7
Education and Training Programs
ABSTRACT. The committee used a variety of sources to assemble estimates of the annual number of master’s-level graduates in the four core occupational safety and health disciplines. Twenty-nine U.S. schools offer such degrees in the occupational safety field, and they graduate about 300 students annually. This number is extremely low, given the incidence of workplace injuries, but the apparent acceptability of baccalaureate degrees in safety (about 600 graduates annually) by employers limits the demand for master’s-level safety professionals. Less than 10 students per year are awarded doctoral degrees, a level low enough to threaten the future of academic departments of occupational safety. The committee’s best estimate of the annual production of master’s-level industrial hygienists is approximately 400, a volume probably consonant with employer demand in the industrial sector that has most commonly used them. Forty institutions offer occupational medicine residencies, and they annually produce about 90 graduates, a number that is probably insufficient for simple replacement of existing occupational medicine specialists. Attracting applicants is a large part of the problem, since the field draws heavily from established physicians, for whom return to full-time student status is not feasible. A similar situation exists in nursing, and 21 schools of nursing award only about 50 master’s-level degrees in occupational health nursing each year.
Curricula in all four OSH disciplines are predominantly technical and science based, with a physical sciences/engineering emphasis in safety and industrial hygiene, and a biological, health, and programmatic emphasis in nursing and medicine. National Institute for Occupational Safety and Health (NIOSH) training programs provide grants totaling approximately $10 million per year in support of OSH professional education, resulting in 300 to 400 master’s degrees (or completed residen-
cies) each year. Occupational medicine has been the recipient of the most funding, reflecting the high cost of postgraduate specialist training for licensed physicians. Industrial hygiene has followed closely, with occupational health nursing receiving about 55 percent of the funding received by occupational medicine, and occupational safety receiving about one-third of the funding received by occupational medicine. Because large numbers of small businesses do not employ OSH professionals, worker and manager training by the Occupational Safety and Health Administration (OSHA) and others is also reviewed. No degrees are associated with this training, which takes many forms, from simple handouts and videotape viewings to 1 to 2 weeks of classroom and hands-on instruction. An exhaustive survey was not attempted, but it is clear that tens of thousands of hours of worker training is done, largely in response to OSHA mandates.
The committee concludes that current problems in the education and training of OSH professionals include lack of sufficient emphasis on injury prevention, which is reflected most clearly in the very small number of doctoral-level graduates in occupational safety, limited support for students doing research in departments other than those that grant OSH degrees, and an inability to attract physicians and nurses to formal academic training in OSH. An existing problem likely to be exacerbated by the many changes under way in the work environment is the narrow focus on OSH personnel who primarily serve large, fixed-site manufacturing industries. A potential problem in responding to these changes in the future workplace is a lack of training in a number of areas of increasing importance. These areas include behavioral health, work organization, communication (especially risk communication), management, team learning, workforce diversity, information systems, prevention interventions, and evaluation methods. The committee also concludes that worker health and safety training, although abundant, is of unknown quality and efficacy and that manager training is rarely demanded, offered, or requested.
Any consideration of the future OSH workforce must include an analysis of the educational “pipeline” as it exists today. This chapter presents the best available estimates of both the number of OSH-related degrees being granted in the United States today and brief summaries of typical curricula. Because of the committee’s concerns about the many small businesses, now and in the future, that do not employ OSH professionals, the chapter also provides a brief review of some of the major sources of continuing education and training for workers and managers, with and without OSH-relevant degrees, who are responsible for worker health and safety.
RESEARCH TRAINING
The development of new knowledge and its timely application are as central to OSH as to all other fields of human endeavor. Because of the toll of illness and disease of occupational etiology, much of the funded research in the field has been of an applied nature, often associated with the toxicology, epidemiology, or control of exposures to particular chemical, physical, biological, and safety hazards. Historically, the budgets of NIOSH or the National Institute of Environmental Health Sciences (NIEHS) to fund occupationally oriented research have been very modest by National Institutes of Health (NIH) standards. In the last several years, NIOSH has been successful in increasing extramural research funding in OSH via collaboration with other federal agencies in its National Occupational Research Agenda activities. NIOSH and NIEHS, have also supported research students via the training grant mechanism with NIEHS focusing largely on the field of toxicology.
As noted in Chapter 2, research relevant to OSH is conducted in diverse settings in the academic, government, and private sectors. In some cases research is carried out from institutional bases identified with OSH and in many others, research is carried out from disciplinary units in, for example, biology, engineering, or psychology. In the academic setting, the numbers of students who carry out work relevant to OSH applications are sparse, as are opportunities for interdisciplinary cross-fertilization. Except for doctoral programs in the traditional OSH fields, this precludes eligibility for standard NIH-type categorical training grants. Hence, support for research students with OSH interests in other fields is largely through individual investigator-initiated research grants from NIOSH, NIEHS, or other NIH sources.
As has been documented elsewhere in this report, changes in the workforce (Chapter 3), workplace (Chapters 4 and 5), and the delivery of health care (Chapter 6) present new research challenges, many of which lie on the fringes of or are completely outside the traditional OSH disciplines. The intersection of the workers’ compensation system with managed care, the ethical challenges of managing the increasing ability to determine genetic susceptibility to workplace chemicals (Frank, 1999), and the quantification of the risk of musculoskeletal injury from repetitive tasks are current research topics only dimly perceived a decade ago. All require the deployment of new competencies into OSH research, and all illustrate the need to recruit a broader array of students to study these issues. In common with most research activities, it is difficult to predict from which approach the practical benefits will arise.
OCCUPATIONAL SAFETY PROGRAMS
According to the 1998 to 1999 College and University Survey conducted by the American Society of Safety Engineers (ASSE), 32 U.S. schools offer programs leading to a bachelor of science degree in safety (American Society of Safety Engineers, 1999). Thirteen more programs at 12 additional schools are reported to offer bachelor of science degrees in more general fields (e.g., applied science, industrial systems) with a concentration or option in safety. Bachelor’s degrees with a minor in safety, 2-year associate of arts and associate of science degrees in safety, and certificates in safety are offered by an additional 24 schools (universities, colleges, technical colleges, and community colleges). Graduate degrees in safety are offered by 31 U.S. universities. Twenty-nine of these schools offer master of arts, master of science, or master of public health degrees, and nine advertise programs that lead to a Ph.D. or doctorate in public health.
As noted in Chapter 2, only seven schools offer programs accredited by the Accreditation Board for Engineering and Technology (ABET). ABET offers accreditation of programs awarding master of science and bachelor of science degrees, but only six Bachelor of Science programs and four Master of Science programs have been accredited to date. ABET does not accredit doctoral programs in safety.
During the summer of 1999 ASSE attempted to collect further information on schools that offer safety-related degrees and solicited historical data on their graduates and faculty. Figure 7-1 shows the numbers and types of degrees awarded by the 54 responding schools (73 programs) since 1990.
The ASSE survey also asked the schools to provide some estimate of the proportion of graduates employed in safety positions. Over the last 5 years, these estimates were fairly steady at about 60 to 70 percent for graduates with associate degrees, 45 to 55 percent for graduates with baccalaureate degrees, and 100 percent for recipients of doctorates. Employment in safety positions for master’s degree graduates has climbed steadily from 75 to 94 percent. These data, especially those for graduates with associates and bachelor’s degrees, should not be taken as reliable estimates of demand, since it is not clear how many were actually seeking employment in the safety field upon graduation, but they do indicate that some caution is in order in estimating supply from the number of graduates.
Perhaps the most worrisome aspect of all of these data is the small number of Ph.D.s being awarded. In only one year (1991) did Ph.D. recipients number exceed eight. Furthermore, analysis of limited data provided to the committee by NIOSH grantees showed only one dissertation in the
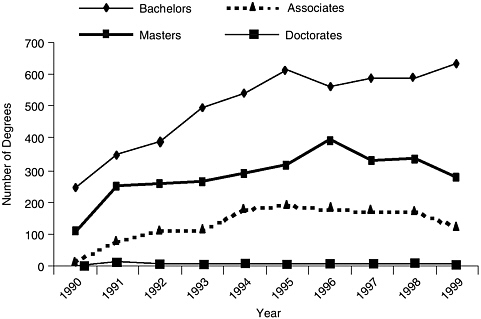
FIGURE 7-1 Number of degrees awarded from 1990 to 1999 by schools responding to ASSE survey on graduates. SOURCE: American Society of Safety Engineers (1999).
previous 5 years that focused on the traditional safety domain of acute traumatic injury prevention. Although few if any industries require safety professionals with doctorates, a critical mass of such individuals is necessary both for the conduct of critical research in injury prevention and for the continued viability of the academic programs that produce practicing safety professionals at the associate, bachelor’s, and master’s degree level.
Curricula
ASSE and the Board of Certified Safety Professionals (BCSP) have jointly published a series of curriculum standards that set forth the minimum academic requirements for both program accreditation and individual eligibility for attempting the Certified Safety Professional examination. The first of these (American Society of Safety Engineers and Board of Certified Safety Professionals, 1991) dealt with baccalaureate degrees, and subsequent efforts have addressed master’s degrees in safety (American Society of Safety Engineers and Board of Certified Safety Professionals, 1994a), safety engineering master’s degrees and safety engineering options in other engineering master’s degrees (American Society of Safety Engineers and Board of Certified Safety Professionals, 1994b), and associ-
ate degrees in safety (American Society of Safety Engineers and Board of Certified Safety Professionals, 1995). No standard for doctoral degree programs has been published.
Baccalaureate Degrees
The standards for baccalaureate-level programs call for at least 120 semester hours of study, 60 of which must be upper-level courses. At least 54 hours of these upper-level courses must be in safety professional courses, and must include 34 hours in “professional core” courses (these are listed below).
Essential “university studies” courses for aspiring safety professionals include courses in six broad subject areas:
-
mathematics and computer science (at least one semester each of calculus, statistics, and information processing);
-
physical, chemical, and life sciences (two semesters each of physics and chemistry, one semester of human anatomy, physiology, or biology, and, if possible, a semester of organic chemistry);
-
behavioral and social sciences and humanities (at least 15 hours, including a one-semester introduction to individual human behavior);
-
management and organizational science (a one-semester introduction to business or management, and a course on business law or engineering law);
-
communication and language arts (one-semester courses in each of rhetoric and composition, speech, and technical writing); and
-
basic technology and industrial processes (applied mechanics, manufacturing processes).
“Professional core” courses are required to develop the basic knowledge and skills specific to the safety field. Subjects to be included are
-
introduction to safety and health,
-
safety and health program management,
-
design of engineering hazard control,
-
industrial hygiene and toxicology (often a series of courses),
-
fire protection,
-
ergonomics,
-
environmental safety and health,
-
system safety and other analytical methods, and
-
an internship or cooperative course at an off-campus work site with a significant hazard control program.
“Required professional subjects” are important topics that may be covered by less than a full course:
-
measurement of safety performance,
-
accident and incident investigations,
-
behavioral aspects of safety,
-
product safety,
-
construction safety, and
-
education and training methods for safety.
The standards conclude with a list of safety elective courses in safety that range from those that are very industry specific (safety in the oil and gas industries) to those that are very general (public policy in safety and simulation and modeling in safety). The list is not definitive, however, and the only requirement is that the program include a number of electives, both general and safety related.
Master’s Degrees in Safety
The authors of these standards recognize that there are two large groups of candidates for master’s degrees: those who have undergraduate degrees in safety for whom the master’s degree in safety is advanced study and those who have trained in a discipline other than safety for whom the master’s degree in safety is initial preparation for a career in safety.
General criteria include a baccalaureate degree with a course structure very similar to that outlined above but allow courses in safety-related subjects such as risk management, industrial psychology, hazardous materials management, and quality control as substitutes for safety courses. Graduate study itself must include a minimum of 30 semester hours of study in a program significantly more specialized and advanced than baccalaureate programs. At least 20 hours must be devoted to safety science and safety professional practice, and the program should provide students with opportunities for participation in internships, field studies, research projects, and other interactive experience. A thesis is not strictly required, but programs without a thesis will be accredited only with a very convincing argument that it is impossible or impractical.
Specific course requirements are very similar to those for baccalaureate safety degrees described above for “professional core” courses.
Safety Engineering Master’s Degrees or Engineering Master’s with a Safety Option
Standards for safety engineering master’s degrees are nearly identical to those for the master’s degree in safety, except that the candidate must hold a baccalaureate degree from an ABET-accredited engineering program or must meet ABET equivalency requirements. To be recognized as a safety or safety engineering option (concentration or specialty are common synonyms) in another engineering master’s degree program, a minimum of 9 semester hours in professional core courses must be included.
Associate Degrees in Safety
The standard for associates degrees in safety, which is primarily relevant to 2-year programs at community or technical colleges, is designed to help individual students prepare for either entry into the workforce as a safety technologist or technician or transfer to a 4-year accredited safety degree program. The standard thus has two tracks: one for transfer programs (i.e., for students who intend to go on to a 4-yr college for a baccalaureate degree in safety) and one for terminal programs (i.e., for students who intend on entering the safety workforce immediately).
Transfer programs give primary emphasis to building a solid foundation for upper level safety courses. The standard therefore calls for most of the university studies specified above for the baccalaureate degree standard and calls for only a limited array of safety courses (6 semester hours). The latter must include an introduction to safety and health, and the standard suggests fire protection, safety and health program management, and design of hazard controls as top choices for additional safety courses.
Terminal programs prepare students for entry-level positions as safety technicians or safety technologists. They emphasize applied knowledge of safety practices, safety laws and regulations, and accepted methods and procedures. The standard therefore calls for fewer hours of foundation subjects (math; physical, life, and behavioral sciences; business management; communication; and industrial processes) and more core and elective safety courses (27 semester hours). Included among the latter should be one industry-specific course (construction, transportation, forestry, chemistry, etc.).
Continuing Education
As noted in Chapter 2, certification is valid for only 5 years, at which point Certified Safety Professionals must provide BCSP with evidence of
participation in professional development activities. Acceptable “continuation of certification” activities include membership in professional safety organizations, committee service for such organizations, and publications and papers but also include professional development, continuing education, and college courses. Although college courses must be taken at institutions accredited by the Council on Higher Education Accreditation, most safety-related professional development and continuing education courses sponsored by recognized organizations and many local, regional, and employer-sponsored conferences and courses are acceptable. Home study courses are acceptable if they award continuing education units or college credits or meet the standards of the Accrediting Commission of the Distance Education and Training Council. “Safety-related” is defined by BCSP as subjects that are included in the Certified Safety Professional examinations. No attempt was made to estimate the total number of such courses, or the number of students who take them each year, but some information of this sort is provided later in the chapter for several of the most prominent sources of such training, including NIOSH and other federal agencies. Additional information on distance education and training is presented in Chapter 8.
Future Needs
A major current need that is likely to become critical within the next decade if it is not remedied is the shortage of classically trained doctorallevel safety professionals. Of the 6.1 million nonfatal injuries and illnesses reported by employers in 1997, 5.7 million were injuries that resulted in lost work time, medical treatment beyond first aid, loss of consciousness, restriction of duties, or transfer to another job (Bureau of Labor Statistics, 1998a). However, as described in a subsequent section of this chapter, NIOSH funding for education of safety professionals is only about one-third of that for occupational medicine physicians and industrial hygienists and about two-thirds of that for occupational health nurses. Although the majority of safety professionals function quite well with a mixture of formal education at the baccalaureate or master’s level, continuing education, and on-the-job experience, a continuing stream of such individuals depends upon a dwindling cadre of Ph.D. scientist-educators. Academic departments need a critical mass to attract both research funding and interested students, so special attention should be given to means of recruiting graduate-level faculty to teach and conduct research in this area. Possible approaches include grant support for regional occupational injury prevention centers similar to those supported by Centers for Disease Control and Prevention’s National Center for [home and recreational] Injury Prevention and Control. The centers approach is especially attrac-
tive because of their inclusiveness: they can draw upon and support faculty and students from a wide variety of academic departments, an important attribute in a field as broad as safety.
INDUSTRIAL HYGIENE PROGRAMS
As indicated in Chapter 2, the most common academic degree for industrial hygienists is the master’s degree, either a Master of Public Health degree with a specialization in industrial hygiene, or a Master of Science degree. The latter are often offered by departments of engineering, chemistry, environmental science, or other departments not readily identifiable as sources of industrial hygiene education. Perhaps for that reason estimates of the number of programs that offer degrees in industrial hygiene range from 40 to 50 (Peterson, 1999) to over 60 (Whitehead and West, 1997). The ASSE 1998 to 1999 College and University Survey identified 54 such institutions. What is known with certainty is that there are ABET-accredited baccalaureate programs at 5 U.S. institutions and ABET-accredited master’s programs at 26 (Accreditation Board for Engineering and Technology, 1999). Of the latter, 21 programs receive NIOSH support. They have awarded an average of 210 master’s degrees per year over the last 5 years. Including an estimate of graduates from nonaccredited programs yields an annual production of 400 to 600 master’s-level industrial hygienists. A realistic estimate would be near the lower end of that range—400 per year. That would be consistent with the steady 300-per-year increase in Certified Industrial Hygienist (CIH) certificates awarded since 1980.
Curricula
The Related Accreditation Commission of ABET, with the assistance of the American Academy of Industrial Hygienists, provides a moderately detailed description of the required curricula for “industrial hygiene and similarly named engineering-related programs.” Master’s programs entail a minimum of 30 semester hours of interdisciplinary instruction and include special projects, research, and a thesis or internship. Research capability, management skills, and government relationships may be the subjects of special emphasis. A minimum of 18 semester hours must be devoted to industrial hygiene sciences and industrial hygiene practice. Epidemiology and biostatistics are examples of the former, which ABET defines as extensions of basic science or mathematics to industrial hygiene. Courses on industrial hygiene practice apply industrial hygiene sciences to specific societal needs and require open-form problem solving, cost and ethical considerations, and independent judgment in inte-
grating specialty areas into professional service. Control of physical and chemical hazards, environmental health, and occupational safety are listed as typical topics. The remaining 12 “unspecified” hours allow further specialization. Common topics are public health, environmental law, and management techniques.
In practice, a typical master’s program might involve the following courses:
-
introduction to industrial hygiene,
-
introduction to safety,
-
introduction to occupational health,
-
biostatistics and epidemiology,
-
toxicology,
-
chemical hazards,
-
physical hazards (including radiation),
-
exposure assessment (with an industrial hygiene laboratory),
-
engineering controls,
-
legal and regulatory issues in occupational health and safety,
-
introduction to ergonomics,
-
internship, and
-
a project or thesis.
Continuing Education
As indicated in Chapter 2, continuing education plays a large role in the training of professional industrial hygienists. Not only is annual participation a requirement for maintaining certification but it has also been the primary means of entry into the field for those unable to devote several years to graduate education and the most common introduction to industrial hygiene for worker and management personnel with responsibility for health and safety in medium-sized to large firms. The American Industrial Hygiene Association, the American Conference of Government Industrial Hygienists, the NIOSH Education and Research Centers and other universities that offer degrees in industrial hygiene and a myriad of private firms offer American Board of Industrial Hygiene (ABIH)-approved courses. A full accounting is beyond the committee’s resources, but in academic year 1996–1997, for example, programs supported by NIOSH alone offered a total of 234 courses to 5,621 people throughout the country.
Future Needs
Whitehead and West (1997) conducted the only quantitative study of
future demand for ABIH-certified industrial hygienists and the ability of current training programs to meet that demand. Their predictions of demand involved application of the current industrial hygienist/worker ratios to the numbers of workers projected for each Standard Industrial Code in 2005 by the Bureau of Labor Statistics. A more elaborate model used a straight-line extrapolation of the upward trend in the industrial hygienist/worker ratio between 1989 and 1995 to the year 2005. Their conclusion was the same in both models: current training capacity is probably adequate to meet the requirements generated by the models. However, it is clear that the changes in work and the workforce documented earlier in this report (see Chapters 3 through 5) demand increased flexibility and innovation in the industrial hygiene curriculum, even for those destined for employment in traditional industrial hygiene positions with medium-sized to large industrial sector employers. Although the core competencies driving graduate training programs must continue to be based in the natural sciences, there are clear needs for these professionals to gain an understanding of:
-
organization, operation, and management in the economic sectors in which they operate;
-
the behavioral and psychosocial factors that affect worker health and safety; and
-
methods for and approaches to the education and training of both workers and managers.
It is not clear that this material can simply be added to the existing curricula, given the constraints of time and accreditation standards, although there is a continuing need to reevaluate both curriculum content and accreditation requirements. An alternative means of encouraging a broader skill set is through modifications in the CIH certification examination or more structured continuing education requirements for certification maintenance.
The most important issue, however, was raised in Chapter 2, and that is that the need for industrial hygienists is much greater than the demand. This assertion is based, first, on the argument that because industrial hygienists and other OSH professionals are hired almost exclusively by medium-sized to large industries, much less than half of the current workforce ever interacts with an OSH professional of any sort, and probably less of the future workforce ever will do so. Second, even within the traditional areas of OSH practice, there has always been a tendency to integrate and merge technical and managerial functions, which can result in assigning industrial hygiene responsibilities to people with administrative and managerial skills instead of scientific and technical skills. The
current trend toward outsourcing industrial hygiene services is another trend that separates the preventive aspects of the hygienist’s role from both workers and workplace decision makers.
The issue facing educators over the next decade is therefore not how to produce more of the same or even similar numbers of slightly different industrial hygienists but how to continue providing the current level of supply while developing a new model of industrial hygiene practice appropriate for small, service-oriented, multisite businesses and their diverse and transient employees.
OCCUPATIONAL MEDICINE RESIDENCIES
As of January 1999, 40 institutions offered occupational medicine residency programs (American College of Preventive Medicine, 1999; Carol O’Neill, American College of Preventive Medicine, personal communication, June 4, 1999). These programs, which are distributed throughout the United States, provide 86 positions for the academic year and 95 positions for the practicum year. Some programs combine the academic and practicum years, but the net result is approximately 90 graduates per year. Data presented below in the section on NIOSH-supported programs indicate that NIOSH provides support to approximately 50 residents annually, so it is clear that such support plays a large role in ensuring the supply of occupational medicine physicians.
Some residencies are in schools of public health and others are in hospitals. The Institute of Medicine (IOM) has issued a report about incorporating the environmental and occupational medicine theme into the medical school curriculum (Pope and Rall, 1995; Goldman et al., 1999), but with less than 25 percent of all medical schools offering an occupational medicine residency program, such incorporation would appear to be difficult for the majority of medical schools in the United States. Medical schools without training programs are less likely to have faculty members knowledgeable in an area than are medical schools with such training programs. Further, not all of these 40 institutions offering occupational medicine residencies are medical schools.
A possible alternative to traditional residencies is suggested by an innovative distance learning program offered by the Medical College of Wisconsin, which provides the required academic program and a Master of Public Health (MPH) degree to physicians by means of a self-paced, computer-based curriculum that requires students on campus only for orientation and graduation. The program, which graduated its first students with an MPH degree in 1988, is almost entirely on-line. The mechanics of the program are discussed in the next chapter, but as of June 1999 the program had graduated 347 students (48 in June 1999) and had
250 students currently taking one of the ten 4-month courses required (Greaves, 1999).
Students from this program have a very favorable rate of passing the American Board of Preventive Medicine board examination. In 1997, for example, 92.5 percent of the graduates of the Wisconsin program passed the examination whereas 80 percent of conventional residency graduates and 61 percent for physicians without residency training who were eligible for the examination via the equivalency route passed the examination. In each of the past 3 years, approximately one-quarter of all physicians who have become board certified in occupational medicine had taken at least one course from the Medical College of Wisconsin Master of Public Health program.
Curricula
As noted in the Chapter 2, a residency entails successful completion of three separate phases of training: a clinical year, an academic year, and a practicum year. The following description of the content of those phases follows very closely that of the Residency Review Committee (RRC) of the Accreditation Council for Graduate Medical Education (ACGME).
The clinical phase, formerly called an “internship,” constitutes a graduate year of clinical education and experience in direct patient care. It must provide broad experience in direct patient care, including ambulatory and inpatient hospital experience, for example, family practice, pediatrics, internal medicine, and obstetrics and gynecology, or in a transitional year; and it must be completed before the start of the practicum phase. The curriculum generally includes at least 3 months of hospital experience in internal medicine. A balanced program of outpatient and inpatient care, including pediatrics, obstetrics and gynecology, and emergency medicine, provides a broad range of exposure to other types of patients.
The academic phase consists of a course of study that leads to the Master of Public Health or equivalent degree in an institution accredited by a nationally recognized accreditation agency. The course of study requires a minimum of 1 full academic year or its equivalent, as determined by RRC. The resident who is in a degree-granting institution must meet all requirements for the degree. When no degree is granted, a postbaccalaureate curriculum of content, depth, and rigor equivalent to a degree program may be acceptable, provided that the curriculum is approved by an appropriate body, such as the graduate school or academic senate of an institution accredited by a nationally recognized accreditation agency. The required course work must include biostatistics, epidemiology, health services organization and administration, environmental and occupa-
tional health, and social and behavioral influences on health. In addition, adequate opportunities should be available for the resident to participate in research activities appropriate to the chosen field of education.
The practicum phase is a year of continued learning and supervised application of the knowledge, skills, and attitudes of preventive medicine in the field. The purpose of this phase is to prepare the resident for the comprehensive practice of occupational medicine and therefore must provide opportunities for the resident to deal with clinical, scientific, social, legal, and administrative issues from the perspectives of workers and their representatives, employers, and regulatory or legal authorities. For at least 4 months the resident engages in supervised practice within the real world of work. Through interaction with occupational health personnel, workers, human resources and industrial relations personnel, line supervisors, worker representatives, and the medical community, the resident must gain experience in the clinical and administrative aspects of direct worker care and job assignment, medical screening and surveillance, health conservation and promotion, environmental assessment, employee assistance, and relevant regulatory compliance.
Appropriate practicum opportunities may be found in a variety of settings. Suitable sites may include firms involved with heavy and light manufacturing; the utility, service, and transportation sectors; and clinics that provide comprehensive services to workers and employers. Although diagnostic and referral clinics that specialize in occupational disease can have a vital role in the education of residents, they do not afford the broad practicum opportunities specified above. This experience need not be obtained at a single site, nor must the experience be received in a single 4-month block. However, sufficient sustained attendance at each facility must occur to permit the assumption of significant clinical and administrative responsibility.
The content of the practicum phase is supposed to offer clinical, administrative, and didactic components in settings in which there are well-organized programs appropriate to the particular field of preventive medicine and supervised application of the knowledge, skills, and attitudes of preventive medicine gained in the academic phase and in the didactic component of the practicum phase.
A didactic component can include structured lectures, journal clubs, symposia, and other activities that focus on:
-
physiological responses to heat, pressure, noise, and other physical stresses;
-
the diagnosis, prevention, and treatment of occupational disease;
-
toxicology and risk assessment;
-
industrial hygiene instrumentation and basic environmental control measures;
-
behavioral factors in accident causation and control and medical support of accident investigations;
-
ergonomics;
-
determining fitness to work, placement of workers, and adaptations of work to accommodate handicaps;
-
employee assistance programs;
-
health education and health promotion; and
-
occupational health data management and analysis.
The clinical component shall include but not be limited to:
-
clinical care of workers in the prevention, diagnosis, treatment, and rehabilitation of work-related disorders;
-
evaluation of the fitness of workers for normal or modified job assignments in a wide variety of work environments and the assessment of impairment and disability; and
-
counseling and education of workers and supervisors with respect to work or environmental hazards, health-related habits of living, and the arrangements of work.
Finally, an administrative component shall provide the resident with opportunities for management responsibilities and shall include but not be limited to each of the following topics:
-
the planning, administration, supervision, and evaluation of a broad program for the protection and promotion of the health and safety of workers in the work setting, including health risk assessment, accident evaluation, and risk reduction;
-
application of administrative and scientific principles to achieve compliance with regulatory requirements and the requirements of workers’ compensation plans; and
-
acquisition, collation, storage, and analysis of health and environmental data.
Continuing Education
Occupational medicine physicians, like all physicians, are required to participate in a certain amount of continuing medical education to keep their medical licenses. In addition, as described earlier in Chapter 2, physicians who become board certified in occupational medicine in or after
1998 must be recertified every 10 years, in part on the basis of continuing education credits.
During 1998 the American College of Occupational and Environmental Medicine (ACOEM) sponsored 26 educational opportunities that reached more than 4,200 participants, and jointly sponsored more than 100 other educational activities, live and via distance leaning (American College of Occupational and Environmental Medicine, 1999b). ACOEM’s two conferences each year—in the spring and fall—provide courses, classes, and presentations at which physicians can obtain continuing education credits. Typical offerings are full-day postgraduate seminars on such topics as myofascial pain syndrome, silica toxicology, occupational skin diseases, and travel medicine, along with medicolegal testimony and occupational medicine self-assessment review. ACOEM also offers professional development courses at other locations and dates. The 1999 courses were Impairment and Disability Evaluation, Medical Review Officer Training, and Occupational Medicine Board Review. The component organizations (regional occupational medicine organizations) also provide continuing education activities with annual or periodic conferences. A survey of ACOEM members (The Gary Siegal Organization, Inc., 1996) found that 75 percent of respondents indicated that they had received some funding for continuing education in 1996. Of those who did, 32 percent received $1,500 or less, 44 percent received between $1,500 and $3,000, and 24 percent received more than $3,000.
Many of the university programs provide 1- to 3-hour long continuing education activities at weekly, fortnightly, or monthly conferences. Universities also offer a regular catalog of 1–3 day conferences or courses on specific areas. Among these varied venues a sufficient number of continuing education activities appear to be available for all physicians both to keep them current and to fulfill their requirements for licensure and recertification.
Future Needs
According to a former president of ACOEM (Anstadt, 1999), the number of graduates from residency programs is insufficient to meet the current and future demands for occupational medicine physicians. The supply is below the numbers needed for replacement of existing occupational medicine physicians. The occupational medicine residencies report difficulties in the following areas:
-
attracting sufficient number of applicants,
-
funding the residents, especially for the academic year, and
-
having sufficient numbers in some programs to constitute a critical mass.
The barriers to attracting potential residents to residencies include the following:
-
Residencies cost institutions $30,000 to $40,000 per year, and unlike more clinically oriented residency programs, occupational medicine residents have relatively little direct patient contact to generate funds.
-
Physicians who anticipate doing nearly 100 percent outpatient clinical activities (the recent trend in occupational medicine) see less value in occupational medicine residency; thus, the supply of future residents may actually decrease.
-
Most importantly, many physicians become interested in occupational medicine some years after graduation from medical school. Pearson and colleagues (1988) surveyed a random sample of preventive medicine specialists and found that of 166 self-identified occupational medicine specialists, 86 percent had entered the field after one or two career changes and 51 percent were 44 years of age or older. Return to full-time student status in an occupational medicine residency is not an attractive option for this population.
The Occupational Physicians Scholarship Fund, an independent organization founded and directed by occupational medicine physicians from both academia and a wide variety of industries, has been successful in providing funding for some residents. However, because of financial limitations, the number of residents that can be supported is limited. To date the fund has provided 122 scholarships to 84 individuals. By the year 2011 the total number of scholarships is expected to be 250. The fund averages 45 applicants per year. Clearly, not all applicants are able to receive funding (Bronstein, 1998). An attractive option is the more widespread use of distance education like that conducted by the Medical College of Wisconsin. This is explored further in Chapter 8, but it addresses only the academic year of residency. The practicum year remains a serious obstacle for most established physicians. A more comprehensive solution requires reexamination of the current pathways to certification in occupational medicine, a major recommendation of the 1991 IOM Committee Addressing the Physician Shortage in Occupational and Environmental Medicine (Institute of Medicine, 1991). That study suggested exploring the possibility of offering certificates of added qualification to physicians who are board certified in internal medicine or family practice and who also have advanced training or experience in occupational medicine (a certificate for added qualification in geriatric medicine is already available). The IOM study also suggested modifying the current pathway to dual certification (internal medicine and occupational medicine) by allowing a year of occupational medicine practice in place of a practicum year. The current IOM committee believes that these ideas should be
explored again. An even simpler alternative would be for the American Board of Preventive Medicine to eliminate the restriction of its existing equivalency (experience) pathway to physicians who graduated before 1985.
OCCUPATIONAL HEALTH NURSING PROGRAMS
As noted in Chapter 2, occupational health nursing programs are a specialty focus generally offered at the graduate level. The American Association of Occupational Health Nurses has identified a total of 21 programs that offer graduate degrees in occupational health nursing. Together they produce about 50 graduates annually. This is accomplished primarily through funding from NIOSH Education and Research Centers and Training Program Grants. These programs may be in schools of public health or schools of nursing offering both master’s and doctoral degree programs. In addition, a few non-NIOSH-funded schools of nursing across the country offer occupational health nursing graduate programs.
Accreditation for all of these programs is provided by the National League for Nursing (NLN) or the Council on Education in Public Health (CEPH). Occupational health nurses work in industry, manage clinics, develop corporate occupational policies, and design and implement health promotion, disease prevention, and health surveillance programs for employees. Although there is no set standard for a program of study for occupational health nursing, the programs offered follow guides set forth by NIOSH and the school discipline accreditation bodies (i.e., NLN and CEPH), with an emphasis on interdisciplinary learning.
Curricula
In general nurses receiving a master’s degree in public health with an occupational health nursing focus take courses with content in public health sciences, occupational health sciences, and occupational health nursing and often have a practicum experience. The public health science course work includes epidemiology, biostatistics, environmental sciences, health administration, and behavioral sciences. Epidemiology provides a foundation for recognizing trends in occupational illness and injury; biostatistics is important in the planning, coordination, and analysis of research; course work in environmental sciences introduces basic concepts of environmental health and recognition of environmental hazards (e.g., air and water pollution, food safety, hazardous substance exposure, and environmental policy and management); course work in health policy and administration focuses on organizational and human resources management; and course work in behavioral science provides an understand-
ing of human behavior and motivational theory and how they relate to health choices. Course work in the occupational health sciences typically covers safety and ergonomics, occupational health, toxicology, and industrial hygiene. Each of these courses provides an introduction to the basic concepts and principles of each discipline. In addition, a framework for interdisciplinary collaboration is enhanced through joint field experiences, workplace walkthroughs, and occupational health problem-solving assignments and seminars. The goal of occupational health nursing content is to have a better understanding of means of assessing of worker and workforce illnesses and injuries as well as a better understanding of health promotion and protection concepts and principles so that effective intervention and prevention strategies can be designed and evaluated to improve worker health and safety and working conditions. Role function and leadership concepts and principles are emphasized.
Field praticum experiences that offer learning opportunities not available in the classroom may be provided. The purpose and potential benefits are to relate theoretical classroom learning to practice situations; gain experience, skills, and confidence in dealing with administrative, educational, and service problems; explore and have an increased understanding of the structure and dynamics (e.g., agency objectives, goals, values, resources, and constraints) of a specific work setting; and identify problems for intervention, prevention, and evaluation. Completion of a master’s paper specific to occupational health and safety and, often, a comprehensive examination of the subject matter conclude the program of study.
A master’s degree in nursing with an occupational health focus is another degree option. It can often have either a management and administration focus or a nurse practitioner focus. The management and administration focus offers course work in nursing administration, financial management, informatics, and management principles applied to the occupational health setting. The nurse practitioner focus offers course work on the theory and practice of adult health maintenance and the assessment and management of common ailments facing working adults. Clinical residencies in specialty clinics and occupational health settings with experts in the field are provided.
In addition to course work in the occupational health sciences, course work may include such topics as advanced physiology and pathology, pharmacology and therapeutics, diagnostic processes, occupational health management principles, and primary care. Practicum experiences relevant to the specialty and nursing role function, research, and a thesis may also be included.
Several programs are offered in occupational health nursing at the doctoral level. Preparation is designed to prepare nurse researchers who
can design studies to address researchable problems in occupational health and safety.
More recently, there has been increasing emphasis in offering graduate occupational health nursing programs in nontraditional formats, such as through distance learning or weekend education. With technological advancements occurring on a daily basis, this type of educational format will grow. These options allow students to take course work through the Internet, or independent study with limited on-campus time or through programs of study offered on campus but in a periodic weekend format.
Continuing Education
Mandatory nursing continuing education varies with state. However to be eligible for optional certification in occupational health nursing and renewal of that certification in 5-year increments, a minimum of 75 continuing education contact hours must be posted within the 5-year period prior to certification and recertification.
Occupational health nurses can obtain continuing education from numerous sources. The professional association for occupational health nurses, AAOHN and its 180 chapters across the nation, provide ample avenues for attainment of continuing education. For example, at the 1999 American Occupational Health Conference, AAOHN offered more than 130 continuing education courses for participants. In addition, universities, particularly those with occupational health and safety programs such as the NIOSH Education and Research Centers, provide seminars, workshops, conferences, and courses to meet the learning needs of the professional occupational health nurse.
Future Needs
The major shortfall in the occupational health nursing field is the same as that of the occupational medicine field; that is, there is not so much a shortage of practitioners as there is a shortage of practitioners with formal training in the field. The barriers to the production of more master’s-level occupational health nurses are also similar to those that inhibit potential occupational medicine residents, especially the reluctance of mid-career professionals to return to full-time student status for 2 years. As with occupational medicine residents, the key to increasing the supply of master’s-level occupational health nurses lies in more accessible educational programs and financial assistance to achieve degree completion.
21ST CENTURY KNOWLEDGE AND EXPERTISE
As is evident from the preceding review of typical curricula in each of the traditional OSH professions, the curriculum for each profession is firmly anchored in the natural sciences, provides a challenging educational experience, and for those who complete it, provides a solid technical preparation for entry-level OSH professionals. Nevertheless, as noted in the section on industrial hygienists, the many changes in the world of the U.S. worker documented in earlier chapters of this report appear to demand knowledge and expertise from all OSH professionals in still more areas. Behavioral health, work organization, communication (especially risk communication), management, team learning, workforce diversity, information systems, prevention interventions, and evaluation methods are some of the most important. To this list one might add methods for effective training of adult workers, the physical and psychological vulnerabilities of members of the workforce by age, gender, and socioeconomic and cultural background; the resources available for help with accident prevention and analysis; business economics and values; health promotion and disease prevention; community and environmental concerns, and the ethical implications of technological advances such as the mapping of the human genome (as well as the dual responsibilities of OSH professionals to workers and employers generally). Physicians, nurses, and other OSH healthcare professionals must be exposed to managed care and team health care delivery during their training, and need a solid grasp of health care financing and its effects on workers’ compensation if they are to maximize their benefit to workers and employers. The use of multidisciplinary teams is one way of providing for all the requisite knowledge, skills, and abilities, but individual professionals must be familiar enough with these areas to know when and where to turn for help.
Simply adding courses in these areas to the curriculum is not feasible because adding months or years to any of these programs is likely to have a strong negative effect on the attractiveness of the programs to prospective students. Substitutions for areas currently in the curriculum will also be difficult because accreditation requirements dictate the current curricula and credentialing examinations reflect much of the current curricula. Academic accreditation bodies should periodically conduct comprehensive evaluations of the training programs that they judge, including empirical measures of graduates’ satisfaction and success, paying special attention to the emerging needs listed here, and altering requirements (or standards) accordingly. Credentialing bodies, which generally dictate continuing education requirements, could use that mechanism to ensure that their technically trained members stay truly current as well.
FUNDING SOURCES FOR OCCUPATIONAL SAFETY AND HEALTH EDUCATION AND TRAINING
The remainder of this chapter describes the current sources, nature, and extent of support for OSH education and training in both the public sector and, less comprehensively, the private sector, beginning with NIOSH, the major source of funding for graduate education in the traditional OSH professions. Because of the committee’s previously noted concern for the large segment of the American workforce that does not typically come in contact with these OSH professionals, subsequent sections describe current sources of funding for continuing education and worker and employer training.
NIOSH Education and Training Programs
NIOSH awards 1- to 5-year training program grants (TPG) and Education and Research Center (ERC) training grants to support educational programs in the fields of industrial hygiene, occupational health nursing, occupational medicine, occupational safety, and other specialized OSH training areas. The objective of this grant program is to award funds to eligible institutions or agencies to assist in providing an adequate supply of qualified professional and paraprofessional OSH personnel to carry out the purposes of the Occupational Safety and Health Act. Any public or private educational or training agency or institution that has demonstrated competency in the occupational safety and health field and that is located in a state, the District of Columbia, or U.S. Territory is eligible to apply for a training grant. NIOSH supports both short-term continuing education courses for OSH professionals and others with worker safety and health responsibilities and also academic degree programs and postgraduate research opportunities in the areas of occupational medicine, occupational health nursing, industrial hygiene, and occupational safety. Appendix D contains a list of the 1999 grant holders, and Figure 7-2 displays the funding for each of these four disciplines between 1995 and 1999. The “other OSH” category includes graduates from academic departments with dual names, e.g., Industrial Hygiene and Safety, Occupational Health and Safety, and Environmental and Occupational Health, and occasional graduates in related fields such as epidemiology and toxicology. (See Chapter 2 for a brief description of a new program to stimulate curriculum development on occupational health psychology.) Occupational medicine has been the recipient of the most funding, reflecting the high cost of postgraduate specialist training for licensed physicians. Industrial hygiene has followed closely, with occupational health nursing, at about 55 percent of occupational medicine, and occupational safety,
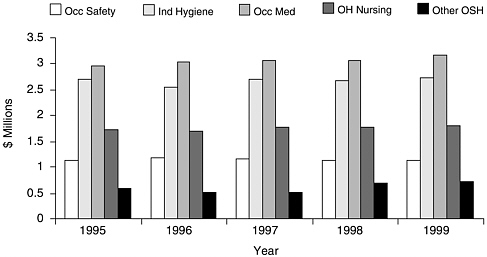
FIGURE 7-2 Funding, by discipline, by NIOSH of ERCs and TPGs, 1995 to 1999. Abbreviations: Occ, occupational; Ind, industrial; OH, occupational health; OSH, occupational safety and health. SOURCE: Susan Board, National Institute for Occupational Safety and Health, personal communication, November 29, 1999.
receiving about one-third of the amount received by occupational medicine. This pattern has been very steady over the 5 years for which the committee has data. The following sections provide information on the products of this spending.
Degree Programs
OSH programs take a variety of forms across the myriad of industries and businesses of the United States, and the educational backgrounds of those who supervise, conduct, and participate in them vary widely as well. This chapter, like Chapter 2, focuses on the four traditional OSH disciplines—occupational medicine, occupational health nursing, industrial hygiene, and occupational safety. As noted in Chapter 2, a large proportion of professionals in these fields have formal education beyond the baccalaureate. A master’s degree is common for practitioners, and a doctorate is almost a requirement for teaching and research (in the case of occupational medicine, these degrees follow receipt of a medical degree and completion of a clinical residency). Figure 7-3 shows the number of master’s degrees awarded in each of the traditional OSH fields by NIOSH-supported programs for each year between 1987 and 1997. The totals include graduates supported by either TPGs or ERC grants.
Industrial hygienists have clearly been the leading recipients of
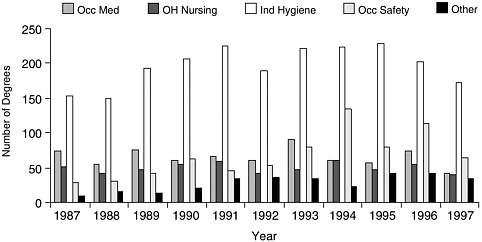
FIGURE 7-3 Master’s degrees awarded with support of NIOSH training programs, 1987 to 1997. Occ, occupational. SOURCES: National Institute for Occupational Safety and Health (1988, 1989, 1990, 1991, 1992, 1993, 1994, 1995, 1996, 1997a, 1998b).
NIOSH support for master’s-level education during the past decade, but Figure 7-3 does not fully represent the extent of NIOSH support for physicians. Most, if not all, of the master’s degrees in occupational medicine represented in Figure 7-3 were awarded to physicians who were completing a residency, but not all institutions offering residencies in occupational medicine provide a degree as part of the process. The height of the occupational medicine bars in Figure 7-3 would be roughly doubled if physicians who successfully completed an occupational medicine residency that did not provide a master’s degree were included. Significantly fewer graduates come out of NIOSH-supported programs in Occupational Safety (about 70 annually) and Occupational Health Nursing (a little less than 50 per year).
As noted in the discussion of Figure 7-2, the “other OSH” category includes academic departments with dual names, for example, industrial hygiene and safety, occupational health and safety, and environmental and occupational health, as well as related fields such as epidemiology and toxicology. NIOSH support for the “other” category is also underrepresented in Figure 7-3, in that this is the only one of the five categories for which NIOSH provides support for undergraduate education. In fact, the vast majority of NIOSH-supported graduates in the “other” category are undergraduates receiving 2-year associate degrees or 4-year bachelor’s degrees (see Figure 7-4). A small number of additional students receive certificates, documenting the completion of approximately 30 credit hours in occupational safety and health.
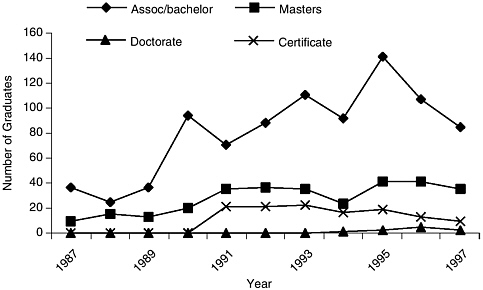
FIGURE 7-4 Graduates of “other” NIOSH-supported educational programs, 1987 to 1997. Assoc, associate degree. SOURCES: National Institute for Occupational Safety and Health (1988, 1989, 1990, 1991, 1992, 1993, 1994, 1995, 1996, 1997a, 1998b).
Continuing Education
In addition to formal degree programs, a wide variety of short courses on specific OSH topics is provided by colleges and universities affiliated with the NIOSH ERCs. Topics may be very general and widely applicable or may be specific to particular industries or businesses, and courses may be as short as a few hours to as long as a week or more. Many institutions provide instruction on the Internet or use other computer applications and off-campus sites to make the courses attractive and accessible to fulltime workers. These courses are not associated with a degree program and do not generally demand prerequisites. As is the case with short-term courses offered by OSHA and the Mine Safety and Health Administration (MSHA), trade unions, industry, and professional organizations, there is no universally recognized accreditation body and, hence, no guarantee of quality, nor is there generally any attempt to assess the efficacies of these courses.
Figure 7-5 shows the number and type of continuing education courses and student-days of continuing education instruction provided by NIOSH-supported ERCs and TPGs. Number of student-days is simply the sum of the product of the number of students and the duration of their course.
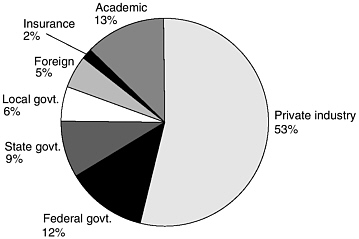
Students who attend these courses are most often employed by pri-
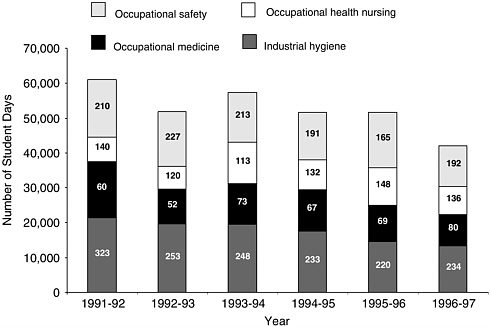
FIGURE 7-5 Student-days of continuing education and number of courses (inside the columns of the histogram) supported by NIOSH, 1991 to 1997. SOURCES: National Institute for Occupational Safety and Health (1988, 1989, 1990, 1991, 1992, 1993, 1994, 1995, 1996, 1997a, 1998b).
vate industry, but government at all levels and academic institutions send substantial numbers of employees as well. Figure 7-6 shows the categories of the employers of the 33,884 students who took NIOSH-supported continuing education courses in 1996-1997. The distributions in the previous years were very similar to those in 1996–1997.
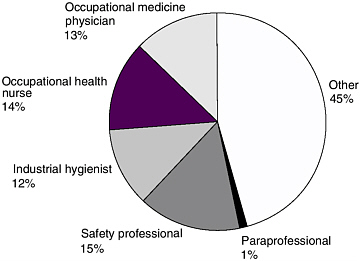
Not all of the students who took these continuing education courses were traditional OSH professionals. In fact, as Figure 7-7 shows, only about half the students who took NIOSH-supported continuing education courses in academic year 1996–1997 were safety professionals, industrial hygienists, occupational physicians, or occupational health nurses. A small number were clearly identified as paraprofessionals, that is, trained aides who assist a professional person, but about half were simply classified as “other.” Some of these students were certainly professionals from other OSH-related disciplines, but a large proportion was no doubt composed of managers, supervisors, and workers with some responsibility for providing or carrying out OSH programs and worker training at their workplaces.
OSHA-Supported Education and Training
Since the passage of the Occupational Safety and Health Act in 1970, NIOSH has been the primary federal agency supporting education and training of OSH professionals, but OSHA assumed responsibility for worker training and more than 100 OSHA regulations (standards) require worker training. Other OSHA standards make it the employer’s responsibility to limit certain job assignments to individuals who are “certified,” “competent,” or “qualified,” presumably by virtue of special previous training in or out of the workplace. A number of standards are quite explicit about what safe practices should be taught, but most are very general (“Methods shall be devised to train operators of powered industrial trucks”). OSHA has provided some voluntary guidelines to assist employers, but it has generally left the content and methods to employers.
A large number of private training entities offer training packages and videotapes to help employers meet these requirements, and OSHA itself has developed more than 80 short courses that it offers through its own facilities and that it makes available for use by others. The OSHA Office of Training and Education offers training and training programs to federal and state OSHA personnel, state consultants, other federal agency personnel, and private-sector employers and employees. This is accomplished through short-term training courses at the OSHA Training Institute in Illinois and 12 regional OSHA Training Institute Education Centers, the Susan Harwood Training Grants Program, and the train-the-trainer Outreach Grants Program.
OSHA Training Institute
OSHA Training Institute courses provide basic and advanced training and education in safety and health. Course subject matter emphasizes OSHA policies and standards as well as hazard recognition and hazard abatement techniques. Courses are designed to build a more effective workforce and to aid in professional development. The schedule contains courses for federal and state compliance officers, state consultants, other federal agency personnel, and private-sector employers, employees, and their representatives.
Approximately 80 different courses are offered, including 7-day overviews of OSHA standards for physicians and nurses and a 14-day course on criminal investigations for OSHA compliance officers. The modal course length is 4 to 5 days. More than 700 courses were taught in fiscal year 1998, and Figure 7-8 shows the extent of this instruction for the last 4 years for which data were available.
Continuing education units (CEUs) are available to participants in all

FIGURE 7-8 Student-days of instruction by OSHA Training Institute, all sites, in fiscal years 1995 to 1998. SOURCES: Office of Training and Education (1996, 1997, 1998).
courses conducted by OSHA Training Institute staff in accordance with the administrative and program criteria guidelines that have been established by the International Association for Continuing Education and Training. These CEUs also meet the criteria of the American Board for Occupational Health Nurses (ABOHN) for certification or recertification. Certification maintenance points are available to certified industrial hygienists who complete courses awarded points under the ABIH maintenance of certification program. All technical safety and health courses except the Collateral Duty Course for Other Federal Agencies meet Board of Certified Safety Professionals criteria for continuance of certification credit.
OSHA Training Institute Education Centers
In recent years the demand for OSHA Training Institute courses from the private sector and from other federal agencies has increased beyond the capabilities of the OSHA Training Institute. To address this increased demand for its courses, the OSHA Training Institute has established regional OSHA Training Institute Education Centers. These centers are nonprofit organizations that were selected after competitions for participation in the program. There are currently 12 centers nationwide, and each center offers 12 core OSHA Training Institute courses, generally on campus, but sometimes at other sites when demand is sufficient. Figure 7-9 shows that they clearly reach an audience different from that reached by the parent institute.
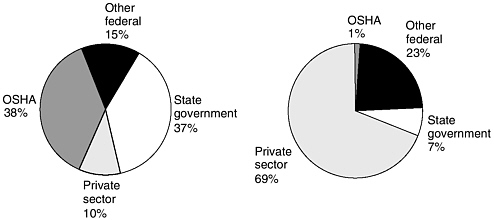
FIGURE 7-9 Source of fiscal year 1998 students for OSHA Training Institute (left) and OSHA Training Institute Education Centers (right). SOURCE: Office of Training and Education (1998).
Susan Harwood Training Grants Program
OSHA began a serious effort to increase and improve worker training in the late 1970s with a program called New Directions in which several million dollars in grants were given to unions and trade associations to develop training materials for workers and to provide training. A very large volume of training materials and training were generated from those initial grants. Many safety and health programs were started at unions and trade associations as a consequence of this seed money. The New Directions program ended in the early 1980s and was subsequently replaced by more targeted grant programs (e.g., programs targeted to certain hazards or hazardous industries) such as the Susan Harwood Training Grants Program.
The Susan Harwood Training Grants Program provides funds to nonprofit organizations to train workers and their employers to recognize and prevent safety and health hazards in their workplaces. It emphasizes three general areas: businesses with less than 250 employees, new OSHA standards, and OSHA-defined high-risk activities. Organizations that receive grants are expected to develop training programs that address a topic named by OSHA, recruit workers and employers for the training, and conduct the training. Awards have been made to safety and health organizations, employer associations, labor groups, educational institutions, and other nonprofit organizations. The competitive grants are for 12 months, although they may be renewed, and average about $100,000 (the grantees must contribute a minimum of 20 percent of the total project
TABLE 7-1 Subject Area and Number of Susan Harwood Training Grants Program Grants Awarded in Fiscal Year 1999
|
Subject Area |
No. of Grants |
|
Construction |
7 |
|
Ergonomics |
8 |
|
Food processing |
4 |
|
Logging |
3 |
|
Scaffolding |
4 |
|
Shipyard safety and health |
5 |
|
Silica in general industry |
2 |
|
Small businesses |
9 |
|
Worker outreach |
4 |
|
Workplace violence |
2 |
|
SOURCE: Occupational Safety and Health Administration (1999a). |
|
cost). The topics for grants can be broad ones that cut across many occupations or extremely narrow ones that focus on one kind of injury in one occupation, and they are specified each year in the application announcement. The subject areas for fiscal year 2000 awards are prevention of amputations in manufacturing, hazards in health services facilities, and prevention of falls by construction workers. Table 7-1 shows the number of awards made in each of the 10 fiscal year 1999 subject areas.
A grant to the Oil, Chemical and Atomic Workers International Union in the area of worker outreach is typical. The union received $151,000 to develop a curriculum covering worker rights under the OSHAct and whistleblower protections administered by OSHA. It will instruct trainers who will then train local union members.
Outreach Grants Program
The OSHA Outreach Grants Program is a train-the-trainer program that authorizes individuals who have completed a 1-week OSHA training course to teach 10- or 30-hour courses in general industry or construction safety and health standards. These authorized trainers are also provided with OSHA course completion cards to give to their students. These cards not only provide workers with portable proof of training but also provide OSHA a means of tracking the amount of training taking place.
There is one course for the construction industry, course 500, and one course for general industry, course 501. These 1-week courses cover material that would-be trainers will subsequently cover in 10- or 30-hr courses
for workers and concentrate on OSHA standards. Prerequisites for enrolling in course 500 (construction industry) are 5 years of construction safety experience and completion of course 510, Occupational Safety and Health Standards for the Construction Industry. The courses are conducted by the OSHA Training Institute and by 12 OSHA Training Institute Education Centers located around the country. Completion of the course authorizes the student to train others for 4 years, after which an update course is required to renew the authorization to provide training for another 4 years.
Subsequent training conducted by graduates of course 500 or 501 is a mixture of mandatory topics and instructor-chosen materials specific to a particular industry or work site, and is up to 10 hours for entry-level participants or 30 hours for students seeking broader of more intensive coverage. In 1998, more than 8,700 such classes were held and more than 150,000 student cards were issued to workers as evidence of course completion (Occupational Safety and Health Administration, 1999b).
State Training and Education Initiatives
Section 18 of the Occupational Safety and Health Act of 1970 encourages states to develop and operate their own job safety and health programs. OSHA approves and monitors state plans and provides up to 50 percent of an approved plan’s operating costs. States must set job safety and health standards that are “at least as effective as” comparable federal standards. (Most states adopt standards identical to federal ones.) States have the option to promulgate standards that cover hazards not addressed by federal standards.
A state must conduct inspections to enforce its standards, cover public (state and local government) employees, and operate OSH training and education programs (Occupational Safety and Health Administration, 1999c). In addition, most states provide free on-site consultation to help employers identify and correct workplace hazards. At present, 23 states and jurisdictions operate complete state plans (which cover both the private sector and state and local government employees), and two states, Connecticut and New York, cover public employees only.
According to the annual report of the Occupational Safety and Health State Plan Association (1999), in fiscal year 1998, states with state plans provided 12,344 training programs for more than 262,000 employers and employees. Topics included confined spaces, communication about hazards of workplace chemicals, excavation safety, bloodborne pathogens, ergonomic hazards, and violence in the workplace. Many states are following OSHA’s lead in making use of the Internet to provide a wealth of OSH information to anyone with computer access. Oregon has gone one
step further and now offers five core workshops and two advanced workshops entirely via the Internet. Students take the classes electronically, respond to questions, receive personal attention from a trainer, and receive a certificate of completion at terminals in homes, workplaces, schools, and libraries anywhere in the state.
NIEHS-Supported Training and Education
NIEHS was given responsibility for initiating a training grants program under the Superfund Amendments and Reauthorization Act of 1986. Although this training is focused on only a few occupations, albeit very hazardous ones, many of the programs developed have been considered among the very best, not simply in content but also in their attention to delivery and posttraining evaluation.
Since initiation of its Superfund Worker Training Grants Program in 1987, NIEHS has been funding non-profit organizations with a demonstrated track record of providing OSH education to develop training for and deliver training to workers involved in handling hazardous waste or in responding to emergency releases of hazardous materials. The major objective of the NIEHS Worker Education and Training Program is to prevent work-related harm by assisting in the training of workers on how best to protect themselves and their communities from exposure to hazardous materials encountered during hazardous waste operations, hazardous materials transportation, environmental restoration of nuclear weapons facilities, or chemical emergency response. During the first 8 years of the Superfund Worker Training Program (fiscal years 1987 to 1995), NIEHS has successfully supported 20 primary awardees. These represent more than 90 different institutions that have trained more than 500,000 workers across the country and presented nearly 25,000 classroom and hands-on training courses, which have accounted for more than 8 million contact hours of actual training. In 1995, eighteen awardees, in conjunction with more than 70 collaborating institutions, delivered 5,348 courses, that reached 87,205 workers. The courses ranged from 4-hour refresher programs through more complex train-the-trainer courses that lasted up to 120 hours.
Funding for the development or expansion of worker training programs from NIEHS depends on reauthorization of Superfund legislation, but through interagency agreements with the Environmental Protection Agency (EPA) and the U.S. Department of Energy (DOE), NIEHS continues to support the development and delivery of model worker health and safety training in three areas: hazardous waste worker training (HWWT), DOE nuclear weapons cleanup training, and the minority worker training program (MWTP). The National Clearinghouse for Worker Safety and
Health Training for Hazardous Materials, Waste Operations, and Emergency Response provides information and communication services for the awardees in these areas (National Clearinghouse for Worker Safety and Health Training, 1999). A brief summary of their activities in the year ending August 31, 1998, is as follows:
-
HWWT—The 17 primary worker training awardees, in conjunction with more than 80 collaborating institutions, delivered 4,820 courses that reached 84,528 workers, accounting for 1,095,405 contact hours of health and safety training.
-
DOE nuclear weapons cleanup training—Seven awardees presented 896 courses to 14,097 workers, which resulted in 191,126 hours of safety and health training.
-
MWT—Ten awardees presented 160 courses to 241 students, representing 215,767 contact hours. This program included over 27 different training courses or subjects. Since 1995, the MWT program has successfully trained 919 urban young adults throughout the United States in preparing them for career-path jobs related to environmental cleanup.
Mine Safety and Health Administration Education and Training
Mining in its many forms had historically been one of the most dangerous of all occupations. The Federal Mine Safety and Health Act of 1977 (the Mine Act) established the MSHA to enforce compliance with mandatory safety and health standards as a means of eliminating fatal accidents, reducing the frequency and severity of nonfatal accidents, and promoting improved safety and health conditions in the nation’s mines. Just as OSHA carries out the mandates of the Occupational Safety and Health Act of 1970 for most industries other than mining, MSHA carries out the mandates of the Mine Act at all mining and mineral processing operations in the United States, regardless of size, number of employees, the commodity mined, or the method of extraction. Although MSHA’s program rests upon its congressional mandate to enforce the Mine Act firmly and fairly, the agency has long held that enforcement alone cannot solve all safety and health problems and has strongly emphasized the education and training of miners and managers in mine safety and health requirements.
MSHA requires that each U.S. mine operator have an approved plan for miner training. This plan must include
-
40 hours of basic safety and health training for new miners who have no underground mining experience, before they begin work underground;
-
24 hours of basic safety and health training for new miners who
-
have no surface mining experience, before they begin work at surface mining operations; and
-
8 hours of refresher safety and health training for all miners each year and safety-related task training for miners assigned to new jobs.
The National Mine Health and Safety Academy
MSHA’s National Mine Health and Safety Academy at Beckley, West Virginia, is the world’s largest educational institution devoted solely to safety and health in mining. The academy serves as the central training facility for federal mine inspectors and mine safety professionals from other government agencies, the mining industry, and labor. The academy’s physical plant has classrooms, a simulated mine and laboratories that can accommodate up to 600 students, a large auditorium, cafeteria, gymnasium, and a residence hall with dormitory space for more than 300 people.
Courses are offered on safety and inspection procedures, accident prevention, investigations, industrial hygiene, mine emergency procedures, technology, management techniques, and other topics. Courses range in duration from 2 hours to 8 days. From fiscal year 1994 through fiscal year 1998 an average of approximately 10,000 students per year took academy courses, either at the academy or at their work site. About 4,000 of these typically were MSHA and other government personnel, and about 6,000 were industry or union representatives (Thomas MacLeod, MSHA, personal communication, July 23, 1999).
Besides providing classroom instruction, the academy staff produces videotapes, films, publications, and a wide variety of technical materials. The academy also provides field training and serves as a technical resource to help meet the mining community’s instructional needs.
Educational Field Services
In 1998, MSHA created the Educational Field Services (EFS) program to optimize the administration’s resources for improving health and safety training for the mining industry. EFS training specialists visit mine sites and work closely with mine management, miners, and mine instructors to develop training methods to improve safety and health. These specialists then coordinate agency resources to best meet each mine’s individual needs.
In addition to mine visits, EFS training specialists work with mining associations, safety organizations, labor unions, and educational institutions to establish partnerships and network resources.
Training Materials
MSHA makes available many training publications, manuals, courses, films and videotapes, and other materials not only through the Mine Academy but also through the MSHA’s district offices. Some of the products available include
-
small mine operator safety kits that assist operators of small underground coal mines in controlling workplace hazards generally found at mines that employ 50 or fewer workers;
-
training materials on safe operation of powered haulage targeted to industry personnel who operate haulage trucks or other types of mobile surface mining equipment;
-
training materials on health issues, including silicosis, diesel exhaust gases and particulate matter, pneumoconiosis (black lung), and other respirable dust problems;
-
best practices techniques developed cooperatively by labor, management, and government groups;
-
comprehensive training modules and a videotape on accepted job safety analysis methods and step-by-step miner task training procedures for use by supervisors and forepersons in diverse types of mining;
-
course materials that review basic ventilation principles and practices for underground coal mines;
-
a training program that features slides that illustrate fatal accidents in mining in recent years; and
-
a monthly bulletin that features articles on topical health and safety issues.
Degree Programs in Mining Engineering
Although in many respects MSHA worker training could be a model worth emulating in other industries, it should be clear from the previous paragraphs that MSHA does not provide any support for university-based educational programs that lead to graduate or undergraduate degrees in mine safety or health. In fact, it has become apparent that university programs in all aspects of mining are in crisis. Mining engineers are educated to design and often manage all aspects of mining enterprises, including the health and safety of mine workers.
Eighteen years ago, 27 schools had ABET-accredited 4-year mining engineering programs, and the programs were viable in university academic environments. Today, 15 schools have ABET-accredited 4-year mining engineering programs, and the programs are hard pressed to continue in very cost-conscious university academic environments. Only one pro-
gram has an undergraduate enrollment of more than 100 (Virginia Polytechnic Institute), and it has a small graduate enrollment, reflective of the recently changed loss of opportunities for mining-specific research funding. The average undergraduate enrollment among the 15 accredited programs was 51 in 1997, but 9 of these programs had less than 50 students. Clearly, market demand for mining engineering students, reflective of intense global competition, has diminished. There also appears to be little demand for students with higher mining engineering degrees in industry, and traditional research funding avenues have vanished, thereby reducing graduate student enrollments.
As a result of this global competition the survival of all but six programs is seriously threatened. The other six programs are also falling under intense scrutiny because of low enrollments and seriously diminished research funding. This scrutiny by university administrators has resulted in reductions of mining engineering faculty to levels just sufficient to maintain accreditation. Further down the road, it is likely that the weaker programs will not survive as senior faculty members retire and are not replaced. Senior professors to the mining schools are older and will be retiring in the next few years, and it has already been difficult to attract new faculty at mining schools that have been permitted to do so (e.g., the University of Utah mining program has twice advertised unsuccessfully for a new faculty member with coal mining experience).
MSHA, labor unions (e.g., the United Mine Workers of America), mine operator associations (e.g., the National Mining Association and the Bituminous Coal Operators of America), and NIOSH are all concerned that skilled mining professionals who will manage mines to protect the health and safety of miners will not be available when needed. The Mine Safety and Health Research Advisory Committee, at its June 10, 1999 meeting, asked NIOSH to examine the weakened state of the nation’s mining schools and their ability to produce qualified personnel in health and safety matters and make recommendations on models of research and education funding that would address this problem. Such an examination of a single industry is beyond the scope of the present report, but the committee recognizes the reported difficulties of the mining engineering field as an instance of the more general problem of the occupational safety field in attracting and retaining doctoral-level scientist-educators to train future generations of safety practitioners.
Industry Training Programs
Corporate America provides nearly 2 billion hours of training to approximately 60 million employees, at a cost of nearly $60 billion (Training Magazine, 1997). Only part of that training is health and safety related, but
large companies generally recognize the value of maintaining professional skills that support the well-being of their employees and workplaces. In a nonrandom survey of 10 health and safety-oriented Fortune 500 companies (Victor Toy, International Business Machines Corporation, personal communication, September 1999), skills development was considered an important priority for health and safety professionals. Although it is not representative of the private sector as a whole, the results of this informal telephone survey illustrate the range of training activities that are undertaken in some large, multinational corporations.
The companies surveyed included companies in the petrochemical, high technology, aerospace, chemical, and pharmaceutical industries that ranged in size from 14,000 to more than 300,000 employees and that employ three to several hundred health and safety personnel. Programs for training and skills development differed between companies. For example, at one end of the spectrum one company focused training in a single specific area, and on the other end of the spectrum another company managed skills more comprehensively on the basis of the identification of strategic requirements to support projected business growth and development on a worldwide basis. All companies surveyed included skills training as an aspect of individual, annual performance reviews, which made it possible to require assignments and educational opportunities for the continued growth of the OHS professional.
Some company training programs included a mapping of skills against the needs of the specific businesses in the corporation. For instance, International Business Machines Corporation (IBM) developed a rigorous process that requires OSH professionals (i.e., industrial hygienists, safety engineers, doctors, and nurses) to attain specified levels of predetermined competencies on the basis of job descriptions aligned to meet a broadened array of employee well-being needs for a global business. In this approach to training and skills management, the employee establishes an annual training and education plan that is validated to meet the predefined skills milestones, and then the plan becomes funded, is executed and is monitored as the individual’s development plan.
The intensity of OSH education and training programs varied widely between and within corporations. Business performance, for example, could cause short-term program changes. Some companies hire people with the skills they need rather than invest heavily in continuing education. Every company surveyed provided at least 1 week of continuing education for each professional per year. Some provided as much as 4 weeks of training in a calendar year. Most also provided additional training and education on an as-needed basis to support the work of the OSH professional. Technical training is generally obtained through external resources locally or nationally, with most being provided by associations
like the National Safety Council, the American Society of Safety Engineers, the American College of Occupational and Environmental Medicine, the American Association of Occupational Health Nurses, and the American Industrial Hygiene Association. Management and business training for OSH leaders and managers, on the other hand, was generally provided through internal corporate organizations. Tuition reimbursement for academic course work and degree programs surveyed was available in nearly all companies.
Corporations with sizable OSH staffs may also develop and conduct internal conferences, training programs, and courses. The format varies from 1-day sessions on a single subject to a full week of training on-site or at a central location. Session topics are issues most relevant to current business operations, although basic training in OSH fundamentals is sometimes provided. One company in the petrochemical industry had a unique program to ensure the development of core skills in its OSH staff. Its “campus hire” program, which follows a structured health and safety curriculum, seeks to ensure that a professional acquires core OSH competencies during the first 2 years before a permanent job assignment is given.
Health and safety-oriented multinational corporations recognize well the limited availability of educational opportunities and OSH skills outside of mature industrialized countries. In these instances, companies often use training programs that develop the necessary skills of local employees through a combination of class and field work. A common format involves senior OSH staff members providing individualized training over a period of weeks to months with on-going mentoring support. In some cases, training plans must be approved by host countries looking to retain employees with OSH skills in the region.
Corporations promote skills development by supporting with time or funding the acquisition or maintenance of a professional certification(s) and the provision of internship experiences or rotations. Nine of the 10 companies interviewed considered professional certification in an employee’s development plan. In two cases, certification was necessary to attain a certain level within a job family. One company also rewarded this achievement through compensation. Internships and rotations are common in industry and provide students and physicians in training with private-sector experiences.
Union- and Labor-Sponsored Training Programs
Unions have long been involved in safety and health training. These efforts were spurred on by the OSHA New Directions program in the late 1970s, in which a few million dollars in grants were given to unions and trade associations to develop training materials for workers and to pro-
vide training. A huge amount of training materials and training was generated from those initial grants. Many safety and health programs were started at unions and trade associations as a consequence of this seed money. That program ended in the early 1980s and was subsequently replaced by smaller more targeted grant programs (e.g., programs targeted to certain hazards or hazardous industries) such as the Susan Harwood Training Grants Program in the 1990s.
Some unions, such as many unions for construction workers, offer all new workers safety training as part of their apprenticeship programs, such as the building trades standardized 10-hour OSHA training curriculum called Smart Mark. Several unions have set up joint safety and health funds, financed by employer contributions of so many cents per hour. Examples of such funds are the United Automobile Workers joint funds with Ford and General Motors, the Laborers’ Health & Safety Fund of North America, and the Laborers-AGC (associated general contractors) Training Fund. These funds develop safety programs that are then used to train members. The Laborers-AGC Training Fund, for example, has more than 70 training centers in the United States and Canada. These centers provide both skills training and safety training to more than 800,000 members. Much of that training is provided to workers before their employment at a specific work site, avoiding the otherwise high risk of injury in the first few days on the job as well as ensuring that an increasingly transient workforce receives this important training regardless of the nature of the employment contract and employer values. The safety and health departments of many international unions not only provide training, but also facilitate joint health and safety committees, provide technical information and conduct inspections, and advocate for stronger state and federal safety and health legislation.
Many programs that offer safety and health training of workers are sponsored by nonprofit organizations, (such as Committees of Occupational Safety and Health [COSH] that consist of coalitions of local unions in an area or city working together on occupational safety and health issues) and labor education programs at universities such as the Labor Occupational Health Program (LOHP) at the University of California at Berkeley. LOHP has, for example, been in the forefront of efforts to train minority workers, non-English speaking workers, and young workers. School-to-Work programs have been a successful innovation. Much of the training by COSH groups and labor education programs is funded through state and federal grants.
FUTURE NEEDS IN WORKER AND EMPLOYER SAFETY AND HEALTH TRAINING
Although this brief review provides only a hint of the number and variety of OSH training courses and programs in use or available today, it is clear from the review and, for example, the October 1999 National Conference on Workplace Safety and Health Training, that the volume of training being conducted is substantial. However, as noted above, with rare exceptions, little is known about the quality of the training that is actually conducted (does it consist of an actual class, a videotape, or just a handout?). Similarly, there is little information on the effects of such training; for example, did the incidence of workplace injuries or illness decrease after training, and what distinguishes successful training from unsuccessful training? Such questions are seldom even asked. Cohen and Colligan (1998) found 80 reports in the published literature, spanning the years 1980 to 1996, in which training was explicitly evaluated as an intervention effort. They concluded that training had universally shown merit in increasing worker knowledge about job hazards and effecting safer work practices, but because training was often coupled with other interventions, a connection to decreased numbers of injuries, a decrease in the amount of time lost from work, or decreased medical costs was never clearly established. The authors also emphasized that because few of the studies reviewed actually manipulated variables like class size, length or frequency of training, trainer qualifications, mode of training, and management involvement, it was impossible to say what factors produce the greatest impact.
Training and education of workers has not traditionally been considered a prime responsibility of most OSH professionals. In fact, most graduates of OSH programs are ill prepared for this assignment. While they have the technical knowledge, many graduates lack skills in adult education, training, and program evaluation. The net result is very uneven training quality. As noted in this chapter, several OSHA, NIOSH, and NIEHS programs have attempted to fill this gap; but these programs have often been limited to selected populations (e.g., hazardous waste workers, emergency responders, etc.) by their enabling legislation. In addition, the inability of these programs to reach a significant portion of the non-union workforce is cause of concern as well as impetus for seeking innovative approaches, perhaps community based, to reach these workers.
The committee urges NIOSH to join with OSHA, NIEHS, unions, industries, and employers to systematically evaluate the efficacy of OSHA and other worker training programs and better define minimum training requirements. Using the successful collaboration that has characterized
the National Occupational Research Agenda (NORA) as a prototype, these agencies should undertake a major effort to: (1) explore how lessons learned from these programs can be used to enhance other worker training efforts, and (2) broaden the scope of worker populations which can benefit from these substantial expenditures of funds. Demonstration project grants should be provided as incentives to develop model training programs for OSH educators and trainers in specific employment sectors.
Earlier sections of this report have noted that OSH professionals are primarily employed by medium-sized to large employers and therefore directly involved with less then half of all U.S. employees. The committee’s analysis of anticipated changes in the nature of work in the United States led it to suggest that small, service-sector businesses would increasingly dominate the employment market and that all sectors of the economy would be characterized by decentralization, flexibility, nonstandard work arrangements, and a highly diverse and transient workforce, making it likely that an even smaller proportion of employees will count OSH professionals among their fellow employees. Day-to-day responsibility for worker safety and health will increasingly fall to managers who have little if any formal education or training in OSH and who may have numerous other responsibilities as well. NIOSH and OSHA should collaborate to develop a program of training for these individuals. The committee believes the two agencies need to reconsider their historical division of training responsibilities (OSH professionals by NIOSH, workers by OSHA) in the light of this trend. The OSHAct of 1970 is far less specific on this division than the agencies’ policies might imply (see Chapter 1). The committee again recommends large-scale demonstration projects that target small- and medium-sized employers and encourages the use of new learning technologies, the development of a recommended set of basic competencies, and the creation or recognition of a new category of OSH personnel, the occupational safety and health manager. The partnering process so successfully used by NORA could be usefully employed in this endeavor as well.
Incentives may still be necessary to induce small businesses in industries not currently covered by specific OSHA standards to invest in either high-quality worker training or education of an OSH manager for their work sites. This is an important consideration, given that it is just these sorts of employers that will be the primary source of new jobs in the coming decade. Clarification of existing OSHA training mandates to include essential elements and measures of efficacy may be one answer to the training quality issue, and OSHA’s draft proposed Safety and Health Program Rule unequivocally fixes responsibility for hazard identification and control and for worker health and safety training on the employer and management. Further inducement depends upon inculcation of a
culture of safety and health in the general public. Accomplishing this is a large, long-term, multifaceted project that will require leadership from the U.S. Department of Health and Human Services and the U.S. Department of Labor and that will involve the mass media, the Internet, K-12 education, and other communications strategies targeted to youth, parents, and workers as well as employers.