4
Risk and Protective Factors for Social Isolation and Loneliness
Aging, independent of other factors, does not cause social isolation or loneliness. However, people who are 50 years of age and older are more likely to experience many of the risk factors that can cause or exacerbate social isolation or loneliness, such as the death of loved ones, worsening health and chronic illness, new sensory impairment, retirement, or changes in income. The relationships between risk factors and social isolation or loneliness can be bi-directional in that being socially isolated or lonely can affect health, while these same health conditions can make experiencing social isolation or loneliness more likely. This chapter focuses on the risk factors for social isolation and loneliness while also providing some context regarding the health impacts of these two factors, reflecting the frequent bi-directionality of these relationships. (See Chapters 2 and 3 for a fuller discussion of the health impacts of social isolation and loneliness.) When considering the risk factors for social isolation and loneliness, it should be noted that some factors may increase the risk of negative health effects while other factors may lower those risks. Mechanisms and moderators will be discussed in Chapter 5.
This chapter reviews the risk and protective factors for social isolation and loneliness, including predisposing physical health factors (e.g., chronic diseases, functional impairments); psychological, psychiatric, and cognitive factors (e.g., depression, anxiety, dementia); socio-cultural factors (e.g., social supports, disruptive life events); and social environmental factors (e.g., transportation, housing). The chapter then summarizes the risks of social isolation and loneliness among specific subpopulations. As described in earlier chapters, research outcomes pertaining to social connection have included a variety of related terms; the specific terms used in individual studies are noted throughout the chapter for greater clarity. It should be kept in mind that the material presented in this chapter provides a
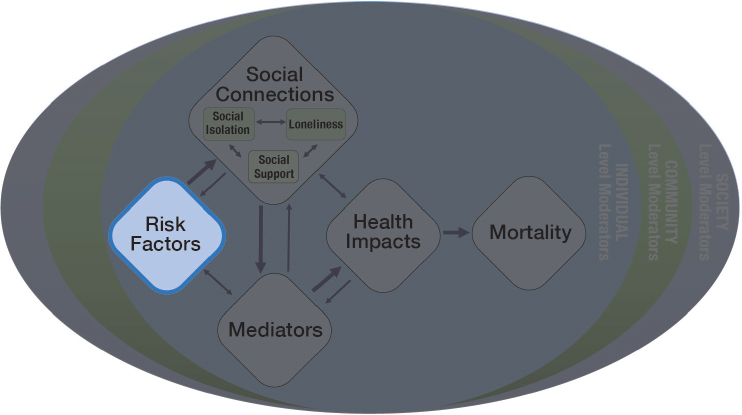
summary of the relevant published literature rather than a comprehensive review of these topics. Gaining a broad understanding of risk factors for social isolation and loneliness and also elucidating which factors are most closely linked to them can lead to new initiatives to improve health outcomes at primary, secondary, and tertiary stages of prevention. This chapter represents the portion of the committee’s guiding framework related to risk factors (see Figure 4-1). Given the complexity of the terminology used in relation to social isolation and loneliness, a reminder of key definitions is provided in Box 4-1.
PHYSICAL HEALTH FACTORS
Various physical health factors are related to social isolation and loneliness, including many common chronic diseases, impairments, and geriatric syndromes. As mentioned earlier, these relationships are often bi-directional. That is, social isolation or loneliness may increase the chances of developing a chronic health condition (see Chapter 3), while, conversely, a chronic health condition may contribute to social isolation or loneliness by interfering with the quality, quantity, or structure of relationships or by worsening pathophysiological processes. The relationships between combinations of conditions and social isolation or loneliness are less well studied, but having multiple chronic conditions has been associated with a lower participation in social activities (Cantarero-Prieto et al., 2018). Similarly, among older adults discharged after an acute coronary syndrome, a greater number of co-existing chronic conditions has been associated with having a limited social network (Tisminetzsky et al., 2016). This section focuses on the role of physical health as a risk factor for experiencing social isolation or loneliness.
Chronic Disease and Conditions
Roughly 60 percent of all adults and about 80 percent of adults aged 65 and older have at least one chronic disease (e.g., heart disease, diabetes, cancer, stroke), and 77 percent have at least two chronic diseases (CDC, 2019; NCOA, 2019). Research indicates that some chronic diseases and conditions can be risk factors for social isolation and loneliness. There is robust evidence, for example, that cardiovascular disease and stroke can increase the risk of social isolation and loneliness and also of low social support; conversely, there is also research indicating that people who have cerebrovascular or cardiovascular disease may have worse outcomes if they are socially isolated or lonely (Air et al., 2016). The deficits that occur as a result of having a stroke can increase the risk of social isolation, which in turn can affect recovery from the stroke (Alun and Murphy, 2019; Glass and Maddox, 1992; Hinojosa et al., 2011). For example, lasting symptoms of stroke may include visual field deficits and dysphagia, which can impair an individual’s ability to interact with others (Cichero and Altman, 2012; Rim et al., 2020).
Other common chronic conditions, such as chronic obstructive pulmonary disease (Castelino et al., 2018) and advanced heart failure (Leeming et al., 2014) as well as many less common and less frequently studied conditions may also increase the risk for social isolation or loneliness. The English Longitudinal Study of Ageing has revealed, for instance, that chronic pain (largely due to musculoskeletal
disease) sometimes results in a reduction in physical and social activity, which may lead to social isolation or reduced social participation (Blyth and Noguchi, 2017). A small study of people with wounds infected with methicillin-resistant staph aureus found that fears of infecting someone else or of being rejected made social isolation more likely (Andersson et al., 2011), and older adults living with HIV may face greater social isolation and loneliness as a result of decreased social participation and engagement due to a loss of friends and social networks and to HIV-related stigma (Greene et al., 2018; Greysen et al., 2013; Nachega et al., 2012; Rueda et al., 2014). Others specific conditions that may influence social isolation and loneliness include Parkinson’s disease, multiple sclerosis, cancer, and spinal cord injury (Andreadou et al., 2011; Benito-León et al., 2009; Buhse, 2015; Deckx et al., 2014; Newman et al., 2016).
Geriatric Syndromes and Impairments
In addition to specific diseases, geriatric syndromes1 and impairments may also increase social isolation and loneliness as a result of the associated embarrassment and stigma or because of associated deficits in communication or comprehension, limited functional abilities, or impaired mobility. For example, oral-health-related quality of life is an independent risk factor for loneliness among older adults, possibly due to embarrassment or stigma (Rouxel et al., 2017; Tonetti et al., 2017). These issues may be exacerbated among some racial or ethnic minorities and low-income older populations who lack preventative and corrective dental care (Griffin et al., 2012).
Frailty and Functional Status
Frailty is a medical syndrome that involves a vulnerability to stressors and a greater risk of worse outcomes from new or co-existing conditions. Different frailty assessment tools differ in their questions pertaining to social connection, and some frailty measures lack a social connection question altogether (e.g., the Fried phenotype defined frailty using five criteria: weight loss, exhaustion, low physical activity, slowness, and weakness) (Fried et al., 2001; Galambos, 2017a,b). This variability contributes to an incomplete understanding of the association of frailty with social isolation and loneliness and the extent to which it is bi-directional. Over a 6-year period the English Longitudinal Study of Ageing found that loneliness predicted frailty for men and women, while social isolation predicted frailty only for men (Gale et al., 2018). These findings provide
___________________
1 Geriatric syndromes are “clinical conditions common among older adults that often do not fit into discrete disease categories. Examples include delirium, depression, falls, sensory impairment, incontinence, malnutrition, and osteoporosis. The syndromes tend to be multifactorial and result from an interaction between identifiable patient-specific impairments and situation-specific stressors” (IOM, 2008, p. 43).
evidence for frailty as a health outcome related to low social connections. In a study based on patient interviews conducted 1 week after discharge from a hospital stay, frailty was found to be a risk factor for social isolation (Andreasen et al., 2015). The co-existence of other geriatric syndromes, such as urinary and fecal incontinence, with frailty compounds the specific contribution of frailty to social isolation and loneliness.
Functional status (measured by factors such as gait speed or difficulties in the activities of daily living) is bi-directionally associated with social isolation and loneliness. Loneliness predicts long-term care admission, independent of functional status (Hanratty et al., 2018). Patients’ perceived social isolation may moderate the relationship between a chronic illness, such as lower back pain, and the degree of functional impairment that they experience related to that illness (Oliveira et al., 2015). Fear of falling has been associated with the risk of falling, poorer mental health, and social isolation (Kumar et al., 2014). Older adults who restrict their activities or avoid leaving their home due to a fear of falling may increase their risk of becoming socially isolated or lonely (Finch et al., 2014; Parry et al., 2016). A recent study also found an association between frailty and social isolation and a fear of falling in older adults; however, physically frail study participants who were also socially isolated reported having fewer falls than participants who were either physically frail or isolated, but not the two combined (Hayashi et al., 2020).
Incontinence
Urinary incontinence increases the risk of social isolation because individuals tend to avoid activities with limited bathroom access or avoid social contacts altogether (Becher et al., 2013). Among the women surveyed in the National Social Life, Health, and Aging Project (Yip et al., 2013), daily urinary incontinence was associated with often feeling isolated. In one large study urinary incontinence was found also to be associated with greater loneliness, but this effect was largely explained by comorbid depression (Fultz and Herzog, 2001; Ramage-Morin and Gilmour, 2013; Stickley et al., 2017). Fecal incontinence increases the chances of nursing home referral and has effects on social isolation that are similar to those of urinary incontinence (Ditah et al., 2013). Furthermore, the social isolation of caregivers may be affected by the incontinence of their care recipients (Santini et al., 2016).
Sensory Impairment
Hearing loss contributes to both social isolation and loneliness (Davis et al., 2016; Mick et al., 2014; Ramage-Morin, 2016; Strawbridge et al., 2000; Wallhagen et al., 1996). Hearing loss has been associated with being less willing to engage in social interactions, and living in a community where access to hearing health
care is limited—such as in some rural communities—can lead to greater isolation than living in an urban community where these services are more accessible (Hay-McCutcheon et al., 2018). Untreated hearing loss has been associated with greater social isolation in the adult population under 70 years of age in particular (Mick and Pichora-Fuller, 2016). Hearing loss as measured by both self-report and an objective measure has been associated with loneliness, particularly among individuals who do not use hearing aids (Mick and Pichora-Fuller, 2016; Pronk et al., 2011). Hearing loss contributes to the broader category of communication difficulty, and such difficulty often has multi-factorial causes. Communication disorders have been linked to social isolation, reduced social participation, and higher rates of loneliness (Palmer et al., 2016).
Visual impairment is associated with loneliness and may be moderated by self-efficacy, which may thus be a target for intervention (Alma et al., 2011). Self-reported visual impairment is associated with social isolation, even after adjustment for demographics, chronic illness, functional limitations, and disability, and it may be a stronger predictor of social isolation than a clinical measure of acuity (Coyle et al., 2017). Furthermore, some data suggest that the spouse of a person with visual impairments is at greater risk for social isolation (Strawbridge et al., 2007).
Dual sensory (vision and hearing) impairment has been associated with loneliness (Guthrie et al., 2018). In one study, the highest rates of loneliness—17 percent—were in the group that experienced dual sensory impairment in addition to cognitive impairment, while the group without any impairments had a 9 percent prevalence of loneliness (Guthrie et al., 2018). Both impairments are associated with worse quality of life, in part due to the mechanism of social isolation (Schneider et al., 2011; Tseng et al., 2018). Even olfactory dysfunction may be associated with loneliness (Sivam et al., 2016).
PSYCHOLOGICAL, PSYCHIATRIC, AND COGNITIVE FACTORS
Psychological symptoms, syndromes, and stressors can all influence whether an individual experiences loneliness or becomes socially isolated. Several of these factors, including anxiety and depression as well as cognitive factors such as dementia, are briefly discussed below. The impacts of social isolation and loneliness on subsequent depression and anxiety and on cognitive decline and incident dementia are summarized in Chapter 3.
Anxiety and Depression
Social isolation and loneliness are more common in older adults with depressive and anxiety disorders than in their non-depressed and non-anxious peers (Evans et al., 2018; Lim et al., 2016). Psychiatric disorders such as major depression, generalized anxiety disorder, and social anxiety disorder have been shown to increase the risk of developing loneliness during middle and late adulthood
(Domènech-Abella et al., 2019; Falk Dahl and Dahl, 2010; Lim et al., 2016; Luo et al., 2012; McHugh Power et al., 2020). Loneliness, in turn, has been linked to increasing social isolation (likely due to the negative social biases and avoidance characteristic of lonely individuals) and to higher rates of depression and anxiety over time (Cacioppo et al., 2010; Domènech-Abella et al., 2019; Luo et al., 2012).
The relationship between depression and loneliness is bi-directional, and these constructs are closely associated. Yet, depression and loneliness are not the same. Depression, particularly major depression, is a clinical syndrome characterized by persistent feelings of sadness or loss of interest and such symptoms as sleep problems, decreased appetite, loss of energy, difficulty concentrating, and suicidal thoughts. Loneliness is not a core diagnostic feature of depression but may be an associated symptom. In some older adults, depression is accompanied by broad deficits in social function and well-being, including high levels of loneliness, low social support, and fewer social connections (Barger et al., 2014; Domènech-Abella et al., 2017). In other older adults depression has been associated with high levels of loneliness that are unrelated to social network size, the level of social support, or individual factors such as personality traits and cognitive function (Domènech-Abella et al., 2017; Evans et al., 2018; Peerenboom et al., 2015). Loneliness may stem from depression-related cognitive biases in which social interactions are appraised more negatively or experienced as less rewarding (Burholt and Scharf, 2014; Lewis et al., 2017). Older adults with generalized anxiety disorder may also be vulnerable to high levels of loneliness even with levels of social contacts that are equivalent to those without anxiety (Evans et al., 2018). Personality characteristics, such as extraversion, neuroticism, and resilience, have been shown to increase the risk of loneliness as well as to moderate this risk in the setting of depression and anxiety (Peerenboom et al., 2015; Teo et al., 2013a; von Soest et al., 2020; Wagner et al., 2016).
Cognitive Function and Dementia
Social withdrawal and other changes in social function are recognized features of dementia in neurodegenerative disorders such as Alzheimer’s disease, frontotemporal dementia, Parkinson’s disease, and Lewy body dementia (McKhann et al., 2011). These changes can also arise in pre-dementia stages of impairment when neurocognitive deficits are less severe or not yet apparent (d’Oleire Uquillas et al., 2018; Donovan et al., 2016; Ismail et al., 2016).
Primary deficits in the core cognitive domains such as memory, reasoning, or language skills may degrade social function. With increasing cognitive impairment, individuals often disengage from community groups and reduce their social ties as they are experiencing parallel functional losses in other aspects of daily living (Morris, 1993). This global process culminates in severe deficits in comprehension, communication, and interpersonal function in late dementia (Reisberg et al., 1982).
Neurodegenerative disorders may also give rise to specific impairments in such social processes as interpreting information from faces (social perception), recognizing the thoughts and feelings of others (theory of mind), displaying empathy and regulating emotions (emotional processing), and behaving within social norms (Desmarais et al., 2018).
Altered neuropsychiatric function may also impair social functioning in individuals who are affected by neurodegenerative disorders. For example, social withdrawal may be part of a broader apathy syndrome, a neuropsychiatric state that is common across dementia types (Lanctôt et al., 2017). Misperceptions or overestimations of social threat may predispose a person with dementia to agitation and aggression (Rosenberg et al., 2015). Anxiety or depressive symptoms may underlie or contribute to social avoidance or withdrawal (Geda et al., 2013).
A small number of studies have examined the experience of loneliness in persons with dementia. A single population-based study of 589 Swedish old adults with a mean age of 84 years found that loneliness was more prevalent in those with dementia (33 percent) than in those without dementia (22 percent) (Holmén et al., 2000). Dementia caregivers, particularly spouses, are also at risk for greater loneliness and depression both during the course of disease and after the caregiving ends (Adams, 2008; Eloniemi-Sulkava et al., 2002). In semi-structured interviews of 70 persons with early-stage dementia and their caregivers, the study participants with dementia spoke of experiencing relationship loss and of the importance of having meaningful relationships and people to converse with (Moyle et al., 2011). The loss of memory function was acknowledged as a barrier to social relationships, whereas an involvement in arts, crafts, and music was identified as a way of reducing feelings of loneliness (Moyle et al., 2011). Caregivers tended to perceive loneliness from observed emotions and behaviors even if loneliness was not explicitly expressed by the person with dementia (Moyle et al., 2011).
Other research in dementia care has led to the concept of “unmet needs” among persons with dementia who are unable to communicate or fulfill their own basic needs (Black et al., 2013; Cohen-Mansfield, 2001). This work has provided insights into the importance of social relationships to persons with dementia, even in late stages. In a review of studies of persons with dementia living in nursing homes, those interviewed identified meaningful relationships and support for grief and loss as two of their eight main concerns (Shiells et al., 2019). The residents with advanced dementia in particular expressed having a fear of loneliness. Many of these participants wrongly believed that family had not visited them even when they had (Cahill and Diaz-Ponce, 2011). In a separate study, 70 percent of nursing home residents with dementia reported feelings of loneliness (Cohen-Mansfield et al., 2015).
Studies of agitated behaviors in nursing home settings have found that verbal agitation (e.g., constant requests for attention, complaining, screaming) was more
common in nursing home residents who were cognitively impaired (Cohen-Mansfield and Libin, 2005) and in those who were lonely (Cohen-Mansfield et al., 2015). An understanding of behavioral symptoms as a form of distress related to unmet needs has led to the development of interventions to reduce loneliness and behavioral symptoms in nursing home residents. In a study of 30 nursing home residents with dementia, both simulated family presence and a music intervention reduced verbal agitation more than usual care (Garland et al., 2007). In a loneliness-focused study of 38 nursing home residents with and without cognitive impairment, individuals who received animal-assisted therapy with either robotic or living dogs, but not those in the control group, reported reduced loneliness ratings (Banks et al., 2008). (See Chapter 8 for more on interventions.)
Loneliness and social isolation are not currently assessed in standard dementia care (Johnston et al., 2011; Sanders et al., 2017), and the established instruments for measuring these constructs have not been validated in persons with dementia. At the same time, there is an emerging interest in understanding how to measure engagement and provide effective opportunities for meaningful activity and engagement in persons with dementia, including those with advanced disease (Cohen-Mansfield et al., 2017).
SOCIAL AND CULTURAL FACTORS
This section explores the societal and cultural factors that can affect how people interact with their environments and whether they experience social isolation or loneliness. Such factors include social support characteristics (including marital status and the quality of relationships with family and friends or pets) and the occurrence of disruptive life events (including bereavement, illness, and retirement).
Social Support Characteristics
Various characteristics of a society, including customs, lifestyles, and values, can affect an individual’s everyday interactions—with family members, friends, or complete strangers—and influence how people live their lives and perceive their places in society. This interplay between individuals and their social and cultural milieus has given rise to a wide array of inter-related research areas. The potential impacts of social support networks as well as the influence of different relationships—with spouses and family members, friends and neighbors, or caregivers—are discussed below.
Impact of Social Support Networks
Individuals’ social support networks directly affect how they interact with and perceive their environments. The individuals who make up a person’s network
(e.g., family members, friends, caretakers, spouse, and neighbors) can play important roles in the person’s life and lessen his or her chances of experiencing social isolation or loneliness. Having an extensive social network is not required in order to achieve a rewarding social network, but rather the rewards of a social network are greatest when the relationships that do exist are of high quality (Chatters et al., 2018; Cohen-Mansfield et al., 2016; Lauder et al., 2006; Pinquart and Sörensen, 2001; Stokes, 1985). Supportive relationships can decrease self-reported loneliness, while difficult or unfulfilling relationships can increase feelings of loneliness (Cohen-Mansfield et al., 2016; Shiovitz-Ezra and Leitsch, 2010). Lonely older adults (mean participant age = 68.5) reported less frequent sexual activity and reduced feelings of intimacy, although not less frequent sexual thoughts, in a study using items from the UCLA Loneliness Scale; however, the directionality of this association was not determined (Kolodziejczak et al., 2019). Relationships with one’s family or spouse have been shown to be beneficial for some facets of health, while relationships with friends, neighbors, community members, and others can help prevent poor mental health and psychological distress (Christakis and Allison, 2006; Fiori et al., 2006; Haslam et al., 2014; Kiecolt-Glaser and Newton, 2001). The totality of these relationships—voluntary and otherwise—can help lead an individual live a life with a sense of meaning, value, and interconnection (Berkman and Glass, 2000).
Family and Marriage
Family can be an important source of social support for older adults, providing social and emotional connection as well as contributing to an individual’s financial and physical well-being (Verdery and Margolis, 2017). Individuals who lack family are more apt to be socially isolated and to experience higher rates of loneliness (Verdery and Margolis, 2017).
Marriage can also protect against loneliness and conditions such as poor cognitive function, stress, and dementia; however, the benefits gained from a spousal relationship are proportional to the overall quality of that relationship, including whether a spouse is considered a trusted confidant (Gow et al., 2007; Håkansson et al., 2009; Hawkley and Kocherginsky, 2018; Hawkley et al., 2008; Nicolaisen and Thorsen, 2017; Qualter et al., 2015; Stack, 1998; Victor and Bowling, 2012; Xu et al., 2016). The close, long-term nature of the spousal relationship tends to make an individual’s partner the most likely person to provide support if and when assistance is needed (Ha et al., 2019). However, the spousal relationship can be either beneficial or detrimental, as loneliness has been found to be inversely associated with spousal support (Hawkley and Kocherginsky, 2018). In particular, remaining in an unhappy relationship can negatively affect an individual’s health and well-being and can be the source of ongoing emotional distress (Evans et al., 2019; Xu et al., 2016). Furthermore, negative spousal behaviors are associated with poorer physical health, and the adverse effects of marital
strain are greater at older ages (Bookwala, 2005; Robles and Kiecolt-Glaser, 2003; Umberson et al., 2006).
Relationships with other family members can also affect an individual’s likelihood of being lonely, as close family bonds are often the source of social, economic, physical, and other forms of support (Berkman et al., 2000; Redfoot et al., 2013; Verdery and Margolis, 2017). As with other social relationships, the amount of support realized from close familial ties varies depending on the geographical distance between family members, the amount of interpersonal contact (in person or through other means), and each person’s willingness to be emotionally and personally invested in maintaining mutually beneficial relationships (Quirke et al., 2019; Verdery and Margolis, 2017). Among older African Americans, family relationships often take precedence over relationships with friends, and social networks tend to be primarily made up of family members (Chatters et al., 2018; Cornwell et al., 2008; Griffin et al., 2006; Taylor et al., 2013). Some families choose to create intergenerational co-residences or live in very close proximity; however, these familial living arrangements are not as prevalent in the United States as in other parts of the world, and their impact on social isolation or loneliness in older adults is mixed (Caputo, 2019; Takagi and Saito, 2019; Teerawichitchainan et al., 2015; Tian, 2016).
Grown children can also provide a measure of support to parents, although their existence or presence is not a panacea for social isolation or loneliness (Cohen-Mansfield et al., 2016; Nicolaisen and Thorsen, 2017). Parent–child relationships are subject to the same limitations described above for social relationships, and therefore these relationships can range in their quality and level of support. Virtual interactions with children and grandchildren are becoming more common, but the success of these interactions is dependent on the computer literacy of the participant (regardless of age), the comfort level with this form of communication, and the availability of and accessibility to computers with reliable Internet access (Cohen-Mansfield et al., 2016). (See Chapter 8 for more on the use of technology.) Increasingly, couples—both unmarried and married—are not having children; in 2018 the number of births in the United States reached its lowest level in 32 years (Hamilton et al., 2019; Verdery and Margolis, 2017). The effect of these demographic dynamics on the rates of social isolation and loneliness among future generations of older adults is unknown.
Single Adults
Single adults—unmarried, widowed, or divorced—may experience social isolation or loneliness differently than adults with partners. While single adults are not destined to be lonely, feelings of loneliness can be more prevalent in this population because of such factors as the lack of a trusted confidant or the lack or loss of a partner (Paúl and Ribeiro, 2009; Theeke, 2009, 2010; Verdery and Margolis, 2017). For others, remaining single is a conscious choice, and many
older couples opt to forego marriage and choose cohabitation without marriage (Brown et al., 2012; Copen et al., 2012; de Jong Gierveld, 2004; Verdery and Margolis, 2017). Rates of divorce are also increasing in adults over 50 years of age, with divorce rates highest among individuals who have been married two or more times, among those with less education and a lower income, and among African Americans (Brown and Lin, 2012).
Regardless of the circumstances, single adults are more apt to live alone, which can tend to make them more lonely and isolated than people who cohabitate (Evans et al., 2019; Finlay and Kobayashi, 2018; Perissinotto and Covinsky, 2014). For lesbian, gay, or bisexual individuals, living alone may be a symptom of larger discriminatory practices or societal stigma (Fredriksen-Goldsen et al., 2013; Kim and Fredriksen-Goldsen, 2016). Some older adults who live alone may go for days without seeing or talking with another person (Finlay and Kobayashi, 2018). Living alone should not necessarily be equated with being sequestered from society, however, as many people who live alone still enjoy active social lives and are no more lonely or isolated from friends than those who live with others (Evans et al., 2019). For some, periods of solitude represent opportunities to reenergize, relax, or engage in other pursuits. The disparate reactions to solitude may be explained by differing reasons for being alone; that is, some individuals may choose to be alone, while others may lack opportunities to interact with others.
Friends and Neighbors
Unlike the case with their family members, individuals have choices concerning whom they become friends with, and these non-familial relationships have the potential to affect social isolation or loneliness. Generally, friendships are based on individuals having similar interests, activities, hobbies, experiences, or beliefs and are likely to occur among people in the same peer group (Chatters et al., 2018; Ha et al., 2019). Feelings of loneliness can be minimized by having friends who can be relied on (Henning-Smith et al., 2019). Though some friendships are situational or fleeting, friendships that last into older ages tend to be characterized by relationships between individuals who share similar experiences and backgrounds. These long-term friendships tend to be superior in quality and richness than friendships that have not stood the test of time (Nicolaisen and Thorsen, 2017; Pinquart and Sörensen, 2000). On the extreme end of the friendship continuum are older patients who have been identified as “unbefriended.” This term is used to describe individuals who, for example, are incapacitated and unable to make medical decisions for themselves; lack an advanced directive; and lack friends, family, or an authorized surrogate to assist in making medical decisions (Farrell et al., 2017).
Proximity to other individuals can influence whether friendships develop. Neighbors can often provide a measure of support when family members or close friends are not geographically close, but engagement with neighbors tends to be
more limited in commitment and scope (Ha et al., 2018; Messeri et al., 1993; Nocon and Pearson, 2000). Communicating with neighbors or others via the telephone can also have an impact on one’s sense of social isolation or loneliness. Loneliness was found to be increased in individuals who had fewer daily phone calls; this was most evident for people who received fewer incoming calls (Petersen et al., 2016). Whether one lives in a rural or an urban area can also influence the likelihood and quality of friendships. (See discussions on rural versus urban living later in this chapter.)
Caregivers
With the rapid aging of the population, the number of older adults who need care continues to grow rapidly (NASEM, 2016b). In the 2-year period of 2015–2016, more than 41 million people provided unpaid elder care for adults 65 years of age and older (BLS, 2017). Typical services provided by family and friends range from routine household activities (e.g., housework, food preparation, transportation) to providing direct physical or medical care (e.g., providing exercise, bathing, or toileting assistance or dispensing medication) (BLS, 2017). Most often a spouse, partner, or adult child will fulfill this family caregiver role, but caregiving responsibilities can also be undertaken by other family members (e.g., siblings or elderly parents), friends, neighbors, or volunteers, and they can be provided in private homes, assisted care, or retirement facilities (BLS, 2017; Li and Loke, 2013).
Increasingly, medical care for older adults is taking place in private homes, often for long periods of time. As a result, home care that involves complex and diverse care needs is more often falling on family caregivers with or without assistance from a member of the formal health care workforce (Li and Loke, 2013; Ris et al., 2019). Having care provided in the home can help older adults and their caregivers maintain relationships with family, friends, and others in the community; however, social isolation and loneliness are often byproducts of this arrangement (Evans et al., 2019; Wiles et al., 2012). The quality of the relationship between the patient and an informal family caregiver is an important factor in determining the effectiveness of these arrangements. For example, better relationship quality between patients and their informal family caregivers has been linked to a reduced risk for patient mortality (Hooker et al., 2015). But older adults and their caregivers often must navigate new or different interpersonal roles, responsibilities, or routines and deal with stressful, emotional, and sometimes life-altering changes. These difficult situations can impede communication between older adults and their caregivers or visitors, creating feelings of social isolation or loneliness. This can be especially true if friends’ visits taper off over time (Northcott et al., 2016).
In addition to the day-to-day interpersonal challenges faced by family caregivers and older adults, families can also experience negative psychological, financial, and social effects; these effects can be especially acute for female spouses,
as they generally bear the largest burden of care (Li and Loke, 2013; Riffin et al., 2019; Zivin and Christakis, 2007). Caregivers commonly suffer from physical issues such as illness, loss of appetite or sleep, or exhaustion as well as mental health issues, trouble maintaining relationships with friends, or difficulty participating in community or social activities (Blum and Sherman, 2010; Dhruva et al., 2012; Haines et al., 2018; Li and Loke, 2013). These difficulties can be compounded by such factors as immigration status, language and cultural barriers, stigma or discrimination issues related to an older adult’s sexual orientation, or the specific needs of patients (Kim and Fredriksen-Goldsen, 2016; Kim, H. J., et al., 2016; Moukouta et al., 2017; Shiu et al., 2016). It can be particularly challenging to care for older adults with mobility issues or those who suffer from dementia or other mental illnesses (Riffin et al., 2019).
Human–Animal Interactions
Interacting with an animal or a pet has long been thought to have health-related benefits, but research into the benefits of these human–animal interactions, including their effects on loneliness or social isolation, has had mixed results (Gilbey and Tani, 2015; Krause-Parello and Gulick, 2013; Needell and Mehta-Naik, 2016; Stanley et al., 2014). Needell and Mehta-Naik (2016) examined the impact of pet ownership on the risk and severity of geriatric depression and concluded that “loneliness and social isolation seemed to be ameliorated by pet ownership” (p. 5). Conversely, a review carried out at about the same time that looked at the association between companion animal interactions and loneliness found “no convincing evidence that companion animals can help to alleviate loneliness” (Gilbey and Tani, 2015, p. 195). The studies agree in their observations that research is sparse and insufficient in this area and that many of the available studies are underpowered or inadequately designed.
Other aspects of human–animal relationships may be related to subsequent social isolation or loneliness in older adults. Interactions with animals can promote social interactions and participation; can add structure, routine, meaning, or purpose to an individual’s day; can increase exercise and physical activity opportunities; and can provide emotional support (Brooks et al., 2018; Friedmann and Krause-Parello, 2018; Gee and Mueller, 2019; Hui Gan et al., 2019; Mueller et al., 2018). Dogs may serve as a stimulus for social interactions and engagement because daily walks with pets have been found to increase the likelihood of engaging with others and increasing one’s sense of community (McNicholas and Collis, 2000; Toohey et al., 2013). A study by Muraco et al. (2018) found that interacting with a companion animal was also associated with increased perceived social support, emotional support, and companionship among older pet owners (older than 65 years of age) in the lesbian, gay, bisexual, and transgender community, especially among individuals who were disabled or who lacked social networks. On the other hand, the emotional difficulties that pet owners may experience when a
pet is ill or dies can rival the effects of caring for a sick family member or coping with the trauma of the death of a close relative (Friedmann and Krause-Parello, 2018; Muraco et al., 2018).
Disruptive Life Events
At any age people can experience disruptive life events that alter their interpersonal relations and how they perceive their lives or their feelings of isolation and loneliness. While older adults are not unique in having these life-altering experiences, some disruptive events are more likely to occur, or to occur at a greater frequency, for people over the age of 50. Such disruptive life events include bereavement, illness or poor health, and retirement. Although research on these topics is sparse, it provides insight into how these experiences can disrupt people’s lives and how they could lead to social isolation or feelings of loneliness.
Bereavement
The loss of a loved one—be it a child, sibling, spouse, partner, or friend—can result in a critical loss of emotional intimacy and everyday support. Bereavement leads to feelings of sadness and loneliness in grieving relatives and friends, and in some cases these feelings can lead to individuals becoming socially withdrawn, isolated, or depressed and can also affect an older adult’s risk for premature mortality (Fried et al., 2015; Holm et al., 2019; Robinaugh et al., 2014; Roelfs et al., 2012). The extent of symptoms associated with grieving can vary depending on the cause of death, when it occurred, the context in which the death occurred, and whether the grieving party believes the deceased individual may have hastened his or her death through habits or lifestyle (Carr, 2009; Fried et al., 2015). Family caregivers may have an especially difficult time after the passing of a loved one under their care because the death may result in the loss of a companion or friend as well as the loss of the personal pride, purpose, or satisfaction they derived from providing care (Holtslander et al., 2017). The loss may be particularly acute when caregivers’ responsibilities have compromised their regular social network while they were providing care, thus leaving them with diminished social support or feelings of isolation after the loved one’s death (Holtslander et al., 2017).
The death of a spouse typically increases feelings of loneliness in the surviving spouse, and these feelings can act as a gateway to subsequent depressive symptoms (Fried et al., 2015). Many widowed individuals report that loneliness is something they cope with on a daily basis (Fried et al., 2015). Data from more than 500 million persons examining spousal bereavement, which increases the risk of social isolation and loneliness, revealed that, after adjusting for age, widowers had a 23 percent increased risk of death in any given year compared with married people (Roelfs et al., 2012). (See Chapter 2 for additional information on mortality risk.) In another study, late-life bereavement was found to be associated with
decreased mortality in widows who had cardiovascular disease and with increased mortality in widowers who did not have cardiovascular disease (Stahl et al., 2016). The authors suggested that the decreased mortality in widows could be due to a decrease in stress or in exposure to suffering or to an increase in self-care after the death of the spouse. Over the long term, however, having been widowed is an enduring risk factor for loneliness in late life, regardless of subsequent marital status (von Soest et al., 2020). Men have a higher likelihood of adjusting poorly to widowhood than women and also have greater feelings of loneliness (Carr et al., 2018). Male veterans may be the exception to this, however; research indicates that some veterans who were exposed to death while serving in the military may experience less loneliness than civilian widowers (Carr et al., 2018). Social support provided by family or friends has been shown to be more helpful for grieving spouses than support from other sources; support from family and friends can help restore function and a sense of cohesion (Chow et al., 2018; Merz and de Jong Gierveld, 2016; Utz et al., 2014). Support is most helpful when it is readily available and when the surviving partner has the opportunity to freely express himself or herself (Merz and de Jong Gierveld, 2016; Utz et al., 2014). Psychological resilience (e.g., emotional stability, extraversion, and conscientiousness) is associated with a more favorable resolution of loneliness in bereaved older adults (Spahni et al., 2015). Addressing the risk factors for loneliness in bereaved individuals may be an important way to reduce the risk of psychiatric morbidity and help shorten the bereavement period and alleviate suffering (Chow et al., 2018; Robinaugh et al., 2014).
Illness and Poor Health
Poor health in older adults has been associated with increased loneliness, and chronically ill individuals are especially vulnerable to becoming socially isolated (Goll et al., 2015; Holley, 2007; Merz and de Jong Gierveld, 2016). Chronic illness is associated with emotional or psychological issues, mobility limitations, a lack of or limitation in transportation or employment options, new or ongoing issues related to coping with disabling conditions, and strained social relationships (Holley, 2007; Warner et al., 2017). In some cases, chronic illness may increase individuals’ social support networks and decrease their likelihood of being socially isolated because addressing health issues may increase social interactions in the form of medical or therapy appointments and other health-related activities (Finlay and Kobayashi, 2018).
Functional Impairment or Disability
Individuals with functional impairment or a disability—including physical, mental, intellectual, sensory, or other—face many unique challenges that leave them especially susceptible to being socially isolated or lonely (von Soest et al., 2020).
The degree to which individuals’ disability affects how they live their life, and the magnitude to which they are dependent on others for some or all of their needs, have both been found to be correlated with their likelihood of experiencing increased feelings of loneliness or vulnerability (Lykke and Handberg, 2019). Impacts on life satisfaction for those with disabilities or functional impairments have been shown to fluctuate depending on age, gender, residency (rural versus urban), and degree of extraversion (Hudson and Doogan, 2019; Puvill et al., 2019; Repke and Ipsen, 2020; von Soest et al., 2020). The existing social networks of people with functional impairment can impact whether people experience loneliness and to what extent. Unmarried individuals with functional limitations experience higher loneliness than happily married individuals with comparable limitations (Warner et al., 2019). Women with functional limitations have been found to experience greater loneliness if they have strained marital relationships while men may experience increased loneliness if they have overly supportive relationships, and people who lacked contact with friends all experienced greater loneliness (von Soest et al., 2020; Warner et al., 2019).
In general, individuals with greater mobility impairments or functional limitations tend to have fewer friends (Chatters et al., 2018; Ha et al., 2019). Additionally, certain life events (e.g., retirement, illness, death of loved ones or friends) can lead to a marked decrease in an individual’s social network; this decrease in friends and in friendships, especially among the oldest older adults, can lead to feelings of loneliness or to becoming isolated (Nicolaisen and Thorsen, 2017). In many cases it is not uncommon for individuals with functional limitations or disabilities to avoid openly expressing feeling of loneliness to others (Wormald et al., 2019).
Employment and Retirement
There is evidence that the relationship between loneliness and occupational function is bi-directional. Loneliness has been shown to be predictive of future work disabilities that occur when mental or physical impairments bring about functional limitations that make it impossible for an individual to perform the duties necessary to maintain paid employment (Morris, 2019). Being lonely can also result in depression, which can then lead to functional limitations and subsequent work disability. Along this pathway, depression can act as a partial mediator between loneliness and work disability.
Retirement can also affect an individual’s likelihood of being socially isolated or lonely. The number of post-retirement individuals in the United States is rising quickly, and retired individuals are living longer (Boyle, 2019; Pew Research Center, 2019a). Baby boomers (i.e., those born between 1946 and 1964) make up of 26 percent of the U.S. population, and their exit from the workforce (due to retirement) will dramatically change their lives (Boyle, 2019; Pew Research Center, 2019a). Each day between 2011 and 2030 an estimated
10,000 baby boomers will reach the age of 65, an age when many people are on the cusp of retiring or have already exited the workforce (Pew Research Center, 2019a). Ideally, most of these workers will decide when and under what conditions they will retire, but unplanned exits due to unexpected health problems (either an individual’s own health problems or those of a loved one) or employment changes (e.g., downsizing, redundancy, payouts for early retirement) are becoming more frequent (Boyle, 2019; Donaldson et al., 2010; Edge et al., 2017). Whether the decisions to retire is planned or unplanned and whether the retiree believes he or she has a choice in the decision can affect how smoothly the transition between being a paid employee and a retiree progresses (Donaldson et al., 2010; Quine et al., 2007).
Being employed can be protective against loneliness as it provides a convenient social environment for workers (Segel-Karpas et al., 2018). The disruption of these daily social interactions and structured routines upon retirement can lead to subsequent socialization difficulties (Morris, 2019). Workers who are lonely are at an increased risk of having difficulty transitioning to retirement and can experience a worsening of depressive symptoms because they often lack an established social network outside of the workplace (Gum et al., 2017; Segel-Karpas et al., 2018). Some retirees feel a loss of identity without their former job title and responsibilities, and some miss the challenges, demands, or appreciation they received at work (Schaap et al., 2018). For others, retiring can mean more time with family and friends and more enriching social interactions (Schaap et al., 2018). Thus, depending on the individual, retirement can favorably or unfavorably influence social connection and feelings of loneliness.
Factors related to a successful retirement include having good physical and mental health, financial stability, good social integration, the option of retiring by choice, and knowing how to enjoy leisure time (Barbosa et al., 2016; Donaldson et al., 2010; Schaap et al., 2018). In general, most retired people are less lonely than employed workers or people who are simply unemployed, and women typically have an easier time transitioning into retirement than men (Lauder et al., 2006; Perren et al., 2003). Roughly 26 percent of people who retire from their careers end up embarking on second careers, which can be similar to their previous jobs but more likely will involve some type of volunteerism (Boyle, 2019; Cook, 2015). These bridge jobs and volunteer positions help to ease the transition into retired living by allowing people to find new meaning in their post-career lives and can help retirees remain active, fulfilled, engaged, and connected within their communities (Boyle, 2019; Cook, 2015).
Religious and Spiritual Organizations
Many people feel that being part of a religious organization is central to their identity, and such affiliations can also be foundational to a person’s social networks. Challenges related to the previously described disruptive life events may
lead some older adults to seek supportive social connections through associations with religious organizations (Idler et al., 2003; Levin and Chatters, 1998; Rote et al., 2013). Active involvement in a religious organization can be a source of social support, and this affiliation may help ease an individual’s feelings of loneliness or social isolation and, some argue, even make people happier (Gonzales et al., 2015; Rizvi and Hossain, 2017; Rokach, 1996; Strawbridge et al., 2001). The intensity of one’s faith may also influence an individual’s feeling of loneliness, as individuals who hold stronger religious beliefs may feel less lonely than those who do not hold such strong beliefs (Lauder et al., 2006). Higher levels of social support and social integration have been associated with religious attendance and also with lower levels of loneliness (Rote et al., 2013). Older women are much more likely to be widowed than older men, and religious organizations may help to meet many of their social needs and help them cope with illness (Idler et al., 2017; Strawbridge et al., 2001). Additionally, several studies have found that women are more likely to be active members and experience greater overall benefits from participation in religious organizations, to have stronger social support and social networks, and to generally be less lonely than men (Gray, 2009; Idler et al., 2017; Kirkpatrick et al., 1999; Lauder et al., 2006; Strawbridge et al., 2001). One study did, however, find that men have stronger social networks—defined as the number of close friends and the frequency of interactions with those friends—than women (Gallicchio et al., 2007).
SOCIAL ENVIRONMENTAL FACTORS
The interactions between individuals and the environments in which they live, work, and play can profoundly influence their propensities for becoming socially isolated or lonely. This section reviews the relationships of several environmental factors, including transportation and housing situation, with social isolation and loneliness.
Transportation
In 2017 nearly 37 percent of the more than 225 million licensed drivers in the United States were 50 years of age or older (FHWA, 2017). Driving is important for adults who want to maintain independence and mobility; however, declines in physical health or cognitive function or deficits in reaction time or coordination can lead older adults to stop driving (Chihuri et al., 2016; Hwang and Hong, 2018; Johnson, 1999, 2008). Additional reasons for driving cessation include an increased insecurity in driving skills or ability; having had previous car accidents or traffic citations; the high cost of driving; being compelled to comply with requests by family members, friends, or a medical professional; or forfeiting driving privileges in compliance with state driving licensure laws (Johnson, 1999; Ratnapradipa et al., 2018). Driving cessation has been associated with a decrease
in social engagement and an increase in social isolation and feelings of loneliness (Barrett and Gumber, 2019; Chihuri et al., 2016; Edwards et al., 2009; Johnson, 1999, 2008). Driving cessation is especially difficult for older adults who live in areas that lack alternative transportation options, such as rural or lower-density neighborhoods (Finlay and Kobayashi, 2018; Herbert and Molinsky, 2019). Without reliable and affordable alternatives to driving, some former drivers may resume their driving despite their initial reasons for stopping (Johnson, 2008).
Impact of Housing or Geographic Location
Different living environments can shape older adults’ interactions with their social networks and with their community at large. Whether one’s home is a private residence, an apartment, or a room in a retirement community or nursing home, this space—and a person’s acceptance of this space—can affect that person’s physical, psychological, mental, and financial well-being as well as how attached he or she is to the community (Bekhet et al., 2009; Kemperman et al., 2019). A particular housing situation may represent a risk factor or protective factor for social isolation and loneliness, depending on the specific details and the characteristics of the individual.
Regardless of where or in what type of housing a person lives, the degree of social isolation or loneliness an individual experiences can be affected by whether he or she feels safe in his or her community. Prior direct or indirect exposure to community violence can lead to increased loneliness or a reduction in perceived social support from friends, thus increasing socially isolation (Tung et al., 2019). Even when older adults are motivated to be more socially engaged, living in a high-crime neighborhood can make people reluctant or afraid to leave their residence or engage with others (Portacolone et al., 2018). These concerns can be exacerbated by personal vulnerabilities (such as having chronic health issues or disabilities, limited social ties, or experiencing poverty), derelict or dangerous environmental conditions in the neighborhood, or a lack of opportunity or interest in engaging with other community members (Portacolone, 2018; Portacolone et al., 2018). Furthermore, the rapidly changing demographic trend continues to influence the need for additional, adequate, and appropriate housing for older adults (Herbert and Molinsky, 2019). Though the available research on issues related to housing type or location is sparse and can be somewhat inconsistent, it provides insight into possible links between a person’s living arrangement and social isolation or loneliness.
Aging in Place
In 2018 more than 32.9 million households were headed by adults aged 65 and older, and that number is projected to increase by 11.1 million households between 2018 and 2028 (JCHS, 2018; U.S. Census Bureau, 2018). Finding
affordable, accessible, and safe housing for older adults will become increasingly challenging (Wick, 2017). Many older adults are choosing to stay in their privately owned houses for personal, practical, and financial reasons, a situation known as aging in place (Benefield and Holtzclaw, 2014; Granbom et al., 2014; Herbert and Molinsky, 2019; Pearson et al., 2019; Wick, 2017). Years of shared history and memories become associated with one’s home, and leaving can be untenable for some (Granbom et al., 2014). In addition, the desire to remain independent and enmeshed in established social networks close to home can be a compelling reason to stay (Benefield and Holtzclaw, 2014; Herbert and Molinsky, 2019). It should be noted, however, that all housing choices, especially for those with disabilities or special needs, are constrained by financial and other limitations, and staying in one’s home is not always a tenable option. Often, accessible housing options are not readily available (Greiman and Ravesloot, 2015).
Aging in place may be both a risk and a protective factor for social isolation and loneliness. While a private home can provide comfort and security, it can also become a hazard if occupants are faced with changes in functional abilities (e.g., trouble walking or navigating stairs) (Herbert and Molinsky, 2019). Aging in place can be isolating if social networks or opportunities for affordable and convenient transportation are not readily available, especially for people who cannot afford sociable leisure activities outside the home (Finlay and Kobayashi, 2018; Herbert and Molinsky, 2019). Changes in physical health can often be accommodated with home modifications (e.g., adding accessible bathrooms or installing ramps) and with increased in-home support services, which provide needed assistance and connection with others, although the expense associated with these accommodations may, in many cases, be cost prohibitive and untenable without outside support (Herbert and Molinsky, 2019; Lane et al., 2019). Assistance from a nurse or supportive caregivers can help aging adults remain in their homes, and the companionship they provide can help alleviate the likelihood of loneliness or isolation for homebound patients (Benefield and Holtzclaw, 2014; Herbert and Molinsky, 2019; Szanton et al., 2019; Taylor et al., 2019). For successful aging in place to occur, a coordinated plan is needed that addresses issues related to health care, housing, financial concerns, social needs, and the use of resources, including technology (Benefield and Holtzclaw, 2014). Older adults who live alone without such support systems in place are more likely to report symptoms related to loneliness and depression (Herbert and Molinsky, 2019).
Co-Housing or Living Groups
A more recent approach to housing may provide some protection against social isolation and loneliness. Resistance to traditional long-term care options and reductions in government resources have led to the development of new and innovative housing options for older adults (Glass and Skinner, 2013; Glass and
Vander Plaats, 2013; Herbert and Molinsky, 2019). Older adults in the United States are increasingly choosing to live in supportive co-housing communities, which can increase these adults’ social connections (Glass and Vander Plaats, 2013; Graham et al., 2014; Lubik and Kosatsky, 2019; Wick, 2017). Resident-managed co-housing communities are often intergenerational and feature private units built around a common green space. Inclusion and participation are valued and encouraged as cohabitants share common meals and activities and help with day-to-day operational matters (Glass and Vander Plaats, 2013). Such living arrangements increase the likelihood of socialization opportunities, which can lead to an open exchange of information and ideas, emotional and mutual support, and shared communal coping, and can help alleviate social isolation and loneliness (Glass and Vander Plaats, 2013).
Federally Subsidized Housing and Senior Housing
Subsidized housing and senior housing are options for older adults who may not be able to afford alternative living arrangements. This lower-cost rental option aims to provide general support, assistance for people with disabilities, opportunities for social connections, and security (Taylor et al., 2018b). Compared with community-dwelling non-renters, older adults living in subsidized housing tend to live alone, have lower fixed incomes (averaging about $10,000 per year), have greater functional limitations or disabilities, have more psychiatric conditions, and have more chronic comorbid conditions (Gonyea et al., 2018; Henning-Smith et al., 2019; Parsons et al., 2011; Redfoot and Kochera, 2005; Taylor et al., 2018b). Although subsidized housing communities, senior housing, and retirement communities all offer similar socialization opportunities (e.g., interactions with peers, planned activities, and meeting spaces), studies suggest that loneliness is pervasive among residents living in subsidized and senior housing communities. An estimated 30–70 percent of residents in subsidized housing classify themselves as having high rates of loneliness, compared with only 19–29 percent among older adults living in homes or unsubsidized apartments (Gonyea et al., 2018; Taylor et al., 2018b). The combination of poor health and difficult financial circumstances may be at the root of the loneliness, but other situations that plague some subsidized housing communities (e.g., crime, alcohol and tobacco use, the use of abusive language) may also lead to social withdrawal (Finlay and Kobayashi, 2018; Gonyea et al., 2018; Kemperman et al., 2019). Subsidized housing residents may also experience depression or negative psychological outcomes stemming from the long-term effects of racial discrimination or living lives marked by disadvantage (Gonyea et al., 2018; Park et al., 2018). Other housing options for low-income or homeless individuals (e.g., permanent supportive housing for chronically homeless individuals) are an option for some older adults, but information regarding their impact on social isolation or loneliness is lacking (Henwood et al., 2019).
Retirement Communities
Many older adults transition from private homes to retirement communities, which offer amenities such as social activities, health-related supervision, and 24-hour supervision (Bekhet et al., 2009). The ease and success of an individual’s move into such a community has much to do with the person’s motivation for moving. For example, such things as the failing health of an individual or the individual’s spouse or partner, a need to minimize responsibility, or social isolation and loneliness all can encourage older adults to relocate to a retirement community (Stimson and McCrea, 2004). Alternatively, older adults may move to be with friends, relocate to a specific locale or community, live closer or have more access to medical facilities, feel safer, or live more affordably (Bekhet et al., 2009; Crisp et al., 2013; Stimson and McCrea, 2004). Voluntary moves, when individuals feel they have options and can make their own decisions and maintain autonomy, are more likely to have a positive outcome than non-voluntary moves (Bekhet et al., 2009). Increasingly, retirement communities offer options that allow residents to transition from independent living arrangements to assisted living if needed (Jeste et al., 2019). Yet, these moves are limited to those older adults who have the financial resources to “buy in” to such communities.
Long-Term Care Service Options: Residential Care and Nursing Homes
Locations that offer long-term care services such as adult day care, nursing homes, and residential care provide older adults with a range of health care, personal care, and supportive services. In 2016 long-term care service providers served more than 8.3 million people in the United States, including 1,347,600 in nursing homes and 811,500 in residential care facilities (Harris-Kojetin et al., 2019).
Long-term care providers offer older adults aid with physical functioning and general quality-of-life tasks by providing a wide range of services such as assistance with daily activities, medication management, and health maintenance tasks (Harris-Kojetin et al., 2019; Rijnaard et al., 2016). Many of these organizations aim to provide home-like accommodations by focusing on psychological and social factors (e.g., autonomy and relationships with family, friends, and pets) and the built environment (e.g., comfortable private spaces, helpful technology, personal belongings) (Rijnaard et al., 2016). In some cases, providing person-centered care that includes fulfilling personal preferences related to care and recreation may be helpful in alleviating loneliness in long-term care residents (Andrew and Meeks, 2018). Nevertheless, long-term care can increase social isolation and loneliness for older adults living in such residencies, a portion of whom may be living far from friends and loved ones. Long-term care residents often may not be able to engage in meaningful social interactions and, in some cases, may share a room with people with whom they are not compatible (Trybusin´ ska and Saracen, 2019).
Rural Versus Urban Environments
Compared with adults who live in urban settings, adults who live in rural environments are more apt to face challenges related to the long distances between homes and businesses or medical facilities, limited public transportation options, unreliable or non-existent access to broadband Internet, and access to fewer health care providers (Douthit et al., 2015; Henning-Smith et al., 2019). Research on the relationship of social isolation and loneliness with living in rural versus urban areas has had mixed results. Henning-Smith and colleagues (2019) found that individuals who lived in areas with fewer than 10,000 people reported having more family members they could count on and more friends than urban dwellers, but these same rural residents also said they felt more left out. Individuals who lived in mid-size population areas (up to 49,999 residents) reported less loneliness overall than people who lived in urban environments, but they were more likely to report not having any friends. On the other hand, Mullen and colleagues (2019) failed to find a significant difference in perceived loneliness between rural and urban primary care patients. Finlay and Kobayashi (2018) found that people who lived closer to a city center reported more social interactions than individuals who lived in the suburbs. City dwellers credited those social interactions to daily connections with others in their residential spaces, relationships with building staff or caretakers, and the existence of numerous places for socialization (e.g., parks, stores, movies, libraries, coffee shops) that provided avenues for impromptu social interactions. Generally, study participants in the outer suburbs reported greater loneliness than those closer to the city center, with loneliness decreasing with moves into the inner suburbs and closer to the city center. Many of the inner suburbs lacked communal places in which to gather, and people who lived in the outer suburbs reported that isolation from neighbors and the long distances to opportunities for socialization increased their social isolation and loneliness, although these results were not consistent among study participants.
AT-RISK POPULATIONS
Determining how the lives of older adults aged 50 and over may be affected by social isolation and loneliness is central to the committee’s charge; however, the scope of the committee’s work also extends to the particular impacts for at-risk (i.e., vulnerable) populations. While it is difficult to specifically define all of the subpopulations or groups of people who would be included as at risk, the committee endeavored to include information pertaining to any special populations for which there is relevant social isolation or loneliness research. Some of these populations include people who were studied on the basis of their racial or ethnic background, sex (i.e., male or female), age, socioeconomic status, health status, or place of residence (e.g., rural, urban). Research pertaining to these populations is included throughout the report. While a fair number of international studies look
at the status of at-risk populations in other countries (e.g., Steptoe et al., 2013; Zebhauser et al., 2014), studies focusing on at-risk subpopulations in the United States are sparse. Two populations in the United States that have been researched more extensively than others are immigrants and individuals who identify as part of the gay, lesbian, bisexual, and transgender community. Research pertaining to these two groups is described below.
Immigrants
Evidence suggests that immigrants are more likely to experience social isolation and possibly loneliness than non-immigrants. For example, Latino immigrants have fewer social ties and lower levels of social integration than U.S.-born Latinos (Ramos et al., 2015; Shelton et al., 2011; Steele et al., 2018; Viruell-Fuentes et al., 2013). On the other hand, one study found no difference in loneliness between more and less acculturated Latinos (Gallo et al., 2012). A study of older, highly acculturated Korean immigrants found lower levels of depression in people who had stronger social support networks (Kim et al., 2012).
In general, immigrants experience many stressors that can increase their social isolation, including language and communication barriers; differences in community, family, or intergenerational dynamics; and new relationships that lack depth or history. This social isolation can be especially acute in first-generation older immigrants (Barrington et al., 2012; Curtin et al., 2017; Gerst-Emerson et al., 2014; Miyawaki, 2015). Immigrants also experience physical, cognitive, and mental health consequences associated with increased loneliness, and this can be especially true for women or people who are unmarried or lack a close confidant (Dong and Chen, 2017; Gerst-Emerson et al., 2014). A study in England found that immigrants, including those from Africa, Bangladesh, the Caribbean, China, and Pakistan, had much higher rates of social isolation and loneliness than their nonimmigrant peers, although Indian immigrants were an exception to this finding (Victor et al., 2012). In a Dutch study of immigrants, Moroccan, Surinamese, and Turkish immigrants reported feeling less healthy and more discriminated against than did Dutch natives, and these factors were related to increased loneliness (Visser and El Fakiri, 2016).
Gay, Lesbian, and Bisexual Populations
A small number of studies have found that an individual’s sexual orientation can affect his or her feelings of loneliness or social isolation, but the findings are inconsistent. In general, studies have found that gay, lesbian, and bisexual individuals tend to experience more loneliness than their heterosexual peers. For example, in the Swedish National Public Health Survey of more than 79,000 individuals 18–84 years of age, the 1,673 who identified as lesbian, gay, or bisexual reported higher levels of social isolation than did those who identified as heterosexual, and social isolation was associated with increased measures of substance
use and psychological distress in these populations (Bränström and Pachankis, 2018). On the other hand, a small study in the Netherlands by Bos et al. (2015) failed to find a similar result in a comparison of primarily middle-aged same-sex and heterosexual couples (median age = 43), and a study by Beam and Collins (2019) did not find that loneliness varied between sexual minority and heterosexual men and women across multiple age ranges.
Several studies have looked at the factors that contribute to loneliness and social isolation among gay, lesbian, and bisexual populations. Jackson et al. (2019) analyzed perceived discrimination and health and well-being in 304 middle-aged and older lesbian, gay, and bisexual individuals (aged 41–85) who participated in surveys in 2010–2011 and 2016–2017. The prospective analysis found that perceptions of discrimination based on sexual orientation increased loneliness. In a study of 912 gay Latino men recruited in bars (primarily aged 20–40 years), experiences of homophobia, racism, financial hardship, and low resiliency all predicted loneliness (Diaz et al., 2001). In a large, nationally representative study of adults in the United States 18 years of age or older, Hatzenbuehler et al. (2011) found that lesbian, gay, and bisexual individuals who were lonely reported higher levels of mood and anxiety disorders than did those who were not lonely. However, the correlation between social isolation and mood disorders differed between those who lived in states with high concentrations of same-sex couples and those who did not. Furthermore, a small study of older lesbian, gay, and bisexual individuals in the Netherlands found that those who had experienced negative social reactions or expected those reactions relative to their sexual preference had the highest levels of loneliness (Kuyper and Fokkema, 2010).
FINDINGS AND CONCLUSIONS
Physical Health Factors
- Physical health risk factors for social isolation and loneliness include many common chronic diseases and conditions, including heart disease, stroke, and cancer.
- The relationships between physical health risk factors and social isolation and loneliness are often bi-directional.
- Functional status (measured by factors such as gait speed or difficulties in the activities of daily living) is bi-directionally associated with social isolation and loneliness.
- Strong evidence links sensory impairment to communication difficulty and, further, to reduced social participation, social isolation, and higher rates of loneliness.
- Hearing loss contributes to both social isolation and loneliness, and remediation of hearing loss has been found to reduce loneliness and improve social functioning.
Psychological, Psychiatric, and Cognitive Factors
- Psychiatric disorders, such as major depression, generalized anxiety disorder, and social anxiety disorder, have been shown to increase the risk of developing loneliness.
- Social isolation and loneliness are more common in older adults with depressive and anxiety disorders than in their non-depressed and non-anxious peers.
- The relationship between depression and loneliness is bi-directional, and these constructs are closely associated. Yet, depression and loneliness are not the same.
- The impairments related to dementia predispose an individual to feelings of loneliness, and caregivers are also at risk for loneliness.
Social, Cultural, and Environmental Factors
- Supportive relationships—especially those with family, friends, and caregivers—can decrease self-reported loneliness, while difficult or unfulfilling relationships can increase feelings of loneliness.
- Losing a spouse is a frequent disruptive event for older adults, particularly for women. Loneliness is a primary symptom of bereavement.
- Research on the benefits of human–animal interactions is mixed.
- Retirement can affect an individual’s likelihood of being socially isolated or lonely.
- Social environmental factors such as driving status, housing status, or location can affect the levels of social isolation and loneliness.
- At younger ages men and women experience similar rates of social isolation and loneliness, but women may be at higher risk as they get older.
- Literature focusing on social isolation and loneliness in at-risk subgroups is sparse.
- Gay, lesbian, and bisexual individuals tend to experience more loneliness than their heterosexual peers.
- Immigrants appear more likely to experience social isolation and loneliness than non-immigrants.
This page intentionally left blank.




























