases received various levels of federal funding, and diabetes, heart disease, cancer, and tobacco control received no federal funding. The former group caused no or few deaths, whereas heart disease, cancer, and tobacco use were responsible for high numbers of deaths. Frieden and colleagues concluded that although maintaining funding for communicable disease control is crucial, “federal, state and local governments should also provide the funds necessary to implement effective programmes to prevent and control chronic diseases” (2008, p. 974).
The failure of public health to tackle the health issues that are resulting in the relatively poor U.S. health rankings among comparable nations is primarily a financing failure. The United States gets the health outcomes that it chooses to pay for. The committee does not believe that the answer is simply to transfer resources from traditional public health domains to new programs. Although public health engagement in contemporary factors that contribute to health is essential, it should not occur at the expense of hard-won gains, such as victories over communicable diseases. Rather, the solution is more nuanced, involving a combination of efficiencies, financing reform and, ultimately, more resources. Before discussing those issues, however, an important next question to address is whether there is evidence that public health could address the current challenges successfully if adequate resources were available.
THE IMPACT OF PUBLIC HEALTH ACTION
The history of public health attests to its ability to achieve major improvements in population health. Historically, action on the leading causes of death and disability in the population has involved public health departments at all levels working in collaboration with researchers, communities, clinical care providers, and other partners to collect data, plan and implement programs, advocate for policy change, enforce laws, and ensure the delivery of services, such as immunizations and occupational safety. The public health infrastructure, including government agencies from CDC and the Food and Drug Administration to the local public health department, works to promote and protect the population against routine threats and to prepare against exceptional ones, such as bioterrorism and pandemics. As noted in earlier Institute of Medicine reports (IOM, 1988, 2003), state and local public health departments play special roles in ensuring that communities receive key public health services.
The power of public health action is evident in its record of successful interventions, including public policy, that have achieved change in health risks and health outcomes. Examples previously discussed in the committee’s
report on law and policy (IOM, 2011a) include the contributions of sanitation and universal childhood vaccination to improving child health and life expectancy; changes in social norms related to tobacco use and the decline in smoking rates; the effects of seatbelt, child restraint, and blood alcohol laws on motor vehicle injuries and fatalities; and the effect of fluoridation of drinking water on rates of tooth decay.5 In many cases, a lack of funding has resulted in insufficiently robust strategies to protect the health of the population and has led to considerable human and economic losses, some of which are described below.
The committee was unable to find a comprehensive and detailed assessment of public health funding and the effects of fluctuations in it over the last few decades. But it did find evidence of the historical instability of public health funding and of the absence of a long-term commitment from Congress and state policymakers to sustain it. In their review of the history of public health policy and funding, Fee and Brown (2002) and Frist (2002) found it filled with ups and downs—fluctuations that reflect major health threats of the moment, political winds, and economic realities. The broader context of government finance, however, is also one of competing priorities, frequent budget deficits, and currently, a serious economic crisis. Sessions, in Appendix D, summarizes several of the social and political factors that have contributed to the government deficits that make it impossible to ensure adequate funding of public health, including globalization and increased competition for American business, political polarization, and the increasing economic and political influence of corporations. In the 1970s and 1980s, for example, public health suffered major cuts whose consequences were seen in part in an inability to mount an effective comprehensive response to the HIV/AIDS epidemic. Fee and Brown concluded that “we have not learned the lessons of our public health history. We continue to mobilize episodically in response to particular threats and then let our interest lapse when the immediate crisis seems to be over” (2002, pp. 41-42).
The defunding of public health tuberculosis control programs in the 1980s led to a resurgence of tuberculosis in 1985-1992 and cost New York City alone over $1 billion in 1991 dollars for efforts to control multiple-drug-resistant tuberculosis (Frieden et al., 1995; U.S. Congress, Office of Technology Assessment, 1993).6 Another example is found in the history of
______________
5Additional examples include safer work environments due to changes in occupational safety, the decline in cardiovascular disease rates (owing to interventions on smoking, blood pressure, and cholesterol), maternal and infant health, the decrease in cervical cancer deaths due to screening, and the decrease in lead poisoning due to the removal of lead from paint and gasoline.
6The example of tuberculosis (TB) also shows inefficiencies in public health side, such as needless TB screening for schools, and directly observed therapy for all cases, among others.
measles vaccination. In the decade or two after a measles vaccine was first licensed in 1963, funding for measles immunization became a function of the measles rate—as disease rates dropped, funding was decreased on the false assumption that the work was completed (Orenstein, 2006). Even as funding of measles vaccination stabilized and vaccination rates increased, access to vaccine services became the next challenge. A major measles epidemic in 1989-1991 became a rallying point for ensuring that adequate funding was available both to provide a higher level of first-dose coverage and to provide a second dose (in addition to policies requiring a second dose of measles vaccine before school entry) (Orenstein, 2006). Researchers have assessed the likely impact of funding cuts in specific areas of public health, such as vectorborne disease control and other infectious and chronic disease control activities, and concluded that inadequate funding leaves public health departments ill equipped to prevent and control disease (LaBeaud and Aksoy, 2010; Meyer and Weiselberg, 2009).
Perhaps one of the starkest examples of the association between financing and public health success is the national experience with tobacco control, one of the most dramatic successes—and failures—of public health. In 2004, CDC published a report on funding for tobacco control activities and found that support for this fundamental public health action was meager: national spending on tobacco control averaged $1.22 per person, less than one-fourth of CDC’s recommended minimum of $5.98 (CDC, 2004). Multiplying the nearly $6 per capita by the current population of the United States, about 311.6 million people, even without translating it into 2011 dollars, yields about $1.9 billion. That amount pales in light of the fact that tobacco use costs the United States $96 billion a year in direct medical expenses and $97 billion in lost productivity and is the largest preventable cause of death and disease (CDC, 2011b). Although the relationship between spending on tobacco control and smoking rates is complex—many factors are at work—there is no doubt that implementing multifaceted prevention efforts, as recommended by the U.S. Task Force on Community Preventive Services, requires adequate and sustained funding.
There is sufficient evidence that when public health is adequately funded, it is capable of protecting and improving population health (Binder et al., 1999; CDC, 1999; Handler and Turnock, 1996; IOM, 2003; Mays et al., 2004). To make progress in improving population health, the nation’s health system needs to maximize the efficiency and effectiveness of the resources that are available for public health and recognize that the scope of the task is such that more resources will be needed. The remainder of this chapter will focus on the first of those two actions in the context of what is required for a strong public health infrastructure.
DYSFUNCTION OF THE CURRENT PUBLIC
HEALTH FUNDING SYSTEM
The U.S. public health financing structure is broken. Well-financed health departments compete more effectively for public health financing. Many of the health departments in the poorest communities and communities that have the poorest health outcomes are among the least-well-funded (Honoré and Schlechte, 2007; Mays and Smith, 2009; Meyer and Weiselberg, 2009; Rehkopf and Adler, 2011; TFAH, 2011).
Public health funding comes from separate appropriation processes at the federal, state, and local levels (Novick et al., 2008). There is little coordination among funders regarding the services and activities that are funded, and each funder has its own rules of accounting, performance, monitoring, and evaluation (Mays and Smith, 2009; Mays et al., 2004; Salinsky, 2010; Salinsky and Gursky, 2006). Little or no funding is available to advance the science base of public health service delivery or interventions (Brownson et al., 2009; Glasgow et al., 2003).
The organization of governmental public health has developed in ways that reflect funder dictates, the flows of money, tightly compartmentalized programmatic categories, and the skill of public health leaders in “braiding” together disparate funding streams and finding new funding sources more closely than the needs of localities, including priorities based on communities’ disease burdens, interests, and capabilities.
Public health funding is a complex patchwork of funding streams, purposes, and funding mechanisms. Figure 2-1 and Appendix E illustrate public health funding in the United States; the structural issues are discussed in this chapter, and the specific financial aspects in Chapter 4.
The committee focuses below on two key consequences of the current funding system dysfunction that are particularly problematic because they occur in combination:
• Compartmentalized inflexible funding, often competitive, which leaves many health departments without financing for key priorities or for needed cross-cutting capabilities (such as information systems and policy analysis).
• Uncoordinated, usually discretionary funding from different levels of government with different rules for use. From a public health financing standpoint, there is no overall point of accountability and no agreement on or definition of a minimum package of services that all funders commit to ensuring in each state and locality.
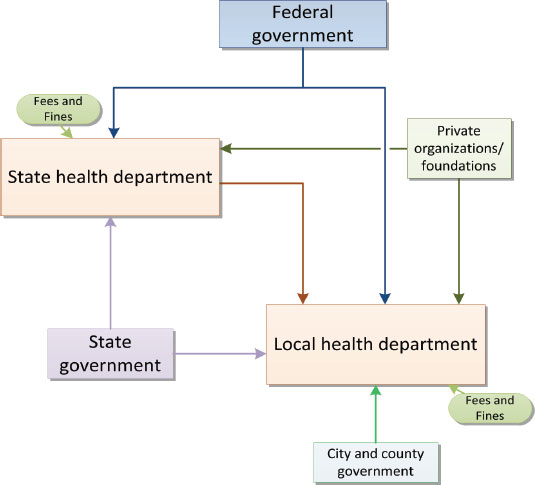
FIGURE 2-1 Public health funding flows.
NOTE: This diagram is a high-level, generalized view but illustrates the major and minor sources and types of revenue that state and local health departments may receive. The federal government disburses funds to state health departments through multiple agencies (such as CDC and the Health Resources and Services Administration) and avenues, including block grants, programmatic grants, and competitive grants, for instance, Title V/Maternal Child Health, Title X/Family Planning, Public Health Emergency Preparedness/Assistant Secretary for Preparedness and Response funds, and the Preventive Health and Health Services Block Grant. The federal government also disburses funds directly to local health departments—typically larger, urban health departments, for example, Ryan White dollars to highly affected HIV/AIDS jurisdictions—or rural health departments—for example, rural health grants to support practice-based research. State health departments are also supported by user fines and fees and by funds from state government. State funds vary widely by state but typically take the form of discretionary or general funds, mandated spending in programmatic areas, or dedicated revenue, for example, from a state tax on cigarettes. Many of the funds are sent on to local health departments as “pass-through” funds from private organizations or federal programs; funds are also often sent in the
Compartmentalized, Inflexible Funding
A great deal of the funding received by public health departments is inflexible, and this precludes strategic alignment of funding from different sources and use of funds to establish or strengthen communication capabilities, information systems, and other elements that are needed in all or most programs (Salinsky and Gursky, 2006). The lack of flexibility is due in large part to the nature of much of public health funding—categorical, often competitive, funds that recipients must use for specified purposes and in prescribed fashions.
The federal government provides funding to states and local governments through two congressionally authorized approaches: (1) categorical grants, which cover a narrow array of eligible activities, and (2) block grants, which offer flexibility in the use of funds (Canada, 2002). In practice, categorical grants are the most widely used approach because Congress views block grants as lacking built-in accountability (Committee on Inspection and Evaluation, 1996). Block grants, for example, are not program-specific, lack oversight, and lack performance measures, all of which characteristics make them less attractive to Congress (OIG, 1995). However, one successful model of flexible funding streams is the Maternal and Child Health block grant. The primary purpose of categorical grants is to ensure that health departments allocate resources for specific activities and services. Categorical grants are thought to ensure recipient accountability to the federal government, to target federal money to defined national
![]()
form of “core” support, as funding for specific programs at the local level, and as reimbursement for services performed by the local health departments on behalf of state health departments. Some local health departments also receive funds from other state or local agencies, for example, in states where Medicaid, substance abuse services, or environmental health services are separate from state health departments. Local health departments receive a substantial amount of their funding from city or county (or multicounty) governments. In addition to fees and fines, local health departments may contract out for services to other local agencies or provide services for which they bill other groups. As discussed in the committee’s second report, on law and policy (IOM, 2011a), there is significant variation in organization (and hence funding) among states; therefore, all these mechanisms vary widely by jurisdiction, so the relative importance of each funding source also varies. Some, like private sources, are generally very small sources of revenue. (See Appendix E for a more detailed diagram and further discussion.)
objectives, and to facilitate “nationwide adoption of innovative programs” (OIG, 1995, p. 6). Beginning in the 1950s, public health financing decisions became more regionally based, and the federal government started to fund public health more regularly on the basis of emerging needs (such as the emergence of HIV and influenza) according to the priorities of Congress (Novick et al., 2008). Congress tends to prefer categorical funding because it allows tighter control. Advocacy groups and other supporters of categorical funding value the fact that it allows them “to concentrate their efforts on lobbying Congress rather than 50 state legislatures” (OIG, 1995, p. 5).
Block grants are available to be administered directly at the state and local levels and therefore reduce some of the burdens of federal funding (such as administrative costs) and shift decision making to the states (CDC, 2011a; Kennan, 2008; OIG, 1995). However, block grants are unstable and vulnerable to decreases in funding and to elimination as a result of fiscal changes or shifts in political will. The president, the Senate, or Congress can call for their removal from the annual budget in attempts to cut costs (Kennan, 2008). Because block grants encompass a large number of combined programs and therefore do not include the specific ways in which the funds will be spent, it is easier for lawmakers to propose cuts in them without constituents’ being able to attach a specific program to the reductions (Kennan, 2008). Funding of the Preventive Health and Health Services Block Grant has been stagnant or declining over the past two decades. It was funded at $87,047,000 in 1986, then had small increases until 1995 (topping off at $157,916,000), and has had small decreases in most years since then; 2010 funding was $102,034,000 (CDC, 2012b).
Categorical funding for public health has been championed by many in public health for its ability to protect resources by dedicating them to important public health issues that might otherwise lose funding. Disease-specific grants, for example, lead to the development of a constituency that would advocate for the dedicated funds if they came under threat. However, the rigidity of categorical funding often leads to the creation of what practitioners call programmatic “silos”—parallel activities and services that overlap, are duplicative and are inefficient (NACCHO, 2011b; Novick et al., 2008; OIG, 1995; PHI, 2010; Salinsky, 2012) and that reduce the ability to fund cross-cutting needs, such as information systems and communication or policy analysis capabilities (NACCHO, 2011b). Categorical funding may also limit the range of practice of public health departments; because categorical streams generally are not dedicated to the broader determinants of health, public health departments may not have funding to consider activities in this part of their purview (for example, gathering, analyzing, and disseminating information on transportation, housing, zoning, and other community factors that are known to be linked with health outcomes) (BARHII and PHLP, 2010).
Funding strategies comparable with federal categorical funding are often used by state and local governments and present similar challenges. For example, studies of two large metropolitan health departments found that local government’s categorical funding does not provide support for basic public health services or core capacities (PHANYC, 2002; PHIP Finance Committee, 2006). State categorical funding limits state and local health department flexibility to meet local needs and maximize impact and entails administrative burdens that require accountability as to how funds are spent and programs are structured rather than attempting to determine what outcomes and effects are achieved (LAO, 2010).
Uncoordinated, Fragmented Government Funding
Federal funds are the largest source of state health agency revenue (about 45 percent in FY 2009), about 60 percent of which goes to support local health departments and community-based organizations (ASTHO, 2011). In 2009, the remainder of funds came from state general funds (23 percent), other state funds (16 percent), fees and fines (7 percent), Medicaid and Medicare7 reimbursement (4 percent), and other sources (5 percent) (ASTHO, 2011).
Federal funding for public health originates in congressional appropriations to the Department of Health and Human Services (HHS) (authorized by the Public Health Act, the Social Security Act, and other legislation) and the U.S. Department of Agriculture (USDA) (for the Women, Infants, and Children). HHS agencies—largely CDC, the Health Resources and Services Administration (HRSA), and the Substance Abuse and Mental Health Services Administration—direct funds to states and selected localities. Funding is overseen by individual program offices, and there are often distinct requirements from each office for use and reporting. In addition to the federal funding for states’ use, some federal funds “pass through” states on their way to local public health departments.
At the local level funding is similarly complex. The National Association of County and City Health Officials (NACCHO) 2010 Profile of Local Health Departments estimates that the largest proportion of local public health department revenue (26 percent) comes from local government, 21 percent comes from state direct funding, and 14 percent from federal pass-through8 funds. The remaining 39 percent is made up of federal direct funding, Medicaid and Medicare reimbursement, fees, and other sources (NACCHO, 2011a). The NACCHO Profile report also found that 40 per-
______________
7Medicare reimbursement of health departments that operate nursing homes.
8Federal pass-through funding refers to funds that come from the federal agencies to the state health department and are then transferred to the local level.
cent of local health departments have difficulty in distinguishing between state direct and federal pass-through funding.
The fragmented funding process hinders effective integration and coordination at the local level. As a consequence, some of the work of local and even state health departments is seemingly the result of an accretion of piecemeal activities that have taken place over the last two to three decades with inadequate attention to how the components fit together or whether they are optimized to meet the needs of the community. One state’s report on its local health departments concluded that “[w]here the funding comes from significantly influences health department functions and focus” (New Jersey Department of Health and Senior Services, 2008, p. 5). CDC’s organization also shows a historical proliferation of parallel programs that often have little interaction, integration, or coordination. A lack of coordination characterizes funding by different HHS agencies, such as CDC and HRSA, and funding by the Department of Homeland Security (Boufford and Lee, 2001; OIG, 1999; Salinsky and Gursky, 2006).
One example of suboptimal coordination occurs when state and local health departments receive federal funding for overlapping purposes or without adequate coordination (for example, the CDC Racial and Ethnic Approaches to Community Health program and the Community Transformation Grants program). A solution lies in enhancing collaboration between state and local health departments, perhaps by using existing organizations, that could lead to better coordination, greater efficiency, and taking advantage of economies of scale. The coordination and collaboration that occurred at the peak of bioterrorism funding offer some useful models.
Given the patchwork quilt of inadequate funding sources, public health departments find themselves trying to mesh federal, state, and local funding streams to cover their needs. For example, a health department may receive state discretionary funds, state consolidated and contract funds, fee and permit funds, general funds, Medicaid funds, and others, and each of those funding streams may have multiple sources (for example, different types of fees). The use of varied funds with varied requirements makes it difficult to manage a budget efficiently, because a health department is actually managing several hundred budgets rather than one overarching one. Changes in the funding practices of federal funders are needed to enable more flexible, rational, and efficient use of resources.
Recommendation 2: To ensure better use of funds needed to support the functioning of public health departments, the committee recommends that
(a) The Department of Health and Human Services (and other departments or agencies as appropriate) enable greater state and local flexibility in the use of grant funds to achieve state and local population health goals.
(b) Congress adopt legislative changes, where necessary, to allow the Department of Health and Human Services and other agencies, such as the U.S. Department of Agriculture, the necessary funding authorities to provide that flexibility.
(c) Federal agencies design and implement funding opportunities in ways that incentivize coordination among public health system stakeholders.
Governmental public health has not clearly articulated in a unified voice what society should be investing in and why, and this has added to the rise of a patchwork and inadequate funding system. There is no agreement among jurisdictions or between policymakers about what capabilities and programs make up the basic level of services all people in the United States should have the right to expect from their health department. Only with such agreement can there be hope of using and integrating resources from disparate funders efficiently. A way forward is described below.
DEFINING THE MINIMUM PACKAGE OF
PUBLIC HEALTH SERVICES
The Three Core Public Health Functions (of assessment, assurance, and policy development) and the 10 Essential Public Health Services9 provide a well-known framework for categorizing activities of state and local health departments. They have been used to communicate with the public and with policymakers, and they form the basis of accreditation and other performance measurement and quality improvement efforts (such as those embodied in the National Public Health Performance Standards Program). Although they are useful for those purposes, they were designed as a framework for categorizing all possible health department activities, so they have not proved useful for planning and setting priorities for the use of limited public health funding. In 2005, NACCHO published a consensus operational definition of a local health department, which was built on the foundation of the Essential Public Health Services. The rationale behind the operational definition was that “everyone, no matter where they live,
______________
9The 10 Essential Public Health Services are: (1) Monitor health status to identify and solve community health problems; (2) Diagnose and investigate health problems and health hazards in the community; (3) Inform, educate, and empower people about health issues; (4) Mobilize community partnerships and action to identify and solve health problems; (5) Develop policies and plans that support individual and community health efforts; (6) Enforce laws and regulations that protect health and ensure safety; (7) Link people to needed personal health services and assure the provision of healthcare when otherwise unavailable; (8) Assure competent public and personal health care workforce; (9) Evaluate effectiveness, accessibility, and quality of personal- and population-based health services; and (10) Research for new insights and innovative solutions to health problems (Public Health Functions Steering Committee, 1994).
should reasonably expect the local health department to meet certain standards” (NACCHO, 2005, p. 2). Although broad agreement was achieved among NACCHO member jurisdictions on the elements included in the report, it was never formally adopted or implemented. It was, however, used to inform the accreditation process developed by the Public Health Accreditation Board (NACCHO, 2012). Like the essential services and core functions, however, the operational definition, although useful for other purposes, does not lend itself directly to use in planning, priority-setting, and in demonstrating accountability. A framework is needed for use in a comprehensive system of tracking and managing revenues and expenditures and showing how spending is related to outcomes. The committee believes that a new framework needs to be built on the foundation provided by the essential services, the core functions, and the operational definition of a local public health department—to be used for the purposes just described.
A Minimum Package of Public Health Services
The committee believes that it is critical to develop a detailed description of a basic set of public health services that must be made available in all jurisdictions. The basic set must be specifically defined in a manner that allows cost estimation to be used as a basis for an accounting and management framework and compared among revenues, activities, and outcomes of different departments. The committee developed the concept of a minimum package of public health services, which includes the foundational capabilities and an array of basic programs no health department can be without (see Figure 2-2).
There are no standards for public health services that should be available in every community. In fact, there is considerable variation from one jurisdiction to another in the array of services defined as public health. In some places, mental health (not just preventive services) and Medicaid might be included; other jurisdictions provide no direct care at all. Public health funding is also discretionary, and critical programs are being cut across the
FIGURE 2-2 Components of the minimum package of public health services.
aOthers have described something roughly equivalent. See for example NACCHO’s 2011 profile of local health departments which provides the following list of “core public health activities that were to constitute the minimum services expected from the local units: vital statistics, sanitation, communicable disease control, maternal and child health, health education, and laboratory services” (NACCHO, 2011a, p. 2).
country (Kuehn, 2011; Kurland et al., 2004; NACCHO, 2011c; TFAH, 2008, 2009). There is little or no dedicated funding to support basic public health capabilities needed for all or most programs (Salinsky, 2010). Instead, financing for those capabilities is subsidized by specialized categorical program funding streams, as described below (Salinsky, 2010).
All organizations, from industry to nonprofits, require capabilities, such as human resources and financing, to function. In the public health literature, some capabilities, such as information systems, are sometimes described as infrastructure, but this is a term also used to describe facilities and utilities. Human resources and other administrative capabilities are not peculiar to public health. In public health practice, there are public health-specific “foundational capabilities” that are required to support programs. For example, common surveillance capabilities are critical whether one is focused on communicable diseases, such as sexually transmitted infections, or on chronic diseases. Policy and other analytic capabilities are essential whether one is working on strengthening immunization uptake or taking steps to reduce childhood injuries. Such capabilities are needed across programs, and in general many of the same human and other resources can be shared among programs. However, current funding methods typically do not support the financing of what the committee considers foundational capabilities that are needed to support effective and efficient programs. Agencies therefore often rely on categorical funding to build such capabilities, which accordingly become program-specific—such as communication for the purpose of preventing and reducing smoking—and are generally inconsistent among programs or public health departments. Furthermore, federal funders, such as CDC, do not have standards pertaining to foundational capabilities.
To develop the concept of the foundational public health capabilities, the committee reviewed pertinent literature and with the help of a consultant gathered information from conversations with 19 public health leaders on several capability domains (see, for example, Bernet, 2007; Brownson et al., 2009; Honoré and Costich, 2009; Mays et al., 2004; Meier et al., 2009; Smith et al., 2007; the commissioned paper by Salinsky, 2012, see Appendix C).10
______________
10The informal interviews focused on the level and type of funding available to support these areas and on the effects of inadequate funding on programmatic activities that depend on the foundational capabilities. The consensus was that most existing funding streams do not fund capabilities. Funders assume that basic capacity (such as for communication or information technology) is present and seldom allow grant funds to be used to establish or strengthen such capabilities. Public health leaders interviewed by Salinsky (see Appendix C) commented, for example, on the fact that categorical funding streams by their very nature do not generally encourage or support communication activities that extend across several program categories.
Some foundational public health capabilities identified by the committee are
• information systems and resources, including surveillance and epidemiology,
• health planning (including community health improvement planning),
• partnership development and community mobilization,
• policy development, analysis, and decision support,
• communication (including health literacy and cultural competence), and
• public health research, evaluation, and quality improvement.11
In most sectors and government agencies outside public health, costs for foundational capabilities are built into the price of products, but there is no corollary for that strategy in public health. In practice, funders of categorical programs often assume some level of existing capacity in information systems or partnership development and are generally unwilling to provide funding to develop or maintain such capabilities. In the rare cases in which funding is provided, it is limited to specific programs, for example, funding to develop communication capacity for tobacco control or surveillance for infectious diseases. As a result, public health departments have developed foundational capabilities unevenly, inefficiently, and incompletely. Where capabilities are present, they often reside within specific programs and do not support a department as a whole (Salinsky, 2012, see Appendix C).
If one were to use a tree as a metaphor for a public health department, foundational capabilities are a major component of the trunk and support the programs and activities represented by the branches and leaves. Ideally, financing will create a strong, sturdy trunk. However, the present public health funding scheme consists primarily of categorical grant mechanisms that underfund foundational capabilities and instead focus on the branches (the programs). Financially, the contemporary health department commonly looks like a tree with heavy branches and a spindly trunk—an unsustainable state.
At the federal level, CDC would ideally take the lead in defining and establishing funding mechanisms to support public health foundational capabilities. The CDC unit that is best positioned to provide expert guid-
______________
11Including review, synthesis, and adoption of evidence-based practices from existing research, performance measurement, evaluation and quality improvement, and participation in practice-based research to discover new and better public health strategies (see Brownson et al., 1999).
ance on developing and strengthening these capabilities is the Office for State, Tribal, Local, and Territorial Support (OSTLTS) (CDC, 2012a), but it lacks adequate funding to support foundational capability building in public health departments. Mechanisms to facilitate such funding could involve placing a tap on each funding stream that CDC allocates to states or localities or giving grantees more flexibility by allowing the use of 15 percent (or a similar proportion) of each grant to establish or enhance foundational capabilities most relevant to the grant, such as information systems infrastructure. This roughly resembles the budgetary item of “indirect costs,” which covers administrative expenses and other “overhead” costs. The National Public Health Improvement Initiative administered by the CDC OSTLTS also allocates resources specifically to improve broad-based public health infrastructure—including capacities for quality improvement, policy development, and analysis—and is not linked to categorical areas (CDC, 2010).
The foundational capabilities pertain to all basic program activities. Whether public health practitioners are working on chronic disease prevention or environmental health, communication capabilities are essential, and some of the same skills and tools are required, and information systems including the ability to conduct surveillance, are a crucial component that enables planning, measurement, and reporting. In addition to the examples of basic programs listed above, dedicated programs could be needed in areas such as healthcare-associated infections, food safety, and emergency preparedness. However, the committee did not provide a detailed discussion of the programs that should be part of the minimum package; rather, it believes that a more complete stakeholder discussion and development process are critical for the concept’s acceptance. There are areas of overlap between some programs that will need to be addressed (e.g., some underlying causes of chronic disease stem from environmental factors, and chronic disease prevention is usually part of comprehensive maternal and child health programs). A related matter is the need for an analysis of the funds required to support the basic programs and the minimum package as a whole. In Chapter 4, the committee makes a recommendation to that end.
Basic programs are activities that no well-run public health department can be without—some are supported by categorical funds, but many are not mandated by federal, state, or local law, and there are no dedicated funds to support them. Without specific enumeration, any given program activity may appear “optional” and thus easier to cut when budgets are tight. A definition of basic programs would clarify what every health department needs to make available (for example, tobacco control programs could never be considered optional). It also would inform funding decisions by all governments. High-level categories of basic programs might include
• Maternal and child health promotion.
• Injury control.
• Communicable disease control.
• Chronic disease prevention (including tobacco control).
• Environmental health.
• Mental health and substance abuse.
The committee envisions the use of a minimum package of public health services as the basis of a uniform system of tracking revenues and expenditures and of comparing investments with outcomes. (This approach is further described in Chapter 3.) The package could also be used as a component of performance measurement, quality assurance in public health, and public health accreditation. A public health department would be obliged to provide all the services in the package up to a uniform performance standard and additional activities and interventions that were based on needs of the community.
Recommendation 3: The public health agencies at all levels of government, the national public health professional associations, policymakers, and other stakeholders should endorse the need for a minimum package of public health services.
To provide support for the minimum package, the federal departments and agencies that fund state and local public health departments would take the steps described in Recommendation 2 earlier. HHS; USDA, which supports local Women, Infants, and Children Supplemental Nutrition Programs; the Environmental Protection Agency, which supports state air quality and other programs; and others could make administrative rule changes and procedural changes in the existing funding streams (such as contracts, grants, and cooperative agreements) to enable more flexible, rational, and efficient use of resources. In the context of “health in all policies” approaches, which the committee discussed in its report on law and policy (IOM, 2011a), similar strategies could be considered to enable other federal departments and agencies to make investments that are more explicitly oriented toward improving population health in addition to achieving their primary objectives, such as in transportation, education, or housing, for the respective departments.
Public health funding could also be structured in ways that emulate the Medicaid financing mechanism, which calls for sharing of responsibilities and cost between the federal and state (and in a few cases, local) levels of government. The federal government sets specific standards and requirements, but the states have additional discretionary authority that can be used to shape benefits in their jurisdictions. Federal agencies could also
encourage state and local matching by creating funding mechanisms and processes by which recipients can get substantial funding by demonstrating capacity, including resource matching or co-financing. Special consideration will be needed to facilitate equity among health departments, inasmuch as smaller jurisdictions may have less access to funds that could be offered as a match. In its report on law and policy, the committee discussed the need to consider collaboration, consolidation, and other types of arrangements that improve the capacity of smaller health departments, and the same idea applies to funding. Matching or co-financing by the federal, state, and local levels is further discussed in Chapter 4.
Public health leaders need the ability to tailor the scope and intensity of their activities to community needs, priorities, and values. However, the structure and administrative requirements associated with categorical funding streams limit that flexibility. Just as patient-centered medical care requires flexibility and an ability to adapt actions to needs and values, so public health requires flexibility to implement population-centered practice to meet the needs of a given community (Honoré et al., 2011). Public health departments need the ability to shift funds between categories, whether the existing categories or the foundational capabilities and basic program activities. It is important to emphasize that what the committee is calling for is not the allocation of funding unencumbered by requirements but the transformation of how funding is allocated to remove barriers to the reasonable, efficient, and accountable use of funds (for example, to permit the sharing of equipment or staff resources between programs).
Faced with competing responsibilities and different priorities among decisionmakers, many health departments have played a smaller role in policy development than they should have. That role needs to expand so that public health departments not only disseminate information about a community’s health and the factors that influence it, but develop the skills and knowledge needed to inform health-pertinent policymaking throughout different sectors (transportation, education, planning, and other elements of government) (Brooks et al., 2009; Honoré and Schlechte, 2007; Turnock et al., 1994). Public health departments could also expand their roles as conveners of relevant constituencies to promote action on high-priority health issues and as the definitive source of population health expertise in intersectoral collaborations (IOM, 2011b). As discussed at some length in the committee’s first and second reports, there are multiple opportunities in government alone to align some of the resources, policies, and activities of non-health agencies so as to achieve population health objectives while meeting primary objectives in education, transportation, criminal justice, or housing. Several current efforts to do so are described in the committee’s report on law and policy and in the National Prevention Council’s 2011 annual report.
USING FINANCING REFORM TO STRENGTHEN
21ST CENTURY PUBLIC HEALTH
Meeting the challenges that are endangering the health and economic competitiveness of the United States ultimately depends on the sufficiency of funding for new and necessary public health competences and programming. It is beyond the scope of this report to provide the entire blueprint for such a process (which would include steps described elsewhere, for example, nurturing public health leaders, developing workforce competences, and strengthening the quality of public health practice (Honoré and Scott, 2010; Honoré et al., 2011). However, the financing reforms recommended here are crucial for enabling the recommendations of the committee’s two previous reports (IOM, 2011a,b) and the roles that public health departments play in improving the health of populations as
• A source of knowledge and analysis on community and population health (part of the assessment function).
• A convener, coalition-builder, and mobilizing force to build health considerations into all aspects of community planning and action (part of the policy development function).
• A steward of the community’s health, assuring that policies and services needed for a healthy population are in place (part of the policy development function).
• A partner of the clinical care delivery system in developing information about effectiveness and appropriateness of service delivery (part of the assurance function).
Those roles of public health are not new, but the last item, referring to the relationship to clinical care, is an elaboration of work that public health departments have already undertaken to various degrees. This topic was introduced in the committee’s report For the Public’s Health: The Role of Measurement in Action and Accountability, and the discussion continues here. The last role has become more important and is a natural application of public health departments’ abilities. The committee recognizes, however, that considerable time and effort (training, planning, and so on) will be needed to enable public health departments to begin to perform all those roles effectively, and it acknowledges that various barriers will need to be addressed, including organizational culture, funding issues, questions of authority, and the potential for adversarial interactions.
As outlined in the committee’s report on measurement, transforming governmental public health departments requires greater and more granular data and information that can be used to implement the functions of assessment, policy development, and assurance. Key knowledge and analytic capabilities specific to public health professional training and background
must be focused sharply on assessing the health of populations. Information derived from assessment needs to be integrated with data gathered from other sources to develop a new understanding of associations and causality (IOM, 2011b; see Chapter 3 for further discussion). Public health professionals must turn knowledge into interventions that maximize health promoting conditions and curtail interventions that detract from a community’s health. Knowledge must be used to engage partners in influencing the actions and policies of private and public entities that are key to the health of communities (IOM, 2011a).
As discussed in the committee’s report on law and policy, changes in regulations and in formal and informal policies in the public and private sectors all can be powerful tools for population health improvement (IOM, 2011a). Policy development requires an understanding of the political and social environment of a community and the contributions of community groups and organizations for policies to be built in a manner that is locally acceptable. Ideally, policies will be developed on the basis of empirical knowledge or strong theory of what approaches and interventions will be most successful in promoting and protecting health. Health departments need to be knowledgeable about evidence-based interventions and about how to adapt them appropriately to the needs of local communities. Public health departments as knowledge organizations also need capacity and skill in communication and mobilization, for example, to facilitate the development, enactment, and implementation of health-related policies that lead to behavior-oriented change (smoking bans, excise taxes intended to curb risky behaviors, such as smoking and alcohol abuse) and to more broad-based “health in all policy” efforts (such as altering the built environment to make neighborhoods more accessible to pedestrians and cyclists).
THE RELATIONSHIP BETWEEN PUBLIC HEALTH AND
CLINICAL MEDICINE: A NEW PARTNERSHIP
The committee’s charge in this report is to “make recommendations for funding state and local public health systems that support the needs of the public after health care reform.” A central issue that the committee grappled with was its vision of the relationship between public health and the medical care delivery system in the context of health care reform (the implementation of the Affordable Care Act [ACA]12).
In examining what is needed to produce an effective partnership between public health and clinical care, the committee found that the relationship requires both better integration and better differentiation. The committee’s report on data and measurement (IOM, 2011b) recommended
______________
12Public Law 111-148; Public Law 111-152.
collaboration between the two sectors to draw on the data (such as indicators of a community’s health) and expertise of public health to improve aspects of clinical care that are relevant to population health outcomes and to familiarize the public with the meaning of high-value (evidence-based, efficient, appropriate) care, in the form of local performance reports on the appropriateness, quality, safety, and efficiency of clinical care services delivered in their community.13 Some health departments that serve small populations may never achieve local capacity, knowledge, and skills for collaborating with clinical care counterparts; in some states or territories, it may require a more centralized function, but governmental public health nevertheless needs to provide information to the medical care system and to the public it serves on the effectiveness and efficiency of its operation. Current examples of this sort of interaction or integration between the public health and clinical care systems include
• Reports of outlier rates of hospitalization for selected diseases.
• Use of procedures consistent with predicted prevalence of population need.
• Cancer and vaccine registries.
• Evidence-based guidelines.
• Health promotion and disease prevention for patients.
Health care reform, through the ACA, also provides an opportunity for health departments to reassess their need to provide clinical services directly to vulnerable populations in their communities. Debates over clinical care service delivery in public health departments have gone on for several decades. The 2003 IOM report on public health emphasized that “adequate population health cannot be achieved without making comprehensive and affordable health care available” to everyone (IOM, 2003, p. 12). Although the provision of clinical services by health departments has been in decline for many years (NACCHO, 2010), about half the local public health departments (NACCHO, 2011a) still provide a range of clinical services to uninsured and underinsured individuals and families through their clinics, through health department–operated community health centers and federally qualified health centers, and, less commonly, through health department–associated hospitals. In some departments, this activity accounts for the largest portion of the overall budget. In many localities, such a role is
______________
13Recommendation 5 of that report (IOM, 2011b): “The committee recommends that state and local public health agencies in each state collaborate with clinical care delivery systems to assure that the public has greater awareness of the appropriateness, quality, safety, and efficiency of clinical care services delivered in their state and community. Local performance reports about overuse, underuse, and misuse should be made available for selected interventions (including preventive and diagnostic tests, procedures, and treatment).”
viewed by the community and its decision makers as a central role of public health, and providing critical services for vulnerable populations in the community can be beneficial for local political support. In addition, some public health departments have been able to defray overall departmental overhead expenses or possibly even cross-subsidize (pay for) key population-based services through reimbursement or fees collected for clinical care services, although the evidence of this is sparse (Elster et al. 2003, p. 186;14 OIG, 1999; Slifkin et al., 2001).
The ACA, signed into law in March 2010, includes provisions to expand health care coverage, and improve quality in the health care delivery system (by changing incentives to support quality, system integration, administrative standardization, and coordinated care) (KFF, 2011). ACA provisions are intended to be phased in over a period of several years, with the final provision of the law becoming effective in 2020. It is likely to have far-reaching ramifications for safety net providers, such as public health departments. Assuming full adoption, it is estimated that the ACA will expand health insurance coverage for as many as 32 million people (KFF, 2011), many through the mechanism of support for lower-income individuals. As the implementation of the ACA advances, the committee believes, other public and private providers will have increased capacity to provide care for formerly uninsured populations for whom governmental public health has served as a safety net provider.
There are, of course, several caveats. At the time of this writing, several provisions of the ACA face congressional challenges on political and fiscal grounds and challenges from 26 states’ attorneys general (NCSL, 2012). The outcome of those challenges may affect the number of people who ultimately gain insurance. Even with full implementation of the ACA, 23 million people will remain uninsured (AcademyHealth, 2011; Hall, 2011; Herrick, 2011). In addition, in the short term, full implementation of the ACA will increase demand for primary care, and safety net capacity may be strained.
Some issues may make it more appropriate for public health departments to provide specific kinds of clinical services directly, for example, specialized programs that have a population health component, such as programs related to control of tuberculosis or sexually transmitted diseases,
______________
14“Because public health departments do not have legally enforceable duties to individuals, they also have greater latitude to commingle funds and engage in cross-subsidization practices to keep their activities afloat. Thus, for example, a public health agency may pool revenues from grants, contracts, patient fees, and third party payments (most typically Medicaid) to support the provision of subsidized personal health-care activities for uninsured people. In this way, shortages in one area can be compensated for by budgetary reallocations of dollars where not prohibited by law. Because grant and contract funding for public health activities tends to be modest and because a large proportion of the patient population is poor, third party revenues, especially Medicaid, take on crucial importance” (Elster et al., 2003, p. 186).
and specialized services delivered in community settings, such as nurse home visiting or community worker health promotion activities. In this context, the ACA provides an important opportunity for health departments to forge new and stronger partnerships with the health care delivery system.
The prominence of the focus on clinical care delivery was viewed by the committee as detracting from the ability of public health to take on other activities that are important for its mission and that others are less able to accomplish. However, the important and continued need for safety net services in many communities will require coordination between public health departments and public and private clinical care providers.15
Recommendation 4: The committee recommends that as clinical care provision in a community no longer requires financing by public health departments, public health departments should work with other public and private providers to develop adequate alternative capacity16 in a community's clinical care delivery system.
FINANCING AND REFASHIONING PUBLIC
HEALTH DEPARTMENTS
Reforms in public health financing—not levels of funding but how funds are disbursed and used—also require changes in public health department organization. The organization of public health departments is critical for their successful functioning. It was not in the committee’s charge to explore organizational issues, but it notes that in a resource-constrained environment, efficiency is obligatory, not only for financial health but for the accountability that the committee outlined in its previous reports.
Many public health departments are too small to possess the foundational capabilities and to deliver the package of public health services needed for them to be fully operational and meet minimum performance measures or gain accreditation.17 Moreover, state–local coordination will be needed in some spheres, such as information technology (this has been discussed
______________
15The committee notes that in some jurisdictions, the public health department operates federally qualified health centers or community health centers.
16Adequate capacity refers not merely to the ability to provide services of similar breadth, quality and accessibility (e.g., cultural competence), but in the context of providing care to the overall community and not on a patient-by-patient basis.
17As the committee has noted previously, 33 percent of local public health departments are staffed by fewer than 10 full-time employees, and 63 percent of 2,565 health departments surveyed in 2010 serve populations of fewer than 50,000 people (NACCHO, 2011a). Santerre (2009) found that the “minimum efficient scale” (the level of population associated with minimum health department efficiency) for a local health department occurs at a population of about 100,000, but 77 percent of local health departments, which serve about 18 percent of the total U.S. population, serve smaller populations.
extensively in the literature on immunization registries, surveillance systems, and other information system components). Arrangements that would leverage economies of scale for public health departments face multiple barriers, but there are various ways to help small departments to work with others to achieve greater capacity, such as consolidation and sharing resources (Kaufman, 2011; Libbey and Miyahara, 2011). As discussed in the committee’s report on law and policy, some states have begun to implement or are considering such arrangements (see Bates et al., 2011; IOM, 2011a; Koh et al., 2008; New Jersey Department of Health and Senior Services, 2008; Stoto and Morse, 2008).
Reform of financing to support foundational capacities and provide programmatic flexibility is a critical early step in refashioning governmental public health to live up to its fundamental mission of “fulfilling society’s interest in assuring conditions in which people can be healthy” (IOM, 1988). The approaches that the committee recommends for reforming current financing will likely foster organizational and infrastructure changes. Those changes alone, however, will not place governmental public health in a position to maximize its contribution to the efficient achievement of better health for the nation in the 21st century. Additional funding, to which the committee turns in Chapter 4, will also be required. In the next chapter, the committee describes tools needed to monitor and build organization and programmatic change and to assess the level of funding that will be required.
Academy Health. 2011. The Impact of the Affordable Care Act on the Safety Net. Washington, DC: Academy Health.
Armour, B. S., E. A. Finkelstein, and I. C. Fiebelkorn. 2009. State-level Medicaid expenditures attributable to smoking. Preventing Chronic Disease 6(3):A84. http://www.cdc.gov/pcd/issues/2009/jul/08_0153.htm (January 6, 2012).
ASTHO (Association of State and Territorial Health Officials). 2011. ASTHO Profile of State Public Health. Vol. 2. Washington, DC: ASTHO.
BARHII (Bay Area Regional Health Inequities Initiative) and PHLP (Public Health Law and Policy). 2010. Partners for Public Health: Working with Local, State, and Federal Agencies to Create Healthier Communities. Oakland, CA: BARHII and PHLP.
Bates, L., B. Lafrancois, and R. Santerre. 2011. An empirical study of the consolidation of local public health services in Connecticut. Public Choice 147(1):107-121.
Bernet, P. M. 2007. Local public health agency funding: Money begets money. Journal of Public Health Management & Practice 13(2):188-193.
Binder, S., A. M. Levitt, J. J. Sacks, and J. M. Hughes. 1999. Emerging infectious diseases: Public health issues for the 21st century. Science 284(5418):1311-1313.
Boufford, J. I., and P. R. Lee. 2001. Health Policies for the 21st Century: Challenges and Recommendations for the U.S. Department of Health and Human Services. New York: Milbank Memorial Fund.
Brooks, R. G., L. M. Beitsch, P. Street, and A. Chukmaitov. 2009. Aligning public health financing with essential public health service functions and national public health performance standards. Journal of Public Health Management and Practice 15(4):299-306.
Brownson, R. C., J. G. Gurney, and G. H. Land. 1999. Evidence-based decision making in public health. Journal of Public Health Management & Practice 5(5):86-97.
Brownson, R. C., J. E. Fielding, and C. M. Maylahn. 2009. Evidence-based public health: A fundamental concept for public health practice. Annual Review of Public Health 30:175-201.
Canada, B. 2002. Federal Grants to State and Local Governments: Overview and Characteristics. Washington, DC: CRS Report for Congress.
CDC (Centers for Disease Control and Prevention). 1999. Ten great public health achievements—United States, 1900-1999. Morbidity and Mortality Weekly Report 48(12):241-243.
CDC. 2004. Sustaining State Funding for Tobacco Control: The Facts. Atlanta, GA: CDC.
CDC. 2005. Annual smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 1997-2001. Morbidity and Mortality Weekly Report 54(25):625-628.
CDC. 2010. National Public Health Improvement Initiative (NPHII): About. http://www.cdc.gov/stltpublichealth/nphii/about.html (March 30, 2012).
CDC. 2011a. Chronic Disease Prevention and Health Promotion. Preventive Health and Health Services Block Grant. A Critical Public Health Resource at a Glance 2011. http://www.cdc.gov/chronicdisease/resources/publications/AAG/blockgrant.htm (January 3, 2012).
CDC. 2011b. Vital signs: Current cigarette smoking among adults aged ≥18 Years—United States, 2005-2010. Journal of the American Medical Association 306(17):1857-1860.
CDC. 2012a. About OSTLTS: State, Tribal, Local, and Territorial Public Health Professionals Gateway. http://www.cdc.gov/stltpublichealth/AboutOSTLTS/index.html (March 15, 2012).
CDC. 2012b. PHHS Block Grant Appropriations History. http://www.cdc.gov/phhsblockgrant/history.htm (April 19, 2012).
Cohen, J. W., and N. A. Krauss. 2003. Spending and service use among people with the fifteen most costly medical conditions, 1997. Health Affairs 22(2):129-138.
Committee on Inspection and Evaluation. 1996. Accountability for Block Grants. Washington, DC: Council of the Inspectors General on Integrity and Efficacy.
Curry, C. W., A. K. De, R. M. Ikeda, and S. B. Thacker. 2006. Health burden and funding at the Centers for Disease Control and Prevention. American Journal of Preventive Medicine 30(3):269-276.
Danaei, G., E. L. Ding, D. Mozaffarian, B. Taylor, J. Rehm, C. J. L. Murray, and M. Ezzati. 2009. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine 6(4):1-23.
Elster, N. R., R. E. Hoffman, and J. R. Livengood. 2003. Public health research and health information. In Law in Public Health Practice. 1st ed, edited by R. A. Goodman, M. A. Rothstein, R. E. Hoofman, W. Lopez, and G. W. Matthews. New York: Oxford University Press.
Fee, E., and T. M. Brown. 2002. The unfulfilled promise of public health: Deja vu all over again. Health Affairs 21(6):31-43.
Foreman, M. 2009. Preventable injuries burden state budgets. Legisbrief—National Conference of State Legislatures 17(3):1-2.
Frieden, T. R., P. I. Fujiwara, R. M. Washko, and M. A. Hamburg. 1995. Tuberculosis in New York City—turning the tide. New England Journal of Medicine 333(4):229-233.
Frieden, T. R., M. T. Bassett, L. E. Thorpe, and T. A. Farley. 2008. Public health in New York City, 2002-2007: Confronting epidemics of the modern era. International Journal of Epidemiology 37(5):966-977.
Frist, B. 2002. Public health and national security: The critical role of increased federal support. Health Affairs 21(6):117-130.
Georgeson, M., L. E. Thorpe, M. Merlino, T. R. Frieden, J. E. Fielding, and The Big Cities Health Coalition. 2005. Shortchanged? An assesessment of chronic disease programming in major US city health departments. Journal of Urban Health: Bulletin of the New York Academy of Medicine 28(2):183-190.
Glasgow, R. E., E. Lichtenstein, and A. C. Marcus. 2003. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health 93(8):1261-1267.
Haberkorn, J. 2012. Health Policy Brief: The Prevention and Public Health Fund. Health Affairs, February 23.
Hall, M. A. 2011. Rethinking safety-net access for the uninsured. New England Journal of Medicine 364(1):7-9.
Handler, A. S., and B. J. Turnock. 1996. Local health departments effectiveness in addressing the core functions of public health: Essential ingredients. Journal of Public Health Policy 17(4):460-483.
Herrick, D. 2011. Crisis of the Uninsured: 2010 and Beyond (Brief Analysis No 723). Dallas, Texas: National Center for Policy Analysis.
Honoré, P. A., and J. F. Costich. 2009. Public health financial management competencies. Journal of Public Health Management & Practice 15(4):311-318.
Honoré, P. A., and T. Schlechte. 2007. State public health agency expenditures: Categorizing and comparing to performance levels. Journal of Public Health Management and Practice 13(2):156-162.
Honoré, P. A., and W. Scott. 2010. Priority Areas for Improvement of Quality in Public Health. Washington, DC: HHS.
Honoré, P. A., D. Wright, D. M. Berwick, C. M. Clancy, P. Lee, J. Nowinski, and H. K. Koh. 2011. Creating a framework for getting quality into the public health system. Health Affairs 30(4):737-745.
IOM (Instititue of Medicine). 1988. The Future of Public Health. Washington, DC: National Academy Press.
IOM. 2003. The Future of the Public’s Health in the 21st Century. Washington, DC: The National Academies Press.
IOM. 2008. Eight Americas: Investigating mortality disparities across races, counties, and race-counties in the United States. In Challenges and Successes in Reducing Health Disparities: Workshop Summary, edited by C. J. L. Murray, S. C. Kulkarnin, C. Michaud, N. Tomijima, M. T. Bulzacchelli, T. J. Iandiorio, and M. Ezzat. Washington, DC: The National Academies Press.
IOM. 2011a. For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges. Washington, DC: The National Academies Press.
IOM. 2011b. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: The National Academies Press.
Kaufman, N. 2011. Summary: Regionalization of Government Services: Lessons Learned & Application for Public Health Service Delivery. Robert Wood Johnson Foundation and The Strategic Vision Group.
Kennan, S. A. 2008. Legislative relations in public health. In Public Health Administration. Principles for Population-Based Management, edited by L. F. Novick, C. B. Morrow and G. P. Mays. Sudbury, MA: Jones and Bartlett Publishers.
KFF (The Henry J. Kaiser Family Foundation). 2011. Summary of New Health Reform Law. http://www.kff.org/healthreform/upload/8061.pdfs (December 27, 2011).
Koh, H. K., L. J. Elqura, C. M. Judge, and M. A. Stoto. 2008. Regionalization of local public health systems in the era of preparedness. Annual Review of Public Health 29:205-218.
Kuehn, B. M. 2011. Public health cuts threaten preparedness, preventive health services. Journal of the Amercican Medical Association 306(18):1965-1966.
Kurland, J., D. K. Walker, and C. L. Hager. 2004. Funding Cuts to Public Health in Massachusetts: Losses Over Gains. Boston: Massachusetts Health Policy Forum.
LaBeaud, A. D., and S. Aksoy. 2010. Neglected funding for vector-borne diseases: A near miss this time, a possible disaster the next time. Neglected and Tropical Diseases 4(10):e847.
LAO (California Legislative Analyst’s Office). 2010. Health and Social Services: 2008-09 Analysis. Sacramento, CA: Legislative Analyst’s Office.
Libbey, P., and B. Miyahara. 2011. Cross-Jurisdictional Relationship in Local Public Health: Preliminary Summary of an Environmental Scan. Princeton, NJ: Robert Wood Johnson Foundation.
Mays, G. P., and S. A. Smith. 2009. Geographic variation in public health spending: Correlates and consequences. Health Services Research 44(5 Pt 2):1796-1817.
Mays, G. P., M. C. McHugh, K. Shim, D. Lenaway, P. K. Halverson, R. Moonesinghe, and P. Honoré. 2004. Getting what you pay for: Public health spending and the performance of essential public health services. Journal of Public Health Management and Practice 10(5):435-443.
Meier, B. M., J. Merrill, and K. Gebbie. 2009. Modernizing state public health enabling statues to reflect the mission and essential services of public health. Journal of Health Management Practice 15(2):112-119.
Meyer, J., and L. Weiselberg. 2009. County and City Health Departments: The Need for Sustainable Funding and the Potential Effect of Health Care Reform on their Operations. Princeton, NJ: Robert Wood Johnson Foundation and National Association of County and City Health Officials.
NACCHO (National Association of City and County Health Officials). 2005. Operational Definitions of a Functional Local Health Department. Washington, DC: NACCHO.
NACCHO. 2010. Trends in Local Health Department Finances, Workforce, and Activities. Washington, DC: NACCHO.
NACCHO. 2011a. 2010 National Profile of Local Health Departments. Washington, DC: NACCHO.
NACCHO. 2011b. Comments of the National Association of County and City Health Officials: On the Draft Vision, Goals, Strategic Directions, and Recommendations for the National Prevention and Health Promotion Strategy. Washington, DC: NACCHO.
NACCHO. 2011c. Local Health Department Job Losses and Program Cuts: State-Level Tables from the 2010 National Profile Study. Washington, DC: NACCHO.
NACCHO. 2012. Operational Definition of a Functional Local Health Department. http://www.naccho.org/topics/infrastructure/accreditation/OpDef.cfm (March 30, 2012).
NCSL (National Conference of State Legislatures). 2012. State Legislation and Actions Challenging Certain Health Reforms, 2011-2012. http://www.ncsl.org/issues-research/health/state-laws-and-actions-challenging-aca.aspx (March 12, 2012).
New Jersey Department of Health and Senior Services. 2008. A Study of New Jersey’s Local Public Health System. New Jersey: New Jersey Department of Health and Senior Services.
Novick, L. F., C. B. Morrow, and G. P. Mays. 2008. Public Health Administration: Principles for Population-Based Management. Sudbury, MA: Jones and Bartlett Publishers.
OIG (Office of the Inspector General). 1995. Federal Approaches to Funding Public Health Programs. Washington, DC: HHS.
OIG. 1999. Public Health and Management Care: Opportunitiess for Collaboration. Washington, DC: HHS.
Orenstein, D. M. 2006. The role of measles elimination in development of a national immunization program. Pediatric Infectious Disease Journal 25(12):1093-1101.
PHANYC (The Public Health Association of New York City). 2002. Public Health at a Crossroads. New York: The Public Health Association of New York City.
PHI (Public Health Institute). 2010. Health Reform and Local Health Departments: Opportunities for the Centers for Disease Control and Prevention. Edited by E. Hall, R. Melton, A. Broderick, and A. Wang. Oakland, CA: Public Health Institute.
PHIP (Public Health Improvement Partners) Finance Committee. 2006. Financing Local Public Health in Washington State: Challenges and Choices. Tumwater, WA: Public Health Improvement Partners.
Public Health Functions Steering Committee. 1994. The Public Health Workforce: An Agenda for the 21st Century. Full Report of the Public Health Functions Project. Washington, DC: HHS.
Rehkopf, D. H., and N. Adler. 2011. Review of Social Determinants of Health for Public Health Departments. Oakland, CA: Public Health Institute and Bay Area Regional Health Inequities Initiative.
Salinsky, E. 2010. Governmental Public Health: An Overview of State and Local Public Health Agencies. Washington, DC: National Health Policy Forum.
Salinsky, E. 2012. Financing Mission-Critical Investments in Public Health Capacity Development. Commissioned Paper, Appendix C. Washington, DC: The National Academies Press.
Salinsky, E., and E. A. Gursky. 2006. The case for transforming governmental public health. Health Affairs 25(4):1017-1028.
Santerre, R. E. 2009. Jurisdiction size and local public health spending. Health Services Research 44(6):2148-2166.
Slifkin, R. T., P. Silberman, and S. Reif. 2001. The effect of Medicaid managed care on rural public health departments. Journal of Rural Health 17(3):187-196.
Smith, T. A., K. J. Minyard, C. A. Parker, R. F. Van Valkenburg, and J. A. Shoemaker. 2007. From theory to practice: What drives the core business of public health? Journal of Public Health Management & Practice 13(2):169-172.
Stoto, M. A., and L. Morse. 2008. Regionalization in local public health systems: Public health preparedness in the Washington metropolitan area. Public Health Reports 123(4):461-473.
TFAH (Trust for America’s Health). 2008. Blueprint for a Healthier America: Modernizing the Federal Public Health System to Focus on Prevention and Preparedness. Washington, DC: TFAH.
TFAH. 2009. Shortchanging America’s Health: A State-By-State Look at How Federal Public Health Dollars are Spent and Key State Health Facts. Washington, DC: TFAH.
TFAH. 2011. Investing in America’s Health: A State-By-State Look at Public Health Funding and Key Health Facts. Washington, DC: TFAH and The Robert Wood Johnson Foundation.
Turnock, B., A. Handler, W. Hall, S. Potsic, R. Nalluri, and E. H. Vaughn. 1994. Local health department effectiveness in addressing the core functions of public health. Public Health Reports 109(5):654-660.
U.S. Congress Office of Technology Assessment. 1993. The Continuing Challenge of Tuberculosis, OTA-H-574. Washington, DC: Government Printing Office.
Woolf, S. H., R. E. Johnson, R. L. Phillips, Jr., and M. Philipsen. 2007. Giving everyone the health of the educated: An examination of whether social change would save more lives than medical advances. American Journal of Public Health 97(4):679-683.
Woolf, S. H., R. M. Jones, R. E. Johnson, R. L. Phillips, Jr., M. N. Oliver, A. Bazemore, and A. Vichare. 2010. Avertable deaths associated with household income in Virginia. American Journal of Public Health 100(4):750-755.






























