8
Education and Training
Relatively little attention has been paid by public health officials and other medical professionals to the importance of loneliness.
Members of the health care workforce (including professionals and direct care workers) are vital in the effort to prevent, identify, reduce, and eliminate the negative health impacts of social isolation and loneliness in older adults. This chapter addresses the education and training of this workforce. In addition to the imperative to increase the knowledge and skills of those employed by the health care delivery system, this chapter considers the opportunity to increase awareness and knowledge about social isolation and loneliness among patients, families, caregivers, volunteers, and the community at large. Given the complexity of the terminology used in relation to social isolation and loneliness, a reminder of key definitions is provided in Box 8-1.
FRAMEWORK FOR THE ROLE OF EDUCATION IN CATALYZING CHANGE
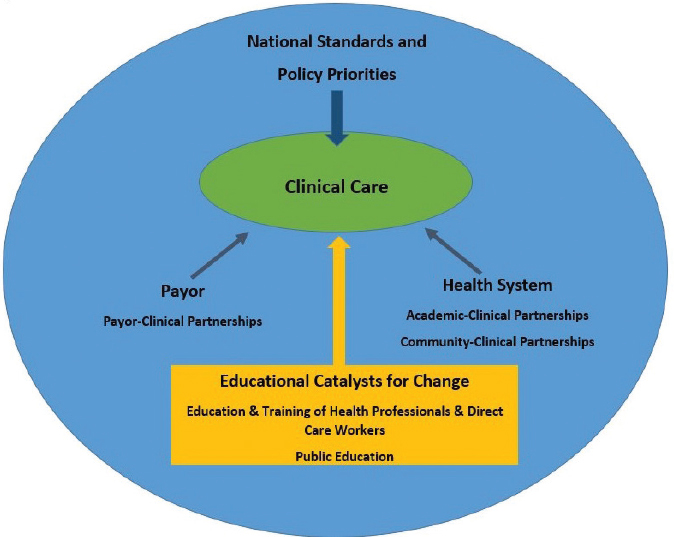
The committee developed a framework to explain the role of education in addressing issues of social isolation and loneliness (see Figure 8-1). The framework emphasizes catalyzing change in clinical care delivery with the goals of preventing, ameliorating, and eliminating social isolation and loneliness in older adults and addressing the health effects of chronic social isolation and loneliness. Clinical care provides an important—and underused—opportunity to address
social isolation and loneliness in older adults. All types of health professions and careers need to be involved, and the necessary changes can be catalyzed through various types of education, including direct care worker education, lifelong learning by health professionals and direct care workers, and public educational campaigns. All learners need to understand how the educational and training context for social isolation and loneliness either creates higher risk or provides avenues for mitigating these problems. This context includes
- The impact of national standards and policy priorities;
- Current education and training approaches;
- How health system design can change practice behaviors and facilitate treatment strategies (e.g., through partnerships with academic environments and communities); and
- How payor policies facilitate or impede addressing social isolation and loneliness.
NATIONAL STANDARDS AND POLICY PRIORITIES
At the highest level, national standards and policy priorities can influence and shape the education of the formal health care workforce. As each profession sets its own standards for education and practice, the topics of social isolation and
loneliness can be incorporated into the standards and competencies expected of students. The compelling evidence base for the health effects of social isolation and loneliness provide faculty and educational leaders with a strong rationale for including this content in educational programs. The following sections highlight several opportunities for influencing the education and training of the formal health care workforce.
Interprofessional Groups
Many interprofessional groups related to the care of older adults need to be partners in improving education and training related to social isolation and loneliness among older adults. Such groups include (but are not limited to) the American Geriatrics Society, the Society for Post-Acute and Long-Term Care Medicine, LeadingAge, the Eldercare Workforce Alliance, and other service provider organizations. The following sections provide examples of a few key partners specifically engaged in professional education.
The Interprofessional Education Collaborative (IPEC), formed in 2009 by a group of health professions education associations to develop a set of competencies for interprofessional education (IPEC, 2016), could address social isolation and loneliness through its focus on team-based approaches. The four initial competencies
and sub-competencies developed by IPEC were updated in 2016 to reflect interprofessional collaboration as the primary organizing construct and to focus more clearly on population health. The updated competencies emphasize collaboration with others outside of the formal health care system. This updated format is particularly germane to addressing social isolation and loneliness in older adults because much of the support needed may come from other sectors, including sources within neighborhoods and communities. Because the interventions needed to address social isolation and loneliness draw on so many different professions and disciplines, including a variety of frontline workers such as direct care workers and community health workers, volunteers, and family caregivers (sometimes called informal caregivers), it would be particularly helpful when promulgating recommendations to note their relevance to the IPEC competencies.
Beyond Flexner1 is an interprofessional group that promotes the inclusion of social determinants of health into all health professions curricula (Kaufman, 2016). Mullen (2017) argued that social, economic, and geographic conditions are fundamental in determining the presence or absence of health inequities and therefore that all health professions schools should educate students about the importance of the social mission. The name, Beyond Flexner, is intended to signify the inclusion of the social mission and learning experiences related to social determinants of health that go above and beyond the biologically and clinically based educational model the founders of this movement assert is currently in use. This social mission could incorporate issues related to social isolation and loneliness and expand health professions education around these issues.
Englander and colleagues (2013) proposed a framework composed of eight domains that they recommended for use within medical education. The domains, developed to be sufficiently broad to be applicable to any health profession, have been adopted by one nurse practitioner residency program (Flintner and Bamrick, 2017) and are being discussed for use in nursing education more broadly (AACN, 2019). The eight domains are:
- patient care;
- knowledge for practice;
- practice-based learning and improvement;
- interpersonal and communication skills;
- professionalism;
- systems-based practice;
- interprofessional collaboration; and
- personal and professional development (Englander et al., 2013, pp. 1091–1092).
___________________
1 In 1910, Abraham Flexner issued a report (now known as the Flexner report) that criticized the quality of medical education at that time and resulted in a reorganization of the medical education system (Flexner, 1910).
The prevention and treatment of the health impacts of social isolation and loneliness in older adults fits within several of these domains. For example, incorporating evidence-based recommendations to prevent or ameliorate social isolation and loneliness in older adults fits within the domains of patient care, interpersonal and communication skills, system-based practice, and interprofessional collaboration.
The Academy for Gerontology in Higher Education (AGHE) is a membership organization of colleges and universities that offer education, training, and research in the field of aging. Interdisciplinary in nature, the goals of AGHE include educating society about aging, preparing service delivery people who work with older adults, and providing leadership on policies and issues related to higher education (AGHE, 2019). AGHE develops, promotes, and publishes gerontology competencies for undergraduate and graduate education. These recommended competencies include foundational competencies, interactional competencies, and contextual competencies (AGHE, 2014). For example, the foundational competencies are in the areas of the biological aspects of aging, the psychological aspects of aging, and the social aspects of aging. Content about social isolation and loneliness could be included within these three aspects of aging and would serve to prepare the workforce with tools to recognize social isolation and loneliness, to understand its impact on older adults, and to ameliorate it. One interactional competency is interdisciplinary and community collaboration. Community collaborative competency work could focus on solutions to address social isolation and loneliness from an interdisciplinary perspective. Finally, the contextual competencies include well-being, health, and mental health as one contextual competency and social health as another. Social isolation and loneliness could be integrated within these competencies. AGHE could provide the leadership to promote social isolation and loneliness in its recommended competency content, and infusion across curriculum standards and within the structure of the AGHE competencies would be possible.
National Goals for Health and Well-Being
The Healthy People national goals provide yet another opportunity for encouraging the inclusion of content related to social isolation and loneliness in health professions education as well as in programs aimed at practicing clinicians and other professionals who care for older adults. Since 1990 Healthy People goals have been developed for each decade, and social cohesion is one of the topics addressed in the section on social determinants of health for Healthy People 2020 (HHS, 2019b). Foundational principles and overarching goals have already been proposed for Healthy People 2030, and the specific goals and objectives are under development at this time (HHS, 2019c). Healthy People goals provide important directions for health professions education. Although the goals and objectives are not educational standards, they influence curricula because they represent national priorities. The overarching goals for Healthy People 2030 are based on a
vision of “a society in which all people can achieve their full potential for health and well-being across the lifespan” (HHS, 2019c). Addressing social isolation and loneliness fits clearly within this broad vision.
An Individual Health Professions Response
Making the prevention and treatment of social isolation and loneliness in older adults a priority of individual health professions is another important strategy. One example has occurred within the social work profession, with the American Academy of Social Work and Social Welfare having adopted the elimination of social isolation as one of its grand challenges (Lubben et al., 2015, 2018). The Grand Challenge initiative2 provides a framework for disseminating evidence-based strategies to solve important social problems and to bring a range of stakeholders together in designing multifaceted solutions. The benefits of grand challenges, such as this one developed by the social work profession, are that they provide a focus, bring leaders to the table, provide a framework for collaboration and interdisciplinary engagement, capture public interest, attract resources, and promote diplomacy (Uehara et al., 2013). The success of this initiative will depend on participation across professional groups, organizations, and communities (Uehara et al., 2013). Indeed, social isolation and loneliness in older adults is a complex issue that will benefit from cross-sector collaborative initiatives such as this.
CURRENT EDUCATION AND TRAINING OF THE HEALTH CARE WORKFORCE
In 2016 an ad hoc committee of the National Academies of Sciences, Engineering, and Medicine (the National Academies) developed a framework for educating health professionals to address the social determinants of health (NASEM, 2016a; see Figure 8-2). The committee concluded that there should be “a holistic, consistent, and coherent framework” of education and training that promotes a systems-based approach aligned across health, education, and other sectors in partnership with communities (NASEM, 2016a, p. 4). This call for a unified approach (based on the three pillars of transformative learning, dynamic partnerships, and lifelong learning) is especially important for a health care workforce concerned with social isolation and loneliness in older, vulnerable populations. Many health professions stress the incorporation of the social determinants of health in general into curricula for students and trainees. However, the nontraditional components of education recommended by the 2016 committee (e.g., experiential learning, collaborative learning, an integrated curriculum, continuing professional development) are not universally deployed.
___________________
2 For more information, see https://grandchallengesforsocialwork.org/about (accessed December 16, 2019).
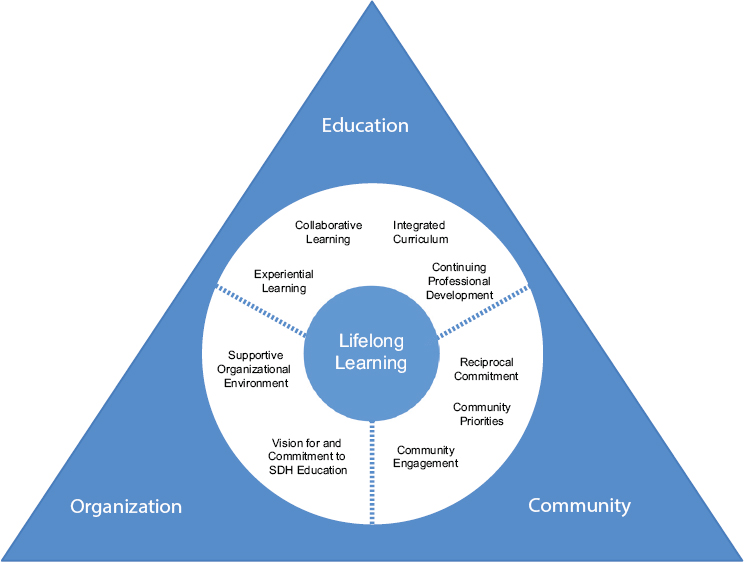
NOTE: SDH = social determinants of health.
SOURCE: NASEM, 2016a.
The 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care discusses the role of education in developing a workforce that can understand and address social factors and recommends the incorporation of competency-based curricula on social care into health professions and continuing education programs (NASEM, 2019). The following sections expand on that report’s recommendation and highlight specific examples and opportunities for the education and training of the health care workforce on issues related to the social isolation and loneliness of older adults.
Health Professions Education
Many individual professions have paid attention to the education and training of their own professionals about the social determinants of health in general. However, except for a few notable examples, little is known about the level of education and training provided on the particular effects of social isolation and loneliness. Aside from formal education programs, the role of certification may
be explored as a way to foster the infusion of these topics into the education and training of health care professionals. The committee recognizes that adding more requirements may add to burden and burnout among health care professionals. However, given the significant impact of social isolation and loneliness on health, the committee asserts that all of these potential options need to be explored as ways to impart critical knowledge. Several examples of these efforts are described below.
Educational Efforts by Individual Professions
The Accreditation Council for Graduate Medical Education sets standards for accrediting U.S. graduate medical education programs and the institutions that sponsor them. The common program requirements for residency govern the professional development of physicians. Program directors are required to “design and conduct the [residency] program in a fashion consistent with the needs of the community” (ACGME, 2018, p. 9). Each program “must understand the social determinants of health of the populations they serve and incorporate them in the design and implementation of the program curriculum” (ACGME, 2018, p. 9). Similarly, “residents must demonstrate an awareness of and responsiveness to the larger context and system of health care, including the social determinants of health, as well as the ability to call effectively on other resources to provide optimal health care” (ACGME, 2018, p. 21). The common program requirements do not specifically address social isolation and loneliness.
The American Association of Colleges of Nursing publishes the Essentials documents that delineate expected core outcomes of nursing education at the baccalaureate, master’s, and doctor of nursing practice levels (AACN, 2006, 2008, 2011). While the Essentials documents are broad, they clearly indicate the expectation that nurses care effectively for all age groups, including older adults. For example, Baccalaureate Essentials (AACN, 2008) states that nurses care for people of all age groups, with special attention to “older adults and the very young” (p. 32). The document also indicates that care should be holistic and account for patient and family preferences and community concerns and that professionalism in nursing involves integrating physical, emotional, and social concerns. Finally, this document indicates that nurses provide a link between hospitals and community environments and supports the importance of nurses’ roles in assessing social and psychological needs as well as physical health needs and making referrals to community services as needed. Master’s and Clinical Doctoral Essentials similarly focuses on comprehensive care based on a full biopsychosocial model that includes the social determinants of health (AACN, 2006, 2008). Similarly, the National League for Nursing has identified competencies for graduates of nursing education programs that address the full age continuum and a holistic approach to caregiving (AACN, 2011).
The Council on Social Work Education’s Educational Policy and Accreditation Standards (EPAS) sets forth guidelines for professional competence. These standards are used to accredit baccalaureate and master’s level social work
programs (CSWE, 2015). The EPAS consists of nine competencies that are guided by a person-in-environment framework, a global perspective, and respect for human diversity (CSWE, 2015). These competencies outline the importance of working with diverse populations within the context of relationship building, interprofessional teamwork, and inter-organizational collaboration. Engagement, assessment, and intervention occur within the intersection of multiple factors, including age, class, culture, disability and ability, ethnicity, gender, gender identity and expression, immigration status, marital status, political ideology, race, religion and spirituality, sex, sexual orientation, and tribal sovereign status. The focus on these factors reinforces the importance of understanding and recognizing the influence of the social determinants of health on the lifelong development of individuals (CSWE, 2015). The EPAS outlines the role that social workers have in assessing and intervening within a practice context that includes working with individuals, families, groups, organizations, and communities toward mutually agreed-upon goals (CSWE, 2015). These competencies reinforce the expectation that social workers are trained to attend to the social and psychological needs of older adults and their families within the context of health and social service settings. Social workers are trained to serve as a bridge to the broader community and are well positioned to make connections between health providers and the larger social service community (CSWE, 2015).
Additionally, the social work profession, under the auspices of the Council on Social Work Education through its Gero Ed Center, developed a Geriatric Social Work Competency Scale with Lifelong Leadership Skills (CSWE, 2019). This scale lists skills recognized by gerontological social workers as important to social workers in their work with and on behalf of older adults and their families. Designed to be used at the baccalaureate, master’s, and post-masters levels of curriculum, it is used for pre–post evaluations of education and field training. Students are rated in four areas of competence:
- Values, ethics, and theoretical perspectives
- Assessment
- Intervention
- Aging services, programs, and policies (CSWE, 2019)
The assessment of social support and human connections is one of the factors that is included in the assessment competency section. Adding content on social isolation and loneliness to the intervention competence could strengthen social work practitioners’ response to at risk older adults.
National Geriatrics Training Program
National training programs in geriatrics, such as the Geriatrics Workforce Enhancement Program (GWEP) funded by the Health Resources and Services
Administration, provide another potential opportunity for improving education and training on social isolation and loneliness in older adults. GWEP provides grants “that improve health care for older adults and maximize patient and family engagement to health professions schools, health care facilities, and programs leading to certification as a certified nursing assistant.”3 Key goals of the program are to “educate and train the primary care and geriatrics workforce to care for older adults in integrated geriatrics and primary care models,” and “to partner with community based organizations to address gaps in healthcare for older adults, promote age-friendly health systems and dementia-friendly communities, and address the social determinants of health.”4 Social isolation and loneliness could be explicitly incorporated into some of these programs, particularly as a key social determinant of health.
Role of Certifications
Certification exams use standards of practice as the basis for exam questions and could include questions about social isolation and loneliness. Specialty gerontologic certification exams are available in, for example, medicine, nursing, physical therapy, psychology, and pharmacy. Certification examinations and credentials are also available for more specific areas, such as diabetes educators (NCBDE, 2019), although none exist for addressing social isolation and loneliness. The development of a certification exam related to preventing and treating social isolation and loneliness, either as a stand-alone exam or by including items related to this topic on a currently existing gerontologic exam, is a potential opportunity for emphasizing the importance of this area.
Direct Care Worker Education and Training
Direct care workers are the paid front line of long-term care in the United States, providing critical, daily support to millions of older people and people with disabilities. As a result, direct care workers, of which there were 4.3 million in 2017 (PHI, 2018a), are well positioned to support older people nationwide in addressing social isolation and loneliness. As interventions directed at social isolation and loneliness in older adults gain traction, direct care workers will need to be properly trained, educated, and supported.
Governing and shaping the direct care workforce are a variety of broad and inconsistent state and federal training requirements in addition to an under-resourced training and public education landscape. The current training for the direct care workforce rarely explicitly addresses social isolation and loneliness in older adults.
___________________
3 See https://bhw.hrsa.gov/grants/geriatrics (accessed December 16, 2019).
4 See https://www.americangeriatrics.org/programs/gwep-coordinating-center (accessed December 17, 2019).
Core Competencies
Ideally, a set of core competencies—manifested as knowledge, skills, and abilities—form the foundation of training for direct care workers, delineating the capabilities that workers should acquire and demonstrate in order to effectively provide care. An array of public and private actors in the long-term care field have created core competency skill sets for direct care workers, which vary widely in terms of content areas (and other aspects). While none of these competency sets explicitly address social isolation and loneliness, many of them include related areas that could allow for more focused attention on these two topics. For example, the Centers for Medicare & Medicaid Services direct service workforce core competencies include a competency area of “community inclusion and networking” (CMS, 2014, p. 7). The following two skill statements are included under that competency area:
- The direct service worker “encourages and assists individuals in connecting with others and developing social and valued social and/or work roles based on his or her choices,” and
- The direct service worker “supports the individual to connect with friends and to live and be included in the community of his or her choice.” (p. 7)
The National Alliance for Direct Support Professionals’ direct support professionals competencies includes a section on “community living skills and supports” and notes that “the competent [direct care worker] supports the participant in the development of friendships and other relationships” (NADSP, 2016, p. 5).
Training Requirements and Credentialing
Direct care workers are subject to an array of federal and state training requirements, which vary widely in terms of their duration and content (among other dimensions) across different direct care occupations, states, and service delivery models.5 While these requirements need significant improvement, they provide opportunities to expand the skills of direct care workers on social isolation, loneliness, and older adults. For example, federal guidelines for home health aides require that the aides must be trained in the “physical, emotional, and developmental needs of and ways to work with the populations served by the Home Health Agency, including the need for respect for the patient, his or her privacy
___________________
5 Federal regulations today require that home health aides and nursing assistants receive at least 75 hours of training, including at least 16 hours of supervised practical or clinical training. They must also complete 12 hours of continuing education every 12 months. Only 17 states and the District of Columbia surpass this 75-hour requirement, and only 6 states and the District of Columbia meet the 120-hour standard encouraged by the Institute of Medicine (IOM, 2008). Personal care aides have no federal training requirement, and state-level requirements vary considerably, typically with little to no uniformity across programs or requirements on duration, content, and methods (PHI, 2019a,b).
and his or her property.”6 Similarly, the federal guidelines for nursing assistants require that workers be trained in the “mental health and social service needs” of older adults.7 Guidelines for both direct care occupations could specify social isolation and loneliness as priority topics.
Personal care aides—the largest-growing segment of the direct care workforce—lack any federal training requirement and have few state-level requirements (PHI, 2019c). A number of states require the use of state-sponsored curricula or training outlines that set forth detailed training content for specific segments of the direct care workforce. Compared with broad regulatory requirements, these curricula and outlines are more prescriptive in terms of their content, instruction methods, and competency assessment, and they could be updated to address social isolation and loneliness in older adults. A few notable examples:
- New York’s curricular outline for personal care aides covers the emotional well-being of consumers (i.e., “safety and security including emotional security”) (NYSDOH, 2002, p. 61).
- Virginia’s curricular outline covers the basic physical and emotional needs of consumers, including “love and belonging” (VDMAS, 2003).
- Arizona’s Principles of Caregiving curriculum addresses social isolation and loneliness in multiple areas, including in a section on the “emotional impact of aging” (Arizona Direct Care Initiative, 2011).
- Washington State’s state-sponsored curriculum encourages home care aides to help consumers stay socially connected. The curriculum also emphasizes the aide’s role in the emotional well-being of consumers (WSDSHS, 2009).
- Maine’s personal support specialist curriculum refers trainees to a companion textbook for content on social isolation (MDHS, 2003).
Other Members of the Health Care Workforce
Aside from health care professionals and direct care workers, many other members of the health care workforce may be especially important to addressing social isolation and loneliness because they are natural connectors of the health care system with the local communities. Community health workers (CHWs) are
lay members of the community who work either for pay or as volunteers in association with the local health care system in both urban and rural environments. CHWs usually share ethnicity, language, socioeconomic status, and life experiences with the community members they serve. (NIH, 2014)
CHWs have been shown to be particularly effective in creating linkages between communities and the health care system and in providing health education
___________________
6 42 CFR § 484.36—Condition of Participation: Home Health Aide Services. 82 FR 4504.
7 42 CFR § 483.152—Requirements for Approval of a Nurse Aide Training and Competency Evaluation Program. 56 FR 48919, 75 FR 21179.
and informal counseling, particularly for underserved communities (HRSA, 2007). While CHWs typically come from the communities in which they serve and often serve as advocates for the individuals in these communities, patient navigators (or patient advocates) tend to be based within the health care system. Patient navigators help patients acquire necessary information and services that may affect their health care (NCI, 2011). For example, patient navigators may assist patients with setting up appointments, reaching out to insurers, and connecting to needed social supports. Case managers (or care managers) focus particularly on coordinating health and social care for individuals with complex needs either in health care systems or with social service agencies (NASEM, 2019). These health care workers and others can serve an important role in connecting the health care system with community-based services.
PUBLIC HEALTH CAMPAIGNS
Public education campaigns can be a powerful method for raising awareness of and support for key issues, among other objectives. For example, public education campaigns have addressed various health topics, including tobacco use; nutrition, physical activity, and obesity; heart disease and stroke; diabetes; and Alzheimer’s disease, among others (NIH, 2019). Such campaigns are used to “help health care professionals, practitioners, and the general public make informed decisions about their health and the health of their patients” (NIH, 2019).
Public education campaigns are often undertaken by specific health care professions and occupations. For example, nonprofit organizations in the direct care sector have used public education campaigns to:
- focus attention on the growing workforce shortage in home care at the national and state levels,
- support specific policy goals,
- reach workers with information about their rights and benefits, and
- explore future solutions for the full elder care workforce (EWA, 2019; PHI, 2018b, 2019d).
The following sections highlight examples of the use of campaigns to spread awareness of issues related to aging in general as well as social isolation and loneliness in particular.
Public Education and Framing Strategies for Aging
Public education campaigns have been increasingly used in the aging and long-term care sector to raise awareness about the realities of aging, the variety of challenges and opportunities facing older people, and the demand for a strong elder care workforce. In recent years, these campaigns have sought, among other goals, to change perceptions of aging through personal stories of older people, to
connect the millennial generation to aging-related concerns, and to inspire policy makers to address the worsening shortage in home care workers (Snelling, 2019).
More broadly, an extensive body of research and applied practice exists to guide communications planning, strategy, and evaluation across social issues, identifying effective techniques for defining and establishing clear goals, objectives, audiences, and evaluation measures. When designed properly, public education campaigns can shape public policy by raising awareness, increasing the numbers of champions and supporters, building constituents, strengthening public will, and sparking policy change. These campaigns can also influence such characteristics as awareness, salience, attitudes and beliefs, self-efficacy, social norms, and behavioral intention and change (Communications Network, 2008).
Furthermore, social scientists and strategic communications experts have recently created and tested a variety of approaches to promoting strong, positive messaging regarding health and older adults and to reducing harmful ideas that perpetuate problematic representations of older adults. This emerging trend builds on a body of research and practice focused on “collective action framing” in social movements worldwide—intentional, large-scale efforts to transform how the public at large understands societal problems, solutions, and related actions (Benford and Snow, 2000). Two current examples related to health and aging are an effort to provide guidance on how to discuss the social determinants of health, led by the Robert Wood Johnson Foundation (RWJF), and the Reframing Aging Project, which seeks to improve messaging about aging and to reduce ageism, led by the FrameWorks Institute, a nonprofit organization focused on advancing ways to communicate about science (FrameWorks Institute, 2019; RWJF, 2010). The two efforts both created research-tested approaches and practical tools for the public and private sectors to frame concerns about health (the RWJF project) and aging (FrameWorks), guiding the creation of effective, strength-based narratives on the topics. Of note, the Reframing Aging Project was steered by a group of leading organizations in the aging services field: AARP, the American Federation for Aging Research, the American Geriatrics Society, the American Society on Aging, the Gerontological Society of America, Grantmakers in Aging, the National Council on Aging, and the National Hispanic Council on Aging (FrameWorks Institute, 2019).
Despite the potential and the proliferation of these types of approaches, researchers and communications strategists have not produced any easily available, research-tested frames, messages, or communications campaigns and tools that are specific to social isolation and loneliness in older adults—a fact that limits strategic, collective action on this pressing concern.
Education by Campaigns and Coalitions Specifically for Social Isolation and Loneliness
As the complexities of mitigating social isolation and loneliness are increasingly acknowledged, some stakeholders support large-scale campaigns and
coalitions to disseminate information and best practices. The increased visibility from such media campaigns has the potential to change public attitudes and social norms, which in turn could indirectly influence behavior change (Holt-Lunstad et al., 2017).
Campaign to End Loneliness (UK)
The Campaign to End Loneliness, a large-scale media campaign, was founded in the United Kingdom in 2011 with the goal of sharing research, evidence, and knowledge in order to connect individuals and communities across the country (Campaign to End Loneliness, 2019b). The campaign is hosted by Independent Age, a charitable organization focused on the well-being of older people, and it is supported by the National Lottery Community Fund, the Calouste Gulbenkian Foundation, the Tudor Trust, and donations from the general public. The campaign has created a series of toolkits, research briefs, and events to raise awareness among public health and health care practitioners about the deleterious health effects of social isolation and loneliness. The campaign has also created the Learning Network (Campaign to End Loneliness, 2019c), which links like-minded organizations, distributes the latest research on social isolation and loneliness, and shares examples of best practices for addressing loneliness, but does not necessarily perform evidence-based assessments of these practices on their own. The campaign has been relatively successful in distributing information and bringing loneliness to the front of public discourse. An evaluation of the campaign’s outreach efforts found that 84 percent of National Health Service health and well-being boards targeted by the campaign had implemented written strategies for addressing loneliness (Cupitt, 2013).
AARP Foundation Connect2Affect
The AARP Foundation has partnered with the Gerontological Society of America, Give an Hour, n4a, and UnitedHealthcare to launch a campaign, Connect2Affect, to address social isolation and loneliness (AARP Foundation, 2019). The major goal of the campaign is to create a network of resources that meets the needs of anyone who is socially isolated or lonely and that helps build the social connections that older adults need to thrive. The campaign has helped to increase awareness of the impact of social isolation and loneliness on older adults, to provide information on service and training resources, and to create networks. The National Good Neighbor Day8 is an example of a community impact activity associated with this campaign.
___________________
8 For more on the National Good Neighbor Day, see https://connect2affect.org/goodneighborday (accessed December 18, 2019).
CHANGING PRACTICE BEHAVIORS
While education is one method for catalyzing change, dissemination and implementation science has shown that an individual’s (or group’s) knowledge of what to do is never enough to institutionalize and sustain change. (See Chapter 10 for more on dissemination and implementation.) Educating users about evidence-based practices (EBPs) is a necessary but not sufficient step to change practice, and didactic education alone does little to change practice behavior (Forsetland et al., 2009; Giguère et al., 2012). Users of the EBPs need to know the scientific bases for EBP recommendations and to have the knowledge and skills to carry out such practices, and health system design and payor policies need to support the implementation of these recommendations.
Lifelong learning opportunities are vital for the ongoing development of health care workers who interact with older adults. Given that the evidence base is continuing to develop in the area of social isolation and loneliness, those working with older adults, families, and communities will need ways to learn about future research developments in this area. Multiple modalities are available for lifelong learning, including just-in-time learning, Web-based modules and webinars, other forms of online learning, conference presentations, and journal articles (IOM, 2009).
Certain roles and responsibilities already present in health systems can be modified to address social isolation and loneliness in older adults. Discharge planning, case management, and transitional care planning are examples of the sorts of roles and functions that can be used to directly address the assessment of and interventions for social isolation and loneliness. Discharge planning and case management are most often provided by social workers and registered nurses. Transitional care planning may be provided by advanced practice nurses and master’s-prepared social workers (Altfeld et al., 2013; Alverez et al., 2016; Eaton, 2018; Naylor et al., 2018). For instance, Naylor et al. (2018) developed a transitional care model designed to prevent rehospitalizations and health complications in older adults with chronic illnesses. An advance practice nurse provides a thorough assessment prior to the discharge and leads the discharge and home follow-up process. Given the extensive nature of the pre-discharge assessment, screening for social isolation and loneliness could be integrated into the assessment process. If social isolation and loneliness are detected in the screening, intervention and follow-up could occur in the community as part of the community visits.
In the Bridge model (Altfeld et al., 2013; Alvarez et al., 2016) a social worker with a master’s degree connects with the patient and family prior to discharge. Inpatient and outpatient providers are also connected with the patient and family to reinforce the continuity of care. This model encourages attention to the social determinants of health, and as social needs are identified, the social work care coordinator addresses them in both health care and community-based settings. Using this model, social isolation and loneliness could be identified before discharge and addressed throughout the care transition process and as the patient integrates back into the community. For example, current team-based models
for identifying frail patients in hospitals (through the use of multi-dimensional assessments) could serve as models for the identification of social isolation and loneliness in the inpatient setting (Ansryan et al., 2018; Borenstein et al., 2013, 2016). Strassner et al. (2019) describe a study planned in Germany that will prepare general practitioners to provide holistic disease management services for frail older adults. These services will include assessments of loneliness, suggesting that the inclusion of this aspect of managing chronic conditions is gaining interest. Team-based approaches to helping older adults manage care over a period of time provide multiple perspectives for incorporating social isolation and loneliness into care plans. (See Chapter 7 for more on the role of the health care system.)
As noted in the 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care, “Understanding the role each member of an interprofessional team plays . . . is important for ensuring effective collaboration among team members and for maximizing their ability to address patients’ social needs” (NASEM, 2019, p. 77). This approach can be adopted when designing education and training models to address social isolation and loneliness. Collaboration and coordination among all members of a health professional team is a critical component in education and training initiatives.
Health Systems: Academic–Clinical Partnerships
Academic–clinical partnerships can catalyze evidence-based practice (Noel et al., 2019). Education and research on the causes and outcomes of social isolation and loneliness in older adults, screening tools, assessment strategies, and effective interventions need to be connected with clinical practice in ways that accelerate improvements in practice, change systems of care when needed, influence payment systems, increase health, and highlight successful teamwork among health professionals, direct care workers, and community members. The 2016 report Advancing Healthcare Transformation: A New Era for Academic Nursing highlights the importance of intentional and systematic academic–practice partnerships in catalyzing improvements in nursing care (AACN, 2016). Alberti et al. (2018) noted that action planning with communities is more likely to generate lasting results in health equity than are less intentional partnerships. The use of relevant clinical guidelines, such as those promulgated by the Hartford Institute for Geriatric Nursing’s Depression in Older Adults (Harvath and McKenzie, 2012), and the development of specific guidelines targeted to the treatment of social isolation and loneliness in older adults can help improve practice. Boston College’s Institute on Aging is another example of an academic–practice partnership, with its emphasis on interdisciplinary education, research, and community partnerships. One product of this Institute is BC Talks Aging,9 which is a series of modules with
___________________
9 For more information on BC Talks Aging, see https://www.bc.edu/centers/ioa/videos.html (accessed December 17, 2019).
free access, developed by established scholars on topics related to aging, and one of these modules specifically addresses social isolation and loneliness. The aim of BC Talks Aging is to provide learning opportunities on aging issues for social workers, nurses, and other health practitioners in the field (BCIA, 2019).
Partnerships between clinical organizations and community organizations are essential to ensuring that a full range of services and care are available for older adults at risk for social isolation and loneliness. The 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care notes the importance of developing cross-sector coalitions and describes the success of multi-sector coalitions in improving health delivery. One successful partnership described in the report was between Johns Hopkins University and the Homewood Community Partners Initiative, which led to the establishment of health enterprise zones, aligning and increasing activity coordination with health departments, health providers, and community organizations. The impact of this partnership was a reduction in inpatient hospital visits resulting in a net cost savings of $93.39 million (NASEM, 2019).
Health Systems: Payor–Clinical Partnerships
Critical to the adoption of clinical interventions is understanding payor policies and inviting payors to the table when changes may be needed. The 2018 Alliance of Community Health Plans (ACHP) report Accelerating the Adoption of Evidence-Based Care: Payer Provider Partnerships found that collaboration among high-performing health plans to influence provider behavior can accelerate the dissemination and adoption of EBPs. Although the research by ACHP did not specifically address social isolation and loneliness, the report highlighted examples of consensus building, customized education, tools, and access to extensive training as a means to disseminate and promote accelerated delivery of evidence-based care best practices across diverse types of payor–provider partnerships (ACHP, 2018).
The 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care concludes that if social care is to be properly addressed in health care, health care financing structures need to recognize the importance of the unique contributions of team members and to ensure adequate reimbursement of clinical partnerships (NASEM, 2019).
FINDINGS AND CONCLUSIONS
- Educating health care professionals, direct care workers, and the general public on the health impacts of social isolation and loneliness is essential.
- National standards and policy priorities influence the education of the formal health care workforce. Social isolation and loneliness can be incorporated into these standards and priorities in order to raise awareness and educate current and future health professionals about these topics.
- Formal and informal education, lifelong learning, and educational campaigns can catalyze change by facilitating learners’ knowledge of the risk factors for social isolation and loneliness and how to prevent and ameliorate these problems.
- Despite limited research on the effectiveness of selected interventions for social isolation and loneliness, health professionals need to learn core content in areas such as the prevalence of social isolation and loneliness, morbidity and mortality related to social isolation and loneliness, risk factors, assessment strategies, referral options and processes for making and following up on referrals, ways to support and encourage older adults and their significant others, partnering with community agencies, and program development and evaluation. This content crosses disciplinary lines and could be included in team-based instruction.
- No certification credential currently exists for health professionals who address social isolation and loneliness in older adults. A unique certification process or questions added to existing gerontologic certification exams could motivate more health professionals to address these topics in depth.
- Direct care workers are the paid front line of long-term care in the United States and are well positioned to support older people in addressing social isolation and loneliness. Providing education and training to these workers about social isolation and loneliness is essential to their ongoing work.
- Although personal care aides are a growing segment of the direct care workforce, there is a lack of federal and state training requirements for this sector. Instructive curricula and outlines for personal care aides should be created or updated in order to recognize social isolation and loneliness in older adults.
- Researchers and communications strategists in the United States have not produced easily available, research-tested frames, messages, or communications campaigns and tools specific to social isolation and loneliness in older adults, which limits strategic, collective action on this issue.
- Addressing social isolation and loneliness is a community-wide concern and requires that health professionals, direct care workers, and members of the community work together to achieve solutions.
NEXT STEPS AND RECOMMENDATIONS
Broadly based workforce development needs to account for the entire range of the health care workforce within formal degree and postgraduate programs for health professionals and in training programs for direct care workers and community members. Education and training of the health care workforce about addressing social isolation and loneliness will require a broad approach similar to the one used to educate the workforce about addressing the social determinants
of health. It will be necessary to educate and train all members of the health care workforce, including professionals, direct care workers, community health workers, volunteers, family caregivers, and members of the larger community, such as police officers and mail carriers, who provide a broad array of services to or regularly interact with older adults.
Improving Overall Awareness
The 2019 National Academies consensus study report Integrating Social Care into the Delivery of Health Care noted that “activities seeking to increase social and health care integration frequently begin with elevating and sustaining awareness about the influence of social risk and protective factors on health outcomes” (NASEM, 2019, p. 36). Based on the significant evidence base concerning the health and medical impacts of social isolation and loneliness (see Chapters 2 and 3), the committee concluded that, as with other public health issues of the same magnitude, a critical step toward preventing, mitigating, or eliminating those impacts will be to improve awareness among the general public and, specifically for this report, among the health care workforce itself. The committee therefore offers the following goal and related recommendations.
GOAL: Improve awareness of the health and medical impact of social isolation and loneliness across the health care workforce and among members of the public.
RECOMMENDATION 8-1: The U.S. Department of Health and Human Services should advocate for including measures of social isolation and loneliness in major large-scale health strategies (e.g., Healthy People) and surveys (e.g., National Health Interview Survey).
RECOMMENDATION 8-2: Health and aging organizations, relevant government agencies, and consumer-facing organizations should create public awareness and education campaigns that highlight the health impacts of social isolation and loneliness in older adults.
- Health care systems, associations representing all types of health care workers (e.g., American Medical Association, American Nurses Association, American Psychological Association, National Association of Social Workers, American Geriatrics Society, American Association for Geriatric Psychiatry, associations representing direct care workers); health-related organizations (e.g., American Heart Association); consumer-facing, health-related organizations (e.g., AARP); aging professional associations (e.g., American Society on Aging, Gerontological Society of America); aging services organizations (e.g., area agencies
-
on aging, state departments on aging); and organizations working with at-risk older adults (e.g., National Hispanic Council on Aging) should actively communicate information about the health impacts of social isolation and loneliness through print and digital media.
- Organizations representing health plans and providers should include consumer-friendly information about the health impacts of social isolation and loneliness in their repository of patient resources (e.g., where the organization provides information about the self-management of various chronic diseases).
A large-scale, public–private sector investment could build awareness and support among the various clinicians, direct care employers and workers, and community members about the need to address social isolation and loneliness in older adults, creating a groundswell to develop comprehensive training and educational programs. These types of campaigns could have several audiences and purposes. For example, given that direct care workers often have the most interaction with the most vulnerable populations of older adults, the direct care sector could create public education campaigns that build awareness and support among direct care employers and workers about the health impacts of social isolation and loneliness. In addition, groups such as the Frameworks Institute could create a research-based framing strategy—similar to the Reframing Aging initiative—that assists in developing effective, strength-based frames and messages on social isolation and loneliness in older adults, including more vulnerable populations.
Strengthening Education and Training
While research-based evidence is not yet available to support curricular content on specific interventions for social isolation and loneliness in older adults (see Chapter 9), enough is known about the health impacts to warrant broad curricular recommendations for all health professions and careers. Health professions students need to learn about the prevalence of social isolation and loneliness in older adults, about its health outcomes and risk factors, and also about how to assess for these problems. The move toward more comprehensive geriatric assessments by interprofessional teams (e.g., Borenstein et al., 2016) provides an ideal opportunity for evaluating social isolation and loneliness. One example of an evidence-based assessment guide that can be helpful is Fulmer SPICES, which was developed as part of the Nurses Improving Care for Health System Elders project (Fulmer, 2007). This guide provides assessment criteria for hospitalized older adults for six key problems: “sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown” (p. 40). While social isolation and loneliness are not included, each of these key problems can lead to or result from social isolation and loneliness and can indicate the need to look more deeply into causative factors and outcomes. The Fulmer SPICES tool
can be used in conjunction with an evidence-based assessment tool that assesses social isolation and loneliness to gauge the influence of social isolation and loneliness on patient health.
Health professionals also need to learn how to work directly with older adults and their significant others to support and encourage ways to prevent or reduce social isolation and loneliness. They need to know how to make and follow up on referrals to community services that may be helpful or that may specifically be intended to address social isolation and loneliness. This includes learning to work with direct care workers (e.g., home health aides, personal care workers), community health workers, family caregivers, and lay community members as part of a team-based approach to helping older adults. They also need to learn how to work with community partners to develop, implement, and evaluate programs for preventing and ameliorating social isolation and loneliness in older adults. Competency in each of these areas will become increasingly important for health professionals as systems of care are developed for preventing and intervening with social isolation and loneliness in older adults. Therefore, the committee offers the following goal and recommendations:
GOAL: Strengthen ongoing education and training related to social isolation and loneliness in older adults for the health care workforce.
RECOMMENDATION 8-3: Health professions schools and colleges as well as direct care worker training programs should include education and training related to social isolation and loneliness in their curricula, optimally as interprofessional team-based learning experiences.
- Health education and training programs should include information on clinical approaches to assessing and intervening when an older adult is at risk for social isolation and loneliness.
- As evidence on effective interventions develops, health education and training programs should provide education on integrating care related to social isolation and loneliness into clinical practice and as part of discharge planning, care coordination, and transitional care planning with community organizations.
RECOMMENDATION 8-4: Health professional associations should incorporate information about the health and medical impacts of social isolation and loneliness on older adults in their advocacy, practice, and education initiatives.
- Health professional associations should include social isolation and loneliness in conference programming, webinars, toolkits, clinical guidelines, and advocacy priorities.
RECOMMENDATION 8-5: Health professional associations, membership organizations, academic institutions, health insurers, researchers, developers of education and training programs, and other actors in the public and private sectors should support, develop, and test different educational and training approaches related to the health and medical impacts of social isolation and loneliness in older adults across different segments of the health care workforce (including health care professionals and direct care workers) in order to determine the most effective ways to enhance competencies. In addition to initial clinical education, these approaches should apply to professional education, continuing education modules, online learning, and other forms of lifelong learning.
Concerning the above recommendations the committee notes that, as discussed in Chapter 10, depending on the complexity of the knowledge to be disseminated or the evidence-based practices to be implemented, a variety of teaching strategies can be considered, including train-the-trainer programs, high-fidelity simulation, and ongoing point-of-care coaching (Brownson et al., 2018a; Titler and Anderson, 2019). Additionally, resource materials could be made available to faculty for inclusion in health professions courses. This information should be included in formal education programs, continuing education, and just-in-time learning. Other educational opportunities include the dissemination of information and resource availability through presentations at scientific meetings and webinars, publications in peer-reviewed journals, toolkits, and other forms of media. Toolkits should contain enough detail for use in practice, including modules, slides, reading materials, interactive exercises, case studies, and other tools that can support a variety of health professional education programs. Real-time and archived webinars and podcasts with faculty development materials to support the inclusion of content and learning activities could be helpful. Aside from developing educational opportunities specific to social isolation and loneliness, the committee recognizes that there are existing educational opportunities that could incorporate issues of social isolation and loneliness, such as those focused on the social determinants of health and those that address the inclusion of social care needs into clinical practice. Finally, as the evidence for interventions evolves, these educational and training opportunities need to expand to include new and updated evidence-based practices for preventing, assessing, and treating the negative health and medical impacts of social isolation and loneliness.
This page intentionally left blank.
























