3
Factors that Contribute to the Hidden Epidemic
|
Highlights
|
STDs are behavior-linked diseases that result from unprotected sex. Behavioral, biological, and social factors contribute to the likelihood of contracting an STD. Wasserheit (1994) has described how microenvironments, including microbiological, hormonal, and immunologic factors, influence individual susceptibility and transmission potential for STDs. These microenvironments are partially determined by an individual's sexual practices, substance use, and other health behaviors. These health behaviors, in turn, are influenced by socioeconomic, epidemiologic, and other macroenvironmental factors. In this chapter, the committee examines biological factors contributing to the spread of STDs and shows how both broad and specific social factors affect exposure to STDs and create obstacles to STD prevention. In Chapter 4, the committee examines behavioral factors contributing to risk of STDs.
Biological Factors
In Chapter 2, several biological factors that affect the risk of acquiring or
transmitting STDs, such as gender and other preexisting or concurrent STDs including HIV infection, were discussed. Other biological factors that contribute to the spread of STDs include the lack of conspicuous signs and symptoms manifested by infected persons, the long lag time from initial infection to signs of severe complications, and the propensity of STDs to more easily infect young women and female adolescents than men. In addition, the committee summarizes the potential impact of male circumcision, vaginal douching, risky sexual practices, and other factors on the spread of STDs or risk of sequelae.
Asymptomatic Infections
As discussed in Chapter 2, many STDs either do not produce acute symptoms or clinical signs of disease or do not produce symptoms sufficiently severe for an infected individual to seek medical attention. For example, as many as 85 percent of women with chlamydial infection are asymptomatic (Fish et al., 1989; Judson, 1990; Stamm et al., 1990). A study of college women seen for routine gynecological examinations found that 79 percent of those who tested positive for chlamydial had no symptoms of disease (Keim et al., 1992). Asymptomatic infection also contributes to the spread of viral STDs including HIV infection, hepatitis B virus infection, genital herpes, and human papillomavirus infection. HIV infection is a prime example of how certain STDs that may go unrecognized for many years allow wide dissemination of infection before it is detected and treated. Lack of awareness that most cases of certain STDs are asymptomatic or otherwise unrecognized leads many susceptible persons to falsely believe that it is possible to tell whether a potential partner is infected with an STD, and similarly explains why many infected asymptomatic persons fail to take precautions to avoid transmitting their infection. Even when symptoms are present, many STDs have nonspecific signs and symptoms, making them difficult to diagnose without laboratory tests. Asymptomatic infection, therefore, is an extremely important biological factor that reduces the likelihood that infected individuals will seek health care and/or receive appropriate diagnoses. This hinders detection and treatment of the infection, increases the period of infectiousness, and thereby promotes the spread of the infection.
Lag Time to Complications
Another biological factor that contributes to the STD epidemic is the long period of time (sometimes years or decades) from initial infection until the appearance of clinically significant problems. The best examples of sexually transmitted pathogens and complications that have long lag times are (a) human papillomavirus and cervical cancer and (b) hepatitis B virus and liver cancer. In both instances, the initial phase of the infection is often asymptomatic and creates obstacles to detection and treatment, as noted above. In addition, the clinical
signs of the associated life-threatening cancers usually do not appear until years or decades after the initial infection. Because of this phenomenon, many cases of STD-related cancers and other long-term complications are not attributed to a sexually transmitted infection. At both individual and population levels, the lack of a perceived connection between sexually transmitted infections and these serious complications reduces both the perceived significance of STDs and the motivation to undertake preventive action. Although the lag time between exposure to HIV and development of clinical symptoms of AIDS likewise can be quite long, there is greater awareness of the link between unprotected sex and the risk of acquiring HIV, and ultimately AIDS, compared to other STDs.
Increased Susceptibility of Women and Female Adolescents
Age and gender may influence risk for an STD. Specifically, as mentioned in Chapter 2, young women and female adolescents are more susceptible to STDs compared to their male counterparts because of the biological characteristics of their anatomy (Cates, 1990). This is because in puberty and young adulthood, specific cells (columnar epithelium) that are especially sensitive to invasion by certain sexually transmitted organisms, such as chlamydial and gonococcus, extend from the inner cervix out over the vaginal surface of the cervix, where they are unprotected by cervical mucus. These cells eventually recede into the inner cervix with age.
In addition to biological factors, women and female adolescents may also find it more difficult than men to implement protective behaviors, partly because of the power imbalance between men and women (Elias and Heise, 1994; IOM, 1994). For example, condoms are the most effective protection against STDs for sexually active persons, but the decision whether to use a condom is ultimately up to the male partner, and negotiating condom use may be difficult for women (Rosenberg and Gollub, 1992). The determinants of condom use are discussed in Chapter 4.
Other Biological Factors
Other biological factors that may increase risk for acquiring, transmitting, or developing complications of certain STDs include presence of male penile foreskin, vaginal douching, risky sexual practices, use of hormonal contraceptives or intrauterine contraceptive devices, cervical ectopy, immunity resulting from prior sexually transmitted or related infections, and nonspecific immunity conferred by normal vaginal flora.
Lack of male circumcision seems to increase the risk of acquiring and perhaps transmitting certain STDs. A review of 30 published epidemiological studies that examined the relationship between HIV infection and male circumcision concluded that most studies found a statistically significant association between
lack of circumcision and increased risk for HIV infection (Moses et al., 1994). In a prospective study of men at high risk for STDs, those who were not circumcised were 8 times as likely to become infected with HIV than circumcised men (Cameron et al., 1989). Another study of gay men suggested that uncircumcised men were twice as likely to be infected with HIV compared to circumcised men (Kreiss and Hopkins, 1993). As a result of these studies, some have proposed that male circumcision be considered an intervention to prevent HIV infection. Several studies have found associations between lack of circumcision and other STDs, including chancroid (Aral and Holmes, 1990). It has been hypothesized that lack of circumcision increases risk for STDs because (a) the cells that line the fold of skin that is removed by circumcision are prone to trauma or infection, (b) this fold of skin may serve as a reservoir for pathogens, and (c) this fold of skin may increase the likelihood that infections will go undetected (Aral and Holmes, 1990).
Vaginal douching seems to increase risk for pelvic inflammatory disease (Forrest et al., 1989; Wolner-Hanssen, Eschenbach DA, Paavonen J, Stevens CE, et al., 1990;). In one study, compared to women who did not douche, women who douched during the previous 3-month period were twice as likely to have clinical pelvic inflammatory disease (Scholes et al., 1993). The risk for pelvic inflammatory disease seems to increase with greater frequency of douching (Wolner-Hanssen, Eschenbach DA, Paavonen J, Stevens CE, et al., 1990; Scholes et al., 1993).
Certain sexual practices such as receptive rectal intercourse predispose to STDs. As mentioned in Chapter 2, STDs such as HIV infection and hepatitis B virus infection are more easily acquired by rectal intercourse than by vaginal intercourse. This may be because the bleeding and tissue trauma that can result from rectal intercourse facilitate invasion by pathogens. Other sexual practices, such as sex during menses and "dry sex," also predispose to acquisition of an STD.
The influence of hormonal contraceptives on acquisition and transmission of STDs is not fully defined. However, several studies have found oral contraceptive use to be associated with increased risk of acquiring chlamydial infection (Critchlow et al., 1995) but with decreased risk of developing pelvic inflammatory disease among women with chlamydial infection (Wolner-Hanssen P, Eschenbach DA, Paavonen J, Kiviat N, et al., 1990; Kimani et al., 1996). Some, but not all, studies have found an association of oral contraceptives with increased risk of HIV acquisition (Cates, in press). A recent study in Kenya has demonstrated that use of oral contraceptives or injectable progesterone among women with HIV-1 infection is associated with increased shedding of HIV-1 DNA from the cervix (Mostad et al., 1996). In one animal model study, monkeys with progesterone implants were several times more likely to become infected with the simian immunodeficiency virus than monkeys who did not have such implants (Marx et al., 1996). More study is indicated, but these data raise the
possibility that hormonal contraceptives may increase the likelihood of infectious genital tract secretions in HIV-infected women and/or increase susceptibility to HIV infection.
Cervical ectopy (extension of columnar epithelial cells present in the adult endocervix onto the exposed portion of the cervix within the vagina) has also been found to be a risk factor for HIV infection (Moss et al., 1991). Among women attending an STD clinic and among college women, cervical ectopy was positively associated with use of oral contraceptives and with chlamydial infection; ectopy disappeared with increasing age (Critchlow et al., 1995).
As previously discussed, other STDs can increase risk for acquiring or transmitting HIV infection. However, prior infection with certain STDs can provide specific immunity against reinfection with the same pathogen (Plummer et al., 1989; Brunham et al., 1994). Cross-immunity (protection conferred by prior infection with a different pathogen) also occurs. For example, a prospective study of women found that asymptomatic shedding of herpes simplex virus type 2 occurs more often during the first three months after acquisition of primary type 2 disease (Koelle et al., 1992). Among persons with herpes simplex virus type 2 infections, previous infection with type 1 virus was associated with a lower rate of asymptomatic viral shedding. This observation suggests that, as prevalence of herpes simplex virus type 1 infections in childhood decline, the risk of herpes simplex virus type 2 infection may be increased when this STD is encountered by a sexually active adult. Nonspecific immunity may make some individuals more resistant to certain STDs even though they have never experienced prior STDs or related infections. For example, the normal vaginal flora contains hydrogen-peroxidase-producing bacteria that have antimicrobial activity. Recent data suggest that women with bacterial vaginosis who lack hydrogen-peroxidase-producting bacteria (lactobacilli) are at increased risk of gonorrhea (Sharon Hillier and King Holmes, University of Washington, unpublished data, 1996; Martin et al., 1996).
Social Factors
On a population level, preventing the spread of STDs is difficult without addressing social issues that have a tremendous influence on transmission of STDs. Some fundamental societal problems such as poverty, lack of education, and social inequity indirectly increase the prevalence of STDs in certain populations. In addition, lack of openness and mixed messages regarding sexuality create obstacles to STD prevention for the entire population and contribute to the hidden nature of the STDs. In the following discussion, the committee highlights several social problems that directly affect the spread of STDs in subpopulations and shows how societal norms regarding sexuality impede prevention of STDs. In Chapter 4 the committee describes interventions that can be used to lessen the
adverse impact of these social problems on STDs, even if these dilemmas are not solved directly.
Poverty and Inadequate Access to Health Care
Health insurance coverage enables individuals to obtain professional assistance in order to prevent potential exposures to sexually transmitted infections and to seek care for suspected STDs. Uninsured persons delay seeking care for health problems longer than those who have private insurance or Medicaid coverage (Freeman et al., 1987; Donelan et al., 1996). Those with private health insurance who are living at or near poverty level have limited access to health care because of copayments and deductibles that are typically part of private insurance coverage (Freeman and Corey, 1993). Medicaid coverage is often less effective than private health insurance coverage since many physicians refuse to treat Medicaid beneficiaries, thereby restricting access to comprehensive health services (Schwartz et al., 1991).
Private health insurance generally provides the most comprehensive coverage with the greatest access to physicians and other health care professionals. However, not all plans offer adequate coverage for STD-related services. Little information is available on coverage for STD-related services in the private health care sector. A recent study of how women pay for reproductive health care suggests that many health plans either do not cover some important STD-related preventive reproductive health services or require copayments and deductibles for these services (WREI, 1994). STD-related diagnostic and treatment services are covered under general clinical care. However, the study found that only about half of all health plans cover preventive care such as routine gynecological examinations that may be important in detection of asymptomatic sexually transmitted infections.
Managed care organizations may provide better coverage for certain STD-related services than do many indemnity health plans, but they pose different challenges to the prevention of STDs, particularly for many Medicaid beneficiaries enrolled in managed care. Most managed care organizations require their enrollees to obtain all their health services from the plan's network of providers. This disrupts established patterns of STD care for many women on Medicaid by denying patients access to their preferred providers. A recent study found that neither the federal government nor the states had taken steps to ensure that Medicaid beneficiaries enrolled in managed care organizations could obtain services from family planning programs or public STD clinics (Rosenbaum et al., 1995). A number of family planning programs have taken the initiative to develop contracts with managed care organizations that serve Medicaid clients, thus both avoiding the problem of nonreimbursed out-of-plan use and retaining an important source of revenue for their program (Orbovich, 1995). This is an especially important policy issue as states increasingly encourage or require Medicaid
beneficiaries to enroll in managed care organizations. The role of managed care organizations and other health plans in STD prevention is further discussed in Chapter 5.
Health insurance coverage influences where people obtain STD services. A recent study found that uninsured women and those covered by Medicaid were far more likely to obtain reproductive health services from a public or community-based clinic rather than a private physician's office, compared to women who were covered by either a managed care organization or other private health insurance (Sonenstein et al., 1995). Even those with adequate insurance coverage may be reluctant to obtain care for potential STDs from their regular health care providers because of the social stigma associated with these infections. A significant number of persons with private insurance are reluctant to bring STD exposures to the attention of their family doctor or health plan and prefer the anonymity of a public STD clinic or other public clinic (Celum et al., 1995).
In 1993, 40.9 million Americans, or 18.1 percent of the nonelderly population, were not covered by any public or private health insurance coverage, up from 39.8 million or 17.8 percent of the nonelderly population in 1992 (EBRI, 1995b). Further analysis of these data revealed that of the 1.1 million increase in uninsured persons from 1992 to 1993, 900,000 or 81.8 percent of the newly uninsured population were children and youth under 18 years of age (EBRI, 1995a).
The age and ethnic groups with the highest rates of STDs are also the groups with the poorest access to health services. One-third of persons in high-risk age groups are uninsured or covered by Medicaid (UCLA Center for Health Policy Research, unpublished data, 1996). Among persons 15-29 years of age, 25 percent are completely uninsured (Figure 3-1), including one in every five persons 15-20 years old and at least one in every four persons 21-29 years old. One in every nine persons 15-29 years old depends on Medicaid or other publicly sponsored insurance for health care access. In addition, Hispanic and African Americans are most likely to lack insurance coverage.
Poverty and other socioeconomic factors also contribute to STD risk in other ways. Even if a person in poverty perceives himself or herself to be at risk for an STD, he or she may not practice preventive behaviors if there are other risks that appear more imminent or more threatening or both (Mays and Cochran, 1988; Ramos et al., 1995). Mays and Cochran (1988:951) point out that poor women of certain ethnic groups face continual danger and have few resources to deal with them: "Competition for these women's attention includes more immediate survival needs, such as obtaining shelter for the night, securing personal safety or safety of their children, or interfacing with the governmental system in order to obtain financial resources." Traditional cultural values associated with passivity and subordination also diminish the ability of many women to adequately protect themselves (Amaro, 1988; Stuntzner-Gibson, 1991).
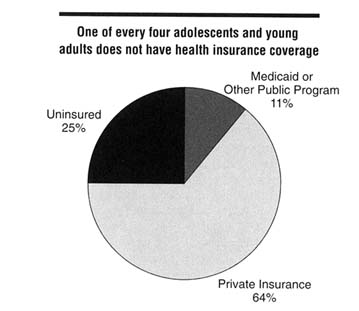
Figure 3-1
Distribution of 15-29-year-old persons in the United States by health insurance coverage, 1993. SOURCE: UCLA Center for Health Policy Research, unpublished data, 1996.
Substance Use
Substance use, especially drugs and alcohol, is associated with STDs at both population and individual levels.1 At the population level, rates of STDs are high in geographic areas where rates of substance use are also high, and rates of substance use and STDs have also been shown to co-vary temporally (Greenberg et al., 1991). At the individual level, persons who use substances are more likely to acquire STDs (Marx et al., 1991; Anderson and Dahlberg, 1992; Shafer et al., 1993). There are several possible reasons for this association. One is that underlying social and individual factors lead both to higher rates of STDs and to greater use of substances. Social factors such as poverty, lack of economic and educational opportunities, and weak community infrastructure may contribute to both outcomes. Individual factors, such as risk-taking and low self-efficacy, could similarly contribute to both outcomes.
Use of substances may also directly contribute to risk of STD infection by undermining an individual's cognitive and social skills, thus making it more difficult to take actions needed to protect themselves against STDs. For example, at low doses cocaine can decrease inhibitions and heighten sexuality, leading to increased numbers of sexual encounters and partners and to increased high-risk sexual behaviors (Marx et al., 1991). In addition, drug users may be at greater risk for STDs as a result of the practice of trading sex for drugs; in these situations, drug users have a large number of high-risk partners (Marx et al., 1991). Those who are involved in frequent and sustained use of substances are most likely to be at risk for STDs.
Data from the National Household Survey on Drug Abuse indicate that, in 1994, approximately 54 percent of the U.S. population age 12 and over and 63 percent of those age 18-25 used alcohol in the prior month (SAMHSA, 1995). In addition, approximately 6 percent of the U.S. population used an illicit drug in the prior month, and there were approximately 500,000 crack cocaine users during the year.
To illustrate the broad impact of substance use on STD transmission, the committee focused on the association of STDs with use of two substances: crack cocaine, often used by disenfranchised groups, and alcohol, which is commonly used by most Americans, especially adolescents. In the following sections, the committee describes the evidence for the association between substance use/abuse and STDs.
Impact of Crack Cocaine on STD Transmission
Numerous studies show that drug use is associated with increased risk of STDs, including HIV infection. Marx and colleagues (1991) reviewed 16 epidemiologic studies that examined drug use, sexual behavior, and STDs. Crack use paralleled the trends for syphilis, gonorrhea, chancroid, and HIV infection, both temporally and among the groups most affected. For example, a study at an STD clinic in 1990 in Trenton, New Jersey, evaluated the relationship between syphilis and behavior related to sexual activity and drug use (Finelli et al., 1993). The study showed that in addition to crack use and lack of condom use within the past three months, a high number of sex partners, drug-using partners, and partners exchanging sex for drugs increased the risk for syphilis, especially for women.
The association of syphilis and crack cocaine may lead to concentrations of the disease in specific social networks and in crack houses. For example, in 1991 and 1992, a series of syphilis outbreaks in four rural towns in Texas were linked to crack users exchanging sex for drugs (Schulte et al., 1994). Three outbreaks were concentrated in neighborhoods where crack cocaine dealers worked and where exchange of sex for drugs or money was common. All 26 cases in one outbreak were linked to a single sex worker. In a second outbreak, all 34 cases were among people frequenting a crack house, 3 of whom were sex workers. In
the third and fourth outbreaks, 12 percent and 50 percent of infected persons, respectively, reported exchanging sex for drugs or money.
Crack cocaine use is associated with high-risk sexual behaviors such as multiple partners and unprotected sex. McCoy and Inciardi (1993) found that in a sample of women who did not inject drugs, crack was found to be the strongest predictor of high-risk sexual behavior. Edlin and others (1994) reported in a multisite study that crack smokers were at greater risk for HIV infection compared to persons who did not smoke crack. In addition, male crack users are more likely than those who do not use crack to choose high-risk partners (Seidman et al., 1994). Compared with heroin users, men who used crack also are more likely to have a greater number of sex partners and to receive money or drugs for sex (Hudgins et al., 1995).
How Drug Use Increases STD Transmission
How does substance use increase STD transmission on a population level? Examining the population-wide impact of crack cocaine may provide answers. Crack cocaine appears to play a central role in the transmission of STDs within various social networks. The transmission and persistence of STDs in a population or social network are dependent on the rate of partner change, the probability of transmission of infection from an infected individual to a susceptible individual, and the duration of infectiousness (May and Anderson, 1987). The rate of partner change can be considered to be a function of a complex set of interactions involving social and sexual networks, sex partner mixing patterns, and other parameters. The rate of partner change is influenced by the exchange of sex for drugs that results from crack cocaine use (Marx et al., 1991; Edlin et al., 1994). The probability of infection per sexual encounter is influenced both by the type of sexual contact and by specific sexual practices and is strongly affected by the use of condoms. The urgency to use crack may overwhelm any consideration of condom use. Because crack use in persons with STDs discourages health-care-seeking behavior (Webber et al., 1993) and modifies social norms with respect to behavior such as engaging in unprotected sex (Finelli et al., 1993) or having multiple sex partners (Greenberg et al., 1992), the duration of infectiousness in these persons may be lengthened. In addition, explosive bursts of new partner acquisition, particularly in crack houses or other settings where addicted persons trade sex for drugs, represent a potentially powerful mechanism for amplifying and maintaining chains of transmission of genital ulcer diseases among crack users. Crack also appears to influence health-care-seeking behavior among pregnant women infected with STDs, resulting in late or absent prenatal care (Warner et al., 1995); frequent changes in prenatal care providers may complicate appropriate follow-up for positive serologic tests.
Association Between Alcohol Use and STDs
Although some studies have failed to find a correlation between alcohol use and unprotected heterosexual intercourse (Leigh and Stall, 1993; Leigh et al., 1994), most studies show that both average and extreme alcohol use are associated with greater risk of STDs. From 1988 to 1990, 2,896 adults completed the General Social Survey, a nationally representative household survey of U.S. adults (Anderson and Dahlberg, 1992). Respondents who reported that they sometimes drink ''more than they should" were more likely to have had the following three outcome variables compared to those who did not: sexual intercourse with two or more partners, intercourse with five or more partners, and intercourse with a stranger in the past year. A household survey in the San Francisco Bay area showed that having ever had an STD was associated with nonmonogamous behavior; with having more than five sex partners in the last five years; and, at a minimum with, three kinds of drinking behavior: going to a bar at least monthly, getting drunk at least annually, and having five or more drinks at one sitting in the last year (Ericksen and Trocki, 1992). In addition, a large nationwide survey in 1991 and 1992 showed that persons who occasionally drank five or more drinks at one sitting were significantly more likely to have multiple partners, be nonmonogamous, and participate in other high-risk sexual activities (Caetano and Hines, 1995).
A number of studies have reported that for men who have sex with men, drug and alcohol use are risk factors for relapse into unsafe sexual behaviors (Stall et al., 1986; Siegel et al., 1989). Alcohol use among adolescents has also been found to be associated with high-risk sexual behaviors (Hingson et al., 1990; Shafer et al., 1993; Lowry et al., 1994). In addition, alcohol use has been found to be a risk factor for HIV-related sexual behaviors among runaway youth (Koopman et al., 1994), the mentally ill (Kalichman et al., 1994), and seronegative female partners of HIV-seropositive men (Kennedy et al., 1993). In a survey of attendees at an STD clinic, drug and alcohol use was found to correlate with unprotected sex during their most recent sexual intercourse (CDC, 1990). In a multiple logistic regression analysis controlling for age, race, income, number of sex partners, and other variables, failure to use condoms was significantly associated with drug and alcohol use at the last sexual encounter for heterosexual men.
Sexual Abuse and Violence
Sexual violence against women and sexual abuse of children are societal problems of enormous consequences. Approximately 500,000 women were raped annually in 1992 and 1993 in the United States (U.S. Department of Justice, 1994), and studies suggest that approximately one in three young girls and one in six young boys may experience at least one sexually abusive episode by the time they reach adulthood (Guidry, 1995). Women who have been sexually abused
during childhood are twice as likely to have gynecological problems, including STDs, compared to women who do not have such a history (Plichta and Abraham, 1996). In addition, women with a history of involuntary sexual intercourse are more likely to have voluntary intercourse at an earlier age (a risk factor for STDs) and to have subsequent psychological problems (Miller et al., 1995).
Transmission of STDs as the result of sexual abuse is particularly salient among prepubescent children and very young adolescents. STDs among children presenting for care after the neonatal period almost always indicate sexual abuse (AAP, Committee on Child Abuse and Neglect, 1991; Gutman et al., 1991; CDC, 1993). Sexually abused children may have severe and long-lasting psychological consequences, may become sexual abusers themselves, and may abuse children (Guidry, 1995). In addition, they may engage in a pattern of high-risk behavior that often puts them at risk for further abuse and subsequent STDs. Guidelines for the clinical management of children with STDs as a result of suspected abuse have been published (CDC, 1993; AAP, Committee on Child Abuse and Neglect, 1991).
Many women who are subjected to sexual violence may not be able to implement practices to protect against STDs or pregnancy (O'Leary and Jemmott, 1995; Plichta and Abraham, 1996). A phenomenon that also may impede protective behaviors among women is the pairing of older men with young women. The age discrepancy between older men and younger, sometimes adolescent, females may predispose to power imbalances in the relationship, thus increasing the potential for involuntary intercourse, lack of protective behavior, and exposure to STDs (Finkelhor and Associates, 1986). In addition, early initiation of sexual intercourse among adolescent males with an older female partner has been shown to increase the number of sex partners later in life (Weber et al., 1992).
STDs Among Disenfranchised Populations
STDs, like most communicable diseases in the United States, disproportionately affect disenfranchised groups and persons who are in social networks where high-risk health behaviors are common. These groups are often of low priority to policymakers since they possess little political power or influence and, without publicly sponsored health services, would not have access to STD-related services. In addition, these groups are difficult to reach, difficult to teach, and difficult to treat (Donovan, 1996). However, they are important from an STD prevention perspective because they represent "core" transmitters of STDs in the population (Thomas and Tucker, 1996). In this section, the committee describes several examples of populations at high risk for STDs that require special attention.
Sex Workers
Sex workers and their clients represent traditional "core" transmitters of STDs (Plummer and Ngugi, 1990). Extremely high rates of STDs, including HIV infection, have been reported among sex workers in the United States (Darrow, 1992). For example, in a national study of more than 1,300 female sex workers, 56 percent had serological evidence of past or current hepatitis B virus infection (Rosenblum et al., 1992). Studies in the late 1970s and early 1980s found that up to 22 percent of sex workers screened in some U.S. cities were infected with gonorrhea (Plummer and Ngugi, 1990). As mentioned previously, exchanging sex for drugs is a major factor in the recent upsurge in syphilis infections in several large cities. In addition to unprotected sex with multiple partners, female sex workers also are likely to have other factors that increase their risk for STDs, such as intravenous drug use, a history of being victims of sexual abuse and violence, and inadequate access to health care (Rosenblum et al., 1992).
Policies related to sex workers have ranged from punitive interventions such as criminalizing prostitution, as in the United States, to legalizing and controlling it, as is the case in many European countries. In those European countries, sex workers must submit to periodic health examinations and testing for STDs (Plummer and Ngugi, 1990). Studies indicate that screening and treatment programs to reduce the prevalence of STDs among sex workers, while ignoring the legal and moral debates regarding prostitution, may be effective in controlling outbreaks of treatable STDs, such as syphilis and chancroid, but less effective for untreatable STDs or STDs that are more widespread in the general population (Plummer and Ngugi, 1990). More recent approaches combine peer health educators, promotion of barrier methods, screening and treatment, and counseling (CDC, 1996a).
Homeless Persons
Estimates of the number of runaway and homeless adolescents in the United States vary from hundreds of thousands to millions (AMA, Council on Scientific Affairs, 1989). Adolescents living on the streets are at risk for many health problems, including STDs (Sherman, 1992). One study showed that approximately one-third of runaways in Los Angeles detention facilities had an STD at the time of detention (Manov and Lowther, 1983). Runaways and homeless adolescents are at increased risk for STDs because they tend to be more sexually active than other adolescents (Hein et al., 1978); have multiple high-risk sexual behaviors that include trading sex for drugs or money (AMA, Council on Scientific Affairs, 1989; Sugerman et al., 1991; Sherman, 1992; Forst, 1994); have high levels of substance use (Manov and Lowther, 1983; Sugerman et al., 1991; Sherman, 1992); and are frequently sexually and physically abused by others (AMA, Council on Scientific Affairs, 1989). A survey of states regarding pregnancy
prevention and family planning policy found that only eight states had a written policy on sexuality education for youths in out-of-home care (i.e., family foster care, group homes, and residential care) (Mayden, 1996).
STDs are also a major problem among homeless adults. For example, a study of homeless women in Chicago seeking gynecological care revealed that 26 percent had trichomoniasis, 6 percent had gonorrhea, and 5 percent had pelvic inflammatory disease (Johnstone et al., 1993). Another study of homeless persons in Baltimore found that 8 percent of men and 11 percent of women had positive gonorrhea or syphilis tests and nearly one-third reported a prior STD (Breakey et al., 1989).
Adolescents in Detention
Adolescents in detention facilities have higher rates of risky sexual and substance use behaviors than do other adolescents (Shafer et al., 1993; Shafer, 1994). Adolescents in detention facilities may represent "core" transmitters of STDs since they have problems, such as high rates of drug and alcohol use and poor access to health care, that place them at continuing risk for STDs (Shafer, 1994). Compared to other adolescents, those in detention facilities tend to have engaged in sexual intercourse earlier and more frequently; have engaged in unsafe sexual practices more often; and have higher rates of STDs (Bell et al., 1985; DiClemente et al., 1991; Weber et al., 1992; Oh et al., 1994). Of 966 sexually experienced male adolescents examined in an Alabama detention center, 48 percent became sexually active before age 13; age at first intercourse ranged from 5 to 17 years (Oh et al., 1994). In a study of 1,580 male adolescents in juvenile detention in rural Florida, 27 percent were sexually active by age 11 (Weber et al., 1992). Multivariate models show that inconsistent condom use, multiple partners, and frequent alcohol use appear to increase the risk of STDs (Shafer et al., 1993). These same factors are likely to play a role in the larger population as well. Although condom use is low among adolescents in detention, those who communicate with their partners regarding their sexual history and who know someone with AIDS are more likely to use condoms (Rickman et al., 1994).
Both male and female adolescents in detention facilities have high rates of STDs. A 1994 national survey of state and local juvenile detention facilities found that the rate of gonorrhea was, respectively, 152 and 42 times greater among confined male and females adolescents than among their counterparts in the general population (CDC, 1996b). In a study of 414 sexually active male adolescents in a San Francisco detention center, 15 percent were diagnosed with at least one STD and 34 percent reported a history or had current evidence of an STD at the time of entry into the facility (Shafer et al., 1993). Twelve percent of male adolescents tested in an Alabama detention center for gonorrhea, chlamydial infection, and syphilis were positive for at least one of the three STDs (Oh et al., 1994). In addition, almost a third of the female adolescents in a King County,
Washington, detention facility, many of whom were sex workers, tested positive for chlamydial, gonorrhea, or both (Bell et al., 1985).
In detention facilities, if STD education is provided, it is usually incorporated into HIV education programs. In 1994, approximately 57 percent of state juvenile detention facilities provided instructor-led HIV education and 7 percent provided peer-led education programs (CDC, 1996b). Only one county correctional system reported making condoms available in its juvenile detention facilities (i.e., Alameda County, California) (Widom and Hammett, 1996).
Adults in Detention
The number of prisoners in the United States is at record levels. A total of 1,104,074 persons were in state or federal prisons in June 1995 (U.S. Department of Justice, 1995). From 1990 through 1995, the number of prisoners grew at an annual rate of 7.9 percent. Inmates in correctional facilities have high levels of communicable diseases, including tuberculosis, hepatitis B virus infection, and HIV infection and other STDs (Glaser and Greifinger, 1993). A study of 6,309 men at the main jail facility for men in Los Angeles County used a rapid test for syphilis to show that the rate of infectious syphilis was 507 cases per 100,000 persons. This was more than 11 times higher than the rate in the general county population (Cohen et al., 1992). Results of routine testing for STDs between 1993 and 1994 show that up to 17 percent of inmates were infected with syphilis, up to 32.5 percent were positive for gonorrhea, and up to 4.4 percent were positive for chlamydial (Hammett et al., 1995). Female detainees are at high risk of STDs because many are involved with drugs and exchange sex for drugs or money. For example, among women prisoners at Rikers Island in New York, 57 percent were jailed because of drug-related offenses and 80 percent had cocaine in their urine at the time of their arrest (Holmes et al., 1993). In 1988, 35 percent of a sample of female inmates at Rikers Island were positive for human papillomavirus (9 percent had abnormal Pap smears) (Bickell et al., 1991); 27 percent had positive cultures for chlamydial; 16 percent were serologically positive for syphilis; and 8 percent had positive cultures for gonorrhea (Holmes et al., 1993).
The prevalence of HIV infection among incarcerated persons in the United States, like other STDs, is many times higher than in the general population (Hammett et al., 1995; CDC, 1996b). Comparing the HIV seroprevalence among entrants into 10 federal and state prisons to the seroprevalence among first-time blood donors, the prevalence among male and female detainees is more than 50 and 130 times, respectively, the rate among blood donors (CDC, 1992b). Anonymous serosurveys of inmates throughout the United States indicate that anywhere from less than 1 percent to as high as 25.6 percent of inmates are HIV-positive and that female inmates often have higher infection rates compared to men (Hammett et al., 1995).
The prevalence of STDs among incarcerated persons reflects both the high
prevalence of STDs in the social networks from which they come and the transmission of STDs among prisoners (Moran and Peterman, 1989). Within prisons, unprotected sex, intravenous drug use, and tattooing are potential modes of transmission of STDs, including HIV infection (Doll, 1988; Dolan et al., 1995; Hammett et al., 1995). A wide range of unprotected consensual and nonconsensual sexual activity occurs among prisoners and between prisoners and staff (Mahon, 1996). Although transmission of STDs has been documented among prisoners (Moran and Peterman, 1989; Mutter et al., 1994), it is unclear if prisoners in correctional facilities are more likely to acquire STDs, including HIV infection, during incarceration or outside in the community (Dolan et al., 1995). While it is possible that the frequency of unprotected sexual intercourse or injecting drug use among prisoners is typically higher while they are not in confinement (Decker et al., 1984; Horsburg et al., 1990), some prisoners have high rates of risky behaviors while incarcerated. For example, one study of male Tennessee prisoners showed that 37 percent of prisoners reported using intravenous drugs while not incarcerated compared to 28 percent who reported such use while in prison, and 7 percent reported engaging in same-sex intercourse while not incarcerated compared to 18 percent who reported such intercourse in prison (Decker et al., 1984).
Correctional systems are more focused on HIV education than for other STD educational programs. A 1994 survey revealed that 75 percent of state and federal correctional systems and 62 percent of city and county systems reported providing instructor-led HIV education (Hammett et al., 1995; CDC, 1996b). In addition, 35 percent of state and federal correctional systems and 7 percent of city and county systems reported peer-led educational programs in at least one facility. In contrast, 49 percent of state and federal systems and 48 percent of city and county systems reported instructor-led STD education.
The National Commission on Correctional Health Care recommends that all inmates be screened for STDs and that a comprehensive education program and "appropriate protective devices" to reduce the risk of HIV/STDs be provided (NCCHC, 1992, 1994). In 1994, 82 percent of state and federal systems and 34 percent of city and county systems reported policies for screening all incoming inmates for syphilis, gonorrhea, and/or chlamydial infection (Hammett et al., 1995). Screening and follow-up treatment of prisoners for STDs are difficult because of the rapid turnover of inmates, and innovative screening programs are needed. An example of such a program for rapid screening and treatment for syphilis is presented in Box 3-1.
Very few correctional facilities provide access to condoms. Facility administrators commonly cite the potential use of condoms as weapons or to conceal drugs or contraband as a reason for denying access (Hammett et al., 1995). In addition, some prison administrators are concerned that providing condoms contradicts official policies that prohibit sexual activity among prisoners. Two state correctional systems (Mississippi and Vermont) and four local jail systems (New
|
BOX 3-1 An Effective Screening and Treatment Protocol for Syphilis in a Correctional Facility A rapid screening and treatment protocol for syphilis was recently evaluated in New York City's major facility for medical screening of female inmates at time of admission. The protocol's strength lies in its ability to accurately identify inmates needing syphilis treatment and to provide that treatment at the time of the obligatory medical evaluation. This service, piloted by the New York City Department of Health, introduced the use of a quick screening test for syphilis (STAT RPR) and the New York City Syphilis and Reactor Registry (which includes syphilis serologic results and treatment history of New York City residents), in addition to the routine medical evaluation data (which includes pregnancy testing), to make on-site treatment decisions. Information from the STAT RPR test and from the Syphilis Registry are available to clinicians at the time of the medical evaluation. Under the protocol, treatment is recommended for women with reactive STAT RPRs (unless this individual completed treatment within the last three weeks); with evidence in the registry of previously untreated syphilis, regardless of current STAT RPR status; and, in cases of pregnancy, with registry documentation of syphilis (unless treatment was completed within the last week). This protocol resulted in an improvement of syphilis treatment rates from 7 percent of seropositive women prior to implementing the protocol to 87 percent of seropositive women and 94 percent of pregnant seropositive women after implementing the protocol (Blank et al., 1994). The protocol also resulted in treatment for women whom the New York City Department of Health had been unable to locate for treatment in the past. SOURCE: Margaret Hamburg, M.D., New York City Department of Health, unpublished data, 1996. |
York City, Philadelphia, San Francisco, and Washington, D.C.) make condoms available to inmates (CDC, 1996b). Among correctional systems with condom availability programs, there have been few or no problems with the use of condoms as weapons or to smuggle contraband (Hammett et al., 1995). Most correctional systems have a policy for notifying partners of inmates who test positive for a treatable STD if the partner is a fellow inmate. The high annual rate of turnover among prisoners, 800 and 50 percent in jails and prisons, respectively, is a major barrier to screening and follow-up treatment for STDs (Glaser and Greifinger, 1993). Follow-up of released detainees who test positive for STDs and notification of partners who are not inmates are considered to be rare.
Migrant Workers
STDs, including HIV infection, are major health problems among migrant workers (Jones et al., 1991; CDC, 1992a). In addition, lack of condom use and other high-risk sexual behaviors are common among these workers (Jones et al.,
1991). Migrant workers tend to be young, uneducated, and from developing countries. They and their families have limited access to health care because of their frequent relocation, language and cultural barriers, and limited economic resources (Bechtel et al., 1995). Traditionally, there have been distinct patterns of movement for migrant workers: north and south along the East and West Coasts and from Texas up through the Midwest. Currently, however, many migrant workers do not follow these patterns but criss-cross the country seeking work (Dougherty, 1996). Among migrant workers, men who are single or not accompanied by their families are at greatest risk for STDs. In some areas, it is common practice for sex workers to visit migrant camps for men and have sex with many men (Oscar Gomez, East Coast Migrant Health Project, personal communication, March 1996). STDs persist in migrant populations because of cultural influences against open discussion of sex and STDs, language barriers, lack of access to health care, and general lack of understanding of disease transmission (Smith, 1988; Bechtel et al., 1995). Social and cultural taboos make discussion of STDs uncomfortable for many migrant workers. For example, there is a reluctance to use condoms or request the use of a condom among migrant workers because there is an implied aspersion that the partner is not trustworthy (Bobbi Ryder, National Center for Farm Worker Health, personal communication, March 1996).
Secrecy as a Contributing Factor
Many of the obstacles to prevention of STDs at both individual and population levels are directly or indirectly attributable to the social stigma associated with STDs. It is notable that although there are consumer-based political lobbies and support groups for almost every disease and health problem, there are few individuals who are willing to admit publicly to having an STD. STDs are stigmatized because they are transmitted through sexual behaviors. Although sex and sexuality pervade many aspects of our culture, and sexuality is a normal aspect of human functioning, sexual behavior is a private—and secret—matter in the United States.
The committee uses the word "secrecy" in this report to describe certain aspects of sexuality in the United States. By the word "secrecy," the committee includes both the passive by-product of the inherent difficulties of discussing intimate aspects of life and the ongoing efforts by some groups to prevent open dissemination of information regarding sexuality and its health consequences. In this section, the committee summarizes the basis for the stigma surrounding STDs, the reticence to deal openly with sexual behaviors, and the impact of these two factors on preventing STDs.
Sexuality and Secrecy in the United States
Perhaps more than any other aspect of life, sexuality reflects and integrates
biological, psychological, and cultural factors that must be considered when delivering effective health services and information to individuals. Sexuality is an integral part of how people define themselves. It influences how, with whom, and with what level of safety people engage in sexual behaviors. However, sexuality is a value-laden subject that makes people—including health care professionals, researchers, educators, and the public—feel anxious and uncomfortable talking about it. The resulting inability to address issues of sexuality places individuals at risk of STDs. The discomfort that many Americans feel discussing sexual behavior is reflected in a recent nationwide survey that showed that, including married couples, approximately one of four women and one of five men surveyed had no knowledge of their partner's sexual history (EDK Associates, 1995).
Sexuality has been described in many ways. The common denominator in all definitions is the recognition that sexuality is an intrinsic part of one's being. It is much more than the sexual act and encompasses more than the anatomy, physiology, and biochemistry of the sexual response system. It is the quality of being human—all that we are as men and women (Hogan, 1980). Sexuality is also an energy, a life force, that is an important aspect of individual behavior and includes personal roles, identity, thoughts, feelings and emotions, and relationships. In addition, sex is entwined with ethical, spiritual, and moral issues and is influenced by sociocultural values and norms, religion, family, and economic status (Chilman, 1978).
It is helpful to examine the origins of secrecy regarding sexuality to understand why it has had such a significant impact on STDs in the United States. STDs were considered to be a threat to the late Victorian social system, which valued discipline, restraint, and homogeneity (Brandt, 1988). Advocates of repressive sexuality perceived that social structure and traditional morality were in danger and wanted to restore order and morality to American society (Sokolow, 1983). During this time, societal sexual mores dictated that sexual intercourse was only acceptable within the context of marriage. The Victorian code of ethics considered all discussion of sexuality and STDs to be inappropriate. According to these ethics, sexuality should be disciplined, not only by law but also by shame, and then concealed by silence (Kosovich, 1978). This code was upheld by key groups and opinion leaders in the community. For example, some physicians hid diagnoses of STDs from their patients and families and did not talk about the "medical secret" (Brandt, 1988). The press also contributed to this code of secrecy by refusing to print any explicit articles regarding STDs. When public health officials were finally able to conduct educational campaigns regarding STDs during the first few decades of the twentieth century, these campaigns emphasized the dangers of sexual activity rather than disease prevention. By focusing on the "loathsome" and disfiguring aspects of STDs, these early campaigns may have contributed to the stigma associated with STDs and encouraged discrimination against persons with STDs (Brandt, 1988). The historical phenomenon of secrecy surrounding sexuality and STDs in the United States offers
some insight into why Americans are reluctant to openly discuss STDs, but some other industrialized societies (e.g., Scandinavia) are not.
The depiction of sexuality has been paradoxical within modern American culture. On the one hand, there is the saturation and sensationalism of sexual images and messages in the mass media, and the public is fascinated with sexual subjects. On the other hand, sexuality remains an extremely private and uniquely complex sphere of human behavior with sociocultural taboos and rules of behavior that make talking openly and comfortably about sexuality difficult. For some individuals, opposition to research in sexual behavior can represent very deep-seated fears and doubts about the role and significance of sexuality in personal life and the appropriateness of addressing this issue in public (di Mauro, 1995). The paradoxical nature of sexuality in the United States is further illustrated by a mass media culture that portrays casual sexual activity as the norm, while data show that most Americans disapprove of adult women having premarital sexual intercourse (Klassen et al., 1989). It is interesting to note that American society has had difficulty in openly discussing many health issues other than sexuality and STDs. For example, public discussion of health problems such as cancer, alcoholism, and mental illness are relatively recent phenomena. This observation provides optimism that sexuality and STDs will eventually be part of public discourse.
Secrecy surrounding sexuality is reflected in individual values, attitudes, and beliefs regarding sexuality that impede a person's ability or willingness to communicate regarding sex (Hyde, 1994). Additionally, this secrecy has a negative impact upon both sexual behavior and the ability to take protective action against STDs. The United States has a diverse population, and people develop their sexual value system based on their culture, religion, family, social status, and community (Woods, 1979). The secrecy regarding sexuality is perpetuated and supported by influences that include the family, partners, peers, and religion (Jemmott and Jemmott, 1992a). If social norms do not support open discussion of sex and sexuality, then the individual is unlikely to do otherwise.
Impact of Secrecy on STD Prevention
An examination of the social history of STDs in the United States is informative. Historically, a moralistic approach to STDs has directly hindered the ability of public health officials and programs to successfully control the epidemic (Brandt, 1985; Cutler and Arnold, 1988). For example, in the 1930s, many hospitals refused admission of patients with STDs and private physicians were reluctant to treat them because persons with STDs were viewed as immoral or not deserving of care (Brandt, 1985). Coupled with the high costs of syphilis treatment, this led many infected persons to turn to quacks and over-the-counter "cures." This practice quickly led to a growing number of untreated individuals and an escalating epidemic. Unwillingness to confront issues regarding sexuality,
and the judgmentalism that often accompanies it, had a detrimental effect on efforts to prevent STDs as early as the nineteenth century. Reflecting on America's efforts around syphilis during the last century, Martensen (1994:269) wrote:
For the predominant voices in the late 19th-century US medicine and society, humans were divided into good (celibate and on the way to being married and monogamous) or not good (the intentionally single and/or unmarried but sexually active). ... Such cultural bifurcations of innocence and evil presented few barriers to T pallidum [the cause of syphilis], and they made it difficult to develop consistent policies for the treatment and containment of venereal contagion.
The portrayal of STDs as symbols of immoral behavior continues today. This phenomenon was especially evident during the early stages of the AIDS epidemic when some in society considered this epidemic to be a symbol of deviant sexual behavior and lapse in societal moral values. In his book on the social history of STDs, Brandt (1985:186) writes:
Medical and social values continue to define venereal disease as a uniquely sinful disease, indeed, to transform the disease into an indication of moral decay. ... Behavior—bad behavior at that—is seen as the cause of venereal disease [STDs]. These assumptions may be powerful psychologically, and in some cases they may influence behavior, but so long as they are dominant—so long as disease is equated with sin—there can be no magic bullet.
Changing sexual behaviors that spread STDs is an important component of prevention. But in order to establish preferred behavior or to change risky behaviors, parents must feel comfortable talking to their children, individuals must be able to discuss sex with their sex partners, and educators and health professionals must be able to communicate with their students and patients. In this section, the committee describes how the constraints on acknowledgment and open discussion of sexuality adversely impact sexuality education programs for adolescents, open communication between parents and their children and between sex partners, balanced messages from the mass media, education and counseling activities of health care professionals, and community activism for STDs.
Impact on Sexuality Education for Adolescents
Traditionally, sexual behavior has been regarded as a personal issue and involvement by schools or health care professionals has been seen as intrusive. Debates regarding access of adolescents to sexuality education in public schools, family planning services, and abortion services have raised questions about who has jurisdiction in matters related to sexual behavior. Although there is widespread agreement that parents should be the major source of information and guidance for their children with regard to sexual behavior, communication does
not occur if parents are uncomfortable in discussing sexuality or lack the requisite knowledge or skills for such discussion. Parents may also deny the possibility that their child is or will be sexually active. Conversations regarding healthy sexual behaviors and STDs do not take place when parents deny that their children are sexually active or that adolescents have sexual drives. Children in these families are unable to seek information from their parents about such issues.
The denial or fear that their children are sexually active may lead some parents to oppose those, including the educational system, providing sexuality education to their children. Opponents of school-based sexuality education and condom availability programs argue that such programs lead to premarital sex and promiscuity. However, there is no scientific evidence that this occurs. Sexuality education appears to make students more tolerant of the attitudes and behavior of others, but it has not been found to increase premarital sex or promiscuity. Numerous evaluations of the ability of school-based education programs to reduce sexual risk behaviors have found no association between having had sexuality education and the probability of initiating sexual activity (Zelnik and Kim, 1982; Furstenberg et al., 1985; Kirby et al., 1994). In fact, there is evidence that responsible sexuality education may have a number of desirable effects in increasing AIDS-related knowledge and promoting positive changes in attitudes and risk-related behavior (Jemmott et al., 1992; Kirby et al., 1994). This issue is discussed further in Chapter 4.
Where do children get their information regarding sex? Relatively few children obtain essential information regarding STDs from their parents. A 1995 survey showed that only 11 percent of teenagers got most of their information regarding STDs from parents and other family members (Figure 3-2). Even parents who attempt to teach their children about sex may do so through general and diffused admonitions that do not recognize or end their child's interest in sex, but rather contribute to concealment and subsequent guilt. Because many parents do not talk to their children about sex, children are more likely to learn about sex through clandestine and secretive exchanges with peers that result in a massive amount of misinformation (Smith and Lanthrop, 1993). Guilty knowledge develops and children learn to keep sexuality a secret, especially from those they love (Hogan, 1980), thus perpetuating the cycle. Effective school-based programs and other means to educate children regarding sexuality might be less important if all parents discussed these issues with their children. Children who do not have open information exchange with their parents or others regarding sexuality may be less likely to communicate openly with their sex partners in the future, and thus be less likely to implement protective behaviors than others.
Impact on Communication Between Sex Partners
In addition to hindering communication between parents and their children, many societal barriers prevent sex partners from talking to each other about sex.
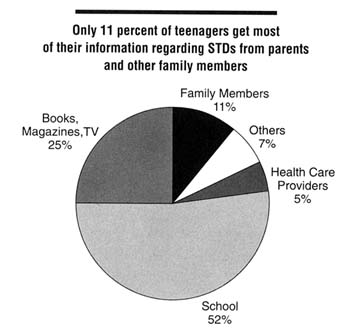
Figure 3-2
Distribution of U.S. teenagers by primary source of information regarding STDs, 1995. SOURCE: ASHA (American Social Health Association). Teenagers know more than adults about STDs, but knowledge among both groups is low. STD News. A quarterly newsletter of the American Social Health Association. Winter 1996;3:1,5.
Ironically, it may require greater intimacy to discuss sex than to engage in it. The kind of communication that is necessary to explore a partner's sexual history, establish STD risk status, and to plan for protection against STDs is made difficult by the taboos that surround sex and sexuality. As Lear (1995:1313) notes, individuals rarely engage in explicit discussions about sex: ''The existing discourse on sex is marked by a lack of vocabulary. ... Sexual encounters, at least early in a relationship, often involve very little spoken communication; communication is rather non-verbal and coded." Barriers to open discussion include gender roles, modesty, and cultural, family or religious beliefs. For instance, the "good woman" or the "modest woman" is not supposed to know about sex, so it is inappropriate for her to bring up subjects like HIV and condoms. Many studies have shown that both adolescents and adult women who are uncomfortable about their sexuality and who have high levels of guilt regarding sexual behavior are less effective in their use of contraceptives than others (Herold et al., 1979; Gerrard, 1982, 1987). Narrow attitudes towards sexuality and sex roles can make it difficult to initiate a conversation regarding sex and safer sex strategies with
one's partner. Two factors that influence women's abilities to communicate with current or new sex partners are their level of confidence in being able to initiate the conversation and perception of their partner's reaction to the conversation. The importance of perceived partner reaction may be related to the woman's level of dependence on her partner, including emotional and financial dependency.
The ability to communicate with sex partners is a critical element for protective behaviors such as condom use. Secrecy hinders an individual's ability to develop skills and ways to normalize condom use. One way to facilitate condom use is to eroticize their use and make them fun and pleasurable for partners (Jemmott and Jemmott, 1992b). To do so, however, requires feeling comfortable about sexuality and having open communication regarding sexual behaviors.
Impact on Mass Media Messages
Americans, especially adolescents, receive unbalanced mass media messages about sexuality, sexual behavior, and sexual responsibility. Premarital sex, cohabitation, and nonmarital relationships are depicted as the norm for adults (Lichter et al., 1994). However, the media provide little frank and informed advice about STDs, sexuality, contraception, or the harsh realities of early pregnancy and parenting. The portrayal of widespread casual sex is contrasted with messages that adolescents receive from other sources of information that premarital sex is not acceptable. American society is ambivalent about sex, and mixed messages from mass media contribute to the confusion and communication problems of many adolescents.
Television is currently the most significant mass media influence for adolescents (Strasburger, 1990). About one-third of an American's free time is spent watching television. That is more time than is spent on the next 10 most popular leisure activities combined (Gerbner, 1993). Children spend more time watching television than they do in school (Dietz and Strasburger, 1991). Television is an important source of information regarding sexual behavior (Strasburger, 1995): 37 percent and 41 percent of men and women surveyed, respectively, cite television talk shows as a primary source of information regarding STDs (STD Communications Roundtable, 1996).
A recent study found an average of 10 incidents of sexual behavior per hour on network television during prime time (Lowry and Schidler, 1993). When the content of promotions for upcoming shows is added, the number of such incidents increases. Analysis of multiple episodes of 11 top Nielsen-rated television talk shows found that topics related to sexual activity were discussed in 34 percent of episodes screened, sexual infidelity in 18 percent, and sexual orientation in 11 percent (Greenberg et al., 1995). Soap operas also have strong sexual content (Lowry and Towles, 1989); the most popular ones have more than six incidents of sexual behavior per hour and only six references to safer sex or
contraception in 50 episodes studied (Greenberg and Busselle, 1994). Most music videos and rock music lyrics, which frequently target adolescents, have strong sexual content (Sherman and Dominick, 1986; Strasburger, 1989). Other forms of media, including cable television, movies, and videotapes, also frequently portray sexual incidents (Brown and Steele, 1996).
Although sex is frequently portrayed on television, protective behavior is rarely shown and references to adverse consequences are rare; casual unprotected intercourse is presented as the norm. Lowry and Shidler (1993) found that there were approximately 25 instances of sexual behavior portrayed on prime-time television for every one instance of protective behavior shown or comment regarding STDs or unintended pregnancy. In addition, the references to protective behavior were portrayed in a nonserious manner. Another study estimated that the average teenager will be exposed to almost 14,000 television messages associated with sex annually, but less than 1 percent of these messages will deal with contraception, refraining from sex, or STDs (Harris and Associates, 1988). There is some evidence that producers may be starting to decrease the sexual content of some television shows (Lowry and Schidler, 1993; Olson, 1994).
In addition to serving as a source of information, mass media may influence social attitudes, and sometimes social behavior. For example, depictions of violence in the mass media have been shown to be a significant factor in real-life violence (Strasburger, 1995). The ability of sexual content in mass media to directly affect sexual behavior is unclear because appropriate longitudinal studies have not been conducted (Strasburger, 1995), but such content has been shown to influence adolescents' attitudes and beliefs regarding sex (Strasburger, 1992, 1995; Buerkel-Rothfuss and Strouse, 1993; Greenberg et al., 1993; Strouse and Buerkel-Rothfuss, 1993). One study found an association between frequent viewing of television programs with strong sexual content and early onset of sexual intercourse among adolescents, but it was not possible to distinguish which factor came first (Brown and Newcomer, 1991). Another recent study that examined the influence of mass media on eight potentially risky behaviors, including sexual intercourse, found that adolescents who had engaged in more risky behaviors listened to radio and watched music videos and movies on television more frequently than those who had engaged in fewer risky behaviors, independent of demographic factors (Klein et al., 1993).
The reluctance and past refusal of mass media to become involved in the dissemination of information regarding STDs and other sexual issues is not new. In his book on the social history of STDs, Brandt (1985) writes about an incident in November 1934. The Columbia Broadcast Company scheduled a live radio broadcast with Thomas Parran, Jr., then New York State Commissioner of Health, to talk about the major public health problems of the time. Just before airtime, Parran was told that he could not mention syphilis or gonorrhea by name. In response, Parran abruptly canceled his appearance and never delivered his talk. He went on to criticize the hypocritical standards in radio broadcasting that
prevented him from mentioning the names of STDs yet allowed "the veiled obscenity permitted by Columbia in the vaudeville acts of some of their commercial programs." More than 60 years later, this hypocrisy still exists among most major television broadcasters and other mass media. Promoting condom use or even mentioning the word "condom" on television is deemed inappropriate for young viewers, but it is accepted practice for young viewers to be exposed to shows and movies that portray persons practicing high-risk sexual behaviors. Similarly, while condom advertisements are not acceptable for prime-time television, it is common for advertisers to sell their products using sexually suggestive advertisements (Kilborne, 1993).
Advertisers and other sponsors have historically exerted considerable control over the content of television programming and magazines because the sponsors represent the major source of income for these media (Brown and Steele, 1995). Advertisers have implicitly supported sexual content in programming but have generally refused to support the incorporation of explicit information regarding protective behaviors for STDs for fear of offending viewers (Strasburger, 1989; Lebow, 1994; Brown and Steele, 1995). Opinion polls, however, show that most Americans support incorporating information regarding STDs and contraceptives in mass media (Harris and Associates, 1987; EDK Associates, 1994), including advertising of condoms on television (Buchta, 1989). Advertisers and sponsors commonly use sexual appeals to sell their products, but until recently the television networks had strictly forbidden advertisements for contraceptives (Lebow, 1994). Condom advertisements on television have been controversial ever since the first such advertisement in 1975 (Lebow, 1994). It was not until 1986 that the word "condom" was first used on prime-time television (Lichter et al., 1994). Recently, the Centers for Disease Control and Prevention (CDC) had to fight to use the word "condom" in its HIV prevention public service announcements (Hall, 1994). Despite agreeing to air the recent HIV prevention announcements promoting condoms, the networks have restricted showing the messages to non-prime-time hours (Hall, 1994). Primarily as a result of the HIV epidemic, in 1991 the Fox Broadcasting Company became the first national television network to run a condom commercial (Elliot, 1991), and some network-owned stations recently have begun to accept condom advertisements with certain restrictions and as long as they are in "good taste'' (Lebow, 1994). Some networks, such as Fox and MTV, are less restrictive in accepting condom advertisements.
Despite the current lack of involvement of mass media in promoting messages regarding healthy sexual behaviors, the mass media can be an extremely powerful ally in efforts to prevent STDs. HIV prevention messages delivered through mass media have been effective in increasing knowledge and changing behavior (Flora et al., 1995). This issue is discussed in further detail in Chapter 4. In addition, a nationwide survey of women found that 83 percent of women surveyed agreed that STDs would be more likely to be prevented if these diseases were more frequently discussed in public (i.e., on television, on the radio, and in
print media) (EDK Associates, 1994). In an effort to address the lack of accurate information regarding STDs in the mass media, the STD Communications Roundtable was formed in 1995. This ad hoc committee of public health experts, communications professionals, and mass media executives met to discuss ways of assisting the mass media in producing and incorporating messages supporting healthy sexual behavior. Building on these discussions, they recently produced a resource guide for media executives (STD Communications Roundtable, 1996). This roundtable, however, does not have plans to reconvene. In addition, the Media Project2 has been working with television producers and writers to improve the content of sexual messages in television shows and to increase the promotion of healthy sexual behaviors. A coalition of organizations with an interest in sexuality education, the National Coalition to Support Sexuality Education, recently issued a consensus statement and suggested guidelines for incorporating information regarding healthy sexual behavior and STDs into the mass media (Box 3-2).
Impact on Clinical Preventive Services
STD-related risk assessment and counseling are not routinely performed by most primary care clinicians. A 1994 nationwide survey of 450 physicians and 514 other primary care providers showed that 60 percent of physicians and 51 percent of other primary care providers do not routinely evaluate all or most new adult patients for STDs (ARHP and ANPRH, 1995). In addition, only 30 percent of physicians and 34 percent of other primary care providers reported collecting information regarding their patients' sexual activity.
Health care providers have two major hurdles to effective communication with their patients regarding sexuality issues. One is their own comfort level in talking about sex and sexual health issues, and the other is reserving time in their schedule to do it. The reluctance to discuss sexual health issues with patients can be partially attributed to the discomfort and embarrassment of some health care professionals in discussing these issues (Risen, 1995). A physician survey found that embarrassment was perceived to be a major reason physicians did not take sexual histories (Merrill et al., 1990). If clinicians are not comfortable talking to their patients about STDs, assessing their patients' risk behavior, and providing information on STD prevention, patients may detect this discomfort and decide not to raise questions or concerns regarding sex with their health care provider. The reluctance of clinicians to discuss sexual health issues may be especially problematic among older clinicians and gay patients (Matthews et al., 1986; Lewis and Freeman, 1987; Lewis and Montgomery, 1990). In order to address
|
BOX 3-2 Media Recommendations for More Realistic, Accurate Images Concerning Sexuality The National Coalition to Support Sexuality Education recommends that the media use their influence to convey more realistic, medically accurate, and health-promoting ideas and images concerning sexuality. It has long been recognized that the media help shape the attitude of the public—particularly young people—on a myriad of topics. The media play a major role in educating Americans about sexuality, gender roles, and sexual behaviors. Sexual images and references may be commonplace in the media, but sexuality is much broader than the media typically portray. Human sexuality encompasses the sexual knowledge, beliefs, attitudes, values, and behaviors of individuals. It deals with one's roles, identity, personality; with individual thoughts, feelings, behaviors, and relationships as well as one's body. Sexual health encompasses sexual development and reproductive health, as well as such characteristics as the ability to develop and maintain meaningful interpersonal relationships, to appreciate one's own body, to interact with both genders in respectful and appropriate ways, and to express affection, love, and intimacy in ways consistent with one's own values. Becoming a sexually healthy adult is a key developmental task of adolescence. The media can enhance adolescent sexual health by communicating accurate information and portraying realistic situations. The media provide opportunities for adolescents to gain clearer insights into their own sexuality and to make more responsible decisions about their behavior. We, the undersigned members of the National Coalition to Support Sexuality Education, strongly encourage writers, producers, film makers, programming executives, performers and program hosts, reporters, advertising professionals, Internet access providers, and others to incorporate the following into their work whenever possible: Sexually Healthy Behavior
|
Sensitivity to Diversity
Accurate Information
Signed April 1996 by: AIDS Action Council Advocates for Youth American Association of Sex Educators, Counselors, and Therapists American Counseling Association American Jewish Congress-Commission for Women's Equality American Medical Association-Department of Adolescent Health |
|
American Orthopsychiatric Association American Psychological Association American School Health Association American Social Health Association Association for the Advancement of Health Education Association for Sex Education and Training Association of Reproductive Health Professionals Association of State and Territorial Health Officials AVSC, International Catholics for a Free Choice Federation of Behavioral, Psychological, and Cognitive Sciences Gay and Lesbian Medical Association Girls, Incorporated Hetrick-Martin Institute Human Rights Campaign National Abortion Federation National Abortion and Reproductive Rights Action League National Asian Women's Health Organization National Association of School Psychologists National Council of the Churches of Christ National Education Association-Health Information Network National Lesbian and Gay Health Association National Minority AIDS Council National Native American AIDS Prevention Center National Resource Center for Youth Services National Women's Law Center Planned Parenthood Federation of America Parents, Family and Friends of Lesbians and Gays Presbyterians Affirming Reproductive Options Religious Coalition for Reproductive Choice Sexuality Information and Education Council of the United States Society for the Scientific Study of Sex The Alan Guttmacher Institute Unitarian Universalist Association University of Pennsylvania, Graduate School of Education Zero Population Growth, Incorporated REPRINTED FROM: SIECUS Report. Sexuality in the media: Part 1. New York: Sexuality Information and Education Council of the United States, 1996:24:22-23. |
this issue, the American Medical Association's Council on Scientific Affairs has recently released guidelines for providing STD-related care to gay and lesbian patients (AMA, Council on Scientific Affairs, 1996).
Limited time and resources also constrain clinicians from communicating with their patients regarding STDs and sexuality. If STDs are not seen as a high
priority, clinicians, who typically have limited time to evaluate patients, will be hesitant to commit the necessary time and resources to STD prevention. This may be reinforced by clinicians' discomfort in dealing with the issues related to their patients' sexuality. Clinicians may not feel that dealing with sexuality is their responsibility. For example, while some consider sexuality to be within the physicians' province, medical training continues to reflect the predominant opinion of society that sexual health issues are private issues; therefore, such training has ignored sexuality (Lief and Karlen, 1976). As further discussed in Chapter 5, medical students learn little beyond the anatomy and physiology of the sexual reproductive system; they are not trained to deal with patients' sexual problems, and many feel uncomfortable with their lack of preparation (Merrill et al., 1990). Moreover, every clinician has biases, beliefs, and preferences related to sexuality, based on his or her own experiences and judgment, that should be recognized.
Health care professionals may subconsciously rebuke those whose sexuality differs from their own and provide services in a superficial or judgmental manner. Clinicians need to develop an awareness of their values in order to avoid unwittingly imposing them on patients or letting their values affect clinical judgment and management (Lief and Karlen, 1976; AMA, Council on Scientific Affairs, 1996). The individual's comfort level with sexuality influences the interaction between the health care professional and patient, and between the health educator and student, in subtle ways that are not always readily perceivable (Woods, 1979). This points to the need for educational and training efforts that will facilitate open and clear discussions of sex and sexuality between health care professionals and their patients (Woods, 1979; Hogan, 1980; Lewis and Freeman, 1987; Poorman and Albrecht, 1987).
Impact on Community Activism
The stigma associated with STDs hinders public discourse and, as a result, community activism for STDs other than HIV infection. Because having an STD is still socially unacceptable, there are few if any patient-based constituent groups who advocate publicly or lobby for STD-related programs. In contrast, persons with cancer and other common diseases have successfully advocated for additional funding for their causes. There also has been good advocacy for HIV infection. In considering why there is a difference in how HIV infection and other STDs are publicly viewed, the committee speculates that the following factors may help explain the disparity: (a) the stakes are higher for HIV infection than other STDs since it is a fatal disease, (b) the HIV epidemic initially spread within an organized and largely educated community (gay men) with a substantial social support network and infrastructure, and (c) HIV infection occurred among and was publicly acknowledged by highly visible opinion leaders such as persons in the arts and entertainment industry.
Experiences of Other Countries
An examination of the social policies and experiences of other developed countries regarding sexuality underscores the adverse impact of the secrecy surrounding sexuality on STD prevention in the United States. For example, the Scandinavian countries have comparable levels of sexual activity, but their rates of many STDs and unintended pregnancy are much lower than in the United States (Piot and Islam, 1994; IOM, 1995). These differences may be largely a result of differences in how sexuality issues are dealt with in these countries. For example, lower rates of STDs and unintended pregnancies in northern and western European countries compared to the United States have been attributed to the pragmatic, rather than moralistic, approach to sexuality issues in these countries. In Denmark, for example, information regarding sexuality and STDs is provided freely in the media and sex education is mandated for all students beginning no later than third grade (age 9) (David et al., 1990). Because school-based sexual health education, mass media interventions, and public discussion regarding sexual health issues are much more common in many other developed countries, it follows that private communication regarding these issues—between parents and children, and between couples—is also more common in those societies than in the United States.
Another major factor that may explain the observed differences in STD rates is universal access to health services in other developed countries. As mentioned previously, a substantial proportion of young people at high risk for STDs in the United States do not have health insurance coverage. The positive impact of better access to clinical services for STDs on STD rates is supported by the observation that the differences in viral STD rates between the United States and other developed countries are much smaller than for curable STDs. In addition, the higher rates of drug use, such as crack cocaine use, in the U.S. population compared to some other developed countries contribute to the higher rates of STDs in the U.S. It is also possible that structural or policy differences play a role. For example, in some developed countries sex workers are licensed and screened and treated for STDs to prevent transmission to others. Another potential contributing factor is the higher level of "conforming" health behaviors (e.g., health-care-seeking behavior for STDs) in many other developed countries compared to the United States. While many factors may be responsible for the observed differences in rates of STDs between the United States and other developed countries, it seems that more appropriate social norms around discussion and education regarding sexual health issues and universal access to health care in other developed countries are major factors.
Research and Training Issues in Sexuality
For the past decade, behavioral research regarding sexuality has been driven
largely by public health efforts to decrease HIV transmission. In the absence of a comprehensive research agenda to study sexual behavior and norms, HIV-related research—as conducted in both the biomedical and social sciences—has produced a wealth of information about STD-related sexual behaviors, particularly regarding efficacy and determinants of condom use. The research spawned by the HIV epidemic has allowed sexual behaviors to be studied at a far greater magnitude than has been possible previously. The number of studies on sexual behavior and sexuality has increased substantially, with many providing important information about the range of sexual behaviors and patterns that exist within populations (Catania et al., 1992; Sonenstein et al., 1991; Leigh et al., 1993; Laumann, Gagnon, et al., 1994). Another significant development is that a new level of sexual discourse is developing, characterized by an increased willingness to talk publicly and explicitly about sexuality topics.
Despite the recent surge of research activity regarding sexual behaviors, the knowledge base is still limited, and many epidemiological studies of human sexuality are outdated (Laumann, Gagnon, et al., 1994). While some government funding has been provided, there has been little major or consistent support from either the government or the private sector for behavioral and social science research on human sexuality since the work of Kinsey and his colleagues (di Mauro, 1995). Comprehensive data on contemporary sexual behaviors, attitudes, and practices are limited, and it is not understood how these factors are shaped by different societal, cultural, and familial contexts (Laumann, Gagnon, et al., 1994; di Mauro, 1995).
Societal ambivalence regarding sexuality poses substantial obstacles to research regarding sexual behavior. For example, in 1991, there was unprecedented political interference with scientific research when federal administration officials, under pressure by congressional critics, blocked funding for studies of adolescent and adult sexual behavior after these studies had been approved for funding by a scientific peer-review process at the National Institutes of Health (Suplee, 1991; Laumann, Michael, et al., 1994). Congressional critics alleged that sexual behavior surveys were intended to solely "legitimize homosexual lifestyles" (Laumann, Michael, et al., 1994). The survey was eventually privately funded and became the National Health and Social Life Survey, which is the most comprehensive survey of sexual behavior in the United States in many years (Laumann, Gagnon, et al., 1994).
Researchers in human sexuality come from diverse disciplines such as anthropology, education, history, medicine, psychology, and sociology. Few researchers, however, have had specific training in designing, conducting, and evaluating research in sexuality (di Mauro, 1995). It has been generally, and incorrectly, assumed that conducting sexuality research requires no specific preparation or training other than the ability to integrate questions about sexual behavior into research design. While the inadequacy of sexuality training is well documented for health care professionals and educators (Lief and Karlen, 1976;
Nathan, 1986; Lewis and Freeman, 1987), there has been no review of the extent to which social scientists studying sexuality lack such preparation.
Trends in Sexual Activity
Although the discomfort and secrecy surrounding sexuality in America have limited scientific knowledge and prevented many parents and others from recognizing that adolescents as well as adults are sexually active, there are some scientific data regarding sexual activity. These data suggest that adolescents and young adults are not only sexually active but have very high rates of high-risk sexual behavior.
In the United States, nearly 70 percent of students in the twelfth grade have had sexual intercourse (Figure 3-3), and 27 percent of twelfth-grade students
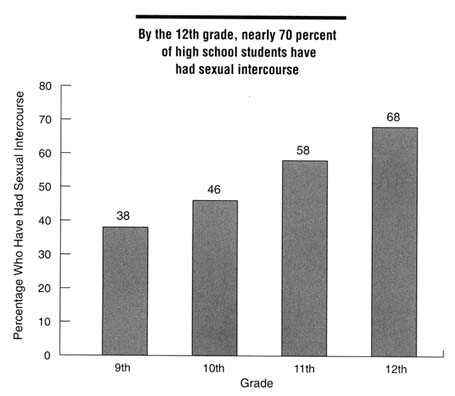
Figure 3-3
Percentage of U.S. high school students who reported ever having sexual intercourse, by grade level, 1993. SOURCE: CDC (Centers for Disease Control and Prevention). Youth risk behavior surveillance—United States, 1993. CDC Surveillance Summaries, MMWR 1995;44(No. SS-1).
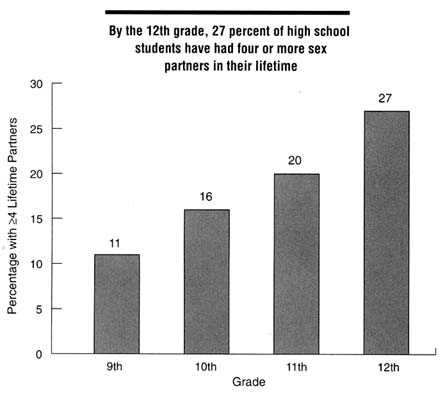
Figure 3-4
Percentage of U.S. high school students reporting four or more lifetime sex partners, by grade level, 1993. SOURCE: CDC (Centers for Disease Control and Prevention). Youth risk behavior surveillance—United States, 1993. CDC Surveillance Summaries, MMWR 1995;44(No. SS-1).
have had sex with four or more partners (Figure 3-4). Intercourse among American adolescents has increased dramatically in the last few decades (Hofferth et al., 1987; CDC, 1992c; Kost and Forrest, 1992). Data from the General Social Survey and the 1988 National Survey of Family Growth show that from 1971 to 1988, the proportion of sexually active adolescents and young women ages 15 to 19 years who have had more than one lifetime sex partner increased nearly 60 percent (Kost and Forrest, 1992). In 1971, approximately 39 percent of adolescents and women surveyed had had more than one partner, compared to 62 percent of those surveyed in 1988 (Figure 3-5). Changes in the past few years have not been as great. Data from CDC's Youth Risk Behavior Surveillance System shows that from 1990 through 1993, the proportion of high school students who reported being sexually experienced, ever having sexual intercourse
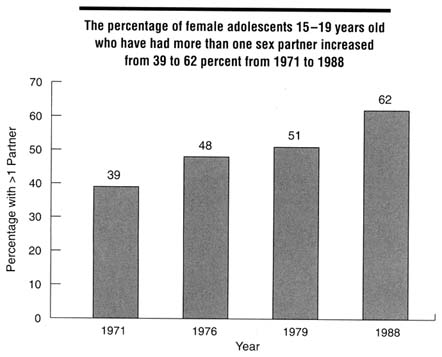
Figure 3-5
Prevalence of multiple sex partners among sexually active U.S. female adolescents, 15-19 years old, by year, 1971-1988. SOURCE: Kost K, Forrest JD. American women's sexual behavior and exposure to risk of sexually transmitted diseases. Fam Plann Perspect 1992;24:244-254.
with four or more partners, being sexually active (intercourse during the three months prior to the survey), or having used alcohol or drugs before last sexual intercourse remained constant (CDC, 1995). These data suggest that HIV and other STD prevention activities targeted towards adolescents beginning in the mid- to late 1980s in response to the HIV epidemic may have had a positive effect on some aspects of adolescent sexual activity.
Sexual activity among adolescents is sometimes initiated before the teenage years. A 1992 survey of 2,248 students in grades 6, 8, and 10 from an urban public school district found that 28 percent of sixth-graders and one-half of eighth-graders reported ever having had sexual intercourse (Barone et al., 1996). In an effort to examine the determinants of early onset of sexual intercourse among high-risk adolescents, Mott and colleagues (1996) analyzed a series of data collected through the National Longitudinal Survey of Youth from 1988 through 1992. They found that children were more likely to have early onset of intercourse if their mother had sex at an early age and if she worked extensively.
In addition, African American heritage and early alcohol use among boys and cigarette smoking among girls were associated with early onset of intercourse. Children who attended church and had friends who attended the same church were less likely to initiate sexual intercourse early.
Studies among college and university students give insight on the extent of sexual activity among young adults. A 1991 survey at in a large Midwestern university showed that 80 percent of male and 73 percent of female students had experienced sexual intercourse and that men reported an average of eight lifetime partners and women had an average of six lifetime partners (Reinisch et al., 1995). A survey of a Hawaiian university population found that a history of an STD was reported by 21 percent of women and 16 percent of men (Hale et al., 1993).
The prevalence of high-risk sexual practices among college students remains high. For example, a major study of female college students who sought gynecological care at a student health center during 1975, 1986, and 1989 examined trends in sexual behavior and practices during this time period (DeBuono et al., 1990). Among sexually active women, the percentage who reported that their partner ''always or almost always" used a condom increased significantly, from 12 percent in 1975, to 21 percent in 1986, to 41 percent in 1989. However, despite the recognition of HIV infection and other STDs during this period, with the exception of increased condom use, there were no significant changes in sexual practices such as number of partners and other high-risk sexual practices among the students surveyed from 1975 through 1989. A follow-up study, however, showed that almost three-quarters of college women reported "always or almost always" using condoms in 1995 (Peipert et al., 1996). Although condom use has increased substantially, absolute rates are still low in many groups.
During the past several decades, the age of entry into marriage has dramatically increased in the United States. For example, approximately 80 percent of men born during the interval 1933-1942 had married by age 27 compared to only 50 percent of men born during the interval 1953-1962 (Laumann, Gagnon et al., 1994). Coupled with the decreasing age at first intercourse during the last several decades, this means that the length of time between first intercourse and marriage has increased greatly. This phenomenon has increased the potential for spread of STDs because single persons tend to have more sex partners than married persons.
Knowledge and Awareness of STDs
Knowledge and awareness of STDs among Americans is poor. In a 1993 national survey of one thousand women from 18 through 60 years of age, almost two-thirds knew nothing or very little about STDs other than HIV/AIDS, and only 11 percent were aware that STDs can be more harmful to women than to men (EDK Associates, 1994). The lack of knowledge among women in high-risk
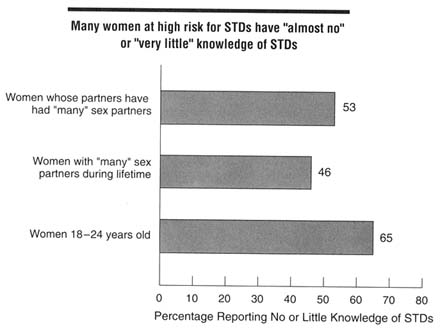
Figure 3-6
Self-reported knowledge of STDs among women by risk groups, 1993. Survey participants were asked to identify number of sex partners as "none," "one," "a few," or "many." SOURCE: EDK Associates, Inc. Women and sexually transmitted diseases: the dangers of denial. New York: American Medical Women's Association, 1994.
groups was dramatic: 65 percent of young women reported "almost none" or "very little" knowledge regarding STDs (Figure 3-6). Survey data suggested that women with greater knowledge and awareness of STDs are more likely to practice protective behaviors such as negotiating for condom use and seeking help from a health care professional.
A recent survey confirmed that many Americans lack sufficient knowledge of STDs (ASHA, 1995). Thirty-two percent of respondents could not name an STD other than HIV/AIDS. Of those who did identify another STD, 44 percent of respondents named syphilis; 37 percent named gonorrhea; few named any other STD. More than half of respondents believed that "all STDs except HIV/AIDS are curable," and they vastly underestimated the prevalence of STDs. Both of those beliefs (that all STDs can be cured and that STD prevalence is not high) are likely to reduce motivation to protect oneself against STDs.
It is interesting to note that adolescents surveyed had greater knowledge of some aspects of STDs than adults (ASHA, 1996). When asked about the prevalence of STDs in the population, 12 percent of the adolescent respondents versus 4 percent of adult respondents correctly stated that the number was one in five
people. Although few adolescents could name an STD other than HIV/AIDS, they were more likely than adults to answer correctly that some STDs (in addition to HIV/AIDS) are incurable and that some STDs are asymptomatic.
STDs are far more common than is generally perceived by the general population or health care professionals. For example, while there is widespread awareness of genital herpes infections, there also are many misperceptions about them. Perhaps the single largest misperception concerns the prevalence of herpes infection. In a recent national survey of sexual behavior (Laumann, Gagnon, et al., 1994), 2 percent of survey respondents age 18-59 reported having had genital herpes. In contrast, population-based studies suggest that the prevalence of antibodies to herpes simplex virus type 2, which causes about 85 percent of initial episodes of genital herpes, was 21.7 percent in 1990 (Johnson et al., 1993). The reason for the substantial differences between the low prevalence of self-reported genital herpes infections and the far higher true prevalence of the disease may be misperceptions regarding the clinical manifestations of genital herpes infections. Herpes is most often described as an episodic illness, typically presenting as a painful genital eruption and recurring with similarly painful lesions of shorter duration. In fact, a quite different clinical spectrum of infection exists. Herpes infection may manifest as mild initial episodes and asymptomatic shedding of the virus (Koutsky et al., 1992). Other studies indicate that most genital herpes infections are spread by asymptomatic individuals who often are unaware of their infections (Mertz et al., 1992).
Conclusions
Biological and social factors contribute to the hidden nature of the STD epidemic. Biological factors, including the lack of signs and symptoms in infected persons, the long lag time from initial infection until signs of severe complications, and the propensity for STDs to more easily infect women than men, contribute to the general lack of awareness of STDs among health professionals and the public. A number of social factors contribute to the risk of STDs and place a disproportionate burden on certain populations in the United States. Poverty and inadequate access to health care, substance use, and sexual abuse all increase an individual's risk for STDs. Lack of health insurance is particularly acute among the age and ethnic groups at greatest risk of STDs. Even for the insured, access to comprehensive STD-related services may be difficult. Sex workers, persons in detention facilities, the homeless, migrant workers, and other disenfranchised persons represent "core" transmitters of STDs in the population. Efforts to prevent STDs in the entire community are not likely to be successful unless these groups receive appropriate STD-related services.
Many Americans are reluctant or unwilling to discuss sexuality and STD-related issues openly or refuse to have the issue appear in the public arena. Such reluctance has devastating consequences for STD prevention efforts. Open and
frank communication and the sharing of information regarding sexuality and STDs are essential to preventing high-risk sexual behavior. In order to change behavior, Americans have to feel comfortable discussing sexual health issues; open communication between parents and children, between sexual partners, between teachers and students, and between health care providers and patients is essential. The secrecy surrounding sexuality impedes sexuality education programs for adolescents, open discussion between parents and their children and between sex partners, balanced messages from mass media, education and counseling activities of health care professionals, and community activism regarding STDs. Opponents of sexuality education programs for adolescents are likely to deny the possibility that their children are sexually active. Unfortunately, denial often eliminates the possibility that parents will communicate with their children regarding STDs, and this encourages high-risk behaviors. Children in these families are likely to get their information, which is often inaccurate, from other sources. Lack of comfort with open discussions of sexuality also makes open communication regarding sexual history and negotiating safer sex difficult. In addition, this discomfort has also resulted in a mass media that has not been involved in promoting healthy sexual behaviors. This industry commonly acquiesces to the public's fascination with sex, yet is generally not willing to incorporate and promote factual information regarding STDs and protective behaviors. Furthermore, discomfort and secrecy among health care providers adversely affects the delivery of health services. As a result, many clinicians do not identify potential problems or are ineffective in counseling their patients regarding healthy sexual behavior. Finally, secrecy hinders community activism for STDs. An effective STD prevention program should focus on overcoming all barriers to open communication.
Despite or because of the secrecy surrounding sexuality, adolescents and young adults are becoming increasingly sexually active. Better research is needed to track the problem of STDs and identify possible solutions; much of the data available in this area are seriously outdated or incomplete. There is a compelling need for further training of clinicians, educators, and researchers in the area of human sexuality. The poor understanding of STDs among Americans strongly supports a coordinated campaign to improve knowledge and awareness.
References
AAP (American Academy of Pediatrics), Committee on Child Abuse and Neglect. Guidelines for the evaluation of sexual abuse of children. Pediatrics 1991;87:254-60.
AMA (American Medical Association), Council on Scientific Affairs. Health care needs of homeless and runaway youths. JAMA 1989;262:1358-61.
AMA, Council on Scientific Affairs. Health care needs of gay men and lesbians in the United States. JAMA 1996;275:1354-9.
Amaro H. Considerations for prevention of HIV infection among Hispanic women. Psychol Women Q 1988; 12:429-43.
Anderson JE, Dahlberg LL. High-risk sexual behavior in the general population: results from a national survey, 1988-1990. Sex Transm Dis 1992;17:320-5.
Aral SO, Holmes KK. Epidemiology of sexual behavior and sexually transmitted diseases. In: Holmes KK, Må PA, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:19-36.
ARHP, ANPRH (Association of Reproductive Health Professionals and Association of Nurse Practitioners in Reproductive Health). STD counseling practices and needs survey. Silver Spring, MD: Schulman, Ronca, and Bucuvalas, Inc., January 1995.
ASHA (American Social Health Association). International survey reveals lack of knowledge about STDs. STD News. A quarterly newsletter of the American Social Health Association. Fall 1995;3:1,10.
ASHA. Teenagers know more than adults about STDs, but knowledge among both groups is low. STD News. A quarterly newsletter of the American Social Health Association. Winter 1996;3:1, 5.
Barone C, Ickovics JR, Ayers TS, Katz SM, Voyce CK, Weissberg RP. High-risk sexual behavior among young urban students. Fam Plann Perspect 1996:28;69-74.
Bechtel GA, Shepherd MA, Rogers PW. Family, culture, and health practices among migrant farmworkers. J Community Health Nurs 1995;12:15-22.
Bell TA, Farrow JA, Stamm WE, Critchlow CW, Holmes KK. Sexually transmitted diseases in females in a juvenile detention center. Sex Transm Dis 1985;12:140-4.
Bickell NA, Vermund SH, Holmes M, Safyer S, Burk RD. Human papillomavirus, gonorrhea, syphilis, and cervical dysplasia in jailed women. Am J Public Health 1991;81:1318-20.
Blank S, Rubin S, Brome-Bunting M, Masterson M, McDonnell D, Fatt DL, et al. Improving syphilis treatment rates among women inmates in New York City. Proceedings of the twenty-seventh meeting, Society for Epidemiologic Research, June 15-18, 1994, Miami, FL. Salt Lake City : Society for Epidemiologic Research, 1994.
Brandt AM. No magic bullet: a social history of venereal disease in the United States since 1880. New York: Oxford University Press, Inc., 1985.
Brandt AM. AIDS in historical perspective: four lessons from the history of sexually transmitted diseases. Am J Public Health 1988;78:367-71.
Breakey WR, Fischer PJ, Kramer M, Nestadt G, Romanovski AJ, Ross A, et al. Health problems of homeless men and women in Baltimore. JAMA 1989;262:1352-7.
Brown JD, Newcomer SF. Television viewing and adolescents' sexual behavior. J. Homosexuality 1991;21:77-91.
Brown JD, Steele JR. Sex and the mass media. Report prepared for The Henry J. Kaiser Family Foundation and presented at "Sex and Hollywood: should there be a government role?" American Enterprise Institute, June 21, 1995, Washington, D.C.
Brown JD, Steele JR. Sexuality and the mass media: an overview. In: SIECUS Report. Sexuality in the media: Part 1. New York: Information and Education Council of the United States, 1996:24:3-9.
Brunham RC, Nagelkerke JN, Plummer FA, Moses S. Estimating the basic reproductive rates of Neisseria gonorrhoeae and Chlamydia trachomatis : the implications of acquired immunity [see comments]. Sex Transm Dis 1994;21:353-6.
Buchta RM. Attitudes of adolescents and parents of adolescents concerning condom advertisements on television. J Adolesc Health Care 1989;10:220-3.
Buerkel-Rothfuss NL, Strouse JS. Media exposure and perceptions of sexual behaviors: the cultivation hypothesis moves to the bedroom. In: Greenberg BS, Brown JD, Buerkel-Rothfuss NL, eds. Media, sex and the adolescent. Cresskill, NJ: Hampton Press, Inc., 1993:225-47.
Caetano R, Hines AM. Alcohol, sexual practices, and risk of AIDS among blacks, hispanics, and whites. J Acquire Immune Defic Syndr 1995;10:554-61.
Cameron DW, Simonsen JN, D'Costa LJ, Ronald AR, Maitha GM, Gakinya MN, et al. Female to male transmission of human immunodeficiency virus type 1: risk factors for seroconversion in men. Lancet 1989; 2:403-7.
Catania JA, Coates TJ, Stall R, Turner H, Peterson J, Hearst N, et al. Prevalences of AIDS-related risk factors and condom use the United States. Science 1992;258:1101-6.
Cates W Jr. Epidemiology and control of sexually transmitted diseases in adolescents. In: Schydlower M, Shafer MA, eds. AIDS and other sexually transmitted diseases. Philadelphia: Hanly & Belfus, Inc., 1990:409-27.
Cates W Jr. Contraception, contraceptive technology and STD. In: Holmes KK, Sparling PF, Mårdh PA, Lemon SM, Stamm WE, Piot P, Wasserheit JN, eds. Sexually transmitted diseases. 3rd ed. New York: McGraw-Hill, Inc., in press.
CDC (Centers for Disease Control and Prevention). Current trends: heterosexual behaviors and factors that influence condom use among patients attending a sexually transmitted disease clinic—San Francisco. MMWR 1990;39:685-9.
CDC. HIV infection, syphilis, and tuberculosis screening among migrant farm workers—Florida, 1992. MMWR 1992a;41:723-5.
CDC. HIV prevention in the U.S. correctional system, 1991. MMWR 1992b;41:389-91, 397.
CDC. Premarital sexual experience among adolescent women—United States, 1970-1988. MMWR 1992c;39:929-32.
CDC. 1993 Sexually transmitted diseases treatment guidelines. MMWR 1993;42(No. RR-14):56-66.
CDC. Trends in sexual risk behavior among high school students—United States, 1990, 1991, and 1993. MMWR 1995;44:124-5, 131-2.
CDC. Community-level prevention of human immunodeficiency virus infection among high-risk populations: the AIDS Community Demonstration Projects. MMWR 1996a;45(RR-6).
CDC. HIV/AIDS education and prevention programs for adults in prisons and jails and juveniles in confinement facilities—United States, 1994. MMWR 1996b;45:268-71.
Celum CL, Hook EW, Bolan GA, Spauding CD, Leone P, Henry KW, et al. Where would clients seek care for STD services under health care reform? Results of a STD client survey from five clinics. Eleventh Meeting of the International Society for STD Research, August 27-30, 1995 , New Orleans, LA [abstract no. 101].
Chilman CS. Adolescent sexuality in a changing American society. Washington, D.C.: U.S. Government Printing Office, 1978 (017-046-00050-1).
Cohen D, Scribner R, Clark J, Cory D. The potential role of custody facilities in controlling sexually transmitted diseases [published erratum appears in Am J Public Health 1992;82:684]. Am J Public Health 1992;82:552-6.
Critchlow CW, Wolner-Hanssen P, Eschenbach DA, Kiviat NB, Koutsky LA, Stevens CE, et al. Determinants of cervical ectopia and of cervicitis: age, oral contraception, specific cervical infection, smoking, and douching. Am J Obstet Gynecol 1995;173:534-43.
Culter JC, Arnold RC. Venereal disease control by health departments in the past: lessons for the present. Am J Public Health 1988;78:372-6.
Darrow WW. Assessing targeted AIDS prevention in male and female prostitutes and their clients. In: Paccaud F, Vader JP, Gutzwiller F, eds. Assessing AIDS prevention. Basel, Switzerland: Birkhäuser Verlag, 1992:215-31.
David HP, Morgall JM, Osler M, Rasmussen NK, Jensen B. United States and Denmark: different approaches to health care and family planning. Stud Fam Plann 1990;21:1-19.
DeBuono BA, Zinner SH, Daamen M, McCormack WM. Sexual behavior of college women in 1975, 1986, and 1989. N Engl J Med 1990;322:821-5.
Decker MD, Vaughn WK, Brodie JS, Hutcheson RH Jr., Schaffner W. Seroepidemiology of hepatitis B in Tennessee prisoners. J Infect Dis 1984;150:450-9.
DiClemente RJ, Lanier MM, Horan PF, Lodico M. Comparison of AIDS knowledge, attitudes, and behaviors among incarcerated adolescents and a public school sample in San Francisco. Am J Public Health 1991;81:628-30.
Dietz WH, Strasburger VC. Children, adolescents and television. Curr Probl Pediatr 1991;21:8-32. di Mauro D. Executive summary of sexuality research in the United States: an assessment of the social and behavioral sciences. New York: Social Science Research Council, 1995.
Dolan K, Wodak A, Penny R. AIDS behind bars: preventing HIV spread among incarcerated drug injectors. AIDS 1995;9:825-32.
Doll DC. Tattooing in prison and HIV infection [letter]. Lancet 1988;1:66-7.
Donelan K, Blendon RJ, Hill CA, Hoffman C, Rowland D, Frankel M, et al. Whatever happened to the health insurance crisis in the United States? Voices from a national survey. JAMA 1996;276:1346-50.
Donovan P. Taking family planning services to hard-to-reach populations. Fam Plann Perspect 1996;28:120-6.
Dougherty S.1996 National Farmworker Health Conference. J Int Assoc Physicians AIDS Care 1996;2:12-16,19.
EBRI (Employee Benefits Research Institute). Children without health insurance. Washington, D.C.: EBRI, Notes, Vol. 16(5), May 1995a.
EBRI. Sources of health insurance and characteristics of the uninsured: analysis of the March 1994 Current Population Survey. Washington, D.C.: EBRI, Special Issue Brief Number 158, February 1995b.
EDK Associates. Women & sexually transmitted diseases: the dangers of denial. New York: EDK Associates, 1994.
EDK Associates. The ABCs of STDs. New York: EDK Associates, 1995.
Edlin BR, Irwin KL, Faruque S, McCoy CB, Word C, Serrano Y, et al. Intersecting epidemics—crack cocaine use and HIV infection among inner-city young adults. The Multi-center Crack Cocaine and HIV Infection Study Team. N Engl J Med 1994;31:1422-7.
Elias CJ, Heise LL. Challenges for the development of female-controlled vaginal microbicides. AIDS 1994;8:1-9.
Elliot S. The sponsor is the surprise in Fox's first condom ad. New York Times, November 19, 1991; Sect. D: 19(col. 1).
Ericksen KP, Trocki KF. Behavioral risk factors for sexually transmitted diseases in American households. Soc Sci Med 1992;34:843-53.
Finelli L, Budd J, Spitalny KC. Early syphilis. Relationship to sex, drugs, and changes in high-risk behavior from 1987-1990. Sex Transm Dis 1993;20:89-95.
Finkelhor D and Associates. A sourcebook on child sexual abuse. Beverly Hills, CA: Sage Publications, 1986.
Fish AN, Fairweather DV, Oriel JD, Ridgeway GL. Chlamydial trachomatis infection in a gynecology clinic population: identification of high-risk groups and the value of contact tracing. Eur J Obstet Gynecol Reprod Biol 1989;31:67-74.
Flora JA, Maibach EW, Holtgrave D. Communication campaigns for HIV prevention: Using mass media in the next decade. In: IOM. Assessing the social and behavioral science base for HIV/AIDS prevention and intervention [workshop summary, background papers]. Washington, D.C.: National Academy Press, 1995:129-54.
Forrest KA, Washington AE, Daling JR, Sweet RL. Vaginal douching as a possible risk factor for pelvic inflammatory disease. J Natl Med Assoc 1989;81:159-65.
Forst ML. Sexual risk profiles of delinquent and homeless youths. J Community Health 1994;19:101-14.
Freeman HE, Blendon RJ, Aiken LH, Sudman S, Mullix CF, Covey CR. Americans report on their access to health care. Health Aff Millwood 1987;6:6-18.
Freeman HE, Corey CR. Insurance status and access to health services among poor persons. Health Serv Res 1993;28:531-41.
Furstenberg R, Moore K, Peterson J. Sex education and sexual experience among adolescents. Am J Public Health 1985;75:1331-2.
Gerbner G. Women and minorities on television: a study in casting and fate. Report presented to the Screen Actors Guild and the American Federation of Radio and Television Artists, Annenberg School for Communications, Philadelphia, June 1993.
Gerrard M. Sex, sex guilt and contraceptive use. J Pers Soc Psychol 1982;42:153-8.
Gerrard M. Sex, sex guilt and contraceptive use revisited: the 1980's. J Pers Soc Psychol 1987;52:975.
Glaser JB, Greifinger RB. Correctional health care: a public health opportunity. Ann Intern Med 1993;118:139-45.
Greenberg BS, Brown JD, Buerkel-Rothfuss NL, eds. Media, sex and the adolescent. Cresskill, NJ: Hampton Press, 1993.
Greenberg BS, Busselle RW. Soap operas and sexual activity. Report submitted to The Henry J. Kaiser Family Foundation, October 1994.
Greenberg BS, Smith S, Ah Yun J, Busselle R, Rampoldi Hnilo L, Mitchell M, et al. The content of television talk shows: topics, guest and interactions. Departments of Communication and Telecommunication, Michigan State University. Report prepared for The Henry J. Kaiser Family Foundation, November 1995.
Greenberg J, Schnell D, Conlon R. Behaviors of crack cocaine users and their impact on early syphilis intervention. Sex Transm Dis 1992;19:346-50.
Greenberg MSZ, Singh T, Htoo M, Schultz S. The association between congenital syphilis and cocaine/crack use in New York City: a case-control study. Am J Public Health 1991;81:1316-8.
Guidry HM. Childhood sexual abuse: role of the family physician. Am Fam Physician 1995;51:407-14.
Gutman LT, St. Claire K, Herman Giddens ME. Prevalence of sexual abuse in children with genital warts [letter; comment]. Pediatr Infect Dis J 1991;10:342-3.
Hale RW, Char DF, Nagy K, Stockert N. Seventeen-year review of sexual and contraceptive behavior on a college campus. Am J Obstet Gynecol 1993;168 (6 Pt 1):1833-7; discussion 1837-8.
Hall J. The networks' condom cover-up. Raleigh News and Observer, January 31, 1994, C10.
Hammett TM, Widom R, Epstein J, Gross M, Sifre S, Enos T. 1994 Update: HIV/AIDS and STDs in correctional facilities. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, National Institute of Justice/U.S. Department of Health and Human Services, Public Health Service, CDC, December 1995.
Harris L and Associates. Attitudes about television, sex and contraception. A survey of a cross-section of adult Americans. Conducted for Planned Parenthood Federation of America. February 1987.
Harris L and Associates. Sexual material on American network television during the 1987-88 season. New York: Planned Parenthood Federation of America, 1988.
Hein K, Cohen MI, Marks A, Schonberg SK, Meyer M, McBride A. Age at first intercourse among homeless adolescent females. J Pediatr 1978;93:147-8.
Herold ES, Goodwin MS, Lero DS. Self-esteem, locus of control, and adolescent contraception. J Psych 1979;101:83-8.
Hingson RW, Strunin L, Berlin BM, Hereen T. Beliefs about AIDS, use of alcohol and drugs, and unprotected sex among Massachusetts adolescents. Am J Public Health 1990;80:295-9.
Hofferth SL, Kahn JR, Baldwin W. Premarital sexual activity among U.S. teenage women over the past three decades. Fam Plann Perspect 1987;19:46-53.
Hogan H. Human sexuality, a nursing perspective. Norwalk, CT: Appleton-Century-Crofts Co., 1980.
Holmes MD, Safyer SM, Bickell NA, Vermund SH, Hanff PA, Phillips RS. Chlamydial cervical infection in jailed women. Am J Public Health 1993;83:551-5.
Horsburgh CR, Jarvis JQ, McArthur T, Ignacio T, Stock P. Seroconversion to human immunodeficiency virus in prison inmates. Am J Public Health 1990;80:209-10.
Hudgins R, McCusker J, Stoddard A. Cocaine use and risky injection and sexual behaviors. Drug Alcohol Depend 1995;37:7-14.
Hyde S. Understanding human sexuality. 5th ed. New York: McGraw Hill, Inc., 1994.
IOM (Institute of Medicine). Understanding the determinants of HIV risk behavior. In: Auerbach JD, Wypijewska C, Brodie HKH, eds. AIDS and behavior. Washington, D.C.: National Academy Press, 1994:78-123.
IOM. Best intentions: unintended pregnancy and the well-being of children and families. Brown SS, Eisenberg L, eds. Washington, D.C.: National Academy Press, 1995.
Jemmott LS, Jemmott JB. Family structure, parental strictness, and sexual behavior among inner-city black male adolescents. J Adolesc Res 1992a;7:192-207.
Jemmott LS, Jemmott JB. Increasing condom-use intentions among sexually active black adolescent women. Nurs Res 1992b;41:273-9.
Jemmott JB, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention. Am J Public Health 1992; 82:372-7.
Johnson R, Lee F, Hadgu A, McQuillan G, Aral S, Keesling S, et al. U.S. genital herpes trends during the first decade of AIDS—prevalences increased in young whites and elevated in blacks. In: Proceedings of the Tenth Meeting of the International Society for STD Research, August 23-September 1, 1993, Helsinki, Finland [abstract No. 22].
Johnstone H, Tornabene M, Marcinak J. Incidence of sexually transmitted diseases and Pap smear results in female homeless clients from the Chicago Health Outreach Project. Health Care Women Int 1993;14:293-9.
Jones JL, Rion P, Hollis S, Longshore S, Leverette WB, Ziff L. HIV-related characteristics of migrant workers in rural South Carolina. South Med J 1991;84:1088-90.
Judson FN. Gonorrhea. Med Clin North Am 1990;74:1353-67.
Kalichman SC, Kelly JA, Johnson JR, Bulto M. Factors associated with risk for HIV infection among chronic mentally ill adults. Am J Psychiatry 1994;151:221-7.
Keim J, Woodard MP, Anderson MK. Screening for Chlamydia trachomatis in college women on routine gynecological exams. J Am Coll Health 1992;41:17-9, 22-3.
Kennedy CA, Skurnick J, Wan JY, Quattronc G, Sheffet A, Quinones M, et al. Psychological distress, drug and alcohol use as correlates of condom use in HIV-serodiscordant heterosexual couples. AIDS 1993;7:1493-9.
Kilborne J. Killing us softly: gender roles in advertising. Adolesc Med: State of the Art Rev 1993;4:635-49.
Kimani J, Maclean IW, Bwayo JJ, MacDonald K, Oyugi J, Maitha GM, et al., Risk factors for Chlamydia trachomatis pelvic inflammatory disease among sex workers in Nairobi, Kenya. J Infect Dis 1996;173:1437-44.
Kirby D, Short L, Collins J, Rugg D, Kolbe L, Howard M, et al. School-based programs to reduce sexual risk behaviors: a review of effectiveness. Public Health Rep 1994;109:339-60.
Klassen AD, Williams CI, Levitt EE. Sex and morality in the U.S. Middletown, CT: Wesleyan University Press, 1989.
Klein JD, Brown JD, Childers KW, Oliveri J, Porter C, Dykers C. Adolescents' risky behavior and mass media use. Pediatrics 1993; 92:24-31.
Koelle DM, Benedetti J, Langenberg A, Corey L. Asymptomatic reactivation of herpes simplex virus in women after the first episode of genital herpes. Ann Intern Med 1992;116:433-7.
Koopman C, Rosario M, Rotheram-Borus MJ. Alcohol and drug use and sexual behaviors placing runaways at risk for HIV infection. Addict Behav 1994;19:95-103.
Kosovich DR. Sexuality throughout the centuries. Psychiatr Opin 1978;15:15-9.
Kost K, Forrest JD. American women's sexual behavior and exposure to risk of sexually transmitted diseases. Fam Plann Perspect 1992;24:244-54.
Koutsky LA, Stevens CE, Holmes KK, Ashley RL, Kliviat NB, Critchlow CW, et al. Underdiagnosis of genital herpes by current clinical and viral-isolation procedures. N Engl J Med 1992;326:1533-9.
Kreiss JK, Hopkins SG. The association between circumcision status and human immunodeficiency virus infection among homosexual men. J Infect Dis 1993;168:1404-8.
Laumann EO, Gagnon JH, Michael RT, Michaels S. The social organization of sexuality: sexual practices in the United States. Chicago, IL: University of Chicago Press, 1994.
Laumann EO, Michael RT, Gagnon JH. A political history of the National Sex Survey of Adults. Fam Plann Perspect 1994;26:34-8.
Lear D. Sexual communication in the age of AIDS: the construction of risk and trust among young adults. Soc Sci Med 1995;41:1311-23.
Lebow MA. Contraceptive advertising in the United States. Women's Health Issues 1994;4:196-208.
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, prevention. Am Psychol 1993;48:1035-45.
Leigh, BC, Temple MT, Trocki KF. The sexual behavior of U.S. adults: results from a national survey. Am J Public Health 1993;83:1400-8.
Leigh BC, Temple MT, Trocki KF. The relationship of alcohol use to sexual activity in a U.S. national sample. Social Science Med 1994;39:1527-35.
Lewis CE, Freeman HE. The sexual history-taking and counseling practices of primary care physicians. West J Med 1987;147:165-7.
Lewis CE, Montgomery K. The AIDS-related experience and practices of primary care physicians in Los Angeles: 1984-89. Am J Public Health 1990;80:1511-3.
Lichter SR, Lichter LS, Rothman S. Prime time. How TV portrays American culture. Washington, D.C.: Regnery Publishing, Inc., 1994.
Lief H, Karlen A. Sex education in medicine. New York: Spectrum Publications, 1976.
Lowry DT, Schidler JA. Prime time TV portrayals of sex, "safe sex" and AIDS: a longitudinal analysis. Journalism Q 1993;70:628-37.
Lowry DT, Towles DE. Soap opera portrayals of sex, contraception, and sexually transmitted diseases. J Communications 1989;39:76-83.
Lowry R, Holtzman D, Truman BI, Kann L, Collins JL, Kolbe LJ. Substance use and HIV-related sexual behaviors among US high school students: are they related? Am J Public Health 1994;84:1116-20.
Mahon N. New York inmates' HIV risk behaviors: the implications for prevention policy and programs. Am J Public Health 1996;86:1211-5.
Manov A, Lowther L. A health care approach for hard-to-reach adolescent runaways. Nurs Clin North Am 1983;18:333-42.
Martensen RL. Syphilis, contagion, and the place of sexuality in late 19th-century America. JAMA 1994;272:69.
Martin HL, Hyange PM, Richardson BA, Chohan B, Hillier SL, Mandaliya K, et al. Association between presence of vaginal lactobacilli and acquisition of HIV and STDs. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. TuC 2692].
Marx R, Aral SO, Rolfs RT, Sterk CE, Kahn JG. Crack, sex, and STD. Sex Transm Dis 1991;18:92-101.
Marx PA, Spira AI, Gettie A, Dailey PJ, Veazey RS, Lackner AA, et al. Progesterone implants enhance SIV vaginal transmission and early virus load. Nature Med 1996;2:1084-9.
Matthews WC, Booth MW, Turner JD, Kessler L. Physicians' attitudes toward homosexuality—survey of California County Medical Society. West J Med 1986;144:106-10.
May RM, Anderson RM. Transmission dynamics of HIV infection. Nature 1987;326:137-42.
Mayden B. Sexuality education for youths in care. A state-by-state survey. Washington, D.C.: Child Welfare League of America Press, 1996.
Mays VM, Cochran SD. Issues in the perception of AIDS risk and risk reduction activities by black and Hispanic/Latina women. Am Psychol 1988;43:949-57.
McCoy HV, Inciardi JA. Women and AIDS: social determinants of sex-related activities. Women Health 1993;20:69-86.
Merrill JM, Laux LF, Thornby JI. Why doctors have difficulty with sex histories. Southern Med J 1990;83:613-17.
Mertz GJ, Benedetti J, Ashley R, Selke SA, Corey L. Risk factors for the transmission of genital herpes. Ann Intern Med 1992;116:197-202.
Miller BC, Monson BH, Norton MC. The effects of forced sexual intercourse on white female adolescents. Child Abuse Negl 1995;19:1289-301.
Moran JS, Peterman T. Sexually transmitted diseases in prisons and jails. Prison J 1989;64:1-6.
Moses S, Plummer FA, Bradley JE, Ndinya-Achola JO, Nagelkerke NJ, Ronald AR. The association between lack of male circumcision and risk for HIV infection: a review of the epidemiological data. Sex Transm Dis 1994;21:201-10.
Moss GB, Clemetson D, D'Costa L, Plummer FA, Ndinya-Achola JO, Reilly M, et al. Association of cervical ectopy with heterosexual transmission of human immunodeficiency virus: results of a study of couples in Nairobi, Kenya. J Infect Dis 1991;164:588-91.
Mostad S, Welch M, Chohan B, Reilly M, Overbaugh J, Mandalya K, et al. Cervical and vaginal HIV-1 DNA shedding in female STD clinic attenders. Eleventh International Conference on AIDS, July 7-12, 1996, Vancouver [abstract no. WeC 333].
Mott FL, Fondell MM, Hu PN, Kowaleski-Jones L, Menaghan EG. The determinants of first sex by age 14 in a high-risk adolescent population. Fam Plann Perspect 1996;28:13-8.
Mutter RC, Grimes RM, Labarthe D. Evidence of intraprison spread of HIV infection. Arch Intern Med 1994;154:793-5.
Nathan SG. Are clinical psychology graduate students being taught enough about sexuality? A survey of doctoral programs. J Sex Res 1986;22:520-4.
NCCHC (National Commission on Correctional Health Care). Standards for health services in jails. Chicago: National Commission on Correctional Health Care, 1992.
NCCHC. Administrative management of HIV in corrections. Position statement. Chicago: National Commission on Correctional Health Care, September 25, 1994.
Oh MK, Cloud GA, Wallace LS, Reynolds J, Strudevant M, Feinstein RA. Sexual behavior and sexually transmitted diseases among male adolescents in detention. Sex Transm Dis 1994;21:127-32.
O'Leary A, Jemmott LS. Future directions. In: O'Leary A, Jemmott, LS, eds. Women at risk: issues in the primary prevention of AIDS. New York: Plenum Press, 1995:257-9.
Olson B. Sex and the soaps: a comparative content analysis of health issues. Journalism Q 1994;71:840-50.
Orbovich C. Case studies of collaboration between family planning agencies and managed care organizations. West J Med 1995;163(3 Suppl):39-44.
Peipert JF, Domagalski L, Boardman L, Daamen M, Zinner SH. College women and condom use, 1975-1995. New Engl J Med 1996;335:211.
Piot P, Islam MQ. Sexually transmitted diseases in the 1990s. Global epidemiology and challenges for control. Sex Transm Dis 1994;21(2 Suppl):S7-S13.
Plichta SB, Abraham C. Violence and gynecological health in women < 50 years old. Am J Obstet Gynecol 1996;174:903-7.
Plummer FA, Ngugi EN. Prostitutes and their clients in the epidemiology and control of sexually transmitted diseases. In: Holmes KK, March P-A, Sparling, PF, Wiesner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:71-6.
Plummer FA, Simonsen JN, Chubb H, Slaney L, Kimata J, Bosire M, et al. Epidemiologic evidence for the development of serovar immunity after gonococcal infection . J Clin Invest 1989;83:1472-6.
Poorman S, Albrecht L. Human sexuality and the nursing process. Norwalk, CT: Appleton & Lange Publishing Co., 1987.
Ramos R, Shain, RN, Johnson L. ''Men I mess with don't have anything to do with AIDS": Using ethno-theory to understand sexual risk perception. Sociol Q 1995;36:483-504.
Reinisch JM, Hill CA, Sanders S, Ziemba-Davis M. High-risk sexual behavior at a Midwestern university: a confirmatory study. Fam Plann Perspect 1995;27:79-82.
Richman RL, Lodico M, DiClemente RJ, Morris R, Baker C, Huscroft S. Sexual communication is associated with condom use by sexually active incarcerated adolescents. J Adolesc Health 1994;15:383-8.
Risen CB. A guide to taking a sexual history. Clin Sex 1995;18:39-53.
Rosenbaum S, Shin P, Mauskopf A, Fund K, Stern G, Zuvekas A. Beyond the freedom to choose. Medicaid, managed care, and family planning. West J Med 1995;163(3 Suppl): S33-S38.
Rosenberg MJ, Gollub EL. Commentary: methods women can use that may prevent sexually transmitted diseases, including HIV [see comments]. Am J Public Health 1992;82:1473-8.
Rosenblum L, Darrow W, Witte J, Cohen J, French J, Gill PS, et al. Sexual practices in the transmission of hepatitis B virus and prevalence of hepatitis delta virus infection in female prostitutes in the United States. JAMA 1992;267:2477-81.
SAMHSA (Substance Abuse and Mental Health Services Administration). National Household Survey on Drug Abuse: population estimates 1994. Rockville, MD: Substance Abuse and Mental Health Services Administration, DHHS Publication No. (SMA) 95-3063, September 1995.
Scholes D, Daling JR, Stergachis A, Weiss NS, Wang SP, Grayston JT. Vaginal douching as a risk factor for acute pelvic inflammatory disease. Obstet Gynecol 1993;81:601-6.
Schulte JM, Ramsey HA, Paffel JM, Roberts MA, Williams RL, Blass CM, et al. Outbreaks of syphilis in rural Texas towns, 1991-1992. South Med J 1994;87:493-6.
Schwartz A, Colby DC, Reisinger AL. Variation in Medicaid physician fees. Health Aff Millwood 1991;10:131-9.
Seidman SN, Sterk-Elifson C, Aral SO. High-risk sexual behavior among drug-using men. Sex Transm Dis 1994;21:173-80.
Shafer MA. Sexual behavior and sexually transmitted diseases among male adolescents in detention. Sex Transm Dis 1994;21:181-2.
Shafer MA, Hilton JF, Ekstrand M, Keogh J, Gee L, DiGiorgio-Haag L, et al. Relationship between drug use and sexual behaviors and the occurrence of sexually transmitted diseases among high-risk male youth. Sex Transm Dis 1993;20:307-13.
Sherman BL, Dominick JR. Violence and sex in music videos: TV and rock 'n' roll. J Communication 1986;36:79-93.
Sherman DJ. The neglected health care needs of street youth. Public Health Rep 1992;107:433-40.
Siegel K, Mesango FP, Chen J, Christ G. Factors distinguishing homosexual males practicing risky and safer sex. Soc Sci Med 1989;28:561-9.
Smith LS. Ethnic differences in knowledge of sexually transmitted diseases in North American black and Mexican-American migrant farmworkers. Res Nurs Health 1988;11:51-8.
Smith L, Lanthrop L. AIDS and human sexuality. Can J Public Health 1993;84(1 Suppl):S14-S18.
Sokolow JA. Eros and modernization: Sylvester Graham, health reform, and the origins of Victorian sexuality in America. Cranbury, NJ: Associated University Presses, Inc., 1983.
Sonenstein FL, Ku L, Schulte MM. Reproductive health care delivery. Patterns in a changing market. West J Med 1995;163(3 Suppl):7-14.
Sonenstein FL, Pleck JH, Ku LC. Levels of sexual activity among adolescent males in the United States [published erratum appears in Fam Plann Perspect 1991;23:225] . Fam Plann Perspect 1991;23:162-7.
Stall R, McKusick L, Wiley J, Coates TJ, Ostro DG. Alcohol and drug use during sexual activities and compliance with safe sex guidelines for AIDS. Health Education Q 1986;13:359-71.
Stamm WE, Holmes KK. Chlamydial trachomatis infections in the adult. In: Holmes KK, Mårdh PA, Sparling PF, Weisner PJ, Cates W Jr., Lemon SM, et al., eds. Sexually transmitted diseases. 2nd ed. New York: McGraw-Hill, Inc., 1990:181-93.
STD Communications Roundtable. STDTALK: spreading the word about sexually transmitted diseases. Washington, D.C.: Ogilvy Adams & Rinehart, 1996.
Strasburger VC. Adolescent sexuality and the media. Pediatr Clin North Am 1989;36:747-73.
Strasburger VC. Television and adolescents: Sex, drugs, and rock 'n' roll. Adoles Med: State of the Art Rev 1990;1:161-94.
Strasburger VC. Adolescent sexuality and the media. Curr Opin Pediatr 1992;4:5948.
Strasburger VC. Adolescents and the media. Medical and psychological impact. Thousand Oaks, CA: Sage Publications, Developmental Clinical Psychology and Psychiatry Series, Vol. 33, 1995.
Strouse JS, Buerkel-Rothfuss N. Media exposure and sexual attitudes and behaviors of college students. In: Greenberg BS, Brown JD, Buerkel-Rothfuss, eds. Media, sex and the adolescent. Cresskill, NJ: Hampton Press, Inc., 1993:277-92.
Stuntzner-Gibson D. Women and HIV disease: an emerging social crisis. Social Work 1991;36:22-7.
Sugerman ST, Hergenroeder AC, Chacko MR, Parcel GS. Acquired immunodeficiency syndrome and adolescents. Knowledge, attitudes, and behaviors of runaway and homeless youths. Am J Dis Child 1991;145:431-6.
Suplee C. Apprehensive NIH defers sex survey; political concerns cited for decision. Washington Post, September 25, 1991, A1.
Thomas JC, Tucker MJ. The development and use of the concept of a sexually transmitted disease core. J Infect Dis 1996;174(Suppl 2):S134-43.
U.S. Department of Justice. Selected findings: violence between intimates, Bureau of Justice Statistics, NCJ-149259. Washington, D.C.: U.S. Department of Justice, 1994.
U.S. Department of Justice. Prisoners at mid-year 1995. Bureau of Justice Statistics, National Prisoner Statistics Series. Washington D.C.: U.S. Department of Justice, December 3, 1995.
Warner DL, Rochat RW, Fichtner RR, Toomey KE, Nathan L, Stoll B, et al. Untreated syphilis in pregnant women: identifying gaps in prenatal care. 123rd Annual American Public Health Association Meeting, October 29-November 2, 1995, San Diego, CA [session 4030].
Wasserheit JN. Effect of changes in human ecology and behavior on patterns of sexually transmitted diseases, including human immunodeficiency virus infection. Proc Natl Acad Sci 1994;91:2430-5.
Webber MP, Lambert G, Bateman DA, Hauser WA. Maternal risk factors for congenital syphilis: a case-control study. Am J Epidemiol 1993;137:415-22.
Weber FT, Gearing J, Davis A, Conlon A. Prepubertal initiation of sexual experiences and older first partner predict promiscuous sexual behavior of delinquent adolescent males—unrecognized child abuse? J Adolesc Health 1992;13:600-5.
Widom R, Hammett TM. Research in brief: HIV/AIDS and STDs in juvenile facilities. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, National Institute of Justice, April 1996.
Wolner-Hanssen P, Eschenbach DA, Paavonen J, Kiviat N, Stevens C, Critchlow C, et al. Decreased risk of symptomatic chlamydial pelvic inflammatory disease associated with oral contraceptive use. JAMA 1990;263:54-9.
Wolner-Hanssen P, Eschenbach DA, Paavonen J, Stevens CE, Kiviat NB, Critchlow C, et al. Association between vaginal douching and acute pelvic inflammatory disease. JAMA 1990;263:1936-41.
Woods H. Human sexuality in health and illness. St. Louis: C.V. Mosby Co., 1979.
WREI (Women's Research and Education Institute). Women's health care costs and experiences. Washington, D.C.: Women's Research and Education Institute, 1994.
Zelnick M, Kim Y. Sex education and its association with teenage sexual activity, pregnancy, and contraceptive use. Fam Plann Perspect 1982;16:117-26.

















































