Health Care: Quality, Access, and Value
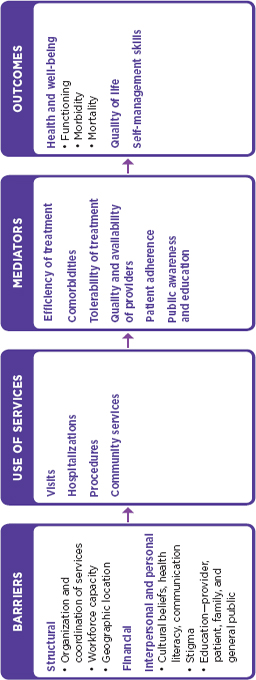
While significant progress has been made in developing seizure medications with fewer adverse effects, as well as in refining medical devices and surgical techniques for select types of epilepsy, much remains to be done to reduce the sometimes lengthy delays in diagnosis and referral to more advanced levels of care, to improve access to care for underserved and rural patients, to improve co-management of patients between primary care and specialty providers, and to improve care for those with refractory epilepsy. Efforts are ongoing to improve the quality of epilepsy care through the development and implementation of physician performance measures and other performance metrics. Involvement of epilepsy centers is critical to providing specialized care. Clarifying the role of primary care providers in epilepsy care is also crucial as is delineating clinical pathways and decision points for referrals. A patient-centered approach to health care is needed with an emphasis on the coordination of epilepsy-specific services with care for comorbidities and with links to community services. Actions needed to ensure that health care for people with epilepsy is evidence based, population based, and patient centered include accrediting epilepsy centers and establishing a network of centers, developing and implementing a quality care framework and performance measures, and enhancing the screening and referral options and protocols for early identification of epilepsy in high-risk populations, of comorbidities, and of refractory epilepsy.
My daughter (now 16) started having seizures when she was 9. Her first seizure was big and we thought she was dying … maybe she was having
a brain hemorrhage … we couldn’t figure it out. It was terrifying…. We were very blessed to meet a good neurologist from the start. He was rare—a small town doctor with the big town connections…. He encouraged us to get a second opinion and was extremely accessible to us. He had personal experience with epilepsy in his family, a real plus. In my volunteering with the Epilepsy Foundation of Virginia, I have encountered many people whose neurologists did not refer them to an epileptologist or a neurologist with a special interest in epilepsy.
-Laurie Kelly
Like other rural-frontier populations, Wyoming’s citizens continually face problems in accessing quality health care and health education. Health care accessibility is particularly problematic in Wyoming, where distance, geography, inclement weather, and isolated communities all present challenges for the state’s residents in gaining education and access to health care.
-Richard Leslie
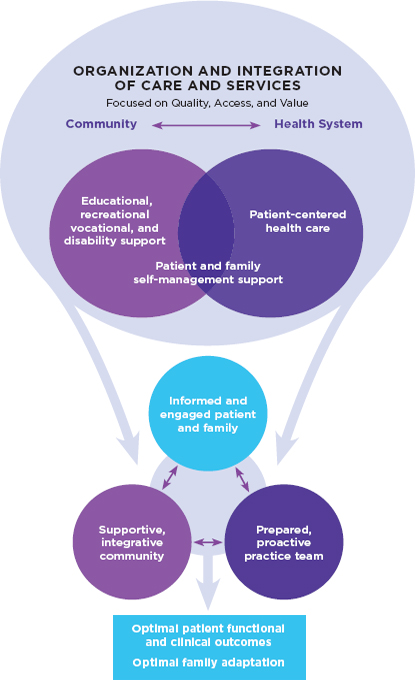
Improving the lives of people with epilepsy and their families involves sustained and coordinated efforts, ranging from increasing the understanding of the biomedical mechanisms of the disorder to enhancing clinical treatment and community services. Because epilepsy is a common neurological disorder that can have many physical, psychological, cognitive, and social manifestations, quality care may require the knowledge and skills of a wide range of health and community service professionals and necessitate that people with epilepsy, family members, and caregivers are knowledgeable about the disorder, can recognize potential danger signs, and are skilled in self-management as appropriate.
The committee’s vision for improving health care for people with epilepsy is that all individuals with epilepsy should have access to patient-centered care that incorporates a comprehensive and coordinated approach to addressing the physiological, psychological, cognitive, and social dimensions relevant for each person and his or her family. This care is best delivered by a coordinated team of professionals that can assess and treat all facets of the patient’s condition and comorbidities and can integrate appropriate community services.
As highlighted in the Institute of Medicine (IOM) report Crossing the Quality Chasm, “Health care should be:
• Safe—avoiding injuries to patients from the care that is intended to help them
• Effective—providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse, respectively)
• Patient-centered—providing care that is respectful of and respon-
sive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions
• Timely—reducing waits and sometimes harmful delays for both those who receive and those who give care
• Efficient—avoiding waste, including waste of equipment, supplies, ideas, and energy, and
• Equitable—providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status” (IOM, 2001, pp. 5-6).
This chapter begins with an overview of epilepsy care (patterns of care, diagnosis, and treatment), followed by a discussion of the key components of improving care—quality, access, and value; it concludes with the committee’s model of patient-centered, collaborative, and high-quality epilepsy care. A comprehensive and coordinated approach to health and human services is explored in this and subsequent chapters.
Patterns of Care
As noted in Chapter 1, when someone first has a seizure the initial medical visit is generally to the emergency department or primary care provider.1 Some health systems have first seizure clinics that explore potential diagnoses (Hamiwka et al., 2007), or patients may be referred to a general neurologist or an epileptologist, particularly if seizures recur frequently; however, little is known about referral patterns other than that there is tremendous variability. The likelihood of a referral may vary according to the seriousness of the patient’s condition, including the presence of comorbidities; the patient’s age; demographic and social factors; the preferences of the patient, family, and health professionals involved; and availability of specialized health professionals. A community-based survey of people with epilepsy explored views and experiences of epilepsy care and found that primary care providers were the first health professionals consulted by 58 percent of respondents (Fisher et al., 2000b). During the course of their disorder, almost all (94 percent) had consulted a neurologist at some point, with 62 percent having a neurologist as their primary physician for epilepsy care at the time of the survey. Respondents were more likely to have consulted a neurologist if they had been diagnosed within the previous
_______________
1 Throughout the report, the term “primary care provider” is used to encompass many health professionals, including family physicians, general internists, general pediatricians, obstetrician-gynecologists, geriatricians, physician assistants, and nurse practitioners.
year, had a seizure in the previous month, were diagnosed before age 12, or had multiple seizure types.
To obtain more information on patterns of epilepsy care, four different health care and surveillance systems (Geisinger Health System, Henry Ford Health System, South Carolina Epilepsy Surveillance System, and the Veterans Health Administration) agreed to assist the committee by querying their databases on health care utilization patterns of people with epilepsy. The data provided by these systems (Appendix B) highlight the variability in patterns of care, but they also reveal three common initial points of care where people are first evaluated: (1) in the hospital emergency department, (2) with a referral to a neurologist, or (3) during a regular visit with a primary care provider. Across the four systems, from 32 to 71 percent of patients’ first encounters were with neurologists. Evidence from several of these systems suggests that people with new-onset epilepsy use more health services than people with prevalent epilepsy. However, the types of services received during the initial year after diagnosis, such as the number of physician visits or diagnostic procedures performed, varied widely across systems. Evidence from some of the health systems seems to confirm that care of individuals with ongoing epilepsy (prevalent epilepsy) tends to stabilize over time, but again, the patterns varied among systems and also among subgroups within each system. For example, over the course of a year, 14 to 48 percent of epilepsy patients were treated in emergency departments, 8 to 55 percent were hospitalized, 21 to 75 percent had a neurologist visit, and 68 to 100 percent received seizure medications. The range in percentages of patients receiving seizure medications was more consistent across sites, ranging from 70 to 80 percent. More needs to be learned about these patterns of care and the extent to which variations in care affect patient outcomes.
Information about patterns of care from non-neurologist health professionals could not be obtained. Although nurses, social workers, psychologists, psychiatrists, and vocational specialists are all described as important members of an interdisciplinary epilepsy care team (Labiner et al., 2010), whether and when patients or families are seen by these professionals varies between health systems. A clearer understanding of how multidisciplinary teams are best implemented and of the individual roles of health professionals in the care trajectory is needed to identify best practices and improve quality of care.
Diagnosis of the Epilepsies
Accurately diagnosing epilepsy is challenging because clinicians rarely have the opportunity to observe seizures and there are many types of seizures and epilepsy syndromes with differing presentations. A clinician
typically diagnoses epilepsy based on the patient’s self-report or a family member’s report of seizures and the patient’s medical history. This is complicated by the fact that a number of medical conditions that are not epilepsy can look like seizures (Chapter 1). Diagnostic tests can provide relevant information, usually starting with the electroencephalogram (EEG) (Table 4-1). However, because the typical duration of an EEG is only 20 to 45 minutes, it is unlikely to coincide with an actual seizure. Further, the initial EEG may not show evidence of seizures in approximately half of people with epilepsy (Marsan and Zivin, 1970; Salinsky et al., 1987). Continuous video-EEG monitoring, which can last from hours to days and is usually conducted in a hospital setting, is often the only way to definitively diagnose the type of seizure and affected areas of the brain.
TABLE 4-1
Diagnostic Studies Used in Evaluating and Treating People with Epilepsy
| Diagnostic Tests | Description | Indication |
| Electroencephalograph (EEG) | Measures electrical activity in the brain | Useful for any individual with suspected seizures |
| Continuous video-EEG monitoring | Combines long-term EEG recording with video recording of an individual′s behavior | Useful in determining seizure type; essential for patients undergoing a surgical evaluation for epilepsy |
| Magnetic resonance imaging (MRI) | Uses magnetic felds to detect structural abnormalities in the brain | Useful for imaging the brain for lesions such as tumors and scar tissue |
| Computerized tomography (CT) | Uses radiation to detect structural abnormalities in the brain | Useful for detecting structural abnormalities such as tumors as well as hemorrhages |
| Magnetoencephalography (MEG) | Uses magnetic signals to detect abnormalities in the brain′s electrical activity | Useful primarily for patients undergoing surgical evaluation |
| Positron emission tomography (PET) or single positron emission tomography (SPECT) | Uses radioactive tracers to assess glucose metabolism or blood flow in the brain | Useful in determining the area of the brain where seizures arise since these areas typically have decreased glucose metabolism and blood flow in between seizures |
| Genetic or metabolic testing | Uses blood, urine, and spinal fluid tests to determine if there is a genetic cause of the epilepsy | Useful for diagnosing epilepsy-related genetic or metabolic disorders. Although many tests are available, there is not yet a standard screen |
SOURCES: Chandra et al., 2006; Engel, 1984; Erbayat Altay et al., 2005; Knake et al., 2006; McNally et al., 2005; Provenzale, 2010; Stockler-Ipsiroglu and Plecko, 2009; Thadani et al., 2000; Wheless et al., 2004.
Advances in technology permit family members and other caregivers to record seizures as they occur. Kotani and colleagues (2007) described a case study where the mother of a teenager with epilepsy was able to capture his seizure on a cell phone camera, which a doctor had not been able to diagnose due to seizure infrequency. Similarly, the improved visualization of seizures through digital cameras with video capabilities and video monitoring in home settings may be particularly beneficial for individuals with infrequent seizures or with more than one type of seizure and for those who do not have easy access to epileptologists and epilepsy monitoring units. Also, the recording of seizures using web-based tracking systems, diaries, or journals can help people with epilepsy and their families maintain records of seizure activity and evaluate patterns with their health care provider (Le et al., 2011). The observation of seizure patterns can help identify a target for medication and lifestyle interventions to improve seizure management.
Treatment of the Epilepsies
For many people with epilepsy, current treatment options are effective in reducing or eliminating seizures. However, medication side effects are a concern, and approximately one-third of people with epilepsy do not respond to medications (Kwan and Brodie, 2000). This report provides only a brief overview of the treatments for epilepsy and its comorbidities, which need to be tailored to the unique diagnostic and treatment considerations of specific individuals and also of specific populations, some of which are highlighted in Table 4-2.
Seizure Medications
The primary method of treatment for the epilepsies is medication aimed at controlling seizure recurrence, typically by decreasing brain excitation or increasing brain inhibition. In a population-based survey, Kobau and colleagues (2008) found that among adults reporting they have active epilepsy, 93 percent were currently taking a medication, and 55 percent had no seizures in the previous 3 months (Table 4-3).
The first medication to be used in the treatment of epilepsy in the 1800s was potassium bromide; more than 35 seizure medications have been introduced since then (Figure 4-1) (Loscher and Schmidt, 2011). Initially medications were developed that blocked sodium channels in neurons, resulting in reduced brain excitation or increasing inhibition of neurons through activation of inhibitory receptors (Brodie, 2010; Rogawski and Loscher, 2004). In the past 20 years, a better understanding of the pathophysiology of the epilepsies and epileptogenesis (the process by which epi-
TABLE 4-2
Diagnostic and Treatment Considerations for Specific Populations
| Population | Diagnostic and Treatment Considerations |
| Children |
• Diagnostic challenges of age-related clinical and electroencephalograph features of seizures • Different side effects and dosing schedules for medications • Identifying seizure medication formulations determined to be appropriate for children • Potential lifelong cognitive and disabling effects of seizures suffered during childhood • Helping children begin to take responsibility for self-management • Education of school personnel in recognition and treatment of seizures |
| Youth |
• Impact of hormonal changes on seizures, side effects of medications, drug interactions, and comorbidities • Increased responsibilities for self-management • Impact of seizures, treatment, and comorbidities on educational and vocational planning and on driving and transportation |
| Older adults |
• Potential for drug interactions with medications for other health conditions • Possible cognitive side effects of some medications • Increased potential for injury • Self management may be in jeopardy, depending on cognitive functioning caregiver assistance may be needed |
| Women |
• Susceptibility to changes in seizures during menstrual cycle or at other times of hormonal fluctuations (e.g., menopause) • Potential impact of seizures and/or medications on reproductive functioning, pregnancy, breastfeeding • Risk for malformations and impaired cognitive development of offspring of women taking seizure medications or suffering seizures during pregnancy |
| Individuals with intellectual disabilities |
• Communication difficulties may hamper diagnosis and ability to delineate the seizure type • Assessing drug toxicity or treatment side effects in patients with severe intellectual disabilities may be challenging • High risk of injury from seizures and side effects of medications • High rate of psychiatric comorbidities |
| Underserved populations |
• Reduced treatment options relative to access to health services • Medication adherence • Other access and health literacy issues, including language barriers and the need, in some cases, for medical interpreters • High rates of comorbidities |
| People with traumatic brain injury |
• Seizures associated with brain injury may be missed or misdiagnosed as mental health conditions or other physical problems • Seizure medications must be selected carefully to avoid exacerbating other problems of traumatic brain injury |
| Oncology patients |
• Interactions of seizure medications with chemotherapeutic drugs that may decrease concentrations of chemotherapeutic agents in the body |
TABLE 4-3
Adults with a History of Epilepsy, Behavioral Risk Factor Surveillance System, 2005
| Total with History of Epilepsy (n = 1,626) | Active Epilepsya (n =< 919) | |
| Currently taking medication to control seizure disorder or epilepsy | ||
| Yes | 48.8 (44.1-53.6) | 93.1 (90.3-95.1) |
| No | 51.2 (46.4-55.9) | 6.9 (4.9-9.7) |
| Number of seizures in previous 3 months | ||
| None | 71.0 (66.5-75.2) | 55.1 (48.6-61.5) |
| One | 8.1 (5.8-11.1) | 15.3 (11.1-20.7) |
| More than one | 15.0 (11.9-18.9) | 28.6 (23.0-34.9) |
| No longer have | 5.9 (4.0-8.6) | 1.0 (0.3-2.8)b |
a Defined as having been told by a doctor they had a seizure disorder or epilepsy and also responded that they were currently taking medication for epilepsy, had 1 or more seizures in the previous 3 months, or both.
b Respondents who reported taking medication for epilepsy.
SOURCE: Kobau et al., 2008.
lepsy develops), as well as the development of animal models that mimic clinically relevant forms of the disorder, have resulted in medications with other specific mechanisms of action that achieve the same effect but with fewer side effects. These mechanisms include targeting calcium and potassium channels and the synaptic release and uptake of neurotransmitters (Brodie, 2010; Loscher and Schmidt, 2011; Rogawski and Loscher, 2004). Seizure medications can be categorized into those used to stop seizures and those used to prevent them. Drugs used to stop seizures are typically given intravenously, rectally, intranasally, or buccally. For example, status epilepticus is treated with intravenous lorazepam, diazepam, phenobarbital, or phenytoin (Abend et al., 2010). Rectal diazepam is often used in children as an outpatient rescue medication to stop seizures (Poukas et al., 2011). The vast majority of seizure medications are used in chronic therapy and taken daily. Chronic seizure medications are either broad-spectrum drugs that are effective in treating a variety of different seizure types or narrow-spectrum drugs that are primarily effective for specific seizure types (e.g., absence, myoclonic, tonic-clonic).
Despite the large number of available drugs for epilepsy, patients remain concerned about the effectiveness of medications in controlling seizures, side effects (e.g., headache, fatigue, cognitive impairment), being able to establish an appropriate dosing schedule, and the high cost of some medications (Fisher et al., 2000b). In a community-based survey, approximately one-third of people with epilepsy reported that they were not
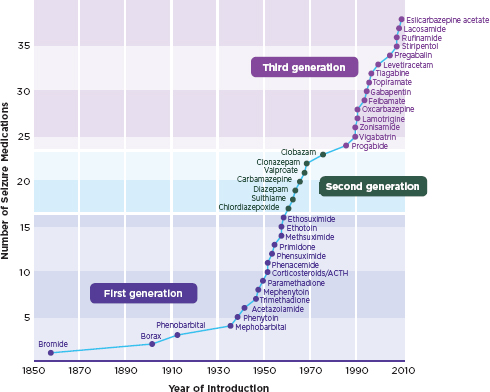
FIGURE 4-1
Seizure medications.
NOTE: Some medications are not available in the United States.
SOURCE: Loscher and Schmidt, 2011. Reprinted with permission from John Wiley and Sons.
fully satisfied with their current seizure medication(s) and noted a range of problems including issues with cognition, energy level, and sexual function (Fisher et al., 2000b).
For people whose seizures do not respond to medications, surgery or medical devices are potential treatment options. However, not all types of epilepsy are amenable to surgery. Today, surgically remediable epilepsy syndromes are easier to recognize than they were previously, largely because of improvements in magnetic resonance imaging (MRI) and other imaging technologies, which allow noninvasive identification of areas in the brain with abnormal neural function. Unfortunately, the length of time from seizure onset to surgery remains quite long, averaging 17 to 23 years (Choi et al., 2009; Cohen-Gadol et al., 2006; Haneef et al., 2010) (see later discussion of access).
A randomized controlled study found that 58 percent of people with mesial temporal lobe epilepsy who received epilepsy surgery were free
of disabling seizures by the end of the first year, compared to 8 percent among those who continued with medical therapy for 1 year (Wiebe et al., 2001). Long-term outcomes also are promising. De Tisi and colleagues (2011) found that 52 percent of adults who had undergone epilepsy surgery remained seizure-free (excluding simple partial seizures) 5 years after surgery and 47 percent were seizure-free after 10 years. Promising new, less invasive types of surgery for epilepsy are being evaluated (Chang and Huang, 2011).
An evidence review that was conducted to develop practice parameters for epilepsy surgery found that surgery’s benefits outweighed the benefits of continued medical therapy in people with mesial temporal lobe epilepsy, while not posing greater risk, and recommended consideration of referral to an epilepsy surgery center for individuals with refractory seizures (Engel et al., 2003). The biological, psychological, and social consequences of uncontrolled seizures have been well documented, but the timing of when these problems develop varies, complicating decisions regarding the timing of surgery. For many people, cognitive and behavioral problems are found early in the course of their epilepsy, and questions may arise as to whether surgery could prevent these problems from becoming disabling. Variability among epilepsy types and syndromes also complicates the question about when or if to consider surgery. This complexity is particularly true for children, some of whom stop having seizures when they get older (Berg et al., 2006; Langfitt and Wiebe, 2008). Further study is needed to assess the most beneficial timing of surgery, as well as its long-term results, impact on quality of life, and effectiveness compared to other forms of treatment.
Devices implanted to electrically stimulate the vagus nerve have been found to reduce or eliminate seizures in some individuals (DeGiorgio et al., 2000, 2001, 2005; Elliott et al., 2011; Handforth et al., 1998; Uthman et al., 2004). Studies of vagus nerve stimulation in adults showed a mean seizure reduction of 49 to 64 percent 2 years after implantation, with the number of seizures at least halved for 43 to 75 percent of patients (Rossignol et al., 2009). This technique also was shown to be cost-effective within 1.5 years of implantation (Helmers et al., 2011). Results among children with epilepsy have been variable (Englot et al., 2011; Rossignol et al., 2009); however, vagus nerve stimulation appears particularly effective for those with Lennox-Gastaut syndrome (Englot et al., 2011; Frost et al., 2001; Rossignol et al., 2009). Other forms of brain stimulation being tested include deep brain stimulation and focal responsive brain stimulation (Morrell, 2011). At present, these invasive therapeutic approaches are reserved for patients who are not good candidates for surgery.
Additional Treatments
Several additional types of treatments have been found to be helpful for controlling seizures, teaching people how to manage their epilepsy, and improving quality of life. Some of these therapies, such as behavioral therapy, are used as complements to medical treatment, while some—such as dietary therapy—may be used as a form of medical therapy. Further efforts are needed to study the effectiveness of some of these therapies.
Dietary therapy is a treatment modality often tried for children with epilepsy. The observation that individuals with epilepsy have fewer seizures during fasting led to diets that reduce carbohydrate ingestion and induce ketosis (Wheless, 2008). Several small studies have shown reductions in seizures for people with epilepsy who adhere to the ketogenic diet, medium-chain triglyceride diet, modified Atkins diet, or low-glycemic-index diet (Kossoff et al., 2009; Payne et al., 2011); however, more research is needed in larger populations. Further, dietary therapy is rigorous, requiring daily adherence to a strict schedule, which can be a challenge for both the individual with epilepsy and his or her family (Kossoff et al., 2009). Many physicians are reluctant to recommend dietary therapy because of the difficulty of adherence and the need for close monitoring by a dietician and clinician.
Certain types of behavioral therapy can be considered a form of self-management2 (the strategies people use to manage their epilepsy and its effects on their daily life). A behavioral therapy is usually intended to change unhealthy behavior and promote positive or healthy behavior. Many of these strategies overlap with educational efforts for patients and families (Chapter 7). For example, trigger management involves teaching people how to recognize or identify possible seizure triggers by observing environmental, personal, or lifestyle factors (such as lack of sleep, flashing lights, fever, or excessive alcohol consumption) that appear to increase their susceptibility to seizures. For many people, seizure control can improve if they avoid these triggers. Teaching about trigger management and lifestyle modifications is a frequent component of epilepsy care provided by nurses and social workers (Legion, 1991; Shafer, 1994).
Other behavioral approaches include seizure control using relaxation, yoga, biofeedback, and counseling; self-control approaches or acceptance and commitment therapy using individual and group sessions; and mind-body techniques (Andrews and Schonfeld, 1992; Lundgren et al., 2006, 2008a,b; Snead et al., 2004; Wagner et al., 2010). Relaxation treatment studies, while limited in number, generally show positive results in reducing seizures and improving quality of life (Dahl et al., 1987; Puskarich et al.,
_______________
2As noted in Chapter 1, the committee adopted the concept of “optimal self-management,” recognizing that it represents a wide range of possibilities and that what is optimal for one person may be beyond the capacity of another.
1992; Rousseau et al., 1985). All such approaches need rigorous review. Other behavioral treatments frequently taught to people with epilepsy and their families focus on knowledge about safety and adapting behavior to prevent injuries (Shafer, 1998). These techniques are generally incorporated into educational programs or cognitive-behavioral techniques for epilepsy self-management.
IMPROVING QUALITY OF HEALTH CARE
I wish we had more information about our daughter’s seizures. We worry that the staring spells are interfering with her ability to learn, but since we cannot see them on the EEG we don’t know for sure how to treat them. It is very worrisome to make decisions without more information. We hope that increased research in the field of epilepsy might provide more information into seizure activity and treatment for people like our little daughter.
-Jon VanWagoner
You would think finally armed with a correct diagnosis, things would get easier. We were educated advocates with resources and FedExed Mark’s MRI and reports to the top international pediatric neurosurgeons and centers worldwide. The diversity of recommendations returned was overwhelming.
-Ilene Miller
Quality has been defined by the IOM as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (IOM, 1990, p. 21). Priority areas identified by the committee for improving quality of health services for the epilepsies include the following:
• Improve the early identification of epilepsy and comorbid conditions.
• Improve treatments.
• Improve communications between the care team and patients.
• Develop a national quality framework for epilepsy care, which involves improving and implementing practice guidelines and developing, implementing, and assessing performance metrics to enhance the quality of epilepsy care.
• Evaluate and accredit epilepsy centers.
This section discusses each of these priority areas and makes suggestions for next steps.
Early Identification of Epilepsy and Comorbid Health Conditions
As discussed in Chapter 3, prevention efforts are needed for epilepsy and comorbid health conditions. A key step toward prevention involves screening efforts, which promote the early identification and diagnosis of epilepsy in populations that may be at risk (e.g., older adults who have had a stroke, children with autism spectrum disorders) and the early identification and diagnosis of comorbid conditions in people diagnosed with epilepsy. The public health value of screening tests is that they provide the early identification of a disease or a disorder that can lead to early intervention, which can potentially eliminate or reduce the health consequences for the individual and reduce the burdens and costs on the health care system.
The state of screening tests and guidelines relevant to epilepsy and its comorbid conditions varies widely. Screening tests for epilepsy (prior to seizure occurrence) that could be used at a health screening or annual physical are not yet available. Research is needed to develop and validate tests and guidelines for early identification that are specific to this disorder. Currently, clinicians may inquire about seizures or seizure symptoms by asking questions about unexplained and episodic changes in awareness, movement, sensation, or behavior. The occurrence of frequent injuries, academic decline, mood changes, or developmental delay may trigger more detailed inquiry into the possibility of seizures or comorbid conditions. In addition, a screening test or protocol is needed that could identify individuals with persistent seizures who need to be referred to an epileptologist for further evaluation and treatment. As discussed later in this chapter and throughout the report, referrals of patients with refractory epilepsy to epilepsy centers often take more than 15 years and the goal is to move toward earlier referral patterns.
Early detection tests for some comorbid conditions relevant to epilepsy, such as bone disease, are fully validated, readily available, and commonly conducted as a part of annual physicals and health screenings for specific populations (e.g., women over the age of 65) (U.S. Preventive Services Task Force, 2011); however, these tests are not consistently administered in people with epilepsy (Chapter 3). While rapid or easily administered screening tests for cognitive impairment that could be conducted in health screenings or at annual physicals are not yet available, validated screening tests are available for depression, anxiety, and attention deficit hyperactivity disorder (Richardson et al., 2010). More complex tests, such as neuropsychological evaluations, are fully validated and available, but they are more time-consuming and not suitable for an initial screen (Chapter 6).
Once well-tested screening tests and guidelines are approved and established, mechanisms should be developed to institute the dissemination and widespread adoption of epilepsy screening as a part of standard health checkups (e.g., following similar timing as the pediatric immunization
schedule or as part of the protocols for follow-up of people who have an increased risk of developing epilepsy, such as those who have had a stroke, brain cancer, or traumatic brain injury) and in routine health screening programs (e.g., Medicaid’s Early and Periodic Screening, Diagnosis, and Treatment program). Additionally, the screening of people with epilepsy for at-risk conditions, including mental health conditions and impaired bone health as a side effect of some seizure medications, needs to be part of the standard protocol for epilepsy care.
Improving Treatment of the Epilepsies
Improving Seizure Medications
Side effects One of the major challenges with some seizure medications has been their adverse side effects. Older seizure medications have been associated with clinically significant problems with cognitive function (e.g., memory, attention, speed of mental processing), mood and behavioral disorders, and in some cases, birth defects when exposure occurs during pregnancy (Brunbech and Sabers, 2002; Meador, 2002; Vining et al., 1987). Although the newer seizure medications are similar in efficacy to first-generation medications, they appear to have better tolerability and fewer side effects (AHRQ, 2011; Brodie et al., 1995; Elger and Schmidt, 2008; Meador et al., 1999, 2001). Improving efficacy and further reducing adverse effects are ongoing goals for seizure medication development.
More information is needed about the efficacy and tolerability of the newer medications for patients with specific epilepsy types and syndromes, such as juvenile myoclonic epilepsy, Lennox-Gastaut syndrome, and absence epilepsy. Furthermore, relatively little information is available on the risks and benefits of the newly introduced seizure medications in vulnerable populations, such as children, pregnant women, and older adults.
Generic medications Because of the lower costs of generic versions of brand-name seizure medications, people with epilepsy may be switched to generic formulations once they are released to the market. In the epilepsy community, discussions continue regarding the safety of changing from brand-name to generic medications or from one generic manufacturer to another, because current studies have mixed conclusions (Andermann et al., 2007; Kesselheim et al., 2010; Sander et al., 2010; Yamada and Welty, 2011). The concern is that differences in bioequivalence between different manufacturers may increase the risk of seizures or adverse events (Andermann et al., 2007). Studies are needed to understand the extent of any variability in efficacy between brand-name seizure medications and their generic formulations, including variations in side effects. Patients need
to be informed about potential changes in their seizure medications (including switching to generics or between generics), and efforts are needed to ensure that medication choices are not driven solely by cost considerations.
Medication adherence Adhering to a medication regimen is a significant challenge for many people with epilepsy. A retrospective review of claims data for adults with epilepsy found that 39 percent did not follow their prescribed regimen at some point during the 27-month follow-up period (Davis et al., 2008). Lack of adherence was associated with an increased likelihood of hospitalization or admission to the emergency department and with increased inpatient and emergency care costs of $1,799 and $260, respectively, per patient per year. Similar results were found in a multiyear study of Medicaid costs in three states, which found that poor adherence can have significant adverse health effects and result in increased mortality and increased hospital and emergency department costs (Faught et al., 2008, 2009).
Understanding the patient perspective on taking medications is critical in developing strategies to promote adherence and, ultimately, to improve seizure control. Among the most commonly reported fears expressed by people with epilepsy (such as experiencing a seizure or losing control during a seizure) is concern about having side effects from taking seizure medications (Fisher et al., 2000a,b; Kucukarslan et al., 2008). An online survey of adults with epilepsy and health care providers supports these conclusions and anecdotal reports suggest that common reasons for not sticking with a prescribed regimen include forgetting to take the medication and not having it available (Hovinga et al., 2008). Methods of managing medications are critical self-management skills that include tracking pill taking, using pill dispensing boxes, using reminders and alarms, modifying lifestyles to make medication taking easier, and participating in counseling to identify and work to overcome other barriers to medication management.
Ensuring appropriate use of seizure medications For epilepsy patients, excessive drug load can lead to suboptimal outcomes, including greater incidence or severity of side effects or even increased frequency of seizures (Perucca and Kwan, 2005; Schmidt et al., 2002). An excessive drug load can occur when one or more seizure medications is not the right choice for the individual’s specific disorder, when higher-than-necessary dosages are prescribed or used, or when medication interactions are not considered. Tailoring epilepsy therapy to meet the needs of the individual patient is one element of the art of epilepsy management (Perucca and Kwan, 2005). As noted by Perucca and Kwan (2005), “Even though the importance of complete seizure control cannot be overemphasized, no patient should be made to suffer more from the adverse effects of treatment than from
the manifestations of the seizure disorder” (p, 897). For some patients with epilepsy, the medication burden can be reduced without increasing seizures (Bourgeois, 2002; Chuang et al., 2007; Pellock and Hunt, 1996). To reduce the inappropriate use of seizure medications, clinicians should assess whether some drugs can be safely reduced, substituted, or eliminated—and at what pace—and should examine potential pharmacokinetic interactions with medications treating comorbidities (Bourgeois, 2002). Decision-support tools for use in seizure medication management are being developed (Legros et al., 2012), and further such efforts are needed.
Comparative effectiveness Approximately half of all treatments delivered today for a wide range of health conditions have not been examined for evidence of effectiveness (IOM, 2009b). Comparative effectiveness research involves comparison of the benefits and harms of various methods of preventing, diagnosing, treating, or monitoring a clinical condition or comparison of various mechanisms of delivery of care (HHS, 2009). Given the many approaches (e.g., medications, devices, surgery, diets, behavioral interventions) used to treat epilepsy, comparative effectiveness studies would be valuable in providing rigorous assessment of these options for different types of epilepsy. Standardized measures and outcomes need to be applied in comparative effectiveness studies in order to determine which medical and nonmedical measures may be most beneficial in different population groups or settings. Determining the most effective therapies would provide the information that people with epilepsy, clinicians, payers, and policy makers need to make informed decisions about improving epilepsy care at both the individual and population levels.
One of the challenges of conducting comparative effectiveness research in epilepsy is specifying the methods and measures that should be used to collect data on the range of outcomes of interest. Seizure frequency is a widely used measure of the clinical efficacy of epilepsy medications, both in clinical practice and in research protocols (Marson et al., 1996). However, the relationship between seizure frequency and the degree of disability resulting from the seizures is poor, and instruments that are sensitive to the behavioral, affective, and cognitive comorbidities and other problems that frequently complicate the management of epilepsy need wider implementation. Such measures include the 31-item Quality of Life in Epilepsy Inventory, Beck Depression Inventory II, Beck Anxiety Inventory, Children’s Depression Inventory, Hospital Anxiety and Depression Scale, Multidimensional Health Locus of Control scale, and the International Classification of Functioning, Disability, and Health (Cramer et al., 1998; Ronen et al., 2011; Sperling et al., 2008; Tracy et al., 2007) (Chapter 2). These measures focus not only on freedom from seizures but also on improved quality of life and decreased disability.
Determining priorities for comparative effectiveness studies is the first important step (Dubois and Graff, 2011). The Patient-Centered Outcomes Research Institute established under the Patient Protection and Affordable Care Act of 2010 (ACA) (P.L. 111-148) is an independent nonprofit organization charged with identifying national priorities for research on patient-centered outcomes (PCORI, 2012). Because there are numerous treatment and management approaches for epilepsy, the research, clinical, and patient communities need to identify priorities for comparative effectiveness research for epilepsy treatment.
Improving Treatment for the Refractory Epilepsies
Epilepsy treatment should be directed to preventing seizures whenever possible and achieving control early in the course of the disorder (Sperling, 2004). While the majority of individuals with epilepsy respond well to seizure medications, approximately one-third continue to have seizures, despite trying multiple medications (Kwan and Brodie, 2000). The operational definition of refractory epilepsy is the failure to control seizures after two seizure medications (whether as monotherapies or in combination) that have been appropriately chosen and used (Kwan et al., 2010). A recent study shows that failure to respond to the first seizure medication predicts an increased risk for refractory epilepsy and adverse health outcomes (Perucca et al., 2011).
Refractory epilepsy often has significant adverse effects on physical, psychological, cognitive, social, and vocational well-being. Individuals with refractory epilepsy are at higher risk for a shortened life span, excessive bodily injury, neuropsychological and mental health impairment, and social disability (Sperling, 2004). Mortality rates are substantially higher in people with refractory seizures (Sillanpää and Shinnar, 2010; Sperling et al., 1999), and injury rates are substantial (Buck et al., 1997; Nei and Bagla, 2007) (Chapter 3). People with refractory epilepsy often have poor quality-of-life scores and high rates of depression and anxiety (Jacoby et al., 2011; Taylor et al., 2011). They face driving restrictions (Drazkowski, 2007) and are frequently unemployed or underemployed (Marinas et al., 2011; Smeets et al., 2007; Sperling, 2004) (Chapter 6). In light of the heightened risk for death and injury, all individuals with refractory epilepsy should have seizure action plans in case of prolonged or frequently recurring seizures. Action plans may include rescue medications that could be used to stop seizures as well as instructions regarding when transport to the emergency room is necessary. School-aged children need detailed seizure action plans for school and camp.
Individuals with persistent seizures need prompt referrals to epilepsy centers to determine whether the diagnosis is correct, medications are ap-
propriate, or devices or surgery are potential treatment options (Smolowitz et al., 2007). In-depth evaluations by an epilepsy specialist and continuous video-EEG monitoring can lead to more definitive diagnoses and are essential when surgery is considered for people with refractory epilepsy (Cascino, 2002). Upon referral to epilepsy centers, up to 40 percent of patients with a diagnosis of refractory epilepsy are found to have been misdiagnosed (Chemmanam et al., 2009); seizure-like events with a psychological basis are a common erroneous diagnosis. Because surgery or devices are not options for everyone with refractory epilepsy, more effort is needed to develop medications or other treatments to reduce the burden of uncontrolled seizures.
Improving the Diagnosis and Treatment of Comorbid Conditions
While stopping seizures is a major goal in the treatment of epilepsy, it is not the only treatment goal. As detailed in Chapter 3, epilepsy is associated with a range of comorbid conditions that may also result in diminished well-being and reduced quality of life. More attention is needed to the full range of side effects including effects on oral health (Karolyhazy et al., 2003). Improving the diagnosis and treatment of these conditions will include greater emphasis on coordination and co-management of care.3 Diagnosis of comorbidities may be delayed in part because office visits with the health care provider are usually short, and many topics and concerns need to be discussed, including seizure frequency and severity, medication and other adverse effects, mood, sleep patterns, fitness, bone health, and endocrine status (Chapter 7). However, allocating time to discuss comorbid conditions is important whether or not seizures are controlled. A division of responsibilities within the care team to diagnose, treat, and manage these conditions can be an effective allocation of skills, time, effort, and cost.
Further, some unique aspects of the relationships between epilepsy and its comorbidities can complicate diagnosis and treatment. For example, a history of depression or depressive symptoms has been reported in up to two-thirds of patients with refractory epilepsy (Lambert and Robertson, 1999), but the side effects of some seizure medications include symptoms of depression (Andersohn et al., 2010; Bell and Sander, 2009; Mula and Sander, 2007). Once the comorbidities are recognized, the clinician needs
_______________
3This report uses the term “co-management” to describe efforts in which health care providers from different disciplines work together and with the patient to make decisions and provide patient-centered care for multiple health conditions. The term “coordinated care” is used as a broader term to discuss efforts across health care and community settings in order to provide health and human services (e.g., health care, housing, education, employment) that meet the needs of the individual with epilepsy. Both co-management and coordinated care are necessary to provide high-quality, patient-centered care.
to determine whether they are related to the occurrence of seizures, seizure medication side effects, or other causes. Diagnostic tools such as the Neurological Disorders Depression Inventory for Epilepsy can be used as practical screening instruments (Barry et al., 2008; Friedman et al., 2009). Selecting the appropriate medications to treat comorbidities also may be difficult. For example, several psychotropic medications may lower seizure threshold, whereas others have been found to have antiseizure properties (Alper et al., 2007). In general, more research is needed on the safety, efficacy, and interactions of medications for epilepsy and comorbid conditions. Working to alleviate or eliminate comorbid conditions often necessitates collaboration across a range of health care and community service providers. Barriers to collaboration include multiple sources of payment, inadequate communication and co-management across providers, and difficulties with scheduling logistics for referrals. Pilot programs developed through the Managing Epilepsy Well Network (described in Chapter 3) are using online tools, support networks, and collaboration between multiple health care providers to provide care and assistance. Treatment programs for comorbidities such as those discussed in Box 4-1 warrant further investigation to see who benefits most, how they may complement traditional medical approaches and epilepsy care, and whether these programs can help bridge the gaps in mental health care for people with epilepsy.
Improving Communication Between Health Care Providers and Patients
Building a trusting and collaborative relationship that enables quality care requires clear communication between health care providers and the individual with epilepsy, family members, and caregivers. Health professionals need to convey information in ways that take into account health literacy and cultural sensitivities. In particular, they need to clearly communicate the risks of epilepsy and be aware of the resources and services that are available, including state and local Epilepsy Foundation affiliates and organizations working to help individuals with specific epilepsy syndromes or types of epilepsy. In Chapter 9 the committee calls for the development of a 24-hour telephone or Internet helpline that would be an information resource for people with epilepsy and their families. This does not need to be a stand-alone effort but could be part of a collaborative effort that builds on an ongoing help line for a related health condition.
Studies have shown that health literacy affects health care utilization, outcomes, and costs (ODPHP, 2010; Parker et al., 2008). Low health literacy is widespread in the U.S. population and is estimated to cost the U.S. economy between $106 billion and $238 billion annually, or between 7 and 17 percent of personal health expenditures (Vernon et al., 2007). Individuals with low health literacy may not understand their treatment options,
Box 4-1 EXAMPLES OF TREATMENT PROGRAMS FOR COMORBIDITIES
The following two multifaceted programs were developed and evaluated as part of the Center for Disease Control and Prevention’s (CDC’s) Managing Epilepsy Well (MEW) Network.
PEARLS (Program to Encourage Active, Rewarding Lives for Seniors) was originally developed to reduce minor depression in medically ill, low-income, older adults through a home-based self-management program (Ciechanowski et al., 2004). Major components of the program, which showed reduced symptoms of depression and improved health status in a randomized controlled trial, included problem solving, encouragement of social and physical activity, and communication between the psychiatrist and the patient’s primary care physician about possible treatment with antidepressants (Ciechanowski et al., 2004). This program was revised for people with epilepsy through collaboration with the MEW Network (Dilorio et al., 2010). In a randomized trial, people with epilepsy were assigned either to receive eight 50-minute problem-solving sessions in the home from a trained therapist and monthly follow-up telephone calls, or to receive usual care. In the intervention group, therapists regularly reviewed progress of the sessions with a team psychiatrist who consulted with the neurologist regarding treatment related to depression. Sessions were modified to encourage people with epilepsy to be active both socially and physically, and unemployed individuals were given contact information for vocational rehabilitation. On aver-age people with epilepsy in the intervention group had 6.2 problem-solving sessions and 2.5 follow-up telephone calls. Results are promising. The intervention group had significantly less depression severity and suicide ideation and greater emotional well-being, compared to the control group (Ciechanowski et al., 2010).
Project UPLIFT (Using Practice and Learning to Increase Favorable Thoughts), which also has the goal of reducing depression, uses a mindfulness approach and cognitive-behavioral therapy. Project UPLIFT was designed to be delivered in eight weekly sessions to small groups by telephone or the Internet (Walker et al., 2010). An initial pilot study demonstrated that people with epilepsy who received the intervention (randomly assigned to phone or Internet) had a greater decline in symptoms of depression and greater increase in knowledge and skills than the control group at 8 weeks (Thompson et al., 2010). Project UPLIFT was effective in using both the Internet and telephone methods; however, participants reported that they would have liked to have been able to participate using both methods (Walker et al., 2010).
may not understand how to take prescribed medications correctly and why that is important, and may not be able to navigate the health system effectively, which can be a particular challenge for people with epilepsy given the multiple services and providers sometimes involved in epilepsy and care for associated comorbidities.
Bautista and colleagues (2009) found that people with epilepsy who had low health literacy (measured by the frequency with which they had someone help them read hospital materials or their confidence in filling out medical forms by themselves) were more likely than others to have poorer
quality-of-life scores. Health professionals need to focus on how they convey information to their patients as well as how they respond to and encourage questions and interactions. Efforts to develop epilepsy-specific tools and materials to assist health professionals in meeting health literacy needs are ongoing, as are efforts to improve the epilepsy-related knowledge of patients and their families (Chapter 7).
Discussions about the risks of epilepsy, possible treatment side effects, and the importance of self-management are critical components of effective communications between clinicians, patients, and families. Elevated rates of death and increased risks of injury in people with epilepsy underscore the seriousness of epilepsy as a public health problem (Chapter 3). Suicidal ideation, suicide attempt, suicide, death as a consequence of a seizure or of status epilepticus, and sudden unexpected death in epilepsy (SUDEP) are potential catastrophic consequences of living with epilepsy but are not commonly discussed with individuals with epilepsy and their families. One of the major areas to be addressed is the discussion of SUDEP (Devinsky, 2011) (see also Chapter 7). A consensus conference on SUDEP (Hirsch et al., 2011), as well as public testimony received by the committee, indicate that people with epilepsy and their families want to know about SUDEP and other epilepsy-related risks, as well as learn about any strategies they can pursue to minimize them. Recommendations of a joint task force of the American Epilepsy Society (AES) and the Epilepsy Foundation urge that SUDEP be discussed in the context of comprehensive epilepsy education (So et al., 2009).
Developing a National Strategy for Performance Measurement
and Quality Improvement in Epilepsy Care: Improving Practice
Guidelines and Implementing Performance Metrics
Evidence-based guidelines provide the basis for ensuring the consistent delivery of high-quality health care. The implementation of evidence-based guidelines can be incentivized through the use of performance metrics4 to track what is being done in clinical practice and to hold health professionals and health care facilities accountable for the quality of care delivered. As defined by Sackett and colleagues and adapted by the IOM in Crossing the Quality Chasm, “Evidence-based practice is the integration of the best research evidence with clinical expertise and patient values” (IOM, 2001, p. 34; Sackett et al., 1996). In 2003, the Living Well with Epilepsy II Con-
_______________
4The term “performance metrics” is being used broadly in this report to encompass the wide range of measures of health care quality that include measures and indicators of clinical care, health care processes, and patient outcomes and satisfaction. The goal for the development and implementation of performance metrics is improvement in the quality of health care.
Box 4-2 EXAMPLES OF PRACTICE GUIDELINES
American Academy of Neurology Practice Guidelinesa
• Antiepileptic Drug Selection for People with HIV/AIDS (Birbeck et al., 2012)
• Update: Management Issues for Women with Epilepsy—Focus on Pregnancy: Obstetrical Complications and Change in Seizure Frequency (Harden et al., 2009a)
• Update: Management Issues for Women with Epilepsy—Focus on Pregnancy: Teratogenesis and Perinatal Outcomes (Harden et al., 2009b)
• Update: Management Issues for Women with Epilepsy—Focus on Pregnancy: Vitamin K, Folic Acid, Blood Levels, and Breast-Feeding (Harden et al., 2009c)
• Evaluating an Apparent Unprovoked First Seizure in Adults (Krumholz et al., 2007)
• Reassessment: Neuroimaging in the Emergency Patient Presenting with Seizure (Harden et al., 2007)
• Diagnostic Assessment of the Child with Status Epilepticus (Riviello et al., 2006)
• Use of Serum Prolactin in Diagnosing Epileptic Seizures (Chen et al., 2005)
• Efficacy and Tolerability of the New Antiepileptic Drugs I: Treatment of New Onset Epilepsy (French et al., 2004a)
• Efficacy and Tolerability of the New Antiepileptic Drugs II: Treatment of Refractory Epilepsy (French et al., 2004b)
International League Against Epilepsy
• Evidence-Based Analysis of Antiepileptic Drug Efficacy and Effectiveness as Initial Monotherapy for Epileptic Seizures and Syndromes (Glauser et al., 2006)
• Guidelines for Imaging Infants and Children with Recent-Onset Epilepsy (Gaillard et al., 2009)
ference highlighted the need to define and establish criteria for quality care of epilepsy (Austin et al., 2006).
Practice Guidelines
The push for evidence-based medicine has resulted in a number of practice guidelines for the evaluation and treatment of epilepsy in the United States and internationally (Box 4-2). Many of the U.S. guidelines are available through the National Guideline Clearinghouse of the Agency for Healthcare Research and Quality (AHRQ, 2012). In these documents, the nature and level of the evidence are detailed for specific clinical services or procedures and the balance of risk versus benefit is discussed. To date, epilepsy-specific practice guidelines have been developed primarily by pro-
American Academy of Pediatrics
• Neurodiagnostic Evaluation of the Child with a Simple Febrile Seizure (AAP Subcommittee on Febrile Seizures, 2011)
• Utility of Lumbar Puncture for First Simple Febrile Seizure Among Children 6 to 18 Months of Age (Kimia et al., 2009)
American Association of Neuroscience Nurses
• Care of the Patient with Seizures. Second edition (AANN, 2009)
American College of Radiology (ACR)
• ACR Appropriateness Criteria® Seizures: Child (Prince et al., 2009)
United Kingdom, National Institute for Health and Clinical Excellence
• CG20 Epilepsy in Adults and Children: Full Guideline (NICE, 2004)
European Federation of Neurological Societies (EFNS)
• EFNS Guideline on the Management of Status Epilepticus (Meierkord et al., 2006)
Scottish Intercollegiate Guidelines Network
• Diagnosis and Management of Epilepsy in Adults. A National Clinical Guideline (Scottish Intercollegiate Guidelines Network, 2003)
_____________
aSome of the AAN Practice Guidelines were developed in conjunction with the American Epilepsy Society, ILAE, or the Child Neurology Society.
fessional associations and organizations. Assessments should be conducted of the need for additional guidelines in epilepsy care and areas should be identified in which robust evidence does not yet exist, so that systematic, transparent, and reproducible methods can be used to develop the needed evidence base.
While the guidelines are based on evidence-based medicine, little is known about how often the guidelines are implemented and followed, the extent to which improvements in patient care result, and why failures in implementation or improved outcomes may occur (Davis et al., 2004; Stephen and Brodie, 2004). For example, Bale and colleagues (2009) assessed whether pediatricians were aware of a practice parameter, or clinical practice guideline, on nonfebrile seizures and, if so, the extent to which they incorporated the parameter into practice. Although most of the respond-
ing pediatricians were caring for children with seizures, 60 percent were not aware of the practice guideline. In responding to a clinical scenario, many said they would order laboratory tests that were not in the guideline. Similarly, a questionnaire sent to UK neurologists asked whether they discussed SUDEP with all epilepsy patients and their families, which has been recommended by the UK National Institute for Health and Clinical Excellence (Morton et al., 2006). Of the validated respondents, only 5 percent discussed SUDEP with all patients, 26 percent with a majority, 61 percent with a few, and 7.5 percent with none.
In addition to educating clinicians and patients about the existence and content of evidence-based guidelines, tools are needed to ensure that the guidelines are implemented at the point of care. Performance metrics (described below) are increasingly being used to incentivize the use of best practices in health care. Additionally, many hospitals and other health care facilities have developed clinical pathways that help health professionals formulate plans for the process of care; for example, epilepsy-specific pathways may focus on care for people with new-onset seizures, for women during pregnancy, or for patients considering surgery. Given the ongoing transition to electronic health records (EHRs) and the potential that EHRs hold for providing immediate information to health professionals and their patients, the epilepsy community must work to incorporate relevant guidelines into EHR development, create decision prompts, keep treatment information current, and ensure integration of relevant clinical information across providers. EHRs also may simplify and lower the cost of conducting audits that can provide feedback to clinicians, patients, and health systems on the alignment of care with evidence-based guidelines and performance metrics.
Performance Measurement and Improvement
The IOM has published several reports defining the quality of health care and outlining the aims for which the health system should strive— safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity (e.g., IOM, 2001, 2006a,b, 2011). To achieve quality in health care and develop the accountability and transparency needed to incentivize change and to allow comparisons within and among health care providers, the focus over the past 20 years has been on developing, implementing, and analyzing performance metrics.
The evolution of performance measurement and improvement Large and small employers, federal agencies, and state governments have worked with health care providers and relevant organizations to develop systems for measuring performance and improving quality and also for understanding
the value of purchased health care services. One example is the Healthcare Effectiveness Data and Information Set (HEDIS), designed by a broad coalition of stakeholders (Committee on Performance Measurement) in collaboration with the nonprofit National Committee for Quality Assurance (NCQA), which measures the performance of the managed care industry (NCQA, 2012). Early and ongoing supporters of the implementation and use of performance metrics include a number of managed care organizations around the country that use the information to assess performance across their organization and compare it to other managed care organizations. Similar performance measurement and improvement efforts for hospitals, physicians, and other providers have been developed or endorsed by the Joint Commission, the National Quality Forum (NQF), the Physician Consortium for Performance Improvement (PCPI), and other organizations, and many of these efforts work through broad coalitions of stakeholders.
Early developers of performance metrics recognized the importance of establishing a set of criteria or a strategy that specified how performance measurement areas would be selected and how specific metrics would be built, tested, used, and eventually, retired. For example, in HEDIS 2000: What’s in It and Why It Matters, the NCQA (1999) outlined the categories (domains) selected for performance measurement (effectiveness of care, access and availability, satisfaction with the experience of care, health plan stability, use of services, cost of care, informed health care choices, and health plan descriptive information) and detailed a set of desirable attributes of performance metrics, which were organized into three broad areas: relevance, scientific soundness, and feasibility. The set of metrics that emerged covered a range of topics but focused on clinical areas in which good evidence existed to support quality improvements. The development of the HEDIS metrics included an emphasis on patient participation. The NQF has a similar set of criteria for measurement adoption (NQF, 2011).
Early efforts in the development of performance metrics aimed to build sets of metrics that would drive toward standardization and the ability to compare providers and provider organizations. These standardization activities emerged in part to add value to the certification and accreditation of hospitals, health maintenance organizations, and other types of health care facilities, recognizing that performance measurement was a prerequisite to improving care. Since that time, the concept of pay-for-performance has continued to evolve, and public and private payers are attempting to financially reward high-quality providers and organizations based on standardized metrics.
Measuring performance and improving quality in epilepsy care The epilepsy community has taken important first steps in the development of performance metrics for high-quality epilepsy care. The American Academy
of Neurology (AAN), in conjunction with the PCPI, sponsored a literature review and assessment, conducted by an expert panel, that identified eight performance metrics that could be used in quality improvement, pay-for-performance, or maintenance of certification programs (Fountain et al., 2011). The eight metrics submitted to the NQF for consideration were evidence based and represented gaps in care of people with epilepsy (Fountain et al., 2011):
• Documentation in the medical record of “Seizure type and current seizure frequency
• Documentation of etiology of epilepsy or epilepsy syndrome
• EEG results reviewed, requested, or test ordered
• MRI/CT [computerized tomography] scans reviewed, requested, or scan ordered
• Querying and counseling about side effects of [seizure medication]
• Surgical therapy referral consideration for [refractory] epilepsy
• Counseling about epilepsy-specific safety issues
• Counseling for women of childbearing potential with epilepsy.”
While the metrics were not endorsed by the NQF, the Centers for Medicare and Medicaid Services (CMS) has adopted three of the metrics (documentation of seizure type and frequency, documentation of etiology of epilepsy, and counseling for women of childbearing potential) to be used by providers participating in the Physician Quality Reporting System (CMS, 2011a). Provider documentation of the CMS quality metrics is currently voluntary but will become mandatory beginning in 2015 in order to qualify for full Medicare reimbursement (CMS, 2011a,b). The epilepsy-specific metrics will apply to any health professional who submits a bill for care of a person with seizures or epilepsy to Medicare. This represents a significant step forward in evaluating the quality of care in epilepsy. However, additional evidence-based performance metrics are needed to focus on the full range of gaps in care, such as referral of people with refractory epilepsy for surgical consultation or evaluation of adverse effects of treatments. The epilepsy community, in conjunction with the CMS, NQF, private insurers, and other organizations involved in performance measurement and quality improvement, should continue to develop, implement, evaluate, and report on evidence-based metrics for care of people with epilepsy.
Further, there are ongoing efforts to develop a set of performance metrics focused on epilepsy care within primary care and general neurology clinics. The QUIET (QUality Indicators in Epilepsy Treatment) study used a multipronged approach of literature and guideline review, patient focus groups, and an expert panel to examine quality of care for adults with epilepsy (Bokhour et al., 2009; Pugh et al., 2007, 2011). The process led to a set of performance metrics (“quality indicators”) consisting of both
evidence- and patient-based metrics (Bokhour et al., 2009; Pugh et al., 2007). The evidence-based metrics were tested in a tertiary medical center (Pugh et al., 2011). The QUIET study then compared chart abstractions for epilepsy-focused medical encounters from primary care and neurology clinics separately, as well as from patients who received care in both neurology and primary care settings. Approximately 44 percent of the 1,985 possible care processes were performed in concordance with the defined metrics (Pugh et al., 2011). People who received care from both groups or “shared care” had the highest rate of concordance with the metrics. Incorporating the patient perspective is an important part of quality-improvement efforts and is integral to ensuring patient-centered care.
Next steps for improving quality in epilepsy care The committee believes that the efforts described above form a solid basis for moving forward to assess and improve the quality of epilepsy care. A national strategy for performance measurement and quality improvement in epilepsy care is needed that would specify the broad areas (domains) that are meaningful for assessing epilepsy care (e.g., access to care for epilepsy and comorbid health conditions, including mental health services, effectiveness of care, quality of life improvements, communications between patient and health care provider, and cost of care) and that would detail the criteria for and attributes of performance metrics that the epilepsy field believes are important to emphasize (e.g., evidence based, patient centered). Development of this strategy should involve people with epilepsy and their families, relevant professional and advocacy organizations, researchers, health and human services professionals, and experts in performance metrics and health care quality improvement.
A national strategy for performance measurement and quality improvement in epilepsy care could
• provide a roadmap for next steps in developing performance metrics to allow for an organized effort to prioritize, develop, evaluate, and approve new metrics;
• establish definitive standards for the attributes that performance metrics must meet in order to be included in a measurement set;
• ensure transparency;
• emphasize a patient-centered focus for quality in epilepsy care; and
• provide an agenda for next steps in effectiveness reviews and the development of additional practice guidelines for epilepsy care.
Evaluating and Accrediting Epilepsy Centers
In 1978, the U.S. Commission for the Control of Epilepsy and Its Consequences noted in a report that there were many gaps in epilepsy care,
including insufficient patient and family education and psychosocial treatment (U.S. Commission for the Control of Epilepsy and Its Consequences, 1978). Epilepsy centers of excellence were then funded in response to a National Institutes of Health (NIH) initiative, and these served as regional treatment and referral networks. The centers spearheaded research into the psychosocial needs of people with epilepsy and developed educational programs to respond to individual, family, and community needs. Subsequent changes in funding mechanisms led to curtailment of NIH funding for epilepsy centers and the eventual establishment of health care facility-based epilepsy centers. The committee looked at the current criteria for the four levels of epilepsy centers and explored how centers for other health conditions are evaluated in order to make recommendations for strengthening the nation’s epilepsy centers.
Current Epilepsy Centers
National Association of Epilepsy Centers Currently, 166 self-designated epilepsy centers are members of the National Association of Epilepsy Centers (NAEC, 2012a). NAEC guidelines for level 3 and level 4 epilepsy centers are voluntary, and each center self-designates based on the level of care it provides (NAEC, 2012b). Level 1 care is designated as that provided by emergency care or primary care providers, while level 2 care is provided by general neurologists (Labiner et al., 2010). Level 3 and level 4 care are provided by epilepsy centers, with both of these levels providing EEG services with long-term monitoring, epilepsy surgery (level 4 centers also provide non-lesional epilepsy surgery), neuroimaging, neuropsychological and psychological services, rehabilitation services, and other specialized services (including pharmacology consultations and interdisciplinary clinical services). Level 4 centers also provide functional cortical mapping, specialized neuroimaging, electrocorticography, and other more specialized services (Labiner et al., 2010).
In a survey conducted for this report (Appendix C) and completed by approximately one-quarter of the NAEC centers, each center served an average of 1,300 patients per year and provided an average of 3,400 outpatient visits with an epileptologist per year. Referral patterns varied significantly across the NAEC centers; approximately 40 percent of patients were referred by primary care providers, 36 percent by neurologists, 16 percent by other specialists, and 4 percent by the Epilepsy Foundation.
Tuberous Sclerosis Alliance specialty clinics The Tuberous Sclerosis Alliance has established criteria for specialty clinics that provide comprehensive treatment for tuberous sclerosis complex—both clinic standards and gold standards are specified and centers are encouraged to meet gold standard
requirements (Tuberous Sclerosis Alliance, 2011). Health care facilities attest that they meet the standards for a specialty clinic and are required to submit an annual report to the Tuberous Sclerosis Alliance to maintain that designation.
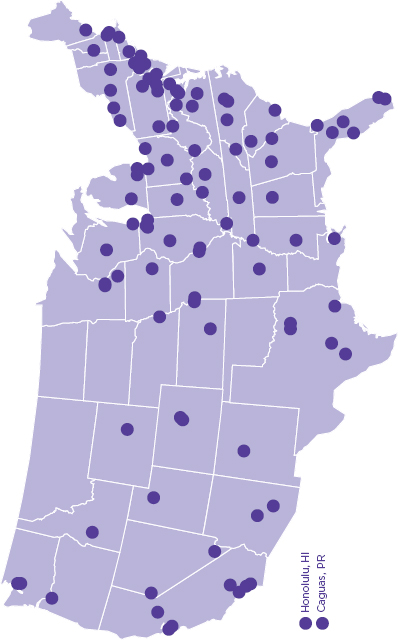
Department of Veterans Affairs (VA) Epilepsy Centers of Excellence The increasing prevalence of epilepsy in older veterans from age-related conditions and in younger veterans with recent war-related injuries led to a recent resurgence of interest in epilepsy at the VA,5 and in 2008, 16 Epilepsy Centers of Excellence were created within the Veterans Health Administration (VA, 2011a,b). Epilepsy Centers of Excellence must be affiliated with a medical school for education and training, and they collaborate with VA Polytrauma Centers to provide care to veterans with traumatic brain injury who are at risk for epilepsy (VA, 2011a). The VA Epilepsy Centers of Excellence provide both inpatient and outpatient care for veterans with seizures, including advanced diagnostics and evaluation services and other clinical care by epilepsy specialists, with co-management between specialists and primary care providers within and external to the VA when appropriate (Parko, 2011; VA, 2011a). The centers collaborate nationally to conduct epilepsy research and provide epilepsy education, and they are developing information systems, national databases, and telehealth programs to improve patient care and research. Clinical pathways have been developed to ensure consistent approaches to care and facilitate access to specialists for people at risk for seizures or comorbid health conditions. The centers have not been operational long enough for publication of evaluation data.
Models of Center Evaluation and Accreditation
In considering next steps for epilepsy centers, the committee looked at processes used to designate and evaluate centers focused on other diseases. Relevant models having some preliminary outcome data and models of quality improvement initiatives include stroke centers, trauma centers, VA cancer centers, and cystic fibrosis centers.
Over the past decade, a coalition of professional organizations established accreditation criteria and a certification process for Primary Stroke Centers (Alberts et al., 2000; Reeves et al., 2010). These centers collect and compare data on 10 quality measures, are evaluated through site visits by the Joint Commission, and are assessed every 2 years for recertification (Rymer, 2011). Plans are under way for a second type of certified stroke
_______________
5An epilepsy monitoring unit was established at a VA hospital in the early 1960s and in 1972 the VA designated several hospitals as epilepsy centers (Parko, 2011).
center, a Comprehensive Stroke Center that would provide more complex care, including surgical care and care for patients with specific types of stroke (Alberts et al., 2005; Joint Commission, 2011a). Few studies to date have compared outcome data for the accredited primary stroke centers; however, studies by Lichtman and colleagues (2011a,b) found that Joint Commission–certified Primary Stroke Centers had lower 30-day mortality risk for two different types of stroke compared to noncertified hospitals, although readmission rates were similar.
The designation of trauma centers follows a different process than that of stroke centers. The American College of Surgeons (ACS) verifies that a hospital has the specific resources needed to provide one of three levels of trauma care (ACS, 2011). A designated team of trauma experts conducts site visits, and verification certificates must be renewed every 3 years. A study of this process, comparing the experience of trauma patients in a community hospital before and after level 2 designation, found that, after designation, patients experienced shorter hospital stays, lower inpatient mortality, and reduced costs (Piontek et al., 2003).
Positive changes in quality of care were documented for veterans with chronic disease following VA restructuring in the mid-1990s that involved integrated networks of care, enhanced use of information technology, quality measurement and performance initiatives, and improved access to care (Jha et al., 2003; Kizer et al., 2000). Cancer centers in the VA are organized into regional comprehensive centers as well as secondary centers (Keating et al., 2011). VA cancer center care for older men (over age 65) with one of four types of cancer (colorectal, lung, prostate, or hematologic) has been found to be equal to or better than that for older men receiving fee-for-service care (through Medicare) in the private sector.
The Quality Improvement Initiative of the Cystic Fibrosis Foundation (CFF) Centers provides a model of how centers are working together to collect and learn from data on a specific disease. The CFF accredits 110 care centers in the United States (CFF, 2012a). The Quality Improvement Initiative involves the collection of data on seven key health measures from each of the accredited centers, including data on lung function, nutritional status, percentage of persons screened for cystic fibrosis-related diabetes, and percentage of people with cystic fibrosis who have had the recommended four clinic visits, one sputum or throat culture, and two lung function tests per year (CFF, 2012b; Kraynack and McBride, 2009; Quon and Goss, 2011). Additionally the CFF supports the Cystic Fibrosis Patient Registry that provides an overview and collated data on more than 25,000 people with cystic fibrosis and issues an annual report on progress in improving care (CFF, 2012a).
External Accreditation of Epilepsy Centers and Development of an Epilepsy Care Network
The committee considered information on the benefits and limitations of external accreditation of epilepsy centers and believes that this process would be valuable to ensure excellence, consistency, clarity, and transparency in the provision of epilepsy care. The challenges of accreditation include cost and time burdens on the centers, but the committee believes that the advantages of accreditation and the rigor and external validation it could bring to the field far outweigh these disadvantages. Currently, each center self-designates as providing one of the four levels of care, but no external evaluation process is used to assess whether the voluntary guidelines are being met.
The Joint Commission has developed a process for Disease-Specific Care Certification that includes epilepsy and requires that programs comply “with consensus-based national standards, effective use of evidence-based clinical practice guidelines to manage and optimize care, and an organized approach to performance measurement and improvement activities” (Joint Commission, 2011b, p. 1). However, epilepsy-specific criteria have not been developed, and only a few programs have pursued this certification.
The committee believes that increasing the level of rigor for epilepsy centers through the use of external evaluation, as well as establishing a research and data-sharing network, would enhance the quality of epilepsy care and lead to advances in the field. Health outcomes data are needed for epilepsy care, and data required for accreditation would help to provide that information. The following qualities of an accredited epilepsy center are deemed critical:
• External evaluation—Processes need to be developed for external review by the Joint Commission or a similar independent external body that will assess an applicant against national standards, criteria, and quality metrics.
• Research and data sharing network—A set of common data elements to measure services, quality, and outcomes could be developed and reported by accredited epilepsy centers for accountability, quality, reporting, and research purposes.
• Interdisciplinary care—Comprehensive and coordinated biopsychosocial approaches to acute and chronic care of epilepsy that involve a wide range of health professions should be implemented with a patient-centered focus.
• Quality improvement—A rigorous quality improvement program should be required that measures the processes and outcomes of a certified center to ensure care is safe, effective, patient centered, timely, efficient, and equitable.
• Co-management of care—Criteria and best practices for the co-management of health care must be established between epilepsy specialists, primary care providers, and specialists treating comorbid conditions, including mental health treatment providers.
• Community outreach—Active efforts should be focused on con-necting with local primary care providers to enhance their knowledge about epilepsy and their care of people with the disorder as well as ensuring that community health programs providing health services for underserved populations are connected to epilepsy specialists.
• Educational and community referral resource—Accredited epilepsy centers should be sites where patients and their families receive education and self-management training, screening for common comorbid conditions, and referrals for support within appropriate community agencies, including schools, day care centers, vocational rehabilitation services, and those providing housing and other independent living resources, financial assistance, and respite care.
• Professional education—Accredited centers should train epilepsy technicians, nurses, and physicians as well as provide a training locus for emergency personnel, general neurologists, primary care providers, and other interested health professionals.
The committee is not specifying a particular system of certification or accreditation for epilepsy centers but emphasizes the need for an accreditation process that uses external evaluation. The approach could involve a tiered system of primary and comprehensive epilepsy centers, such as the system being put in place for Joint Commission-certified stroke centers or the ACS-designated trauma centers, or it could involve some other organizational structure.
Accredited epilepsy centers are envisioned as having strong links to each other and to community resources through an Epilepsy Care Network of Accredited Epilepsy Centers. This network could promote research advances through collaborative clinical and health services research. More needs to be known about the use of health services by people with epilepsy in order to identify and close gaps (Reid et al., 2012). Each center should be well integrated into the health system and locality that it is a part of as well as into the network of centers. Strong ties and partnerships with state health departments and other health care providers, particularly those focused on other neurological disorders, could expand the reach of coverage to people with epilepsy who are in rural and underserved areas through use of telemedicine, outreach clinics, and other relevant mechanisms. People with epilepsy and their families, as well as
researchers and health care providers, could also benefit from the compilation and analysis of quality, outcomes, and health services data provided by all centers in the network.
IMPROVING ACCESS TO HEALTH CARE
Common challenges for patients in getting to their epilepsy appointments are transportation need, not being able to afford to go to their doctor, and getting a referral from their primary care or neurology provider.
–Sandra Helmers
Access to health care was defined in a 1993 IOM report as the “the timely use of personal health services to achieve the best possible health outcomes” (p. 4). This study went on to point out that “access problems are created when barriers cause underuse of services, which in turn leads to poor outcomes” (IOM, 1993, p. 35).
For individuals with epilepsy, as with all people, having adequate access to care involves being able to obtain and keep public or private health insurance coverage and navigate through the complex U.S. health system in a timely and effective way to obtain services they need. Challenges arise due to many factors, including the limited number of specialty care providers, variability in the skills and knowledge of epilepsy by primary care providers, and limited options for epilepsy care offered by hospitals and communities. Connections need to be strengthened and referrals available— when appropriate—among the different care options that include primary care providers, neurologists, epileptologists, and specialists in the various comorbidities of epilepsy. Further, referrals may be needed to obtain the services of other professionals, such as social workers, occupational specialists, or nutritionists. Limitations in access may result from the location of services in multiple health care and community facilities with limited transportation options, as well as from limits in health insurance plans for the coverage of certain services.
Recent studies provide evidence that disparities exist in access to specialized epilepsy care in populations with low socioeconomic status (SES) and in racial/ethnic minority populations. In a study of patients at four neurology clinics in Houston and New York City, low-SES patients had more frequent emergency room visits and higher hospitalization rates than people in higher-income groups (Begley et al., 2009). In a California population survey, low-income people with epilepsy (incomes below poverty level) were 50 percent less likely to report taking seizure medications (Elliott et al., 2009). African Americans were found to have poorer adherence to seizure medications (Bautista et al., 2011). People using emergency rooms for treatment of seizures were more likely to be uninsured (Farhidvash et al., 2009). Use of neurologists was relatively
similar, regardless of SES, in a study of people with epilepsy in Houston and New York City (Begley et al., 2011), although other studies have found a lower rate of neurologist visits for uninsured individuals (Halpern et al., 2011) and greater difficulties for children enrolled in Medicaid to obtain neurologist appointments (Bisgaier and Rhodes, 2011). Studies examining disparities for racial/ethnic minority populations found that African American individuals were more likely than whites to use emergency departments for epilepsy care (Kelvin et al., 2007) and less likely to have epilepsy surgery (Berg et al., 2003; Burneo et al., 2005; McClelland et al., 2010). African American and Hispanic individuals had lower rates of epilepsy-related visits to specialists than white individuals (Begley et al., 2009). However, for those who did have surgery, race and SES did not appear to affect outcomes (Burneo et al., 2006).
These subgroup differences reflect broader challenges faced by people with epilepsy and people with other neurological conditions in trying to access specialized care. Child neurologists reported wait times for new patients averaging 53 days, while returning patients had to wait 44 days (Polsky et al., 2005). Physicians serving patients covered by public insurance (Medicaid and the Child Health Insurance Program) reported difficulty finding a neurologist to whom to refer patients (GAO, 2011).
Disparities in access to epilepsy care as reflected in treatment gaps are major concerns internationally, as well as in the United States, as noted in Chapter 1. While research has documented disparities in receiving equitable and timely epilepsy care, the reasons for these inequities, their importance for health outcomes, and their magnitude in relation to overall gaps in care have to be better understood in order to improve access to care. The committee developed a framework for considering the many factors that affect access to care (Figure 4-2) to assist in identifying priority areas for additional research and for improvement. These priorities are
• strengthen epilepsy care by primary care providers and clarify clinical pathways for referrals and for care by specialists,
• promote a collaborative and patient-centered approach to the care of epilepsy and comorbid conditions,
• ensure a robust, well-educated health professional workforce for epilepsy care,
• reach rural and underserved populations,
• provide smooth transitions of care, and
• make health insurance coverage affordable and readily available.
Strengthen Epilepsy Care by Primary Care Providers and Clarify Clinical Pathways for Referrals and Care by Specialists
One of the biggest challenges to improving access to care of people with epilepsy is ensuring timely, adequate care by the appropriate health care and human services providers. Often primary care providers are the first to see the patient after an initial seizure (Browne and Holmes, 2001; Mantoan and Kullmann, 2011; Reuter and Brownstein, 2002). In a community-based survey of people with epilepsy, 40 percent of respondents reported that they first saw a family or general practitioner, 32 percent a neurologist, 13 percent a pediatrician, 5 percent an internist, and 5 percent an emergency room physician (Fisher et al., 2000b). Further, primary care providers may often provide the long-term management of epilepsy care for people whose seizures are well controlled. In a survey by Fisher and colleagues (2000b), the respondents who noted that they were currently seeing a primary care provider for their epilepsy care were generally those who had not had a seizure in the past year and had received their diagnosis of epilepsy 5 years ago or more. A survey involving primary care physicians found that the majority referred at least half of their patients having seizures to a neurologist, while a smaller percentage was comfortable treating most patients with seizures themselves (Moore et al., 2000). Because there is a significant role for primary care providers in the care of epilepsy patients (often over the lifetime of their patients), it is critical that they are knowledgeable about epilepsy care (Chapter 5), are communicating with their patients about care options and the risks associated with epilepsy (Chapter 7), and have clear direction on the timing and options for referrals to epilepsy centers and epileptologists.
As noted earlier in this chapter, concerns have been raised about the length of time that some patients with refractory epilepsy wait for referrals to an epilepsy monitoring unit for further evaluation and a surgical consultation. Clinical practice guidelines and recommendations from professional organizations suggest that when the diagnosis is in question, or seizure control is not achieved after (1) a trial of two or three appropriate seizure medications or (2) 1 year of care with a general neurologist, patients should be referred to an epileptologist or epilepsy center (Cross et al., 2006; Labiner et al., 2010). However, one center studied in the 5 years after release of an AAN practice parameter that specified referral to an epilepsy surgery center after appropriate trials of seizure medications had failed to stop seizures from recurring and found that in that center, approximately 18 years elapsed between therapeutic intervention and surgical evaluation (Engel et al., 2003; Haneef et al., 2010). Similarly, a retrospective review of adult admissions to an epilepsy monitoring unit and surgical referrals found wide variations in time from onset of seizures to referral, with a median elapsed time of 15 years (Smolowitz et al., 2007).
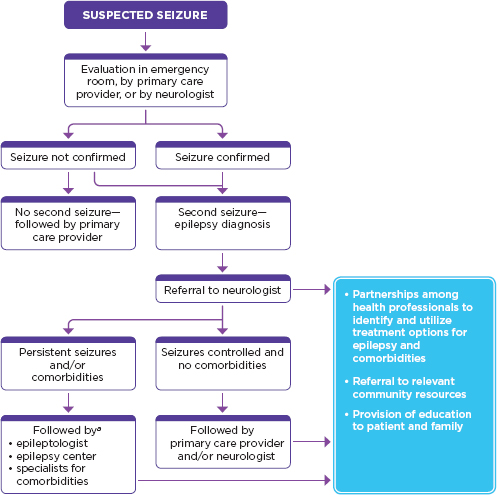
FIGURE 4-3
Treatment pathway for individuals with epilepsy.
aWhen seizures become controlled, the patient can receive ongoing care from a primary care provider or neurologist, with care provided for comorbid health conditions as needed by specialists or primary care providers.
Figure 4-3 illustrates the committee’s view of the potential decision points for referrals to various providers and emphasizes that strong connections are needed with community resources throughout. In brief, the figure follows practice guidelines stipulating that epilepsy care for patients who are diagnosed and have seizures that are easily controlled with medical therapy may continue treatment with a general neurologist or primary care provider (Labiner et al., 2010). When the diagnosis is in question or when seizure control is not achieved, then the patient should be referred to an epilepsy specialist or center (Cross et al., 2006; Labiner et al., 2010).
Clearly delineated professional roles and responsibilities could increase the efficiency of care. A survey of epileptologists and neurologists found perceptions of overlapping roles and responsibilities and that territorial issues and financial considerations can, in some cases, influence referral decisions (Hayes et al., 2007). The survey also noted recommendations that an interdisciplinary guideline for clinical practice of epilepsy care—a continuum-of-care map—be developed. Enhancing the possibility of successful implementation of a clear and concise clinical pathway for epilepsy care would require the efforts of professional associations and organizations across the relevant primary care professions in addition to neurology, mental health, and epilepsy-specific professional associations.
Because epilepsy is a spectrum of disorders that ranges broadly in severity, the care needs of individuals vary from the time of initial diagnosis to long-term management and from one individual to another. Clear clinical pathways should be laid out for people with epilepsy so that they are aware of their options, informed about available specialist care, and understand when to talk with the health care team about moving to another level of care. Another purpose in establishing clinical pathways is to move toward consistent protocols and accountability within and across institutions. Quality metrics that emphasize timely referrals and co-management will make important progress toward this goal.
Promote a Patient-Centered and Collaborative Approach to the Care of Epilepsy and Comorbid Health Conditions
The committee emphasizes the need for a patient-centered, collaborative, and comprehensive approach to epilepsy care. Historically, the medical model of health care has centered on physicians and hospitals and the policies and systems needed to support their proper functioning. Outcomes of care were (and still are in many cases) measured in numbers of outpatient visits, procedures performed, and hospitalizations, with limited reporting of patient outcomes. The focus of care was on the disease or disorder. By contrast, while patient-centered care still requires strong health systems and the active engagement of physicians, nurses, and an array of other health professionals, in this model the patient and family are the focus, not the disease. In patient-centered care, shared models of decision making are made possible through effective communication between patients and providers and through respect for each individual’s strengths, expertise, and experiences. Other dimensions of patient-centered care include respect for the patient’s experiences, values, preferences, and needs; involvement in decision making; and coordination of care (Gerteis et al., 1993). From a patient-centered perspective, the ideal goal for quality care is “providing the care that the patient needs in the manner the patient desires at the
time the patient desires” (Davis et al., 2005). The epilepsy community has measures to evaluate quality of life, self-efficacy, self-management, and other patient-related outcomes and processes that, if deployed in clinical settings, could improve care. These tools need to be validated (if they have not previously been validated) and more widely used. New tools to assist in patient-centered decision making and choices of care are also needed.
A patient-centered, collaborative approach also would provide comprehensive management for epilepsy comorbidities. In a set of focus groups conducted by the AES (Personal communication, C. A. Tubby, AES, 2011), epileptologists and other professionals in epilepsy care stated that managing comorbidities is a major challenge in their professional practice and one in which they wished they had more training. The current organization of health care and reimbursement systems can create barriers to collaborative management across various types of specialists or between primary and specialty care. While managed care plans may offer a more systematic way of caring for people with chronic and multiple conditions than traditional fee-for-services approaches, individuals with refractory epilepsy or comorbid conditions who require specialized evaluation and treatment may find it difficult to gain access to appropriate care. Organized health care delivery models (e.g., integrated delivery systems, medical or health homes, accountable care organizations) promoted under health reform—the ACA (P.L. 111-148)—may provide and incentivize coordinated, high-quality, and more efficient care to people with complicated chronic conditions (McCarthy, 2011; Takach, 2011). Partnerships with organizations, such as the Association of Maternal and Child Health Programs and the Association of University Centers on Disabilities, that work across disease-specific lines and focus on the whole patient’s needs will be important to further improving the quality of care for people with epilepsy.
An ongoing initiative to improve access to quality epilepsy care is focused on children and youth with epilepsy in medically underserved and rural areas (HRSA, 2011). Project Awareness and Access to Care for Children and Youth with Epilepsy (Project Access) was started in 2003 by the federal Health Resources and Services Administration’s (HRSA’s) Maternal and Child Health Bureau and the Epilepsy Foundation. The project is now in its third phase and is anticipated to continue through 2013. As part of the HRSA initiative, statewide demonstration projects in 17 states have established partnerships among health care providers and community service providers, including schools and nonprofit organizations (HRSA, 2012a). One of the grant requirements has been participation by an interdisciplinary and interagency team in a Learning Collaborative, based on the Institute for Healthcare Improvement’s Breakthrough Series for quality improvement (IHI, 2003). Best practices from the learning collaborative and the state grants are posted on the Project Access website (Box 4-3) (Epilepsy Founda-
Box 4-3 EXAMPLES OF LESSONS LEARNED AND TOOLS DEVELOPED FROM THE LEARNING COLLABORATIVES
University of Southern California’s Learning Collaborative
Strategies for improving care identified during the course of the Learning Collaborative include the following:
• Provide quarterly training to primary care providers.
• Enter into a service agreement with ambulatory clinics and large community pediatric practice groups to outline referral criteria and communications methods.
• Hire a pediatric nurse practitioner to oversee follow-up appointments and assist neurologists.
• Hire a part-time health educator to work with families.
• Work with a social worker to support families in accessing community services.
• Extend visit intervals based on patient needs, not on a standard return policy.
• Schedule return appointment prior to the patient or family’s departure from the clinic.
• Track referrals from primary care to specialty care and provide follow-up to families.
The following tools were developed from the work of many states participating in Project Access and the Epilepsy Learning Collaborative to assist patients, families, and health care providers:
• Parent Notebook: Binder with information (some of which would be completed by the parents, such as medical history template, seizure log, provider list, and notes on visits with health care providers). Other information, such as the resource lists, could be provided by the health care or community services staff.
• Home Medication Sheet: Designed to help parents keep a history of their child’s medications and to reconcile medications with their child’s health care provider during an appointment.
• Seizure Description Tool: Designed to help parents and caregivers describe the child’s seizures; uses simple graphics.
• Seizure Action Plan: Designed to help parents define a consistent plan with their doctor to use when their child has a seizure. This tool could be used by teachers or other family members.
• Resource Guide for Parents: Includes information on community resources, treatment options, federal laws that protect the rights of children with epilepsy in school, first aid for seizures, and finding support, among other resources.
_____________
SOURCE: University of Southern California et al., 2008.
tion, 2011). Because each grant team can choose its project’s priorities and the variables to be assessed, the program has few common metrics to assess progress in improving access to care broadly, which hampers comparisons of results across projects.
Nevertheless, progress on improving the percentage of children with seizure action plans has been noted and a number of tools have been developed and lessons learned about collaborative approaches to epilepsy care (National Initiative for Children’s Healthcare Quality, 2011). Project Access provides the epilepsy community with a starting point for improving access to and coordination of care for individuals with epilepsy. The committee urges wider dissemination of the best practices identified by Project Access grantees and increased opportunities for discussion of their broader implementation.
Collaborative efforts to care for people with epilepsy should benefit from ongoing efforts to improve clinical information systems, particularly EHRs, as noted previously. Another avenue to improve collaborative and patient-centered epilepsy care that deserves more exploration is the use of patient navigators; these individuals—who often are current patients, former patients, or family members and also often are volunteers—have been through the rigors of navigating the health care system and are willing to use their knowledge and additional training to help others. Further, patient navigators can help bridge cultural and language differences that may exist between the health care team and the patient. The patient navigator concept began in the 1990s to provide assistance to people with low incomes who had abnormal findings in cancer screenings as they followed up on medical appointments to have a biopsy (Freeman et al., 1995). Expansion of the patient navigator approach has enabled positive results not only in screening, diagnosis, and treatment adherence, but also in improving quality-of-life outcomes (Robinson-White et al., 2010). While informal navigator programs and family networks currently exist, including support groups, a more systematic approach is desirable and could be explored by epilepsy centers. Medical interpreters also provide another resource to patients that can provide the translation services needed to facilitate discussions and allow more in-depth patient education.
Ensure a Robust, Well-Educated Health Professional Workforce for Epilepsy Care
Waiting times for appointments with epilepsy specialists present another challenge for access to specialized epilepsy care. Limitations in the number and geographic distribution of epileptologists and pediatric neurologists are a major cause of these delays. An International League Against Epilepsy report noted that the geographic “distribution of neurologists is very uneven” in the United States, with the highest concentrations in the Northeast and Midwest, especially in metropolitan areas (Theodore et al., 2006, p. 1708). In a survey of NAEC epilepsy centers, responding centers indicated that the time for a new patient to see an epilepsy specialist aver
aged 32 days, with a median of 21 days (Appendix C). Waiting time for an inpatient evaluation to the center’s epilepsy monitoring unit averaged 25 days, with a median of 21 days.
The AES reports that it has approximately 1,875 physician members, but the number of epileptologists in this group is uncertain (Personal communication, Kathy Hucks, AES, October 17, 2011). A new subspecialty certification for epilepsy by the American Board of Psychiatry and Neurology (discussed in Chapter 5) may allow a more precise determination of the number of U.S. epileptologists and may encourage more neurologists to specialize in epilepsy care. Pediatric neurologists—who care for a range of neurological disorders, including epilepsy—are in particularly short supply. A 2005 survey of child neurologists found there were 904 full-time child neurologists in the United States, or 1.27 per 100,000 children (Polsky et al., 2005).
In addition to increasing the number of physicians trained in epilepsy, increasing the number of nurses, social workers, and other care providers with epilepsy expertise will also improve access to care. Currently, nurses specializing in epilepsy are found primarily at epilepsy centers. This limits the availability of nursing care and epilepsy education for people who do not have access to the centers or who do not require specialized epilepsy care. The use of epilepsy specialist nurses or epilepsy health educators more consistently in epilepsy centers and in community settings could alleviate some pressure on the physician supply and provide a greater depth of resources for people with epilepsy and families. UK studies suggest that nurses can provide the important—although time-consuming—roles of coordinating care for comorbid health conditions and educating patients and families, and the United Kingdom has worked to strengthen its provision of epilepsy care through the work of epilepsy specialist nurses (Box 4-4). In the United States, there is no certification for epilepsy specialist nurses, although many nurses work in epilepsy centers and epilepsy monitoring units. Further efforts to define these roles and explore epilepsy health educator certification (Chapter 7) are needed.
Reach Rural and Underserved Populations
Ensuring that high-quality epilepsy care is available throughout the United States, including rural and underserved areas, is an access goal for epilepsy care in the decades ahead. As is evident in Figure 4-4, epilepsy centers are not available in every state and can be located far from individuals with epilepsy. In addition to geographic challenges, there are also challenges in reaching epilepsy patients who do not have adequate health care coverage.
Improving access to high-quality epilepsy care for underserved popula-
Box 4-4 EPILEPSY SPECIALIST NURSES
The United Kingdom has implemented a systematic approach to the use of epilepsy specialist nurses to remediate documented problems with poor patient education services and gaps in counseling and coordination of care (Kwan et al., 2000). A survey of epilepsy nurse specialists found that they were in diverse practice settings, with many working in nurse-run clinics and the majority in multidisciplinary hospitals or community practices (Goodwin et al., 2004). Common to the practice of most epilepsy specialist nurses was that care was guided primarily by individual patient needs and that they worked to enhance co-management practices between hospitals and primary care providers.
A literature review found that attempts to quantify outcomes of epilepsy nurse specialist care are complicated by the diversity of patients and families encountered, geographical diversity of practice settings, and different scopes of practice (Bradley and Lindsay, 2001). No statistically significant changes in health outcomes were found. However, some studies noted improvements in quality of life, knowledge about epilepsy, communication with health care providers, and satisfaction with care. The impact of epilepsy specialist nursing care on patients’ ability to manage their epilepsy—a major outcome of self-management education and care—was not evaluated by any of the studies examined and requires more review. Opportunities to further explore the potential roles and responsibilities of epilepsy specialist nurses are needed.
tions will involve building stronger links between epilepsy specialists and primary care providers in community health centers and in other local health programs. Accomplishing these efforts can include working with the many local programs that provide health care for underserved populations, including the efforts of Federally Qualified Health Centers and Title V Maternal and Child Health programs at the state and local levels.6 For example, the University of Virginia has developed satellite clinics in rural areas of the state in which a nurse coordinator works with patients to help them access a range of health care and community services. The project is supported in part through Care Connection for Children, an effort that is part of the Title V Children with Special Health Care Needs programs in Virginia (Carter, 2011). In addition, several epileptologists visit satellite clinics in the community each month, and referrals are made to clinics at the University of Virginia, including the epilepsy monitoring unit, for care that cannot be performed in satellite locations.
The increased use of video technologies is opening additional care op-
_______________
6The goal of the Federally Qualified Health Center Program is to “enhance the provision of primary care services in underserved urban and rural communities” (CMS, 2012a). The Title V Maternal and Child Health Services Block Grant Program administered by HRSA provides resources (primarily to state health departments) to support services for underserved women and children (HRSA, 2012b).
tions in rural areas. Telemedicine programs are viable and valuable alternatives to in-person physician visits in rural and geographically isolated areas, as well as for patients for whom travel is difficult (Larner, 2011; Rasmusson and Hartshorn, 2005). Initiatives in teleneurology focus on neurological consultations and interactions among the patient, the community health care provider, and epileptologists or other specialists via video links. Such links also provide opportunities for patient education. A study in Alberta, Canada, found that epilepsy patients’ costs for travel and lost time at work were significantly reduced by using a telemedicine clinic and that 83 percent of telemedicine patients preferred that their next visit also be through telemedicine (Ahmed et al., 2008). Similar outcomes in seizure control and medication adherence were achieved by telemedicine and conventional clinics in a study in southeast Texas (Rasmusson and Hartshorn, 2005). Further, as noted above, some patient and family information needs could be addressed through a 24-hour telephone or Internet epilepsy help line that would serve to provide nonmedical information and direct people to the appropriate resources. A survey of Canadian epileptologists found that obstacles to clinicians’ use of telemedicine included lack of infrastructure support and reimbursement concerns as well as limited clinical examinations (Ahmed et al., 2010).
Internationally, a variety of approaches are being tried to reduce distance barriers. These include nurse-led clinics in Cameroon (Kengne et al., 2008), mobile clinics and training of district medical officers in India, training of village doctors in rural areas of China, and improving the epilepsy expertise of community health workers in Kenya (Scott et al., 2001).
Ongoing technology innovations in recording and transmitting home videos of seizures will continue to provide ways to reduce geographic barriers. More studies are needed to determine cost-effective approaches for the utilization of specialists (epileptologists and neurologists) and primary care providers, including nurse practitioners and physician assistants, in the management of epilepsy, including in rural communities, cultures, and societies. Efforts in conjunction with the Indian Health Service could be explored to learn more about ensuring quality epilepsy care in rural areas. Social workers and case managers can help coordinate these efforts, yet more work is needed to establish effective designs for care management that take into consideration local cultural beliefs and values.
A number of questions remain for the relatively small but growing field of disparities research in epilepsy care. Of critical importance is whether differences in care patterns lead to differences in health, quality of life, and mortality. More information also is needed on the relative importance of various factors associated with disparities, such as individual patient characteristics and behaviors or variations in provider practices and practice settings.
Provide Smooth Transitions in Health Care
Transitions in epilepsy care most often occur as youth move into adult health care and as some older adults with epilepsy move into long-term care. Models and evidence-based evaluation tools (described below) have been developed to promote effective older adult transitions from independent living into nursing homes or other community care options, with more dissemination needed of best practices. Additional efforts are necessary to ensure smooth transitions for young adults.
While epilepsy has not been a primary focus of research on transitional care for older adults, patient-centered transitional services following hospital stays for older adults, including individuals with congestive heart failure, have been shown to reduce readmissions (Naylor et al., 1999; Rich et al., 1995) and hold promise for older adults with epilepsy. A model developed by Coleman and colleagues (2006) found that four domains are critical for successful transitions in care for older adults: a patient record that is owned by the patient to facilitate transfer of information between providers, timely follow-up with primary and specialty care providers, support for medication self-management, and information on “red flags” that indicate the potential for a worsening condition along with instructions on how to respond. In a randomized controlled trial of older patients, Coleman and colleagues (2006) consistently found that older patients who received transition coaching following these four domains had lower rates of rehos-pitalization and lower hospital costs, compared to patients who did not. Advanced practice nurses served as the transition coaches and encouraged effective strategies that included communicating needs, recognizing when a condition was worsening, and knowing how to contact the appropriate physicians.
Transitional models for youth with epilepsy moving from pediatric to adult health care need to be developed. During a time when young adults’ concerns expand to include careers, college, driving, and independence, fragmented transitional care can produce conflicting recommendations, misdiagnoses, and medication errors (Appleton et al., 1997; Smith et al., 2002). Young adults with comorbid health conditions may face many challenges in the transition from pediatric to adult providers (Camfield et al., 2011). Further, many parents of young adults with epilepsy experience anxiety as they relinquish decision making to their children. Although the transitional process should begin in adolescence and give youth increasing levels of responsibilities for independent decision making and self-management, few guidelines or programs are available to assist health professionals or parents. One tool that has been explored is the use of a transfer checklist to help in planning and preparation (Viner, 1999). The timing and readiness for transferring care can be assessed with questionnaires and interviews (Tuffrey and Pearce, 2003).
As discussed below, changes in health policy will facilitate continuity of insurance coverage and the development of new service delivery models that could enable more comprehensive, coordinated, and patient-centered epilepsy care and facilitate transitions across care settings. Efforts are needed to assess the impact of these policy reforms for people with epilepsy broadly and to include successful care transitions for young adults and older adults through evidence-based performance metrics.
Improve Health Insurance Coverage
Advances in medications and therapies offer the promise of improved health and reduced burden of epilepsy. However, as discussed earlier in this chapter, evidence suggests that current health care for people with epilepsy is less optimal for those who have public insurance or no coverage than it is for those with private insurance. Further, the fragmented nature of systems for health care, including mental health care and dental care, often presents people with epilepsy with challenges in navigating the system and paying for care. Rising health care costs threaten the sustainability of public and private health insurance programs, as well as the affordability of health insurance purchased by individuals. Among the efforts to slow the growth in health spending have been numerous payment reforms that have implications for epilepsy care.
Current information is limited on health insurance coverage of people with epilepsy. A recent study of patients who presented at a hospital emergency department in Arizona found similar proportions of non-epilepsy and epilepsy patients who had private insurance and who were uninsured (Ouellette et al., 2011). However, patients with epilepsy were more likely to have public insurance.
The ACA (P.L. 111-148) offers opportunities to address some of the shortfalls of health insurance coverage faced by people with epilepsy. New coverage initiatives under the ACA intend to expand insurance coverage, eliminate lapses in coverage, and improve the organization and delivery of health services. The federal emphasis on health information technology, particularly EHRs, is intended to increase system efficiency and improve quality of care. For epilepsy care, the coverage expansions will eliminate exclusion of preexisting conditions (and have already done so for children and youth under age 19). Temporary federal high-risk insurance pools are available for individuals with preexisting conditions. Individuals who need high-cost care may not be subject to lifetime or annual caps, may not lose their coverage because of their health condition, and will have coverage for essential medical services such as rehabilitative care. Premium assistance to individuals with low or moderate incomes should make it possible for people with epilepsy to access affordable health insurance even if they are
not able to work and are not yet eligible for Medicaid or Medicare. Assistance may also be available to cover high out-of-pocket costs. Medicare patients will be able to receive medically necessary outpatient therapy without limits, and the Medicare prescription drug “doughnut hole” is being eliminated. In addition, coverage of preventive services has expanded with no copays and will potentially benefit from Medicare provider reforms to improve care coordination between primary and specialty care providers in outpatient and inpatient settings. These changes could be particularly relevant to people with refractory epilepsy. The net effects of these changes on the continuity, efficiency, and equity of epilepsy care should be monitored, so that policies can be adjusted to ensure greater value in health care.
IMPROVING VALUE OF HEALTH CARE
Value in health care has been defined as “the physical health and sense of well-being achieved relative to the cost. This means getting the right care at the right time to the right patient for the right price” (IOM, 2009a, p. 95). By this definition, value centers around the patient and depends on results—in terms of both physical and mental functioning and quality of life. Value in health care is a goal that is widely sought but challenging to measure and to achieve, because many stakeholders—patients, health care providers, payers, facilities, and suppliers—all contribute to value with differing views on where improvements are needed. Given the scarcity of resources for health care and the opportunity cost of using resources in one way versus another, value also encompasses the concept of efficiency or achieving the best results with the least expenditure.
The total cost burden of epilepsy encompasses the direct costs of health and social services (e.g., costs related to physician visits, hospital use, seizure medications, counseling, rehabilitation, training) and the indirect costs related to lost productivity, reduced functioning, and early mortality. As noted elsewhere in this report, the majority of the costs of epilepsy are attributable to indirect costs (Begley et al., 2000). The total direct cost of care and the indirect costs of impairment due to epilepsy are beginning to be documented; however, to date there is insufficient information to accurately estimate a comprehensive set of direct costs or to evaluate the cost-effectiveness of specific health care services for epilepsy. This section highlights the data available on the cost of health care for epilepsy and discusses improving the value of epilepsy care by examining the cost and effectiveness of seizure medications.
Cost of Health Care for Epilepsy
The lack of standardized study methods and data sources has led to widely diverging estimates of the overall economic burden of epilepsy
and difficulties in comparing the costs of services across settings of care and treatment approaches. A study published in 2009, based on 9 years of Medical Expenditure Panel Survey (MEPS) data7 from 1996 to 2004, found that the average cost of medical care due to epilepsy was $4,523 per person per year, which was the cost of excess medical expenditures (in 2004 dollars) for people with epilepsy compared to costs for those without the condition (Yoon et al., 2009). This result was higher than reported in some previous research (Begley et al., 2000; Halpern et al., 2000), in part because it took into account total medical expenditure differences, not just those directly attributed to epilepsy. The excess cost estimates were similar for children and adults.
Another U.S. study, conducted using claims data for enrollees in private insurance plans rather than the all-payer data used in MEPS, estimated that the annual excess expenditures for each enrollee with focal onset seizures (identified by the International Classification of Diseases, Ninth Edition coding) were $7,190 (in 2005 dollars) (Ivanova et al., 2010). Total annual direct medical costs per enrollee with focal onset seizures were $11,276, compared to $4,087 for enrollees without epilepsy. Enrollees with focal onset seizures were found to have significantly higher rates of mental health conditions, migraine and other neurological disorders, and other comorbidities compared to other enrollees, which contributed to the difference in total costs. Costs of seizure medications and health services directly attributed to epilepsy or seizures were $3,290 per person and accounted for less than half of the cost differential between enrollees with focal onset seizures and those without epilepsy (Ivanova et al., 2010).
The direct costs associated with managing epilepsy are generally highest following the initial onset of seizures and diagnosis, due to the costs of diagnostic evaluation and initial treatment (Table 4-4) (Begley et al., 2000). Studies have found that direct costs are highest for people with refractory seizures and people with new-onset seizures (Argumosa and Herranz, 2004; Begley et al., 2000; Guerrini et al., 2001). Decreases in service use and the associated costs are seen over time for those whose seizures are controlled with treatment.
In terms of total costs to the health care system, the authors of the MEPS study cited above estimated that the excess health care costs experienced by patients with epilepsy amounted to $9.6 billion a year (in 2004 dollars) (Yoon et al., 2009). An AHRQ Statistical Brief identified approximately 277,000 hospital stays in 2005 in which patients had a principal diagnosis of epilepsy or seizures, generating nearly $1.8 billion in hospital costs alone (Holmquist et al., 2006).
Additional estimates of the overall medical care costs for epilepsy are needed using comprehensive and representative data on health care service
_______________
7See Chapter 2 for a description of the MEPS study and methodology.
TABLE 4-4
Direct Costs of Epilepsy, 1995 Dollars
| Lifetime costa (in thousand $) | % of total cost | Annual costb (in thousand $) | % of total cost | |
| Direct Costs | ||||
| Physician and hospital services | 669,391 | 38.2 | 658,988 | 39.1 |
| Diagnostic procedures | 237,174 | 13.7 | 185,859 | 13.1 |
| Laboratory tests | 140,462 | 8.0 | 126,603 | 7..6 |
| Emergency transportation and other services and procedures | 70,368 | 5.0 | 86,180 | 5.1 |
| Drug treatment | 512,710 | 29.2 | 522,586 | 31.0 |
| Surgery | 123,774 | 7..1 | 106,388 | 6.3 |
| Total | 1,753,879 | 100.0 | 1,686,605 | 100.0 |
aAverage cost of epilepsy care from onset to death of new cases (incident) identified in 1995.
bAverage cost of epilepsy care for 1 year of all cases (prevalent) in 1995.
SOURCE: Adapted from Begley et al., 2000. Reprinted with permission from John Wiley and Sons.
use, including care of comorbidities, as well as social services, to reconcile the different estimates that currently exist (Chapter 2). In addition, estimates are needed of the cost to families of the “informal care” they provide. Too little is currently known about these important markers of the burden of epilepsy on the health care system.
Cost-Effectiveness of Specific Services
One of the areas in health care value that has received considerable attention regarding epilepsy care is the cost and cost-effectiveness of seizure medications. A recent review of 12 studies completed between 2003 and 2007, including 5 cost-minimization analyses and 7 cost-effectiveness studies, found that when used alone (monotherapy), newer seizure medications had similar effectiveness in terms of seizure remission, but were significantly more expensive than older medications (Beghi et al., 2008). At the same time, newer medications may offer the advantages of reduced side effects, particularly when compared with the long-term side effects associated with earlier seizure medications and their potential to cause birth defects (Knoester et al., 2005; Sheehy et al., 2005). The newer drugs also may produce fewer adverse drug interactions. A recent meta-analysis by AHRQ examined the evidence on the effectiveness and safety of newer seizure medications (available since 1993) versus older medications and innova-
tor versus generic seizure medications in patients with epilepsy (AHRQ, 2011). The evaluation of newer versus older antiepileptic medications was predominantly limited to newer seizure medications in comparison with carbamazepine, valproic acid, and phenytoin. The wide variety of seizure types makes it difficult to compare seizure medications. Further studies are needed to examine the balance of cost, efficacy, and adverse side effects of different seizure medications for specific types of epilepsy, patient populations, and various combinations of polytherapy. Studies are also needed on the cost of specific services such as routine EEG monitoring and certain MRI protocols, to assess their value in different populations.
CONCLUSION: DEVELOPING AN EPILEPSY CARE MODEL
As noted throughout this report, epilepsy is a complex disorder that requires the active involvement of the individual with epilepsy, family and friends, and other caregivers; the time and expertise of many health care providers; and the knowledge and skills of varied community services providers. To emphasize the need for a patient-centered and collaborative approach to providing high-quality and efficient care, the committee conceptualized the following model for epilepsy care.
The committee started with the biopsychosocial approach that acknowledges the multidimensional interactions of early life (e.g., genetics, environmental factors), physiologic factors (e.g., seizures, cognitive changes, treatments, adverse events, other neurological problems), and psychosocial factors (e.g., social support, psychological state, life stressors, adaptation) that can have an impact on an individual’s symptoms, behavior, and health outcomes (e.g., seizure control, quality of life, self-management) (Borrell-Carrio et al., 2004; Engel, 1977). This approach emphasizes the dynamic and synergistic relationships that occur in a disorder such as epilepsy and can help guide the approach to care.
Building on the biopsychosocial approach, the committee then explored the Chronic Care Model developed by Wagner and colleagues (Wagner, 1998; Wagner et al., 2001, 2005). This model’s approach to the care of chronic health conditions recognizes that the partnership between a competent clinical team and a patient skilled in self-management is foundational, but to be most effective, the partnership also needs to include family members and community service providers. Three themes emphasized in the development of the Chronic Care Model resonate for epilepsy care:
• Care should be evidence-based with treatments and care approaches based on the best clinical evidence.
• Care should be population-based, with all who need care receiving equitable, timely, and high-quality health care and community services for their epilepsy and other medical conditions.
• Care should be patient-centered, with meaningful interactions among providers and patients and support for self-management skills, to improve health and quality of life (Austin et al., 2000).
The model of epilepsy care developed by the committee (Figure 4-5) illustrates the emphasis placed on an integrated and collaborative approach to health care and community services. The model necessitates that community and health care systems are organized to provide access to and delivery of education and services that support self-management by the person with epilepsy and his or her family. Harmonization among services is essential to achieve high-quality outcomes. Implementing this model of epilepsy care is feasible and should be pursued through various organizational, financial, and payment strategies. Demonstration projects are needed of collaborative approaches to care, such as those currently sought by the CMS Center for Medicare and Medicaid Innovation (CMS, 2012b). The model should be the basis for accreditation, certification, guideline development, performance evaluation activities, and initiatives in epilepsy care.
The patient-clinician encounter takes place in the context of a larger health care system, which, in turn, operates within the context of the broader community. Because the majority of health decisions are made by the individual with epilepsy within the context of his or her family and community, patients must have the education, skills, and tools to manage their epilepsy appropriately day-to-day (Chapter 7). This model recognizes that self-management is a critical element in achieving quality health outcomes. By being patient-focused, self-management approaches promote support by the patient’s network of health care providers and community resources. The patient and family are responsible for setting goals and implementing recommendations from their health care team and community services providers in a way that allows them to receive the care and support that are needed at the right time and in the way they can use it best. In addition, community resources and policies are vital to quality of life (Chapter 6).
The main focus of this model is on the individual with epilepsy and his or her family—not the health care system—with efforts made to identify patient needs, recommend services, remove barriers to treatment, and facilitate care, including co-management of comorbid health problems when appropriate. Collaboration among care team members is critical to ensure that patients’ needs are being met.
To achieve a coordinated and collaborative approach to epilepsy care will involve focused efforts across a range of research and implementation priorities. Throughout this chapter, the committee has provided the basis for the research priorities and recommendations regarding improvements needed in health care for people with epilepsy that are detailed in Chapter 9. Research on new screening and decision-support tools is needed as
are comparative effectiveness studies of epilepsy treatment options and prioritization of those studies. The health services evidence base for epilepsy care needs to be bolstered, including a focus on the workforce and ensuring value in epilepsy care. Actions needed to improve health care for people with epilepsy include accrediting epilepsy centers and establishing a network of centers, developing and implementing a quality care framework and performance measures, and enhancing the screening and referral options and protocols for early identification of epilepsy in high-risk populations, of comorbidities, and of refractory epilepsy.
AANN (American Association of Neuroscience Nurses). 2009. Care of the patient with seizures, second edition. AANN clinical practice uideline series. Glenview, IL: AANN.
AAP (American Academy of Pediatrics) Subcommittee on Febrile Seizures. 2011. Febrile seizures: Guideline for the neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics 127(2):389-394.
Abend, N. S., A. M. Gutierrez-Colina, and D. J. Dlugos. 2010. Medical treatment of pediatric status epilepticus. Seminars in Pediatric Neurology 17(3):169-175.
ACS (American College of Surgeons). 2011. Verified trauma centers. http://www.facs.org/trauma/verified.html (accessed January 5, 2012).
Ahmed, S. N., C. Mann, D. B. Sinclair, A. Heino, B. Iskiw, D. Quigley, and A. Ohinmaa. 2008. Feasibility of epilepsy follow-up care through telemedicine: A pilot study on the patient′s perspective. Epilepsia 49(4):573-585.
Ahmed, S. N., S. Wiebe, C. Mann, and A. Ohinmaa. 2010. Telemedicine and epilepsy care: A Canada wide survey. Canadian Journal of Neurological Sciences 37(6):814-818.
AHRQ (Agency for Healthcare Research and Quality). 2011. Effectiveness and safety of antiepileptic medications in patients with epilepsy. http://www.effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productid=896 (accessed February 14, 2012).
——. 2012. National guideline clearinghouse. http://www.guideline.gov (accessed February 15, 2012).
Alberts, M. J., G. Hademenos, R. E. Latchaw, A. Jagoda, J. R. Marler, M. R. Mayberg, R. D. Starke, H. W. Todd, K. M. Viste, M. Girgus, T. Shephard, M. Emr, P. Shwayder, and M. D. Walker. 2000. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA 283(23):3102-3109.
Alberts, M. J., R. E. Latchaw, W. R. Selman, T. Shephard, M. N. Hadley, L. M. Brass, W. Koroshetz, J. R. Marler, J. Booss, R. D. Zorowitz, J. B. Croft, E. Magnis, D. Mulligan, A. Jagoda, R. O′Connor, C. M. Cawley, J. J. Connors, J. A. Rose-DeRenzy, M. Emr, M. Warren, and M. D. Walker. 2005. Recommendations for comprehensive stroke centers: A consensus statement from the Brain Attack Coalition. Stroke 36(7):1597-1616.
Alper, K., K. A. Schwartz, R. L. Kolts, and A. Khan. 2007. Seizure incidence in psychopharmacological clinical trials: An analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biological Psychiatry 62(4):345-354.
Andermann, F., M. S. Duh, A. Gosselin, and P. E. Paradis. 2007. Compulsory generic switching of antiepileptic drugs: High switchback rates to branded compounds compared with other drug classes. Epilepsia 48(3):464-469.
Andersohn, F., R. Schade, S. N. Willich, and E. Garbe. 2010. Use of antiepileptic drugs in epilepsy and the risk of self-harm or suicidal behavior. Neurology 75(4):335-340.
Andrews, D. J., and W. H. Schonfeld. 1992. Predictive factors for controlling seizures using a behavioural approach. Seizure 1(2):111-116.
Appleton, R. E., D. Chadwick, and A. Sweeney. 1997. Managing the teenager with epilepsy: Paediatric to adult care. Seizure 6(1):27-30.
Argumosa, A., and J. L. Herranz. 2004. Childhood epilepsy: A critical review of cost-of-illness studies. Epileptic Disorders 6(1):31-40.
Austin, B., E. Wagner, M. Hindmarsh, and C. Davis. 2000. Elements of effective chronic care: A model for optimizing outcomes for the chronically ill. Epilepsy and Behavior 1(4):S15-S20.
Austin, J. K., D. A. Carr, and B. P. Hermann. 2006. Living Well. II: A review of progress since 2003. Epilepsy and Behavior 9(3):386-393.
Bale, J. F., Jr., D. A. Caplin, J. D. Bruse, and D. Folland. 2009. Practice parameters in child neurology: Do pediatricians use them? Journal of Child Neurology 24(12):1482-1485.
Barry, J. J., A. B. Ettinger, P. Friel, F. G. Gilliam, C. L. Harden, B. Hermann, A. M. Kanner, R. Caplan, S. Plioplys, J. Salpekar, D. Dunn, J. Austin, and J. Jones. 2008. Consensus statement: The evaluation and treatment of people with epilepsy and affective disorders. Epilepsy and Behavior 13(Suppl. 1):S1-S29.
Bautista, R. E., E. T. Glen, N. K. Shetty, and P. Wludyka. 2009. The association between health literacy and outcomes of care among epilepsy patients. Seizure 18(6):400-404.
Bautista, R. E., C. Graham, and S. Mukardamwala. 2011. Health disparities in medication adherence between African-Americans and Caucasians with epilepsy. Epilepsy and Behavior 22(3):495-498.
Beghi, E., L. Atzeni, and L. Garattini. 2008. Economic analysis of newer antiepileptic drugs. CNS Drugs 22(10):861-875.
Begley, C. E., M. Famulari, J. F. Annegers, D. R. Lairson, T. F. Reynolds, S. Coan, S. Dubinsky, M. E. Newmark, C. Leibson, E. L. So, and W. A. Rocca. 2000. The cost of epilepsy in the United States: An estimate from population-based clinical and survey data. Epilepsia 41(3):342-351.
Begley, C. E., R. Basu, T. Reynolds, D. R. Lairson, S. Dubinsky, M. Newmark, F. Barnwell, A. Hauser, D. Hesdorffer, N. Hernandez, S. C. Karceski, and T. Shih. 2009. Sociodemographic disparities in epilepsy care: Results from the Houston/New York City Health Care Use and Outcomes Study. Epilepsia 50(5):1040-1050.
Begley, C., R. Basu, D. Lairson, T. Reynolds, S. Dubinsky, M. Newmark, F. Barnwell, A. Hauser, and D. Hesdorffer. 2011. Socioeconomic status, health care use, and outcomes: Persistence of disparities over time. Epilepsia 52(5):957-964.
Bell, G. S., and J. W. Sander. 2009. Suicide and epilepsy. Current Opinion in Neurology 22(2):174-178.
Berg, A. T., B. G. Vickrey, J. T. Langfitt, M. R. Sperling, T. S. Walczak, S. Shinnar, C. W. Bazil, S. V. Pacia, and S. S. Spencer. 2003. The multicenter study of epilepsy surgery: Recruitment and selection for surgery. Epilepsia 44(11):1425-1433.
Berg, A. T., B. G. Vickrey, F. M. Testa, S. R. Levy, S. Shinnar, F. DiMario, and S. Smith. 2006. How long does it take for epilepsy to become intractable? A prospective investigation. Annals of Neurology 60(1):73-79.
Birbeck, G. L., J. A. French, E. Perucca, D. M. Simpson, H. Fraimow, J. M. George, J. F. Okulicz, D. B. Clifford, H. Hachad, and R. H. Levy. 2012. Evidence-based guideline: Antiepileptic drug selection for people with HIV/AIDS. Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Ad Hoc Task Force of the Commission on Therapeutic Strategies of the International League Against Epilepsy. Neurology 78:139-145.
Bisgaier, J., and K. V. Rhodes. 2011. Auditing access to specialty care for children with public insurance. New England Journal of Medicine 364(24):2324-2333.
Bokhour, B. G., M. J. Pugh, J. K. Rao, R. Avetisyan, D. R. Berlowitz, and L. E. Kazis. 2009. Improving methods for measuring quality of care: A patient-centered approach in chronic disease. Medical Care Research and Review 66(2):147-166.
Borrell-Carrio, F., A. L. Suchman, and R. M. Epstein. 2004. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Annals of Family Medicine 2(6):576-582.
Bourgeois, B. F. 2002. Reducing overtreatment. Epilepsy Research 52(1):53-60.
Bradley, P., and B. Lindsay. 2001. Specialist epilepsy nurses for treating epilepsy. Cochrane Database of Systematic Reviews 4:CD001907.
Brodie, M. J. 2010. Antiepileptic drug therapy—The story so far. Seizure 19(10):650-655.
Brodie, M. J., A. Richens, and A. W. Yuen. 1995. Double-blind comparison of lamotrigine and carbamazepine in newly diagnosed epilepsy. UK Lamotrigine/Carbamazepine Monotherapy Trial Group. Lancet 345(8948):476-479.
Browne, T. R., and G. L. Holmes. 2001. Epilepsy. New England Journal of Medicine 344(15): 1145-1151.
Brunbech, L., and A. Sabers. 2002. Effect of antiepileptic drugs on cognitive function in individuals with epilepsy: A comparative review of newer versus older agents. Drugs 62(4):593-604.
Buck, D., G. A. Baker, A. Jacoby, D. F. Smith, and D. W. Chadwick. 1997. Patients’ experiences of injury as a result of epilepsy. Epilepsia 38(4):439-444.
Burneo, J. G., L. Black, R. C. Knowlton, E. Faught, R. Morawetz, and R. I. Kuzniecky. 2005. Racial disparities in the use of surgical treatment for intractable temporal lobe epilepsy. Neurology 64(1):50-54.
Burneo, J. G., L. Black, R. Martin, O. Devinsky, S. Pacia, E. Faught, B. Vasquez, R. C. Knowlton, D. Luciano, W. Doyle, S. Najjar, and R. I. Kuzniecky. 2006. Race/ethnicity, sex, and socioeconomic status as predictors of outcome after surgery for temporal lobe epilepsy. Archives of Neurology 63(8):1106-1110.
Camfield, P. R., P. A. Gibson, and L. M. Douglass. 2011. Strategies for transitioning to adult care for youth with Lennox-Gastaut syndrome and related disorders. Epilepsia 52(Suppl. 5):21-27.
Carter, D. 2011. Care coordination: Improving transitions and coordination between health care providers and intersections with community services. PowerPoint presented at the IOM Workshop on Public Health Dimensions of the Epilepsies, June 28. http://iom.edu/~/media/Files/Activity%20Files/Disease/Epilepsy/Panel%203%20Carter.pdf (accessed December 14, 2011).
Cascino, G. D. 2002. Clinical indications and diagnostic yield of video-electroencephalographic monitoring in patients with seizures and spells. Mayo Clinic Proceedings 77(10): 1111-1120.
CFF (Cystic Fibrosis Foundation). 2012a. Patient registry, annual data report 2010. http://www.cff.org/UploadedFiles/LivingWithCF/CareCenterNetwork/PatientRegistry/2010-Patient-Registry-Report.pdf (accessed February 17, 2012).
———. 2012b. Quality improvement initiative. http://www.cff.org/treatments/CareCenterNetwork/QualityImprovementInitiative/ (accessed February 17, 2012).
Chandra, P. S., N. Salamon, J. Huang, J. Y. Wu, S. Koh, H. V. Vinters, and G. W. Mathern. 2006. FDG-PET/MRI coregistration and diffusion-tensor imaging distinguish epileptogenic tubers and cortex in patients with tuberous sclerosis complex: A preliminary report. Epilepsia 47(9):1543-1549.
Chang, F., and Q. Huang. 2011. Noninvasive investigations are essential tools for epilepsy surgery in developing countries: Extrapolating results from Chinese studies. Annals of Indian Academy of Neurology 14(3):225-226.
Chemmanam, T., A. Radhakrishnan, S. P. Sarma, and K. Radhakrishnan. 2009. A prospective study on the cost-effective utilization of long-term inpatient video-EEG monitoring in a developing country. Journal of Clinical Neurophysiology 26(2):123-128.
Chen, D. K., Y. T. So, and R. S. Fisher. 2005. Use of serum prolactin in diagnosing epileptic seizures: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 65(5):668-675.
Choi, H., R. Carlino, G. Heiman, W. A. Hauser, and F. G. Gilliam. 2009. Evaluation of duration of epilepsy prior to temporal lobe epilepsy surgery during the past two decades. Epilepsy Research 86(2-3):224-227.
Chuang, E., M. M. Guerreiro, S. Y. Tsuchie, A. Santucci, C. A. Guerreiro, and M. A. Montenegro. 2007. First, do no harm: The risks of overtreating children with epilepsy. Arquivos de Neuro-Psiquiatria 65(1):1-4.
Ciechanowski, P., E. Wagner, K. Schmaling, S. Schwartz, B. Williams, P. Diehr, J. Kulzer, S. Gray, C. Collier, and J. LoGerfo. 2004. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA 291(13):1569-1577.
Ciechanowski, P., N. Chaytor, J. Miller, R. Fraser, J. Russo, J. Unutzer, and F. Gilliam. 2010. PEARLS depression treatment for individuals with epilepsy: A randomized controlled trial. Epilepsy and Behavior 19(3):225-231.
CMS (Centers for Medicare and Medicaid Services). 2011a. Medicare program; payment policies under the physician fee schedule, five-year review of work relative value units, clinical laboratory fee schedule: Signature on requisition, and other revisions to Part B for CY 2012. Federal Register 76(228):73026-73474.
———. 2011b. Overview EHR incentive program. http://www.cms.gov/ehrincentiveprograms/ (accessed February 14, 2012).
———. 2012a. Federally qualified health center. http://www.cms.gov/mlnproducts/downloads/fqhcfactsheet.pdf (accessed February 22, 2012).
———. 2012b. Center for Medicare and Medicaid Innovation. http://innovations.cms.gov (accessed February 24, 2012).
Cohen-Gadol, A. A., B. G. Wilhelmi, F. Collignon, J. B. White, J. W. Britton, D. M. Cambier, T. J. Christianson, W. R. Marsh, F. B. Meyer, and G. D. Cascino. 2006. Long-term outcome of epilepsy surgery among 399 patients with nonlesional seizure foci including mesial temporal lobe sclerosis. Journal of Neurosurgery 104(4):513-524.
Coleman, E. A., C. Parry, S. Chalmers, and S. J. Min. 2006. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine 166(17): 1822-1828.
Cramer, J. A., K. Perrine, O. Devinsky, L. Bryant-Comstock, K. Meador, and B. Hermann. 1998. Development and cross-cultural translations of a 31-item quality of life in epilepsy inventory. Epilepsia 39(1):81-88.
Cross, J. H., P. Jayakar, D. Nordli, O. Delalande, M. Duchowny, H. G. Wieser, R. Guerrini, and G. W. Mathern. 2006. Proposed criteria for referral and evaluation of children for epilepsy surgery: Recommendations of the Subcommission for Pediatric Epilepsy Surgery. Epilepsia 47(6):952-959.
Dahl, J., L. Melin, and L. Lund. 1987. Effects of a contingent relaxation treatment program on adults with refractory epileptic seizures. Epilepsia 28(2):125-132.
Davis, J., R. Roberts, D. L. Davidson, A. Norman, S. Ogston, J. M. Grimshaw, P. Davey, J. Grant, and D. Ruta. 2004. Implementation strategies for a Scottish national epilepsy guideline in primary care: Results of the Tayside Implementation of Guidelines in Epilepsy Randomized (TIGER) trial. Epilepsia 45(1):28-34.
Davis, K., S. C. Schoenbaum, and A. M. Audet. 2005. A 2020 vision of patient-centered primary care. Journal of General Internal Medicine 20(10):953-957.
Davis, K. L., S. D. Candrilli, and H. M. Edin. 2008. Prevalence and cost of nonadherence with antiepileptic drugs in an adult managed care population. Epilepsia 49(3):446-454.
de Tisi, J., G. S. Bell, J. L. Peacock, A. W. McEvoy, W. F. Harkness, J. W. Sander, and J. S. Duncan. 2011. The long-term outcome of adult epilepsy surgery, patterns of seizure remission, and relapse: A cohort study. Lancet 378(9800):1388-1395.
DeGiorgio, C., S. C. Schachter, A. Handforth, M. Salinsky, J. Thompson, B. Uthman, R. Reed, S. Collins, E. Tecoma, G. L. Morris, B. Vaughn, D. K. Naritoku, T. Henry, D. Labar, R. Gilmartin, D. Labiner, I. Osorio, R. Ristanovic, J. Jones, J. Murphy, G. Ney, J. Wheless, P. Lewis, and C. Heck. 2000. Prospective long-term study of vagus nerve stimulation for the treatment of refractory seizures. Epilepsia 41(9):1195-1200.
DeGiorgio, C., J. Thompson, P. Lewis, S. Arrambide, D. Naritoku, A. Handforth, D. Labar, P. Mullin, and C. Heck. 2001. Vagus nerve stimulation: Analysis of device parameters in 154 patients during the long-term XE5 study. Epilepsia 42(8):1017-1020.
DeGiorgio, C., C. Heck, S. Bunch, J. Britton, P. Green, M. Lancman, J. Murphy, P. Olejniczak, J. Shih, S. Arrambide, and J. Soss. 2005. Vagus nerve stimulation for epilepsy: Randomized comparison of three stimulation paradigms. Neurology 65(2):317-319.
Devinsky, O. 2011. Sudden, unexpected death in epilepsy. New England Journal of Medicine 365(19):1801-1811.
DiIorio, C. K., Y. A. Bamps, A. L. Edwards, C. Escoffery, N. J. Thompson, C. E. Begley, R. Shegog, N. M. Clark, L. Selwa, S. C. Stoll, R. T. Fraser, P. Ciechanowski, E. K. Johnson, R. Kobau, and P. H. Price. 2010. The prevention research centers’ Managing Epilepsy Well Network. Epilepsy and Behavior 19(3):218-224.
Drazkowski, J. 2007. An overview of epilepsy and driving. Epilepsia 48(Suppl. 9):10-12.
Dubois, R. W., and J. S. Graff. 2011. Setting priorities for comparative effectiveness research: From assessing public health benefits to being open with the public. Health Affairs (Millwood) 30(12):2235-2242.
Elger, C. E., and D. Schmidt. 2008. Modern management of epilepsy: A practical approach. Epilepsy and Behavior 12(4):501-539.
Elliott, J. O., B. Lu, B. F. Shneker, J. L. Moore, and J. W. McAuley. 2009. The impact of “social determinants of health” on epilepsy prevalence and reported medication use. Epilepsy Research 84(2-3):135-145.
Elliott, R. E., A. Morsi, O. Tanweer, B. Grobelny, E. Geller, C. Carlson, O. Devinsky, and W. K. Doyle. 2011. Efficacy of vagus nerve stimulation over time: Review of 65 consecutive patients with treatment-resistant epilepsy treated with VNS > 10 years. Epilepsy and Behavior 20(3):478-483.
Engel, G. L. 1977. The need for a new medical model: A challenge for biomedicine. Science 196(4286):129-136.
Engel, J., Jr. 1984. A practical guide for routine EEG studies in epilepsy. Journal of Clinical Neurophysiology 1(2):109-142.
Engel, J., Jr., S. Wiebe, J. French, M. Sperling, P. Williamson, D. Spencer, R. Gumnit, C. Zahn, E. Westbrook, and B. Enos. 2003. Practice parameter: Temporal lobe and localized neocortical resections for epilepsy: Report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology 60(4):538-547.
Englot, D. J., E. F. Chang, and K. I. Auguste. 2011. Efficacy of vagus nerve stimulation for epilepsy by patient age, epilepsy duration, and seizure type. Neurosurgery Clinics of North America 22(4):443-448.
Epilepsy Foundation. 2011. National Center for Project Access. http://www.epilepsyfoundation.org/projectaccess/ (accessed December 14, 2011).
Erbayat Altay, E., A. J. Fessler, M. Gallagher, H. P. Attarian, F. Dehdashti, V. J. Vahle, J. Ojemann, J. L. Dowling, and F. G. Gilliam. 2005. Correlation of severity of FDG-PET hypometabolism and interictal regional delta slowing in temporal lobe epilepsy. Epilepsia 46(4):573-576.
Farhidvash, F., P. Singh, B. Abou-Khalil, and A. Arain. 2009. Patients visiting the emergency room for seizures: Insurance status and clinic follow-up. Seizure 18(9):644-647.
Faught, E., M. S. Duh, J. R. Weiner, A. Guerin, and M. C. Cunnington. 2008. Nonadherence to antiepileptic drugs and increased mortality: Findings from the RANSOM study. Neurology 71(20):1572-1578.
Faught, R. E., J. R. Weiner, A. Guerin, M. C. Cunnington, and M. S. Duh. 2009. Impact of nonadherence to antiepileptic drugs on health care utilization and costs: Findings from the RANSOM study. Epilepsia 50(3):501-509.
Fisher, R. S., B. G. Vickrey, P. Gibson, B. Hermann, P. Penovich, A. Scherer, and S. Walker. 2000a. The impact of epilepsy from the patient’s perspective. I: Descriptions and subjective perceptions. Epilepsy Research 41(1):39-51.
———. 2000b. The impact of epilepsy from the patient’s perspective. II: Views about therapy and health care. Epilepsy Research 41(1):53-61.
Fountain, N. B., P. C. V. Ness, R. Swain-Eng, S. Tonn, and C. T. Bever. 2011. Quality improvement in neurology: AAN epilepsy quality measures. Report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Journal of Neurology 76(1):94-99.
Freeman, H. P., B. J. Muth, and J. F. Kerner. 1995. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Practice 3(1):19-30.
French, J. A., A. M. Kanner, J. Bautista, B. Abou-Khalil, T. Browne, C. L. Harden, W. H. Theodore, C. Bazil, J. Stern, S. C. Schachter, D. Bergen, D. Hirtz, G. D. Montouris, M. Nespeca, B. Gidal, W. J. Marks, Jr., W. R. Turk, J. H. Fischer, B. Bourgeois, A. Wilner, R. E. Faught, Jr., R. C. Sachdeo, A. Beydoun, T. A. Glauser, and Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. 2004a. Efficacy and tolerability of the new antiepileptic drugs. I: Treatment of new onset epilepsy. Neurology 62(8):1252-1260.
———. 2004b. Efficacy and tolerability of the new antiepileptic drugs. II: Treatment of refractory epilepsy. Neurology 62(8):1261-1273.
Friedman, D. E., D. H. Kung, S. Laowattana, J. S. Kass, R. A. Hrachovy, and H. S. Levin. 2009. Identifying depression in epilepsy in a busy clinical setting is enhanced with systematic screening. Seizure 18(6):429-433.
Frost, M., J. Gates, S. L. Helmers, J. W. Wheless, P. Levisohn, C. Tardo, and J. A. Conry. 2001. Vagus nerve stimulation in children with refractory seizures associated with Lennox-Gastaut syndrome. Epilepsia 42(9):1148-1152.
Gaillard, W. D., C. Chiron, J. H. Cross, A. S. Harvey, R. Kuzniecky, L. Hertz-Pannier, L. G. Vezina, and ILAE Committee for Neuroimaging Subcommittee for Pediatric Neuroim-aging. 2009. Guidelines for imaging infants and children with recent-onset epilepsy. Epilepsia 50(9):2147-2153.
GAO (Government Accountability Office). 2011. Medicaid and CHIP: Most physicians serve covered children but have difficulty referring them for specialty care. GAO-11-624. Washington, DC: GAO.
Gerteis, M., S. Edgman-Levitan, J. Daley, and T. L. Delbanco. 1993. Through the patient’s eyes: Understanding and promoting patient-centered care. San Francisco, CA: Jossey-Bass.
Glauser, T., E. Ben-Menachem, B. Bourgeois, A. Cnaan, D. Chadwick, C. Guerreiro, R. Kalviainen, R. Mattson, E. Perucca, and T. Tomson. 2006. ILAE treatment guidelines: Evidence-based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia 47(7):1094-1120.
Goodwin, M., S. Higgins, J. H. Lanfear, S. Lewis, and J. Winterbottom. 2004. The role of the clinical nurse specialist in epilepsy. A national survey. Seizure 13(2):87-94.
Guerrini, R., R. Battini, A. R. Ferrari, P. Veggiotti, D. Besana, G. Gobbi, M. Pezzani, E. Berta, A. Tetto, E. Beghi, M. L. Monticelli, F. Tediosi, L. Garattini, S. Russo, P. Rasmini, A. Amadi, P. Quarti, and R. Fabrizzi. 2001. The costs of childhood epilepsy in Italy: Comparative findings from three health care settings. Epilepsia 42(5):641-646.
Halpern, M., A. Rentz, and M. Murray. 2000. Cost of illness of epilepsy in the U.S.: Comparison of patient-based and population-based estimates. Neuroepidemiology 19(2):87-99.
Halpern, M. T., J. M. Renaud, and B. G. Vickrey. 2011. Impact of insurance status on access to care and out-of-pocket costs for U.S. individuals with epilepsy. Epilepsy and Behavior 22(3):483-489.
Hamiwka, L. D., N. Singh, J. Niosi, and E. C. Wirrell. 2007. Diagnostic inaccuracy in children referred with “first seizure”: Role for a first seizure clinic. Epilepsia 48(6):1062-1066.
Handforth, A., C. M. DeGiorgio, S. C. Schachter, B. M. Uthman, D. K. Naritoku, E. S. Tecoma, T. R. Henry, S. D. Collins, B. V. Vaughn, R. C. Gilmartin, D. R. Labar, G. L. Morris, 3rd, M. C. Salinsky, I. Osorio, R. K. Ristanovic, D. M. Labiner, J. C. Jones, J. V. Murphy, G. C. Ney, and J. W. Wheless. 1998. Vagus nerve stimulation therapy for partial-onset seizures: A randomized active-control trial. Neurology 51(1):48-55.
Haneef, Z., J. Stern, S. Dewar, and J. Engel, Jr. 2010. Referral pattern for epilepsy surgery after evidence-based recommendations: A retrospective study. Neurology 75(8):699-704.
Harden, C. L., J. S. Huff, T. H. Schwartz, R. M. Dubinsky, R. D. Zimmerman, S. Weinstein, J. C. Foltin, W. H. Theodore, and the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. 2007. Reassessment: Neuroimaging in the emergency patient presenting with seizure (an evidence-based review). Neurology 69(18):1772-1780.
Harden, C. L., J. Hopp, T. Y. Ting, P. B. Pennell, J. A. French, W. Allen Hauser, S. Wiebe, G. S. Gronseth, D. Thurman, K. J. Meador, B. S. Koppel, P. W. Kaplan, J. N. Robinson, B. Gidal, C. A. Hovinga, A. N. Wilner, B. Vazquez, L. Holmes, A. Krumholz, R. Finnell, C. Le Guen, the American Academy of Neurology, and the American Epilepsy Society. 2009a. Management issues for women with epilepsy-focus on pregnancy (an evidence-based review): I. Obstetrical complications and change in seizure frequency. Epilepsia 50(5):1229-1236.
Harden, C. L., K. J. Meador, P. B. Pennell, W. A. Hauser, G. S. Gronseth, J. A. French, S. Wiebe, D. Thurman, B. S. Koppel, P. W. Kaplan, J. N. Robinson, J. Hopp, T. Y. Ting, B. Gidal, C. A. Hovinga, A. N. Wilner, B. Vazquez, L. Holmes, A. Krumholz, R. Finnell, D. Hirtz, C. Le Guen, the American Academy of Neurology, and the American Epilepsy Society. 2009b. Management issues for women with epilepsy—Focus on pregnancy (an evidence-based review): II. Teratogenesis and perinatal outcomes. Epilepsia 50(5):1237-1246.
Harden, C. L., P. B. Pennell, B. S. Koppel, C. A. Hovinga, B. Gidal, K. J. Meador, J. Hopp, T. Y. Ting, W. A. Hauser, D. Thurman, P. W. Kaplan, J. N. Robinson, J. A. French, S. Wiebe, A. N. Wilner, B. Vazquez, L. Holmes, A. Krumholz, R. Finnell, P. O. Shafer, C. L. Le Guen, the American Academy of Neurology, and the American Epilepsy Society. 2009c. Management issues for women with epilepsy—Focus on pregnancy (an evidence-based review): III. Vitamin K, folic acid, blood levels, and breast-feeding. Epilepsia 50(5):1247-1255.
Hayes, S. M., J. D. Melin, M. Dupuis, S. Murray, and D. M. Labiner. 2007. Assessing the true learning needs of health care professionals in epilepsy care. Epilepsy and Behavior 11(3):434-441.
Helmers, S. L., M. S. Duh, A. Guerin, S. P. Sarda, T. M. Samuelson, M. T. Bunker, B. D. Olin, S. D. Jackson, and E. Faught. 2011. Clinical and economic impact of vagus nerve stimulation therapy in patients with drug-resistant epilepsy. Epilepsy and Behavior 22(2):370-375.
HHS (Department of Health and Human Services), Federal Coordinating Council for Comparative Effectiveness Research. 2009. Report to the President and the Congress. http://www.hhs.gov/recovery/programs/cer/cerannualrpt.pdf (accessed February 14, 2012).
Hirsch, L. J., E. J. Donner, E. L. So, M. Jacobs, L. Nashef, J. L. Noebels, and J. R. Buchhalter. 2011. Abbreviated report of the NIH/NINDS Workshop on Sudden Unexpected Death in Epilepsy. Neurology 76(22):1932-1938.
Holmquist, L., C. A. Russo, and A. Elixhauser. 2006. Hospitalizations for epilepsy and convulsions, 2005: Statistical brief 46. Rockville, MD: AHRQ.
Hovinga, C. A., M. R. Asato, R. Manjunath, J. W. Wheless, S. J. Phelps, R. D. Sheth, J. E. Pina-Garza, W. M. Zingaro, and L. S. Haskins. 2008. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: Survey of patients with epilepsy and physicians. Epilepsy and Behavior 13(2):316-322.
HRSA (Health Resources and Services Administration). 2011. Project Access: Children and youth with epilepsy. http://www.hrsa.gov/communitiesofpractice/AtaGlance/epilepsy.pdf (accessed January 5, 2012).
———. 2012a. Improving care to children and youth with epilepsy. http://www.mchb.hrsa.gov/programs/epilepsy/ (accessed February 15, 2012).
———. 2012b. Title V. Maternal and Child Health Services Block Grant Program. http://mchb.hrsa.gov/programs/titlevgrants/index.html (accessed February 22, 2012).
IHI (Institute for Healthcare Improvement). 2003. The Breakthrough Series: IHI’s collaborative model for achieving breakthrough improvement. http://www.ihi.org/knowledge/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx (accessed December 14, 2011).
IOM (Institute of Medicine). 1990. Medicare: A strategy for quality assurance. Washington, DC: National Academy Press.
———. 1993. Access to health care in America. Washington, DC: National Academy Press.
———. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2006a. Improving the quality of health care for mental and substance-use conditions: Quality chasm series. Washington, DC: The National Academies Press.
———. 2006b. Performance measurement: Accelerating improvement. Washington, DC: The National Academies Press.
———. 2009a. HHS in the 21st century: Charting a new course for a healthier America. Washington, DC: The National Academies Press.
———. 2009b. Initial national priorities for comparative effectiveness research. Washington, DC: The National Academies Press.
———. 2011. Child and adolescent health and health care quality: Measuring what matters. Washington, DC: The National Academies Press.
Ivanova, J. I., H. G. Birnbaum, Y. Kidolezi, Y. Qiu, D. Mallett, and S. Caleo. 2010. Direct and indirect costs associated with epileptic partial onset seizures among the privately insured in the United States. Epilepsia 51(5):838-844.
Jacoby, A., S. Lane, A. Marson, and G. A. Baker. 2011. Relationship of clinical and quality of life trajectories following the onset of seizures: Findings from the UK Mess Study. Epilepsia 52(5):965-974.
Jha, A. K., J. B. Perlin, K. W. Kizer, and R. A. Dudley. 2003. Effect of the transformation of the Veterans Affairs health care system on the quality of care. New England Journal of Medicine 348(22):2218-2227.
Joint Commission. 2011a. Comprehensive stroke center certification. http://www.jointcommission.org/comprehensive_stroke_center_certification/ (accessed December 14, 2011).
———. 2011b. Facts about disease-specific care certification. http://www.jointcommission.org/assets/1/18/Facts_about_Disease_Specific_Care_Certification.pdf (accessed December 14, 2011).
Karolyhazy, K., E. Kovacs, P. Kivovics, P. Fejerdy, and Z. Aranyi. 2003. Dental status and oral health of patients with epilepsy: An epidemiologic study. Epilepsia 44(8):1103-1108.
Keating, N. L., M. B. Landrum, E. B. Lamont, S. R. Bozeman, S. H. Krasnow, L. N. Shulman, J. R. Brown, C. C. Earle, W. K. Oh, M. Rabin, and B. J. McNeil. 2011. Quality of care for older patients with cancer in the Veterans Health Administration versus the private sector: A cohort study. Annals of Internal Medicine 154(11):727-736.
Kelvin, E. A., D. C. Hesdorffer, E. Bagiella, H. Andrews, T. A. Pedley, T. T. Shih, L. Leary, D. J. Thurman, and W. A. Hauser. 2007. Prevalence of self-reported epilepsy in a multiracial and multiethnic community in New York City. Epilepsy Research 77(2-3):141-150.
Kengne, A. P., L. L. Fezeu, P. K. Awah, E. Sobngwi, S. Dongmo, and J. C. Mbanya. 2008. Nurse-led care for epilepsy at primary level in a rural health district in Cameroon. Epilepsia 49(9):1639-1642.
Kesselheim, A. S., M. R. Stedman, E. J. Bubrick, J. J. Gagne, A. S. Misono, J. L. Lee, M. A. Brookhart, J. Avorn, and W. H. Shrank. 2010. Seizure outcomes following the use of generic versus brand-name antiepileptic drugs: A systematic review and meta-analysis. Drugs 70(5):605-621.
Kimia, A. A., A. J. Capraro, D. Hummel, P. Johnston, and M. B. Harper. 2009. Utility of lumbar puncture for first simple febrile seizure among children 6 to 18 months of age. Pediatrics 123(1):6-12.
Kizer, K. W., J. G. Demakis, and J. R. Feussner. 2000. Reinventing VA health care: Systematizing quality improvement and quality innovation. Medical Care 38(6 Suppl. 1):I7-I16.
Knake, S., E. Halgren, H. Shiraishi, K. Hara, H. M. Hamer, P. E. Grant, V. A. Carr, D. Foxe, S. Camposano, E. Busa, T. Witzel, M. S. Hamalainen, S. P. Ahlfors, E. B. Bromfield, P. M. Black, B. F. Bourgeois, A. J. Cole, G. R. Cosgrove, B. A. Dworetzky, J. R. Madsen, P. G. Larsson, D. L. Schomer, E. A. Thiele, A. M. Dale, B. R. Rosen, and S. M. Stufflebeam. 2006. The value of multichannel MEG and EEG in the presurgical evaluation of 70 epilepsy patients. Epilepsy Research 69(1):80-86.
Knoester, P. D., A. J. Boendermaker, A. C. Egberts, Y. A. Hekster, A. Keyser, J. L. Severens, W. O. Renier, and C. L. Deckers. 2005. Cost-effectiveness of add-on lamotrigine therapy in clinical practice. Epilepsy Research 67(3):143-151.
Kobau, R., H. Zahran, D. J. Thurman, M. M. Zack, T. R. Henry, S. C. Schachter, and P. H. Price. 2008. Epilepsy surveillance among adults—19 states, Behavioral Risk Factor Surveillance System, 2005. Morbidity and Mortality Weekly Report Surveillance Summaries 57(6):1-20.
Kossoff, E. H., B. A. Zupec-Kania, P. E. Amark, K. R. Ballaban-Gil, A. G. C. Bergqvist, R. Blackford, J. R. Buchhalter, R. H. Caraballo, H. Cross, M. G. Dahlin, E. J. Donner, J. Klepper, R. S. Jehle, H. D. Kim, Y. M. C. Liu, J. Nation, D. R. Nordli, Jr., H. H. Pfeifer, J. M. Rho, C. E. Stafstrom, E. A. Thiele, Z. Turner, E. C. Wirrell, J. W. Wheless, P. Veggiotti, and E. P. Vining. 2009. Optimal clinical management of children receiving the ketogenic diet: Recommendations of the International Ketogenic Diet Study Group. Epilepsia 50(2):304-317.
Kotani, K., Y. Asai, and Y. Kurozawa. 2007. Mobile-phone movies to help capture physical manifestations. Internal Medicine Journal 46(15):1277-1278.
Kraynack, N. C., and J. T. McBride. 2009. Improving care at cystic fibrosis centers through quality improvement. Seminars in Respiratory and Critical Care Medicine 30(5):547-558.
Krumholz, A., S. Wiebe, G. Gronseth, S. Shinnar, P. Levisohn, T. Ting, J. Hopp, P. Shafer, H. Morris, L. Seiden, G. Barkley, J. French, the Quality Standards Subcommittee of the American Academy of Neurology, and the American Epilepsy Society. 2007. Practice parameter: Evaluating an apparent unprovoked first seizure in adults (an evidence-based review). Neurology 69(21):1996-2007.
Kucukarslan, S., A. L. Reeves, and J. W. McAuley. 2008. Patient-perceived risk associated with epilepsy and its medication treatment. Epilepsy and Behavior 13(3):449-453.
Kwan, I., L. Ridsdale, and D. Robins. 2000. An epilepsy care package: The nurse specialist’s role. Journal of Neuroscience Nursing 32(3):145-152.
Kwan, P., and M. J. Brodie. 2000. Early identification of refractory epilepsy. New England Journal of Medicine 342(5):314-319.
Kwan, P., A. Arzimanoglou, A. T. Berg, M. J. Brodie, W. Allen Hauser, G. Mathern, S. L. Moshe, E. Perucca, S. Wiebe, and J. French. 2010. Definition of drug resistant epilepsy: Consensus proposal by the Ad Hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51(6):1069-1077.
Labiner, D. M., A. I. Bagic, S. T. Herman, N. B. Fountain, T. S. Walczak, and R. J. Gumnit. 2010. Essential services, personnel, and facilities in specialized epilepsy centers: Revised 2010 guidelines. Epilepsia 51(11):2322-2333.
Lambert, M. V., and M. M. Robertson. 1999. Depression in epilepsy: Etiology, phenomenology, and treatment. Epilepsia 40(Suppl. 10):S21-S47.
Langfitt, J. T., and S. Wiebe. 2008. Early surgical treatment for epilepsy. Current Opinion in Neurology 21(2):179-183.
Larner, A. J. 2011. Teleneurology: An overview of current status. Practical Neurology 11(5): 283-288.
Le, S., P. O. Shafer, E. Bartfeld, and R. S. Fisher. 2011. An online diary for tracking epilepsy. Epilepsy and Behavior 22(4):705-709.
Legion, V. 1991. Health education for self-management by people with epilepsy. Journal of Neuroscience Nursing 23(5):300-305.
Legros, B., P. Boon, B. Ceulemans, T. Coppens, K. Geens, H. Hauman, L. Lagae, A. Meurs, L. Mol, M. Ossemann, K. van Rijckevorsel, M. Van Zandijcke, P. Vrielynck, D. Wagemans, and T. Grisar. 2012. Development of an electronic decision tool to support appropriate treatment choice in adult patients with epilepsy: Episcope®. Seizure 21(1):32-39.
Lichtman, J. H., S. B. Jones, E. C. Leifheit-Limson, Y. Wang, and L. B. Goldstein. 2011a. 30-day mortality and readmission after hemorrhagic stroke among Medicare beneficiaries in Joint Commission primary stroke center-certified and noncertified hospitals. Stroke 42(12):3387-3391.
Lichtman, J. H., S. B. Jones, Y. Wang, E. Watanabe, E. Leifheit-Limson, and L. B. Goldstein. 2011b. Outcomes after ischemic stroke for hospitals with and without Joint Commission-certified primary stroke centers. Neurology 76(23):1976-1982.
Loscher, W., and D. Schmidt. 2011. Modern antiepileptic drug development has failed to deliver: Ways out of the current dilemma. Epilepsia 52(4):657-678.
Lundgren, T., J. Dahl, L. Melin, and B. Kies. 2006. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: A randomized controlled trial in South Africa—A pilot study. Epilepsia 47(12):2173-2179.
Lundgren, T., J. Dahl, and S. C. Hayes. 2008a. Evaluation of mediators of change in the treatment of epilepsy with acceptance and commitment therapy. Journal of Behavioral Medicine 31(3):225-235.
Lundgren, T., J. Dahl, N. Yardi, and L. Melin. 2008b. Acceptance and commitment therapy and yoga for drug-refractory epilepsy: A randomized controlled trial. Epilepsy and Behavior 13(1):102-108.
Mantoan, L., and D. M. Kullmann. 2011. Evaluating first seizures in adults in primary care. Practitioner 255(1743):25-28, 22-23.
Marinas, A., E. Elices, A. Gil-Nagel, J. Salas-Puig, J. C. Sanchez, M. Carreno, V. Villanueva, J. Rosendo, J. Porcel, and J. M. Serratosa. 2011. Socio-occupational and employment profile of patients with epilepsy. Epilepsy and Behavior 21(3):223-227.
Marsan, C. A., and L. S. Zivin. 1970. Factors related to the occurrence of typical paroxysmal abnormalities in the EEG records of epileptic patients. Epilepsia 11(4):361-381.
Marson, A. G., Z. A. Kadir, and D. W. Chadwick. 1996. New antiepileptic drugs: A systematic review of their efficacy and tolerability. BMJ 313(7066):1169-1174.
McCarthy, D. 2011. Integrative models and performance. In Health care delivery in the United States. 10th ed., edited by A. R. Kovner, J. R. Knickman, and V. D. Weisfeld. New York: Springer. Pp. 205-231.
McClelland, S., 3rd, H. Guo, and K. S. Okuyemi. 2010. Racial disparities in the surgical management of intractable temporal lobe epilepsy in the United States: A population-based analysis. Archives of Neurology 67(5):577-583.
McNally, K. A., A. L. Paige, G. Varghese, H. Zhang, E. J. Novotny, Jr., S. S. Spencer, I. G. Zubal, and H. Blumenfeld. 2005. Localizing value of ictal-interictal spect analyzed by SPM (ISAS). Epilepsia 46(9):1450-1464.
Meador, K. J. 2002. Neurodevelopmental effects of antiepileptic drugs. Current Neurology and Neuroscience Reports 2(4):373-378.
Meador, K. J., D. W. Loring, P. G. Ray, A. M. Murro, D. W. King, M. E. Nichols, E. M. Deer, and W. T. Goff. 1999. Differential cognitive effects of carbamazepine and gabapentin. Epilepsia 40(9):1279-1285.
Meador, K. J., D. W. Loring, P. G. Ray, A. M. Murro, D. W. King, K. R. Perrine, B. R. Vazquez, and T. Kiolbasa. 2001. Differential cognitive and behavioral effects of carbamazepine and lamotrigine. Neurology 56(9):1177-1182.
Meierkord, H., P. Boon, B. Engelsen, K. Göcke, S. Shorvon, P. Tinuper, and M. Holtkamp. 2006. EFNS guideline on the management of status epilepticus. European Journal of Neurology 13(5):445-450.
Moore, J. L., J. W. McAuley, D. Mott, A. L. Reeves, and B. Bussa. 2000. Referral characteristics of primary care physicians for seizure patients. Epilepsia 41(6):744-748.
Morrell, M. J. 2011. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology 77(13):1295-1304.
Morton, B., A. Richardson, and S. Duncan. 2006. Sudden unexpected death in epilepsy (SUDEP): Don’t ask, don’t tell? Journal of Neurology, Neurosurgery, and Psychiatry 77(2):199-202.
Mula, M., and J. W. Sander. 2007. Negative effects of antiepileptic drugs on mood in patients with epilepsy. Drug Safety 30(7):555-567.
NAEC (National Association of Epilepsy Centers). 2011. Membership directory. http://www.naeclocator.org/locator/default.asp (accessed December 13, 2011).
———. 2012a. Epilepsy centers. http://www.naeclocator.org/locator/resultsall.asp (accessed January 5, 2012).
———. 2012b. Find an epilepsy center. http://naec-epilepsy.org/find.htm (accessed January 18, 2012).
National Initiative for Children’s Healthcare Quality. 2011. Final report: Spread of quality improvement for children and youth with special healthcare needs: An integrated systems strategy for building the Title V infrastructure. Boston, MA: National Initiative for Children’s Healthcare Quality.
Naylor, M. D., D. Brooten, R. Campbell, B. S. Jacobsen, M. D. Mezey, M. V. Pauly, and J. S. Schwartz. 1999. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA 281(7):613-620.
NCQA (National Committee for Quality Assurance). 1999. HEDIS 2000: Narrative: What’s in it and why it matters. Washington, DC: NCQA.
———. 2012. HEDIS and quality compass. http://www.ncqa.org/tabid/187/default.aspx (accessed February 15, 2012).
Nei, M., and R. Bagla. 2007. Seizure-related injury and death. Current Neurology and Neuroscience Reports 7(4):335-341.
NICE (National Institute for Health and Clinical Excellence). 2004. The epilepsies: The diagnosis and management of the epilepsies in adults and children in primary and secondary care. Clinical guideline 20. London, UK: National Institute for Health and Clinical Excellence.
NQF (National Quality Forum). 2011. Measure evaluation criteria. http://www.qualityforum.org/Measuring_Performance/Submitting_Standards/Measure_Evaluation_Criteria.aspx (accessed December 14, 2011).
ODPHP (U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion). 2010. National action plan to improve health literacy. Washington, DC: HHS.
Ouellette, E., J. Chong, K. Drake, and D. M. Labiner. 2011. Emergency department care of seizure patients: Demographic trends in southern Arizona. Epilepsy and Behavior 21(4):382-386.
Parker, R. M., M. S. Wolf, and I. Kirsch. 2008. Preparing for an epidemic of limited health literacy: Weathering the perfect storm. Journal of General Internal Medicine 23(8):1273-1276.
Parko, K. L. 2011. Epilepsy centers of excellence: Department of Veterans Affairs. PowerPoint presented at the IOM Workshop on Public Health Dimensions of the Epilepsies, Washington, DC, June 28. http://iom.edu/~/media/Files/Activity%20Files/Disease/Epilepsy/Panel%201%20Parko.pdf (accessed January 5, 2012).
Payne, N. E., J. H. Cross, J. W. Sander, and S. M. Sisodiya. 2011. The ketogenic and related diets in adolescents and adults: A review. Epilepsia 52(11):1941-1948.
PCORI (Patient-Centered Outcomes Research Institute). 2012. Patient-Centered Outcomes Research Institute. http://www.pcori.org/ (accessed February 22, 2012).
Pellock, J. M., and P. A. Hunt. 1996. A decade of modern epilepsy therapy in institutionalized mentally retarded patients. Epilepsy Research 25(3):263-268.
Perucca, E., and P. Kwan. 2005. Overtreatment in epilepsy: How it occurs and how it can be avoided. CNS Drugs 19(11):897-908.
Perucca, P., D. C. Hesdorffer, and F. G. Gilliam. 2011. Response to first antiepileptic drug trial predicts health outcome in epilepsy. Epilepsia 52(12):2209-2215.
Piontek, F. A., R. Coscia, C. S. Marselle, R. L. Korn, and E. J. Zarling. 2003. Impact of American College of Surgeons verification on trauma outcomes. Journal of Trauma 54(6):1041-1046.
Polsky, D., J. Weiner, J. F. Bale, Jr., S. Ashwal, and M. J. Painter. 2005. Specialty care by child neurologists: A workforce analysis. Neurology 64(6):942-948.
Poukas, V. S., J. R. Pollard, and C. T. Anderson. 2011. Rescue therapies for seizures. Current Neurology and Neuroscience Reports 11(4):418-422.
Prince, J. S., R. Gunderman, B. D. Coley, D. Bulas, K. Holloway, B. Karmazyn, J. S. Meyer, C. Paidas, D. J. Podberesky, J. Ragheb, W. Rodriguez, J. M. Rosenow, and the Expert Panel on Pediatric Imaging. 2009. ACR appropriateness criteria® seizures: Child. Reston, VA: American College of Radiology.
Provenzale, J. M. 2010. Imaging findings of structural causes of epilepsy in children: A guide for the radiologist in the emergency room. Emergency Radiology 17(6):479-486.
Pugh, M. J. V., D. R. Berlowitz, G. Montouris, B. Bokhour, J. A. Cramer, V. Bohm, M. Bollinger, S. Helmers, A. Ettinger, K. J. Meador, N. Fountain, J. Boggs, W. O. Tatum, J. Knoefel, C. Harden, R. H. Mattson, and L. Kazis. 2007. What constitutes high quality of care for adults with epilepsy? Neurology 69(21):2020-2027.
Pugh, M. J., D. R. Berlowitz, J. K. Rao, G. Shapiro, R. Avetisyan, A. Hanchate, K. Jarrett, J. Tabares, and L. E. Kazis. 2011. The quality of care for adults with epilepsy: An initial glimpse using the QUIET measure. BMC Health Services Research 11:1.
Puskarich, C. A., S. Whitman, J. Dell, J. R. Hughes, A. J. Rosen, and B. P. Hermann. 1992. Controlled examination of effects of progressive relaxation training on seizure reduction. Epilepsia 33(4):675-680.
Quon, B. S., and C. H. Goss. 2011. A story of success: Continuous quality improvement in cystic fibrosis care in the USA. Thorax 66(12):1106-1108.
Rasmusson, K. A., and J. C. Hartshorn. 2005. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia 46(5):767-770.
Reeves, M. J., C. Parker, G. C. Fonarow, E. E. Smith, and L. H. Schwamm. 2010. Development of stroke performance measures: Definitions, methods, and current measures. Stroke 41(7):1573-1578.
Reid, A. Y., A. Metcalfe, S. B. Patten, S. Wiebe, S. Macrodimitris, and N. Jetté. 2012. Epilepsy is associated with unmet health care needs compared to the general population despite higher health resource utilization: A Canadian population-based study. Epilepsia 53(2):291-300.
Reuter, D., and D. Brownstein. 2002. Common emergent pediatric neurologic problems. Emergency Medicine Clinics of North America 20(1):155-176.
Rich, M. W., V. Beckham, C. Wittenberg, C. L. Leven, K. E. Freedland, and R. M. Carney. 1995. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. New England Journal of Medicine 333(18):1190-1195.
Richardson, L. P., E. McCauley, D. C. Grossman, C. A. McCarty, J. Richards, J. E. Russo, C. Rockhill, and W. Katon. 2010. Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatrics 126(6):1117-1123.
Riviello, J. J., Jr., S. Ashwal, D. Hirtz, T. Glauser, K. Ballaban-Gil, K. Kelley, L. D. Morton, S. Phillips, E. Sloan, and S. Shinnar. 2006. Practice parameter: Diagnostic assessment of the child with status epilepticus (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 67(9):1542-1550.
Robinson-White, S., B. Conroy, K. H. Slavish, and M. Rosenzweig. 2010. Patient navigation in breast cancer: A systematic review. Cancer Nursing 33(2):127-140.
Rogawski, M. A., and W. Loscher. 2004. The neurobiology of antiepileptic drugs. Nature Reviews: Neuroscience 5(7):553-564.
Ronen, G. M., N. Fayed, and P. L. Rosenbaum. 2011. Outcomes in pediatric neurology: A review of conceptual issues and recommendations. The 2010 Ronnie Mac Keith lecture. Developmental Medicine and Child Neurology 53(4):305-312.
Rossignol, E., A. Lortie, T. Thomas, A. Bouthiller, D. Scavarda, C. Mercier, and L. Carmant. 2009. Vagus nerve stimulation in pediatric epileptic syndromes. Seizure 18(1):34-37.
Rousseau, A., B. Hermann, and S. Whitman. 1985. Effects of progressive relaxation on epilepsy: Analysis of a series of cases. Psychological Reports 57(3 Pt. 2):1203-1212.
Rymer, M. 2011. Performance measures and centers of excellence for the care of stroke patients. PowerPoint presented at the IOM Workshop on Public Health Dimensions of the Epilepsies, Washington, DC, June 28. http://iom.edu/~/media/Files/Activity%20Files/Disease/Epilepsy/Panel%202%20Rymer.pdf (accessed De-cember 14, 2011).
Sackett, D. L., W. M. Rosenberg, J. A. Gray, R. B. Haynes, and W. S. Richardson. 1996. Evidence based medicine: What it is and what it isn’t. BMJ 312(7023):71-72.
Salinsky, M., R. Kanter, and R. M. Dasheiff. 1987. Effectiveness of multiple EEGs in supporting the diagnosis of epilepsy: An operational curve. Epilepsia 28(4):331-334.
Sander, J. W., P. Ryvlin, H. Stefan, D. R. Booth, and J. Bauer. 2010. Generic substitution of antiepileptic drugs. Expert Review of Neurotherapeutics 10(12):1887-1898.
Schmidt, D., C. Elger, and G. L. Holmes. 2002. Pharmacological overtreatment in epilepsy: Mechanisms and management. Epilepsy Research 52(1):3-14.
Scott, R. A., S. D. Lhatoo, and J. W. Sander. 2001. The treatment of epilepsy in developing countries: Where do we go from here? Bulletin of the World Health Organization 79(4):344-351.
Scottish Intercollegiate Guidelines Network. 2003. Diagnosis and management of epilepsy in adults: A national clinical guideline. Edinburgh, UK: Scottish Intercollegiate Guidelines Network.
Shafer, P. O. 1994. Nursing support of epilepsy self-management. Clinical Nursing Practice in Epilepsy 2(1):11-12.
———. 1998. Counseling women with epilepsy. Epilepsia 39(Suppl. 8):S38-S44.
Sheehy, O., J. M. St-Hilaire, G. Bernier, P. Godfroid, and J. J. LeLorier. 2005. Economic evaluation of levetiracetam as an add-on therapy in patients with refractory epilepsy. Pharmacoeconomics 23(5):493-503.
Sillanpää, M., and S. Shinnar. 2010. Long-term mortality in childhood-onset epilepsy. New England Journal of Medicine 363(26):2522-2529.
Smeets, V. M., B. A. van Lierop, J. P. Vanhoutvin, A. P. Aldenkamp, and F. J. Nijhuis. 2007. Epilepsy and employment: Literature review. Epilepsy and Behavior 10(3):354-362.
Smith, P. E., V. Myson, and F. Gibbon. 2002. A teenager epilepsy clinic: Observational study. European Journal of Neurology 9(4):373-376.
Smolowitz, J. L., S. C. Hopkins, T. Perrine, K. E. Eck, L. J. Hirsch, and M. O’Neil Mundinger. 2007. Diagnostic utility of an epilepsy monitoring unit. American Journal of Medical Quality 22(2):117-122.
Snead, K., J. Ackerson, K. Bailey, M. M. Schmitt, A. Madan-Swain, and R. C. Martin. 2004. Taking charge of epilepsy: The development of a structured psychoeducational group intervention for adolescents with epilepsy and their parents. Epilepsy and Behavior 5(4):547-556.
So, E. L., J. Bainbridge, J. R. Buchhalter, J. Donalty, E. J. Donner, A. Finucane, N. M. Graves, L. J. Hirsch, G. D. Montouris, N. R. Temkin, S. Wiebe, and T. L. Sierzant. 2009. Report of the American Epilepsy Society and the Epilepsy Foundation Joint Task Force on Sudden Unexplained Death in Epilepsy. Epilepsia 50(4):917-922.
Sperling, M. R. 2004. The consequences of uncontrolled epilepsy. CNS Spectrums 9(2):98-101.
Sperling, M. R., H. Feldman, J. Kinman, J. D. Liporace, and M. J. O’Connor. 1999. Seizure control and mortality in epilepsy. Annals of Neurology 46(1):45-50.
Sperling, M. R., C. A. Schilling, D. Glosser, J. I. Tracy, and A. A. Asadi-Pooya. 2008. Self-perception of seizure precipitants and their relation to anxiety level, depression, and health locus of control in epilepsy. Seizure 17(4):302-307.
Stephen, L. J., and M. J. Brodie. 2004. Epilepsy guidelines in the real world: The sound of music? Epilepsia 45(1):1-3.
Stockler-Ipsiroglu, S., and B. Plecko. 2009. Metabolic epilepsies: Approaches to a diagnostic challenge. Canadian Journal of Neurological Sciences 36(Suppl. 2):S67-S72.
Takach, M. 2011. Reinventing Medicaid: State innovations to qualify and pay for patient-centered medical homes show promising results. Health Affairs 30(7):1325-1334.
Taylor, R. S., J. W. Sander, R. J. Taylor, and G. A. Baker. 2011. Predictors of health-related quality of life and costs in adults with epilepsy: A systematic review. Epilepsia 52(12):2168-2180.
Thadani, V. M., A. H. Siegel, P. Lewis, A. M. Siegel, K. L. Gilbert, T. M. Darcey, D. W. Roberts, and P. D. Williamson. 2000. SPECT in neocortical epilepsies. Advances in Neurology 84:425-433.
Theodore, W. H., S. S. Spencer, S. Wiebe, J. T. Langfitt, A. Ali, P. O. Shafer, A. T. Berg, and B. G. Vickrey. 2006. Epilepsy in North America: A report prepared under the auspices of the Global Campaign Against Epilepsy, the International Bureau for Epilepsy, the International League Against Epilepsy, and the World Health Organization. Epilepsia 47(10):1700-1722.
Thompson, N. J., E. R. Walker, N. Obolensky, A. Winning, C. Barmon, C. Diiorio, and M. T. Compton. 2010. Distance delivery of mindfulness-based cognitive therapy for depression: Project UPLIFT. Epilepsy and Behavior 19(3):247-254.
Tracy, J. I., V. Dechant, M. R. Sperling, R. Cho, and D. Glosser. 2007. The association of mood with quality of life ratings in epilepsy. Neurology 68(14):1101-1107.
Tuberous Sclerosis Alliance. 2011. TSC clinics. http://www.tsalliance.org/pages.aspx?content=17 (accessed December 14, 2011).
Tuffrey, C., and A. Pearce. 2003. Transition from paediatric to adult medical services for young people with chronic neurological problems. Journal of Neurology, Neurosurgery and Psychiatry 74(8):1011-1013.
University of Southern California, University Center for Excellence in Developmental Disabilities, and Children’s Hospital Los Angeles. 2008. California learning collaborative team: Replicable models, tools and learning collaborative outcomes. http://www.epilepsyfoundation.org/projectaccess/bestpractices/loader.cfm?csModule=security/getfile&PageID=5150 (accessed December 14, 2011).
U.S. Commission for the Control of Epilepsy and Its Consequences. 1978. Plan for nationwide action on epilepsy. Bethesda, MD: U.S. Department of Health, Education and Welfare.
U.S. Preventive Services Task Force. 2011. Screening for osteoporosis: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine 154(5):356-364.
Uthman, B. M., A. M. Reichl, J. C. Dean, S. Eisenschenk, R. Gilmore, S. Reid, S. N. Roper, and B. J. Wilder. 2004. Effectiveness of vagus nerve stimulation in epilepsy patients: A 12-year observation. Neurology 63(6):1124-1126.
VA (Department of Veterans Affairs). 2011a. Epilepsy Centers of Excellence. http://www.epilepsy.va.gov/EPILEPSY/Library/ecoe.pdf (accessed January 12, 2012).
———. 2011b. Epilepsy centers of excellence: Epilepsy regional map. http://www.epilepsy.va.gov/ecoe.asp (accessed January 5, 2012).
Vernon, J. A., A. Trujillo, S. Rosenbaum, and B. DeBuono. 2007. Low health literacy: Implications for national health policy. http://www.gwumc.edu/sphhs/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf (accessed January 5, 2012).
Viner, R. 1999. Transition from paediatric to adult care. Bridging the gaps or passing the buck? Archives of Disease in Childhood 81(3):271-275.
Vining, E. P., E. D. Mellitis, M. M. Dorsen, M. F. Cataldo, S. A. Quaskey, S. P. Spielberg, and J. M. Freeman. 1987. Psychologic and behavioral effects of antiepileptic drugs in children: A double-blind comparison between phenobarbital and valproic acid. Pediatrics 80(2):165-174.
Wagner, E. H. 1998. Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice 1(1):2-4.
Wagner, E. H., B. T. Austin, C. Davis, M. Hindmarsh, J. Schaefer, and A. Bonomi. 2001. Improving chronic illness care: Translating evidence into action. Health Affairs 20(6):64-78.
Wagner, E. H., S. M. Bennett, B. T. Austin, S. M. Greene, J. K. Schaefer, and M. Vonkorff. 2005. Finding common ground: Patient-centeredness and evidence-based chronic illness care. Journal of Alternative and Complementary Medicine 11(Suppl. 1):S7-S15.
Wagner, J. L., G. Smith, P. Ferguson, K. van Bakergem, and S. Hrisko. 2010. Pilot study of an integrated cognitive-behavioral and self-management intervention for youth with epilepsy and caregivers: Coping openly and personally with epilepsy (COPE). Epilepsy and Behavior 18(3):280-285.
Walker, E. R., N. Obolensky, S. Dini, and N. J. Thompson. 2010. Formative and process evaluations of a cognitive-behavioral therapy and mindfulness intervention for people with epilepsy and depression. Epilepsy and Behavior 19(3):239-246.
Wheless, J. W. 2008. History of the ketogenic diet. Epilepsia 49(Suppl. 8):3-5.
Wheless, J. W., E. Castillo, V. Maggio, H. L. Kim, J. I. Breier, P. G. Simos, and A. C. Papanicolaou. 2004. Magnetoencephalography (MEG) and magnetic source imaging (MSI). Neurologist 10(3):138-153.
Wiebe, S., W. T. Blume, J. P. Girvin, and M. Eliasziw. 2001. A randomized, controlled trial of surgery for temporallobe epilepsy. New England Journal of Medicine 345(5):311-318.
Yamada, M., and T. E. Welty. 2011. Generic substitution of antiepileptic drugs: A systematic review of prospective and retrospective studies. Annals of Pharmacotherapy 45(11):1406-1415.
Yoon, D., K. D. Frick, D. A. Carr, and J. K. Austin. 2009. Economic impact of epilepsy in the United States. Epilepsia 50(10):2186-2191.