Catastrophic disasters occurring in 2011 in the United States and worldwide—from the tornado in Joplin, Missouri, to the earthquake and tsunami in Japan, to the earthquake in New Zealand—have demonstrated that even prepared communities can be overwhelmed. In 2009, at the height of the influenza A (H1N1) pandemic, the Assistant Secretary for Preparedness and Response (ASPR) at the Department of Health and Human Services (HHS) asked the Institute of Medicine (IOM) to convene a committee of experts to develop national guidance for use by state and local public health officials and health-sector agencies and institutions in establishing and implementing standards of care that should apply in disaster situations—both naturally occurring and manmade—under conditions of scarce resources.
In its letter report, released the same year, the Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations defined these “crisis standards of care” (CSC) to be a “substantial change in the usual health care operations and the level of care it is possible to deliver . . . justified by specific circumstances and . . . formally declared by a state government in recognition that crisis operations will be in effect for a sustained period” (IOM, 2009, p. 3). CSC, planned and implemented in accordance with ethical values, are necessary for the allocation of scarce resources. Public health disasters justify temporarily adjusting practice standards and/or shifting the balance of ethical concerns to emphasize the needs of the community rather than the needs of individuals. Therefore, professional care delivered in a catastrophic disaster may need to be modified to address the demands of the situation, including by focusing more intently on the needs of the entire affected community.
The committee’s 2009 letter report also enumerated five key elements that should underlie all CSC plans:
• a strong ethical grounding that enables a process deemed equitable based on its transparency, consistency, proportionality, and accountability;
• integrated and ongoing community and provider engagement, education, and communication;
• the necessary legal authority and legal environment in which CSC can be ethically and optimally implemented;
• clear indicators, triggers, and lines of responsibility; and
• evidence-based clinical processes and operations.
Following publication of the 2009 letter report, ASPR, the Department of Veterans Affairs, and the National Highway Traffic Safety Administration requested that the IOM reconvene the committee to conduct phase two of the study, which involved building on that report, examining its impact, and developing templates to guide the efforts of individuals and organizations responsible for CSC planning and implementation. The committee also was charged with identifying metrics to assess the development of crisis standards of care protocols and developing a set of tools for use at the state and local levels in engaging the public as a necessary step in the development of CSC plans.
REPORT DESIGN AND ORGANIZATION
This report has a functional format and design that reflect its purpose of providing a resource manual for all stakeholders involved in a disaster response. It is organized as a series of stand-alone resources for ease of use and reference. The first volume includes Chapters 1 through 4. Chapter 1 provides an introduction to the report, including a summary of key elements of CSC identified in the committee’s 2009 letter report, the recommendations from that report, and discussion of the report’s impact as essential context for phase two of the committee’s work. The next three chapters establish a framework for a systems approach to the development and implementation of CSC plans (Chapter 2), and address the legal issues (Chapter 3) and the ethical, palliative care, and mental health issues (Chapter 4) that agencies and organizations at each level of a disaster response should address.
The next four chapters are bound as separate volumes, each aimed at a key stakeholder group—state and local governments (Chapter 5), emergency medical services (EMS) (Chapter 6), hospitals and acute care facilities (Chapter 7), and out-of-hospital and alternate care systems (Chapter 8). The text of the chapters defines the roles and responsibilities of these stakeholders, describes operational considerations associated with their development and implementation of CSC plans, and provides brief descriptions of templates that outline the specific functions and tasks for each stakeholder when allocating scarce resources in response to a disaster. The templates are easily located at the end of each chapter by the red bar that runs the length of each page.
Chapter 9, again published as a separate volume, includes a brief description of the committee’s work to design the public engagement toolkit and the tools themselves.1
The final volume of the report consists of six appendixes: a glossary of terms used in the report (Appendix A), a sample hospital CSC plan (Appendix B), a listing of potentially scarce medical resources (Appendix C), a listing of resource challenges by disaster type (Appendix D), the committee’s statement of task (Appendix E), and biographical sketches of the committee members (Appendix F).
FRAMEWORK FOR A SYSTEMS APPROACH TO CRISIS STANDARDS OF CARE
CSC are just one aspect of broader disaster planning and response efforts; they are a mechanism for responding to situations in which the demand on needed resources far exceeds the resources’ availability. A systems
_________________
1 The templates in Chapters 5-8 and the public engagement toolkit can also be downloaded via the project’s website: http://iom.edu/Activities/PublicHealth/DisasterCareStandards.aspx.
approach to disaster planning and response is therefore required to integrate all of the values and response capabilities necessary to achieve the best outcomes for the community as a whole.
Successful disaster response depends on coordination and integration across the full system of the key stakeholder groups: state and local governments, EMS, public health, emergency management, hospital facilities, and the outpatient sector. Vertical integration among agencies at the federal, state, and local levels also is crucial. At the cornerstone of this coordination and integration is a foundation of ethical obligations—the values that do not change even when resources are scarce—and the legal authorities and regulatory environment that allow for shifts in expectations of the best possible care based on the context of the disaster in which that care is being provided.
Conceptualizing a Systems Approach to Disaster Response
This section broadly outlines a systems framework for disaster response of which CSC is only one, albeit a critical, aspect. However, the development and implementation of CSC plans are the means to mount a response to an incident that far exceeds the usual health and medical capacity and capabilities. Therefore, the same elements that come together to build any successful disaster response should also be used to develop robust CSC plans and guide their implementation.
A systems approach is defined as a “management strategy that recognizes that disparate components must be viewed as interrelated components of a single system, and so employs specific methods to achieve and maintain the overarching system. These methods include the use of standardized structure and processes and foundational knowledge and concepts in the conduct of all related activities” (George Washington University Institute for Crisis, Disaster and Risk Management, 2009, p. 59).
The systems framework that the committee believes should inform the development and implementation of CSC plans (see Figure 2-1) is based on the five key elements of planning set forth in the 2009 letter report. These key elements served as the starting point for the development of the committee’s recommendations in that report and are foundational for all disaster response planning.
The two cornerstones for the foundation of this framework are the ethical considerations that govern planning and implementation and the legal authority and legal environment within which plans are developed. Ethical decision making is of paramount importance in the planning for and response to disasters. Without it, the system fails to meet the needs of the community and ceases to be fair, just, and equitable. As a result, trust—in professionals, institutions, government, and leadership—is quickly lost. The legal authority and legal environment within which CSC plans are the other cornerstone of the framework’s foundation. The legal authority and environment support the necessary and appropriate actions in response to a disaster. Between those two cornerstones of the foundation are the steps needed to ensure that the development and implementation of CSC plans occur. They include provider and community engagement efforts, development of a process that permits individual communities to identify regionally coordinated and consistent indicators that denote a change in the usual manner of health care delivery during a disaster, and the triggers that must be activated in order to implement CSC. These lead to the top step, the implementation of clinical processes and operations that support the disaster response. All of these efforts are supported and sustained by an ongoing performance improvement process, an important element of any systems approach to monitor demand (ensuring situational awareness), evaluate the impact of implementation actions, and establish/share best
practices. This process includes education of and information sharing among organizations and individuals responsible for both the planning and response phases of a disaster.
The pillars of medical surge response—hospital and outpatient medical care; public health; EMS; and emergency management/public safety agencies, organizations, and authorities—stand on this strong base. Each of these pillars is an element of the disaster response system, representing a distinct discipline, but all need to be well integrated to ensure a unified disaster response. One acting independently of the others may delay, deter, and even disrupt the delivery of medical care in a disaster. Many of these disciplines work together during daily operations. For example, EMS transports bridge the outpatient and hospital communities, public health bridges the public safety and hospital communities, and emergency management bridges the hospital and public health communities. But rarely, and in few communities, do all of these response elements come together in a manner that can ensure oversight and care for an overwhelming number of disaster victims. The more complex and dynamic the incident, the more important strong and effective coordination and integration among the pillars becomes, as emphasized by a systems approach. Priorities and objectives should be shared across the entire system to inform the development of unified strategies and the coordinated tactics required to implement them. Applying National Incident Management System/ National Response Framework principles and systems can help improve coordination and ensure the desired outcomes.
Atop the pillars are local, state, and federal government functions. Government at all three levels has an overarching responsibility for the development, institution, and proper execution of CSC plans, policies, protocols, and procedures. Good governance encompasses the functions of monitoring and evaluation, as well as accountability and meaningful contributions to policy development (Gostin and Powers, 2006). These functions are especially important in developing plans related to incidents in which the confidence of the public in government institutions may come into question, and the risk of cascading failures and multisector disruption, exacerbated by a lack of coordinated response, can mean the difference between thousands of lives lost and saved.
Milestones to Guide CSC Planning
To ensure that this systems coordination and integration occur, the committee offers specific milestones, enumerated in Box S-1. This systems approach to CSC, and disaster response more generally, provides the context for this report. It balances the specific functions and tasks of each stakeholder group, but also provides a structure for coordinating and integrating their operations to enable a more flexible and dynamic overall response effort while still emphasizing a robust, efficient chain of command.
LEGAL ISSUES
An array of relevant legal issues should be identified and addressed before disaster strikes. For example, states should evaluate what legal liability protections are in place for their health care workers, volunteers, and health care coalitions, and should determine whether these protections are sufficient or require augmentation. Health care personnel and entities, too, should understand what protections are available to them and
BOX S-1
Milestones for Planning and Implementation
for Crisis Standards of Carea
1. Establish a State Disaster Medical Advisory Committee.b
2. Ensure the development of a legal framework for CSC implementation.
3. Promote understanding of the disaster response framework among elected officials and senior (cabinet-level) state and local government leadership.
4. Develop a state health and medical approach to CSC planning that can be adopted at the regional/local level by existing health care coalitions, emergency response systems (including the Regional Disaster Medical Advisory Committee),c and health care providers.
5. Engage health care providers and professional associations by increasing their awareness and understanding of the importance and development of a CSC framework.
6. Encourage participation of the outpatient medical community in planning.
7. Ensure that local and state CSC plans include clear provisions that permit adaptation of EMS systems under disaster response conditions.
8. Develop and conduct public community engagement sessions on the issue of CSC.
9. Support surge capacity and capability planning for health care facilities and the health care and public health systems.
10. Plan for an alternate care system capability.
11. Support scarce resource planning by the RDMAC (if developed) for health care facilities and the health care system.
12. Incorporate crisis/emergency risk communication strategies into CSC plans.
13. Exercise CSC plans at the local/regional and interstate levels.
14. Refine plans based on information obtained through provider engagement, public/community engagement and exercises, and real-life events.
15. Develop a process for continuous assessment of disaster response capabilities.
a Given the variability in both how state and local agencies are organized, CSC planning and potential activation will need to take into account varying structures and relationships of governments across states and localities throughout the United States.
b See Appendix A, Volume 7 for definition.
c See Appendix A, Volume 7 for definition.
the fact that these may be role and location dependent. The potential complexity and consequences of the financing and reimbursement of disaster response efforts also should be understood and addressed within and between communities. Thorough comprehension of these legal issues among relevant response stakeholders is crucial to their being resolved prior to a disaster—an opportunity not always afforded for other issues and challenges involved in CSC implementation. In considering the legal environment in a CSC situation, policy makers at all levels must insist that professionals act professionally. There is never a justification for careless decision making or willful misconduct, especially in the setting of a disaster response, when patients are at their most vulnerable.
CROSS-CUTTING ISSUES: ETHICS, PALLIATIVE CARE, AND MENTAL HEALTH
A number of issues are relevant to all four stakeholder groups—governments, EMS, health care facilities, and out-of-hospital and alternate care systems—with roles in the development and implementation of CSC plans. These cross-cutting issues, reviewed briefly below, are incorporated into the guidance and templates provided in this report for each stakeholder group.
Ethics
Plans and protocols that shift desired patient care outcomes from the individual to the population must be grounded in the ethical allocation of resources, which ensures fairness to everyone. Developing consensus on what a reasonable health care practitioner would do in the event of a disaster will facilitate the transition from conventional to contingency and crisis response during such an incident.2 The emphasis in a public health emergency must be on improving and maximizing the population’s health while tending to the needs of patients within the constraints of resource limitations.
With respect to fairness, an ethical policy does not require that all persons be treated in an identical fashion, but does require that differences in treatment be based on appropriate differences among individuals. If particular groups receive favorable treatment, such as in access to vaccines, this priority should stem from such relevant factors as greater exposure or vulnerability and/or promote important community goals, such as helping first responders or other key personnel stay at work. Policies should account for the needs of the most at risk and support the equitable and just distribution of scarce goods and resources.
Implementation of CSC should ideally facilitate the delivery of care to patients to the extent possible by allocating resources to those who are most likely to benefit. The implementation of CSC should ultimately bring better care to more patients and a more equitable distribution of resources to those most likely to benefit. The needs of all potentially affected populations must be addressed to ensure fair and equitable plans. Particular attention should also be paid to the needs of the most at-risk and marginalized people, such as the poor and those with mental or physical disabilities.
Ultimately, the committee’s understanding of CSC implementation is within the context of supporting public health efforts through fair and rational processes. The committee’s 2009 letter report outlined an ethical approach to guide CSC planning and responses, and the committee continues to emphasize the importance of an ethical foundation for the fair allocation of scarce medical, public health, and relevant community resources (see previous key principles).
The ethical basis for CSC planning has particular implications for policy decisions regarding the allocation of scarce resources. Community engagement in the assessment of ethical values that underlie such decisions can help ensure that the decisions are aligned with community values and that those values are integrated by agencies responsible for developing CSC plans where appropriate. The key elements in plan-
_________________
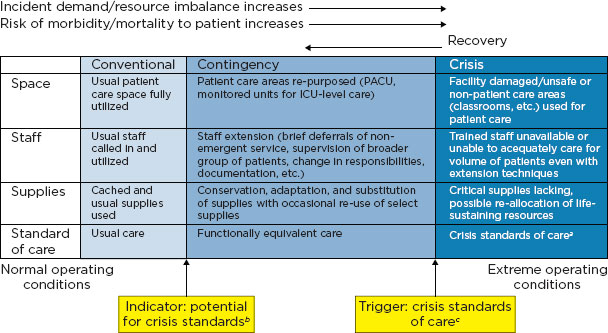
2 The surge capacity following a mass casualty incident falls into three basic categories, depending on the magnitude of the incident: conventional, contingency, and crisis. These categories also represent a corresponding continuum of patient care delivered during a disaster. As the imbalance increases between resource availability and demand, health care—emblematic of the health care system as a whole—maximizes conventional capacity; then moves into contingency; and, once that capacity is maximized, moves finally into crisis capacity. A crisis situation may lead to an overwhelming demand for services and result in shortages of equipment, supplies, pharmaceuticals, personnel, and other critical resources, necessitating operational adjustments.
ning and implementing CSC are particularly relevant to ensuring fair access to resources by disadvantaged or at-risk populations. As a general matter, ethical values do not constitute a process for determining what is the most “ethical” course of action. However, a clear grasp of those values helps policy makers and the public determine which options are within the bounds of ethically viable choices. Moreover, an understanding of ethical values often can illuminate clearly wrong decisions, such as those that would place an unreasonably high share of the burden on a single population (e.g., the elderly, the disabled, the uninsured). Therefore, the committee offers guidance on how to adjust clinical practice in the face of severe resource deficits in a manner consistent with ethically valid goals and desired outcomes using a population-based approach.
Palliative Care
Providing palliative care is an important ethical and medical imperative and, especially with regard to end-of-life care, should include a holistic and humane approach to CSC implementation. Setting the expectation that all patients will receive some care, regardless of the availability or scarcity of resources, is an important component of CSC efforts. Incorporating into CSC planning the capabilities necessary to provide palliative care assures the public that even when curative acute care cannot be provided, every attempt to offer pain management and comfort care to disaster victims will be made, even if comfort care may mean nonpharmaceutical interventions such as holding a hand or offering words of comfort.
Mental Health
The social consequences of a disaster and the need to implement CSC will certainly impact the mental health of patients, their families, health care providers, and the general public. The very real potential for mass fatalities during such an incident will undoubtedly tax the system as a whole and exacerbate mental health issues at a population level. Setting appropriate expectations and planning for mental health resilience are important considerations at each level of response by all of the stakeholders developing and implementing CSC plans. While addressing mental health issues is challenging, there are unique opportunities to mitigate mental health impacts by incorporating mental health and resilience provisions into the preparedness, response, and recovery components of CSC planning.
GOVERNMENTS
A systems approach to disaster response requires that federal, state, and local governments work together to plan and implement CSC, even though each level of government has specific and differing authorities and access to resources.
Federal Government
The federal government should continue to provide leadership in supporting and encouraging the establishment of guidelines for CSC for use in disaster situations at the state and local levels, whether through direct contact with public health departments and other relevant stakeholders or through the relevant state
governors’ offices. These efforts should emphasize the importance of coordinating such planning within the larger context of surge capacity planning, all as part of a disaster response framework. Inclusion of specific language in the HHS Hospital Preparedness Program and the Centers for Disease Control and Prevention’s Public Health Emergency Preparedness cooperative agreements is the best means of ensuring continued emphasis on this planning. In addition, agencies such as the Centers for Medicare & Medicaid Services are important because of their capacity to influence provider practice, reimbursement, and waivers. Finally agencies such as the the Department of Homeland Security, the Department of Defense, the Department of Transportation, and the Department of Veterans Affairs have relevant grant programs that should include funding opportunities for the planning and implementation of CSC. The federal government can positively influence state government planning, and in the context of the framework established, must be the ultimate driver behind such efforts.
State Government3
Emergencies rising to a level that necessitates CSC generally are expected to be multijurisdictional, statewide, or even multistate events that entail various local, regional, state, and federal roles and authorities. Therefore, considerable state-level coordination with intra- and interstate as well as federal partners is essential. As recommended in the committee’s 2009 letter report, states in particular should lead the development and implementation of CSC protocols “both within the state and through work with neighboring states, in collaboration with their partners in the public and private sectors” (IOM, 2009, p. 4). Depending on the specific nature of the incident, various state agencies, as well as private health care entities, should be involved in CSC planning and response activities because no single agency or health or emergency response entity alone can be expected to handle the challenges presented by a CSC incident. Variations in state agency structures and authorities will often dictate emergency response leadership roles. Therefore, states should have the flexibility to develop the organizational structure for CSC planning and implementation that makes the most sense for them. Recognizing that a variety of state agencies and leaders will have pivotal CSC roles, however, the state health department is fundamentally the most appropriate agency to lead and coordinate CSC planning and implementation at the state level and to advise state leadership on CSC issues.
Local Government
When considering the role of local government in CSC efforts, it is important to remember that, based on how states are structured constitutionally and functionally, vastly different local government structures and relationships exist from state to state. Despite these variations, however, the role of local government in CSC planning and implementation remains crucial. Even though a CSC incident may be widespread and require a systems approach that involves coordinating with all providers and across all levels of government, especially as the geographic area of impact increases, all disasters are ultimately local. At some point, the state CSC plan will need to be incorporated into or adapted for local planning efforts (e.g., development of the health and medical annex of the local emergency operations plan) and will help guide local activities during the response to a catastrophic disaster response.
_________________
3 For the purposes of this report, the term “states” encompasses states, tribal jurisdictions, and territories.
Local political leaders (e.g., mayor, county executive) and agency leadership also will be involved in local decision making and resource requests during a CSC emergency. This means that local CSC coordination, consistent with state planning and response actions, is critical to achieving the envisioned systems-based CSC response. Local governments are uniquely positioned in the organizational structure of states to intersect with both state government partners and the communities in their local jurisdiction(s). Therefore, the involvement of both state and local government leadership is paramount to ensuring that CSC planning and implementation occur. This is especially true because public health and government EMS agencies operate under the direct auspices of state and local government authority. Addressing CSC planning outside of the governmental sphere, especially in the private health care sector, is more difficult. In this regard, emphasis on the importance of a systems approach to CSC planning ensures unified efforts, particularly with respect to the consistency of plan development and implementation.
PREHOSPITAL CARE: EMERGENCY MEDICAL SERVICES
State EMS offices and prehospital care agencies should be actively engaged in the development and implementation of CSC plans. Adjustments to scopes of practice, treatment modalities, and ambulance staffing and call response will all figure significantly into state, local, and EMS agency-specific disaster response plans. Other areas that can be leveraged to maximize scarce EMS resources include the authority to activate restricted treatment and transport protocols, which may entail modifying the emergency medical dispatch criteria implemented at public safety answering points (i.e., 911 call centers). CSC planning should be integrated with the efforts of public health planners to ensure consideration of case management (advice line) call centers, poison control, use of alternate care system destination points for ambulance patients, and limitation of care to on-scene treatment without transport. It should also be recognized that much EMS activity in the United States is volunteer based and occurs in rural communities, where resources often are limited on a regular, ongoing basis. These limitations should be addressed through the incorporation of EMS-specific disaster response and CSC plans into relevant disaster preparedness grant guidance.
In this context, an important factor in operationalizing the CSC framework set forth in the committee’s 2009 letter report and reiterated in Chapter 2 of this report is specific enumeration of EMS roles, responsibilities, and actions in CSC plans. Accordingly, the state agency taking the lead role in coordinating a systems-based catastrophic disaster response should establish consistent triggers and thresholds that indicate the transition from conventional to contingency to crisis care, define a clear mechanism for authorizing CSC activation, provide liability protection for EMS personnel and altered modes of transportation, coordinate emergency operations across the affected region, and address reimbursement issues directly. While standardizing this planning will contribute to consistency in implementing CSC, the different environments in which EMS operates also should be taken into account.
HOSPITALS AND ACUTE CARE FACILITIES
Clinical operations in hospitals, ambulatory care clinics, and private practices make up the largest single element of the response framework in which CSC will be implemented. Implementation of CSC in the hospital setting will occur through the use of a clinical care committee at each hospital, along with a bi-
directional reporting mechanism with state and local governments. Therefore, careful planning is required at both at the local and regional levels, including plans to ensure intraregional coordination and cooperation. Consistent with the Hospital Preparedness Program and Public Health Emergency Preparedness cooperative agreements, disaster response plans should delineate protocols for a shift from the conventional standard of care to ensure that essential health care services will be sustained during the response. CSC plans will be implemented under conditions in which the usual safeguards may not be possible and when resources will be insufficient to allow for the delivery of care under usual operating conditions. It is assumed that under catastrophic disaster response conditions, resources are unavailable or undeliverable to health care facilities from elsewhere in the region or state; similar strategies are being invoked by other health care delivery systems; and patient transfer to other facilities is not possible or feasible, at least not in the short term. Furthermore, it is recognized that access to key medical countermeasures (e.g., vaccines, medications, antidotes, blood products) is likely to be limited, and these resources should be delivered to patients using guidance that aims to optimize benefits and minimize potential harms. It is also assumed that available local, regional, state, and federal resource caches (of key equipment, supplies, and pharmaceuticals) have already been distributed, and no short-term resupply of such stocks is foreseeable.
Although hospitals providing acute care to the community are the focus of this discussion, other health care facilities—such as free-standing surgery centers, urgent care facilities, ambulatory clinics, free-standing emergency departments, nursing homes, federally qualified health centers, and other facilities that can be adapted to provide acute or critical care—can play key roles in a surge response and should be included in planning for and implementation of CSC. All health care facilities providing acute medical care to the community have a “duty to plan” for mass casualty and catastrophic disaster incidents, including planning for the expansion of clinical operations. Hospitals should examine their hazard vulnerability analysis and ensure that they are as prepared as possible for the hazards affecting their community, including the ability to operate as autonomously as possible for up to 96 hours (Joint Commission emergency medicine standards), or more if the risk of isolation of the facility is high. The importance of conducting exercises in crisis situations, from the provider to the incident command level, cannot be overemphasized.
The goal of incident management in situations involving mass casualties or catastrophic failure of critical infrastructure is to get the right resources to the right place at the right time. This may involve anticipating shortfalls, adapting responses, partnering with other stakeholder agencies to provide alternate care sites for patient volumes that cannot be accommodated within the usual medical facilities, and other strategies. Therefore, a regionally coordinated response is imperative to facilitate consistent standards of care within all affected communities after a disaster. Regional coordination enables the optimal use of available resources; facilitates obtaining and distributing resources; and provides a mechanism for policy development and situational awareness that is critical to avoiding crisis situations and, when a crisis does occur, ensuring fair and consistent use of resources to provide a uniform level of care across the region.
OUT-OF-HOSPITAL AND ALTERNATE CARE SYSTEMS
While much of disaster and surge capacity planning focuses on hospital-based care, approximately 89 percent of health care is delivered in outpatient settings (Hall et al., 2010; Schappert and Rechtsteiner, 2011). Especially during an epidemic, failure to leverage outpatient resources may result in catastrophic overload of inpatient and hospital-affiliated resources. For this reason, efforts to improve the integration of outpatient care assets into disaster response are critical, not only to ensure the provision of crisis care but also to avoid crisis care. However, the value of the outpatient sector—its diversity—is also its challenge: the numbers and varying types of clinics and providers in a given area (in addition to long-term care, outpatient surgery, and other medical facilities) hamper detailed coordinated planning. Unlike other emergency response entities (e.g., municipal or county-run EMS), private health care facilities and providers cannot simply be “assigned” by public health officials to develop outpatient surge capacity, and private health care cannot assume that public health can provide the clinical leadership or resources (especially medical providers) needed to establish effective alternate care systems. Both have a joint responsibility for and distinct but equally necessary roles in efforts to advance outpatient CSC planning to ensure that the health care goals of catastrophic disaster response can be accomplished through coordinated efforts.
PUBLIC ENGAGEMENT
The committee’s 2009 letter report highlighted meaningful public engagement as one of the five key elements of CSC planning. Policy makers should involve the public in a structured dialogue about the implications and likelihood of having to allocate health care delivery and essential vaccines or medicines ethically in the event of a catastrophic disaster. To facilitate this involvement, the committee developed a public engagement toolkit. This resource should support CSC planning efforts by enabling state and local health departments and other interested planners to initiate conversations with the community regarding these difficult issues. Community engagement probably is best timed to start after the planning teams (the state and regional disaster medical advisory committees) have had an opportunity to consider all of the pertinent issues and draft a plan, but before a plan is finalized.
RECOMMENDATION
To enhance and elaborate on the recommendations from its 2009 letter report, which it still fully supports, the committee developed a set of templates identifying the core functions and tasks for individuals and organizations involved in CSC planning and implementation. In developing these resources, the committee emphasized the use of a systems approach that integrates CSC planning into the larger context of overall surge capacity planning. The entire emergency response system—each component acting both independently and as part of a coherent and integrated group—should adopt such a framework to deliver the best care possible to the largest number of patients.
RECOMMENDATION: Federal, state, tribal, and local governments should develop a systems-based framework for catastrophic disaster response, which must be integrated into existing emergency response plans and programs. To facilitate the implementation of this framework, the committee specifically recommends that:
• Each level of government should ensure coordination and consistency in the active engagement of all partners in the emergency response system, including emergency management, public health, emergency medical services, public and private health care providers and entities, and public safety.
• Each level of government should integrate crisis standards of care into surge capacity and capability planning and exercises.
• The Department of Health and Human Services/Assistant Secretary for Preparedness and Response (e.g., through its regional emergency coordinators) should facilitate crisis standards of care planning and response among state and tribal governments within their region.
• In crisis standards of care planning and response efforts, states should collaborate with and support local governments.
• Federal disaster preparedness and response grants, contracts, and programs in the Department of Health and Human Services, the Department of Homeland Security, the Department of Defense, the Department of Transportation, and the Department of Veterans Affairs—such as the Hospital Preparedness Program, Public Health Emergency Preparedness Program, Metropolitan Medical Response System, Community Environmental Monitoring Program, and Urban Areas Security Initiative—should integrate relevant crisis standards of care functions.
REFERENCES
George Washington University Institute for Crisis, Disaster and Risk Management. 2009. Emergency management principles and practices for health care systems: Unit 5: Appendices. Washington, DC: George Washington University, http://www.vibha.info/uploads/2/9/3/6/2936979/air_ambulance_5.pdf (accessed February 28, 2012).
Gostin, L. O., and M. Powers. 2006. What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Affairs 25(4):1053-1060.
Hall, M. J., C. J. DeFrances, S. N. Williams, A. Golosinskiy, and A. Schwartzman. 2010. National hospital discharge survey: 2007 summary. Report no. 29. Hyattsville, MD: National Center for Health Statistics.
IOM (Institute of Medicine). 2009. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press, http://www.nap.edu/catalog.php?record_id=12749 (accessed September 6, 2011).
Schappert, S. M., and E. A. Rechtsteiner. 2011. Ambulatory medical care utilization estimates for 2007. Vital and Health Statistics 13(169):1-38.
The last 2 years have seen catastrophic disasters in Haiti, Japan, New Zealand, and the United States. These incidents have been a stark reminder of the ability of disasters to overwhelm even the most advanced health systems and impact resource allocation. All of these incidents—earthquakes, a tsunami, a powerful tornado—were sudden and unexpected, and all resulted in a disruption of infrastructure, including extreme stress and strain on health care systems. During each incident, albeit to varying degrees, the delivery of medical services was impacted by the disruption. The need to allocate scarce resources during a catastrophic disaster is not unique to no-notice natural disasters; such circumstances may also arise in the aftermath of a catastrophic terrorist incident, particularly one due to the release of a bioagent or the detonation of a nuclear device, or a slow-onset event such as pandemic influenza.
This report differentiates between a catastrophic disaster and other disasters or emergencies. A catastrophic disaster is characterized by four attributes: (1) most or all of the community’s infrastructure is impacted (it is the relative, rather than the total, infrastructure loss that matters); (2) local officials are unable to perform their usual roles for a period of time extending well beyond the initial aftermath of the incident; (3) most or all routine community functions—at places of work, recreation, worship, and education—are immediately and simultaneously interrupted; and (4) surrounding communities are similarly affected, and thus there are no regional resources to come to the aid of the affected local communities (Quarantelli, 2000). Each of these four attributes should be judged relative to the impact on the community in question rather than by an absolute standard: for instance, an incident that results in the inability of one hospital to function in a large metropolitan city may be classified as a disaster, but could be classified as catastrophic in a rural community. Similarly, while the initial phase of a disaster may include all four of these attributes, a catastrophic disaster is marked by their persistence into the recovery phrase, well after the incident occurs.
In 2009, at the height of the influenza A (H1N1) pandemic, the Assistant Secretary for Preparedness and Response (ASPR) at the Department of Health and Human Services (HHS) asked the Institute of Medicine (IOM) to convene a committee of experts to develop national guidance for use by state and local public health officials and health-sector agencies and institutions in establishing and implementing standards of care that should apply in catastrophic disaster situations—both naturally occurring and manmade—under conditions of scarce resources. In its letter report, released the same year, titled Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations (IOM, 2009), the Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations defined these “crisis standards of care”
(CSC) to be a “substantial change in the usual health care operations and the level of care it is possible to deliver . . . justified by specific circumstances and . . . formally declared by a state government in recognition that crisis operations will be in effect for a sustained period” (IOM, 2009, p. 3). CSC, planned and implemented in accordance with ethical values, are necessary for the allocation of scarce resources. Professional care delivered in a catastrophic disaster may need to be modified to address the demands of the situation, including by focusing more intently on the needs of the entire affected community. The committee’s 2009 letter report also enumerated five key elements that must underlie all CSC plans:
• a strong ethical grounding that enables a process deemed equitable based on its transparency, consistency, proportionality, and accountability;
• integrated and ongoing community and provider engagement, education, and communication;
• the necessary legal authority and legal environment in which CSC can be ethically and optimally implemented;
• clear indicators, triggers, and lines of responsibility; and
• evidence-based clinical processes and operations.
PHASE TWO: STUDY GOALS AND METHODS
At the request of ASPR, the Committee on Guidance for Establishing National Standards of Care for Use in Disaster Situations reconvened for a second phase of work. The task of phase two was to operationalize the CSC framework set forth in the 2009 letter report. Box 1-1 presents the phase two statement of task.
Building on the work of phase one, the committee developed detailed templates enumerating the functions and tasks of the key stakeholder groups involved in CSC planning and implementation—state1 and local governments, emergency medical services (EMS), hospitals and acute care facilities, and out-of-hospital and alternate care systems. Additionally, a key component of CSC planning, as recommended in the 2009 letter report, is public engagement. In recognition of the challenges associated with simultaneously educating and receiving input from the public, the committee was tasked with providing public engagement tools that can be adapted by state and local jurisdictions based on where they are in the planning process, their communities’ experiences, and available resources. It is important to note that this report is not intended to be a detailed guide to emergency preparedness or disaster response. What is described in this report is an extrapolation of existing incident management practices and principles.
The reconvened committee continued to represent the diverse expertise of the fields and sectors responsible for implementing CSC, including emergency medicine, ethics, public health law, state and local public health, the public and private sectors, disaster response, nursing, palliative and mental health care, and EMS. Biosketches of the committee members can be found in Appendix F. To fully understand the challenges of developing and implementing CSC plans, the committee held two public meetings in May and July 2011. Presentations and comments were provided by a myriad of experts and practitioners, including representatives of state and local health departments, EMS, large and small health care systems, pediatric and maternal patient and provider groups, and the federal government (including ASPR, the U.S. Department of Trans-
_________________
1 For the purposes of this report, the term “states” encompasses states, tribal jurisdictions, and territories.
BOX 1-1
Abbreviated Phase Two Statement of Taska
The committee will:
• Review the impact of its 2009 letter report including progress made by state and local governments and health care organizations in establishing crisis standards of care guidance.
• Identify metrics to assess the development of crisis standards of care protocols.
• Develop templates for states, emergency medical services (EMS) systems, hospitals and individual clinicians to use to guide decision making. These templates will:
o Address the inclusion of all critical components of the emergency response and health care system necessary to plan for and respond to crisis standards of care situations.
o Examine the specific process of declaring a shift to crisis standards of care,
o I dentify clinical and administrative indicators that govern the transition from conventional surge response and conventional standards of care to crisis surge response and crisis standards of care.
o Define terms and provide consistent language (e.g., definitions, situational markers) for communicating across jurisdictions and levels of government the status of health care systems related to crisis standards of care.
In addition, the IOM will develop a template for state and local governments for community engagement tools.
a The complete statement of task can be found in Appendix E, Volume 7.
portation, and the Centers for Disease Control and Prevention [CDC]). The committee also conducted a thorough review of the relevant literature to understand and build on the progress made in developing and operationalizing CSC at the federal, state, and local levels since its letter report was published in 2009.
To fulfill its task of creating public engagement tools, the committee tapped the expertise of external consultants. The committee then piloted the materials developed by these experts in fall 2011 in two settings—Boston and Lawrence, Massachusetts. The pilots were not intended to collect participant data, but to refine the public engagement techniques and materials and broaden them so they can be adapted to suit individual local jurisdictions. These materials and pilots are discussed in greater depth in Chapter 9.
2009 LETTER REPORT: KEY ELEMENTS AND RECOMMENDATIONS
The committee’s 2009 letter report identified five key elements of CSC planning and implementation and offered six recommendations.
Five Key Elements
The 2009 letter report described the framework and foundational elements for the development and implementation of CSC. The committee’s vision for this original framework was based on fairness (i.e., standards are evidence based and recognized as fair by all they affect); equitable processes for decision making and implementation (i.e., transparency, consistency, proportionality, and accountability); community and provider engagement, education, and communication through formalized processes; and the rule of law (i.e., the authority to take necessary and appropriate response actions and an environment that facilitates the implementation of response actions through appropriate laws and regulations). Based on this vision, the committee, in its letter report, recommended the five key elements for CSC protocol development shown in Table 1-1 and described in the following subsections.
Ethical Considerations
Health care professionals must adhere to ethical norms even in conditions of overwhelming scarcity that limit practitioner and patient choices. As a starting point for CSC planning deliberations, ethical values should include the concept of fairness, together with professional duties to care for patients and steward resources. The CSC development process should be guided by key ethical values, including transparency, consistency, proportionality, and accountability.
Community and Provider Engagement, Education, and Communication
Meaningful, integrated, and ongoing engagement of CSC stakeholders (e.g., the public, at-risk populations, health care providers) is critical for effective CSC planning and implementation. State and local governments involved in CSC planning should ensure that strong public engagement occurs and that it promotes trust and transparency in the process, delineates roles and responsibilities, and gives particular attention to the needs of at-risk populations and those with special medical needs. Active engagement should contribute, as appropriate, to developing and refining CSC protocols, developing communication and educational messages/tools for the public and health care practitioners, developing and implementing strategies for community resilience, and improving future CSC responses.
Legal Authority and Environment
Establishing and implementing CSC plans requires careful consideration of the substantial legal challenges involved, including potential liability. Among the legal topics the committee identified as requiring assessment and potential resolution during the course of CSC planning efforts are emergency declarations (local, state, federal), medical versus legal standards of care, mutual-aid agreements, liability risks (including medical malpractice), liability protections (e.g., Public Readiness and Emergency Preparedness [PREP] Act) during emergencies, licensing and credentialing, regulation of EMS and health care facilities, and health care practitioners’ scopes of practice.
Indicators and Triggers
For the assessment and potential management of CSC incidents, CSC planning efforts should include identifying specific indicators, including those based on situational awareness (e.g., hospital bed availability, ventilator availability, EMS call volume, divert status) and on factors specific to the incident (e.g., incidence
TABLE 1-1
Five Key Elements of Crisis Standards of Care Protocols and Associated Components from the 2009 Letter Report
| Key Elements of Crisis Standards of Care Protocols |
Components |
| Ethical considerations |
• Fairness • Duty to care • Duty to steward resources • Transparency • Consistency • Proportionality • Accountability |
| Community and provider engagement, education, and communication |
• Community stakeholder identification with delineation of roles and involvement with attention to vulnerablepopulations • Community trust and assurance of fairness andtransparency in processes developed • Community cultural values and boundaries • Continuum of community education and trust building • Crisis risk communication strategies and situationalawareness • Continuum of resilience building and mental healthtriage • Palliative care education for stakeholders |
| Legal authority and environment |
• Medical and legal standards of care • Scope of practice for health care professionals • Mutual-aid agreements to facilitate resource allocation • Federal, state, and local declarations of
• Special emergency protections (e.g., PREP Act, Section1135 waivers of sanctions under EMTALA and HIPAAPrivacy Rule) • Licensing and credentialing • Medical malpractice • Liability risks (civil, criminal, Constitutional) • Statutory, regulatory, and common-law liability protections |
| Indicators and triggers |
Indicators for assessment and potential management
• Situational awareness (local/regional, state, national) • Incident specific
Triggers for action • Critical infrastructure disruption • Failure of “contingency” surge capacity (resource-sparing strategies overwhelmed)
|
| Key Elements of Crisis Standards of Care Protocols | Components |
| Clinical process and operations |
Local/regional and state government processes to include
• State-level “disaster medical advisory committee” andlocal “clinical care committees” and “triage teams" • Resource-sparing strategies • Incident management (NIMS/HICS) principles • Intrastate and interstate regional consistencies in theapplication of crisis standards of care • Coordination of resource management • Specific attention to vulnerable populations and thosewith medical special needs • Communications strategies of the health system, including public health, emergency medical services, long-term care, primary care, and home care Clinical operations based on crisis surge response plan:
• Decision support tool to triage life-sustaining interventions • Palliative care principles • Mental health needs and promotion of resilience |
NOTE: EMTALA = Emergency Medical Treatment and Active Labor Act; HICS = hospital incident command system; HIPAA = Health Insurance Portability and Accountability Act; NIMS = National Incident Management System; PREP = Public Readiness and Emergency Preparedness. SOURCE: IOM, 2009, pp. 21-23.
and severity of illness or injury; disruption of social and community functioning; availability of resources, such as vaccines and oxygen). Planning efforts should also include establishing triggers for action (e.g., disruption of critical infrastructure, failure of surge capacity strategies).
Clinical Process and Operations
CSC plans should acknowledge the continuum of clinical capacity (i.e., conventional, contingency, crisis) during a disaster and should also establish local, regional, and state government clinical processes and operations—including the state disaster medical advisory committee, regional disaster medical advisory committees, and local clinical care committees and triage teams—that implement incident command system principles, resource-sparing strategies, and communication strategies. In addition, CSC plans should ensure that intra- and interstate plans for CSC implementation are consistent, but not necessarily identical; that resource management is coordinated; that specific attention is given to protecting the interests of at-risk populations and those with special medical needs; and that coordination occurs across all levels and elements of the health care system (e.g., EMS, public health, primary care, home care, long-term care).
Overview of Recommendations
The above five key elements remained the foundation—as well as the springboard—for the second phase of the committee’s work. In its phase two deliberations, the committee reviewed the six recommendations presented in the letter report (Box 1-2) and reaffirmed their fundamental validity and relevance to ongoing planning for catastrophic disaster response.
IMPACT OF THE 2009 LETTER REPORT
The six recommendations of the 2009 letter report are as relevant today as they were when the report was released. Since then, a number of private health care systems, as well as federal, state, and local governments, have begun CSC planning (as described below). Assessing the impact of the 2009 letter report not only provided the committee with feedback on how well the report met past needs, but also identified present needs and grounded the committee’s second phase of work with respect to addressing remaining gaps. This qualitative assessment of impact made use of search engines—Google, Medline, LexisNexis—to explore the potential impact on state and local CSC plan development processes.2 Impact also was assessed through discussions with the National Association of County and City Health Officials (NACCHO) and the Association of State and Territorial Health Officials (ASTHO) on behalf of their members, identification of salient presentations at conferences and workshops, and evidence from direct contact with state and local jurisdictions. The discussion below includes some notable examples of the letter report’s impact, but is not an exhaustive summary (e.g., because not all ongoing plans or efforts are published or publicly available). The committee recognizes that many state and local jurisdictions throughout the country continue to make significant progress in this and related areas.
Federal Impact
Centers for Disease Control and Prevention’s Public Health Preparedness Capabilities: National Standards for State and Local Planning
In March 2011, CDC published Public Health Preparedness Capabilities: National Standards for State and Local Planning as a guide for state and local health officials developing all-hazards preparedness capabilities. This guidance is among the first to focus on capabilities rather than a checklist of activities, leaving jurisdictions to decide where preparedness gaps currently exist and how to build sustainable, measurable capability in those areas; it identifies 15 core capabilities (CDC, 2011). For the first time, CSC plans are made a priority among medical surge capabilities. Specifically, “written plans should include processes (e.g., MOUs [memorandums of understanding] or other written agreements) to work in conjunction with [all entities involved in disaster response] to develop written strategies that clearly define processes and indicators as to when the jurisdiction’s [health care system] transition[s] into and out of conventional, contingency, and crisis standards of care” (CDC, 2011, p. 94). The 2009 letter report is listed as the first “suggested resource” to which states are advised to turn for specific guidance on priority issues. The inclusion of CSC as a priority in both the Hospital Preparedness Program (HPP) and Public Health Emergency Preparedness cooperative agreements opens up a potential source of federal funding for states and local jurisdictions to develop CSC plans (ASPR, 2011). In fact, the 2012 HPP guidance announcement specifically references the present report (ASPR, 2012), identifying both the text and templates as reference material useful to grantees in developing and implementing CSC plans as part of their broader surge capability. In delineating requirements for CSC plans, the 2012 HPP guidance mirrors the ethical principles, utility, and systems approach
_________________
2 The committee employed the following search parameters at several intervals during the period between February and November 2011 to capture information on impact. Databases searched: MedLine; Google Scholar; LexisNexis; New York Academy of Medicine; and the public websites of HHS, CDC, NACCHO, and ASTHO. Index terms included: Crisis Standard of Care, Altered Standard of Care, Allocation of Scarce Resources, Disaster Medicine, and Medical Practice Liability During Disasters. Limits: English; published on or after August 2009.
BOX 1-2
Recommendations from the 2009 Letter Report
Recommendation: Develop Consistent State Crisis Standards of Care Protocols with Five Key Elements
State departments of health, and other relevant state agencies, in partnership with localities should develop crisis standards of care protocols that include the key elements—and associated components—detailed in this report:
1. a strong ethical grounding;
2. i ntegrated and ongoing community and provider engagement, education, and communication;
3. assurances regarding legal authority and environment;
4. clear indicators, triggers, and lines of responsibility; and
5. evidence-based clinical processes and operations.
Recommendation: Seek Community and Provider Engagement
State, local, and tribal governments should partner with and work to ensure strong public engagement of community and provider stakeholders, with particular attention given to the needs of vulnerable populations and those with medical special needs, in
• developing and refining crisis standards of care protocols and implementation guidance;
• creating and disseminating educational tools and messages to both the public and health professionals;
• developing and implementing crisis communication strategies;
• developing and implementing community resilience strategies; and
• learning from and improving crisis standards of care response situations.
Recommendation: Adhere to Ethical Norms During Crisis Standards of Care
When crisis standards of care prevail, as when ordinary standards are in effect, health care practitioners must adhere to ethical norms. Conditions of overwhelming scarcity limit autonomous choices for both patients and practitioners regarding the allocation of scarce health care resources, but do not permit actions that violate ethical norms.
that were foundational for the committee’s 2009 letter report and that continue to inform and are expounded upon in the present report.
2011 National Level Exercise: Catastrophic Earthquake
The National Level Exercise (NLE) is an annual federally organized exercise designed to test and evaluate local, state, regional, and federal responses to a disaster. The scenario used in 2011 was a massive earthquake in the New Madrid Seismic Zone affecting eight states (Alabama, Arkansas, Illinois, Indiana, Kentucky,
Recommendation: Provide Necessary Legal Protections for Health Care Practitioners and Institutions Implementing Crisis Standards of Care
In disaster situations, tribal or state governments should authorize appropriate agencies to institute crisis standards of care in affected areas, adjust scopes of practice for licensed or certified health care practitioners, and alter licensure and credentialing practices as needed in declared emergencies to create incentives to provide care needed for the health of individuals and the public.
Recommendation: Ensure Consistency in Crisis Standards of Care Implementation
State departments of health, and other relevant state agencies, in partnership with localities should ensure consistent implementation of crisis standards of care in response to a disaster event. These efforts should include
• Using “clinical care committees,” “triage teams,” and a state-level “disaster medical advisory committee” that will evaluate evidence-based, peer-reviewed critical care and other decision tools and recommend and implement decision-making algorithms to be used when specific life-sustaining resources become scarce;
• Providing palliative care services for all patients, including the provision of comfort, compassion, and maintenance of dignity;
• Mobilizing mental health resources to help communities—and providers themselves—to manage the effects of crisis standards of care by following a concept of operations developed for disasters;
• Developing specific response measures for vulnerable populations and those with medical special needs, including pediatrics, geriatrics, and persons with disabilities; and
• Implementing robust situational awareness capabilities to allow for real-time information sharing across affected communities and with the “disaster medical advisory committee.”
Recommendation: Ensure Intrastate and Interstate Consistency Among Neighboring Jurisdictions
States, in partnership with the federal government, tribes, and localities, should initiate communications and develop processes to ensure intrastate and interstate consistency in the implementation of crisis standards of care. Specific efforts are needed to ensure that the Department of Defense, Veterans Health Administration, and Indian Health Services medical facilities are integrated into planning and response efforts.
Mississippi, Missouri, and Tennessee), which required coordinated disaster response over a period of days (FEMA, 2011). NLEs are constructed so that each element of the scenario corresponds to a measured task; the New Madrid scenario involved overwhelming participating emergency departments with hourly arrivals of trauma patients, sometimes at a ratio of 10:1 arriving trauma patients to available beds. This specific scenario element was meant to drive discussions of, among other things, CSC. The final NLE report had not been released as of this writing; however, the inclusion of CSC as a topic in an NLE demonstrates the issue’s penetration in federal emergency preparedness circles since 2009.
Department of Health and Human Services’ Response to the 2010 Haiti Earthquake
In her statements to the committee during the open session of its second meeting, ASPR’s Deputy Director for Preparedness Planning described how ASPR utilized the letter report to help guide its response to the 2010 Haiti earthquake (Knebel, 2011). As is typical of a no-notice disaster, the initial stages of international response were reactive, unstructured, and driven by clinical realities. Officials coordinating the U.S. response emphasized that treating injured Haitians locally was preferred to evacuating them to the United States. This decision was made in an effort to avoid further undermining the reconstruction of local medical infrastructure. It was also meant to avoid creating expectations for complex care that simply would not be available upon the repatriation of Haitian patients once their medical stabilization in the United States had been completed. For this reason and consistent with the committee’s 2009 letter report, ASPR established a Medical Review Board to guide medical evacuation decision making. The composition of the Medical Review Board included, but was not limited to, representatives from the Department of Defense, the U.S. Agency for International Development, HHS, the State Department, the Department of Homeland Security, and several nongovernmental organizations. Participants represented a variety of clinical specialties and administrative authorities. The Medical Review Board sought to establish consistent evaluation criteria for patients whose physicians were requesting evacuation, and reevaluated these initial criteria one week into the crisis based on dynamic situational realities. Its decision-making process was iterative and allowed for appeals based on the emerging medical circumstances of a patient. ASPR’s use of the letter report represents the first attempt to operationalize the guidance therein, and provided valuable real-world feedback for phase two of the committee’s work.
Department of Defense’s Response to the 2010 Haiti Earthquake
With the dispatch to Haiti of the USNS Comfort, a 1,000-bed hospital ship with 80 intensive care unit beds and numerous operating facilities, following the earthquake, the U.S. Navy initiated a “health care ethics committee” on board the ship in accordance with policies supported by the Navy’s Bureau of Medicine and Surgery. This committee comprised eight clinicians (four doctors and four nurses), one health care administrator, one lawyer, one chaplain, and a hospital corpsman. Its purpose was to help make decisions regarding the types of care rendered in this setting of limited resources. In addition, the committee ensured that such decisions were made in conjunction with input from the Haitian Ministry of Public Health and Population (Etienne et al., 2010).
Department of Health and Human Services’ Adaptation of the Letter Report into a Clinician’s Toolkit
In response to the letter report’s release, HHS convened a working group that adapted the letter report into an operational toolkit targeting state and local public health officials, health care institutions, and clinicians (HHS, 2009). Guidance for Crisis Standards of Care for Use in Disaster Situations: A Toolkit for Healthcare Practitioners (IOM, 2009) was designed to educate these groups on how to develop systematic and comprehensive protocols for allocating scarce resources during a disaster. The toolkit was offered to practitioners as one of HHS’s primary resources on the subject, to be coupled with simultaneous working group efforts on strategic planning for emergency department, outpatient, and inpatient management of the 2009 H1N1 pandemic.
Agency for Healthcare Research and Quality’s Evidence Review on the Allocation of Scarce Resources during Mass Casualty Events
To build on the work of the 2009 letter report, the Agency for Healthcare Research and Quality (AHRQ), through its Evidence-based Practice Centers, along with ASPR, commissioned a report comparing existing procedures and systems for allocating scarce resources during a mass casualty event (AHRQ, 2012). Before developing the present report, the committee had access only to a draft version of the AHRQreport, made available for public comment. The AHRQreport documents the quality and breadth of existing evidence on best practices for developing and implementing CSC at the federal, state, and local government levels and in the public and private sectors. To this end, a comprehensive, systematic review of the published literature on the allocation of scarce resources was conducted, and relevant governmental and nongovernmental plans, practice guidelines, and reports were examined. The provisional conclusion included in the draft for public comment is that research on the most effective ways to plan for the allocation of scarce resources is still nascent. The report proposes that ongoing efforts continue to focus on identifying the best protocols, techniques, and means for improving the capability and capacity to respond to mass casualty events at all levels of government.
State Impact
With the 2009 H1N1 influenza pandemic as a major driver, several states have initiated CSC planning efforts as part of broadening their overall surge capacity plans. Examples of plans that specifically reference the letter report’s framework demonstrate its impact. However, use of the framework as a guide has varied among states, and some states clearly are further ahead than others in their CSC planning efforts. The following is not an exhaustive summary of state efforts, and the committee recognizes that there are ongoing efforts in multiple states throughout the country not recorded here.
In Georgia, a public-private collaboration between the Department of Community Health and the Georgia Hospital Association adapted the letter report’s guidance into a template for regional hospitals. Both organizations further recommended the letter report as guidance for use by individual hospitals in specific organizational planning and potentially in implementation. As of April 2011, 86 percent of “eligible Georgia hospitals [had] submitted a signed Crisis Standards of Care Response Plan” incorporating the letter report’s best practices for managing and allocating scarce resources (Georgia Hospital Association, 2011).
In Texas, a multidisciplinary medical ethics workgroup was convened by the Texas Department of State Health Services in fall 2009 to make recommendations on state-owned critical resources for pandemic influenza. The final document, released in August 2010, included recommendations on the allocation and distribution of state-owned critical resources such as vaccines, antiviral medications, medical surge resources, and ventilators in an influenza pandemic. In addition to utilizing content from other ongoing state and local work, the workgroup was provided with the letter report for reference purposes (Texas Department of State Health Services, 2010).
Late in 2009, the Louisiana Department of Health and Hospitals, in conjunction with leaders of major hospitals and hospital coalitions, drafted CSC guidelines that, while not directly citing the letter report, retain its hallmarks of public-private collaboration. The guidelines delineate metrics describing when CSC
might go into effect; a standardized, regionalized CSC template (although each hospital can decide individually whether to adopt the plan); and patient characteristics that would drive CSC decisions depending on the specific resources in scarcity (Fink, 2009). Like the letter report, the Louisiana draft guidance incorporates public engagement as a hallmark of public education (through the opportunity for public comment) and allows for flexibility should clinical judgment be at odds with the developed guidance (especially when that judgment is based on an evolving incident). In September 2011, the Louisiana Department of Health and Hospitals referenced and incorporated the constructs of the letter report in its CSC documents (Louisiana Department of Health and Hospitals, 2011).
The state of Ohio finalized draft guidance on CSC planning—the Ohio Medical Coordination Plan. This plan was developed through a partnership between the Ohio Hospital Association and the Ohio Department of Health, and references the letter report as the foundation for its own ethical and legal considerations and standards for care in a disaster (Ohio Hospital Association and Ohio Department of Health, 2011). The plan also utilizes the care continuum detailed in the letter report. It recognizes that a “catastrophic event will lead to excessive demand over capacity and capability,” and therefore defines concrete “triggers” related to this divide between demand for and supply of available resources (Ohio Hospital Association and Ohio Department of Health, 2011, p. 4). The triggers indicate transitions along the care continuum from conventional to contingency to crisis care. As the present report was being published, the Ohio Hospital Association was leading the preparation of public engagement events to allow the public to comment on the new CSC strategy, a specific recommendation in the letter report (see Box 1-2).
Most recently, Michigan published finalized guidance titled Ethical Guidelines for Allocation of Scarce Medical Resources and Services during Public Health Emergencies in Michigan, in development throughout the course of both phases of the committee’s work (State of Michigan, 2012). Like the letter report, the Michigan plan identifies criteria for the allocation of scarce medical resources that can be adapted according to the particulars of a disaster. The plan provides specific guidance to relevant stakeholders, including EMS and health care facilities, and on broader issues such as the legal considerations associated with allocating scarce resources. The ethical principles on which the Michigan plan is founded closely resemble those laid out in the letter report while expanding on them to reflect a more specific sense of the values in the state. The Michigan plan sets forth allocation criteria that are generally acceptable as means of differentiating among patients (their relative medical prognoses and essential social functions, such as provision of health care); criteria that are acceptable only if prioritization within otherwise indistinguishable patient groups is required by the scarcity of resources (age; lottery; and first-come, first-served); and criteria that are unacceptable as a basis for making allocation decisions (e.g., race, ethnicity, general perceptions of social worth). The plan goes on to recommend strategies for implementing these criteria, including identifying triggers that signal the need to transition to CSC. Throughout the document, robust surge capacity planning and exercising are strongly encouraged to obviate the need for CSC in the first place.
Local Impact
At the committee’s first phase two meeting in April 2011, representatives of local public health departments briefed on the letter report’s impact at the level of local public health departments. One of the architects of the Seattle-King County Department of Public Health’s planning effort described the letter report as a
foundational framework that approached CSC planning from a multistakeholder perspective (Lien, 2011). Among a number of highlights, the identification of potential partnerships for the development of CSC plans was noted as a specific contribution. The deputy commissioner of the Chicago Department of Public Health said the letter report filled a need for national-level guidance that had previously been unmet (McKinney, 2011).
On the other hand, beyond its contribution to the literature, a representative of the Napa County, California, Department of Public Health said the letter report had had minimal penetration in many local health departments, especially the smaller, more rural ones. Among respondents to an informal (and limited) survey of some members of NACCHO, half had not heard of the letter report, and only one had used it to guide the CSC planning process (Smith, 2011). A number of factors contributed to this low penetration rate, especially the burden on local health departments of handling competing responsibilities and/or having to comply with federal, state, and other requirements. As a result of increasingly reduced funding, many health departments were undergoing a loss of departmental infrastructure (including that in the area of emergency preparedness) due to reductions in programs and personnel. Additionally, at the time of the letter report’s release, there was a pressing need to catalog the response to the H1N1 influenza outbreak, including the implementation of mass vaccination efforts in communities across the country. Nevertheless, progress had been made to date by some local public health departments across the nation in utilizing the letter report. Examples include those in Seattle-King County and Harris County (Texas), among others; some of these efforts are referenced later in this report (King County Healthcare Coalition et al., 2011; Shah, 2012). The difficulty of building an operational strategy for local health departments of varying resources and capabilities was a priority issue for the committee, and is discussed in greater detail in Chapter 5.
Impact on the Private Sector and Health Care Providers
While the private sector incorporates many of the health care providers who respond in a crisis, it also includes other actors that can contribute to CSC guidance at the state and national levels. An example of the letter report’s impact within the private sector is the March 2011 resolution adopted by the Alaska Public Health Association entitled Support for Legal Protections for Health Care Professionals Implementing Crisis Standards of Care (APHA, 2011). The resolution quotes and endorses the six recommendations in the letter report (Box 1-2). This example further demonstrates the ability of the letter report to act as a common foundation for planning efforts at the state level, whether those efforts are spurred by state governments, as in the Georgia and Louisiana examples above, or by private-sector stakeholders.
As was the case for local public health officials, the letter report had maximum penetration among individual health care providers in areas where the issue was already a priority (e.g., large metropolitan areas) (Smith, 2011). As was the case with local health departments, however, many providers that served medium-sized and small populations likely were unaware of the report. One of the greatest impediments to involving private-sector providers in CSC planning is related to the general disconnect that exists between private practitioners and the formal emergency response system at the local, regional, state, and federal levels. At a July 2011 provider workshop in Seattle-King County—where the public health department has made substantial progress in developing CSC plans, has conducted public engagement sessions on CSC, and has worked with a coalition of private-sector providers to leverage community resources—participants who
were aware of the letter report thought of it as primarily a foundational document (King County Healthcare Coalition et al., 2011). While they valued the context and standard guidance the letter report provided, they were interested in the operational details of the roles they might have to assume in planning and implementing CSC.
Conclusion
The following chapters of this phase two report and the templates therein build on the foundation of the 2009 letter report and the progress that continues to be made on plans for the development and implementation of CSC. An apparent conclusion from the committee’s review of the impact of its first report is that practical guidance for relevant stakeholders remains a burgeoning field; governments, EMS, hospitals, and providers within and external to the hospital system each have roles and responsibilities in preparing to allocate scarce resources, but the entire system should integrate its efforts if it is to be capable of responding successfully to a catastrophic disaster.
This report has a functional format and design that reflect its purpose of providing a resource manual for individuals and organizations responsible for planning and implementing disaster response. It is organized as a series of stand-alone resources for ease of use and reference. The first volume includes Chapters 1 through 4. Following this introduction, the next three chapters establish a framework for a systems approach to the development and implementation of CSC plans (Chapter 2), and address the legal issues (Chapter 3) and the ethical, palliative care, and mental health issues (Chapter 4) that agencies and organizations at each level of a disaster response should address.3
The next four chapters are bound as separate volumes, each aimed at a key stakeholder group—state and local governments (Chapter 5), EMS (Chapter 6), hospitals and acute care facilities (Chapter 7), and out-of-hospital and acute care systems (Chapter 8). The text of the chapters defines the roles and responsibilities of these stakeholders, describes operational considerations associated with their development and implementation of CSC plans, and provides brief descriptions of templates that outline the specific functions and tasks for each stakeholder when allocating scarce resources in response to a disaster. The templates are easily located at the end of each chapter by the red bar that runs the length of each page.
Chapter 9, again published as a separate volume, includes a brief description of the committee’s work to design the public engagement toolkit and the tools themselves.4
The final volume of the report consists of six appendixes: a glossary of terms used in the report (Appendix A), a sample hospital CSC plan (Appendix B), a listing of potentially scarce medical resources (Appendix C), a listing of resource challenges by disaster type (Appendix D), the committee’s statement of task (Appendix E), and biographical sketches of the committee members (Appendix F).
_________________
3 All figures included in the report are original and generated by the committee, unless otherwise indicated.
4 The templates in Chapters 5-8 and the public engagement toolkit can also be downloaded via the project’s website: http://iom.edu/Activities/PublicHealth/DisasterCareStandards.aspx.
AHRQJAgency for Healthcare Research and Quality). 2012. Allocation of scarce resources during Mass Casualty Events (MCEs) [draft for public comment]. Rockville, MD: AHRQ.
APHA (Alaska Public Health Association). 2011. Support for legal protections for health care professionals implementing crisis standards of care. Fairbanks, AK: APHA, http://www.alaskapublichealth.org/images/stories/Resolutions/2011-03_Legal_Protection_during_Crisis.pdf (accessed June 3, 2011).
ASPR (Assistant Secretary for Preparedness and Response). 2011. FY11 Hospital Preparedness Program (HPP) guidance. Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/hpp/Documents/fy2011-hpp-funding-guidance.pdf (accessed January 18, 2012).
ASPR. 2012. Healthcare preparedness capabilities: National guidance for healthcare system preparedness. Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/hpp/reports/Documents/capabilities.pdf (accessed February 14, 2012).
CDC (Centers for Disease Control and Prevention). 2011. Public health preparedness capabilities: National standards for state and local planning. Atlanta, GA: CDC, http://www.cdc.gov/phpr/capabilities/DSLR_capabilities_July.pdf (accessed March 30, 2011).
Etienne, M., C. Powell, and D. Amundson. 2010. Healthcare ethics: The experience after the Haitian earthquake. American Journal of Disaster Medicine 5(3):141-147.
FEMA (Federal Emergency Management Agency). 2011. National Level Exercise 2011 (NLE 11): Quick Look Report (QLR). Washington, DC: FEMA, http://www.fema.gov/pdf/media/factsheets/2011/nle11_quick_look_report.pdf (accessed June 17, 2011).
Fink, S. 2009 (December 27). Louisiana health professionals drafting guidelines on access to critical care during a disaster. ProPublica and New Orleans Times-Picayune, http://www.propublica.org/article/louisiana-professionals-draftingdisaster-critical-care-access-guidelines (accessed June 1, 2011).
Georgia Hospital Association. 2011. Crisis standards of care in Georgia. Atlanta, GA: Georgia Hospital Association, https://www.gha.org/weekly/ZipPack0421.pdf (accessed June 1, 2011).
HHS (Department of Health and Human Services). 2009. H1N1 compendium: A resource for H1N1-specific response guidance. Washington, DC: HHS, http://www.flu.gov/professional/hospital/h1n1compendium.pdf (accessed October 11, 2011).
IOM (Institute of Medicine). 2009. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press, http://www.nap.edu/catalog.php?record_id=12749 (accessed September 6, 2011).
King County Healthcare Coalition, Swedish Medical Center, and Public Health-Seattle and King County. 2011 (July 14). Planning for crisis standards of care: Establishing the path forward for King County. Seattle, WA: King County Healthcare Coalition.
Knebel, A. 2011 (July 11). The role of the federal government in CSC during a disaster. Remarks presented at the Second Meeting of the IOM Committee on Guidance on Establishing Standards of Care for Use in a Disaster Situations, Washington, DC.
Lien, O. 2011 (May 10). Impact of2009 IOM letter report: Implementation progress, challenges, and metrics for Public Health-Seattle and King County. Remarks presented at the First Meeting of the IOM Committee on Guidance on Establishing Standards of Care for Use in a Disaster Situations, Washington, DC.
Louisiana Department of Health and Hospitals. 2011. Crisis standards of care summary. Baton Rouge, LA: Louisiana Department of Health & Hospitals, http://new.dhh.louisiana.gov/assets/oph/Center-PHCH/Center-CH/infectious-epi/InfluenzaZCSOCPublicFLYERvs210132011.pdf (accessed February 5, 2012).
McKinney, S. 2011 (May 10). Impact of 2009 IOM letter report: Implementation progress, challenges, and metrics for Chicago Department of Public Health. Remarks presented at the First Meeting of the IOM Committee on Guidance on Establishing Standards of Care for Use in a Disaster Situations, Washington, DC.
Ohio Hospital Association and Ohio Department of Health. 2011 (June 10). Ohio medical coordination plan. Columbus, OH: Ohio Hospital Association and Ohio Department of Health.
Quarantelli, E. L. 2000. Emergencies, disaster and catastrophes are different phenomena. University of Delaware Disaster Research Center Preliminary Paper #304, http://dspace.udel.edu:8080/dspace/bitstream/handle/19716/674/PP304.pdf?sequence=1 (accessed February 1, 2012).
Shah, U. 2012 (January 13). Summary of HCPHES pandemic influenza public and Pandemic Influenza Public and partner engagement projects Partner Engagement Projects. Harris County, TX: Harris County Public Health and Environmental Services.
Smith, K. 2011 (May 10). Impact of 2009 IOM letter report: Implementation progress, challenges, and metrics for Napa County Health and Human Services, California. Remarks presented at the First Meeting of the IOM Committee on Guidance on Establishing Standards of Care for Use in Disaster Situations, Washington, DC.
State of Michigan. 2012. Ethical guidelines for allocation of scarce medical resources and services during public health emergencies in Michigan. Lansing, MI: Department of Community Health, Office of Public Health Preparedness.
Texas Department of State Health Services. 2010. Final after action report: Texas Department of State Health Services response to the novel H1N1 pandemic influenza (2009 and 2010). Report number DSHS-2010-01-FINAL. Austin, TX: Texas Department of State Health Services, http://pandemicpreparations.org/files/566/566_aar.pdf (accessed February 13, 2012).
Volume 1 2: Catastrophic Disaster Response
Creating a Framework for Medical Care Delivery
When the committee reconvened in May 2011, it became clear that while the key elements and recommendations of the 2009 letter report, summarized in Chapter 1, remained a valid starting point for discussion of the issues related to crisis standards of care (CSC) planning, the depth, complexity, and scope of CSC planning and implementation would benefit from the use of a complex, dynamic systems approach. A system is composed of regularly interacting or interrelated components that can function independently (Merriam-Webster Dictionary, 2012). A systems approach is defined as a “management strategy that recognizes that disparate components must be viewed as interrelated components of a single system, and so employs specific methods to achieve and maintain the overarching system. These methods include the use of standardized structure and processes and foundational knowledge and concepts in the conduct of all related activities” (George Washington University Institute for Crisis, Disaster and Risk Management, 2009, p. 59). A systems approach views any organization as a unified, purposeful system composed of interrelated parts that, when woven together, create effective and efficient processes that improve upon the independent functioning of each individual component.
Where investments in disaster preparedness have proved successful in the decade since September 11, 2001, efforts to integrate the spectrum of relevant emergency response disciplines—health care, emergency medical services (EMS), public health, public safety, and emergency management—have been a priority. Much of this work has been focused on conventional disaster incidents that do not stress the capacity and capabilities of the health care system in a sustained or unprecedented way, allowing health and medical care to be delivered in the usual manner. The capacity and capabilities (Barbera and MacIntyre, 2007) required to manage such disaster incidents are in place, albeit in varying states of configuration, maturity, and functionality. However, systems to manage the truly catastrophic incidents that are the subject of this report, in which overwhelming numbers of casualties and cascading failures of infrastructure compound the incident, are rudimentary at best. As a result, in its renewed deliberations on developing and implementing CSC, the committee recognized the demand for a rigorous systems approach.
CONCEPTUALIZING A SYSTEMS APPROACH TO DISASTER RESPONSE
This section broadly outlines a framework for disaster response of which CSC is only one, albeit a critical, aspect. However, the development and implementation of CSC plans are the means to mount a response
to an incident that far exceeds the usual health and medical capacity and capabilities. Therefore, the same elements that come together to build any successful disaster response should also be used to develop robust CSC plans and guide their implementation.
Figure 2-1 illustrates the systems framework that the committee believes should inform the development and implementation of CSC plans. It is based on the five key elements of planning set forth in the 2009 letter report (see Table 1-1 in Chapter 1), which served as the starting point for the development of the committee’s recommendations in that report and are foundational for all disaster response planning. The figure depicts a strong foundation of underlying principles; steps needed to achieve the implementation of disaster response; and the pillars of the disaster response system, each separate and yet together supporting the jurisdictions—local, state, and federal governments—with the overarching authority for ensuring that CSC planning and implementation occur.
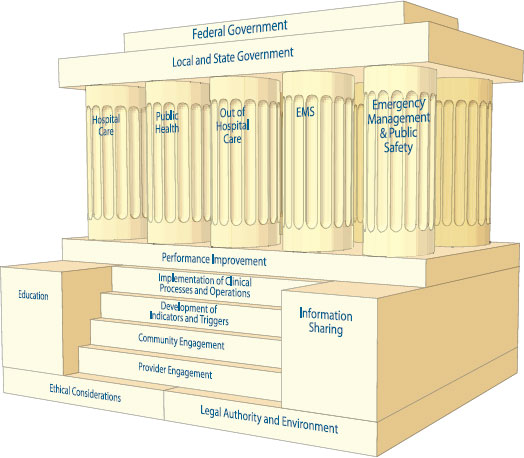
FIGURE 2-1
The foundation for CSC planning comprises ethical considerations and legal authority and environment, located on either side of the steps leading up to the structure. The steps represent elements needed to implement disaster response; education and information sharing are the means for ensuring that performance improvement processes drive the development of disaster response plans. The response functions are performed by each of the five components of the emergency response system: hospitals and acute care, public health, out-of-hospital and alternate care systems, prehospital and emergency medical services, and emergency management/public safety. While these components are separate, they are interdependent in their contribution to the structure; they support and are joined by the roof, representing the overarching authority of local, state, and federal governments.
The two cornerstones for the foundation of this framework are the ethical considerations that govern planning and implementation and the legal authority and legal environment within which plans are developed. Ethical decision making is of paramount importance in the planning for and response to disasters. Without it, the system fails to meet the needs of the community and ceases to be fair, just, and equitable. As a result, trust—in professionals, institutions, government, and leadership—is quickly lost.
For public health, emergency responders, and health care professionals, the duty to care resonates deeply, and the duty to plan for such incidents is an ethical imperative. All stages of planning and implementation of disaster response should be guided by the universal ethical values of fairness, transparency, consistency, proportionality, and accountability. Adherence to ethical values is particularly important when professionals must operate in a crisis in which resources are scarce and the needs of the population should be considered. Incorporating these principles ensures that in stewardship of available scarce resources, the best possible care is given to individuals and the population as a whole. Thus, delivery of health care under crisis standards is ultimately about maximizing the care delivered to the population as a whole under austere circumstances that may limit treatment choices for both providers and patients. Ethical guidance ensures that decisions about allocating scarce resources stem from ethically and legally sound policies that promote population health and align with community values. Individuals who may not meet criteria for intensive curative measures should still receive compassionate palliative care.
The legal authority and legal environment within which CSC plans are developed are the other cornerstone of the framework’s foundation. The legal authority and environment support the necessary and appropriate actions in response to a disaster.
Between those two cornerstones of the foundation are the steps needed to ensure that the development and implementation of CSC plans occur. They include provider and community engagement efforts, development of a process that permits individual communities to identify regionally coordinated and consistent indicators that denote a change in the usual manner of health care delivery during a disaster, and the triggers that should be activated in order to implement CSC. These lead to the top step, the implementation of clinical processes and operations that support the disaster response. All of these efforts are supported and sustained by an ongoing performance improvement process, an important element of any systems approach to monitor demand (improving situational awareness), evaluate the impact of implementation, and establish/share best practices. This process includes education of and information sharing among organizations and individuals responsible for both the planning and response phases of a disaster.
The pillars of medical surge response—hospital and out-of-hospital medical care; public health; EMS; and emergency management/public safety agencies, organizations, and authorities—stand on this strong base. Each of these pillars is an element of the disaster response system, representing a distinct discipline, but all need to be well integrated to ensure a unified disaster response. One acting independently of the others may delay, deter, and even disrupt the delivery of medical care in a disaster. Many of these disciplines work together during daily operations. For example, EMS transports bridge the out-of-hospital and hospital communities, public health bridges the public safety and hospital communities, and emergency management bridges the hospital and public health communities. But rarely, and in few communities, do all of these response elements come together in a manner that can ensure oversight and care for an overwhelming number of disaster victims (Arlington County, 2002; Commission on the Prevention of WMD Proliferation and Terrorism, 2008). The more complex and dynamic the incident, the more important strong and effective
coordination and integration among the pillars becomes, as emphasized by a systems approach. Priorities and objectives should be shared across the entire system to inform the development of unified strategies and the coordinated tactics required to implement them. Applying National Incident Management System/ National Response Framework principles and systems can help improve coordination and ensure the desired outcomes.
Atop the pillars are local, state, and federal government functions. Government at all three levels has an overarching responsibility for the development, institution, and proper execution of CSC plans, policies, protocols, and procedures. Good governance encompasses the functions of monitoring and evaluation, as well as accountability and meaningful contributions to policy development (Gostin and Powers, 2006). These functions are especially important in developing plans related to incidents in which the confidence of the public in government institutions may come into question, and the risk of cascading failures and multisector disruption, exacerbated by a lack of coordinated response, can mean the difference between thousands of lives lost and saved (OSTP, 2010).
FUNDAMENTAL FACTORS THAT INFLUENCE THE IMPLEMENTATION OF CRISIS STANDARDS OF CARE
While the previous section sets forth a broad systems approach to the development and implementation of CSC, this section addresses three fundamental factors that influence the need to implement CSC. First is the impact of situational awareness on decision making during a disaster. Without it, triage decisions will likely be made in the absence of information about the scope or scale of the demand on resources. Those providing care may not know when to adjust their approach to medical care delivery and which resources require conservation. In the worst-case scenario, this lack of knowledge may exacerbate the scarcity of already limited resources. Second, the extent to which a community can adjust to care for a significantly larger patient population, or its ability to implement surge capacity plans, will influence the need to implement CSC in response to a catastrophic disaster. Finally, individual communities can prepare several medical and public health supply-side mechanisms as a bulwark against the large patient increases expected during a disaster, thus reducing or eliminating the need to implement CSC.
The Impact of Situational Awareness on Decision Making During a Disaster
The equitable, just, and effective delivery of care under disaster response conditions begins with the need to establish good situational awareness, with a common operating picture shared by all components of the disaster response system. At the outset of any disaster incident, particularly one in which there is a no-notice impact, decision making about resource allocation will necessarily be based on reactive choices. A lack of context, including the scope and scale of the incident and the number of casualties generated, will likely lead to ad hoc decision making that may result in greater numbers of casualties if dwindling resources are not appropriately conserved, as well as inequities in allocating scarce resources, unethically disadvantaging some from receiving care. As the 2009 letter report emphasized, situational awareness is critical to transitioning decision making from a reactive to a proactive mode. A proactive approach to patient triage and resource allocation will, of necessity, be a structured, systems approach that weighs demand against resource avail-
TABLE 2-1
Reactive Versus Proactive Triage for Various Features of a Disaster
| Feature | Reactive | Proactive |
| Incident type | Often no-notice incident (usually static or short timeline [e.g., earthquake, bombing]); triage occurs early in incident time frame | No-notice incident or anticipated, often dynamic incident (e.g., pandemic influenza); triage occurs later in incident time frame |
| Incident management implemented fully? | No (full implementation is transition point to proactive mode) | Yes |
| Situational awareness | Poor | Good |
| Resource availability | Extremely dynamic (over hours) | Relatively static or more gradual changes |
| Resource shortfall(s) | Stabilization care through definitive care | Definitive care, selection of medications or therapies |
| Dominant triage* | Primary, secondary | Tertiary |
| Most likely resource triaged | Operative care (may not be able to provide any operative care if massive incident), diagnostic imaging, fluid resuscitation or medications | Mechanical ventilation/critical care (improvised nuclear device is an exception because of delayed radiation illness) |
| Triage decision maker | Triage officer(s) on initial assessment | Triage team |
| Triage decision basis | Clinical assessment | Clinical assessment plus diagnostics (decision tool) |
| Decision making | Unstructured, ad hoc | Structured |
| Regional and state guidance and legal protections | No or limited | Yes |
| Regional partner assistance | Available | Unavailable (usually) |
* Primary triage: performed at first assessment and prior to any interventions (e.g., triage upon entry to the emergency department or by emergency medical services (EMS) providers at a disaster scene). Secondary triage: performed after additional assessments and initial interventions (e.g., triage performed by surgery staff after administration of intravenous fluids and initial CT scan). Tertiary triage: performed after definitive diagnostics and medical care are performed or are ongoing (e.g., triage performed by critical care staff after intubation and mechanical ventilation with assessment of physiologic variables).
ability. Table 2-1 lists the characteristics of reactive versus proactive triage for various features of a disaster. Boxes 2-1 and 2-2, respectively, present examples of these two modes of response. Developing an approach to proactive triage helps optimize the potential health care outcomes, reducing morbidity and mortality in public health emergencies.
Surge Capacity and Capability
CSC planning should be linked to ongoing planning efforts by federal, state, and local governments and health care institutions focused on surge capacity and capability (see Box 2-3 for definitions). The Medical Surge Capacity and Capability (MSCC) framework, for instance, is a management system for integrating medical and health resources during disasters that was incorporated into the Hospital Preparedness Program guidance in 2006 (HHS, 2007). The integration of CSC into this framework is discussed in detail in the next section (HHS, 2007). In the MSCC framework, as in emergency response systems in general, much of the planning effort is focused on mass casualty and disaster incidents, including the expansion of clinical
BOX 2-1
An Example of Reactive Crisis Care: The Joplin, Missouri, Tornado
On May 22, 2011, an EF-5 tornado struck the town of Joplin, Missouri, at 5:17 PM, with direct impact on Mercy/St. John’s Medical Center, which held 183 patients at the time. Major structural damage occurred, and all critical systems were lost. Gas and water leaks, falling debris, and other hazards were pervasive. Within minutes, patients were presenting to the emergency department for care even though the structure was unsafe. Inpatient units rapidly evacuated patients to predesignated areas, and private vehicles (with some emergency medical services [EMS] assistance) were used to shuttle them to other area hospitals.
In the emergency department, usual supplies and medications could not be accessed because of electronic controls on pharmaceuticals and damage to supplies, but life-saving procedures continued to be performed in the dark, with limited equipment. These included intubations, insertion of chest tubes, and hemorrhage control. The emergency physicians on duty balanced the hazards in the department with the threats to life and made decisions about what interventions could not wait until patients could get to a safer area.
Communications were difficult to nonexistent, and each unit had to rely on its personnel and their levels of training and comfort in taking action to move patients to safety and provide life-saving interventions. The hospital was successfully evacuated in 90 minutes, a tremendous credit to the personnel and their training and ability to adapt. Emergency services were transitioned to a nearby hospital, and an alternate care site was established and supplied with staff and materials as better communications and situational awareness were obtained. The following key points emerge from this example:
• In reactive crisis care, actions of unit personnel are critical to success.
• Appropriate training, exercising, and job aids are core aspects of preparedness for unit staff.
• Hospital evacuation plans may have to be implemented with minimum central coordination.
• Triage decisions should balance interventions (and their complexity and time demands) against the benefits of the interventions and any hazards of the environment.
• Reactive triage decisions rely on the clinical training of providers and the supplies at hand.
• Supplies (especially pharmaceuticals) may be inaccessible if power is lost, and contingencies should be available.
• An alternate care site plan is important, particularly if the hospital is the only such facility in the immediate area.
SOURCE: Kikta, 2011; http://www.mercy.net/joplin/media-coverage.
operations, commonly referred to as surge capacity (Barbera and MacIntyre, 2007; Barbisch and Koenig, 2006; Hanfling, 2006; Hick et al., 2004, 2009; Hodge and Brown, 2011; Kaji et al., 2006). Surge capacity can be envisioned as occurring along a continuum based on resource availability and demand for health care services (see Box 2-4). One end of this continuum is defined by conventional responses—those services that are provided in health care facilities on a daily basis and are expanded for disaster planning and response. At
the other end of the continuum is crisis care, when the best possible care is provided to the population of patients as a whole because of the very limited resources available. Significant changes are made in the methods and locations of care delivery, and decision-making shifts from patient-centered to population-centered outcomes. Crisis surge planning should be an integral part of overall surge capacity planning. Emergency plans, training, and exercises should reflect the continuity of care along this continuum, as opposed to the development of separate, stand-alone plans. Figure 2-2 illustrates how a surge response may shift across the continuum from conventional to crisis care based on the demand and supply mismatch that may occur over time, particularly as it affects the availability of patient care spaces; staff; and needed supplies, equipment, and pharmaceuticals. This crisis component remains a significant deficit in many emergency plans (Bascetta, 2010).
The Effect of Preparedness on Crisis Response
The continuum of surge capacity—conventional, contingency, or crisis—and the corresponding standards of care will be greatly influenced by supply-demand factors. Any incident in which the available resources are outstripped by the demand for care will necessarily result in a shift in the delivery of care from conventional toward contingency or even crisis standards (Figure 2-3). Note that contingency care is defined as providing “functionally equivalent” care, although care is rendered using different methodologies, medications, and locations. The difficulty arises as care shifts toward a crisis standard, whereby care may not be initiated and may conceivably be withdrawn from selected patients so it can be reallocated to others who may be considered more likely to survive.
Pandemic influenza preparations over the past few years highlight the importance of expanding surge capacity response from the traditional health care setting to the community. These preparations included the development of plans for delivering care in alternate care systems (Cinti et al., 2008; Lam et al., 2006; Weiss et al., 2010); developing more robust home health care options (DHS, 2009); changing EMS destination choices, EMS unit dispatch options, and the scope of practice of EMS agencies (AHRQ, 2009; Courtney et al., 2010) ensuring the availability of traditional, private practice, ambulatory-based care (CDC, 2009); and exploring the use of “flat-space” areas in the management of patients in nontraditional areas of a hospital (Cruz et al., 2010; Hick et al., 2004; Kelen et al., 2009). The intent of creating a stratified model of health care delivery during emergency incidents is to preserve the hospital setting for those patients who are most in need of hospital-level care (Hanfling, 2009). Stratification implies the matching of patients’ health care needs with a level of care capable of meeting those needs. This matching is more likely to be effective in a slow-onset sustained incident, such as a pandemic, as opposed to a sudden, no-notice incident, in which the time required to establish this stratified system presents obvious difficulties. Yet the importance of such efforts, even in the no-notice context, cannot be discounted. For example, current planning for response to detonation of an improvised nuclear device, the ultimate no-notice incident, includes the development of an alternate care system (Coleman et al., 2009). The greater the extent to which such systems are developed before the onset of an incident, the more likely such efforts are to be successful (Schultz et al., 2003).
Utilizing the full range of available medical resources, not simply relying on hospital-based care, is of paramount importance in a disaster to avoid having to shift to CSC. Resource availability influences the supply side of the health care delivery balance. Resources in the acute care sector include not just hospi-
BOX 2-2
An Example of Proactive Incident Response: The H1N1 Pandemic
The 2009 H1N1 pandemic provided an opportunity for hospitals to test plans for surge capacity and allocation of scarce resources. Although not perceived to be a “crisis” (the pandemic was relatively mild), the incident required structured and evidence-based use of allocation criteria. While the resulting mortality (12,469 victims) was substantially less than in prior seasonal influenza epidemics, the pandemic provided an opportunity to further develop and evaluate systems for future, more severe epidemics. Notably, as a result of variations in priority group policies and distribution of vaccine, significant public relations issues developed within communities and across state borders (for example, health care workers with similar functions were a priority group for vaccination in one state and not another).
This incident featured the following key aspects of allocation/policy development:
Federal:
• Emergency use authorizations for selected antivirals
• Public health emergency declaration
• Allocation guidance for vaccine (priority groups)
• Allocation guidance for antiviral medications (priority groups)
• Guidance on use of personal protective equipment (PPE)
• Distribution of Strategic National Stockpile (SNS) masks, antivirals, and other materials
• Epidemiologic monitoring
State:
• Refinement of priority groups and distribution of limited vaccine
tal beds but also the equipment, supplies, pharmaceuticals, and staff needed to attend to patients. These resources can be augmented through a variety of strategies (Hanfling, 2006; Minnesota Department of Health, 2008; Rubinson et al., 2008a,b), including the development of hospital-based caches of supplies, equipment, and pharmaceuticals or expansion of such efforts as part of the development of local stockpiles. Resources may also become available from external supplies through resupply from vendors, access to external disaster caches (such as the Strategic National Stockpile), or materiel support via hospital coalitions and other mutual-aid agreements.
In addition, health care providers can take specific steps to steward available medical resources, making them last longer during an incident in which those resources may be in short supply or the means to replace them compromised. The 2009 letter report described the resource-sparing strategies that can be implemented when an incident occurs (Hick et al., 2009), which range from conservation; to substitution and adaptation of specific items in short supply; to reuse; to, in the worst-case scenario, reallocation. These strategies, too, are directly correlated with the prevailing standard of care under which treatment is delivered to patients during a disaster: conservation and substitution would be expected to occur under conditions of
• State and local guidance on utilization of N95 masks and PPE, distribution of SNS materials
• Coordination of policies among hospitals, clinics, and emergency medical services (EMS)
• Coordination of risk communication
• Situational status monitoring between local and federal levels
• Refinement of guidance on allocation of ventilators and other scarce resources for possible use
Local/coalition:
• Distribution and use of caches and supplied N95 masks and medications
• Triage mechanism for durable medical equipment
• Development (and in some cases activation) of “flu centers"
• Use of surge capacity plans, especially for outpatient surge, and particularly at children’s hospitals and those serving pediatric populations
• Use of alternate care sites associated with hospitals and clinics for outpatient care overflow
• Provision of joint information to the community
• Coordination with EMS on transport of suspect cases and coordination of “when to transport” if the situation worsens
• Coordination of vaccine and antiviral distribution
• Standard policies for PPE use by health care workers (which, in at least one case, was noted by the Occupational Safety and Health Administration [OSHA] as a best practice)
• Standard visitor infection control policies and hours among hospitals
• Phone triage/hotline information
SOURCES: CDC, 2010a,b; Chung et al., 2011; Scarfone et al., 2011; http://www.flu.gov/planning-preparedness/hospital/hospitalchecklist.pdf.
conventional or contingency surge response; adaptation and reuse would be expected to occur under conditions of contingency or crisis surge response; and reallocation of scarce resources would most likely occur only under CSC.
Figure 2-3 shows that as the demand for health care services (y-axis, left) rises rapidly over time (x-axis)—thereby resulting in a decrease in the immediate availability (supply) of resources (y-axis, right)—there may be a shift from conventional to contingency or crisis care. Figure 2-4 shows these same relationships with the added variable of preparedness. The degree to which any community demonstrates enhanced versus limited preparedness will likely affect the transition to contingency or crisis standards of care, represented graphically as the area between the intersecting lines. What is apparent from the analysis of these relationships is that a combination of positive influences on the supply of resources—especially management of the demand and expectations for patient care along with efforts to improve preparedness—will have an ameliorating effect that essentially allows conventional standards of care to continue for a longer period of time than if no such influences were present. Indeed, negative influences on supply and demand, such as poor risk communication strategies, decreased availability of medical providers, and a lack of preparedness efforts, may place
BOX 2-3
Surge Capacity and Capability
Surge Capacity: “The ability to evaluate and care for a markedly increased volume of patients—one that challenges or exceeds normal operating capacity. The surge requirements may extend beyond direct patient care to include such tasks as extensive laboratory studies or epidemiological investigations” (ASPR, 2010a).
Surge Capability: The ability to manage patients requiring unusual or highly specialized medical evaluation and care. Surge requirements span the range of specialized medical and health services (expertise, information, procedures, equipment, or personnel) that are not normally available at the location where they are needed (e.g., pediatric care provided at nonpediatric facilities or burn care services at a nonburn center). Surge capability also includes patient problems that require special intervention to protect medical providers, other patients, and the integrity of the medical care facility (ASPR, 2010b).
BOX 2-4
Conventional, Contingency, and Crisis Care
Conventional Capacity: The spaces, staff, and supplies used are consistent with daily practices within the institution. These spaces and practices are used during a major mass casualty incident that triggers activation of the facility emergency operations plan.
Contingency Capacity: The spaces, staff, and supplies used are not consistent with daily practices but provide care that is functionally equivalent to usual patient care. These spaces or practices may be used temporarily during a major mass casualty incident or on a more sustained basis during a disaster (when the demands of the incident exceed community resources).
Crisis capacity: Adaptive spaces, staff, and supplies are not consistent with usual standards of care, but provide sufficiency of care in the context of a catastrophic disaster (i.e., provide the best possible care to patients given the circumstances and resources available). Crisis capacity activation constitutes a significant adjustment to standards of care.
SOURCE: Hick et al., 2009.
a community in greater jeopardy of exceeding the availability of health care resources, resulting in an earlier transition from conventional to contingency or crisis standards of care.
The precious factor of time also affects the well-being of any community afflicted by disaster. Delays in attaining situational awareness, anticipating resource shortfalls, or making appropriate requests for assistance
FIGURE 2-2
Allocation of specific resources along the care capacity continuum.
NOTE: ICU = intensive care unit; PACU = postanesthesia care unit.
a Unless temporary, requires state empowerment, clinical guidance, and protection for triage decisions and authorization for alternate care sites/ techniques. Once situational awareness achieved, triage decisions should be as systematic and integrated into institutional process, review, and documentation as possible.
b Institutions consider impact on the community of resource use (consider “greatest good” versus individual patient needs—e.g., conserve resources when possible), but patient-centered decision making is still the focus.
c Institutions (and providers) must make triage decisions—balancing the availability of resources to others and the individual patient’s needs—shift to community-centered decision making. SOURCE: IOM, 2009, p. 53.
all can result in a crisis situation (Figure 2-4). Elimination of these delays requires practiced incident management, a common operating picture in place, recognition of indicators of the need for contingency and crisis response, and establishment of CSC plans, all within the overarching construct of the disaster response framework.
GUIDANCE FOR DISASTER RESPONSE STAKEHOLDERS
Following is a brief overview of the roles and responsibilities of each pillar of the disaster response framework—federal, state, and local governments; EMS agencies; hospital and acute care facilities; and out-of-hospital and alternate care systems—in developing and implementing CSC plans. A detailed discussion of the functions and tasks of each stakeholder can be found in Chapters 5-8, respectively. Complementing this specific guidance is the discussion of legal issues relevant to CSC in Chapter 3 and the examination of core cross-cutting issues that affect organizations and agencies at each level of disaster response in Chapter 4.
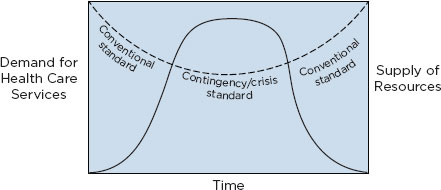
FIGURE 2-3
Demand for health care services and supply of resources as a function of time after disaster onset.
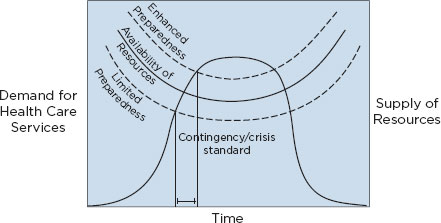
FIGURE 2-4
Demand for health care services and supply of resources as a function of time after disaster onset, taking into account care capacity as a function of time.
Federal, State, and Local Governments
Federal Government
The federal government (primarily the Department of Health and Human Services [HHS]) will continue to lead efforts to support and encourage the development of CSC plans for use in catastrophic disaster situations, primarily through continued emphasis on the importance of coordinating such planning within the larger context of surge capacity planning as part of a disaster response framework. Inclusion of specific language in HHS’s Hospital Preparedness Program and the Centers for Disease Control and Prevention’s (CDC’s) Public Health Emergency Preparedness cooperative agreements is the best way for the federal government to exert a positive influence on state government planning, which should be the ultimate driver of such efforts.
Federal agencies, particularly HHS (e.g., the Assistant Secretary for Preparedness and Response and
CDC), will play critical roles in helping to define triage strategies for available resources, such as access to vaccines or other medical countermeasures that may be in short supply. The federal government will also play an important role in augmenting health care delivery as part of the disaster response effort. The National Disaster Medical System (NDMS) can provide personnel, supplies, and patient evacuation services within affected areas and patient care outside of immediately affected areas. And the Strategic National Stockpile, managed by CDC, has the goal of getting an initial infusion of necessary medical countermeasures and equipment on the ground at a disaster site within 12 hours, and supplementing those resources with continued shipments in the days following the incident. There may also be a role for federal responders to serve as members of interstate triage teams, possibly under the auspices and legal protection of the NDMS.
The Department of Defense (DOD) and the Department of Veterans Affairs (VA) play major roles in disaster planning and response. DOD medical treatment facilities and VA medical centers and community-based outpatient clinics should support regional and state plans to implement CSC. Although these government facilities are part of a national health care delivery system, support to local communities is an important part of their humanitarian mission. Should a large region be affected, coordination with all affected health care systems and levels of government will be required; therefore, inclusion of DOD and the VA in the planning process is of major significance.
Finally, although states have primary responsibility for legal standards relating to tort liability, scope of practice, and the like, the federal government has a role to play here as well, particularly for health professionals who respond under the auspices of the NDMS. The federal government can also waive regulatory restrictions or sanctions (e.g., for failing to comply with certain Emergency Medical Treatment and Active Labor Act requirements) and waive the documentation requirements of Medicare and Medicaid, all of which facilitate the delivery of medical care under crisis conditions.
State and Local Governments
The leadership of state and local governments is paramount in the initiation of CSC planning and implementation. This is especially true because public health and governmental EMS agencies operate under the direct auspices of state and local government authority. It becomes more difficult to address CSC planning outside of state and local government influence, especially in the private health care sector. In this regard, a systems approach to planning ensures the unification of efforts, particularly with respect to the consistency of plan development and implementation.
One useful way to envision the relationship among hospital, public health, and local, state, and federal government functions is to think of CSC planning in the context of the Medical Surge Capacity and Capability framework (Barbera and MacIntyre, 2007). In Figure 2-5, this framework is adapted to include some of the specific functional elements described in the 2009 letter report, including the creation of state and regional disaster medical advisory committees and the role of triage teams, clinical care committees, and palliative care teams. The figure depicts how CSC planning and implementation occur across the continuum from individual health care institutions, to health care coalitions spanning multiple jurisdictions, to the state and federal levels. The figure shows the locations at which key emergency management functions occur, and so demonstrates how and where the appointed planning and response teams are expected to interact in the promulgation of CSC recommendations and decisions. The key responsibilities of the entities shown in the figure are listed in Table 2-2.
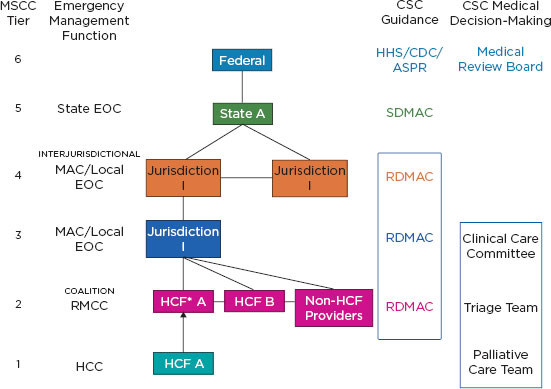
FIGURE 2-5
Integrating crisis standards of care planning into the Medical Surge Capacity and Capability framework.
NOTES: Further detail is provided in Table 2-2. The clinical care committee, triage team, and palliative care team may be established at MSCC tiers 1, 2, or 3. ASPR = Assistant Secretary for Preparedness and Response (Department of Health and Human Services); CDC = Centers for Disease Control and Prevention; CSC = crisis standards of care; EOC = emergency operations center; HCC = health care coalition; HCF = health care facility; HHS = Department of Health and Human Services.
Emergency Medical Services
Because of their critical role in linking patients in the outpatient environment to hospitals and the delivery of care, EMS agencies should play a major part in the development and implementation of CSC plans. Adjustments to scopes of practice, treatment modalities, ambulance staffing, and call response will figure significantly in state, local, and EMS-specific disaster response plans. Other areas that can be leveraged to manage scarce EMS resources include the authority to activate restricted treatment and transport protocols. Integration of CSC planning with the efforts of public health planners will be necessary to ensure consideration of case management (advice line) call centers, poison control, use of alternate care system destination points for ambulance patients, and limitation of care to on-scene treatment without transport. It should also be recognized that much EMS activity in the United States is provided by volunteer staff in rural communities, where resources are often limited on a regular, ongoing basis.
Hospitals/Acute Care Facilities and Out-of-Hospital/Alternate Care Systems
Clinical operations in hospitals, ambulatory care clinics, and private practices make up the largest single element of the response framework in which CSC will be implemented. Therefore, careful planning
TABLE 2-2
Key Responsibilities of Entities Shown in Figure 2-5
| Function | Key Responsibilities |
| State Emergency Operations Center (EOC) State Health Department |
• Communicates declarations and regulatory relief provided by the governor’s office to response partners and the public • Maintains situational awareness • Brokers resource requests from local/regional EOCs and conveys resource needs to the federal government • Coordinates and ensures consistency of interstate implementation of disaster response plans • Convenes state disaster medical advisory committee (SDMAC) to establish plans and guidelines • Provides situational awareness to state EOC and regional medical coordination center (RMCC) and hospitals • Requests declarations and regulatory relief from governor’s office and manages requests to the federally controlled Strategic National Stockpile • Oversees and ensures regional consistency in the execution of disaster response plans • Makes declaration of emergency (e.g., disaster, health emergency, or public health emergency), which provides support for CSC implementation |
| State Disaster Medical Advisory Committee (SDMAC) |
• Formulates guidance for the development and implementation of crisis standards of care (CSC) plans • Convenes to provide expert advisory input to state agencies during a response effort • Reviews intrastate (regional) and interstate application of CSC plans to ensure consistency |
| Regional Medical Coordination Center (RMCC) |
• Maintains and provides situational awareness for member health care systems • Acts as a clearinghouse for management of health care issues • Manages resources and executes preincident memorandums of understanding and memorandums of agreement • Coordinates with local emergency response system partners to develop policies and guidance necessary for CSC response • Develops and implements regional triage plans and performance improvement processes for the oversight of medical care during a disaster |
| Regional Disaster Advisory Committee (RDMAC) |
• May be convened by RMCC to assist in the evaluation and implementation of state guidance • May organize and compose a regional triage team that can assist with the implementation of performance improvement processes during the implementation of CSC guidance • Provides subject matter expertise to RMCC and health care coalition members |
| Health Care Coalition |
• Develops strategies and tactics to support emergency preparedness, response, and recovery activities of substate regional health care systems involving member organizations • Provides multiagency coordination for the interface with the appropriate level of emergency operations to assist with the provision of situational awareness and the coordination of resources for health care organizations during a response |
| Clinical Care Committee (health care facility and/or regional) |
• Implements clinical care guidance based on SDMAC/regional disaster medical advisory committee (RDMAC) inputs • Institutes performance measures for triage decision making • Institutes performance measures for allocation of scarce resource • Ensures coordination of CSC plan implementation with existing surge capacity plans • Reviews requests for patient appeals |
| Triage Team (health care facility and/or regional) |
• Reviews and implements guidance developed by SDMAC/RDMAC and clinical care committee • Implements triage processes |
| Palliative Care Team (health care facility and alternate care systems) |
• Ensures availability and implementation of comfort care for victims of a disaster |
is required at both the local and regional levels, including plans to ensure intraregional coordination and cooperation. Disaster response plans should delineate protocols for a shift from conventional standards of care to ensure that essential health care services will be sustained during the response. It is assumed that under disaster response conditions, resources—including state, regional, and federal caches; access to medical countermeasures; and the ability to transfer patients—are unavailable elsewhere in the region or state and will not be resupplied in the short term.
MILESTONES FOR CRISIS STANDARDS OF CARE PLANNING AND IMPLEMENTATION
Listed below are critical milestones that can be used to assess the progress of CSC planning, along with the proposed lead agency responsible for facilitating discussion, plan development, and implementation for each milestone.
• Establish a state disaster medical advisory committee (SDMAC) or equivalent with representation that includes all emergency response partners (EMS, public health, emergency management, health care systems, community-based practitioners, public safety, others) (governor’s office, state health department).
• Ensure the development of a legal framework for CSC implementation in the state in collaboration with the state emergency management agency and EMS offices and the SDMAC (governor’s office, state legislature, state attorney general’s office, state health department, state emergency management agency).
• Promote understanding of the disaster response framework among elected officials and senior (cabinet-level) state government leadership (state health department, state emergency management agency).
• Develop a state health and medical approach to CSC planning that can be adopted at the regional/ local level by existing health care coalitions, emergency response systems (including the regional disaster medical advisory committee [RDMAC]), and health care providers (RDMAC, state health department).
• Engage health care providers and professional associations by increasing their awareness and understanding of the importance and development of a CSC framework (state and local health departments and EMS agencies, health care coalitions and member organizations).
• Encourage participation of the out-of-hospital medical community in planning for disaster response, including the development of plans to maximize the effective use of all available materiel and personnel resources (state and local health departments, health care coalitions, professional health care organizations).
• Ensure that local and state plans include clear provisions that permit an adaptation of EMS systems under disaster response conditions, including changes in protocols, destinations, practices, and personnel (state and local health departments, state EMS agencies).
• Develop and conduct public community engagement sessions on the issue of CSC (state and local health departments).
• Support surge capacity and capability planning for health care facilities and the health care system, including the development of plans for allocating scarce resources and promotion of community resilience and mental health in surge response efforts (state and local health departments, health care coalitions).
• Plan for an alternate care system capability to manage a surge in demand for health and medical services (state and local health departments, health care coalitions).
• Support scarce resource planning by the RDMAC for health care facilities and the health care system so these plans can coalesce at the (regional) hospital coalition level (state and local health departments, health care coalitions).
• Incorporate risk communication strategies into CSC plans (governor’s office, state and local health departments, EMS and emergency management agencies, health care coalitions and member organizations).
• Exercise CSC plans at the local/regional level with state participation (including having the state exercise regional, intrastate, and interstate coordination if feasible) (governor’s office, state and local health departments, emergency management and EMS agencies, health care coalitions and member organizations).
• Exercise CSC plans at the interstate level (governor’s office, HHS regional emergency coordinators, state health department, state EMS and emergency management agencies).
• Use information identified during provider engagement, public/community engagement, and exercise events as elements of a process improvement cycle in order to further refine the development of disaster response plans (governor’s office, state and local health departments and EMS agencies, health care coalitions and member organizations).
• Develop a process for continuous assessment of disaster response capabilities based on existing information and knowledge management platforms, and create a mechanism for ensuring that these CSC planning milestones are being achieved (governor’s office, state health department and emergency management agency).
IMPLEMENTATION OF THE DISASTER RESPONSE FRAMEWORK
Regardless of the disaster response discipline—whether health care facility leadership, EMS, or public health—a number of steps should be considered during a real-time response to the potential need to initiate CSC. The “A Frame” approach (see Box 2-5) depicts the decision-making process that should be considered in the immediate aftermath of an incident. Modeled after what the emergency management community refers to as the “Planning P” (FEMA, 2008), this process helps establish the strategic implementation of disaster response capabilities. It provides a systematic approach to issue evaluation and decision points that help in determining whether health care delivery should remain at the conventional level, or contingency plans and/or crisis response may be necessary.
BOX 2-5
Implementation of the Surge Response Framework: Conventional, Contingency, and Crisis Response Cycle
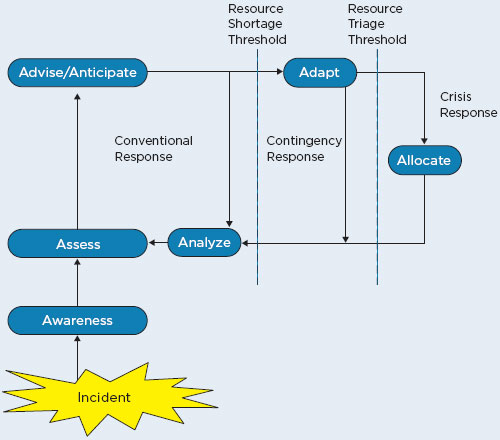
After an incident occurs, the first priority is to develop situational Awareness, and then to Assess the situation relative to the available resources. The incident commander, along with relevant technical experts and/or the clinical care committee (in a proactive response/longer-term incident) Advises on strategies and Anticipates any resource deficits (and recommends obtaining necessary supplies, staffing, etc.). If a resource is scarce, Adaptive strategies (such as conservation, substitution, adaptation, and reuse) should be implemented. In a crisis, a deliberate triage decision to Allocate/reallocate resources may be necessary. In all cases, the response and any strategies should be Analyzed at regular intervals as part of the disaster response planning cycle, and the elements repeated until the incident concludes. The terms in this figure can be further described as follows:
Awareness
• Incident commander recognizes current or anticipated resource shortfall(s) and assesses impact of current strategies.
Assess
• Technical experts are assigned to specific questions or areas of expertise.
• Clinical care committee performs assessment for more complex situations or when allocation of critical care resources is required during an ongoing incident.
• Logistics and liaison officers coordinate (across agencies) with suppliers, area public health and health care stakeholders, and emergency management as needed to obtain additional resources or assistance.
Advise/Anticipate
• Clinical care committee examines available resources, data, decision tools, and predictions of demand and determines possible adaptive actions. This analysis should also include what is happening within the region; the likely time frame for the crisis situation; and future impacts on demand, supplies, and staffing.
• Clinical care committee provides input to the planning section (or incident commander, depending on assignment) as to the specific adaptations necessary to accommodate ongoing demands and any recommended decision tools or policies. The committee also facilitates the transition back to conventional care as soon as possible.
• Public information and liaison officers coordinate with the planning section to ensure that the situation and adaptive strategies are included in risk communications provided to staff, patients, their families, and the community. A mechanism for addressing questions should also be available.
Adapt
• Clinical services are augmented or curtailed to allow the institution to focus on saving lives (e.g., subspecialty clinics may repurposed for outpatient acute care).
• Auxiliary equipment or spaces are utilized, including on-campus or off-campus alternate care sites, to support outpatient or inpatient overflow.
• Administrative changes involve little risk to patients and are usually the first adaptations.
• Changes are made in record-keeping and administrative duties.
• Ancillary personnel are used to provide basic hygiene and feeding services.
• Clinical changes involve escalating risk to patients and providers.
• Significant changes are made in shift lengths or number of patients supervised.
• Changes are made in criteria for evaluation (outpatient) and admission, as well as in criteria for admission to certain units (use of monitored units for critical care, for example).
• Changes are made in therapeutics, such as ventilation techniques and medication administration.
Allocate
• After approval of the incident commander, the plan is activated for the next operational period (during which the cycle begins again).
• Allocation policies are circulated (for example, use of medications or blood products).
• Reallocation decisions are made. A triage team is appointed if required for scarce critical care interventions, consisting of at least two specialists practicing and ex-
BOX 2-5 Continued
perienced in the clinical specialty affected (e.g., critical care, infectious disease, nephrology) (this team may be institutional, health system, or regional).
• Triage team utilizes decision tools to determine prognoses and, when a clear difference in prognosis exists, recommends treatment for patients with a predicted better outcome (first-come, first-served applies if there is no difference in prognosis substantial enough to justify reassignment).
• Triage team decisions are communicated to the medical branch director (or designated unit supervisor), who orders appropriate patient movement and actions to implement the team’s recommendations.
• Triage team decisions are documented in the medical record, as well as in the team’s daily activity log.
• Transition plans are in place to maintain the dignity and comfort of patients (and their families) who should have certain forms of care withdrawn or are receiving only palliative care.
Analyze
• Quality assurance is performed for ongoing allocation strategies: Is new information available? Are the policies and procedures appropriate for the situation being followed?
• Situational and resource information is updated, and the current strategies are analyzed, with feedback to the incident commander.
Resource Shortage Threshold
• The resource shortage threshold denotes the “indicators” (described in the committee’s letter report) (IOM, 2009) that demonstrate a point at which a potential or actual resource shortfall is recognized; however, substitution or other strategies may suffice to mitigate the problem.
Resource Triage Threshold
• The resource triage threshold denotes the “triggers” (described in the committee’s letter report) that demonstrate that specific resources are in short supply or are altogether unavailable. Therefore, an allocation schema must be implemented, and access to a specific care resource must be triaged because of demand. The triage decision involves an assessment of need, benefit, and duration of use.
To enhance and elaborate on the recommendations from its 2009 letter report, which it still fully supports, the committee developed a set of templates identifying the core functions and tasks for individuals and organizations involved in CSC planning and implementation. In developing these resources, the committee emphasized the use of a systems approach that integrates CSC planning into the larger context of overall surge capacity planning. The entire emergency response system—each component acting both indepen-
dently and as part of a coherent and integrated group—should adopt such a framework to deliver the best care possible to the largest number of patients.
RECOMMENDATION: Federal, state, tribal, and local governments should develop a systems-based framework for catastrophic disaster response, which must be integrated into existing emergency response plans and programs. To facilitate the implementation of this framework, the committee specifically recommends that:
• Each level of government should ensure coordination and consistency in the active engagement of all partners in the emergency response system, including emergency management, public health, emergency medical services, public and private health care providers and entities, and public safety.
• Each level of government should integrate crisis standards of care into surge capacity and capability planning and exercises.
• The Department of Health and Human Services/Assistant Secretary for Preparedness and Response (e.g., through its Regional Emergency Coordinators) should facilitate crisis standards of care planning and response among state and tribal governments within their region.
• In crisis standards of care planning and response efforts, states should collaborate with and support local governments.
• Federal disaster preparedness and response grants, contracts, and programs in the Department of Health and Human Services, the Department of Homeland Security, the Department of Defense, the Department of Transportation, and the Department of Veterans Affairs—such as the Hospital Preparedness Program, Public Health Emergency Preparedness Program, Metropolitan Medical Response System, Community Environmental Monitoring Program, and Urban Areas Security Initiative—should integrate relevant crisis standards of care functions.
AHRQ_(Agency for Healthcare Research and Quality). 2009. Disaster alternate care facilities: selection and operation. Publication no. 09-0062. Rockville, MD: AHRQ, http://archive.ahrq.gov/prep/acfselection/dacfreport.pdf (accessed February 28, 2012).
Arlington County. 2002. After-action report on the response to the September 11 terrorist attack on the Pentagon. http://www.arlingtonva.us/departments/Fire/Documents/after_report.pdf (accessed February 29, 2012).
ASPR (Assistant Secretary for Preparedness and Response). 2010a. Medical surge capacity handbook: What is medical surge? Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/mscc/handbook/chapter1/Pages/whatismedicalsurge.aspx (accessed February 1, 2012).
ASPR. 2010b. Medical surge capacity handbook: Glossary. Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/mscc/handbook/Pages/appendixd.aspx (accessed February 1, 2012).
Barbera, J. A., and A. G. MacIntyre. 2007. Medical surge capacity and capability: A management system for integrating medical and health resources during large-scale emergencies. 2nd ed. Washington, DC: HHS.
Barbisch, D. F., and K. L. Koenig. 2006. Understanding surge capacity: Essential elements. Academic Emergency Medicine 13(11):1098-1102.
Bascetta, C. A. 2010 (January 25). State Efforts Plan for Medical Surge Could Benefit from Shared Guidance for Allocating Scarce Medical Resources. Statement of Cynthia A. Bascetta, Director, Health Care, GAO before the U.S. House of Representatives, Committee on Homeland Security, Subcommittee on Management, Investigations, and Oversight, http://www.hsc-democrats.house.gov/SiteDocuments/20100125111234-95004.PDF (accessed February 29, 2012).
CDC (Centers for Disease Control and Prevention). 2009. Pandemic influenza pediatric office plan template: Product of a pediatric healthcare response to pandemic H1N1 influenza stakeholders meeting. http://www.bt.cdc.gov/healthcare/pdf/pediatric_office_plan.pdf (accessed November 13, 2011).
CDC. 2010a. Estimates of deaths associated with seasonal influenza—United States, 1976-2007. Morbidity and Mortality Weekly Report 59(33):1057-1062.
CDC. 2010b. 2009 H1N1-related deaths, hospitalizations and cases: Details of extrapolations and ranges: United States, Emerging Infections Program (EIP) data. http://www.cdc.gov/h1n1flu/pdf/Exact%20Numbers_AprilN.pdf (accessed November 13, 2011).
Chung, S., S. Monteiro, T. Hogencamp, F. J. Damian, and A. Stack. 2011. Pediatric alternate site of care during the 2009 H1N1 pandemic. Pediatric Emergency Care 27(6):519-526.
Cinti, S. K., W. Wilkerson, J. G. Holmes, J. Shlafer, C. Kim, C. D. Collins, K. Bandy, F. Krupansky, M. Lozon, S. A. Bradin, C. Wright, J. Goldberg, D. Wagner, P. Rodgers, J. Atas, and B. Cadwallender. 2008. Pandemic influenza and acute care centers: Taking care of sick patients in a non-hospital setting. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 6(4):335-344.
Coleman, C. N., C. Hrdina, J. L. Bader, A. Norwood, R. Hayhurst, J. Forsha, K. Yeskey, and A. Knebel. 2009. Medical response to a radiologic/nuclear event: Integrated plan from the Office of the Assistant Secretary for Preparedness and Response, Department of Health and Human Services. Annals of Emergency Medicine 53(2):213-222.
Commission on the Prevention of WMD Proliferation and Terrorism. 2008. World at Risk: The Report of the Commission on the Prevention of WMD Proliferation and Terrorism. New York: Vintage Books, http://documents.scribd.com/docs/15bq1nrl9aerfu0yu9qd.pdf (accessed February 29, 2012).
Courtney, B., R. Morhard, N. Bouri, and A. Cicero. 2010. Expanding practitioner scopes of practice during public health emergencies: Experiences from the 2009 H1N1 pandemic vaccination efforts. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 8(3):223-231.
Cruz, A. T., B. Patel, M. C. DiStefano, C. R. Codispoti, J. E. Shook, G. J. Demmler-Harrison, and P. E. Sirbaugh. 2010. Outside the box and into thick air: Implementation of an exterior mobile pediatric emergency response team for North American H1N1 (swine) influenza virus in Houston, Texas. Annals of Emergency Medicine 55(1):23-31.
DHS (Department of Homeland Security). 2009. Preparedness planningfor home health care providers. Washington, DC: DHS, http://www.dhs.gov/files/programs/gc_1221055966370.shtm (accessed February 29, 2012).
FEMA (Federal Emergency Management Agency). 2008. Incident Command System Training: Review Material. Washington, DC: FEMA, http://training.fema.gov/EMIWeb/IS/ICSResource/assets/reviewMaterials.pdf (accessed February 29, 2012).
George Washington University Institute for Crisis, Disaster and Risk Management. 2009. Emergency Management Principles and Practices for Health Care Systems: Unit 5: Appendices. Washington, DC: George Washington University, http://www.vibha.info/uploads/2/9/3/6/2936979/air_ambulance_5.pdf (accessed February 28, 2012).
Gostin, L. O., and M. Powers. 2006. What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Affairs 25(4):1053-1060.
HHS (Department of Health and Human Services). 2007. Medical surge capacity and capability. Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/mscc/handbook/Documents/mscc080626.pdf (accessed February 13, 2012).
Hanfling, D. 2006. Equipment, supplies, and pharmaceuticals: How much might it cost to achieve basic surge capacity? Academic Emergency Medicine 13(11):1232-1237.
Hanfling, D. 2009. Alternate care systems: Stratification of care. http://www.iom.edu/~/media/Files/Activity%20Files/Public Health/MedPrep/Jun-10-11-2009-Commissioned%20Papers/Jun-10-11-2009-Commissioned-Paper-Alternate-Care-Systems-Stratification-of-Care.ashx (accessed October 30, 2011).
Hick, J. L., D. Hanfling, J. Burstein, C. DeAtley, D. Barbisch, G. Bogdan, and S. Cantrill. 2004. Healthcare facility and community strategies for patient care surge capacity. Annals of Emergency Medicine 44:253-261.
Hick, J. L.., J. A. Barbera, and G. D. Kelen. 2009. Refining surge capacity: Conventional, contingency, and crisis capacity. Disaster Medicine and Public Health Preparedness 3(Suppl. 2):S59-S67.
Hodge, J. G., and E. F. Brown. 2011. Assessing liability for health care entities that insufficiently prepare for catastrophic emergencies. Journal of the American Medical Association 306(3):308-309.
IOM (Institute of Medicine). 2009. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press, http://www.nap.edu/catalog.php?record_id=12749 (accessed September 6, 2011).
Kaji, A., K. L. Koenig, and T. Bey. 2006. Surge capacity for healthcare systems: A conceptual framework. Academic Emergency Medicine 13(11):1157-1159.
Kelen, G. D., M. L. McCarthy, C. K. Kraus, R. Ding, E. B. Hsu, G. Li, J. B. Shahan, J. J. Scheulen, and G. B. Green. 2009. Creation of surge capacity by early discharge of hospitalized patients at low risk of untoward events. Disaster Medicine and Public Health Preparedness 3(Suppl. 2):S10-S16.
Kikta, K. 2011. 45 seconds: An ED physician in a tornado. ACEP News, July, http://www.acep.org/Content.aspx?id=80810 (accessed November 3, 2011).
Lam, C., R. Waldhorn, E. Toner, T. V. Inglesby, and T. O’Toole. 2006. The prospect of using alternative medical care facilities in an influenza pandemic. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 4(4):384-390.
Merriam-Webster Dictionary. 2012. Definition of “system’. Springfield, MA: Encyclopaedia Britannica, http://www.merriam-webster.com/dictionary/system?show=0&t=1328115597 (accessed February 1, 2012).
Minnesota Department of Health. 2008. Minnesota healthcare system preparedness program standards of care for scarce resources. http://www.health.state.mn.us/oep/healthcare/standards.pdf (accessed September 8, 2009).
OSTP (Office of Science and Technology Policy). 2010. Executive Office of the President Homeland Security Council Interagency Policy Coordination Subcommittee for Preparedness and Response to Radiological and Nuclear Threats, Planning Guidance for Response to a Nuclear Detonation (June 2010). www.ostp.gov (accessed February 1, 2012).
Rubinson, L., J. L. Hick, D. Hanfling, A. V. Devereaux, J. R. Dichter, M. D. Christian, D. Talmor, J. Medina, J. R. Curtis, J. A. Geiling; Task Force for Mass Critical Care. 2008a. Definitive care for the critically ill during a disaster: A framework for optimizing critical care surge capacity. Chest 133(Suppl. 5):18S-31S.
Rubinson, L., J. L. Hick, J. R. Curtis, R. D. Branson, S. Burns, M. D. Christian, A. V. Devereaux, J. R. Dichter, D. Talmor, B. Erstad, J. Medina, J. A. Geiling; Task Force for Mass Critical Care. 2008b. Definitive care for the critically ill during a disaster: Medical resources for surge capacity. Chest 133(Suppl. 5):32S-50S.
Scarfone, R. J., S. Coffin, E. S. Fieldston, G. Falkowski, M. G. Cooney, and S. Grenfell. 2011. Hospital-based pandemic influenza preparedness and response: Strategies to increase surge capacity. Pediatric Emergency Care 27(6):565-572.
Schultz, C. H., K. L. Koenig, and R. J. Lewis. 2003. Implications of hospital evacuation after the Northridge, California Earthquake. New England Journal of Medicine 348(14):1349-1355.
Weiss, E. A., J. Ngo, G. H. Gilbert, and J. V. Quinn. 2010. Drive-through medicine: A novel proposal for rapid evaluation of patients during an influenza pandemic. Annals of Emergency Medicine 55(3):268-273.
Volume 1 3: Legal Issues in Emergencies
As noted in the committee’s 2009 letter report, significant legal challenges are associated with catastrophic disasters involving the allocation of scarce health care resources and the establishment of crisis standards of care (CSC). These issues cut across nearly all levels of the public and private sectors involved in coordinating and providing emergency care during disaster response. To assist state and local public health and emergency planners, this chapter explores how key principles of law and policy can impede or facilitate the provision of public health and health care services during a disaster. It also addresses inherent conflicts related to the need to balance individual and communal health interests during such incidents. At the core of these issues is the need to transition rapidly from individual- to population-centric health services to save as many lives as possible and prevent injuries among patients, practitioners, and responders.
MEDICAL AND LEGAL STANDARDS OF CARE
In its letter report, the committee addressed several key issues related to distinctions between medical and legal standards of care, as well as scopes of practice for licensed health care workers. Modern studies consistently note how health care services must change during emergencies pursuant to what have been labeled “altered,” “situational,” and now “crisis” standards of care (AHRQ, 2005; AMA, 2007; Christian et al., 2006; Devereaux et al., 2008; GAO, 2008; Kanter, 2007). While the development and implementation of CSC are distinct from an assessment of prevalent liability protections, emergency planners and responders may consider whether additional liability protections are warranted in their jurisdictions, as discussed below.
The letter report described how changes in medical standards of care during an emergency may not be reflected in the corresponding legal standards of care, a disconnect that can lead to potential liability exposure for health care practitioners, volunteers, and entities during their response efforts. While medical and legal standards of care often are regarded as interchangeable, by one view they are in fact distinct concepts. According to this view, medical standards of care describe the types and levels of medical care dictated by professional norms, professional requirements, and institutional objectives (AHRQ, 2005; Hick et al., 2009; Pegalis, 2009). These standards of care vary (1) among different types of health care facilities, such as hospitals, clinics, and alternate care facilities (Hick et al., 2009); and (2) based on prevailing circumstances,
including during emergencies.1 Although existing, routine medical standards of care are flexible, they do not reflect the guidance needed to assist health care practitioners attempting to allocate scarce resources and make difficult decisions (including the potential withholding or withdrawal of life-sustaining treatment) during austere conditions in a public health emergency (GAO, 2008). Legal standards of care, on the other hand, may be defined as the minimum amount of care and skill a health care practitioner should exercise in particular circumstances based on what a reasonable and prudent practitioner would do in similar circumstances (Mastroianni, 2006).2 Legal standards of care are necessarily fact-specific, flexible, and subject to differing interpretations by different courts (Dobbs, 2000). They may reflect medical standards, but do not always. For example, prior courts assessing standards of care have determined at times that prevailing medical practice was insufficient or unacceptable in exceptional cases.3,4 In these instances, practitioners have been found liable for their actions even though, based on the circumstances, their acts were consistent with the prevailing medical standards of care.
Another view suggests that legal standards of care are intrinsically tied to medical standards of care. This view assumes that changes in the medical standards, such as those during a crisis, are automatically incorporated into the way courts and other legal authorities assess whether a particular actor has breached the standards through negligence or intentional acts because the legal standards of care by definition are based on what a reasonable practitioner would do under the particular circumstances (Annas, 2010). Given the flexibility of legal standards of care, some suggest that laws offering immunity or other protections from liability for health care workers, volunteers, or entities are unnecessary or even detrimental to the extent that they may deny patients recourse for injuries caused by ne gligent acts (ABA, 2011).5 During some disasters (e.g., Hurricane Katrina in 2005), patients in specific at-risk populations, such as the elderly, racial minorities, and those of lower socioeconomic status, may suffer disproportionately relative to others. To some, it appears unfair to deny these patients direct recourse against potentially negligent health care workers. In prior national emergencies, government has created compensation funds for those impacted to help provide recourse for direct harms they may have sustained as a result of the emergency.
However, federal, state, and local governments, public health agencies, and public health and health care organizations have consistently supported limited liability or indemnification protections for health care and public health actors, especially volunteers, during emergencies. In 2008, the American Medical Association (AMA) endorsed states’ consideration of the provisions of the Uniform Volunteer Emergency Health Practitioners Act for potential enactment, specifically including provisions that protect volunteer health care practitioners from liability claims grounded in negligence (AMA, 2008).6 In 2005, the AMA
_________________
1 Note that medical standards of care should not be confused with a health care provider’s scope of practice or associated privileges (Curie and Crouch, 2008; Pegalis, 2009). Scope of practice refers to the extent of a licensed professional’s ability to provide health services in accordance with his or her competence and license, certification, privileges, or other authority to practice (AHRQ, 2005; Wise, 2008).
2Hood v. Phillips, 554 S.W.2d 160, 165 (Tex. 1977).
3Helling v. Carey, 83 Wash. 2d 514, 519 P.2d 981 (1974).
4Canterbury v. Spence, 464 F.2d 772 (D.C. Cir. 1972).
5 The American Bar Association’s House of Delegates has expressed opposition to the adoption of laws that “would alter the legal duty of reasonable care in the circumstances owed to victims of a natural or manmade disaster by relief organizations or health care practitioners.” It suggests that the flexible nature of the legal standards of care provides adequate assurance of protection from unwarranted liability claims without the need to deny patients their right to bring claims through immunity protections.
6 “RESOLVED, That our American Medical Association support the enactment in state legislatures of the National Conference of Commissioners on Uniform State Laws [NCCUSL] Uniform Emergency Volunteer Health Practitioners Act with the liability language of Alternative A as formally adopted by the NCCUSL in August 2007.”
adopted a resolution declaring the need for “national legislation that gives qualified physician volunteers . . . automatic medical liability immunity in the event of a declared national disaster or federal emergency” (AMA, 2005).
Underlying the AMA’s and other health care professionals’ positions is the recognition that adherence to reasonable legal standards of care based on prevailing circumstances may lead to unpredictable outcomes when legal disputes arise. Lacking sufficient legal precedents, the provision of reasonable care through medical triage in a crisis may be viewed by many as insufficient or negligent because it may deviate extensively from normal standards as a result of the scarcity of resources. The development of national guidance on CSC may obviate some claims by clarifying the roles and responsibilities of practitioners during an emergency, against which the reasonableness of their actions or omissions may be adjudicated. Such results, however, are not assured. Facing potential uncertainty as to how courts or other arbitrators will assess claims arising from crisis care, qualified health care practitioners, volunteers, and entities naturally are concerned about their actual or perceived risks of liability. Nonetheless, all levels of government provide limited legal liability protections for many practitioners and entities responding during emergencies to offer assurances and incentives for their participation in emergency response efforts (as detailed later in the chapter).
There are two predominant paths to assessing and resolving potential negligence claims resulting from the implementation of CSC. One path is to suggest a policy of adhering to the standards of care as they evolve along the continuum described in Chapter 2 (Box 2-4). Via this path, a negligence claim arising during the implementation of CSC should be assessed later by experts and courts based on what a reasonable practitioner would do under similar circumstances. The other path reflects a different policy approach entailing how key legal liability protections from negligence claims take effect once a state of emergency has been declared. Instead of requiring adherence to evolving standards of care, these protections, documented further below, may dispel future negligence-based claims against practitioners, volunteers, and entities in recognition of the extreme variations in the provision of population-centric care in triage-like environments, when the applicable standards of care are constantly being evaluated and changing.
THE CHANGING LEGAL ENVIRONMENT IN DECLARED EMERGENCIES
Clarity concerning CSC is necessitated in part by the changing nature of the legal environment in declared emergencies. In nonemergencies, existing laws and policies offer reasonable guidance on the empowerment of actors and entities to allocate health resources and deliver health care. During declared emergencies, however, the legal environment changes. Emergency declarations trigger an array of nontraditional powers designed to facilitate response efforts by the public and private sectors. Emergency laws may (1) provide governments with sufficient flexibility to respond (e.g., by waiving specific regulatory requirements); (2) mobilize central commands and infrastructures; (3) encourage response efforts by limiting liability; (4) authorize interstate recognition of health care licenses; (5) allocate health care personnel and resources; (6) permit the provision of health care or public health services at nontraditional, alternate care sites; and (7) facilitate essential changes to the delivery of medical services and scopes of practice (Courtney et al., 2010; Hodge et al., 2009).
The extent of legal variations during emergencies, however, depends on the type of emergency declared. The federal government, every state, many territories, and some local governments may declare either general
states of “emergency” or “disaster” in response to crises that affect the public’s health (Hodge and Anderson, 2008). Such declarations largely authorize emergency management agencies and others to use general legal powers to coordinate emergency responses. The Department of Health and Human Services (HHS) and more than half the states may also declare states of “public health emergency” (Hodge et al., 2008) based in part on the Model State Emergency Health Powers Act (Centers for Law and the Public’s Health, 2001).7 Collectively, these declarations authorize an array of expedited public health powers coordinated by public health agencies in conjunction with emergency managers and other partners. The federal government and some states may declare states of both “emergency” or “disaster” and “public health emergency” in response to the same incident, such as during Hurricane Katrina and the 2009 H1N1 pandemic. These dual declarations can lead to confusion as divergent governmental powers and actors seek to respond in overlapping and potentially inconsistent ways (Hodge and Anderson, 2008).
LEGAL ISSUES IN DECLARED EMERGENCIES
From these varying emergency declarations arise a host of powers and protections that may impact the delivery of health care services depending, in part, on real-time legal interpretations. Health care practitioners and entities responsible for emergency preparedness should consider numerous legal issues that arise in responding to events along the continuum of care leading up to a declared state of emergency, as documented in Table 3-1 and summarized in relevant subsections below.
Legal Authorization to Allocate Personnel, Resources, and Supplies
Emergency declarations and ensuing orders, as noted above, can help shift how and where care is delivered and how resources (e.g., personnel, medical supplies, physical space) are allocated.8,9 Many states’ statutory emergency laws, for example, recognize out-of-state health care licenses for the limited duration of a declared emergency (Hodge et al., 2008). These “licensure reciprocity” provisions allow for the interstate sharing of out-of-state health care personnel whose licenses are viewed as in-state licenses for the duration of the declared emergency (although providers may still be subject to liability risks if they exceed their scope of practice in their home jurisdiction during their emergency response efforts). Memorandums of understanding, mutual-aid agreements, compacts, and other agreements can also facilitate the sharing of health care and other necessary resources during resource-scarce emergencies (CDC, 2011). The Emergency Management
_________________
7 While many states may have authorities to declare states of “public health emergency,” the following states have authorities based on the Model State Emergency Powers Act: Alabama, Arizona, Connecticut, Delaware, District of Columbia, Florida, Georgia, Illinois, Indiana, Iowa, Louisiana, Maine, Maryland, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, South Carolina, South Dakota, Texas, Virginia, Washington, Wisconsin, and Wyoming.
8 The Commonwealth of Virginia provides immunity protections for health care practitioners during resource-scarce disasters following the declaration of a state or local emergency. “In the absence of gross negligence or willful misconduct, any health care provider who responds to a disaster shall not be liable for any injury or wrongful death of any person arising from the delivery or withholding of health care when (i) a state or local emergency has been or is subsequently declared in response to such disaster, and (ii) the emergency and subsequent conditions caused a lack of resources, attributable to the disaster, rendering the health care provider unable to provide the level or manner of care that otherwise would have been required in the absence of the emergency and which resulted in the injury or wrongful death at issue.” Code of Virginia § 8.01225.02 (2008).
9 Louisiana Senate Bill No. 301, SB 301, 2008 Regular Session, Louisiana Legislature, Act No. 538 ( June 30, 2008), http://www.legis.state.la.us/billdata/streamdocument.asp?did=503696 (accessed February 1, 2012).
TABLE 3-1
Selected Legal Issues of Concern to Health Care Practitioners and Entities Responsible for Emergency Preparedness
| Subject | Legal Issues |
| Organization of Personnel |
• How are employees, independent contractors, and volunteers legally distinguished for the purpose of coordinating services and benefits during an emergency? • Do existing labor contracts or union requirements affect the ability of the entity and its personnel to respond to an emergency? • Have appropriate contractual or other mechanisms been executed to facilitate the delivery of services by employed or volunteer personnel, ensure worker safety, or ensure the availability of workers’ compensation or other benefits during an emergency? |
| Access to Treatment |
• Has the entity assessed its strategy for conducting medical triage under legal requirements for treating existing and forthcoming patients? • Is the entity prepared to screen and potentially divert excess numbers of patients during an emergency consistent with the Emergency Medical Treatment and Active Labor Act (EMTALA), absent its waiver during a declared emergency? • Do health care personnel who are designated to treat existing and forthcoming patients pose any risks to patients either through (1) exposure to infectious or other conditions or (2) the use of personal protective equipment that may impede the delivery of medical services? |
| Coordination of Health Services |
• Are health care personnel aware of the legal effects of a shift to crisis standards of care and changes relating to scopes of practice during a declared emergency? • Are health care personnel knowledgeable about conditions related to the issuance of emergency use authorizations (EUAs) by the Food and Drug Administration (FDA), including accompanying mandatory emergency use information for patients and providers? • Are adequate mechanisms in place to ensure compliance with surveillance, reporting, testing, screening, partner notification, quarantine, isolation, and other public health mandates during an emergency? • Are legal issues concerning the use of volunteer health professionals during an emergency addressed through the entity’s emergency plan? |
| Patients’ Interests |
• Can patients with physical or mental disabilities be accommodated during the emergency consistent with disability protection laws? • Do patients have adequate access to available medical countermeasures to ensure their health and safety? • Are appropriate measures in place for attempting to ascertain patients’ informed consent? • Barring waiver of national, state, or local privacy laws through emergency declarations, are the entity and its personnel prepared to respect patients’ health information privacy rights during an emergency? • Is the entity prepared to evacuate at-risk patients in response to an emergency? |
| Allocation of Resources |
• Is there a legitimate process for determining allocation of limited resources that is fair, reasonable, nondiscriminatory, and credibly based on protecting the health of patients and the public? • Are there federal, state, and/or local policies regarding resource allocation that should be followed? • Can government appropriate existing resources (with just compensation) for communal purposes during an emergency? |
| Liability |
• When may the entity and its personnel be liable for their actions in treating patients under crisis standards of care during an emergency? • What legal protections from liability for entities, their health care personnel, independent contractors, and volunteers (including insurance coverage) apply during an emergency? • May entities and their personnel face potential liability for failure to adequately plan or train for emergencies? |
| Subject | Legal Issues |
| Reimbursement |
• Are there established reimbursement protocols for treating patients during an emergency? • Are private health insurers or other payers legally required to reimburse for care delivered to patients in furtherance of the public’s health? • Are entities organized to seek federal and state reimbursement through the Centers for Medicare & Medicaid Services, the Federal Emergency Management Agency, or other sources for care delivered in off-site facilities operated by the entity? • Have federal/state authorities accelerated, altered, or waived Medicare/Medicaid requirements for reimbursement during an emergency? |
| Interjurisdictional Cooperation |
• Has the entity executed memorandums of understanding, mutual-aid agreements, or other agreements to facilitate interjurisdictional coordination of emergency health care services? • Are these agreements consistent with federal (Department of Health and Human Services/Assistant Secretary for Preparedness and Response or Centers for Medicare & Medicaid Services; Department of Homeland Security/National Incident Management System) or other government requirements? • Is the entity’s all-hazards emergency plan integrated with community-level emergency planning and objectives? • Have state or local governments on international borders addressed specific concerns through lawful agreements across borders? |
SOURCE: Hodge et al., 2009.
Assistance Compact (EMAC),10 for example, formalizes interstate mutual aid among all states, several territories, and the District of Columbia. Similar compacts at the regional, tribal, and municipal levels further facilitate care and distribute resources.
Liability Risks and Protections for Health Care Practitioners
As noted above, liability exposure is a prominent concern among health care practitioners and entities. The implementation of CSC is a dynamic process that entails difficult decisions, intense trade-offs, constant assessments of specific courses of action, and potentially unconventional acts (including denying or withdrawing health care services because of limited resources). Virtually any patient may feel aggrieved by failing to receive state-of-the-art medical care during an emergency that would have been provided in routine health care environments. Against this backdrop, the potential arises for legal action resulting from perceived or actual denial or limitation of health care services during a crisis. High-profile cases involving health care practitioners responding during Hurricane Katrina, for example, have garnered national attention.11Potential liability claims can result from alleged civil, criminal, and constitutional violations by health care practitioners, volunteers, and government or private entities (Hodge et al., 2009). Liability may stem from claims of medical malpractice, discrimination, invasions of privacy, or violations of other state and federal statutes (e.g., the Emergency Medical Treatment and Active Labor Act [EMTALA]).12 Recently, Tenet
_________________
10 Public Law 104-321. EMAC was approved by Congress in 1996. All states, the District of Columbia, Puerto Rico, Guam, and the U.S. Virgin Islands have enacted EMAC legislation.
11 The most publicized case of criminal liability associated with a health care professional’s decisions during a resource-scarce situation is that of Dr. Anna Pou, a physician from Memorial Medical Center in New Orleans. Dr. Pou was charged with second-degree murder for allegedly hastening the deaths of several patients during Hurricane Katrina. While she was not criminally indicted, she also faced several civil wrongful death claims. In response, Louisiana enacted civil liability immunity protection laws aimed at protecting health care workers who act in good faith during emergencies. See, e.g., Louisiana Senate Bill No. 301, Act No. 538 (2008).
12 The Emergency Medical Treatment and Active Labor Act (EMTALA), 42 U.S.C.A. § 1395dd (1986). EMTALA, for example, requires hospitals that participate in Medicare and have a dedicated emergency department to provide a medical screening examination within their capability to individuals who report to the emergency department and request such an examination or treatment for a medical condition.
Health Systems, which operated Memorial Medical Center in New Orleans, settled claims brought by Hurricane Katrina victims for $25 million. The victims’ claims entailed negligence not only for Tenet’s failure to respond, but also for its failure to plan and prepare properly for the emergency itself (Hodge and Brown, 2011). Such cases reaffirm the essential role of advance planning and preparedness activities in mitigating, at least in part, prospective liability claims.
While not all legal causes of action are viable or proliferate, health care practitioners and entities remain apprehensive about their potential exposure to liability risks especially during emergencies, when their actions and responsibilities may exceed the norm. After the unsuccessful indictment in 2006 of Dr. Anna M. Pou and other health care personnel on criminal charges related to their handling of several patients at Memorial Medical Center during Hurricane Katrina, the AMA, the Louisiana State Nurses Association, and other organizations expressed concern that the case would cause practitioners to reconsider whether to help people during disasters (Jervis, 2007). In developing additional guidance for the implementation of CSC, the committee heard directly from numerous state and local public health and emergency management representatives about their concerns regarding how liability risks may impact the willingness of practitioners and volunteers to participate in emergency response efforts. In addition to numerous anecdotal accounts documented by the committee and other credible sources, some empirical data support similar findings.
In 2006 the Community Health Planning and Policy Development Section of the American Public Health Association (APHA) conducted an electronic survey of prospective volunteer health practitioners. More than 1,000 responses were received. When asked, as a potential volunteer, “how important is your immunity from civil lawsuits in deciding whether to volunteer during emergencies,” almost 70 percent of respondents indicated it was “important” (35.6 percent) or “essential” (33.8 percent) (Carpenter et al., 2008). A survey of 1,057 prospective Medical Reserve Corps (MRC) volunteers in Hawaii, published in 2008, found that liability protections were among respondents’ primary concerns during operations (Quereshi et al., 2008). Concerns regarding liability risks (among others) also are noted in another study of prospective MRC volunteers conducted in 2007 (Schechter, 2007). A 2009 qualitative study of UK health care workers’ willingness to respond during an influenza pandemic (conducted after substantial inquiries following the London bombings in 2005) found “both clinical and non-clinical participants were worried about being asked to perform a role they had not been trained for, and had concerns both about being a danger to patients and being subject to litigation if something went wrong…. It was clear that many participants would be reluctant to take on extended roles without some assurance that they would be protected from litigation [emphasis added] (Ives et al., 2009).
Despite liability concerns during emergencies, there are no comprehensive national liability protections for health care practitioners or entities in all settings. Instead, an array of liability protections at all levels of government covers practitioners and entities—particularly volunteers and government entities and officials—that act in good faith and without willful misconduct, gross negligence, or recklessness (Hoffman, 2008; Hoffman et al., 2009; Rosenbaum et al., 2008; TFAH, 2008). Similar to protections bestowed upon emergency managers, police, firefighters, and other responders, emergency liability protections in all states may immunize or indemnify public health and health care actors or entities from specific claims or monetary damages. Federal or state suspensions of legal requirements or waivers of sanctions for failing to comply with
EMTALA also includes requirements for stabilizing and transferring patients. Physicians and health care entities that negligently fail to comply with EMTALA may be excluded from participation in the Medicare program and incur monetary penalties.
certain federal or state statutes during declared emergencies may offer additional protections.13 Some liability protections, including Good Samaritan statutes (HHS ASPR, 2009), volunteer protection acts,14,15 and tort claims acts,16 may apply outside of an emergency declaration. Other protections, such as those pursuant to EMAC17 or emergency laws, are triggered only by an emergency declaration (Centers for Law and the Public’s Health, 2004). Table 3-2 lists specific statutory or regulatory language that currently provides various levels of liability protection for health care practitioners, volunteers, and entities.
Specific federal declarations provide targeted liability protections and authorize the emergency use of medical countermeasures needed for a response. For example, the federal Public Readiness and Emergency Preparedness (PREP) Act18 provides strong liability protections for individuals and entities implementing certain covered medical countermeasures (i.e., countermeasures that are Food and Drug Administration [FDA]-approved, authorized for investigational use, or authorized by an emergency use authorization [EUA]) (Binzer, 2008). Upon a PREP Act declaration by the Secretary of HHS, limited protection from tort liability is extended to “covered persons” (e.g., the United States, manufacturers of the countermeasures, drug distributors, pharmacies, state and local program planners) involved in the development, distribution, and administration of the medical countermeasure(s).19 The act expressly establishes a compensation fund for individuals injured as a result of the administration or use of covered countermeasures (HRSA, 2005). PREP Act liability protections, however, are limited. They apply only to persons and covered countermeasures specified by HHS: one lower court decision in New York, currently on appeal, suggests that the PREP Act liability protections do not immunize a school system or health practitioner involved in allegedly “bad faith” administration of the H1N1 vaccine to a minor student whose parents did not provide their consent.20 PREP Act declarations also are effective only for a specified period of time; however, the effective date of a declaration can precede the date of issue (see, for example, HHS, 2007, issued February 1, 2007, but effec-
_________________
13 42 U.S.C. § 1320b-5 (2008). Under section 1135 of the Social Security Act, the Secretary of HHS may temporarily waive or modify certain program requirements for Medicare, Medicaid, and the State Children’s Health Insurance Program. For example, sanctions for failing to comply with certain EMTALA requirements may be waived by the Secretary during public health emergencies.
14 Public Law 105-19; 42 U.S.C. § 14501 et seq. All states and the District of Columbia have adopted state volunteer protection acts.
15 The Uniform Emergency Volunteer Health Practitioners Act (UEVHPA) was developed in 2007 in response to a lack of uniformity in states’ protections for medical and other volunteers. It “establishes a system whereby health professionals may register either in advance of or during an emergency to provide volunteer services in an enacting state. Registration may occur in any state using either governmentally established registration systems, such as the federally funded ‘ESAR VHP’ [Emergency System for Advance Registration of Volunteer Health Professionals] or Medical Reserve Corps programs” (http://www.uevhpa.org/DesktopDefault.aspx).
16 Under the Federal Tort Claims Act, for example, a “covered employee [is] not personally liable for negligent acts committed within [the] scope of Federal employment” (HHS, Federal Public Health Emergency Law: Implications for State and Local Preparedness and Response [teleconference], April 28, 2009).
17 “Under EMAC, a person from one state who renders assistance in another and who holds a license, certificate, or other permit for the practice of professional, mechanical, or other skills is considered to be licensed, certified, or permitted to exercise those duties in the requesting state, subject to limitations or conditions set by the requesting state’s Governor.” Still, licensure reciprocity is not automatically extended to volunteer health care practitioners who do not provide services pursuant to an EMAC request for assistance (Congressional Research Service, 2009).
18 42 U.S.C. § 247d-6d.
19 “Countermeasures covered under a PREP Act declaration include products that are approved, cleared, or licensed under the FD&C [Food, Drug, and Cosmetics] Act or the PHS [Public Health Service] Act, authorized for investigational use under the FD&C Act, or authorized under an EUA. For example, if a person is given a countermeasure that is lawfully authorized for emergency use under an EUA, that person may be eligible under the PREP Act for compensation through the CICP [Countermeasures Injury Compensation Program] if serious physical injury or death results from use of the countermeasure.” See http://www.fda.gov/EmergencyPreparedness/Counterterrorism/ucm269226.htm#prepcoverage.
20 Parker v. St. Lawrence County Public Health Department, No. 44-1-2011-0204 (Sup. Ct. N.Y. St. Lawrence County decided July 5, 2011) (unpublished decision).
TABLE 3-2
Selected Statutory and Regulatory Health Care Liability Protections in Emergencies
| Source | Applies to | Provision |
| Model State Emergency Health Powers Act (MSEHPA) | Out-of-state emergency health care professionals (among others) | These professionals “shall not be held liable for any civil damages as a result of medical care or treatment related to the response to the public health emergency unless such damages result from providing, or failing to provide, medical care or treatment under circumstances demonstrating a reckless disregard for the consequences so as to affect the life or health of the patient.“a |
| Uniform Emergency Volunteer Health Practitioners Act (UEVHPA) | Volunteer health practitioners (VHPs) (whether public or private sector) | Alternative A: VHPs are not liable for their actions or omissions while providing services during an emergency. This provision does not apply to VHPs engaged in willful, wanton, or grossly negligent acts, or to incidents involving criminal conduct, intentional torts, breaches of contract, or acts and omissions relating to the operation of vehicles. Alternative B: Protections similar to those of Alternative A, but applies only to VHPs who receive compensation of $500 or less per year (not including reimbursement for reasonable expenses and continuation of salary while on leave). |
| Emergency Management Assistance Compact (EMAC) | State or local officers or employees | "Officers or employees of a party state rendering aid in another state pursuant to this compact shall be considered agents of the requesting state for tort liability and immunity purposes"b Those rendering aid are protected from civil liability, provided that they act in good faith and without “willful misconduct, gross negligence, or recklessness."c |
| Federal Public Readiness and Emergency Preparedness (PREP) Act,dhttp://www.uevhpa.org/ DesktopDefault.aspx |
Covered persons” (e.g., U.S. government, manufacturers, distributors, pharmacies, state and local program planners) | "A covered person shall be immune from suit and liability under Federal and State law with respect to all claims for loss caused by, arising out of, relating to, or resulting from the administration to or the use by an individual” if he or she is administering an approved countermeasure during the declaration of an appropriate emergency or public health emergency.e |
| Federal Volunteer Protection Act (VPA) | Uncompensated, individual volunteers of nonprofit organizations or governmental entities | Volunteers shall not be liable for harm caused by their acts or omissions on behalf of the organization or entity so long as they are: (1) acting within the scope of the volunteer’s responsibilities; (2) properly licensed, certified, or authorized by the appropriate authorities as required by law in the state in which the harm occurred; (3) have not engaged in willful or criminal misconduct, gross negligence, reckless misconduct, or a conscious, flagrant indifference to the rights or safety of the individual(s) harmed by the volunteer; and (4) have not caused the harm by operating a motor vehicle, vessel, aircraft, or other vehicle for which the state requires its operator to possess an operator’s license or maintain insurance.f |
| Source | Applies to | Provision |
| Virginia Emergency Code | Health care providers | "In the absence of gross negligence or willful misconduct, any health care provider who responds to a disaster shall not be liable for any injury or wrongful death of any person arising from the delivery or withholding of health care when (i) a state or local emergency has been or is subsequently declared in response to such disaster, and (ii) the emergency and subsequent conditions caused a lack of resources, attributable to the disaster, rendering the health care provider unable to provide the level or manner of care that otherwise would have been required in the absence of the emergency and which resulted in the injury or wrongful death at issue."g |
| Louisiana State Statutes | Health care entities and providers | "(b) During a state of public health emergency, any private person, firm or corporation and employees and agents of such person, firm or corporation in the performance of a contract with, and under the direction of the state or its political subdivisions . . . shall not be civilly liable for causing the death of, or injury to, any person or damage to any property except in the event of gross negligence or willful misconduct. (c) During a state of public health emergency, any health care providers shall not be civilly liable for causing the death of, or, injury to, any person or damage to any property except in the event of gross negligence or willful misconduct. “h |
| Maryland State Torts Claims Act | State personnel (including unpaid individuals performing state functions)i | Provides state personnel immunity for acts or omissions within the scope of their dutiesj |
| Minnesota Indemnification Protections | Volunteers | Volunteers during an emergency or disaster are deemed employees of the state for purposes of torts claims defense and indemnification.k |
| Model Intrastate Mutual Aid Legislation (MIMAL) | All persons, including volunteers, responding under the operational control of the government entity requesting aid (these persons are considered employees of the government entity) | "Neither the participating political subdivisions nor their employees . . . shall be liable for the death of or injury to persons, or for damage to property when complying or attempting to comply with the statewide mutual aid system.” Immunity does not apply to acts of willful misconduct, gross negligence, or bad faith.l |
a MSEHPA § 608(b)(3).
b EMAC, art. VI.
c EMAC § 2, art. VI.
d 42 U.S.C.A. § 247d-6d.
e 42 U.S.C.A. § 247d-6d.
f 42 U.S.C.A. § 14503 (2004).
g Va. Code Ann. § 8.01-225.02 (2008).
h La. Rev. Stat. Ann. § 29:771 (2003).
i Md. Code. State Gov’t § 12-101 (2005).
j Md. Code Ann. Cts. & Jud. Proc. § 5-522(b) (2005).
k Minn. Stat. Ann. § 12.22 (West).
l National Emergency Management Association, Model Intrastate Mutual Aid Legislation, Art. X (2004).
tive from December 1, 2006). This can be done at the discretion of the Secretary of HHS to extend liability protections to covered persons acting in response to a disaster but prior to a PREP Act declaration.
Liability protections may also be extended through the federal emergency allowance of specific drugs or other medical products that might otherwise be unavailable to the public. When the requisite emergency determination is in place (i.e., by the Secretary of HHS, the Department of Homeland Security [DHS], or the Department of Defense), the Secretary of HHS may declare an emergency justifying the authorization of emergency use for certain medical products. The FDA then can issue an EUA to allow the emergency use of drugs or other medical products that are either (1) not yet approved by the FDA for use or (2) sought for an unapproved use.21 EUAs were issued, for example, during the 2009 H1N1 pandemic to allow unapproved uses of zanamivir (Relenza®) and oseltamivir (Tamiflu®) for treatment and prophylaxis of young children and hospitalized patients (CDC, 2010). To issue an EUA, the Commissioner of the FDA must conclude that
• the agent specified in the declaration poses the risk of a serious or life-threatening disease or condition;
• it is reasonable to believe that the product may be effective in diagnosing, treating, or preventing the agent;
• the known and potential benefits of use of the product outweigh the known and potential risks; and
• no adequate, approved, and available alternative to the product exists to address the agent.22
EUAs remain in effect for the duration of the emergency declaration (up to 1 year unless revoked). Both the declaration and EUAs issued under the declaration may be renewed if justified (FDA, 2009), as was the case with the antimicrobial doxycycline for prophylaxis of inhalational anthrax.23
Once issued, EUAs take effect nationally irrespective of any additional state legal action in support of the authorization (FDA, 2007). The Commissioner of the FDA can set conditions on activities under an EUA to protect the public’s health, including ensuring that health care professionals and patients are informed of risks, benefits, and alternatives and that adverse events are monitored through manufacturers, health care entities, or public health authorities.24 From a liability perspective, EUAs allow the temporary use of a drug or product that would otherwise be prohibited, thus mitigating potential claims related to the unwarranted dispensing of unapproved drugs or other issues.
Although lacking consistency across all emergency responders and entities, the existing patchwork of liability protections can facilitate emergency planning and response efforts by providing assurances of liability protection against negligence claims during and after declared emergencies. These laws collectively provide an umbrella of protections covering hundreds of thousands of practitioners, volunteers, and entities that
_________________
21Project Bioshield Act of 2004, Public Law 108-276, § 564(a)-(b).
22Project Bioshield Act of 2004, Public Law 108-276, § 564(c). For more information on how these determinations are to be made and what information is included in a request for EUA consideration, see FDA guidance on EUAs (http://www.fda.gov/RegulatoryInformation/Guidances/ucm125127.htm#intro).
23 76 FR 44926. HHS’s declaration justifying the emergency use of doxycycline hyclate tablets accompanied by emergency use information was originally issued in 2008 and subsequently renewed in 2009 and 2010 in response to continuing national security concerns. The declaration was also renewed and amended in 2011. An EUA (issued under that declaration) for doxycycline hyclate tablet emergency kits for U.S. Postal Service participants and their household members was originally issued in 2008 and subsequently amended in 2009, 2010, and 2011.
24Project Bioshield Act of 2004, Public Law 108-276, § 564(e).
are expected or asked to play critical roles in emergency response. Yet there are significant limits to liability protections overall. As noted above, some legal protections cover individuals or entities only for their acts during declared emergencies, and the effective date of a declaration of emergency may precede the actual date of the declaration. HHS’s declarations pursuant to the PREP Act, for example, may be retroactive. In most cases, however, liability and other protections emanating from emergency declarations commence only on the date of the declaration and end the moment the declaration is terminated. This may leave some responders whose efforts precede or exceed the time period of the formal declaration unprotected.
Even when liability protections do apply, virtually none of the protections immunize or indemnify practitioners or entities for acts that constitute gross negligence, willful or wanton misconduct, or crimes. Volunteers seeking protection may have to be registered with government or private systems (Hoffman et al., 2009), follow government disaster plans or protocols, or act specifically under government authority.25,26 Liability protections for volunteers do not similarly immunize health care employees working alongside them (some of whom may be covered by medical malpractice insurance subject to insurers’ exceptions), although some states also immunize compensated workers.27,28 Liability protections for health care entities, including hospitals, clinics, pharmacies, and others, are more limited than individual protections.29
Health care practitioners may also be concerned about whether malpractice and other forms of insurance will cover unintentional errors or care given outside a provider’s scope of practice under CSC. In the APHA survey noted above, prospective volunteer respondents were asked, “As a clinician, to what degree does knowing that you have medical malpractice insurance coverage influence your decision to travel out of state to volunteer in a clinical capacity during an emergency?” Nearly 60 percent of respondents indicated such coverage was “important” (24.3 percent) or “essential” (35.4 percent) (Carpenter et al., 2008). While malpractice insurance coverage differs across states and is dependent on specific insurance policy language, plans may not cover a practitioner’s or volunteer’s actions during a declared emergency if they fall outside the individual’s normal scope of activities. To protect volunteers and other health care practitioners from rate increases following frivolous malpractice claims, Delaware state law restricts medical malpractice insurance
_________________
25 For example, under HHS’s National Disaster Medical System, “an individual appointed under paragraph (1) shall, while acting within the scope of such appointment, be considered to be an employee of the Public Health Service performing medical, surgical, dental, or related functions. With respect to the participation of individuals appointed under paragraph (1) in training programs authorized by the Assistant Secretary for Preparedness and Response or a comparable official of any Federal agency specified in subsection (a)(2)(B) of this section, acts of individuals so appointed that are within the scope of such participation shall be considered within the scope of the appointment under paragraph (1) (regardless of whether the individuals receive compensation for such participation).” 42 USC § 300HH-11.
26 “Intermittent disaster-response personnel benefit from the same immunity from civil liability granted to employees of the U.S. Public Health Service. The only remedy for damages for personal injury, including death, resulting from the performance of medical, surgical, dental, or related functions by any commissioned officer or employee of the Public Health Service (acting within the scope of office or employment) is against the United States, and not against the officer or employee (or her estate) whose act or omission gave rise to the claim. The U.S. Attorney General is also required to defend these individuals” (Centers for Law and the Public’s Health, 2005).
27Code of Virginia § 8.01225.02 (2008).
28Louisiana Senate Bill No. 301, Act No. 538 (2008).
29 Entities may also be covered under state liability protection laws for Good Samaritan entities during emergencies. However, most state Good Samaritan laws leave significant gaps of liability exposure for both private and nonprofit organizations that are willing to assist government agencies voluntarily in responding to emergencies. As a result, at least 28 states and the District of Columbia have developed specific emergency liability protections for business and nonprofit organizations that act in good faith to assist government agencies voluntarily during emergencies. See, e.g., Louisiana House Bill 554 (2009) RS 29:735.3.1 (http://www.legis.state.la.us/billdata/streamdocument.asp?did=662505).
carriers from increasing the premiums of health care practitioners for their acts or omissions in providing relief care in declared emergencies.30
Ultimately, health care practitioners, volunteers, and entities, in collaboration with emergency managers, legal representatives, and policy makers, should assess the gamut of legal liability protections in their jurisdictions and determine whether additional protections are needed to facilitate the implementation of CSC. Depending on their analyses, gaps may be addressed through existing models for legislative or policy reform (e.g., Model State Emergency Health Powers Act, Uniform Emergency Volunteer Health Practitioners Act), as well through real-time efforts to issue emergency orders, waive liability claims, or ensure malpractice coverage for claims that may arise.
Balance Between Individual Legal Rights and Responsibilities and Communal Objectives
At the core of emergency-related legal issues is the need to balance individual and communal interests to protect the public’s health. Balancing respective legal interests in emergencies is complex. The interests of individuals and the community may conflict, leading to difficult issues in the establishment and implementation of CSC. Due process and other constitutional protections may differ among autonomous adults and children or other wards of the state (e.g., prisoners, persons lacking mental competence) (Gostin, 2008). Nonautonomous individuals may enjoy special constitutional protections intended to prevent individual harms. For example, government may be legally required to protect the health of minors (Courtney and Hodge, 2011) or other “wards,” even though autonomous adults may not be similarly protected (Hodge, 2009).
The Constitution affords everyone procedural due process protection if the state deprives an individual of a “liberty” interest. During a public health emergency, health professionals will have to make difficult decisions to allocate scarce medical resources (O’Callaghan, 2008).31 It is unclear whether a decision to withdraw or withhold certain treatment during an emergency would trigger due process protection. Even if individuals were entitled to some fair process, the Supreme Court has made clear that due process is a flexible concept that may entail a hospital-based impartial review of the facts under the applicable standards of care.32
Individual privacy interests also should be assessed against the need for government or others to provide adequate care or share identifiable health data for public health reporting, research, or other communal purposes (Hodge et al., 2004). Decisions concerning standards of care that disproportionately affect individuals on grounds of ethnicity, religion, race, or other protected characteristics may raise claims of violation of equal protection (Congressional Research Service, 2009).
_________________
30 “No act or omission of qualified medical personnel during such relief operations and activities shall affect an insured physician’s liability coverage in any way.” Del. Code Ann. tit. 20, § 3129(b) (TFAH, 2008, p. 26).
31 “By its terms the due process clause applies to particularized governmental decisions about whether an individual is to be granted a benefit or to be subjected to a burden” (O’Callaghan, 2008).
32 In ascertaining the due process procedures that are constitutionally required, the courts weigh three factors—the extent of the deprivation of liberty or property, the risk of an erroneous decision, and the burdens that additional procedures will entail. Thus, the procedures in any given circumstance depend on the public health context and vary from case to case. The process required can range from a full-blown hearing to an informal, nonadversarial review (Gostin, 2008). In Parham v. J.R., for example, the Supreme Court ruled that the state did not have to provide a formal hearing. Since juvenile admission to a mental hospital was “essentially medical in character,” an independent review by hospital physicians was sufficient for due process purposes. Parham v. J.R., 442 U.S. 584, 609 (1979) (holding juvenile commitment decision when made by a “neutral factfinder” sufficient to satisfy due process requirements).
In summary, numerous critical issues of law and policy relate to the development and implementation of CSC. Emergency planners, public health officials, and others working within state and local governments and private-sector entities to plan for (or execute) CSC in declared emergencies should (1) be highly knowledgeable about prevalent legal concerns, (2) objectively evaluate the need for legal or policy changes or clarification, and (3) generate meaningful legal solutions in advance of and during emergencies to facilitate real-time implementation of CSC. This may include instituting reforms to provide enhanced liability protection for health care workers, volunteers, and entities working to implement CSC, depending on the policy objectives and preferences within their jurisdictions.
ABA (American Bar Association). 2011. Report to the House of Delegates Resolution 125 (revised August 6, 2011). In American Bar Association House of Delegates: Delegate Handbook. Chicago, IL: ABA, http://www.americanbar.org/content/dam/aba/administrative/house_of_delegates/final_new_delegate_handbook_2011_2012.authcheckdam.pdf (accessed February 29, 2012).
AHRQ_(Agency for Healthcare Research and Quality). 2005. Altered standards of care in mass casualty events: Bioterrorism and other public health emergencies. Publication no. 05-0043. Rockville, MD: AHRQ.
AMA (American Medical Association). 2005. House of Delegates Resolution 803: Emergency preparedness. Dallas, TX: AMA.
AMA. 2007. Basic Disaster Life Support Manual Version 2.6. Chicago, IL: AMA.
AMA. 2008. House of Delegates Resolution 206: Uniform Emergency Volunteer Health Practitioners Act. Chicago, IL: AMA.
Annas, G. J. 2010. Standard of care—in sickness and in health and in emergencies. New England Journal of Medicine 362:2126-2131.
Binzer, P. 2008. The PREP Act: Liability protection for medical countermeasure development, distribution, and administration. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 6(4):293-298.
Carpenter, M., J. G. Hodge, and R. Pepe. 2008. Deploying and using volunteer health practitioners in response to emergencies: Proposed uniform state legislation provides liability protections and workers’ compensation coverage. American Journal of Disaster Medicine 3(4):17-23.
CDC (Centers for Disease Control and Prevention). 2010. Termination of the Emergency Use Authorization (EUA) of medical products and devices. http://www.cdc.gov/h1n1flu/eua/ (accessed September 5, 2011).
CDC. 2011. Mutual aid. http://www2a.cdc.gov/phlp/mutualaid/ (accessed August 20, 2011).
Centers for Law and the Public’s Health. 2001. The Model State Emergency Health Powers Act (2001). http://www.turning-pointprogram.org/Pages/pdfs/statute_mod/phsm_emergency_law.pdf (accessed August 23, 2011).
Centers for Law and the Public’s Health. 2004. Public health emergency legal preparedness checklist. Civil legal liability and public health emergencies. http://www.publichealthlaw.net/Resources/ResourcesPDFs/Checklist%203.pdf (accessed February 29, 2012).
Centers for Law and the Public’s Health. 2005. Hurricane Katrina response: Legal protections for intermittent disaster response personnel under a Federal Declaration of Public Health Emergency. http://www.publichealthlaw.net/Research/PDF/Katrina%20-%20Federal%20PH%20Dec%20and%20IDRP.pdf (accessed February 29, 2012).
Christian, M.D., L. Hawryluck, R. S. Wax, T. Cook, N. M. Lazar, M. S. Herridge, M. P. Muller, D. R. Gowans, W. Fortier, and F. M. Burkle. 2006. Development of a triage protocol for critical care during an influenza pandemic. Canadian Medical Association Journal 175(11):1377-1381.
Congressional Research Service. 2009. The 2009 influenza A(H1N1) outbreak: Selected legal issues. Washington, DC: Library of Congress.
Courtney, B., and J. G. Hodge. 2011. Legal considerations during pediatric mass critical care events. Pediatric Critical Care Medicine 12(6):S152-S156.
Courtney, B., R. Morhard, N. Bouri, and A. Cicero. 2010. Expanding practitioner scopes of practice during public health emergencies: Experiences from the 2009 H1N1 pandemic vaccination efforts. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 8(3):223-231.
Curie, J., and R. Crouch. 2008. How far is too far? Exploring the perceptions of the professions on their current and future roles in emergency care. Emergency Medicine Journal 25:335-339.
Devereaux, A. V., J. R. Dichter, M. D. Christian, N. N. Dubler, C. E. Sandrock, J. L. Hick, T. Powell, J. A. Geiling, D. E. Amundson, T. E. Baudendistel, D. A. Braner, M. A. Klein, K. A. Berkowitz, J. R. Curtis, and L. Rubinson. 2008. Definitive care for the critically ill during a disaster: A framework for allocation of scarce resources in mass critical care. From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest 133(Suppl. 5):S51-S66.
Dobbs, D. 2000. The Law of Torts. St. Paul, MN: West Group.
FDA (Food and Drug Administration). 2007. Guidance—emergency use authorization of medical products. http://www.fda.gov/RegulatoryInformation/Guidances/ucm125127.htm#preemption (accessed September 5, 2011).
FDA. 2009. Emergency use authorizations questions and answers. http://www.fda.gov/NewsEvents/PublicHealthFocus/ucm153297.htm (accessed September 5, 2011).
GAO (Government Accountability Office). 2008. Emergency preparedness: States are planning for medical surge, but could benefit from shared guidance for allocating scarce medical resources. GAO-08-668. http://www.gao.gov/new.items/d08668.pdf (accessed August 23, 2011).
Gostin, L. O. 2008. Public health law: Power, duty, restraint, 2nd ed. Berkeley, CA: University of California Press.
HHS (Department of Health and Human Services). 2007. Pandemic Countermeasures; Declaration Under the Public Readiness and Emergency Preparedness Act. Federal Register 72(21):4710-4711, http://edocket.access.gpo.gov/2007/E7-1635.htm (accessed February 13, 2012).
HHS ASPR (Department of Health and Human Services Assistant Secretary for Preparedness and Response). 2009. Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP): Legal and regulatory issues. Washington, DC: HHS, pp. 1-184.
Hick, J. L., J. A. Barbera, and G. D. Kelen. 2009. Refining surge capacity: Conventional, contingency, and crisis capacity. Disaster Medicine and Public Health Preparedness 3(Suppl. 2):S59-S67.
Hodge, J. G. 2009. The legal landscape for school closures in response to pandemic flu or other public health threats. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 7(1):45-50.
Hodge, J. G., and E. D. Anderson. 2008. Principles and practice of legal triage during public health emergencies. New York University Annual Survey of American Law 64(2):249-291.
Hodge, J. G., and E. F. Brown. 2011. Assessing liability for health care entities that insufficiently prepare for catastrophic emergencies. Journal of the American Medical Association 306:308-309.
Hodge, J. G., E. Brown, and J. O’Connell. 2004. The HIPAA privacy rule and bioterrorism prevention, planning, and response. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 2(2):73-80.
Hodge, J. G., E. Anderson, L. A. Gable, J. V. Vernick, and S. P. Teret. 2008. Emergency System for Advance Registration of Volunteer Health Professionals (ESAR-VHP): Legal and regulatory issues. Washington, DC: HHS, pp. 1-187.
Hodge, J. G., A. M. Garcia, A. D. Anderson, and T. Kaufman. 2009. Emergency legal preparedness for hospitals and health care personnel. Disaster Medicine and Public Health Preparedness 3(Suppl. 1):S37-S44.
Hoffman, S. 2008. Responders’ responsibility: Liability and immunity in public health emergencies. Georgetown Law Journal 96:1913.
Hoffman, S., R. A. Goodman, and D. D. Stier. 2009. Law, liability, and public health emergencies. Disaster Medicine and Public Health Preparedness 3(2):117-125.
HRSA (Health Resources and Services Administration). 2005. Countermeasures Injury Compensation Program. http://www.hrsa.gov/gethealthcare/conditions/countermeasurescomp/ (accessed February 1, 2012).
Ives, J., S. Greenfield, J. M. Parry, H. Draper, C. Gratus, J. I. Petts, T. Sorell, and S. Wilson. 2009. Healthcare workers’ attitude to working during pandemic influenza: A qualitative study. BMC Public Health 9:56-69.
Jervis, R. 2007. Charges against La. doctor dropped. USA Today. http://www.usatoday.com/news/nation/2007-07-24-katrina_N.htm (accessed August 23, 2011).
Kanter, R. K. 2007. Strategies to improve pediatric disaster surge response: Potential mortality reduction and tradeoffs. Critical Care Medicine 35:2837-2842.
Mastroianni, A. C. 2006. Liability, regulation and policy in surgical innovation: The cutting edge of research and therapy. Health Matrix 16:351-442.
O’Callaghan, N. 2008. Dying for due process: The unconstitutional medical futility provision of the Texas Advance Directives Act. Baylor Law Review 60:527, 587.
Pegalis, S. E. 2009. Physician and surgeon liability: Standard of care, generally. American Law of Medical Malpractice 3(3).
Quereshi, K., R. M. Gershon, and F. Conde. 2008. Factors that influence Medical Reserve Corps recruitment. Prehospital and Disaster Medicine 23(3):s27-s34.
Rosenbaum, S., M. B. Harty, and J. Sheer. 2008. State laws extending comprehensive legal liability protections for professional health-care volunteers during public health emergencies. Public Health Reports 123:238-241.
Schechter, S. 2007. Medical Reserve Corps volunteers’ ability and willingness to report to work for the Department of Health during catastrophic disasters. PhD diss., Naval Postgraduate School.
TFAH (Trust for America’s Health). 2008. TFAH liability protections relevant statutes. http://healthyamericans.org/reports/bioterror08/pdf/legal-preparedness-law-review-of-state-statutes-and-codes.pdf (accessed February 1, 2012).
Wise, E. 2008. Competence and scope of practice: Ethics and professional development. Journal of Clinical Psychology 64:626-637.
Volume 1 4: Cross-Cutting Themes
Issues related to ethics, palliative care, and mental health cut across the sector-specific guidance offered in Chapters 5-8 and are relevant at each stage of a disaster response. These issues are discussed in detail in this chapter; relevant aspects of each are reiterated in Chapters 5-8 where applicable.
The ethical allocation of scarce resources, discussed in the first section of this chapter, underlies any discussion of crisis standards of care (CSC). The committee’s 2009 letter report recognized seven key features of ethics on which CSC must stand: (1) fairness, (2) the duty to care, (3) the duty to steward resources, (4) transparency, (5) consistency, (6) proportionality, and (7) accountability. The framework of these key features sharply distinguishes between clinical practice that is acceptable in an environment of scarce resources and behaviors that are unacceptable regardless of the resource environment. However, the framework goes further to make the case that each stakeholder group—from the public, to health care providers, to health care institutions, to governments—has certain responsibilities and is afforded certain protections during a disaster.
The ethical framework lists fairness as its first operating principle. In doing so, it recognizes that the environment of a catastrophic disaster necessarily means it may not be possible to give everyone the care needed to survive. The framework recognizes that being unable, because of the situation, to provide all desired or even required services to each individual is not inherently unfair. Rather, fairness relates to how limited resources are distributed in these unusual situations. The second section of this chapter, therefore, addresses the importance of providing palliative care when curative care is unavailable and describes ways to strengthen this aspect of disaster response planning and implementation.
The third section addresses the issue of mental health, which, like palliative care, must be incorporated into CSC plans and affects their implementation at all levels of a disaster response. The discussion of this issue explores recent examples that demonstrate comprehensive plans to consider the mental health needs of the general public and those involved in a disaster response. It also explores how mental health care is a vital component of community resilience. Building on past progress, the committee posits essential elements of mental health care during and after a disaster strikes.
Each of these three cross-cutting issues directly impacts individuals and organizations responsible for developing and implementing CSC plans. This chapter should therefore be viewed as an accompaniment to Chapters 5-9. Application of the principles set forth in this chapter is necessary to ensure a holistic and humane disaster response.
As noted above, the committee’s 2009 letter report outlined an ethical framework to serve as the basis for designing ethically and clinically sound policies for CSC. In constructing this framework, the committee kept two key concepts in mind. First, groups that are most at risk before a disaster are those most vulnerable during a disaster. Ethically and clinically sound planning will aim to secure equivalent resources and fair protections for these at-risk groups. Second, some health care professionals question whether they can maintain core professional values and behaviors in the context of a disaster. Providers ask how to recognize when core ethical values draw a clear line separating behaviors that are acceptable during a disaster from those that are unacceptable at any time. An effective framework can help guide those who wish to behave as ethical professionals even in the austere circumstances imposed by a public health emergency. The committee reiterates its recommendation from the letter report:
Recommendation: Adhere to Ethical and Professional Norms in Crisis Standards of Care. When crisis standards of care prevail, as when ordinary standards are in effect, health care practitioners must adhere to ethical and professional norms. Conditions of overwhelming scarcity limit autonomous choices for both patients and practitioners regarding the allocation of scarce health care resources, but do not permit actions that violate ethical norms. (IOM, 2009, p. 6)
The above recommendation sets hard limits on ethically acceptable behavior, irrespective of conditions of scarcity or other aspects of public health disasters. CSC not only do not condone but are specifically designed to prevent the commission of acts that are clearly outside of ethical standards at any time. Instead, CSC incorporate ethically and clinically viable guidance on how to adjust clinical actions under austere conditions.
Key Features
The ethical framework set forth in the letter report includes substantive and process features and should support ethical behavior for those at every level of disaster response, from government planners to individual providers. Its key features are as follows:
• fairness,
• the duty to care,
• the duty to steward resources,
• transparency,
• consistency,
• proportionality, and
• accountability.
Each of these features is discussed in turn below.
Fairness
An ethical policy does not require that all persons be treated in an identical fashion, but does require that differences in treatment be based on appropriate differences among individuals. If particular groups receive
favorable treatment, such as in access to vaccines, this priority should stem from such relevant factors as greater exposure or vulnerability and/or promote important community goals, such as helping first responders or other key personnel stay at work (CDC, 2009). Policies should account for the needs of the most at risk and support the equitable and just distribution of scarce goods and resources.
Different communities may have different priorities for allocating scarce resources in a catastrophic disaster. Through appropriate public engagement processes (Chapter 9), for example, some communities may decide that such factors as age or function within the community (e.g., first responder) should be considered in allocating scarce resources in a catastrophic disaster. However, community preferences should adhere to parameters set by ethical norms and laws. For instance, irrespective of community views, it would not be ethically or legally viable for a community to refuse to provide health care resources to inmates in a local prison or to disabled residents of a residential facility. Similarly, both ethical standards and existing laws prevent communities from allocating scarce health resources on the basis of such irrelevant factors as race, ethnicity, or religious affiliation. Public health authorities are urged to engage their communities in setting priorities within appropriate ethical and legal parameters. Particular attention is due to those whose vulnerabilities and specific needs require accommodation in disaster plans. Relevant groups might include those with mobility impairments, existing significant medical conditions, pharmacologic dependence, lack of English language proficiency, or other ethnic or cultural needs (HHS, 2011).
Duty to Care
Health professionals, by virtue of their training, have an obligation to provide care, especially during a disaster. However, they are educated to care for individuals rather than for populations and thus may need to adjust the goals of care as dictated by the situation. Recognizing that scarce resources may restrict treatment choices, clinicians must not abandon, and patients should not fear abandonment, when a catastrophic disaster forces a shift to CSC. Ethical elements of disaster policies should support the professional’s duty to care. For instance, policies should separate triage responsibilities from the provision of direct care whenever possible. Those caring for individual patients should work to improve those patients’ health and not simultaneously make decisions intended to benefit the group rather than the individual patient.
While professionals have a duty to care for patients, health care institutions have a reciprocal duty to support health care workers (Pandemic Influenza Ethics Initiative Workgroup of the Department of Veterans Affairs, 2009). Personal protective equipment, engineering controls, and a variety of other mechanisms to reduce the risk of infection operationalize institutional obligations to protect workers who face risks in providing care (IOM, 2010).
Of note, the health care professional’s duty to provide care is neither absolute nor likely to be the only ethical obligation he or she faces. School closures and other shifts in services during a disaster may increase family obligations just when a professional is most needed at work. Among nurses, the vast majority are women, and many have primary child care responsibilities. A nurse who is also a responsible parent cannot leave a minor child at home unattended because of the duty to provide health care. Similarly, many emergency medical services (EMS) workers are volunteers who have full-time jobs and/or family responsibilities. These workers, too, face conflicting ethical obligations. As a logistical matter, such workers may not be available to serve for EMS during a disaster, and planning efforts should address this possibility. The reality of conflicting ethical obligations leads back to the concept of reciprocal obligations from systems to those who
serve within them. An ethically robust disaster response system should provide support that permits critical workers to meet personal obligations so they will also be able to meet professional obligations.
Duty to Steward Resources
Health care institutions, public health officials, physicians, and other health care professionals have a duty to steward scarce resources. The context of disaster, by definition, creates scarcity, since demand overwhelms supply. Ill-considered and wasteful use of limited medicines or other critical material may result in unnecessary deaths. The goal of preserving lives requires that professionals accept the responsibility to plan and to use resources prudently. As scarcity increases, balancing the obligation to honor the duties of care and stewardship will require more difficult choices (ACEP, 2006, 2008; Iserson and Pesik, 2003).
Transparency
A public engagement process is crucial for drafting ethical policies that reflect a community’s values and merit its trust. Officials should communicate clearly those plans currently in place, and should also work with the community to ensure that policies reflect local values and preferences. An inclusive process will incorporate input from professional groups and other organized stakeholders, as well as from those who are less well represented in the political process but may be greatly affected by policy choices. An ethical process will likely be iterative, characterized by responsible planning, transparency in underlying values and priorities, robust efforts toward public engagement, response to public comment, commitment to ongoing revision of policy based on dialogue and data, and accountability for support and implementation (see the detailed discussion in Chapter 9). Public engagement events in Harris County, Texas, on pandemic influenza issues (sponsored by Harris County Public Health and Environmental Services [HCPHES]) and in Seattle (Washington), Minnesota, and Michigan in conjunction with their guidance on the allocation of scarce resources illustrate the public interest in participating in the process and the valuable feedback these events provide for policy makers (see also Chapter 1). For example, the series of eight day-long public engagement events held in Harris County, Texas, in summer 2011 saw diverse participation from more than 600 members of the general public (Shah, 2012). Thirty service organizations were represented at a corresponding day-long stakeholder engagement event as well (Shah, 2012). The outcome of these events was productive identification and subsequent discussion of the community’s underlying values in allocating scarce resources during a disaster such as pandemic influenza. Officials at HCPHES reported to the committee that these deliberations are being incorporated into ongoing pandemic influenza planning efforts, including plans drafted by the Harris County Committee on Pandemic Influenza Medical Standards of Care. In addition to these public engagement efforts, HCPHES hosted more than 100 participants for a 2.5-day mass care/mass fatality planning workshop in summer 2011 aimed at convening multisector response partners who would have important roles in a severe influenza pandemic (Shah, 2012). Finally, the Louisiana Pandemic Flu Clinical Forum has engaged hospitals, providers, ethicists, religious leaders, attorneys, and the public to develop a CSC plan that addresses an extreme scenario—similar to that in the movie Contagion—wherein the severity of morbidity and mortality far exceeds the collective resources of health care available throughout the state or the nation (Louisiana Department of Health and Hospitals, 2011).
Consistency
Consistency in treating like groups alike is one way of promoting fairness. The public may feel that scarce resources have not been allocated fairly if patients at different hospitals in the same affected area receive vastly different levels of care. At the same time, however, efforts to keep policies consistent across institutions or geographic regions may limit local flexibility in implementing guidance.
Proportionality
Disaster policies may require burdensome recommendations, including social distancing, school closures, or quarantine. These burdens should be commensurate with the scale of the disaster and offer clear benefits in proportion to the burden.
Accountability
Effective disaster planning requires that individuals at all levels of the health care system (public and private sectors) accept and act upon appropriate responsibilities. Government entities are accountable to their communities for planning and implementing policies related to disasters, as outlined in this report. Accountability before, during, and after a disaster is key to building trust.
The Need to Make Difficult Choices
A major objective of public health preparedness is to build surge capacity so adequate medical care can be maintained even when numbers of patients rapidly increase and access to outside resources may not exist. Nonetheless, a disaster may force a community, at least temporarily, to confront the question of how to allocate medical resources that are insufficient for all those in need. Many different allocation systems may be proposed. Any ethically acceptable allocation system should adhere to the principles detailed above, including, most important, the principle of fairness. Generally, an allocation system will be more likely to pass the test of fairness if it reflects the additional principles of transparency, consistency, proportionality, and accountability. The ethics framework’s greatest potential for impact is during the development of CSC plans. Personnel with the responsibility for ensuring that CSC plans incorporate such ethical principles benefit the process best when they themselves are well versed in the specific issues affecting and affected by CSC plans and their implementation. It is also important to recognize how those issues expand upon and differ from ethical issues associated with routine medical practice. To ensure that the issues entailed in the process are resolved in a way that reflects community values, the committee recommends that the public be engaged in a dialog to help establish the standards that will be applied (see Chapter 9).
Any resource allocation system will reflect underlying values regarding who should receive limited resources, irrespective of whether the plan is simple or complex. For instance, plans that attempt to assess survival by using such tools as the Sequential Organ Failure Assessment (SOFA) score reflect particular value choices, in this case that resources are best used for those likely to survive rather than for those who will not survive despite access to treatment. This particular ethical choice reflects a desire to save the most lives by using resources prudently. Although saving the most lives is a widely accepted goal, it is a value-based choice, and not all may accept it. Others may wish to give priority to the young and thus not necessarily save the most lives, but the greatest number of years of life. In a discussion of values, health care providers, public health officials, and others may have strong views about what groups to privilege or what principles
to uphold. Professionals have special training that helps them determine how best to achieve certain goals. However, their expertise regarding values is no greater than that of community members. This equality in expertise regarding values is why community engagement is so crucial. Professionals cannot use medical resources to support the goals and values of the community unless they know what those goals and values are.
Some ethicists have argued that no fair allocation system can be devised other than a random lottery (Peterson, 2008). However, such a system would fail to adhere to the principle of stewardship of resources. Use of a lottery with no reference to prognostic factors in the allocation of scarce medical resources would result in excess mortality since some patients would receive treatment despite having a high probability of mortality with or without treatment, while others who might have survived would die without it. For specific cohorts for whom differences in morbidity and mortality are particularly difficult to predict and no validated scoring system exists, as is the case with critically ill children, some authors believe use of a lottery may be justified (Pediatric Emergency Mass Critical Care Task Force, 2012).
Age as a Factor in Allocating Scarce Medical Resources
The question of whether age is an appropriate factor in determining access to scarce health care resources arises repeatedly in allocation discussions. For instance, the United Network for Organ Sharing sets policy for the allocation of solid organs for transplant. Recently proposed revisions for the allocation of kidneys to adults include changes that take age into account by assessing how long a potential recipient will likely survive with the donated kidney (Organ Procurement and Transplantation Network, 2011). In this context, as in others, consideration of age in allocating scarce resources has been controversial (Hippen et al., 2011).
Critical care physicians have expressed discomfort with using age as a prognostic indicator, as there is substantial physiological variability among elders of similar chronologic age. Age-related changes to organ function may, of course, be reflected in the SOFA score or other variables used by the triage team, even when age is not an overt criterion for allocation. Critical care physicians surveyed expressed a reluctance to triage specifically based on age until age 85 (Society of Critical Care Medicine Ethics Committee, 1994). Yet using age-based allocation only for those older than 85 severely limits the utility of the variable, as only 1.2 percent of the U.S. population falls into this range (Census Scope, 2011). Nonetheless, a Canadian workgroup developed guidance for the allocation of scarce resources in an influenza pandemic and listed age above 85 as an exclusion criterion (Christian et al., 2006). Others have incorporated age into their triage criteria, arguing that younger patients deserve an opportunity for a full life (Persad et al., 2009; Williams, 1997). Community engagement discussions in Minnesota and Seattle supported this general concept, although there was no consensus on age ranges or differences in age, or on how important age should be in the allocation process (Garrett et al., 2011; Public Health-Seattle and King County, 2009). While not specifically focused on age, a community engagement project in Massachusetts produced contrasting results: both consumers and health care providers objected to an allocation process that offered critical care resources only to those with an expected life span of more than 6 months (Levin et al., 2009). Additionally, participants in the community engagement discussions of a severe pandemic in Harris County, Texas, felt that using age alone as a factor in decisions about allocating critical resources was unacceptable; when age was shown to play a role in vulnerability to the disease, however, it was deemed a viable consideration (Shah, 2012). Finally, it is important to note that not all cultural groups value the young; some groups prize their elders and would not agree with giving younger patients priority.
There is no easy answer to the question of age as a triage criterion. Some participants in the disaster planning process see significant relevance in the “fair innings” argument, while others do not. However, all agree that decisions around age should incorporate community values. In particular, community engagement processes should address the following questions:
• How important is age? For example, should age be a criterion in itself, or only when two patients who are otherwise similar in terms of medical prognosis both require a scarce resource?
• What age ranges/differences should be considered? Should age be considered across the life span, or is there a ceiling above which advanced age should limit care options?
• How does this community weigh age in relation to other factors, such as prognosis or a critical work role (e.g., as a first responder)?
The Role of Families in Supplementing Scarce Health Care Resources
Families provide substantial amounts of medical care to injured and ill loved ones every day across the country. The role of family in protecting at-risk members of the population is of more, not less, importance in the setting of a disaster. Tragically, family advocacy can mean the difference between life and death. In the aftermath of Hurricane Katrina, some families in New Orleans were able to overcome a policy forbidding evacuation of patients with do-not-resuscitate orders, while patients who lacked successful advocates stayed and perished (Fink, 2009).
The question of whether families can appropriately supplement medical care in a disaster arises in a number of contexts. Family members may accompany ill relatives into the acute care setting. Indeed, many facilities will likely ask family members to serve as volunteers for nontechnical tasks, such as delivering food trays to acute care patients, to free trained personnel for more complex tasks. Facilities should be mindful, however, of whether family efforts benefit all patients or only the family member. For instance, a family member performing general assistance and custodial chores helps all patients and staff; in contrast, seeking out and harassing overtaxed staff to supply a higher level of care for a loved one than is available to other patients may benefit a single individual while disadvantaging many others. The possibility of threats to staff from family members may increase if and when resources become truly scarce. Facilities will need to consider plans for limiting family access to critical care settings in those circumstances.
The lack of family can be as life-threatening a scarcity as the lack of access to medical resources, and there is no public consensus on how to address the various consequences of social isolation. This problem arises with the question of using bag-valve ventilation as a supplement when critical care resources are in short supply. Those with family members may have willing volunteers to provide manual ventilation, while at-risk members of the community, including many elderly patients, may not have such volunteers. Among the options is to require those who are willing to provide manual ventilation to enter a lottery so they will not know to whom they will be assigned. This approach would allow those connected to large volunteer groups, such as through their church or family, to share their resources with those who are isolated. Depending on the nature of the disaster, other facilities may choose not to permit or encourage manual ventilation, citing its likely lack of efficacy or the exceptionally large use of labor, a scarce resource, needed to support a small number of patients in this fashion.
Summary
CSC permit clinicians to allocate scarce resources so as to provide necessary and available treatments to patients most likely to benefit. CSC do not permit clinicians to simply ignore professional norms and act without ethical standards or accountability. CSC justify limiting access to scarce treatments, but neither the law nor ethics support the intentional hastening of death, even in a crisis.
The nation may at any time be confronted with a disaster that can threaten its way of life or how Americans perceive it as a resource-rich, humane country. In the event of a mass casualty incident, such as pandemic influenza or the detonation of an improvised nuclear device, resources for the delivery of health care may be depleted, and resupply may be either slow or nonexistent. One problem that can be anticipated in a catastrophic disaster situation is having more people who require care than available resources to provide that care.
Despite a resource-poor situation, the obligation remains to provide people with care, comfort, and symptom management throughout a disaster. Although a relatively new component of disaster planning, the principle of palliative care (with specific regard to supportive care at the end of life) should include a holistic and humane approach to public health and health care services during such an incident, and should be considered in the development of community plans for disaster response. The provision of palliative care in the context of a disaster with scarce resources can be considered a moral imperative of a humane society.
The Imperative to Provide Palliative Care
Palliative care is a specialty that focuses on relief of pain and other symptoms of serious illness, with the goal of preventing and easing suffering and distress while offering patients and their families the best possible quality of life. Palliative care is appropriate at any stage of a serious or life-threatening illness and is not dependent on prognosis. It can also be provided at the same time as curative and life-prolonging treatment. The provision of palliative care improves health care quality in three key areas:
• relief of pain and other symptoms and emotional suffering for patients and families;
• enhanced communication and decision making among patients, health care practitioners, and families; and
• improved coordination of care across multiple health care settings.
In its 2009 letter report, the committee stated that palliative care should be available to all people affected by a disaster (IOM, 2009). The key services include comfort, compassion, and maintenance of dignity—services that can be provided with essentially no physical resources other than the presence of another human being.
The public would likely benefit from understanding that palliative care, in ordinary times or during a disaster, prevents a sense that society or its health care professionals have abandoned the patient or deliber-
ately caused death. Instead, palliative care respects the humanity of those who will die soon, minimizes their discomfort, supports their loved ones, and provides aggressive treatment of symptoms (e.g., pain, shortness of breath) (Domres et al., 2003; Matzo et al., 2009).
Ethical considerations and principles associated with scarce resources and CSC should be incorporated into CSC planning. As noted earlier, public health disasters justify temporarily adjusting practice standards and/or shifting the balance of ethical concerns from a focus on the needs of individuals to a focus on the needs of the community (Orr, 2003). Yet while the primary goal of a coordinated response to a disaster should be to maximize the number of lives saved, a practical plan also should provide the greatest comfort for those who will live for a while before dying as a result of the incident (Holt, 2008). Palliative care can play an important role in mass casualty incidents when resources are scarce. Special attention should be given to the planning and resources necessary to maximize care for patients with serious, advanced illness prior to a disaster, as well for those facing the end of life as a result of the disaster.
Resiliency in the face of a disaster requires a fully integrated and coordinated strategy to address how services will work together. All sectors of the health care system will be called upon to respond and save lives, or when that is not possible, to ensure a comfortable death. Advanced illness and end-of-life care pose particular challenges during health emergences, given complex care needs and the often competing demands for health care practitioners, supplies, and space. Palliative care surge capacity will be needed across settings. This need brings many challenges, including educating professional staff unfamiliar with delivering palliative care, stockpiling and providing necessary medications for effective symptom management at the end of life, and establishing protocols for symptom management for at-risk populations. Meeting these challenges will require training nonprofessional caregivers in basic comfort measures and ensuring broad-based coordination among EMS, hospitals, hospice and palliative care professional organizations, home care agencies, long-term care facilities, and state and local public health authorities. The emerging role of health care coalitions will also be instrumental in the successful integration of palliative care planning and implementation into regional protocols for disaster response.
What should first responders, disaster personnel, and health care providers do when all in their care cannot reasonably survive given the scope of injuries, the magnitude of exposure, environmental conditions, and pre-existing medical conditions? At a minimum, disaster response palliative care services should include relief of severe symptoms and comfort as people are facing death. There will be a sizable number of people for whom death can be expected, although they may live for hours, days, or weeks. Those who are not expected to survive cannot simply be consigned to holding areas while still alive, nor should they and their family advocates overwhelm hospitals and EMS systems that could be addressing the needs of potential survivors (Matzo et al., 2009).
Those who are dying or near death as a result of or during a disaster can be cared for humanely if plans and protocols for such care are established in advance of the incident. When all people cannot reasonably be saved because of the immediacy and scope of mass injuries and in the face of suddenly scarce resources, choices should be made as to who will most likely benefit from life-saving treatment (i.e., survive in the short as well as long term). The ethical assessment of benefit, burden, and efficacy may shift in the context of a disaster. Facilities should devise plans to meet the needs of excess patients in a disaster. If, despite these planning efforts, triage policies are triggered, scarce curative treatment will likely be directed to those patients most likely to survive the short-term effects of acute injury and/or illness, although the potential for
long-term survival will be equally important, taking into consideration the prognosis for pre-existing chronic underlying medical condition(s) for patients in hospital or chronic care facilities.
Identifying transition points in a person’s condition helps the patient, the family, and health care practitioners prepare for the final stage of life. A transition point can be defined as an incident in the trajectory of an illness or injury that moves the patient closer to death. For example, a patient with chronic obstructive pulmonary disease may experience no change in her condition until she contracts influenza and never fully recovers; for that patient, contracting influenza is a transition point in her condition (Berry and Matzo, 2004). Prognostication, aided by a risk index or scale, enables health care practitioners to formulate clinical strategies during a crisis situation. These tools may be helpful in determining whether a patient’s illness has reached a terminal phase (Matzo, 2004). Providing a treatment category of “palliative care” for those not likely to survive will be an important service option for responders and triage officers. Acknowledging that a person is not likely to survive typically leads to discussions regarding goals of care, appropriateness of interventions, and efforts to help the patient and family begin to say goodbye (Matzo, 2004).
The Agency for Healthcare Research and Quality (AHRQ) published a report outlining principles to guide community planning for the delivery of health care in the face of overwhelming numbers of casualties (AHRQ, 2005). The intent of this planning guide was to assist state and local planners in developing plans that would optimize their ability to provide direct care for as many people as possible while protecting the rights of individuals to the extent possible under the circumstances. To achieve this goal, plans should promote the fair and equitable use of scarce resources. These resources may include emergency department, hospital, intensive care unit, or specialty care beds; transport assets; pharmaceuticals/countermeasures; medical equipment and materiel; and personnel. As in all situations of scarce medical resources, clinicians will use available triage tools and their professional judgment in identifying those individuals whose health condition suggests they will obtain the greatest benefit from the available resources (AHRQ, 2005).
A survey of disaster planning and palliative care key informants found that few in the disaster preparedness community or the palliative care community had been involved in coordinated planning activities in which the role of palliative care in emergency response was recognized (Matzo et al., 2009). Key informant discussions and an expert panel dialogue highlighted the importance of palliative care (e.g., aggressive symptom management) in a holistic and humane community disaster planning and response capability (Matzo et al., 2009). These discussions led to several recommendations: that specific roles and responsibilities and incident-driven resource requirements in all settings (e.g., the location of an incident, acute care hospitals, nursing homes and other alternate care sites, home) should be identified, defined, and provided; that palliative care services should be fully incorporated into all levels of state and local disaster planning/ training guidelines, protocols, and activities; and that first responder personnel and local and regional disaster response planners (e.g., EMS; fire, police, and public health departments; community health clinics; local and regional government entities) should be involved in identifying and developing clear specifications for what levels of care are to be delivered in what settings (at the incident, in alternate care sites, in existing secondary referral sites such as nursing homes or individuals’ homes) and by whom (e.g., first responders, rescue personnel, palliative care personnel, long-term care personnel). As discussed in Chapter 8, alternate care sites offer an opportunity to incorporate palliative or end-of-life care. For example, Michigan uses the Modular Emergency Medical System model and has been planning for end-of-life care consistent with the alternate care facilities planning guides (Cantrill et al., 2009).
Pain is the primary symptom in need of management in both disaster and war; “to prevent chronic pain and neuropathic pain as a result of amputation, burn injuries, delayed wound healing, malnutrition or infection, pain relief in disaster victims is of paramount importance” (Domres et al., 2003). Therefore, effective pain and symptom management should be a basic minimum in service delivery and training for palliative care during a disaster. Training for palliative care should be competency based, with programming specific to the individual’s role in emergency response. It should cover, at a minimum, the basic philosophy and goals of palliative care, basic symptom management (e.g., pain, anxiety, shortness of breath), the use and titration of oral and injectable narcotic analgesics for patients in pain and/or near death, symptom recognition in the case of pandemic influenza or a chemical or radiological attack, and basic psychosocial counseling and support. Disaster planning should take into account the potential benefits of stockpiling palliative care medications at accessible sites, including away from acute care hospitals (e.g., in nursing homes), and should include training for disaster responders in how to locate, access, and use these medications. The committee recognizes that federal, state, and local governments are already engaged in creating and maintaining pharmaceutical stockpiles, and while issues may exist with respect to stockpile management and rotation, those issues are beyond the scope of the committee’s charge and expertise.
A Triage Model
A triage model for use in palliative care includes categories not typically seen in other triage models (Cone and MacMillian, 2005; Janousek et al., 1999). Figure 4-1 presents the model of triage used for the expert
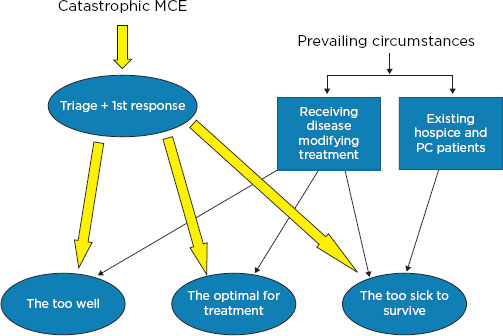
FIGURE 4-1
A triage and response model.
NOTE: MCE = mass casualty event; PC = palliative care.
SOURCE: AHRQ, 2007, p. 107.
discussion cited above (Matzo et al., 2009). The term “likely to die” was defined as those people who are too sick or injured to survive hours, days, or weeks, most often categorized as the “expectant/black,” “nonsalvageable,” or “non-savable” victims. In practice, however, this category may also include those labeled “immediate” if needed medical resources are unavailable. This category could also include cases in which an individual is already dependent upon the usual health care system to survive (e.g., ventilator-dependent patients), has an existing life-threatening illness (e.g., extensive cancer), or has illness secondary to injuries sustained in the disaster (Matzo et al., 2009).
The “likely to die” category is very broad but reflects the current state of the triage classification. Established triage schemes have substantial limitations when applied to the special circumstances of a disaster and the provision of palliative care. For example, many of the schemes do not attend to the likelihood of survival for patients with critical pre-existing medical conditions. Furthermore, there is a paucity of data addressing the critical question of whether correctly sorting casualties into the categories of any particular triage system results in improved outcomes, and one system may not handle all potential triage decisions in all triage settings (Cone and MacMillian, 2005). In practice, moreover, the “expectant” category often is applied only to those patients who are not breathing after one attempt at repositioning and opening the airway; all other critically ill or injured persons are treated as “immediate” or “delayed” (red or yellow). Finally, the usual triage schemes do not include palliative and comfort care measures as an alternative to curative treatment (Cone and MacMillian, 2005; Matzo et al., 2009).
A triage system for allocation of scarce resources will function best if it is transparent; fair; valid; consistent across settings and events; dynamic (applied at multiple places and times); and flexible enough to address changing circumstances, including responding when patients triaged as likely to die actually improve or when additional treatment resources become available (Matzo et al., 2009). Preserving a functioning health care system during and after a disaster will require the adoption of principles of field triage, limits on the use of ventilators and surgery, and the creation of alternate care sites. Research is beginning to provide a scientific underpinning for triage (Sacco et al., 2005), as well as to identify basic criteria for critical care triage during a disaster in which medical resources are scarce (Devereaux et al., 2008; Wilkinson et al., 2007). Future research will have to address the applicability of triage to palliative care, as well as the role of palliative care in disaster response. The arguments for incorporating palliative care into disaster response—humane treatment, diversion of dying people away from overburdened hospitals, more effective use of scarce resources, and the provision of care that patients want—have moral weight on their own, but research should still assess their impact.
In developing CSC plans, state and local public health agencies should work with hospice and other relevant partners to incorporate palliative care into disaster response plans. These efforts should include the development of
• evacuation plans for those who would be likely to benefit from palliative care;
• a community response plan, staffing plans, and training programs for first responders and other relevant medical personnel;
• transparent, community-based, explicit triage criteria for those not likely to survive;
• community conversations to engage, educate, and prepare the public;
• a plan for stockpiling needed medications and supplies at hospitals and at sites located away from hospitals (Wilkinson et al., 2007); and
• out-of-hospital considerations that may warrant moving individuals expected to die to care sites other than acute care hospitals.
In addition, palliative care professionals should participate in disaster planning, response and recovery training, and public education (Holt, 2008). First responders and health care providers at all disaster care sites (incident sites, alternate care sites, and hospitals) should have training in effective pharmacological pain and symptom management and psychosocial support. It is recognized that the burden to educate all of these personnel would be out of scope, but just-in-time training for those faced with palliative care responsibilities should be developed as part of the planning process.
Rebmann and colleagues’(2009) survey of 633 infection control professionals found that fewer than one-quarter of hospitals had convened their ethics committee to discuss preparedness issues or developed policies/procedures for CSC during a catastrophic disaster. During Hurricane Katrina, absent supplies and direction, the palliative care response was erratic and inefficient. One way to ameliorate a chaotic palliative care response is to form palliative care response teams comprising psychologists, chaplains, and health care providers with knowledge of palliative care as a core component of the emergency response process. Crosstraining of personnel in other areas to serve in this capacity is also important. As the volume of patients
BOX 4-1
Essential Elements of Palliative Care Under Crisis Standards of Care Conditions
• Principles of palliative care integrated into response structures/plans
• Rapid palliative care response team trained to provide palliative care at all service delivery sites (hospitals, local/regional and state response systems) in near real time:
o education regarding pain and symptom management;
o training for all community members of the response team in how to use narcotic analgesics, anxiolytics, and other medications to manage pain and symptoms until licensed personnel are available to manage these symptoms themselves;
o consideration of stockpiling these medications for use under CSC; and
o basic counseling and supportive training and support care as an integral part of all basic disaster training and for all responders.
• Education for all first responders and providers that includes
o how to access the medication stockpile;
o how to titrate opiates for people in pain and near death;
o how to use the medications to manage symptoms so individuals experience a comfortable death; and
o basics of psychosocial counseling and support for peer-to-peer and providerpatient services under mass casualty incident scenarios.
triaged to palliative care expands, so, too, will the strain of providing mass palliative care. Periodic emotional and psychological relief will be necessary for these palliative care providers through their rotation to other groups; this will be an important consideration for the welfare and morale of the provider corps as a whole.
Management of the dead can be one of the most difficult aspects of disaster response, and it has profound and long-lasting consequences for survivors and communities. Immediately after a catastrophic disaster, identification and disposal of human remains often are performed by local communities, primarily through local funeral directors and homes.
Summary
Facing the deaths of large numbers of its members while ensuring that those deaths are as pain and symptom free as possible is a major challenge for a community. Boxes 4-1 through 4-3 summarize key considerations in incorporating palliative care into CSC planning and implementation. Box 4-1 lists essential elements of palliative care under CSC conditions; Box 4-2 presents discussion topics for palliative care planning; and Box 4-3 details key points related to the implementation of palliative care in disaster situations.
BOX 4-2
Discussion Topics for Palliative Care Planning
• Define common medications for community stockpile and cache locations as a potential part of the regional planning effort.
• Develop the skills, materials, and memorandums of understanding needed to shelter and/or evacuate people with palliative care needs.
• Develop decision guidelines for who should receive palliative care, how it should it be delivered, and how to handle large numbers of people expected to die and those already very sick or disabled.
• Develop criteria for allocating scarce and highly specialized clinical resources for palliative care.
• Identify differences and similarities in general considerations for the delivery of palliative care in a mass casualty event versus such events as bioterrorism and avian influenza.
• Determine whether the current system, given needs for shelter and evacuation, is sufficient, and if not, what additional support is required.
• Determine whether evacuation decisions are to be made for those requiring palliative care as part of overall regional evacuation planning efforts.
• Develop the key skills required for first responders regarding palliative care.
• Modify documentation standards to ensure that medical records reflect the delivery of palliative care without posing an undue administrative burden.
• Develop a plan for respectfully managing a large number of deaths and disposal of the bodies.
• Develop treatment protocols for those who are dying, in pain, or experiencing symptoms.
SOURCES: AHRQ, 2007; Wilkinson et al., 2007.
BOX 4-3
Implementation of Palliative Care in Disasters: Key Points for Planners
Incident Command and Operations
• Request the participation of local, regional, and state disaster planning leadership to form a network of leaders in home health, palliative care, hospice care, and long-term care that will be engaged in disaster planning.
• Integrate palliative care (e.g., clinical and spiritual/psychosocial support for casualties and providers) into command and operations. Consider
o the role of opioids, steroids, diuretics, etc.; and
o the role of providers.
• Coordinate with public health and emergency management to develop a registry of vulnerable populations. Oversee the development of planning and training efforts that support the delivery of palliative care.
o Integrate palliative care planning into the development of alternate care systems.
o Develop evacuation plans for existing and new palliative care patients.
o Use social media (e.g., texting) and other methods to help family members stay in touch with each other.
o Develop a community response plan, staffing plans, and training programs for first responders and other relevant medical personnel.
• Establish transparent, community-based, and explicit triage criteria for casualties not likely to survive.
o Develop a public education program.
o Consider stockpiling needed palliative care medications and supplies.
o Have planners participate in otherwise provider-oriented disaster planning, response, and recovery training.
Planning Key Points
• I ncorporate community-based long-term care and palliative care providers in all phases of planning, response, and recovery as integral members of the response team.
• I ntegrate specific planning for those likely not to live long into all established scenarios (all-hazards approach) and response plans. Include in planning issues of palliative care for pediatric and at-risk populations.
Training
• I ncorporate palliative care training for disaster responders as an integral part of exercises, planning, and response, building on existing disaster planning and command and control structures.
• Determine who should deliver this care:
o hospice staff/long-term care registered nurses/certified nursing assistants, etc.;
o clergy/mental health professionals;
o rehabilitation personnel; and/or
o volunteers.
• Identify the training/certification needed to deliver palliative care successfully in the setting of a disaster.
o Identify personnel who would be qualified to participate in the delivery of palliative care.
o Examine an expanded role for family participation in care.
o Coordinate with mental health resiliency efforts to support those responders engaged in the delivery of palliative care.
Development of Triage and Treatment Decisions
• Work with first responder personnel and local and regional disaster response planners (e.g., emergency medical services [EMS]; fire, police, and public health departments; community health clinics; local and regional government entities) to develop clear guidelines and protocols addressing the following issues:
o Triage
![]() Develop criteria for triage into levels of care (achieving the greatest good for the greatest number; prioritization not based on social worth but on societal need). Demand for interventions will be progressive with the increased demand for resources.
Develop criteria for triage into levels of care (achieving the greatest good for the greatest number; prioritization not based on social worth but on societal need). Demand for interventions will be progressive with the increased demand for resources.
![]() Develop a classification of existing patients who are chronically ill; pediatric; geriatric; and in community, health care, or long-term care facilities (e.g., by prognosis from MDS/OASIS/Surprise Question, “Would you be surprised if this person were dead in 6 months?"): those expected to die imminently or in the very near future from injuries sustained in the disaster; those clinicians would expect to die in less than 6 months (from injuries or previously established disease)*; and those likely to live more than 6 months. Also develop criteria for reversal of triage decisions.
Develop a classification of existing patients who are chronically ill; pediatric; geriatric; and in community, health care, or long-term care facilities (e.g., by prognosis from MDS/OASIS/Surprise Question, “Would you be surprised if this person were dead in 6 months?"): those expected to die imminently or in the very near future from injuries sustained in the disaster; those clinicians would expect to die in less than 6 months (from injuries or previously established disease)*; and those likely to live more than 6 months. Also develop criteria for reversal of triage decisions.
The population-level impact of a disaster reflects a continuum of risk and resilience, and can include prevalence rates of mental health disorders among 30-40 percent of direct victims (Galea and Resnick, 2005). In addition, many individuals will experience transitory, subsyndromal distress that will dissipate as a result of resilience.
Comprehensive planning for the mental health and social consequences of CSC requires consideration of the full continuum of risk and resilience. The focus includes patients, their families, health care providers, and the general public. The use of CSC and the broader context in which it is required will significantly challenge the resilience of the community (and even the nation). There will also be unique opportunities to
![]() Decide what will be done about those expected to die imminently who do not (and establish a process for retriage).
Decide what will be done about those expected to die imminently who do not (and establish a process for retriage).
o Alternate care sites for palliative care
![]() Decide what equipment (e.g., dialysis, oxygen, monitors/pulse oximeters/laboratory equipment/x-ray) is needed.
Decide what equipment (e.g., dialysis, oxygen, monitors/pulse oximeters/laboratory equipment/x-ray) is needed.
![]() Determine the need for beds/facilities (e.g., nursing homes, retirement communities)—specific spaces vs. integrated.
Determine the need for beds/facilities (e.g., nursing homes, retirement communities)—specific spaces vs. integrated.
![]() Will mass casualties require facilities other than the ones they are in at the time of the incident (e.g., target patients in acute care facilities, alternate care sites)? Long-term care providers could provide shelter and daily care to at-risk elderly and disabled persons who ordinarily live at home at a time when home environments are unsafe (lack of power, water, etc.).
Will mass casualties require facilities other than the ones they are in at the time of the incident (e.g., target patients in acute care facilities, alternate care sites)? Long-term care providers could provide shelter and daily care to at-risk elderly and disabled persons who ordinarily live at home at a time when home environments are unsafe (lack of power, water, etc.).
o What levels of care are to be delivered in what settings and by whom?
o Clearly identify lines of authority and responsible personnel.
• Address issues related to supplies/drugs (stockpiled where/by whom, how to deliver, shelf life, security, storage, controlled substance administration, subcutaneous butterfly needles [tegraderm so syringes can be reused to connect to the subcutaneous port for ongoing medication administration]). Consider specific drugs to alleviate symptoms:
o opioids—oral and injectable—to treat anxiety, pain, dyspnea, agitation;
o antianxiety drugs—benzodiazepines, antipsychotics (oral and injectable);
o acetaminophen and other nonprescription, nonopioid comfort medications (nonsteroidal anti-inflammatory drugs [NSAIDs], diphenhydramine);
o diuretics to treat dyspnea;
o steroids to manage pain from inflammation and dyspnea; and
o antinausea and antidiarrheal medications.
*Note that this determination needs to accord with community expectations/priorities, and any triage scheme should be uniform, not designed to address a specific population (e.g., patients in long-term care). SOURCES: Holt, 2008; Wilkinson et al., 2007.
mitigate these impacts by incorporating the social and psychological aspects of disaster response into CSC planning, as proposed in the committee’s 2009 letter report (IOM, 2009).
Scope of the Issue and Range of Impact
CSC poses unique challenges for all involved in a disaster, including health care providers (and their families), patients receiving health care, and the public.
Although health care providers may confront life-and-death decisions on a daily basis and routinely experience the loss of patients, CSC differs from these experiences both quantitatively and qualitatively. For example, as soon as care shifts from a focus on the needs of individual patients to a focus on the greatest good
for the most people, the entire health care team may have very different experiences with life-and-death decisions. If a disaster results in mass casualties, a significant threat to the mental health of the health care workforce may result. If not sufficiently addressed, these foreseeable mental health consequences may further degrade the functionality of the health care system and its ability to implement CSC optimally. Health care workers may bear the double burden of stress due to their professional roles and that due to seeing their families and friends requiring care within the CSC context. In some public health emergencies, moreover (such as the epidemic of severe acute respiratory syndrome [SARS]), health care workers themselves are subject to elevated health and mental health risks (Hawryluck et al., 2004; Lin et al., 2007).
Patients and families also will face significant psychosocial impact. The idea that CSC treatment decisions are based on the most good for the most people may run counter to their previous experiences, expectations, and wishes. If patients encounter CSC decisions that involve life-and-death consequences for their loved ones (which also may include disproportionate numbers of children and their parents), a significant population-level mental health burden and even the potential to unravel the social fabric of communities may result. Relationships between providers and their patients and patients’ families will face unprecedented complexities as CSC decisions are communicated and implemented and their consequences unfold at the clinic or bedside. Following the anthrax attacks in 2001, for example, the complexity of evolving risk communications and perceptions of differences in care among patient groups reflected episodic confusion among local and federal public health officials, medical providers, and patients (see Gursky et al. [2003] for a review). Public health emergencies that involve both CSC and social distancing may be particularly challenging as common sources of support, and hence resilience, are reduced (Gostin, 2006).
When these issues evolve on a regional or national scale, the potential for the perception of inequality in the application of CSC grows, and the protective impact of the sense that “we are in this together” is diminished, posing a threat to resilience. Although prosocial behavior is by far the most commonly observed collective response after a disaster (Glass and Schoch-Spana, 2002), planning should take into account the potential for negative social behaviors that may include aspects of panic. Indeed, there is limited consensus that certain features of emergency situations can trigger panic-like phenomena. For example, following the Three Mile Island nuclear incident, for every person that was asked to evacuate, 45 actually did, creating unintended gridlock. The prospect of pandemic influenza, which could entail significant morbidity and mortality, may also generate some undesirable collective behaviors among those attempting to avoid contagion, such as obtaining nonrecommended antiviral prophylaxis. Following the recent nuclear meltdown in Japan, for example, sales of potassium iodide, a treatment that prevents uptake of radioactive iodine by the thyroid gland, skyrocketed. Worldwide availability of potassium iodide ceased altogether for a period of time despite the quadrupling of prices (Aleccia, 2011). Factors that may be tied to the potential for mass panic in the CSC context include
• a belief that there is a small chance of escape from the agent,
• perceived high risk,
• available but limited treatment resources,
• no perceived effective response, and
• loss of credibility of authorities (DeMartino, 2001).
A high-mortality incident entailing CSC may have sufficient triggers to ignite panic behavior in some individuals and subpopulations. These risks occur against a backdrop of the recent finding that only 35 percent “of the American public is confident in the health care system’s readiness to respond effectively to a deadly flu pandemic” (National Center for Disaster Preparedness, 2005, p. 1). For example, among respondents to the Los Angeles County Health Survey, which included questions regarding terrorism preparedness, 17 percent reported having developed an emergency plan and 28 percent maintaining additional supplies of food, water, and clothing (Eisenman et al., 2006).
The full range of these impacts at the public level needs to be considered more fully. Traditional risk communications that focus on content are necessary but not sufficient to facilitate resilience and manage the emotional fallout that public health emergencies can engender. Engagement of the public (and health care providers) is essential to maintaining individual and community resilience (see Chapter 9). In fact, it should be regarded as a fundamental component of preparedness such that it is incorporated throughout the stages of response in a public health emergency that requires CSC.
Finally, there is a largely uncharted opportunity to leverage social media to facilitate national resilience in the face of a disaster. These media could be used to convey the notion that, despite challenges and traumatic outcomes for some, “we are in this together,” and to clarify the use of a common CSC approach governed by the ethical principles outlined in this report.
Patients with Psychiatric Emergencies as a Particular Crisis Standards of Care Subpopulation
In many communities across the United States, the allocation of scarce resource is already necessary to address chronic shortages of inpatient mental health beds for adults and children (Geller and Biebel, 2006; SAMHSA, 2007). In some communities, patients presenting to the emergency department with life-threatening mental health conditions are never transferred to an appropriate level of care or must wait days in the emergency department environment before receiving definitive psychiatric care (Schumacher Group, 2010). In some disaster scenarios, demand on these resources may be even greater, magnifying the need to develop CSC specific to psychiatric emergencies that entail immediate danger to those gravely disabled by their psychiatric illness or others. The development of CSC specific to the management of highly limited involuntary psychiatric resources will also be necessary. Strategies will need to consider cases in which psychiatric patients with comorbid medical conditions require care under CSC (see the HHS [2012] definition of at risk).
Operational Guidance to Enhance Resilience and Manage the Mental Health Consequences of Crisis Standards of Care
The 2009 letter report offered specific strategies and described several national best-practice initiatives with respect to managing the mental health consequences of mass casualty events (IOM, 2009). Here the committee offers more detailed operational guidance tailored to patients, providers, and the general public. At the various levels of hospital facility, local/regional, and state planning, the following elements are necessary to address the continuum of resilience and mental health issues tied to CSC (see also Box 4-4):
BOX 4-4
Functions for Mental Health Response to Crisis Standards of Care
• Suggested: Concept of mental health operations in CSC integrated into incident command system and other response structures and plans
• Specific capabilities and capacities required for patients/families, providers, and the general public in response to CSC:
o Rapid mental health triage system with “floating triage algorithm” linking disaster systems of care, including hospitals, clinics, etc., with local/regional and state response systems in near real time (Pynoos et al., 2004; Schreiber, 2005); real-world examples: PsySTART Rapid Triage System in Los Angeles County, State of Minnesota Department of Public Health, American Red Cross’s Disaster Mental Health Triage and Surveillance System
o Continuum of acute phase evidence-based interventions
o Psychological first aid adapted specifically for community resilience/social support enhancement in a CSC context and for use by the general public, health care workers, and disaster systems of care; example: Los Angeles Department of Public Health’s community resilience program with “Listen, Protect and Connect—neighbor to neighbor, family to family” psychological first aid/social support
o Development of behavioral coping component of risk communications (NBSB, 2008), including creation of new “coping with CSC” messaging
o Gap analysis with action plan to build key local disaster mental health and spiritual care capacities without mutual aid, including capacity to leverage novel, evidence-based Internet interventions for posttraumatic stress disorder (PTSD), depression, anxiety, and substance abuse
o Development of health care provider resilience capabilities and approaches with preincident stress inoculation, “individual/family resilience planning,” acute phase self-triage and Internet-based interventions for higher-risk subset (see Ruggiero et al., 2011); example: the “Anticipate, Plan, and Deter” health protection/resilience system, which includes preincident preparedness (stress inoculation), development of responder “resilience plans” (including family plans, social support systems, and basic psychological first aid), and identification of cumulative stress burden with Internet-based interventions for those at risk
SOURCE: Pynoos et al., 2004; Schreiber, 2005.
• A disaster mental health concept of operations and operational disaster mental health plan should be developed.
o These plans may guide the disaster mental health response in an all-hazards context but include incidents that trigger CSC (and surge demand) for mental health resources.
o The plans should address the full continuum of those affected, from those with pre-existing mental illness, to those directly affected by the implementation of CSC and their families, to health care workers who must implement CSC, to the general public.
• Plans should address the anticipated consequences of CSC incidents through a gap analysis of the range of expected mental health impacts versus current resources. When informed by such an
analysis, triage decisions reflect a rational allocation of limited disaster mental health resources. During response, near-real-time awareness of needs and resources informs a floating triage algorithm of risk levels versus resources, guided by the ethical framework set forth in this report.
• Evidence-based interventions should be identified for the high-risk subset of providers; patients; and surviving family members, including children (e.g., trauma-focused cognitive-behavioral therapy for children, prolonged-exposure cognitive-behavioral therapy for adults, and other commonly employed techniques [IOM, 2007; Stokes and Jones, 1995]).
• Core competencies and training curricula should be developed for
o mental health, social services, and spiritual care staff;
o health care providers; and
o the public—basic strategies for community resilience that community members can use with friends and family (such as very basic psychological first aid, created specifically for these populations) (see also Chapter 9 on public engagement).
• Site, local/regional, and state-level incident command operations should be augmented to integrate mental health operations into emergency operations center operations. These efforts should encompass mental health needs assessment and operations for patients/disaster victims and responders (including health care workers and their families) to create user-defined situational awareness of acute mental health gaps, including
o a user-defined/common operating picture of the continuum of population-level mental health risks (traumatic loss, multiple traumatic losses);
o a user-defined/common operating picture of the continuum of mental health risks to health care workers; and
o a user-defined/common operating picture of mental health resources, including telephone, triage, and novel Internet-based interventions.
• Comprehensive resilience programs for health care workers/responders should be developed that integrate personal behavioral coping and agency preparedness. These programs should encompass preincident stress inoculation, development of personal resilience “plans,” simple peer-to-peer psychological first aid, self-triage, and linkage to Internet-based interventions for those at higher risk who desire further support.
For Patients and Their Families
In a mass casualty event involving high rates of illness, injury, and mortality, disaster mental health resources, like health care resources generally, are likely to experience significant surge demand. Although there may be considerable individual and community resilience, many others will be at risk for developing new-incidence comorbid disorders, such as posttraumatic stress disorder, depression, and substance abuse. Others with preexisting mental health disorders, including those that are severe and persistent, may experience relapse or worsening of illness episodes (NBSB, 2008). The phenomenon known as “traumatic grief” can result when
the death of a loved one occurs in a particularly traumatic context; CSC may be such a context for many and thus could lead to widespread traumatic grief (NCTSN, 2004). When adults or children develop symptoms of traumatic grief, they require specialized interventions, such as trauma-focused cognitive-behavioral therapy for children and prolonged-exposure cognitive-behavioral therapy for adults (IOM, 2007). While resilience is common after the loss of loved ones, rates of resilience may drop by as much as 50 percent when traumatic grief is present (Norris, 2005; Shear et al., 2005). Therefore, the capacity to provide evidence-based care for traumatic loss is a key requirement under CSC.
There is also growing evidence that certain evidence-based interventions, when provided early after a traumatic incident, may significantly reduce long-term mental health consequences (Bisson, 2008; Roberts et al., 2010; Shalev et al., 2012). However, early rapid triage is needed to allocate these resources to those at risk (Schreiber, 2005; Schreiber et al., in press). The ability to provide a continuum of evidence-based care, based on triage risk, is a hallmark of community resilience planning. Both specific coping information on traumatic grief (NCTSN, 2004) and additional coping information specific to expected reactions to CSC need to be developed. Potential risk factors include experiencing traumatic loss (including missing family members); seeing many dead or injured or hearing cries of pain; being trapped or unable to evacuate; and experiencing persistent stressors, such as ongoing injury or illness due to a disaster, home loss, and disasterinduced relocation.
Therefore, strategies employed at the population level should utilize evidence-based rapid triage to help identify those at greatest risk for more sustained and serious consequences and allocate limited mental health resources to those at the highest level of evidence-based risk for sustained disorder and impairment. One example is the PsySTART disaster mental health rapid triage system, currently used by the American Red Cross and the Minnesota Department of Health, and available to 83 Los Angeles–area hospitals and community clinic agencies in the Los Angeles County Emergency Medical Services Agency Hospital Preparedness Program. Although there are certainly challenges to implementing such strategies, the ability to align and allocate limited mental health resources is necessary to address the needs of those at higher risk for acute psychiatric emergencies and enduring psychological consequences. The Los Angeles EMS agency has operationalized this model in proposed modifications to the hospital incident command system and evaluated its use in a recent statewide disaster medical exercise, which revealed acceptable levels of mental health triage accuracy in a simulated countywide mass casualty incident (Schreiber et al., 2011). There are certainly daily challenges in accessing care for psychiatric emergencies. Within the CSC/disaster context, however, there are unique opportunities to advance surge management of risk and to improve population-level resilience by employing the combination of rapid disaster mental health triage (using a shifting or “floating” triage algorithm of dynamic alignment of resources with highest risk); “stepped” care case management (Zatzick et al., 2011), which involves maximizing population-level mental health impact or reach through timely triage-informed allocation of high-intensity treatment resources and increasing service intensity only after lower-intensity efforts are found insufficient; and evidence-based, nternet-based interventions (Ruggiero et al., 2011), which address surge demands and stigma through targeted modules for depression, posttraumatic stress, substance abuse, and anxiety.
For Health Care Providers
As noted above, responders and health care workers typically exhibit high levels of resilience following a disaster response. When CSC must be utilized, however, this may not be the case. A number of features of CSC—the potential for dramatically high mortality rates, including pediatric deaths; the stress of implementing and communicating about CSC with individual patients, their families, and others—pose severe mental health threats to health care workers. Available research suggests that many or most health care workers expect to face major barriers to their ability and/or willingness to perform hypothetical emergency health care roles (Chaffe, 2009; DiGiovanni et al., 2003; DiMaggio et al., 2005). In this regard, strategies needed for providers mirror those needed for patients—the use of rapid triage to identify those at highest risk and those with other concerns, and to align limited disaster mental health resources rationally and ethically to providers with the greatest needs.
A number of localities have developed pilot efforts to enhance resilience in disasters. Los Angeles County, one of several examples, has initiated a provider resilience project, called Anticipate, Plan and Deter, that leverages stress inoculation in the preparedness phase, including aspects of CSC, and self-triage/ monitoring in the response phase for the creation of a “personal resilience plan” for the health care workforce (Schreiber and Shields, 2011; Schreiber et al., in press).
Psychological first aid is another approach that can be used by mental health workers, health care providers, and patients and their families, as well as the general public. Currently, there are a number of different models for psychological first aid: one that is among the most comprehensive and intended for use by trained mental health care providers (NCTSN, 2006); another that is intended for use by community disaster responders with no mental health background (American Red Cross, 2006); and yet another, called Listen, Protect and Connect, designed specifically for the provision of basic psychological first aid and psychosocial support by all members of the community (Gurwitch and Schreiber, 2010). Listen, Protect, and Connect is a method for enhancing social support using three simple principles at the family, neighborhood, and community levels. It is intended as an achievable community resilience capability to strengthen social ties at the most basic levels of social connection. So-called “Mhealth” versions and provider versions for CSC are currently in development as part of the Los Angeles County Community Disaster Resilience Project. Aimed at the general community, Listen, Protect, and Connect has versions for children and parents and for teachers, as well as a “neighbor-to-neighbor, family-to-family” all-ages version. These versions were recently adapted for the Los Angeles County Department of Public Health and its community disaster preparedness partners, including the medical reserve corps, community health clinics, hospitals, public health workers, schools, and first responders.1
_________________
1 These versions are available without cost from http://www.cdms.uci.edu/protect.pdf.
ACEP (American College of Emergency Physicians). 2006. Disaster medical services. Irving, TX: ACEP, http://www.acep.org/Content.aspx?id=29176 (accessed March 4, 2012).
ACEP. 2008. Disaster planning and response. Irving, TX: ACEP, http://www.acep.org/Content.aspx?id=40342 (accessed March 4, 2012).
AHRQJAgency for Health Research and Quality). 2005. Altered standards of care in mass casualty events: Bioterrorism and other public health emergencies. Publication no. 05-0043. Rockville, MD: AHRQ.
AHRQ. 2007. Mass medical care with scarce resources: A community planning guide. Publication no. 07-0001. Rockville, MD: AHRQ, http://archive.ahrq.gov/research/mce/ (accessed February 28, 2012).
Aleccia, J. 2011 (March 17). Popping potassium iodide already? Really bad idea. http://www.msnbc.msn.com/id/42135438/ns/health-health_care/ (accessed March 4, 2012).
American Red Cross. 2006. Psychological First Aid: Helping Others in Times of Stress. DSCLS206A. Washington, DC: American Red Cross, http://www.cincinnatiredcross.org/pdf/Psychological%20First%20Aid%20Participant%20Workbook.pdf (accessed March 1, 2012).
Berry, P. H., and M. Matzo. 2004. Death and an aging society. In Gerontological palliative care nursing, edited by M. Matzo, and D. W. Sherman. St. Louis, MO: Mosby. Pp. 31-51.
Bisson, J. I. 2008. Using evidence to inform clinical practice shortly after traumatic events. Journal of Traumatic Stress 21(6):507-512.
Cantrill, S. V., P. T. Pons, C. J. Bonnett, S. Eisert, and S. Moore. 2009. Disaster alternate care facilities: Selection and operation. Prepared by Denver Health under Contract No. 290-20-0600-020. AHRQ Publication no. 09-0062. Rockville, MD: AHRQ.
CDC (Centers for Disease Control and Prevention). 2009. 2009 H1N1 vaccination recommendations. http://www.cdc.gov/h1n1flu/vaccination/acip.htm (accessed March 4, 2012).
Census Scope. Social science data analysis network. http://www.censusscope.org/us/chart_age.html (accessed February 25, 2011).
Chaffe, M. 2009. Willingness of health care personnel to work in a disaster: An integrative review of the literature. Disaster Medicine and Public Health Preparedness 3(1):42-56.
Christian, M. D., L. Hawryluck, R. S. Wax, T. Cook, N. M. Lazar, M. S. Herridge, M. P. Muller, D. R. Gowans, W. Fortier, and F. M. Burkle. 2006. Development of a triage protocol for critical care during an influenza pandemic. Canadian Medical Association Journal 175(11):1377-1381.
Cone, D. C., and D. S. MacMillian. 2005. Mass-casualty triage systems: A hint of science. Academic Emergency Medicine 12(8):739-741.
DeMartino, R. 2001 (unpublished). Planning for the unexpected: Behavioral health in a new era of bioterrorism [at the National Summit on Addressing Terrorism]. Rockville, MD: SAMHSA (Department of Health and Human Services, Substance Abuse and Mental Health Agency).
Devereaux, A. V., J. R. Dichter, M. D. Christian, N. N. Dubler, C. E. Sandrock, J. L. Hick, T. Powell, J. A. Geiling, D. E. Amundson, T. E. Baudendistel, D. A. Braner, M. A. Klein, K. A. Berkowitz, J. R. Curtis, and L. Rubinson. 2008. Definitive care for the critically ill during a disaster: A framework for allocation of scarce resources in mass critical care. From a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest 133(Suppl. 5):S51-S66.
DiGiovanni, C., Jr. 2003. The spectrum of human reactions to terrorist attacks with weapons of mass destruction: Early management considerations. Prehospital and Disaster Medicine 18(3):253-257.
DiMaggio, C., D. Markenson, G. Loo, and I. Redlener. 2005. The willingness of U.S. emergency medical technicians to respond to terrorist incidents. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 3(4):331-337.
Domres, B., A. Manger, I. Steigerwald, and S. Esser. 2003. The challenge of crisis, disaster, and war: Experience with UN and NGOs. Pain Practice 3(1):97-100.
Eisenman, D. P., C. Wold, J. Fielding, A. Long, C. Setodji, S. Hickey, and L. Gelberg. 2006. Differences in individual-level preparedness in Los Angeles County. American Journal of Preventative Medicine 30(1):1-6.
Fink, S. 2009. Deadly choices at memorial. NY Times Magazine, August 27.
Galea, S., and H. Resnick. 2005. Posttraumatic stress disorder in the general population after mass terrorist incidents: Considerations about the nature of exposure. CNS Spectrums 10(2):107-115.
Garrett, J. E., D. E. Vawter, K. G. Gervais, A. W. Prehn, D. A. DeBruin, F. Livingston, A. M. Morley, L. Liaschenko, and R. Lynfield. 2011. The Minnesota Pandemic Ethics Project: Sequenced, robust public engagement processes. Journal of Participatory Medicine 3, http://www.jopm.org/evidence/research/2011/01/19/the-minnesota-pandemic-ethics-project-sequenced-robust-public-engagement-processes/ (accessed January 18, 2012).
Geller, J. L., and K. Biebel. 2006. The premature demise of public child and adolescent inpatient psychiatric beds. Psychiatric Quarterly 77:251-271.
Glass and Schoch-Spana. 2002. Bioterrorism and the people: How to vaccinate a city against panic. Clinical Infectious Diseases 34(2):217-23.
Gostin, L. O. 2006. Public health strategies for pandemic influenza. Journal of the American Medical Association 295(14):1700-1704.
Gursky, E., T. V. Inglesby, T. O’Toole. 2003. Anthrax 2001: Observations on the medical and public health response. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 1(2):97-110.
Gurwitch, R., and M. Schreiber. 2010. Coping with disaster, terrorism and other trauma. In The parent’s guide to psychological first aid, edited by G. Koocher and A. LaGreca. Boston, MA: Oxford University Press. Pp. 342-351.
Hawryluck, L., W. Gold, S. Robinson, S. Pogorski, S. Galea, and R. Strya. 2004. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases 10(7):1208-1212.
HHS (Department of Health and Human Services). 2011. Guidance for integrating culturally diverse communities into planning for and responding to emergencies: A toolkit. Washington, DC: HHS Office of Minority Health, http://www.hhs.gov/ocr/civilrights/resources/specialtopics/emergencypre/omh_diversitytoolkit.pdf (accessed January 11, 2012).
HHS. 2012. At-risk individuals. Washington, DC: HHS, http://www.phe.gov/Preparedness/planning/abc/Documents/at-risk-individuals.pdf (accessed February 13, 2012).
Hippen, B., R. Thistlethwaite, and L. Ross. 2011. Risk, prognosis, and unintended consequences in kidney allocation. New England Journal Medicine 364(14):1285-1287.
Holt, G. R. 2008. Making difficult ethical decisions in patient care during natural disasters and other mass casualty events. Otolaryngology—Head & Neck Surgery 139(2):181-186.
IOM (Institute of Medicine). 2007. Treatment of PTSD: An Assessment of The Evidence. Washington, DC: The National Academies Press.
IOM. 2009. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press, http://www.nap.edu/catalog.php?record_id=12749 (accessed September 6, 2011).
IOM. 2010. Preventing transmission of pandemic influenza and other viral respiratory diseases: Personal protective equipment for healthcare personnel update 2010. Washington, DC: The National Academies Press.
Iserson, K.V., and N. Pesik. 2003. Ethical resource distribution after biological, chemical, or radiological terrorism. Cambridge Quarterly of Healthcare Ethics 12(4):455-465.
Janousek, J. T., D. E. Jackson, R. A. DeLorenzo, and M. Coppola. 1999. Mass casualty triage knowledge of military medical personnel. Military Medicine 164(5):332-336.
Levin, D., R. O. Cadigan, P. D. Biddinger, S. Condon, H. K. Koh; Joint Massachusetts Department of Public Health-Harvard Altered Standards of Care Working Group. 2009. Altered standards of care in an influenza pandemic: Identifying ethical, legal and practical principles to guide decision-making. Disaster Medicine and Public Health Preparedness 3(Suppl. 2):1-9.
Lin, C. Y., Y. C. Peng, Y. H. Wu, J. Chang, C. H. Chan, and D. Y. Yang. 2007. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerging Medicine Journal 24(1):12-7.
Louisiana Department of Health and Hospitals. 2011. Crisis standards of care summary. Baton Rounge, LA: Louisiana Department of Health and Hospitals, http://new.dhh.louisiana.gov/assets/oph/Center-PHCH/Center-CH/infectious-epi/Influenza7CSOCPublicFLYERvs210132011.pdf (accessed February 5, 2012).
Matzo, M. L. 2004. Palliative care: Prognostication and the chronically ill. American Journal of Nursing 104(9):40-50.
Matzo, M., A. Wilkinson, J. Lynn, M. Gatto, and S. J. Phillips. 2009. Palliative care considerations for mass casualty events with scarce resources. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 7(2):199-210.
National Center for Disaster Preparedness. 2005. Survey of Confidence in Government’s Abilities in Face of Hurricanes, Pandemic Flu, and Threats of Terrorism. New York: Columbia University Mailman School of Public Health, http://www.ncdp.mailman.columbia.edu/files/Marist%20Survey%202005%20press%20release%20final.pdf (accessed February 28, 2012).
NBSB (National Biodefense Science Board). 2008. Disaster mental health recommendations: report of the disaster mental health subcommittee of the National Biodefense Science Board. Washington, DC: NBSB, http://www.phe.gov/Preparedness/legal/boards/nbsb/Documents/nsbs-dmhreport-final.pdf (accessed February 28, 2012).
NCTSN (National Child Traumatic Stress Network). 2004. What is childhood traumatic grief. Los Angeles, CA: NCTSN, http://www.nctsn.org/trauma-types/traumatic-grief/what-childhood-traumatic-grief (accessed January 18, 2012).
NCTSN. 2006. Psychological First Aid: field operations guide 2nd edition. Los Angeles, CA: NCTSN, http://www.nctsn.org/sites/default/files/pfa/english/2-psyfirstaid_final_no_handouts.pdf (accessed March 4, 2012).
Norris, F. H. 2005. Range, multitude, and duration of the effects of disasters on mental health: Review update, 2005. Hanover, NH: Dartmouth College and the National Center for PTSD.
Organ Procurement and Transplantation Network. 2011. Concepts for kidney allocation. http://optn.transplant.hrsa.gov/SharedContentDocuments/KidneyConceptDocument.pdf (accessed March 4, 2012).
Orr, R. D. 2003. Ethical issues in bioterrorism. Bioterrorism email module #12. Burlington, VT: Fletcher Allen Health Care in conjunction with the University of Vermont College of Medicine.
Pandemic Influenza Ethics Initiative Workgroup of the Department of Veterans Affairs. 2009 (April). Meeting the Challenge of Pandemic Influenza: Ethical Guidance for Leaders and Health Care Professionals in the Veterans Health Administration. Washington, DC: VA (Department of Veterans Affairs), http://www.ethics.va.gov/docs/pandemicflu/Meeting_the_Challenge_of_Pan_Flu-Ethical_Guidance_VHA_20100701.pdf (accessed March 4, 2012).
Pediatric Emergency Mass Critical Care Task Force. 2012. Ethical issues in pediatric emergency mass critical care. Pediatric Critical Care Medicine.
Persad, G., A. Wertheimer, and E. Emanuel. 2009. Principles for allocation of scarce medical interventions. Lancet373:423-431.
Peterson, M. 2008. The moral importance of selecting people randomly. Bioethics 22(6):321-327.
Public Health-Seattle and King County. 2009. Public engagement project on medical service prioritization during an influenza pandemic: Health care decisions in disasters, September 2009. http://s3.amazonaws.com/propublica/assets/docs/seattle_public_engagement_project_final_sept2009.pdf (accessed March 4, 2012).
Pynoos, R., M. Schreiber, A. Steinberg, and B. Pfefferbaum. 2004. Impact of Terrorism on Children. In Kaplan and Sadock’s Comprehensive Textbook of Psychiatry, 8th ed., edited by B. Sadock and V. Sadock. Philadelphia, PA: Lippincott, Williams and Witkins. Pp. 3551-3564.
Rebmann, T., R. Wilson, S. LaPointe, B. Russell, and D. Moroz. 2009. Hospital infectious disease emergency preparedness: A 2007 survey of infection control professionals. American Journal of Infection Control 37(1):1-8.
Roberts, N. P., N. J. Kitchiner, J. Kenardy, and J. I. Bisson. 2010. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews 17(3):CD007944.
Ruggiero, K. J., H. S. Resnick, L. A. Paul, K. Gros, J. L. McCauley, R. Acierno, M. Morgan, and S. Galea. 2011. Randomized controlled trial of an internet-based intervention using random-digit-dial recruitment: The Disaster Recovery Web project. Contemporary Clinical Trials 33(1):237-246.
Sacco, W. J., M. Navin, K. E. Fiedler, and R. K. Waddell. 2005. Precise formulation and evidence-based application of resource-constrained triage. Academic Emergency Medicine 12(8):759-771.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2007. Prolonged Exposure Therapy for Posttraumatic Stress Disorders. Rockville, MD: HHS (Department of Health and Human Services), http://nrepp.samhsa.gov/ViewIntervention.aspx?id=89 (accessed March 1, 2012).
Schreiber, M. 2005. Learning from 9/11: Toward a national model for children and families in mass casualty. In On the ground after 9/11: Mental health responses and practical knowledge gained, edited by Y. Daneili. New York: Haworth. Pp. 605-609.
Schreiber, M., and S. Shields. 2012. Anticipate, Plan, and Deter: Building resilience in emergency health responders. Presented at the 2012 NACCHO (National Association of City and County Health Officials) Public Health Preparedness Summit, Anaheim, California.
Schreiber, M., K. Koenig, C. Schultz, S. Shields, and D. Bradley. 2011. PsySTART Rapid Disaster Mental Health Triage System: Performance During a Full Scale Exercise. Academic Emergency Medicine 18(5):s59 (supplement).
Schreiber, M., B. Pfefferbaum, L. Sayegh, and J. Coady. In press. The way forward: The national children’s disaster mental health concept of operations. Disaster Medicine and Public Health.
Schumacher Group. 2010. Emergency department challenges and trends: 2010 survey of hospital emergency department administrators. Lafayette, LA: Schumacher Group, http://schumachergroup.com/_uploads/news/pdfs/ED%20Challenges%20and%20Trends%2012.14.10.pdf (accessed March 4, 2012).
Shah, U. 2012 (January 13). Summary of HCPHES pandemic influenza public and partner engagement projects. Harris County, TX: Harris County Public Health and Environmental Services.
Shalev, A. Y., Y. Ankri, Y. Israeli-Shalev, T. Peleg, R. Adessky, and S. Freedman. 2012. Prevention of posttraumatic stress disorder by early treatment: Results from the Jerusalem trauma outreach and prevention study. Archives of General Psychiatry 69(2):166-76.
Shear, K., E. Frank, P. R. Houck, and C. F. Reynolds. 2005. Treatment of complicated grief: A randomized controlled trial. Journal of the American Medical Association 293(21):2601-2608.
Society of Critical Care Medicine Ethics Committee. 1994. Consensus statement on the triage of critically ill patients. Journal of the American Medical Association 271(15):1200-1203.
Stokes, J., and F. D. Jones. 1995. Combat stress control in joint operations in War Psychiatry. Alexandria, VA: Department of the Army.
Wilkinson, A., M. Matzo. M. Gatto, and J. Lynn. 2007. Chapter VII: Palliative care. In Mass medical care with scarce resources: A community planning guide. Publication no. 07-0001. Rockville, MD: AHRQ, http://archive.ahrq.gov/research/mce/ (accessed February 28, 2012). Pp. 101-116.
Williams, A. 1997. Intergenerational equity: An exploration of the “fair innings” argument. Health Economics 6(2):117-132.
Zatzick, D., F. Rivara, G. Jurkovich, J. Russo, S. G. Trusz, J. Wang, A. Wagner, K. Stephens, C. Dunn, E. Uehara, M. Petrie, C. Engel, D. Davydow, and W. Katon. 2011. Enhancing the population impact of collaborative care interventions: Mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. General Hospital Psychiatry 33(2):123-134.