6
Establishing an Effective National System to Prevent STDs
The committee concludes that prevention of STDs is technically feasible today in the United States, but an effective national system for STD prevention currently does not exist, and, as a result, STDs are a severe health burden in the United States. Many components of an effective system for STD prevention (described in Chapters 4 and 5), such as a surveillance system to measure STD incidence, public and private sector clinical services, and public education programs, exist in many areas in various stages of development, but these and other components are neither adequate nor coordinated locally, statewide, or nationally.
As outlined in the previous chapters, the current strategy for preventing STDs is based primarily on categorical STD programs run by state and local health departments with guidance and funding from the CDC. Other federal agencies, including the U.S. Department of Justice (Bureau of Prisons), the Agency for Health Care Policy and Research, the Food and Drug Administration, the Health Care Financing Administration, the Health Services and Resources Administration, the Indian Health Service, the National Institutes of Health, the Office of Population Affairs (Department of Health and Human Services), and the Substance Abuse and Mental Health Services Administration, also provide or support STD-related services or research, as do their state and local counterparts.
Public health agencies, private practitioners and medical groups, and community-based clinics all provide STD-related services, but many providers work in relative isolation. Dedicated public STD clinics, family planning clinics, and other community-based clinics serve the uninsured and other populations at high risk for STDs, but often do not coordinate their services. Publicly sponsored STD
programs consider containment of STDs to be their primary mission, but collaborate with other public sector health programs infrequently and even less often with private sector health programs. Federal demonstration projects to prevent infertility associated with chlamydial and gonococcal infections, however, are beginning to improve service coordination among family planning clinics, dedicated public STD clinics, and public sector laboratories. In addition, private sector health care professionals often do not recognize the importance of their role in preventing STDs.
The lack of an effective system is particularly acute for noncurative prevention programs for STDs, which are far less developed than programs for curative services. In addition, despite the interrelationship between STDs, HIV infection, unintended pregnancy, and cancer, prevention programs for these health conditions are typically neither integrated nor coordinated.
The fragmented system of STD-related services directly hinders effective prevention of STDs in many ways. For example, as described in Chapter 5, the national surveillance system collects information regarding reportable STDs among persons who use public STD clinics and community-based services. However, information about the privately insured population is incomplete because many private clinicians do not report STD cases and some cases are presumptively treated. Without a comprehensive system for surveillance that involves all potential caregivers for STDs, it is difficult to accurately monitor disease trends or effectiveness of interventions.
A fragmented system of clinical services can result in lapses in coverage and ineffective treatment. As documented in Chapter 5, STD-related clinical care is provided by a variety of clinicians in many settings, and the training of these clinicians, including physicians, in diagnosis, treatment, and prevention of STDs is inadequate. Despite the growing role of private sector primary health care professionals in delivering services, there are large gaps in health professional school training and continuing education regarding STD-related skills. Inadequate training and poor awareness of STDs perpetuates the lack of involvement in prevention activities, such as evaluation and treatment of sex partners, by health plans and private practice clinicians. Inadequate training and poor awareness of STDs among health care professionals also result in clinicians who may fail to diagnose and treat STDs or do not have the skills or confidence to promote behavior change in their patients. The failure to adequately diagnose and treat STDs or become involved in certain prevention activities, therefore, leads to lost clinical opportunities to prevent STDs, and thus, to incomplete or fragmented clinical services.
As discussed in Chapter 5, because health plans do not assume responsibility for those who are not plan members, there is no assurance that sex partners of infected plan members will receive appropriate evaluation and treatment. In prisons and jails, prisoners may be screened and found to be positive for an STD, but may be released before treatment is given. Without linkages to community providers,
their infections will likely go untreated and spread to others in the community at large. As a final example, a fragmented system of information and educational services for STDs can result in inadequate awareness and misperceptions of risk. Data presented in Chapters 3 and 4 show that awareness of STDs in the United States is low and misperceptions of risk are common, even among those at highest risk for STDs. This is likely a result of the lack of open public education about STDs and the failure of the mass media to provide accurate information regarding the consequences of high-risk sexual behavior.
To develop an effective system for STD prevention, many existing programs need to be redesigned and improved through innovative approaches and closer collaboration. In addition, new programs and initiatives that address important gaps in the current fragmented system of prevention services need to be designed and implemented. In this chapter, the committee proposes an effective national system of STD prevention that can be developed from the currently fragmented set of services and funding streams for STDs. Unless otherwise indicated, the background and support for the committee's strategic plan for reducing the adverse health and economic impact of STDs in the United States are found in Chapters 2 through 5.
Laying The Foundation For A National System
In formulating a national strategy to prevent STDs, the committee developed the following vision statement and principles to guide its deliberations (Box 6-1).
To realize this vision, the committee recommends that:
- An effective national system for STD prevention be established in the United States.
The committee uses the word ''system" to describe an interacting or independent group of services and organizations that function as a whole. By an "effective" system, the committee means a system that is coherent, comprehensive, and coordinated. A coherent system is founded on a clear strategy for prevention that ensures that the components of the system are logically consistent and synergistic. A comprehensive system fully utilizes all types of relevant approaches and effective interventions. A coordinated system ensures that the components of the system relate to each other in order to maximize efficiency and effectiveness. By a "national" system, the committee means a system that is based on a national policy coordinated at all levels and composed of local, state, and national (including federal) programs. A nationally coordinated system is necessary because STDs are a threat to the nation's health and do not recognize geographic borders. In addition, many interventions are most effectively or efficiently developed and implemented at the national level. It is expected that state and local systems will be developed and implemented concurrently and coordinated at all levels. Coordination
of interventions for HIV infection and other STDs, in particular, is an important aspect of an effective national system.
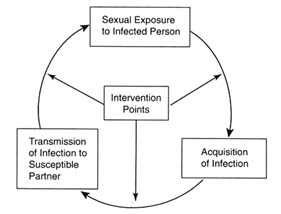
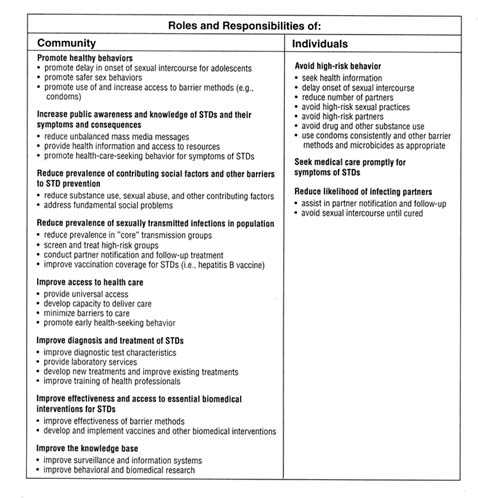
An effective national system for STD prevention should: (a) provide comprehensive curative and noncurative preventive services; (b) provide STD-related services in the context of primary care; (c) coordinate public and private sector services; (d) coordinate local, state, and federal programs; and (e) ensure universal access to STD-related services for all persons in the United States. The committee proposes a model for carrying out the functions of a national system for prevention in the context of community and individual roles and responsibilities in Figure 6-1.
In the context of the model, the term "community" refers to all persons and entities that have a potential role in STD prevention besides the individual. The committee's model is based on the recognition that both individuals and the community have a role and responsibilities in preventing STDs. In some cases, such as reducing high-risk behaviors, the degree of individual responsibility may exceed that of the community. Even then, however, the community plays a role in setting social norms and providing the knowledge and resources needed for behavior change to occur. In other cases, such as ensuring access to health care, the community's responsibility is clearly greater. Many responsibilities and functions are best shared; many overlap and are related; and some will likely change as the system evolves or as conditions warrant. In addition, responsibilities for specific functions need to be tailored to the local community environment. In the case of STDs, the committee believes that communities have a special responsibility to become involved because STDs and other communicable diseases threaten the health of the community at large, not just the infected individual. In addition, many of the underlying factors that contribute to the STD epidemic, such as lack of awareness, lack of access to health care, and unbalanced messages regarding sexual behavior, are most effectively addressed through community-based interventions.
The committee believes that it is inappropriate to advocate that the STD epidemic be solved by individuals without the support of community interventions. It is the community's responsibility to provide individuals with the support, information, and tools that are needed to prevent STDs. Many factors that are often beyond the control of the individual, especially sociocultural factors, directly influence individual behavior and risk of STDs (Wasserheit, 1994).
It has been proposed that the various biomedical and behavioral health professionals currently involved in STD prevention, including clinicians, epidemiologists, public health workers, microbiologists, psychologists, and social scientists, develop and participate in interdisciplinary approaches to prevention (Sparling and Aral, 1991). The committee proposes that an even wider range of individuals and institutions is needed. In addition to the professionals mentioned above, health plans, pharmaceutical and medical device companies, educators, and other individuals and entities that have not traditionally been involved in
|
BOX 6-1 Vision and Guiding Principles for a National System for STD Prevention Vision An effective system of services and information that supports individuals, families, and communities in preventing STDs including HIV infection, and ensures comprehensive, high-quality STD-related health services for all persons Guiding Principles Prevention STDs can be prevented by implementing individual- and population-based interventions that:
Responsibility In an effective system for STD prevention:
Implementation/Operational Issues An effective system for STD prevention should have:
Access and Financing An effective system for STD prevention should have:
|
STD prevention should also become involved. These include mass media companies, social service agencies, employers and businesses, labor unions, religious organizations, and other community-based organizations. A list of potential stakeholders in the community envisioned in the model system is presented in Table 6-1. Given the wide spectrum of stakeholders in STD prevention, the committee advocates a substantial emphasis on coordination and collaboration (IOM, 1996a).
The committee's proposed system is founded on the simple infectious disease prevention model of (a) preventing exposure to infection, (b) preventing acquisition of infection when exposed, and (c) preventing transmission to others once infected. In this system, there are multiple points at which to intervene and multiple approaches or interventions at both the individual and the community levels. Programs that focus only on preventing exposure, acquisition, or transmission are unlikely to succeed because no single intervention is totally effective in isolation. Although existing interventions are not perfect, they can have an additive impact in reducing the risk of STDs in the population (Cates, 1996). Therefore,
| Complete Box on previous page. |
resources committed to multiple intervention points are necessary. An effective system must have both behavioral and biomedical approaches that are complementary and intertwined. Biomedical interventions may be ineffective without behavioral components to support them, and behavioral approaches must incorporate biomedical tools for prevention.
The committee's model is consistent with the multifaceted, holistic approaches for STD and HIV prevention previously advocated by several experts in STDs (Sparling and Aral, 1991; Wasserheit, 1994; Stryker et al., 1995; Cates, 1996). Similar approaches cited in Chapter 4, such as Wisconsin's comprehensive chlamydial prevention program, have been successful. While primarily a screening program, this initiative included public-private partnerships, leadership from legislators, expanded laboratory services, expanded screening in family planning and STD clinics, education of health care professionals, and integrated information systems. Another example of a successful multifaceted program implemented on a national level is the Thai "100% Condom Program" as described
TABLE 6-1 Potential Community Stakeholders in STD Prevention
|
Academic Health Centers |
|
Schools of medicine, dentistry, nursing, pharmacy, public health, allied health, and related other health-disciplines |
|
Biomedical and Social Science Researchers |
|
Universities; private industry; government agencies |
|
Biomedical Industry |
|
Pharmaceutical, biotechnology, and medical device companies |
|
Businesses and Organized Labor |
|
Small businesses; corporations; labor unions |
|
Clinical Laboratories |
|
Public sector laboratories; hospital and private laboratories |
|
Community-Based Organizations |
|
Voluntary organizations; churches, synagogues, and other religious organizations; private social service agencies and programs for women, children, runaways, homeless, migrants |
|
Government Agencies and Programs |
|
Federal agencies (e.g., AHCPR, CDC, FDA, HCFA, HRSA, IHS, NIH, SAMSHA, Department of Justice); state and local health departments; government social service agencies and programs for special populations (e.g., women, children, runaways, homeless, migrants) |
|
Health Care Professionals and Organizations |
|
Physicians, nurses, pharmacists and other health care professionals; managed care organizations and other health plans; hospitals (emergency rooms); community health centers; health professional organizations, including medical societies and member organizations |
|
Health Programs for High-Risk Populations |
|
Juvenile detention health services; jail and prison health services; drug and alcohol treatment programs; migrant health programs; health programs for the homeless |
|
Individuals and Families |
|
Mass Media |
|
Television; radio; print and electronic media; commercial sponsors and advertisers |
|
Policymakers |
|
Federal, state, and local legislators; government health agency leaders; private health care sector leaders |
|
Private Foundations |
|
Purchasers of Health Services |
|
Private employers; government employee benefits groups; purchasing coalitions; Medicaid and other publicly sponsored programs |
|
School-Based Programs |
|
K-12 school-based programs; educators; school administrators; school boards; college and university health services |
|
STD-Related Programs and Clinics |
|
Dedicated public STD clinics; family planning clinics, prenatal clinics, HIV clinics |
in Chapter 4. With a mass media advertising campaign to change risky sexual behaviors, increased access to condoms, and environmental interventions, this initiative seemed to be highly successful because it involved high-level government and community leaders, different sectors of government (e.g., health, education, and law enforcement agencies), and businesses (owners of commercial sex establishments). Coupled with programs to provide STD-related services, this initiative led to substantial positive behavior change among young men, and the incidence of HIV infections declined.
Formulating a National Policy and Strategy
A national system for STD prevention must be based on sound national policy and a coherent strategy. Currently, a comprehensive national policy regarding STD prevention does not exist. The elements of a national strategy to prevent bacterial STDs are more fully developed than those needed to prevent viral STDs, for which a national strategy for prevention is not well articulated. Furthermore, a national strategy to prevent STD risk behaviors has not been developed. Since almost all sexually transmitted pathogens that infect people do not have animal reservoirs, many STDs can theoretically be eradicated. Although this goal is probably not attainable in the near future for many STDs, it may be an appropriate intermediate-term goal for some STDs. For example, Sweden has virtually eliminated transmission of three major STDs (syphilis, gonorrhea, and chancroid) among the native population, and several U.S. states have reduced transmission of syphilis and chancroid to very low levels. The committee believes that elimination of ongoing transmission of syphilis within the United States is an attainable goal that should now be attempted.
To establish a national system for STD prevention, the committee recommends four major strategies for public and private sector policymakers at the local, state, and national levels:
- Overcome barriers to adoption of healthy sexual behaviors.
- Develop strong leadership, strengthen investment, and improve information systems for STD prevention.
- Design and implement essential STD-related services in innovative ways for adolescents and underserved populations.
- Ensure access to and quality of essential clinical services for STDs.
The establishment of an effective national system for STD prevention and implementation of these strategies is a difficult, long-term process that involves intermediary steps. Efforts consistent with these strategies should be initiated immediately and concurrently. The committee suggests that the Department of Health and Human Services consider the goals and strategies outlined in this
report in developing and updating its national health objectives (e.g., Healthy People 2000) related to STDs.
In the committee's strategic plan for an effective national system for STD prevention, four strategies and a number of tactics are presented. Because of the comprehensive nature of the committee's approach, implementation of all the recommended tactics may seem daunting to some communities. While the committee believes that each component of the national system identified in its deliberations is essential to preventing STDs, it recognizes that not all communities will be able to, or need to, implement every tactic described in this chapter. In addition, it is likely that many communities will need to adapt some of the committee's recommendations to maximize their effectiveness under local conditions. The committee purposely has not prioritized the recommendations in this report because it believes that this process should be locally driven. Which interventions are most effective for a particular community will vary depending on the local epidemiology of STDs, the status of STD-related services, and the prevalence of STD risk behaviors. For example, in areas where rates of STDs and risky behaviors are low and access to clinical services for STDs is problematic, improving training of and access to primary care providers and interventions to maintain low rates of risky behaviors may be emphasized. In contrast, in communities where rates of STDs and risky behaviors are high, outreach to health plans, improving public STD clinics, and community-based behavioral interventions may be priorities. The committee proposes that the local health department and community representatives collaboratively prioritize the recommended tactics in this chapter.
The committee's recommendations for accomplishing its vision for STD prevention are presented in the remainder of this chapter. Before turning to these recommendations, however, the committee first discusses and makes recommendations about two important concepts that need to be considered in formulating a national strategy for STD prevention: the impact of STDs on HIV transmission and the impact of STDs on cancer.
Recognizing the Impact of STDs on HIV Transmission
Studies cited in Chapter 2 show that STDs increase the risk of HIV acquisition and transmission. Individuals infected with an STD are more likely to acquire HIV infection when exposed, and individuals coinfected with HIV and another STD are more likely to transmit HIV to their sex partners. Mathematical models and epidemiologic and biologic data collectively provide strong evidence that improved prevention of STDs would reduce sexual transmission of HIV in this country. A major study has shown that improved management of STDs through extensive training of primary health workers, ensuring treatment for STDs, and promoting health-seeking behavior for STDs can significantly reduce the incidence of HIV infection in communities (Grosskurth et al., 1995). Although initial studies documenting the impact of STD prevention on HIV transmission
have been conducted in other countries, current estimates suggest that a large proportion of heterosexually transmitted HIV infections could be prevented by reducing the prevalence of STDs in the United States.
The interrelationship between HIV infection and other STDs is clearly documented and supports the concept that prevention of other STDs should be an essential component of HIV prevention programs. As discussed in Chapters 2 and 3, many of the populations at high risk for STDs are also at high risk for HIV infection. Interventions designed to increase awareness of HIV infection or other STDs and to reduce high-risk sexual behavior (such as condom promotion) are likely to have a positive impact on prevention of both HIV infection and other STDs. Therefore, programs for HIV and STD prevention, especially those focused on similar populations, need to be coordinated to maximize the effectiveness and efficiency of both intervention efforts. Educational programs for HIV prevention should disseminate information related to other STDs without making the message too diffuse. Examples of public messages that may not be widely known include: (a) HIV infection is not the only STD with serious health consequences, (b) other STDs increase the risk for HIV infection, (c) condoms and safer sex behaviors prevent both HIV infection and other STDs, (d) the cardinal signs of STDs (e.g., genital sores or discharge or pelvic pain in women), and (e) prompt treatment for STDs prevents complications. Similarly, STD and HIV surveillance systems and research studies need to improve monitoring and assessment of the impact of interventions on both HIV infection and other STDs. For example, population-based serosurveys for HIV infection should also include testing for other STDs, and both HIV and other STD infection rates should be used as outcome measures when evaluating effectiveness of interventions as appropriate. The committee also believes that greater access to STD-related services in clinical HIV programs could reduce sexual transmission of HIV.
During the past several years, far more attention has been given to developing HIV prevention than to other STD prevention programs. The strong interest in HIV prevention is justified, but inadequately addresses the prevention of other STDs. HIV prevention programs should support the incorporation of STD prevention activities into HIV prevention efforts. It is important to integrate and coordinate STD and HIV prevention activities without weakening either effort. The intent of the committee is not to divert resources away from HIV prevention efforts to prevention of other STDs, but rather to increase investment in prevention of all STDs.
Therefore, the committee makes the following recommendation:
- Improved prevention of STDs should be an essential component of a national strategy for preventing sexually transmitted HIV infection. As part of this effort, federal, state, and local health agencies should review current HIV and STD programs and should coordinate STD and HIV activities related to health education and prevention, clinical services, surveillance, and research and
- evaluation that focus on similar populations. The Health Resources and Services Administration and the CDC should develop financial incentives for communities to demonstrate coordination of STD- and HIV-related services. At a minimum, health agencies should ensure that:
- educational activities for STD and HIV prevention focused on similar populations include information on both HIV infection and other STDs;
- HIV prevention programs incorporate STD prevention activities and commit necessary resources to improve these activities;
- program managers of STD- and HIV-related programs develop a formal mechanism for regular communication and for coordinating program planning, implementation, and evaluation;
- STD and HIV program staff are educated regarding the relationship between STDs and HIV transmission;
- clinicians are educated about the importance of early diagnosis and treatment of STDs to reduce the risk of sexually transmitted HIV infection;
- public STD and HIV clinics, including HIV testing and counseling sites, provide both STD- and HIV-related clinical services to the extent appropriate for the clinical setting;
- HIV and STD surveillance and data collection activities gather information on both HIV and other STDs when appropriate;
- epidemiological, behavioral, and biomedical studies examine the relationship between HIV infection and other STDs;
- evaluations of STD and HIV interventions examine the impact of the interventions on both HIV infection and other STDs; and
- HIV/AIDS clinical programs in health plans are encouraged to provide clinical services for other STDs, and HIV prevention programs in health plans also provide interventions for other STDs.
Recognizing the Impact of STDs on Cancer
Several cancers, including cervical, liver, and other cancers, are associated with sexually transmitted infections that are typically acquired during adolescence or early adulthood. The association between STDs and cancer supports the incorporation of STD prevention information, especially information regarding human papillomavirus and hepatitis B virus infection, into appropriate cancer prevention programs. Specific strategies now available for preventing STD-associated cancers that should be expanded include behavioral interventions to prevent risky sexual behaviors, Pap smears for early detection of cervical cancer in women not currently reached by existing programs, and hepatitis B vaccination. Supporting STD prevention as a strategy for preventing cancer is indicated because many STD-related cancers are not curable and are potentially fatal. In addition, preventing and treating STDs is less costly than treatment for cancer.
The role of STDs in cervical, liver, and other cancers is not well recognized by health professionals and the public, and information regarding this link needs to be disseminated widely.
Therefore, the committee makes the following recommendation:
- Government agencies and private organizations concerned with cancer prevention should support STD prevention activities as an important strategy for prevention of STD-related cancers. Agencies and organizations that fund research and other activities in cancer prevention (e.g., the National Cancer Institute at the National Institutes of Health, the American Cancer Society) should support biomedical and prevention-oriented research and programs related to STDs, and they should expand their public education efforts to include prevention of STDs as a means of preventing cervical, liver, and other STD-related cancers. As with the prevention of many cancers, prevention efforts for STD-related cancers should focus on the challenge of linking behaviors initiated during adolescence and young adulthood with health consequences that manifest much later in life.
The committee's discussion of, and recommended tactics for implementing, its four strategies for establishing a national system for STD prevention are now presented.
Strategy 1:
Promote Healthy Sexual Behaviors
Strategy 1 is to overcome barriers to adoption of healthy sexual behaviors. Barriers to effective STD prevention efforts include biological, social, and structural factors. Biological factors reviewed in Chapters 2 and 3 include preexisting or concurrent STDs, the impact of asymptomatic infections, the long lag time to clinical complications, increased susceptibility of women and female adolescents to sexually transmitted pathogens, lack of curative treatment for viral STDs, lack of vaccines against most STDs, and immunological factors. Many of these factors are difficult to alter. In addition, some social factors, such as poverty, inadequate access to health care, substance use, sexual abuse, and violence, are enormously complex issues, with solutions beyond the scope of this committee. However, the committee believes that the major social factor that contributes to the STD epidemic-the reluctance of American society to openly confront issues regarding sexuality and STDs-can eventually be overcome by a concerted long-term national effort. This issue is a major focus of Strategy 1. Tactics for addressing structural factors, such as the organization of clinical services, are described under Strategy 4.
Under Strategy 1, the committee recommends that (a) a new social norm of healthy sexual behavior be established, (b) knowledge and awareness of STDs be increased; (c) the mass media assist in efforts to reduce risky sexual behaviors;
(d) clinicians and others be trained to address sexual health issues; and (e) research regarding sexual health behaviors be supported.
Catalyzing Change Through Open Discussion
A new social norm of healthy sexual behavior should be the basis for long-term prevention of STDs. This is because, as discussed in Chapter 4, in one way or another, all interventions to prevent STDs are partly dependent on, and must be integrated with, healthy behaviors. Despite the progress made in improving awareness of protective behaviors as a result of HIV prevention efforts in recent years, there is still a substantial gap between current practices and the desired social norm of healthy sexual behavior.
The committee expects that the definition of ''healthy sexual behavior" and its interpretation will vary substantially among individuals and communities. The National Commission on Adolescent Sexual Health has identified the characteristics and behaviors of a "sexually healthy adolescent" in the context of the adolescent's relationship to self, parents and other family members, peers, and romantic partners (NCASH, 1995). The committee believes that many of the attributes and characteristics of a "sexually healthy adolescent" that are described in this consensus statement, which has been endorsed by 48 national organizations, also are relevant in considering the parameters and components of a social norm of healthy sexual behavior for adults.
It is clear that a new social norm regarding healthy sexual behavior is a long-term goal, and cannot occur without intermediate steps and bold initiatives. In order for societal norms regarding sexual behavior to change, open discussion of and access to information regarding sexual behaviors, their health consequences, and methods for protecting against STDs must occur. These issues need to be openly discussed in both private (between partners and among families) and in public arenas. Open discussion is important because history has shown that moralistic approaches against STDs, including censorship, have hindered the ability of public health officials and programs to successfully prevent these diseases. The means to achieve a new norm of healthy sexual behavior include mass media interventions, school-based programs, and population- and individual-based interventions. The committee makes specific recommendations regarding these efforts later in this chapter. In Chapter 3, the committee showed how constraints on acknowledging and discussing issues related to sexuality impede sexuality education programs for adolescents, hinder communication regarding protective behaviors between sex partners, promote misleading messages from mass media, and hamper education and counseling activities of health care professionals. Little is known about the basis for the reluctance of many in American society to acknowledge and openly discuss sexuality and its health consequences. In addition, lack of open communication and information regarding sexuality fosters misperceptions and may actually encourage high-risk sexual behaviors.
The committee believes that a significant national Campaign to catalyze social change toward a new norm of healthy sexual behavior in the United States is necessary. Highly visible leadership and active participation of nationally recognized opinion leaders are particularly important in promoting open public discussions regarding healthy sexual behaviors and STDs. These opinion leaders are also essential as role models for social change. Leadership at the highest levels, especially from elected officials, is also needed to ensure that a national Campaign to change social norms of sexual behavior is sufficiently visible.
The committee recognizes that the CDC is the primary federal agency with responsibility for STD prevention on a national level, and believes that the CDC should continue to be a leader in federal agency efforts in this area. However, the committee is concerned that the CDC or any other government agency would be unable to fully promote public awareness of healthy sexual behaviors and establish a comprehensive national system of prevention services. Political constraints too often prevent government agencies from adequately addressing controversial issues associated with STD-related programs. Based on experience with past initiatives, limitations on government agencies regarding public education programs related to sexuality are particularly problematic. Therefore, an independent entity is needed to promote a social norm of healthy sexual behavior. Because of their independence, nonpartisanship, and resources, private foundations are particularly well suited to provide leadership and support for a bold national campaign in this area.
There are several examples of independent, nonpartisan organizations that have been established around other controversial health issues and appear to be successful in developing wide support for their missions. Two major recently established initiatives include the National Campaign to Prevent Teenage Pregnancy and the National Center for Tobacco-Free Kids. The campaign was formed "to prevent teen pregnancy by supporting values and stimulating actions that are consistent with a pregnancy-free adolescence." The center was founded to prevent tobacco use among children and has a mandate "to change the social environment and public policies to reduce tobacco use by children." These organizations were established in 1996 with initial funding primarily from private foundations and other organizations. Both the National Campaign to Prevent Teenage Pregnancy and the National Center for Tobacco-Free Kids have attracted a broad range of participants, including representatives from a wide array of health, religious, business, and community organizations, as well as political leaders. An example of an independent, nonpartisan organization that was effective in changing social norms around a major social health problem is MADD (Mothers Against Drunk Driving). Since 1980, this organization has successfully promoted both social (e.g., improving public knowledge, awareness, and practices) and structural changes (i.e., legislation) to reduce the practice of driving under the influence of alcohol. It seems that this behavior recently has become socially unacceptable.
The spectrum of agencies and organizations involved in STD prevention and the controversial nature of STD-related programs require that the proposed Campaign be nonpartisan and independent, especially from special interests and political constraints. The Campaign's work would be developed by its participants, and it is the committee's hope that the Campaign will use this report as a blueprint for its initial efforts.
Therefore, the committee makes the following recommendation:
- An independent, long-term, national Campaign should be established to serve as a catalyst for social change toward a new norm of healthy sexual behavior in the United States. This Campaign should:
- provide new, highly visible leadership to promote healthy sexual behaviors and the implementation of a national system for STD prevention;
- promote public discussion and awareness of healthy sexual behaviors and STDs among all population groups;
- provide assistance to local community efforts to promote a new norm of healthy sexual behavior;
- advocate for additional public and private investment in STD prevention;
- work collaboratively with existing campaigns and other activities to prevent HIV infection, unintended pregnancy, and STD-associated cancers;
- include nationally recognized public opinion leaders such as entertainment industry representatives, sports figures, business and labor leaders, elected officials and other policymakers, and mass media executives as members;
- represent the spectrum of perspectives on STDs and sexual health issues; and
- be funded by a broad range of sponsors, including private foundations, private sector health plans, the biomedical industry, employers, and the Department of Health and Human Services. The Campaign should be funded primarily by a coalition of private foundations with an interest in STDs; these foundations should provide leadership for initiating and maintaining the Campaign and provide "seed" money to establish it.
Promoting Knowledge and Awareness
As shown in Chapter 2, the scope of STDs and their consequences is broad. STDs infect all population groups in the United States. They can cause health problems for all infected persons, but the complications are most severe for women and their infants. Surveys cited in Chapter 3 show that there is little recognition of the spectrum of health consequences of STDs. In particular, the contribution of STDs to severe health complications, such as genital and liver cancer, pelvic inflammatory disease, ectopic pregnancy, infertility, chronic liver
disease, neurological disorders, and perinatal illness, is not well known or understood by policymakers, many health professionals, or the general public.
In Chapter 3, the committee found that a major barrier to healthy sexual behavior is the lack of awareness regarding STDs and misperception of individual risk, especially among adolescents and young adults. The committee also found that accurate information is important in preventing misperceptions of risk. Programs to promote STD awareness and education, therefore, should result in increased motivation to prevent STDs. Increasing awareness of STDs among health professionals is important because it encourages clinicians to evaluate their patients for STDs when appropriate, thus improving the likelihood of early detection and treatment.
A national initiative to increase public awareness of STDs requires active participation of, and support from, various agencies and organizations from both the private and public sectors. Because of the sensitive nature of effective STD education programs, and the potential constraints upon government-run educational campaigns, an independent organization should develop and implement an appropriate STD education initiative. Along with a national educational initiative, however, it should be recognized that barriers to implementing healthy behaviors also must be reduced. Public health agencies and private health care professionals have a responsibility both to educate and to provide accurate public health information to the community, because providing disease prevention information is an essential component of clinical practice.
Innovative methods for increasing awareness and reaching the public need to be developed. Recent advances in information technology will have a great impact on access to health information among both health professionals and segments of the public. These new technologies should be harnessed to improve awareness and knowledge of STDs and ways to avoid them. Appropriate methods of disseminating information on STDs and local health services include the use of hotlines and evolving information technology, such as the Internet and other electronic methods of disseminating information. The Internet may be an especially effective method for disseminating information to adolescents and young adults because many users of such technology are young.
Therefore, the committee makes the following recommendation:
- The independent Campaign to establish a new norm of healthy sexual behavior should support and implement a long-term national initiative to increase knowledge and awareness of STDs and to promote ways to prevent them. The initiative should:
- be coordinated with HIV- and pregnancy-prevention campaigns;
- include a substantial mass media component;
- provide information both on how to implement health-protective behaviors and on STDs;
- provide information regarding the association of STDs and specific cancers and incorporate STD information into current cancer awareness and education activities;
- focus on specific groups and audiences, including public and private sector policymakers, health care and public health professionals, employers and other purchasers of health care, health plans, and the public, particularly women and adolescents;
- include an evaluation component; and
- use new information technology to disseminate information. As part of this initiative, the CDC, the Health Resources and Services Administration, and the National Institutes of Health should increase support for innovative ways to educate and train health care professionals through the use of new information technology.
Promoting Balanced Mass Media Messages
The mass media do not portray sexuality in a healthy way, and mass media messages supporting healthy sexual behavior are rare. Changes in social norms regarding healthy sexual behaviors will be difficult to achieve unless the content of programming in mass media supports these behaviors. As discussed in Chapter 3, children and adolescents are most influenced by mass media messages. Adolescents spend a large amount of time watching television and participating in other forms of mass media, and they undoubtedly are influenced by the explicit and implicit messages in such media. Many adolescents are not receiving appropriate information regarding STDs and healthy sexual behavior from their parents, peers, public health officials, or family doctors to counter misleading mass media messages. Therefore, the committee believes that mass media companies should incorporate messages regarding STDs and healthy sexual behaviors, including delaying sexual intercourse and using condoms, in television and radio programming and the print media, with a special focus on reaching adolescents and young adults.
In spite of advertisers' use of sexually suggestive advertisements to promote their products, and in spite of polls showing that most Americans support promoting condoms on television, most mass media companies still refuse to allow STD-related public service announcements and condom advertisements on prime-time television or in widely read publications. The committee calls on mass media and advertising executives to recognize the hypocrisy of this practice and to help promote healthy sexual behaviors.
It is important that mass media and other public health messages regarding STDs be clear. The public should be informed that the only sure way to prevent STDs is either not to have sexual intercourse or to have intercourse only with an uninfected partner who is also monogamous. Adolescents should be encouraged to delay sexual intercourse. Despite these messages, however, many individuals
will engage in unprotected sex. Therefore, media messages also must provide information regarding the methods for safer sex, including the correct and consistent use of condoms. Such messages should be comprehensive and incorporate public health messages regarding HIV and other STDs, sexual abuse, and unintended pregnancy.
As reviewed in Chapter 4, mass media methods of educating and increasing the awareness of the general public have been shown to be effective. Innovative media programs that use popular media, such as those developed by the Harvard School of Public Health related to drinking and driving, can complement public service announcements or more targeted public health campaigns. Although there have been few evaluations of such programs, they can reach audiences not touched by traditional approaches and should be evaluated further. The Media Project, described in Chapter 3, is a potential model for developing material regarding STDs. In addition, initiatives such as the STD Communications Roundtable, which functions as an expert resource on STDs for mass media companies, are important to ensure that mass media messages regarding STDs and safer sex behaviors are accurate. The STD Communications Roundtable could be used as a model for a standing committee of experts to facilitate the development of sexual health messages in mass media.
Therefore, the committee makes the following recommendations:
- The independent Campaign to establish a new norm of healthy sexual behavior should develop a standing committee comprised of public health experts, mass media and advertising executives, public communications experts, and consumer representatives to function as an expert resource and to develop guidelines and resources for incorporating messages regarding STDs and healthy sexual behaviors into all forms of mass media. Public health officials, including the CDC and state and local health departments, should also function as expert resources for mass media companies in developing and incorporating such messages.
- Television, radio, print, music, and other mass media companies should accept advertisements and sponsor public service messages that promote condom use and other means of protecting against STDs and unintended pregnancy, including delaying sexual intercourse. Adolescents are at high risk for STDs and are susceptible to mass media messages; therefore, such advertising and public service messages should be permitted to air during times when adolescents are likely to be watching or listening or should appear in print media that adolescents commonly read. Commercial advertisers and sponsors should support mass media companies in such efforts.
Improving Professional Skills in Sexual Health Issues
The committee believes that many individuals in the community should
become more involved in educating others regarding STDs. These key individuals include parents, educators, health professionals, persons in the mass media, and religious leaders. It is important that clinicians, educators, and researchers become more skilled at discussing sexuality and learn more about sexuality. Improved skills in these areas will not only improve the effectiveness of behavioral interventions for STDs, but also for reproductive health problems in general. Clinicians, in particular, need to understand the context in which high-risk sexual behaviors occur, as well as the social and cultural factors that reinforce these behaviors. It is often difficult for professionals to remain objective during clinical interactions because sexuality is an emotionally charged issue, especially when the professional's own beliefs and behaviors differ from those of the patient.
Research on sexuality provides the basis for understanding the determinants of risky sexual behaviors. Two formidable barriers to strengthening and developing social and behavioral research in sexuality and STD-related risk behaviors are the lack of comprehensive research training in sexuality and inadequate funding of both basic (e.g., research on determinants of behavior change) and applied (e.g., behavior change interventions) research. The continuing fragmentation of the social science fields in sexuality research, the low status given to sexuality research, and lack of sufficient research funding all hinder training in this area. Inadequate dissemination of existing data has also hampered development of interventions and policy initiatives.
All appropriate clinical opportunities to counsel patients regarding healthy sexual behaviors should be utilized. To improve effectiveness of behavioral interventions, clinicians, educators, and researchers need training and skills to deal with issues related to human sexuality and STDs among their patients and students. Providing new, and enhancing existing, continuing education courses for clinicians, educators, and researchers will help these professionals become more comfortable working with sexual health issues. Courses designed to educate all these professionals about sexuality, attitudes, alternative lifestyles, and cultural factors will provide a fuller understanding of sexual behavior.
Therefore, the committee makes the following recommendation:
- The Health Resources and Services Administration, health professional schools and associations, and schools and associations for training educators should support comprehensive sexuality training for health care professionals, educators, and researchers in order to increase their comfort in working with sexual health issues and to increase their effectiveness in sexual behavior counseling. Health professional schools and associations should sponsor continuing education courses in sexuality for clinicians and incorporate appropriate instruction in undergraduate and graduate education programs. The focus of these programs should be to provide instruction in basic, effective intervention counseling and clinical skills that are appropriate for any setting or population.
Supporting Sexual Health Behavior Research
Health behavior research provides the basis for developing interventions to prevent high-risk sexual behaviors. Population-based surveys mentioned in Chapter 5 that collect information on STD-related health behaviors are critical for monitoring trends in health behaviors among the general population and in developing effective interventions. In addition to improving STD prevention efforts, research on sexual behavior has direct benefits in improving prevention programs for HIV and unintended pregnancy. To address the barriers to adoption of healthy sexual behaviors, there needs to be considerably more research regarding the psychological and sociocultural, including religious, factors responsible for the secrecy surrounding sexuality and additional evaluation of approaches (that are respectful of individual beliefs) to successfully overcome these barriers. There is limited information available regarding the origins of sociocultural strictures on open discussion of sexuality and STDs. Understanding this factor should be useful in developing strategies to overcome societal constraints on preventing STDs.
Population-based surveys and studies to assess STD-related health behaviors are not only justified but are necessary for the development of effective interventions to prevent high-risk behaviors. Such surveys, particularly those for adolescents, have been severely criticized by some policymakers and interest groups. This committee, while recognizing the sincere concerns expressed by some of these groups, strongly believes that collecting information on STD-related health behaviors, especially among adolescents, is critical to STD prevention, because sexual behaviors are usually initiated during adolescence. The committee found no evidence to support the belief that asking questions about sexual activity in any way promotes or increase sexual activity among survey respondents or changes attitudes of respondents regarding these activities (Halpern et al., 1994). Without data on sexual behaviors, it is more difficult to prevent the very behaviors that concern the critics of such surveys.
Federal legislation has been introduced that would require prior written parental consent for minors to participate in federally funded survey research if the survey or questionnaire contains questions in several specific areas, including sexual behavior.1 The committee strongly believes that such restrictions would seriously jeopardize both behavioral research and the ability to prevent high-risk behaviors among adolescents. Requiring parental consent or prior written consent for a minor's participation in survey research would make it practically impossible to conduct research in settings where minors obtain confidential health services, such as STD and family planning clinics, because parents could not be notified. Yet it is precisely in these types of settings that it is particularly important
to collect information regarding sexual behavior. The committee believes that current federal and state regulations are adequate to protect the interests of minors in survey research. Current federal regulations allow for waivers of parental permission in cases where acquiring such permission would be considered unreasonable. Consensus guidelines for adolescent health research have been developed to clarify these regulations and to ensure that research involving adolescents has adequate mechanisms to protect minors (SAM, 1995). The committee believes that these guidelines appropriately balance the potential risks and benefits of health research that involve adolescents. In addition, the committee believes that it is critical to preserve the peer-review process for scientific research. It is potentially very damaging to the objectivity and integrity of this process specifically, and to scientific research in general, if external forces are allowed to influence the outcome of peer review.
Therefore, the committee makes the following recommendation:
- The National Institutes of Health and other federal agencies should continue to support research on health behaviors, including sexual behaviors, and their relationship to STDs. Both basic and applied research on sexual behavior and determinants of behavior change should be supported. Research should include study of the origins and maintenance of current societal strictures against open discussion of sexuality and STDs. Such research initiatives should be coordinated among federal agencies by the National Institutes of Health. Findings of these studies and surveys should be widely disseminated to policymakers, health care professionals, educators, community leaders, and the general public. In addition, these data should be used to promote appropriate behavior change and prevention. Under the conditions specified in the consensus guidelines for adolescent health research, the committee strongly believes that waivers of parental consent for a minor's participation in research that poses minimal risk to the participant should be preserved.
Strategy 2:
Develop Leadership
Strategy 2 is to develop strong leadership, strengthen investment, and improve information systems for STD prevention. Building a national system for STD prevention requires active participation from both the public and private sectors, and requires strong leadership at the national, state, and local levels. Public and private health agencies, especially those concerned with adolescent, women's, and reproductive health; communicable diseases; cancer prevention; delivery and financing of health services; community health; and public health in general, should strongly advocate for an effective system for STD prevention. National and state health professional societies and organizations and organizations with a special interest in STDs and adolescent, women's, and reproductive health also should work together to ensure that STDs are a priority in both the
private and public sectors. Advocacy by the above public and private organizations is important because, unlike many other health problems, there are virtually no patient-based constituent groups for STDs other than HIV infection. As discussed in Chapter 3, this is because having an STD is still perceived as socially unacceptable.
Developing Leadership in the Private Sector
Traditionally, public health agencies have led the efforts to improve STD-related services and have assumed most of the responsibility for STD prevention because private sector clinicians refused or were reluctant to provide STD-related services. The committee believes that the private sector needs to assume more responsibility and leadership (Showstack et al., 1996), and that the organizational norms of some private sector organizations regarding responsibility for STD prevention need to change. This is because, although the public sector must continue to play a major role in preventing STDs, the public sector does not have the resources or the organizational reach to fully implement a national system of STD-related services. Developing leadership in the private sector may be a challenge, given the heterogeneity of the organizations potentially involved in STD prevention. As mentioned previously, independent private nonprofit organizations, such as foundations, may be key in bringing these disparate organizations together.
Therefore, the committee makes the following recommendation:
- Private sector organizations and clinicians should assume more leadership and responsibility for STD prevention. The committee proposes the following major responsibilities in STD prevention for private sector organizations and clinicians:
- Health Plans and Clinicians. Provide confidential, comprehensive, high-quality STD-related clinical services to enrollees/patients and their sex partners; implement clinical practice guidelines for management of STDs; and ensure complete and accurate reporting of surveillance information.
- Employers and Purchasers of Health Services. Ensure that comprehensive STD-related services are available to employees/beneficiaries and their sex partners.
- Health Plan Accrediting Organizations. Develop and promote health plan performance measures for STD-related services.
- Mass Media Companies, Commercial Sponsors, and Advertisers. Improve public awareness and knowledge of STDs and promote healthy sexual behaviors.
- Health Professional Membership Organizations. Improve awareness and
- knowledge of STDs among the membership and support and sponsor training of health care professionals in STD-related clinical management.
- Private Foundations. Sponsor initiatives and provide independent, nonpartisan leadership for activities that improve collaboration among various organizations and encourage universal participation in STD prevention efforts.
- Health-Related Nonprofit Organizations. Improve public awareness and knowledge and integrate STD prevention efforts into other relevant disease prevention strategies.
- Academic Health-Related Institutions. Sponsor continuing education activities for clinicians and provide adequate STD-related training to health professional and other students; collaborate with health agencies to improve STD-related services; and conduct STD-related research.
- Biomedical Industry. Develop and improve biomedical interventions for diagnosis, treatment, and prevention (e.g., vaccines, microbicides) of STDs; ensure that new and existing interventions are affordable for publicly sponsored STD programs; and assist in efforts to educate health care professionals.
- School-Based Programs (including public sector programs). Provide confidential, comprehensive, high-quality STD-related clinical services for students and provide instruction regarding STDs and healthy sexual behaviors.
- Community-Based Social Service Organizations. Improve public awareness and knowledge of STDs and promote healthy sexual behaviors.
- Laboratories. Ensure high-quality diagnostic services for STDs.
Discussion of the rationale for the above recommendations and more specific recommendations for private sector organizations are presented later in this chapter.
Developing Leadership in the Public Sector
In this section, the committee proposes a set of responsibilities and functions for which federal, state, and local public health agencies should assume leadership. The committee believes that the proposed functions are most effectively and efficiently performed by government agencies in collaboration with private sector organizations.
Promoting Federal Leadership
Government agencies have the ultimate responsibility for ensuring the public health. At the national level, the Public Health Service Act gives the Secretary of Health and Human Services legislative authority to assist states in preventing communicable diseases. Ultimate responsibility for coordinating government efforts to establish a national system for STD prevention most logically rests in the office of the Secretary because the Secretary has authority over most of the
federal health agencies with activities in this area. The Secretary needs to charge these agencies to develop and implement the public sector components of the proposed national system and to provide these agencies with sufficient resources to do so. From a technical expertise and program implementation perspective, the CDC is the appropriate agency to provide national leadership in many aspects of STD prevention. The leadership of the Department of Health and Human Services, especially the CDC, must give higher priority to STD prevention programs. For example, in its fiscal year 1997 budget proposal to Congress,2 the administration requested reduced funding for STD prevention at a time when the CDC lacks the capacity to adequately provide technical assistance to states. Other health agencies, such as the National Institutes of Health, the Health Resources and Services Administration, the Health Care Financing Administration, the Substance Abuse and Mental Health Services Administration, the Agency for Health Care Policy and Research, the Food and Drug Administration, and the Indian Health Service, also need to assume leadership roles in their areas of responsibility. The Department of Health and Human Services needs to ensure that the agencies within its purview collaboratively provide bold innovative standards, guidance, technical assistance, and resources to state and local health departments and appropriate community-based organizations.
Therefore, the committee makes the following recommendation:
- Federal government efforts in STD prevention, under the leadership of the Secretary of Health and Human Services, should:
- provide guidance for STD-related clinical services and provide guidance and financial and technical assistance to states and local communities for STD prevention programs;
- develop scientifically based standards for STD-related services, including clinical services, such as screening and counseling, diagnosis and treatment, laboratory services, and prevention programs; such standards should be sufficiently flexible and applicable to all states and communities and to all types of practitioners and programs that provide STD-related care;
- develop and coordinate a comprehensive national surveillance system that collects STD-related data from public, private, and community-based providers and programs;
- ensure that high-quality STD-related services, including all supporting disease prevention activities, and effective community-based prevention programs are coordinated and integrated as appropriate and are available and accessible to every person, regardless of insurance status, income, state of residence, or urban or rural location;
- improve public and health professional awareness and knowledge of STDs and promote healthy behaviors on a national basis;
- ensure that health professionals are appropriately and adequately trained to provide STD-related services, including clinical services, disease prevention activities, and community-based prevention programs;
- ensure that STD prevention activities are an integral part of national HIV and cancer prevention programs;
- support and conduct research to improve strategies for STD prevention;
- coordinate STD prevention programs, including research activities, among states and relevant federal agencies, including the CDC, the National Institutes of Health, the Health Resources and Services Administration, the Health Care Financing Administration, the Substance Abuse and Mental Health Services Administration, the Agency for Health Care Policy and Research, the Food and Drug Administration, and the Indian Health Service; and
- expand and maximize existing funding streams and develop new and increased resources from both public and private sources to support this system at all levels.
Promoting State Leadership
Within state and local governments, the health department is responsible for implementing STD-related programs and is the logical agency to lead STD prevention efforts. Other agencies and state and local elected officials, however, need to support the efforts of these health departments, because the health department may not have sufficient authority or resources to implement interventions. In cases where direct responsibility for some aspects of STD-related clinical care is under the purview of another agency, the health department needs to assume a coordinating role.
State and local health departments vary considerably in their capacity and technical ability to provide clinical and outreach services and to conduct disease surveillance, quality assurance, and training activities. Most state and local health agencies, however, will require substantial additional funding and technical assistance to fully establish an effective system of STD prevention in their jurisdiction.
Therefore, the committee makes the following recommendation:
- State government efforts in STD prevention, through the leadership of the state health department and with support and technical assistance from the CDC, should:
- develop, implement, and support a comprehensive STD prevention system throughout the state;
- provide guidance and financial and technical assistance to local health
- departments to ensure that STD-related services are appropriately provided and coordinated among the various private and public community-based providers;
- collect information on reportable STDs from local health departments and private sector health care providers, analyze the information to monitor statewide trends in STDs, and report these data to the CDC;
- assess the need for STD-related services in the state;
- ensure that STD-related services are of high quality and are accessible to all state residents;
- improve public and health professional awareness and knowledge of STDs and promote healthy behaviors statewide;
- ensure that adequate funds are available to support provision of STD-related services to the uninsured; and
- provide training and technical assistance to all local jurisdictions to improve the quality and effectiveness of clinical services and prevention programs.
Promoting Local Leadership
Regarding local government leadership, the committee makes the following recommendation:
- Local government efforts in STD prevention, through the leadership of the local health department, with support and technical assistance from the state health department and the CDC, and in collaboration with community representatives, should:
- coordinate all providers of STD-related clinical services and prevention programs, including private providers, schools, and other community-based programs, to develop a comprehensive prevention system in the community;
- collect information on reportable STDs from all public and private providers, analyze the data to monitor trends in STD incidence and prevalence, and identify high-risk groups and areas for special interventions;
- assess the need for STD-related services in the community;
- ensure that STD-related services are appropriate and are accessible to every member of the community;
- improve public and health professional awareness and knowledge of STDs, and promote healthy behaviors in the community;
- ensure that adequate funds are available to provide STD-related clinical services to the uninsured; and
- provide training and technical assistance to providers of STD-related clinical services and prevention programs.
The proposed responsibilities and functions of federal, state, and local governments and health departments are similar to those proposed by special committees
of the Association of State and Territorial Health Officials (ASTHO, 1995a, b, c) and the National Association of County and City Health Officials (NACCHO, 1994), and a previous IOM committee (IOM, 1988). Many state and local governments have already addressed some or many of the responsibilities outlined above; the committee, however, believes that state and local government efforts generally need to be more consistent, more innovative, and better supported.
The monitoring and assessment role of government agencies requires them to monitor the prevalence of STDs in the community, identify high-risk populations or communities, and assess the adequacy of treatment and prevention efforts. This role also requires these agencies to monitor and ensure compliance with minimum standards of quality and accessibility of services. Effective performance of these roles requires collaborative relationships among local health departments and community-based health services, private sector health care professionals, health plans, laboratories, and others in the community. STD services and programs in most local health departments currently are relatively isolated from other providers in the community. Such isolation reduces opportunities for collaborative efforts, such as sharing of disease surveillance data, to improve STD prevention. The performance of local and state government agencies in ensuring and improving STD-related services should be monitored by consumer groups, elected officials, health professional organizations, and the federal government as appropriate (IOM, 1997).
Catalyzing Change Through Partnerships
The barriers to an effective national system for STD prevention are found in government, private sector organizations, and political factors and social norms. Overcoming these barriers is a challenge that requires the active participation of all levels of government, the private health care sector, businesses, labor leaders, the mass media, schools, and many community-based organizations. Many of the committee's recommendations regarding health agencies and private sector organizations involve sharing of responsibility and technical expertise and information; coordination of programs; and forming partnerships both within agencies and organizations and between the public and private sectors. In developing and implementing a national system for STD prevention, it is important that stakeholders be involved in all steps of the process; however, a formal mechanism for collaboration among agencies and organizations does not exist. Therefore, a neutral forum is needed to maximize the range of participants and to catalyze the collaborative process.
To establish an effective national system for STD prevention, the committee believes that a long-term national Roundtable for public agencies and private sector organizations is needed to catalyze the development and implementation of a comprehensive system of STD prevention in the United States. Independence
of the Roundtable from special interests and political constraints is especially critical. As with the Campaign to catalyze social change toward a new norm of healthy sexual behavior, while the committee recognizes the important role of government agencies in establishing a comprehensive system of STD prevention, it believes that political constraints on such agencies may sometimes impede the development of collaborations between the public and private sectors. In addition, some potential Roundtable participants may be reluctant to join in a government-agency-led activity. To maximize the range of Roundtable private sector participants, the committee believes that ensuring that all potential Roundtable members have an opportunity to participate on an equal basis is important. The Roundtable would not have bureaucratic functions or be an administrative hurdle for agencies or the private sector, because it would not have administrative authority over government agencies or private organizations. The Roundtable's work would be determined by its participating agencies and organizations. Although the Roundtable's activities should be coordinated with the activities of the previously proposed national Campaign (e.g., through regular joint meetings and appointed liaisons), the two entities would be independent. Independence of the two entities is necessary because, in the case of the Campaign, government agency participation is likely to constrain the effectiveness of its work; in the case of the Roundtable, the participation of government agencies is critical.3 The activities of the two entities, however, must be coordinated to ensure that they are not only complementary, but synergistic.
An example of a roundtable that brought disparate agencies and organizations together toward a common, although more limited, goal was the IOM Roundtable for the Development of Drugs and Vaccines Against AIDS that operated from 1988 through 1994. The purpose of this roundtable was to identify and help resolve the impediments to the rapid availability of effective drugs and vaccines for HIV infection and AIDS. Roundtable participants included leaders from government, the pharmaceutical industry, academia, and affected communities.
Leadership is needed to establish and maintain a Roundtable on STD prevention. At the current time, there is a lack of leadership among private health care sector organizations in this area. The Department of Health and Human Services, therefore, is the logical agency for ensuring the establishment of the Roundtable because of its mission and its oversight of the major government activities and agencies involved in STD prevention. These include: the CDC (prevention services, technical assistance, and surveillance); the National Institutes of Health (biomedical and behavioral research); the Agency for Health Care Policy and
Research (health services research); the Health Resources and Services Administration, the Indian Health Service, and the Substance Abuse and Mental Health Services Administration (primary care and other health services); the Health Care Financing Administration (financing mechanisms for some STD treatment), and the Food and Drug Administration (drug, biologic, and medical device evaluation and approval).
Therefore, the committee makes the following recommendation:
- An independent, long-term national Roundtable should be established as a neutral forum for public and private sector agencies and organizations to collaboratively develop and implement a comprehensive system of STD-related services in the United States. The Roundtable should:
- coordinate public and private sector STD-related services;
- disseminate information on, and promote implementation of, ''best practices" and quality standards in STD prevention;
- develop consensus regarding the appropriate roles and responsibilities of the various providers of STD-related services;
- promote partnerships and dialogue among public and private sector agencies and organizations on the state and community level;
- recruit and involve public agencies and private organizations, including health plans, employers and other purchasers of health services, health professional organizations, pharmaceutical and medical device companies, and other providers of STD-related services;
- seek input from, provide guidance to, actively involve, and communicate with providers of STD-related services on local and state levels; and
- be funded by a broad range of sponsors, including private foundations, private sector health plans, the biomedical industry, employers, and the Department of Health and Human Services, but primary funding should come from the Department of Health and Human Services. The Secretary of Health and Human Services should take responsibility for initiating and provide ongoing support for the Roundtable, but it should be housed at a private, nonprofit institution that can ensure a neutral environment for Roundtable participants.
Strengthening Investment in STED Prevention
STDs are a tremendous economic burden on the people of the United States, but the costs of STDs are largely unrecognized. As discussed in Chapter 2, the committee estimates that approximately $10 billion is spent on costs associated with major STDs in the United States annually. The committee's cost estimate is not precise because it is based on incomplete data regarding the incidence and costs of STDs. Not all STD-related costs are accounted for; thus, the true cost of STDs is likely to be much higher than the committee's estimate. For example,
this estimate does not include costs associated with newly described STD-related syndromes such as premature delivery in pregnant women and low birth weight associated with bacterial vaginosis. Comprehensive and accurate data regarding the economic costs of STDs are essential for cost-effectiveness analyses of prevention programs, but cost and morbidity data are not currently available for many STDs and related syndromes. Therefore, the CDC or other appropriate federal agency should conduct or support a comprehensive analysis of the economic consequences of STDs and associated sequelae. This analysis should include estimates of direct and indirect costs and appropriate cost-benefit and cost-effectiveness analyses of interventions.
The current national response to STDs is not commensurate with their health and economic costs. STDs are a formidable health problem and should be a national public health priority. An effective national system requires additional investment to avert the much higher long-term costs of STDs. Current public resources allocated for STD prevention are extremely low. As discussed in Chapter 5, the committee estimates that only $1 is invested in STD prevention for every $43 spent on the costs of STDs and their complications every year. Similarly, only $1 is invested in biomedical and clinical research for every $94 spent on the costs of STDs. Studies cited in Chapter 4 show that STD prevention efforts are cost-effective and sometimes cost-saving. Investing in preventive services will avert substantial human suffering and save billions of dollars in treatment costs that result from the costly complications of STDs and lost productivity. The CDC estimates that for every $1 spent on early detection and treatment of chlamydial and gonococcal infection, approximately $12 in associated costs could be saved (CDC, DSTD/HIVP, 1995).
There is a widespread belief among clinicians and researchers who work in STDs that the social and economic costs of STDs in the United States justify expenditures of much more money and effort than currently are devoted to this area. This type of statement often is made for many types of prevention, but the committee is of the opinion that the situation is worse in STDs than in many other areas. The committee also recognizes, however, that devoting resources to prevention programs is not always cost-effective (Russell, 1994). Unfortunately, there is surprisingly little data either on absolute expenditures for STD prevention or the cost-effectiveness of different types of expenditures. Thus, the committee recommends that rigorous analyses of the cost-effectiveness of different types of prevention programs be conducted. This kind of research should be supported by the National Institutes of Health, the Agency for Health Care Policy and Research, and other agencies.
The committee recognizes that establishing a national system for STD prevention requires additional funding and that this may be very difficult in an era of shrinking federal and state budgets. The committee proposes that additional funding to establish a national system for STD prevention come from all levels of government and the private sector. Regardless of whether additional funds can be
found for STD programs, it is clear that more efficient and effective use of existing resources is also needed. By providing STD-related services in primary care settings and coordinating public and private sector programs, a more effective and efficient system for prevention can be achieved.
Who Is Currently Paying and Who Should Pay?
Who is currently paying for the substantial economic costs of STDs? The answer is all Americans. Local, state, and the federal governments pay STD-related costs by funding services through the Medicaid and Medicare programs (for STD-related complications that manifest among older persons, such as cancer), public STD clinics, family planning clinics, community health centers, and other publicly sponsored health care programs. Businesses pay for STD-related costs through higher health insurance premiums for their workers and lost productivity of employees with STDs. Hospitals pay for uncompensated STD-related care. Managed care organizations pay STD-related costs by providing expensive treatment for the complications of STDs that can be averted. In short, all Americans eventually pay for the costs of STDs through their tax dollars and through increased health insurance premiums. Therefore, all public and private health-related agencies and organizations, including federal, state, and local governments, employers and other purchasers of health care, businesses, and health plans should invest in and support STD prevention efforts. It is in both the national and local community interest to invest in STD prevention.
Public funding for STD prevention is justified because STDs are communicable diseases that, when left unchecked, potentially endanger the health of the community. Public investment in STD prevention is especially important because the stigma associated with these diseases may hinder availability of clinical services in the private sector, especially for disenfranchised groups who represent a reservoir of infection for other members of the community, as described in Chapter 3.
The committee believes that the financial responsibility for supporting STD prevention is currently not equitable since both the private and public health care sectors benefit from lower STD rates. The private sector, including health plans, employers and other purchasers, and health care providers, needs to assume more responsibility for supporting public health services, including STD-related services, that benefit "the insured" population and ultimately benefit their financial results. Health plans, therefore, should provide their enrollees with access to STD-related services in the public sector through equitable reimbursement agreements. Reasons why the private sector should become more involved in preventive services and provide STD-related services to sex partners of infected persons and prevent STDs in the general community are presented in later discussions.
Aral and colleagues (1996) have proposed a way of thinking about the issue of who should pay for STD prevention according to the emphasis placed on
prevention efforts. If preventing acquisition of STDs by susceptible individuals in a community is emphasized, then the entire community assumes the financial costs of the interventions and the intangible costs associated with appropriate behavior change. In this situation, the community also receives the benefits of avoiding STDs. In the case where preventing transmission of STDs from infected individuals to the community is emphasized, members of the highest-risk groups primarily incur the costs associated with behavior change, and the community benefits from avoiding acquisition of STDs and averting future STD-associated public health costs. Therefore, in both cases, the entire community directly benefits from preventing STDs and should assume financial responsibility for STD prevention. Specific potential mechanisms for ensuring funding for STD-related services may include allowing public STD clinics to be contract providers for health plans, requiring health plans to reimburse STD and other public health clinics for out-of-plan use of services, and imposing an assessment on health plans for services and programs that benefit the broad community. Economists recognize the need for public support when "externalities" (e.g., the potential for widespread transmission of disease from an infected individual) transcend the market system for allocating services based on supply and demand. It is important to recognize the fundamental public responsibility for preventing communicable diseases such as STDs.
Increased support should be given to effective prevention programs, including the programs to change STD-related risk behaviors that are described in Chapter 4. Support for education and counseling in publicly sponsored programs is needed. Education and counseling in private health care settings may be covered or reimbursed through either capitation or fee-for-service payments. In addition, communityand school-based interventions that target high-risk groups require a broad funding base that reflects the benefits they generate for the entire community. Finally, a secure source of funding for STD-related services for uninsured persons is essential. Cutbacks in state and local funding for indigent health care have dramatically reduced the availability and accessibility of public health services for the uninsured. Federal funding is essential to enable state and local governments to maintain and improve their STD prevention programs. The fragile successes in containing bacterial STDs in much of the country are endangered by reductions in access to services and underscore the importance of retaining categorical federal funding for STDs.
State and local governments traditionally have had full responsibility for supporting STD-related clinical services and also share responsibility with the federal government for supporting STD prevention efforts. However, state and local governments vary significantly in their investment in STD-related programs and generally need to increase their support of such programs. The CDC's STD Accelerated Prevention Campaigns program, which seeks to encourage collaboration between dedicated public STD clinics and community-based health care professionals, has an enhanced component that requires the grantee to partially
match federal funds. Such matching requirements should be encouraged to expand local commitment of resources to STD prevention.
A common question relates to the appropriate criteria for reducing funding for public health programs. In the case of STD-related programs, while it is possible that funding could be reduced without harmful consequences as STDs are reduced in the distant future, the committee believes that the United States is far from reaching this stage. In addition, sustained funding for programs are necessary because STDs operate under a dynamic equilibrium-the nature of the most effective interventions and the focus on different population groups will change with time and the phase of the epidemic (Wasserheit and Aral, 1996). For example, as the prevalence of STDs decreases in a population, there would be less emphasis on screening programs, but increased emphasis on population-based interventions to maintain healthy sexual behaviors in the community. In all cases, surveillance of STDs and assessment of health behaviors are important in providing feedback to the program planning and implementation process.
Therefore, the committee makes the following recommendation:
- Federal, state, and local elected officials should provide additional funding for STD prevention. Local health departments, in particular, will require additional funding and technical assistance from the CDC and the state health department to fully assume the responsibilities of ensuring access to STD-related services. If federal staff assistance to states and localities is reduced, resources should be redirected back into state and local STD programs to ensure that the state and local infrastructure can be incrementally shifted from reliance on federal direct assistance to a state and locally directed program.
Evaluating and Improving Categorical Funding
The advantages and disadvantages of categorical funding and block grants are summarized in Chapter 5. Categorical funding for STDs has encouraged programmatic rigidity and excess administrative costs for local agencies, fostered services that often ignore local conditions and other health problems, and discouraged innovation. Federal funding rules have resulted in local programs adapting to federal requirements rather than local programs adapting to community needs. This is an unintended effect of a policy intended to maintain high national standards for services. In addition, categorical funding has encouraged narrowly defined programs because of the traditional methods used to measure program effectiveness.
Despite the problems in the current system of categorical funding, the committee strongly believes that moving to a system of block grants for STDs would have a devastating impact on STD prevention and that categorical funding for STDs should be preserved. In an ideal world, funding decisions would be based on assessments of public health need, but past experience suggests that state
politics, rather than objective consideration of public health or social needs, may determine funding for public health programs, especially those with a limited political constituency such as STDs. Because STDs are often perceived to be a problem of marginalized groups, they will fare poorly in competing with other more visible and "acceptable" health conditions for their share of decreasing state health budgets. In many states, STD prevention programs may end up as political orphans because STDs are problems that public officials are reluctant to acknowledge. Funding for these programs is likely to be challenged by well-organized, powerful interest groups that are opposed to open discussion and public education regarding STDs. Many states have weak public health and health policy infrastructures and limited economic resources. Therefore, the likelihood that they will successfully evade pressures to limit or eliminate funding for STD prevention is reduced. With no enforceable national standards and substantial variability in the use of public-health-based decision-making in state legislatures, some states are likely to reduce or eliminate funding for STD programs. In the absence of national standards and mandates, block grants would create wide variability and unevenness in program quality and effectiveness among the states that could undermine a cohesive national system for prevention. Block grant funding is also more vulnerable to budget reductions at the national level. The diffuse purposes of block grants make them more vulnerable to reductions in congressional funding than most categorical programs.
Moving from categorical programs to block grants or Performance Partnership Grants (which the committee considers to be a form of a block grant, as described in Chapter 5) would also dramatically change both funding and accountability relationships among federal, state, and local governments. States would have more flexibility regarding resource allocation for public health. They also would be less accountable to federal agencies and would receive less guidance and support from the federal government. In addition, state and local health agencies may end up with less money than they currently have for STDs, unless state and local governments increase funding. Many elected state officials favor block grants because it gives them more discretion over resource allocation. However, state and local public health officials and STD program managers throughout the nation-the very people whose programs are supposed to benefit from block grants-warned the committee that block grants are likely to weaken and undermine STD prevention efforts.
Federal categorical funding programs can be improved by redesigning, rather than abandoning, current categorical programs. Performance standards that focus on health outcomes and process, rather than on program inputs, can help communities and states set priorities and objectives and measure their progress in achieving specific goals (IOM, 1997; NRC, in press). Process measures that are known to be characteristic of high-quality programs can help communities and states evaluate the quality of their programs. Process measures should focus on cardinal characteristics of prevention systems, such as awareness of and access to programs,
consistency of follow-up, quality of prevention advice and treatment services, and continuity of care. Currently, there are no validated measures of these characteristics for prevention systems, but the development and implementation of such measures would greatly increase the capacity to monitor and improve the efficiency and quality of public health programs for STD prevention. It would be most logical for state and local governments to conduct performance monitoring under federal guidelines.
Performance standards would also give the federal government a more meaningful method of holding states accountable for federal funds. Accountability should focus on reducing STDs, including HIV infection, among high-risk populations and the community at large. The Department of Health and Human Services should develop and provide incentives for states and local governments to make substantial financial contributions to STD prevention and to make progress in containing STDs in their jurisdictions. Funding of programs can also be made responsive to local needs by providing more options for local modifications and flexibility. In addition, waivers should be granted for promising innovative programs that may not comply with all federal requirements. With current HIV and STD categorical programs, however, states should be encouraged to coordinate, integrate, and consolidate services and education programs.
Therefore, the committee makes the following recommendation:
- The CDC should retain and immediately redesign categorical funding for STD programs. New accountability measures that monitor performance toward achieving community health objectives and outcomes and new process measures should be developed and implemented. In addition, mechanisms should be established to increase local flexibility and program innovation and to encourage integration and coordination of local programs. Regardless of the type of funding mechanism, the CDC should ensure that all state and local governments, as a condition of receiving federal funds:
- maintain current funding levels for STDs or provide matching funds, whichever amount is greater, and set aside a specified minimum proportion of funding for essential programs and services, and for high-risk populations;
- develop performance objectives in collaboration with local communities and health departments;
- meet minimum national quality standards for STD-related services (see recommendations for improving the quality of dedicated public STD clinics for more details); and
- report federally recommended morbidity data as part of a national surveillance system.
In addition, as an incentive for state and local governments to expand their efforts in STD prevention, the CDC should provide whatever technical assistance
is required and match new state and local funds allocated toward these efforts. Because the CDC currently does not have sufficient resources to provide comprehensive technical assistance to state and local health departments, the agency will require additional funding for STD prevention.
Strengthening Global STD Prevention Efforts
STDs are emerging infections and a global public health problem. As discussed in Chapter 2, new STDs with a potentially devastating impact are likely to emerge and become established in the United States. This is a consequence of increasing global travel, inadequate international public health safeguards, and continuing high-risk sexual practices. In addition, inappropriate treatment practices may be leading to the rise of antibiotic resistance among certain sexually transmitted pathogens. Current STD surveillance systems are not adequate to monitor the emergence of new infections or the resurgence of recognized STDs. International travel has enabled persons with infectious diseases to expose persons on different continents within hours or days. Strategies to prevent STDs in the United States should consider the potential impact of global STD rates. The reason for emphasizing the emerging nature of STDs is to strengthen global surveillance, improve international efforts against STDs, and promote behavioral and ecological changes to decrease pressures for the emergence of new infections. Many STDs, such as syphilis and gonorrhea, can survive only in the human host, and theoretically can be eradicated. Eradication or elimination of any STD will require substantial international investment and collaboration. The United States, therefore, has a national interest in preventing STDs worldwide in order to minimize the likelihood of emerging STDs in this country.
Therefore, the committee makes the following recommendation:
- The federal government, through the Department of Health and Human Services and the U.S. Agency for International Development, and international organizations, such as the World Health Organization and the World Bank, should provide resources and technical assistance to global efforts to prevent STDs. The CDC should provide more technical assistance in these international efforts.
Improving Surveillance and Other Information Systems
Surveillance and other information systems are necessary to monitor and evaluate the components of a national system for prevention. Data from these information sources are critical to long-term program planning as well as to day-to-day management of programs.
Surveillance and population-based survey data are important in monitoring the status of STDs and STD-related behaviors. These data are the basis for developing
and targeting interventions, prioritizing resources, detecting epidemics, and evaluating program effectiveness. As discussed in Chapter 5, current surveillance systems do not give accurate estimates of disease incidence because not all persons with STDs seek medical care and because surveillance data do not reflect all clinical encounters with community health care professionals, especially those in private sector health care settings. The limitations of the current surveillance system are summarized in Chapter 5.
Enhancing the Current System
Certain limitations and weaknesses of the current passive notifiable diseases surveillance system are inherent in passive disease reporting systems, but several enhancements to the current system are indicated. It is critical that a systematic, comprehensive evaluation of the national surveillance system be conducted to describe the attributes of the system and to provide guidance for future improvements. STD surveillance systems need to include and link information from public sector, community-based, and private health care professionals. In particular, public health agencies need to work with the private health care professionals to improve compliance with disease reporting. Private practice clinicians and laboratories should understand that disease reporting and feedback of local epidemiological surveillance information concerning STDs and other emerging infections will greatly assist them in their clinical practice. By minimizing the time delay in reporting of cases from clinicians and laboratories to the local health department, and then to the state health department and the CDC, local and multistate outbreaks can be detected promptly.
Local health departments, with both the skills and the responsibility for collecting health data from a wide array of sources, will continue to be the pivotal agency in monitoring the health of communities. With technical assistance from the CDC and state health departments, they will need to develop effective reporting systems and actively work with community-based and private health care professionals to ensure accurate and complete reporting. Their responsibilities should include feedback regarding local STD trends to health care professionals to inform and engage them in STD prevention efforts. Although not widespread, some local health departments have already taken a collaborative approach to surveillance by developing relationships with private clinicians. One specific disease reporting issue that needs to be resolved at the national level is the lack of reporting guidelines for laboratories that confirm STD diagnoses among out-of-state persons.
The ideal surveillance system for STDs should be robust enough to accurately and promptly identify national and local trends in STD incidence, and flexible enough to provide state and local health officials with necessary data to direct local activities and evaluate interventions. In the future, as resources permit, STD information systems should identify and incorporate data elements that
permit surveillance of infection rates within communities and allow assessment of the effectiveness of STD-related services. This information, which requires reliable population-based data as well as data from STD-related clinical services, is necessary to identify and focus on high-risk groups and areas and to evaluate broader public policies.
As mentioned in Chapter 5, sentinel surveillance projects are valuable tools for supplementing and validating information from the national notifiable disease reporting system. For example, the CDC-sponsored Gonococcal Isolate Surveillance Project is a model for how other sentinel systems might operate with close collaboration and communication among local and state STD programs, state laboratories, and the CDC. Another sentinel surveillance system of potential benefit could be developed by collecting and analyzing the results of prenatal testing for gonorrhea, syphilis, and chlamydial infection. Testing of pregnant women for such infections is already being performed in most states, but the resulting data are not systematically captured or analyzed by STD surveillance systems. Such data could provide age-specific rates of STDs (number found infected per number tested) in women. Infection rates among young pregnant women may be good, although not perfect, surrogates for STD rates among the general population of women who do not use contraception. Trends in STD prevalence among young pregnant women also may be particularly sensitive to STD interventions. This sentinel surveillance system would have increasing coverage of the U.S. population over time and could be coordinated with prenatal HIV surveillance systems. In addition, surveillance of STDs within correctional systems and drug treatment facilities could help motivate and evaluate interventions to prevent STDs in these settings.
Therefore, the committee makes the following recommendation:
- The CDC should lead a coordinated national effort to improve the surveillance of STDs and their associated complications and improve the monitoring of STD prevention program effectiveness. Specific areas for improvement include the following:
- The CDC and the states should improve reporting from private sector health care professionals and laboratories and collect data on the number of persons tested for STDs through the national surveillance system. In addition, the CDC should systematically assess the attributes of the current surveillance system, including validity, sensitivity, representativeness, acceptability, and timeliness, in relation to alternative approaches to active or sentinel surveillance. This effort should take into account the potential impact of changes in clinical practice patterns, such as changes in utilization of diagnostic tests or types of tests used, and changes in reimbursement for clinical services on reported STD rates and surveillance for emerging antimicrobial resistance.
- Disease surveillance systems should be better coordinated with the information systems of community-based clinics, private sector providers and laboratories, and public STD clinics. Special emphasis should be placed on educating clinicians about reporting and collaborating with, and collecting data from, private sector providers, including managed care organizations and other health plans. Training is also needed at all levels of the surveillance system to improve data collection, management, analysis, and dissemination. The use of new information technology to improve surveillance by minimizing reporting delays should be supported.
- The current passive surveillance system should be supplemented with active surveillance components as appropriate. These activities should include serosurveys or testing of urine and saliva using nationally representative health surveys, including the National Health and Nutrition Examination Survey (NHANES) and the National Survey of Adolescent Males, to estimate rates of STDs and to assess the attributes of passive surveillance systems.
Utilizing Health Services Performance Measures
Surveillance data can be used to evaluate program effectiveness, but current systems to monitor effectiveness, as described in Chapter 5, are inadequate. If surveillance data are to be used as a program management tool, state and local health departments need to develop greater capacity in data management and analysis. The current capacity is inconsistent among local health departments, and is often limited even at the state health department level. Therefore, federal technical assistance to improve data management and analysis capacity at the local and state level is needed.
In addition to disease surveillance, health indicators that measure program effectiveness and support program evaluation are important components of a comprehensive information system for STDs. Disease prevention programs will continue to require timely data to support decision-making in programmatic areas (e.g., prevention and education, partner notification and follow-up, clinic services) and outcome measures to assess the effectiveness of interventions on both individual and community levels. Performance measures and information systems need to be designed to collect data from a variety of health care settings in addition to public STD clinics. These settings include family planning clinics, community health centers, hospital emergency rooms, correctional institutions, substance abuse programs, health plans, and other private sector health care providers. Performance monitoring should not be used exclusively to allocate funding, but also as a tool for program management (IOM, 1997). The ability of public STD clinics and health departments to effectively monitor arrangements or contracts with private health plans will be contingent upon the capacity of STD-related information systems to generate relevant and timely information on program performance measures. Existing data systems of STD programs are not
adequate for overall program assessment. In addition, it is important that performance measures be valid and reflect the quality and health impact of services. For example, it can be expected that reported STD rates will rise with expansion of screening efforts. Potential areas for which STD clinical practice performance measures should be developed include:
- patient reports regarding care;
- access, availability, and utilization of services;
- cost and affordability of services;
- time interval between seeking of care and examination, time interval between initial examination and treatment, and percentage of diagnosed persons treated;
- incidence of reinfections or persistent infections; and
- appropriateness of clinician diagnosis, treatment, and counseling; knowledge and compliance with treatment protocols; compliance with precautions and management of adverse reactions; and disease reporting.
The automated information systems of many managed care organizations and other health plans are a valuable source of data on patient encounters, disease diagnoses, and clinical outcomes. The Health Plan Employer Data Information Set (HEDIS), in particular, and other health services performance measures will be particularly valuable as new indicators related to preventive and public health services are developed and implemented. These data represent an excellent opportunity to conduct outcomes research and evaluate the effectiveness of interventions. Not all managed care organizations, however, are currently using such performance monitoring tools; STD-related data from other health plans will also need to be captured.
STD-related information systems should be developed and planned in the context of, and be consistent with, broader information system development initiatives to monitor a range of community health issues (IOM, 1997). Information systems should take into account evolving disease prevention management requirements and opportunities; promote and support cost containment and efficient resource allocation; optimally utilize current and evolving technology; and consider the analytic capacity necessary to maximize available information.
Therefore, the committee makes the following recommendations:
- Federal, state, and local STD programs should encourage and provide technical assistance to employers and other purchasers of health care (including Medicaid programs), managed care organizations and other health plans, and other health care professionals to develop and utilize information systems that effectively integrate preventive services performance data with community health status indicators and STD program data. STD-related information systems should support assessment and evaluation of anticipated
- system impacts from changes in health program structure and funding such as managed care, Medicaid changes, and block grants. The information system should also monitor the capacity of state and local health departments to execute essential public health functions and services. The CDC should provide adequate technical assistance to state and local health agencies to support the development of STD-related surveillance and other information systems and data analysis capacity at the local level.
- STD-related performance measures should be included in the Health Plan Employer Data Information Set (HEDIS) and other health services performance measures to improve quality-assurance monitoring of STDs. The National Committee for Quality Assurance and other relevant organizations, in conjunction with public health agencies and health plans, should continue to develop and promote performance measures related to STD prevention.
Strategy 3:
Focus On Adolescents And Underserved Populations
Strategy 3 is to design and implement essential STD-related services in innovative ways for adolescents and underserved populations. Specific populations requiring special emphasis in an effective national system for STD prevention include adolescents and disenfranchised populations. Reasons for the greater risk of STDs among these groups and their importance in prevention strategies are documented in Chapters 2 and 3. Many members of these groups lack access to STD-related services and are difficult to reach through traditional clinical settings and approaches. Under Strategy 3, the committee recommends that prevention of STDs be a central focus in designing interventions for these populations and that innovative methods for delivering STD-related services to such populations be immediately implemented.
Focusing On Prevention
Ultimately, social norms regarding sexual behavior need to change before a sustained reduction in STDs can be realized. Population-based preventive services are the primary means for changing social norms and attitudes by creating an environment that supports such changes. A national strategy for STDs needs to emphasize prevention because averting illness is desirable, many STDs are incurable, and STD-related complications may be irreversible. As summarized in Chapter 4, there are many existing prevention-oriented approaches that are effective in averting long-term health problems and costs. The committee believes that an approach to STD prevention involving multiple interventions at the individual and the community levels is critical. This is because many interventions are highly effective, but no single intervention is sufficient on its own. Complementary behavioral and biomedical approaches to STD prevention are essential. Interventions
to promote healthy sexual behavior need to be complemented by access to clinical services, training and education of health professionals, surveillance and research, and community-based programs. Many prevention efforts, such as community- and school-based programs, remain underfunded and weak because of social and political constraints. The committee believes that population-based interventions should be objectively evaluated for funding and implementation based on their scientific merit and potential public health impact.
Prevention programs must address the roles of both men and women in transmitting infection. Many screening programs are appropriately targeted toward women and conducted in facilities exclusively providing services to women. In order to interrupt the transmission cycle of STDs, however, infections among men also need to be addressed. STD prevention efforts should include both screening programs for asymptomatic men and male-specific behavioral interventions, such as promotion of responsibility for condom use. In addition, programs providing health services to women should ensure that sex partners are appropriately evaluated and treated.
Expanding Prevention-Related Research
New research may be used to develop effective prevention programs, but such programs need to be modified regularly based on continuous evaluation of existing programs and changes in the epidemiology of STDs and the health care environment. Prevention-related research allows program managers to maximize the effectiveness of interventions and policymakers to maximize available resources. Professionals responsible for STD prevention efforts should ensure that regular program evaluation and quality improvement activities are integral parts of their programs.
There are many available interventions for STD prevention, but some have not been fully evaluated, and new interventions need to be developed. Wasserheit and Hitchcock (1992), in their assessment of future directions in STD prevention research, concluded that a multidisciplinary approach to research is necessary; prevention research should be given top priority; the long-term sequelae of STDs should be given greater emphasis; and communication and coordination within the research infrastructure should be improved. A recent panel charged to evaluate the social, behavioral, and prevention research areas for the National Institutes of Health found that only 3.4 percent of the total National Institutes of Health budget for research on AIDS was devoted to prevention and intervention research in the behavioral and social sciences (NIH, 1996). The panel recommended the following: intervention and behavioral research be given the highest priority and coordinated with biomedical research; a paradigm shift to develop models that are domain-specific with regard to sexuality (and drug use) and recognition that risk behavior is embedded within personal, interpersonal, and situational contexts; research on individual differences in human sexuality (and
drug use) that takes into account cognitive, affective, cultural, and neurophysiological variables; studies on direct effects of intoxicants on self-regulatory mechanisms; and studies regarding maintenance of behavior change.
The committee agrees with the above assessments and recommends that general areas of additional research in STD prevention include behavioral, biomedical, and operational research. In addition, the committee recommends that the following specific topics be studied: determinants of sexual behavior and sustained behavior change on an individual and community level; determinants of initiation of sexual intercourse among adolescents; influence of social and other community-related factors on risk of STDs; interventions to improve condom use and reduce high-risk behaviors; effectiveness of sexual risk behavior assessment and counseling; biomedical interventions that do not rely primarily on individual behavior, such as vaccines; female-controlled prevention methods; cost-effectiveness of preventive interventions, including partner notification and treatment techniques; methods for preventing STDs among disenfranchised populations; interventions for preventing STDs among persons of all sexual orientations; and methods to measure prevention program effectiveness.
Therefore, the committee makes the following recommendation:
- The National Institutes of Health and the CDC should continue to support and expand both basic and applied research in STD prevention. Research results should be made widely available and should be used by government agencies, public and private health programs, and health professional organizations to improve STD prevention services.
Developing Female-Controlled Methods for Protecting Against STDs
Although women bear the larger burden of disease associated with STDs, the most effective means for preventing transmission of STDs during intercourse (i.e., the male condom) is largely dependent on the behavior of men. Except for the female condom, there are no female-controlled methods that are sufficiently protective against STDs. Additional methods of protection over which women have greater control need to be made available, and additional effective mechanical and chemical methods for protection against STDs need to be developed. Dual protection (i.e., use of one method to protect against pregnancy and one method to protect against STDs) is important because, as discussed in Chapter 4, no single method of preventing STDs or pregnancy confers the maximum level of protection for both conditions.
Therefore, the committee makes the following recommendation:
- The National Institutes of Health, the Food and Drug Administration, and pharmaceutical, biotechnology, and medical device companies should collaboratively develop effective female-controlled methods for preventing
- STDs. Clinicians and STD (including HIV) prevention programs, like family planning programs, should teach that use of a condom (male or female) along with an effective contraceptive for pregnancy is necessary to obtain maximum protection against both STDs and unintended pregnancy. This should be the standard approach for both men and women who are not in a mutually monogamous relationship with an uninfected partner.
Focusing On Adolescents
Many of the severe health consequences of STDs, such as cervical, liver, and other cancers, manifest themselves among older adults because they may not appear until decades after infection. This phenomenon contributes to the under-recognition of the impact of STDs among older adults. These complications, however, usually result from infections acquired or health behaviors initiated during adolescence or early adulthood. Therefore, STD prevention programs need to focus on adolescents. The committee's proposed focus and recommendations regarding appropriate policies to prevent STDs among adolescents are similar to those of numerous health professional and other organizations (AMA, 1996).
Ensuring Effective, Early Interventions and Confidentiality
As outlined in Chapters 2 and 3, three million teenagers acquire an STD each year and high-risk sexual activity among adolescents has become more common during the past two decades, increasing the number of adolescents and young adults at risk for STDs. Current data indicate that almost 40 percent of adolescents in the ninth grade have already had sexual intercourse (CDC, 1995). Adolescents are at greater risk of exposure to and infection with STDs than are adults. This is due to high-risk sexual behavior, increased biological susceptibility of the adolescent cervix to infectious diseases, and the greater likelihood of exposure to the social factors contributing to STD risk.
Many opponents of education for adolescents about sexuality and STDs believe that adolescents should only be told not to have sexual intercourse and that other forms of education are not appropriate. At the other end of the spectrum, some advocate that adolescents should be assumed to be sexually active and given appropriate education regarding STDs, without any messages regarding the appropriateness of sexual intercourse among adolescents. The committee believes that some aspects of both perspectives are valid and should be part of a national initiative to prevent the initiation of high-risk sexual activity among adolescents. Adolescents should be strongly encouraged to delay sexual intercourse until they are emotionally mature enough to take responsibility for this activity. In spite of messages to delay intercourse, most individuals will initiate sexual intercourse during adolescence. They should have access to information
and instruction regarding STDs, unintended pregnancy, and methods for preventing both. As reviewed in Chapter 4, such instruction does not increase sexual activity among adolescents. Because information is a necessary but not always sufficient condition for behavior change, interventions and policies to facilitate development of behavioral skills are also necessary.
To prevent STDs among adolescents, it is necessary to provide them with accurate, comprehensive information and give them instruction in ways to implement healthy sexual behaviors. As discussed in Chapter 3, adolescents experience a large information gap regarding STDs. Surveys show that they receive much of their information regarding sexuality and STDs from their peers, the mass media, or other unreliable sources of information rather from their parents or health care professionals. Studies cited in Chapter 4 show that many school-based programs and mass media education campaigns are effective in improving knowledge about STDs and in promoting healthy sexual behaviors. Therefore, the committee believes that school-related programs (including school-based and school-linked programs) and mass media campaigns should comprise two major components of an effective prevention strategy for adolescents.
Although school-based prevention programs should be a major means for preventing risky sexual behaviors among adolescents, it is not realistic to expect that such programs will be successful in all situations or that they will be effective in isolation. This is because such programs cannot control other influences on adolescent health behaviors, such as the mass media and peer and community norms regarding sexual behavior. In addition, the wide variability in the quality of and support for school-based programs in communities is a barrier to effectiveness of programs. Therefore, as with other interventions proposed by the committee, school-based programs must be implemented along with individual- and community-based interventions to promote healthy sexual behaviors. In evaluating school-based programs and other behavioral interventions to prevent STDs, it should be recognized that the outcomes of interest (e.g., reduction in STDs, reduction in risky sexual behaviors) are influenced by factors other than the intervention being studied. Therefore, evaluations of program effectiveness should account for other influences that exist under real world conditions.
Clinical services for adolescents need to be more accessible for reasons outlined in Chapter 3. Adolescents are one of the age groups least likely to have health insurance coverage: they infrequently present to regular health care facilities, and confidentiality is a major concern for them. In addition, the cost of health services may be a significant barrier. Many adolescents are seen at routine exams, including physical examinations for participation in sports, in school-related and family planning clinics, and by primary care professionals. Clinicians should utilize these and other appropriate clinical encounters to educate all and screen sexually active adolescents for STDs. For example, all adolescents should be counseled regarding methods to protect against STDs when prescriptions for
nonbarrier contraceptives are given and when they are evaluated for an unintended pregnancy.
As discussed in Chapters 4 and 5, ensuring confidentiality of services is extremely important, especially for adolescents. Given that most adolescents are unwilling to seek medical attention for an STD unless confidentiality is ensured, adolescents should be able to consent to STD-related services without parental knowledge. Forty-nine states and the District of Columbia currently have laws that give a minor explicit authority to consent to diagnostic and treatment services for STDs (AGI, 1995). Of these states, 16 allow physicians to notify parents of treatment provided. Pending federal legislation may interfere with a minor's ability to consent to STD-related services and could have a harmful impact on efforts to prevent STDs among adolescents. 4 As discussed in Chapter 5, billing and claims-processing procedures of some health plans may be a major barrier to confidential STD-related services. The committee believes that parental notification of treatment for an STD, either by providers or indirectly through billing or claim-processing procedures, is likely to discourage adolescents from seeking health care for potential STDs, and thereby increase the potential for STD-related complications and transmission to others.
There are significant numbers of adolescents who are disenfranchised. As documented in Chapter 3, a substantial number of adolescents live in detention facilities and group homes, or are sex workers or runaways or otherwise homeless persons. In addition, a substantial number of these adolescents were sexually abused as children. As a result, these youth often behave in a high-risk manner that puts them at increased risk for STDs and other health problems. All of these young people have significant problems obtaining health care and need access to comprehensive, high-quality health services in general and STD-related services in particular. Although school-based programs will reach the overwhelming number of adolescents, interventions for those who do not attend school should also be developed and implemented.
Therefore, the committee makes the following recommendations:
- A major part of a national strategy to prevent STDs should focus on adolescents, and interventions should begin before sexual activity is initiated, which may be before adolescence is reached. Interventions should focus on preventing the establishment of high-risk sexual behaviors.
- All health plans and health care providers should implement policies in compliance with state laws to ensure confidentiality of STD- and family-planning-related services provided to adolescents and other individuals. The following actions should be taken to ensure confidentiality of services:
- health plans should review billing or claims-processing procedures to ensure that they preserve confidentiality of services;
- the National Committee for Quality Assurance and other organizations that accredit health plans should ensure that a health plan's ability to ensure confidential access to STD-related services is appropriately assessed;
- state and local health professional organizations should disseminate information regarding the importance of maintaining patient confidentiality to their members; and
- the Academy of Pediatrics and other health professional organizations should educate pediatricians and other clinicians who provide health services to adolescents regarding the negative impact of parental notification for STD-related services.
Expanding School-Based Programs
Schools are critical venues for STD prevention activities. Survey data show overwhelming public support for school-based HIV/STD education programs. Studies cited in Chapter 4 show that school-based education programs are effective in improving knowledge regarding STDs, delaying adolescent initiation of sexual intercourse, and increasing use of condoms. Most teenagers indicate that the school is their primary source of information regarding STDs; this indicates that other sources of information are lacking.
Scientific studies and evaluations of school-based programs for STD prevention do not support the contention that such programs encourage students to have sex. Unfortunately, these programs have become highly controversial and efforts to provide STD-related education outside the home have been consistently resisted by certain groups. The committee recognizes that some parents and interested groups have sincere, deeply held personal beliefs regarding sex and STD education in schools that prevent them from supporting such programs. However, the committee believes that the scientific evidence presented in Chapter 4 in support of school-based educational programs for STD prevention is strong; that adolescence is the critical period for adopting healthy behaviors; and that school is one of the few available venues for reaching adolescents.
The committee believes that it is important to distinguish opposition to school-based programs and other STD prevention efforts that are primarily based on religious and personal beliefs from that based on systematic evaluations of program effectiveness or scientific research. Understanding the underlying reasons for such opposition can help communities resolve differences. Because of the controversial nature of the issue, health departments and other agencies and organizations desiring to implement a school-based STD prevention program should work closely with school administrators, health educators, teachers, parents, and students throughout the planning and implementation process.
Surveys cited in Chapter 4 show that many states specifically require schools
to offer instruction on HIV and/or STD prevention, and most health education teachers reported teaching STD prevention. However, studies indicate that instruction, when it exists, is not consistently implemented at an early enough age. In addition, teaching materials for STDs need to be developed. Current instruction is of inconsistent quality and effectiveness, and variable content and time is devoted to it. Besides providing information, school-based education programs need to provide students with the skills to implement healthy sexual behaviors. The committee believes that it is possible to increase knowledge, change attitudes, and influence behavior of adolescents by expanding the use of school-based health education curricula and by providing the training and support necessary to improve existing programs.
Given the high rates of sexual intercourse among adolescents and the significant barriers that hinder the ability of adolescents to purchase and use condoms (as cited in Chapter 4), the committee believes that the current evidence is sufficiently strong to recommend expansion of condom availability in schools. Definitive data regarding the effectiveness of condom availability programs in schools are limited, because such programs are relatively new and few have been designed for measurements of effectiveness. However, available data regarding school- and community-based condom availability programs cited in Chapter 4 suggest that such programs are effective. Data also show that both parents and students are highly supportive of such programs and believe that they have a positive effect on prevention of HIV infection and other STDs among adolescents. None of the studies reviewed by the committee suggests that access to condoms in schools results in increased sexual activity among students. Legal challenges to these programs based on constitutionality arguments have been found to be largely without merit. Because of the sensitive nature of this issue, it is clear that schools, school boards, public health officials, health plans, parents, and students will have to work closely together in establishing condom availability programs.
As discussed in Chapters 3 and 5, students in universities and colleges also are at high risk for STDs. The scope and quality of STD-related services in these institutions, however, are unclear. Because many adolescents and young adults do not have private health insurance, school and student health clinics should ensure that confidential and comprehensive STD-related services are available.
Hepatitis B vaccine is highly effective and recently has been recommended for all infants and adolescents (11- and 12-year-olds), as well as for other adolescents and adults at high risk for hepatitis B virus infection. Many adolescents and adults at high risk for this infection, however, have not been vaccinated. Immunizing adolescents is difficult because of their relatively infrequent encounters with health care professionals and inadequate access to health care. Until childhood hepatitis B immunization ensures that all adolescents are protected, all clinical opportunities to immunize adolescents against hepatitis B virus infection need to be utilized. This includes school-based and school-linked clinics and
dedicated public STD clinics. Ideally, all adolescents should be immunized before they become sexually active.
Therefore, the committee makes the following recommendations:
- All school districts in the United States should ensure that schools provide essential, age-appropriate STD-related services, including health education, access to condoms, and readily accessible and available clinical services, such as school-based clinical services, to prevent STDs. Ultimately, parents, teachers, health professionals, and others in the community should decide what kinds of instruction and services are most appropriate for specific grade levels. Specifically, school districts should:
- require that information regarding the prevention of STDs, including HIV infection, and unintended pregnancy be part of required health education instruction for all students. Such instruction should be part of a comprehensive health education curriculum that is sequential, age appropriate, and given every year. Instruction regarding STDs, including HIV infection, and unintended pregnancy should start before adolescents in the school become sexually active. Because the quality of health education in schools is currently variable, schools should modify and implement model programs, such as those identified and evaluated by the CDC or other organizations. Public health departments and nongovernmental, voluntary organizations should assist departments of education in developing or modifying health education curricula for local needs and in evaluating and disseminating effective school-based curricula and other interventions to reduce high-risk sexual behaviors. In addition, state and local departments of education should support or provide training for teachers and school administrators involved in instructing or advising students regarding STDs;
- ensure that condoms are available to students as part of a comprehensive STD prevention program. Condoms should be made available along with information regarding sexual decision-making, including delaying of sexual intercourse. Condom availability programs should also include instruction on proper use of the condom and should have an evaluation component to assess effectiveness. Local health departments, health plans, and other private sector organizations should form partnerships with schools to establish and maintain these and other STD prevention programs; and
- ensure that school-based and school-linked health clinics provide STD-related clinical services, such as counseling for high-risk sexual behaviors; screening, diagnosis, and treatment of STDs; and hepatitis B immunization for all students. Health plans should develop collaborative agreements with school-based and school-linked clinics, including payment for confidential STD-related services for plan enrollees that are provided by such clinics. Schools should work with local health plans to ensure fair reimbursement rates and confidentiality of
- services. In addition, universities and colleges should ensure that their student health services provide the above services.
- All health plans, clinicians, and publicly sponsored health clinics should provide or arrange for hepatitis B immunizations for their infant, adolescent, and adult patients according to the Advisory Committee on Immunization Practices (ACIP) guidelines. Given the difficulty in reaching adolescents in health care settings, public health officials should ensure that adolescents who are not immunized in health care settings are immunized through school-based or other community programs. Additional infrastructure and programs for vaccinating adolescents and adults at risk for hepatitis B virus infection, through settings such as public STD clinics, should be developed and implemented. This infrastructure may also be used when vaccines against other STDs become available. In addition, communities should consider including hepatitis B immunization for adolescents and children in the local immunization campaigns that have traditionally focused only on vaccines for young children.
Establishing New Venues for Interventions
The risk of STDs among disenfranchised groups can be significantly reduced through appropriate innovative interventions. Venues for intervention need to be expanded because these groups are difficult to reach through traditional health care settings. Health services for disenfranchised persons do not have popular support; as a result, such services have been marginalized and underfunded. However, because these groups represent reservoirs of infection for the community, and for other reasons, it is important that they receive appropriate STD-related services.
Currently, knowledge of sociocultural factors related to transmission of STDs is not sufficient to fully explain why some ethnic and racial groups in the United States have higher STD rates than the general population. As discussed in Chapter 2, poverty and sexual behavior do not entirely explain the higher rates of STDs in some groups. Other potential explanations, discussed in Chapter 3, that are associated with increased risk of STDs and their associated complications are known to vary across racial or ethnic groups. These explanations include inadequate access to health care, lack of awareness and knowledge of STDs, and substance use behaviors. Further research is needed to evaluate the role of sociocultural and other factors in STD transmission among different ethnic and racial groups.
It is important to recognize that the underlying cause of STDs is high-risk sexual behavior that is common among all racial and ethnic groups in the United States. Therefore, in this report, the committee proposes an approach to STD prevention that is focused on the specific behaviors and ecological factors that
put all individuals at risk. Race- and ethnic-specific rates of STD should not be used to stigmatize specific groups as high-risk populations, but rather they should be used to justify adequate attention and allocation of resources to reduce STD rates among these population groups. The committee recognizes that by its emphasis on behaviors common among all groups, it is possible that funds may be diluted and redirected away from certain high-risk communities to more general, lower-risk populations. The committee, however, does advocate focusing interventions on certain high-risk groups as discussed later in this section. The notion of focusing on behaviors that put all persons at risk rather than certain high-risk groups is reflected in current health policies. For example, the recommendation to screen all pregnant women for HIV, rather than screen only certain groups of pregnant women, reflects the notion that all pregnant women have had unprotected sexual intercourse. In order to appropriately address target behavioral risk factors, however, surveillance of sexual behaviors and STDs is essential.
Most of the research regarding drugs, alcohol, and STD transmission cited in Chapter 3 is cross-sectional in nature and does not allow for determination of cause and effect. The committee, therefore, cannot definitively estimate the impact of substance use on STD transmission. The associations between drug and alcohol use and STD transmission, however, are substantial and have important implications for improving STD prevention. Substance use increases the risk of STDs on an individual level by making it more difficult for persons to take protective actions against STDs. In the case of crack cocaine, drug use not only increases personal risk for STDs, but also has an effect on the prevalence of STDs in certain communities by altering social structures. An increased emphasis on outreach services for substance users is indicated because health services for such persons are fragmented and often not accessible. STD prevention efforts need to include individuals who are at risk for substance use and specifically target venues where substance users can be effectively reached with tailored interventions.
The increasing number of persons in correctional facilities represents a growing pool of people at risk of STDs and a potential source of infection for others when inmates are released. Data cited in Chapter 3 indicate that screening and treatment of all prisoners and detainees is an important public health strategy for the following reasons: (a) the prevalence of STDs is extremely high in this population; (b) treatment may reduce the spread of STDs in the community once detainees are released; (c) detention represents an ideal opportunity to screen for health problems in a population that does not ordinarily have access to health care; and (d) treatment reduces spread of STDs within detention facilities and averts associated long-term health care costs. Rapid screening and treatment of persons in detention facilities represent an opportunity to effectively contain STDs in a high-risk group. Because of lags in obtaining laboratory results, rapid turnover of detainees, poor treatment compliance, drug contraindications during pregnancy, and other issues, the optimal screening and treatment program for
detention facilities varies with the characteristics of the facility and population. At a minimum, all persons entering detention facilities should be screened and treated for STDs. As reviewed in Chapter 3, in addition to having high rates of STDs upon entry, some inmates continue to have high rates of unprotected sex and drug use while in prison. Therefore, diagnostic and treatment services, risk reduction, and other prevention programs for prisoners are needed. Prevention, early detection, and treatment are appropriate even for long-term prisoners because such a strategy is more cost-effective for the correctional system than treating the severe long-term complications of STDs.
Few correctional facilities currently provide access to condoms. Although condoms can be used as weapons or to conceal contraband, as cited in Chapter 3, the experience of correctional systems with condom availability programs indicates that such programs do not increase these problems. Given the circumstances under which sexual intercourse occurs among prisoners, research regarding the effectiveness of condom availability programs and other methods for reducing the prevalence of unprotected sexual intercourse within correctional facilities is indicated and should be supported by the Department of Justice and the Department of Health and Human Services.
Sex workers, runaways, and the homeless are at high risk of STDs and almost always lack health insurance and are difficult to reach. These populations, however, may be more accessible through nontraditional venues and mobile clinics. Examples of effective approaches to reach these groups are cited in Chapters 3 and 4. Migrant workers need access to STD-related services in an environment that minimizes cultural and language barriers. Because of the lack of education of most migrant workers, health education for STDs must begin at the most basic level. To address cultural and language barriers, peer educators may be effective in reaching many migrants and other groups.
Nontraditional venues for delivering STD-related services, such as detention facilities, drug treatment clinics, alcohol treatment facilities, and other sites where disenfranchised persons can be found, are appropriate sites for prevention activities. Most nontraditional venues for STD prevention have not been targeted by STD program staff, and there are many problems that may arise in implementing STD-related services in such settings. Appropriately trained staff and tools that are suitable for such situations are essential. For example, outreach workers commonly need multiple language and cultural sensitivity skills in order to effectively deliver services to these ethnically and culturally diverse groups. Despite the barriers that make delivery of services in these settings challenging, it is critical that STD-related services be provided in places where persons at high risk for STDs are frequently encountered. Such services may either be furnished by staff of these facilities or supplied through partnerships with local health departments, health plans, and other organizations. Given the evolving epidemiology of STDs, health officials need to continually monitor and reassess the most appropriate and effective community-based venues for prevention.
New biomedical, epidemiological, and behavioral tools are needed to contain persistent epidemics of STDs among disenfranchised populations. One of the major barriers to effective screening programs for disenfranchised populations is the relative lack of diagnostic tests that can be used outside of the health-care setting. Ideally, to maximize their usefulness in field situations, tests should be inexpensive and rapid and use noninvasive clinical specimens, such as urine or saliva. The ability to diagnose STDs using noninvasive clinical samples presents tremendous potential opportunities for innovative STD prevention programs. For example, this technology may enable more widespread clinician use of laboratory testing, allow for expansion of screening programs in venues not traditionally targeted by STD programs, and improve health-seeking behavior for STDs. In addition, improvements in the following areas would be beneficial in providing services to disenfranchised persons: rapid diagnostic tests for genital ulcer diseases; effective oral therapies that are suitable for use in community-based prevention campaigns; protocols for rapid assessments of community substance use patterns; and guidelines for STD screening in a variety of traditional and nontraditional health care settings. Innovative, effective, and rapid screening and treatment protocols for syphilis, such as that implemented in New York City's major facility for admission medical screening of female inmates (described in Chapter 3), should be considered.
Various government agencies have responsibility for delivering health services to disenfranchised persons but may not coordinate such services, thus gaps in services result. For example, a prisoner may be screened for an STD upon arrival but, unless the results are available before release, there is no assurance that the individual will be treated by a health care provider in the community. Given the variety of agencies that provide services to substance users, the Department of Health and Human Services, including the CDC and the Substance Abuse and Mental Health Services Administration, should work with other federal agencies to coordinate STD prevention programs for substance users. Providing STD-related services to disenfranchised persons requires innovative approaches, additional planning, and resource commitments because of the special considerations and staff skills that are needed to reach these populations.
Therefore, the committee makes the following recommendations:
- Federal, state, and local agencies should focus on reducing STDs among disenfranchised populations (e.g., substance users, persons in detention facilities, sex workers, the homeless, migrant workers) by:
- coordinating their various health-related programs to ensure effective, comprehensive STD-related services for populations at high risk for STDs. Coordination of services and sharing of resources are especially important for federal agencies (e.g., the Department of Health and Human Services, the Department of Justice) and should be priorities both among and within agencies;
- ensuring that STD prevention programs establish linkages with correctional facilities, substance use treatment programs, homeless and runaway programs, migrant health programs, and other facilities and programs that serve high-risk populations to ensure appropriate screening, diagnosis and treatment, and follow-up of infected persons and their partners. Such linkages should ensure that all adolescents and adults living in environments where the risk for STDs is high have access to confidential, comprehensive, high-quality STD-related services. In addition, the CDC, in collaboration with other appropriate agencies, should develop STD screening guidelines suitable for use in venues that have not been traditionally targeted by STD screening programs; and
- developing and implementing interventions and services for STDs that are (a) focused, sustained, and culturally appropriate; (b) provided by a spectrum of health care professionals, including potential non-health-care professionals such as educators, peers, and community volunteers; (c) delivered through a variety of settings, including nontraditional settings such as substance use treatment centers, mobile clinics, and the streets; and (d) reinforced at multiple points and venues to sustain and maximize effectiveness.
Strategy 4:
Ensure Access To Services
Strategy 4 is to ensure access to and quality of essential clinical services for STDs. As demonstrated in Chapter 5, both public and private sector clinical
services for STDs are currently fragmented, inadequate, and sometimes of poor quality. Timely access to clinical services for STDs is vital to prevent further transmission. Access to clinical services is supported by the absence of financial barriers to obtaining health services, minimization of nonfinancial barriers, assurance that patients will not be stigmatized, and assurance that services are sensitive to sociocultural diversity. Assuring access, however, is not a sufficient method of ensuring that clinical services are effective. Providing access in both the public and private sectors allows those who need services to get them, while quality assurance improves the likelihood that services will be effective when delivered. Ensuring access to and quality of clinical services maximizes coverage and effectiveness of STD-related services. Therefore, universal and timely access to high-quality clinical services should be the goal of the clinical care system.
Under Strategy 4, the committee proposes to improve and expand clinical services for STDs by (a) ensuring access to services at the local level, (b) improving dedicated public STD clinics, (c) expanding the role of health plans and purchasers of health services, (d) improving the training of clinicians, and (e) improving clinical management of STDs.
Ensuring Access to Community Services
Access to services is facilitated by expanding availability of STD-related services through primary care clinicians and by coordinating services at the local level.
Incorporating STD-Related Services into Primary Care
Effective STD-related care encompasses biomedical interventions (e.g., diagnosis and treatment); behavioral interventions (e.g., patient counseling); and social interventions (e.g., substance use prevention and treatment). Primary care providers can be effective coordinators of these types of health and social services in the community (IOM, 1996b). This is especially important for disenfranchised persons who are at high risk for STDs and other infectious diseases and require multiple services. Because primary care treats the individual in the context of other physical and mental health problems and fosters ongoing relationships between the clinician and the individual, the likelihood of early STD detection and effective preventive interventions, such as regular clinician counseling, increases. In addition, incorporating STD-related services into primary care may improve access to services since primary care clinicians are much more numerous than public STD clinics. Primary care providers diagnose the majority of STDs in the United States, and it is likely that primary care health professionals in the private sector will play a greater role in STD prevention.
Another reason for incorporating STD-related clinical services into primary care is the wide variation in the quality, scope, accessibility, and availability of
services currently provided by many public STD clinics. However, limited research has been performed regarding the quality and scope of STD-related services in primary care settings. While the committee is optimistic regarding the ability of primary care clinicians to improve STD-related services, it recognizes that barriers to their ability to provide comprehensive services, as outlined in this report, are substantial. Although many of these barriers need to be addressed before primary care clinicians are fully able to provide comprehensive STD-related services, the committee believes that the long-term process of incorporating STD-related services into primary care should begin as these barriers are addressed.
Whether in a fee-for-service or a managed care setting, privately insured patients usually receive STD-related services as part of comprehensive primary care or, for women, gynecological care. However, such services are isolated from public sector services and broader efforts to prevent STDs in the community. With very few exceptions, it appears that private health care professionals are unaware of both the prevalence of STDs among privately insured persons and the serious and expensive sequelae of undetected infections.
Therefore, the committee makes the following recommendation:
- Comprehensive STD-related services should be incorporated into primary care, including reproductive health services. Primary care should include the full range of STD-related services, including screening, diagnosis and treatment, partner notification and treatment, health education and counseling, and community outreach. Such services should be delivered by health care professionals with training in STD clinical management. These professionals may be STD specialists or primary care providers who have received STD-specific training. Regardless of the clinical setting, the provision of such services by poorly qualified health care professionals with no specific training in STDs is not recommended because it will result in inadequate diagnosis and treatment and poor coordination with other STD-related services.
Coordinating Services at the Community Level
Communities differ widely in their health needs and capacity to support a system of STD-related services. Therefore, the organization of community STD prevention services must be tailored to local needs and conditions. No single model will be appropriate for all communities. For example, only some communities will be able to depend on the teaching and research support of academic health centers that have established model STD prevention programs, including clinical capacity. Clinicians with training in STDs may be readily available in the private sector in urban areas, but difficult to find in rural areas. Communities with large numbers of high-risk persons and high STD rates may need a system of dedicated STD clinics, but communities with low STD rates may only require
primary care providers trained in STD prevention, diagnosis, and treatment. In addition, dedicated public STD clinics are not likely to be cost-effective in some rural communities that have high rates of STDs but relatively small populations.
Each community, through the leadership of the local health department, should ensure universal access to high-quality, comprehensive STD-related services. At a minimum, public and private sector health services should be coordinated to increase coverage and ensure optimal use of resources. Depending on local conditions, public health departments should incorporate STD-related services into other public and private primary health care services. Depending on epidemiologic patterns, health insurance coverage, population density, and other community characteristics, communities may continue to support dedicated public STD clinics or may shift such services to community-based clinics or the private sector. Dedicated public STD clinics may be phased out in communities with relatively few uninsured high-risk persons if public-private contractual arrangements ensure that STD-related clinical services will be provided by community-based and private sector clinicians in a timely manner. However, communities with a high prevalence of STDs, a large number of uninsured residents, or difficulty forging public-private partnerships are likely to find that public STD clinics are necessary to ensure universal access to comprehensive STD-related services.
Public health agencies may consider one or a combination of alternative models for providing services, including provision of services through contracts or agreements with public sector health programs, community-based health programs, universities or teaching hospitals, or private health care professionals, including managed care organizations and other health plans. Contracts and partnerships may include agreements regarding patient referral for specific services, sharing of resources, or shared administration and management of programs. Regardless of how community services are organized, local health departments must provide leadership in the community to ensure universal access, promote preventive services, conduct disease surveillance, ensure confidentiality of services, assess the effectiveness of services, train clinicians, and implement policies to prevent STDs (IOM, 1988).
Therefore, the committee makes the following recommendation:
- Local health departments, with the assistance of the state health department and in consultation with the community, should determine how to provide high-quality, comprehensive STD-related clinical services that meet federal and state quality standards most effectively in their communities.
Improving Dedicated Public STD Clinics
Public STD clinics are the primary source of STD-related services for the uninsured and provide an important focus for STD prevention at the community
level. The management and quality of services provided by dedicated public STD clinics, as described in Chapter 5, need significant improvement to ensure confidential, comprehensive, high-quality STD-related services for all persons. The committee has witnessed the wide variation in the quality, scope, accessibility, and availability of services provided by public STD clinics firsthand during their site visits and through their professional experience. Some public programs, usually university-affiliated, provide STD-related services that are personalized and efficient, and provide STD diagnostic and treatment services along with counseling and education, HIV testing and counseling, and family planning services. Many local health departments, especially in metropolitan areas, however, operate dedicated STD clinics that are isolated from other public health and personal health services, including HIV screening and counseling clinics. In many clinics, quality of care, monitoring, and assessment have not been a priority.
Ensuring Access and Quality
As discussed in Chapter 5, dedicated public STD clinics historically have emphasized serving large numbers of patients and their sex partners, who are identified through patient interviews. These clinics seldom emphasize the long-term disease management that chronic viral STDs require or effective long-term behavioral interventions that require multiple sessions. Examples of other appropriate long-term disease management activities include early management of HIV and hepatitis B virus infection, suppression of recurrent genital herpes, Pap smear screening and managing cervical dysplasia, administration of complete vaccination series for hepatitis B, and treatment of genital warts. In large cities, public STD clinics tend to be overwhelmed with patients, and provide impersonal care. Recruiting high-quality health care professionals to work in these settings is also difficult. In many small communities, dedicated STD clinics may be open for only several hours each week, relying on health personnel who may be inadequately trained in STDs and may have too many competing responsibilities. Moreover, these clinics often suffer from fragmentation and frequently are inefficiently managed.
Dedicated STD clinics help set community standards and train health professionals in STD prevention, including screening, risk assessment, diagnosis and treatment, partner notification, and education and counseling. In some areas, dedicated STD clinics serve as the focus for training of health professionals, performing clinical research in STDs, and setting standards for STD services in the public and private sectors. Although many small communities and communities with low STD rates do not require dedicated public STD clinics, nearly all states in the United States have one or more cities with such clinics. Again, local health officials need to assess the status of clinical services in their communities and determine the most appropriate model for delivering services. In all cases, health departments that operate dedicated public STD clinics should ensure that
these clinics collaborate with community-based health clinics, including family planning clinics and school-based programs, university and hospital medical centers, and private sector health care professionals, to improve the scope and quality of care in dedicated public STD clinics.
As previously mentioned, the committee supports incorporating STD-related services into primary care. The committee believes that, in some communities and situations, dedicated public STD clinics should continue to be an important component of STD prevention because, in most areas, persons who use public STD clinics usually are uninsured. Data cited in Chapter 5 indicate that convenience, confidentiality, low cost, and perception of expert care at public STD clinics are important to clinic users. The populations at greatest risk for STDs-the young, disenfranchised groups, and certain ethnic and racial groups-tend to have the least access to health care. One of every four persons 15-29 years old is uninsured. Lack of private health insurance and dependence on Medicaid suggest why some ethnic groups and persons with lower incomes account for a disproportionately large share of public STD clinic visits in many urban areas. Therefore, without universal health care coverage in the United States or improved access to STD-related services in the public and private sector, effective STD prevention will continue to require public STD programs to ensure access to STD-related services for the uninsured.
The committee is particularly concerned regarding the potential adverse public health impact of the recently enacted welfare reform legislation, proposals to restrict social and health services to immigrants, and the proposed reductions in the rate of growth of Medicaid funds. It is likely that such legislation will increase the number of persons without health insurance coverage, and thus without financial access to health services. It is also possible that the above policies will indirectly promote certain behaviors that increase risk for STDs or inhibit prompt health-seeking behaviors. Adding to these public policies, the continuing decline in employer-provided health insurance also is likely to increase the number of uninsured. These developments raise grave concerns that even larger numbers of persons will be dependent on publicly financed STD clinics, increasing the importance of this safety net at the same time that such services are being curtailed in some places.
Therefore, the committee makes the following recommendations:
- Based upon local conditions and health department determination, dedicated public STD clinics should continue to function as a ''safety net" provider of STD-related services for uninsured and disenfranchised persons and for those who prefer to obtain care from such clinics. Should universal health care coverage in the United States be achieved, or if proposed changes in the existing delivery system for STD-related clinical services, including incorporating STD-related clinical services into primary care and improved access to
- STD-related services in the public and private sector, are realized, the role of public STD clinics should be assessed.
- The CDC, in collaboration with state and local health departments, should ensure that services provided by dedicated public STD clinics are of high quality. This involves initiating the development of quality indicators and implementing and monitoring performance measures that reflect quality of services and health outcomes rather than program operation. quality standards are recommended in the following three general areas: (1) technical standards (e.g., diagnostic capability in STDs), (2) operational standards (e.g., hours of operation and convenience of services, staffing), and (3) program content standards (e.g., scope of services and referral networks). Quality standards for STD-related services should apply to services provided by both public and private sector health care professionals.
Collaborating with Academic Health Centers
Some of the most promising models for STD prevention in the United States have involved collaborative efforts between local public health departments and academic medical centers. Several such models (e.g., Albuquerque, Birmingham, Baltimore, Boston, Cincinnati, Raleigh (NC), Chicago, Indianapolis, Minneapolis, New Orleans, San Francisco, St. Louis, Seattle) have involved joint health department/medical center recruitment and appointments of medical staff and collaborative training of medical students and house staff. In some cases, the health department has contracted with the medical center for delivery of medical services while retaining direct control of outreach and laboratory support services. Less extensive collaboration models have been established in many other cities to provide medical staffing, training, research, and reference laboratory capabilities. These models most closely parallel the pattern of delivery of clinical services in other developed countries.
Although it is difficult to measure the impact of the academic health center/public health department collaboration model on community STD rates, the apparent success of these models in the United States is evidenced by their relatively greater effectiveness in obtaining local, state, and federal funding for programs; their role in training clinical and public health leaders in STD and HIV prevention; their roles as regional training centers for public and private sector clinicians; their development and early adoption of innovative methods for diagnosis, treatment, and behavioral intervention; and their role in surveillance and early recognition of emerging STDs. Although such models are effective in areas where they are implemented, the model is less feasible for rural areas and small communities with more limited access to academic health centers. Nevertheless, these partnerships have steadily increased and, in nearly every instance, have resulted in improved patient care and training for health care professionals and have increased the number of high-quality public STD programs. Such collaborations
are particularly important not only in improving quality of dedicated STD clinics, but also in providing professional training required to expand STD-related services into the private sector.
Therefore, the committee makes the following recommendation:
- Health professional schools, including schools of medicine, nursing, and physician assistants, should partner with a local health department for purposes of STD clinic staffing, management, and professional training. Support from federal and state governments should be provided as incentives for such collaboration.
Involving Managed Care Organizations and Other Health Plans
The committee believes that, if certain concerns are adequately addressed, there is substantial potential for managed care health plans to improve both the quality of and access to STD-related services. As summarized in Chapter 5, managed care organizations have several characteristics that represent important opportunities for enhancing STD-related services among persons enrolled in managed care health plans. Compared with other health plans, the structure and resources of many managed care organizations allow for improved coordination and integration of care, accountability of services, incentives to provide preventive services, and quality monitoring of services through information systems. Managed care organizations have the potential to provide higher quality, more comprehensive STD-related services than traditional indemnity health insurance plans and independent private practice clinicians, who may have little incentive to provide preventive services.
The committee identified some notable and impressive STD-related programs and activities among managed care organizations, as described in Appendix H. Some managed care organizations have developed and implemented STD or HIV prevention activities for both plan members and the community. Some large group- and staff-model managed care organizations are fully incorporating STD-related clinical services into routine practice. For example, Group Health Cooperative of Puget Sound, Harvard Pilgrim Health Care, and Kaiser-Permanente of Southern California offer a range of STD-related services, including education, screening, diagnosis, and treatment, relying on public health agencies for outreach, partner notification, and, often, counseling.
Although the committee believes that managed care health plans are capable of improving STD-related services, it recognizes that they have not yet fully demonstrated this capacity. Therefore, as managed care expands in the United States, the performance of such health plans in providing STD-related services should be carefully monitored and evaluated to determine the impact of such health plans on access and quality of services, especially among persons at high risk for STDs.
The potential concerns related to expanding the role of managed care organizations in STD prevention are summarized in Chapter 5. Practice constraints and financial incentives and methods for financing managed care and other health plans are potential barriers to health plans providing comprehensive STD-related services. As long as purchasers of health services are generally basing their decisions on premium costs rather than on enrollee health outcomes, many health plans are unlikely to fulfill their potential as providers of comprehensive STD-related care. It is important to note that there is great variation in the types of managed care plans and also variation within the types of managed care organizations. The extensive STD-related programs of a few group- and staff-model managed care organizations should not be assumed to reflect the interest or commitment of the less-structured health plans, which are far more numerous and cover a larger proportion of the population. In addition, the community outreach prevention programs of a few not-for-profit managed care organizations may not reflect the commitments or programs of investor-owned, for-profit managed care organizations. The committee is particularly concerned with the rapidly growing, less-structured health plans that do not have integrated delivery systems, lack health professionals with training in STDs, and have less-developed information systems. Some of these health plans do not fully participate in quality assurance activities or adequately monitor performance. Given the great variability in managed care organizations and other health plans, quality assurance and accrediting organizations, such as the National Committee for Quality Assurance, should promote measures that monitor the quality of STD-related services provided by health plans.
With very few exceptions, STDs are not yet high priorities among managed care organizations, and most are not involved in activities to prevent STDs in the general community. The committee's assessment is based on anecdotal information and was validated by a committee survey of managed care organizations that were considered to be likely providers of community health services (Appendix H). Given the limited data available regarding the scope and quality of STD-related services provided within the range of private sector health care settings, the CDC, in collaboration with the American Association of Health Plans, the National Committee for Quality Assurance, and the Health Insurance Association of America, should jointly sponsor or conduct a study to examine such services provided in private sector settings, including managed care organizations and other health plans.
There are several explanations for the general lack of involvement of managed care organizations and other health plans in STD prevention activities. STDs are not perceived as widespread problems among plan members or by purchasers and therefore are not a priority for many health plans. Second, the general lack of involvement in community-based prevention activities is consistent with market conditions. Driven by employers' and other purchasers' demands for lower premiums, virtually no health plan can afford to provide clinical
services without payment. To do so would add to their cost base and increase their premiums, an undesirable action in a competitive market. It is in a plan's best interest to invest in preventive services if the member stays with the plan long enough to lower his or her use of more expensive treatment services, such as services required to treat late sequelae such as cervical cancer. It may be less expensive for health plans simply to treat STD infections than to invest in specialized training for clinicians and to support more comprehensive STD prevention programs. Plans that have a small market share or operate in a volatile market may be unlikely to invest significantly in disease prevention because of the high turnover rate of enrollees. Finally, many health plans have not supported STD prevention activities because they have traditionally relied on the availability of services in public STD clinics and, as a result, have not developed the capacity to deliver comprehensive STD-related care.
STD prevention services may be in the long-term interests of enrollees and of the community, but the plan itself may not realize the rewards of that investment in the short term. It is interesting to note that certain preventive services have been widely adopted by health plans. In the case of childhood immunizations, which are typically provided by health plans, the benefit of the intervention is likely to be realized within a span of a few years. In the case of cancer prevention services, such as tobacco cessation services, which are not as widely covered by health plans, the greatest benefit (averting lung cancer) usually occurs many years later, but some benefits (decrease in respiratory disease) may occur in a shorter time period. Similarly, some sequelae of STDs occur within a few years (e.g., pelvic inflammatory disease, infertility, ectopic pregnancy, preterm delivery), while others occur only after many years (e.g., cervical and liver cancer, AIDS). Further, coverage of childhood immunizations by health plans has been stimulated in part by consensus guidelines. The U.S. experience indicates that only with structural, enabling, societal changes (e.g., requiring immunizations for entrance to school) have major advances occurred in widespread support for childhood immunizations. This paradigm suggests that practice guidelines and structural pressures (e.g., Medicaid contract requirements to provide services) are necessary to strengthen STD prevention efforts.
The prevalence of STDs among health plan members is underrecognized. Managed care organizations and other health plans need to develop capacity and become more involved in STD prevention activities directed toward both plan members and the community in which they operate. Preventive services for STDs, such as risk assessment and screening, are likely to avert significant health care costs associated with serious complications of STDs, such as cancer, infertility, and perinatal problems. For example, a previously mentioned study conducted in a managed care organization showed that screening and treating women at increased risk for asymptomatic chlamydial infection dramatically reduced the rate of pelvic inflammatory disease in one year (Scholes et al., 1996). In addition, by aiding STD prevention efforts among persons in the community who are not plan
members, health plans reduce the likelihood that their plan members will be exposed to infected partners. Health plans should also realize that screening and treating sex partners of plan members who are infected with an STD is in the interest of the health plan because such a strategy is likely to avert reinfections in the plan member. Finally, by participating in community-oriented activities and improving community health, health plans will help prevent long-term complications of STDs among persons who are not currently plan members, but may be in the future. Although the committee believes that health plans should develop capacity to provide comprehensive STD-related services, it recognizes that this will be a long process for many health plans. This is because some obstacles to full participation of health plans, such as assurance of confidentiality of services, coordination of services with public agencies, and legal considerations, must be addressed on several levels. In these cases, health plans, public health agencies, and purchasers of health services need to collaboratively address these issues.
It is important to note that, regardless of whether managed care and other health plans are successful in improving the scope and quality of STD-related care, private health plans are unlikely to provide services to uninsured persons in the near future. Therefore, this group of potentially high-risk individuals currently requires access to publicly sponsored services.
Therefore, the committee makes the following recommendation:
- Health plans should provide for or cover comprehensive STD-related services, including screening, diagnosis and treatment, and counseling regarding high-risk behavior for plan members and their sex partners , regardless of the partners' insurance status. The following actions should be taken to ensure that comprehensive STD-related services are available through health plans:
- Federal, state, and local health agencies and health plan member associations should educate health plan executives regarding the need for, and benefits of, providing comprehensive STD-related services.
- Employers and other purchasers of health services should require that STD-related services be provided as part of covered services in contracts with health plans.
- State and local governments should require health plans participating in Medicaid contracts to provide or cover such services.
Involving Employers and Other Purchasers of Health Care
Employers, government agencies, and other purchasers of health care services have a potentially powerful influence on the scope and quality of STD-related services provided by health plans. Purchasers are the key to ensuring that managed care organizations and other health plans provide comprehensive, high-quality
STD-related services. The committee believes that employers should be interested in the health of the general community because employers within a region are essentially drawing from the same employee pool. However, few managers who negotiate contracts with health plans are aware of the health and economic impact of STDs on their employees. Therefore, the public health community will need to encourage purchasers to consider STD prevention as a priority. Employers are interested in including preventive health services in their negotiated benefits packages, especially if the services are shown to be cost-saving for the company or organization. Some STD-related services are cost-effective, but may not be recognized as cost-saving; these services also need to be supported.
Therefore, the committee makes the following recommendation:
- Federal, state, and local health agencies should educate employers, Medicaid programs, and other purchasers of health care regarding the broad scope and impact of STDs and the effectiveness of preventive services for STDs.
Evaluating the Privatization of Services
In an effort to reduce costs, improve quality of services, or incorporate clinical services in primary care settings, many local governments are considering privatizing clinical services traditionally provided by local public health departments. Pressures on local health agencies, such as reduced funding for STD-related services and the enrollment of Medicaid beneficiaries into managed care health plans, are resulting in the shifting of services within the public sector and between the public and private sectors. Some agencies have begun to provide STD-related clinical services along with more comprehensive primary care services, and many are seeking ways to shift STD-related services to the private sector.
The costs, benefits, and sustainability of privatizing STD-related services should be carefully weighed. Several factors reduce the attractiveness of local health departments contracting out community-wide STD-related care to private health plans or private medical groups and clinics. First, health plans and private medical groups and clinics have generally shown little interest in providing clinical or other services to the entire community beyond their plan membership. Secondly, few health plans or private groups and clinics have experience providing comprehensive, high-quality STD-related services, especially to populations at high risk for STDs. Finally, and perhaps most important, many persons with STDs do not have health insurance and will not be served by any health plan. Although some private medical groups and clinics have offered to take over the role of public health clinics, they generally insist on receiving public funds to
fulfill that responsibility. It is not clear that this approach would be cost-effective or would result in more effective STD prevention.
Further, there is concern among local health departments that, even if more health plans develop strong STD-related clinical services, some privately insured persons will continue to seek STD-related care from public programs. Some Medicaid enrollees and privately insured persons who may have an STD or have been exposed to an infected person may not feel confident in obtaining STD-related services from their health plan provider or in having their condition recorded in the medical records of their health plan. Effective prevention of STDs requires that all persons exposed to an STD and at risk of acquiring an STD, especially adolescents, have access to services in an environment that ensures confidentiality.
Proponents of contracting out STD-related clinical services argue that directly providing clinical services is not an essential role of public health departments and that these services are most efficiently and effectively provided by the private sector. The committee is aware of both successful and unsuccessful attempts to privatize STD-related clinical services. As discussed earlier, some partnerships with medical schools have improved the quality of services in dedicated public STD clinics. Current data are not sufficient to determine under what circumstances, if any, privatization is cost-effective or results in better clinical care for persons with STDs. Regardless of whether local health departments choose to privatize such services, it is essential that local health departments, with assistance from state health departments, ensure that access is available and quality of services is regularly monitored and evaluated. The monitoring and assessment role of public health agencies requires agencies to monitor the prevalence of STDs in the community, identify high-risk populations or communities, and assess the adequacy of treatment and prevention efforts. This role also requires that government agencies monitor and ensure compliance with minimum standards for quality and accessibility of services. Effective performance of these roles requires improved collaboration among local health departments and community-based health services, private sector health care professionals, health plans, and other community stakeholders.
The recent trend toward managed care in many states is increasing the proportion of Medicaid beneficiaries who will have to obtain their health care from managed care organizations. These changes could potentially improve their access to primary care services. Most health plans, however, will require beneficiaries to obtain STD-related services from specific providers, and thereby reduce access to STD-related services provided by out-of-plan providers. Therefore, standards for access and quality should be developed for STD-related services provided by managed care organizations, other health plans, and by public-private sector arrangements.
Medicaid could be an important source of reimbursement for STD clinics, but the rapid spread of Medicaid managed care requires STD clinics to obtain
reimbursement for Medicaid patients from their health plans. To receive such payment, the clinics must become contract providers with the plans or receive payment for out-of-plan use of services, both of which could be encouraged or required by state Medicaid contracts. Agreements requiring managed care organizations and other health plans that participate in Medicaid contracts to reimburse public sector providers for STD-related services provided to plan beneficiaries, such as that developed by the Los Angeles County Department of Health Services, help ensure more equitable responsibility for supporting services (County of Los Angeles Department of Health Services, 1995). Local health departments should also consider incorporating performance requirements for STD-related services into any contracts with health plans. In addition, many federally supported STD clinics have provided free services to their patients. This has limited the ability of public STD clinics to obtain reimbursement from Medicaid for eligible patients. Public STD clinics should look to public health programs with a tradition of collecting patient fees and obtaining revenues from medical assistance programs, such as prenatal programs, community health centers, and family planning programs, as models. Health plans should provide enrollee access to public sector providers. As discussed in Chapter 5, some privately insured individuals may elect to go to a public STD clinic out of confidentiality or anonymity concerns or because of the perceived lack of quality or expertise in their health plan to provide STD-related services. Local health departments generally have not been prepared to bill private health plans for STD-related services, and since public sector providers are generally not in managed care organization networks, their services are considered "out of plan" and not reimbursed. This problem is made worse because health plans require enrollee permission for a provider to bill for services, thus threatening the very confidentiality sought by the enrollee.
Therefore, the committee makes the following recommendation:
- Health plans, including managed care organizations, should develop collaborative agreements with local public health agencies to coordinate STD-related services, including payment for STD-related services provided to plan enrollees by public sector providers, including public STD clinics. Local health departments should work with health plans to ensure fair reimbursement rates and confidentiality of services. State and local governments should require health plans that participate in Medicaid contracts to develop such agreements with local health departments. Collecting reimbursement for services will require health departments to develop billing capability for services, to seek permission from patients to bill, and, if this is denied, to require direct payment by the patient. In such cases, it is critical that patient confidentiality is not compromised. Given the current lack of data, federal health agencies such as the Health Care Financing Administration, the Health Resources and Services Administration, the CDC, and health plans should sponsor thorough evaluations of
- the impact of privatization of STD-related services on access and quality of such services in various communities before such privatization can be confidently endorsed.
Improving Training and Education of Health Care Professionals
Many factors, including availability of diagnostic and therapeutic resources, are important determinants of effective clinical management of STDs. However, more than any other factor, effective clinical management of STDs is dependent on adequate training and education of health care professionals. No matter how efficacious a clinical intervention may be under ideal conditions, it will not be effective unless the clinician delivering the intervention knows when and how to use it. The current system of clinical training for health care professionals, as outlined in Chapter 5, is inadequate in preparing clinicians to effectively manage patients with STDs. Studies examined by the committee suggest that many health care practitioners in both public or private settings are not sufficiently prepared to provide STD-related clinical services. Unless they are accompanied by appropriate training, changes in policy, increased funding, and implementation of clinical practice guidelines are not sufficient to ensure quality clinical care. Programs to train health professional students and practicing health care professionals in STD prevention are critical to increasing the capacity of the health care system to address STDs. The committee is encouraged by the apparent increase in clinical training in STDs in medical schools during the 1980s and urges all health professional schools to build upon this improvement and focus on the gaps in training identified in Chapter 5.
Inadequate professional training no doubt also contributes to the widespread tendency of clinicians to oversimplify and underestimate the importance of STDs. While STD diagnosis and management receives relatively little attention in health care training curricula, even less time is allocated to teaching STD risk assessment, patient counseling skills, methods of reducing risks for STDs, or treatment of sex partners. Training in diagnosis and treatment of sex partners is particularly important for health professionals who primarily treat persons of one gender. Discussion of risk and personal responsibility for sexual behavior is often awkward and uncomfortable for both the patient and health professional. As mentioned in Chapters 4 and 5, widespread misconceptions are shared by health professionals and their patients regarding STD risks, the signs and symptoms of STDs, and the importance of treating STDs promptly. These misconceptions contribute to the failure of many individuals with STDs, or at risk for STDs, to seek care and the failure of many health professionals to improve their own abilities to provide such services. There are limited data regarding the knowledge, skills, and training needs of specific types of health care professionals, and an assessment of these issues is necessary.
Familiarity with population-based health promotion and disease prevention
techniques, skills in evidence-based clinical decision-making, and patient communication skills are essential for every clinician. Many clinicians, however, do not have these skills or are not being consistently trained to use them to effectively prevent disease or diagnose and treat patients with STDs. Given the limited amount of time that is available in educational curricula, it may be most appropriate to focus primary care training on a core set of clinical competencies. The clinical skills needed to effectively manage patients with STDs are consistent with those identified as essential for primary care providers (IOM, 1996b).
Expanded training programs are urgently needed to ensure expertise in STD case management at the primary care level. In areas with university-affiliated public STD clinics, it is most efficient for primary care clinicians to develop expertise in STD case management given the high volume and range of STDs seen in these facilities. Thus, courses specifically designed for primary care providers should present the management of STDs within a primary care context, where patient care issues and other clinical resources are different from those of dedicated STD clinics. Continuing medical education courses should include STD practice management in settings without the specific diagnostic testing resources of an STD clinic and should emphasize patient management and partner treatment issues appropriate for a primary care setting.
Given evidence that health information provided by primary care clinicians has resulted in positive individual behavior change, the committee believes that communicating effectively with patients regarding sexuality issues and STDs is a critical skill for primary care professionals. Training in this area can be conducted in a number of ways and environments. Training modules should be modified to ensure that primary care providers will be able to fully incorporate this type of training into their practice situation.
The committee believes that training and education of health care professionals are paramount, but also recognizes the need to address other major factors that influence a clinician's ability to provide comprehensive services. These factors include practice format constraints such as inadequate time for risk assessment and counseling, especially within managed care environments that emphasize high productivity levels, and lack of systematically promulgated and institutionally supported approaches for risk assessment, screening, diagnostic testing, and counseling for STDs. In some situations, these factors may be problems of equal or greater importance than training.
New computer and telecommunications technology should be applied to improve training of health care professionals. Awareness and clinical knowledge of STDs among health care professionals should be improved by distance learning activities such as televised courses, developing interactive software modules for teaching clinical skills, and increasing electronic access to clinical information such as clinical practice guidelines. For example, medical and other health professional students may be able to practice STD-related diagnostic and patient communication skills with interactive computer software. In addition, primary
care practitioners in rural areas or areas where specialized training in STDs in not available may be able to access training modules or courses sponsored by the CDC, professional societies, or other organizations through distance learning programs. Staff in academic infectious disease clinics, dedicated STD clinics, federal, state, and local health departments, and primary care providers can develop shared information networks to exchange new information and epidemiologic data regarding STDs in order to improve clinical and public health practice. In addition, through telemedicine, infectious disease specialists may be able to assist in diagnosis and treatment of patients with STDs.
Therefore, the committee makes the following recommendation:
- The training of primary care providers in STD prevention should be improved by:
- training based on a core set of clinical competencies, including population-based health promotion and disease prevention techniques, evidence-based clinical decision-making skills, and patient communication skills. The training experience should include experience in both dedicated STD clinics and primary care settings and instruction regarding techniques to promote individual behavior change and improve disease reporting;
- improving medical student training in STDs by encouraging medical schools to provide clinical instruction in STD clinics to ensure that students see a sufficient variety of STDs;
- conducting an annual survey of medical schools through the Liaison Committee on Medical Education of the Association of American Medical Colleges and the American Medical Association to determine the extent to which medical schools are providing appropriate instruction in STD diagnosis and treatment;
- expanding collaborations among federal, state, and local STD programs; health professional organizations; graduate medical education; and other health professional training programs to include STD diagnosis and treatment as part of continuing medical education for all primary care providers;
- providing additional federal support to academic health centers to establish clinical expertise and clinic-based training opportunities for STDs; and
- encouraging state and local public health departments to identify primary care clinicians and clinics serving populations with high rates of STDs and provide STD-related education materials, training modules, and other technical assistance to them. The CDC should work with STD clinical training centers to develop training programs specifically designed for primary care providers.
Improving Clinical Management of STDs
The major components of effective clinical management for STDs include appropriate screening, diagnosis and treatment, risk reduction counseling and
education, and identification and treatment of sex partners. Each of these components represents essential responsibilities of every clinician and needs to be improved and expanded. Appropriate clinical management of STDs also requires access to quality laboratory services for screening and evaluation of potential STDs.
Improving and Expanding Screening Programs
Screening allows for the detection of infected persons who would otherwise remain undetected, develop complications of STDs, and potentially transmit the infection to their partners. Screening is only effective, however, if appropriate treatment and counseling are provided to identified persons. As summarized in Chapter 4, the U.S. Preventive Services Task Force has identified effective clinical preventive services for STDs, and several agencies and health professional organizations have published similar recommendations. These guidelines are important in establishing preventive services for STDs as standard clinical practice for all clinicians. The full implementation of clinical guidelines will require additional investment of resources, but, as discussed earlier, many of these preventive services are cost-effective and some are cost-saving.
Although the recommendations of various health professional groups regarding clinician screening are generally very similar, many of these organizations' recommendations differ in their definition of appropriate populations for screening. These and other differences in clinical guidelines can lead to confusion among clinicians and make it more difficult to ensure a consistent standard for STD-related clinical care.
There is considerable need to expand screening programs for STDs, especially for chlamydial infection and certain other STDs.5 Studies cited in Chapter 4 (e.g., Scholes et al., 1996), clearly show that associated serious health complications of STDs such as pelvic inflammatory disease and other reproductive health problems can be prevented by treatment of infections identified through screening. Expanded screening for STDs, particularly for chlamydial infection and in regions or population groups with inadequate access to health services, will have a significant impact in preventing health consequences of STDs among women. The committee does not recommend diagnostic screening for those viral STDs for which curative treatment or a clinically important intervention is not available. Given the association between HIV infection and other STDs and the impact of STDs on transmission of HIV, persons who utilize HIV testing and counseling services should also be screened for STDs as appropriate for the clinical setting.
Screening programs should be appropriately focused and should be based on
surveillance data and knowledge of the populations or geographic prevalence of STDs. These expanded programs should utilize diagnostic tests that are appropriate for screening persons in a variety of settings. Family planning clinics, prenatal clinics, facilities that provide pregnancy termination services, and other settings where obstetric or gynecological care is available should screen and treat women and their partners for sexually transmitted infections.
Premarital testing for syphilis, as a requirement for marriage licenses, is unnecessary and contributes little to containing syphilis because persons applying for marriage licenses are generally at lower risk for syphilis compared with the general population. Although these tests represent a source of revenue for some states, studies cited in Chapter 4 indicate that the number of previously undetected cases identified through premarital testing is extremely low; the tests are not cost-effective; and they have little public health impact. In addition, unnecessary testing may undermine public support for more appropriate screening programs, such as syphilis screening of women during early pregnancy.
Therefore, the committee makes the following recommendations:
- All primary care providers, including managed care organizations and other health plans, should implement the recommendations of the U.S. Preventive Services Task Force and the CDC regarding clinical screening and management of STDs. The CDC, the Agency for Health Care Policy and Research, the National Institutes of Health, and other federal agencies should collaborate with health professional organizations and representatives of health plans to develop comprehensive, consensus clinical practice guidelines for primary care clinicians for STD-related services including screening, risk assessment, and counseling and other clinical interventions to promote healthy sexual behaviors. These guidelines should build on the work of the U.S. Preventive Services Task Force and the CDC STD treatment guidelines. These agencies and organizations should also work together to minimize any differences in current recommendations regarding clinical screening and management of STDs and to promote consistent clinical guidelines.
- States that still have laws requiring premarital syphilis testing as a condition for marriage licenses should repeal these laws. Resources devoted to such testing would be more effective if used in other ways. States that rely heavily on revenue generated by such testing should consider alternative sources of revenue.
Improving Diagnosis and Treatment
The CDC's STD Treatment Guidelines are a valuable resource that represent the standard for treatment of STDs. Such treatment guidelines help to promote appropriate therapy for STDs on a national basis. Compliance with treatment guidelines is important because it helps ensure that patients receive the most
effective therapy. However, as documented in Chapter 5, there is limited awareness of, and compliance with, these guidelines, especially among private sector health care professionals in some regions. Appropriate diagnosis and treatment of STDs is most effectively accomplished by improving awareness and training of clinicians. Clinicians are ultimately responsible for ensuring that patients and their sex partners who are diagnosed with STDs are appropriately followed up and treated. When the diagnosis of an STD is laboratory-based, a mechanism for communicating results and following up on treatment should be established between the patient and the clinician.
Single-dose therapy for bacterial STDs is important in preventing complications and further transmission of STDs because it averts the problems of ineffective treatment associated with the failure of infected individuals to return for subsequent treatment or to take multiple doses of drugs. This attribute is especially valuable when treating disenfranchised persons. Single-dose therapy is most effective when it is directly provided and observed by the clinician, thereby ensuring patient compliance. Although single-dose therapy is more expensive than multidose therapy, it may be more cost-effective from a public health perspective for those populations in which compliance or follow-up are problematic.
Therefore, the committee makes the following recommendations:
- All clinicians should follow STD treatment guidelines recommended by the CDC and national medical professional organizations. The CDC should continue to publish and update the STD Treatment Guidelines. All health plans and national and state professional organizations, such as the American Medical Association, the American Academy of Pediatrics, the American College of Obstetrics and Gynecology, and the American Academy of Family Practitioners, should assist in the dissemination of these guidelines to their members and clinical staff.
- Single-dose therapy for bacterial and other curable STDs should be available and reimbursable in all clinical settings where STD-related clinical care is routinely provided to populations in which treatment compliance or follow-up are problems. Such therapy should be reimbursed by Medicaid programs and private health insurance plans. Although the pharmaceutical industry has been willing to provide single-dose therapies to public STD clinics at reduced contract prices, some public STD clinics and other public programs still lack sufficient funds to offer single-dose therapy in all situations where it is clinically indicated. Therefore, the pharmaceutical industry should consider further price reductions for public providers of STD treatment.
Improving Counseling and Education
Risk reduction counseling and education of patients during routine clinical encounters and during evaluations for potential STDs are important components
of STD clinical management. The U.S. Preventive Services Task Force and other professional organizations have recommended that all primary care providers counsel patients regarding the avoidance of high-risk sexual behaviors as part of the periodic health examination. The committee believes that although the ability of clinician counseling in primary care settings to change behavior is unproven, focused counseling in both specialized and general clinical settings has great potential for changing behaviors related to the transmission of STDs. The effectiveness of client-centered counseling for STD prevention in a randomized behavioral intervention trial (Project RESPECT) was mentioned in Chapter 4. Thus, counseling is most likely to be highly effective when it is tailored to the individual and is provided in the context of, and reinforced by, other individual-focused and community-based interventions. The experience of STD infection presents an important opportunity to motivate behavior change.
Counseling and education are especially important for adolescents and other groups at high risk of STDs. Major barriers described in Chapters 4 and 5 that hinder clinicians from providing counseling are primarily lack of training and skills in counseling, lack of time allocated for counseling, and lack of reimbursement for such services. To maximize the time available for individualized counseling, new methods of providing information, such as interactive computer software programs and use of other clinic-based counseling staff, should be used to supplement person-to-person counseling by time-constrained clinicians. It is important to develop and evaluate such innovative approaches to counseling and education because some clinicians may be unable, for various reasons, to provide comprehensive preventive services in all the primary care areas that are expected from them. These approaches not only reinforce prevention messages delivered directly by clinicians, but also allow clinicians an opportunity to provide more effective, individually tailored prevention messages.
Therefore, the committee makes the following recommendation:
- All health care professionals should counsel their patients during routine and other appropriate clinical encounters regarding the risk of STDs and methods for preventing high-risk behaviors. Counseling for STDs, including HIV infection, should be reimbursed without copayments or other financial disincentives by Medicaid programs, managed care organizations, and other health plans. The recommendations of the U.S. Preventive Services Task Force regarding counseling for high-risk sexual behaviors should be implemented. Clinical encounters, such as the new diagnosis of an STD or unintended pregnancy, evaluation for HIV infection, or the prescribing of contraceptives, present unique teaching opportunities, when patients may be particularly receptive to health education and counseling; these opportunities should be utilized.
Improving Partner Notification and Treatment
As discussed in Chapter 4, identification and treatment of partners is an essential component of STD clinical management because it reduces further transmission of STDs, prevents reinfection, and reduces risk of long-term complications of STDs in the infected partner. The case-finding activities of STD disease intervention specialists have been effective in containing outbreaks of bacterial STDs in discrete communities by promptly identifying and treating infected partners. In some countries, such as Sweden, partner notification for gonorrhea, syphilis, and chlamydial infection has been highly effective. However, the current methods of partner notification utilized by public STD clinics in the United States are extremely resource-intensive, inefficient, and in need of redesign. This is especially important given the high incidence of STDs among persons whose partners are unidentifiable, not easily reached, or uncooperative (and often participate in extended sexual networks).
No single model for partner notification is appropriate for all communities. One approach is to identify sex-partner networks in high morbidity areas and screen and treat members of the network. Another option is to replace the current method of notification with a combination of outreach efforts to identify partners and other individuals at high risk for STDs. The optimal combination of activities that are most effective at reaching persons at risk for STDs will vary depending on the local epidemiology of STDs, available resources, and the spectrum of local public and private health care professionals treating STDs.
STD programs need to develop new strategies and techniques for community outreach in partnership with other health care professionals rather than relying solely on health department or public STD clinic staff. It is essential that disease intervention specialists be sensitive to the local community. Other approaches include involving community-based organizations, designing and implementing outreach and screening activities, motivating private health care professionals to assist in partner notification, and assisting and motivating index patients to notify and assist their partners in seeking treatment. Limited data are available regarding the effectiveness and potential benefits of different approaches to partner notification, and further research is urgently needed to identify innovative and more cost-effective strategies for partner outreach at the individual and community levels.
As reflected in the committee's model, notifying partners of potential exposure to an STD should be a major responsibility of those persons who are infected. Community norms regarding the roles of groups or individuals in patient and partner referral need to be changed. However, health professionals need to recognize that certain individuals, especially adolescents and women, may experience difficulty notifying their partners and will require assistance in doing so. Few efforts have been made to explore the factors that affect the willingness or
ability of individuals to participate in patient referral, and research in this area is important to improve the overall effectiveness of patient referral.
Partner treatment should be addressed as part of the comprehensive STD care of anyone with an STD, whether managed in the private or public sector. A comprehensive strategy for partner outreach needs to include private sector health care professionals, because they treat a large proportion of STDs. Health care professionals who primarily treat patients of one gender (e.g., obstetricians and gynecologists) should be given appropriate training to improve clinical management of sex partners. Managers of clinical settings need to identify and address other potential clinic-specific barriers to effective partner diagnosis and treatment.
The concept that partner treatment is part of standard STD clinical management should be reinforced among private sector clinicians as well as among health plans. The committee believes that health care professionals and health plans have an ethical and public health obligation to ensure that the sexual contacts of their patients with STDs are notified promptly of potential exposures, counseled regarding risk factors for infection, and offered diagnostic testing and treatment. The responsibility for these activities in private health care settings historically has been relegated to public health agencies. This is often an inappropriate or ineffective method of ensuring prompt notification, counseling, testing, and treatment. The committee also believes that this obligation extends beyond health plan members because health plans have a responsibility to improve the health of the communities from which they draw their revenue (Showstack et al., 1996). As previously mentioned, treating partners in the community is in the long-term interest of both the health plan and health plan members.
Therefore, the committee makes the following recommendations:
- State and local health departments, with the assistance of the CDC, should redesign current partner notification activities for curable STDs in public health clinics to improve outreach, mobilize public health staff in new ways, and enlist support from community groups or other programs that provide services to high-risk populations. Changes in the system should be driven by results of cost-effectiveness research and formal prevention intervention trials on innovative approaches to partner notification. Communities and clients should also be involved in designing partner notification approaches to improve effectiveness and acceptability. Identifying sex-partner networks in high morbidity areas, with screening and outreach activities occurring within high-risk networks, should be one component of refocused partner notification activities. The CDC should support research to identify and evaluate innovative and cost-effective strategies for partner outreach and to determine those factors that may influence personal behavior or responsibility related to patient referral. In addition, local health departments should promote the coordination of partner notification
- activities by establishing linkages with other public agencies and private health plans.
- All health plans and clinicians should take responsibility for partner treatment and provide STD diagnosis and treatment to sex partners of plan members or others under their care as part of standard clinical practice. Diagnosis and treatment of partners should be reimbursable by third-party payers, including Medicaid, or by the partner's health plan if he or she is insured. All health plans and appropriate private health care professionals should participate, and develop capacity, in partner notification. Health professional organizations should educate their members regarding the importance of partner diagnosis and treatment.
Improving Availability and Capability of Laboratory Services
As reviewed in Chapter 4, access to appropriate laboratory testing is critical for accurate diagnosis of STDs and STD screening programs. Clinicians may have limited access to materials for diagnosis or laboratories with appropriate diagnostic tests. Therefore, qualified laboratories need to be available on a regional basis and do not need to be located in every clinical facility. Quality control and standardization of diagnostic tests are essential and should be systematically performed. Qualified public sector laboratories are available in many areas, but long-term availability of these laboratories may be jeopardized if health plans do not provide reimbursement for services or if competition with established commercial or hospital-based laboratories increases. Clinicians need to be aware that specimen adequacy and proper handling and transport of diagnostic specimens are needed to ensure accurate test results. Even with access to diagnostic testing, clinicians must have adequate training to appropriately select and interpret such tests. Use of nucleic acid detection rather than culture and sensitivity analysis, and syndromic diagnosis rather than laboratory-based diagnosis, may reduce the capability of public sector laboratories to perform certain public health functions such as the monitoring of antibiotic resistance of sexually transmitted pathogens. Public STD laboratory expertise should be maintained at the federal, state, and local levels to support clinical care of patients, monitor microbial resistance, and support surveillance of emerging STDs.
Therefore, the committee makes the following recommendation:
- Public sector laboratories should be reimbursed for STD-related laboratory tests performed on persons who have private health insurance coverage. Such laboratories should develop mechanisms to bill health plans for laboratory services. State and local health departments should negotiate adequate reimbursement for such services from health plans. In addition, public sector laboratories should ensure that the quality and cost of their services are competitive with those in the private sector. Qualified STD reference laboratories should
- be preserved at the regional level and strengthened where regional capabilities are lacking. Outsourcing and collaboration with private or university-based STD reference laboratories should be considered in sustaining and developing public sector reference laboratory capabilities.
Collaborating To Improve Services
In this section, the committee describes potential models for how the various providers of clinical services can work together to improve access to, and quality of, clinical services. In examining potential models for delivering services, the committee considered the many ongoing programs that they visited and heard about during the course of the study. The committee believes that the programs summarized in Appendix I serve as valuable models for agencies and organizations that are planning to develop collaborative activities. Because most of these programs have not been systematically evaluated for effectiveness, the committee does not necessarily endorse these specific programs, but rather encourages agencies and organizations to use these examples as the basis for developing collaborations to improve services.
Collaborating with Other Public Sector Health Programs
As in the case of community-based and private sector clinics, local health departments that provide STD-related clinical services should ensure that such services are provided in primary care settings, including reproductive health programs. The DeKalb County health department in Georgia, for example, has integrated STD and HIV screening and counseling services and is beginning to provide both services in family planning and primary care clinics. Some of the most promising efforts to provide STD-related services along with other public health services are focused on high-risk populations. For example, the Teen Services Program, sponsored by Emory University at Grady Memorial Hospital in Atlanta, and the Young Adult Clinic, operated by the Chicago Health Department with Vida/Sida, a community outreach program, target high-risk adolescents and young adults in inner-city communities. These projects focus on the comprehensive health and social needs of populations and individuals within the community, not just STDs. They bring together high-priority services for adolescents and young adults, such as STD screening and treatment, HIV testing and counseling, and contraceptive services and pregnancy testing, in a comprehensive health care setting. Although the Chicago project focuses on STDs, including HIV infection, and the Atlanta project focuses on pregnancy prevention, both emphasize education and behavior change related to sexuality. They are also both closely linked to schools; the Grady program is closely aligned with the Atlanta middle-school curriculum. Both programs also utilize ''peer experts" who provide outreach and education to other adolescents.
These various models reflect many of the characteristics of the Youth Clinics implemented in Sweden in 1972. There are 187 such clinics in existence in Sweden-a country with a population under nine million. These clinics provide comprehensive services to adolescents and are credited with a major positive impact on prevention of STDs and unintended pregnancy.
Collaborating with Community-Based Health Programs
Community-based health providers such as community health centers, family planning programs, and school-based health clinics are potentially important sources of STD-related services because they serve a patient population with a high prevalence of STDs. Although many community-based health programs currently provide STD-related clinical services, most have not made STD prevention a priority, despite its high prevalence in their patient population, and some do not have expertise in providing such services. There are, however, some notable exceptions to this observation.
Programs that provide family planning services, for example, have long recognized the importance of integrating STD clinical and educational services into family planning services, although not all programs provide STD-related services. In Chicago, Planned Parenthood provides STD- and HIV-related services in the context of comprehensive primary care for women and adolescents, while focusing on reproductive health. Using a population-based public health approach, the Chicago Planned Parenthood program provides outreach and education services directly to several high schools and through its clinics. The West End Community Health Center in Atlanta has developed a substantial STD program and provides STD-related services along with extensive primary care services. In this comprehensive model, clients receive STD screening, diagnosis, and treatment through their primary care provider of choice. Outreach, follow-up, and special counseling and education are available through clinic-based staff in collaboration with the local health department STD program staff. Most important, services are centered on the patient, coordinated by a primary care provider, documented in a single medical record, and monitored by relevant public health agencies.
In addition, local health departments in several cities (e.g., Baltimore, Boston, Denver, Minneapolis, and Portland) have developed collaborative pilot programs linking school-based health centers sponsored by the health department with local managed care organizations (Schlitt et al., 1995; Zimmerman and Reif, 1995). These programs provide comprehensive primary care, easily accessed at school, and multidisciplinary health education, health promotion, and mental health and social services. All routine STD- and reproductive-health-related care is provided through these centers. Agreements with the participating managed care organizations have enabled the providers in the school-based health center to
act as primary care providers, referring plan enrollees to other plan services as needed.
An example of an effort to promote collaboration at the national level is the CDC's National Partnership to Prevent STD-Related Infertility, which is intended to prevent infertility and other serious complications of chlamydial and gonococcal infections. The partnership seeks to prevent these infections through collaborations with a variety of traditional and nontraditional stakeholders in STD prevention. The action plan for the partnership focuses on coordination and integration of STD-related services, public education, health professional education, quality assurance for diagnosis and treatment, community-level behavior change, and surveillance and program evaluation (CDC, DSTD/HIVP, 1995). In addition, the demonstration projects cosponsored by the CDC and the Office of Population Affairs are increasing collaboration among dedicated public STD clinics, family planning clinics, and public laboratories. The committee believes that these types of collaborative approaches should be expanded to all STDs.
Concluding Statement
STDs are hidden epidemics of tremendous health and economic consequence in the United States. They are hidden because many Americans are reluctant to address sexual health issues in an open way and because of the biologic and social characteristics of these diseases. STDs are diseases of national and global importance that have a dramatic impact on local communities. All Americans have an interest in STD prevention because all communities are impacted by STDs, and all individuals directly or indirectly pay for the costs of these diseases. STDs are public health problems that lack easy solutions because they are rooted in human behavior and fundamental societal problems. Indeed, there are many obstacles to effective prevention efforts. The first hurdle will be to confront the reluctance of American society to openly address issues surrounding sexuality and STDs. Despite the barriers, there are existing individual- and community-based interventions that are effective and can be implemented immediately. Although these interventions are not perfect, they can have a synergistic, positive impact in reducing the risk of STDs in the population. That is why a multifaceted approach is necessary at both the individual and community levels. Populations at high risk, such as adolescents and disenfranchised persons, will need special attention.
An effective system of STD prevention in the United States will have to be developed at the local, state, and national levels, with full participation of both the public and private sectors. Many of the essential components of an effective system already exist, but they need to be integrated or coordinated, particularly at the local level. Many of these components also need to be improved and redesigned in order to maximize effectiveness and optimize resources. This means that many stakeholders need to redefine their mission, refocus their efforts, modify
how they deliver services, and accept new responsibilities. In this process, strong leadership, innovative thinking, partnerships, and adequate resources will be required. The additional investment required to effectively prevent STDs may be considerable, but it is negligible when compared with the likely return on the investment. The process of preventing STDs must be a collaborative one. No one agency, organization, or sector can effectively do it alone; all members of the community must do their part. A successful national initiative to confront and prevent STDs requires widespread public awareness and participation and bold national leadership from the highest levels.
References
AGI (Alan Guttmacher Institute). Lawmakers grapple with parents' role in teen access to reproductive health care. Issues in Brief. New York and Washington, D.C.: AGI, 1995.
AMA (American Medical Association). Policy compendium on reproductive health issues affecting adolescents. Gans Epner JE, ed. Chicago: AMA, 1996.
Aral SO, Holmes KK, Padian N, Cates W. Overview: individual and population level approaches to the epidemiology and prevention of sexually transmitted diseases and human immunodeficiency virus infection. J Infect Dis 1996;174(Suppl 2):S127-33.
ASTHO (Association of State and Territorial Health Officials). Access and managed care: oxymoron or reality? Washington, D.C.: ASTHO, Managed Care Monograph Series, November, 1995a.
ASTHO. Communicable disease control in a managed care environment. Washington, D.C.: ASTHO, Managed Care Monograph Series, November, 1995b.
ASTHO. Ensuring and improving the quality of care in a managed care environment. Washington, D.C.: ASTHO, Managed Care Monograph Series, November, 1995c.
Cates W Jr. Contraception, unintended pregnancies, and sexually transmitted diseases: why isn't a simple solution possible? Am J Epidemiol 1996;143:311-8.
CDC (Centers for Disease Control and Prevention). Trends in sexual risk behavior among high school students-United States, 1990, 1991, and 1993. MMWR 1995;44:124-5, 131-2.
CDC, DSTD/HIVP (Division of STD/HIV Prevention). Plan for a national partnership to prevent STD-related infertility. Draft internal document, January 10, 1995.
County of Los Angeles Department of Health Services. Draft agreement between the County of Los Angeles and plan. March 29, 1995.
Grosskurth H, Mosha F, Todd J, Mwijarubi E, Klokke A, Senkoro K, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomized controlled trial [see comments]. Lancet 1995;346:530-6.
Halpern CT, Udry JR, Suchindran C. Effects of repeated questionnaire administration in longitudinal studies of adolescent males' sexual behavior. Arch Sex Behav 1994;23:41-57.
IOM (Institute of Medicine). The future of public health. Washington, D.C.: National Academy Press, 1988.
IOM. Healthy communities: new partnerships for the future of public health. Stoto MA, Dievler A, Abel C, eds. Washington, D.C.: National Academy Press, 1996a.
IOM. Primary care: America's health in a new era. Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Washington, D.C.: National Academy Press, 1996b.
IOM. Improving health in the community: a role for performance monitoring. Durch JS, Bailey LA, Stoto MA, eds. Washington, D.C.: National Academy Press, 1977.
NACCHO (National Association of County and City Health Officials). Blueprint for a healthy community: a guide for local health departments. Washington, D.C.: NACCHO, July 1994.
NCASH (National Commission on Adolescent Sexual Health). Facing facts: sexual health for America's adolescents. New York: SIECUS, 1995.
NIH (National Institutes of Health). NIH AIDS Research Program Evaluation. Behavioral, social science, and prevention research area review panel. Findings and recommendations. Bethesda, MD: National Institutes of Health, 1996.
NRC (National Research Council). Assessment of performance measures in public health. Phase 1 report. Washington, D.C.: National Academy Press, in press.
Russell LB. Educated guesses. Making policy about medical screening tests. Berkeley, CA: University of California Press, 1994.
SAM (Society for Adolescent Medicine). Special issue on guidelines for adolescent health research. J Adolesc Health 1995;17:259-332.
Schlitt JJ, Rickett KD, Montgomery LL, Lear JG. State initiatives to support school-based health centers: a national survey. J Adolesc Health 1995;17:68-76.
Scholes D, Stergachis A, Heidrich FE, Andrilla H, Holmes KK, Stamm WE. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. New Engl J Med 1996;334:1362-6.
Showstack J, Luire N, Leatherman S, Fisher E, Inui T. Health of the public. The private-sector challenge. JAMA 1996;276:1071-4.
Sparling PF, Aral SO. The importance of an interdisciplinary approach to prevention of sexually transmitted diseases. In: Wasserheit JN, Aral SO, Holmes KK, Hitchcock PJ, eds. Research issues in human behavior and sexually transmitted diseases in the AIDS era. Washington, D.C.: American Society for Microbiology, 1991:1-8.
Stryker J, Coates TJ, DeCarlo P, Haynes-Sanstad K, Shriver M, Makadon HJ. Prevention of HIV infection. Looking back, looking ahead. JAMA 1995;273:1143-8.
Wasserheit JN. Effect of changes in human ecology and behavior on patterns of sexually transmitted diseases, including human immunodeficiency virus infection. Proc Natl Acad Sci 1994;91:2430-5.
Wasserheit JN, Aral SO. The dynamic topology of sexually transmitted disease epidemics: implications for prevention strategies. J Infect Dis 1996; 174 (Suppl 2):S201-13.
Wasserheit JN, Hitchcock PJ. Future directions in sexually transmitted disease research. In: Quinn TC, ed. Sexually transmitted diseases. New York: Raven Press Ltd., 1992:291-325.
Zimmerman DJ, Reif CJ. School-based health centers and managed care health plans: partners in primary care. J Public Health Manage Prac 1995;1:33-9.