Federal policy and funding are the greatest levers available to the Health Resources and Services Administration (HRSA) and the Centers for Disease Control and Prevention (CDC) to encourage the integration of primary care and public health on the ground. While the passage of the Patient Protection and Affordable Care Act (ACA) is arguably the most significant health policy event since the creation of Medicare and Medicaid in 1965, other advocacy and legislative efforts have recently been undertaken that create opportunities for primary care and public health to work together. These efforts attest to the momentum that exists for improving the health system, as well as the commitment to incorporating population health goals into health policy.
One of the policy efforts endorsed by the Obama administration is “place-based initiatives.” As explained in a memorandum:
Place-based policies leverage investments by focusing resources in targeted places and drawing on the compounding effect of well-coordinated action. Effective place-based policies can influence how rural and metropolitan areas develop, how well they function as places to live, work, operate a business, preserve heritage, and more. Such policies can also streamline otherwise redundant and disconnected programs. (The White House, 2009, p. 1)
The place-based initiatives policy is based on findings from social epidemiology that place-based factors act as determinants of health, independently of other factors (Poundstone et al., 2004). This policy recognizes that different approaches are needed for different geographic areas and that
leveraging multiple actions with a shared goal has a cumulative effect. It also encourages agencies to cooperate in the development of initiatives and to coordinate funding streams. For example, the Sustainable Communities Regional Planning Grant Program is a collaborative effort of the Department of Housing and Urban Development, the Department of Transportation, and the Environmental Protection Agency to support planning for community improvement and address, among other issues, public and environmental health concerns.
Another effort under way is the Health in All Policies movement. Health in All Policies refers to the consideration of “health, well-being and equity during the development, implementation and evaluation of policies and services” (WHO, 2010, p. 2). It recognizes that policies that affect health often are not “health policies” per se; rather, policies in all sectors of society can affect the health of the population. For example, a study undertaken by the University of North Carolina (Bell and Standish, 2005) showed the positive impact on the dietary habits of surrounding African American communities when political and business decisions were made to relocate and facilitate access to supermarkets. The recent Institute of Medicine (IOM) report For the Public’s Health: Revitalizing Law and Policy to Meet New Challenges (IOM, 2011b, p. 9) recommends that “states and the federal government develop and employ a Health In All Policies (HIAP) approach to consider the health effects—both positive and negative—of major legislation, regulations, and other policies that could potentially have a meaningful impact on the public’s health.”
Linked to the Health in All Policies concept is the health impact assessment, defined by the World Health Organization (WHO) as “a combination of procedures, methods, and tools by which a policy, program, or project may be judged as to its potential effects on the health of a population, and the distribution of those effects within the population” (European Centre for Health Policy, 1999, p. 4). Health impact assessments provide an assessment of the health effects of a policy prior to its implementation. Dannenberg and colleagues (2008) surveyed the use of health impact assessments in the United States and cited 27 examples, including one that examined the socioeconomic effects of an after-school program in Los Angeles; another that examined how a rental voucher program for low-income families in Massachusetts impacted housing affordability, housing stability, and the neighborhood environment; and another that looked at the effects of a community redevelopment project on physical activity. A recent report of the National Research Council (2011) describes the growing popularity of health impact assessments in the United States and proposes a framework for organizing and explaining their necessary elements.
An example of a legislative effort focused on health system improvement is the American Recovery and Reinvestment Act (ARRA) of 2009.
Designed as an economic stimulus bill, ARRA included approximately $150 billion directed at health and health care (Steinbrook, 2009). In addition to $87 billion for Medicaid and $1.1 billion for comparative effectiveness research, a few other programs are worth mentioning. For example, $2 billion was allocated to HRSA for health centers, specifically for construction, equipment, health information technology, and the provision of services; $1 billion was allocated for prevention and wellness, including clinical and community-based prevention activities designed to address chronic diseases; and the National Health Service Corps and other HRSA-supported workforce programs received $500 million.
Also included in ARRA was the Health Information Technology for Economic and Clinical Health (HITECH) Act, designed to improve the way the health care system operates (Blumenthal, 2010) by encouraging the collection and use of patient-level data through electronic health records. Using these data to inform population-level policies is one way in which primary care practices and public health departments can work together around a shared goal. Although many of ARRA’s provisions ended after 2 years, it is important to recognize that even before the ACA became law, there was a movement to invest in and improve the nation’s health system.
The remainder of this chapter examines provisions of the ACA, key policy components that should be incorporated into future legislation to facilitate the integration of primary care and public health, and funding streams that provide levers for achieving integration.
THE PATIENT PROTECTION AND AFFORDABLE CARE ACT
That the ACA touches on virtually every aspect of health policy that has been debated over the last 25 years belies its expeditious and opportunistic origin. As a legislative feat, the ACA stands on its own merit. As an all-encompassing piece of health policy that addresses the potential to institutionalize population health, it is an incomplete blueprint.
In all fairness, the very title of the law speaks to its main aim—to safeguard health insurance coverage “for those that have it” and to make health insurance more affordable and accessible to the 51.5 million nonelderly Americans who are medically uninsured (Carrier et al., 2011). The majority of the act’s provisions deal with health insurance reform and regulations and the structural basis for enabling those who have been crowded out of affordable health insurance to obtain coverage.
Within the building blocks of this reconstruction of Americans’ health care coverage are policy elements covering the health care workforce and its training; innovation in care delivery; health disparities; data mining; and renewed investments in primary care, public health, and prevention. While these provisions were well promulgated, the ACA neither set out to nor
provides a strategy to achieve population health improvement. Similarly, it does not explicitly address the integration of primary care and public health. Instead, it provides a menu of initiatives on which agencies and communities might converge to make gains in improving population health.
The ACA, by being about health insurance reform at its core, suggests that the long-term success of expanded insurance coverage must be accompanied by a set of activities that reset the basis on which health care is considered and rendered. In other words, health insurance deals only with payment of medical costs, whereas population health investments provide an opportunity for containing and maintaining health care costs within an affordable trajectory. The committee believes that within the numerous provisions of the ACA lie the seeds of opportunity to catalyze the integration of primary care and public health and embed population health improvement as an objective in achieving wellness and health for Americans.
Of particular note, the ACA authorizes both HRSA and CDC to launch a number of new programs that on their own merit promise to be noteworthy, but if coordinated and managed collaboratively from their inception could generate significant momentum toward population health improvement at the national, state, and local levels. In its review of HRSA and CDC activities in the ACA, the committee sought to identify provisions with the potential to yield long-lasting change in the integration of primary care and public health. Although other Department of Health and Human Services (HHS) agencies, notably the Centers for Medicare & Medicaid Services (CMS), and other federal departments and agencies have significant roles to play in promulgating a population health perspective, HRSA and CDC have unique roles under health care reform.
Ultimately, the extent to which HRSA and CDC are able to build upon this movement toward population health improvement is as much dependent on how these agencies, and more generally HHS, operate as on how they implement new programs. Leadership in the two agencies will need to reinvent the process and culture for implementing categorical grant programs, meeting congressional mandates, and complying with regulations while spurring the collaboration and cross-cutting accountability that are critical to establishing population health improvement as an operational imperative.
The following subsections highlight what the committee believes are particularly promising opportunities within the ACA. They fall into four categories: community investments and benefits, coverage reforms, health care transformation, and reshaping of the workforce.
Community Investments and Benefits
The ACA makes direct investments in community health transformation and brings new focus to community benefit activities.
Community Transformation Grants
The Community Transformation Grants program,1 established through allocations from the Prevention and Public Health Fund, is a particularly compelling example of a public health-led initiative that could be used to integrate primary care and public health. The program consists of two parts: Community Transformation Grants and a National Network.
Community Transformation Grants have been awarded to 61 state and local government agencies, tribes and territories, and national and community-based organizations (CDC, 2011). The goal of the program is to reduce chronic disease rates, prevent secondary conditions, reduce health disparities, and assist in developing a stronger evidence base for effective prevention programs. These goals are to be met by supporting the implementation, evaluation, and dissemination of community preventive health activities that are grounded in evidence. Implemented by CDC, the program will support up to 75 communities across the country over a 5-year period, with projects increasingly expanding their scope and reach if federal resources allow. Funding is available for capacity building or implementation, and activities must grow out of an area health assessment (HHS, 2011).
Under CDC guidelines, the Community Transformation Grants program gives priority to the prevention and reduction of type 2 diabetes and the control of high blood pressure and cholesterol. Clinical preventive services are embedded in the basic structure of the Community Transformation Grants program, making health care providers a core partner in the types of broad-based coalitions whose involvement is essential to the program. All applicants are expected to focus on tobacco-free living; active living and healthy eating; and increased use of high-impact, quality clinical preventive services. Applicants also may choose to address social and emotional wellness and a healthy and safe physical environment (HHS, 2011).
The National Network is aimed at community-based organizations that are positioned to accelerate the speed with which communities adopt promising approaches to health transformation. Under the award program, network members can carry out this dissemination activity in two ways: first, by disseminating Community Transformation Grants strategies to their partners and affiliates, and second, by supporting and funding subrecipients
_________________
1Patient Protection and Affordable Care Act of 2010 (ACA), Public Law 148, 111th Cong., 2d sess. § 4201 (March 23, 2010).
in the use of Community Transformation Grants strategies to initiate change locally. Support for subrecipients can include helping them create leadership teams and providing technical assistance and guidance.
The Community Transformation Grants program and the National Network share a set of important purposes: to launch multiple interventions whose goal is making fundamental improvements in population health; to lessen the burden on the health care system while achieving its central involvement in the effort; to develop a new approach to the collection and use of public health information in order to bring an immediacy and action orientation to long-standing surveillance practices; and to accelerate the rate at which public health innovations are replicated nationally, regardless of whether the replication sites receive support from the Community Transformation Grants program. In this sense, the Community Transformation Grants program can be viewed as the public health counterpart to the CMS Innovation Center (CMMI) discussed later in this chapter, whose mission is to test and speed the acceleration of health care system transformation. Nowhere in the ACA is this potential parallelism developed more deeply, and it would be advantageous for both HRSA and CDC to be aware of the communities in which the Community Transformation Grants program and CMMI are involved. As community resources for wellness improve through the Community Transformation Grants program, it may be possible to begin to link those resources to CMMI pilots, which must be able to link their patients and physician practices to community resources. Similarly, the Community Transformation Grants sites will be important to HRSA in guiding health centers engaged in efforts to strengthen their clinical preventive service activities, including the development of affiliations with other community resources in such areas as nutrition, exercise, mental health and wellness, and cessation of tobacco use.
Community Health Needs Assessments
One of the most important potential sources of community support created by the ACA may be the community benefit obligations of nonprofit hospitals that seek federal tax exempt status. A critical step HRSA and CDC might take jointly is a national collaboration with hospitals in ensuring that primary care and community health are given priority as hospitals move forward with their mandatory community health needs assessments and development of implementation strategies. Internal Revenue Service (IRS) guidelines in advance of formal regulations were issued in July 2011,2 and the first mandatory reporting period for hospitals will be in 2012.
_________________
2IRS Notice 2011-52 (July 7, 2011).
In brief, section 501(c)(3) of the Internal Revenue Code3 establishes the legal standard for determining whether nonprofit hospitals will be treated as tax exempt for federal income tax purposes. In 1969 the IRS issued Revenue Ruling 69-545,4 which significantly rolled back previous reduced-cost care obligations in favor of a broader community benefit standard. This standard effectively went unenforced for years. In recent years, congressional scrutiny increased, culminating in amendments to the ACA5 spelling out new obligations of all hospitals seeking federal tax exempt status (it is important to know that most state tax codes parallel the federal code). A 2006 Congressional Budget Office (CBO) report valued the total tax exemption at $12.6 billion in 2002 (CBO, 2006).
The ACA amends the Internal Revenue Code by adding new section 501(r), “additional requirements for certain hospitals.”6 The new requirements apply to all facilities licensed as hospitals, as well as organizations recognized by the Treasury Secretary as hospitals.7 In the case of multihospital chains, each separate facility is held independently to the new requirements.8 Hospitals failing to meet their obligations are subject to an excise tax of $50,000 for any taxable year in which they are not in compliance;9 in addition, they will experience the adverse publicity of being found out of compliance.
The amendments impose new standards designed to ensure financial assistance to indigent persons, curb excessive charges for medically indigent patients, bar aggressive collection tactics, and ensure compliance with federal emergency care requirements. Of greatest interest to the committee is the obligation to undertake a community health needs assessment.
The community health needs assessment is a triennial process10 that must commence no later than the taxable year 2 years after the ACA’s enactment. The assessment must be accompanied by an implementation strategy that grows out of the needs assessment and, as discussed below, ongoing reporting on implementation efforts. The process is dynamic, evolving, and action oriented.
The ACA also establishes minimum requirements for the assessment itself. Under the law, an assessment must “take into account input from
_________________
326 USC 501(c)(3).
4Rev. Rul. 69-545, 1969-2 C.B. 117. In the IRS’s words, Revenue Ruling 69-545 “remove[d] the requirements relating to caring for patients without charge or at rates below cost” (Rev. Rul. 69-5454, 1969-2 C.B. 117).
5ACA § 9007 adding IRC § 501(r).
6ACA § 9007 adding IRC § 501(r), 26 U.S.C. § 501(r).
7Internal Revenue Code (IRC) § 501(r)(2).
8IRC § 501(r)(2)(C).S
9IRC § 4959, added by ACA § 9007.
10IRC § 501(r)(3).
persons who represent the broad interests of the community served by the hospital facility” (IRS, 2011, p. 7). It is important to stress that the term used is “community,” not the specific patients served by the hospitals. That is, the statute appears to require that hospitals assess the needs of the entire community covered by their service area, including members of the community who may, for a variety of reasons, receive care elsewhere, or receive no care at all. Furthermore, for a specialty hospital with a large geographic reach (e.g., a children’s hospital or a hospital with a regional shock trauma unit), the needs assessment presumably will need to cover a community that is coextensive with this larger service area.
The development of the community health needs assessment must include individuals with public health expertise, thereby underscoring the obligation of facilities to involve knowledgeable individuals, not merely use public health data. In other words, the law emphasizes an assessment process that, with respect to both content and process, is inclusive of public health practice and expertise. Even the term “community health needs assessment” is drawn from the public health literature (see, e.g., Jordan et al., 1998; Robinson and Elkan, 1996), furthering the connection between hospital obligations and public health practice. While the legislative history refers to hospitals’ ability to use public health information (Rosenbaum and Margulies, 2010), the text itself underscores the inclusive nature of the obligations.
The IRS’s July 2011 notice reinforces these obligations, defining ambiguous terms and calling for an active and inclusive needs assessment process and, more important, an implementation strategy that is responsive to the needs assessment. The results of a needs assessment certainly could be reinvestment of hospital resources in uncompensated inpatient care discounts. But this would be the case only if the needs assessment were not carried out with heightened attention to primary care and community prevention needs. Hospitals now have a reason to focus on these investments as well, given the emergence of a Medicare payment policy that penalizes excessive readmissions and that serves as a model for state Medicaid programs and private payers. Accordingly, it may be possible for HRSA and CDC to engage with community hospitals and national hospital associations in developing approaches to hospital community benefit planning and implementation strategies that can support the types of activities touched on in this report for which sufficient investment funding is lacking. Examples of these activities include the extension of primary care services into nontraditional settings; the formation of collaboratives among community primary care providers and local health departments, with the aim of strengthening primary care; community health promotion activities involving diet, exercise, and injury risk reduction; and other population-level interventions.
Coverage Reforms
When the ACA is fully implemented, it will expand coverage under Medicaid and the Children’s Health Insurance Program (CHIP) to 17 million Americans and reduce the number of uninsured to 23 million (CBO, 2011). Americans with incomes below 133 percent of the poverty level will be eligible for Medicaid coverage (CBO, 2011; The Henry J. Kaiser Family Foundation, 2011).
Medicaid Preventive Services
One of the ACA’s provisions concerns preventive services for Medicaid populations. The ACA effectively creates two groups of eligible beneficiaries: individuals entitled to coverage under pre-ACA state plan standards and those entitled to coverage under the Medicaid eligibility expansion. In the case of traditional beneficiaries, the act clarifies that full coverage of all preventive services specified for privately insured persons is a state option and further incentivizes coverage through an increase in the federal medical assistance rate.11 In the case of newly eligible adults, preventive services, as defined under the law, are a required element of Medicaid “benchmark” coverage, a somewhat different coverage standard from that used for the traditional population.12
In meeting this provision, primary care providers and public health departments can become participating Medicaid providers and furnish preventive services to adult and child populations. In addition, HRSA and CDC might consider collaborating with CMS on the development of joint guidance regarding coverage of preventive services. Such guidance might explain both the required and optional preventive service provisions of the law, as well as federal financing incentives for coverage of such services. The guidance also might describe best practices in making preventive services more accessible to Medicaid beneficiaries through the use of expanded managed care provider networks; out-of-network coverage13 in nontraditional locations such as schools, public housing, workplace sites, and other places; qualification criteria for participating providers; recruitment of providers; measurement of quality performance; and assessment of impact on population health.
The ACA establishes a grant program under which the secretary of HHS will award grants to states that seek to incentivize the use of preventive
_________________
1142 U.S.C. § 1396d(a)(13) and 1396d(b) as amended by ACA § 4106.
1242 U.S.C. § 1396u-7(b), as amended by ACA § 2001.
13Medicaid agencies are free under federal law to add out-of-network coverage for services also covered on an in-network basis. Many agencies take such an approach for certain types of services, such as school health services.
services by Medicaid beneficiaries.14 The aim of the program is not simply increased participation in prevention programs but actual outcomes showing reduced health risks; thus, its purpose is to achieve behavioral change and scalability in other states. Program priorities include smoking cessation, weight loss, lower cholesterol and blood pressure, and avoidance of the onset of diabetes. Because of the serious shortage of Medicaid providers in many communities, HRSA and CDC have a crucial role to play in the implementation of state demonstrations, particularly in outreach to community providers, training and technical support to state Medicaid agencies, active outreach to public health departments and health centers in demonstration states, and collaboration with CMS in the development of outcome standards and scalability criteria.
Community Health Centers
One major challenge to the rapid expansion of health insurance coverage is the need for expanded capacity for primary care delivery (Adashi et al., 2010). In Massachusetts between 2005 and 2009, the number of uninsured individuals dropped from 657,000 to 295,000, and health centers and other safety net providers proved to be valuable assets in meeting the increased demand. Health centers’ service volume increased by 31 percent. The uninsured in these practices fell from 35 percent to 19 percent, but by 2009, health centers were seeing 38 percent of all the uninsured in the state—up from 22 percent in 2005 (Ku et al., 2011).
The ACA and its companion Health Care and Education Reconciliation Act allocate a major infusion of funding to the expansion of health centers.15 This is unquestionably one of the most important opportunities in the ACA to better integrate primary care and public health because of the unique practice characteristics of health centers. The original vision of health centers reflected what later came to be known as community-oriented primary care, that is, an approach to primary care practice that embeds public health principles into daily practice. These principles include needs assessments, prioritization of services based on population health characteristics, comprehensiveness, financial and cultural accessibility, evidence-based practice using tools such as modern health risk assessment approaches, continuous interaction with the community, and measurement of performance against community health goals, in addition to measures of individual patient-oriented clinical quality indicators. These aspirations still can be seen in the overall direction and management of health centers, but
_________________
14ACA § 4108.
15ACA § 5601.
health centers also have been under increasing pressure to improve clinical productivity, particularly in an era of limited resources.
An imperative for HRSA and CDC is to preserve the hybrid qualities of health centers and promote activities and linkages that maintain the health centers’ primary role in clinical preventive services and community engagement. When possible, for example, health centers should be partners in Community Transformation Grants. Similarly, research on the experiences of health centers in the delivery of clinical preventive services is essential to understanding how the delivery of clinical preventive services might be improved for at-risk populations. Of necessity, outreach campaigns to promote clinical preventive services in underserved communities, as well as initiatives aimed at improving the quality of primary care for populations with serious and chronic health conditions, must focus on how to improve the performance of health centers.
Most important perhaps, every effort should be made to forge what often has been an uneasy relationship between health centers and public health departments. Many factors feed into this unease, including the historical roots of health centers as a counter to the segregation in health care that once pervaded a large region of the United States (Geiger, 2002, 2005), the fact that health centers have no direct legal financial accountability to health departments, and the different cultures found in health centers and public health departments. That said, there are instances in which partnerships between health centers and public health departments line up well. Typically, these are situations in which health departments have a declared interest in monitoring and intervening in the clinical care of patients who represent a perceived public health risk. For example, patients who are infected with tuberculosis (TB) can be managed by a primary care physician, but often public health departments are responsible for following up with patient contacts to establish the risk of spread in a given community. The level of public health intervention is likely to be even more pronounced if the patient is immunocompromised, as in the case of HIV-infected individuals, or if the patient has a case of active TB, with a high risk of infecting members of a community. In communities where TB is a significant public health concern, there can be explicit agreements between health centers and health departments regarding mutual notification of TB cases, care coordination, and follow-up. Similar arrangements may be in place for communities with high rates of sexually transmitted diseases.
In addition to areas that have traditionally provided opportunities for working together, such as infectious diseases and emergency preparedness, there are many anecdotal examples of collaboration between health centers and public health departments addressing the broader determinants of health. In California, for example, through the Black Infant Health Program, many health centers and public health departments worked to
address high rates of infant mortality, particularly among African Americans (California Department of Public Health, 2010). Health centers, as a principal provider of prenatal care, work with public health departments to identify patients at risk. Maternal and child health workers are then deployed to provide home visits, make referrals to social service agencies, and promote maternal access to regular prenatal care. Such examples should be systematically identified; examined to determine their key elements; and replicated through collaborative efforts, much like the health disparities collaboratives developed by HRSA a decade ago. The failure of health centers and public health departments to act collaboratively would cost HRSA and CDC one of the greatest local levers for community change because their interests in population health are so aligned.
Health Care Transformation
The ACA contains provisions whose aim is to stimulate new approaches to the organization and operation of health systems in order to improve effectiveness, efficiency, and quality.
The National Prevention, Health Promotion and Public Health Council and the National Prevention Strategy
The National Prevention, Health Promotion and Public Health Council16 provides coordination and leadership at the federal level to address health and efforts centered on disease prevention, wellness promotion, and public health. The council incorporates a broad view of health and accordingly comprises 17 different federal agencies, including HHS; the Departments of Agriculture, Education, Transportation, Labor, and Homeland Security; the Environmental Protection Agency; and others. The council is chaired by the Surgeon General. Its mission is to create a national strategy that identifies attainable goals for improving the health status of Americans and provides clear measures that will help agencies achieve those goals. Released in June 2011, the National Prevention Strategy: America’s Plan for Better Health and Wellness (National Prevention, Health Promotion and Public Heath Council, 2011) promotes collaboration between stakeholders, and includes recommendations on the foundational elements of health (strategic directions) and on specific areas that strongly influence personal and public health (priorities). These strategic directions and priorities are listed in Box 4-1.
The National Prevention, Health Promotion and Public Health Council represents a mechanism through which HRSA and CDC can develop collaborations
_________________
16ACA § 4001.
BOX 4-1
Strategic Directions and Priorities of the
National Prevention Strategy
|
Strategic Directions • Healthy and safe community • Clinical and community preventive • Empowered people • Elimination of health disparities |
Priorities • Tobacco-free living • Preventing drug abuse and excessive • Healthy eating • Active living • Injury-and violence-free living • Reproductive and sexual health • Mental and emotional well-being |
SOURCE: National Prevention, Health Promotion and Public Health Council, 2011.
with each other and other federal agencies to impact the nation’s health. As stated in the National Prevention Strategy, “the Council helps each agency incorporate health considerations into decision making, enhances collaboration on implementing prevention and health promotion initiatives, facilitates sharing of best practices, and, as appropriate, coordinates guidance and funding streams” (National Prevention, Health Promotion and Public Health Council, 2011, p. 8). By maximizing the potential of the council, HRSA and CDC could mount powerful initiatives, especially around the seven priorities. With the help of the Departments of Agriculture and Education, for example, CDC could aggressively target the implementation of healthier lunch options in schools. Likewise, HRSA could work with the Department of Transportation to fund programs that would provide transportation assistance to new mothers.
CMS Innovation Center
The mission of CMMI17 is to test new payment and service delivery models that advance clinical integration, health care quality, and efficiency. CMMI is intensely Medicare focused and therefore closely linked to the delivery of personal health care services. However, a number of community-and population-oriented approaches are being explored, indicating the potential for primary care and public health interaction. One of CMMI’s enumerated areas of focus is “community and population health
_________________
17ACA § 3021.
models” (Center for Medicare and Medicaid Innovation, 2011). Through these models, CMMI can evaluate methods for linking the role of primary care to activities traditionally within the domain of public health, such as population-level behavioral interventions and prevention activities. To the extent that this has not already occurred, HRSA and CDC could engage with CMMI in the identification of community and population health models. In the provisions of the law that focus on CMMI and elsewhere in the ACA, a major thrust of health care reform is attention to dually eligible Medicare and Medicaid beneficiaries. The population dually eligible for these programs has been a special concern for CMS and, to a lesser extent, CMMI, state Medicaid programs, the Medicaid and CHIP Payment and Access Commission (MACPAC), the Medicare Payment Advisory Commission (MedPAC), and Congress. HRSA and CDC could target these dually eligible beneficiaries by developing an initiative aimed at improving their health and health care. In HRSA’s case, health centers represent one of the most important sources of care for these populations, while CDC’s expertise in chronic disease measurement is important as well. Local health departments may have a central role to play in creating the types of practice support environments and tools that are essential to transforming the quality of care available to dual enrollees.
Accountable Care Organizations
The ACA establishes accountable care organizations (ACOs) as a formally defined approach to health care practice as part of the new Medicare Shared Savings Program.18 The ACO model grew out of recommendations by MedPAC (MedPAC, 2009) aimed at introducing practice management techniques that can increase health care quality and efficiency while achieving improved health outcomes across a broad patient population. CMS’s final rule, issued in fall 2011 (CMS, 2011), was revised significantly in response to voluminous comments on the administration’s initial approach to implementation, which included allowing federally qualified health centers (FQHCs) and rural health clinics to participate in ACOs, as well as form independent ACOs. The final rule stipulates that ACOs that meet quality and savings goals can keep a percentage of the savings. This provision is designed to encourage participating providers to redesign their practices innovatively and include a focus on improved health for populations (U.S. National Archives and Records Administration, 2011).
This provision creates the opportunity for a partnership between HRSA and CDC around safety net ACOs and public health departments. HRSA might encourage health centers to create their own ACOs or align with
_________________
18Social Security Act § 1899, added by ACA § 3022.
other ACOs that may be forming in their communities and support collaboration with health departments in these institutions. To the extent that health centers move in this direction, HRSA and CDC might develop collaboration models between health centers acting as and collaborating with other ACOs and public health departments. Such collaboration models might emphasize the role of public health in needs assessment, performance measurement and improvement, health promotion, and patient engagement, all of which are central elements of ACOs.
Patient-Centered Medical Homes and the Community Health Team
Patient-centered medical homes are defined in Section 3502 of the ACA as a mode of care that includes “(a) personal physicians or other primary care providers; (b) whole person orientation; (c) coordinated and integrated care; (d) safe and high-quality care through evidence-informed medicine, appropriate use of health information technology, and continuous quality improvements; (e) expanded access to care; and (f) payment that recognizes added value from additional components of patient-centered care.”19 These “homes” are designed to care for the whole person as a complex system of needs and challenges and provide a continuum of care that encourages healthy living and a healthy lifestyle. Patient-centered medical homes are supported by “community health teams,” a concept that is established and supported by grant funding under the ACA. Section 3502 also authorizes the secretary of HHS to award community health team grants or contracts to eligible entities for the establishment of community-based interdisciplinary, interprofessional teams (health teams), which support primary care providers and receive capitated payments for their services. The model is based on prior work by health care experts who have focused on the task of strengthening the capacity of the primary health care system to address the highest-cost patients (IOM, 2010; Wagner, 2000). This strengthening of capacity is envisioned as not simply upgrading practice but essentially embedding practice in a broader public health model. Entities eligible for grants are state or tribal entities that can demonstrate a plan for long-term financial sustainability and a plan for incorporating prevention initiatives, patient education, and care management resources into the delivery of health care in a highly integrated fashion.20 Teams must be interdisciplinary; the statute contains references to the full range of medical, nursing, nutritional, social work, and mental health professionals. Most important, teams must agree to serve not only Medicare beneficiaries but also Medicaid beneficiaries receiving care through state medical home initiatives.
_________________
19ACA § 3502.
20ACA § 3502.
Numerous challenges arise, all of which create collaboration opportunities for HRSA and CDC working with state and local health departments, health centers, and professional organizations. These challenges involve creating the teams; developing team practice approaches that fulfill all requirements of the law with respect to team composition and the scope, depth, and range of activities, community support services, and performance reporting; and integrating public health and public health work into the team model. Primary care providers must be enlisted, collaborations must be developed, health information technology must be utilized, and practice performance must be measured. The most significant challenge may be developing sustainability models for Medicare and Medicaid that can be translated into private health insurance and across varying population demographics. At the same time, the potential to transform community primary care practice into a model that can better manage the highest-risk populations through partnerships between private professionals and public health departments and safety net providers is great.
Reshaping of the Workforce
In the context of system transformation, the ACA falls short in the area of workforce improvement. Yet while major workforce investments are absent in the law, there are some opportunities for reshaping the workforce that HRSA and CDC, working together, could exploit.
Primary Care Extension Program
The ACA authorizes the Agency for Healthcare Research and Quality (AHRQ) to establish the Primary Care Extension Program (PCEP). This program is modeled after the U.S. Department of Agriculture’s Cooperative Extension Program, which revolutionized farming over the last decade, speeding the translation of research to plow and bringing learning from innovative farms back to universities (Grumbach and Mold, 2009; Vastag, 2004). The PCEP can help speed the transformation of care based on best evidence, whether from research or from innovative practices. PCEP agents will establish relationships with practices, much as pharmaceutical representatives did during the last 50 years, but with a detailing function geared to incorporating evidence-based techniques, preventive medicine, health promotion, chronic disease management, and mental and behavioral health services into primary care practices. The goal is to facilitate adoption of the principles of the patient-centered medical home and population health management. AHRQ funded four existing state-based PCEP programs, three of which are required to help three additional states develop similar PCEP programs (the fourth also needs to be scalable to other states). Thus,
more than 13 states will be involved in PCEP efforts over the next 2 years (AHRQ, 2010). Fully fledged, the PCEP could function through grants received by PCEP State Hubs and Local Primary Care Extension Agencies. The State Hubs could include state health departments, state Medicaid and Medicare program administrators, and the departments of academic institutions that train providers in primary care. In addition to these entities, State Hubs might include such entities as hospital associations, primary care practice-based research networks, and state primary care associations. Local Primary Care Extension Agencies are required to perform a number of tasks under the ACA. These tasks include assisting primary care providers in implementing the principles of the patient-centered medical home model, developing and supporting primary care learning communities to enhance dissemination of best practices and improve the involvement of local providers in research, and developing a plan for financial sustainability after the scheduled reduction of federal funding.
While the PCEP is the domain of AHRQ, HRSA and CDC have many reasons to work with AHRQ to elevate the PCEP to a priority within HHS and seek collaboration with CMMI to fund PCEP models that evidence shows can improve personal and population health. The ACA expressly mentions that the PCEP could help support health centers, rural health clinics, and National Health Service Corps (NHSC) sites. In addition, the PCEP could be a bridge between primary care and public health in every county of the country. Once more mature, the PCEP could “participate in community-based efforts to address the social and broad determinants of health, strengthen the local primary care workforce, and eliminate health disparities.”21 In working with AHRQ, HRSA and CDC could help ensure that the program includes a public health orientation and integrates community health issues into practice-and clinic-based primary care improvement activities. For these mutual reasons, the three agencies could build a case for why HHS should support the program, and could also provide guidance on the development of measures for evaluating the program’s effectiveness in involving public health in clinical practice.
National Health Service Corps
The NHSC,22 whose loan and scholarship recipients constitute a significant proportion of all health professionals in health center practice, has received an important infusion of funding. Given the goals of clinical preventive services, one important area of collaboration between HRSA and CDC might be in prioritizing the recruitment and placement of NHSC
_________________
21ACA § 5405. p. 584.
22ACA § 5207.
resources. NHSC loan and scholarship recipients play a vital role in the staffing of health centers. To the extent that other practice sites are feasible, combining information on designated health professions shortage areas with community public health data on community-wide health risks could guide the selection of placement sites. HRSA and CDC may want to explore linkages between the NHSC and the Epidemic Intelligence Service (EIS), particularly with EIS officers placed in state and local health departments (the EIS is discussed further later in the chapter).
Teaching Health Centers
Although virtually all workforce development provisions of the ACA face the prospect of no implementation funding, one provision that did receive an appropriation under the act is the teaching health centers program.23 A teaching health center is defined as a community-based patient care center that operates a residency program. Teaching health centers expand training in FQHCs and rural health clinics to expose resident physicians to caring for the underserved. The training expansion grants include physicians ($167.3 million), physician assistants ($30.1 million), and advanced practice nurses ($31 million). The program is limited to 5 years of funding and then will expire (HHS, 2010).
Because entities must operate a residency training program to qualify for developmental grants and the special payment programs, the focus of the award itself is on training programs that can demonstrate a strong community basis—formal affiliations and partnerships with entities such as health centers, urban Indian health clinics, and other community health care providers that have strong community roots and can share in the direction and oversight of the program. The teaching health centers program not only awards grants for the development of centers but, more important, provides ongoing training support through a mandatory appropriation that is part of the ACA.
Collaboration between HRSA and CDC might merit particular attention in examining the possibilities for teaching health centers. For example, all teaching health centers might be linked to community transformation activities in communities that receive Community Transformation Grants, discussed earlier. Centers also could benefit from the national educational component of the Community Transformation Grants program in order to learn about models of integration that are working and could be replicated in other communities.
Teaching health centers presumably would be ideal locations for ensuring
_________________
23ACA § 5508, Public Health Act of 1944, Public Law 410, 78th Cong. 2d sess. § 749A (July 1, 1944).
access to the clinical preventive services that must be part of all programs funded by Community Transformation Grants. HRSA and CDC might consider working with the centers on training programs whose aim is to produce competency to work in community health teams, given the emphasis placed on teams under the ACA. Teaching health center programs and residents also might focus on health care for dual enrollees, given the large number of health center sites that undoubtedly will serve high concentrations of low-income Medicare beneficiaries.
In sum, the teaching health centers program offers HRSA and CDC an opportunity to address the shortage of providers trained in a model of primary care that incorporates principles of public health practice and emphasizes the management of populations that are the most difficult to serve and whose clinical challenges may be matched only by their social needs. Exploiting this opportunity may be particularly important given that the funding to support the residency placements is set to expire.
While by no means a complete list of relevant provisions in the ACA, Table 4-1 presents an overview of those provisions the committee believes offer the most promising opportunities for HRSA and CDC to work together to foster the integration of primary care and public health.
|
Affordable Care Act Provision |
HRSA and CDC Opportunities |
|
Community Transformation Grants (ACA §§ 4002 and 4201) The provision authorizes and funds community transformation grants to improve community health activities and outcomes. |
• Given that Community Transformation Grants can be viewed as the public health counterpart to the Centers for Medicare & Medicaid Services (CMS) Innovation Center (CMMI) pilots, HRSA and CDC should be aware of the communities where both of these programs are involved. • As community resources for wellness improve through the Transformation Grant system, it may be possible to encourage state and local health department recipients to develop linkages with primary care providers as a central focus of their program planning. • CDC could also begin to link those resources to CMMI pilots, which must be able to link their patients and physician practices with community resources. |
|
Affordable Care Act Provision |
HRSA and CDC Opportunities |
|
Community Health Needs Assessments (ACA § 9007) The provision amends the Internal Revenue Code by adding new section 501(r), “additional requirements for certain hospitals.” The new requirements apply to all facilities licensed as hospitals and organizations recognized by the Treasury secretary as hospitals and spell out new obligations for all hospitals seeking federal tax exempt status. |
• HRSA and CDC could engage with community hospitals and national hospital associations to develop approaches to hospital community benefit planning, as well as promote approaching jointly the selection of interventions and implementation strategies to address identified problems—for example, the extension of primary care services into nontraditional settings; the formation of collaboratives among community primary care providers and local public health and other agencies; and community health promotion activities involving diet, exercise, and injury risk reduction, as well as other population-level interventions. |
|
Medicaid Preventive Services (ACA §§ 4106 and 2001) (ACA § 4108) The provision gives states the option to improve coverage of clinical preventive services for traditional eligibility groups, as well as Medicaid benchmark coverage for newly eligible persons, redefined to parallel the act’s definition of essential health benefits, which includes coverage for preventive services. It also provides Medicaid incentives for prevention of chronic diseases. |
• Primary care providers and public health departments could become participating Medicaid providers and collaborate in designing programs to furnish preventive services to adult and child populations. • HRSA and CDC could collaborate with CMS on the development of joint guidance regarding coverage of preventive services. Such guidance might explain both the required and optional preventive service provisions of the law, as well as federal financing incentives for coverage of those services. Such guidance also might describe best practices in making preventive services more accessible to Medicaid beneficiaries through the use of expanded managed care provider networks and out-of-network coverage in nontraditional locations such as schools, public housing, and workplace sites; qualification criteria for participating providers; recruitment of providers; measurement of quality performance; and assessment of impact on population health. • HRSA and CDC have a crucial role to play in the implementation of state demonstrations, particularly in outreach to community providers to enlist them as active participants in such demonstrations, training and technical support to state Medicaid agencies, outreach to public health departments and health centers in demonstration states, and collaboration with CMS on the development of outcome standards and scalability criteria. |
|
Affordable Care Act Provision |
HRSA and CDC Opportunities |
|
Community Health Centers (ACA § 5601) The provision expands funding for health centers. |
• An imperative for HRSA is to preserve and strengthen the role of health centers as core safety net providers of clinical care and prevention in the communities they serve. Incentives could be built into funding for these centers to promote activities and linkages with local public health departments and encourage community engagement and partnerships for community-based prevention. • Outreach campaigns to promote clinical preventive services in underserved communities, as well as initiatives aimed at improving the quality of primary care for populations with serious and chronic health conditions, could focus on how to improve the performance of health centers. |
|
National Prevention, Health Promotion and Public Health Council and the National Prevention Strategy (ACA § 4001) The provision creates the National Prevention, Health Promotion and Public Health Council to create a collaborative national strategy to address health in the nation. |
• HRSA and CDC could use the Council as a mechanism for working with other agencies around the integration of primary care and public health. |
|
CMS Innovation Center (CMMI) (ACA § 3021) The provision establishes CMMI to develop, conduct, and evaluate pilots for improving quality, efficiency, and patient health outcomes in both the Medicare and Medicaid programs, with an emphasis on dual enrollees. |
• HRSA and CDC could engage with CMMI in the implementation of its community health innovation program to develop models that would leverage clinical care to achieve a broader impact on population health. • In the CMMI provisions of the ACA and elsewhere in the act, a major thrust of health care reform is attention to dually eligible Medicare/Medicaid beneficiaries. HRSA and CDC could develop an initiative aimed at improving the health and health care of this population. |
|
Affordable Care Act Provision |
HRSA and CDC Opportunities |
|
Accountable Care Organizations (ACOs) (ACA § 3022) The provision authorizes the secretary of the Department of Health and Human Services (HHS) to enter into agreements with ACOs on a shared savings basis to improve the quality of patient care and health outcomes and increase efficiency. |
• HRSA could encourage health centers to form ACOs and link with public health departments in this endeavor. • HRSA and CDC could develop models of collaboration between public health departments and ACOs that include safety net providers. Such models might emphasize the role of public health in needs assessment, performance measurement and improvement, health promotion, and patient engagement, all of which are central elements of ACOs. |
|
Patient-Centered Medical Homes (ACA § 3502) The provision authorizes state Medicaid programs to establish medical homes for Medicaid beneficiaries with chronic health conditions, and authorizes the secretary of HHS to award grants for the establishment of health teams to support primary care. |
• HRSA and CDC could collaborate on further development of the medical home model and its team-based approach to care and encourage the inclusion of local public health departments in that model. • HRSA and CDC could provide technical support to state Medicaid agencies seeking to pursue the medical home model, imparting best practices in the design and development of a medical home that is comprehensive, efficient in care delivery, and patient/family-centered. This support also could be expanded to include the development of performance measurement tools for measuring progress in these areas. • HRSA and CDC could develop a sustainable model for the medical home in Medicare and Medicaid that encourages inclusion of local public health departments, supports multiple population types, and can be translated for private health insurance as well. |
|
Primary Care Extension Program (ACA § 5405) The provision authorizes the Agency for Healthcare Research and Quality (AHRQ) to award competitive grants to states for the establishment of Primary Care Extension Programs to improve the delivery of primary care and community health. |
• HRSA and CDC could work with AHRQ to ensure that Primary Care Extension Programs include a public health orientation and integrate community health issues into practice- and clinic-based primary care improvement activities. • HRSA and CDC, working jointly with AHRQ, could seek collaboration with CMMI to fund Primary Care Extension Program models for which there is evidence for improving personal and population health. |
|
Affordable Care Act Provision |
HRSA and CDC Opportunities |
|
National Health Service Corps (ACA § 5207) The provision expands funding for the National Health Service Corps. |
• HRSA and CDC could collaborate in prioritizing the recruitment and placement of National Health Service Corps resources and developing linkages with existing Epidemic Intelligence Service (EIS) officers placed in state and local health departments. |
|
Teaching Health Centers (ACA § 5508) The provision authorizes and funds the establishment of and ongoing operational support for teaching health centers, which must be community-based. |
• HRSA could work with teaching health centers to adopt the patient-centered medical home curriculum and ensure that any curriculum used to train residents includes strong community and public health components—ideally with residents working on projects that concretely promote primary care-public health integration. • HRSA and CDC could work with the centers on training programs that would be aimed at producing competency to work in community health teams, given the emphasis placed on teams under the ACA. |
NOTE: ACA = Patient Protection and Affordable Care Act.
While the ACA does present some opportunities that can be leveraged to integrate primary care and public health, this was, as noted earlier, not its purpose. This section describes key policy components that should be considered for incorporation into future legislation as a way to foster integration and begin to build an infrastructure that will facilitate the alignment of primary care and public health.
Alignment of Payment and Incentive Structures to Encourage
the Integration of Primary Care and Public Health
Creating momentum for the integration of primary care and public health will require changes in the way both are funded. Current primary care payment systems reward volume rather than value (Robert Wood Johnson Foundation et al., 2009). Fee-for-service payments create little incentive or accountability for individual patient outcomes, much less for monitoring and management of population health outcomes (Roland, 2004). Health care systems in the United States and in other countries that achieve better value in terms of quality and outcomes typically incentivize both measures of value through their payment systems (Roland, 2004). Most often, such payment systems include some form of capitation, frequently as a blend of fee-for-service and per-member-per-month payment
and rewards for measurable reporting of care measures or actual outcomes. In systems or countries that outperform the United States broadly, the capitated or blended payments to primary care providers often represent a larger proportion of total health care spending than is the case in the overall U.S. health care system (Campbell et al., 2007). In these better-performing systems, the rewards or incentives are also sizable and can make up a significant proportion of total revenue. This revenue often translates into increased income, but also reflects increased investment in the capacity of practices to deliver higher-quality care and to focus on the total health of their patient panel (Gulliford et al., 2007).
Funding for public health comes from a mix of federal, state, and local funds. An analysis by the Trust for America’s Health (2011) found wide variability in funding amounts for states and localities, with no overarching strategy for directing funds to address the most pressing health needs. Moreover, most funding for public health is in the form of categorical grants, allowing grantees little flexibility. To promote integration with primary care, funding streams for public health should be flexible enough to encourage grantees to try innovative approaches to improving population health by partnering with primary care. Currently, payment for primary care services and funding for public health services neither align nor facilitate partnering.
While it may appear out of scope or capacity for HRSA or CDC to focus on payment or quality incentives, the two agencies have both an internal and an external role to play. HRSA has supported quality improvement efforts for safety net programs under its purview, for example, and currently hosts voluntary quality improvement technical assistance and accreditation support (HRSA, 2009). In addition, the grants it oversees through Section 330 of the Public Health Service Act24 could be used to promote population health goals in health centers. As a condition for receiving 330 funds, for example, health centers could be asked to demonstrate awareness of the 10 essential public health services (Box 1-2 in Chapter 1), as well as provide access to and coverage for all preventive health services recommended by the U.S. Preventive Services Task Force. Through the National Center for Health Statistics and its ties to public health departments, CDC has an important role in presenting health outcomes and disparities by community. These two capacities could help in identifying areas with poor outcomes and high disparities in the vicinity of primary care safety net services and public health departments, and in developing incentives and support programs, alone and with Medicare and Medicaid, with a focus on joint interventions and ultimately integration. Where poor outcomes and large disparities exist without primary care safety net services, public health departments,
_________________
2442 U.S.C. § 254b.
or both, HRSA and CDC could work with CMS to create incentives for providers to locate in these areas, with strong incentives to create linkages with regional public health entities. In addition, as a condition for receipt of certain funds for state health departments, CDC could ask that they demonstrate awareness of and establish a working relationship with all safety net providers in their state.
Investments That Grow and Reengineer a Workforce
That Can Deliver on Population Outcomes
Orienting the U.S. health system to facilitate the integration of primary care and public health will require the development of a workforce that is capable of transcending the traditional boundaries of the two sectors to foster a collaborative environment. Workforce training initiatives have the potential to teach health professionals about the valuable interactions between personal and population-based health services and encourage relationships across disciplines. Specific training initiatives could include emphasizing team-based training, population health management competencies, epidemiology, and community-based health policy training within profession-specific training; training professionals in the community in practices that model integration and team-based care; training health care specialists to collaborate more closely with patients’ primary care and community care teams; and expanding specialization in community-based epidemiology, geospatial health care analysis, population health management, practice transformation and improvement, and community care integration. A number of funding and policy opportunities already in place could assist in the development of a workforce with the capacity to carry out the principles of integration; however, the purpose of those funding opportunities may require significant changes.
Both HRSA and CDC could contribute to the creation of this workforce through their existing workforce programs. Since passage of the ACA, HRSA has made important investments to expand primary care training in 11 teaching health centers (discussed earlier) (HRSA, 2011) and a 5-year, $228 million expansion of primary care workforce training (HHS, 2010). HRSA also has a long-term stake in medical and nursing workforce pipeline programs covered by Titles VII and VIII of the Public Health Service Act. Title VII funds a number of programs, including predoctoral, residency, and faculty development training grants, as well as physician assistant programs. Title VIII provides similar support for nursing training. The Title VII programs focus on supporting primary care education programs that promote interprofessional education, training to meet the needs of a diverse population, and increased diversity in the workforce (Reynolds, 2008). HRSA also supports the development of the public health workforce
through public health traineeships, public health training centers, and preventive medicine residency programs. In addition to building linkages between these existing HRSA programs, HRSA should consider partnering with CDC around its workforce programs.
The largest of CDC’s workforce programs is the EIS, a 2year postgraduate training program that provides service and on-the-job learning for health professionals interested in the practice of applied epidemiology (CDC, 2012). The program is modeled after a traditional medical residency program, where much of the education occurs through experiential learning. About 75 percent of EIS graduates remain in public health at CDC or in state or local health departments, and many become field leaders around the world (CDC, 2012). While the EIS program currently is focused heavily on infectious diseases, it has the potential to fill an important gap in what is needed to achieve the goal of improving population health. With expansion of its scope and size, the EIS could create a public health workforce that could serve as a bridge between primary care and public health in two key areas: (1) transformation of primary care practice toward the capacity to monitor and manage population health, and (2) public health informatics and the capacity to turn patient and population health data into information that clinicians and public health workers can use to improve health in their communities.
The first of these areas could support the Primary Care Extension Program by helping practices learn how to use information technology to become better personal and population health managers within their practices. This assistance would include demonstrating how the new population health data streams can support clinical decisions at the point of care, as well as teaching health coaches or other practice health care workers how to use the new data streams to better manage and monitor chronically ill patients and coordinate preventive care services. Creating new population health information technology systems will not prepare clinics for using them effectively. An expanded EIS workforce could continue to employ sophisticated physician and nursing EIS agents but also develop a master of public health (MPH) and informatics cadre trained in the use of population health information technology systems at the community level—fulfilling their function for the public health system—and able to train practices in the use of these systems as an outreach from and bridge to public health. Within the public health system, their relationships with practices would help them understand how to connect partnering practices to patients or communities in their service area that were experiencing disparities in health. They could also bring public health resources to bear in determining how to assess and engage failing communities in partnership with practices. Fulfilling these obligations would require additional, specialized training for EIS agents. However, the benefit of expanding the skill set of those participating
in the EIS program is that it would create a bridge between primary care and public health by broadening an existing program.
Another opportunity for HRSA and CDC to play an important role in workforce development is through interdisciplinary primary care and public health training. One means to this end would be to provide leadership to CMS in the development of related regulations for funding of graduate medical education and nurse training. The education advisory committees staffed by HRSA could be instrumental in providing this guidance. Many of the needed new or expanded functions in public and community health may best fall within the purview of CDC, especially those focused on turning personal and public health data into information that can drive interventions and practice improvement. HRSA and CDC should collaborate in reviewing their workforce programs to determine how they could be deployed to promote the production of health care workers who are able to integrate primary care and public health for the betterment of population health.
Support for Population-Level Data
With the right design, important information to guide clinical decision making, public health interventions, and the integration of the two could be at the fingertips of health care providers. The advent of electronic health records may be seminal in introducing a new era of alignment between primary care and public health. HRSA has invested heavily in supporting the adoption of electronic health records among health centers, which in their full implementation will capture data for up to 20 million patients. Many of these health centers already have the means to capture some population health metrics, and a fully developed health information infrastructure at health centers should be capable of capturing information about population characteristics, as well as care management patterns and trends. Of course, health centers are not alone in undertaking the implementation of electronic health records. Through a myriad of initiatives, including “meaningful use” incentives administered by the Office of the National Coordinator, the United States is being ushered into the digital era of health care. Whether the full potential of this enterprise in generating population health improvement will be realized remains to be seen. But undeniably, the elements of success are there: a desire to reinvest in new models of care delivery with primary care at its core; an understanding that health care costs will continue to escalate uncontrollably unless prevention and social determinants are addressed; and the technological means to capture information that can serve the dual goals of improved clinical care and optimized population health, as well as create a link between the two (although it should be noted that the investment in health information technology for public
health has been significantly less than the investment for primary care) (Steinbrook, 2009).
In For the Public’s Health: The Role of Measurement in Action and Accountability (IOM, 2011a, p. 2), the IOM states “that the United States lacks a coherent template for population health information that could be used to understand the health status of Americans and to assess how well the nation’s efforts and investments result in improved population health.” To gauge performance in addressing health disparities and improving population health, well-developed measures are needed at all levels—local, state, and national. Efforts to develop measures, coordinate data collection, analyze outcomes, and translate this information for decision makers are being undertaken in some locations. In the Geisinger system, optimal outcomes were identified and used as the basis for developing short-and long-term metrics. This approach, along with the use of real-time data from electronic health records and insurance claims, has contributed to improved outcomes and cost reductions (Steele et al., 2010). Another example is WellMed, a primary care-based ACO in Texas. The measurement and accountability systems WellMed has implemented have contributed to lowered mortality rates and better outcomes compared with state outcomes for the over-65 population (Phillips et al., 2011).
In contrast to these examples, in which coordination was crucial to success, efforts currently under way by CMS, the National Committee for Quality Assurance, certifying boards, and payers are disjointed. The efforts undertaken by the various stakeholders could be coordinated and structured to become a routine part of patient care.
In addition to coordination, an important element related to metrics is how the collected data are used. Ideally, measures should be used as a feedback loop in the provision of care, giving providers quality measures for their patient panel, and perhaps even as decision support at the point of care. Collected data also can be used to identify groups or communities with poor outcomes that may be small in number or distributed across multiple practices, and therefore not easily recognized by individual practices. Aggregated data can be used to identify these groups so they can be targeted by collaborative outreach, engagement, and improved services.
Shared Community Resources for Primary
Care and Public Health Integration
The most important way to encourage the integration of primary care and public health is to prevent further erosion of either sector. As states seek to reduce health care spending, public health funding is an easy target for program cuts. One way to combat these cuts is to physically unite or collocate public health departments with local health centers. Doing so would
reduce the infrastructure costs of maintaining separate operating resources. Also, communities could find ways to join public health initiatives with primary care practices. For instance, HRSA could recommend the use of public health workers in health centers as community agents responsible for patient education, behavioral and lifestyle modification, and assistance to patient communities in overcoming social determinants that adversely affect community health. These workers could utilize training and tools developed by CDC to achieve these goals, and would be responsible for relaying community health metrics to CDC and state and local health departments for inclusion in local, state, and national data reports. These shared resources, embedded in the community and community relationships, would help provide complex care management; assist with practice transformation, health information technology connectivity, care, and coordination of community services; and assist in monitoring the health of the public. This consolidation also could provide an opportunity for patients to receive all of their personal care and public health services in one stop and lead to improved economies of scale due to shared space, shared resources, and shared staff.
Another opportunity for sharing community resources is around workforce. For example, the Vermont Blueprint for Health employs community care teams as a link between primary care practices and public health services, including community-based chronic disease prevention programs, as well as social and economic support programs. While team composition is determined locally, all teams are led by a nurse, and most consist of behavioral health counselors and social workers (Bielaszka-DuVernay, 2011). Community care teams can be based in primary care practices and assist patients with such tasks as making appointments, completing insurance paperwork, or arranging child care. Thus, these teams ensure that people have comprehensive services to support their health and well-being by connecting the work of primary care practices to community-based preventive and other social services.
Box 4-2 presents some examples in which sharing of community resources to support the integration of primary care and public health is working well.
The shared capacity to use patient and population data is another example of a resource available to promote the integration of primary care and public health. Important efforts are under way at HRSA to share patient data in a safe way (compliant with the Health Insurance Portability and Accountability Act [HIPAA]) and combine them with population data to produce information of value to practices and communities. While HRSA is making these efforts, CDC could work to ensure that its data analyses are not so far removed from the community level as to be of little use to providers at the local level. To this end, it may be necessary to develop programs that not only aggregate data to the state and national levels
BOX 4-2
Examples of Shared Community Resources
In Yavapai County, Arizona, Community Health Services oversees both the community health center and the public health department. Community Health Services promotes the integration of the two by collocating services in the same buildings and using their separate boards as a vehicle for bridging their activities. The County Board of Supervisors, the community health center board, and the board of health have overlapping representation, including the same physician, nurse, and county representative (Personal communication, Robert Resendes, Director of Yavapai County Community Health Services, March 28, 2011).
Hudson River HealthCare, a primary care network in upstate New York, uses an innovative workforce to link with public health. Patient care partners assist patients with prescription assistance programs, referrals to outside agencies, and food and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) assistance, as well as patient education and self-management support. Community care partners provide similar services but are physically located in the community. They work in homeless shelters, after-school programs, community centers, and hospital emergency rooms. Hudson River HealthCare considers staff working in both of these positions to be integral to its work (Personal communication, Kathy Brieger, CEO, Hudson River HealthCare, May 2, 2011).
but also are capable of disaggregating the data based on geographic location and patient composition, as well as a nationally accessible platform for storing and disseminating these data. This disaggregation, which could be done at the state and local levels, would allow primary care providers not only to view their geographic population, but also to compare their population with similar populations across the state and nation. Currently, most practices lack the fundamental capability to turn their patient data into information that allows them to compare their practice with the practices of peers, to identify learning opportunities and areas of shared concern, and to look at their data in the context of community. Shared data resources, particularly with an analytic component to keep the data sharing safe and useful, would be important for primary care and public health integration.
In addition to legislation, funding streams can be used as a lever to encourage integration. To better understand this lever, it is helpful to understand the role of HRSA and CDC (as well as CMS) in funding health centers and health departments.
Funding for Health Centers and Health Departments
Health centers, state health departments, and local health departments receive revenue from a variety of sources. Figures 4-1, 4-2, and 4-3 show the average sources of revenue for health centers, state health departments, and local health departments, respectively. While the data do not reveal whether federal funding was primarily from HRSA or CDC, the nature of the two agencies’ activities suggests the likely source: federal direct and pass-through funding for health centers would be supplied primarily by HRSA, while federal funding received by state and local health departments could be assumed to be received primarily from CDC.
Figure 4-1 shows that federal direct and pass-through funding accounted for only 23.2 percent of health center revenues in 201025 (Kaiser Family Foundation, 2010). The other 78 percent comprises Medicare and Medicaid funding (5.8 and 37.7 percent, respectively), other public and private insurance (9.5 percent), direct payment by users (5.9 percent), and other funds provided through state and local grants and contracts and other sources (Kaiser Family Foundation, 2010).
Figure 4-2 shows that in 2009, 45 percent of state health departments’ budgets were derived from federal funding, with an additional 4 percent provided directly by Medicare and Medicaid. This funding comprised a number of federal resources, including CDC funding and other federal grants, contracts, and cooperative agreements, such as WIC vouchers and Environmental Protection Agency funding. The remainder of funds consisted of state general funds (23 percent), other state or territorial funds (16 percent), other sources of revenue (5 percent), and fees and fines (7 percent) (ASTHO, 2011).
Figure 4-3 shows that on average in 2010, only 23 percent of local health department revenue was derived from federal funding outside of Medicare and Medicaid funding. This 23 percent includes federal funds granted directly to local health departments (6 percent); federal pass-through funds, which are granted to states for dispersal throughout various state programs (14 percent); and ARRA and Public Health Emergency Preparedness (PHEP) grant funding (1 and 2 percent, respectively). The largest single source of local health department revenues was local funding (26 percent) (NACCHO, 2011).
_________________
25This figure varies widely across the states, from 11.2 percent in Wisconsin to 43.8 percent in Arkansas. Fifteen states and the District of Columbia rely on federal grants for less than 20 percent of their annual budgets, while 13 states and Puerto Rico receive more than a third of their income from federal grants (Kaiser Family Foundation, 2010).
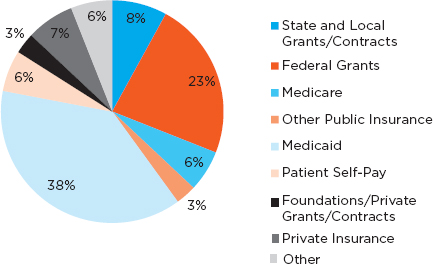
FIGURE 4-1 Percentage of total annual funding for health centers by revenue source, 2010.
SOURCE: Kaiser Family Foundation, 2010.
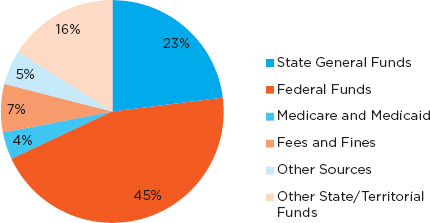
FIGURE 4-2 Percentage of total annual funding for state health departments by revenue source.
SOURCE: ASTHO, 2011.
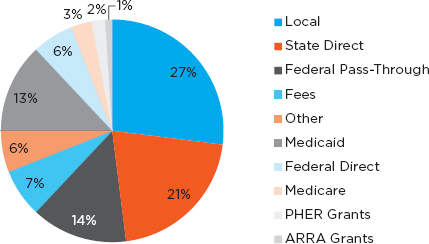
FIGURE 4-3 Percentage of total annual local health department revenues by revenue source.
NOTE: ARRA = American Recovery and Reinvestment Act; PHER = Public Health and Emergency Response.
SOURCE: NACCHO, 2011.
Federal Funding Opportunities
Given that HRSA and CDC jointly represent only 1.8 percent of the HHS budget (see Appendix A), it is prudent to look beyond them to other agencies that can assist in funding the integration of primary care and public health. Numerous offices and agencies within HHS have programs designed to promote the health and well-being of individuals, children, families, and communities. Partnering with them could assist HRSA and CDC in fostering integration. For example, the National Institutes of Health (NIH) provides funding for 229 research/disease areas, including cardiovascular disease, colon cancer, stroke, tobacco use, nutrition, and obesity (NIH, 2011). In addition, NIH oversees the Clinical and Translational Science Awards. These awards promote collaboration among diverse sets of stakeholders to identify local health challenges and design practical solutions, and could serve as a mechanism for encouraging integration.
The Social Services Block Grant (SSBG) is one of the most flexible funding sources, providing states with funds for a wide variety of social service and health-related programs. Moreover, up to 10 percent of a state’s annual SSBG allotment can be transferred to three health care block grants (the Preventive Health and Health Services Block Grant, the Maternal and
Child Health Services Block Grant, and the Substance Abuse Prevention and Treatment Block Grant) and the Low-Income Home Energy Assistance Program (U.S. House of Representatives Committee on Ways and Means, 2000). Within the Administration for Children and Families is the Community Services Block Grant, which provides services and activities addressing employment, education, housing, nutrition, emergency services, and health (HHS Administration for Children and Families, 2011).
Similarly, CMS oversees programs such as the Children’s Health Insurance Program (CHIP), which funds primary care services for children, and the Medicaid program. The Medicaid program pays for health and long-term care services for certain low-income individuals, including children, the elderly, and people with disabilities. States have broad authority to define eligibility, benefits, provider payments, and delivery systems. As a result, Medicaid programs vary widely by state. As mentioned above, CMS also administers the Medicaid Incentives for Prevention of Chronic Disease Program, which provides incentives to Medicaid beneficiaries who participate in prevention programs and demonstrate changes in health risks and outcomes, and the newly created CMMI, which is working on primary care and public health issues.
Finally, the Substance Abuse and Mental Health Services Administration promotes public health for mothers and children through a variety of programs, such as the Substance Abuse Prevention and Treatment Block Grant, the Mental Health Services Block Grant, and the Children’s Mental Health Services Program. It also focuses on integrating behavioral health and primary care, as well as reducing the use of tobacco and promoting health and wellness workplace programs.
Implications of the Current System
In examining the current funding system for primary care and public health, it becomes clear that the system is not well positioned to promote integration. For example, a number of grants from HRSA, CDC, and other agencies are aimed at addressing the same issues, and as a result create overlap on the ground. These competing funding streams have the effect of creating silos at the local level rather than encouraging cooperation across entities. Similarly, as discussed in more detail in Appendix A, funding streams from HRSA and CDC (with the exception of the Preventive Health and Health Services Block Grant) are inflexible. This inflexibility limits what local entities can do with the funds and how they could be used for integration.
Finally, it should be noted that the funds available to HRSA and CDC for supporting and integrating primary care and public health are small
compared with what is available to CMS. By joining forces, the three agencies could create much more momentum toward integration.
Adashi, E. Y., H. J. Geiger, and M. D. Fine. 20\10. Health care reform and primary care—the growing importance of the community health center. New England Journal of Medicine 362(22):2047-2050.
AHRQ (Agency for Healthcare Research and Quality). 2010. Impact infrastructure for maintaining primary care transformation. http://www.ahrq.gov/research/impactaw.htm (accessed January 31, 2012).
ASTHO (Association of State and Territorial Health Officials). 2011. ASTHO profile of state public health. Arlington, VA: ASTHO.
Bell, J., and M. Standish. 2005. Communities and health policy: A pathway for change. Health Affairs 24(2):339-342.
Bielaszka-DuVernay, C. 2011. Vermont’s blueprint for medical homes, community health teams, and better health at lower cost. Health Affairs 30(3):383-386.
Blumenthal, D. 2010. Launching HITECH. New England Journal of Medicine 362(5):382-385.
California Department of Public Health. 2010. Black infant health program. http://www.cdph.ca.gov/programs/BIH/Pages/default.aspx (accessed February 15, 2012).
Campbell, S., D. Reeves, E. Kontopantelis, E. Middleton, B. Sibbald, and M. Roland. 2007.
Quality of primary care in England with the introduction of pay for performance. New England Journal of Medicine 357(2):181-190.
Carrier, E., T. Yee, and R. L. Garfield. 2011. The uninsured and their health care needs: How have they changed since the recession? The Henry J. Kaiser Family Foundation: Kaiser Commission on Medicaid and the Uninsured.
CBO (Congressional Budget Office). 2006. Nonprofit hospitals and the provision of community benefits. Washington, DC: U.S. Congress Congressional Budget Office.
CBO. 2011. CBO’s analysis of the major health care legislation enacted in March 2010: Before the Subcommittee on Health Committee on Energy and Commerce. Washington, DC: U.S. Congress Congressional Budget Office.
CDC (Centers for Disease Control and Prevention). 2011. Community transformation grants. http://www.cdc.gov/communitytransformation/index.htm (accessed November 21, 2011). CDC. 2012.
Epidemic Intelligence Service (EIS). http://www.cdc.gov/EIS/index.html (accessed February 10, 2012).
Center for Medicare and Medicaid Innovation. 2011. Health care innovation challenge. http://innovations.cms.gov/About/index.html (accessed December 15, 2011).
CMS (Centers for Medicaid & Medicare Services). 2011. Regulations, guidance & standards. https://www.cms.gov/home/regsguidance.asp (accessed December 15, 2011).
Dannenberg, A. L., R. Bhatia, B. L. Cole, S. K. Heaton, J. D. Feldman, and C. D. Rutt. 2008. Use of health impact assessment in the U.S. 27 case studies, 1999–2007. American Journal of Preventive Medicine 34(3):241-256.
European Centre for Health Policy. 1999. Health impact assessment: Main concepts and suggested approach. Brussels: WHO.
Geiger, H. J. 2002. Community-oriented primary care: A path to community development. American Journal of Public Health 92(11):1713-1716.
Geiger, H. J. 2005. The first community health centers: A model of enduring value. Journal of Ambulatory Care Management Community Health Centers’ 40th Anniversary Issue October/December 28(4):313-320.
Grumbach, K., and J. W. Mold. 2009. A health care cooperative extension service. Journal of the American Medical Association 301(24):2589-2591.
Gulliford, M. C., M. Ashworth, D. Robotham, and A. Mohiddin. 2007. Achievement of metabolic targets for diabetes by English primary care practices under a new system of incentives. Diabetic Medicine 24(5):505-511.
The Henry J. Kaiser Family Foundation. 2011. Focus on health reform: Summary of new health reform law. Menlo Park, CA: The Henry J. Kasier Foundation.
HHS (Department of Health and Human Services). 2010. News release: “HHS awards $320 million to expand primary care workforce.” http://www.hhs.gov/news/press/2010pres/09/20100927e.html (accessed December 15, 2011).
HHS. 2011. Prevention and public health fund: Community transformation grants to reduce chronic disease. http://www.healthcare.gov/news/factsheets/2011/05/grants05132011a.html (accessed February 10, 2012).
HHS Administration for Children and Families. 2011. Fact sheet. http://www.acf.hhs.gov/programs/ocs/csbg/aboutus/factsheets.htm (accessed January 16, 2012).
HRSA (Health Resources and Services Administration). 2009. Accreditation initiative update: Program assistance letter 2009-12. http://bphc.hrsa.gov/policiesregulations/policies/pal200912.html (accessed December 21, 2011).
HRSA. 2011. HHS announces new teaching health centers graduate medical education program. http://www.hrsa.gov/about/news/pressreleases/110125teachinghealthcenters.html (accessed December 15, 2011).
IOM (Institute of Medicine). 2010. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: The National Academies Press.
IOM. 2011a. For the public’s health: The role of measurement in action and accountability. Washington, DC: The National Academies Press.
IOM. 2011b. For the public’s health: Revitalizing law and policy to meet new challenges. Wahington, DC: The National Academies Press.
IRS (Internal Revenue Service). 2011. Notice 2011-52, notice and request for comments regarding the community health needs assessment requirements for tax-exempt hospitals, edited by IRS. http://www.irs.gov/pub/irs-drop/n-11-52.pdf (accessed November 17, 2011).
Jordan, J., J. Wright, J. Wilkinson, and R. Williams. 1998. Assessing local health needs in primary care: Understanding and experience in three English districts. Quality Health Care 7(10180795):83-89.
Kaiser Family Foundation. 2010. Distribution of revenue by source for federally-funded federally qualified health centers, 2009. http://www.statehealthfacts.org/comparemaptable.jsp?ind=428&cat=8 (accessed October 24, 2011).
Ku, L., E. Jones, P. Shin, F. R. Byrne, and S. K. Long. 2011. Safety-net providers after health care reform: Lessons from Massachusetts. Archives of Internal Medicine 171(15):1379-1384.
MedPAC (Medicare Payment Advisory Commission). 2009. Accountable care organizations. Washington, DC: MedPAC.
NACCHO (National Association of County and City Health Officials). 2011. 2010 national profile of local health departments. Washington, DC: NACCHO.
National Prevention, Health Promotion and Public Health Council. 2011. National prevention strategy: America’s plan for better health and wellness. Rockville, MD: National Prevention, Health Promotion and Public Health Council.
NIH (National Institutes of Health). 2011. Estimates of funding for various research, condition, and disease categories (RCDC). http://report.nih.gov/rcdc/categories/ (accessed November 11, 2011).
NRC (National Research Council). 2011. Improving health in the United States: The role of health impact assessment. Washington, DC: The National Academies Press.
Phillips, R. L., S. Bronnikov, S. Petterson, M. Cifuentes, B. Teevan, M. Dodoo, W. D. Pace, and D. R. West. 2011. Case study of a primary care-based accountable care system approach to medical home transformation. The Journal of Ambulatory Care Management 34(1):67-77.
Poundstone, K. E., S. A. Strathdee, and D. D. Celentano. 2004. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiologic Reviews 26(1):22-35.
Reynolds, P. P. 2008. A legislative history of federal assistance for health professions training in primary care medicine and dentistry in the United States, 1963-2008. Academic Medicine 83(11):1004-1014.
Robert Wood Johnson Foundation, Network for Regional Health Care Improvement, and Pittsburgh Regional Health Initiative. 2009. From volume to value: Recommendations of the 2008 NRHI healthcare payment reform summit. Pittsburgh, PA: Network for Regional Healthcare Improvement.
Robinson, J., and R. Elkan. 1996. Health needs assessment: Theory and practice. London: Churchill Livingstone.
Roland, M. 2004. Linking physicians’ pay to the quality of care—A major experiment in the United Kingdom. New England Journal of Medicine 351(14):1448-1454.
Rosenbaum, S., and R. Margulies. 2010. New requirements for tax-exempt charitable hospitals. Health Reform GPS, http://www.healthreformgps.org/resources/new-requirementsfor-tax-exempt-charitable-hospitals (accessed November 16, 2011).
Steele, G. D., J. A. Haynes, D. E. Davis, J. Tomcavage, W. F. Stewart, T. R. Graf, R. A. Paulus, K. Weikel, and J. Shikles. 2010. How Geisinger’s advanced medical home model argues the case for rapid-cycle innovation. Health Affairs 29(11):2047-2053.
Steinbrook, R. 2009. Health care and the American Recovery and Reinvestment Act. New England Journal of Medicine 360(11):1057-1060.
Trust for America’s Health. 2011. Investing in America’s health: A state-by-state look at public health funding and key health facts. Washington, DC: Trust for America’s Health.
U.S. House of Representatives Committee on Ways and Means. 2000. Section 10. Title XX Social Services Block Grant program. In 2000 green book background material and data on programs within the jurisdiction of the Committee on Ways and Means. Washington, DC: U.S. Congress.
U.S. National Archives and Records Administration. 2011. Medicare program; Medicare shared savings program: Accountable care organizations. Federal Register 76(212):67802.
Vastag, B. 2004. Donald M. Berwick, MD, MPP advocate for evidence-based health system reform. Journal of the American Medical Association 291(16):1945-1947.
Wagner, E. H. 2000. The role of patient care teams in chronic disease management. British Medical Journal 320(7234):569-572.
The White House. 2009. Memorandum for the heads of executive departments and agencies. http://www.whitehouse.gov/the_press_office/Memorandum-for-the-Heads-of-Executive-Departments-and-Agencies-Subject-Government (accessed November 11, 2011).
WHO (World Health Organization). 2010. Adelaide statement on Health in All Policies: Moving towards a shared governance for health and well-being. Geneva, Switzerland: WHO.






































