6
The Primary Care Workforce
This chapter focuses on the principal types of primary care clinicians—physicians, physician assistants (PAs), and nurse practitioners (NPs). They are the personnel most likely, under state practice acts, hospital or health plan credentialing, or customary practice, to have significant patient care authority. The chapter reviews trends in the supply of these components of the health workforce (noting the extreme difficulties of producing reliable and valid estimates of supply and, especially, requirements for clinicians or clinicians' services); it also briefly comments on the education and training infrastructure for such personnel (a topic taken up in greater detail in Chapter 7). The chapter then advances four recommendations concerning important directions that, in the committee's view, the production and use of primary care clinicians ought to take.
The committee's definition of primary care draws attention to the concept of a primary care clinician, where clinician is defined by the committee as "an individual who uses a recognized scientific knowledge base and has the authority to direct the delivery of personal health services to patients" (see Chapter 2). This individual might or might not be a physician;1 that is, the committee view is that primary care clinicians as likely to include at least physicians, PAs, and Nps;
that is how the term is used in, for instance, Chapter 5. The committee recognizes that the broader primary care team will include various other health care personnel, such as therapists, nutritionists, social workers, allied health personnel, and office staff. This range of professionals is reflected, for example, in the vignettes used in Chapter 3 to illustrate the scope of primary care. Finally, yet other health professionals, such as dentists, deliver primary care within their own fields and disciplines (IOM, 1995a), but as they are not likely to be responsible for the large majority of health care needs of all people, they are not discussed further here.
Workforce Trends And Supply Projections: Physicians
Overall Levels of Supply
An extremely contentious set of issues in the United States in recent years has involved the numbers of physicians and their distribution by geographic area and specialty. Today, essentially all experts agree that the overall levels of physicians in the country point to a surplus; some in fact would characterize the level as a significant oversupply.
These issues were explored in a recent report by an Institute of Medicine committee on aggregate physician supply (IOM, 1996a, pp. 3–4). The report concluded that
- the nation, at present, clearly has an abundant supply of physicians—which some members of the committee were prepared to label a surplus;
- judgments about the implications of those numbers must be made in the context of the overall U.S. health care system and the components of that system of greatest concern—the quality and costs of health care and access to services;
- the increase in the numbers of physicians in training and entering practice each year is sufficient to cause concern that supply in the future will be excessive, regardless of the assumptions made about the structure of the health care system; and
- the steady growth in numbers of physicians coming into practice is attributable primarily to ever-increasing numbers of IMGs [international medical graduates], about which the committee is very concerned.
Other very recent publications are divided. For example, a minority viewpoint has been laid out by Cooper (1995), who argues that projections of the demand for and supply of physicians using more up-to-date assumptions show "no evidence of a major impending national surplus" (p. 1534). Cooper also draws attention to more than twofold differences across the states in the physician-to-population ratios; to the rapid growth of a wide array of nonphysician clinicians (including NPs and PAs); and to the need to develop policies that take
into account the full range of practitioners (not just physicians) who will be delivering services to patients in the next century.
In rebuttal, Tarlov (1995) notes the near unanimity of projections of substantial physician surpluses in analyses since 1980 and draws attention to the considerable uncertainties that surround the Cooper assumptions. Tarlov also calls for more creative actions on the part of many parties to deal not only with workforce supply issues but also to achieve other health goals as well, including reducing the disparities in access for underserved populations and increasing the representation of minorities in the medical profession. The most recent publication of the Pew Health Professions Commission comes down forcefully on the side of surplus, using language such as "a large oversupply" that will result in a "dislocation of crisis proportions" (Pew Health Professions Commission, 1995, p. 42). By and large, the IOM committee reporting here subscribes to the majority view; namely, that the nation does face a meaningful oversupply of physicians, in the aggregate, in coming years.
Figure 6-1 provides some basic data on the growth in physicians in this country over the past nearly 50 years. According to federal statistics, the number of active nonfederal M.D. physicians per 100,000 population in 1950, for example, was 126.6; the figure rose to 127.4 in 1960 and 137.4 in 1970 (DHHS, 1993). In effect, for 35 years or so since the end of World War II, the nation believed it had a considerable shortage of physicians. Steps were taken in the 1960s and 1970s both to expand the production of physicians within the country and to liberalize the rules by which foreign (now international) medical graduates could enter the United States for training and remain to practice.
The change in U.S. physician supply was dramatic.2 Between 1970–1971 and 1991–1992 the annual number of medical school graduates increased from approximately 9,000 to more than 15,000 (for allopathic schools, or M.D.s) and from 500 to more than 1,500 (for osteopathic schools, or D.O.s). As a result of these increases and federal policies that allowed more IMGs to practice in the United States, the number of physicians per 100,000 population increased dramatically between 1970 and 1990.
Active physicians numbered 151.4 per 100,000 population in 1970 and 267.5 per 100,000 in 1992 (IOM, 1996a). Put another way, the nation had 1 active physician for every 584 persons in the country in the mid-1970s (DHEW, 1977) and 1 for every 398 persons by the early 1990s. For active nonfederal M.D.s, the physician-to-population figures were 137.4 M.D.s per 100,000 population in 1970 and 219.5 in 1991, a rise of 60 percent. The percentage increase in the ratio of active nonfederal D.O.s was 104 percent (on a considerably smaller base), from 5.7 D.O.s per 100,000 persons in 1970 to 11.6 in 1991.
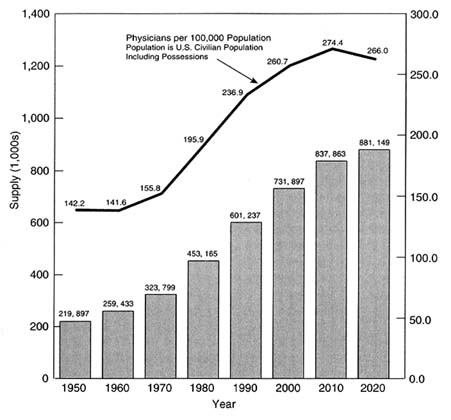
FIGURE 6-1 Numbers of physicians (M.D.s and D.O.s) and physicians per 100,000 population, selected years 1950–2020. SOURCE: IOM, 1996a. Reprinted with permission. Original source: Unpublished data from the Bureau of Health Professions (BHP) provided November 1, 1995. Data for 1950 through 1990 adjusted by BHP from American Medical Association Physician Masterfile and unpublished American Osteopathic Association data. Basic format of figure adapted from Rivo and Satcher (1993, p. 1077).
Table 6-1 provides further information on the U.S. physician supply (both M.D.s and D.O.s) according to various activity categories (e.g., active patient care, research, teaching) for selected years. Of interest is that, in the nearly quarter-century covered by these data, the total numbers of active physicians in patient care and the total numbers in residency training essentially doubled, whereas those in other professional activities rose only a fraction. Table 6-2a shows that, counting all physicians (including those who were inactive or had unknown addresses), the total numbers of federal and nonfederal physicians were 334,028 in 1970; 615,421 in 1990; and 670,336 in 1993.
TABLE 6-1 Supply of Physicians in the United States, 1970, 1980, 1992, by Type of Activity
|
Type of Activity |
Number of Physiciansa |
Number of Physicians per 100,000 populationa |
||||
|
|
1970 |
1980 |
1992 |
1970 |
1980 |
1992 |
|
TOTAL |
328,020 |
462,276 |
685,291 |
160.9 |
203.5 |
267.5 |
|
|
|
|
|
|
|
|
|
Total Active Physiciansb |
308,487 |
436,667 |
627,723 |
151.4 |
192.2 |
245.0 |
|
Total active physicians in patient carec |
222,657 |
310,533 |
461,405 |
109.2 |
136.7 |
180.1 |
|
Total active physicians in other professional activity |
31,582 |
38,009 |
39,816 |
15.5 |
16.7 |
15.5 |
|
teaching |
NA |
NA |
8,293 |
NA |
NA |
3.2 |
|
research |
NA |
NA |
16,398 |
NA |
NA |
6.4 |
|
administration |
NA |
NA |
15,125 |
NA |
NA |
5.9 |
|
Total physicians in training providing patient cared |
50,687 |
61,450 |
99,138 |
24.9 |
27.1 |
38.7 |
|
Not classifiede |
3,561 |
26,675 |
27,364 |
1.7 |
11.7 |
10.7 |
|
Total Inactive Physicians |
19,533 |
25,609 |
57,568 |
9.6 |
11.3 |
22.5 |
|
NOTE: NA=not available. a Data for 1970 and 1980 are for allopathic physicians (M.D.s) only; data for 1992 include both allopathic and osteopathic physicians. b Includes all physicians and physicians in training except those specifically identified as "inactive." c Although physicians in training clearly provide considerable patient care, they are not included in this total; see their separate line item, below. d "Physicians in training" is defined for 1970 and 1980 as "interns and residents, all years"; for 1992 the term is defined as "residents and fellows." e "Not classified'' includes, for 1970 and 1980, those physicians for whom an address is not known. SOURCES: IOM, 1996a, Table 2-1. Reprinted with permission. Data for 1970 and 1980 adapted from NCHS, 1983, Tables 1 and 55. Data for 1992 adapted from Kindig 1994, Table 1 and text. |
||||||
TABLE 6-2a Number of Active Federal and Nonfederal Physicians (M.D.s Only) by Specialty, Selected Years
|
Specialty |
1970 |
1980 |
1990 |
1994 |
|
Primary Care Specialties |
||||
|
General practice |
57,948 |
32,519 |
22,841 |
18,454 |
|
Family practice |
NAa |
27,530 |
47,639 |
54,709 |
|
General internal medicine |
39,924 |
58,462 |
76,295 |
84,951 |
|
General pediatrics |
17,950 |
27,582 |
36,519 |
41,906 |
|
|
|
|
|
|
|
Total primary care specialties |
115,822 |
146,093 |
183,294 |
200,020 |
|
|
|
|
|
|
|
Other Specialties |
||||
|
|
|
|
|
|
|
Obstetrics-gynecology |
18,876 |
26,305 |
33,697 |
36,649 |
|
Internal medicine subspecialtiesb |
1,948 |
13,069 |
22,054 |
26,476 |
|
Pediatrics subspecialtiesc |
869 |
1,880 |
5,380 |
7,451 |
|
All other specialties |
173,414 |
227,569 |
302,885 |
334,752 |
|
|
|
|
|
|
|
Total other specialtiesd |
195,107 |
268,823 |
364,016 |
405,328 |
|
Not classified physicians |
NAe |
20,629 |
12,678 |
14,283 |
|
Total active physiciansf |
310,929 |
435,545 |
559,988 |
619,751 |
|
|
|
|
|
|
|
Total Physiciansg |
334,028 |
467,679 |
615,421 |
684,414 |
|
NOTE: Data for 1990 and after are as of January 1. Data prior to 1990 are as of December 31. a Data on family practice were not available before 1975. b Internal medicine subspecialties include diabetes; endocrinology, diabetes, and metabolism; hematology; hepatology; cardiac electrophysiology; infectious diseases; clinical and laboratory immunology; geriatric medicine; sports medicine; nephrology; nutrition; medical oncology; and rheumatology. c Pediatric subspecialties include adolescent medicine; pediatric critical care medicine; neonatalperinatal medicine; pediatric allergy; pediatric cardiology; pediatric endocrinology; pediatric pulmonology; pediatric emergency medicine; pediatric gastroenterology; pediatric hematology/oncology; clinical and laboratory immunology; pediatric nephrology; pediatric rheumatology; and sports medicine. d Does not include, for 1994, 120 family practice subspecialty practitioners. Data on family practice subspecialties were not available before 1992. e Data not available before 1972. f Excludes those who are inactive and those for whom the address is unknown. g Includes those who are active, inactive, and those for whom the address is unknown. SOURCE: AMA, 1996. |
||||
Primary Care Physicians
Who Is Included
A major part of the physician workforce debate has centered on whether the supply of primary care physicians is sufficient. Although the committee wishes to underscore its view that primary care needs to be considered as a function and that the core of primary care delivery is a team of clinicians (and others), for the purposes of this chapter some denomination of the kinds of physicians typically considered as belonging to the area of primary care is necessary. Thus, to be able to show some numbers relating to supply and to trends over time, the committee focused on the primary care physicians practicing or trained in general practice, family practice, general internal medicine, and general pediatrics.
For purposes of counting practitioners, the committee did not bring obstetricians-gynecologists (OB-GYNs) into its primary care category. It did recognize that many women use OB-GYN specialists as their main, or even sole, health care providers, and the committee agreed that some regular use of this specialty is essential, if only to ensure that women see a physician at least yearly. As discussed in Chapters 2 and 5, however, the committee did not believe that OB-GYNs in general are likely to take on responsibility for "the large majority of health care needs" of their patients (and clearly they are not a source of primary care for men); thus, as a general proposition the practice of OB-GYN does not dovetail with the committee's definition of primary care. Some researchers and others in the workforce policy area, however, do include them in the primary care category, and some elements of the OB-GYN community have successfully argued that they are a part of the primary care workforce.
In general, other specialists and subspecialists are not, for workforce planning purposes, considered primary care physicians. The committee acknowledges that many other types of physicians may render what is recognizably primary care, for at least some of their patients or at least some of the time. No current estimates are available, however, to indicate what proportion of the practices of these other types of specialists is primary care. Thus, for purposes of understanding or influencing workforce policy, the committee is not considering physician specialties beyond those specified above.
Trends in Supply
The supply of primary care clinicians has been studied for many years. The IOM report on primary care in 1978 (IOM, 1978), the report of the Graduate Medical Education National Advisory Committee (GMENAC, 1981), and more recent studies by the Physician Payment Review Commission (PPRC, 1992, 1995) and numerous statements of the Committee on Graduate Medical Education (COGME, especially the fourth and seventh reports [1994, 1995]) have all
expressed concern about the adequacy of the supply of primary care physicians. This issue was also addressed in several of the proposals for health care reform, most extensively in the Health Security Act (CCH, 1993). The prevailing view is that the nation has had, and still does, an imbalance between generalists and specialists—too few of the former and too many of the latter.
Specifically, as already noted, the United States has experienced a dramatic change in the composition of its physician workforce. In the early 1930s, 87 percent of private practice physicians were in general practice; 30 years later, only about 50 percent were generalists. Since then, the proportion of primary care physicians has continued to decline—leveling off at about one-third of all active physicians.
Tables 6-2a, 6-2b, and 6-2c provide information on specialty distribution for allopathic physicians for several years beginning with 1970; this information pertains only to M.D.s and takes only active physicians into account. Counting generalist M.D.s to be those in general and family practice, general internal medicine, and general pediatrics, the numbers in primary care increased from about 116,000 (in 1970) to 200,020 (in 1994); the total of all other specialties rose
TABLE 6-2b Physicians (M.D.s only) by Specialty Category as a Percentage of Total Active Physicians, Selected Years
TABLE 6-2c Percentage Changes in Numbers of Physicians (M.D.s only) in Primary Care During Selected Periods
|
Category |
1970–1990 |
1990–1994 |
1970–1994 |
|
All primary care |
58.3 |
8.7 |
72.7 |
|
General/family practice |
21.6 |
3.8 |
26.3 |
|
General internal medicine |
91.1 |
11.4 |
112.8 |
|
General pediatrics |
103.4 |
14.8 |
133.5 |
|
SOURCE: Based on data from AMA, 1996 (see Table 6-2a). |
|||
from about 195,000 to more than 405,328 in the same period. In percentage terms (see Table 6-2b), primary care doctors as a percentage of total active physicians went from about 37 percent in 1970 to just over 32 percent in 1994; other specialties were about 63 and 65 percent of all active physicians in those years.
Said another way, in the nearly quarter-century from 1970 to 1994 the total number of M.D.s in the United States more than doubled (from 334,000 to 684,414), and the total of active physicians nearly doubled (about 311,000 to almost 620,000). Most of the growth in the number of allopathic physicians was in specialty medicine—a rise of 108 percent over the period. The primary care workforce (general and family practice, general internal medicine, and general pediatrics) increased by about 73 percent (see Table 6-2c). The percentage increases during 1970–1994 were about 133 percent for general pediatrics, about 113 percent for general internal medicine, and about 26 percent for general and family medicine combined; if just family medicine is considered, the percentage increase from 1980 (the first year of family practice data noted in Table 6-2a) to 1994 was 99 percent. By 1994, of all primary care M.D.s in the United States, 43 percent were in internal medicine, 36 percent in general and family practice (mostly the latter), and 21 percent in pediatrics.
More recently, various expert groups and researchers have concluded that the future demand for physician services including primary care physicians may be attenuated by the rapid growth of managed care plans, which use fewer physicians per enrollee than are used by the rest of the population (Kindig et al., 1993; COGME, 1995; Davis et al., 1995; Gamliel et al., 1995; PPRC, 1995; ProPAC, 1995; Scheffler, Appendix E). Other factors also suggest that the aggregate supply of primary care clinicians may be adequate in the near future. These include the rapid growth in the supply of primary care professionals other than physicians; the provision of primary care by specialist physicians (probably a significant number, although recent data are not available); and a recent turnaround in the numbers of medical students choosing primary care (perhaps a delayed response to market signals that are increasing the incomes of generalists both absolutely and in relationship to specialists incomes). As COGME (1996) notes in its eighth report, however, although projections of the numbers of generalist physicians may suggest that supply will be adequate, there is no guarantee of appropriate geographic distribution of those practitioners.
Education, Training, and Licensure
Today, the United States has a total of 125 schools of allopathic medicine3 and another 16 schools of osteopathic medicine; up to four new osteopathic
schools are in various stages of planning. Together they currently graduate approximately 17,500 physicians a year—a figure that has been fairly constant for about 15 years. Specifically, the number of M.D. graduates in 1994 was 15,579 (Barzansky et al., 1995), and the number of D.O. graduates that year was 1,775 (Singer, 1994). Graduates from allopathic schools alone are projected to number about 16,400 for the academic years through 1998–1999 (Jonas et al., 1994).
Information on enrollments in allopathic schools is instructive. Total enrollment in 1993–1994 was nearly 66,500; of these, about 40 percent were women. With respect to race and ethnic background, 15.6 percent were Asian and Pacific Islander; nearly 8 percent were Mexican American, Puerto Rican, or of other Hispanic background; 7.2 percent were non-Hispanic African American; 0.6 percent were Native American or Alaskan Native; all other students (white but not of Hispanic origin, and non-U.S. foreign students of any race or ethnicity) made up nearly 70 percent of all students. Of interest is that the ratio of students applying to U.S. medical schools to those accepted is about 2.5 to 1. With respect to the primary care workforce, it is evident from the small proportion of minority students enrolled in medical schools that achieving significant representation of minorities who are trained and practicing in primary care will be difficult, at least in the near term.
Newly graduated physicians take graduate medical education (GME) training in a highly developed graduate training system in this country. Accredited single-specialty and combined-specialty GME programs numbered 7,277 in 1993 (JAMA, 1994), with a total of 97,370 resident physicians. 4 Of these programs, 407 are in family practice, 416 in nonsubspecialty internal medicine, and 215 in nonsubspecialty pediatrics; respectively, the total numbers of positions in these programs were on the order of 8,500 (family medicine), 21,300 (internal medicine), and 7,750 (pediatrics).5 According to Whitcomb (1994), most GME programs (more than 90 percent) are affiliated with a medical school (or a closely related entity).
Groups in both the public and private sectors have sought, over the years, to increase the production of primary care physicians (see also Chapter 7). In the public sector, these steps have included support under Title VII of the Public Health Service Act for the training of primary care physicians. Several state governments have also pressed the medical schools within the state to increase
production of primary care physicians (including Arizona and California). Several private foundations also support programs to increase the training of generalists.
Geographic Distribution of Primary Care Physicians
Of considerable importance is the continuing lack of sufficient primary care clinicians in some geographic areas, particularly rural and some poor urban areas. By and large, problems of geographic maldistribution are set out in terms of aggregate physician presence, not the availability of primary care physicians (or primary care clinicians). For example, in 1993 metropolitan areas had an average ratio of physicians to population of 226 per 100,000 persons, whereas for non-metropolitan areas the ratio was 118 per 100,000 persons (Cooper, 1995). More telling is Cooper's analysis of physician-to-population ratios across the states, which shows a high of 294 in Maryland and the District of Columbia and a low of 118 in Mississippi. Cooper argues that the nation can be characterized as having five regions as follows (physician-to-population ratios are given in parentheses): the Boston-Washington corridor (227 to 294 per 100,000 persons); east and west "arms" including Florida (190 to 212); the central zone (147 to 181); the northern Rockies and Alaska (132 to 143); and Mississippi (118).
Workforce developments in the past 25 years provide ample evidence that increases in aggregate supply, by themselves, are not adequate to correct the problem of shortages in some areas of the country. Although physicians have been moving to smaller or more rural areas since the early 1980s (Schwartz et al., 1980; Williams et al., 1981; Newhouse et al., 1982a, 1982b), the fact that rural areas and inner cities continue to face access problems cannot be gainsaid. Geographic maldistribution in rural areas (e.g., for counties of fewer than 50,000 residents) is worsening, not improving, according to recent data from COGME (1995), a pattern consistent with the data reported by Cooper (1995). The committee returns to the geographic maldistribution issue later in this Chapter 7.
Workforce Trends And Supply Projections: Nurse Practitioners
According to a recent report on nurse staffing in hospitals and nursing homes (IOM, 1996b), the largest group of health care providers in the United States is registered nurses (RNs); in 1992, more than 2.2 million individuals were licensed to practice as RNs, or about 750 RNs per 100,000 population. RNs are prepared in one of three different educational tracks that can take two, three, or four years. 6 In 1993, there were 129 diploma programs, 857 associated degree programs,
and 507 baccalaureate programs, which together produced nearly 95,000 graduates; baccalaureate programs alone in 1994 had nearly 113,000 enrollees. Given this diversity of training, RNs differ in terms of both basic and advanced clinical education and skills; consequently, their clinical responsibilities may vary as well, from providing direct patient care at a fairly basic level to managing care for complex cases to directing complex nursing departments in institutions and community sites.
Nurse practitioners are one of a category of advanced practice nurses 7 with significant involvement in primary care. Nurse practitioners have, in general, an average of 580 hours of clinical training (AACN, 1995). NPs "are usually prepared at the master's degree level and also certified in a specialty area of practice, such as pediatrics, family practice, or primary care. Their usual responsibilities include managing clinical care; they conduct physical examinations, track medical histories, make diagnoses, treat minor illnesses and injuries, and perform an array of counseling and educational tasks. [NPs] may also, in some circumstances, order and interpret diagnostic tests and prescribe medications" (IOM, 1996b, 99–100).8 As for RNs generally, the scope of practice for NPs is governed by state nurse practice acts, which vary considerably across the nation.
Based on a 1992 survey of RNs, approximately 48,200 nurses had formal training as NPs (Moses, 1994). Of this number, roughly three-fifths are certified by a national or state organization, and approximately one-half are practicing as NPs (Moses, 1994).
Table 6-3 shows the growth in number of employed RNs who have nurse practitioner (or nurse midwife) in their title—from nearly 15,500 in 1980 to about 20,600 in 1988 and almost 23,700 in 1992, using data from a national sample survey of nursing that is conducted periodically. In percentage terms, a substantial increase took place between 1984 and 1988 (about 22 percent), with another 14.6 percent rise between 1988 and 1992; the overall percentage change in employed RNs who were either NPs or nurse midwives was more than 53 percent between 1980 and 1992.
The total number of NPs who are practicing is difficult to determine because licensing and educational requirements vary significantly across states (Morgan, 1993; Washington Consulting Group, 1994). For example, some NPs, although graduates of NP programs, do not have and do not need state certification to practice in a health maintenance organization (HMO); thus a count of currently
TABLE 6-3 Employed Registered Nurses with Nurse Practitioner or Nurse Midwife in Their Titles, Selected Years, and Percentage Changes between Years
|
Year |
Number of Nurse Practitioners (or Nurse Midwives) |
Percentage Change from Previous Year Given |
|
1980 |
15,443 |
|
|
1984 |
16,886 |
9.3 |
|
1988 |
20,649 |
22.3 |
|
1992 |
23,658 |
14.6 |
|
SOURCE: National Nursing Sample Survey, 1980, 1984, 1988, 1992 (Bureau of the Health Professions, Health Resources and Services Administration, unpublished). |
||
certified NPs in a given state is likely to result in underestimating those who might be in practice.
Primary Care Nurse Practitioners
The National Nursing Sample Surveys do not specifically break out NPs who are practicing primary care, but the large majority of NPs are thought to be doing so. Table 6-4 shows the number of NP graduates in 1992 by their area of specialization. Most of the categories shown might be considered to have a major primary care focus. Certainly, NPs graduating with a principal area of expertise in family, pediatric, and adult health, and possibly gerontology and women's health, would fall into this category, and together those groups account for about 80 percent of NPs graduating that year.
What is not known, however, is in what areas the nearly 24,000 currently employed NPs are actually practicing. Some NPs who are practicing in what appears to be primary care, for example, consider themselves specialists in a given area, such as diabetes counseling and management of diabetic adolescents. However, the number of such NPs has never been documented, and the extent to which they might also provide large amounts of routine primary care is certainly not known.
Trends in Supply
The number of NPs is expected to grow considerably in the years ahead as a result of the establishment of new education and training programs. A recent survey by the American Association of Colleges of Nursing provides considerable detail on these NP programs. Currently, 644 institutions of higher learning offer at least baccalaureate programs in nursing and, of these, 287 offer master's
TABLE 6-4 U.S. Graduations of Nurse Practitioners by General Area of Practice, 1992
|
Area of Practice |
Number |
Percentagea |
|
Family |
485 |
29.5 |
|
Pediatric |
281 |
17.1 |
|
Adult |
276 |
16.8 |
|
Gerontology |
118 |
7.2 |
|
Midwifery |
110 |
6.7 |
|
Psychiatric/mental health |
53 |
3.2 |
|
Women's health |
142 |
8.6 |
|
School |
1 |
0.1 |
|
Other |
179 |
10.9 |
|
|
|
|
|
Total |
1,645 |
100.1 |
|
NOTE: American Samoa, Guam, Puerto Rico, and the Virgin Islands are not included. a Total is more than 100 percent because of rounding. SOURCE: NLN, 1994, Section 2-3, Table 10A. |
||
programs. In all, 206 institutions (32 percent of the baccalaureate-level programs, and 72 percent of those with master's level programs, chiefly in universities) also provide NP education at the level of master's or post-master's training (AACN, 1995, p. 7, Tables 7 and 9);9 of these, about 30 percent offer a doctoral program as well. In addition, 75 institutions are reported to be planning to add master's degree or post-master's NP education programs to their curricula, a trend that represents rapid growth in NP training programs.
According to the AACN survey (1995), 32,049 individuals were enrolled as of fall 1994 in master's level nursing programs. Of these, 37 percent were in NP areas of study (11,536 in traditional master's programs and 289 in so-called generic programs for persons who had nonnursing college degrees); an additional 3 percent of this entire student body were in combined NP and clinical nurse specialist (CNS) programs (1,023 in traditional and 59 in generic programs). The AACN (1995, p. 3) notes a "dramatic growth in [recent] NP enrollment."
From August 1993 through July 1994, the number of NPs graduating from traditional or generic master's programs totaled 2,153 (AACN, 1995); 183 graduated with combined NP-CNS degrees. Of the 7,999 graduates in that period NPs alone represented about 27 percent and NP-CNSs 2 percent. Comparing these
graduating figures with enrollment data cited just above suggests that the output of nurses with NP (or NP-CNS) training (as a proportion of all nurses being trained at the master's level) will rise in the coming years.
The question of primary care focus within NP training is of interest. Of 125 NP institutions reporting information on this question in the AACN survey (1995), 91 report specialty tracks in family health, 42 tracks in adult health (and an additional 10 in adult acute care), 41 in pediatrics, 27 in gerontology/geriatrics, and 23 in OB-GYN or women's health (other than midwifery). Of the 1,946 full-time and part-time students enrolled in these institutions, nearly 89 percent are enrolled in these specialty areas, suggesting a considerable interest in primary care. The rapid growth in post-master's training may in part reflect the downsizing of hospitals and a shift of hospital-based master's prepared clinical specialists to primary care.
Current Work Environments and Responsibilities
Approximately 29 percent of NPs work in private practices or HMOs, 23 percent in hospital outpatient departments, 23 percent in public or community health centers, and 11 percent in inpatient hospital departments (Washington Consulting Group, 1994). Thus, only about 1 in 10 NPs work in inpatient settings, in contrast to RNs. About two-thirds of RNs work in hospitals, and although available data do not permit a breakdown of inpatient and outpatient settings, it is generally believed that a majority of hospital-based RNs are in inpatient settings (IOM, 1996b; Moses, 1994).
Nearly 70 percent of NPs have primary responsibility for a specific group of patients under either a team or panel approach (PPRC, 1994). NPs in nine states can establish independent practices (Birkholz and Walker, 1994; Henderson and Chovan, 1994; Pearson, 1994). About 1 in 10 NPs have hospital admitting privileges, and 1 in 3 have hospital discharge privileges (Washington Consulting Group, 1994).
Workforce Trends And Supply Projections: Physician Assistants
Physician assistants are health personnel who are typically trained in two or more years to render basic health care services that in earlier decades were performed only by physicians (Scheffler and Gillings, 1982; Jones and Cawley, 1994). They represent a ''new" category of health personnel that has emerged only since the early 1960s, partly in response to the desire to make good use of experienced hospital corpsmen and combat medics returning from Vietnam. Early models of PA training aimed to produce personnel who would be able to assist doctors in ways that would foster better use of both physicians and nurses. To this day, PAs work under a form of physician supervision (not necessarily direct
physical supervision), in which PAs are "agents of their supervising physicians" (Jones and Cawley, 1994, p. 1,269); supervising physicians define the standard to which PA services will be held and are, in effect, vicariously liable for those services (by virtue of being responsible for selecting and supervising PAs).
PA responsibilities have been described by Jones and Cawley (1994) in six areas: evaluation, monitoring, diagnostics, therapeutics, counseling, and referral. Within these categories, the state laws that describe and delimit the scope of PA practice are quite varied. PAs are regulated under states' medical practice acts—a circumstance different from that for nurses, who are regulated under nurse practice acts. This difference means that PAs and nurses may, in some jurisdictions, carry out similar functions, but NPs do so independently and PAs under the supervision (even if distant) of physicians. In any case, the great variation in PA statutes has the effect of not permitting PAs trained in similar ways and exhibiting essentially the same skills to perform the same functions across the nation.
Accurate counts of the number of PAs being graduated in this country date only to about 1967, and figures for the aggregate supply of PAs only to about 1970. The data are collected by the American Academy of Physician Assistants (AAPA), which conducts census surveys of its members; the 1995 mid-year report gives considerable information from a survey of nearly 13,500 PAs (AAPA, 1995). As shown in Table 6-5, in 1967 (the first year that any data were collected) there were 4 new PA graduates; by 1995, the number exceeded 2,100. In the nearly 30 years since any organization began counting, 32,215 PAs have been produced in this country.
Currently, 64 PA programs are operating in the United States. This number includes four new programs begun in the past year (Steven Crane, AAPA, personal communication, November 1995). More than half (55 percent) of entering PA students have baccalaureate degrees, and entering students generally have
TABLE 6-5 New and Cumulative Graduates from Physician Assistant Programs, Selected Years
TABLE 6-6 Number and Percentage of Physician Assistants, by General Area of Practice, Mid-1995
|
Practice Area |
Number |
Percentage |
|
Primary Care Specialties |
5,922 |
47.2 |
|
Family/general medicine |
4,652 |
37.9 |
|
General internal medicine |
958 |
7.8 |
|
General pediatrics |
312 |
2.5 |
|
|
|
|
|
Other Specialties |
6,612 |
52.8 |
|
Emergency Medicine |
1,043 |
8.3 |
|
Obstetrics-gynecology |
373 |
3.0 |
|
Industrial and occupational medicine |
396 |
3.2 |
|
Geriatrics |
115 |
0.9 |
|
Internal medicine subspecialties |
925 |
7.5 |
|
Pediatric subspecialties |
229 |
1.9 |
|
All surgical specialties |
2,767 |
22.1 |
|
All other specialties |
764 |
6.1 |
|
|
|
|
|
Total |
12,534 |
100.0 |
|
SOURCE: AAPA, 1995, Table 22a. |
||
had more than four years of health care experience in fields such as nursing and allied health or experience as paramedics and emergency medical technicians (Eugene Jones, personal communication, 1995). PAs in primary care practice with and are supervised by primary care physicians, although in some practices in rural areas the link is electronic and periodic rather than comprising a traditional team practice with shared office space.
Primary Care Physician Assistants
According to a 1995 AAPA report, 5,922 of 12,534 PAs responding to the survey were practicing in federally defined primary care specialties—internal medicine, general pediatrics, and family medicine (Table 6-6). This number represents 47 percent of the respondents (and approximately 34 percent of all PAs surveyed). Although PA practice settings remain diverse, an increasing plurality remain employed in primary care.
Current Work Environments and Settings
According to the AAPA (1995) survey, about 40 percent of PAs work in solo or group practice physician offices, about 10 percent in clinics, nearly 7 percent in health maintenance organizations, and about 25 percent in hospitals. This is a pattern not unlike that for NPs (see above).
TABLE 6-7 Physician Assistants in Practice, by Region, 1994–1995
|
Region |
Number |
Percentage |
|
North Central |
2,353 |
19.8 |
|
Northeast |
3,017 |
25.4 |
|
Southeast |
2,867 |
24.1 |
|
South Central |
1,631 |
13.7 |
|
West |
2,020 |
17.0 |
|
Total |
11,888 |
100.0 |
|
SOURCE: AAPA, 1995, Table 6. |
||
Table 6-7 illustrates the geographically uneven distribution of PAs (AAPA, 1995). In 1994–1995, almost one-half (49 percent) were in the East, one-third (34 percent) in the North and South Central regions, and one-sixth (17 percent) in the West.
Other First-Contact Providers
First-contact providers such as dentists, optometrists, and pharmacists play an important role in the provision of basic health care services. The committee did not have the resources to track trends in supply of these types of providers, but in general it did not foresee a significant shift in either their numbers or their roles in the near term. With respect, however, to the role of the dental professions in overall health care in this country, a recent IOM report on dental education (IOM, 1995a) calls attention to the following broad health objective (p. 78): "promoting attention to oral health (including the oral manifestations of other health problems) not just among dental practitioners but also among other primary care providers, geriatricians, educators, and public officials" (emphasis in the original). This committee is generally in agreement with these views.
More broadly, the committee encourages greater coordination between these types of first-contact professionals and primary care clinicians. It believes that a continuation of the typical roles of first-contact providers is not likely to affect the demand for primary care clinicians to any meaningful degree in the near term, and thus it did not explore issues relating to these types of practitioners further.
Comment On Workforce Estimation
The history of workforce projection in health care is not encouraging. 10 The problems lie in the marked difficulties of estimating "need" or "demand" (that is,
requirements) for either health care services or health care personnel and the somewhat less troublesome challenges of projecting supply. Tarlov (1995, p. 1,559) notes that some agreement exists about certain factors, such as the state of health of Americans, use of health care, medical training, and growth of nonphysician clinicians; he believes these offer some common ground for making assumptions about supply and requirements that can be used in full-scale workforce models, but he is careful to underscore the uncertainties. Among the trends that complicate forecasting today are the following (Feil et al., 1993): the rate of growth of managed care plans; innovations in the patterns of use of primary care professionals in the future, including the wider use of teams; the rate of spread of those innovations; the acceptance of new patterns of primary care providers by patients as they choose among competing health plans; the degree to which specialists seek to expand their provision of primary care as the pending surplus of specialists cuts back on the opportunities within specialties; the ability of academic health centers and other health organizations to support training of primary care clinicians when the financial viability of the training programs is threatened by the competitive health care market seeking to avoid training costs; and the probable reductions in federal and state budgets for health professional education, including support for GME and nursing training under the Medicare program. In the committee's view, drawing inferences about the expected adequacy of supply relative to requirements must be done with considerable caution, especially for the more distant future, and especially for NPs.
As noted by Scheffler (Appendix E), estimates of the overall impact of NPs and PAs on the size and composition of the future health workforce vary widely because of the different assumptions that forecasters make about patient utilization rates, physician delegation rates, the extent to which HMOs and other managed care organizations are willing to use NPs and PAs, and other variables. The varying assumptions about managed care organizations reflect the fact that so far, researchers have been able to obtain detailed data on physician and nonphysician staffing patterns for only a handful of HMOs, and staffing patterns vary widely among those HMOs that have made data accessible to researchers (Weiner, 1993, 1994).
The case study conducted by Scheffler for the committee compared staffing patterns in two mature HMOs. He found, first, that merely counting physicians and specialist physicians does not provide a useful staffing analysis in a managed care world. Researchers must also examine the use of PAs, NPs, and other
nonphysician clinicians. Second, to make inferences about productivity, researchers cannot merely compare the number of health professionals used by the plan to the total plan enrollment. They need to investigate differences in enrollee and other plan characteristics, including enrollee age and sex distribution, patient severity of illness, patient outcomes, staff productivity, and the organizational structure of the clinical practice. Third, staffing numbers alone cannot reveal some important health workforce parameters, such as complementarity and substitution possibilities within health care teams.
Another salient issue regarding workforce estimates is the lack of current knowledge of the content of clinicians' practices—whether physicians, NPs, or PAs. Regardless of the disciplines in which they receive training, we know little about the proportion of their practice that is, in fact, primary care. Although clearly the numbers of NPs and PAs will increase in the years ahead, their roles in an evolving health care system are uncertain. They may well be used in both specialty care and primary care, for example, making the size of their representation within the primary care clinician category quite problematic at this stage.
Conclusions And Recommendations About The Supply Of Primary Care Clinicians
Training Programs for Primary Care Clinicians
Basic Goals
Taking all the figures cited above in the admittedly difficult-to-predict context of health care restructuring in this country, the committee concluded that, at the moment, the nation probably has a modest aggregate shortage of primary care clinicians. (Aggregate, in this instance, refers to the combination of physicians, NPs, and PAs in primary care.) In the near term, the aggregate "shortages" may disappear because of several factors. Some relate to demand for health care; others involve current supply and production of various types of primary care professionals.
Market-driven changes will affect the effective economic demand for primary care clinicians. These changes include the growth of managed care, the development by some managed care organizations of innovative models of personnel substitution, and the increased use of primary care teams. All have the potential to affect the demand for primary care clinicians. Because some changes may increase demand and others decrease it, it is difficult to predict the net effect.
Furthermore, the cutbacks in Medicare and Medicaid that can be expected in coming years may attenuate the rate of growth in demand (at least per capita demand) from the elderly population. Certainly the demand for provision of health care services to low-income, disabled, and disadvantaged populations can be expected to drop, if federal entitlements to the Medicaid program are eliminated
in favor of state options for health care block grants. The rise in the number of persons underinsured or uninsured in any one year will also affect demand for health care services. So, too, will increases in mandatory out-of-pocket costs, such as higher health care premiums, higher deductibles and copayment requirements, and cutbacks in coverage of certain services such as those for mental health.
Economic demand for health care services is not equivalent to potential need for such services. As Tarlov (1995, p. 1559) notes:
[A]lso affecting requirements are the emergence of new diseases, sharp changes in demographic composition and the different needs of special populations including the poor, immigrants, some minority groups, children, military personnel, veterans, retirees, elders, and people in underserved rural and urban areas. …
The committee is under no illusions: Developing a national consensus about service requirements—i.e., the human need for health care services—is, and will remain, a profound challenge.
Changes on the supply side can be expected to help eliminate shortages in the future. Among these changes are the probable increase in the number of specialists and subspecialists who expand their delivery of primary care services, a rising interest in primary care careers on the part of medical students, and continued rapid growth in training of NPs and PAs.
In general, the committee supports these trends, but it remains unconvinced that the supply of well-prepared primary care clinicians will be sufficient to meet the demand for their services, at least in the short term. In the longer term, of course, these steps may well suffice, but the committee is not persuaded that, collectively, they will produce adequate numbers of appropriately competent personnel able to function in the model of a primary care team and to provide adequate quality of care. To address these concerns, the committee has two points it wishes to emphasize concerning the future of programs that produce primary care physicians, PAs, and NPs.
Recommendation 6.1 Programs Regarding the Primary Care Workforce
The committee recommends (a) that the current level of effort to increase the supply of primary care clinicians be continued and (b) that these primary care training programs and delivery systems focus their efforts on improving the competency of primary care clinicians and on increasing access for populations not now receiving adequate primary care.
General Issues of Access and Quality of Care
In the committee's judgment, the nation does still have an imbalance in the supply of primary care clinicians relative to clinicians (chiefly physicians) in specialty and subspecialty disciplines. Recommendation 6.1 is intended to help right that balance, without tipping the scale toward a future excess of primary care clinicians of any type. Its language about the output of current training programs is, therefore, chosen advisedly. That is, the committee believes that the present levels of production of primary care physicians, NPs, and PAs should be maintained—not accelerated, but also not diminished. The committee does not recommend the introduction of major new initiatives aimed at increasing the aggregate supply of primary care clinicians. Rather, as noted just below, the aim is to improve access to primary care for all Americans, taking into account expertise, geographic distribution, ethnic and cultural representation within the primary care workforce, or other factors important to the delivery of high-quality primary care.
The committee's further focus with respect to primary care training programs is on improving primary care competencies. These issues are explored more fully in Chapter 7 on training and education and are touched on in Chapter 8 with respect to accountability for quality of care.
This committee, like others at the IOM, endorses the IOM's stated position about universal access to health care coverage for all Americans (IOM, 1993) and has explicitly offered its own recommendation in this area (Recommendation 5.1). Fulfilling this aim is regarded as especially pertinent for primary care, because of the centrality of primary care to well-rounded, integrated health care, access to appropriate specialists, and better patient outcomes. It is even more important for those populations that do not now receive adequate primary care.
Thus, the committee is especially concerned that training programs be configured so as to prepare students for careers in the full range of settings needed to serve all the American people. These points are also addressed more fully in Chapter 7 in discussions of undergraduate medical education in primary care sites (see Recommendation 7.1) and graduate medical education in nonhospital sites such as HMOs, community clinics, physician offices, and extended care facilities (see Recommendation 7.6).
Minority Participation in Primary Care Training and Practice
The committee also wishes to go on record as supporting special initiatives that will increase the percentage of underrepresented minorities in the health professions, including primary care. This is in keeping with recent recommendations of other IOM committees, especially one on minority representation in the health professions (IOM, 1994) and another on aggregate physician supply (IOM,
1996a); it is also consistent with the "3000 by 2000" goals of the Association of American Medical Colleges.
Specifically, the committee would like to see the ethnic and cultural mix of the present and future supply of primary care clinicians be modified over time by an increase in the proportion of minorities. In this regard, the committee draws attention not only to the problems of underrepresentation among practitioners (i.e., physicians, NPs, or PAs) but also among the health professions faculty and researchers. Consistent with the sentiment of the IOM report Balancing the Scales of Opportunity: Ensuring Racial and Ethnic Diversity in the Health Professions (IOM, 1994), the committee is sensitive to the need for health professions schools to develop programs that reflect genuine appreciation and respect for students' various backgrounds, values, and perspectives. It also underscores the need for health professions schools and professional organizations to engage in more outreach to prospective students at the university (indeed, at the high school) level. This view dovetails with the discussion in the next chapter about the need for training programs, professional organizations, and similar groups to emphasize cultural sensitivity and appropriate communication skills (see Recommendation 7.4).
Monitoring Supply And Requirements
Recommendation 6.2 Monitoring the Primary Care Workforce
The committee recommends that state and federal agencies carefully monitor the supply of and requirements for primary care clinicians.
In keeping with the increasingly interdisciplinary nature of primary care, the committee urges that state and federal agencies compile a composite database of primary care clinicians—including physicians, NPs, and PAs providing primary care services. This would help analysts, policymakers, educators, and others understand the changing requirements for primary care clinicians and monitor utilization patterns of employment, geographic distribution, and insurance status of patients served.
Market forces may be able in the future to correct the modest shortage of primary care clinicians. The restructuring presently taking place, however, remains fluid so that the committee cannot be certain that market forces will induce and maintain appropriate responses in training and practice choices. Moreover, the committee remains concerned about the rapid changes taking place in the health care sector as a whole. It concludes that ongoing monitoring of supply and requirements is essential to ensure that appropriate public policy and private career decisions can be made.
Currently, the Bureau of the Health Professions (of the Health Resources and Services Administration [BHP/HRSA]), the Council on Graduate Medical Education
(COGME), and the National Committee on Nursing Education and Practice have responsibility for monitoring primary care clinician supply and requirements. The committee endorses their efforts and notes the recommendations from a parallel IOM committee (IOM, 1996a) on the same point. Specifically, that panel advocated (p. 90) that
the Department of Health and Human Services, chiefly through the Health Resources and Services Administration, regularly make information on physician supply and requirements and the status of career opportunities in medicine available to policymakers, educators, professional associations, and the public … [and that] the American Medical Association, the Association of American Medical Colleges, the Osteopathic Association, the American Association of Colleges of Osteopathic Medicine, and other professional associations cooperate with the federal government in widely disseminating such information to students indicating an interest in careers in medicine.
Clearly, those recommendations pertain to physicians (and to all physicians, not just those in primary care). This committee would extend that advice to include nurses (especially advanced practice nurses or NPs) and PAs (see IOM, 1996b, for a detailed discussion of the needs for better data on the nurse workforce). Nurses and PAs are health care practitioners of direct interest to BHP/HRSA. The analogous collaboration and cooperation would be sought with a wide array of professional associations, including but not limited to the American Academy of Physician Assistants, American Association of Colleges of Nursing, the American Association of Physician Assistants, American Nurses Association, the National League for Nurses, and the National Organization of Nurse Practitioner Faculties.
Apart from general monitoring of the several professions relevant to primary care (e.g., in terms of current size and composition and future projections of supply and requirements), efforts should also be made to obtain current information on the use of primary care clinicians by managed care plans and integrated health delivery systems. Of particular interest are patterns of substitution across physicians, NPs, and PAs and the impact of the complex interactions of these practitioners on health care costs, access, and quality of care. These points are revisited in Chapter 8 with respect to a primary care research agenda.
Geographic Maldistribution of the Primary Care Workforce
The committee is concerned by the continuing geographic maldistribution of the primary care workforce; there are too few clinicians in inner cities and rural areas. Despite many attempts to address this shortage, the nation simply has not adequately improved access to primary care services in these underserved areas.11 Although programs such as the National Health Service Corps have filled
the gap to some extent (especially for rural areas) (Mullan, 1995), significant disparities remain. The latest, dramatic evidence of this for physicians was presented by Cooper (1995), cited earlier; equivalently detailed information for NPs and PAs is not available.
The incompatibility between articulated public policy goals and objectives and the financing mechanisms put in place to support them have created an expansion of the physician supply without actually achieving an adequate workforce supply in underserved areas. Neither ''trickle-down" physician workforce policy nor market forces to date have been notably successful in alleviating the problems of inequitable distribution of primary care services and clinicians, across the nation.
The committee has dealt—essentially throughout this report—with the widely recognized issues of maldistribution of physicians by generalist or specialty training and practice. The problem of maldistribution by geographic location is another, and troubling, matter. The committee regards the goal of overcoming imbalances in the geographic distribution of primary care clinicians as an especially significant one. It also believes that, with the rapid changes now taking place in the private sector, managed care organizations and integrated health delivery systems have a significant duty to address this question head-on.
Recommendation 6.3 Addressing Issues of Geographic Maldistribution
The committee recommends that federal and state governments and private foundations fund research projects to explore ways in which managed care and integrated health care systems can be used to alleviate the geographic maldistribution of primary care clinicians.
For purposes of this recommendation, the committee regards rural and inner city jurisdictions as appropriate targets for such projects and for specific attempts to redress the shortage of primary care clinicians in these areas. Clearly, as between rural areas and the core metropolitan areas, the problems, the likely solutions, and the types of personnel and configurations of primary care teams are all likely to differ. In fact, rural areas themselves will vary along these dimensions, as will inner cities.
The committee believes that managed care organizations may be able to deal with some maldistribution problems where earlier efforts have not worked. For instance, integrated delivery systems that wish to expand their businesses into previously uncovered catchment areas, whether rural or inner city, can provide financial incentives, collegial relationships, and telecommunications capabilities that will attract physicians (as well as NPs and PAs) into those areas. Academic health centers may also operate community or school clinics or other types of ambulatory care networks, especially in poor sections of metropolitan areas, that essentially also represent good business and expanded catchment opportunities. The inducements may include acceptable practice sites, competitive salaries, hospital privileges, professional relationships and backup, and appropriate referral networks, but the growing scarcity of practice openings in more affluent areas should not be discounted. The precise combinations of fiscal and professional incentives that might work best for particular types of underserved areas are clearly not known today. Thus, demonstration and evaluation of current efforts would be particularly useful, in the committee's view.
The committee did not call for testing or evaluation of specific approaches that managed care and integrated systems might use to address the geographic maldistribution problems of these areas. Consistent with the principles laid out in Chapter 2, however, the committee notes that it would not subscribe to solutions that were based solely on one type of primary care clinician; it believes that innovative programs involving physicians, NPs, and PAs are more desirable, and indeed it would advocate that strategies involving the entire primary care team be investigated.
Finally, this recommendation is couched in terms of research projects and thus should be considered in conjunction with the broad research agenda laid out in Chapter 8. The committee advances it here to underscore the policy issues—specifically, a very uneven presence of primary care clinicians across the states that severely hinders any efforts to bring greater parity in access to health care services to large portions of the U.S. population. Because managed care organizations and integrated systems are gaining such a prominent role in the whole restructuring of the nation's health care system, it was felt that demonstration and evaluation projects conducted by them or under their auspices would shed the most light on how best to address this access issue. In short, the committee believes that as managed care plans and approaches expand, they bring opportunities to improve access to primary care in rural and inner city areas; that efforts to encourage that possibility are called for; and that the successes and failures of such efforts should be thoroughly understood.
Impediments to the Use of Nurse Practitioners and Physician Assistants
"Scope of practice" laws, established by the states, govern what NPs and
PAs are permitted to do. Collectively, these laws constitute a crazy quilt of permitted or disallowed practices and activities. Thus, the legal restrictions on the scope of practice for NPs and PAs in some states seriously impede the involvement of these types of personnel in primary care in some settings and circumstances.
This fact has a number of health care policy and delivery implications. For example, for managed care enterprises that operate in more than one state, the configurations they can use to organize their primary care teams may be different, depending on the state in question. It is not clear to this committee why different structures for the delivery of high-quality primary care ought to turn on what may be quite idiosyncratic or outmoded state practice acts.
Recommendation 6.4 State Practice Acts for Nurse Practitioners and Physician Assistants
The committee recommends that state governments review current restrictions on the scope of practice of primary care nurse practitioners and physician assistants and eliminate or modify those restrictions that impede collaborative practice and reduce access to quality primary care.
The committee is concerned that state statutes presently on the books create obstacles to innovative collaboration among members of primary care teams and that those ordinances by default hinder the provision of effective and efficient health care. These limitations may involve the degree and nature of supervision (such as the requirement in some states for on-site supervision of PAs), the ability to prescribe pharmaceuticals, or the ability to order other services needed by the patient without a physician's case-by-case approval.
A recent analysis of the practicing environment in 10 states for NPs and PAs assigned weighted scores regarding scope of practice, requirements for physician supervision, prescriptive and dispensing authority, reimbursement, and so forth. It found total average scores of 63.9 in these 10 states with scores ranging from 0 in Illinois and Ohio where NPs are not recognized at all, to scores over 90 in Maryland, Montana, New Hampshire, and Oregon. Similarly, PAs scores in the same states averaged 60.5 with a range from 0 in Mississippi to over 90 in Iowa, Massachusetts, and Montana (RTI, 1995).
The committee believes that more freedom to structure the divisions of duties and responsibilities should be given to the primary care team. Clearly, reconsideration by the states of these practice acts might also enable some to address their shortage-area problems (discussed earlier) more creatively as well, in part by enabling managed care organizations and integrated delivery systems to develop efficient models of primary care practice that work within their own
corporate structures and yet are adaptable to the particular needs of specific frontier, rural, or inner city populations.
Summary
This chapter has reviewed trends in the supply of the principal types of primary care clinicians—physicians, NPs, and PAs—taking care to observe the great difficulties of developing reliable and valid estimates of supply and, especially, requirements for clinicians or clinicians' services. It also briefly comments on the education and training infrastructure for such personnel, which leads into the next chapter. The present chapter then advances four recommendations concerning important directions that, in the committee's view, the production and use of primary care clinicians ought to take. These involve (1) continuing the current level of effort to increase the supply of primary care clinicians but ensuring that primary care training programs and delivery systems focus their efforts on improving the competency of primary care clinicians and on increasing access for populations not now receiving adequate primary care; (2) encouraging state and federal agencies to carefully monitor the supply of and requirements for primary care clinicians; and (3) exploring ways in which managed care and integrated health care systems might be used to alleviate the geographic maldistribution of primary care clinicians; and (4) examining how state practice acts for NPs and PAs might be amended to eliminate outmoded restrictions on practices that currently impede efficient and effective functioning of primary care teams and that reduce access to needed health care.
References
AAPA (American Academy of Physician Assistants). 1995 AAPA Membership Census Mid-Year Report, September 1995. Alexandria, Va.: AAPA, 1995.
AACN (American Association of Colleges of Nursing). 1994–1995. Special Report on: Master's and Post-Master's Nurse Practitioner Programs, Faculty Clinical Practice, Faculty Age Profiles, and Undergraduate Curriculum Expansion In Baccalaureate and Graduate Programs in Nursing . Publ. No. 94-95-4. Washington, D.C.: AACN, 1995.
AMA (American Medical Association). Physician Characteristics and Distribution in the US. 1995/1996 Edition. Chicago: AMA, 1996.
Barzansky, B., Jonas, H.S., and Etzel, S.I. Educational Programs in U.S. Medical Schools, 1994–95. Journal of the American Medical Association 274:716–722, 1995.
Birkholz, G., and Walker, D. Strategies for State Statutory Language Changes Granting Fully Independent Nurse Practitioner Practice. Nurse Practitioner 19:54–58, 1994.
BPHC (Bureau of Primary Health Care, Health Resources and Services Administration, Department of Health and Human Services). Health Professional Shortage Area (HPSA) Designations: 1978–1994. Unpublished material from the Division of Shortage Designation, March, 1995.
CCH (Commerce Clearing House). Health Security Act (President Clinton's Health Care Reform Proposal and Health Security Act). Presented to Congress on October 27, 1993. Chicago, Ill.: Commerce Clearing House, 1993.
COGME (Council on Graduate Medical Education). Recommendations to Improve Access to Health Care Through Physician Workforce Reform. Fourth report to Congress and the Department of Health and Human Services Secretary. Rockville, Md.: Health Resources and Services Administration, Department of Health and Human Services, January 1994.
COGME. COGME 1995 Physician Workforce Funding Recommendations for Department of Health and Human Services' Programs. Seventh report to Congress and the Department of Health and Human Services. Rockville, Md.: Health Resources and Services Administration, Department of Health and Human Services, June 1995.
COGME. Eighth Report. Patient Care Physician Supply and Requirements: Testing COGME Recommendations. Rockville, Md.: Health Resources and Services Administration, Department of Health and Human Services, 1996.
Cooper, R.A. Special Communication. Perspectives on the Physician Workforce to the Year 2020. Journal of the American Medical Association 274:1534–1543, 1995.
Davis, K., Collins, K.S., Schoen, C., et al. Choice Matters: Enrollees' Views of Their Health Plans. Health Affairs 14:99–112, Summer 1995.
Desmarias, H.R. Community Service in U.S. Medical Training and Practice: An Overview. In Social and Community Service in Medical Training and Professional Practice. Proceedings of a Conference. G. Herrerra, ed., assisted by G. Carrino and L.G. Herrera. New York: Josiah Macy, Jr. Foundation, 1995.
DHEW (Department of Health, Education and Welfare). Health United States 1976–1977. DHEW Publ. No. (HRA) 77-1232. Hyattsville, Md.: Department of Health, Education and Welfare, Health Resources Administration, 1977.
DHHS (Department of Health and Human Services). Factbook. Health Personnel, United States. March 1993. DHHS Publ. No. HRSA-P-AM-93-1. Washington, D.C.: Department of Health and Human Services, 1993.
Feil, E.C., Welch, H.G., and Fisher, E.S. Why Estimates of Physician Supply and Requirements Disagree. Journal of the American Medical Association 269:2659–2663, 1993.
Gamliel, S., Politzer, R.M., Rivo, M.L., et al. Managed Care on the March: Will Physicians Meet the Challenge? Health Affairs 14:131–142, Summer 1995.
GMENAC (Graduate Medical Education National Advisory Committee). Summary Report to the Secretary, Department of Health and Human Services . Vol. 1. DHHS Publ. No. (HRA) 81-651. Washington, D.C.: Health Resources Administration, Department of Health and Human Services, April 1981.
Henderson, T., and Chovan, T. Removing Practice Barriers of Nonphysician Providers: Efforts by States to Improve Access to Primary Care. Washington, D.C.: Intergovernmental Health Policy Project, The George Washington University, 1994.
IOM (Institute of Medicine). A Manpower Policy for Primary Health Care: Report of a Study. Washington, D.C.: National Academy Press, 1978.
IOM. Assessing Health Care Reform. M.J. Field, K.N. Lohr, and K.D. Yordy, eds. Washington, D.C.:National Academy Press, 1993.
IOM. Balancing the Scales of Opportunity: Ensuring Racial and Ethnic Diversity in the Health Professions. M. E. Lewin and B. Rice, eds. Washington, D.C.: National Academy Press, 1994.
IOM. Dental Education at the Crossroads: Challenge and Change. M.J. Field, ed. Washington, D.C.: National Academy Press, 1995a.
IOM. Health Services Research: Work Force and Educational Issues. M.J. Field, R.E. Tranquada, and J.C. Feasley, eds. Washington, D.C.: National Academy Press, 1995b.
IOM. Nursing, Health, and the Environment: Strengthening the Relationship to Improve the Public's Health. A.M. Pope, M.A. Snyder, and L.H. Mood, eds. Washington, D.C.: National Academy Press, 1995c.
IOM. The Nation's Physician Workforce: Options for Balancing Supply and Requirements. K.N. Lohr, N.A. Vanselow, and D.E. Detmer, eds. Washington, D.C.: National Academy Press, 1996a.
IOM. Nursing Staff in Hospitals and Nursing Homes: Is It Adequate? G.S. Wunderlich, F. Sloan, and C.K. Davis, eds. Washington, D.C.: National Academy Press, 1996b.
JAMA (Journal of the American Medical Association). Appendix II. Graduate Medical Education. Appendix II, Table 1. Resident Physicians on Duty in ACGME-Accredited and in Combined Specialty Graduate Medical Education (GME) Programs in 1993. Journal of the American Medical Association 272:725–726, 1994.
Jonas, H.S., Etzel, S.I., and Barzansky, B. Educational Programs in U.S. Medical Schools, 1993–1994. Journal of the American Medical Association 272:694–701, 1994.
Jones, P.E., and Cawley, J.F. Physician Assistants and Health System Reform: Clinical Capabilities, Practice Activities and Potential Roles. Journal of the American Medical Association 271:1266–1272, 1994.
Kindig, C.A. Counting Generalist Physicians. Journal of the American Medical Association 271:1505–1507, 1994.
Kindig, D.A., Cultice, J.M., and Mullan, F. The Elusive Generalist Physician. Can We Reach a 50% Goal? Journal of the American Medical Association 270:1069–1073, 1993.
Lee, R.C. Current Approaches to Shortage Area Designation. Journal of Rural Health 7(4 Supl.):437–450, 1991.
Morgan, W.A. Using State Board of Nursing Data to Estimate the Number of Nurse Practitioners in the United States. Nurse Practitioner 18:65–66, 69–70, and 73–74, 1993.
Moses, E. The Registered Nurse Population: Findings from the National Sample Survey of Registered Nurses, 1992. Division of Nursing, Health Resources and Services Administration, Public Health Service. Washington, D.C.: U.S. Government Printing Office, 1994.
Mullan, F. The National Health Service Corps: Service Conditional Medical Education in the United States. In: Social and Community Service in Medical Training and Professional Practice. Proceedings of a Conference. G. Herrera, ed., assisted by G. Carrino and L.G. Herrera. New York: The Josiah Macy, Jr., Foundation, 1995.
NCHS (National Center for Health Statistics). Health, United States, and Prevention Profile, 1983. DHHS Publ. No. (PHS) 84-1232. Washington, D.C.: U.S. Government Printing Office, December 1983.
Newhouse, J.P., Williams, A.P., Bennett, B.W., and Schwartz, W.B. Where Have All the Doctors Gone? Journal of the American Medical Association 247:2392–2396, 1982a.
Newhouse, J.P., Williams, A.P., Schwartz, W.B., and Bennett, B.W. The Geographic Distribution of Physicians: Is the Conventional Wisdom Correct? Publ. No. R-2734-HJK/HHS/RWJ/RC. Santa Monica, Calif.: RAND Corporation, 1982b.
NLN (National League of Nursing). Nursing Datasource 1994. Volume 1, Graduate Education in Nursing. Advanced Practice Nursing Pub. No. 19-2643. New York: NLN Press, 1994.
NRC (National Research Council). Meeting the Nation's Needs for Biomedical and Behavioral Scientists. Washington, D.C.: National Academy Press, 1994.
Pearson, L. Annual Update of How Each State Stands on Legislative Issues Affecting Advanced Nursing Practice. Nurse Practitioner 19:11–53, 1994.
Pew Health Professions Commission. Critical Challenges: Revitalizing the Health Professions for the Twenty-First Century. San Francisco: Pew Health Professions Commission, 1995.
PPRC (Physician Payment Review Commission). Annual Report to Congress, 1992. Washington, D.C.: PPRC, 1992.
PPRC. Annual Report to Congress, 1994. Washington, D.C.: PPRC, 1994.
PPRC. The Changing Labor Market for Physicians. Chapter 14 in Annual Report to Congress, 1995. Washington, D.C.: PPRC, 1995.
ProPAC (Prospective Payment Assessment Commission). Report and Recommendations to Congress, March 1, 1995. Washington, D.C.: ProPAC, 1995.
Rivo, M.L., and Satcher, D. Improving Access to Health Care Through Physician Workforce Reform. Directions for the 21st Century. Journal of the American Medical Association 270:1074–1078, 1993.
RTI (Research Triangle Institute). Characteristics of Practice Environments for Nurse Practitioners and for Physician Assistants. Final Report Deliverable Item 13. Research Triangle Park, N.C.: RTI, July 7, 1995.
Scheffler, R.M., and Gillings, D.B. Survey Approach to Estimating Demand for Physician Assistants. Social Science and Medicine 16:1039–1047, 1982.
Schwartz, W.B., Newhouse, J.P., Bennett, B.W., et al. The Changing Geographic Distribution of Board-Certified Physicians. New England Journal of Medicine 303:1032–1038, 1980.
Singer, A.M. 1994 Annual Statistical Report. Rockville, Md.: American Association of Colleges of Osteopathic Medicine, 1994.
Tarlov, A.R. Estimating Physician Workforce Requirements. The Devil Is in the Assumptions. Journal of the American Medical Association 274:1558–1559, 1995.
Washington Consulting Group. Survey of Certified Nurse Practitioners and Clinical Nurse Specialists: December 1992 Final Report to the Bureau of Health Professions. Washington, D.C.: U.S. Government Printing Office, 1994.
Weiner, J.P. Assessing the Impact of Managed Care on the U.S. Physician Workforce. Policy paper commissioned by the Bureau of Health Professions of the U.S. Department of Health and Human Services on behalf of the Council on Graduate Medical Education. Supported by HRSA P.O. No. 03-339-P. Baltimore, Md.: Weiner, Johns Hopkins University School of Hygiene and Public Health, November, 1993.
Weiner, J.P. Forecasting the Effects of Health Reform on U.S. Physician Workforce Requirement: Evidence from HMO Staffing Patterns. Journal of the American Medical Association 272:222–230, 1994.
Whitcomb, M.E. The Role of Medical Schools in Graduate Medical Education. Journal of the American Medical Association 272:702–704, 1994.
Williams, A.P., Schwartz, W.B., Newhouse, J.P., and Bennett, B.W. How Many Miles to the Doctor? New England Journal of Medicine 309:958–963, 1981.































