7
MARIJUANA AND MUSCLE SPASTICITY

Coping with stiff, aching, cramping muscles is a way of life for most of the 2.5 million people in the world who have multiple sclerosis. Many of the 15 million people with spinal cord injuries also suffer from the same symptoms, which cause pain, limit movement, and rob people of needed sleep. Although several conventional medications can reduce these patients' discomfort, taking them rarely provides complete relief. Often the drugs cause weakness, drowsiness, and other side effects that some patients find intolerable.
Given this outlook, it is not hard to understand why some people with multiple sclerosis and spinal cord injuries have sought relief through marijuana. Several such patients told the IOM team that their muscle spasms decreased after smoking marijuana (see Chapter 2). Some also said they valued the drug because it relieved nausea or helped them sleep. Likewise, in a 1982 survey of people with spinal cord injuries, 21 of 43 respondents reported that marijuana reduced muscle spasticity1 (a condition in which muscles tense reflexively and resist stretching), while nearly every participant in a 1997 survey of 112 regular marijuana users with multiple sclerosis replied that the drug lessened both pain and spasticity.2 This is not to say that most people with multiple sclerosis find relief with marijuana but only that the marijuana users among them do.
Animal research, too, suggests that marijuana calms muscle spasticity. Spasms are thought to originate in areas of the brain that control movement, including several sites with abundant cannabinoid receptors. In one experiment, researchers found that rodents became more animated under the influence of small amounts of cannabinoids but less active when they received larger doses. Many marijuana users also note that the drug affects movement, making their bodies sway and their hands unsteady. The exact mechanism(s) by which cannabinoids exert these effects remains unknown.
Despite these suggestive findings and the depth of anecdotal evidence, marijuana's antispasmodic properties remain largely untested in the clinic. The few existing reports are extremely limited in scope; for example, none of the studies discussed in this chapter included more than 13 patients, and some were conducted on a single patient. Also, in several cases the patients' subjective evaluations of improvement contrasted with objective measures of their physical performance. Still, the lack of good universally effective medicine for muscle spasticity is a compelling reason to continue exploring cannabinoid drugs in the clinic.
MULTIPLE SCLEROSIS
Multiple sclerosis (or MS) is a progressive disease of the nervous system with no known cure. It appears to result from a malfunction of the immune system, which inflames nerves in the brain, brain stem, and spinal cord. Specifically, the disease destroys the protective coating called myelin that sheaths the neural fibers like insulation on electrical wire. Without an intact myelin layer, nerve cells lose some or all of their ability to transmit impulses. This situation produces an array of symptoms, including fatigue, depression, vertigo, blindness, incontinence, and loss of voluntary muscle control, as well as muscle spasticity. MS is characterized by scarring—“sclerosis ”—that occurs in the white matter of the central nervous system after nerves and myelin are lost.
Approximately 90 percent of MS patients develop spasticity. Some people experience this condition merely as muscle stiffness; others endure constant ache, cramps, or involuntary muscle contractions (spasms) that are both painful and debilitating. These
spasms often affect the legs and can disrupt sleep. Most people with MS experience intermittent “attacks” of spasticity that become increasingly disabling the longer they have the disease. In the worst cases, patients become partially or even completely paralyzed.
The drugs most commonly prescribed to treat the symptoms of MS include baclofen (Lioresal) and tizanidine (Zanaflex) which relieve both spasticity and muscle spasms but often only partially and sometimes not at all. Both are sedatives, so they cause drowsiness; additional side effects include dry mouth and muscle weakness. The latter is especially problematic for people with MS, whose muscles get weaker as the disease progresses.
Both marijuana and THC have been tested for their ability to relieve spasticity in small but rigorous clinical studies. One double-blind experiment (see Introduction to Part II for an explanation of double-blind methods) included both MS patients and unaffected individuals.3 Before and after smoking a single marijuana cigarette that contained approximately 15 milligrams of THC—enough to make most people feel “high” and to impair their motor control—patients were videotaped as they stood on a platform that slid back and forth at unpredictable times. The researchers then measured participants ' shoulder movements as an index for how well they kept their balance.
Participants with MS often thought that their symptoms had improved after smoking marijuana. But while their spasticity may indeed have decreased (it was not measured), their posture and balance were actually impaired; this was also the case with the 10 participants who did not have MS. The MS patients had greater difficulty maintaining their balance before smoking and were more negatively affected by marijuana than the healthy participants.
While the fact that every MS patient in the previous study experienced relief is intriguing, it does not constitute strong evidence that marijuana relieves spasticity because marijuana-induced euphoria or pain relief might decrease patients' perceptions of muscle stiffness or spasticity. The same is true of respondents to the surveys described earlier. Moreover, surveys cannot measure the degree to which respondents feel better simply because they expect to do so. Such placebo effects are signifi-
cant; for example, in controlled trials of pain medications, as many as 30 percent of the participants who received a placebo reported feeling relief. This does not mean that placebo effects are not “real.” It is possible that the psychological effects of taking a placebo drug cause physiological changes in the brain. But it does mean that the effects are not directly due to the medication being tested.
THC's effects on spasticity were tested in three separate clinical studies, which together enrolled a total of 30 MS patients.4 All three were open trials in which participants knew they would be receiving THC. Perhaps not surprisingly, most of the patients —or in one case the investigators who examined them—reported that treatment with THC improved their symptoms (see Figure 7.1). The drug was not effective for all patients, however, and frequently caused unpleasant side effects.
Objective measurements of patients' symptoms in these studies were often at odds with their subjective reports. In one study researchers measured muscle tremor with a mechanical device, which showed detectable change in only two of eight patients, seven of whom had reported improved symptoms.5 In another study standardized physician's measures showed that treatment with THC had not produced any changes in spasticity despite reports of reduced spasticity by 11 of 13 patients. 6 It may be that the measuring techniques used in both studies were not sensitive enough to detect subtle improvements. It is also possible that patients' reports of symptom improvement were influenced by placebo effects or by effects of THC, such as anxiety reduction, that are only indirectly related to spasticity. Neither possibility can be ruled out due to the small size of these studies.
In addition to these experiments on THC, a single patient who tested the THC analog nabilone—a synthetic compound that activates the same cellular receptors as THC—also reported an improvement in spasticity as well as in other MS symptoms (see Figure 7.2).7
These clinical results are considerably less dramatic than survey and anecdotal reports of marijuana's effectiveness in relieving muscle spasms. It is possible, however, that a series of larger, better-designed clinical trials would produce stronger evidence in favor of marijuana-based medicines for MS. At this writing
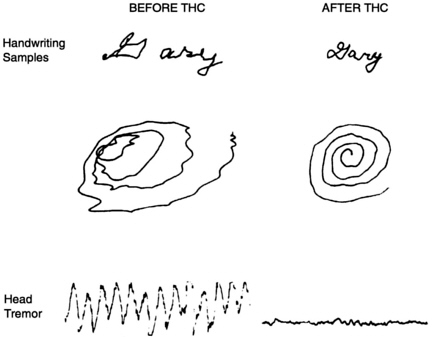
FIGURE 7.1 Effect of THC on tremor caused by multiple sclerosis. In this experiment, a 30-year-old man with multiple sclerosis who suffered from a disabling tremor was treated with 5 milligrams of THC. Researchers compared the man's handwriting and head movement before, and 90 minutes after, receiving the drug. (Reprinted by permission of D.B. Clifford and the Annals of Neurology. Tetrahydrocannabinol for tremor in multiple sclerosis. 1983. Annals of Neurology 13(6):669-671.)
such studies are in the planning stages in Britain, where a large proportion of medical marijuana users are people with MS. For example, researchers have proposed a clinical trial to compare the effectiveness of three types of treatment for MS: marijuana extract, delivered by inhaler; dronabinol (Marinol); and placebo.
Clinical trials usually require preliminary experiments on animal models of a disease, which enable researchers to predict its effects on humans. With that knowledge scientists can then design trials that accurately measure the ability of the drug to relieve patients ' symptoms. Existing animal models mimic some MS symptoms, but so far none have succeeded in duplicating spasticity. But researchers can use the best-available indicator of
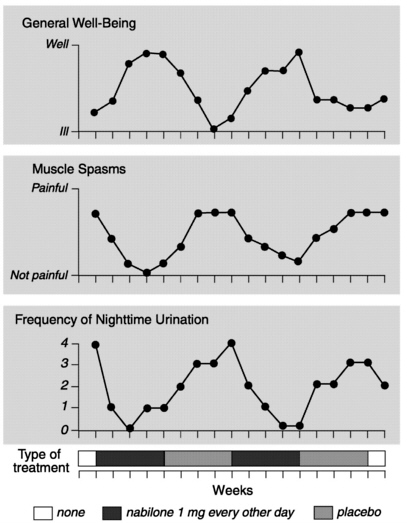
FIGURE 7.2 Effect of nabilone on multiple sclerosis symptoms. This chart shows the results of a trial in which a 45-year-old man with MS received treatments with the THC analog nabilone, alternating with a placebo. While the results suggest that THC might relieve spasticity, the study has several flaws. First, nabilone sedated the patient, which may have caused him to feel some relief; the placebo did not. Second, instead of measuring spasticity, the researchers measured the patient 's perception of pain, which may have been relieved without any improvement in spasticity.
Because nighttime urination is not governed by conscious control, improvement in this symptom appears to provide stronger evidence that THC reduced spasticity. On the other hand, it may merely indicate that THC helped the patient sleep better. While intriguing, this single-patient trial does not prove that THC can reliably relieve spasticity.
(Figure used by permission of C.N. Martyn and The Lancet. Nabilone in the treatment of multiple sclerosis. The Lancet 345(March 4, 1995):579.)
the condition, known as the pendulum test, to study the effectiveness of antispasticity drugs in human subjects.
Participants in this test lie on an examining table with their legs extending over the edge. They let their legs fall, and a video camera records the resulting motion, which is affected by muscle resistance. Computer analysis of the recording enables researchers to determine the degree to which spasticity impeded each patient's movement. Since THC is mildly sedating it is important to distinguish this effect from any actual decrease in spasticity produced by the drug. Researchers could make such a distinction by using the pendulum test to compare THC's effects with those of other mild sedatives, such as benzodiazepines.
If an antispasmodic drug is developed from THC, its sedative effect could prove beneficial to MS patients whose muscle spasms interrupt their sleep. Drowsiness at bedtime might be welcome, and any mood-altering side effects might be less of a problem than when the patient was awake. It is also possible, however, that THC might disrupt normal sleep patterns in some people.
TOWARD BETTER TREATMENTS
While the same physiological process causes spasticity in both MS and spinal cord injury, it produces quite different symptoms in the two diseases. People with MS tend to experience occasional “attacks ” of intense pain, stiffness, or muscle spasms at unpredictable intervals, while people with spinal cord injuries experience only minor fluctuations and persistent discomfort. Nevertheless, it is very likely that the same drugs could be adapted to treat the two groups of patients. People with MS and those with spinal cord injury alike would benefit from medications that relieve pain, stiffness, and spasms without muscle weakening, which occurs with the best currently available treatments. Because of the harms associated with long-term marijuana smoking, it should be discouraged as a means of treating chronic conditions such as spinal cord injury or MS.
Whether marijuana could yield useful medicines for spasticity remains to be determined, for the clinical evidence to date is too sparse to accept. But the few positive reports of the ability of THC and nabilone to reduce spasticity, together with numerous
anecdotal accounts from marijuana users with MS and spinal cord injuries, suggest that carefully designed clinical trials testing the effects of cannabinoids on muscle spasticity would be worthwhile.
Two factors complicate the design of such trials. First, while MS patients report that marijuana relieves spasticity, it negatively affects their ability to balance, exacerbating another symptom of the disorder. It may be that patients would become tolerant to the balance-impairing effects of cannabinoids relatively quickly yet continue to get relief from spasticity. It might also be possible to separate these effects by creating chemical variants of natural cannabinoids. Second, human trials should rule out any masking or enhancing effect of anxiety reduction due to THC, since anxiety worsens spasticity in many patients.
If THC or a related compound does prove to relieve spasticity, it would make sense for some patients to take the drug orally. In this way patients could take advantage of THC's ability to remain active in the body for several hours. People with spinal cord injury, whose symptoms vary little throughout the day, could get extended relief from a pill taken at bedtime or in the morning. On the other hand, MS patients might find more use for an inhaled form of THC to relieve their more intermittent symptoms. Unlike pills, this delivery method would allow patients to feel the drug's effects quickly and with a minimum of sedation. At nighttime MS patients might actually prefer pills that cause drowsiness as well as relieve spasticity.
People with MS may soon be able to test a cannabinoid inhaler if the previously described British clinical trials receive funding. Additional trials may take place in Canada, where in July 1999 the government issued a request for research proposals to study medical uses of marijuana. While the official announcement did not prescribe specific research topics, it mentioned multiple sclerosis as a possible subject for a clinical trial.
NOTES
1. Malec J, Harvey RF, Cayner JJ. 1982. “Cannabis effect on spasticity in spinal cord injury.” Archives of Physical Medicine and Rehabilitation 63:116-118.
2. Consroe P, Musty R, Rein J, Tillery W, Pertwee RG. 1997. “The per-
ceived effects of smoked cannabis on patients with multiple sclerosis. ” European Neurology 38:44-48.
3. Greenberg HS, Werness SA, Pugh JE, Andrus RO, Anderson DJ, Domino EF. 1994. “Short-term effects of smoking marijuana on balance in patients with multiple sclerosis and normal volunteers.” Clinical Pharmacology and Therapeutics 55:324-328.
4. Clifford DB. 1983. “Tetrahydrocannabinol for tremor in multiple sclerosis.” Annals of Neurology 13:669-671; Petro D and Ellenberger Jr C. 1981. “Treatment of human spasticity with delta-9-tetrahydrocannabinol.” Journal of Clinical Pharmacology 21:413S-416S; Ungerleider JT, Andrysiak TA, Fairbanks L, Ellison GW, Myers LW. 1987. “Delta-9-THC in the treatment of spasticity associated with multiple sclerosis.” Advances in Alcohol and Substance Abuse 7:39-50.
5. Clifford DB. 1983.
6. Ungerleider JT, et al. 1987.
7. Martyn CN, Illis LS, Thom J. 1995. “Nabilone treatment of multiple sclerosis.” Lancet 345:579.









